Behavioral Healthcare Services Utilization between Health Savings Account Members and
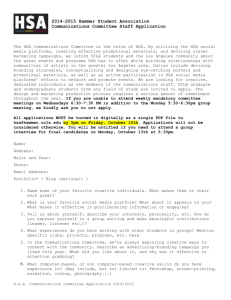
advertisement

Behavioral Healthcare Services Utilization between Health Savings Account Members and Traditional Health Plan Members Nancy A. Hardie*, Anthony Lo Sasso** and Regina A. Levin* * United Healthcare, Minneapolis, MN ** University of Illinois at Chicago, Chicago, Ill Objective To estimate the effects of switching from traditional health plans to health savings accounts (HSAs) on: • Initiation of behavioral health treatment • Intensity of behavioral health outpatient treatment once initiated 2 Study Design • Quasi-Experimental (difference-in-differences) • Retrospective • Pre - Post Study (pre/post offer of HSA) • Cohorts 1. Traditional plan take-up (“Stayers”) 2. HSA plan take-up (“Switchers”) 3 Study Design Cohorts 2005 Pre HSA Offer Stayers 2006 Post HSA Offer 2007 Post HSA Offer Traditional Plans Traditional Plans HSAs HSAs Traditional Plans Only Switchers All Cohort Members: 36 Months Continuous Enrollment 4 Data Source • All data were extracted from the data repository of UnitedHealthcare, which provides a full complement of traditional plan designs in addition to being the leading provider of consumer driven healthcare plans in the country. • The data contain linkable datasets of member, employer, medical and pharmacy claims information. • Data have been aggregated to the person-year level. 5 Employer Criteria • Employed between 2 and 4,999 persons • Offered medical and pharmacy coverage • 2005: offered only traditional plans (Pre-year) • 2006 & 2007: offered an option to choose • CDHP with HSA or • Traditional health plan • Coverage started on January 1st in all study years (2005, 2006 and 2007) This resulted in 251 employers 6 Member Criteria • Members and subscribers age < 65 on last day of study • No coordination of benefits • 36 months of continuous membership in commercial insurance plan • Remained in traditional plans in 2006 and or2007 (Post-years) or switched to an HSA in 2006 and remained in HSA in 2007 This resulted in 60,294 members 7 Study Design Cohorts 2005 Pre HSA Offer 2006 Post HSA Offer Traditional Plans N =50,316 Stayers 2007 Post HSA Offer Traditional Plans N =50,316 Traditional Plans Only N=60,294 Switchers All Cohort Members: (251 Employers) HSAs N=9,978 HSAs N=9,978 36 Months Continuous Enrollment 8 Methods • Employer and member selection • Data Extraction • Data Verification • Descriptive data summaries • Multivariate analyses 9 Methods Dependent variables: • Behavioral health treatment (0/1) in each year [Logistic regression] • First primary ICD9 codes (290-314) per year • Log of outpatient treatment visits in each years conditional on initiation [OLS regression] • Primary ICD9 codes (290-314) 10 Methods Independent variables: • • • • • • • • • Post year variables (2006 & 2007) Cohort Post year variables & cohort interaction terms Health risk score (Symmetry ETG Grouper) Age (2005) Gender Region (2005) Employer size (2005) Seven psychiatric disorder indicators (for intensity regression) • • • • • • Anxiety disorders, Major depression, Schizophrenia and bipolar disorders, Alcohol and substance abuse disorders, Conduct disorders, personality disorders and Other behavioral disorders 11 Dependent Variables Percent (%) Initiating Behavioral Health Treatment per Year 12.0% 10.0% 9.7% 9.5% 8.4% 7.5% 8.0% 7.4% 7.5% 6.0% 4.0% 2.0% 0.0% Stayers N=50,316 Switchers N=9,978 2005 2006 2007 12 Dependent Variables Behavioral Health Intensity (Among Members Who Received Outpatient Treatment) Mean Outpatient Visits PMPY 2005 2006 2007 2005 2006 2007 Mean 6.52 6.62 6.34 6.07 6.18 5.76 SD 9.53 9.36 9.17 8.45 8.89 8.14 4,202 4,872 4,751 744 739 747 N Stayers Switchers 13 Independent Variables Pre-Offer of HSA: 2005 Variables Mean (SD) Retrospective Risk Score Stayers Switchers 1.09 (1.7) 0.93 (1.6) 32.7 (17.6) 32.0 (17.5) % Female 50.7% 49.3% % Northeast (reference) 10.9% 6.6% % South 47.8% 43.2% % Midwest 29.1% 41.4% % West 12.2% 8.8% % Large Firm (vs. small) 93.6% 65.6% N 50,316 9,978 Mean (SD) Age 14 Initiation of Behavioral Health Treatment Logistic Regression Coeff SE OR Post Year 2006 * Switcher -0.043 0.015 0.96 0.0037 Post Year 2007 * Switcher -0.032 0.015 0.97 0.0306 Post Year 2006 0.022 0.015 1.02 0.1343 Post Year 2007 0.018 0.015 1.02 0.2272 -0.132 0.016 0.88 <.0001 Switcher (Stayer reference) P-value N = 60,291 members Model also controls for age, gender, risk score, region, large/small firm 15 Intensity of Behavioral Health Treatment (Log of Days in Outpatient Treatment) OLS Regression Variable β Post Year 2006 * Switcher -0.018 0.056 0.750 Post Year 2007 * Switcher -0.039 0.056 0.480 Post Year 2006 0.006 0.021 0.761 Post Year 2007 -0.041 0.021 0.049 0.017 0.040 0.673 Switcher (Stayer reference) SE β Probability-value N = 16,053 members Model also controls for age, gender, risk score, region, large/small firm, and indicators for type of behavioral health disorder. 16 Conclusions • Our results indicate that there is a relative decline in behavioral treatment initiation associated with enrollment in an HSA, though this was driven by an increase in initiation among stayers not a decline in use among switchers. • Conditional on behavioral health treatment, we did not observe a significant difference in outpatient visit intensity between HSA and traditional plan enrollees. • Importantly, our results are not sensitive to the inclusion/exclusion of explanatory variables such as the Ingenix retrospective risk score, supporting our quasiexperimental design 17 Implications for Policy Delivery or Practice • Our findings support the notion - dating back to the RAND Health Insurance Experiment - that greater demand side cost sharing affects initiation into treatment, but has more modest effects on intensity of treatment • The logic of this is that consumers have more discretion over the decision to initiate treatment while providers have more discretion over the intensity of treatment • For a serious chronic condition like a behavioral health disorder, our results are a mixed message • While treatment initiation does not decline in absolute terms, it falls modestly in relative terms • However, conditional on any use, we find little differences in outpatient mental health treatment use compared to traditional plan enrollees • Future work will explore the type of care mental health received (outpatient vs. pharmacy), costs, and quality 18 Collaborators • Mona Shah, Health Services Research Manager • Grace Shen, SAS Programmer 19 Psychiatric Disorders (in OLS Regression) 7 Percent 6 5 4 3 2 1 0 2005 2006 2007 Stayers 2005 2006 2007 Switchers Anxiety Disorders Major Depression Schizophrenia & Bipolar Disorders Alcohol and Substance Abuse Disorders Conduct Disorders Personality Disorders Other Behavioral Disorders 20