Healthcare System Improvement Through HIT: Case Study at VNSNY
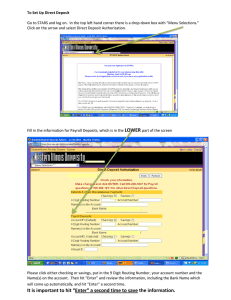
advertisement
Healthcare System Improvement Through HIT: Case Study at VNSNY Carol Raphael, President and CEO Visiting Nurse Service of New York June 24, 2006 Overview • Drivers of HIT Investment • HIT Solutions • Lessons Learned Drivers of HIT Investments 1. Highly decentralized service system – Large scale / scope of services – Dispersed multi-disciplinary field staff – Communication often not “face to face” 2. Shifts in Payment & Regulatory Requirements • In 2000, Medicare moved to PPS – Tied to OASIS assessment • Increased managed care admissions & reporting 3. External Measures of Quality • Required to submit OASIS scores on functional improvements & adverse events • CMS Æ Public Disclosures – “Home Care Compare” – Benchmark Æ National averages • Movement to Pay for Performance 4. Labor Market Pressures • How to increase capacity of current staff? • What tools do staff need to facilitate their jobs? • How does an organization continually educate staff? HIT Solutions & Systems at VNSNY 1. Electronic Health Records • Mobile Pen Tablets Components: – – – – – – – Assessments Progress notes Plan of Care Monitoring of outcomes Problem lists Medication management Standardized best-practice “decision tree” VNSNY Mobile Pen Tablets 2. Quality Measurement System • Measures in 4 domains collected for clinical teams quarterly. – Process, outcomes, cost/utilization, satisfaction • Targets set annually in different areas – “Improvement” & “Priority” indicators • Easy access by front-line staff – Measures how team is doing compared to other teams & targets – Outcomes website Reduction in Emergent Care of Wound Patients: 2001-YTD 2005 36 26% Reduction 35 34 33 32 31 30 29 28 27 26 2001 2002 2003 2004 Y TD 2 0 0 5 3. Tele-monitoring • Speech Tele-health – Target people w/ strokes & Parkinson’s – 206% improvement in staff productivity – 98% patient satisfaction Tele-health Pilot • 284 patients • Equipment guides patients to collect vital signs in 8 languages • Data transmitted to central RN station Æ info triaged 4. e-Exchange Partnerships • MD Web-Based Portal – Shares patient medical information – Improves communication between nursing staff & MDs – Stakeholder Benefits: • Promotes self-care management • Increases efficiency, communication, patient outcomes, & MD satisfaction • NY Community Home Health Interoperability Project – Goal Æ Electronic exchange of patient’s clinical information • VNSNY key lead with – 4 MD Practices – 2 Community Health Centers – 3 Labs, SNF, & Adult Day Center • Participant in 4 Regional Health Information Organizations 5. E-Learning • Goals • • Improve field staff access to best practices Reduce training time & costs • Piloting Diabetes Self-Management Module • • • Planned roll-out to 1,700 RNs 53% of RNs think “learning is easier” 75% of RNs believe course strengthened ability to teach patients about self-care management “Lessons Learned” 1. The way technology & info is used produces advantages – Before adapting technology, tackle core processes that cross silos: • Job design • Incentives 2. Implementation takes considerable resources & support 3. Difficult to project & achieve ROI 4. Clear governance structure needed to facilitate decision making & establish accountability VNSNY I.S. Steering Committee key functions: • Develops priorities tied to strategies • Determines allocation of I.T. expenditures • Monitors projects, timelines, costs, & budget • Quarterly status presented to Board Technology Committee 5. Strong project management systems vital to success • Provide early warnings • Measure total-multi-year costs, resource utilization, deliverables • VNSNY Model Æ Moved to 2 phases – Phase I: Early estimates, strategic rationale, cost/benefit analysis – Phase II: More precise, detailed plan VNSNY Quality Capacity Efficiency Picture: Southwest Missouri State University, Hammons Field opening: April 2004 Conclusions & Reactions 1. Investment in IT solutions can enable deliverables in three key areas: – Improving quality – Gaining efficiencies – Enhancing capacity 2. Technology can enable virtual systems & interconnectivity with other parts of health care – Relies on the building of partnerships & flexibility 3. Technology needs to be part of a long term, broader strategy both within the organization & in public policy arena • Technology as a vehicle to promote independent living – Key factors: • Ease of use • Affordable • Shift from a provider-driven orientation • Privacy issues are paramount • Support of research