Effect of Surrounding Tissue on Vessel Fluid and Solid Mechanics Wei Zhang
advertisement

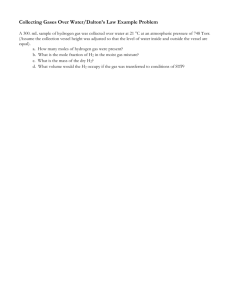
Effect of Surrounding Tissue on Vessel Fluid and Solid Mechanics Wei Zhang Carly Herrera Satya N. Atluri Ghassan S. Kassab Department of Mechanical and Aerospace Engineering and Department of Biomedical Engineering, University of California, 204 Rockwell Engineering Center, Irvine, CA, 92657, USA There is no doubt that atherosclerosis is one of the most important health problems in the Western Societies. It is well accepted that atherosclerosis is associated with abnormal stress and strain conditions. A compelling observation is that the epicardial arteries develop atherosclerosis while the intramural arteries do not. Atherosclerotic changes involving the epicardial portion of the coronary artery stop where the artery penetrates the myocardium. The objective of the present study is to understand the fluid and solid mechanical differences between the two types of vessels. A finite element analysis was employed to investigate the effect of external tissue contraction on the characteristics of pulsatile blood flow and the vessel wall stress distribution. The sequential coupling of fluid-solid interaction (FSI) revealed that the changes of flow velocity and wall shear stress, in response to cyclical external loading, appear less important than the circumferential stress and strain reduction in the vessel wall under the proposed boundary conditions. These results have important implications since high stresses and strains can induce growth, remodeling, and atherosclerosis; and hence we speculate that a reduction of stress and strain may be atheroprotective. The importance of FSI in deformable vessels with pulsatile flow is discussed and the fluid and solid mechanics differences between epicardial and intramural vessels are highlighted. 关DOI: 10.1115/1.1824128兴 Keywords: Blood Flow, Vessel Stress, Strain, Muscle Contraction, Fluid-Structure Interaction I Introduction There is no doubt that cardiovascular disease is one of the most serious health problems in America. Approximately 60% of all human deaths are caused by diseases of the cardiovascular system. It is well accepted that fluid and solid mechanics of the blood vessel are important determinants of the health and disease of the cardiovascular system 共see review in Ref. 关1兴兲. Atherosclerosis, a major disease of the cardiovascular system, is associated with abnormal stress and strain 关2,3兴. The coronary arteries that perfuse the heart muscle are particularly susceptible to atherosclerosis 关4兴. The coronary arteries may be classified into two types: those that remain on the surface of the heart 共epicardial arteries兲 and those that penetrate into the heart muscle 共intramural arteries兲 关5兴. An interesting observation is that the epicardial arteries develop atherosclerosis while the intramural arteries do not 关6兴. Atherosclerotic changes involving the epicardial portion of the coronary artery stop where the artery enters the myocardium. The cyclically contracting heart compresses the intramural arteries during the cardiac cycle. The compression is greatest during systole and smallest during diastole. The external compression of the intramural arteries may affect both the fluid mechanics of the blood flow in the vessel lumen and the solid mechanics of the vessel wall. An additional example of vessels that are devoid of atherosclerosis due to the mechanical influence of the surrounding tissue is the vertebral artery. Angiograms of the vessel reveal an alternating pattern of disease where the portion surrounded by bone is disease free, while the intervertebral segments are prone to atherosclerosis 关7兴. Numerous studies have shown that the effects of wall shear stress, intramural wall stress, and strain on atherosclerosis may be mediated by the endothelium and smooth muscle cells 共see review in Ref. 关1兴兲. The goal of the present study is to determine the stress and strain of those vessels that are less susceptible to athCorresponding author; electronic address: gkassab@uci.edu Contributed by the Bioengineering Division for publication in the JOURNAL OF BIOMECHANICAL ENGINEERING. Manuscript received by the Bioengineering Division January 7, 2004; revision received June 15, 2004. Associate Editor: Fumihiko Kajiya 760 Õ Vol. 126, DECEMBER 2004 erosclerosis. Our hypothesis is that the surrounding tissue of a blood vessel can influence the biomechanics of the vessel, and hence affect atherogenesis. Our rationale is to simulate the fluidsolid interaction 共FSI兲, to determine the flow and stress fields in the vessel lumen and wall, respectively, for vessels with and without the influence of surrounding tissue. On the fluid mechanics side, the external compression may have a ‘‘wash out’’ effect on the blood flow; i.e., reduce the transit time of blood flow and hence reduce the transport time of low-density lipoprotein across the vessel wall. On the solid mechanics side, the vessel wall stress may be decreased because the surrounding tissue bears some of the stress and strain. 2 Methods 2.1 Finite Element Model. The ANSYS Multiphysics finite element software has recently integrated both the fluid dynamics and structural analysis codes into one package 关8兴. This considerably reduces the effort in developing interfaces between different commercial codes. In the present study, we took advantage of this feature. The two-dimensional fluid element FLUID141 and solid element PLANE182 were used in an axisymmetric model, where a 3 cm long segment of an artery was considered, assuming a circular cross sectional area 共CSA兲 and a straight centerline 关as shown in Fig. 1共a兲.兴 We further assumed that the CSA did not change along the axial direction and the vessel wall thickness was uniform. Finally, the vessel wall was considered smooth and impermeable. The blood and vessel regions consisted of 5000 and 1500 quadrilateral linear elements, respectively. Figure 1共b兲 shows a portion of the discretized finite element model near the inlet. To maintain a good mesh quality in the fluid domain, and to allow for the fluid mesh following the FSI boundary, the Arbitrary Lagrangian-Eulerian formulation was employed, to update the fluid mesh automatically during the computation. The sequential weak-coupling algorithm 关8兴 was inherently employed, to take into account the interactions between fluid and solid domains. The conservative formulation for load transfer was selected to allow forces to transfer from fluid to solid; and displacements and velocities to transfer from solid to fluid across the FSI interface. Copyright © 2004 by ASME Transactions of the ASME Ē i ⫽ 2 共 ¯ i2 ⫺1 兲 共 i⫽r,z, 兲 1 (4) The normalized stretch ratios are defined as the corresponding principal stretch ratios ( r , z , ), divided by the cubic root of the third invariant (J⫽ r z ) of the deformation gradient ¯ r ⫽ r J ⫺1/3, ¯ z ⫽ z J ⫺1/3, ¯ ⫽ J ⫺1/3 (5) The Cauchy stress tensor and the Hencky 共logarithmic兲 strain tensor are the proper measures of true stress and strain for large deformations 关12兴. ANSYS uses these mechanical measures and also provides them in the user subroutine USERMAT through which we implemented Fung’s pseudo-elastic strain energy function as described in the Appendix. The Cauchy stress-tensor is conjugate to the Hencky strain-tensor for isotropic materials 关12兴. For anisotropic materials, however, the stress-strain relation should be properly established between the second Piola-Kirchhoff 共P-K兲 stress and the Green’s-Lagrange strain 关12兴. The second P-K stresses are given by the derivatives of strain energy function. The principal logarithmic strains are defined as i ⫽ln i 共 i⫽r,z, 兲 (6) The Cauchy stresses, with the incompressibility of blood vessels being taken into account by the method of a Lagrangian multiplier, can be expressed by i j⫽ Fig. 1 „a… Schematic of the axisymmetric model „not to scale…. „b… Finite element mesh near the inlet. 2.2 Incompressible Fluid Model. In the present study, blood was modeled as an incompressible Newtonian fluid with density ⫽1050 kg/m3 and viscosity ⫽0.004 kg m⫺1 s⫺1 共0.04 poise兲. The dynamic flow is governed by the continuity, and Navier-Stokes equations, respectively, as 冉 ⵜ• ⫽0 冊 ⫹ •ⵜ ⫽⫺ⵜp⫹ ⵜ 2 t (1) (2) where is the velocity vector, and p is the pressure. Various boundary conditions were considered as discussed in Sec. 2.4. 2.3 Orthotropic Exponential Pseudo-Elastic Model. It has been experimentally determined that Kirchhoff stress-tensor increases exponentially with the Green strain-tensor for arterial vessels 共e.g., 关1,9,10兴兲. Here, the behavior of the arterial wall was assumed to obey an orthotropic, pseudo-elastic, incompressible, exponential model proposed by Fung 共e.g., 关11兴兲. The pseudostrain energy density W̄ can be written as c0 W̄⫽ 关 exp兵 c 1 Ē r2 ⫹c 2 Ē z2 ⫹c 3 Ē 2 ⫹2 共 c 4 Ē r Ē z ⫹c 5 Ē z Ē 2 ⫹c 6 Ē Ē r 兲 其 ⫺1 兴 (3) where Ē r , Ē z , and Ē represent the normalized Green’s strains in the radial, longitudinal, and circumferential directions, respectively. These strains are related to the normalized stretch ratios by Journal of Biomechanical Engineering x j x i W̄ ⫹ 共 i, j, ␣ ,  ⫽r,z, 兲 0 X ␣ X  E ␣ ij (7) where x i and X ␣ denote coordinates, and and 0 represent densities, in the deformed and reference states, respectively. Here, (J)⫽(J⫺1) 2 is selected as the penalty function to impose the volume-conserving constraint 关13兴. The parameter reflects the incompressibility of the material. For ideally incompressible materials, J⫽1 and ⫽ 0 , the above equations correspond to those presented by Chuong and Fung 关11兴. We chose the same material properties for rabbit thoracic artery, as used by Chuong and Fung 关11兴: c 0 ⫽22.40 kPa, c 1 ⫽0.0499, c 2 ⫽0.4775, c 3 ⫽1.0672, c 4 ⫽0.0585, c 5 ⫽0.0903, c 6 ⫽0.0042. The constant c 0 scales all the stresses at certain strains. In other words, c 0 represents the overall rigidity of the vessel wall. The constants c 1 , c 2 , and c 3 reflect the relative elasticity in the principal directions, i.e., the mechanical anisotropy of the vessel wall. The constants c 4 , c 5 , and c 6 reflect the Poisson’s ratio of the vessel wall. A relatively large penalty parameter ⫽1000 kPa was adopted. The density of the blood vessel wall was assumed to be ⫽1100 kg/m3 . Rachev et al. 关14兴 showed that under the assumption of incompressibility, and based on the finite deformation theory, the principal stretch ratios can be expressed as r⫽ R , z r z z⫽ , Z ⫽ r R (8) where R denotes the radius of an arbitrary point at zero-stress state 共an open sector兲, r is the radial coordinate in the deformed configuration, ⫽ /( ⫺⌽) is a factor depending on the opening angle ⌽ defined as the angle subtended by two radii connecting the midpoint and the endpoints of the open sector. For the no-load state, we have ⫽2.53 from the experimental data by Chuong and Fung 关11兴, while assuming z ⫽1. The relationship between the undeformed coordinate and the deformed 共no-load兲 coordinate can be written as 关14兴 R⫽ 冑 共 r 2 ⫺r i2 兲 ⫹R i2 (9) The inner and outer radii at no-load state and zero-stress state were obtained from Chuong and Fung 关11兴 r i ⫽1.39, r e ⫽1.99, R i ⫽3.92, R e ⫽4.52 mm, which correspond to an opening angle ⌽⫽108.6 deg. Given Eqs. 共6兲, 共8兲, and 共9兲, we computed the distributions of residual strains at the no-load state. The constitutive model was coded and linked to ANSYS through user subroutine USERMAT as outlined in the Appendix. DECEMBER 2004, Vol. 126 Õ 761 Fig. 2 „a… The pulsatile inlet and outlet pressures. „b… The difference between inlet and outlet pressures. „c… External compression of outer surface „10% change of outer radius… due to muscle contraction. „d… Inlet velocity boundary condition. 2.4 Boundary Conditions. To simulate physiological conditions, we first stretched the artery 共e.g., stretch ratio z ⫽1.5) from the no-load configuration, then pressurized the inner vessel surface by increasing the inlet and outlet pressures simultaneously. To accomplish these maneuvers, the inlet of the vessel was not allowed to move longitudinally 关the displacement in the z direction was fixed at zero, see Fig. 1共a兲兴, and the displacement of the outlet along the axial direction was ramped from zero to the desired stretch ratio within 1 s and kept constant thereafter; the inlet and outlet pressures were then increased linearly from 0 to 16 kPa 共120 mmHg兲 and 15.92 kPa 共119.4 mmHg兲, respectively, from t⫽1 to t⫽2 s and kept constant until t⫽3 s. Starting from t⫽3 s, sinusoidal pulses with magnitudes of 40 and 39.6 mmHg were added to the inlet pressure and the outlet pressure 关see Fig. 2共a兲兴, resulting in a pressure drop from the inlet to the outlet as shown in Fig. 2共b兲. During the pulsatile flow process, the stretch ratio was maintained constant. It should be noted that a stabilization process was needed 共from t⫽2 to 3 s兲 to establish stress equilibrium state in the vessel. The position of the outer surface at t⫽3.5 s was taken as the initial value, followed by a timedependent sinusoidal displacement, in order to simulate the movement caused by the surrounding tissue contraction 关Fig. 2共c兲兴 as described below. The displacement was negative because it was used to simulate muscle contraction 共relative to the loaded dimension at t⫽3.5 s). We conducted one and a half cycles (t ⫽3.5– 5 s) and used the result from the last cycle (t⫽4 – 5 s) to eliminate the artificial effect that may be caused by the change from ‘‘static’’ to ‘‘pulsatile’’ flow. It is clear from Fig. 2, that end systole occurs at t⫽4 and 5, and end diastole occurs at t⫽3.5 and 4.5 s. Fluid-solid interaction was defined at the interface of blood and the vessel wall. To assess the effect of surrounding tissue, we considered the following three boundary conditions on the outer 762 Õ Vol. 126, DECEMBER 2004 surface: 共1兲 zero traction, 共2兲 zero displacement, and 共3兲 periodic displacement with a 10% change of outer radius. The zero-traction condition corresponds to the in vitro case 共i.e., the vessel is dissected away from the surrounding tissue兲 and was used as the control simulation. The zero-displacement condition may correspond to the case of a vertebral artery surrounded by a rigid bone. Finally, the periodic external displacement case may correspond to an intramural vessel in the contracting myocardium. These three simulations will be referred to as Cases I, II, and III, respectively. We used both the pressure, and the more common blunt shape velocity, boundary conditions at the inlet. For the pressure boundary condition, the pressure drop was taken as a sinusoidal pulse with a small magnitude, as shown in Fig. 2共b兲, which causes a variable pressure gradient in the vessel 共frequency, f ⫽1 Hz). The average pressure drop in one cycle was equal to ⌬ P⬇53.3 Pa. The average flow velocity was estimated to be V⬇0.11 m/s 共from Poiseuille’s law V⫽⌬ Pr i2 /8 L), resulting in a moderate Reynolds number Re⫽2riV/⬇78.3. The Womersley number, Wo ⫽r i 冑2 f / , was another important quantity that was used to describe the unsteady manner of fluid flow in response to a dynamic pressure boundary 关15兴. In the current simulation, the Womersley number was approximately 1.8. Note that both the Reynolds and Womersley numbers are evaluated at the no-load configuration, and they will change due to the distension of blood vessel under physiological conditions 共i.e., they will increase slightly兲. For the velocity boundary condition, the velocity at the inlet was increased from 0 to 0.2 m/s as shown in Fig. 2共d兲. The outlet pressure was assumed to vary with time, in a manner similar to the inlet pressure boundary condition 关see outlet pressure in Fig. 2共a兲兴. We estimated the phase difference between the inlet and the outlet boundary conditions which resulted in a pressure Transactions of the ASME Fig. 3 „a… Typical velocity profile half way along the length of the vessel „ z Ä L Õ2… for Case III „periodic displacement boundary… with pressure boundary condition. „b… Axial flow velocity versus time at the midpoint of the centerline „ r Ä0,z Ä L Õ2…. „c… Typical velocity profiles „at z Ä4 L Õ5… for Case III with velocity boundary condition. „d… Axial flow velocity versus time „at r Ä0, z Ä4 L Õ5… when velocity boundary is applied. drop as shown in Fig. 2共b兲. For an isotropic, elastic, thin tube, the pulse wave velocity can be calculated from the Moens-Korteweg equation as C⫽ 冑ET/2 r i where E is Young’s modulus 关16兴. The travel time of the wave was subsequently computed from the velocity for a 3-cm long vessel. Based on the model parameters, the time delay between the inlet and the outlet was estimated to be 0.0035 s, which gave a 1.26 deg phase difference. The phase delay is due to the elasticity of the vessel wall and it is expected to increase with an increase in length of vessel and frequency of flow. 3 Results We performed all of the simulations on a single CPU DELL desktop computer running Windows XP Professional. A typical run for full analysis required about 6 h. 3.1 Role of Residual Strain. We compared the circumferential stress distribution in the presence and absence of residual strain. For a stretch ratio of 1.5 and an internal pressure of 100 mmHg, it was found that the maximum circumferential Cauchy stress is ten times larger on the inner surface as compared to the outer surface, when residual strain was not included. However, the stress ratio 共inner to outer兲 reduced to a number smaller than two when residual strain was included. Since the residual strain strongly influences the wall stress distribution, it was included in all simulations. 3.2 Flow Field and Wall Shear Stress. The radial distribution of axial velocity profiles were examined for Cases I, II, and III. It was noted that the fully developed velocity profile mimics the parabolic shape of a laminar flow. Although the pulsatile boundary conditions 关Figs. 2共a兲 and 2共d兲兴 were applied to all of Journal of Biomechanical Engineering the three cases, it was noted that the axial flow was similar to the flow in a rigid tube despite the elasticity of the vessel wall. The phase difference between the inlet and the outlet pressure was small 关unnoticeable in Fig. 2共a兲兴 since the blood vessel was short and the pulsatility was low. Figure 3共a兲 shows the results of the simulated velocity profiles at different time points in the pulsatile cycle for Case III 共periodic displacement of outer surface兲 under the pressure boundary condition. It should be mentioned that the radius of the vessel is normalized to unity. Figure 3共b兲 shows a comparison of the time course of velocity at the midpoint of the centerline 共the maximum velocity兲 between the three cases. Interestingly, we did not find significant differences between the velocity profiles of Cases I and II, but the maximum velocity in Case III is significantly smaller than that of the other two cases. Figure 3共c兲 shows the fully developed axial flow velocity profiles when the inlet velocity boundary condition is used for Case III. Figure 3共d兲 shows the temporal axial flow velocity 共at r⫽0, z⫽4L/5) under the velocity boundary condition 关Figure 2共d兲兴. It is apparent that the flow velocity attained under the inlet velocity boundary condition is lower than that of pressure boundary condition 关e.g., compare Figs. 3共a兲 to 3共c兲 and 3共b兲 to 3共d兲兴. Figure 4共a兲 summarizes the temporal variation of the wall shear stress 共WSS兲 for the three cases during a loading cycle 共with the pressure boundary兲 and Fig. 4共b兲 shows the corresponding temporal WSS with the velocity boundary condition. It can be seen from Fig. 4 that Case III reveals a decrease in WSS under the pressure boundary condition and an increase in WSS under the velocity boundary condition. 3.3 Vessel Wall Stress Distribution. The principal stresses 共circumferential, axial, and radial兲 were computed throughout the cardiac cycle. Figures 5共a兲–5共c兲 show the transmural distribution DECEMBER 2004, Vol. 126 Õ 763 Fig. 4 „a… The temporal variation of wall shear stress at r Ä r i and z Ä L Õ2 „midpoint of the inner surface…. „b… The temporal variation of wall shear stress „at z Ä4 L Õ5… when velocity boundary is used. of radial, axial, and circumferential stresses, respectively, at various time points for the pressure boundary condition in Case III. The radial stress is seen to be compressive and its magnitude was significantly smaller than the tensile axial and circumferential stresses. All of the stresses decreased from the inner to the outer side of the vessel wall. The circumferential 共or hoop兲 stress had the largest transmural stress gradient. The transmural stresses and corresponding strains were averaged over the vessel thickness, and plotted as functions of loading cycle in Figs. 6 and 7, respectively. Figures 6共a兲, 6共b兲, and 6共c兲 correspond to the three principal stresses for each of the three cases. In comparison to the zero-traction condition 共Case I兲, the stresses decrease for Case III. It can be noted that the circumferential and axial stresses decrease dramatically as the vessel wall is compressed by the surrounding tissue. For example, the circumferential stress at maximum contraction (t⫽5 s) is less than one-third the maximum circumferential stress at t⫽4.5 s 共when the surrounding tissue relaxes兲. The stress gradients in the vessel wall are also reduced by the compression and thus more uniformly distributed stresses are obtained at the maximum contraction. Similarly, Figs. 7共a兲, 7共b兲, and 7共c兲 correspond to the logarithmic strains. It is interesting to see that the minimum radial stress 关Fig. 6共a兲兴 corresponds to the maximum radial strain 关Fig. 7共a兲兴 in Case III. This is caused by the surrounding muscle contraction. 3.4 Effect of Fluid-Solid Interaction. The simulation results suggest that the FSI cannot be neglected, as the diameter of vessel and the wall stresses are found to be affected by the pressure pulse 共e.g., Fig. 6兲. Moreover, Case III advocates that larger deformation of vessel wall can be produced by the surrounding muscle. Accordingly, the flow pattern near the inner surface of the vessel wall may also be affected. Figures 8 shows the radial velocity profiles at various time points of the loading cycle for Case III with the pressure inlet boundary condition. The radial flow velocity for Case I showed similar profiles where the maximum 764 Õ Vol. 126, DECEMBER 2004 Fig. 5 Stress distribution in vessel wall for Case III „periodic displacement boundary…: „a… radial stress; „b… axial stress; and „c… circumferential stress velocity was less than one-third of that for Case III, and the radial flow velocity for Case II was approximately zero. To study the influence of tissue compression on the circumferential stress gradient in arteries, we carried out a systematic simulation. While keeping all the other parameters constant, we varied the degree of compression by 0%, 5%, 10%, 15%, and 20% of the outer radius, and summarized the temporal variation of circumferential stress gradient in Fig. 9. The stress gradient was defined as the difference of the circumferential stress between the inner and outer surface divided by the updated wall thickness since the wall thickness changes during the cardiac cycle. The zero shrinkage case 共solid line in Fig. 9兲 is the case where the outer surface is attached to a rigid body 共Case II兲. Figure 9 shows that the stress gradient can be dramatically reduced by a small amount of external contraction 共see curve for 5% compression兲. It is noted that the stress gradient may become negative, i.e., the stress on the inner surface is smaller than the stress on the outer surface, when the external compression is large 共see curve for 20% compression兲. 4 Discussion 4.1 Fluid Mechanics Hypothesis. Knowledge of the instantaneous velocity field is important because it determines the Transactions of the ASME Fig. 6 Average stresses as a function of time in the vessel wall: „a… radial stress; „b… axial stress; and „c… circumferential stress. spatial and temporal wall shear stress distribution, which influences the biochemical response of endothelial cells lining the arterial lumen. The velocity field also dictates the flow residence times, which influences mass transfer rates for blood-borne particles 共e.g., low-density lipoprotiens兲 to the endothelium and affects atherogenesis. We investigated the pulsatile blood flow in a large artery loaded by either a rigid boundary, or by cyclical external compression, using finite element analysis. The model takes into account FSI, exponential and orthotropic material properties, as well as physiologically realistic boundary conditions. The simulation results indicate that under the pressure boundary condition, the flow velocity decreases when the external tissue contracts onto the vessel 关Fig. 3共b兲兴, which is contrary to the notion of ‘‘wash out’’ effect. These results imply that the transit time would increase and the wall shear stress would decrease 关Fig. 4共a兲兴, due to the added flow resistance 共decrease of vessel diameter兲 during contraction. Figure 3共b兲 shows that the maximum flow velocity under the rigid surJournal of Biomechanical Engineering Fig. 7 Average logarithmic strains versus time in the vessel wall: „a… radial logarithmic strain; „b… axial logarithmic strain; and „c… circumferential logarithmic strain. face condition can be slightly lower than in the case with zerotraction boundary since in the former, there is a smaller CSA because the diameter does not increase at systole. Thus the flow Fig. 8 Radial flow velocity profiles „at z Ä L Õ2… for Case III „periodic-displacement on the outer surface…. DECEMBER 2004, Vol. 126 Õ 765 tain a temporal profile of WSS that is very similar to Fig. 4. This implies that the widely used Poiseuille’s formula 共e.g., 关18 –20兴兲 is still an excellent measure of WSS when FSI is considered. Fig. 9 The temporal variation of circumferential stress gradients „at z Ä L Õ2… during the loading pressure boundary conditions. The various curves correspond to different amplitudes of displacement with 0% as no displacement corresponding to Case III followed by 5%, 10%, 15% and 20% maximum change of outer radius. resistance is larger and the flow velocity does not increase as much. The centerline axial velocity in Case III seems to be lower than the other two cases. The local flow near the inner surface is strongly influenced by the movement of the vessel wall. Hence, the mass transfer rate between the blood and the vessel wall could be altered by the movement of surrounding tissue. Therefore, some other parameter 共in addition to transit time兲 may be needed to describe the ‘‘wash out’’ effect. Furthermore, it can be argued that more complex geometry such as curvature and bifurcations may change the flow pattern. The present conclusion, however, holds for a straight vessel. In addition to the pressure inlet boundary conditions, we also examined the velocity boundary condition 关see Fig. 2共d兲兴, by maintaining the same outlet pressure as in the pressure boundary condition. It is noted that the fully developed flow velocity maintains the parabolic shape, but some negative flow is also seen near the wall when the inlet velocity is small 关Fig. 3共c兲兴. The maximum flow velocity increases slightly due to the tissue compression 关Case III in Fig. 3共d兲兴. Thus the ‘‘wash out’’ may occur under the velocity boundary conditions 关such as Fig. 3共d兲兴. However, the effect is rather small in terms of average axial flow velocity and the flow field is not significantly different in the three cases. If we consider Case III with a larger amplitude 共e.g., 20% change of outer radius兲, we can further enhance the wash out effect, increase the phase differences, and produce negative flows at the centerline 共data not shown兲. The larger deformation of the vessel is physiologically feasible since intramural arteries are likely to undergo significant compression during the cardiac cycle 共see review in Ref. 关17兴兲. Figure 4共b兲 indicates that the WSS may increase due to the contraction of vessel wall, which is due to the increase of inlet flow velocity 关Fig. 2共d兲兴. This also implies that the wall movement will change the local flow near the inner wall. It is interesting to see that some negative WSS appear when the inlet velocity is close to zero 关Fig. 4共b兲兴. The time course of axial velocity for the velocity boundary condition 关Fig. 3共d兲兴 is more realistic than that corresponding to the pressure boundary condition 关Fig. 3共b兲兴. The radial flow velocity 共Fig. 8兲, though very small compared with the axial flow near the centerline, is comparable to the axial flow velocity near the vessel wall due to the no-slip flow condition. Hence, the local hemodynamics near the inner surface may affect molecular transport. This also implies that the FSI effect is very important in simulating blood flow in deformable vessels. The radial velocity in the rigid surface case is always zero because the vessel diameter does not change. It should be noted that if we integrate the velocity profiles 共Fig. 3兲 over the entire cross-sectional area to compute flow rate Q 共volume per unit time兲, and then use Poiseuille’s equation ⫽4 Q/ r i3 to calculate the mean wall shear stress, we will ob766 Õ Vol. 126, DECEMBER 2004 4.2 Solid Mechanics Hypothesis. Although the effect of surrounding tissue on blood flow was found to be small, the effect on stress distribution was very significant 共Fig. 5兲 especially for the moving external boundary condition. Our simulations predict that stress will become more uniform, when the outer surface is compressed by the surrounding tissue 共see Fig. 9兲. This is a significant finding since elevated stress is known to cause growth and remodeling of blood vessels 共see review in Ref. 关21兴兲. Furthermore, although the bio-fluid mechanics community attributes the prevalence of atherosclerosis at sites of bifurcation and in curved vessels to complex fluid fields with regions of low WSS 关2兴, the bio-solid mechanics view suggests that atherogenesis is due to elevated stress and possibly stress concentration in those regions 共关3,22兴兲. Figure 9 shows an interesting effect of muscle contraction on the circumferential stress gradient in the vessel wall. The rate of change of stress gradient seems to decrease when the diameter is being further compressed. This observation stems from the high nonlinearity of the vessel material property. The existence of residual stress was found to reduce the magnitude of the stress gradient significantly which is consistent with previous reports 关11兴. Hence, although the residual stress is relatively small compared to wall stresses under physiological loading, it contributes a great deal to the transmural homogeneity of circumferential stress. This consequence is attributed to the large nonlinearity of the stressstrain relationship of vessel wall. The major finding of the present study is the significant reduction of intramural circumferential stress and strain for a vessel under rigid external support 共Case II; e.g., vertebral artery兲 or periodic external compression 共Case III; e.g., coronary artery兲. This result has important implication since it is well known that high stresses and strains can induce growth, remodeling, and atherosclerosis 关22,1兴. Hence, we hypothesize that a reduction of stress and strain may be atheroprotective. The test of this hypothesis remains a task of future investigation. 4.3 Comparison With Other Studies. Various computational fluid dynamics 共CFD兲 codes have been used to simulate the hemodynamics of blood; e.g., 关23兴 used CFD 2000 Professional to study the physiologic pulsatile blood flow in healthy and stenosed vessels; Taylor et al. 关24兴 and Cebral et al. 关25兴 employed their own codes to simulate blood flow in realistic vessel geometries reconstructed from computer tomography or magnetic resonance imaging. Changes in vessel geometry were found to strongly influence the local fluid field. Solid mechanics has been utilized to analyze stress distributions in passive blood vessels 共e.g., 关11兴兲 and in active arteries with smooth muscle contraction 关26兴. It was concluded that both residual stress and basal muscular tone help to homogenize the stress along the vessel wall. Previous investigations, however, have seldom considered the interaction between blood flow and vessel wall due to the difficulty in solving coupled fluid and solid equations. Sequential coupling method has been recently attempted by using separate commercial packages for fluid and solid, respectively 关27–29兴. Nevertheless, an additional interface is required to exchange the coupling-loads across the fluid-solid interface during the iteration process. De Hart et al. 关30兴 developed a fictitious domain method that is capable of simulating FSI phenomenon. In their work, the opening and closing behavior of an aortic valve during the diastolic phase was simulated. 4.4 Critique of Model. The convergence of the current simulation results was verified by using finer meshes. It was found that no significant change of flow velocity and vessel wall stresses occurred by reducing the current element size by one half. The average radial stress on the wall surfaces, however, was found to more accurately approach the exact boundary conditions 关e.g., raTransactions of the ASME dial stress is zero on the external surface, see Fig. 5共a兲兴. The time step was carefully tested and a minimum increment of 0.005 s was found to result in convergent results in pulsatile flows. Smaller time steps did not yield significant changes of fluid velocity and wall stress. Although we used the term transient flow, the inertial effect is not obvious in the current simulations due to the small frequency 共1 Hz兲. This also explains why the flow profiles and wall shear stress differ so little in the three cases. The FSI simulation, which includes the time-depending boundary conditions, can be viewed as a series of ‘‘quasi-steady’’ simulations. It is natural, however, to consider the problem as ‘‘transient’’ because of the boundary conditions. A number of simplifying assumptions were made in the current analysis, which ignore the non-Newtonian properties of blood, vessel bifurcations, taper, curvature, permeability, and heterogeneity of vessel wall, etc. The two-dimensional axisymmetric model was used to reduce the computational cost and to facilitate the implementation of the nonlinear anisotropic model. Threedimensional flow analysis in more complex geometries has been successfully simulated by various authors, but none considered the fluid-solid interaction in a complex model with anisotropic material properties. All these higher order effects can be considered in future studies to assess their relative importance. It must be emphasized that atherogenesis is multifactorial involving physical, biochemical, and biological effects. For example, it is well known that physical 共hypertension兲 and chemical 共diabetes, cigarette smoke, and hypercholestermia兲 factors are important risk factors for atherogenesis. These chemical factors are global, however, and affect the entire vascular system. The focus of the present study is the local physical 共fluid and solid mechanics兲 factors and hence the conclusions are limited to the mechanical point of view. The boundary condition for Case III was selected because the maximum blood pressure is reached at systole; i.e., at maximum contraction. Hence, we idealized the phase difference between the blood pressure and the contraction of the vessel wall; i.e., maximum pressure corresponds to minimum lumen diameter. The phase differences between blood pressure and extravascular compression may be different, however, for different intramural vessels. The phase differences as well as the amplitudes and the patterns of those periodic boundary conditions may yield different results regarding washout effect, WSS, and intramural stress. A systematic analysis of these factors is a laudable goal of a future investigation. 4.5 Summary and Significance of the Study. The commercial finite element software ANSYS in conjunction with a constitutive equation of an artery was utilized to investigate the blood flow velocity profile, the stress distribution in the vessel wall, and the wall shear stress in a simplified arterial blood vessel subjected to various boundary conditions. Our simulation results indicate that the average flow velocity and wall shear stress change slightly when zero-traction, zero-displacement, and periodic displacement boundary conditions are applied to the outer surface. However, the stress variations in the vessel wall differ significantly under these different boundary conditions. The compression from the surrounding tissue seems to considerably reduce the stress level and stress gradient in the wall. This study provides a biomechanical understanding of vessels with predilection for atherogenesis. Although the fluid forces acting on the endothelium have been greatly acknowledged in the literature 关1兴, the present study suggests that the solid mechanics of the vessel wall should be equally considered. The development of a therapeutic rationale for prevention and future reduction of atherosclerosis must consider both the fluid and solid mechanical status of the vessel wall. Journal of Biomechanical Engineering Acknowledgments This research was supported in part by the National Institute of Health-National Heart, Lung, and Blood Institute Grant No. 2 R01 HL-055554-06, UCI’s COCLR No. MI-2002-2003-15, and the US Army Research Office. W.Z. thanks Dr. Z. D. Han for helpful discussions regarding the ANSYS code. Dr. S. S. K. is an American Heart Association Established Investigator. Appendix: Formulation of Pseudo-Elastic Model In the axisymmetric model, we considered Fung’s type exponential pseudoelastic strain energy as W̄⫽ c 0 Q¯ c 0 e ⫽ exp兵 c 1 Ē r2 ⫹c 2 Ē z2 ⫹c 3 Ē 2 ⫹2 共 c 4 Ē r Ē z ⫹c 5 Ē z Ē 2 2 2 ⫹c 6 Ē Ē r ⫹c 7 Ē rz 兲其 (A1) 2 c 7 Ē rz The energy density function includes an extra term, because the in-plane rotation provides another degree of freedom in the axisymmetric model. Since in the current analysis the shear deformation is negligible, we selected a relatively large value of c 7 ⫽4.2 to force the shear strain Ē rz ⫽E rz to zero. For an incompressible material, we selected the following penalty function: 共 J 兲 ⫽ 共 J⫺1 兲 2 ⫽ 共 r z ⫺1 兲 2 ⫽ 关 冑共 1⫹2E r 兲共 1⫹2E z 兲共 1⫹2E 兲 ⫺1 兴 2 ⫽0 (A2) To enforce the incompressibility of blood vessel, we take Eq. 共A2兲 as a penalty function. Cauchy stress can then be written a i j⫽ x j x i W̄ ⫹ 共 i, j, ␣ ,  ⫽r,z, 兲 0 X ␣ X  E ␣ ij (A3) Using Eqs. 共4兲–共6兲 and E i ⫽( i2 ⫺1)/2, we can express the principal Cauchy stresses in terms of normalized Green’s strains as ¯ r2 r ⫽ W̄ Ē r ¯ ⫹ J⫽c 0 共 1⫹2Ē r 兲共 c 1 Ē r ⫹c 4 Ē z ⫹c 6 Ē 兲 e Q ⫹ J (A4) ¯ z2 z ⫽ W̄ Ē z ¯ ⫹ J⫽c 0 共 1⫹2Ē z 兲共 c 2 Ē z ⫹c 4 Ē r ⫹c 5 Ē 兲 e Q ⫹ J (A5) Fig. 10 A flow chart of the sequential coupling of fluid-solid interaction adapted from ANSYS Inc, 2003 DECEMBER 2004, Vol. 126 Õ 767 ¯ 2 ⫽ W̄ Ē 共 J 兲 共 J 2 ⫺J 兲 J ⫽2 ⫽2 共 2J⫺1 兲 ⫽2 共 2J 2 ⫺J 兲 ⫽ i i i (A8) ¯ ⫹ J⫽c 0 共 1⫹2Ē 兲共 c 3 Ē ⫹c 5 Ē z ⫹c 6 Ē r 兲 e Q ⫹ J (A6) where ⫽ ⬘ (J)⫽2(J⫺1)⫽2 关 冑(1⫹2E r )(1⫹2E z )(1⫹2E ) ⫺1 兴 . The shear stress was calculated as r z W rz ⫽ ⫽c 0 c 7 冑共 1⫹2E r 兲共 1⫹2E z 兲 E rz e Q 2 E rz where is a scalar and i⫽r, z or . In the user subroutine USERMAT provided by ANSYS, the Jacobian matrix is defined between Cauchy stress and logarithmic strain. Considering the relationship between logarithmic strain and Green’s strain, as well as the relation between normalized and non-normalized Green’s strains, we can finally write the Jacobian matrix as (A7) The shear strain is assumed to be small in Eq. 共A7兲. Finally, we have the relationships J⫽2 (J 2 ⫺J) and J⫽exp(r⫹z⫹) which can be expressed as 冤 共 1⫹2Ē r 兲 共 1⫹2Ē r 兲 共 1⫹2Ē r 兲 r Ē r z Ē r Ē r ⫹ 共 1⫹2Ē z 兲 ⫹ 共 1⫹2Ē z 兲 ⫹ 共 1⫹2Ē z 兲 0 r Ē z z Ē z 0 where rz / Ē rz ⬇ rz / rz ⬇ rz / E rz ⬇c 0 c 7 冑共 1⫹2E r 兲共 1⫹2E z 兲 e Q . In our simulations, we verified that shear strain is small. Hence, the above formulation is not applicable to problems involving large rotation or shear deformation. The use of the above model was relatively simple. In the user subroutine USERMAT, ANSYS provides the current logarithmic strains. The strains were used to calculate the stresses and the Jacobian matrix and were passed back to ANSYS for computation of new strains. The USERMAT was compiled and linked with ANSYS using a batch command provided in the ANSYS package to create a new executable. When we ran the simulation, the new executable was used. In the input file, the material model for the vessel wall was defined as a user material 共to call user subroutine USERMAT兲. Other procedures were similar to the standard usage of the software. The flow chart of the sequential coupling of fluid-solid interaction is shown in Fig. 10 关8兴. References 关1兴 Fung, Y. C., 1997, Biomechanics: Circulation, Springer-Verlag, New York. 关2兴 Caro, C. G., Fitzgerald, J. M., and Schroter, R. C., 1971, ‘‘Atheroma and arterial wall shear–observation, correlation and proposal of a shear dependent mass transfer mechanism for atherogenesis,’’ Proc. R. Soc. London, Ser. B, 177共1046兲, pp. 109–159. 关3兴 Robicsek, F., and Thubrikar, M. J., 1994, ‘‘The freedom from atherosclerosis of intramyocardial coronary arteries: Reduction of mural stress—A key factor,’’ Eur. J. Cardiothorac Surg., 8共5兲, pp. 228 –235. 关4兴 DeBakey, M. E., Lawrie, G. M., and Glaeser, D. H., 1985, ‘‘Patterns of atherosclerosis and their surgical significance,’’ Ann. Surg., 201共2兲, pp. 115–131. 关5兴 Kassab, G. S., 2000, ‘‘The coronary vasculature and its reconstruction,’’ Ann. Biomed. Eng., 28共8兲, pp. 903–915. 关6兴 Kenyon, D., 1979, Anatomical and physiological characteristics of arteries. S., Wolf and N. T., Werthessen, eds., Dynamics of Arterial Flow, Vol 115, Plenum Press, New York, p. 48. 关7兴 Meyer, W. W., and Naujokat, B., 1964, ‘‘Uber die rhythmishe Lokalisation der atherosklerotischen Herde im cervikalen Abschnitt der vertebralen Arterie,’’ Beitr Pathol. Anat., 130, pp. 24 –39. 768 Õ Vol. 126, DECEMBER 2004 Ē z ⫹ 共 1⫹2Ē 兲 ⫹ 共 1⫹2Ē 兲 ⫹ 共 1⫹2Ē 兲 0 r Ē z Ē Ē ⫹ 0 ⫹ 0 ⫹ 0 rz Ē rz 冥 (A9) 关8兴 ANSYS Inc., 2003, ANSYS 7.1 Online Documentation 共provided with the ANSYS software under University research license兲. 关9兴 Zhou, J., and Fung, Y. C., 1997, ‘‘The degree of nonlinearity and anisotropy of blood vessel elasticity,’’ Proc. Natl. Acad. Sci. U.S.A., 94共26兲, pp. 14255– 14260. 关10兴 Hamza, L. H., Dang, Q., Lu, X., Mian, A., Molloi, S., and Kassab, G. S., 2003, ‘‘Effect of passive myocardium on the compliance of porcine coronary arteries,’’ Am. J. of Physiology-Heart and Circulatory Physiology, 285共2兲, pp. H653–H660. 关11兴 Chuong, C. J., and Fung, Y. C., 1986, ‘‘On residual-stresses in arteries,’’ J. Biomech. Eng., 108共2兲, pp. 189–192. 关12兴 Atluri, S. N., 1984, ‘‘Alternate stress and conjugate strain measures, and mixed variational formulations involving rigid rotations, for computational analyses of finitely deformed plates and shells. Part-I: Theory,’’ Comput. Struct., 18共1兲, pp. 93–116. 关13兴 Atluri, S. N., and Reissner, E., 1989, ‘‘On the formulation of variational theorems involving volume constraints,’’ Comput Mech., 5共5兲, pp. 337–344. 关14兴 Rachev, A., Stergiopulos, N., and Meister, J. J., 1996, ‘‘Theoretical study of dynamics of arterial wall remodeling in response to changes in blood pressure,’’ J. Biomech., 29共5兲, pp. 635– 642. 关15兴 Loudon, C., and Tordesillas, A., 1998, ‘‘The use of the dimensionless Womersley number to characterize the unsteady nature of internal flow,’’ J. Theor. Biol., 191共1兲, pp. 63–78. 关16兴 Zamir, M., 2000, The Physics of Pulsatile Flow, Springer Verlag, New York. 关17兴 Hoffman, J. I. E., and Spaan, J. A. E., 1990, ‘‘Pressure-flow relations in the coronary circulation,’’ Physiol. Rev., 70, pp. 331–390. 关18兴 Kassab, G. S., and Fung, Y. C., 1995, ‘‘The pattern of coronary arteriolar bifurcations and the uniform shear hypothesis,’’ Ann. Biomed. Eng., 23, pp. 13–20. 关19兴 Wellnhofer, E., Bocksch, W., Hiemann, N., Dandel, M., Klimek, W., Hetzer, R., and Fleck, E., 2002, ‘‘Shear stress and vascular remodeling: Study of cardiac allograft coronary artery disease as a model of diffuse atherosclerosis,’’ J. Heart Lung Transplant, 21共4兲, pp. 405– 416. 关20兴 Kavdia, M., and Popel, A. S., 2003, ‘‘Wall shear stress differentially affects NO level in arterioles for volume expanders and Hb-based O-2 carriers,’’ Microvasc. Res., 66共1兲, pp. 49–58. 关21兴 Kassab, G. S., Gregersen, H., Nielsen, S. L., Liu, X., Tanko, L., and Falk, E., 2002, ‘‘Remodeling of the coronary arteries in supra-valvular aortic stenosis,’’ J. Hypertens., 20共12兲, pp. 2429–2437. 关22兴 Thubrikar, M. J., and Robicsek, F., 1995, ‘‘Pressure-induced arterial-wall stress and atherosclerosis,’’ Ann. Thorac. Surg., 59共6兲, pp. 1594 –1603. 关23兴 Marques, P. F., Oliveira, M. E. C., Franca, A. S., and Pinotti, M., 2003, ‘‘Modeling and simulation of pulsatile blood flow with a physiologic wave pattern,’’ Artif. Organs, 27共5兲, pp. 478 – 485. Transactions of the ASME 关24兴 Taylor, C. A., Hughes, T. J. R., and Zarins, C. K., 1998, ‘‘Finite element modeling of blood flow in arteries,’’ Comput. Methods Appl. Mech. Eng., 158共1–2兲, pp. 155–196. 关25兴 Cebral, J. R., Yim, P. J., Lohner, R., Soto, O., and Choyke, P. L., 2002, ‘‘Blood flow modeling in carotid arteries with computational fluid dynamics and MR imaging,’’ Acad. Radiol., 9共11兲, pp. 1286 –1299. 关26兴 Rachev, A., and Hayashi, K., 1999, ‘‘Theoretical study of the effects of vascular smooth muscle contraction on strain and stress distributions in arteries,’’ Ann. Biomed. Eng., 27共4兲, pp. 459– 468. 关27兴 Zhao, S. Z., Xu, X. Y., Hughes, A. D., Thom, S. A, Stanton, A. V., Ariff, B., and Long, Q., 2000, ‘‘Blood flow and vessel mechanics in a physiologically Journal of Biomechanical Engineering realistic model of a human carotid arterial bifurcation,’’ J. Biomech., 33共8兲, pp. 975–984. 关28兴 Lee, K. W., and Xu, X. Y., 2002, ‘‘Modelling of flow and wall behavior in a mildly stenosed tube,’’ Med. Eng. Phys., 24共9兲, pp. 575–586. 关29兴 Penrose, J. M. T., and Staples, C. J., 2002, ‘‘Implicit fluid-structure coupling for simulation of cardiovascular problems,’’ Int. J. Numer. Methods Fluids, 40共3– 4兲, pp. 467– 478. 关30兴 De Hart, J., Peters, G. W. M., Schreurs, P. J. G., and Baaijens, F. P. T., 2003, ‘‘A three-dimensional computational analysis of fluid-structure interaction in the aortic valve,’’ J. Biomech. Eng., 36共1兲, pp. 103–112. DECEMBER 2004, Vol. 126 Õ 769