Carotid Revascularization: Who, When, and How
advertisement
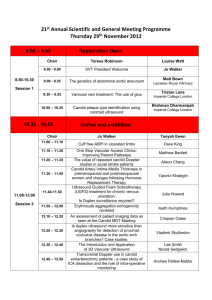
Carotid Revascularization: Who, When, and How JAMES T DEVRIES, MD, FACC, FSCAI ASSISTANT PROFESSOR OF MEDICINE GEISEL SCHOOL OF MEDICINE AT DARTMOUTH DIRECTOR, CARDIAC CATHETERIZATION LAB DARTMOUTH-HITCHCOCK MEDICAL CENTER DISCLOSURES None of the planners or presenters of this session have disclosed any conflict or commercial interest Carotid Revascularization: Who, When, and How OBJECTIVES: 1. Describe symptomatic and asymptomatic carotid artery disease. 2. Review the research related to revascularization. 3. Explain which procedure is indicate depending on the specific patient evaluation. Outline Background Part 1: Asymptomatic carotid disease Part 2: Symptomatic carotid disease Part 3: Stenting versus surgery Overall conclusions PART 1: Asymptomatic Carotid Stenosis Clinical Question #1 A 67 yo male is seen in clinic follow up. He has an asymptomatic left carotid bruit and a duplex demonstrates a 50-79% stenosis of the left internal carotid artery. He has known CAD and hyperlipidemia and is on aspirin and atorvastatin. He has a normal creatinine. The one year risk for an ipsilateral stroke is: A. 1% B. 3% C. 5-7% D. >10% Clinical Question #2 The patient in question #2 wants the best therapy possible for his carotid stenosis, telling you “I don’t want a stroke.” You recommend: A. . Add clopodigrel (Plavix) to his medications and monitor with serial duplex B. Referral for immediate carotid artery stent (CAS) with embolic protection device C. Referral for immediate carotid endarterectomy (CEA) D. Continue current medical therapy with serial duplex exams Stroke: By the Numbers 800,000 strokes/year in the United States Approximately 80% are ischemic, 20% hemorrhagic 8-10% of ischemic strokes are attributed to carotid stenosis; mechanism is plaque rupture and embolism In the year 2012, in the United States we performed: ~8,000 carotid artery stent (CAS) procedures 140,000 carotid endarterectomy (CEA) procedures CEA is one of the most common procedures performed in vascular surgeons’ daily practice Asymptomatic Carotid Stenosis By age 75, about 7% of the population will have some degree of asymptomatic stenosis In the Medicare population over age 65, 1-2% will have high grade asymptomatic carotid stenosis Management of these patients is controversial, based in part on variable or small benefits for revascularization in randomized trials and improvements in medical therapy since pivotal trials have been published What would NEJM readers do? Common problem; common procedure, so….. WHY THE CONTROVERSY? ACAS and ACST: Pivotal Trials ACAS and ACST Results: 5 year Outcomes ACAS and ACST: Issues Medical therapy arm had essentially no therapy: statins, BP control, antiplatelet therapy Surgical sites were highly selected: best outcomes (3% stroke risk during surgery) Population studied: Men!! Sooooo- the best surgeons compared to the worst medical therapy had a very small benefit, maybe none in women? Are we sure about this?? Annual Stroke Risk for Asymptomatic Disease Medical Therapy: A Moving Target Changes in Stroke Risk over Time Statin Use in ACST Lancet 2010;376:1074 Effect of Statin Use on Outcomes The writing is on the board: Statins work! Guidelines: 2011 Update for Asymptomatic Class I Class IIA Guidelines: 2011 Update for Asymptomatic Class IIb How to Pick? Management of Asymptomatic Stenosis Clinical Question #1 A 67 yo male is seen in clinic follow up. He has an asymptomatic left carotid bruit and a duplex demonstrates a 50-79% stenosis of the left internal carotid artery. He has known CAD and hyperlipidemia and is on aspirin and atorvastatin. He has a normal creatinine. The one year risk for an ipsilateral stroke is: A. 1% B. 3% C. 5-7% D. >10% Clinical Question #2 The patient in question #2 wants the best therapy possible for his carotid stenosis, telling you “I don’t want a stroke.” You recommend: A. . Add clopidogrel (Plavix) to his medications and monitor with serial duplex B. Referral for immediate carotid artery stent (CAS) with embolic protection device C. Referral for immediate carotid endarterectomy (CEA) D. Continue current medical therapy with serial duplex exams Part 2: Symptomatic Carotid Stenosis Clinical Question A 67 y.o. male presents with right eye amaurosis fugax lasting for 5 minutes three days ago. His symptoms resolved spontaneously and he underwent duplex scanning of the carotid arteries, revealing an 80% RICA stenosis with some “plaque ulceration.” He has known paroxsymal atrial fibrillation, hypertension, and lower extremity PAD. His medications include aspirin, lisinopril, atorvastatin, and coumadin. INR is 1.9. Best next therapy is: A. Add clopidogrel (Plavix) to medications and monitor B. Refer for immediate CEA C. Refer for immediate CAS D. TEE E. Double statin dose and repeat duplex in 3 months Symptomatic Carotid disease Clinical symptoms are related to hemispheric stroke/TIA from an unstable carotid plaque Symptoms occurred within the previous 6 months Pivotal Trials which have shaped guidelines are: NASCET (North American Symptomatic Carotid Endarterectomy Trial) published 1991 in NEJM ECST (European Carotid Surgery Trial) published in Lancet in 1998 Outcomes: ECST and NASCET Determining Stenosis Severity in Trials ECST and NASCET had different stenosis determination ECST 80%= NASCET 60% Relationship Between % Stenosis and Stroke 95-99% 70-95% stenosis Relationship between % Stenosis, Age, Stroke Relationship between Plaque Ulceration and Stroke Timing of Surgery CEA in Symptomatic Disease In trials, surgical stroke risk with CEA is ~6% in experienced hands Most data supports early revascularization (within 24 weeks of index event) owing to high risk of recurrent TIA/stroke with waiting, particularly in those with higher grade lesions Women (again) underrepresented but did have benefit, although not as great as men Elderly benefit Guidelines Clinical Question A 67 y.o. male presents with right eye amaurosis fugax lasting for 5 minutes three days ago. His symptoms resolved spontaneously and he underwent duplex scanning of the carotid arteries, revealing an 80% RICA stenosis with some “plaque ulceration.” He has known paroxsymal atrial fibrillation, hypertension, and lower extremity PAD. His medications include aspirin, lisinopril, atorvastatin, and coumadin. INR is 1.9. Best next therapy is: A. Add clopidogrel (Plavix) to medications and monitor B. Refer for immediate CEA C. Refer for immediate CAS D. TEE E. Double statin dose and repeat duplex in 3 months Part 3 STENTING (CAS) OR SURGERY (CEA)FOR CAROTID REVASCULARIZATION The Data: CAS and CEA CREST Trial Methods Randomized, controlled trial with blinded end- point 117 centers in US and Canada (108 US) Proceduralists in study were certified to enroll patients if: >12 procedures/year Rates of complications and death < 3% among asymptomatic pts and <6% among symptomatic pts. Methods - Patient Selection Symptomatic = TIA, amaurosis fugax, or minor disabling stroke involving study carotid w/in 180 days before randomization. Eligibility: 50%+ on angiography 70%+ on u/s, CTA, MRA In 2005, included asymptomatic pts with: 60+% on angiography 70+% on u/s 80+% on CTA or MRI if u/s showed 50-69%. Methods - Patient Selection Exclusion criteria: Previous CVA Atrial fibrillation w/in preceding 6 months MI within previous 30 days UA Anatomical reasons CAS & CEA CAS Involved RX Acculink stent, when feasible RX Accunet embolic protection device Pretreatment with ASA 325mg BID, Clopidogrel 75mg QD, at least 48 hrs prior to CAS If CAS scheduled within 48hrs of randomization, ASA 650mg and Clopidogrel 450mg given 4 or more hours before procedure Post-CAS: ASA 325mg or 650mg dail + Clopidogrel 75 or Ticlopidine 250mg BID x 4 weeks.+ CAS & CEA CEA 48+ hrs prior, ASA 325mg daily for 1 year or more (or ticlopidine 250mg BID or Clopidogrel 75mg daily, ASA 81mg daily, Dipyridamole BID) F/U Assessment of End-Points Neuro evaluation at baseline, 18-54 hrs post procedure, 1 month, q6 months thereafter. Cardiac biomarkers measured pre-procedure, 6-8 hrs after, 1 month. ECG before CAS/CEA, 6-48hrs after, 1 month after. Carotid u/s before CAS/CEA, 1, 6, and 12 months, and annually thereafter Phone f/u at 3 months and 6 months thereafter Endpoints Primary end-point: CVA, MI, or death during periprocedural period or ipsilateral CVA within 4 years after randomization. N=2502 Results - Primary End Point Results Stroke more common after CAS MI more common after CEA Overall composite endpoint showed no statistical difference Primary End Point (4yr) Primary End Point by Age Results Primary end point did NOT differ among symptomatic or asymptomatic pts. Peri-procedural cranial-nerve palsies less frequent among CAS patients. 4-yr CVA or death 6.4% (CAS) vs 4.7% in CEA (p=0.03). Symptomatic pts: 8% vs 6.4% (p=0.14) Asymptomatic pts: 4.5% vs 2.7% (p=0.07) Post-hoc Analyses Major/minor CVA found to have effect on physical health at 1 year; periprocedural MI less clear. Minor CVA had significant effect on mental health at 1 year Likelihood of primary end point not significantly affected by the specialty of the interventionist performing CAS (p=0.51). CREST 10 Year Data (published 2016) Brott et al. Long term results of stenting versus endarterectomy for carotid stenosis. NEJM, 374(11), 2016 . ACT 1 Limitations Overall, a very well conducted study! Highly trained proceduralists - may be more than the average in practice. One stent platform used. Medical Rx not specifically tested. Summary - CREST CAS and CEA associated with similar combined rates of periprocedural CVA, MI, or death and subsequent ipsilateral CVA (symptomatic and asymptomatic men and women). Incidence of periprocedural stroke lower in CEA cohort; incidence of MI lower in CAS cohort. Younger pts had slightly fewer events after CAS; older pts had fewer events after CEA. Medical therapy similar in both groups Overall Conclusions (TIME TO WAKE UP) Conclusions and Summary Asymptomatic carotid stenosis is common, and for many patients medical therapy is all that is needed Selected patients with good life expectancy and moderately high grade stenosis (in the hands of good surgeons) may be appropriate for CEA Controversy exists over how to select the best asymptomatic patients for carotid revascularization. Conclusions and Summary Symptomatic patients with high grade stenosis should be considered for CEA or CAS CAS and CEA should be considered as similar procedures, with the choice of procedure dependent on patient factors and local expertise Medical therapy is crucial in the management of any carotid stenosis, regardless of symptoms Unknown how modern medical therapy fares against revascularization for symptomatic patients- stayed tuned! Hopefully not too vague!! THANK YOU JAMES.DEVRIES@HITCHCOCK.ORG