Supporting a Healthy Workforce Professor Diana Kloss MBE
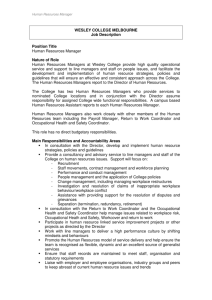
advertisement
Supporting a Healthy Workforce Professor Diana Kloss MBE Chair, Council for Work and Health Working for a Healthier Tomorrow • This was the first report of Dame Carol Black (2008) about the health of the working population and the importance of OH services. She said: • “Achieving a comprehensive service for the future requires much more than simply integration. It demands leadership from the professions to seize this opportunity and to make the specialty of occupational health relevant to present-day needs. It can only be done by expanding the remit of OH to include all those of working age, and working with other specialtiesboth medical and non-medical-in order to achieve this.” • The report led to a system of accreditation of OH services, recently extended to physiotherapists (SEQOHS) • It led to the introduction of the GP fit note, followed by the Black/Frost report (2011) on sickness absence, which gave birth to the Fit for Work Service, which has now been rolled out throughout England, Wales and Scotland, providing publicly funded skilled advice to employees and employers about return to work after sickness absence of 4 weeks The Council for Work and Health www.councilforworkandhealth.org.uk • And it led to the creation of a Council for Work and Health, representing all the organisations involved in protecting the health of the working population and providing occupational health services • It has the great strength that it is multidisciplinary and includes representatives from the health and safety professionals as well as those providing care • It also includes representatives from the TUC, the CBI, PHE, and the Department of Health For the future? • Things have been moving fast in the health, work and wellbeing field • There is an even greater need for the professions to speak with one voice • The proposal that the Faculty and Society of Occupational Medicine should become a single organisation has not achieved the necessary support of all their members, but they are now working closely together, eg the July conference in Manchester • However, at present the Council is the only body that represents all the professions • A National School of Occupational Health was launched by Health Education England in 2014. At present it only deals with doctors, but the plan is gradually to extend it to other health professionals, especially nurses and physiotherapists Planning the future • In 2013 a Project Working Group was set up by the Council to deliver a vision of good work and health in the UK for the next 5-20 years and the professional resources to deliver it. It is chaired by Professor John Harrison, an occupational physician and Dean of the National School, and the research fellow is Leonie Dawson, an occupational physiotherapist • The research is supported by funds from Syngentis and Public Health England, and from the Council • The first part of the report was published in April 2014 (see the Council website) and the second part is nearing completion NICE PHAC Committee • Workplace health: policy and management practices [NG 13] • Date of publication: June 2015 • www.nice.org.uk • It concentrates particularly on the role of the line manager Principal recommendations • Create an organisation committed to workplace health and wellbeing, ensure a safe and healthy physical work environment, create a supportive environment to help employees avoid the negative effects of stress, ensure fairness and justice throughout the organisation, encourage participation, provide leadership, empower line managers, design jobs that are not damaging and if possible have a positive effect on health and wellbeing • Management makes the decisions, but they need the advice and assistance of well-trained competent professionals What do they do? • They advise managers on their legal obligations and assist them to comply with the law, for example: • Safety officers on prevention of accidents and disease, eg control methods, protective equipment, RIDDOR Statutory health surveillance, for example under the Control of Vibration at Work Regulations 2005 (nurses and doctors), monitoring of noise and dust levels (hygienists) to comply with COSHH Advise on the avoidance of musculoskeletal disease and the treatment of MSD (ergonomists and physiotherapists) Advise on the definition of disability under the Equality Act 2010 and make recommendations for reasonable adjustments for disabled employees, supporting employees in the process of rehabilitation (doctors, nurses, vocational rehabilitation specialists, occupational therapists) Advise on the prevention of undue workplace stress and provide treatment for stressed workers (psychologists) • • • • What do they do? • They assist the manager in assessing fitness for work both preemployment and in employment, eg blood tests for HCWs with blood-borne viruses, physical fitness tests for police and firefighters • They assist the manager in advising on sickness absence and return to work, and if this is not possible dismissal and ill-health retirement • NB the NICE guidelines suggest that over aggressive return to work procedures can encourage presenteeism to the detriment of the organisation • Reducing the numbers of days off sick should not be the only yardstick for an efficient service • The Work Foundation Report (2010) estimated that employees’ substandard performance at work when unfit costs one and a half times more to the economy that the cost of sickness absence What do they do? • They assist in advising on and developing healthy living policies and programmes in the workplace • This is achieving wide recognition, for example see Simon Stevens’ “Five Year Forward”, statement on the future of the NHS (2014): • NHS Employers should create new incentives to support 1.3m employees to stay healthy and be “health ambassadors”, eg providing healthy food, especially on the night shift, encouraging weight reduction, quitting smoking, adopting the HSE Management Standards for Work Related Stress, and “review with the Faculty of Occupational Medicine the strengthening of occupational health”. • Simon Stevens announced an ambitious programme to promote the health and wellbeing of NHS employees on 2 September 2015, concentrating on healthy food, opportunities for exercise in the workplace, free health checks of mental health and MSK health for employees over 40, and OH service for GPs suffering from stress. What needs to be done? • We need to recruit and train more health professionals, particularly doctors and nurses, in occupational health • We need to define the essential competencies of the professionals in order to optimise training and assessment • We need to persuade employers that the health of their workers is a vital economic resource and that they cannot afford not to support healthy living programmes • We need to encourage employees to take responsibility for their own health • We need to audit and to do research into what works best