Fever
advertisement

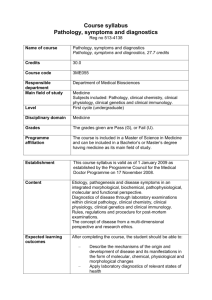
Fever Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Case 1: 7 months old girl • • • • 3 days fever General condition worsening last 2 days Sleepy, but gives good contact when awake Eats less than usual, but drinks OK and has wet dipers • No rhinorrhea, coughing, vomiting or diarrhea • Previously healthy Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Examination • Sleeps initially, but wakes up and gives contact • No smile, uncomfortable, but the mother is able to calm her • Skin color and turgor normal. Mucus membranes wet • Tonus OK • Capillary refill time 2 sec • RR 45, HF 160, T 39,5, SaO2 95% • Auscultation: normal heart and lung sounds Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Lab • CRP 235 • Urine bag sample: leukocytes +++, blood +, protein +, nitritis – • Catheter sample confirms the results, with positive microscopi Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Management • • • • Diagnosis? Admit to hospital? Other solutions? Follow up? Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Urinary Tract Infections Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat History • General condition – Feeding – Consciousness – Hydration (diuresis) • • • • Fever Focal infectious symptoms? Vomiting Previous history: ultrasound during pregnancy Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Clinical examination • Typically no focal signs of infection • General appearance – septic? – – – – – – Respiratory frequence Heart Rate Capillary refill time Skin colour Consciousness Activity Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Laboratory investigations • Urine sample – – – – – Leukocytes sensitive, nitritis specific Collection bag sample can only be used to exclude UTI! Midflow sample, catheter or bladder puncture Microscopy Urine culture • Blood sample – CRP, WBC, kreatinin, Na, K, Hb, urea, blood gases – Blood culture Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Imaging • • • • Chest x-ray? Ultrasound Voiding cystourethrogram DMSA – Scintigraphy – Acute diagnostic of pyelonephritis and chronic renal scarring Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Treatment • Oral – Mecillinam, Trimetoprim-sulpha, (3rd gen cefalosphorin), (Amoxicillin-clavulanate) • i.v – ampicillin-gentacimin, mecillinam, cefotaxim Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Risk factors • • • • • • • • • <6months Septic No effect of treatment within 48 hours Pathologic prenatal ultrasound Residiving pyelonephritis Non E.coli Unusual presentation (older boys) Heredity for vesikuloureteral reflux High kreatinin or BP Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Case 2: 2 months old boy • • • • High fever 1,5 day No vomiting or diarrhea Eats ok, diuresis normal General condition slightly reduced, more sleepy Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Examination • No smile, but excellent contact. Good activity • No focal signs • Auscultation: normal Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat Lab: • CRP 131 • Urine sample (mid flow): Leukocytes 3+, blood 2x, protein 2+, nitritis + • Admit to hospital? Medisinsk Fakultet, Institutt for Klinisk Medisin, Oslo Universitetssykehus, Barneklinikken, Håvard Ove Skjerven, Klinisk Stipendiat