Redacted for Privacy
advertisement

AN ABSTRACT OF THE THESIS OF
Duncan J. Gilroy for the degree of Doctor of Philosophy in Toxicology
presented October 18, 1990.
Title: Paracellular/Transcellular Perturbations in Hepatobiliary Dysfunction
Redacted for Privacy
Abstract approved: /
Robert E. Larson
Biliary excretion is an important excretory route for numerous toxicants. Though
mechanisms underlying impairment of bile flow and hepatic transport are poorly
understood, evidence suggests that specific paracellular and/or transcellular
dysfunctions are important. The present investigation was undertaken to evaluate the
significance of these changes relative to the cholestasis and organic anion retention
induced by the anticancer drug 1,3-bis(2-chloroethyl)-1-nitrosourea (BCNU) and the
experimental hepatotoxicant a-napthylisothiocyanate (ANIT).
BCNU induced a time-dependent decrease in bile flow in Sprague-Dawley rats.
Leakage of exogenous horseradish peroxidase (HRP) and endogenous inorganic
phosphate (P1) into bile indicated the bile/plasma permeability barrier had been
compromised.
Kinetics analysis of HRP leakage in a perfused liver system
demonstrated increased rapid phase (paracellular) and decreased slow phase
(transcellular) movement into bile. Electron microscopic examination of lanthanum-
perfused livers confirmed penetration of hepatocellular
tight junctions. Albumin-
bound Evans blue dye, found to be excluded from paracellular
movement during
conditions of increased permeability, was utilized
to evaluate transcellular effects of
BCNU in isolation. Colchicine and BCNU induced similar
decreases in Evans blue
excretion. A time-dependent decrease in active transport of the organic anion
bromosulfophthalein (BSP) was also observed with BCNU treatment. Similar time-
dependent increases in bile Pi, BSP retention, and cholestasis were observed
following ANIT treatment. Comparative thin layer
chromatography of BSP and
functional changes with various cotreatments indicated that BCNUand ANITinduced alterations in permeability, organic anion excretory capacity, and bile flow
were separable events.
Histologic examination of livers from BCNU- and ANIT-treated rats revealed bile
duct necrosis and a marked portal inflammation with
edema, fibrin deposition, and
inflammatory cell infiltration. Cotreatment with the glucocorticoid
triamcinolone and
the 5-lipoxygenase inhibitor esculetin protected against BCNU- and ANIT-induced
functional and morphologic changes. Cyclooxygenase
inhibition was not effective.
These results suggest that an inflammatory mediator may have an etiologic role in
the hepatotoxicity induced by BCNU or ANIT.
Changes in portal mast cell
number/activation state with the various cotreatments indicate that this mediator
may be mast cell-derived.
Paracellular/Transcellular Perturbations in
Hepatobiliary Dysfunction
by
Duncan J. Gilroy
A THESIS
submitted to
Oregon State University
in partial fulfillment of
the requirements for the
degree of
Doctor of Philosophy
Completed October 18, 1990
Commencement June 1991
APPROVED:
Redacted for Privacy
Professor] of Pharmacology and Toxicology in charge of major
Redacted for Privacy
Chairman of the Toxicology Program
Redacted for Privacy
Dean of Gradt School
Date thesis is presented
6
October 18. 1990
Typed by Duncan J. Gilroy for
Duncan J. Gilroy
ACKNOWLEDGMENT
I want to express my sincere gratitude for the support provided
by the National
Institutes of Health, the Toxicology Program, and the College of Pharmacy. I also
want to thank my advisor, Dr. Larson, for his guidance, Barb for her amazing
patience, and Wendy and Bob for originally sparking my interest in science.
Table of Contents
page
I.
General Introduction
1
Overview of Liver Structure
and Function
1
Bile Flow
5
The Transcellular Pathway
9
The Paracellular Pathway
Mechanisms of Cholestasis
Toxicants: BCNU and ANIT
II.
III.
IV.
V.
VI.
VII.
VIII.
IX.
X.
General Methods
Cholestatic Effects of BCNU and ANIT
Increased Paracellular Permeability with BCNU
and ANIT
Evans Blue Excretion: Inhibited Fluid-phase
Endocytosis with BCNU Treatment
Altered BSP Excretion with BCNU and ANIT
Treatment
Metabolic Studies: Changes in BCNU- and ANITinduced Hepatic Dysfunctions with Phenobarbital
Pretreatment
16
21
28
34
40
46
70
78
98
Potential Role of Inflammatory Mediators in the
Hepatotoxicity of BCNU and ANIT
113
ANIT- and BCNU-induced Liver Histopathology
143
Summary and Conclusions
References
Appendix
193
203
227
List of Figures
page
1.
Electron micrograph of control liver
2.
Change in bile flow with time following
BCNU treatment
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Change in bile flow with time following
ANIT treatment
Time course of horseradish peroxidase (HRP)
penetration into bile in vivo with BCNU
treatment
HRP excretion kinetics in vivo with BCNU
treatment
HRP excretion in the single-pass perfused
liver with BCNU and colchicine treatment
Biphasic kinetics of HRP excretion in the
single-pass perfused liver with BCNU
treatment
Dose-response relation of bile inorganic
phosphate (Ps) and BCNU
2
41
43
52
53
55
56
58
Correlation between bile P, and bile HRP
following BCNU treatment
59
Time course of Pi penetration into bile
following BCNU treatment
60
Lack of correlation between change in bile
flow and bile P, with time following ANIT
treatment
61
Time course of P, penetration into bile
following BCNU treatment, 2 doses
62
Lanthanum penetration of junctional complexes
64
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
Lack of correlation between change in bile
flow and bile Pi with time following BCNU
treatment
Decreased Evans blue excretion following
BCNU or colchicine treatment
74
Bile concentrations of Evans blue following
BCNU or colchicine treatment
76
Decreased hepatic BSP exctraction with
BCNU treatment
Decreased maximal bile BSP with BCNU
treatment
Regression analysis of influent and effluent
BSP with BCNU treatment
Perfusate BSP retention following BCNU
treatment
Perfusate BSP decay kinetics for 24-hour BCNU
and 12-hour ANIT livers
Decreased BSP excretion in bile with BCNU
treatment
Perfusate BSP retention following ANIT
treatment
24.
Thin layer chromatography
25.
Perfusate BSP decay kinetics for livers
from corn oil controls and phenobarbital
controls
26.
27.
28.
68
82
83
84
85
87
88
91
92
103
Decreased BCNU-induced perfusate BSP retention
with phenobarbital pretreatment
104
Increased bile [BSP] in BCNU-treated livers
with phenobarbital pretreatment
105
Increased maximal BSP excretion in BCNU-treated
livers with phenobarbital pretreatment
106
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
Decreased BCNU-induced perfusate BSP retention
with triamcinolone treatment
128
Decreased ANIT-induced perfusate BSP retention
with triamcinolone treatment
129
Increased BSP excretion in BCNU- and ANITtreated livers with triamcinolone treatment
Reversal of ANIT-induced BSP retention with
esculetin treatment
Normal BSP excretion following treatment with
ANIT and esculetin
130
131
132
No change in BCNU- or ANIT-induced perfusate
BSP retention with indomethacin treatment
133
Lack of a protective effect toward increased
perfusate BSP retention in livers from rats receiving
esculetin and perfused 48 hours after ANIT
treatment
134
Control liver (H/E stain)
147
Histopathologic changes with time following
treatment with 26 mg/kg BCNU (H/E stain)
148
Histopathologic changes with time following
treatment with 250 mg/kg ANIT (H/E stain)
151
Histopathologic changes in livers from rats
treated with BCNU and cotreated with
triamcinolone
or esculetin (H/E stain)
Histopathologic changes in livers from rats
treated with ANIT and cotreated with triamcinolone
or esculetin
Portal section from a control rat (toluidine blue
stain)
156
158
161
Histopathologic changes with time following
treatment with 26 mg/kg BCNU (toluidine blue stain)
162
Histopathologic changes with time following
treatment with 250 mg/kg ANIT (toluidine blue stain)
164
44.
45.
46.
47.
48.
Histopathologic changes with BCNU + TCN or
BCNU + ESC (toluidine blue stain)
166
Histopathologic changes with ANIT + TCN or
ANIT + ESC (toluidine blue stain)
168
Histopathologic changes with ESC + ANIT(48h)
(toluidine blue stain)
170
Histopathologic changes with BCNU + INDO
or ANIT + INDO (toluidine blue stain)
171
EM section from a BCNU-treated rat
188
List of Tables
page
1.
2.
3.
4.
5.
6.
7.
8.
9.
Perfused liver viability criteria for
control and BCNU-treated rats
38
Bile and plasma bilirubin, 48 hours after
26 and 34 mg/kg BCNU
42
Control Evans blue plasma concentrations
and excretion in vivo
73
BSP partial clearance constants following
BCNU treatment
89
Effects of phenobarbital pretreatment on
ANIT- and BCNU-induced cholestasis and bile
inorganic phosphate
101
Effect of eicosanoid synthesis inhibitors on
BCNU-induced cholestatic and permeability changes
126
Effect of eicosanoid synthesis inhibitors on ANITinduced cholestatic and permeability changes
127
Change in inflammatory parameters with BCNU plus
cotreatments
154
Change in inflammatory parameters with ANIT plus
cotreatments
155
List of Appendix Figures
1.
2.
3.
4.
5.
6.
Decrease in control bile flow with bile
duct cannulation and liver perfusion
227
Increase in liver/body weight ratio with
BCNU or ANIT treatment
228
HRP excretion in the perfused liver with
ANIT treatment
229
Difference in time course of increased bile
P, following ANIT treatment between SpragueDawley and Wistar rats
230
Time course of change in bile flow and bile
P, in Wistar rats with ANIT treatment
231
Lack of correlation between bile P, and bile
flow with BCNU treatment
232
List of Appendix Tables
1.
Decreased bile flow and increased bile inorganic
phosphate with CCNU treatment
233
PARACELLULAR/TRANSCELLULAR PERTURBATIONS
IN HEPATOBILIARY DYSFUNCTION
I. GENERAL INTRODUCTION
OVERVIEW OF LIVER STRUCTURE AND FUNCTION
The liver, strategically interposed between the gut and the rest of the body, has
a critical role in determining to what extent and in what form absorbed materials
(e.g. nutrients and toxicants) enter the systemic circulation. Portal
blood, draining
the stomach, intestines, spleen, gall bladder, and pancreas, joins arterial blood in
the liver sinusoids, bathes hepatocytes, is collected by central veins, and eventually
empties into the inferior vena cava (1,2).
Sinusoids are the liver's specialized capillaries, lined with endothelial and Kupffer
cells (Figure 1). Fenestrae between these cells, in clusters called sieve plates,
are
freely permeable to substances up to 250,000 MW.
These openings allow
unrestricted passage of most blood components (excluding RBCs) into the space
of Disse, which communicates directly with the hepatocyte surface (1).
Sixty per cent of the liver's cells are hepatocytes. Except for a few specialized
functions (e.g. urea cycle, bile acid synthesis), the structure and function of the
hepatocyte is similar to that of other cells, though quantitative differences do exist.
2
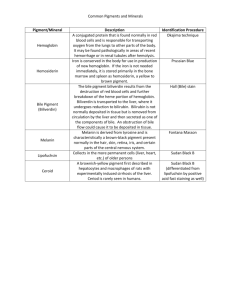
Figure 1. Electron micrograph of control liver. S: sinusoid; SD: Space of Disse;
N: hepatocyte nucleus; K: Kupffer cell; I: intercellular space; E: endothelial cell;
my: microvilli. Arrows identify sinusoidal fenestrations x6600.
3
Hepatocytes have two distinct domains: a basolateral domain, exposed to plasma
in the Space of Disse, and an apical domain, exposed to the biliary
compartment.
This polar structure is similar to that of other epithelial cells. However, unlike
other epithelia with basolateral (serosal) and apical (mucosal)
surfaces on
opposite sides of the cell, hepatocytes are arranged in plates, such that both sides
are exposed to blood; the apical surface is restricted to minute canaliculi, the
smallest branches of the biliary tree. Canaliculi are too small (1 ym) for direct
sampling, which is one reason relatively little is known
about hepatocyte function,
compared with other epithelia (1).
The classical liver unit is the hepatic lobule, consisting of a region of hepatocytes
with a hepatic vein branch at the center and portal
tracts (branches of the portal
vein, hepatic artery, and bile ducts) at the periphery, in a more or less hexagonal
arrangement. It has been recognized
more recently, however, that the actual
functional unit of the liver is an acinus, first proposed by Rappaport
(3), which is
a 3-dimensional mass of hepatocytes surrounding a portal tract.
Blood flows
outward from the portal tract and empties into 2 or 3 terminal hepatic venules
(central veins). Bile flows opposite to blood, anastomosing
into larger and larger
ducts until it exits the liver via the common bile duct (1).
The spatial arrangement of hepatocytes produces a zonation of function. Those
hepatocytes closest to the afferent blood supply, termed zone 1 cells, receive blood
4
richer in oxygen, nutrients, and toxicants than cells in the periphery (zone 3 cells).
Though there are some actual zonal differences in hepatocyte function (e.g. bile
salt transport is predominant in periportal cells; zone 3 cells are primarily
responsible for biotransformations), retrograde infusions and zonal cell
destruction
have demonstrated that many (though not all) of these differences are not
absolute, but are rather a function of the particular location of the cell (1).
5
BILE FLOW
Bile serves two primary functions: 1) a secretory function,
which involves delivery
to the small intestine of bile salts to aid in fat digestion
and polymeric IgA to
protect the gut from infection, and 2) an excretory function involving the
removal
of endogenous and exogenous toxicants from the organism (4).
Loss of bile flow
(cholestasis) may have substantial pathophysiologic consequences.
Bile Components
Bile fluid is a complex mixture of organic anions, lipids,
electrolytes, and proteins.
The predominant organic anions are bile salts, which
are amphipathic, acidic
sterols that exist in bile as amino acid (e. g. taurine and
glycine) conjugates.
Inorganic electrolytes, present in concentrations similar
to plasma, include Na+
(the major cation), K +, Ca2+, HCO3 , Cl", and Mg2+. Most of
the proteins found
in
bile are serum proteins, though they exist at less than 0.2%
serum
concentrations (5).
Mechanisms of Bile Flow
Mechanisms underlying the formation and flow of bile are poorly understood (6).
The major driving force appears to be one of "osmotic filtration",
in which the
active transport of certain solutes (e.g. bile salts) into the canalicular
space
6
obligates water influx. The developing pressure head is relieved by passage down
the biliary tree (7,8). As bile salts tend to aggregate into micelles--and thereby lose
much of their osmotic activity--it is believed that osmotic obligation in bile is
primarily due to counterions, which passively follow the actively-secreted bile salts
(7,8).
Bile flow can be separated into 3 interdependent processes: 1) bile salt-dependent
flow (BSDF), which is a direct result of the concentrative secretion of bile salts
(and subsequent counterion influx); 2) canalicular bile salt-independent flow
(BSIF), which is due to transport of certain ions (not yet clearly identified); and
3) fluid reabsorption and secretion by bile ductules and ducts (7).
BSDF/BSIF
A correlation between bile salt concentration and bile flow has been demonstrated
in a number of species. Though this relationship is not entirely linear due to bile
salt aggregation, a correlative plot of bile flow vs. bile salt concentration can
nevertheless be obtained. In most species, however, extrapolation of this line to
zero bile acid concentration yields a positive y-intercept. This residual flow is
considered the bile salt independent fraction (9).
Though there is substantial evidence for the existence of BSIF (e.g. barbiturates
7
increase bile flow and erythritol clearance but not bile salt secretion
of bile salt-free bile
is choleretic), its
rates; infusion
overall significance and underlying
mechanisms are still highly speculative. Most studies suggest BSIF is probably
a
result of active secretion of certain ions directly into the
canaliculus (9), though
the identity of these ions is not yet established. Evidence has been presented
implicating Na, + bicarbonate, and glutathione (as well
as others). Evidence that
BSIF is mediated by sodium transport comes from studies correlating
changes in
BSIF and Na+,K+-ATPase activity (9). Thus, ethinyl estradiol
decreases BSIF and
Na+,1(+-ATPase activity and phenobarbital increases BSIF and Na+,K+-ATPase
activity.
Evidence for bicarbonate involvement includes the observation that
decreasing [bicarbonate] in the perfusate of isolated livers concomitantly decreases
BSIF by 50% (10) and, conversely, stimulating BSIF is
accompanied by increased
bile bicarbonate concentration
(11). A canalicular C1-/HCO3 antiporter has
been identified (12).
There is increasing evidence that secretion of glutathione
(gamma-L-glutamylcysteinyl glycine; GSH) is a major driving force for BSIF.
Studies have
demonstrated that: 1) GSH is the most abundant organic compound
in rat bile
(5,13); 2) biliary transport of GSH is carrier-mediated
(14); and 3) agents that
alter GSH secretion cause a parallel change in bile flow
(13).
8
Cytoskeletal Involvement in Bile Flow
The potential involvement of cytoskeletal elements (i.e. microtubules and
microfilaments) in bile flow is receiving increasing attention.
Cytoskeletal
elements are ubiquitous in eukaryotic cells. The functions of these elements, still
far from completely understood, include maintenance of cell shape, cell
movement, intracellular transport, and endo- and exocytosis (15). The hepatocyte
has an extensive network of microtubules, which may play a role in vectorial
transport; however, the exact nature of this role is controversial (see below).
Microfilaments have been identified adjacent to the sinusoidal and canalicular
membranes (16). Of particular significance is the "pericanalicular web" (17),
which surrounds the canaliculus and extends into microvilli and the junctional
complex. Though the role of microfilaments in bile flow is not yet established, it
is likely the pericanalicular web provides tone to the canaliculus, maintaining it
in a partially contracted state. Canalicular dilatation and loss of microvilli
associated with cholestasis may be due, in part, to damaged microfilaments
(18,19)(see below).
Phillips, et al (20,21) have used time lapse cinephoto-
micrography to record ordered canalicular contractions, which decrease with
microfilament inhibition. Bile salts increase the rate of these contractions (22).
The importance of this contractile activity is still speculative.
9
THE TRANSCELLULAR PATHWAY
Transcellular movement contributes significantly to the biliary secretion of a
number of substances (e. g. proteins, > 95%) and minimally to others (erythritol).
Some substances, such as sucrose, enter bile largely transcellularly
but have a
significant paracellular component as well (23,24).
Mechanisms of uptake, transcellular transport, and canalicular secretion of
bile
components are largely unknown.
mechanisms:
However, studies suggest at least three
1) receptor-mediated diffusional transport; 2) receptor-mediated
vesicular transport; and 3) non-receptor-mediated (fluid phase) vesicular
transport.
Diffusional Transport: Bile Salts
Bile salt secretion is a multistep process, involving return of bile salts from the
small intestine (enterohepatic circulation),
active uptake by hepatocytes,
transcytotic movement, and secretion into the canalicular space (25). Uptake at
the sinusoidal membrane, though not entirely understood, is the most well-
characterized of these processes. Uptake satisfies the criteria of a carriermediated process: it is saturable, sodium-dependent, and is subject to competitive
inhibition (4,7,9,26).
Photoaffinity probes have identified putative transport
proteins of 48 and 54(58) kD on the sinusoidal surface (4,27).
accomplished by "secondary active transport"; that
is,
Uptake is
an extracellular to
intracellular sodium gradient is maintained by a sinusoidal Na+,K+-ATPase
pump
10
and bile acid entry is coupled with sodium influx. Bile acids are bound to albumin
in the blood and there is some evidence that this protein plays a role in the
uptake process (the "albumin receptor theory") (9). However, this concept is still
speculative and is disputed.
In addition to the sodium-dependent system, which appears to be the more
important, there is evidence for a second, sodium-independent uptake system bile
acids may share with other anions such as BSP and bilirubin (see below). Uptake
of bile salts does not appear to be rate-limiting for transport, as the overall bile
salt excretion Vmax is much less than that of uptake (9).
Though uptake of bile salts has been fairly well-characterized, transport across the
cell and canalicular secretion have not.
Two mechanisms for transcellular
movement have been proposed: 1) diffusion, with the possible involvement of
binding proteins, and 2) vesicular movement (28). Evidence against a vesicular
pathway for bile salts comes from studies of excretion kinetics and vesicular
transport inhibition. Bile salts appear in bile within two minutes of infusion,
which is too rapid for vesicular transport (29).
Colchicine treatment, which
apparently inhibits vesicular transport, has no effect on bile salt secretion (30).
It thus appears that bile salts are transported across the cytosol as discrete
molecules. Transport may be facilitated by cytosolic binding proteins(4,9).
11
Canalicular secretion of bile salts is accomplished against a substantial
concentration gradient (0.2 mM intracellular vs 2mM extracellular). This
steep
gradient is partially--but apparently not totally--offset
by the membrane potential
difference (-40mV) and bile salt micelle formation
(the "micellar sink") (9).
Canalicular transport appears to be a sodium-independent,
saturable, carriermediated process (31) which is different from that of other organic anions
(7).
Less is known about the transport of non-bile salt organic
anions (bilirubin, BSP),
though there is some evidence that mechanisms similar
to bile salt transport are
involved (4,7,9,32,33).
Uptake is sodium-independent and may involve the
albumin receptor. A Cl- antiporter has been suggested
(4). Competitive uptake
among non-bile salt organic anions has been demonstrated
(33). Transport across
the cell is by diffusion and apparently involves
binding proteins. There is some
competition between these anions and bile salts for
uptake (34) and the overall
transport process (35).
Vesicular Transport: Proteins
Entry into bile of a number of proteins, including
horseradish peroxidase (HRP),
immunoglobulin A (IgA), insulin, epidermal growth
factor, asialoglycoproteins,
lipoproteins, and haptoglobin, has been studied (15).
Three routes of protein
entry have been identified: 1) sieving through tight
junctions, which is dependent
on molecular size (see below); 2) receptor-mediated
endocytosis; and 3) non-
12
receptor-mediated (fluid phase) endocytosis.
All eukaryotic cells ingest bits of their plasma membrane, forming vesicles
containing extracellular fluid and dissolved and membrane-bound
substances (4).
Cultured hepatocytes endocytose the equivalent of 20% of
their volume and 5
times their plasma membrane surface each hour (36). Formed vesicles,
on the
order of 1000 Angstroms in diameter, may 1) bypass
lysosomes and be delivered
directly to the biliary space, 2) be taken up by lysosomes and
degraded, or 3) be
returned to the plasma membrane (37). Most ( > 80%)
are returned; only 2%
reach bile (36). The latter vesicles either follow an "indirect" route, which involves
fusion with the Golgi, or a "direct" route, in which Golgi
do not appear to be
involved (38).
Receptor-mediated Endocytosis: IgA
IgA and a few other proteins (e.g. haptoglobin)
are transported via a receptormediated process and are found in bile at concentrations
greatly exceeding that
of plasma (39). IgA accounts for up to 40% of total
protein in rat bile (2) and is
actively transported for two apparent reasons: to serve as an immunoglobulin in
the gut where incoming food leaves the acidic environment
of the stomach, and
to remove antigens from the blood (5). Circulating IgA
(which, unlike most other
plasma proteins is not synthesized in the hepatocyte but in specialized plasma
cells) binds secretory component (the IgA receptor)
on the hepatocyte plasma
13
membrane; binding initiates endocytosis (4,40).
Transcellular movement of
labeled IgA has been visualized by autoradiography and takes 25-30 minutes (4).
Lysosomes do not appear to be involved (16,39).
Non-receptor-mediated (Fluid Phase) Endocytosis: HRP
HRP is a large (40,000 Mr) protein that undergoes the same type of vesicular
transport as many physiologic proteins (16)
and has been utilized fairly
extensively for this study. It is not clear if HRP uptake by the hepatocyte is
receptor-mediated or not (39). Various studies (7,38,39,41,42) have demonstrated
one or the other, or both. HRP may, in fact, be taken up by both mechanisms
(38), though non-receptor-mediated entry appears to predominate. HRP is bound
by some receptors (7).
Unlike IgA, most HRP taken up is transported to
lysosomes and degraded. A time lag before HRP appears in bile compared to
transcellular sucrose indicates that other compartments are interposed between
uptake and canalicular secretion (42). Canalicular secretion is probably via simple
exocytosis, though this has not been studied in detail.
The function of fluid phase endocytosis in hepatocytes is unclear.
Vesicles
containing HRP appear identical to those observed when no marker is present (5)
and following taurocholate infusion (43). Fluid phase endocytosis does not appear
to contribute significantly (6-8%) to biliary excretion of water and solutes or to
bile flow (37,44). As tight junctions prevent sinusoidal membrane components
14
from migrating to the apical membrane, it has been
suggested that supply of
plasma membrane and associated proteins to the biliary surface is the primary
reason for this transport. Such a mechanism has been identified in
epithelial cells
of the intestine (45).
Cytoskeletal Involvement in Transcellular Transport
There is substantial evidence implicating the involvement
of cytoskeletal elements
(microtubules and microfilaments) in transcellular
transport processes (4,46).
These conclusions are based primarily on observation
of transport changes
following cytoskeletal disruption.
Various studies have demonstrated potential
microtubule involvement in uptake
and/or transcellular movement of hexoses (47), lipids
(48), asialoglycoproteins
(49), amino acids (50), IgA (16,36,39,40,46), HRP
(32,39,40,41,51), insulin (36),
and fluorescein diacetate (32). Microtubules
appear to play only a minor role in
bile salt excretion, though overall transport
can be inhibited by high doses of the
microtubule inhibitor colchicine (16,52,53). The site of inhibition
may be uptake
(52). Microfilaments may also have some role (52).
Vesicular transport appears to be mediated by the
cytoskeleton. Microtubuleassociated proteins (MAPS) have been identified that may bind vesicles
to
microtubules (7). Colchicine has been shown to inhibit HRP endocytosis,
though
15
the results are contradictory (16). A decrease in the
number of HRP-containing
vesicles with coichicine treatment has been observed (16,41).
Colchicine inhibits
exocytosis of HRP into the canaliculus (32).
Lumicolchicine, which does not
affect microtubules, is not effective.
Both microtubules and microfilaments appear to play a role in vesicular
of IgA (40). Four basic steps are required for IgA transfer
of secretory component (the IgA receptor) from
transport
to bile: 1) movement
the Golgi apparatus to the plasma
membrane; 2) internalization (endocytosis) of bound IgA
and formation of the
endosomal compartment; 3) vesicular transport across the cell; 4) extrusion of
vesicular contents into the canalicular space. Two of
these processes--movement
of secretory component to the plasma membrane
and of IgA-containing vesicles
to the canaliculus--are inhibited by coichicine, indicating
microtubule involvement
(46). Endocytosis and canalicular secretion are not affected (36,46). Vinblastine,
which disrupts existing microtubules, also inhibits
IgA transport (40).
16
THE PARACELLULAR PATHWAY
The paracellular pathway is an important route for water and solute entry into bile
(54).
Permeating solutes not only include various ions (e.g. counterions for
BSDF), but relatively high molecular weight substances such as proteins, inulin,
and sucrose as well. Sieving through tight junctions may be the major route of
entry for most plasma proteins into bile (55).
Integral to paracellular processes is the junctional complex, composed of the
zonulae adherens, desmosomes, gap junctions, and the zonulae occludentes (ZO)
(56). The ZO, or "tight junction", which is the most apical (nearest the canalicular
space) of these structures, has been identified as the anatomical site where
penetration of the paracellular space is regulated (57).
Tight Junctions: Structure and Function
Structure of the tight junction is largely unknown. Freeze fracture replicas show
an anastomosing web of filamentous strands immediately adjacent to the apical
domain (58). Closer observation has revealed that these filaments are actually
strings of particles, apparently cross-linked with one another (56,59).
These
particles represent contact points between adjacent plasma membranes and have
been described as "kisses in the dark" (60). Monoclonal antibodies have identified
a 220 kD protein in this area ("Z0-1") but the exact function of this protein
is
17
unknown (57).
Epithelial tight junctions act as both a "gate" and a "fence"; that is, they allow free
movement of certain substances (such as Nat) but partially or totally restrict the
passage of others. Permeability is widely variable, depending on the needs of the
particular epithelium (57).
Studies indicate hepatocyte tight junctions are
intermediate between the "impermeable" tight junction, such as that of the
amphibian urinary bladder and skin, and "permeable", as that in the rat jejunum
and renal proximal tubule (54). Structurally, there appears to be a correlation
between the "tightness" (as measured by transepithelial electrical resistance) of
tight junctions and the number and depth of filaments (54,56,57). Boyer et al.
(56) identified a mean strand number of 4.1 in hepatocyte tight junctions, which
is intermediate between "leaky" tight junctions with 1 or 2 strands and "tight" with
10 or more. Induced changes in permeability of a single tissue are generally
reflected in a change in strand number also (56).
However, there is wide
variability in strand number within a tissue and even at specific sites. At least one
study (61) has demonstrated permeability changes without observable change in
strand count number, and the authors suggest that permeability may correlate
better with changes in strand conformation (e.g. loss of interstrand cross-linking,
dilatation of interstrand compartments) than actual strand number.
The ZO has two basic functions: 1) to restrict proteins (transporters, pumps, etc.)
18
to the apical or basolateral membrane, thereby maintaining the polarity required
for vectorial transepithelial transport; and 2) to act as a diffusion barrier, helping
to retain fluid composition differences (57,59). Immunohistochemical studies have
demonstrated that the boundary between the apical and basolateral membrane
proteins occurs at the ZO. Cell dissociation causes respective proteins to intermix
(62).
The hepatocyte ZO is a relative, rather than absolute, barrier (59). Evidence that
certain solutes enter bile through tight junctions generally comes from kinetics
studies, demonstrating biliary access of infused solutes too rapidly for transcellular
transport. Studies with HRP (39), inulin (44), and sucrose (63) demonstrate the
establishment of bile/plasma[perfusate] equilibria significantly prior to maximal
intracellular solute concentrations. Colchicine does not affect this access (39). ZO
permeability also appears to be dynamic (57), providing a means by which these
cells control the flow of water and solute between them (59).
Infusion of
dehydrocholate and taurocholate increased marker (ionic lanthanum) conductivity,
indicating that the hepatocyte junctional complex may respond to changing
osmotic gradients like other epithelia (54).
Certain hormones (vasopressin,
epinephrine, angiotensin II) increase permeability in a dose-dependent manner
(64). Effective hormones are those which act via alterations in intracellular
calcium levels. Tight junction integrity is dependent on calcium concentrations
(57).
19
Permeability of the ZO is charge and size selective. Discrimination based on
charge is not unique to the hepatocyte, having been documented in capillary
tissues, gallbladder epithelia, and rabbit ilea (cited by 65). The ZO is negativelycharged and cation/neutral selective. Hardison et al. (65) demonstrated this fairly
definitively in the hepatocyte by derivatizing HRP to strongly anionic and strongly
cationic isozymes and infusing them into perfused livers.
Anionic species
permeability was less than half that of neutral ions and cations. Similar effects
have been demonstrated with neutral methoxyinulin and an anionic derivative (33)
as well as others (7). This charge selectivity may serve to retard the efflux of bile
acids and other anionic solutes (e.g. xenobiotic conjugates) back across the tight
junctions once they have been deposited in bile (4,56).
Various studies have demonstrated tight junction selectivity based on molecular
size (53,66). Relative amounts of plasma proteins in human bile appear to be
consistent with this hypothesis (55). Aggregation of bile salts into micelles may
help retain them in the biliary tract (56).
The cytoskeleton appears to play an important role in the maintenance of tight
junction integrity and in junctional permeability changes. Evidence for this
involvement comes primarily from studies correlating permeability changes and
effects on cytoskeletal function.
Alteration of the cytoskeleton
is
often
20
accompanied by increased permeability, and, conversely, increasing permeability
generally alters cytoskeletal function (67). Cytochalasins (agents that disrupt
microfilaments) increase paracellular permeability in various epithelia (57).
Observed dynamic changes may be due to tensile forces from the cytoskeleton
(67). A band of actin and myosin wraps the apical side of cells below the ZO and
these filaments can be stimulated to contract (59).
junction structure and permeability (67).
Contraction alters tight
21
MECHANISMS OF CHOLESTASIS
As bile flow processes are poorly understood, it is not surprising that mechanisms
underlying loss of bile flow (cholestasis) are poorly understood as well. Numerous
potential mechanisms have been proposed (28), including:
1) poisoning of
metabolic processes (resulting in altered bile acid synthesis, bile acid transport,
and other energy-requiring activities); 2) alteration of sinusoidal and/or
canalicular membranes (which could adversely affect membrane components and
increase membrane permeability); and 3) disruption of cytoskeletal structure and
function (leading to increased paracellular permeability, decreased canalicular
contractility, and inhibited transcellular transport).
Poisoning of metabolic functions was implicated in early studies as a causative
factor in cholestasis. However, though bile flow is an energy-requiring process and
metabolic activities are integral to various aspects of bile flow (e.g. bile acid
synthesis), the fact that MFO inhibitors, uncouplers of oxidative phosphorylation,
and other metabolic poisons do not consistently induce cholestasis has led to a
fairly general consensus that observed metabolic changes may be secondary to the
initiating event. In general terms, cholestasis initiation is now believed to be most
likely a function of cell membrane and/or cytoskeletal alterations.
22
Alterations of the Cell Membrane: Ethinyl Estradiol
Cholestasis in late pregnancy and in some women taking oral contraceptives
stimulated interest in estrogens as cholestatic agents (68,69). Investigations have
focused on the synthetic estrogen, ethinyl estradiol (EE).
Various studies have shown that EE decreases bile flow (primarily BSIF) and
secretion of organic anions (68). Forker et al. (70) postulated that these changes
might be a function of increased paracellular permeability and subsequent reflux
of bile constituents. However, others have disputed this, demonstrating that bile
flow could be restored with a choleretic infusion (68). As documented with the
depot estrogen estradiol valerate, evidence has been presented that increased
permeability resulting from EE treatment, though it does occur, is a secondary
effect. It is now believed that the hepatotoxicity of EE is initiated by an increase
in cholesterol content of hepatocyte plasma membranes. The subsequent decrease
in fluidity adversely affects membrane proteins integral to enzymatic and transport
processes (25). Pretreatment with S-adenosyl-L-methionine, which reverses the
change in membrane fluidity, protects against EE-induced cholestasis (25).
Inhibited Na+,K+ -ATPase activity may be responsible for the observed decrease
in bile salt excretion and BSDF with EE (71). There is evidence that the change
in membrane fluidity with EE occurs primarily at the sinusoidal membrane;
however, changes in canalicular membrane fluidity, if they occur, may directly
affect canalicular transport of bile salts and anions involved in BSIF (72). Mg-
23
ATPase could also be inhibited. Though the role of this enzyme is poorly
understood, it may be important for microfilament function (73). Following bile
stasis, the increased concentration of bile salts could result in damage to tight
junctions and subsequent increased permeability.
Alterations of the Cytoskeleton: Phalloidin, the Cytochalasins, and Colchicine
The cytoskeleton appears to play an important role in various aspects of bile flow
(above). Cytoskeletal elements may be essential for transcellular and paracellular
functions. Evidence for this involvement derives, in part, from observed changes
following alteration of cytoskeletal elements.
Numerous studies have associated paracellular and transcellular changes with
cholestasis (18,25,52,56,63,68,74,75). However, the exact relationship between
these effects is not at all clear.
Microfilament dysfunction has been observed clinically in cholestatic patients
(76,77). The most obvious histologic change observed in these studies was a
thickening of the pericanalicular web and an increase in microfilament density
near the tight junctions of hepatocytes. Hyperplasia of actin filaments was also
observed in bile ductular cells. No change in microtubules was apparent. These
authors noted that the observed changes were similar in appearance to those seen
in rat hepatocytes exposed to phalloidin, a cyclic peptide from the mushroom
24
Amanita phalloides.
Phalloidin
Under normal conditions, actin exists in an equilibrium between filamentous (F)
actin (i.e. microfilaments) and globular (G) actin (78). It is believed phalloidin
binds F-actin and prevents its depolymerization, shifting the equilibrium in favor
of the filamentous form (78). However, densitometric tracings of sedimented
proteins show an increase in F-actin with little or no change in G-actin following
phalloidin treatment, indicating that synthesis of F-actin may also be increased
(78).
Chronic administration of phalloidin to rats results in a progressive hyperplasia of
microfilaments in the canalicular region (15,53). Canalicular dilatation and loss
of microvilli are also observed. Functionally, there is a steady increase in biliary
[14C]sucrose and [3H]inulin with phalloidin treatment (63,79,80), indicating
increased paracellular permeability. Decreased basal and bile salt-stimulated bile
flows are also observed (15,53,63,79). A number of attempts have been made to
correlate these changes. However, hyperplasia of actin filaments is generally
observed somewhat prior to the onset of cholestasis (15) and increased permea-
bility is a late event (79). Though this time course does not necessarily discount
a causal relation between increased microfilaments and cholestasis, the
permeability changes are very likely secondary events, as with EE.
25
The Cytochalasins
The cytochalasins are fungal alkaloids that bind actin and inhibit its
polymerization into microfilaments (18). Various studies have demonstrated that
cytochalasins decrease microfilament-mediated contractile activities of cells,
including clot retraction, pinocytosis and phagocytosis, axonal growth, and
secretion (cited by 18). In the hepatocyte, cytochalasin B (CB) treatment resulted
in detachment of microfilaments from the plasma membrane, dilatation of
canaliculi and loss of microvilli, decreased canalicular contraction, decreased
taurocholate uptake, decreased taurocholate and IgA transcellular transport, and
inhibition of tight junction formation (cited by 18). Any of these changes could
induce cholestasis.
Phillips et al. (21) have used isolated hepatocyte couplets, which retain their
polarity and form vesicular "canaliculi" in vitro, to elucidate the role of canalicular
contractility in bile flow. Using cinephotomicrography, they have demonstrated
apparent active contraction of these "canaliculi" and extrusion of vesicular
contents.
"Contractions" are inhibited by cytochalasin,
suggesting that
microfilaments may have a role in this activity. Though the mechanism of this
inhibition is unclear, canaliculi-enriched membrane fractions from CB-treated rats
revealed that actin filaments in this region had become detached. The authors
suggest that this detachment may prevent the contractions from occurring (21).
26
Kacich et al. (16) showed that cytochalasin D, which is apparently a more potent
inhibitor of microfilament formation than CB, caused a parallel decrease in
taurocholate secretion and bile flow. Taurocholate uptake did not appear to be
affected. Observed increased concentrations of HRP and other proteins were
attributed totally to the decreased bile flow; vesicular protein transport was not
inhibited.
Colchicine
Colchicine has been utilized extensively in the study of transcellular processes
(above). Reichen et al. (52) found that colchicine non-competitively inhibited
uptake of taurocholate by isolated hepatocytes. Others (25) have demonstrated
decreased bile salt secretion with colchicine treatment. Vesicle formation and
vesicular transport are also inhibited (16,41,46). Phillips et al. (60) demonstrated
that taurocholate-stimulated contractile activity was decreased following colchicine
treatment. The significance of these changes is not clear.
Most studies have found a slight, but usually not significant, decrease in basal bile
flow with colchicine treatment. However, though basal bile flow does not appear
to be affected, bile salt choleresis may be (60). The mechanism of this inhibition
is not known.
Though colchicine transiently increases permeability, few investigators have found
27
the change significant.
The notable exception is Bajwa and Fujimoto (51).
However, it is probable the retrograde infusion used in these studies caused
excessive biliary pressure and disruption of intercellular barriers
(54). Vesicular
material may be important for the formation and maintenance of tight junctions
(25); inhibition of vesicular transport by colchicine may make tight junctions less
resilient to biliary tree pressure changes.
Colchicine potentiated the cholestatic effect of phalloidin (79).
It has been
suggested that a major function of vesicular transport is to continuously supply
new materials (e.g. lipids, proteins) to the canalicular membrane (30).
Interruption of this supply by colchicine under cholestatic conditions could result
in membrane damage by increased concentrations of bile salts. Transport proteins
could also be affected, which would explain the decreased anion secretion
observed with colchicine treatment.
28
TOXICANTS: BCNU AND ANIT
BCNU
Numerous clinical and laboratory studies have shown that BCNU is a potent
antineoplastic agent, with significant activity against various cancers.
These
include: Hodgkins disease (82), malignant gliomas (83,84), malignant lymphomas
(85), disseminated malignant melanoma (86), and multiple myeloma (87). BCNU
has shown particular utility against CNS tumors due to its lipophilicity, which
allows it fairly unrestricted passage across the blood/brain barrier.
The biologic fate of BCNU is complex. Biotransformation is rapid. Intact drug
has a chemical half-life in man of five minutes and biological half-life of 15-20
minutes (88). 80% of labeled metabolites are recovered in the urine within 24
hours (89).
Microsomal enzymes appear to play some role in degradative
processes. Levin et al. (90) showed that phenobarbital pretreatment completely
eliminated the antitumor activity of BCNU, concluding that hepatic enzymes had
a significant role in the drug's metabolism. Nonenzymatic degradation is also
significant, however. Colvin (91) analyzed the chemical degradation of BCNU,
determining a chloroethyl carbonium ion is a major intermediate and the
alkylating species. An S-(2-chloroethyl)-glutathione metabolite has been identified
(92). The other major product, which may play a role in the compound's toxicity,
is chloroethylisocyanate (93). Hepatoxicity is not uncommon following BCNU
29
treatment in humans (82,94,95) and animals (96). Early work (97) showed
progressive histopathological alterations of the bile ductules and hepatic blood
vessels, with pericholangitis, increased fibroblastic activity, and bile duct
proliferation and necrosis. Functionally, these studies demonstrated a dosedependent BSP retention and prolongation of pentobarbital hypnosis followed by
hyperbilirubinemia.
Bilirubin was primarily of the conjugated form.
Serum
bilirubin continued to rise while BSP retention diminished, indicating that
hyperbilirubinemia could only partly be explained by impaired secretory capacity.
Minor increases in hepatic enzymes were also observed.
Hoyt et al. (35) demonstrated BCNU causes significant bile flow reduction and
BSP retention in intact rats. The BSP retention preceded cholestasis and was not
reversed up to 15 days posttreatment. Indocyanine green (ICG) excretion was also
impaired. As ICG excretion apparently does not involve metabolism (98), it was
concluded that a metabolic explanation (e.g. decreased conjugation) for this
dysfunction was not sufficient (99). This conclusion is supported by the finding
that it is primarily the conjugated form of bilirubin that is elevated in plasma with
BCNU treatment (97).
Bile salt secretion does not appear to be affected by BCNU treatment (35),
though results are conflicting (Krell and Larson, unpublished observations). Hoyt,
et al (35) has postulated that the bile salt independent fraction of bile flow is
30
preferentially affected by BCNU. It is provocative, in this regard, that BCNU
decreases glutathione content in bile (99), in light of the evidence for glutathione
involvement in BSIF (13).
Recent studies indicated BCNU increased hepatocyte tight junction permeability.
Krell and Larson (unpublished observations) observed a parallel increase in bile
to plasma sucrose concentration ratio and decreased bile flow in the isolated
perfused liver with BCNU treatment. Taurocholate secretory capacity was also
reduced. Kinetics analysis of [14C]sucrose bile efflux in the isolated liver revealed
the change in bile concentrations following omission of marker from the perfusate
could be fitted to a two-compartment model with a paracellular ("rapid phase")
pathway, and a transcellular ("slow phase") pathway (24). Using this model, these
authors concluded the paracellular pathway was being preferentially affected by
BCNU (i.e. hepatocyte tight junctions were being altered). These conclusions are
in conflict with those of Hoyt et al. (99). Though increased permeability was
suggested in the latter study as a possible explanation for the observed decrease
in GSH concentration, other results (e.g. bile-to-plasma osmolarity ratio >
1,
retained capacity to concentrate bile salts in bile) led these authors to conclude
that permeability changes were not resulting from BCNU treatment.
31
ANIT
The hepatotoxic profile of ANIT is remarkably similar to that of BCNU. Becker
and Plaa (100,101) demonstrated that mice exposed to ANIT (150 mg/kg)
developed cirrhotic changes, bile duct hyperplasia, hyperbilirubinemia, and
cholestasis. The hyperbilirubinemia was observed as early as 10 minutes following
administration, with the predominant species conjugated.
Significant BSP
retention was seen by 180 minutes. Prolongation of pentobarbital hypnosis was
also observed. Cholestasis was significant at 6 hours. Some of these effects were
persistent, lasting up to a month after a single dose.
Later studies in the rat revealed similar changes (69,102).
Onset of
hyperbilirubinemia occurred between 12 and 24 hours posttreatment, maximized
at 5 days, but declined to normal by 7 days (69). The hyperbilirubinemia was
attributed in part to increased synthesis; however, it was concluded that uptake
and/or excretory processes were also being affected. ANIT was also shown to
significantly decrease BSP excretion. This effect was obvious as early as 3 or 4
hours after treatment. Decreased bile flow was not significant until 16-24 hours
posttreatment.
Recent isolated liver work by Krell et al. (74,75) on the development of cholestasis
following ANIT treatment has shown a temporal correlation between decreased
BSP
and
taurocholate
secretion
and
increased
equilibrium
perfusate
32
concentrations of these solutes. Basal and taurocholate-stimulated bile flows were
significantly reduced.
Use of labeled markers showed a correlation between
changes in BSP and taurocholate equilibrium concentrations and increased
permeability of the bile/perfusate barrier. Freeze fracture replicas of hepatocyte
tight junctions showed decreased strand number and disrupted continuity following
ANIT treatment (75). The authors feel these changes are similar to those
observed following bile duct ligation, which is in conflict with the conclusions of
Becker and Plaa (101).
A number of other studies have analyzed the permeability changes induced by
ANIT. Kan et al. (66) measured a peak permeability to proteins 10-12 hours after
ANIT treatment, and an inverse relation between biliary access and protein
molecular weight (insulin > HRP = ovalbumin > pig gamma globulin). Bile flow
was not significantly reduced until 14 hours after treatment. These authors point
out that measured permeability changes coincide with the hyperbilirubinemia
observed with ANIT treatment and suggest that this dysfunction may be due in
part to paracellular reflux. Pretreatment with phenobarbital indicated that a
metabolite of ANIT was responsible for the permeability changes.
Similarities between the hepatotoxic effects of BCNU and ANIT were recognized
in early studies. Thompson and Larson (97) noted that, although there were
marked differences in time course, the functional and histological changes effected
33
by these compounds were generally similar.
Because of this similarity, they
speculated that the moiety responsible for the hepatotoxicity of BCNU could be
the isocyanate.
Isocyanates carbamylate proteins (92,103,104,105). The inactivation by BCNU of
glutathione reductase, alcohol dehydrogenase, and transglutaminase (cited by 92)
is likely due to carbamylation by the chloroethylisocyanate intermediate. Studies
on the effect upon tubulin polymerization of several 2-chloroethyl nitrosoureas
(106) revealed that inhibition relative to isocyanate yield was stoichiometric.
Inhibition by BCNU was dose-dependent.
Effects of a number of other agents (e.g. phalloidin, colchicine, the cytochalasins)
on paracellular permeability and/or transcellular transport have been attributed
to disruption of elements of the cytoskeleton. It is possible that the changes
induced by BCNU and ANIT are, at least in part, mediated by carbamylation, and
consequent deactivation, of cytoskeletal elements also.
34
II. GENERAL METHODS
A perfused liver system was used for many of these experiments. Liver perfusion
offers numerous advantages over the whole animal in the study of liver function.
Primarily, it allows for the analysis of liver-only functions, free from other-organ,
nerve, and hormonal influences. Variables that may be important in whole animal
studies, such as circadian rhythm changes and ductular bile modification, are not
significant when the liver is perfused (4,74,107).
A particular advantage of the perfused liver in kinetic studies is that, under single
pass conditions, paracellular (rapid phase) and transcellular (slow phase) processes
of bile entry can be discriminated. Markers used for analysis of slow and rapid
phase transport processes often enter bile by both routes.
An example is
[14C]sucrose, which is frequently used as a marker of increased paracellular
permeability. This use was questioned by some investigators when infused sucrose
was identified within vesicles (108) and was therefore believed to have a
transcellular component (42). Jaeschke et al. (24) used the isolated liver to
quantify paracellular and transcellular contributions to the total biliary clearance
of sucrose, demonstrating that the transcellular route contributes approximately
18% to the total clearance. Similar studies have been conducted with HRP, which
moves primarily transcellularly but has a paracellular component as well (39).
A favorable comparison of liver function parameters has been made among the
35
hemoglobin-free perfused liver, livers perfused with erythrocyte-containing media,
and the intact animal (107). Hemoglobin-free perfusion has the added
advantages
of lowered viscosity (and therefore less chance of altered flow distribution) and
lack of interference from red cell metabolism.
The studies presented here have utilized an in situ perfused liver system. The in
situ system has two advantages over the isolated organ: 1) the liver remains in
its
anatomical position and therefore does not suffer the trauma of removal; and 2)
perfusions can be accomplished much more rapidly and efficiently. In situ systems
have been used elsewhere (18, 64, 66).
Chemicals
BCNU was obtained as a gift from Bristol Laboratories, Evansville, IN.
Triamcinolone (Kenalog-40) was purchased from E. R. Squibb and Sons, Inc.
(Princeton, NJ), esculetin (6,7-dihydroxycoumarin) from Biomol Research Lab,
Inc. (Plymouth Meeting., PA), and indomethacin from Merck and Co., Inc.
(Rahway, N.J.).
(Rockville, MD).
Cacodylate was obtained from Touisimis Research Corp.
ANIT, horseradish peroxidase, lactate dehydrogenase,
colchicine, and lanthanum were purchased from Sigma Chemical Co. (St.
Louis,
Missouri). All chemicals were of the highest reagent grade available
and were
used without further purification.
36
Treatment of Animals and Liver Perfusion
Male Sprague-Dawley rats (250-350 g) were used throughout. The animals were
housed in a constant-temperature (21-22 °C), 12 hr. light/dark cycle environment
and given free access to a standard laboratory diet (Wayne Rodent Blox). Unless
otherwise indicated, animal treatment was as follows: a) BCNU was dissolved in
corn oil (26 mg /ml) and injected i.p. (1.0 ml/kg body wt.) 24, 36, 48, 72, 96, or 192
hours prior to experimental manipulations; b) ANIT, suspended in corn oil (125
mg/ml), was administered intragastrically (2.0 ml/kg) under light ether anesthesia
12, 24, 36, or 48 hours before manipulations; c) colchicine was dissolved in normal
saline (10 mg /ml) and injected i.p. (1.0 ml/kg) 2 1/2 hours before manipulations;
d) phenobarbital sodium was dissolved in normal saline (80 mg/ml) and injected
i.p. (1.0 ml /kg /day) for three days prior to BCNU or ANIT treatment; e)
triamcinolone was dissolved in normal saline (2.0 mg/ml) and injected i.p. (1.0
ml/kg) 24 hours before and after BCNU treatment or 24 hours before and 12
hours after ANIT treatment; f) esculetin, dissolved in 0.1 M phosphate buffer, pH
8.5, (0.6 mg/ml), was injected i.p. (2.0 ml/kg) 1/2 hour before and at 6-hour
intervals after ANIT or BCNU treatment; g) indomethacin was dissolved in corn
oil (5 mg/ml) and given i.p. (1.0 ml/kg) one hour before and at 8-hour intervals
after ANIT or BCNU treatment. Controls were treated similarly with the
respective vehicle.
Liver perfusion. Animals were anesthetized with sodium pentobarbital (60-80
37
mg/kg, i.p.) and the bile duct cannulated with PE 10 tubing (Clay Adams,
Parsippany, N.J.) inserted to a point just distal to the liver hilus. A single, 10-
minute in vivo bile sample was taken at this time for inorganic phosphate
determinations. The portal vein was then catheterized with a 16-gauge needle and
the liver perfused in situ with hemoglobin- and albumin-free Krebs-Henseleit
bicarbonate buffer, pH 7.4, containing 117.6 mM NaC1, 5.4 mM KCI, .57 mM
MgSO4, 2.5 mM CaC12, 1.2 Mm NaH,PO4, 25.0 mM NaHCO3, and 11.1 mM
glucose. The perfusion medium was aerated with 0,/CO2 (19:1) and the
temperature maintained at 37 ± .05 °C. The medium was pumped through the
liver at a constant rate of 22-24 ml/min with a Gilson Minipuls 2 peristaltic pump
and could be switched between open (single pass) perfusion or recirculation.
Effluent LDH activity, 02 consumption, and perfusion pressure were monitored
to assure sustained liver viability (Table 1). Cumulative LDH release, 0, uptake,
and net portal perfusion pressure were in agreement with accepted viability
criteria (107). No significant difference in 02 uptake or perfusion pressure was
observed between treated and control animals.
A significant increase in
cumulative LDH release was observed with BCNU treatment; however, after 60
minutes perfusate LDH activity was less than 2% total liver LDH, which is within
acceptable range.
Bile flow was determined gravimetrically, assuming a bile density of 1.0 g/ml, and
expressed as ,u1/min/g liver. The in vivo bile flows are the initial 10 minute flows
38
Table 1. Perfused liver viability criteria for control and BCNU-treated
rats.
TREATMENT
CONTROL
BCNU
oxygen consumption
(Amol/min/g liver)
1.91 + 0.04
2.15 ± 0.1
perfusion pressure
4.5
5.0
+ 0.5
± 1.4
(cm H2O)
LDH releases
(U/hr/g liver)
2.15 + 0.04b
9.05 + 1.6bid
Values are means + SE; n = 3. aRelease rate at the end of the experimental
period (60 minutes after start of perfusion) in a recirculating system. For total
liver LDH: livers were minced and homogenized in 2 volumes cold phosphatebuffered saline (PBS), pH 7.4, and centrifuged for 10 minutes at 15,000 x g; the
supernatant was diluted 1000x in cold PBS for assays. '0.34% total liver LDH.
`1.47o total liver LDH. dSignificantly different from control, P < 0.05.
39
collected immediately upon cannulation of the bile duct. Isolated liver bile flows
are basal flows, taken at least 25 minutes after cannulation (Appendix Figure 1).
Bile flow is expressed in terms of liver mass as there was substantial loss of body
weight (due to transient anorexia) following BCNU or ANIT treatment (Appendix
Figure 2).
Statistical analysis: Results are expressed as means ± SE. Statistical significance
was estimated using Student's t-test, P < 0.05 being considered significant.
40
III. CHOLESTATIC EFFECTS OF BCNU AND ANIT
Cholestasis following BCNU or ANIT treatment has been previously reported
(35,74,97). The effects of BCNU and ANIT treatment on bile flow in the present
studies are shown in Figures 2 and 3. In vivo bile flow had decreased significantly
24 hours after BCNU treatment (1.48 ± .15 ,ul /min /g liver compared with 1.82
± .04 ,u1/min/g liver for controls). In vivo bile flow had further decreased 48
hours after BCNU treatment (.98 + .10 /21/min/g liver) but then remained
essentially unchanged through 96 hours (1.11 + .12 and .98 + .06 /21/min/g liver
for 72 and 96 hours posttreatment, respectively). In contrast, bile flow in the
perfused liver (i.e. BSIF), though significantly decreased 48 hours after treatment
(.51 ± .05 compared with .97 ± .05 ,u1/min/g liver for controls) was normal at 24,
72 and 96 hours. A dose-dependent increase in plasma bilirubin was observed
following BCNU treatment (Table 2).
In the ANIT-treated rats (Figure 3), bile flow was normal 12 hours after treatment
but was significantly decreased at 24 hours (.58 + .12 ,ul /min /g liver in vivo and
.22 ± .06 ul /min /g liver in the perfused liver), continuing to decline to near zero
at 36 hours (.15 ± .003 and .13 + .02 ul/min/g liver for in vivo and perfused liver
flows, respectively). No bile flow was detectable 48 hours after ANIT treatment.
These results are generally in agreement with those of other investigators. Hoyt
41
0
24
48
72
96
120
TIME (HR)
Figure 2. Change in bile flow with time following BCNU treatment. In vivo and
perfused liver bile flows were measured 24, 48, 72, or 96 hours after BCNU
treatment (26 mg/kg, i.p.). Bile flow was determined gravimetrically, assuming 1
g/ml. Values are means ± SE; n = 10-17. *Significantly different from control,
P < 0.05.
42
Table 2.
Bile and plasma bilirubin, 48 hours after 26 and 34 mg/kg BCNU.
TREATMENT
BILIRUBIN
BILE (AM)
PLASMA (mg%)
CONTROL
200
+
11
BCNU(26)
206
+
51
.78
+ .08a
BCNU(34)
134
+
58
1.20
+ .16b
ND
Values are means + SE; n = 3-5. '20% conjugated. b29% conjugated. ND: not
detectable.
43
2.5
--..
L...
>1)
;)-0 IN VIVO
o
2.0
PERF LIVER
al
c
o_J
1.5
1.0
Li_
T
0
w 0.5
*
cTo
0.0
0
I
I
12
24
*
1
*
36
48
TIME (HR)
Figure 3. Change in bile flow with time following ANIT treatment. In vivo and
perfused liver bile flows were measured 12, 24, 36, or 48 hours after ANIT
treatment (250 mg/kg, gavage). Bile flow was determined gravimetrically,
assuming 1 g/ml. Values are means ± SE; n = 3-15. *Significantly different from
control, P < 0.05.
44
et al. (35,99) found a significant decrease in bile flow in vivo 48 and 96 hours after
BCNU treatment. Krell and Larson (unpublished observations) measured a
decrease in bile flow in the perfused liver 48 hours after BCNU treatment;
however, bile flows at later time points were not measured in that study. It is
noteworthy in the present work that bile flow in the perfused liver, though also
significantly depressed at 48 hours, was not different from controls at the 24, 72,
and 96 hour time points. Though the significance of this surprising finding is not
clear, it is possible that the perfusion fluid was supplying a component necessary
for bile flow that was not available in the intact animal. However, it is also
possible that this reversal is occurring in vivo as well but is being masked by a
continued decrease in BSDF (that is, BSDF is continuing to decrease while BSIF
returns to normal; thus, net flow doesn't change).
Hoyt et al. (35) concluded that the bile salt-independent fraction (BSIF) of bile
flow is being preferentially affected by BCNU. There is increasing evidence that
glutathione secretion has an important role in BSIF (above). Hoyt et al. (99)
measured glutathione content in liver and bile after BCNU treatment and found
a significant reduction of bile glutathione at 48 but not 72 hours after treatment,
speculating that the decrease at 48 hours could be due to either decreased
canalicular secretion or increased biliary permeability. As the time course of
BCNU-induced biliary [glutathione] changes correlates with BSIF cholestasis and
its reversal measured here, it is possible that there is a causal relation between
45
these effects (i.e. decreased bile glutathione is resulting
directly in the bile flow
decrease). Though glutathione excretion was not measured in the present studies,
it is provocative that paracellular permeability
changes, as reflected by bile
inorganic phosphate levels, show a similar time course as the reported changes
in bile glutathione (see below).
46
IV. INCREASED PARACELLULAR PERMEABILITY WITH BCNU AND ANIT
Introduction
Numerous substances have been used as markers in the study of bile flow and
other hepatic functions. The inert solutes erythritol and mannitol, having small
enough radii to pass freely through pores in hepatocyte plasma membranes and
thus diffuse passively with water movement (9),
are commonly used for
distinguishing the bile salt-dependent and bile salt-independent fractions of bile
flow.
Though there are some difficulties associated with the quantitative
interpretation of results obtained with these markers, they can at least provide
qualitative information.
Studies of changes in paracellular functions use probes that are large enough to
be restricted from passive transcellular movement (109). Two markers that have
been used fairly extensively for this purpose are sucrose and inulin, with normal
bile to plasma (B/P) ratios in the range of .2 and .06, respectively (107). Under
conditions of increased permeability, B/P ratios approach 1, indicating that
restriction to the plasma compartment is being compromised. As with erythritol
and mannitol, there are problems associated with the use of these markers.
Transcellular transport may contribute significantly to bile concentrations (24).
Also, bile concentrations tend to increase subsequent to cholestasis (110).
47
However, if such limitations are taken into account (e.g. by monitoring kinetics
and correcting for bile flow), these markers can still have some utility (24).
Three permeability markers were used in the present studies: horseradish
peroxidase (HRP), inorganic phosphate (P,), and ionic lanthanum.
HRP has been used extensively as a marker of transcellular and paracellular
functions and dysfunctions (38,39,41,51,66). In control livers, most ( > 80%) of
HRP endocytosed is returned to plasma/perfusate. Virtually all the rest is either
degraded or moved across the cell to bile (above); very little is sieved through
tight junctions under control conditions. However, when junctional permeability
is increased, paracellular movement of HRP increases significantly (39).
HRP is a particularly useful marker in the perfused liver. Though recirculating
HRP can blur the transcellular and paracellular components of bile entry in the
intact animal, in the single pass perfused liver these pathways can be distinguished
(below).
Inorganic phosphate (P,), though it has several advantages over other permeability
markers, has had only limited use (74,110,111,112).
The fact that P is an
endogenous substance (rat serum concentration is approximately 2.5 mM; 111) not
only simplifies experimental procedures but also assures that B/P ratios are at
48
equilibrium.
Distribution kinetics are not a factor (74).
Due in part to its
negative charge, P; is greatly excluded from bile (74), with normal B/P ratios in
the range of .01, which is at least an order of magnitude less than that of sucrose.
Because of this great difference in concentration, and the fact that P, is small, very
subtle permeability changes can be detected (112). Though it is feasible other
factors could be contributing to elevated bile P close correlations between bile
P, and infused [14C]sucrose (74,110), [32P]phosphate (74), and HRP (below)
provide evidence that the observed increase in P, is due to leakage across tight
junctions.
A major difficulty with the use of most markers for monitoring permeability
change is that increased bile concentrations alone do not provide conclusive
evidence that penetration is occurring at the level of the tight junction and not
farther down the biliary tree. Visualization of penetration with an electron dense
marker such as lanthanum provides a means by with this question can be
definitively addressed.
Ionic and colloidal lanthanum have been used to visualize permeability changes
in a number of different tissues, including the liver, gut, kidney and skin
(54,63,113,114,115).
In the liver, lanthanum is completely excluded by tight
junctions of control rats but penetrates freely under conditions of increased
permeability. In the studies presented here, electron microscopic visualization of
49
lanthanum penetration provided morphological evidence of measured permeability
changes.
Methods
HRP Excretion in vivo and in the Perfused liver. For in vivo studies, anesthetized
rats were minimally opened 24, 48, 72, 96, and 192 hours after BCNU treatment
and HRP (25 mg in 1.0 ml saline) was introduced as a bolus directly into the
inferior vena cava. Bile was then collected on ice in pretared tubes at t = 5, 10,
20, 30, 40, and 50 minutes.
An open (non-recirculating) system was used for HRP excretion experiments in
the perfused liver. Following liver isolation, 25 mg HRP in 1.0 ml saline was
infused over a period of one minute. Bile was then collected on ice at 5-minute
intervals for 60 minutes.
HRP activity was determined spectrophotometrically according to an established
method. Bile samples (50 ,u1) were added to a reaction cuvette containing
hydrogen peroxide (7.8mM) and pyrogallol (1.5 mM) in water. Cuvettes were
mixed by inversion and the rate of decomposition of H202 by peroxidase was
determined by monitoring the change in absorbance at 420 nm.
One unit of
activity was taken to be equivalent to a change of one absorbance unit/minute.
50
Activity was corrected for bile flow.
Inorganic Phosphate Excretion in vivo. P, concentrations in bile were determined
24, 48, 72, 96, and 192 hours after 26 mg/kg BCNU, 24, 48, and
96 hours after 34
mg/kg BCNU, or 12, 24, 36, and 48 hours after 250 mg/kg ANIT (see General
Methods).
Inorganic phosphate concentration was determined by a modified Penney
method
(116). 190 ,u1 precipitating reagent (12.5% trichloroacetic acid in
1.25 N HCl)
were added to 10µl bile in a microcentrifuge tube and the tubes spun at 15,000
x g for 2 minutes. 150 Ail of the supernatant were added to a cuvette containing
1.08 ml HC1-molybdate (equal volumes 2.5 N HC1
and 107 mM sodium
molybdate), 30 ul 1.36 mM malachite green oxalate, and 300 ,u1 H2O. Cuvettes
were mixed by inversion and the absorbance at 650 nm recorded.
Lanthanum perfusion. Lanthanum perfusion and perfusion fixation were carried
out after Layden et al. (54). Livers were perfused at 15 cm H,0 pressure with a
5 mM tris-buffered balanced salt solution (305 mOsm/L, pH
7.4) containing 5 mM
lanthanum chloride. After 21/2 minutes the livers were perfusion-fixed with 25 ml
2.5% glutaraldehyde/0.1 M cacodylate buffer, sectioned, and diced into 1 mm3
cubes. Tissues were then loaded onto an automated tissue processor where they
were washed in cacodylate buffer and postfixed in 1.0% osmium tetroxide
for one
51
hour.
Tissues were then rinsed, dehydrated through graded acetone, and
embedded in Medcast-Araldite 502 resin and polymerized at 60 °C for 24 hours.
Semithin sections were stained with methylene blue/azure II/basic fuchsin (117).
Ultrathin sections were cut on a Sorvall MT-5000 Ultramicrotome and examined
(unstained) with a Zeiss EM 10/A transmission electron microscope at an
accelerating voltage of 60 kV.
Results
HRP Excretion in vivo. The time course of HRP penetration into bile in vivo with
BCNU treatment is shown in Figure 4. Recorded values are maximal HRP
activities, which were observed in the 10 minute samples (below). HRP was
negligible in bile from control animals (average: 3.6 U/min) and animals
evaluated 24 hours after BCNU treatment (6.48 ± 2.29 U/min). However, 48
hours after treatment HRP activity had greatly increased (149.75 + 10.62 U/min).
Peak activity was followed by a sharp decline, then remained essentially
unchanged though 96 hours.
HRP Excretion Kinetics in vivo and in the Perfused Liver.
In vivo HRP
permeability kinetics at 48 and 72 hours after BCNU treatment in presented in
Figure 5. Maximal activity was measured in the 10 minute samples at both time
points. Recirculation of HRP in the intact animal precluded the isolation of
52
200
150
1 00
C.)
a_
50
0
0
24
48
72
96
120
144
168
192
TIME (HR)
Figure 4. Time course of horseradish peroxidase (HRP) penetration into bile in
vivo with BCNU treatment. HRP (25 mg in 1.0 ml normal saline) was introduced
into the inferior vena cava of minimally-opened rats 24, 48, 72, 96, or 192 hours
after BCNU (26 mg/kg, i.p.) or corn oil (1.0 ml/kg) treatment. Bile was then
collected on ice in pretared tubes and assayed for HRP as described. Shown are
maximal activities, which were observed in the 5-10 minute samples. Values are
means ± SE; n = 3-6. *Significantly different from control, P < 0.05.
53
200
z 150
D
>
100
17-:
CD
<
cL
50
=
0
0
10
20
30
40
50
60
TIME (MIN)
Figure 5. HRP excretion kinetics in vivo with BCNU treatment. HRP (25 mg in
1.0 ml normal saline) was introduced into the inferior vena cava of minimallyopened rats 48 or 72 hours after treatment with BCNU (26 mg/kg, i.p.) or corn
oil (1.0 ml/kg). Bile was then collected on ice in pretared tubes at the indicated
times and assayed for HRP as described. Values are means ± SE; n = 5-12.
*Significantly different from control, P < 0.05.
54
paracellular and transcellular phases of bile entry. This obstacle was overcome
in the perfused liver.
Kinetics of HRP appearance in bile in perfused livers following BCNU and
colchicine treatment is shown in Figures 6 and 7. HRP activity was detected in
the initial (0-5 minute) bile samples of control livers (Figure 6). However, peak
activity did not occur until the 20-25 minute sample, consistent with transcellular
movement of HRP. Livers isolated 48 hours after BCNU treatment showed a
biphasic excretion (Figure 7) with maximal activity (approximately 15x controls)
in the first sample, followed by a rapid decline (Figure 6). Maximal activity in the
0-5 minute sample was also observed after colchicine treatment, though the
increase was not significant. No second peak was evident following either BCNU
or colchicine treatment.
HRP Excretion Following ANIT Treatment. Numerous attempts were made to
analyze, as a positive control, HRP excretion kinetics following ANIT treatment.
However, out of approximately 25 rats attempted, only 2 had enough sustained
bile flow for this analysis. (The observed pattern of excretion in these 2 rats was
similar to that following BCNU treatment; Appendix Figure 3). Other studies
(39,66) that have demonstrated HRP permeability with ANIT treatment have used
Wistar rats, initiating perfusion approximately 12 hours after ANIT treatment (the
period of maximal permeability in these animals). A comparative study in the
55
0.5
2
0-0 CONTROL
0.4
BCNU
- COLCHICINE
1
0.3
0.2
0.1
T/c2
T
O
*-
o.o
ce)
0
10
20
30
40
50
60
TIME (MIN)
Figure 6. HRP excretion in the single-pass perfused liver with BCNU and
colchicine treatment. Livers were perfused 48 hours after BCNU treatment (26
mg/kg, i.p.) or 2 1/2 hours after colchicine treatment (10 mg/kg, i.p.). 10 minutes
after start of the perfusion, HRP (25 mg in normal saline) was added to the
influent line over a period of one minute. Bile was then collected on ice in
pretared tubes at 5-minute intervals and assayed for HRP as described. Values
are means ± SE; n = 3-6. 'Significantly different from control, P < 0.05.
56
0.5
0.4
0.3
0.20.1
0.0
i
0
10
20
.---ir---.--lir*--11---40--30
40
50
60
TIME (MIN)
Figure 7. Biphasic kinetics of HRP excretion in the single-pass perfused liver
with BCNU treatment. Livers were perfused 48 hours after BCNU treatment (26
mg/kg, i.p.). 10 minutes after start of the perfusion, HRP (25 mg in normal
saline) was added to the influent line over a period of one minute. Bile was then
collected on ice in pretared tubes and assayed for HRP as described. Values are
means; n = 3-6.
57
present investigation revealed a marked difference in time course of permeability
increase between Wistar and Sprague-Dawley rats. Sprague-Dawley rats were
found to have negligible permeability increase at 12 hours; maximum permeability
did not occur until 24 hours after treatment, when bile flow was substantially
reduced (Appendix Figure 4).
Increased bile Pi with BCNU and ANIT Treatment. The increase in bile P, with
BCNU treatment was dose related (r = .99) (Figure 6). A close correlation (r =
.93) was observed between P, and HRP activity with BCNU treatment (Figure 9).
The time course of increased P, in bile with BCNU and ANIT treatment is shown
in Figures 10 and 11. Very low P, concentrations were observed in control bile
(.17 + .02 mM) and in bile 24 hours after BCNU treatment (.35 + .06 mM) and
12 hours after ANIT treatment (.31 ± .09 mM). Bile P, maxima in treated rats,
observed 48 hours after BCNU treatment (1.52 ± .03 mM) and 24 hours after
ANIT treatment (1.37 + .05 mM), were followed by a significant decline (.88 +
.08 mM and .62 + .05 mM 72 and 96 hours after BCNU treatment, respectively,
and .76 ± .09 mM 36 hours after ANIT treatment). Complete bile stasis
precluded measurement of bile P, 48 hours after ANIT treatment. Rats treated
with 34 mg/kg BCNU showed a similar time course of P, increase in bile as rats
receiving 26 mg/kg (Figure 12), but had a greater maximum at 48 hours (2.16 +
58
2.5
0.5
1.10
1.35
1.60
LOG DOSE (mg/kg)
Figure 8. Dose-response relation of bile inorganic phosphate (P) and BCNU.
Bile was collected 48 hours after BCNU treatment (15, 20, or 34 mg/kg, i.p.) and
assayed for P, as described. A close correlation (r = .99) between BCNU dose
and bile Pi was observed. Values are means ± SE; n = 4-6.
59
2.0
1-1-)
_1
olose
05
0.0
0
50
100
150
200
HRP ACTIVITY (U/min)
Figure 9. Correlation between bile Pi and bile HRP following BCNU treatment.
Bile was collected 48 hours after BCNU treatment and assayed for P, or HRP as
described. A close correlation (r = .93) between bile Pi and bile HRP was
observed. Values are from individual rats; n = 28.
60
2.0
0
0 CONTROL
- BCNU
*
O
0
0.0
0
24
48
72
96
120
144
168
192
TIME (HR)
Figure 10. Time course of Pi penetration into bile following BCNU treatment.
Bile was collected 24, 36, 48, 72, 96, or 192 hours after treatment with BCNU (26
mg/kg, i.p.) or corn oil (1.0 ml/kg) and assayed for Pi as described. Values are
means ± SE; n = 3-10. 'Significantly different from control, P < 0.05.
61
2.0
0
N
1.5
E
1.0
T
.1.
--I
0.5
CD
0
0.0
0
12
24
36
48
TIME (HR)
Figure 11. Lack of correlation between change in bile flow and bile Pi with time
following ANIT treatment. Bile was collected 12, 24, or 36 hours after ANIT
treatment and assayed for P, as described. In vivo bile flows are shown. No
correlation between bile flows and bile P, was observed. Values are means ± SE;
n = 3-15. 'Significantly different from control, P < 0.05.
62
2.5
0-0 CONTROL
- 26 mg/kg
- 34 mg/kg
2.0
1.51.0
0.5
0
0
0.0
0
24
48
72
96
120
TIME (HR)
Figure 12. Time course of P1 penetration into bile following BCNU treatment, 2
doses. Bile was collected 24, 36, 48, or 96 hours after treatment with BCNU (26
or 34 mg/kg, i.p.) or corn oil (1.0 ml/kg) and assayed for P, as described. A
similar time course with a higher peak value at 48 hours was observed with the
higher BCNU dose. Values are means + SE; n = 3-9. `Significantly different
from control, P < 0.05.
63
.10 mM).
Lanthanum-perfused livers. Increased paracellular permeability with BCNU and
ANIT treatment was confirmed with electron microscopic examination of
lanthanum-perfused livers. In controls, lanthanum aggregated along sinusoidal
membranes and in the intercellular spaces but did not penetrate the junctional
complexes (Figure 13A). However, livers isolated from BCNU-treated (Figure
13B) and ANIT-treated (Figure 13C) rats showed significant lanthanum
penetration of junctional areas and deposition in canaliculi.
In no case was
lanthanum observed in hepatocytes, interstitium, or bile ducts.
Discussion
These results provide strong evidence that BCNU increases paracellular
permeability in rat livers. As indicated, three general conditions should be met
to demonstrate increased hepatocyte junctional permeability.
First, the
permeability marker used must be at equilibrium between plasma (perfusate) and
bile.
This was accomplished here with the endogenous marker Pi.
Second,
increased paracellular movement should be distinguished from possible increased
transcellular transport, which has been documented (51). This was accomplished
in the present studies by evaluating HRP excretion kinetics in the isolated liver,
64
Figure 13. Lanthanum penetration of junctional complexes. Rats were treated
with corn oil (1.0 ml/kg), BCNU (26 mg/kg), or ANIT (250mg/kg). Livers were
perfused with lanthanum chloride 48 hours after BCNU treatment or 12 hours
after ANIT treatment, perfusion-fixed, and prepared for electron microscopy as
described. (A) Control liver. Lanthanum has entered the intercellular spaces but
has not penetrated the tight junctions (arrow) (magnification: 7400x; bar = 5 um.
BC: bile canaliculus). (B) BCNU-treated liver. Lanthanum has penetrated the
tight junctions and entered the canaliculus (arrow) (magnification: 7800x; inset
magnification: 21500x; bar = 1 ,um. BC: bile canaliculus). (C) ANIT-treated
liver. Lanthanum has penetrated the tight junctions and entered the canaliculus
(magnification: 20,000x; bar = 1 sum. BC: bile canaliculus).
65
Figure 13. Lanthanum penetration of junctional complex with BCNU treatment.
(A) Control. (B) BCNU-treated.
66
Figure 13 (cont.) (C) Lanthanum penetration of junctional complex with ANIT
treatment.
67
where the paracellular and transcellular components were isolated. Third, the
penetration must be shown to be occurring at the level of the hepatocyte
junctional complex. Visualization of ionic lanthanum penetration demonstrated
this. Additionally, a dose-response relation between BCNU and permeability was
demonstrated. The utility of P, as a marker of permeability was shown by the
strong correlation with HRP, which is commonly used in permeability studies.
These experiments, then, have demonstrated conclusively that BCNU, in a manner
similar to ANIT, increases permeability of hepatocyte tight junctions. The general
significance of permeability changes in the cholestasis and other dysfunctions
associated with these compounds will be addressed in detail below; however, a few
observations can be made here. Though there does appear to be a temporal
correlation between perfused liver bile flow and P, in the BCNU-treated animals,
the correlation does not hold in vivo, where 1) bile flow is significantly decreased
24 hours after treatment while P, is normal and 2) bile flow remains low after P,
has declined (Figure 14). The correlation also does not hold in the case of ANIT,
where both in vivo and perfused liver bile flows continue to decline in the face of
declining P, concentrations (Figures 3 and 11). In the Wistar rats, a direct, rather
than inverse, correlation was observed between bile flow and P, (Appendix Figure
5). Lack of a direct relation between bile P, and bile flow was also apparent when
the dose of BCNU was increased. While bile P, was greater with 34 mg/kg BCNU
than with 26 mg/kg (2.18 + .10 vs. 1.52 + .03 mM), a parallel decrease in bile
68
2.0
1.5
1
.0
0.5
0.0
0
24
48
72
96
120
TIME (HR)
Figure 14. Lack of correlation between change in bile flow and bile Pi with time
following BCNU treatment. Bile was collected 24, 48, 72, or 96 hours after BCNU
treatment (26 mg/kg, i.p.) and assayed for P, as described. In vivo bile flows are
shown. No correlation between bile flows and bile P, was observed. Values are
means ± SE; n = 10-17.
69
flow was not observed (1.18 ± .25 and .98 ± .10 ,ul /min /g liver for 34 and 26
mg/kg, respectively). An attempt to correlate individual rat bile flow and bile P,
was also unsuccessful (Appendix Figure 6).
If the proposed mechanism for permeability-induced cholestasis is accurate (that
reflux of osmotically-active bile constituents is responsible), it would be expected
that permeability changes could be directly correlated with changes in bile flow.
In these studies this was not the case. It thus appears at this point that increased
permeability, if it is related to cholestasis, is at most only an initiating event. It
is possible that these changes are not causally related at all but are simply
coincidental.
70
V. EVANS BLUE EXCRETION: INHIBITED FLUID-PHASE ENDOCYTOSIS
WITH BCNU TREATMENT
Introduction
HRP excretion kinetics in the isolated liver following BCNU treatment indicated
that, in addition to a substantial increase in rapid phase biliary access, slow phase
transport was also being inhibited (Figure 6). However, HRP results were not
definitive, as it could be argued that the decrease in bile HRP was simply due to
a bile to perfusate washout effect upon removal of HRP from the perfusate (that
is, once the HRP infusion had stopped, the concentration gradient would shift in
favor of movement from bile through the leaky tight junctions to the perfusate)'.
The effect of BCNU on transport was evaluated in isolation using albumin-bound
Evans blue dye (T-1824), which was found to be too large (Mr = 69,000) to
penetrate leaky tight junctions. Evans blue dye is an ideal fluid phase marker.
In addition to not penetrating opened tight junctions, it does not appear to
influence bile flow, bind hepatocyte receptors, or be metabolically altered, diluted,
or concentrated as it traverses the hepatocyte (37).
1There are a number of studies showing that this actually does not occur to a
significant extent (66).
71
Methods
Evans Blue Excretion in vivo. Evans blue plasma concentrations and excretion in
bile over time were evaluated in control rats. Animals were anesthetized and
opened minimally. When bile flow had decreased to basal levels (20-25 minutes
after bile duct cannulation), Evans blue (1.0 mg/100 g body weight in normal
saline/4% albumin) was slowly injected directly into the inferior vena cava. Blood
samples (0.4 ml) were collected by cardiac puncture at t = 20, 40, and 60 minutes
into sodium oxalate tubes and spun for 10 minutes at 4 °C. Bile was collected on
ice in pretared tubes at t = 20, 40, and 60 minutes.
Evans Blue Excretion in the Perfused Liver. Evans blue (10 mg in one ml
saline/4% albumin) was added to the influent line 15 cm before it entered the
liver and infused over a period of one minute. Bile was then collected on ice at
t = 20, 40, and 60 minutes.
Evans blue concentration was determined by a modification of the method of
Zween and Frankena (37). Equal volumes of bile or plasma and polyethylene
glycol 4000 were added to a microcentrifuge tube and the non-albumin protein
fraction allowed to precipitate. The tubes were then spun at 15,000 x g for 10
minutes, the supernatant diluted to a usable volume with distilled water, and the
absorbance at 580 nm recorded. Actual concentrations were determined with the
72
aid of a standard curve prepared from 5 dilutions of stock Evans blue in rat
plasma or bile ( r = .996 and .998, respectively).
Results
Evans blue plasma concentrations and biliary excretion over time in control rats
are shown in Table 3. Plasma concentrations in the first 20-minute sample (150.0
± 13.8 yg/ml) had decreased slightly (but not significantly) by 60 minutes.
Excretion in bile, 0.26 + 0.06 ,ug/hr/g liver during the first 20 minutes, also did
not change significantly with time.
These values are within range of those
reported by others (37). Bile flow was not significantly affected by Evans blue
injection.
As recirculation in vivo precluded the fine analysis of transcellular kinetics, this
experiment was continued in the single pass perfused liver, which permitted study
of the transcytosis of a single pulse of dye. Saturating conditions were used.
Control livers showed a fairly constant dye excretion rate of 0.58 ± 0.08 ,ug/hr/g
liver (Figure 15). Excretion was significantly reduced with colchicine (.30 ± .05
ug /hr /g liver) or BCNU (.23 ± .06 ,ug/hr/g liver) treatment. Though the
decreased excretion of Evans blue with BCNU treatment could be accounted for
in part by decreased bile flow, initial bile samples from BCNU animals also had
73
Table 3. Control Evans blue plasma concentrations and excretion in vivo. Control
rats were minimally opened and Evans blue (1.0 mg/100 g in normal saline/4%
albumin) was introduced into the inferior vena cava. Blood and bile samples were
collected at t = 20, 40, and 60 minutes and assayed for Evans blue as described.
Time(min)
Plasma Conc
(µg /ml)
Bile flow
(Al/minig liver)
Excretion in bile
(Ag/hrig liver)
20
150.0
+ 13.8
1.88 + .09
.26
+ .06
40
118.4
+
9.9
1.70 + .08
.29
+ .04
60
128.0
+ 31.1
1.77 + .08
.31
+ .06
Values are means ± SE; n = 11.
74
0.8
0.6
I
0.4
*
*
0.2
0.0
CONTROL
BCNU
COLCHICINE
Figure 15. Decreased Evans blue excretion following BCNU or colchicine treatment.
Evans blue (10 mg in one ml saline/4% albumin) was infused into perfused livers 48
hours after corn oil (1.0 ml/kg) or BCNU (26 mg/kg) treatment or 21/2 hours after
colchicine treatment (10 mg/kg). Bile was collected at t = 20, 40, and 60 minutes
and assayed for Evans blue as described. A significant decrease in excretion was
observed with BCNU or colchicine treatment. Values are means ± SE; n = 3.
*Significantly different from control, P < 0.05.
75
significantly lower Evans blue concentrations (5.2 ± .78 ug /m1 compared with
10.22 ± 1.69 µg /ml for controls), indicating that transcellular movement was indeed
impaired (Figure 16). The increasing concentrations of dye in bile of the BCNUtreated animals could be accounted for entirely by the cholestasis.
Discussion
Evans blue was found to be an ideal fluid phase marker in other studies (37). This
was confirmed here. In the HRP infusion studies (Chapter 2), increased paracellular
movement under conditions of increased permeability was evidenced by maximal
HRP activity occurring in the first sample. No initial increase was detected with
infused Evans blue in the present studies, indicating that the upper boundary to the
"window of leakage" following BCNU treatment is between 40,000 MW (HRP) and
69,000 MW (albumin-bound Evans blue).
By eliminating the paracellular
component, it was possible to evaluate transcellular effects of BCNU in isolation.
Numerous studies have demonstrated that colchicine inhibits certain aspects of
receptor-mediated
and
non-receptor-mediated
vesicular
transport
(above).
Colchicine had a similar effect in this study, halving the excretory rate of a fluid
phase marker. A comparable decreased excretion rate and decreased initial bile
concentration of Evans blue with BCNU treatment indicates that this agent may be
inhibiting vesicular movement as well. The observed decrease in concentration
76
15.0
0 -0 CONTROL
BCNU
COLCHICINE
0.0
0
20
40
60
TIME (MIN)
Figure 16. Bile concentrations of Evans blue following BCNU or colchicine
treatment. Evans blue (10 mg in one ml saline/4% albumin) was infused into
perfused livers 48 hours after corn oil (1.0 ml/kg) or BCNU (26 mg/kg) treatment
or 21 hours after colchicine treatment (10 mg/kg). Bile was collected at t = 20, 40,
and 60 minutes and assayed for Evans blue as described. A significant decrease in
Evans blue concentration in bile was observed with BCNU treatment. Values are
means ± SE; n = 3. 'Significantly different from control, P < 0.05.
77
cannot be explained by a delay in delivery to the collection vial as a result of
decreased bile flow. Considering the estimated volume of the biliary tree and
cannula (3-4 /41/g liver according to Peterson et al., 118), the maximal delay would
have been less than 5 minutes. Further evidence that retarded collection is not a
factor comes from the HRP studies (above) where maximal activity was measured
in the first samples.
The similar effects of colchicine and BCNU on fluid phase transport suggests a
common mechanism. Decreased transcellular transport with colchicine treatment is
probably mediated by its inhibition of tubulin assembly into microtubules. Reed et
al. (106) showed that BCNU-derived isocyanates inhibit tubulin polymerization in
vitro.
It is possible that the decreased transport seen here with BCNU could be
mediated by a microtubule effect. As the relation of transcellular processes and bile
flow in general is still not understood (above), it is unclear what role this microtubule
inhibition by BCNU may have in BCNU-induced cholestasis.
78
VI. ALTERED BSP EXCRETION WITH BCNU AND ANIT TREATMENT
Introduction
Mechanisms of hepatocellular uptake and transcytosis of organic anions other than
bile salts (e.g. bromsulphalein, bilirubin) are poorly understood (above). As with
bile salts, these anions are tightly bound to albumin in plasma. Though the
albumin appears to play a role in uptake (the "albumin receptor" phenomenon),
the exact nature of this role is uncertain.
Interaction with the hepatocyte
sinusoidal surface apparently facilitates dissociation of the ligand from albumin,
making it available for movement across the membrane (9,119).
Numerous studies have provided evidence that organic anion uptake is carrier-
mediated. High bile/plasma concentration ratios, transport maxima, and energy-
dependency have been reported. Competitive uptake has been demonstrated
among BSP, bilirubin, and indocyanine green (but not taurocholate) (120).
Experiments with sinusoidal membrane preparations have revealed competitive
binding of these anions for high affinity sites.
One of these sites has been
characterized and is immunologically distinct from the sodium-linked bile salt
transporter. The driving force for uptake is unknown but may be linked to
chloride transport, as in the kidney tubule (4). Uptake is independent of sodium.
79
Evidence suggests that transcellular transport is diffusional and involves binding
to cytosolic binding proteins, which may facilitate uptake (33).
Though most
anions undergo biotransformation and/or conjugation during transport, a few do
not (e.g. indocyanine green, rose bengal). Canalicular secretory mechanisms for
these anions have not been well-characterized. A canalicular transporter has been
identified (4).
BSP has had extensive clinical and research use as an indicator of liver
dysfunction. Though retention (prolonged plasma residence time) of this anion
is only a rough measure and provides no information as to the defect locus
(whether altered membrane binding, uptake, transcellular movement, conjugation,
or canalicular secretion), it is a reliable indicator of functional deficit; further
study, as with isolated membrane preparations or pretreatments, may elucidate the
mechanistic basis for the defect.
Retention of BSP has been demonstrated following BCNU and ANIT treatment
in other studies (74,99). An analysis of this retention was undertaken in the
present work to determine what relationship, if any, exists between this effect and
permeability and cholestatic changes.
80
Methods
BSP excretion. A recirculating system was used for BSP excretion experiments.
For extraction determinations, livers were perfused 48 hours after BCNU
treatment. BSP was then slowly added to the perfusate reservoir (0.9 ,umolf min)
with a syringe pump and 10 minute bile and influent and effluent perfusate
samples collected. For BSP clearance determinations, livers were perfused at the
indicated times posttreatment and BSP (5 ymol) added as a bolus to the
recirculation reservoir (initial perfusate concentration: 25 ,uM). Bile and perfusate
samples were collected as indicated.
BSP concentrations were determined according to Hoyt and Larson (35). For
perfusate BSP determinations, equal volumes (750 RI) of perfusate and alkaline
buffer (229 mM Na2HPO4, 10.2 mM Na3PO4, 10.2 mM sodium toluene-p-sulfonate,
pH 10.6) were added to sample tubes. Bile was diluted 1000x with dH2O and
alkalinized with 0.1 N NaOH. Absorbance at 580 nm was determined.
Thin layer chromatography. Samples of perfusate (50 ,u1) and bile (5 ,u1) were
spotted on thin layer plates (Eastman Kodak Co., Rochester, N.Y.) and developed
for 2.5 hours in n-butanol:glacial acetic acid:water (40:10:50). Plates were then
dried and viewed over ammonia fumes.
81
Results
Decreased BSP extraction with BCNU treatment.
The effect of BCNU on
maximal BSP extraction is shown in Figure 17. Transhepatic extraction was
calculated according to the formula
Extraction =
BSPinf
BSPinf
BSPeff
where BSPinf and BSPeff are the concentrations of BSP in the perfusate influent
and effluent, respectively.
A significant difference in BSP extraction in livers from controls and BCNU-
treated rats was detected at all time points between 10 and 80 minutes. This
difference was reflected in a substantial lowering of equilibrium BSP
concentrations in bile of these livers (3.7 mM compared with 10.3 mM for
controls) (Figure 18). A plot of effluent [BSP] as a function of influent [BSP]
(Figure 19) yielded regression lines with similar abscissa intercepts for controls
and treated animals, indicating that BSP uptake was not markedly affected by
BCNU treatment.
Altered BSP excretion kinetics with BCNU and ANIT treatment. Decay kinetics
for livers 24, 48, and 72 hours after BCNU treatment is shown in Figure 20. In
82
100
0
80
60
40
20
0-0 CONTROL
BCNU
0
20
40
60
80
TIME (MIN)
Figure 17. Decreased hepatic BSP extraction with BCNU treatment. Livers were
perfused 48 hours after corn oil (1.0 ml/kg) or BCNU (26 mg/kg) treatment with
recirculation of the effluent. BSP was slowly added (0.9 ymol/min) to the per-
fusate reservoir using a syringe pump and 10-minute perfusate (influent and
effluent) samples collected. Perfusate BSP was assayed as described. Extraction
across the liver was calculated according to the formula
Extraction = BSP,f -
BSPeff
BSPinf
where BSP,f and BSPeff are BSP concentrations in the perfusate influent and
effluent, respectively. A significant decrease in extraction was observed in treated
livers at all time points between 10 and 80 minutes. Values are means ± SE; n
= 3. *Significantly different from control, P < 0.05.
83
12.0
0-0 CONTROL
BCNU
0
9.0
(f)
m
0
1
6.0
0
*
*
*
*
55 3.0
a
0.0
0
,
20
40
60
80
TIME (MIN)
Figure 18. Decreased maximal bile BSP with BCNU treatment. Livers were
perfused 48 hours after corn oil (1.0 ml/kg) or BCNU (26 mg/kg) treatment with
recirculation of the effluent. BSP was slowly added (0.9 ,umol/min) to the
perfusate reservoir using a syringe pump and 10-minute bile samples collected.
Bile BSP was assayed as described. A significant decrease in maximal bile BSP
was observed in treated livers in all but the first sample. Values are means + SE;
n = 3. *Significantly different from controls, P < 0.05.
84
200
e^.
150
ri.
0co
ii 100
1z
LJJ
D
_I
w
50
0
0
50
100
150
200
250
INFLUENT [BSP] (uM)
Figure 19. Regression analysis of influent and effluent BSP with BCNU
treatment. Livers were perfused 48 hours after corn oil (1.0 ml/kg) or BCNU (26
mg/kg) treatment with recirculation of the effluent. BSP was slowly added (0.9
ymol/n-iin) to the perfusate reservoir using a syringe pump and 10-minute
perfusate (influent and effluent) samples collected. Perfusate BSP was assayed as
described. Similar abscissa intercepts for controls and treated livers were
observed.
85
25.0
0
0 CONTROL
A 24 HOUR
A
ID 48 HOUR
20.0
0 72 HOUR
Lcar-,7). 15.0
m
-------
, 10.0
S.*.
i
,i;
i
- .11,....--,.
7 ---''-,------0
(I
N Z ± ,/gi.
a
E
a_
,..-----
.-----<>
o
LiJ
t*
g
5.0
I
0.0
0
(i)
I
10
20
30
I
40
50
60
70
TIME (MIN)
Figure 20. Perfusate BSP retention following BCNU treatment. Livers were
perfused 24, 48, or 72 hours after BCNU treatment (26 mg/kg, i.p.) with
recirculation of the effluent and BSP (5 /mop was added to the perfusate
reservoir as a bolus. Perfusate samples were collected at 2.5, 5, 10, 15, 20, 25, 30,
35, 40, 50, and 60 minutes and assayed for BSP as described. Values are means
± SE; n = 3-6. A significant difference (P < 0.05) in perfusate BSP was observed
between BCNU-treated (48 and 72 hour) and control rats at all time points after
5 minutes and between 48- and 72-hour BCNU livers between 5 and 50 minutes.
Open symbols: influent; filled symbols: effluent.
86
control livers, BSP was cleared rapidly from the influent and was not detectable
in the effluent. Livers perfused 24 hours after BCNU treatment showed decay
kinetics similar to controls (Figure 21). However, a marked perfusate retention
of BSP was observed in livers perfused 48 or 72 hours after BCNU treatment
(equilibrium perfusate concentrations:
respectively).
12.39 + .10 ,uM and 14.93 ± .16 uM,
Maximal perfusate [BSP] was measured in the 72-hour livers.
Perfusion retention was reflected in a significant reduction in peak bile BSP
(Figure 22), with a 70% decrease at 48 hours and an 80% decrease at 72 hours.
Retention had begun to decline at 96 hours (data not included in graph for
clarity).
An analysis of partial clearances of BSP at early time intervals provided further
evidence that BSP uptake was not affected by BCNU (Table 4). Clearance
constants k1, k2, and k3, for the intervals 2.5-5 minutes, 5-10 minutes, and 10-15
minutes, respectively, were calculated according to the formula
k = (log Ca - log Cb)
(tb
ta)
Where C is the concentration of the dye in the perfusate at intervals a and b and
t is the time in minutes (121). Livers perfused 24 hours after BCNU treatment
showed no significant difference in BSP clearance constants at any of the three
intervals. Livers perfused 48 and 72 hours after BCNU treatment had kl constants
not significantly different from controls but k2 and k3 constants significantly
decreased.
87
1.5
0
U.)
CO
LIJ
1
.
0
LL
12 h ANIT
LiJ
a- 0.5
(13.4)
cp
C
CONTROL
24 h BCNU
(10.7)
0.0
I
0
10
(11.3)
I
I
20
30
40
TIME (MIN)
Figure 21. Perfusate BSP decay kinetics for 24-hour BCNU and 12-hour ANIT
livers. Livers were perfused 12 hours after ANIT treatment (250 mg/kg, gavage)
or 24 hours after BCNU treatment (26 mg/kg, i.p.) with recirculation of the
effluent and BSP (5 /mop was added to the perfusate reservoir as a bolus.
Perfusate samples were collected at 2.5, 5, 15, 15, 20, 25, 30, 35, 40, 50, and 60
minutes and assayed for BSP as described. Number in parentheses is the t1/2.
Nonlinearity is due to sinusoidal efflux (Ref. 122). Values are means of 3 livers.
No significant difference in BSP decay was observed between controls and treated
livers at these time points.
88
15.0
CONTROL
--A 24 HOUR
48 HOUR
72 HOUR
0.0
0
10
20
30
40
50
60
70
TIME (MIN)
Figure 22. Decreased BSP excretion in bile with BCNU treatment. Livers were
perfused 24, 48, and 72 hours after BCNU treatment (26 mg/kg, i.p.) with
recirculation of the effluent and BSP (5 ,umol) was added to the perfusate
reservoir as a bolus. Bile samples were collected at 10, 20, 30, 40, 50, and 60
minutes and assayed for BSP as described. Values are means + SE; n = 3-6. No
significant difference was observed between control livers and livers perfused 24
hours after BCNU treatment. A significant difference (P < 0.05) was observed
between control livers and livers perfused 48 and 72 hours after BCNU treatment
at all time points.
89
Table 4. BSP partial clearance constants following BCNU treatment. Livers were
isolated 24, 48, and 72 hours after BCNU treatment and evaluated for BSP clearance
from perfusate. k1, k2, and k3 are the perfusate clearance constants for the 21/2-5
minute, 5-10 minute, and 10-15 minute intervals after BSP addition, respectively.
CONTROLS
24hr
48hr
72hr
kl
.043 + .012
.048 ± .002
.041 + .002
.048 + .003
k2
.069 + .004
.060 + .001
.044 + .002a
.022 + .002a
k3
.080 + .002
.074 + .003
.023 + .006a
.006
Values are means ± SE.
aSignificantly different from control, p < 0.05.
+ .034a
90
BSP decay kinetics not significantly different from controls were also observed in
livers removed from rats 12 hours after ANIT treatment (Figure 21,23). Retention
was significant at 24 and 48 hours. In contrast to BCNU-treated livers, measurable
BSP was present in the initial (21/2 minute) samples and perfusate equilibria were not
established.
BSP concentration in bile 12 hours after ANIT treatment was not
significantly different from controls (not shown). Insufficient bile flow in the 24 hour
and 48 hour ANIT rat livers precluded measurement of bile BSP.
Thin layer chromatography. Thin layer chromatography revealed a steady loss of
parent compound and increase in a single conjugate in the perfusate for both
treatments (Figure 24 A,B). No unconjugated BSP was detected in the perfusate
after 30 minutes. The perfusate conjugate was not detected in bile. Bile samples
incubated with 4% albumin comigrated with non-incubated samples (Figure 24C).
Discussion. Organic anion retention following BCNU and ANIT treatment has been
reported in other studies. Thompson and Larson (97) demonstrated that BCNU
caused a dose-dependent BSP and bilirubin retention in intact rats. At early time
points the bilirubin was predominantly of the conjugated form, indicating that uptake
and metabolic processes were still functional. Hoyt and Larson (35,99) further
characterized this defect in vivo, noting that the retention preceded cholestasis and
had not reversed by 15 days posttreatment, though bile flow had been restored. As
secretion of indocyanine green, which is not metabolized, was also decreased,
91
0
0 CONTROL
0
24 HOUR
0 48 HOUR
A-A 12 HOUR
25.0
20.0
(-07
TzT
m15.0cf-)
(r) 10.0_
RAN
a_
5.0
ON
0.0
A-A
0
-A
10
20
30
I
40
50
60
70
TIME (MIN)
Figure 23. Perfusate BSP retention following ANIT treatment. Livers were perfused
12, 24, or 48 hours after ANIT treatment (250 mg/kg, gavage) with recirculation of
the effluent and BSP (5 ,umol) was added to the perfusate reservoir as a bolus.
Perfusate samples were collected at 2.5, 5, 10, 15, 20, 25, 30, 35, 40, 50, and 60
minutes and assayed for BSP as described. Values are means + SE; n = 3. No
significant difference in perfusate BSP was observed between controls and livers
perfused 12 hours after ANIT treatment. A significant difference (P < 0.05) was
observed at all time points between controls and livers from rats perfused 24 or 48
hours after ANIT treatment. Open symbols: influent; closed symbols: effluent.
92
A B BIS! 7 6 5 4 3 2 1 7 6 5 4 3 2
BILE
1
BCNU PERF BSP
TC
TA
PB
EA
BILE BSP
3
2
1
B + ALB
B
65432
1
654321 654321
ANIT PFRF Flq13
C
Figure 24. Thin layer chromatography. (A) A: Bile BSP, ANIT(24h); B: bile BSP,
BCNU(48h); S: BSP standard; BCNU PERF BSP: perfusate BSP of 2 livers from rats
treated with BCNU(48h), samples taken at 5-minute intervals after BSP addition to
perfusate. (B) Perfusate BSP of 3 livers from rats treated with ANIT(24h), samples
taken at 5-minute intervals after BSP addition to perfusate. (C) Bile BSP with
cotreatments. TC: triamcinolone control; TA: triamcinolone + ANIT(24h); PB:
phenobarbital + BCNU; EA: esculetin + ANIT; B + ALB: BCNU bile incubated
with 4% albumin. (D) Bile BSP, control.
93
impairment of metabolic processes was not considered significant. The observation
that BCNU-treated animals retained the capacity to concentrate bile salts suggested
to these authors that increased paracellular permeability, as demonstrated with ANIT
treatment (74), was also not an adequate explanation for the observed retention.
They postulated that the defect was occurring at the level of canalicular secretion.
BSP retention following ANIT treatment was examined in early studies. Becker and
Plaa (100,101) measured significant BSP retention in mice by 180 minutes after
treatment. As with BCNU, uptake and metabolic processes did not appear to be
affected. Krell et al. (74) characterized decreased BSP excretory capacity with ANIT
treatment in the isolated perfused rat liver.
These investigators observed a
significant decrease in the ability of treated livers to concentrate BSP in bile between
4 and 7 hours after ANIT treatment. Decreased capacity was temporally correlated
with increased equilibrium perfusate concentrations of BSP, taurocholate, and
[14C]sucrose, but preceded cholestasis. Uptake, metabolism, and excretion of BSP
appeared normal. In the opinion of these authors, these results provided sufficient
evidence for causality between permeability changes and BSP retention (that is,
opening of tight junctions was allowing paracellular reflux of biliary BSP back into
the perfusate) (74).
In the present work, BCNU- and ANIT-induced BSP retention was closely examined
in the in situ perfused rat liver. Results indicate that retention is coincident with, but
94
not a function of, the increased permeability associated with these compounds.
An analysis of the time course of perfusate BSP retention with BCNU treatment
(Figures 20 and 22) revealed a significant retention of BSP 48 and 72 hours
posttreatment. The negligible initial effluent BSP concentrations (when influent
concentrations were maximal) and the slow rise in perfusate concentration over the
course of the perfusion indicate that uptake processes were not affected by BCNU
in these experiments. This was confirmed by the lack of a significant difference
between control and treated clearance constants for the 2.5-5 minute time interval
(Table 4).
TLC results (progressive loss of parent compound and increased
conjugate) provide evidence that metabolism of BSP was also functional (Figure 24).
If, as these and other studies indicate, uptake and metabolic processes are normal
following BCNU treatment while paracellular permeability is increased, it is not
unreasonable to associate retention with paracellular reflux (that is, normal BSP
uptake, conjugation, and secretion into bile is followed by return to the perfusate
through opened tight junctions).
However, though paracellular reflux may be
contributing somewhat to the retention, results here indicate that this is not a
sufficient mechanism.
Maximal retention was observed 72 hours after BCNU treatment, when increased
permeability had significantly recovered from the 48-hour maximum. Peak HRP and
P bile concentrations at 72 hours were, respectively, 1/5 and 1/2 that at 48 hours
95
(Figures 4 and 10). Evidence against causality was also provided by the TLC results.
If paracellular leakage of BSP were occurring to a significant extent, it would be
expected that the biliary form of BSP would predominate in the perfusate. This was
not the case.
The predominant BSP conjugate in bile was not detected in
equilibrium perfusate and vice versa.
A clear argument against BCNU-induced BSP retention being solely a function of
increased permeability is that the increase in perfusate concentration is too rapid to
be accounted for by bile input. During the 2nd 10-minute sampling period, the time
of rapid increase in perfusate concentrations, the average increase in perfusate BSP
for the BCNU-treated rats was 5.2 ,uM, or approximately 1 ,umol added to the 0.2
liter system. However, during this same period, the BCNU-treated rats could only
have released a maximum of approximately 0.12 itmol BSP from bile:
(7.2mM)
(ave. control bile
[BSP] during sample
period)
(1.7mM)
=
(ave. BCNU bile
1BSP] during sample
5.5mM
(difference
with treatment)
period)
(5.5mM) x (.022 ml)
=
(ave. ml bile
flow during sample
period)
.12 gmol BSP
Thus, if all the BSP that did not appear in the bile of the BCNU rats during this
period entered the perfusate it could account for no more than 12% of the BSP that
accumulated.
Similar results were obtained with ANIT. Though complete bile stasis precluded the
96
Similar results were obtained with ANIT. Though complete bile stasis precluded the
measurement of P, at 48 hours, P, was half its maximal value 36 hours after treatment
(when bile flow had almost stopped) and it is likely that it was further decreased at
48 hours. As was shown (Figure 23) maximal BSP retention occurred in the 48-hour
animals.
In contrast to BCNU, ANIT appeared to inhibit BSP uptake (Figure 23). Livers
perfused 24 and 48 hours after ANIT treatment showed substantial BSP in the first
(21/2-minute) samples, indicating that some BSP was not being taken up in the first
pass. These results are at odds with those of other investigators (74,100,101). It is
noteworthy also that, in livers from the 24-hour animals, equilibrium perfusate
concentrations were not attained (Figure 23).
This is indicative of retarded
intracellular movement (i.e. decreased transcellular transport) prior to release, which
also conflicts with other studies. It is possible that these conflicting results are due
to the rat strain used. As was noted in chapter 2, the Sprague-Dawley rat was found
to have a dramatically different permeability time course than the Wistar rat, the
strain traditionally used most in ANIT studies (Appendix Figure 4).
It appears, then, that increased permeability is not a sufficient explanation for the
BSP retention observed with these treatments. In the present studies early retention
actually correlated better with onset of cholestasis than with increased permeability.
However, bile flow in livers from BCNU-treated rats had returned to normal at 72
97
hours, the time of maximal BSP retention (Figure 2). Though it was not observed
here, other investigations with BCNU (35,99) and ANIT (74,100) have measured
significant BSP retention prior to cholestasis onset. It is also possible to influence
these changes in isolation (below).
Glutathione-S-transferase B (ligandin) and other glutathione-S-transferase (GSH)
isozymes are cytosolic enzymes that, in addition to their metabolic activity, have a
significant role as intracellular binding proteins (33,123). Binding of organic anions
to these proteins facilitates uptake and limits sinusoidal efflux (back-diffusion across
the sinusoidal membrane).
Binding is probably an important factor in overall
transport. BCNU and ANIT have been shown to inhibit a number of enzyme
activities (69,92).
It is possible that the increased BSP retention resulting from
BCNU and/or ANIT treatment could be due, in part, to an alteration of this binding
activity and subsequent increased sinusoidal efflux (124). Decreased efflux of tracer
bilirubin from isolated hepatocytes with phenobarbital pretreatment was shown to be
secondary to increased ligandin concentration (33). Phenobarbital pretreatment of
BCNU-treated rats partially protected against BSP retention (below).
These results are not inconsistent with inhibition of canalicular transport of BSP, as
proposed by Hoyt and Larson (99); consequent increased intracellular concentrations
could also result in sinusoidal efflux.
98
VII. METABOLIC STUDIES: CHANGES IN BCNU- AND ANIT-INDUCED
HEPATIC DYSFUNCTIONS WITH PHENOBARBITAL PRETREATMENT
Introduction
Various studies have demonstrated altered effects of ANIT and BCNU with
metabolic changes. Early studies (69) showed that metabolic inducers could
potentiate and inhibitors attenuate the hyperbilirubinemic response to ANIT.
Hyperbilirubinemia and cholestasis were also decreased with hypothermia and
protein synthesis inhibition (69). These and other studies demonstrated fairly
conclusively that the cholestatic and hyperbilirubinemic effects of ANIT were
mediated by a metabolic product. Recent work has revealed that ANIT-induced
permeability changes are also metabolite-mediated.
Kan and Coleman (66)
studied the effects of phenobarbital (PB) and SKF525A pretreatment on ANIT-
induced junctional permeability to infused proteins.
PB pretreatment greatly
increased the rapid (paracellular) phase of HRP entry into bile; SKF525A
pretreatment had the opposite effect. Slow phase (transcellular) transport was not
influenced by either pretreatment.
There are conflicting opinions regarding the role of metabolism in the degradation
of BCNU (90,125).
Though it has been generally believed that chemical
breakdown has the major role (90,126), metabolic manipulation has been shown
to have pronounced effects on the therapeutic and toxic effects of BCNU. Levin
99
et al. (90) found that phenobarbital pretreatment completely eliminated the
antitumor activity and decreased the systemic toxicity of BCNU in rats. Plasma
decay analysis revealed that pretreated rats had markedly reduced plasma drug
residence times; the decrease was consistent with enzymatic induction. The effect
of PB pretreatment on the hepatoxicity of 1-(2-chloroethyl)-3-cyclohexy1-1nitrosourea (CCNU), a congener of BCNU with similar therapeutic and toxic
effects (96; Appendix Table 1), was studied by Ahmed et al. (127). Pretreated rats
had decreased serum enzyme levels and organic anion retention, fewer bile duct
lesions, and normal bile flow.
These authors postulated that phenobarbital
pretreatment was either a) altering the metabolism of CCNU and thereby
increasing its detoxication, or b) increasing bile flow and consequently increasing
excretion of toxic metabolites.
The metabolic studies presented here were undertaken for two primary reasons:
1) to clarify the significance of metabolism in the toxicity of BCNU and ANIT,
and, 2) by these manipulations, to better understand and define relations between
the various hepatotoxic manifestations of these agents.
Methods
Altered in vivo liver functions with PB pretreatment. Rats received phenobarbital
(80 mg/kg/day, i.p.) for 3 days prior to BCNU or ANIT treatment, SKF525A (40
100
mg/kg, i.p.) 45 minutes before BCNU treatment, or chloroethylisocyanate (12.8
mg/kg, i.p.).
Liver function was assessed 48 hours
after BCNU or
chloroethylisocyanate treatment or 12 hours after ANIT treatment.
Altered perfused liver functions with PB pretreatment.
The effects of PB
pretreatment on ANIT- and BCNU-induced hepatic dysfunction were further
evaluated in the perfused liver. Rats received PB as above and livers were
perfused 48 hours after BCNU treatment or 12 hours after ANIT treatment. Bile
flow and BSP excretory capacity were evaluated as previously described.
Results
The effects on bile flow and bile P, of chloroethylisocyanate and of PB
pretreatment of BCNU and ANIT are shown in Table 5. Rats receiving PB alone
had in vivo and perfused liver bile flows significantly higher than controls (2.07 +
.13 and 1.28 ± .04 ,ul /min /g liver for in vivo and perfused liver bile flows,
respectively, compared with 1.82 + .04 and .97 + .05 ,u1/min/g liver for controls).
The cholestatic effect of BCNU was reversed in vivo (1.69 ± .09 ,u1/min/g liver)
but not in the perfused liver (.62 ± .09 ,u1/min/g liver) with PB pretreatment. No
difference was observed between bile P, in PB-pretreated and non-pretreated rats.
Bile flow in rats 12 hours after ANIT treatment was significantly higher than
controls in vivo (2.02 ± .06 ,ul /min /g liver) but not in the perfused liver
101
Table 5. Effects of phenobarbital pretreatment on ANIT- and BCNU-induced
cholestasis and bile inorganic phosphate. Phenobarbital was dissolved in normal
saline (80 mg/ml) and injected i.p. (1.0 ml/kg/day) for 3 days prior to treatment with
BCNU (26 mg/kg), ANIT (250 mg/kg), or chloroethylisocyanate (12.8 mg/kg). Liver
functions were evaluated 48 hours after BCNU or chloroethylisocyanate treatment
or 12 hours after ANIT treatment.
TREATMENT ( n )
IN VIVO
CONTROL (30)
BILE FLOWa
PERF LIVER
BILE Pib
.97 + .05
.17 + .02
1.82 + .04
BCNU (17)
.98 + .10c
ANIT(15)
2.02 + .06c
CI (6)
1.00 + .21c
PB (9)
2.07 + .13c
1.28 + .04c
BCNU/PB(8)
1.69 + .09d
.62 + .09c
ANIT/PB(8)
Cl/PB(3)
.01 + .003c'd
1.93 + .10d
.51 + .05c
.85 + .06
ND
1.52 + .03c
.31 + .09
.29 + .06
.17
+ .02
1.52 + .06c
Oc'd
.80 + .10c'd
ND
.20 + .03
a/.11/111ill/g liver
bmM.
`Significantly different from control, P < 0.05.
dSignificantly different from non-pretreated, P < 0.05. ND: not determined.
102
(.85 ± .06 ,u1/min/g liver). With PB pretreatment, bile flow was reduced to near
zero in both cases while bile P, was significantly increased (.80 + .10 compared with
.17 + .02 mM for controls). Chloroethylisocyanate (CI) treatment decreased in vivo
bile flow to a similar degree as BCNU (1.0 + .21 ,u1/min/g liver and .98 ± .10
,ul /min /g liver for CI and BCNU treatments, respectively) but did not increase bile
Pi over controls.
As with BCNU, phenobarbital pretreatment eliminated the
cholestatic effect of CI in vivo but did not change bile P,.
Comparative studies were also conducted with the microsomal enzyme inhibitor,
SKF525A.
However, though some interesting results were obtained, this agent
consistently induced substantial cholestasis alone and was therefore not studied
further (data not shown).
Perfusate BSP decay kinetics in livers from rats receiving PB alone were not
significantly different from corn oil controls (Figure 25). Equilibrium perfusate BSP
concentrations (Figure 26) were significantly lower in livers from rats pretreated with
PB than from those receiving BCNU alone (6.3 ,uM vs. 12.4 /AM). This difference was
reflected in a parallel increase in peak bile BSP (8.26 mM and 3.97 mM for livers
from PB-pretreated and non-pretreated rats, respectively) (Figure 27) and in maximal
BSP excretion (1.91 + .37 nmol/min/g liver for PB-pretreated compared with .59 +
.21 nmol/min/g liver for BCNU alone (Figure 28).
103
Figure 25. Perfusate BSP decay kinetics for livers from corn oil controls and
phenobarbital controls. Rats were treated with normal saline or phenobarbital (80
mg/kg, i.p.) for 3 days and corn oil (1.0 ml/kg) on the fourth day. Livers were
perfused 48 hours later with recirculation of the effluent and BSP (5 ymol) was
added to the perfusate reservoir as a bolus. Perfusate samples were collected at 2.5,
5, 10, 15, 20, 25, 30, 35, 40, 50, and 60 minutes and assayed for BSP as described.
Number in parentheses is t1/2. No significant difference in BSP decay was observed
between corn oil controls and phenobarbital controls. Values are means of 3 livers.
Slight nonlinearity is due to sinusoidal efflux of BSP (Ref. 122).
104
25.0
0-0 CONTROL
A-A PB
20.0
0-0 BCNU
0-0 PB/BCNU
15 0
=,--,
azgg
(cro) 10.0
T
5.0
0.0
1
IV.
0
5N
I
10
20
cP
30
40
50
60
70
TIME (MIN)
Figure 26. Decreased BCNU-induced perfusate BSP retention with phenobarbital
pretreatment. Rats were treated with normal saline or phenobarbital (80 mg/kg, i.p.)
for 3 days and corn oil (1.0 ml/kg) or BCNU (26 mg/kg) on the fourth day. Livers
were perfused 48 hours later with recirculation of the effluent and BSP (5 /mop was
added to the perfusate reservoir as a bolus. Perfusate samples were collected at 2.5,
5, 10, 15, 20, 25, 30, 35, 40, 50, and 60 minutes and assayed for BSP as described.
Values are means ± SE; n = 3-7. A significant difference (P < 0.05) in perfusate
BSP was observed between livers from pretreated and non-pretreated animals at all
time points after 21/2 minutes.
105
15.0
0-0 CONTROL
-A PB
BCNU
PB/BCNU
0.0
0
10
20
30
40
50
60
70
TIME (MIN)
Figure 27. Increased bile [BSP] in BCNU-treated livers with phenobarbital
pretreatment. Rats were treated with normal saline or phenobarbital (80 mg/kg, i.p.)
for 3 days and corn oil (1.0 ml/kg) or BCNU (26 mg/kg) on the fourth day. Livers
were perfused 48 hours later with recirculation of the effluent and BSP (5 ,umol) was
added to the perfusate reservoir as a bolus. Bile samples were collected at 10, 20,
30, 40, 50, and 60 minutes and assayed for BSP as described. Values are means ±
SE; n = 3-7. A significant difference (P < 0.05) in bile [BSP] was observed between
livers from pretreated and non-pretreated animals at all time points after 10 minutes.
106
(;) 1 0.0
cn
c
E
8 .0
c 6.0
0
1=
4.0
1-11
2.0
w
n..
w
co
.<><
x\-\\
0.0
CONTROL
PB
BCNU
PB/BCNU
Figure 28. Increased maximal BSP excretion in BCNU-treated livers with
phenobarbital pretreatment. Rats were treated with normal saline or phenobarbital
(80 mg/kg, i.p.) for 3 days and corn oil (1.0 ml/kg) or BCNU (26 mg/kg) on the
fourth day. Livers were perfused 48 hours later with recirculation of the effluent and
BSP (5 umol) was added to the perfusate reservoir as a bolus. Bile samples were
collected at 10, 20, 30, 40, 50, and 60 minutes and assayed for BSP as described. BSP
excretion was determined as the product of bile [BSP] and bile flow. Values are
means ± SE; n = 3-7. Significantly different from BCNU alone, P < 0.05.
107
Discussion
Numerous investigations have demonstrated that the hepatotoxicity of ANIT is
mediated by a metabolite.
This was confirmed in the present studies.
Rats
evaluated 12 hours after ANIT treatment had normal bile flows'- and bile Pi; with
PB pretreatment bile flow was dramatically reduced and bile P, was increased. As
bile flow was reduced from control levels to near zero with PB pretreatment at this
early time point, it was not considered productive to evaluate rats at 24 hours. Lack
of bile flow in the perfused livers precluded analysis of ANIT-induced BSP retention
with PB pretreatment.
PB pretreatment reversed BCNU-induced cholestasis in vivo but not in the perfused
liver. The mechanism of this selective effect is not clear. Hoyt (128) found that
pretreatment with the barbiturate pentobarbital protected against BCNU-induced
cholestasis and organic anion retention in vivo, postulating that these effects might
be a function of increased BSIF or accelerated BCNU metabolism. Neither of these
mechanisms appear to be mediating the protective effects of phenobarbital in the
present investigation.
Phenobarbital (PB), as in previous studies (129,130), was observed here to stimulate
2The in vivo bile flow was significantly higher than normal. This has been observed
at early time points in other studies (74).
108
control bile flow significantly (14% and 32% increases over corn oil controls for in
vivo and perfused liver flows, respectively). However, in rats receiving BCNU, PB
pretreatment selectively reversed cholestasis in vivo; cholestasis in the perfused liver
(i.e. BSIF) was unchanged, though PB stimulated the latter flow to a greater extent
in controls. Thus, a BSIF stimulatory mechanism for cholestasis reversal does not
appear tenable.
Altered BCNU metabolism with PB pretreatment also may not provide an adequate
explanation for these effects. Though PB pretreatment has been shown to decrease
the efficacy of BCNU (90), no difference in bile P, was observed in the present study.
As bile P, is dose-related to BCNU (Figure 8), it would be expected that detoxication
would be reflected in a decrease in this toxic endpoint. Histologic evidence (below)
also argues against accelerated detoxication as a potential mechanism of PB
protection. However, it is possible that PB pretreatment is causing a shift in the
metabolic profile of BCNU with a consequent shift in its specific hepatotoxic effects.
BCNU decomposes to strongly alkylating and carbamylating intermediates (131) and,
predictably, has been shown to inhibit various enzyme activities (131). Results of the
present work are consistent with inhibition by BCNU of proteins integral to anion
transport and bile flow processes.
Reported elevations of K+ and depressed Na+ in plasma of BCNU-treated animals
109
(35) suggests Na+,K+-ATPase inhibition. Inhibition of this enzyme in the liver could
be mediating, in part, the decreased BSIF observed with BCNU treatment. The
Na+,K+-ATPase responsible for BSIF appears to be localized on the lateral,
intercellular spaces of hepatocytes and BSIF is apparently driven to a large extent by
Na+ being pumped into the intercellular space and passing through cation-selective
channels in the tight junctions (72). BCNU may have a direct effect on this activity.
Inhibition of Na+,K+-ATPase would also be expected to decrease uptake/transport
of bile salts (which is also dependent on activity of this enzyme) and thus decrease
BSDF as well.
Decreased bile salt excretion with BCNU treatment has been
observed, though results are conflicting. Hoyt and Larson (35) found no significant
decrease in basal excretion of total bile salts 48 hours after treatment with 20 mg/kg
BCNU. However, in another study (Krell and Larson, unpublished observations), 24
mg/kg BCNU significantly decreased maximal taurocholate secretion at 48 hours and
maximal bile taurocholate concentrations at 30 hours.
Numerous studies have demonstrated that PB selectively induces the bile salt
independent fraction of bile flow (130,132). This was evidenced in the present
experiments by a 2-fold greater increase in perfused liver bile flow (i.e. BSIF) than
in total, in vivo flow with PB pretreatment. Studies have also shown that the increase
in BSIF with PB may be mediated by its stimulation of Na +,K+ -ATPase activity
(133,134). If Na+,K+-ATPase is inhibited by BCNU, PB could be countering this
effect and thereby restoring bile salt transport. That protection did not extend to
110
BSIF in the present studies may be because inhibition of Na+,1C--ATPase is only one
component of BSIF inhibition by BCNU.
There is evidence junctional
permselectivity for cations (e.g. Na+) is compromised when permeability is increased
(66). Thus, the increased permeability resulting from BCNU may antagonize net
Na+ flow into the canaliculus; increased intercellular Na+ following Na+,K+-ATPase
induction with PB might tend to diffuse back into plasma and not into the
canaliculus.
Other factors, such as periportal edema (below), loss of biliary
glutathione(128), or inhibition of transport proteins may also be important.
Cytosolic binding proteins (e.g. glutathione-S-transferase B, ligandin) could also be
adversely affected by BCNU. These proteins appear to have an integral role in the
uptake and transcellular transport of organic anions, including bile salts (9,33,123).
It may be that an active product of BCNU inhibits the binding activity of some of
these proteins and thereby decreases bile salt uptake/transport (above). Induction
of these proteins by PB could be countering this effect in vivo. A correlation has
been observed between increased net bile salt uptake and levels of total glutathione-
S-transferase in hepatocytes isolated from PB-pretreated rats (135).
Phenobarbital pretreatment partially protected against BCNU-induced BSP retention
(Figure 26). Equilibrium perfusate concentrations of BSP were halved and biliary
excretion was increased 3-fold when rats were treated with PB prior to BCNU. This
increase was probably not due to an additive effect, as BSP excretion in PB controls
111
was not elevated (Figure 28). It also cannot be attributed to increased bile flow, as
no change in bile flow in these livers was observed (Table 5). Wolkoff et al. (33)
showed that PB pretreatment resulted in a parallel increase in ligandin concentration
and net uptake of tracer bilirubin into hepatocytes. As with bile salts, PB induction
of ligandin and other binding proteins in the present studies could be countering the
opposing effects of BCNU. TLC results suggest that PB pretreatment induced a
change in BSP metabolism (Figure 24).
Chloroethylisocyanate (CI), the putative carbamylating product of BCNU (131),
effected cholestasis in a manner similar to BCNU. As with BCNU, CI-induced
cholestasis was reversed with PB pretreatment. If the decreased bile flow and/or
BSP transport observed with BCNU treatment is, in fact, mediated by a decrease in
protein function, these preliminary results suggest the chloroethylisocyanate moiety
may be responsible. Perfusion of livers from CI-treated rats with and without PB
pretreatment could directly address this question.
Though in vivo cholestasis was reversed when BCNU-treated rats were pretreated
with PB, bile P, was unchanged.
These results strengthen the argument that
increased permeability and cholestasis may not be related. A decrease in bile flow
with CI similar to that of BCNU without a parallel increase in P, also strengthens this
argument.
112
The decrease in BCNU-induced BSP retention without a parallel increase in bile P,
following PB pretreatment provides further evidence that increased permeability and
BSP retention are separate events.
113
VIII. POTENTIAL ROLE OF INFLAMMATORY MEDIATORS IN THE
HEPATOTOXICITY OF BCNU AND ANIT
Introduction
Leukotrienes are biological regulators that have an integral role in inflammatory
and immediate hypersensitivity reactions.
This class of substances was first
described in 1938 by Feldberg and Kellaway (136) as a smooth muscle relaxing
factor found in the lung perfusates of guinea pigs exposed to cobra venom. The
factor was referred to as slow-reacting substance of anaphylaxis (SRS-A) until
1979 when the structures of its components were identified (137,138). SRS-A was
found to be a combination of the cysteinyl leukotrienes leukotriene C4 (LTC4) and
its metabolites leukotriene D4 (LTD4) and leukotriene E4 (L I E4) (138). The
name "leukotriene" was introduced by Bengt Samuelsson and co-workers to
describe these compounds as they were identified in leukocytes and had in
common a conjugated triene (138,139).
A major obstacle in the identification and characterization of the leukotrienes has
been the fact that, in addition to their lability, they exist in extremely
concentrations in most biological systems;
low
normal plasma levels are in the
picomolar range, increasing to the nanomolar range under certain pathological
conditions (140). The traditional bioassay for leukotrienes, monitoring of isolated
guinea pig ileum contractile activity, has been augmented by advances in
114
radioimmunoassay, HPLC, and mass spectrometric techniques, which have greatly
facilitated the isolation and identification of these compounds (139,140,141).
Biosynthesis of eicosanoids (prostaglandins and leukotrienes) is initiated by the
hydrolytic release of arachidonic acid from the 2 position of certain cell membrane
phospholipids (140). Hydrolysis is catalyzed by phospholipase enzymes, primarily
phospholipase A2 (140). Under normal physiological conditions, free arachidonic
acid concentrations are quite low; release from membranes, which is the ratelimiting step in eicosanoid formation (142), is highly regulated. Once released,
arachidonic acid can be 1) re-esterified into cell membranes by acetyl CoA
transferase, 2) acted on by cyclooxygenases to form prostaglandins, or 3) converted
to leukotrienes through the action of lipoxygenases (140,143).
The three
important lipoxygenase
enzymes
produce 5-,
12-,
or
15-
hydroperoxyeicosatetraenoic acid (HPETE) by inserting oxygen at the C-7, C-10,
or C-13 positions, respectively (143). Further conversion via the 5-lipoxygenase
pathway yields the unstable epoxide leukotriene A4 (LTA4), which is the precursor
for LTB4, LTC4, LTD4, and L'1 E4, the leukotrienes which appear to have the most
pathological significance. LTB4 is formed by the addition of water to LTA4
(138,140,143). LTA4 is converted to LTC4 by conjugation with glutathione at
carbon atom 6 (140). The latter reaction is catalyzed by glutathione-S-transferase
4-4 (140,142). This isozyme has been isolated from the 100,000 g pellet fraction
115
of rat basophil leukemia (RBL) cells and is distinct from the cytosolic enzyme that
acts on aryl halides, such as 1-chloro-2,4-dinitrobenzene (CDNB) (144).
Sequential elimination from LTC4 of glutamic acid and glycine results in the
formation of LTD4 and L 1 E4, respectively (138,143).
While formation of prostaglandins via the cyclooxygenase pathway is ubiquitous
in biological systems, leukotriene production occurs in only a limited number of
cell types (140). In the liver, major producers are leukocytes (137,140,145,146),
Kupffer cells (147,148), mast cells (140,146,149), and possibly hepatocytes (150).
The biological effects of leukotrienes can be separated into 2 broad categories:
1)
effects on blood cells and
2)
effects on vascular permeability and
vascular/airway resistance. LTB4 is highly chemotactic for polymorphonuclear
leukocytes (PMNs) and has an integral role in inflammatory infiltrations
(137,139,142,143,151).
Its chemotactic potency
is
comparable to that of
complement-derived C5a and the synthetic cytotaxin FMLP (formyl-methionylleucyl-phenylalanine) (139,151,152).
LTB4 also induces adhesion of PMNs to
endothelial cells (137,146) and release of lysosomal enzymes and superoxide
(137,138,142,146,152,153). The cysteinyl leukotrienes, LTC4, LTD4, and LTE4,
mediate various biological activities, including changes in airway and vascular
resistance, cardiac function, and microvascular permeability (137,138,139,140,
142,143,146,154,155).
Cysteinyl leukotrienes are potent bronchoconstrictors in
116
several species, including humans (154). Constriction is selective for peripheral
over central airways (156). LTC4 and LTD4 may play a role in the pathogenesis
of asthma (137).
In the cardiovascular system, release of the cysteinyl
leukotrienes produces an initial hypertension followed by a prolonged hypotension
(140,149, 156). The hypertension is a consequence of transient vasoconstriction;
the subsequent hypotension is due to a direct negative inotropic effect coupled
with increased postcapillary leakage, leading to a loss of plasma volume
(138,140,146, 149,154). The hypotension can result in lethal shock (140). The
mechanism of plasma exudation appears to be a direct effect on the endothelial
cells of postcapillary venules (138,139).
Leukotriene-induced exudation
is
potentiated by vasodilator prostaglandins, such as PGE2 and PGI2 (138). The
potentiation may be due to a reversal by the prostaglandins of the vasoconstriction which accompanies the plasma exudation induced by LTC4 and LTD4
(139).
There is increasing evidence that leukotrienes may play a role in certain
pathological conditions.
inflammatory
disease
The first evidence of leukotriene involvement in
was
the
identification
of
high
levels
of
12-
hydroxyeicosatetraenoic acid (12-HETE) in the skin of people with psoriasis (157).
Cysteinyl leukotrienes have since been isolated from the sputum of asthmatics and
cystic fibrosis patients and the bronchial lavage fluid of infants with primary
hypertension.
LTB4 was found in the synovial fluid of rheumatoid arthritis
117
patients (158). Leukotrienes have also been associated with myocardial infarction,
atherosclerosis, gout, and other diseases (139,143,157,158,159).
HPLC analysis
has revealed parallel increases in the concentration of leukotrienes and leukocyte
numbers in some of these diseases (143,157). An early increase in PMNs and proinflammatory mediators
(prostaglandins, thromboxanes, and
lipoxygenase
products) has been demonstrated in the progression of myocardial ischemia (159).
Prostaglandins and thromboxanes may mediate, potentiate, or antagonize some of
the effects of the leukotrienes (154). Elevated plasma levels of leukotrienes have
also been measured following various types of trauma, such as burn injury and
bone fracture (154).
A number of studies have implicated leukotrienes in
inflammatory liver disease (below).
The potential etiological involvement of leukotrienes in disease is based on two
types of indirect evidence: 1) levels of leukotrienes are increased in certain disease
states and 2) some of these disease symptoms can be duplicated in animals by
administration of leukotrienes.
However, to demonstrate causality it is also
desirable to show that inhibition of leukotriene production can alleviate disease
symptoms (160). There has been some success in this regard (159).
Eicosanoid synthesis may be inhibited either at the level of the phospholipase,
decreasing the available arachidonic acid, or at the level of the cyclooxygenase or
lipoxygenase, inhibiting the formation of prostaglandins or leukotrienes,
118
respectively. Corticosteroids (e.g. dexamethasone, hydrocortisone, triamcinolone)
inhibit phospholipase activity, apparently by inducing the synthesis of an antiphospholipase A2 protein (138,161,162).
Phospholipase activity can also be
inhibited by acetylenic analogs of arachidonic acid, such as eicosatetraenoic acid
(161).
Aspirin, indomethacin, and other non-steroidal antiinflammatory drugs (NSAIDS)
inhibit the synthesis of prostaglandins via the cyclooxygenase pathway (138). This
may be part of the mechanism of their antiinflammatory activity clinically (163).
However, blockage of this pathway has been shown to shift released arachidonic
acid to the lipoxygenase pathway, resulting in a substantial increase in leukotriene
synthesis and possible adverse clinical consequences (139).
Cyclooxygenase
inhibition is used to increase leukotriene synthesis for analysis (160).
The
first
recognized
specific
inhibitor
of leukotriene
formation
was
diethylcarbamazine, which prevented SRS-A generation (158). Numerous other
nonselective inhibitors of leukotriene synthesis exist, including various antioxidants
and flavenoids (160).
Cysteinyl leukotriene synthesis can be prevented by
inhibition of glutathione-S-transferase activity, as with the prostacyclin analogue
U-60,257 (158).
In recent years, a number of specific lipoxygenase inhibitors have been discovered.
119
Because these substances specifically inhibit leukotriene formation, they have been
used effectively to evaluate the extent of leukotriene involvement in pathological
conditions. Investigations have demonstrated selective inhibition of 5-lipoxygenase
by the coumarin derivative esculetin (6,7-dihydroxycoumarin), a component of
extracts of the bark of Aesculus hippocastanum and Fraxinus japonica (164). The
latter extract, called Shinpi, has been used in oriental medicine as an analgesic
and has been shown to have acute antiinflammatory activity (165). Sekiya et al.
(165) studied the effects of esculetin and related coumarins on platelet
lipoxygenases and found esculetin to be a potent lipoxygenase inhibitor.
Cyclooxygenase activity was stimulated. Neichi et al. (166) demonstrated a dosedependent inhibition of 5-lipoxygenase in mouse mastocytoma cells with esculetin
pretreatment; the cyclooxygenase product, 5-HETE, was increased. The latter was
attributed to scavenging by esculetin of oxygen radicals that inhibit phospholipase
activity. Inhibition of 5-lipoxygenase activity in PMNs has also been demonstrated
(167).
Numerous studies have identified the liver as a major source of leukotrienes and
the primary organ for leukotriene detoxification and elimination. Studies with
labeled leukotrienes have shown a very rapid removal from plasma by the liver.
Denzlinger et al. (154) measured a plasma t1/2 of injected [3H]LTC4 of 30 seconds,
with most being removed by the liver and secreted in bile. Appelgren and
Hammarstrom (168) used autoradiography to follow the elimination of leukotriene
120
C3 in the mouse. Injected LTC3 rapidly accumulated in the liver and bile, with
60% of injected radioactivity appearing in the feces. In the isolated liver, Ormstad
et al. (169) showed that 80% of [3H]LTC3 had been removed from the perfusate
by 30 minutes. Radioactivity was detected in bile at 10 minutes. The isolated
kidney also removed LTC3 but at a slower rate (169).
Mechanisms of hepatic transport of leukotrienes have had limited investigation.
Uptake of LTC3 by hepatocytes was temperature and ATP-dependent, indicating
an active process (155,169). Following uptake, leukotrienes bind ligandin which
may facilitate transfer from blood to bile. Sun et al. (170) documented binding
of LTC4 to the Mr 23,000 subunit 1 of the dimeric glutathione-S-transferase;
bilirubin competed for this binding (170), as did BSP (171). Canalicular secretion
of leukotrienes has not been studied.
In addition to its role in leukotriene elimination per se, the liver also has an
important role in leukotriene detoxification.
Detoxification of the cysteinyl
leukotrienes is accomplished by conversion of LTE4, which is still fairly potent, to
the inactive N-Acetyl-LTC4 (LTE4-NAc) derivative.
Hagmann et al. (141)
identified this derivative as the major leukotriene metabolite in rat bile. LTE4NAc is formed via the mercapturic acid pathway, which is an important metabolic
route for exogenous toxicants (141). This conversion has been demonstrated in
isolated hepatocytes as well as in vivo (172)
and is catalyzed by cysteine-S-
121
conjugate-N-acetyl transferase (EC 2.3.1.80) (142).
Because of its central role in leukotriene synthesis, detoxification, and elimination,
during conditions of increased leukotriene production and/or decreased excretory
capacity the liver can become a target organ of leukotriene toxicity.
The potential involvement of leukotrienes in liver disease has been studied fairly
extensively (140,145,146,173).
Many of these studies have utilized the
endotoxin/galactosamine model. Endotoxins are lipopolysaccharides from gram
negative bacteria that cause widespread hepatic necrosis, inflammatory infil-
tration, and cholestasis.
Treatment with endotoxin increases synthesis of
leukotrienes while it decreases elimination (145,155,174). Hagmann et al. (155)
studied the elimination of [3H}LTD4 in endotoxin-treated mice.
Endotoxin
treatment resulted in a dose- and time-dependent inhibition of elimination, which
was much more than could be accounted for by the decreased bile flow. The
decreased elimination was attributed to inhibited canalicular secretion, as the
bile/liver ratio of leukotrienes was decreased.
Inhibition of RNA synthesis sensitizes the liver to endotoxin. D-galactosamine,
which depletes UTP (175) and is a liver-specific inhibitor of RNA synthesis,
increases hepatic sensitivity to endotoxin thousands of times (155). Livers from
mice treated with D-galactosamine + endotoxin (Ga1N /E) show a normal pattern
122
in the immediate periportal areas but fulminant necrosis in the central areas
(173). Serum enzymes are also markedly increased.
Though a mechanistic basis for GaIN/E-induced liver injury has not been
established, there is evidence that leukotriene-mediated ischemia/hypoxia and/or
reperfusion injury is involved. Under normal conditions, periportal cells may be
exposed to 100 ,uM 02 while central cells only receive 1-5 ,uM (176).
Vasoconstriction with leukotrienes may further decrease oxygen supply to central
hepatocytes, leading to the centrizonal necrosis characteristic of GaIN/E exposure.
Hypoxic cells are more sensitive to leukotrienes than normoxic cells (176).
Wendel et al. (177) demonstrated that iloprost, a potent vasodilator, was
protective when given simultaneously with endotoxin but not 90 minutes later; a
similar protective effect with the xanthine oxidase inhibitor allopurinol and the
reactive oxygen scavenging enzymes superoxide dismutase and catalase suggested
to these authors that oxygen radicals, produced during the reperfusion phase
following transient endotoxin/leukotriene-induced vasoconstriction/hypoxia, may
be responsible for leukotriene-mediated liver injury. Krell et al. (178) studied the
effects of LTC4 on the isolated perfused rat liver. Decreased 0, consumption,
increased portal pressure, increased glucose and lactate efflux, and a small
decrease in bile flow were observed. The decreased oxygen consumption was
reversed with the vasodilators nitroprusside and isoproterenol. Changes were
attributed to microcirculatory redistribution of perfusate flow and subsequent
123
changes in oxygen supply.
These authors hypothesized that the long-term
deleterious effects of leukotrienes may result from ischemia and hypoxia (178).
The protective effect of leukotriene synthesis inhibition has been studied in the
Ga1N /E model.
Various studies have shown protection of GaIN/E-induced
hepatocellular necrosis, lethality, and inflammatory infiltration with phospholipase
and/or lipoxygenase, but not cyclooxygenase, inhibition (146,155,173). Tiegs et al.
(173) protected mice from GaIN/E-induced hepatitis with dexamethasone
pretreatment. Depletion of GSH and inhibition of gamma glutamyl transferase
were also effective, indicating cysteinyl leukotriene involvement. Hagmann et al.
(155) demonstrated protection of GaIN/E-induced lethality, cholestasis and
[3H]LTD4 retention with dexamethasone, FPL 55712 (a selective antagonist of
cysteinyl leukotrienes), and diethylcarbamazine (an inhibitor of leukotriene
biosynthesis). Indomethacin was only partially protective.
In the present studies, histological evaluation of livers from BCNU- and ANIT-
treated rats revealed necrosis, edema, fibrin deposition, and inflammatory cell
infiltration in portal areas (Chapter 7).
Accordingly, an investigation was
undertaken to evaluate the potential role of inflammatory mediators in the
hepatoxicity of these compounds. Assessment of liver function parameters and
124
histologic evaluation (below) following pretreatment/cotreatment with
the
corticosteroid triamcinolone, the cyclooxygenase inhibitor indomethacin, and the
5-lipoxygenase inhibitor esculetin provided evidence that certain of the hepatotoxic
effects of ANIT and BCNU may be leukotriene-mediated.
Methods
Rats received the following treatments (see General Methods): 1) triamcinolone,
2.0 mg/kg, 24 hours before and after BCNU treatment or 24 hours before and 12
hours after ANIT treatment; 2) esculetin, 1.2 mg/kg, 30 minutes before and at
6-hour intervals after BCNU or ANIT treatment; or 3) indomethacin, 5 mg/kg,
one hour before and at 8-hour intervals after BCNU or ANIT treatment. Livers
were perfused 48 hours after BCNU treatment or 24 or 48 hours after ANIT
treatment. Bile and perfusate samples were collected as indicated. Bile flows,
bile P and BSP clearances were determined as previously described.
Results
Protective effects of eicosanoid synthesis inhibition on BCNU-and ANIT-induced
cholestasis and permeability changes.
The effects of triamcinolone (TCN),
indomethacin (INDO), and esculetin (ESC) treatment on BCNU- and ANITinduced changes in bile flow and bile P, are shown in Tables 6 & 7. Treatment
1.2.5
with triamcinolone or esculetin alone did not result in bile flows or
P,
concentrations significantly different from controls; indomethacin significantly
increased bile flow in vivo. Livers from rats receiving the corticosteroid TCN and
perfused 48 hours after BCNU treatment (Table 6) or 24 hours after ANIT
treatment (Table 7) had normal bile flows; bile P, was significantly higher than
with BCNU or ANIT treatment alone.
Treatment with the cyclooxygenase
inhibitor indomethacin reversed BCNU-induced cholestasis in vivo but otherwise
did not change bile flows or P, from non-pretreated animals.
In contrast,
treatment with the lipoxygenase inhibitor esculetin eliminated the cholestasis
induced by either BCNU or ANIT(24h) and significantly decreased bile P,. Livers
from rats treated with esculetin and perfused 24 hours after ANIT treatment had
bile P, concentrations not significantly different from controls.
Protective effect of eicosanoid synthesis inhibition on BCNU-and ANIT-induced
BSP retention. The effects of TCN, ESC, and INDO treatment on BCNU- and
ANIT-induced BSP retention are presented in Figures 29 through 35. BSP decays
for TCN (Figure 29), ESC (Figure 32), and INDO (Figure 34) controls were not
different from corn oil controls. TCN treatment significantly decreased BCNUand ANIT-induced retention (equilibrium perfusate concentrations: 3.8 ,uM and
2.2 ktM for BCNU/TCN and ANIT/TCN, respectively, compared with 12.4 ,uM
126
TABLE 6. Effect of eicosanoid synthesis inhibitors on BCNU-induced cholestatic
and permeability changes. Rats were treated with 1) triamcinolone (TCN), 2.0
mg/kg, 24 hours before and after BCNU treatment; 2) esculetin (ESC), 1.2 mg/kg,
1/2 hour before and at 6 hour intervals after BCNU treatment; or 3) indomethacin
(INDO), 5 mg/kg, one hour before and at 8 hour intervals after BCNU treatment.
Livers were perfused 48 hours after BCNU treatment.
TREATMENT
CONTROL
TCN
INDO
ESC
BCNU
BCNU/TCN
BCNU/INDO
BCNU/ESC
Bile Flowa
IN VIVO
PERF LIVER
1.82
1.70
2.20
1.95
0.98
1.85
1.95
2.01
0.04
0.08
0.13
0.03
0.10c
0.24d
0.39d
0.23d
0.97
0.83
0.83
0.81
0.51
0.92
0.37
0.82
Values are means + SE; n = 3-6.
a,uL/min/g liver
bmM.
`Significantly different from control, P < 0.05
'Significantly different from BCNU alone, P < 0.05.
.05
.07
.20
.13
.05c
.12d
.05c
.07d
p ib
0.17
0.09
0.12
0.18
1.52
1.71
1.47
1.05
. 0 2
.03
. 03
.05
03c
.03c,d
.
.
08c
.23c,d
127
TABLE 7. Effect of eicosanoid synthesis inhibitors on ANIT-induced cholestatic
and permeability changes. Rats were treated with 1) triamcinolone (TCN), 2.0
mg/kg, 24 hours before and 12 hours after ANIT treatment; 2) esculetin (ESC), 1.2
mg/kg, 1/2 hour before and at 6 hour intervals after ANIT treatment; or 3)
indomethacin (INDO), 5 mg/kg, one hour before and at 8 hour intervals after ANIT
treatment. Livers were perfused 24 or 48 hours after ANIT treatment.
TREATMENT
CONTROL
TCN
INDO
ESC
ANIT(24h)
ANIT(48h)
ANIT(24h)/TCN
ANIT(24h)/INDO
ANIT(24h)/ESC
ANIT(48h)/ESC
p
Bile Flowa
IN VIVO
PERF LIVER
1.82
1.70
2.20
1.95
0.58
0.04
0.08
0.13
0.03
0.12c
0
2.02
0.98
2.00
0.37
0.97
0.83
0.83
0.81
0.22
+
+
+
+
+
0.05
0.07
0.20
0.13
0.06c
0.17
0.09
0.12
0.18
1.38
0.20d
0.10c
0.13d
0.03c
1.63
1.56
0.27
0.61
+
+
+
0.12d
0.16c
0.12d
0.12c
1.00
0.17
0.89
0.10
+
+
+
+
+
.02
.03
.03
.05
.08c
ND
0
±
b
±
+
+
+
Values are means + SE; n = 3-6.
a,uL/min/g liver
bnim.
'Significantly different from control, P < 0.05
dSignificantly different from ANIT alone, P < 0.05
ND: not determined.
+
+
+
.05c'd
.08c
.06d
+ 0.12c
128
25.0
0-0 CONTROL
o -o
20.0
TON
BCNU
0-0 BCNU/TCN
rf37
mv.)
15 0
1)-
LJ
10.0
Li)
LL
E 5.0
0.0
0
111-4.--t
10
7
e\
20
1
30
40
50
60
70
TIME (MIN)
Figure 29. Decreased BCNU-induced perfusate BSP retention with triamcinolone
treatment. Rats were treated with triamcinolone (TCN), 2.0 mg/kg, 24 hours
before and after treatment with corn oil (1.0 ml/kg) or BCNU (26 mg/kg). Livers
were perfused 48 hours after corn oil or BCNU treatment with recirculation of the
effluent and BSP (5 sumo') was added to the perfusate reservoir as a bolus.
Perfusate samples were collected at 2.5, 5, 10, 15, 20, 25, 30, 35, 40, 50, and 60
minutes and assayed for BSP as described. Values are means ± SE; n = 3. No
significant difference was observed between TCN controls and corn oil controls.
A significant difference (P < 0.05) in BSP perfusate retention was observed
between livers from rats receiving TCN + BCNU and those receiving BCNU
alone at all time points after 21/2 minutes. Open symbols: influent; filled symbols:
effluent.
129
25.0
0
0 0 CONTROL
\T
TCN
0 0 ANIT
0
I,
0 AN IT/TCN
aT
gal 15.0-
1\T
iii
Q 10.0
------
o
W
LLJ
0
_.... I
r:]_.__Ii.....--
5.00.0
i
;
*:"-A
0
t
10
i
8
20
,
30
1
40
50
60
70
TIME (MIN)
Figure 30. Decreased ANIT-induced perfusate BSP retention with triamcinolone
treatment. Rats were treated with triamcinolone (TCN), 2.0 mg/kg, 24 hours
before and 12 hours after treatment with corn oil (1.0 ml/kg) or ANIT (250 g/kg).
Livers were perfused 24 hours after corn oil or ANIT treatment with recirculation
of the effluent and BSP (5 ,umol) was added to the perfusate reservoir as a bolus.
Perfusate samples were collected at 2.5, 5, 10, 15, 20, 25, 30, 35, 40, 50, and 60
minutes and assayed for BSP as described. Values are means ± SE; n = 3. No
significant difference was observed between TCN controls and corn oil controls.
A significant difference (P < 0.05) in BSP perfusate retention was observed
between livers from rats receiving TCN + ANIT and those receiving ANIT alone
at all time points. Open symbols: influent; filled symbols: effluent.
130
..---,
k_
(')
1 0. 0
CP
c 8.0
E
-6
E
c 6.0
.........,
z0
17--
Li
it
4.0
CC
C_)
X
LLJ
m
2.0
u-)
m
x<
T
N\
0.0
CONTROL
TCN
BCNU
ANIT
TCN/BCNU TCN/ANIT
Figure 31. Increased BSP excretion in BCNU- and ANIT-treated livers with
triamcinolone treatment. Rats were treated with triamcinolone (TCN), 2.0 mg/kg,
24 hours before and after BCNU treatment (26 mg/kg, i.p.) or 24 hours before
and 12 hours after ANIT treatment (250 mg/kg, gavage). Livers were perfused
48 hours after BCNU treatment or 24 hours after ANIT treatment with
recirculation of the effluent and BSP (5 ymol) was added to the perfusate
reservoir as a bolus. Bile samples were collected at 10, 20, 30, 40, 50, and 60
minutes and assayed for BSP as described. BSP excretion was determined as the
product of maximal bile [BSP] and bile flow. Values are means ± SE; n = 3.
*Significantly different from non-cotreated, P < 0.05.
131
25.0
20.0
0 -0 CONTROL
A
A ESC
0-0 ESC/ANIT
O
O ESC/BCNU
can 15.0
CO
n
T
10.0
r
ao 01
_.L.L.1
0_
5.0
1
7
0.0
10
20
111
30
40
50
60
70
TIME (MIN)
Figure 32. Reversal of ANIT-induced BSP retention with esculetin treatment.
Rats were treated with esculetin, (ESC), 1.2 mg/kg, 1/2 hour before and at 6-hour
intervals after treatment with BCNU (26 mg/kg, i.p.) or ANIT (250 mg/kg,
gavage). Livers were perfused 48 hours after BCNU treatment or 24 hours after
ANIT treatment with recirculation of the effluent and BSP (5 pmol) was added
to the perfusate reservoir as a bolus. Perfusate samples were collected at 2.5, 5,
10, 15, 20, 25, 30, 35, 40, 50, and 60 minutes and assayed for BSP as described.
Values are means ± SE; n = 3. No significant difference in BSP clearance was
observed between livers from corn oil and esculetin controls. Esculetin treatment
eliminated ANIT-induced BSP retention but had no effect on BCNU-induced
retention. Open symbols: influent; filled symbols: effluent.
132
0-0 CONTROL
ESC
AN1T/ESC
BCNU /ESC
TIN
E (MIN)
Figure 33. Normal BSP excretion following treatment with ANIT and esculetin.
Rats were treated with esculetin, (ESC), 1.2 mg/kg, '1/2 hour before and at 6-hour
intervals after treatment with BCNU (26 mg/kg, i.p.) or ANIT (250 mg/kg,
gavage). Livers were perfused 48 hours after BCNU treatment or 24 hours after
ANIT treatment with recirculation of the effluent and BSP (5 ymol) was added
to the perfusate reservoir as a bolus. Bile samples were collected at 10, 20, 30,
40, 50, and 60 minutes and assayed for BSP as described. Values are means ± SE;
n = 3. No significant difference in bile [BSP] was observed between livers from
corn oil or esculetin controls. BSP excretion in livers from rats receiving ANIT
+ ESC was not significantly different from controls. BSP excretion in livers from
rats receiving BCNU + ESC was not significantly different from that of BCNU
alone.
133
25.0
0
0 CONTROL
A INDO
A
0
0 INDO/ANIT
0 INDO/BCNU
O
Cr;
m
I-J
15.0
(.1) 10.0
D
a_
5.0- inly
\
T,
0. 0
0,
I
0
10
I ----.°
20
*-A-41
30
40
4
50
4
60
70
TIME (MIN)
Figure 34. No change in BCNU- or ANIT-induced perfusate BSP retention with
indomethacin treatment. Rats received indomethacin (INDO), 5 mg/kg, one hour
before and at 8-hour intervals after BCNU or ANIT treatment. Livers were
perfused 48 hours after BCNU treatment or 24 hours after ANIT treatment with
recirculation of the effluent and BSP (5 ,umol) was added to the perfusate
reservoir as a bolus. Perfusate samples were collected at 2.5, 5, 10, 15, 20, 25, 30,
35, 40, 50, and 60 minutes and assayed for BSP as described. Indomethacin treatment had no effect on ANIT- or BCNU-induced BSP retention. Open symbols:
influent; filled symbols: effluent.
134
25.0
0 0 0 CONTROL
a
a 20.0
A
A ESC
D ESC/ANIT
a
can 15.0
m
LJ
<
(f)
10.0
L_
LJ
fa_
5.0
0.0
bfp
0
10
20
30
A
t
40
50
60
70
TIME (MIN)
Figure 35. Lack of a protective effect toward increased perfusate BSP retention
in livers from rats receiving esculetin and perfused 48 hours after ANIT treatment. Rats were treated with esculetin, (ESC), 1.2 mg/kg, 1/2 hour before and at
6-hour intervals after ANIT treatment (250 mg/kg, gavage). Livers were perfused
48 hours after ANIT treatment with recirculation of the effluent and BSP (5 ymol)
was added to the perfusate reservoir as a bolus. Perfusate samples were collected
at 2.5, 5, 10, 15, 20, 25, 30, 35, 40, 50, and 60 minutes and assayed for BSP as
described. No significant difference in perfusate BSP retention was observed
between livers from rats receiving ESC + ANIT and rats receiving ANIT alone.
Open symbols: influent; filled symbols: effluent.
135
for BCNU alone and 13.43 for ANIT alone) (Figures 29 and 30). Though the
increase in bile [BSP] with TCN treatment was not significant due to relatively
large standard deviations, a significant increase in maximal BSP excretion was
observed (Figure 31). TCN treatment appeared to have a greater protective effect
on ANIT-treated rats than on BCNU-treated rats; however, there was insufficient
bile flow in rats receiving ANIT alone to determine BSP excretion.
Esculetin dramatically reversed the effect of ANIT on BSP excretion in livers
perfused 24 hours after ANIT treatment. Perfusate (Figure 32) and bile (Figure
33) [BSP] were not significantly different from controls. In contrast, treatment
with esculetin did not affect BCNU-induced BSP retention (equilibrium perfusate
concentrations: 11.7 ,uM for ESC/BCNU vs. 12.4 uM for BCNU alone) (Figures
32 and 33). Indomethacin treatment did not change equilibrium perfusate [BSP]
with either ANIT(24h) or BCNU treatment (Figure 34). Insufficient bile flow
precluded measurement of bile [BSP] in both cases.
Lack of a protective effect of esculetin on ANIT-induced hepatic changes at 48
hours. The protective effect of esculetin treatment on ANIT-induced toxicity did
not extend to 48 hours. At this time, cholestasis and increased bile P, were again
evident (Table 7). BSP retention 48 hours after ESC/ANIT was not different
3Average for final twenty minutes; equilibrium perfusate concentrations were
not attained with ANIT.
136
from that of ANIT alone (Figure 35).
Discussion
The present studies provide fairly strong evidence for leukotriene involvement in
certain hepatotoxic effects of ANIT and BCNU. Treatment with the lipoxygenase
inhibitor esculetin reversed ANIT-induced cholestasis and permeability (Table 7);
perfusate retention of BSP was also significantly reduced (Figure 32)4. Treatment
with the cyclooxygenase inhibitor indomethacin was not protective. The dual
cyclooxygenase/ lipoxygenase inhibitor triamcinolone also reversed ANIT-induced
cholestasis. Neither ESC nor TCN alone were choleretic (Table 6). Generally
similar results were obtained with BCNU, though esculetin treatment did not
protect against BCNU-induced BSP retention. The reason for the selective
reversal of BCNU-induced cholestasis in vivo with indomethacin is unclear. A
similar effect was observed when BCNU-treated rats were pretreated with
phenobarbital (above). It is possible that the mild choleretic effect of
indomethacin was sufficient to counter the cholestatic effect of BCNU in vivo
(Table 6). Choleresis was only observed with indomethacin treatment in vivo.
4As was noted in the introduction to this chapter, esculetin is a component of
a bark extract called "Shinpi", which is used in oriental medicine. Interestingly, a
recent study (179) demonstrated several other bark extracts used in Chinese
medicine are protective against ANIT-induced cholestasis and liver injury.
137
Evidence for leukotriene involvement in cholestasis has been presented in other
studies (139,140,145,146,155). Though a mechanistic basis for this effect has not
been established, inhibited canalicular secretion of essential bile constituents, as
mentioned above, may be a factor. The locus of this inhibition could be a
canalicular transporter (155) or, alternatively, cytosolic binding proteins.
Competitive binding of ligandin by LTC4 and bilirubin (170) and LTC4 and BSP
(171) has been documented. Leukotriene-induced cholestasis may also be related
to edema in portal
tracts with subsequent impingement on bile ducts
(25,140,146,155). Hua et al. (149) observed extensive extravasation in guinea pig
portal areas following LTC4 and LTD4 administration. Substantial edema and
fibrin leakage in portal areas were observed in the present studies following
BCNU and ANIT treatment (Chapter 7). Fibrin and edema were reduced with
triamcinolone and esculetin cotreatment, particularly in the case of ANIT. Edema
was unchanged or increased with indomethacin cotreatment.
The decrease in BCNU- and ANIT-induced paracellular permeability (bile P,)
with esculetin but not indomethacin treatment suggests a leukotriene-mediated
event. However, treatment with the dual cyclooxygenase/lipoxygenase inhibitor
triamcinolone significantly increased bile P,.
Though this was an unexpected
finding, it may be explained mechanistically in terms of concomitant decreases in
hepatotoxic leukotrienes and cytoprotective prostaglandins. Prostaglandins have
been shown to be cytoprotective in other studies. PGE administration protected
138
against hepatic lesions induced by CCL4, D-galactosamine, hepatitis virus, and
ANIT (180,181).
Ruwart et al. (181) showed that 16,16-dimethyl-PGE2
administration protected rats against ANIT-induced elevated serum enzymes, bile
duct necrosis, and inflammatory infiltrations. Though the etiological progression
of hepatotoxic effects of BCNU and ANIT is not entirely clear, morphologic
changes (below) suggest that the initial event is damage to biliary epithelial cells
with subsequent bile duct necrosis, as postulated by Ahmed et al. for CCNUinduced hepatotoxicity (127). Damage may be due to direct action of the drug
or a metabolite but may also be mediated by a leukotriene. Evidence for the
latter is the protection afforded by the lipoxygenase inhibitor esculetin (total
protection in the case of ANIT and partial in the case of BCNU) and lack of
protection in either case with indomethacin treatment (below). It is also possible
that protection observed with lipoxygenase inhibition is due to a shift of the
arachidonic acid to the cyclooxygenase pathway with a resultant increase in
prostaglandins. Increased prostaglandin concentrations could be protective against
the necrosis in a manner similar to that observed in the studies referenced above.
Cotreatment with triamcinolone did not reduce bile duct necrosis.
Damage to bile ducts may be the initiating event for the portal inflammation
observed with BCNU and ANIT treatment. Leukotrienes, released from resident
or recruited mast cells and or/infiltrating PMNS (Chapter 7), may be responsible
for the subsequent extravasation from portal venules. BCNU- and ANIT-induced
139
edema and fibrin deposition were reduced or eliminated with esculetin treatment,
somewhat reduced with triamcinolone treatment, and unchanged or reduced with
indomethacin treatment. These results are also consistent with prostaglandin
involvement.
As mentioned above, vasodilator prostaglandins potentiate
leukotriene-mediated extravasation (139).
The increase in paracellular permeability appears to be secondary to the portal
inflammation induced by ANIT and coincident with the portal inflammation
induced by BCNU. Marked inflammatory changes were observed histologically
12 hours after ANIT treatment (below) though bile P, was not significantly
elevated above controls at this time (Figure 11).
With BCNU, portal
inflammation was not apparent until 36 hours, when bile P, was significantly
elevated (Figure 10). The increased P, may be a result of centrizonal hypoxia.
Microcirculatory changes subsequent to portal edema and/or vasoconstriction by
leukotrienes may be decreasing blood flow and 0, supply to central areas. These
changes could be increasing centrizonal hypoxia to the point of damage. Though
no pathological changes to central hepatocytes were observed with BCNU or
ANIT treatment in the present work (Chapter 7) the lanthanum studies revealed
a substantially greater occurrence of canalicular penetration in central than in
portal areas. During HRP infusions, occasional accidental anoxic conditions
(death of rat immediately prior to perfusion, brief cessation of oxygen flow)
greatly increased bile HRP (observation; data not shown). The significant increase
140
in P, with TCN cotreatment over ANIT or BCNU alone could be due to a
decrease in the formation of cytoprotective prostaglandins. As demonstrated in
other studies (139), vasodilatation by prostaglandins may counter the vasocon-
strictive effects of the leukotrienes. Consistent with this hypothesis was the
observation that inhibition of prostaglandin synthesis with indomethacin
cotreatment induced a mild centrilobular necrosis; this was not observed with
other treatments. It is noteworthy that TCN/ANIT and TCN/BCNU treatments
also resulted in a decrease in portal inflammatory infiltrate (Chapter 7). Cysteinyl
leukotrienes are deactivated in vitro by myeloperoxidase released from activated
neutrophils and monocytes (182) and by hydroxyl radicals from neutrophils during
a respiratory burst (183). Steroid antiinflammatory drugs have also been shown
to stabilize inflammatory cell membranes, inhibiting release of cytoplasmic
contents (184).
These studies provide some evidence that BSP retention following BCNU or
ANIT treatment may be leukotriene-mediated.
Cotreatment with TCN
significantly reduced BSP retention 48 hours after BCNU treatment and 24 hours
after ANIT treatment (Figures 29 and 30). This was not simply an additive effect,
as TCN alone did not increase BSP excretion over corn oil controls (Figure 31).
TCN cotreatment appeared to alter the metabolic profile of BSP in bile (Figure
24). Esculetin had an even greater protective effect than TCN on BSP retention
in livers from 24-hour ANIT rats (Figures 32 and 33). However, no significant
141
difference in BSP retention was observed between rats treated with BCNU/ESC
and BCNU alone. Indomethacin did not alter BSP retention with BCNU or
ANIT. Impaired BSP excretion has been associated with leukotrienes in other
studies.
Endotoxin treatment induced BSP retention in humans (185); multi-
compartmental analysis indicated that this retention was due to reflux secondary
to decreased hepatic storage capacity. Similar results were observed in the
isolated liver (121). In the latter study, indocyanine green excretion was also
reduced, indicating that metabolic alteration was not a factor. These results are
consistent with a decrease in binding protein activity. Evidence was presented in
chapter 5 for decreased ligandin binding capacity and subsequent sinusoidal efflux
as a mechanistic component of ANIT- and/or BCNU-induced BSP retention.
However, though TCN treatment protected against BCNU-induced BSP retention
(Figure 29) esculetin did not (Figure 32). These results suggest that leukotrienes,
though they appear to have a role in ANIT-induced BSP retention, may not be a
major factor in the retention induced by BCNU.
The protective effects of esculetin on ANIT-induced cholestasis, P and BSP
retention were not due to altered metabolism and/or distribution of ANIT. The
increase in ANIT hepatotoxicity observed with phenobarbital pretreatment
(chapter 5) and other reports indicate that the toxic effects of ANIT are mediated
by a metabolite; thus, a change in metabolic activity or distribution has to be
considered with a protective agent. However, no change in BSP metabolism was
142
observed with ESC cotreatment (Figure 24); additionally, livers from rats treated
with esculetin and perfused 48 hours after ANIT treatment had bile flows and BSP
excretory capacities not significantly different from ANIT alone (Table 7; Figure
35); bile Po though still lower than that observed with ANIT, was significantly
higher than controls (Table 7). It thus appears that inhibiting the synthesis of
leukotrienes by esculetin is protective in the short term only. Though too little is
known about esculetin to provide an explanation for this short-term effect, it is
possible that induction of leukotriene receptors or esculetin-metabolizing enzymes
is occurring.
In addition to the evidence for leukotriene involvement in ANIT- and BCNUinduced liver injury, these studies also provided further support for the hypothesis
that cholestasis and BSP retention are not related to permeability changes.
Though TCN treatment potentiated BCNU- and ANIT-induced increases in bile
P it protected against BCNU- and ANIT-induced cholestasis and BSP retention.
In conclusion, these preliminary results provide evidence for leukotriene
involvement in BCNU- and ANIT-induced cholestasis and permeability changes
and in ANIT-induced BSP retention. These studies also provide additional
support for increased paracellular permeability and cholestasis/BSP retention
being separate events.
143
IX. ANIT- AND BCNU-INDUCED LIVER HISTOPATHOLOGY
Histopathologic changes in the liver following BCNU treatment have had limited
investigation. Thompson and Larson (97) reported changes induced by 30 mg/kg
BCNU in the rat. A progressive lesion was observed, with pericholangitis evident
at 3-4 days followed by increased fibroblastic activity and connective tissue
deposition. Bile duct proliferation was observed 63 days posttreatment. Larson
and Rall (186) reported similar changes, with thickening of hepatic blood vessel
walls and obliteration of bile ductules. Ahmed et al. (127) and Kretschmer et al.
(187) evaluated rat hepatic morphology following administration of 1-(2chloroethyl)-3-cyclohexy1-1-nitrosourea (CCNU), a less potent congener of BCNU.
Edema, fibrin leakage, and PMN infiltration were observed in larger portal areas
as early as 6 hours after treatment. At 24 hours, necrotic bile ducts and epithelial
sloughing were noted. Focal hepatocellular necrosis was also observed. The latter
was limited to small clusters of hepatocytes adjacent to altered bile ducts and was
considered a secondary event.
Electron microscopic examination revealed
widened intercellular spaces between bile duct epithelial cells. Bile ductules were
normal. Canaliculi were dilated with loss of microvilli; bile thrombi and lamellar
membranous whorls were also observed.
These investigators postulated that
CCNU is taken up preferentially by bile duct epithelial cells where an alkylating
moiety is formed; subsequent cell damage leads to cholestasis and regurgitation
of bile components across epithelial cells into portal lymphatics or sinusoids (127).
144
Changes in hepatic morphology following ANIT treatment have been fairly
extensively investigated. Eliakim et al. (cited by
69)
were the first to describe
ANIT-induced hepatic alterations. Twenty-four hours after a single treatment
increased numbers of granulocytes were observed in portal areas. Necrosis and
desquamation of bile ducts with mucus plug formation were also observed.
Mclean and Reese (cited by
in portal spaces
6
69)
reported edema and inflammatory cell infiltration
hours after a single dose of ANIT.
hepatocytes was also noted. Goldfarb et al.
(188)
Some damage to
described similar changes. In
the latter study, necrosis had decreased substantially by
48
hours and at
19
days
livers appeared normal. Chronic feeding (1:1000 in food) resulted in similar
inflammatory changes with increased fibroblastic activity at 2 weeks and fibrosis
at 7 weeks. Moran et al.
changes.
(189)
and Desmet et al. (cited by
Ultrastructurally, Schaffner et al.
(190)
69)
reported similar
reported mitochondrial and
Golgi changes in portal hepatocytes and bile ductular cells as early as 3 hours
after a single dose (100 mg/kg). Endothelial swelling, canalicular dilatation,
increased ER, and glycogen depletion were also noted. Similar changes were
observed by Balazs et al. (cited by
69);
livers appeared normal by 7-10 days in the
latter study.
In a recent investigation by Connolly et al.
(191),
300 mg/kg ANIT resulted in
portal edema with inflammatory cell infiltration at 6 hours. At
8
hours some bile
duct damage was observed and numerous bile ducts were destroyed by 24 hours.
145
Focal necrosis of parenchymal cells and an increase in connective tissue were also
apparent.
Some
evidence
of regeneration was noted
at 48
hours.
Ultrastructurally, 4 hours after ANIT treatment bile ducts were dilated with loss
of microvilli. Vacuolation of endoplasmic reticulum and apparent "opening" of
bile duct epithelial cell tight junctions was observed at 6 hours.
Few
hepatocellular changes were noted. These authors concluded that ANIT was
exerting a direct toxic effect on bile duct lining cells resulting in mechanical
obstruction of bile ducts, cholestasis, and reflux of bile constituents.
The present histological evaluations were undertaken to further characterize and
compare the progression of hepatic changes induced by BCNU and ANIT and to
attempt to provide morphologic evidence for observed functional changes.
Methods
Rats were treated with BCNU (26 mg/kg, i.p.) or ANIT (250 mg/kg, gavage).
Livers were removed 24, 36, 48, 55, 60, or 72 hours after BCNU treatment or 12,
24, or 48 hours after ANIT treatment. Triamcinolone (TCN), esculetin (ESC),
indomethacin (INDO), and phenobarbital (PB) were administered as described
in chapter 6. For hematoxylin and eosin (H/E) analysis 1 mm liver sections were
placed in 10% neutral buffered formalin and prepared according to standard
146
methods.
Selected sections were stained with toluidine blue for mast cell
identification. Livers used for ultrastructural studies were perfusion-fixed with 25-
40 ml 2.5% glutaraldehyde/0.1 M cacodylate buffer and processed as previously
described (Chapter 2).
Results
Histopathologic changes following ANIT and BCNU treatment. Control livers had
tightly-adhering hepatocellular terminal plates; bile ducts and vessels were intact
with no visible edema (Figure 36). Few changes from controls were observed in
livers removed 24 hours after BCNU treatment, though occasional areas of
individual bile duct epithelial cell attenuation and necrosis with limited
periductular edema and inflammatory infiltrate were noted in larger portal areas
(Figure 37A). Thirty-six hours after treatment (not shown) most of the larger
portal areas showed partial necrosis of bile ducts, more extensive edema, and
occasional fibrin deposition.
observed.
Limited inflammatory cell infiltrate was also
No changes in hepatocytes were noted at 24 or 36 hours after
treatment. Forty-eight hours after BCNU administration bile duct necrosis was
often complete with total loss of epithelial cells and occasional basement
membrane as well (Figure 37B). Edema was extensive, often separating terminal
plates and extending into smaller portal areas. Condensed fibrin was observed
147
NIEV'mpet.,2.4afv,.. irms,
Figure 36. Control liver (H/E stain). Portal section from
a control liver showing
portal vein (V), artery (A), and bile duct
(B) x120.
148
Figure 37. Histopathologic changes with time following treatment with 26 mg/kg
BCNU (H/E stain). (A) Portal area 24 hours after BCNU treatment. Edema and
inflammatory infiltrate are limited. Bile duct (B) is intact (V: portal vein) x120.
(B) Portal area 48 hours after BCNU treatment. Necrosis of bile duct (B) is
complete, with sloughing of epithelium. Edema and inflammatory infiltrate are
extensive (V: portal vein) x120.
149
Figure 37. Histopathologic changes with time following treatment with 26 mg/kg
BCNU (H/E stain).
150
around bile ducts with occasional fibrin thrombi. Swelling and contraction of
portal radical endothelium was apparent, particularly adjacent to damaged bile
ducts. Lymphatics were often dilated. No arterial changes were noted. Extensive
infiltration of neutrophils, histiocytes, and mast cells were also observed. These
changes extended into the common bile duct (not shown). Occasional individual
hepatocellular necrosis was observed adjacent to the portal damage. Otherwise
hepatocytes appeared normal. Similar changes, with increasing severity, were
observed 55, 60, and 72 hours after treatment (not shown).
Though the time course differed, histological changes induced by ANIT treatment
were remarkably similar to those with BCNU. At 12 hours partial necrosis of
biliary epithelium was common.
Limited edema was observed (Figure 38A).
Edema did not extend into smaller portal spaces. No leakage of fibrin was
apparent. Inflammatory cell infiltration was moderate. At 24 hours bile duct
necrosis had progressed to complete in many of the larger portal areas (Figure
38B). Portal edema, with some fibrin deposition, was extensive but did not extend
to smaller portal spaces. Substantial inflammatory cell infiltrate was observed.
At 48 hours partial regeneration of bile duct epithelium was apparent, though
portal edema and inflammatory infiltrate were still extensive (below).
Altered histologic changes with triamcinolone, esculetin, phenobarbital, and
indomethacin cotreatment. Changes in histopathology when ANIT- and BCNU-
151
Figure 38. Histopathologic changes with time following treatment with 250 mg/kg
ANIT (H/E stain). (A) Portal area 12 hours after ANIT treatment. Interstitial
edema and inflammatory infiltrate are limited. Necrosis of bile duct (B) is
moderate. (V: portal vein) x120. (B) Portal area 24 hours after ANIT treatment.
Edema and inflammatory infiltrate are extensive. Necrosis of bile duct (B) is
complete, with sloughing of epithelium. (V: portal vein) x120.
152
Figure 38. Histopathologic changes with time following
treatment with 250 mg/kg
ANIT (H/E stain).
153
treated rats were cotreated with triamcinolone (TCN), esculetin (ESC), and
indomethacin (INDO) are shown in Tables 8 and 9. Two to five livers were
evaluated per treatment group. Three of the most severely affected portal areas
were chosen at low power (25x) for grading. Grading scale for inflammatory cells
ranged from 1-3, with 1 = 0-2 cells, 2 = 3-6 cells, and 3 = > 6 cells per high
power field (320x). Fibrin and edema were graded as either present or not (1 or
0). Bile duct necrosis was scaled as none = 0, partial (affecting only individual
cells) = 1, and complete = 2.
TCN did not markedly alter the bile duct necrosis, portal edema, or fibrin
deposition resulting from BCNU treatment (Table 8; Figure 39A). Inflammatory
cell infiltrate was reduced somewhat, with a substantial decrease in mast cell
numbers (below). Similar results were observed in livers from rats receiving
BCNU + ESC (Figure 39B). Treatment with BCNU + INDO and BCNU + PB
yielded histologic results not markedly different from BCNU alone (Table 8).
Livers from rats receiving TCN + ANIT(24h) had decreased inflammatory
infiltrate, decreased edema, and no fibrin (Table 9; Figure 40A). No bile duct
necrosis, edema, or fibrin were observed in livers from rats treated with ESC +
ANIT(24h); limited inflammatory infiltrate was observed (Figure 40B). Treatment
with INDO + ANIT(24h) and PB + ANIT(24h) resulted in livers with more
severe changes than with ANIT alone (Table 9). Livers removed from rats 48
hours after ANIT + ESC treatment were similar to those from rats treated with
154
Table 8. Change in inflammatory parameters with BCNU plus cotreatments.
TREATMENT
MC
IC
CONTROL
BCNU
BCNU/TCN
BCNU/ESC
BCNU/INDO
BCNU/PB
1.1
2.5
1.4
1.4
1.0
2.4
1.7
1.7
2.3
1.3
.5
1.6
0
0
.8
.7
.9
.5
1.0
1.9
1.7
1.3
1.8
1.3
Grading: 2-5 livers were evaluated per treatment group. 3 of the most severelyaffected portal areas were selected at low power (25x) and examined for grading in
a high power field (HPF; x320). Scale: mast cells (MC) and general inflammatory
cells (IC): 1 = 0-2; 2 = 3-6; 3 = > 6 per HPF; fibrin (F) and bile duct necrosis (N):
1 = present; 0 = not present.
155
Table 9. Change in inflammatory parameters with ANIT plus cotreatments.
TREATMENT
MC
IC
CONTROL
ANIT(24h)
ANIT/TCN
ANIT/ESC
ANIT/INDO
ANIT(12h)
ANIT(12h)/PB
ANIT(48h)
ANIT(48h)
/ESC
1.1
2.3
1.2
1.5
2.7
2.0
2.3
2.9
2.9
1.0
2.6
1.4
1.1
1.3
1.4
2.7
2.4
1.0
0
0
.5
1.7
1.3
1.0
2.0
0
0
0
.5
0
1.0
.7
1.0
2.0
1.3
1.3
Grading: 2-5 livers were evaluated per treatment group. 3 of the most severelyaffected portal areas were selected at low power (25x) and examined for grading in
a high power field (HPF; x320). Scale: mast cells (MC) and general inflammatory
cells (IC): 1 = 0-2; 2 = 3-6; 3 = > 6 per HPF; fibrin (F) and bile duct necrosis (N):
1 = present; 0 = not present.
156
Figure 39. Histopathologic changes in livers from rats treated with BCNU and
cotreated with triamcinolone or esculetin (H/E stain). Rats received
triamcinolone (TCN), 2.0 mg/kg, 24 hours before and after BCNU (26 mg/kg)
treatment or esculetin (ESC), 1.2 mg/kg, 1/2 hour before and at 6-hour intervals
after BCNU treatment. Livers were removed 48 hours after BCNU treatment.
(A) Portal area after BCNU + TCN treatment. Necrosis of bile duct (B) is
complete, with sloughing of biliary epithelium. Interstitial edema is extensive.
Inflammatory infiltrate is somewhat reduced (V: portal vein) x120. (B) Portal
area after BCNU + ESC treatment. Necrosis of bile duct (B) is complete and
interstitial edema extensive. Inflammatory infiltrate is reduced. (V: portal vein)
x120.
157
Figure 39. Histopathologic changes in livers from rats treated with BCNU and
cotreated with triamcinolone or esculetin (HIE stain).
158
Figure 40. Histopathologic changes in livers from rats
treated with ANIT and
cotreated with triamcinolone or esculetin. Rats received triamcinolone
(TCN), 2.0
mg/kg, 24 hours before and 12 hours after ANIT (250 mg/kg) treatment
or
esculetin (ESC), 1.2 mg/kg, 1/2 hour before and at 6-hour intervals after ANIT
treatment. Livers were removed 24 hours after ANIT treatment. (A) Portal area
after ANIT + TCN treatment. Necrosis of bile duct cells is
minimal. Little or
no edema or inflammatory infiltrate are apparent. (V: portal vein; B: bile
duct)
x120. (B) Portal area after ANIT + ESC treatment. Bile duct (B) is normal.
Little or no edema or inflammatory infiltrate can be seen. (V: portal vein) x120.
159
....lasmswoomellMINI3b
Figure 40. Histopathologic changes in livers from rats
treated with ANIT and
cotreated with triamcinolone or esculetin.
160
ANIT alone.
Mast cell number and activity with ANIT or BCNU: changes following TCN,
ESC, and INDO cotreatment. Mast cell grading was the same as that for other
inflammatory cells (1 = 0-2 cells, 2 = 3-6 cells, and 3 = > 6 cells). Few mast
cells were observed in control livers (Figure 41). Progressive increases in mast
cell number and degranulation were observed in portal areas 24 and 48 hours
after BCNU treatment (Figure 42) and 12 and 24 hours after ANIT (Figure 43).
These increases were partially inhibited with TCN or ESC cotreatment (Figures
44 and 45). Mast cell counts 48 hours after ANIT/ESC treatment were higher
than with ANIT alone (Figure 46). Livers from rats treated with BCNU + INDO
had fewer mast cells than with BCNU alone; no difference was observed in mast
cell numbers between rats treated with ANIT + INDO and those receiving ANIT
alone (Figure 47).
Discussion
These results are consistent with mast cell-derived inflammatory mediator
involvement in the hepatotoxicity of ANIT and, to a lesser extent, BCNU.
Inflammation is a biphasic response (192,193,194,195,196). The acute reaction,
initiated by various stimuli, lasts 30-60 minutes and is manifested by transient
161
Figure 41. Portal section from a control rat (toluidine
blue stain) A few resident
mast cells are visible in the interstitium (arrows). (V: portal
vein; A: artery; B:
bile duct) x320.
162
Figure 42. Histopathologic changes with time following
with 26 mg/kg
BCNU (toluidine blue stain). (A) Portal area 24 hourstreatment
after BCNU treatment.
Liver is similar to control. Mast cells are visible in
the connective tissue (arrows).
(V: portal vein A: artery; B: bile duct) x320. (B)
Portal area 48 hours after
BCNU treatment. Bile duct necrosis, edema, and
inflammatory cell infiltrate with
numerous mast cells (large arrows) are visible. Many of the
mast cells are in the
process of degranulating and dispersed granules can be seen (small arrows). (V:
portal vein B: bile duct; F: condensed fibrin) 320x.
163
Figure 42. Histopathologic changes with time
following treatment with 26 mg/kg
BCNU (toluidine blue stain).
164
Figure 43. Histopathologic changes with time following treatment with 250 mg/kg
ANIT (toluidine blue stain). (A) Portal area 12 hours after ANIT treatment.
Limited edema can be seen. Mast cells (arrows) are more numerous than in
controls and are less densely-staining, indicating activation. (V: portal vein; A:
artery; B: bile duct) x320. (B) Portal area 24 hours after ANIT treatment.
Extensive edema, bile duct necrosis, and inflammatory cell infiltrate can be seen.
Numerous mast cells (large arrows), many of which are degranulating, are also
apparent. Dispersed granules (small arrows) are scattered throughout. (V: portal
vein; A: artery; B: bile duct; N: neutrophils) x320.
165
Figure 43. Histopathologic changes with time following
treatment with 250 mg/kg
ANIT (toluidine blue stain).
166
Figure 44.
Histopathologic changes with BCNU + TCN or BCNU + ESC
Portal area after treatment with TCN + BCNU. Rats
were treated with TCN, 2.0 mg/kg, 24 hours before and after BCNU (26 mg/kg)
treatment and liver was removed 48 hours after BCNU treatment. Bile duct
necrosis, edema, and inflammatory cell infiltrate are visible. Numerous mast cells,
many of which are degranulating, can be seen (arrows). (A: artery; B: bile duct;
F: condensed fibrin) x320. (B) Portal area after BCNU + ESC treatment. Rats
were treated with ESC, 1.2 mg/kg, 1/2 hour before and at 6-hour intervals after
(toluidine blue stain)
.
(A)
BCNU (26 mg/kg) treatment and liver was removed 48 hours after BCNU
treatment. Bile duct necrosis, edema, and inflammatory cell infiltrate with
numerous mast cells (arrows) can be seen. Bile duct necrosis is not as severe as
with BCNU alone. (V: portal vein A: artery; F: condensed fibrin) x320.
167
Figure 44. Histopathologic changes
with BCNU + TCN or BCNU + ESC
(toluidine blue stain) .
168
Figure 45. Histopathologic changes with ANIT + TCN or ANIT + ESC (toluidine
blue stain). (A) Portal area after treatment with TCN + ANIT. Rats were
treated with TCN, 2.0 mg/kg) 24 hours before and 12 hours after ANIT (250
mg/kg) treatment and liver was removed 24 hours after ANIT treatment. Bile
duct necrosis, edema, and inflammatory cell infiltrate with mast cells (arrows) can
be seen. Bile duct necrosis is less severe than with ANIT alone. Mast cells are
more densely-staining, indicating a less-active state. Few dispersed granules can
be seen. (B: bile duct) 320x. (B) Portal area after treatment with ESC + ANIT.
Rats were treated with ESC, 1.2 mg/kg, 1/2 hour before and at 6-hour intervals
after ANIT (250 mg/kg) treatment and liver was removed 24 hours after ANIT
treatment. Liver is virtually identical to controls. A few densely-staining mast
cells can be seen (arrows). (V: portal vein; A: artery; B: bile duct) x320.
169
Figure 45. Histopathologic changes with ANIT + TCN or ANIT + ESC (toluidine
blue stain).
170
Figure 46. Histopathologic changes with ESC + ANIT(48h) (toluidine blue
stain). Rat received ESC, 1.2 mg/kg, 1/2 hour before and at 6-hour intervals after
ANIT (250 mg/kg) treatment; liver was removed 48 hours after ANIT treatment.
Bile duct necrosis, edema, and inflammatory cell infiltrate can be seen. Mast
cells, many of which are degranulating, are apparent (arrows). (A: artery; B: bile
duct; F: condensed fibrin) x320.
171
Figure 47. Histopathologic changes with BCNU + INDO or ANIT + INDO
(toluidine blue stain). (A) Rats received INDO, 5 mg/kg, one hour before and
at 8-hour intervals after BCNU (26 mg/kg) treatment; livers were removed 48
hours after BCNU treatment.
Extensive edema, bile duct necrosis, and
inflammatory cell infiltrate with numerous mast cells (large arrows) can be seen.
Many of the mast cells are in the process of degranulating, and dispersed granules
are visible (small arrows). (A: artery; B: bile duct; F: condensed fibrin) x320.
(B) Rats received INDO, 5 mg/kg, one hour before and at 8-hour intervals after
ANIT (250 mg/kg) treatment; livers were removed 24 hours after ANIT
treatment. Extensive bile duct necrosis, edema, and inflammatory cell infiltrate
with mast cells (large arrows) can be seen. Many of the mast cells are in the
process of degranulating and dispersed granules are visible (small arrows). (V:
portal vein; A: artery; B: bile duct) x320.
172
Figure 47. Histopathologic changes with BCNU + INDO or ANIT + INDO
(toluidine blue stain).
173
vasoconstriction followed by vasodilatation in the affected area. The latter results
in a local slowing of blood flow and margination of inflammatory cells. Contrac-
tion of postcapillary endothelial cells initiates the "late phase response", marked
in the early stages by extravasation of plasma, neutrophil and eosinophil infil-
tration, and fibrin deposition, and, later, by infiltration of macrophages and
fibroblasts. The late phase response generally lasts for 1-2 days; however, under
certain conditions, it may continue indefinitely, producing chronic inflammation
(196).
The involvement of mast cells in inflammation has been recognized for over a
century (197). Ubiquitous in the organism, mast cells predominate in loose
connective tissue surrounding blood vessels, nerves, and glandular ducts
(193,198,199). Activation of mast cells is generally initiated by cross linking of
mast cell surface Fc receptors by IgE antibody and subsequent increased calcium
influx; activated microtubules and microfilaments move granules to the cell
surface, and, within seconds, granules fuse with the plasma membrane and are
extruded, releasing an estimated 100 substances (193,199,200,201). Release of the
primary mediators of inflammation--histamine, eosinophil and neutrophil
chemotactic factors, and arachidonic acid derivatives--results in increased vascular
permeability, vasodilatation, and chemotaxis (194).
Infiltrating neutrophils,
eosinophils, and macrophages have been shown to release a factor (HRA-N;
neutrophil-derived histamine releasing factor) which induces further granule
174
release from mast cells (160,195). A cyclic process may thus ensue, with mast cell
activation leading to PMN infiltration and release of HRA-N leading to a
recrudescence of mast cell activation (160). Hydrolytic enzymes (e.g. acid and
neutral hydrolases), released during neutrophil death and during neutrophil and
macrophage phagocytosis, may further damage host tissue, contributing to a
chronic inflammatory condition (192).
The mast cell provides three sources of inflammatory mediators:
preformed
mediators, rapidly synthesized substances, and granule matrix constituents
(192,193,202,203,204,205).
Preformed mediators include the biogenic amines
histamine and--in the rodent--serotonin, chemotactic peptides (e.g. eosinophil
chemotactic factor of anaphylaxis) and various enzymes. Histamine increases
vascular permeability via vascular endothelial contraction, is chemotactic for
eosinophils (192,193), and activates fibroblasts (below).
Eicosanoids are
synthesized when mast cells degranulate. Pre-loading of mast cells with labeled
arachidonic acid results in the release of labeled eicosanoids. A parallel time
course has been observed for histamine and eicosanoid release with various
secretagogues, such as 48/80 (193,201). However, investigations with cytochalasin
(206) and certain lipoxygenase inhibitors (207) have demonstrated that release of
these mediators is separable. It now appears that cross-linking of mast cell surface
receptors by IgE molecules increases phospholipase A, activity and arachidonic
acid release; histamine is subsequently released by 5-lipoxygenase products (200).
175
There is also evidence that mast cells can induce eicosanoid synthesis in adjacent
tissues (198).
It has been known for some time that mast cells have an integral role in allergic
reactions (208,209). However, there is also increasing evidence for an etiologic
association between mast cells/mast cell mediators and various inflammatory
diseases, including those
of the
skin, joints, intestine, lung interstitium,
myocardium, and others (193,210). Numerous studies have implicated mast cells
in the pathogenesis of asthma (196,208) and in rheumatoid arthritis (193,211).
Balazs et al. (212) studied the involvement of mast cells in ulcerative colitis,
demonstrating a close correlation between mast cell numbers, mast cell
degranulation, and colitis activity. Gastric damage by ethanol (213,214,215) and
other agents has been associated with mast cell activity. Galli et al. (213) showed
that ethanol induced degranulation of gastric mucosal mast cells; mast celldeficient WBB6F1 -W /w mice developed less gastric injury than congenic normal
mice.
Mast cell stabilizers, such as sodium cromoglycate and FPL-52694,
protected against ethanol-induced gastric injury in the rat; indomethacin treatment
partially reversed this protection (214). Reimann et al. (215) demonstrated that
the synthetic PGE analog misoprostol decreased the gastric damage induced by
ethanol, aspirin, or stress. Plasma histamine and local mast cell counts were also
decreased following treatment. Perdue et al. (216) showed a correlation between
the extent of gut epithelial injury from the nematode parasite Nippostrongylus and
176
mucosal mast cell activity; a parallel elevation in leukotrienes LTB4, LTC4, and
LTE4 was also measured. Increased numbers of mast cells have also been found
in human gastric ulcers (213).
Lynes et al. (217) investigated mast cell
involvement in interstitial cystitis of the urinary bladder. A correlation was
demonstrated between mast cell density in the detrusor muscle and epithelial
inflammation and ulceration.
Release of proteolytic enzymes from mast cells was shown to contribute to
demyelination in the central and peripheral nervous systems (218). Release of
proteins from damaged myelin stimulated further mast cell degranulation. Mast
cell degranulation has also been demonstrated in the experimental demyelination
disease experimental allergic neuritis (218).
Cardiovascular toxicity induced by SK&F 101926, a vasopressor analog, has been
associated with mast cells (219). Macia et al. found that SK&F 101926 caused the
release of histamine from isolated rat peritoneal mast cells in vitro and increased
rat paw edema. The latter effect was decreased with the histamine/serotonin
antagonist cyproheptadine, which also protected against cardiovascular toxicity.
These authors postulated that SK&F 101926 produced hypotension and death in
rats by inducing the degranulation of mast cells and release of serotonin.
Resident myocardial mast cells also appear to mediate a large component of heart
reoxygenation injury (220). Keller et al. found that mast cell peroxidase (a marker
177
of mast cell degranulation) was not released into the perfusate of isolated rat
hearts during normoxic or a 60-minute hypoxic period; however, an immediate and
sustained release was measured during reoxygenation. Stabilization of mast cells
with lodamide tromethamine decreased myocardial infarct size.
Increased
histamine levels and mast cell metachromasia were also reported during
reperfusion of the guinea pig heart (221). The authors of this study suggested that
histamine may play a role in reperfusion-induced arrhythmias. Decorti et al. (222)
reported mast cell and histamine involvement in the cardiomyopathy induced by
the antitumor drug adriamycin.
Numerous studies have implicated mast cells in certain types of lung pathology.
Day et al. (223) and Keith et al. (224) found increased mast cell numbers and
histamine and serotonin levels in lung cells isolated from rats exposed to asbestos
fibers. Kalenderian et al. (225) found an increased number of mast cells and
secretion of histamine releasing factor from alveolar
macrophages in
bronchoalveolar lavage fluid of smoking patients.
There is some evidence for mast cell involvement in certain liver diseases. Gittlen
et al. (226) found increased plasma histamine in two types of cholestatic liver
disease--primary biliary cirrhosis and sclerosing cholangitis.
These authors
speculated that the increased plasma histamine may be responsible for the pruritus
associated with cholestasis. They postulated that bile acids may act directly on
178
tissue mast cells, inducing degranulation. Inhibition of mast cell degranulation
with lodoxamide tromethamine decreased endotoxin-induced liver changes (227).
Mast cell involvement has been documented in fibrotic liver disease (below).
Glucocorticoids have been shown to inhibit release of mast cell mediators.
Wakajtys-Rode et al. (228) demonstrated prevention of concavalin A- or antigeninduced histamine release from rat peritoneal mast cells by dexamethasone. The
5-lipoxygenase pathway also appeared to be inhibited.
However, the
cyclooxygenase pathway was apparently increased with dexamethasone, as an
increase in PGD, was measured. Similar results were obtained by Daeron et al.
(229) and Robin et al. (230) in mouse marrow-derived mast cells. The latter
authors suggested that, as PGD, was increased while LTB4 and LTC4 were
decreased with dexamethasone treatment, it did not appear that glucocorticoids
were operating solely via phospholipase inhibition. Scleimer et al. (231) compared
the potency of various glucocorticoids for inhibition of histamine release from
human basophils. The order of potency was triamcinolone > dexamethasone >
prednisolone > hydrocortisone.
Triamcinolone was 2.5 x as potent as
dexamethasone. This order is generally consistent with the antiinflammatory
potency of these compounds in man (163).
A similar potency has been
demonstrated for TCN inhibition of histamine release from mouse peritoneal mast
cells (231, personal communication) and arachidonic acid release from perfused
guinea pig lung (232).
179
In the present work, a decrease in inflammatory activity was observed following
TCN cotreatment with BCNU or ANIT. A slight decrease in bile duct necrosis
and a significant decrease in inflammatory cell number were also observed
(Figures 39 and 40; Tables 8 and 9). Mast cells were decreased in number and
were more densely-staining, indicating a less active state; fewer dispersed granules
were observed (Cf. Figures 42B/44A; 43B/45A). Though it is speculative at this
point, it is possible that the observed protective effect of the glucocorticoid was
due, in part, to decreased lability of mast cell membranes (184) and consequent
decreased release of mast cell-derived inflammatory mediators, including
chemotactic substances. Decrease of the latter would be expected to result in less
neutrophil and eosinophil infiltration and decreased mast cell recruitment.
The alteration of BCNU- and ANIT-induced morphologic changes with TCN
cotreatment reflected functional changes (Chapter 6). For both BCNU and ANIT,
TCN cotreatment reversed cholestasis and decreased BSP retention, though bile
Pi was significantly increased (Tables 6 & 7; Figures 29, 30, 31). It has been
suggested that, at least in the case of ANIT, cholestasis may be secondary to bile
duct necrosis and formation of bile plugs (181). However, little if any change in
necrosis was observed here with TCN cotreatment, though bile flow was restored
to normal. The cholestasis also does not appear to be secondary to portal edema
(149) as there was also little change in edema with the cotreatment. The present
results suggest that ANIT-and BCNU-induced cholestasis may be due to a direct
180
effect of a mast cell mediator. Decreased BSP retention with TCN cotreatment
could be simply a function of restored bile flow.
The increased leakage into rat bile of HRP and P, with BCNU and ANIT
treatment may be a result of mast cell activation.
Murray et al. (233)
demonstrated increased bowel wall permeability to HRP following infection of
Hooded Lister rats with Nippostrongylus brasiliensis. These authors concluded that
the nematode secreted a mast cell degranulator antigen; released mediators
(vasoactive amines, proteolytic enzymes) subsequently damaged the epithelial cells
and their junctional complexes, allowing greater permeability to HRP. A temporal
correlation was observed between the increased permeability and the rise in
mucosal mast cell number. Mast cell numbers, leukotriene release, and epithelial
damage were also associated in the study by Perdue et al. (216). It is also possible
that the increased permeability is not a direct result of mast cell mediator release
but is secondary to neutrophil immigration.
Milks et al. (234) measured a
decreased transepithelial resistance during neutrophil immigration. These results
support the hypothesis that the increased permeability observed in the present
studies is mast cell-associated.
However, in contrast to the present results,
treatment of nematode-infected rats with cortisone by Murray et al. (233)
decreased permeability. If the steroids are, in fact, stabilizing mast cells, the latter
results are more consistent. However, though a decrease in ANIT-induced portal
inflammation with cortisone treatment was reported by Moran et al. (189), the
181
protective effect was strongly dependent on timing of the steroid administration.
It is possible that the unexpected results obtained in the present investigation may
be related to the particular dosing regimen. Glucocorticoids have also been
shown to increase production of certain prostaglandins, such as PGD, (230). It
may be that the permeability changes are mediated by these arachidonic acid
products. It is also possible that, although increased junctional permeability of
hepatocytes following BCNU or ANIT treatment was conclusively demonstrated
with the lanthanum studies (Chapter 2), biliary leakage also occurs across or
around bile duct epithelial cells. Though no lanthanum was observed in bile
ductules, bile ducts, which are preferentially damaged by BCNU and ANIT
treatment, were not examined closely under EM. Little decrease in bile duct
necrosis was observed with TCN cotreatment. Still, this does not explain the
increase in bile P, that was observed. Comparative studies at earlier time points,
when bile duct necrosis is not yet extensive, could address this question.
Esculetin cotreatment partially protected against the histologic changes induced
by BCNU and totally protected against the changes induced by ANIT (Figures
39B and 40B). Inflammatory cell/mast cell counts were similar to those following
TCN/BCNU and TCN/ANIT treatments (Tables 8 and 9). Bile duct necrosis was
reduced somewhat when rats were cotreated with esculetin + BCNU and was
eliminated when rats received ESC + ANIT(24h) (Tables 8 and 9). These effects
paralleled functional changes (Chapter 6). As esculetin is a specific inhibitor of
182
5-lipoxygenase, it is tempting to speculate that the histologic changes induced by
BCNU and ANIT are mediated, in part, by a 5-lipoxygenase product (i.e. a
leukotriene). However, esculetin may also be a free radical scavenger (165) and
it is possible that the toxicities of BCNU and ANIT are mediated, in part, by free
radicals.
The free radicals could have a toxic effect on tissues directly, or,
alternatively, through mast cell activation. There is substantial evidence for free
radical-induced mast cell degranulation. Masini et al. (235) demonstrated a
correlation between histamine release and increased levels of malondialdehyde
and conjugated dienes; free radical scavengers (GSH, a-tocopherol) decreased
histamine release. The oxidative burst of eosinophils and neutrophils has also
been shown to induce mast cell degranulation (236). Peroxidation of arachidonic
acid generates hydroxyl radical (192).
Though it is not clear at this point if esculetin is protective via its inhibition of
lipoxygenase or via free radical scavenging, the former appears more likely as
esculetin had less protective effect with BCNU, for which there is evidence of free
radical involvement (237), than with ANIT, for which there is not. Comparative
studies with other free radical scavengers and with lipoxygenase inhibitors that are
not scavengers could address these questions. As was mentioned in Chapter 6,
metabolic alteration can likely be discounted as a potential mechanism of
esculetin protection, as functional changes were similar to ANIT alone when rats
received ANIT + ESC and were evaluated 48 hours later (Figure 35; Table 7).
183
A parallel loss of protective effect was observed histologically (Figure 46; Table
9).
Indomethacin cotreatment generally had little effect on the morphologic changes
induced by BCNU (Table
8).
The reduction of mast cell counts with
indomethacin + BCNU treatment was a surprising finding.
decrease may not be actual.
However, this
Numerous studies have reported an apparent
decrease in mast cell number in acutely inflamed tissue (197,217,238). The
apparent decrease is due to complete degranulation, which renders mast cells
invisible with mast cell stains ("phantom mast cells"). Evidence of increased
degranulation with indomethacin + BCNU treatment in the present studies was
provided by the identification of dispersed granules in portal areas of INDOtreated livers (Figure 47A, small arrows) and by the observation that a greater
percentage of the observed mast cells with INDO + BCNU treatment appeared
to be degranulating than with BCNU alone. It should also be noted that mast cell
counts were done with H/E sections; as mast cells are not highly visible with H/E
staining (229), the counts may not be entirely accurate. The ANIT + INDO
combination treatment generally increased the inflammatory response over that
of ANIT alone (Table 9). Mast cell number was increased over ANIT alone, with
extensive degranulation (Figure 47B). As previously pointed out (Chapter 6),
indomethacin cotreatment was not functionally protective.
184
Indomethacin and other nonsteroidal antiinflammatory drugs have been shown to
potentiate histamine release from mast cells and certain aspect of the
inflammatory response in general (239). The mechanism of potentiation may be
via a decrease in prostaglandins, which have been shown to suppress release of
inflammatory mediators from mast cells and neutrophils (193,200); shift of
arachidonic acid to the lipoxygenase pathway may also be significant (239). High
doses of indomethacin apparently increase lability of the mast cell membrane
directly (239).
In addition to the acute injury induced by BCNU and ANIT, mast cells could have
an etiologic role in BCNU- and ANIT-induced fibrosis. There is increasing
interest in the potential role of mast cells in fibrotic disease.
mechanism of fibrosis
is
Though the
still not completely understood, it can be defined
generally as an overaccumulation of collagen (240). The pathogenesis of fibrosis
is commonly 1) tissue injury followed by an inflammatory reaction with increased
vascular permeability and plasma extravasation; 2) chemotactic factor attraction
of neutrophils, eosinophils, and macrophages; 3) inflammatory cell release of
collagenases and other proteases which degrade the connective tissue matrix; 4)
matrix constituent attraction of fibroblasts from surrounding tissues; 5) excessive
repair activity by fibroblasts, leading to collagen accumulation (237,240,241,242).
In addition to fibroblasts, chondroblasts, smooth muscle cells, hepatocytes, and Ito
cells have been shown to produce collagen (237,240).
185
Numerous investigations have implicated mast cell involvement in various fibrotic
diseases. Nishioka et al. (243) measured an increase in mast cell number and
inflammatory infiltrate in skin biopsies of patients with scleroderma, a fibrotic
disease of the skin (238).
Increased mast cell numbers have also been reported
in biopsies of patients with neurofibromatosis (244,245); the latter have responded
favorably to the mast cell stabilizer ketotifen.
Exposure to bleomycin, an
antitumor agent, increased lung mast cell number and histamine content and
induced pulmonary fibrosis (246,247); similar results were obtained with asbestos
exposure (223,224).
Triamcinolone treatment prevented the increase in lung
collagen following exposure to bleomycin (237,247).
It has been established for some time that chronic injury with hepatotoxicants can
induce hepatic fibrosis (227,248).
There is some evidence for mast cell
involvement in this condition. Hepatic infiltration of inflammatory cells and
fibrosis have been documented in patients with systemic mast cell disease (199).
A correlation was obtained between numbers of mast cells and the intensity of the
fibrosis (249,250). Mast cells are found in very low concentrations in the normal
liver (199,250,251). Narayanan et al. (252) reported portal and sinusoidal mast
cell infiltration, portal hypertension, ascites, and fibrosis in a patient with systemic
mastocytosis. An increase in mast cell number and hydroxyproline (indicative of
collagen synthesis) has been documented in the early stages of liver cirrhosis
(251). In a recent study, Umezu et al. (253) investigated changes in plasma and
186
liver histamine and hydroxyproline levels in rat hepatic fibrosis resulting from
chronic CC14 (12 weeks) and acute dimethylnitrosamine (DMN) exposure. A
strong correlation was obtained between liver hydroxyproline and histamine
content for both treatments, though the increase in histamine preceded
hydroxyproline in the case of DMN. Histologic examination revealed increased
collagen fibers in portal tracts and increased mast cell density. These authors
postulated that mast cell-derived mediators, such as histamine or leukotrienes,
may have an etiologic role in hepatic fibrosis. BCNU has been shown to induce
a fibrotic condition in the liver. Larson et al. (97) reported that 28 days after
BCNU treatment increased fibroblastic activity and connective tissue deposition
were observed. At later time points connective tissue had invaded the hepatic
parenchyma.
Though mast cell hyperplasia has been reported in fibrotic lesions associated with
these and other inflammatory disorders, a mechanistic basis for mast cell
involvement has not been established. Several mast cell mediators may have a
potential role. Histamine has been shown to stimulate fibroblast growth and
collagen synthesis in vitro and increase collagen synthesis in vivo (197,243,254).
Stimulated fibroblasts produce
elevated levels
of collagenase
hexosaminidase, which may destroy connective tissue (243).
and
13-
In addition to
histamine, other mast cell-derived mediators that may have a role in fibrosis
include: 1) heparin, which influences maturation of collagen fibers; 2) proteolytic
187
enzymes, which may act on connective tissue components; and 3) tumor necrosis
factor, which has been shown to stimulate fibroblast proliferation (254).
Mast cell/fibroblast interactions have been documented in several studies
(255,256). Fibroblasts readily take up released mast cell granules in vivo (254).
Mast cells also interact directly with fibroblasts and other cells through a process
termed transgranulation, where they extend granule-filled pseudopodia and
extrude granules directly into the adjacent cell's cytoplasm (197,254).
This
interaction was documented by Choi et al. (254) using time-lapse cinematography;
mast cells were observed interacting with fibroblasts and endothelial cells.
An apparent mast cell/fibroblast interaction was also observed in the present
studies following BCNU treatment (Figure 48). It is interesting to speculate that,
in addition to the early toxic effects of BCNU and ANIT, mast cell mediators may
have a role in the fibrosis induced by these compounds.
Lung fibrosis is a
common side effect of clinical BCNU treatment (257,258,259,260). Aronin et al.
(259) found that 20% of BCNU-treated patients developed the disease; occurrence
was related to cumulative BCNU dose. Schuller et al. (261) observed that rats
receiving a dosing regimen similar to that used clinically developed progressive
alterations of type II alveolar cells; pericapillary edema and plasma cell infiltration
were obvious at 8 weeks. Fibroblasts and collagen bundles were also observed.
At 12 weeks diffuse interstitial fibrosis was apparent. These authors speculated
188
Figure 48. EM section from a BCNU-treated rat. Rat received BCNU, 26 mg/kg,
and liver was removed 72 hours after treatment. Mast cells (MC) can be seen
interacting with fibroblasts (FB) (inset). (V: portal vein; A: artery; BD: bile
ductule; C: collagen fibrils) x3500; inset magnification = 6000x.
189
that the observed decrease in a-l-proteinase inhibitor activity and increased PMN
elastase activity could be responsible for the increased tissue damage and collagen
deposition. Jarvi (237) reported similar findings, suggesting that the decrease in
functional a-1-proteinase could be either secondary to BCNU-induced liver
disease or a direct effect of a BCNU-derived alkylating or carbamylating product.
In the latter study, lung collagen was increased to 159% of controls by 28 days.
Though a histologic evaluation was not done in this study, there was evidence for
neutrophil recruitment; these authors suggested that infiltrating neutrophils could
be releasing active oxygen species which would break down tissue matrix. In
addition to its fibrotic effects on the liver and the lungs, BCNU has also been
shown to induce fibrotic conditions in the heart (262). Mast cells/mast cell
mediators could potentially provide an underlying mechanism for these conditions.
Interestingly, treatment with glucocorticoids limits the lung fibrosis induced by
BCNU (259,261).
A mechanistic basis for mast cell/mast cell mediator involvement in the early
hepatotoxicity of ANIT and BCNU is not entirely clear. Mast cells release various
proteolytic enzymes during degranulation. Superoxide anion is also released (198).
These substances could obviously damage tissue. Chemotactic agents released by
mast cells (e.g. LTB4) attract other inflammatory cells (neutrophils, eosinophils,
histiocytes); these cells release proteases and active oxygen species as well.
190
Elastase released from infiltrating neutrophils has been shown to be an important
factor in the pathogenesis of asthma (221). Dahm et al. (263) protected rat livers
against ANIT toxicity by inhibiting neutrophil infiltration. It is also possible that
leukotriene release induces an ischemia/reperfusion injury (178).
Degranulation of mast cells could be directly stimulated by the toxicants or by the
toxicant damage to adjacent tissues. Tissue trauma has been shown to induce
mast cell degranulation (217). Alternatively, bile acids leaking from damaged bile
ducts could be stimulating mast cells. Little et al. (264) showed that bile acids can
act as calcium ionophores, promoting calcium uptake by mast cells and thereby
inducing degranulation.
Though the results presented here are interesting and provocative, they are
preliminary. The protective effect of TCN could be due to something other than
phospholipase A, inhibition, such as stabilization of cell membranes (e.g. mast
cells, biliary epithelial cells, hepatocytes).
glucocorticoid treatment
is
It is also possible that the
increasing production of an antiinflammatory
prostaglandin, as has been demonstrated (230).
16,16-dimethyl PGE,
administration significantly decreased ANIT-induced bile duct necrosis and
cholangitis (181). TCN treatment could also be altering metabolic processes.
Thin layer chromatography of bile BSP with TCN/BCNU treatment indicates that
metabolism of BSP was changed with TCN cotreatment (Cf. Figure 24A-A, C-TC,
191
C-TA, and D-C). Comparison with other membrane stabilizers and phospholipase
inhibitors would help address these questions. Comparative dosing regimens would
also be informative.
The protection afforded by esculetin of ANIT-induced hepatotoxicity was
remarkable. Whether these effects were due to scavenging of free radicals or to
a decrease in lipoxygenase products would be a fairly straightforward problem to
address. Comparative studies with other free radical scavengers and lipoxygenase
inhibitors would be informative. Lack of a change in BSP metabolism (Cf. Figure
24A-A and C-EA) and the return of toxic effects 48 hours after treatment suggest
that altered metabolism was not a factor. The apparent delay--rather than
absolute protection--of the toxic effect of ANIT with esculetin cotreatment should
be investigated further.
The most straightforward method for assessing leukotriene/prostaglandin
involvement in the toxicity of these compounds would be to measure plasma and
bile eicosanoid levels following treatment. Comparing histologic and functional
changes induced by ANIT and BCNU to those induced by particular eicosanoids
would also be informative. Potential mast cell involvement could be definitively
assessed by comparing the toxic effects of ANIT and BCNU while altering mast
cell lability (e.g. with a mast cell stabilizer such as lodamide tromethamine or a
secretagogue such as 48/80). Histamine and serotonin levels could be measured.
192
Comparative studies with mast cell-deficient animals would also be revealing
(265).
The potential role of mast cells in ANIT- and BCNU-induced fibrosis could be
definitively evaluated by observing long-term histological changes following
cotreatment with these compounds and a mast cell stabilizer. If increased plasma
histamine/serotonin levels are measured following BCNU or ANIT treatment, it
would also be informative to follow these levels over time and attempt a
correlation with fibrosis progression.
193
X. SUMMARY AND CONCLUSIONS
BCNU treatment induced a time-dependent decrease in bile flow in SpragueDawley rats. In vivo bile flow was significantly decreased 24 hours after treatment
and remained low through 96 hours; bile flow in the perfused liver was
significantly decreased at 48 hours but was normal 24, 72, and 96 hours after
BCNU treatment. A dose-dependent increase in plasma bilirubin was also
observed. Treatment with ANIT (250 mg/kg) caused a significant decrease in in
vivo and perfused liver bile flows at 24 hours; bile flow was further depressed at
36 hours and had ceased at 48 hours posttreatment after ANIT treatment.
Both ANIT and BCNU induced dramatic increases in the movement of
permeability markers from plasma/perfusate to bile. Penetration into bile of
infused horseradish peroxidase (HRP) was 15x controls 48 hours after BCNU
treatment and remained elevated though 192 hours posttreatment.
HRP
penetration was not different from controls 24 hours after BCNU treatment. A
similar time course was observed for penetration into bile of endogenous inorganic
phosphate (P,) following BCNU treatment. The increase in bile P, with BCNU
was dose-related. A strong correlation was observed between bile HRP activity
and P, with BCNU treatment. These results provide strong evidence for increased
paracellular permeability with BCNU treatment. Though the time course differed,
similar increases in permeability were measured following ANIT treatment.
194
Attempts to monitor ANIT-induced bile penetration of infused HRP indicated an
unexpected time course for permeability changes. A subsequent comparative
study revealed a substantial strain difference in permeability time course between
the Sprague Dawley and Wistar rat, which has traditionally been used in
permeability studies. Peak P, penetration was observed 12 hours after ANIT
treatment in Wistar rats and 24 hours after treatment in Sprague-Dawley rats.
Electron microscopic visualization of lanthanum particles in canaliculi of
lanthanum-perfused livers of BCNU-and ANIT-treated animals confirmed
increased permeability at the level of the hepatocyte tight junctions. An apparent
lobular distribution (centrizonal > periportal) of lanthanum penetration was
noted. Kinetics analysis in the perfused liver confirmed an increase in rapid phase
(paracellular) bile penetration of HRP with BCNU treatment; additionally, BCNU
appeared to inhibit, in a manner similar to colchicine, slow phase (transcellular,
fluid-phase) movement. Albumin-bound Evans blue, which proved to be too large
(Mr 69,000) for paracellular penetration under conditions of increased
permeability, was utilized to investigate the effects of BCNU on transcellular
transport in isolation. Treatment with BCNU or colchicine retarded movement
of Evans blue into bile. This was provocative, as both of these compounds have
been shown to inhibit the polymerization of tubulin, which has an integral role in
certain transcellular transport processes.
In addition to increasing paracellular permeability and decreasing fluid-phase
195
transcytosis, BCNU inhibited active transport. Maximal extraction of the organic
anion bromosulphthalein (BSP) from perfusate was markedly inhibited by BCNU;
a time course study revealed a significant decrease in the ability of livers from
BCNU-treated rats to transport BSP 48 and 72 hours posttreatment. Maximal
retention was observed 72 hours posttreatment. Comparison of partial clearance
constants revealed that uptake processes were not affected by BCNU. ANIT
treatment also resulted in a time-dependent increase in perfusate BSP retention;
however, in contrast to BCNU, ANIT appeared to inhibit uptake processes. Thin
layer chromatography of perfusate BSP revealed an apparent coincident loss of
parent compound and increase in a single conjugate for both treatments. No
unconjugated BSP was detected in bile. Bile BSP incubated with 4% albumin did
not comigrate with equilibrium perfusate BSP, indicating that the latter was an
actual conjugate and was not differentially migrating due to albumin binding.
Phenobarbital (PB) pretreatment reversed BCNU-induced cholestasis in vivo but
did not alter bile P from BCNU treatment alone. BSP excretion was increased
when rats were pretreated with PB prior to BCNU. A decrease in bile flow
similar to that following BCNU treatment was observed in rats treated with
chloroethylisocyanate (CI), a major putative metabolite of BCNU. However, CI
did not increase bile P, over controls. As with BCNU, pretreatment of CI-treated
animals with PB eliminated the induced cholestasis. PB pretreatment potentiated
ANIT-induced cholestasis and increased bile P;. The latter results support the
196
hypothesis that a metabolite is responsible for ANIT-induced cholestasis and
permeability changes.
Chioroethylisocyanate appeared to be the metabolic
product responsible for BCNU-induced cholestasis but not permeability changes.
As bile P, was unchanged with PB + BCNU treatment, the protection afforded by
PB pretreatment toward BCNU-induced cholestasis was attributed to induction of
transport-associated mechanisms, rather than accelerated BCNU detoxication.
Previous studies have suggested a causal relation between increased permeability
and cholestasis (that is, that increased permeability allows paracellular reflux of
osmotically-active biliary components, thus decreasing bile flow). Results of the
present investigation strongly indicate that permeability changes and cholestasis
induced by ANIT and BCNU are separate events. Evidence for this conclusion
includes: 1) in vivo bile flow was significantly decreased 24 hours after BCNU
treatment though bile P, was normal; 2) in vivo bile flow remained depressed
after bile P, had peaked and decreased significantly; 3) lack of a parallel decrease
in bile flow and increased P, with a higher BCNU dose; 4) lack of any correlation
between bile flows and bile P for individual rats; 5) reversal of BCNU-induced
cholestasis with PB pretreatment without a parallel decrease in P,; 6) a similar
decrease in bile flow following BCNU and CI treatment, though the latter failed
to elevate bile
P,.
A similar lack of correlation between bile flow and
permeability changes was observed with ANIT treatment. A direct, rather than
expected inverse, correlation was observed between bile P, and bile flow in Wistar
197
rats following ANIT treatment. These results provide strong evidence against
BCNU- and ANIT-induced cholestasis being causally related to increased
permeability, and, by extension, question the significance of permeability changes
in cholestasis generally. However, it should be noted that a similar time course
of increased permeability, perfused liver bile flow, and reported bile glutathione
concentrations following BCNU treatment does suggest that inhibitory effects of
BCNU on bile salt independent flow (BSIF) may be due, in part, to paracellular
reflux of glutathione. The potential role of glutathione in BSIF has not been
adequately investigated.
Permeability changes have also been suggested as a primary causative factor in
ANIT- and BCNU-induced BSP retention. However, maximal BSP retention
following BCNU treatment was observed 72 hours after treatment, though
maximal permeability was observed 48 hours after treatment. Further evidence
against a causal relation between permeability changes and BSP retention was
provided by 1) the rate of increase of perfusate BSP after addition to the
perfusate reservoir was much more than the loss from bile; 2) TLC results, where
a different BSP conjugate was observed in the equilibrium perfusate and bile; 3)
a significant decrease in BSP retention without a decrease in bile P, with PB +
BCNU treatment. The present results are consistent with inhibition of cytosolic
binding protein or transporter activity. In either case, decreased movement into
bile would result in increased sinusoidal efflux.
198
An inflammatory mediator, possibly mast cell-derived, may have an etiologic role
in the hepatotoxicity induced by ANIT or BCNU.
Cotreatment with the
glucocorticoid triamcinolone (TCN) restored bile flow and decreased BCNU- and
ANIT-induced BSP retention. This protective effect was not simply additive, as
bile flow and BSP excretion were not increased in TCN controls. TLC analysis
of BSP in bile with TCN cotreatment suggested altered metabolism could be a
factor. The finding that bile P, was increased while BSP retention and cholestasis
were decreased with TCN cotreatment provides further evidence against causality
between these effects.
Cotreatment with the 5-lipoxygenase inhibitor esculetin (ESC) reversed ANIT- and
BCNU-induced cholestasis. Bile P, was significantly reduced following treatment
with BCNU + ESC compared with BCNU treatment alone; livers from rats
cotreated with ANIT + ESC had bile P, not significantly different from corn oil
controls. Cotreatment with ESC did not reduce BCNU-induced BSP retention but
eliminated the retention induced by ANIT. Livers from rats cotreated with ANIT
+ ESC and evaluated 48 hours later were cholestatic and had elevated bile P.
Indomethacin cotreatment did not alter BCNU- or ANIT-induced cholestasis, bile
Pi, or BSP retention.
BCNU and ANIT treatment resulted in similar histologic changes. A progressive
199
increase in bile duct necrosis, edema, and fibrin deposition in portal areas was
observed following either treatment.
Substantial inflammatory infiltrate with
numerous mast cells was also noted. Though occasional hepatocellular necrosis
was observed in areas immediately adjacent to portal tracts, hepatocytes were
generally not affected.
Histologic changes with TCN, ESC, and INDO cotreatments reflected functional
changes. TCN cotreatment caused a limited decrease in ANIT- and BCNUinduced bile duct necrosis and inflammatory cell infiltration; mast cells were
decreased in number and appeared less active. The reversal of cholestasis with
limited decrease in necrosis and edema with TCN cotreatment argues against a
major etiologic role for these factors in ANIT- and BCNU-induced cholestasis.
ESC cotreatment partially protected against the morphologic changes induced by
BCNU and completely protected against those induced by ANIT. Inflammation
was reduced in both cases; livers from rats cotreated with ANIT + ESC were not
different from controls 24 hours after ANIT treatment but at 48 hours were
similar to livers receiving ANIT alone. Cotreatment with indomethacin did not
significantly alter the morphologic changes induced by ANIT or BCNU.
These results support the involvement of an inflammatory mediator, possibly mast
cell-derived, in the hepatoxicity of ANIT and BCNU. As mast cells predominate
in larger portal areas, mast cell involvement could explain the observation that
200
larger portal areas are affected preferentially by ANIT or BCNU. The protection
afforded by TCN could be due to mast cell stabilization. The ESC results suggest
that the inflammatory mediator responsible for ANIT-and BCNU-induced
hepatoxicity may be a leukotriene. Mast cells are a major source of leukotrienes
in the liver.
Coincident tissue damage, increased mast cell numbers, and
increased leukotriene concentrations have been documented in some extrahepatic
pathologic conditions. The lack of protection following cotreatment with the
cyclooxygenase inhibitor indomethacin supports leukotriene involvement.
It may thus be tentatively concluded from these studies that portal inflammation
is an etiologically significant event following exposure of rat livers to ANIT and,
to a lesser extent, BCNU. Mast cell activation appears to be an early event in this
inflammatory condition. Mast cell activation could be occurring 1) by direct mast
cell membrane damage by toxicants; 2) secondary to tissue trauma (e.g. bile duct
damage by the toxicant or a metabolite); or 3) by contact with bile salts leaking
from damaged bile ducts. Released leukotrienes may 1) competitively inhibit
transport/binding protein activity and thus decrease organic anion excretion and
increase sinusoidal efflux; 2) induce centrizonal vasoconstriction and hypoxia,
leading
to
increased
centrizonal
paracellular
permeability
and/or
ischemia/reperfusion injury; 3) induce infiltration of inflammatory cells
(neutrophils, eosinophils, additional mast cells) which may contribute to tissue
damage and increased permeability. Mast cell-derived proteolytic enzymes may
201
directly damage tissue. Activated mast cells, either directly or though mediators
(e.g. histamine) may also have a significant role in BCNU- and ANIT-induced
fibrosis. Prostaglandins and histamine may play a role in these changes. As with
endotoxin, ANIT and BCNU could be decreasing elimination of these mediators
in addition to increasing their production and release. Decreased elimination
could be secondary to cholestasis/increased permeability or inhibition of transport-
associated proteins. Leukotriene metabolism could be inhibited.
The goal of this investigation was to provide a mechanistic basis for the
hepatoxicity of ANIT and BCNU and, through extension, other cholestatic agents.
This goal was partially realized. It can be concluded that ANIT- and BCNU-
induced cholestasis and BSP retention are not a direct function of permeability
changes. Altered cytosolic binding proteins or transporters appear to be involved,
though further study is merited. Evidence has been provided for the involvement
of an inflammatory mediator in the functional and morphologic changes induced
by BCNU and ANIT. Comparative studies with other antiinflammatory agents
(glucocorticoids, eicosanoid inhibitors) would help define this role. Monitoring
of hepatic and plasma levels of eicosanoids and comparative studies with
eicosanoid administration would also be informative.
Though the protection
afforded by ESC of ANIT-induced hepatic changes was remarkable, the reversal
of
this protection
at
48
hours
should
be
investigated.
Mast
cell
stabilization/labilization, comparative studies with mast cell-deficient mice, and
202
monitoring of plasma histamine/serotonin levels would help define the role of
mast cells in these changes. Long-term studies could clarify the significance of
mast cell involvement in fibrotic changes.
A research goal that was not realized in these investigations was elucidation of the
potential role of cytoskeletal alterations in the hepatoxicity induced by BCNU and
ANIT. The inhibition of fluid-phase transcytosis with BCNU suggests microtubule
involvement. Leakage of tight junctions following BCNU and ANIT treatment
implies microfilament and/or microtubule alterations. The general significance
of cytoskeletal changes in hepatic dysfunction and the possible involvement of a
mast cell-derived mediator in these changes warrants further investigation.
203
REFERENCES
1.
2.
Arias, I.M., H. Popper, W.B. Jakoby, D. Schachter, and D.A. Shafritz, eds.
The Liver: Biology and Pathology. New York: Raven Press, 1988.
Corless, J.K. and H.M. Middleton (1983): Normal liver function. Arch.
Intern. Med., 143:2291-2294.
3.
Rappaport, A.M., Z.J. Borowy, and W.M. Lougheed (1954): Subdivision of
hexagonal liver lobules into a structural and functional unit: role in hepatic
physiology and pathology. Anat. Rec., 119:11-27.
4.
Coleman, R. (1987): Biochemistry of bile secretion. Biochem. J., 244:249261.
5.
Mullock, B.M. and R.H. Hinton (1981): Transport of proteins from blood to
bile. Trends Biochem. ScL, 6:188-191.
6.
Boyer, J.L. (1980): New concepts of mechanisms of hepatocyte bile
formation. Physiol. Rev., 60:303-322.
7.
Er linger, S. (1988): Bile flow. In: The Liver: Biology and Pathobiology.
I.M. Arias, W.B. Jakoby, H. Popper, D. Schachter, and D.A. Shafritz, eds.,
New York: Raven Press, 643-661.
8.
Reuben, A. (1984): Bile formation: sites and mechanisms. Hepatology, 4:15S24S.
9.
Strange, R.C. (1984): Hepatic bile flow. Physiol. Rev., 64:1055-1102.
10.
Hardison, W.G., and C.A. Wood (1978): Importance of bicarbonate in bile
salt independent fraction of bile flow. Am. J. Physiol., 235:E158-E164.
11.
Barnhart, J.L., and B. Combes (1978): Characterization of SC 2644-induced
choleresis in the dog: evidence for canalicular bicarbonate secretion. J.
Pharmacol. Exp. Titer., 206:190-197.
12.
Meir, J.P., R. Knickelbeim, R.H. Moseley, and J.L. Boyer (1985): Evidence
for a carrier-mediated chloride/bicarbonate exchange in canalicular rat liver
plasma membrane vesicles. J. Clin. Invest., 75:1256-1263.
13.
Ballatori, N., and A.T. Truong (1989): Relation between biliary glutathione
excretion and bile acid-independent bile flow. Am. J. Physiol., 256:G22-G30.
204
14.
Inoue, M., R. Kinne, T. Tran, and I.M. Arias (1983): The mechanism of
biliary secretion of reduced glutathione: analysis of transport process in
isolated rat liver canalicular membrane vesicles. Eur. J. Biochem., 134:467-
471.
15.
Gabbiani, G., R. Montesano, B. Tuchweber, M. Salas, and L. Orci (1975):
Phalloidin-induced hyperplasia of actin filaments in rat hepatocytes. Lab.
Invest., 33:562-569.
16.
Kacich, R.L., R.H. Renston, and A.L. Jones (1983): Effects of cytochalasin
D and colchicine on the uptake, translocation, and biliary secretion of
horseradish peroxidase and [14C]sodium taurocholate in the rat. Gastroenterology, 85:385-394.
17.
Oda, M., V.M. Price, M.M. Fischer, and M.J. Phillips (1974): Ultrastructure
of bile canaliculi, with special reference to the surface coat and the
pericanalicular web. Lab. Invest., 31:314.
18.
Phillips, M.J., M. Oda, E. Mak, M.M. Fisher, and K.N. Jeejeebhoy (1975):
Microfilament dysfunction as a possible cause of intrahepatic cholestasis.
Gastroenterology, 69:48-58.
19.
French, S.W. (1976): Is cholestasis due to microfilament failure? Hum.
Pathol., 7:243-244.
20.
Oshio, C., and M.J. Phillips (1981):
Contractility of bile canaliculi:
implications for liver function. Science, 212: 1041-1042.
21.
Phillips, M.J., C. Oshio, M. Miyairi, H. Katz, and C.R. Smith (1982): A
study of bile canalicular contractions in isolated hepatocytes. Hepatology,
2:763-768.
22.
Oshio, C., M.J. Phillips, and M. Miyairi (1981): Influence of sodium
taurocholate on bile canalicular contractions (abstr). Hepatology, 1:535.
23.
Lake, J.R., R.W. Van Dyke, and B.F. Scharschmidt (1985): Biliary secretion
of fluid-phase markers by isolated perfused rat liver. Role of transcellular
vesicular transport. J. Clin. Invest., 76:676-684.
24.
Jaeschke, H., H. Krell, and E. Pfaff (1987): Quantitative estimation of
transcellular and paracellular pathways of biliary sucrose in isolated perfused
rat liver. Biochem. J., 241:635-640.
205
25.
Reichen, J., and F.R. Simon (1988): Cholestasis. In: The Liver: Biology and
Pathobiology. I.M. Arias, W.B. Jakoby, H. Popper, D. Schachter, and D.A.
Shafritz, eds., New York: Raven Press, 643-661.
26.
Blitzer, B.L., S.L. Ratoosh, C.B. Donovan, and J.L. Boyer (1982): Effects of
inhibitors of Natcoupled ion transport on bile acid uptake by isolated rat
hepatocytes. Am. J. Physiol., 243:G48-G53.
27.
Wieland, T., M. Nassal, W. Kramer, G. Fricker, U. Bickel, and G. Kurz
(1984): Identify of hepatic membrane transport systems for bile salts,
phalloidin, and anamanide by photoaffinity labeling. Proc. Natl. Acad. Sci.
USA, 81:5232-5236.
28.
Oelberg, D.G., and R. Lester (1986): Cellular mechanisms of cholestasis.
Ann. Rev. Med., 37:297-317.
29.
Lowe, P.J., S.G. Barnwell, and R. Coleman (1984): Rapid kinetic analysis of
the bile-salt-dependent secretion of phospholipid cholesterol and a plasmamembrane enzyme into bile. Biochem. J., 222:631-637.
30.
Barnwell, S.G., P.J. Lowe, and R. Coleman (1984): The effects of colchicine
on secretion into bile of bile salts, phospholipids, cholesterol and plasma
membrane enzymes: bile salts are secreted unaccompanied by phospholipids
and cholesterol. Biochem. J., 220:723-731.
31.
Meier, P.J., C. Barrett, and J.L. Boyer (1984): Mechanisms of taurocholate
transport in canalicular and basolateral rat liver plasma membrane vesicles.
J. Biol. Chem., 259:10614-10622.
32.
Kawahara, H., N. Marceau, and S.W. French (1989): Effects of agents which
rearrange the cytoskeleton in vitro on the structure and function of
hepatocytic canaliculi. Lab. Invest., 60:692-704.
33.
Wolkoff, A.W., C.A. Goresky, J. Se llin, Z. Gatmaitan, and I.M. Arias (1979):
Role of ligandin in transfer of bilirubin from plasma into liver. Am. J.
Physiol., 236:E638-E648.
34.
Vonk, R.J., P.A. Jekel, D.K. Meijer, and M.J. Hardonk (1978): Transport of
drugs in isolated hepatocytes: the influence of bile salts.
Biochein.
Pharmacol., 27:397-405.
35.
Hoyt, D., and R.E. Larson (1989): Cholestatic effect of carmustine in rats.
J. PharmacoL Exp. Ther., 249:165-171.
206
36.
Scharschmidt, B.F., J.R. Lake, E.L. Renner, V. Licko, and R.W. Van Dyke
(1986): Fluid phase endocytosis by cultured rat hepatocytes and perfused rat
liver: implications for plasma membrane turnover and vesicular trafficking
of fluid phase markers. Proc. Natl. Acad. Sci. USA., 83:9488-9492.
37.
Yousef, I.M., B. Tuchweber, A. Weber, and C.C. Roy (1988): Contribution
of the fluid phase endocytosis to bile flow in cholestasis and choleresis in
rats. Proc. Soc. Exp. Biol. Med., 189: 147-151.
38.
Renston, R.H., D.G. Maloney, A.L. Jones, G.T. Hradek, K.Y. Won, and I.D.
Goldfine (1980): Bile secretory apparatus: evidence for a vesicular transport
mechanism for proteins in the rat, using horseradish peroxidase and
[125I]insulin. Gastroenterology, 78:1373-1388.
39.
Lowe, P.J., K.S. Kan, S.G. Barnwell, R.K. Sharma, and R. Coleman (1985):
Transcytosis and paracellular movements of horseradish peroxidase across
liver parenchymal tissue from blood to bile. Effects of ANIT and colchicine.
Biochem. J., 229:529-537.
40.
Gebhardt, R. (1984): Participation of microtubules and microfilaments in the
transcellular biliary secretion of immunoglobulin A in primary cultures of rat
hepatocytes. Experientia, 40:269-271.
41.
Sakisaka, S., N.G. Oi Cheng, J.L. Boyer (1988): Tubulovesicular transcytotic
pathway in isolated rat hepatocyte couplets in culture: effect of colchicine
and taurocholate. Gastroenterology, 95:793-804.
42.
Lake, J.R., V. Licko, R.W. Van Dyke, and B.F. Scharschmidt (1985): Biliary
secretion of fluid-phase markers by the isolated perfused rat liver: role of
transcellular vesicular transport. J. Clin. Invest., 76:676-684.
43.
Schwenk, M., R. Burr, L. Schwarz, and E. Pfaff (1976): Uptake of bromosulfophthalein by isolated liver cells. Eur. J. Biochem., 64:189-197.
44.
Lorenzini, I., S. Sakisaka, P.J. Meier, and J.L. Boyer (1986): Demonstration
of a transcellular vesicle pathway for biliary excretion of inulin in rat liver.
Gastroenterology, 91:1278-1288.
45.
Quaroni, A., K. Kirsch, and M.M. Weiser (1979): Synthesis of membrane
glycoproteins in rat small-intestinal villus cells. Biochem. J., 182:213-221.
207
46.
Mullock, B.M., R.S. Jones, J. Peppard, and R.H. Hinton (1980): Effect of
colchicine on the transfer of IgA across hepatocytes into bile in isolated
perfused rat livers. Febs Letters., 120:278-282.
47.
Kletzien, R.F., J.F. Perdue, and A. Springer (1972): Cytochalasin A and B:
inhibition of sugar uptake in cultured cells. J. Biol. Chem., 247:2964-2966.
48.
Gregory, D.H., Z.R. Vlahcevic, M.F. Prugh, P. Schatzki, and L. Swell (1978):
Mechanism of secretion of biliary lipids: role of a microtubular system in
hepatocellular transport of biliary lipids in the rat. Gastroenterology, 74:93100.
49.
Kolset, S.O., H. Tolleshaug, and T. Berg (1979): The effects of colchicine
and cytochalasin B on uptake and degradation of asialoglycoproteins in
isolated rat hepatocytes. Exp. Cell Res., 122:159-167.
50.
Tauber, R., and W.A. Reutter (1980): A colchicine-sensitive uptake system
in Morris hepatomas. Proc. Natl. Acad. Sci. USA, 77:5282-5286.
51.
Bajwa, R.S., and J.M. Fujimoto (1983): Effect of colchicine and S,S,S-tributyl
phosphorotrithioate (DEF) on the biliary excretion of sucrose, mannitol and
horseradish peroxidase in the rat. Biochem. Pharmacol., 32:85-90.
52.
Reichen, J., M.D. Berman, and P.D. Berk (1981): The role of microfilaments
and of microtubules in taurocholate uptake by isolated rat liver cells.
Biochim. Biophys. Acta, 643:126-133.
53.
Dubin, M., M. Maurice, G. Feldmann, and S. Er linger (1980): Influence of
colchicine and phalloidin on bile secretion and hepatic ultrastructure in the
rat: possible interaction between microtubules and microfilaments.
Gastroenterology, 79:646-654.
54.
Layden, T.J., E. Elias, and J.L. Boyer (1978): Bile formation in the rat: the
role of the paracellular shunt pathway. J. Clin. Invest., 62:1375-1385.
55.
Mullock, B.M., J.L. Shaw, B. Fitzharris, J. Peppard, M.J. Hamilton, M.T.
Simpson, T.M. Junt, and R.H. Hinton (1985): Sources of proteins in human
bile. Gut, 26:500-509.
56.
Boyer, J.L. (1982): Hepatocellular junctional complexes and the paracellular
pathway: a regulatory role in bile formation. In: The Paracellular Pathway,
edited by S.E. Bradley and E.F. Purcell, Josiah Macy, Jr. Foundation, NY,
209-221.
208
57.
Gumbiner, B. (1987): Structure, biochemistry, and assembly of epithelial
tight junctions. Am. J. PhysioL, 253:C749-C758.
58.
Chalcroft, J.P., and S. Bullivant (1970): An interpretation of liver cell
membrane and junction structure based on observation of freeze-fracture
replicas of both sides of the fracture. J. Cell BioL, 47:49-60.
59.
Madara, J.L. (1988): Tight junction dynamics: is paracellular transport
regulated? Cell, 53:497-498.
60.
Phillips, M.J., S. Poucell, and M. Oda (1986): Biology of disease:
mechanisms
of cholestasis. Lab. Invest., 54:593-608.
61.
Marcial, M.A., and J.L. Madara (1987): Analysis of absorptive cell occluding
junction structure-function relationships in a state of enhanced junctional
permeability. Lab. Invest., 56:424-434.62.
62.
Hubbard, A.L., J.R. Bartles, and L.T. Braiterman (1985): Identification of
rat hepatocyte plasma membrane proteins using monoclonal antibodies. J.
Cell BioL, 100:1115-1125.
63.
Elias, E., Z. Hruban, J.B. Wade, and J.L. Boyer (1980): Phalloidin-induced
cholestasis: a microfilament-mediated change in junctional complex
permeability. Proc. Natl. Acad. Sci. USA, 77:2229-2233.
64.
Lowe, P.J., K. Miyai, J.H. Steinback, and W.G. Hardison (1988):
Hormonal
regulation of hepatocyte tight junctional permeability. Am. J. PhysioL,
255:G454-G461.
65.
Hardison, W.G.M., P.J. Lowe, and M. Shanahan (1989): Effect of molecular
charge on para- and transcellular access of horseradish peroxidase into rat
bile. Hepatology, 9:866-871.
66.
Kan, K.S., and R. Coleman (1986):
1-napthylisothiocyanate-induced
permeability of hepatic tight junctions to proteins. Biochem. J., 238:323-328.
67.
Madara, J.L. (1987): Intestinal absorptive cell tight junctions are linked to
cytoskeleton. Am. J. PhysioL, 253:C171-C175.
68.
Jaeschke, H., H. Krell, and E. Pfaff (1983): No increase of biliary
permeability in ethinylestradiol-treated rats. Gastroenterology, 85:808-814.
69.
Plaa, G.L., and B.G. Priestly (1977): Intrahepatic cholestasis induced by
drugs and chemicals. Plzarmacol. Rev., 28:207-273.
209
70.
Forker, E.L. (1969): The effect of estrogen on bile formation in the rat. J.
Clin. Invest., 48:654-663.
71.
Keefe, E.B., B.F. Scharschmidt, N.M. Blankenship, and R.K. Ockner (1979):
Studies of relationships among bile flow, liver plasma membrane Na+,K+ATPase, and membrane microviscosity in the rat. J. Clin. Invest., 64:15901598.
72.
Er linger, S. (1982): Does Na+,K+ -ATPase have any role in bile secretion?
Am. J. PhysioL, 243:G243-247.
73.
Oda, M., and M.J. Phillips (1977): Bile canalicular membrane pathology in
cytochalasin B induced cholestasis. Lab. Invest., 37:350-356.
74.
Krell, H., H. Hoke, and Erich Pfaff (1982): Development of intrahepatic
cholestasis by a-napthylisothiocyanate in rats. Gastroenterology, 82:507-514.
75.
Krell, H., J. Metz, H. Jaeschke, H. Hoke, and E. Pfaff (1987): Drug-induced
intrahepatic cholestasis: characterization of different pathomechanisms.
Arch. Toxicol., 60:124-130.
76.
Adler, M., K.W. Chung, and F. Schaffner (1980): Pericanalicular hepatocytic
and bile ductular microfilaments in cholestasis in man. Am. J. PathoL,
98:603-616.
77.
Weber, A.M., B. Tuchweber, I. Yousef, P. Brochu, C. Turgeon, G. Gabbiani,
C.L. Morin, and C.C. Roy (1981): Severe familial cholestasis in North
American Indian children: a clinical model of microfilament dysfunction?
Gastroenterology, 81:653-662.
78.
Phillips, M.J., C. Oshio, M. Miyairi, S. Watanabe, and C.R. Smith (1983):
What is actin doing in the liver cell? Hepatology, 3:433-436.
79.
Dubin, M., M. Maurice, G. Feldmann, and S. Erlinger (1978): Phalloidin-
induced cholestasis in the rat: relation to changes in microfilaments.
Gastroenterology, 75:450-455.
80.
Fuhrman-Lane, C.L., C.P. Erwin, J.M. Fujimoto, and M.J. Dibben (1981):
Altered hepatobiliary permeability induced by Amanita phalloides in the rat
and the protective role of bile duct ligation. Tax. AppL PharmacoL, 58:370378.
210
81.
Miyairi, M., C. Oshio, S. Watanabe, C.R. Smith, I.M. Yousef, and M.J.
Phillips (1984): Taurocholate accelerates bile canalicular contractions in
isolated rat hepatocytes. Gastroenterology, 87:788-792.
82.
Anderson, T., V.T. De Vita, and R.C. Young (1976): BCNU (NSC-409962)
in the treatment of advanced Hodgkin's
induction and maintenance.
disease: its role in remission
Cancer Treat. Reports, 60:761.
83.
Walker, M.D. and E.A. Gehan (1976): Clinical studies in malignant gliomas
and their treatment with the nitrosoureas. Cancer Treat. Reports, 60:713.
84.
Levin, V.A., and C.B. Wilson (1976): Nitrosourea chemotherapy for primary
malignant gliomas. Cancer Treat. Reports, 60:719.
85.
Bennett, J.M., R.F. Bakemeier, P.P. Carbone, E. Ezdinli, and R.E. Lenhard,
Jr. (1976): Clinical trials with BCNU
(NSC-409962) in malignant
lymphomas by the Eastern Cooperative Oncology Group. Cancer Treat.
Reports, 60:739.
86.
Ahmann, D.L. (1976): Nitrosoureas in the management of disseminated
malignant melanoma. Cancer Treat. Reports, 60:747.
87.
Salmon, S.E. (1976): Nitrosoureas in multiple myeloma.
Reports, 60:789.
Cancer Treat.
88.
De Vita, V.T., C. Denham, J.D. Davidson, and V.T. Oliverio (1967): The
physiological disposition of the carcinostatic 1,3-bis(2-chloroethyl)-1nitrosourea (BCNU) in man and animals. Clin. Phannacol. Ther., 8:566-577.
89.
Henner, W.D., W.P. Peters, J.P. Eder, K. Antman, L. Schnipper, and E.
Frei, III (1986): Pharmacokinetics and immediate effects of high-dose
carmustine in man. Cancer Treat. Reports, 70:877.
90.
Levin, V.A., J. Stearns, A. Byrd, A. Finn, and R.J. Weinkam (1979): The
effect of phenobarbital pretreatment on the antitumor activity of BCNU,
CCNU, PCNU, and on the plasma pharmacokinetics and biotransformation
of BCNU. J. Pharmacol. Exp. Ther., 208:1.
91.
Colvin, M., J.W. Cowens, R.B. Brundrett, B.S. Kramer, and D.B. Ludlum
(1974): Decomposition of BCNU (1,3-bis[2- chloroethyl]-1- nitrosourea) in
aqueous solution. Bioclzem. Biophys. Res. Comm., 60:515-520.
92.
Reed, D.J. (1985): Nitrosoureas. In: Oxidative Stress, Academic Press, Inc.,
115-130.
211
93.
Kann, H.E., Jr. (1978): Comparison of biochemical and biological effects of
four nitrosoureas with differing carbamoylating activities. Cancer Res.,
38:2363-2366.
94.
Wassermann, T.H. (1976): The nitrosoureas: an outline of
schedules and toxic effects. Cancer Treat. Reports, 60:709.
clinical
95.
De Vita, V.T., P.P. Carbone, A.H. Owens, Jr., G.L. Gold, M.J. Krant, and
J. Edmonson (1965): Clinical trials with 1,3-bis(2-chloroethyl)-1-nitrosourea,
NSC-409962. Cancer Res., 25:1876-1881.
96.
Thompson, G.R., and R.E. Larson (1972): A toxicologic comparison of the
potency and activity of 1,3-his(2- chloroethyl)-1-nitrosourea (BCNU) and 1(2-chloroethyl)-3-cyclohexy1-1-nitrosourea (CCNU) in mice and rats. Tox.
Appl. Pharmacol., 21:405-413.
97.
Thompson, G.R., and R.E. Larson (1969): The hepatotoxicity of 1,3-bis(2chloroethyl)-1-nitrosourea (BCNU) in rats. J. Plzannacol. Exp. Ther.,
166:104-112.
98.
Gregus, Z., and C.D. Klaasen (1982): Comparison of biliary excretion of
organic anions in mice and rats. Tox. Appl. Pharmacol., 63:13-20.
99.
Hoyt, D., and R.E. Larson (1989): Effect of 1,3-bis(2-chloroethyl)-1nitrosourea on cholephilic dye metabolism and excretion in anesthetized
rats. J. Pharmacol. Exp. Ther., 249:450-455.
100.
Becker, B.A., and G.L. Plaa (1965): Quantitative and temporal delineation
of various parameters of liver dysfunction due to a-napthylisothiocyanate.
Tox. Appl. Phannacol., 7:708-718.
101.
Becker, B.A., and G.L. Plaa (1965): The nature of a-napthylisothiocyanateinduced cholestasis. Tox. Appl. Pharmacol., 7:680-685.
102.
Capizzo, F., and R.J. Roberts (1971): a-napthyl-isothiocyanate(ANIT)induced hepatotoxicity and disposition in various species. Tox. Appl.
Pharmacol.,
103.
19:176-187.
Babson, J.R., D.J. Reed, and M.A. Sinkey (1977): Active site specific
inactivation of chymotrypsin by cyclohexyl isocyanate formed during
degradation of the carcinostatic 1-(2-chloroethyl)-3-cyclohexyl -1-nitrosourea.
Biochemistry, 16:1584-1589.
212
104. Baril, B.D., E.F. Baril, J. Laszio, and G.P. Wheeler (1975): Inhibition of rat
liver DNA polymerase by
activities.
nitrosoureas with differing carbamoylating
Cancer Res., 35:1-5.
105. Fornace, A.J., Jr., K.W. Kohn, and H.E. Kann, Jr. (1978): Inhibition of the
ligase step of excision repair by 2-chloroethyl isocyanate, a decomposition
product of 1,3-bis(2-chloroethyl)-1-nitrosourea. Cancer Res., 38:1064- 1069.
106. Reed, D.J., A.E. Brodie, and J.R. Babson (1980): Inhibition of tubulin
polymerization by nitrosourea-derived isocyanates. Biochem. Pharmacol.,
29:652-654.
107. Krell, H., H. Jaeschke, H. Hoke, and E. Pfaff (1984): Bile secretion in
hemoglobin-free perfused rat liver.
Hoppe-Seyler's Z. Physiol. Chem.,
365:1115-1122.
108. Graf, J. (1983): Canalicular bile salt-independent bile formation: concepts
and clues from electrolyte transport in rat liver. Am. J. Physiol., 244:G233G246.
109. Peterson, R.E., and J.M. Fujimoto (1977): Increased biliary tree permeability produced in rats by hepatoactive agents. J. Pharmacol. Exp. Pier.,
202:732- 739.
110. Jaeschke, H., E. Trummer, and H. Krell (1987): Increase
in biliary
permeability subsequent to intrahepatic cholestasis by estradiol valerate in
rats.
Gastroenterology, 93:533-538.
111. Mos len, M.T., M.F. Kanz, and A.E. Ferguson (1988): A stable colorimetric
assay to measure toxin elevation of inorganic phosphate in bile. Anal.
Biochem., 168:405- 410.
112. Krell, H., E. Trummer, and H. Fromm (1988): Paracellular transport of
inorganic phosphate into bile in intrahepatic cholestasis. In: Cellular
Calcium and Phosphate in Health and Disease, Alan R. Liss, Inc., 293- 298.
113. Meyer, R.A., D. McGinley, and Z. Posalaky (1986): Effects of aspirin on
tight junction structure of the canine gastric mucosa. Gastroenterology,
91:351-359.
114. Machen, T.E., D. Erlij, and F.B. Wooding (1972): Permeable junctional
complexes: the movement of lanthanum across rabbit gallbladder and
intestine. J. Cell. Biol., 54:302-312.
213
115. Martinez-Palomo, A., D. Erlij, and H. Bracho (1971):
Localization of
permeability barriers in the frog skin epithelium. J. Cell Biol., 50:277-287.
116. Penney, C.L. (1976): A simple micro-assay for inorganic phosphate. Anal.
Biochem., 75:201-210.
117. Hayat, M.A. (1986): Basic Techniques for Transmission Electron Microscopy.
Academic Press, Inc., Orlando, Fl, 226.
118. Peterson, R.E., J.R. Olson, and J.M. Fujimoto (1976): Measurement and
alteration of the capacity of the distended biliary tree in the rat. Tox. AppL
PharmacoL, 36:353-368.
119. Berk, P.D., W. Stremmel, R. Nunes, B.J. Potter, H. Okuda, N. Tavoloni, S.
Kochwa, C.L. Kiang, M. Shepard, B. Blades, and M.T. Jones (1985):
Progress in understanding the mechanisms of organic anion uptake by the
liver. In: Trends in Hepatology, edited by L. Bianchi and H. Popper, MTP
Press, Limited, Hingham, MA, 41-52.
120. Scharschmidt, B.F., J.G. Waggoner, and P.D. Berk (1975): Hepatic organic
anion uptake in the rat. J. Clin. Invest., 56:1280-1292.
121. Utili, R., C.O. Abernathy, and H.J. Zimmerman (1976): Cholestatic effects
of Eschericizia coli endotoxin on the
isolated perfused rat liver.
Gastroenterology, 70:248-253.
122. Goresky, C.A., and A.J. Schwab (1988): Flow, cell entry, and metabolic
disposal: their interactions in hepatic uptake. In: The Liver: Biology and
Pathobiology, I.M. Arias, W.B. Jakoby, H. Popper, D. Schachter, and D.A.
Shafritz, eds. New York: Raven Press, 807-832.
123. Kaplowitz, N. (1980): Physiological significance of glutathione-S-transferases.
Am. J. Physiol., 239:G439- G444.
124. Hoke, H., H. Krell, and E. Pfaff (1980): Are findings with isolated rat livers
after short calcium free perfusion relevant for isolated cells? Arch. ToxicoL,
44:23-30.
125. Hill, D.L., M.C. Kirk, and R.F. Struck (1975): Microsomal metabolism of
nitrosoureas. Cancer Res., 35:296-301.
126. Weinkam, R.J., and H.S. Lin (1979): Reactions of 1,3- bis(2-chloroethyl)-1nitrosourea and 1-( 2- chloroethyl )- 3- cyclohexyl -1- nitrosourea in aqueous
solution.
214
127. Ahmed, Ahmed E., M. Grissom, R.E. Azhary, A. Hague, P.J. Boor, and J.
Costanzi (1987): Studies on the mechanism of 1-(2-chloroethyl)-3-cyclohexyl1-nitrosourea (CCNU)- induced hepatotoxicity. II. Biochemical and
morphological characterization of the injury and its
phenobarbital. Cancer Chemother. Pharmacol., 19:103-108.
prevention by
128. Hoyt, D. Impaired Organic Anion Excretion and Cholestasis Caused by 1,3bis(2-chloroethyl)-1-nitrosourea (carmustine or BCNU) in Rats. Ph.D. Thesis,
Oregon State University, Corvallis, Oregon, 1985.
129. Berthelot, P., S. Erlinger, D. Dhumeaux, and A.M. Preaux
(1970):
Mechanism of phenobarbital-induced hyper-choleresis in the rat. Am. J.
Physiol., 219:809- 813.
130. Klaasen, C.D. (1971): Studies on the increased biliary flow produced by
phenobarbital in rats. J. Pharmacol. Exp. Ther., 176:743-751.
131. Reed, D.J. (1984): Synthesis and characterization of nitrosoureas.
In:
Anticancer and Interferon Agents, edited by R.M. Ottenbrite and G.B. Butler,
Marcel Dekker, Inc., New York, 177-202.
132. Klaasen, C.D. (1970): Plasma disappearance and biliary excretion of
sulfobromophthalein and phenol -3,6- dibromophthalein disulfonate after
microsomal enzyme induction. Biochem. Pharmacol., 19:1241-1249.
133. Simon, F.R., M. Gonzalez, E. Sutherland, L. Accatino, and R.A. Davis
(1980): Reversal of ethinyl estradiol-induced bile secretory failure with
triton WR-1339. J. Clin. Invest., 65:851-860.
134. Simon, F.R., E. Sutherland, and L. Accatino (1977): Stimulation of hepatic
(Na+,K+ ) activated ATPase activity by phenobarbital: its possible role in
regulation of bile flow. J. Clin. Invest., 59:849-861.
135. Willson, R.A., J. Hart, T. Hall, and S.H. Vincent (1990): Inverse
relationship between total glutathione-S-transferase content and bile acid
release in isolated hepatocytes from untreated, phenobarbital pretreated,
and hypothyroid rats. Pharmacol. ToxicoL, 66:121-127.
136. Feldberg, W., and C.H. Kellaway (1938): Liberation of histamine and
formation of lysocithin-like substances by cobra venom. J. Physiol., 94:187.
137. Hammarstrom, S. (1983): Leukotrienes. Ann. Rev. Biochem., 52:355-377.
215
138. Samuelsson, B. (1983): Leukotrienes: mediators of
immediate
hypersensitivity reactions and inflammation. Science, 220:568-575.
139. Piper, P.J. (1984): Formation and actions of leukotrienes. Physiol. Rev.,
64:744-761.
140. Keppler, D., H. Wolfgang, S. Rapp, C. Denzlinger, and H.K. Koch (1985):
The relation of leukotrienes to liver injury. Hepatology, 5:883-891.
141. Hagmann, W., C. Denzlinger, S. Rapp, G. Weckbecker, and D. Keppler
(1986): Identification of the major endogenous leukotriene metabolite in the
bile of rats as N-acetyl leukotriene E4. Prostaglandins, 31:239-251.
142. Hagmann, W., and D. Keppler (1988): Leukotrienes and other eicosanoids
in liver pathophysiology. In: The Liver: Biology and Pathobiology, I.M.
Arias, W.B. Jakoby, H. Popper, D. Schachter, and D.A. Shafritz, eds. New
York: Raven Press, 793-806.
143. Ford-Hutchinson, A.W. (1985): Leukotrienes: their formation and role as
inflammatory mediators. Fed. Proc., 44:25-29.
144. Brash ler, J.R., M.K. Bach, aitd D.R. Morton, Jr. (1983): The terminal step
in the biosynthesis of thioether leukotrienes: solubilization and initial
characterization of the LTA4 glutathione-S-transferase from rat basophil
leukemia cells (abstr). Fed. Proc., 42:6379.
145. Kaminski, D.L. (1989): Arachidonic acid metabolites in
hepatobiliary
physiology and disease. Gastroenterology, 97:781-792.
146. Keppler, D., C. Forsthove, W. Hagmann, S. Rapp, C. Denzlinger and H.K.
Koch (1985): Leukotrienes and liver injury. In: Trends in Hepatology, edited
by L. Bianchi and H. Popper, MTP Press, Limited, Hingham, MA, 137-145.
147. Birmelin, M., and K. Decker (1984): Synthesis of prostanoids and cyclic
nucleotides by phagocytosing rat Kupffer cells. Eur. J. Biochem. 142:501508.
148. Dieter, P., A. Schulze-Specking, and K. Decker (1986):
Differential
inhibition of prostaglandin and superoxide production by dexamethasone in
primary cultures of rat Kupffer cells. Eur. J. Biochem., 159:451-457.
149. Hua, X.Y., S.E. Dahlen, S. Hammarstrom, and P. Hedquist (1985): Leukotrienes C4, D4, and E4, cause widespread and extensive plasma extravasation
in the guinea pig. Naunyn-Schmiedeberg's Arch. Pharmacol., 330:136-141.
216
150. Roll, F.J., D.M. Bissell, and H.D. Perez (1986): Human hepatocytes
metabolizing ethanol generate a non-polar chemotactic factor for human
neutrophils. Biochem. Biophys. Res. Comm., 137:688-694.
151. Smith, M.J.H., A.W. Ford-Hutchinson, and M.A. Bray (1980): Leukotriene
B: a potential mediator of inflammation. J. Pharm. Phannacol., 32:517-518.
152. Rae, S.A. and M.J.H. Smith (1981): The stimulation of lysosomal enzyme
secretion from human polymorphonuclear leucocytes by leukotriene B4. J.
Pharm. Pharmacol., 33:616-617.
153. Serhan, C.N., A. Radin, J.E. Smolen, H. Korchak, B. Samuelsson, and G.
Weissmann (1982): Leukotriene B4 is a complete secretagogue in human
neutrophils: a kinetic analysis. Biochem. Bioplzys. Res. Comm., 107:10061012.
154. Denzlinger, C., S. Rapp, W. Hagmann, and D. Keppler (1985): Leukotrienes
as mediators in tissue trauma. Science, 230:330-332.
155. Hagmann, W., C. Denzlinger, and D. Keppler (1984): Role of peptide leukotrienes and their hepatobiliary elimination in endotoxin action. Circ. Shock,
14:223- 235.
156. Drazen, J.M., K.F. Austen, R.A. Lewis, D.A. Clark, G. Goto, A. Marfat, and
E.J. Corey (1980): Comparative airway and vascular activities of leukotrienes C-1 and D in vivo and in vitro. Proc. Natl. Acad. Sci. USA, 77:43544358.
157. Higgs, G.A. (1986): Source of leukotrienes in inflammation and their effect
on vascular permeability. In: The Leukotrienes: Their Biological Significance, edited by P.J. Piper, Raven Press, New York, 135-140.
158. Lewis, R.A., and K.F. Austen (1984): The biologically active leukotrienes:
biosynthesis, metabolism, receptors, functions, and pharmacology. J. Clin.
Invest., 73:889- 897.
159. Moncada, S. (1986): Prospects for inhibition of leukotriene biosynthesis.
In: The Leukotrienes: Their Biological
Significance, edited by P.J. Piper,
Raven Press, New York, 99-107.
160. Bach, M.K. (1984): Inhibitors of leukotriene synthesis and action. In: The
Leukotrienes: Chemistry and Biology, edited by L.W. Chakrin and D.M.
Bailey, Academic Press, Inc., Orlando, Florida, 163-194.
217
161. Bhattacherjee, P., and K.E. Eakins (1984): Lipoxygenase products:
mediation of inflammatory responses and inhibition of their formation. In:
The Leukotrienes: Chemistry and Biology, edited by L.W. Chakrin and D.M.
Bailey, Academic Press, Inc., Orlando, Florida, 195-214.
162. Hirata, F., E. Schiffmann, K. Venkatasubramanian, D. Salomon, and J.
Axelrod (1980): A phospholipase A2 inhibitory protein in rabbit neutrophils
induced by glucocorticoids. Proc. Natl. Acad. Sci. USA, 77:2533- 2536.
163. Haynes, R.C., Jr., and F. Murad (1985): Adrenocorticotropic hormone;
adrenocortical steroids and their
adrenocortical steroid biosynthesis.
synthetic analogs; inhibition of
In: Goodman and Gilman's The
Pharmacological Basis of Therapeutics, edited by A.G.
Gilman, L.S.
Goodman, T.W. Rall, and F. Murad, Macmillan Pub. Co., New York, 14591489.
164. Tubaro, A., P. Del Negro, E. Ragazzi, S. Zampiron, R. Della Loggia (1988):
Anti-inflammatory and peripheral analgesic activity of esculetin in vivo.
PharmacoL Res. Comm., 20:83-85.
165. Sekiya, K., H. Oduda, and S. Arichi (1982): Selective inhibition of platelet
lipoxygenase by esculetin. Biochim. Biophys, Acta, 713:68-72.
166. Neichi, T., Y. Koshihara, and S. Murota (1983):
Inhibitory effect of
esculetin on 5-lipoxygenase and leukotriene biosynthesis. Biochim. Biophys.
Acta, 753:130-132.
167. Kimura, Y., H. Okuda, S. Arichi, K. Baba, and M. Kozawa (1985): Inhibition of the formation of 5-hydroxy-6,8,11,14-eicosatetraenoic acid from
arachidonic acid in polymorphonuclear leukocytes by various coumarins.
Biochim. Biophys. Acta, 834:224-229.
168. Appelgren, L., and S. Hammarstrom (1982): Distribution and metabolism
of 3H-labeled leukotriene C3 in the mouse. J. Biol. Chem., 257:531-535.
169. Ormstad, K., N. Uehara, S. Orrenious, L. Orning, and S. Hammarstrom
(1982): Uptake and metabolism of leukotriene C3 by isolated rat organs and
cells. Biochem. Biophys. Res. Comm., 104:1434-1440.
170. Sun, F.F., L. Chau, B. Spur, E.J. Corey, R.A. Lewis, and K.F. Austen
(1986): Identification of a high affinity leukotriene C4-binding protein in rat
liver cytosol as glutathione-S-transferase. J. BioL Chem., 261:8540- 8546.
218
171. Bhargava, M.M., N. Ohmi, I. Listowsky, and I.M. Arias (1980): Structural,
catalytic, binding, and immunological properties associated with each of the
two subunits of rat liver ligandin. J. Biol. Chem., 255:718-723.
172. Hagmann, W., S. Parthe, and I. Kaiser (1989): Uptake, production, and
metabolism of cysteinyl leukotrienes in the isolated perfused rat liver.
Biochem. J., 261:611- 616.
173. Tiegs, G., and A. Wendel (1988): Leukotriene-mediated liver injury.
Biochem. Pharmacol., 37:2569-2573.
174. Hagmann, W., C. Denzlinger, and D. Keppler (1985): Production of peptide
leukotrienes in endotoxin shock. Febs Letters, 180:309-313.
175. Keppler, D., J. Pausch, and K. Decker (1974): Selective uridine triphosphate
deficiency induced by D- galactosamine in liver and reversed by pyrimidine
nucleotide precursors. Effect on ribonucleic acid synthesis. J. BioL Chem.,
249:211-216.
176. Trudell, J.R., M. Bendix, and B. Bosterling (1984): Hypoxia potentiates
killing of hepatocyte monolayers by leukotrienes, hydroperoxyeicosa-
tetraenoic acids, or calcium ionophore A23187. Biochim. Biophys. Acta,
803:338-341.
177. Wendel, A., G. Tiegs, and C. Werner (1987): Evidence for the involvement
of a reperfusion injury in galactosamine/endotoxin-induced hepatitis in
mice.
Biochem. PharrnacoL, 36:2637-2639.
178. Krell, H., and E. Dietze (1989): Hemodynamic and metabolic responses to
leukotriene C4 in isolated perfused rat liver. Hepatology, 10:300-305.
179. Sasaki, T., S. Ohta, A. Kamogawa, and M. Shinoda (1990): Protective
effects of various Chinese traditional medicines against experimental
cholestasis. Chem. Pharm. Bull., 38:513-516.
180. Stachura, J., A. Tarnawski, K.J. Ivey, T. Mach, J. Bogdal, J. Szczudrawa, and
B. Klimczyk (1981): Prostaglandin protection of carbon tetrachlorideinduced liver cell necrosis in the rat. Gastroenterology, 81:211-217.
181. Ruwart, M.J., B.D. Rush, N.M. Friedle, J. Stachura, and A. Tarnawski
(1984): 16,16-dimethyl-PGE, protection against a-napthylisothiocyanateinduced experimental cholangitis in the rat. Hepatology, 4:658-660.
219
182. Lee, C.W., R.A. Lewis, and A.I. Tauber (1983): The myeloperoxidasedependent metabolism of leukotrienes C4, D4, and E4 to 6-transleukotriene B4 diastereoisomers and the subclass-specific S-diastereoismeric
sulfoxides. J. Biol. Chem., 258:15004-15010.
183. Henderson, W.R. and S.J. Klebanoff (1983): Leukotriene production and
inactivation by normal, chronic granulomatous disease and myeloperoxidasedeficient neutrophils. .1. Biol. Chem., 258:13522-13527.
184. Davies, P. and A.C. Allison (1978): The release of hydrolytic enzymes from
phagocytic and other cells participating in acute and chronic inflammation.
In: Inflammation, edited by J.R. Vane and S.H. Ferreira, Springer, New
York, 267-294.
185. Blaschke, T.F. and R.J. Elfin (1973): Effect of induced fever on sulfobromophthalein kinetics in man. Ann. Inter. Med., 78:221-226.
186. Larson, R.E. and D.P. Rall (1965): A study of the toxicity of 1,3-bis(2chloroethyl)-1-nitrosourea (BCNU, NSC-409962) (abstr). Pharmacologist,
7:180.
187. Kretschmer, N.W., P.J. Boor, R.A. el Azhary, A.E. Ahmed, and E.S.
Reynolds (1987): Studies on the mechanism of 1-(2-chloroethyl)-3-cyclohexyl1-nitrosourea (CCNU)-induced hepatotoxicity. III. Ultra-structural
characterization of bile duct injury. Cancer Chemother. PharmacoL, 19:109117.
188. Goldfarb, S., E.J. Singer, and H. Popper (1962): Experimental cholangitis
due to alpha-napthyl-isothiocyanate (ANIT). Am. J. Pathol, 40:685-695.
189. Moran, E., M. Eliakim, and H. Ungar (1965): The effect of cortisone on
cholangitis induced by a-napthylisothiocyanate in rats. Gastroenterology,
48:773-783.
190. Schaffner, F., H. Scharnbeck, and F. Hutterer, H. Denk, H.A. Greim, and
H. Popper (1973): Mechanism of chole- stasis. VII. a-napthylisothiocyanateinduced jaundice. Lab. Invest., 28:321-331.
191. Connolly, A.K., S.C. Price, J.C. Connelly, and R.H. Hinton (1988): Early
changes in bile duct lining cells and hepatocytes in rats treated with anapthylisothiocyanate. Tox. Appl. PharmacoL, 93:208-219.
220
192. Dawson, W., and D.A. Willoughby (1985): Inflammation: sites and
mechanisms. In: Nonsteroidal Antiinflammatoty Drugs, edited by J.G.
Lombardino, John Wiley and Sons, New York, 79-109.
193. Raud, J. (1989): Intravital microscopic studies on acute mast cell-dependent
inflammation. Acta Phys. Scand. Suppl. 578:6-53.
194. Oertel, H.L. and M. Ka liner (1981): The biologic activity of mast cell
granules. III. Purification of inflammatory factors of anaphylaxis (IF-A)
responsible for causing late-phase reactions. J. Immunol., 127:1398-1402.
195. White, M.V. and M.A. Ka liner (1987): Neutrophils and mast cells. I.
Human neutrophil-derived histamine-releasing activity. J. Immunol.,
139:1624-1630.
196. Ka liner, M. (1989): Asthma and mast cell activation. J. Alley
Immunol., 83:510-520.
Clin.
197. Atkins, F.M. (1987): Mast cells and fibrosis. Arch. DermatoL, 123:191-193.
198. Metcalfe, D.D. and M.A. Donlon (1981): The mast cell. CRC Crit. Rev.
Immunol., 3:23-74.
199. Parwaresch, M.R., H.P. Horny, and K. Lennert (1985): Tissue mast cells in
health and disease. Path. Res. Pract., 179:439-461.
200. Peters, S.P., M.I. Siegel, A.K. Sobotka, and L.M. Lichtenstein (1981):
Lipoxygenase products modulate histamine release in human basophils.
Nature, 292:455-457.
201. Sullivan, T.J. and C.W. Parker (1976): Pharmacologic
modulation of
inflammatory mediator release by rat mast cells. Am. J. Pathol., 85:437-464.
202. Tannenbaum, S., H. Oertel, W. Henderson, and M. Ka liner (1980): The
biologic activity of mast cell granules. I. Elicitation of inflammatory
responses in rat skin. J. Immunol., 125:325-335.
203. Galli, S.J. (1987): New approaches for the analysis of mast cell maturation,
heterogeneity, and function. Fed. Proc., 46:1906-1914.
204. Chock, S.P. and E.A. Schmauder-Chock (1988): Synthesis of prostaglandins
and eicosanoids by the mast cell secretory granule. Biocizem. Biophys. Res.
Comm., 156:1308-1315.
221
205. Heavey, D.J., P.B. Ernst, R.L. Stevens, A.D. Befus, J. Bienenstock, and K.F.
Austen (1988): Generation of leukotriene C4, leukotriene B4, and prostaglandin D2 by immunologically-activated rat intestinal mucosa mast cells.
J. Immunol., 140:1953-1957.
206. Orange, R.P. (1975): Dissociation of the immunologic release of histamine
and slow reacting substance of anaphylaxis from human lung using cytochalasins A and B. J. Immunol., 114:182-186.
207. Warner, J.A., L.M. Lichtenstein, and D.W. MacGlashan, Jr. (1988): Effects
of specific inhibitor of the 5-lipoxygenase pathway on mediator release from
human basophils and mast cells. .1. Pharmacol. Exp. Ther., 247:218-222.
208. Peters, S.P., R.P. Schleimer, R.M. Naclerio, et al.
(1987): The
pathophysiology of human mast cells: in vitro and in vivo function. Am. Rev.
Respir. Dis., 135:1196-1200.
209. Marone, G., V. Casolaro, R. Cirillo, C. Stellato, and A. Genovese (1989):
Pathophysiology of human basophils and mast cells in allergic disorders.
Clin. Immunol. Immunopatlzol., 50:S24-S40.
210. Stevens, R.L. and K.F. Austen (1989): Recent advances in the cellular and
molecular biology of mast cells. Immunol. Today, 10:381-386.
211. Malone, D.G., R.L. Wilder, A.M. Saavedra-Delgado, and D.D. Metcalfe
(1987): Mast cell numbers in rheumatoid synovial tissues: correlations with
quantitative measures of lymphocytic infiltration and modulation by
antiinflammatory therapy. Arth. Rheum., 30:130-137.
212. Balazs, M., G. Illyes, and G. Vadasz (1989): Mast cells in ulcerative colitis:
quantitative and ultrastructural studies. Virchows Archiv. B Cell Pat hot.,
57:353-360.
213. Galli, S.J., B.K. Wershil, R. Bose, P.A. Walker, and S. Szabo (1987):
Ethanol-induced acute gastric injury in mast cell-deficient and congenic
normal mice. Evidence that mast cells can augment the area of damage.
Am. J. Pathol., 128:131-140.
214. Beck, P.L., G.P. Morris, and J.L. Wallace (1988): Reduction of ethanolinduced gastric damage by sodium cromoglycate and FPL-52694. Role of
leukotrienes, prostaglandins, and mast cells in the protective mechanism.
Can. J. Physiol. Pharmacol., 67:287-293.
222
215. Reimann, H.J., J. Lewin, U. Schmidt, P. Wendt, G. Gleuml, and E.Z.
Dajani (1987): Misoprostol prevents damage to the gastric mucosa by
stabilizing the mast cells. Prostaglandins, 33(Suppl.):105-116.
216. Perdue, M.H., J.K. Ramage, D.B. Burget, J. Marshall, and S. Masson
(1989): Intestinal mucosal injury is associated with mast cell activation and
leukotriene generation during Nippostrongylus-induced inflammation in the
rat. Dig. Dis. ScL, 34:724-731.
217. Lynes, W.L., S.D. Flynn, L.D. Shortliffe, et al. (1987): Mast cell involvement
in interstitial cystitis. J. Via, 138:746-752.
218. Johnson, D., P.A. Seeldrayers, and H.L. Weiner (1988): The role of mast
cells in demyelination. 1. Myelin proteins are degraded by mast cell
proteases and myelin basic protein and P2 can stimulate mast cell
degranulation. Brain Res., 444:195-198.
219. Macia, R.A., A.C. Silver, R.A. Gabel, G.K. Campbell, N. Hanna, and M.J.
Di Martino (1990): Hypotension induced by vasopressin antagonists in rats:
role of mast cell degranulation. Tox. AppL Pharmacol., 102:117-127.
220. Keller, A.M., R.M. Clancy, M.L. Barr, C.C. Marboe, and P.J. Cannon
(1988): Acute reoxygenation injury in the isolated rat heart: role of resident
cardiac mast cells. Circ. Res., 63:1044-1052.
221. Masini, E., E. Giannella, S. Bianchi, and P.F. Mannaioni (1987): Histamine
and lactate dehydrogenase (LDH) release in ischemic myocardium of the
guinea pig. Agents Actions, 20:281-283.
222. Decorti, G., F.B. Klugmann, L. Candussio, and L. Baldini
(1987):
Adriamycin-induced histamine release from rat peritoneal mast cells: role
of free radicals. Anticancer Res., 7:497-500.
223. Day, R., S. Lemaire, D. Nadeau, I. Keith, and I. Lemaire (1987): Changes
in autacoid and neuropeptide contents of lung cells in asbestos-induced
pulmonary fibrosis. Am. Rev. Respir. Dis., 136:908-915.
224. Keith, I., R. Day, S. Lemaire, and I. Lemaire (1987): Asbestos-induced
fibrosis in rats: increase in lung mast cells and autacoid contents. Exp. Lung
Res., 13:311-327.
225. Kalenderian, R., L. Raju, W. Roth, L. Schwartz, and A. Janoff (1988): Elevated histamine and tryptase levels in smokers' bronchoalveolar lavage fluid.
Do lung mast cells contribute to smoker's emphysema? Chest, 94:119-123.
223
226. Gittlen, S.D., E.S. Schulman, and W.C. Maddrey (1990): Raised histamine
concentrations in chronic cholestatic liver disease. Gut, 31:96-99.
glucose after
compound 48/80 treatment is not related to hepatic mast cell degranulation
227. Dimlich, R.V. and F.D. Reilly (1986): Elevated blood
in rats. Proc. Soc. Exp. Biol. Med., 183:321-327.
228. Wakajtys-Rode, E., A. Dabrowski, H. Grubek-Jaworska, B. Machnicka, and
W. Droszcz (1988): Binding of dexa-methasone and its effect on histamine
release from rat mast cells. Int. J. Immunopharmacol., 10:925-930.
229. Daeron, M., A.R. Sterk, F. Hirata, and T. Ishizaka (1982): Biochemical
analysis of glucocorticoid-induced inhibition of IgE-mediated histamine
release from mouse mast cells. J. Immunol., 129:1212-1218.
230. Robin, J.L., D.C. Seldin, K.F. Austen, and R.A. Lewis (1985): Regulation
of mediator release from mouse bone marrow-derived mast cells
by
glucocorticoids. J. Immunol., 135:2719-2726.
231. Schleimer, R.P., L.M. Lichtenstein, and E. Gillespie (1981): Inhibition of
basophil histamine release by anti- inflammatory steroids. Nature, 292:454455.
232. Blackwell, G.J., R.J. Flower, F.P. Nijkamp, and J.R. Vane (1978): Phospholipase A, activity of guinea pig isolated perfused lungs: stimulation and
inhibition by antiinflammatory steroids. Br. J. PharacoL, 62:79-89.
233. Murray, M., W.F.H. Jarrett, and F.W. Jennings (1971): Mast cells and
macromolecular leak in intestinal immunological reactions. The influence
of sex of rats infected with Nippostrongylus brasiliensis. Immunology, 21:1731.
234. Milks, L.C., G.P. Conyers, and E.B. Cramer (1986): The effect of neutrophil
migration on epithelial permeability. J. Cell BioL, 103:2729-2738.
235. Masini, E., B. Pamerani, F. Gambassi et al. (1990): Histamine release from
rat mast cells induced by metabolic activation of polyunsaturated fatty acids
into free radicals. Biochem. PhannacoL, 39:879-889.
236. Fantaozzi, R., S. Brunelleschi, A. Rubino et al. (1986): FMLP-activated
neutrophils evoke histamine release from mast cells. Agents Actions, 18:155158.
224
237. Jarvi, E.J. Biochemical Changes Associated with BCNU- Induced Pulmonary
Toxicity. Ph.D. Thesis, Oregon State University, Corvallis, Oregon, 1986.
238. Claman, H.N. (1989): On scleroderma: mast cells, endothelial cells, and
fibroblasts. JAMA, 262:1206-1209.
239. Gomes, J.C. and F.L. Pearce (1988): Comparative studies on the effect on
non-steroidal antiinflammatory drugs (NSAID) on histamine release from
mast cells of the rat and guinea pig. Agents Actions, 24:266-271.
240. Last, J.A. (1985): Changes in the collagen pathway in fibrosis. Fund. Appl.
Toxicol., 5:210-218.
241. Popper, H., and S. Udenfriend (1970): Hepatic fibrosis.
Am. J. Med.,
49:707-721.
242. Fuller, G.C. (1985): Symposium: development and assessment of fibrosis.
Fund. Appl. Toxicol., 5:207-209.
243. Nishioka, K., Y. Kobayashi, I. Katayama, and C. Takijiri (1987): Mast cell
numbers in diffuse scieroderma. Arch. Dennatol., 123:205-208.
244. Claman, H.N. (1987): New hope for neurofibromatosis? The mast cell
connection. JAMA, 258:823.
245. Giorno, R., J. Leiber, and H.N. Claman (1989): Ultrastructural evidence for
mast cell activation in a case of neurofibromatosis. Neurofibromatosis, 2:3541.
246. Tomioka, M., T. Goto, T.D.G. Lee, J. Bienenstock, and A.D. Befus (1989):
Isolation and characterization of lung mast cells from rats with bleomycininduced pulmonary fibrosis. Immunology, 66:439-444.
247. Sterling, K.M., T. Di Petrillo, K.R. Cutroneo, and A. Prestayko (1982):
Inhibition of collagen accumulation by glucocorticoids in rat lung after
intratracheal bleomycin instillation. Cancer Res., 42:405-408.
248. Rojkind, M., and L.D. De Leon (1970): Collagen biosynthesis in cirrhotic
rat liver slices: a regulatory mechanism. Biochim. Biophys. Acta, 217:512522.
249. Yam, L.T., C.C. Chan, and C.Y. Li (1986): Hepatic involvement in systemic
mast cell disease. Am. J. Med., 80:819-826.
225
250. Horny, H., E. Kaiser ling, M. Campbell et al. (1989): Liver findings in
generalized mastocytosis: a clinicopathologic study. Cancer, 63:532-538.
251. Murata, K., M. Okudaira, and K. Akashi() (1973): Mast cells in human liver
tissue. Acta Dermat., Suppl. 73:157-166.
252. Narayanan, M.N., J.A. Liu Yin, S. Azzawi, T.W. Warnes, and W.P.G. Turck
(1989): Portal hypertension and ascites in systemic mastocytosis. Postgrad.
Med. J., 65:394-396.
253. Umezu, K., S. Yuasa, and A. Sudoh (1985): Change of hepatic histamine
content during hepatic fibrosis. Biochem. Pharmacol., 2007-2011.
254. Choi, K.L., and H.N. Claman (1987): Mast cells, fibroblasts, and fibrosis.
New clues to the riddle of mast cells. Immunol. Res., 6:145-152.
255. Ginsburg, H., M. Amira, J. Padawer, and S. Davidson (1989): Structural
alterations in fibroblast monolayers caused by mast cell degranulation. J.
Leuk. Biol., 45:491-497.
256. Levi-Schaffer, F., E.T. Dayton, K.F. Austen et al. (1987): Mouse bone
marrow-derived mast cells cocultured with fibroblasts. J. Immunol.,
139:3431-3441.
257. Rall, M.B., and D.M. McCarthy (1963): 1,3-bis(2- chloroethyl)-1-nitrosourea
(BCNU): toxicity and initial clinical trial (abstr). Proc. Am. Ass. Cancer
Res., 4:55.
258. Melato, M., and G. Tuveri (1980): Pulmonary fibrosis following low-dose
1,3-bis(2-chloroethyl)-1-nitrosourea (BCNU) therapy. Cancer, 45:1311-1314.
259. Aronin, P.A., M.S. Mahaley, Jr., S.A. Rudnick et al. (1980): Prediction of
BCNU pulmonary toxicity in patients with malignant gliomas. An assessment of risk factors. N. Engl. J. Med., 303:183-188.
(1981): Early
pulmonary toxicity after administration of high-dose BCNU. Cancer Treat.
260. Litam, J.P., D.H. Dail, G. Sptizer, L. Vellekoop et al.
Reports, 65:39-44.
261. Schuller, H.M., A.0 Smith, M. Gregg, and M.R. Boyd (1985): Sequential
pathological changes induced in rats with the anti-cancer drug 1,3-bis(2chloroethyl)-1-nitrosourea (BCNU). Exp. Lung Res., 9:327-339.
226
performance in
262. Rawson, C.L., and R.E. Larson (1989): Cardiovascular
anesthetized rats pretreated with 1,3- bis(2-chloroethyl)-1-nitrosourea
(BCNU). Res. Comm. Chem. Path. Pharmacol., 64:407-419.
263. Dahm, L.J., and R.A. Roth (1990): Depletion of circulating neutrophils
The
attenuates a-napthyl-isothiocyanate (ANIT)-induced liver injury (abstr).
Toxicologist, 10:275.
264. Little, J.M., K. Cage, D.G. Oelberg, and R. Lester (1985): Pathogenesis of
the pruritus of cholestasis: an initial hypothesis (abstr). Hepatology, 5:1005.
265. Galli, S.J., N. Arizono, T. Murakami, A.M. Dvorak, and J.G. Fox (1987):
Development of large numbers of mast cells at sites of idiopathic chronic
dermatitis in genetically mast cell-deficient WBB6FI-W/Wv mice. Blood,
69:1661-1666.
APPENDIX
227
3.0
2.5
2.0
1.5-
1.0-
ISOLATED LIVER
0-e-e-e-e-ii
\0-s
'
40,
0.5
0.0
0
10
20
30
40
50
MIN AFTER BILE DUCT CANNULATION
Appendix Figure 1. Decrease in control bile flow with bile duct cannulation and
liver perfusion. Bile was collected in pretared tubes at 2-minute intervals. Bile
flow was determined gravimetrically, assuming 1 g/ml. Values are for a single
animal. The static flow after 20 minutes represents basal flow.
228
.06
0
p.05
a- .04
0
LJJ
> .03
.02
24
48
72
96
5 weeks
TIME (FIRS)
Appendix Figure 2. Increase in liver/body weight ratio with BCNU or ANIT
treatment. Livers were removed from rats 12, 24, 36, or 48 hours after ANIT
treatment (250 mg/kg) or 24, 36, 48, 72, or 96 hours or 5 weeks after BCNU
treatment (26 mg/kg). Livers were patted dry with paper towels before weighing.
A steady increase in liver/body weight ratio was observed with either ANIT or
BCNU treatment. Values are means + SE; n = 3-18. *Significantly different from
control, P < 0.05.
229
1 .5
0.0
0
10
20
30
40
50
TIME (MIN)
Appendix Figure 3. HRP excretion in the perfused liver with ANIT treatment.
(250 mg/kg, gavage). 10
Livers were perfused 48 hours after ANIT treatmentnormal saline) was infused
minutes after start of the perfusion, HRP (25 mg in
ice in pretared tubes at
over a period of one minute. Bile was then collected on
Values
are the average of
5-minute intervals and assayed for HRP as described.
2 rats.
230
2.0
- SPRAGUE-DAWLEY
-A WISTAR
T
E 1.5
1-1
[LI 1.0
cn
ILI
0.5
m
H-
0.0
0
12
24
36
48
TIME (HR)
Appendix Figure 4. Difference in time course of increased bile Pi following ANIT
treatment between Sprague Dawley and Wistar rats. Bile was collected 12, 24, or
36 hours after ANIT treatment (250 mg/kg, gavage) and assayed for Pi as
described. A marked difference in time course of Pi penetration into bile was
observed. Values are means ± SE; n = 3-15. `Significantly different from Wistar,
P < 0.05.
231
2.0
1.5
1.0
0.5
0.0
0
12
24
36
48
TIME (HRS)
Appendix Figure 5. Time course of change in bile flow and bile Pi in Wistar rats
with ANIT treatment. Bile was collected 12, 24, or 36 hours after ANIT treatment
(250 mg/kg, gavage) and assayed for P, as described. In vivo bile flows are shown.
An apparent direct, rather than inverse, correlation between these parameters was
observed. Values are means + SE;
n = 3-4.
232
3.0
.."'N.
L(1)
>
2.5
:
cp
\c_ 2.0
E
--.,
1.5
2
lb
8
00
0
01110
0
_1
1.0
1
LI_
LI
.0
%
0.5
c-6"
0.0
0.00
0.50
1.00
1.50
2.00
BILE PHOSPHATE (mM)
Appendix Figure 6. Lack of correlation between bile Pi and bile flow with BCNU
treatment. Bile was collected 24, 48, 72, or 96 hours after BCNU treatment (26
mg/kg, i.p.) and assayed for Pi as described. No correlation between bile flow and
bile Pi was observed. Values are from individual rats; n = 56.
233
Appendix Table 1. Decreased bile flow and increased bile inorganic
phosphate with CCNU treatment. CCNU was dissolved in corn oil,
28 mg/ml, and administered i.p. 1.0 ml/kg.
TREATMENT
BILE FLOW
Pi
CONTROL
1.82 + .04
.17 + .02
CCNU(24h)
2.10 + .23
.52 + .07a
CCNU(48h)
.91 + .18a
2.37 + .16a
CCNU(96h)
1.15 + .37a
.74 + .35a
Values are means ± SE.
aSignificantly different from control, P < 0.05.