Infants in respiratory distress
advertisement

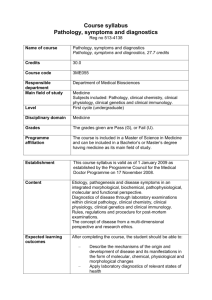
Infants in respiratory distress Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Case 1: 6 months old boy • 1 week cold, general condition OK then • 1,5 day: – – – – mild fever wheezing coughing able to fulfill meals with short breaks • No previous history of bronchial obstruction or atopy Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Examination • • • • • Unhappy, resists examination Coughing attacks during consultation Retractions intercostal and subcostal RR 45, HF 130, T 38,5, SaO2 95% Auscultation: moderate crepitations, some expiratory wheeze • Skin turgor, capillary refill 1-2 sec, mucous membrane wet Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Lab • CRP 30 • pH 7.30, pCO2 5,0 • Diagnosis? • Admit to hospital? • Other solutions? Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Acute viral bronchiolitis Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat History • Wheezing, degree of respiratory distress • Duration of symptoms, developing from common cold? • Eating: able to complete meals? • Urine output • 2 year older sibling in kindergarden • (atopic excema, previous BO, family history) Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Clinical examination • Retractions – Jugular, Intercostal, Subcostal • Respiratory frequence • Conciousness/general appearance • Auscaltation – Fine crepitations – Prolonged expirium – Expiratory wheeze • SaO2 • Nasal flaring Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Clinical examination • Hydration level – (skin turgor, capillary refill, mucus membrane, fontanel) • Heart rate Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Laboratory investigations • Blood gases – pH, pCO2 • Dehydration assessment – bicarbonate, urea, BE • Na, K, Hb, WBC, glukose, kreatinin Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Imaging • Chest x-ray Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Treatment • Oksygen • Nutrition – Nasogastric tube • Intravenous fluid • Respiratory support – CPAP – Conventional respirator • Nasal spray Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Treatment • Inhalations? – – – – Saline Racemic adrenaline (epinephrine) Salbutamol? Hypertonic saline? • Corticosteroids? Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Case 2: 4 weeks old girl • 2 year old brother in kindergarden with a cold last week • Upper airway infection 3 days • Much coughing last 24 hours • 2 apnoes of 10 seconds each last 12 hours • eats OK, but must have some breaks Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Examination • Smiles, excellent contact. Good activity • Mild subcostal retractions • Auscultation: some fine crepitations, no ekspiratory wheezing or prolonged expirium • HR 140, RF 55 • (Capillary refill time 2 sec, mucus membranes wet, turgor OK) Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Lab • CRP 7, pCO2 6,5 • Admit to hospital? Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat