Pain Management Program in a Skilled Nursing Facility Nancy Flinn, PhD OTR/L
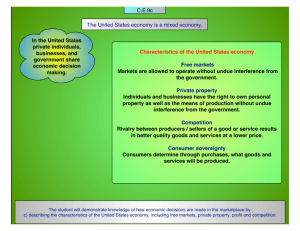
advertisement

Pain Management Program in a Skilled Nursing Facility Nancy Flinn, PhD OTR/L Tom Kelley MA 1 Courage Center • A community–based resource and rehabilitation facility • 81 years old, provides • Direct traditional rehabilitation services (OT/PT/SP/Psych) • Advocacy (grass-roots organizing, lobbyists representing issues for persons with disabilities, works with Minnesota Consortium for Citizens with Disabilities) • Community based services (Drivers Assessment and Treatment, Vocational Services, Independent Living Skills Program, Community Reintegration Program, Sports and Recreation, Camp) 2 Courage Center Transitional Rehabilitation Program • 46 bed unit, licensed as a skilled nursing facility • Holistic, individualized, goal-focused program to increase independence, address adjustment to new life changes, and discharge to more independent setting. • Average length of stay is 2.9 months. • 93% of clients discharged to community setting during this project • Project ran from October of 2007 to January 2010 3 Minnesota Department of Human Services Pay for Performance Grant • Project focused on measuring and addressing pain in our inpatient program • Our MDS Pain ratings were higher than other SNFs • Our objectives: • Measure pain in a systematic way • Measure interference of pain with activity • Decrease pain • Decrease interference of pain with activity. 4 Admitting Diagnosis Other 10% SCI 28% Brain Injury 20% Stroke 42% 5 So, based on the literature for our diagnosis: • We expected pain rates for individuals with SCI between 48% and 79%. • We expected pain rates for individuals with brain injury to be in the 52% to 73%. • We did not know what to expect about pain interference with activity. • We needed a better way to measure and manage pain. 6 Pain at Courage Center • Our pain ratings on the MDS were high • This was a concern for Courage Center and Minnesota Department of Human Services • We received a Pay for Performance Grant through Minnesota Department of Human Services to cover this project (5% increase in our Medicaid rate) • Project team included the Director and Director of Nursing of the Transitional Rehabilitation Program, Director of Outcomes and Research, and Data Analyst. 7 Choosing a measurement tool The Modified Brief Pain Inventory was developed for use with individuals with SCI • 4 questions regarding severity of pain • 2 questions about relief of pain • 10 questions about the degree to which pain interferes with activity 8 The MBPI has been modified for use with individuals with disabilities • “Walking” changed to “Ability to Get Around” • Some additional activities added to “Pain Interference” scale • Self Care • Recreational activities • Social activities 9 Implementing the measurement tool • The MBPI was completed with each client monthly while they were in the Transitional Rehabilitation Program • The data was analyzed once a month and the grant team met to review the data • Reviewed charts for groups of clients, or tried to make meaning of the data. 10 Data collected on our clients • There were 431 clients admitted during this period • 379 (88%) had at least 1 data point • Missing data • Not able to answer the questions, either because of language or cognitive difficulties • Incomplete data for other reasons (very early discharge, rehospitalization) • 341 (79%) had more than 1 data point 11 Pain Severity Maximum Score = 40 Minimum Score = 0 Clients 12 Pain severity scores • 48% admitted with no pain, at the lower range of the data in the literature • Some clients were admitted with no pain, but discharged with pain • Some clients were admitted with pain, had increased pain during stay. 13 Pain severity and pain interference scores Patients Reporting Pain at Admission: % Reporting Decreased Pain Rating & Interference by Quarter of Discharge 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 70% 58% 76% 64% 63% 54% Q123 n=59 Q456 n=80 Pain Rating Decreases at Discharge Q789 n=51 Pain Interference Decreases at Discharge 14 Changes in pain severity and pain interference effect sizes Effect Sizes of Decreases in Pain and Pain Interference 1 0.8 0.6 0.4 0.38 0.23 0.2 0 0.44 0.06 Q123 PAIN RATING 0.30 0.33 Q456 Q789 PAIN INTERFERENCE 15 Pain Severity Maximum Score = 40 Minimum Score = 0 Clients 16 Some clients came in with no pain, discharged with pain. • These clients were often were admitted on narcotic pain medications • Some clients had increased pain with increased activity in rehabilitation 17 Pain Severity Maximum Score = 40 Minimum Score = 0 Clients 18 Came in with some pain, got better or got worse • About 1/3 of those whose pain increased during our stay had chronic pain issues prior to the injury that brought them to us. • Again, some of these clients were on strong pain medication at admission • Some clients with SCI developed neuropathic pain during their stay 19 Neuropathic pain • A type of chronic pain resulting from changes in the central or peripheral nervous system • It occurs in individuals with spinal cord injury • For individuals with SCI, time of onset is “weeks to months” post injury. 20 Case Study Group 2 • Mike 56 year old, Spinal cord injury and history cardiovascular problems. • Admit pain range 3 least, 10 worst and average 5 • Increased to 8 and interference with all activities • Discharged with no pain and no interference 21 Pain Severity Maximum Score = 40 Minimum Score = 0 Clients 22 Case Study Group 3 • Julie 35 year old spinal cord injury • Admit pain 0 least, 3 average, 10 worst with minimal interference • Mid-way pain 2 least, 4 average, 9 worst with interference in all areas • Discharge pain 3 least, 6 average, 8 worst with interference in sleep and enjoyment of life 23 Six Month Follow-up 67% of Discharges Incidence of Joint and Muscle Pain 6 Months after Discharge 40 35 Percentage of Clients 35 30 25 26 28 30 31 22 Clients Discharged in 2008 22 20 Clients Discharged in 2009 15 10 6 5 0 Not a Problem Mild Problem Moderate Problem Significant Problem 24 Interventions: Medication management • Manage medications •Reduce/eliminate dependency on narcotics •Add as appropriate: antidepressants, anti-inflammatory, anti-epileptics, muscle relaxants, sleeping medications, anti-anxiety agents, and nonnarcotic analgesics • Injections: phenol, botox, joint and localized injections, etc. • Incorporate pain scores into rehabilitation rounds, address pain in therapy 25 Interventions • Incorporate mind-body techniques into therapy and nursing care • Yoga • Biofeedback • Relaxation/imagery • Breath work • Spiritual approaches • Acupuncture • Massage • Self-hypnosis 26 Interventions • Sleep hygiene and control • Nutrition and dietary measure • Focus on activities of daily living • Education • Being with others with similar problems and strengths • Individual counseling and adjustment • Making and taking steps to solve problems 27 Interventions • Planning for meaningful life activities • Vocational/avocational planning: return to work • Recreational activities • Distraction • Family involvement and counseling • Stress management • Addressing other psychosocial concerns 28 Effects of those interventions • The effects of these interventions have increased the number of clients discharged with decreased pain significantly. • However, we still have slightly more than 24% of our clients who are discharged with pain 29 Pain Management • For many of our clients, pain is likely to be a lifelong problem • Teaching clients how to deal with it requires an intensive model 30 Adjustment • Our clients also struggle with adjustment issues – Clients are discharged to the community early after injury – In 2001, the average length of stay at Courage Center was almost a year, often following several months of inpatient rehabilitation – Now clients are discharged from the TRP to the community before they would have left 31 inpatient rehab 10 years ago Adjustment • The clinical question that has come up in our discussions is “to what degree is the pain we observe in our clients really a reaction to disability?” • We have started a Coping with Disability Program, modeled after the Pain Program • These two programs may end up interweaving or merging, as we move forward 32 What’s next? • Continue to measure pain regularly • Continue to educate staff, clients, and families about pain issues • Refine the Coping with Disability Program • Examine outcomes, continue to redesign the management program 33