Quality Report 2012 - 2013 Cambridgeshire and Peterborough NHS Foundation Trust
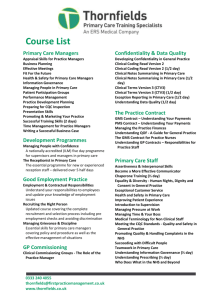
advertisement

Quality Report 2012 - 2013 Cambridgeshire and Peterborough NHS Foundation Trust CONTENTS INTRODUCTION TO THE QUALITY ACCOUNT All NHS Trusts are required to produce an annual Quality Report. The purpose of this report is to show how well we have performed in the past year and the areas where we feel we could make further improvements. We aim for transparency and openness to provide you with accurate, appropriate and sufficient information with which to assess our performance and the priorities we have set for the future. The key requirements of the Quality Report are set out in three sections below. PART 1: STATEMENT ON QUALITY FROM THE CHIEF EXECUTIVE This is a statement from our Chief Executive, Dr. Attila Vegh, on behalf of the Board of Directors setting out what quality means to us, what improvements we have made in the past year and where we need to make further improvements, and our vision for the future. Chief Executive’s Statement 3 PART 2: PRIORITIES FOR IMPROVEMENT AND STATEMENTS OF ASSURANCE We present our strategic objectives that we believe will help us achieve our goal of becoming a top 5 mental and community healthcare provider. We also review our progress on quality priorities in 2012/13 identified in our 2011/12 Quality Report and in previous years, and outline our quality improvement priorities for 2013/14. The Statement of Assurance is a mandatory requirement and we confirm that the Trust is able to meet all of the mandated requirements for the Trust. Priorities for Improvement 6 Statements of Assurance 20 Mandatory Core Set of Quality Indicators 33 PART 3: OTHER INFORMATION We report on performance against local quality performance indicators and key national priorities. Review of Performance Against Other CPFT Quality Indicators and Key National Priorities 41 ANNEX ANNEX 1 Our Quality Diamond Strategy 60 ANNEX 2 Definitions of Key National Quality Indicators 64 ANNEX 3 Statements from the Clinical Commissioning Board, the Local Healthwatch and the Overview and Scrutiny Committees 67 ANNEX 4 Statement of Directors' Responsibilities in Respect of the Quality Report 70 ANNEX 5 External Audit Report 72 Page 2 of 74 PART ONE: A STATEMENT ON QUALITY FROM THE CHIEF EXECUTIVE Introduction I am delighted to present our fourth Quality Report, and my second as Chief Executive of Cambridgeshire and Peterborough NHS Foundation Trust (CPFT). Over the past year, we have achieved many great things which I am very proud to present to you in this report. What do we mean by quality? Quality is at the core of everything we do, it is inherent within our values, our mission and our vision. We view quality from the perspective of the people who experience it - our patients, their families and carers, visitors to our premises and our staff – and this underpins our priorities for quality which are outlined below. Back in 2011 we developed a Quality Dashboard, mapped against the Care Quality Commission’s Essential Standards of Quality and Safety, which sets out the key areas that we felt we could reliably measure and that would tell us whether or not we are providing a good service. During the year, this was translated into Divisional quality dashboards and embedded into our reporting and governance framework. For 2013/14, we will focus on our vision to become a top 5 mental and community healthcare provider. To help us achieve this goal, we have developed four strategic objectives which are outlined in our Quality Diamond Strategy. They cover the areas of patient safety, patient experience, staff engagement and value for money. We have also reviewed our progress on quality priorities identified in previous years and developed new priorities which are set around the three domains of quality – patient experience, patient safety and clinical effectiveness. We believe these quality objectives and priorities will further improve the care and outcomes for the people who use our services, and also the experience and well being of our staff. Our staff have helped us to identify these priorities through a series of Town Hall events organised across the organisation to find out what their views were and what they thought was important. We have also worked with our commissioners, governors and other key partners; and also reviewed the range of data and other information that was available to us, including information from audits, incidents, comments and complaints about our services, and the results of service reviews to help us identify the areas that we need to focus on for improvement in 2013/14. What have we done well this year? Two years ago, CPFT was judged non-compliant in seven of the CQC standards of care and was considered one of the worst performing Trusts in the East of England. I took up my post as Chief Executive of the Trust in October 2011 and we began the difficult and challenging work of turning the Trust around. Coming into 2012/13, we were faced with many difficult challenges. We were still non-compliant in two of the CQC standards and had improvement actions required in two more. Following an inspection in June 2012, we were found to be non-compliant in one other standard around the management of medicines. As we approached the end of 2012/13, we were declared fully compliant across the organisation. This is a massive achievement and I believe the most important for CPFT to date and this is all down to the phenomenal hard work and dedication shown by our staff. Without them, this wouldn’t have been possible. We also reviewed our governance and operational structures to further strengthen our systems and processes and help us deliver on our objectives and priorities. In January 2013, we implemented our new governance framework. Our Clinical Divisions were reduced from five to three, and developed around diagnosis and needs as opposed to age groups. We believe that this will enable us to deliver better care and outcomes for the people who use our services. In terms of our Quality Accounts, we have met four out of nine quality priorities for 2012/13 and partially met one, and six out of eight CQUIN goals for the year. Page 3 of 74 But that is not all. Despite the areas of concern highlighted by the CQC, we have continued to excel in our practice and service delivery. Some of the many achievements CPFT have made over the past year are outlined below. In June 2012 the Cambridgeshire Child and Adolescent Substance Use Service (CASUS) won the Virgin Business Media and Guardian’s “innovation nation” award for collaboration. CASUS is part of the AMBIT collaboration - a group of teams who are all working with extremely vulnerable and high-risk youth who have multiple and complex problems. CPFT’s Youth Offending Service was rated in the top 5 in the UK CPFT’s Dementia Carers’ Support Service won a Cambridge News Community Award. The opening a new dementia research facility at the refurbished Windsor House in Fulbourn. The facility is the new home of the Dementia and Neurodegenerative Diseases Research Network East Anglia. The opening of Recovery College East, the first of its kind in the East of England. Courses will be held at venues throughout Cambridgeshire and Peterborough, and will include subjects such as helping people return to employment, staying well at work, getting the best from mental health services and physical health and recovery. CPFT was re-awarded the Ministry of Defence contract to provide local in-patient mental health care for serving military personnel in the eastern region at The Cavell Centre in Peterborough. What do we need to do better? We recognise that we have a lot do to rebuild staff morale in the coming year. Successfully implementing a major turnaround programme required a lot of hard work and changes to our ways of working and this has been reflected in our staff survey scores in 2012, both from the national survey and our internal Pulse Surveys. Our commitment to our staff is embedded in our Quality Diamond Strategy through the initiatives to become a top 5 community and mental health organisation for staff engagement. Over the coming months, we will introduce a range of initiatives to improve the experience of our staff. We also need to focus on the areas in our quality priorities where we have not met the targets set in 2011/12. This includes better compliance with our mandatory training programme and improving staff satisfaction with the response times to IT requests. We have developed a range of actions to help us do this, which is outlined in Part 2 of this report. In addition, we have identified other areas where we need to do better particularly around provision of psychological therapies and physical health outcomes for our patients. These are included in our priorities for 2013/14. A huge thanks to our staff All of the achievements we have made in the past year would not have been possible without the hard work, dedication and commitment of our staff so I would like to take this opportunity to formally thank them for everything that they have done which has brought us to where we are today. I am very proud of every member of our staff and I know that together, we have the capability and energy to continue to achieve many more great things in the years to come. Some of the many initiatives we have started during the year to show our appreciation to our staff include giving out the Quality Heroes and the Quality Champion awards. We also celebrated our very first ever Staff Awards ceremony in February 2013, to recognise the achievements of individuals in categories of patient experience, patient safety, staff engagement, productivity, good governance and research innovation and education, among others. Over the coming months, we will continue to think of ways to thank our staff and recognise their achievements. What others think of us? We welcome opportunities for external bodies to review our services to see how well we are meeting the standards of quality and safety. During the year, the CQC assessed our services against these standards on two occasions and they have judged us fully compliant against the standards they examined. They also conducted specific visits to review our compliance with the Page 4 of 74 Mental Health Act. I am proud to say that the feedback we have received has been extremely positive. We took part in a number of accreditation schemes during the year. For example, The Croft Child and Family Centre was accredited by QNIC (Quality Network for Inpatient CAMHS) in October 2012, and our Adults and Learning Disability inpatient units are accredited under AIMS (Accreditation for Inpatient Mental Health Services). We also value the comments and learning that we get from PALS (Patient Advice and Liaison Service) and Complaints and also from the results of our internal patient and staff survey as these give us a very useful insight into the areas that we can and need to improve. Statement of accuracy I confirm that to the best of my knowledge the information in this document is accurate. DR ATILLA VEGH CHIEF EXECUTIVE 24 MAY 2013 Page 5 of 74 PART TWO: PRIORITIES FOR IMPROVEMENT AND STATEMENTS OF ASSURANCE FROM THE BOARD 1.0 PRIORITIES FOR IMPROVEMENT In this section we introduce our overarching strategy for quality which is embedded in our Quality Diamond Strategy below. We also report on our performance in 2012/13 against the quality priorities set in 2011/12. It is important to show continuity when reviewing quality priorities between accounts especially where priorities have changed over time. We therefore look back at our priorities from previous years and provide an update on progress we have made during 2012/13 and state how we will continue to measure, maintain and develop these priority areas. Finally, we present our quality priorities for 2013/14. 1.1 QUALITY DIAMOND STRATEGY 2011/12 was a difficult and challenging year for the Trust due to the demands placed on the organisation to consistently achieve all of the CQC essential standards of quality and safety. During 2012/13 we also developed our ambition to become a top 5 mental and community healthcare provider which we have outlined over the following pages. At the beginning of 2012/13, we started work to build on our successes and look forward to 2013/14. The second phase of the staff Town Hall events was held in June 2012 to identify the key areas that everyone within the organisation wanted to prioritise in order to improve the quality and experience of our services. Over 2,000 of our staff attended the events and their ideas have helped us to formulate our strategic objectives for 2013/14. These strategic objectives are outlined within the Quality Diamond which we published in December 2012, and are shown in the diagram on this page. The four strategic objectives are: To become top 5 nationally for patient safety To become top 5 nationally for patient experience To become top 5 nationally for engaged staff To become top 5 nationally for value for money We have set out further details in Annex 1. Our Quality Diamond Strategy underlines our quality priorities and quality dashboard for 2013/14. We have already started implementing a number of these initiatives, and over the coming months we will continue to roll out a series of actions and initiatives to support the achievement of these objectives. We will publish regular reports on our progress against the Quality Diamond priorities on our public website. Page 6 of 74 A Review of Our Quality Priorities for Improvement Patient Experience 2010/11 Priority 1 Improvement in annual Patient Survey responses for overall satisfaction rating Priority 2 Ensure 95% of patients have a care plan Patient Safety Priority 3 Reduce all suicides by patients in contact with secondary mental health services by 20% by 2013 Priority 4 Reduce the number of physical assaults within Trust services by 20% by 2013 Priority 1 To develop routine patient feedback mechanisms across all care pathways Priority 2 To develop and implement a Carer Strategy Priority 3 To establish with primary care a Suicide Prevention Strategy Priority 4 Reduce the risk of absconsion through a review of clinical risk assessment observations, access and therapeutic programmes Priority 5 Significantly strengthening patient safety training in adult safeguarding, clinical risk assessment and physical interventions Priority 5 Compliance with 18 week referral to treatment waiting time target Clinical Effectiveness 2011/12 Priority 6 Ensure that 95% of CPA patients have a HoNOS outcome assessment in a 12 month period Priority 6 To develop and implement a consistent recovery outcome measure which involves service users directly in planning their care 2012/13 2013/14 Priority 1 To provide safe and effective care which provide excellent customer services 1. Full compliance with CQC standards 2. 95% of care plans across the Trust will sustainably achieve 7Cs standards 3. 80% inpatients and 74% community patients will recommend CPFT to family & friends Priority 1 To improve the experience of our patients and our staff 1. 65% of our patients will be satisfied with the quality of our services and recommend our services to their family and friends 2. 60 % of our staff will recommend CPFT to care for their friends and family 3. 60% of our staff will recommend CPFT to friends and family as a good place to work Priority 2 To provide an estate and IT infrastructure that is safe, moderns and fit for purpose. 1. All premises will achieve at least 4 stars against our environmental standards 2. 85% of our people will describe IT response times as good or very good Priority 2 To strengthen the culture of safety in CPFT. 4. Our teams will achieve a Trust wide average InCA score of 95% by Qtr4 of 2013/14 5. 95% of our people will complete safeguarding adults and safeguarding children training 6. 65% of our people will describe IT response times as good or very good Priority 3 To provide services through empowered staff with the right skills, attitudes and behaviour 1. 85% of our people will state they are able to make changes they feel necessary for excellent patient care 2. We will achieve national upper 20% in the number of our people who state that they will recommend CPFT to their family and friends as a place to work 3. 95% of our people will have completed all their mandatory training 4. No more than 5% of our inpatient shifts will have temporary staff greater than 20% of all staff at work Priority 3 To improve outcomes of care for our patients 1. 98% of relevant admissions to our acute wards gatekept by Crisis Resolution Home Treatment Team 2. Achieve the 60% national target in the proportion of people referred for psychological therapy who receive psychological therapy 3. Improve physical health outcomes for our patients Page 7 of 74 1.2 REVIEW OF QUALITY PRIORITIES 2012/13 We have reviewed our performance against the nine indicators within our quality priorities for 2012/13. We have fully met four indicators, partially met one and not met four. This is described below. 1.2.1 PRIORITY 1: PATIENT EXPERIENCE 2012/13 Priority To provide safe and effective care which provide excellent customer experience. Trust indicators 1. Full compliance with the Care Quality Commission (CQC) Essential Standards for Quality & Safety in any Trust registered location 2. 95% of care plans across the Trust will sustainably achieve the 7Cs standards. 3. 80% of inpatients and 74% of community service users will recommend CPFT to their family and friends Performance 1. Full compliance with the Care Quality Commission (CQC) Essential Standards for Quality & Safety in any Trust registered location As of March 2013, the current registration status of CPFT with the CQC is ‘Registered Without Conditions’. Please refer to section 2.6 for further details on our achievements in this area. 2. 95% of care plans across the Trust will sustainably achieve the 7Cs standards. The 7Cs standards were developed to help us drive up the quality of our assessments and care planning processes and documentation. The 7Cs assessment process was later incorporated into the InCA (Integrated Compliance Assessment) process. 7Cs scores are reported through our quality dashboards. Thresholds were set on an incremental basis from 75% to 95%. The overall combined Trust average score for Quarter 4 is 94% across all participating teams. It is worth noting that the results of our National Community Patient Survey 2012 show improvements in our scores overall, with the biggest improvements in the questions around care planning. Refer to section 3.1.3 for details. Quality improvements Care Planning Guidelines booklet developed to support the 7Cs standards and to articulate the standards around involvement of patients and carers in the assessment & care planning process Care Planning Policy was reviewed and updated to clarify required standards of practice and incorporate the 7Cs standards. InCA was developed as an Excel-based tool and later converted into an iPad application in September 2012. This is used to assess and provide assurance of compliance with all 16 CQC Outcomes on a monthly basis and incorporates our 7Cs care planning and 5 star environmental standards. Teams undertake self assessments with quarterly peer reviews. Page 8 of 74 3. 80% of inpatients and 74% of community service users will recommend CPFT to their friends and family This target was originally set based on the results of the national patient surveys for both inpatients and community services. During 2012/13, however, CPFT along with many others in the East of England (EoE), decided, at the instigation of the EoE Strategic Health Authority, to change the way that this indicator was calculated to one based on the net promoter score (NPS) methodology. This resulted in the revisions to the targets that are set out below. The average score for the Trust and its constituent Divisions as at year end March 2013 are shown in Table 1 below. Table 1: Friends & family test Revised Target Division 12/13 Acute Care Service Community Service Specialist Service 30% 30% 30% Performance as of March 2013 Total Trust average score March 2013 26% 62% 34% 40.7% Scores are collected from our internal patient surveys and are reported through our quality dashboards (see sections 3.1.4 and 3.1.5). Overall, the Trust has exceeded the targets for this indicator although recognising that patient experience is variable across our different Divisions. In 2013/14 we have agreed differential targets for patient experience to reflect the nature of the services we provide. This has been carried forward as our quality priority for 2013/14 with an ambition to see substantial improvements across all three Divisions. Page 9 of 74 1.2.2 PRIORITY 2: PATIENT SAFETY 2012/13 Priority To provide an estate and IT infrastructure that is safe, modern and fit for purpose. Trust Indicators 1. All premises will achieve at least 4 stars against our 5 star environmental standards. 2. 85% of our people will describe IT response times as good or very good Performance 1. All premises will achieve at least 4 stars against our 5 star environmental standards The 5 star standards were developed to assess the safety and suitability of our environment and equipment. The 5 star standards incorporated requirements around infection control, cleanliness, privacy and dignity. Wards have to score 100% to be awarded a ‘star’ against each of the five domains. This was introduced in our wards in January 2012 with varying results in the first three months of roll out. The 5 star standards were later incorporated into the InCA assessment process (see notes in Priority 1.2.1). Scores throughout the year, reported as part of our quality dashboard, show that all of our 21 wards have achieved at least 4 stars during the period. We continue to monitor our performance on this indicator regularly through our quality dashboards to ensure that issues are identified and acted upon in a timely manner. This shows our commitment to maintaining the quality of our environment and equipment to protect the safety of our patients, visitors and staff. Quality improvement Environmental work was undertaken in all of our inpatient units throughout the year particularly focusing on the removal of ligature points, reinforcing our doors and windows, making our wards compliant with Same Sex Accommodation standards and overall redecoration and refurbishment. Outside, entrances to the wards were improved, fences were raised and benches secured, among others. Environmental work has now been rolled out to our community premises. 2. 85% of our people will describe IT response times as good or very good This was a new indicator for the Trust and data was collected during the year through our staff Pulse Surveys which appears on the computer screens when staff log on. As of March 2013, the total average scores across the three Divisions show that only 43% of staff rate IT response times as ‘good’ or ‘very good’. Actions taken Further work will be undertaken to determine the specific areas of performance that staff are not happy about. Discussions are being held with SERCO, our IT service provider, in order to address these areas and ensure improvement of staff satisfaction scores around IT response time. This has been carried forward as our quality priority for 2013/14. Page 10 of 74 1.2.3 PRIORITY 3: CLINICAL EFFECTIVENESS 2012/13 Priority To provide services through empowered staff with the right skills, attitudes and behaviours. Trust Indicators 1. 85% of our people will state that they are able to make the changes that they feel necessary for excellent patient care. 2. We will achieve the national upper 20% in the number of our people who state that they will recommend CPFT to family and friends as a place of work. 3. 95% of our people will have completed all their mandatory training. 4. No more than 5% of inpatient shifts will have temporary staff greater than 20% of all staff on that shift. Performance 1. 85% of our people will state that they are able to make the changes that they feel necessary for excellent patient care. This was a new indicator for the Trust. Data is collected through our staff Pulse Surveys and scores are reported through our quality dashboards. Trust scores for 2012/13 show that, on average, only 46% of staff stated that they are able to make changes necessary for excellent patient care. We are introducing a range of quality improvement initiatives to promote and support staff engagement and involvement in matters that are important to patient care as part of our ‘Big Conversation’ programme. These are outlined section 5 of this report (Workforce Factors). Actions for this indicator are linked to the Trust National Staff Survey action plan which includes developing a Workforce Strategy in consultation with staff (see section 5). 2. We will achieve the national upper 20% in the number of our people who state that they will recommend CPFT to family and friends as a place of work. The 2012 National NHS Staff Survey results show that CPFT is in the bottom quartile when compared to similar Trusts for the percentage of our staff who would recommend CPFT to family and friends as a place of work, scoring 33% (against the national average of 53%) compared to 48% in 2011. Data from our own internal Pulse Surveys is currently showing a much higher score of 48% as of March 2013. We recognise that this is largely due to the challenges faced by our staff in the past year as part of the quality turnaround programme. We are introducing a range of improvement initiatives to improve the experience of our staff through our ‘Big Conversation’ programme which is outlined in section 5 (Workforce Factors). However, we acknowledge that we have a lot to do improve the way our staff feel about their work and CPFT. Actions for this indicator are linked to the Trust National Staff Survey action plan (see section 5) Our commitment to our staff is reflected in our Quality Diamond Strategy (Objective 2) and this measure has been carried forward as our quality priority for 2013/14. Page 11 of 74 3. 95% of our people will have completed all their mandatory training. As of March 2013, overall mandatory training stands at 85%, as follows: 94% for mandatory gateway E-learning 82% for mandatory physical skills modules 80% for mandatory clinical skills modules Performance against this indicator is reported through our quality dashboards. Although falling short of the 95% target that we have set ourselves, this represents a significant improvement over 68% in 2011/12. Classroom-based training data is collected from ESR (Electronic Staff Records) while e-learning data is collected from LMS (Learning Management Systems). A Project Group was formed during the year to drive achievement of this target. This has been continued in 2013/14 to ensure continued improvements. 4. No more than 5% of inpatient shifts will have temporary staff greater than 20% of all staff on that shift. Ensuring that our wards have the right staffing levels with the right skills is a priority of the Trust, and our commitment to achieving this is embedded in Objective 2 of our Quality Diamond Strategy. This was a new indicator for the Trust. Data is collected from our electronic rostering system (MAPS) and reported through our quality dashboard. During the year this indicator was reviewed and revised and is now reported in our quality dashboard as the percentage of bank and agency shifts used as a proportion of total shifts on the ward. As of March 2013, this came to 24.70% which is significantly over our target of 5% This remains a priority of the Trust and is monitored through our quality dashboards. We have undertaken a major review of inpatient and community establishments during 2012 including the use of temporary staff through the PET Project (see below). The implementation of the findings of this review will ensure that the use of temporary staff will reduce to 5% by mid 2013/14 PET (Productivity, Establishment & Temporary Staff) Project The PET project was established in January 2013 following a detailed review of ward establishments and use of temporary staff in late 2012. There are three key work streams in Phase 1 which is due to be completed in September 2013: Work stream 1: Delivering the new 333 staffing establishment model. This is currently being rolled out in selected inpatient units in the Cambridge area. Work stream 2: Making operational changes. This includes looking at shift pattern changes, eradicating restrictive shift patterns, absence management and looking at areas where productivity can be improved (e.g. administrative support and introduction of the RiO electronic patients records system). Work stream 3: This looks at the performance and effective sourcing of bank staff and effective utilisation of MAPS, our electronic rostering system. Phase 2 focuses on productivity and new ways of working and is planned to be completed by March 2014 Page 12 of 74 REVIEW OF QUALITY PRIORITIES SET IN PREVIOUS YEARS In this section, we look back at the priorities we set in 2010/11 and 2011/12 and provide an update on progress made to March 2013. This allows us to show how we continue to measure, maintain and develop these areas even when new priorities become the focus of improvement. Patient Safety Patient Experience 2010/11 As of March 2013, we have met three out of six of our quality priorities and partially met three from 2010/11, and we have met five out of six quality priorities and partially met one from 2011/12. These are outlined below. Clinical Effectiveness 1.3 Quality Priority Priority 1 Improvement in annual Patient Survey responses for overall satisfaction rating Priority 2 Ensure 95% of patients have a care plan Priority 3 Reduce all suicide by patients in contact with secondary mental health services by 20% by 2013 Priority 4 Reduce the number of physical assaults within secondary mental health services by 20% by 2013 Priority 5 Compliance with 18 week referral to treatment waiting time target Priority 6 Ensure that 95% of CPA patients have a HoNOS outcome assessment in a 12 month period Update on Progress as of March 2012/13 Results of our annual National Community Patient Survey show an overall improvement in our scores for 2012 and an improving trend over time (see section 4.1.2 for further details). This remains a Trust priority and is reported in Part 3 of this Quality Report. We have consistently achieved this target over the last three years. In 2012/13, we changed the focus to improving the quality of our care plans which we have also achieved (see sections 1.2.1 and 4.3.1 for further details). This remains a Trust priority and is reported in Part 3 of this Quality Report and monitored throughout the year through our quality dashboard. Data available as of March 2013 shows an 11% reduction between 2010/11 and 2012/13 in the total number of deaths with a verdict of suicide and probable suicides, where the verdict was misadventure, accidental death, cause unknown/unexpected, or cases where we have not yet received a verdict from the coroner. This remains a Trust priority, and we have commissioned an independent review of inpatient Serious Incidents (SIs) by Professor Louis Appleby from Manchester University to help us identify the areas where we can make further improvements. As of March 2013 there was an 11% reduction between 2010/11 and 2012/13 in the total number of physical assaults reported. This remains a Trust priority and we have improved our training on the assessment and management of violence and aggression. We will continue to monitor this through our quality dashboard. Although our children’s community services had breaches in two of their services, the Trust’s overall average referral to treatment time was 1.97 weeks as of March 2013 compared to 4.08 weeks in 2011/12. This remains a Trust priority and is reported through our quality dashboard. As of March 2013, 85% of CPA patients had a HoNOS assessment. This remains a Trust priority and we are addressing the issues around the electronic Mental Health Clustering Tool (MHCT) and our electronic Clinical Documents Library (CDL) system. This is reported through our quality dashboards. Page 13 of 74 2011/12 Patient Experience Quality Priority Priority 1 To develop routine patient feedback mechanisms across all care pathways Update on Progress as of March 2012/13 Meridian, the IT solution to collect patient experience information, was rolled out to inpatient teams in January 2012 and community teams in April 2012. Routine patient feedback is collected using an iPad every month and results are reported as part of the quality dashboards. This remains a Trust priority and is reported in Part 3 of our Quality Report (see sections 4.1.3 & 4.1.4). Priority 2 To develop and implement a Carer Strategy The Partnerships Strategy 2013-2016 was developed during the year and is due to be approved in May 2013. This will drive forward our approach to develop and improve the way we inform, consult, listen, involve and empower people involved in our services. This remains a Trust priority moving forward. Patent Safety Priority 3 To establish with primary care a Suicide Prevention Strategy Priority 4 Reduce the risk of absconsion through a review of clinical risk assessment, observations, access and therapeutic programmes Within the region, Public Health England is leading on the suicide prevention agenda and is in the process of developing a regional Suicide Prevention Strategy. The Trust is a member of the Joint Countywide Suicide Prevention Group. CPFT is currently developing its own Suicide Prevention Strategy, ensuring that this links with the Public Health agenda and reflects the national strategy. This is due to be ratified in May 2013. This remains a Trust priority and will be reported in Part 3 of the Patient Safety section of future Quality Reports. We have put measures in place such as improving our clinical risk assessment training, developing a policy and improving arrangements around access to our wards, carrying out environmental work, which includes reinforcing doors and windows, raising the height of garden walls and moving garden benches away from the garden walls, among others. These measures have resulted in a 10% reduction in the number of absconsions between 2011/12 and 2012/13. This remains a Trust priority and is reported through our quality dashboard. Clinical Effectiveness Priority 5 Significantly strengthening patient safety training in adult safeguarding, clinical risk assessments and physical interventions Priority 6 To develop and implement a consistent recovery outcome measure which involves service users directly in planning their care Although we have just missed the target of 95% as of March 2013, compliance rates in mandatory training is much improved and we are only slightly below our agreed target. This remains a Trust priority and is reported through our quality dashboard. We have introduced measures to support this objective, such as the introduction of the HoNOS outcome scales, strengthening collaborative care planning and the involvement of patients and carers in planning their care through the development of 7Cs standards. We are now working with Clinical Divisions to help them identify Patients Reported Outcome Measures (PROMs) that are specific to their services and the needs of their patient group. These will be incorporated into their Divisional quality dashboards. Page 14 of 74 1.4 QUALITY PRIORITIES FOR 2013/14 The priorities for quality improvement for 2013/14, outlined below, have been developed as a result of the following: We have listened to feedback from our patients and their families, our staff, our commissioners, governors, regulators and other stakeholders. We have reviewed information from various sources such as PALS and Complaints, patient and staff surveys, serious incidents, incidents and near misses, clinical audits, research, service development projects and external service reviews. We commissioned external auditors to review our systems to support effective quality governance within the Trust. Please refer to the summary of our Quality Diamond Strategy in Annex 1 for additional details on the improvement initiatives. 1.4.1 PATIENT EXPERIENCE Priority 1: To improve the experience of our patients and our staff. 1 65% of our patients will be satisfied with the quality of our services and recommend our services to their family and friends 2 60% of our staff will recommend CPFT to care for their friends and family 3 60% of our staff will recommend CPFT to friends and family as a good place to work Rationale for Inclusion We believe that a basic indicator of quality is when people state they are satisfied with the quality of the services that we offer and are happy to recommend CPFT to their family and friends. We also believe that there is a strong correlation between staff satisfaction and patient satisfaction. If our staff believe that they are respected, valued and supported, this will have a direct impact on the quality of their interaction with our patients and the care that they provide. We have chosen these indicators as our Net Promoter Scores (NPS), in conjunction with the Department of Health (DH) guidance. Measurement Data for these indicators will be taken from our internal monthly patient satisfaction survey and staff Pulse Survey. Improvement initiatives We are working with our commissioners to refine the questions around the quality of our services in our patient and staff Pulse surveys. Patient experience Develop Care Pathway services Implement year 1 action plan from Engagement Strategy Continue to roll out our Recovery College East Develop a new Social Care Strategy Implement Big Conversation initiatives Staff experience Continue to roll out the CPFT Academy To continue with the ‘Quality Heroes’ and ‘Team Champions’ initiative Continue to strengthen staff communication (e.g., Webex sessions, Town Hall events& Diamond Talkback) Implement Big Conversation initiatives Monitoring and Reporting Monthly quality dashboard reporting, Divisional Performance Review meetings and regular reporting to Quality & Performance Committee and the Trust Board. Page 15 of 74 1.4.2 PATIENT SAFETY PRIORITY 2: To strengthen the culture of safety in CPFT 1 2 3 Our teams will achieve a Trust wide average InCA score of 95% by Qtr4 of 2013/14 95% of our people will complete safeguarding adults and safeguarding children training 65% of our people will describe IT response times as good or very good Rationale for Inclusion The quality of assessments, risk assessments and care planning have a direct impact on the provision of safe and effective care. The standards around these are embedded in InCA which is used to assess the performance of our clinical teams. InCA also covers all 16 CQC outcomes which include standards around premises and equipment, safeguarding and safety, cleanliness and infection control, among others. Compliance with these standards will help us ensure the safety and wellbeing of our patients, visitors and staff. Providing quality service is dependent upon having staff with the right skills, knowledge and experience, and providing them with appropriate systems and processes. Safeguarding training is mandatory and as of March 2013, our compliance rates are 94% for safeguarding adults and 88% for safeguarding children. We need to improve on these compliance rates to ensure that our staff know how to recognise and act appropriately when they observe safeguarding incidents. Finally, we need to ensure that our staff have the information that they need in a timely manner to provide safe and effective care. This is dependent upon having IT systems that are appropriate, responsive and fit for purpose. Measurement Data for these indicators will be taken from monthly InCA assessments, quality dashboards, incident reporting and staff Pulse Surveys. Improvement initiatives Regular review of the InCA assessment tool and process, development of servicespecific standards and roll out to the rest of our community-based services. Pilot the ‘No Force First’ initiative in selected inpatient services Roll out of RiO, our electronic clinical records system, to the rest of the Trust. Monitoring and Reporting Monthly quality dashboard reporting, Modern Matrons meetings, Divisional Performance Review meetings and regular reporting to the Clinical Executive, Quality & Performance Committee and the Trust Board. Page 16 of 74 1.4.3 CLINICAL EFFECTIVENESS PRIORITY 3: To improve outcomes of care for our patients 1 2 3 98% of relevant admissions to our acute wards are gatekept by Crisis Resolution Home Treatment Teams (CRHTT) Achieve the 60% national target across all three IAPT services for the proportion of people referred for psychological therapy who receive psychological therapy. Improve the physical health outcomes for our patients Rationale for Inclusion Assessment by the CRHTT prior to admission into acute inpatient units ensures that only patients who need inpatient care are admitted into our wards and that the patient has the most appropriate plan of care agreed by all relevant parties, including the patient. As of March 2013, our internal reports show that 95% of patients admitted to CPFT inpatient units were assessed by CRHTT. Data reported by the Health and Social Care Information Centre (HSCIC) as of December 2012 shows the national average at 98% with 29% (n=18) of mental health Trusts achieving 100% compliance. We need to improve on this performance. NICE guidance and quality standards recommend the use of psychological therapies for the treatment of psychological disorders either on its own or alongside traditional medication. The Department of Health has promoted the use of psychological therapies through the establishment of IAPT (Improving Access to Psychological Therapies) services. As of March 2013, not all of our IAPT services met the national 60% target for the proportion of our patients referred for psychological therapy who receive psychological therapy. We need to achieve this target across the Trust. A high level scoping of physical health monitoring in CPFT shows that we need to improve our arrangements in this area. This is supported by findings from national and local audits. This is also a CQUIN target for 2013/14 covering inpatient services. . Measurement For priorities 1 and 2, data will be taken from the quality dashboards and contractual performance reports. In regards to the physical health priority, we will review the existing policies on physical health (inpatient and community) and develop an inclusive Physical Health Policy. develop a Physical Health dashboard. This will provide us with baseline information from which we can set improvement targets for 2014/15. Improvement Initiatives Review and update the Psychological Therapies Strategy Review the referral process and pathway into care across all three IAPT services to streamline the process and achieve consistency across the Trust. Trust wide review of Physical Health monitoring arrangements (new project) to identify gaps and develop appropriate actions. Develop Physical Health Policy, Physical Health dashboard and improve training around physical health for frontline staff Monitoring and Reporting Monthly quality dashboard reporting, Divisional Performance Review meetings and regular reporting to the Clinical Executive, Quality & Performance Committee and the Trust Board. Page 17 of 74 1.5 HOW WE WILL MONITOR THESE PRIORITIES We reviewed our governance structure based on recommendations from PwC to strengthen the quality governance arrangements in the Trust. The new governance framework, which will provide assurance that the Trust is meeting our strategic objectives and priorities, was approved by our Board of Directors in February 2012. 1.5.1 ASSURANCE AT TRUST LEVEL The governance committee structure responsible for monitoring our Trust’s objectives and priorities is outlined below. Board of Directors Audit & Assurance Committee Patient Safety, Risk & Experience Group Quality & Performance Committee Executive Management Group Performance & Risk Executive Clinical Effectiveness Group Finance Executive Research & Development Group Mental Health Legislation Group Clinical Executive Workforce Executive Professional Development & Education Group The Audit & Assurance Committee and the Quality and Performance Committee have the primary responsibility for obtaining assurance, on behalf of the Trust Board, that the Trust is discharging its duties properly and that it is meeting its strategic objectives. The Executive Management Group is chaired by the Chief Executive and has an operational management responsibility for the Executive committees, which are responsible for reviewing and making recommendations on the strategic direction of the Trust. The Quality & Performance Committee is the main Board subcommittee responsible for monitoring our compliance against the quality improvement priorities throughout the year through position summaries on a regular basis. It will also inform the Board of our delivery against these priorities alongside the regular reports on the Divisional quality dashboards to provide assurance of continued improvements in the delivery of care across the Trust. 1.5.2 ASSURANCE AT OPERATIONAL LEVEL Clinical and integrated governance has its foundations on having effective processes at team level. We believe that patient and staff relationship lies at the heart of improving quality. We therefore see governance as a pyramid based on the quality of interaction between our staff and our patients. This is supported by robust governance processes and a dynamic performance management framework at Divisional level. Page 18 of 74 Within this governance framework, we have introduced a set of standards for team governance which is known as ‘how are we doing?’ meetings. The standards are outlined below. Team Governance Framework 1 The purpose of team governance is to ensure and improve the quality of patient and carer experience, patient safety and to identify, mitigate or escalate the risks to the delivery of this. 2 Team governance will follow the five steps of governance process, from patient experience through to monitoring progress. 3 Team governance should take place in a spirit of openness, constructive challenge and willingness to reflect and learn. They shouldn’t be afraid to raise risks and issues if they don’t believe they can manage this. 4 Teams must produce a governance report once a year. 5 Team governance meetings will take place at least monthly and can either be stand alone meetings or form part of multi-disciplinary team meetings with protected time for governance. 6 Team governance processes will be multi-disciplinary and include representatives of all staff groups, this includes administrative and housekeepers as well as health and social care professionals. 7 Teams will discuss and agree how patients and carers are involved in their governance processes. We will provide teams with the necessary training, support and practical tools to help them undertake these meetings effectively. This will include: provision of relevant and timely information to help them make decisions and develop appropriate actions self-assessment and peer review tools such as the InCA which provides teams with the basis from which they can evaluate their compliance with the CQC essential standards establishing a new process and system of risk management which will form the backbone of governance within the organisation, through the development and maintenance of team risk registers that will feed into the Divisional and Board Assurance Framework (BAF). Divisional Governance Framework We have introduced ‘Divisional Accountability Governance Agreements’ (DAGA) which are designed to clearly set out the expectations of the Board of Directors in regard to both quality, safety and risk management arrangements as well as financial performance. This will encompass the following processes: Each Division will have monthly reviews through the Performance and Risk Executive which considers all aspects of performance, risk management and service planning. Divisions will be required to hold internal governance meetings to look at team governance and specific safety, quality and effectiveness issues. This will include reports about their compliance with the CQC essential standards through the InCA process, risks identified at team level, incident reports and complaints. Both team and Divisional governance frameworks will feed into and provide assurance to the Trust Board that we are meeting our objectives and quality priorities. Page 19 of 74 2.0 STATEMENTS OF ASSURANCE We have reviewed the data available to us during the year covering the three dimensions of quality – patient safety, clinical effectiveness and patient experience. There have not been any significant concerns with the data that have impeded us in the preparation of this Quality Report. 2.1 REVIEW OF SERVICES Cambridgeshire and Peterborough NHS Foundation Trust (CPFT) is a partnership organisation providing mental health and specialist learning disability services across Cambridgeshire and Peterborough, and also children's community services in Peterborough. We are a teaching Trust and work with the Department of Psychiatry at the University of Cambridge. CPFT is also a member of Cambridge University Health Partners (CUHP), one of only five Academic Health Science Centres in England. The Trust provides the following: Children’s mental health and community services; Adult mental health services; Older people’s mental health services; Primary care therapy and liaison psychiatry services; Forensic and specialist mental health services; Substance misuse services; and Specialist learning disability services. We also provide some specialist services on a regional and national basis. Full details of our services are available on the Trust Website. www.cpft.nhs.uk. Community learning disability services are provided by the Cambridgeshire Learning Disability Partnership and the Peterborough Learning Disability Partnership. Inpatient intensive assessment and support services are provided by the Trust in collaboration with the Learning Disability Partnerships. Around 2,000 staff working across over 75 sites in Cambridge, Huntingdon, Peterborough, Fenland, Mid Essex and Norfolk. Three Clinical Divisions o Acute Care Services o Community Services o Specialist Services Our partners include: o Cambridgeshire County Council o Peterborough City Council o NHS Cambridgeshire o NHS Peterborough Note: The new CCGs (Clinical Commissioning Groups) replaced NHS Cambridgeshire and NHS Peterborough in April 2013. During 2012/13 CPFT provided and/or sub-contracted NHS services in seven relevant health services (outlined above): The Trust has reviewed all the data available to us on the quality of care in all seven of these relevant health services. The income generated by the relevant health services reviewed in 2012/13 represents 100% of the total income generated from the provision of NHS services by CPFT for 2012/13. 2.2 PARTICIPATION IN CLINICAL AUDITS During 2012/13, two national clinical audits and one national confidential enquiry covered relevant health services that CPFT provides. During 2012/13 CPFT participated in 100% national clinical audits and 100% national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. Page 20 of 74 The national clinical audits and national confidential enquiries that CPFT was eligible to participate in during 2012/13 are as follows: Prescribing Observatory for Mental Health (POMH) National Confidential Inquiry (NCI) into Suicide and Homicide by People with Mental illness (NCI/NCISH) National Audit of Psychological Therapies (NAPT) The national clinical audits and national confidential inquiries that CPFT participated in, and for which data collection was completed during 2012/13, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or inquiry. Table 2: National audits that CPFT participated in during 2012/13 Audit % Cases submitted University of Manchester 20 questionnaires sent by NCISH between April 2012 and March 2013, 20 completed and submitted by National Confidential Inquiry into Suicide CPFT (100%) and Homicide by People with Mental Illness (NCISH) 3 homicide questionnaires sent (2 in March 2013 so not yet due at time of report) and 1 completed and submitted by CPFT (100%) National Programme of Prescribing Observatory for Mental Health (POMH) POMH-UK 1f & 3f Prescribing high-dose and combination antipsychotics: 7 participating teams acute/PICU, rehabilitation/complex needs, 79 questionnaires submitted and forensic psychiatric services. POMH-UK 2f: Screening for metabolic 7 participating teams side effects of antipsychotic drugs 105 questionnaires submitted POMH-UK 11b: Prescribing antipsychotic 11 participating teams medication for people with dementia 169 questionnaires submitted POMH-UK 12a: Prescribing for people 13 participating teams with personality disorder 77 questionnaires Royal College of Physicians 74 Service user questionnaires returned, 82 case National Audit of Psychological Therapies note audit cases submitted and 28 therapist questionnaires returned. The reports of six national clinical audits were reviewed by the provider in 2012/13. These are: a) Prescribing Observatory for Mental Health (POMH) audits POMH-UK 1f: Prescribing high dose & combined antipsychotics in Adult in acute adult inpatient or psychiatric intensive care wards POMH-UK 2f: Screening for metabolic side effects of antipsychotic drugs POMH-UK 3f: Prescribing high dose and combined antipsychotics in Forensic wards POMH-UK 11b: Prescribing antipsychotic medication for people with dementia POMH-UK 12a: Prescribing for people with personality disorder b) National Audit of Schizophrenia and CPFT intends to take the following actions to improve the quality of healthcare provided. Page 21 of 74 Develop a Medication & Physical Health Dashboard to drive up standards in prescribing and physical health monitoring Review existing guidelines and procedures for poly pharmacy and prescribing over BNF limits to ensure clarity of procedures and requirements. Develop a Trust wide tool to record the history of prescribed interventions (medication, psychological therapies and other interventions) , to include documentation of side-effects and benefits Add a standard line in the standard letter to the GP which is sent prior to a care review requesting information about physical health investigations and most recent list of prescribed medication. Review the protocol about whether psychological treatments should be prioritised for patients with treatment resistant schizophrenia as opposed to first episode or both. Develop a register to record all deaths in any age (to include age at death, ICD10 diagnoses, MH cluster. and causes of death) to create a data set that will inform future service developments. Disseminate results of the Shimme Project (Shared decision making in medicines management) when completed and ensure that learning around shared decisionmaking in medicines management is shared and implemented in practice. An identified Trust staff will link with Cambridge University Department of Public Health to promote research on diabetes in people with mental disorder The reports of 24 local clinical audits were reviewed by the provider in 2012/13 and CPFT has taken/intends to take the following actions to improve the quality of healthcare provided: 1. Standards and quality of documentation and record keeping Form a Task & Finish Group to review and develop clear and specific guidance on the practice and requirements around record keeping and documentation. Review the Clinical Record Keeping Policy to clarify standards of practice and procedures around competency assessments and countersigning delegation Include the assessment of competence for record keeping in the Trust competency framework for non-qualified staff Compile all Trust approved forms and make these accessible on the Trust intranet 2. Medications management Update the Medication Competency Workbook to include the need to document the reason for administering the PRN (as required) medication and the outcome of the PRN Add information about what is a rapid tranquilisation and the monitoring requirements following rapid tranquilisation in the Medication Competency Workbook Include examples of medicines reconciliation in the activity section of the medicines management training for nurses 3. Review of policy and procedures Review the Discharge Policy and clarify procedures around discharge planning and documentation requirements Review the Section 17 Policy and clarify the procedures particularly in relation to the responsibility of the nurse in charge to ensure that a risk assessment is carried out prior to allowing the patient to leave the ward for an agreed leave, reviewing planned leave with the patient, and the required documentation regarding these areas Review the forms currently attached to the Falls Policy: (Falls screen, Falls assessment, & Post-falls checklist) to clarify requirements for documentation Page 22 of 74 Revise the ‘risk assessment’ section in the Safeguarding Adults Policy to include agreed timescales for completion of investigation, emphasise requirement for correct filing of documentation, and include requirement for the checklist to be signed off. Develop a pro-forma to guide doctors on the completion of In-patient and CTO (Community Treatment Order) reports. Develop a Trust DoL (Deprivation of Liberty) policy to replace the DoLs guidelines and develop a robust implementation plan. Review the Mental Capacity Act Policy and redesign the CPA capacity form replacing text requirements with tick boxes where possible, and to reduce the length of the form by replacing the legal language with plain English. Revise Medicines Policy to include explicit requirement to document discussion about side effects and benefits of medication Develop a Trust policy on the procedures and standards for Advance Directives Review and update the Continence Policy. Following implementation of actions from audits completed in 2011/12, improvements were made in the quality of our services in 2012/13. Examples include: 1. Medicines management The action to develop and pilot a new form to record discussions about new medication with patients and carers in Phoenix ward has been successful and is reported to have improved engagement and information support for patients and carers. (POMH10a: antipsychotic medicine in CAMH audit) A Medication Competency Workbook was adapted from a London-based Trust and attached to the Medicines Policy to provide clear guidance to nursing on medicines administration, review and documentation. This has made demonstrable improvements on medicines management practice in the wards (Omission of Prescribed drugs audit). The following actions were implemented following the POMH11b: prescribing antipsychotic medication for people with dementia audit, and have resulted in improved results for the 2012/13 round of the audit. o Development of CPFT-specific guidelines which specifies that all letters to GPs for patients with dementia with an antipsychotic medication initiated by the Trust should have an instructions to GPs to review the medication within 6 weeks o Development of joint guidelines on the use of antipsychotics for BPSD (Bipolar Spectrum Disorder) across primary and secondary care which included recommendations for appropriate documentations for appropriate documentation and review dates of medication. 2. Practice improvement Various improvements were implemented from findings of the Record Keeping team-based monitoring audits. This included: o In the Peterborough child health community services, making modifications to Systm1 (electronic records system) to improve processes around countersigning entries made by non-qualified staff, recording of ethnicity data and recording diagnosis and needs at the point of referral. o In the IAPT services, development of guidance around documentation practice requirements and completion of risk assessments, among others. CG45: Antenatal & postnatal mental health audit o A new specialist mental health midwife has been appointed in The Rosie (maternity hospital in Addenbrookes) following results of the audit. Joint planning meetings are held regularly with adult mental health services to coordinate pre birth planning meetings for women Page 23 of 74 3. Policy/guidance development The ‘Use of Physical Interventions in the Management of Violence & Aggression Within Mental Health & Learning Disability Policy’ was reviewed and updated to clearly specify the requirement for documentation around physical restrain (NICE CG25: Violence audit). A Perinatal Standard Operating Procedure was developed to provide staff with guidance on the safe management of women with serious mental illness (SMI) or at significant risk of relapse of SMI in the perinatal period (CG45: Antenatal & postnatal mental health audit) Consent forms for Children’s services were revised and incorporated in the Consent Policy (Children Act 1989 Consent to treatment audit in Phoenix ward) and arrangements put in place to make copies of Consent forms easily accessible to staff. The Reading of Rights form was amended to evidence informing patients of their rights to see an IMHA (Independent Mental Health Advocate Audit) 2.3 PARTICIPATION IN CLINICAL RESEARCH 2.3.1 RESEARCH AND DEVELOPMENT (R&D) Participation in clinical research demonstrates the Trust’s commitment to improving the quality of care we offer and to making our contribution to wider health improvement. CPFT is the host for the National Institute for Health Research (NIHR) Mental Health Research Network that supports well designed research studies adopted to the UK Clinical Research Network (UKCRN) portfolio. The number of patients receiving relevant health services provided or sub-contracted by CPFT in 2012/13 that were recruited during that period to participate in research approved by a research ethics committee was 1,029. This surpasses the Trust’s target of 800 for the year which is positive progress. It is expected that the results for the year will inform the Trust’s financial allocation from the Comprehensive Local Research Network (CLRN) for 2013/14 enabling re-investment in Trust research programmes. As of March 2013, there were 105 active studies in the Trust of which 69 were adopted on the NIHR portfolio. There were 10 portfolio studies in set up. A total of 37 studies were approved in 2012/13, and there are a further 30 studies currently seeking Trust approval. Examples of quality improvement actions relating from research include: CRIS database: CPFT has ethical approval to establish a research database (Case Registry Interactive Search) that will facilitate recruitment of participants into research studies and pilot work is on going DeNDRoN (Dementias and Neurodegenerative Diseases Research Network): New team base and research facility has been launched in December in Windsor House, Fulbourn MHRN (Mental Health Research Network) A transition plan has been developed by the Department of Health that will bring about key changes for the current set up of the NIHR Clinical Research Network (CRN). By April 2014 the NIHR CRN will comprise of 15 Local Clinical Research Networks, each with a single host organisation. The appropriate host organisations will be confirmed by Autumn 2013 through NHS competition. The boundaries of the networks have yet to be decided but they will align with the Academic Health Science Networks. Page 24 of 74 2.3.2 CLAHRC CP CPFT is also the lead NHS Trust for the NIHR Collaboration for Leadership in Applied Health Research and Care for Cambridgeshire and Peterborough (CLAHRC CP), a centre for mental health research that will accelerate health research into patient care. As of March 2013, CLAHRC CP had over 100 projects on its portfolio, 23 of which were classed as priority projects, across the five themes: Adults, Child and Adolescent, Old Age and End of Life Care, Public Health and Design and Implementation. Examples of CLAHRC studies that have led to improved outcomes of care include: Transfer of Care at 17 pilot study Strong collaborations and partnerships with NHS and social care partners have ensured findings from this study, which focuses on the transition period from adolescent to adulthood, have been incorporated into care pathways. Dementia register The Old Age theme has conducted a scoping exercise on the feasibility of establishing a dementia register in Cambridgeshire and the project is being taken forward by the NIHR Biomedical Research Centre (BRC). Cognitive therapies The East of England SHA has adopted the research outputs of an NIHR CLAHRC CP project on the comparative effectiveness of cognitive therapies delivered face to face and over the telephone in the Improving Access to Psychological Therapies (IAPT) programme. The outcome of which is that regional training for telephone sessions has been delivered. The NIHR CLAHRC CP has continued to produce a successful Fellowship Scheme over the past two years involving 3 cohorts, 33 professionals and 14 partner organisations. Findings from several fellows’ projects have been translated into service change and resulted in published journal articles. An example of service change is the introduction of training for District Nurses in evidence-based end of life care in Peterborough. 2.3.3 SERVICE USER AND CARER ENGAGEMENT IN RESEARCH Service User and Carer Involvement is a key priority area within the Trust’s R&D activities. The R&D department runs a programme to support and strengthen meaningful involvement of Experts by Experience in all stages of the research. This service is available to all potential and established NHS researchers, service users and carers. During 2012/13 we recruited and supported 18 service users and carers to be involved in 11 research activities as service user advisors or researchers. Advice and support was provided to 15 researchers. Key achievements during the year include: Development of a pilot introductory research training for new members of our service user and carer group in collaboration with CLAHRC CP. The programme provides a basic introduction to research and involvement in research. Nine people attended the first training course in March 2013 with very positive feedback. Since September 2012 service user and carer involvement has become a step in the process of obtaining CPFT R&D approval. As of March 2013, 80% of all locally developed research projects that have gone through R&D approval have been reviewed by members of our service user and carer research group to ensure that their project has appropriate service user and carer involvement. Page 25 of 74 2.4 COMMISSIONING FOR QUALITY AND INNOVATION (CQUIN) PAYMENT FRAMEWORK A proportion of CPFT’s income in 2012/13 was conditional upon achieving quality improvement and innovation goals agreed between CPFT and any person or body they entered into a contract, agreement or arrangement with for the provision of relevant health services, through the Commissioning for Quality and Innovation payment framework. Further details of the agreed goals for 2013/14 and for the following 12 month period are available online at: https://www.gov.uk/government/publications/using-thecommissioning-for-quality-and-innovation-cquin-payment-framework-guidance-on-new-nationalgoals-for-2012-13 The total value of the payment for completion of our quality goals in 2012/13 amounts to £1,345,282 compared to £1,364,674 for our 2011/12 CQUIN. The Trust’s Lead Commissioner is NHS Cambridgeshire with whom the Trust agreed a number of quality goals for 2012/13. It is worth noting that the goals agreed at the beginning of 2012/13 as reported in our Quality Report 2011/12 were further reviewed and finalised in July 2012. These are outlined below: Table 3: CQUIN performance against 2012/13 goals CQUIN 2012/13 GOALS Performance Goal 1 The Trust has carried out monthly NHS Safety Thermometer surveys of wards for Theme: NHS Safety Thermometer older people and learning disabilities. Improve collection of data in relation to Quarter 1: Achieved 97.6% harm free care pressure ulcers, falls, urinary tract Quarter 2: Achieved 98.8% harm free care infection with a catheter, and VTE. Quarter 3: Achieved 97.1% harm free care Quarter 4: Achieved 98.2% harm free care Goal 2 Indicator 1 Theme: Dementia The Trust has, in collaboration with all Improve awareness and diagnosis of Acute Providers within the locality, dementia by training staff in other local developed and implemented over 70 NHS providers. training sessions. Indicator 1 Key outcomes: Number of dementia training sessions Feedback received shows that 95% of delivered to each Provider Trust participants learnt lot about the subject highlighted above to enable these as a result of the training service Providers to deliver their 86% of participants reported a change provider specific CQUIN schemes in their attitude and approach to people relating to dementia. with dementia. Indicator 2 Improve access to prompt advice and support for people and their carers recently diagnosed or identified as potentially at risk of dementia following screening in hospital or community services. Goal 3 Theme: Patient experience Improve responsiveness to personal needs of patients. Indicator 1 To ensure that providers have real time systems in place to monitor patient experience. Indicator 2 There is initial evidence to show that referrals to Liaison Services within CUHFT (Cambridge University Hospitals NHS Foundation Trust) have increased as a result of the training. Indicator 1 CPFT has developed, with Meridian, a web based patient survey system to routinely collect real-time patient experience data across all inpatient and community teams using iPads. Results are discussed at our monthly Divisional Performance Review meetings with clear lines of accountability up to the Trust Board Page 26 of 74 Indicator 2 To demonstrate improvements in patient experience using the Net Promoter Score (NPS). Indicator 2 The Trust’s overall average NPS score of 47% for the year. This shows a 13% increase from the baseline figure in April 2012. Goal 4 Theme: Making Every Experience Count Clinical Staff working in the agreed areas have appropriate knowledge and skills to make to make a “brief advice” intervention for alcohol/smoking or both and to signpost or refer as appropriate in line with the ‘Making Every Contact Count’ Initiative. Goal 5 Theme: Measuring Outcomes Routine reporting of outcome measures for each of CAMH (IAPT), Adult (Recovery Star) and OPMH CORE 10 and QALY AD. We provide an e-learning training package to our staff within the Rehabilitation and Recovery Pathway to equip them with the knowledge and skills to engage with their patients around healthy lifestyle issues and refer them on to the appropriate agency, where required. We have not met the target as of March 2013 The Trust will continue to roll out the e-learning package to the remainder of staff in early 13/14. CAMH IAPT: Our staff have been trained in undertaking the CYP-IAPT Outcomes Measures during 12/13. We encountered a number of challenges around putting the technology in place but by Q4 the necessary systems were in place to support greater usage of outcomes measures in 2013/14. Adult: During 2012/13 we trained over 80% of our staff within the Rehabilitation and Recovery Pathway to use the Recovery Star which gets a patient to look at recovery as a journey with different stages. Using this approach has led to a change in the culture, care delivered and supporting documentation resulting in better outcomes for the patient. OPMH CORE 10/QALY AD: 70% of service users in the specified pathways have undertaken the specified outcome measures. As per the NICE Guidelines we give priority access to perinatal patients with the average waiting time across the locality being 25 days during 2012/13. Goal 6 Theme: Perinatal Mental Health Delivery of NICE guidelines for priority access to IAPT for pregnant and postnatal women. Goal 7 Theme: Learning disability Improve access to mental health services for people with learning disability, based upon the annual selfassessment of progress that CPFT has completed and reinforcing the subsequent Action Plan. Goal 8 Theme: ADHD Training of core staff within Intake and Treatment Teams in diagnosis and advice on patient management for ADHD. The Trust has continued to deliver against the Learning Disability Performance Indicators Access to Healthcare Action Plan. CPFT staff have delivered ADHD training to staff within the Department of Psychiatry and the Intake and Treatment Team during 2012/13, based on training materials developed through CPFT and the University. Page 27 of 74 2.5 CQUIN GOALS 2013/14 As part of our contractual agreement with NHS Cambridgeshire for 2013/14, the Trust will work towards the achievement of a range of quality goals which will support further improvements in patient experience, patient safety and clinical effectiveness. We will report on our achievements in meeting these goals as part of next year’s quality report. The proposed goals for 2013/14 which are still under discussion as of the date of this report are outlined below. Develop a service specification to improve the smooth transition and have a person centred planning and flexible approach to the transition of children and adolescent service users into the adult mental health services To improve physical health outcomes for patients given the impact of physical morbidity in mental health users and the mortality among those with mental illness Patient Access - development of a Directory of Services for Choose and Book and selfreferral to the Advice Referral Centre 2.6 CARE QUALITY COMMISSION (CQC) REGISTRATION The Care Quality Commission (CQC) is the independent regulator of all health and social care services in England. Its primary role is to ensure that the care people receive meets essential standards of quality and safety and to encourage on going improvements by those who provide or commission care. CPFT is required to register with the Care Quality Commission and its current registration status is ‘Registered Without Conditions’. The Care Quality Commission has not taken enforcement action against CPFT during 2012/13. CPFT has participated in two investigations by the Care Quality Commission relating to the areas outlined in the following page during 2012/13. 2.6.1 CQC INSPECTIONS We had two conditions on our registration at the beginning of 2012/13 resulting from investigations carried out in the previous year: minor concern on Outcome 16 (Assessing and monitoring the quality of service provision), and moderate concern on Outcome 1 (Respecting and involving people who use services). A summary of the CQC inspections and reviews during the year and the outcomes thereof is outlined in Table 4. Improvement actions were also identified in our inpatient units on the following areas: Fulbourn Hospital site: Outcome 10 (Safety and suitability of premises) around providing better facilities that allow patients to access peaceful and private spaces or rooms Cavell Centre site: Outcome 4 (Care & welfare or people who use the services) around ensuring that care records provide clear information about any untoward event experienced by patients, and Outcome 10 (Safety and suitability of premises) around ensuring that patients have freer access to outside areas and this is managed according to their assessed risk. The inspection carried out in June 2012 in the Fulbourn Hospital site found us to be fully compliant with Outcomes 1, 4 and 14. They identified concerns in Outcome 9 (Management of medicines), particularly in relation to recording of medicines administration and the recording of medicines used on a discretionary basis (PRN) to control a person’s challenging behaviour. The CQC also identified concerns against Outcome 16 (Assessing and monitoring the quality of service provision) to fully strengthen and develop its Board of Directors and to deliver a clear and effective strategy to improve, monitor and maintain the quality of its services. Page 28 of 74 The CQC carried out a table top review of evidence for Outcome 9 and 16, and an inspection in the Cavell Centre site in December 2012. The report was published in February 2013 which declared the Trust fully compliant in all areas covered by the review. Table 4: Summary of investigations carried out during 2012/13 Fulbourn Hospital Cavell Centre Inspection CQC dates CQC Outcomes Judgement Judgement Outcomes As of 31 March 2012 Outcome 10 Outcome 16 Outcome 4 Outcome 9 minor concern Outcome 14 Outcome 16 December 2012 table top review minor concern Outcome 1 June 2012 inspection improvement actions Outcome 4 Outcome 10 Outcome 16 minor concern Outcome 1 moderate concern moderate concern Outcome 16 Outcome 18 Outcome 20 Outcome 1 Outcome 1 Outcome 7 December 2012 inspection Outcome 13 Outcome 16 Outcome 4 As of 31 March 2013 Outcome 9 Outcome 10 Outcome 14 Outcome 16 improvement actions Outcome 9 Outcome 1 improvement actions Outcome 7 Outcome 13 Outcome 16 Outcome 18 Outcome 20 A number of actions were taken in 2012/13 that secured full compliance with the CQC standards by the end of the year. A summary of the key actions and excerpts from CQC reports are presented in the following pages. Page 29 of 74 Excerpts from CQC reports July 2012 report People told us that staff treated them respectfully and in a way that they liked. One person commented, "Some staff are really good, really on the ball, quite sensitive to how you're feeling". Another person who had been a patient previously told us, "It's so nice having my own room now. I sleep better and have privacy to lie down for half an hour if I want". Another person commented, "I've recently started water tablets so having the en suite toilet is a god send". (pg 8) As part of our inspection we undertook a short SOFI (Short Observational Framework for Inspection) on Willow Ward. SOFI is a tool which provides us with information about people's experiences of their care, their general mood state and their engagement and interaction with those providing their care. Throughout our observation we noted that people showed signs of well being and were calm, relaxed and engaged in what was going on around them on the ward. The quality of interaction between people and staff was mostly very good, with staff showing respect and empathy to people. For example, we observed two staff members assist one person to move between an armchair and a dining room chair. This was done well with staff explaining to the person throughout the transfer what they were doing and also reassuring them appropriately when they became agitated during the move. We saw a member of staff talk to one person about his mother's Irish stew (which was on the menu that day), resulting in much laughter between them. On another occasion we noted that one person's unusual request for what they wanted for their lunch was fully respected by staff. We witnessed staff knocking on people's bedroom doors and waiting for a response before they entered, and people (both staff and patients) being refused entry to the ward's clinical room when treatment was being given to people. (pg 9) January 2013 report We inspected a ward for older people living with dementia. Staff on this ward were busy, but people's needs were met in a calm, professional and unhurried manner. We spoke with relatives, one of whom said, "The staff are beautiful, they're angels. They're all nice, there's not one nasty one. There are plenty of staff." Another relative told us that all the staff are "…fine" but said there were times, when the ward was full and in the evenings, when "…they could do with more staff." Senior staff on this ward told us they had introduced a 'twilight shift' to improve the service offered in the evening and that there were enough staff to meet people's needs. (pg 8) Our inspection of February 2012 identified that there was an inconsistent approach to the way in which people's dignity was upheld and maintained. In their declaration of compliance with this regulation, the trust told us they had done a lot of work to turn this around. They had introduced a number of measures to check that people had a positive experience during their admission to the wards. One of these measures, REV (Respect, Empower, Value), involved assessments and audits of each ward, carried out by a member of staff from another ward. During our inspection on 12 December 2012 we saw improvements on Maple 1 in the way that staff spoke with people, the way they treated people and the ways they now worked to promote people's dignity. We spent some time on the ward observing the interactions between people on the ward and the staff. Staff worked well as a team to support people. They spoke kindly and patiently to people, without being patronising, and they listened when people wanted to talk with them. The staff noted when someone was becoming agitated or behaving in a way that might upset someone else, and they responded appropriately, distracting the person and calming them. Communication on the ward had also improved. Senior staff told us that they had introduced and strengthened systems to ensure that communication between staff, people on the ward and their relatives was as good as possible. Relatives we spoke with told us that they were fully involved in the care their family member received. They felt comfortable with speaking with staff at any time, could telephone the ward for information if they were not able to visit and were confident that they would be communicated with when necessary. One relative told us they had been invited to attend the doctor's round at the end of the week. A notice board on the ward gave people information such as how to contact local support groups and advocacy services. (pg 6) Page 30 of 74 Trust actions in response to CQC findings 1. Guiding Coalition and Satellite Team The Guiding Coalition was formed in January 2012, consisting of 80 staff members from all staff groups across the Trust, to develop solutions on the areas identified for improvement and input directly into the turnaround board. A Satellite Team of around 94 staff was also formed to support the Guiding Coalition to deliver change at local level. These two groups continued into 2012/13 which made a significant impact on the success of our turnaround programme. 2. 7Cs standards of care planning The 7Cs standards were developed to assess the quality of our assessments and care planning process and documentation. Monthly peer assessments were carried out by senior clinicians involving an examination of care records and interviews with patients and staff. 7Cs was initially implemented in our inpatient units and later rolled out to community-based teams. Scores were reported as part of the quality dashboards and shared on a Trust wide basis. 3. Environmental refurbishment and repairs We started a wide ranging programme of refurbishment and repairs of all inpatient units in December 2011 following a systematic and comprehensive review of our facilities. We continued with this programme of improvement throughout 2012 and have extended the work to cover our community-based services and corporate offices coming into 2013. 4. 5 star environmental standards 5 star environmental standards were developed in the last quarter of 2011/12 and initially implemented in our inpatient units. This also involved monthly peer assessment carried out by senior staff and clinicians and reported as part of the quality dashboards. The 5 star assessments were piloted in our community-based teams in November 2012 – March 2013. 5. REV (Respect, Enable and Value) standards REV was developed to address the concerns around Outcome 1, and implemented in our inpatient units on a peer review basis. Teams were scored against the standards based on observations made around patient-staff interactions. Scores were reported as part of the quality dashboards. This has driven up the standards around patient-staff interactions. 6. InCA (Integrated Compliance Assessment) InCA was developed to enable teams to assess their compliance with all 16 CQC Outcomes on a monthly basis, and involved a self assessment and peer review process. It incorporates the 7Cs and 5 star standards. InCA was implemented in our inpatient units in June 2012 and piloted in selected community-based teams in March 2013. It will be rolled out to all community-based teams by the end of 2013. This provides the Trust with assurance of our compliance with the CQC Outcomes and enables us to focus our resources on areas that require action in a timely manner. 7. Medicines management action plan A set of actions were put in place to improve compliance with the standards around medicines management. Specifically, this included increasing awareness amongst nursing staff of medicines administration recording requirements and the implementation of a new ‘when required’ medicines policy. Other general actions included ones identified from audit projects and the annual medicines reviews, such as the development of the Medications Competency Workbook, improving the training programme and regular monitoring of practice through the InCA process and the audit programme 8. Performance management framework Monthly triangulation meetings are undertaken with the aim of gathering all relevant information from all sources. This enabled us to use information strategically and identify possible reasons that give rise to problem areas. This information informed the Divisional Performance Review meetings. This has strengthened Divisional accountability over performance issues and ensured that appropriate actions are taken in a timely manner. Page 31 of 74 2.6.2 MENTAL HEALTH ACT INSPECTIONS Throughout the year, the CQC conducted a number of reviews in respect of Trust services provided for persons detained under the Mental Health Act (MHA). The results are outlined on the right. In total, 8 MHA visits were carried out, 7 of them were unannounced. The one planned 2-day visit to the Cavell Centre in Peterborough was carried out by Commissioners accompanied by an ‘Expert by Experience’, and included representatives from Peterborough City Council and Cambridge County Council. The visit focused on monitoring the compliance with the “Assessment, application for detention and admission under the MHA” process. The Commissioners reported very positive feedback from patients about their experience in the wards, their involvement, care and their relationship with staff. They found the relationship between the Trust and external agencies to be effective and engaging and reported good governance and procedural arrangements. They also found the Approved Mental Health Professionals (AMHPs) assessment procedure to be effective and were satisfied with the Mental Health Act Administration, quality assurance processes, and compliance with the Act’s legal requirements. Minor concerns around the unit’s 136 suite environment were raised (Section 136 -Place of safety) and at the time of this report, the Trust still awaits the formal CQC recommendations, which will aide the current review of S136 functions across the Trust. Following their visits to other sites within the Trust, the visiting commissioners were satisfied that patients’ were detained by the Trust lawfully their rights were read adequately and regularly activity programmes were in place, were of a good standard and individualised. MHA inspections in 2012/13 7 unannounced visits 1 planned visit 12 units inspected 14 sets of case notes scrutinised Good practice noted. Completion of previous recommendations Compliance with reading and reminding patients of their rights Good patient involvement in care planning Good interaction and engagement between patient and staff Access to advocacy services Clean and safe environment Good activity programmes in place Recommendations for S58 Improve practice around recording of capacity to consent treatment assessments Review recording process of risk assessments carried out prior to authorising S17 leave These findings were also highlighted by our local audits. Actions have been developed to address these areas. The commissioners reported good staff patient interaction. The care plans inspected were comprehensive and were reviewed regularly and patients’ involvement was evident. The visiting commissioners also noted that the units visited were clean, well presented and safe. The CQC were satisfied that most of their recommendations around ligature and environmental improvements from previous visits were completed, or that there was a plan in place to ensure their completion. The CQC has not published the Mental Health Act annual statement for the review period 2012/13, as of the date of this report. Page 32 of 74 2.7 DATA QUALITY AND INFORMATION GOVERNANCE CPFT submitted records during 2012/13 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in published data: which included the patient’s valid NHS number was: o 99% for admitted patient care which included the patient’s valid General Practitioner Registration Code o 99% for admitted patient care CPFT’s Information Governance Assessment Report overall score for 2012/13 was 79% and was graded GREEN The Trust was not subject to the Payment by Results clinical coding audit during the reporting period by the Audit Commission. CPFT will be taking the following actions to improve data quality: Rolling out RIO Electronic Care Record System across all Clinical Divisions and teams Undertaking monthly non compliance audits of 7 day follow up and CRHT gatekeeping indicators Developing an automated system for the capture and reporting of Mental Health Act compliance A data cleansing exercise for ESR and an exercise to support the standardisation of roles Developing and rolling out InCA to record and report upon compliance with the 7Cs care planning standards Developing a protocol which outlines the calculation methodology for all performance indicators on the Trust dashboard. 2.8 MANDATORY CORE SET OF QUALITY INDICATORS From 2012/13, all Trusts are required to report against a core set of quality indicators using data for the last two reporting periods provided by the Health and Social Care Information Centre (HSCIC). The indicators that are relevant to CPFT are listed below. Table 5: Mandatory core quality indicators for 2012/13 Prescribed information 1. The percentage of patients on Care Programme Approach who were followed up within 7 days after discharge from psychiatric in-patient care. 2. The percentage of admissions to acute wards for which the Crisis Resolution Home Treatment Team acted as a gatekeeper. 3. The percentage of staff employed by, or under contract to, the Trust who would recommend the trust as a provider of care to their family or friends. 4. The Trust’s “Patient experience of community mental health services” indicator score with regard to a patient’s experience of contact with a health or social care worker. 5. The number and, where available, rate of patient safety incidents reported within the Trust, and the number and percentage of such patient safety incidents that resulted in severe harm or death. Where the data reported in the HSCIC indicator portal does not reflect the most current data, we have provided current data available from the Trust. Note: For a full definition of the quality indicators 1, 2 and 5 see page 64 in Annex 2. Page 33 of 74 2.8.1 Patients on Care Programme Approach who were followed up within 7 days after discharge from psychiatric inpatient care during the reporting period. Table 6: Patients on CPA followed up within 7 days CPFT considers that this data is as described for the following reason: Table 6 shows that CPFT is only two points below the national average rate of 97.60% in 2011/12, while four Trusts achieved 100%. Reporting period 2012/13 (CPFT data) CPFT 93.75% Oct-Dec 2012 95.2% (HSCIC data) (n=334/351) Jul-Sept 2012 95.7% (HSCIC data) (n=337/352) England average Highest rate Lowest rate Target 95% Not yet available from HSCIC (CPFT) 97.60% 100.00% 93.00% 97.20% 100.00% 89.80% 95% (national) Trust performance as of March 2013 is 93.75%, which is just under the target of 95% during the period 2012/13. Chart 1: Patients on CPA followed up within 7 days CPFT intends to take/has taken the following actions to improve this 93.75%, and so the quality of its services, by: reviewing our Discharge Policy and procedures continuing to monitor and report on our performance against this indicator through our quality dashboards 2.8.2 Admissions to acute wards for which the Crisis Resolution Home Treatment Team acted as a gatekeeper during the reporting period. Table 7: Admissions gatekept by CRHTT CPFT considers that this data is as described for the following reason: Table 7 shows that CPFT had the lowest rate nationally for the period Oct-Dec 2012, with 18 Trusts achieving 100%. Reporting CPFT period 2012/13 93.17% (CPFT data) Oct-Dec 2012 90.7% (HSCIC data) (n=390/430) Jul-Sep 2012 91.7% (HSCIC data) (n=409/446) England average Highest rate Lowest rate Target 95% Not yet available from HSCIC (CPFT) 98.40% 100% 90.70% 98.10% 100% 84.00% no national target Trust figures as of March 2013 is 93.17% which is just under the target of 95% and shows an improvement from 91.74% in 2011/12. Chart 2: Admissions gatekept by CRHTT CPFT intends to take/has taken the following actions to improve this 95.24%, and so the quality of its services, by: redesign of our clinical services monitoring performance through our quality dashboards making this our quality priority under the Clinical Effectiveness domain for 2013/14. Page 34 of 74 2.8.3 Staff employed by, or under contract to, the Trust during the reporting period who would recommend the Trust as a provider of care to their family or friends. Table 8 below shows the proportion of our staff who would recommend CPFT as a provider of care to their family and friends in 2011 and 2012, compared with the average, highest and lowest scores for all mental health Trusts and all healthcare providers in England who took part in the survey. In 2012, we scored the lowest among all mental health Trusts. Table 8: Staff who would recommend CPFT as a provider of care to their family or friends. Average rates Reporting period 2012 2011 Highest rates Lowest rates CPFT Mental Health England (all Trusts) Mental Health England (all Trusts) Mental Health England (all Trusts) 39% 50% 58% 58% 63% 60% 80% 83% 94% 96% 39% 43% 35% 22% CPFT considers that this data is as described for the following reason: The major turnaround programme implemented during the year affected staff morale. This is discussed in more detail in sections 1.2.3 and 5.2. Chart 3: Staff who would recommend CPFT CPFT intends to take/has taken the following actions to improve this 39%, and so the quality of its services, by: talking to our staff to find out the issues they are facing and what we need to do to make it better. developing an action plan to address the issues that came out of the National NHS Staff Survey. developing a Workforce Strategy in consultation with our staff. 2.8.4 “Patient experience of community mental health services” indicator score with regard to a patient’s experience of contact with a health or social care worker during the reporting period. The weighted average of our scores for these questions is shown in Chart 4 below, compared with the average, highest and lowest scores of all community mental healthcare providers in England who took part in the survey. Chart 4: Patient experience scores This indicator uses the weighted average for the following questions in the CQC survey of community mental health services: Thinking about the last time you saw this NHS health worker or social care worker for your mental health condition… …Did the person listen carefully to you? …Did this person take your views into account? …Did you have trust and confidence in this person? …Did this person treat you with respect and dignity? Page 35 of 74 It is worth noting that our scores are higher than the national average for this indicator in both years (see section 3.1.3 for further details on our national CQC Community Patient Survey 2012). We believe that the heart of a quality service lies in the relationship between a member of staff and their patients. Quality comes when this relationship is based on values of trust, respect, and mutual endeavour to improve the patient’s health, well being and quality of life. All members of our staff are expected to uphold and promote these principles which are embedded in our four key values outlined below: CPFT’s Four Key Values Patient first: we focus on the needs of the whole person, we aim to consistently 1 exceed the expectations of our patients and their carers by making every interaction with them count 2 Only the best: we have high standards in all that we do, we are uncompromising in our pursuit of excellence, we only do what is known to work, we evaluate everything that we do and share the data with others to allow them to hold us to account. 3 Staff matter: we trust, value and develop each other, we build a great place to work where people are inspired to be the best they can be, where they are engaged in decisions that affect them and where they are empowered to deliver better and safer services. 4 Together as one: we value our teams and our partners and believe we can achieve more by working together for the benefit of the people we serve. The graph below is taken from the 2012 CQC Community Patient Survey report. The black diamond in the bar represents the score for CPFT while the green bar represents the scores of the best performing Trusts in the country. We are very pleased with these results and we are very proud of our staff for the commitment and dedication that they have shown to their work and most importantly, their patients. CPFT considers that this data is as described for the following reason: All the changes we have made in the past year around care planning, involvement and other ways of working have had a positive impact on the experience of our patients. CPFT has taken the following actions to improve this 89.32%, and so the quality of its services, by: sharing these results with our staff and developing a Trust action plan to address the issues identified in the patient survey results developing a Partnership Strategy 2013-2016 appointing a Head of Patient Experience and Engagement Page 36 of 74 2.8.5 The number, and where available, rate of patient safety incidents reported within the Trust during the reporting period, and the number and percentage of such patient safety incidents that resulted in severe harm or death. The data reported in the HSCIC indicator portal, which is derived from the NRLS (National Reporting and Learning System), are presented in six month periods up to March 2012. For comparison purposes, we have only taken figures reported by mental heath providers that have submitted six months worth of data per 1000 bed days. It is worth noting that: all mental health providers calculate their rates per 1000 bed days 12 PCTs also reported 6 months worth of data which were calculated per 1000 bed days, these were excluded from the figures presented in this section. Within this group, one PCT reported an incident rate of 157, two PCTs reported 118, and one of each reported an incident rate of 95 and 77. The highest rate reported by a mental health provider is 59. Other healthcare providers (Acute Specialist, Ambulance, large Acute, medium Acute, small Acute and PCTs with inpatient provision) that report data calculated per 100 admissions were excluded from the comparative figures as our data would not have been comparable with the data reported by these healthcare providers. We have also presented data for incidents reported in the Trust during 2012/13 that are not yet reflected in the HSCIC indicator portal as of the date of this report in order to present our most up to date performance data. CPFT considers that the data presented in this section is as described for the following reasons: CPFT is in the highest quartile of 57 reporting mental health providers in the country. Over the past two years, we have worked hard to improve our training programme and raise awareness around patient safety incidents. Charts 7 and 8 show that we report higher numbers of ‘no harm’ incidents which may explain the higher rates of patient safety incidents reported by CPFT as compared to the national average. The proportion of patient safety incidents that resulted in severe harm or death was only around 1.6% of our total reported patient safety incidents in 2011/12, reducing to 1.3% in 2012/13. CPFT has taken the following actions to improve this 0.73 and 0.48 (rate of patient safety incidents that resulted in severe harm or death), and so the quality of its services, by: We have reviewed our Policy and Procedure for Reporting, Managing and Investigating Incidents Including Serious Incidents (SIs). The revised version has been approved and ratified. We have started to deliver additional Root Cause Analysis (RCA) training We have established a Serious Incident Group We have appointed a Patient Safety Lead for the Trust who will lead and work with the Clinical Divisions on the management of incidents and serious incidents in the Trust We are working with our commissioners and with our partner organisations in the development of an over arching Suicide Prevention Strategy for CPFT that links with the national and regional strategy We are monitoring all relevant data and information around incidents and serious incidents through our quality dashboards reporting framework We have commissioned Professor Louis Appleby to undertake a review of selected serious incidents in order to identify further areas for improvement We are undertaking a Trust wide Clinical Risk Assessment audit to investigate compliance with our Clinical Risk Assessment and Care Planning Policies, planned in 2013/14 Page 37 of 74 1. Number of patient safety incidents Data available from the HSCIC indicator portal during the reporting periods April – September 2011 and October – March 2012 are presented below. 2012/13 data is not yet available from the HSCIC indicator portal. Trust data showing figures for 2012/13 are shown in Table 9 in the following page. Chart 5: Number of patient safety incidents Data reported by NRLS shows that CPFT is in the highest quartile of 57 reporting mental health providers in the country. Chart 5 shows that the number of patient safety incidents reported by CPFT is comparable to the average numbers reported by other mental health providers. 2. Rate of patient safety incidents Data available from the HSCIC indicator portal during the reporting periods April – September 2011 and October – March 2012 are presented below. Chart 6: Patient Safety Incidents per 1000 bed days Chart 6 shows that CPFT’s rate of patient safety incidents is higher than the average for mental health providers but much lower than the highest rate reported. Refer to item 4 for additional information. Note: The Trust’s reporting of all incidents, including serious incidents, has been subject of rigorous review by the CQC and as a consequence changes to our reporting processes were put in place from 2010. Patient safety has been one of our main focuses in the past couple of years. We have improved training and raised awareness of patient safety incidents. We have worked with our Divisions and clinical teams in reviewing the incident reporting process and procedures. We have processes in place to monitor, through our governance arrangements, patient safety incidents. This has resulted in a higher rate of reporting. According to NPSA, ‘Organisations that report more incidents usually have a better and more effective safety culture’ (NRLS patient safety incidents monthly reports for CPFT). Page 38 of 74 Chart 7: Oct 11 – Mar 2012 (NRLS 2012) Charts 7 and 8 show that a higher proportion of our incidents result in ‘no harm’, as compared to other mental health Trusts. This indicates a good culture of reporting in CPFT. However, a slightly higher proportion of our reported incidents result in moderate harm and death which is reflected in the data reported in item 4. Data for the top 10 incident types reported by NRLS (see Chart 9 below) shows that CPFT is reporting higher rates of selfharming behaviour. This may be explained by our Complex Cases ward and our Adolescent ward, which are part of our Acute Care Service, and who are reporting over half of the incidents in the Trust. We are reporting significantly lower rates of incidents relating to patient accidents and medication. Chart 8: Apr - Sep 2012 (NRLS 2012) Improving patient safety is a Trust priority. We have adopted the ‘7 steps to patient safety in mental health’ published by the National Patient Safety Agency (NPSA) to better support our staff to ensure they manage risk effectively and improve the safety of our patients. Chart 9: Apr – Sep 2012 Top 10 incident types (NRLS 2012) Page 39 of 74 3. Proportion of CPFT patient safety incidents that resulted in severe harm or death Data available from the HSCIC indicator portal during the reporting periods April – September 2011 and October – March 2012 are presented in Table 9 below, along with CPFT data for the period 2012/13 as follows: April – September 2012 submitted and reflected in the NRLS website October 2012 – March 2013 submitted to the NRLS system but not yet final Table 9: Incidents resulting in severe harm or death Reporting period Oct 12-Mar 13 (CPFT data) Apr 12-Sep 12 (NRLS data) No. of incidents reported Incidents Total incidents Incidents resulting in resulting in resulting severe severe harm in death harm or death % 2282 12 23 35 1.5% 2268 9 17 26 1.1% Oct 11-Mar 12 (HSCIC data) 2527 11 31 42 1.6% Apr 11- Sep 11 (HSCIC data) 1981 4 26 30 1.5% 4. Rate of patient safety incidents that resulted in severe harm or death Chart 10: Incidents resulting in severe harm or death Data available from the HSCIC indicator portal during the reporting periods April – September 2011 and October – March 2012 are shown in Chart 10 on the right. Note: Data for 2012/13 is not yet available from HSCIC. However, Table 9 shows a 15% reduction in our incidents resulting in severe harm or death during 2012/13 (72 in 2011/12 to 61 in 2012/13). The proportion of incidents resulting in severe harm or death is also slightly lower from 1.6% in 2011/12 to 1.3% in 2012/13. During the year, we made significant improvements in our ward environments. This includes removing all ligature points in our wards and any fixture that patients could use to harm themselves or others. We also put measures in place to reduce the risk of absconsions which includes reinforcing doors and windows, raising the height of garden walls and moving garden benches away from the garden walls, among others. In addition we developed a policy and improved arrangements around access to our wards and improved clinical risk assessment training which showed increased levels of attendance during the year. These measures appear to have made a positive impact on our patient safety incidents during the year. Moving forward, the review currently being undertaken by Professor Louis Appleby will provide us with valuable learning in order to make improvements in this area. Page 40 of 74 PART 3: OTHER INFORMATION 3.0 OTHER CPFT QUALITY PERFORMANCE INDICATORS 2012/13 The quality performance indicators presented in this section have been identified through the following: We discuss performance on our quality dashboard through the monthly Performance and Risk meetings between our Executive team and Divisional managers; and regular reports to the Trust Board on the outcome of these meetings. We work closely with our commissioners and other appropriate stakeholders to review our performance against quality indicators and the overall quality of our services. During the year, we have also worked closely with the Adults Wellbeing and Health Overview and Scrutiny Committees in Cambridgeshire and Peterborough around our planned service improvements and to identify areas for further improvement. This is reflected in their commentaries in Annex 3 of this report. For 2012/13, we have reported on additional quality performance indicators not included in the 2011/12 report, as follows: We have improved the way we collect and monitor our performance on Reading of Rights and this was added to our quality dashboard during the year We have made significant improvements around MRSA screening during the year following its inclusion in the Patient Safety Thermometer as part of our CQUIN goal 1 (see section 2.4). We have presented data on breastfeeding to better reflect the diversity of the services we provide. This has also been an area of concern for the Trust and is subject to on going discussions with our commissioners. We have included care planning as a separate item in this section in order to report on the significant achievements we have made in this area in the past year. 3.1 PATIENT EXPERIENCE 3.1.1 Mental Health Act Compliance – Reading of Rights Chart 11: Reading of Rights Reading of Rights was added as a quality indicator during the year and is the first item in our quality dashboard. We have a target of 100%. As of March 2013, the total average compliance rate was 91%. Prior to January 2012, compliance on this indicator was audited based on a sample of cases only. This explains why we only have figures available for Q4 2011/12 (January – March 2012) as shown in Chart 11. From January 2012, data is collected by our MHA administration team on all patients detained under the MHA and reported as part of our quality dashboard. This shows our commitment to improving our performance in this area and ensuring that patients are given information about their rights. From July 2013, we will be monitoring the completion of capacity assessment for patients who lack capacity to understand their rights. We are working with our Modern Matrons and Ward Managers to highlight the importance of this statutory requirement. This is also monitored through our InCA process. Page 41 of 74 3.1.2 Complaints and Patient Advice and Liaison (PALS) There was a 37% reduction in the number of complaints received from 118 to 74 in 2012/13. This figure is relatively small when taken in the context of the total number of episodes of care (approximately 22,144 during 2012/13). Monthly trends are shown in Chart 12. Chart 12: Complaints during 2012/13 Greater engagement between complainants and our staff, together with the revised complaints process and the implementation of effective action plans, has increased carer and patient confidence in the process. Actions taken that have contributed to this improvement include: Better engagement with families Early PALS involvement Clear and timely information with patients and carers Working with Complaints Advocacy Chart 13: PALS contacts in 2012/13 There was a very small reduction in PALS contacts from 538 in 2011/12 to 500 in 2012/13. The monthly figures are shown in Chart 13. Data is collected by our Complaints & PALS team and is monitored through the monthly Quality and Safety reports to the Quality & Performance Committee and the Trust Board. 3.1.3 Mandatory CQC Community Patient Survey Chart 14: CPFT scores for quality of care over time (Quality Health 2012) The results of our CQC Community Patient Survey 2012 shows an overall improvement in our scores in 2012. This is largely due to the work we have done around improving the quality of our care plans and the involvement of patients and carers in planning their care. CPFT results on the overall satisfaction rating have steadily increased over time as shown in Chart 14. Page 42 of 74 It is worth noting that these results are supported by findings from the National Audit of Schizophrenia 2012, whereby 81% of our patients reported a positive experience of our service against the national average of 76%, while 84% reported positive outcomes of care against a national average of 78%. Our top 5 and bottom 5 scores are shown below. This shows that our patients are happy with the quality of their relationship with our staff and their involvement in planning their care. These scores are reflected in our internal patient surveys. Table 11 below also shows that we have improved in three out of the five bottom scoring items in the survey. Table 10: Top 5 scores Questions Did this person (health and social care worker) treat you with respect and dignity? Did this person listen carefully to you? Did this person take your views into account? Do you have trust and confidence in this person? Were you given a chance to express your views? 2011 2012 9.2 9.4 8.8 8.6 8.2 8.1 9 8.7 8.6 8.6 2011 2012 5.2 5 4.4 5.1 4.9 5.2 5.2 5.3 5.4 5.4 Change Table 11: Bottom 5 scores Questions In the last 12 months , have you received support in getting help with your care responsibilities? In the last 12 months , have you received support in getting help with finding or keeping work? Has anyone in the NHS mental health services ever asked you about your use of non-prescription drugs? In the last 12 months , have you received support in getting help with your physical health needs? Were you told about possible side effects of the medication? 3.1.4 Change Trust Inpatient Survey Inpatient survey data collection commenced on 26 January 2012. The inpatient survey consists of 19 questions that are taken from the national patient survey. This is shown below. At the end of March 2013, 2,655 questionnaires were completed with an overall satisfaction rating of 82% (January 2012 – March 2013). Trust inpatient survey questions 1 2. 3. 4. 5. 6. 7. 8. 9. When you arrived on the ward did the staff make you feel welcome? Do you feel safe during your stay? Do you have trust and confidence in our staff? Do you feel you are treated with respect and dignity by our staff? Are you involved as much as you want to be in decisions about your care and treatment? Do you know who your care coordinator or named nurse or lead professional is? Do you have a care plan? Do you understand what is in your care plan? Have you had a care review meeting to discuss your care? 10. Are the purposes of medication and treatments explained in a way you can understand? 11. Are there enough activities available for you?? 12. Do staff listen carefully to you? 13. How would you describe the food on the ward? 14. Have you been offered a choice of food at mealtimes? 15. Have you been offered support in finding or keeping accommodation? 16. Have you been offered support in finding or keeping work? 17. Have you been offered support in seeking help with financial advice or benefit? 18. How would you rate the care you receive? 19. How likely is it that you would recommend this Trust to your friends and family Page 43 of 74 Table 12: Top 5 scores Questions When you arrived on the ward did the staff make you feel welcome? Do you have a care plan? Have you been offered a choice of food at mealtimes? Do you have trust and confidence in our staff? Do you feel you are teated with respect and dignity by our staff? Q1 Q2 Q3 Q4 Overall 2012/13 96 96 95 91 92 96 96 94 91 92 98 95 95 95 94 97 97 94 90 92 97 96 94 92 92 Three of our top scoring areas are around the quality of the staff relationship with our patients which mirrors the results of our National Community Patient Survey. It is also worth noting that patients report highly around having a copy of their care plan. Examples of comments made by patients and carers are shown below. “I am writing to express our thanks and appreciation to CPFT. I am a mother of a 17 year old girl who has just been discharged from CPFT, having spent 5 years being treated for anorexia and depression, both as an outpatient and an inpatient. The care and support our daughter received was truly outstanding. We feel so fortunate to have received such support from dedicated professionals with years of specific experience in treating adolescents with eating disorders. We know from talking to parents of sufferers in other parts of the country how this level of expertise and experience is not common and yet it was vital to our daughter’s progress and to the wellbeing of the wider family. The critical factor in our daughter’s recovery has been the wisdom, skill and kindness of the staff in teaching both her and ourselves how to manage her condition.” “Thank you for listening to me, talking and comforting me after my bad dream yesterday. I would very much like to thank all of the nurses that have been working here looking after me. (name of staff) saved my life not directly but by talking to me and making himself approachable, like all staff have. I felt comfortable to go to him and tell him the thoughts I was having…I will always be grateful to the staff here for what they are doing for me and for others. Without knowing it you save lives by instilling the belief that we will get over our afflictions. I think when I am fully recovered and out of the army I will try to help those in a similar position because I see that it is a very important job that does not seem to get much recognition… “I can’t believe how well my dad has come out of your ward (Older people’s service). He was a very difficult patient and you have done wonders to put him on the road to recovery. Take care all and keep up the good work. Dad will miss you all.” “I wanted to thank you for the kindness and understanding you have shown (my son) who has had a lot of knockbacks in his life…His girlfriend and I are already seeing the old (name) who is kind and very comical. I realise we have such a long way to go, but you have made us very happy seeing (name) like this and not upset and angry.” Page 44 of 74 Comments received from (Meridian) patient surveys Staff attitude “The service from the team and the Trust has been fantastic and I cannot thank them enough for my care and treatment in helping me get through a very difficult time. The facilities and activities available are far more that I would have expected and I feel this is just as important or even more important in certain situations than the use of only drugs.” “The care staff have gone above and beyond anything that I could have expected, they are a very special kind of people.” Care planning I’ve been involved in my treatment more than I expected. I’ve been allowed to voice my opinion without feeling afraid or scared. I’ve been listened to and given very important advice for during and after treatment.” “Every decision has been made clear and I am thankful for that.” Food “Good food and friendly staff.” “High standards of food received whilst on the ward. Flexibility of visits by my family members.” Table 13: Bottom 5 scores Questions How likely is it that you would recommend this Trust to your friends and family? How would you describe the food on your ward? Have you been offered support in finding or keeping work? Have you been offered support in seeking help with financial advice or benefits? How would you rate the care you receive? Q1 Q2 Q3 Q4 Overall 2012/13 26 20 19 23 20 40 48 40 50 42 64 44 65 41 55 66 66 68 73 67 71 70 70 70 70 Table 13 above shows the specific areas that we need to focus on. It is worth noting that while our patients are happy with the choice of food, we need to work on improving the standard of the food on our wards. We have established a ‘Food Focus Group’ to drive up the standards and quality of the food on our wards. We are also working with our provider around improving the presentation of the food as well as the environments in which these are being served. We are also working on embedding recovery principles in our practice and services. The Recovery College East which was opened in November 2012 will enable people who use or have used secondary services from CPFT to develop new skills or increase their understanding of the mental health challenges that they have. Our Peer Support Worker programme also provides valuable support to our patients. We are leading on this initiative and have the most number of PSWs among similarly sized mental health Trusts. Our lowest scoring item in this survey is the Friends and Family test with an overall average score of 20%. This was our quality priority in 2012/13 and we are carrying this forward as our quality priority for 2013/14. Page 45 of 74 3.1.5 Trust Community Survey Community survey data collection commenced in April 2012. A phased roll out across all community teams was completed by the end of November. The survey consists of 14 questions which are shown below. 3,987 questionnaires were completed by the end of March 2013. The overall satisfaction rating was 90%. Trust community survey questions 1 Are staff polite and approachable? 2. Do you have trust and confidence in our staff? 3. Do you feel you are treated with respect and dignity by our staff? 4. Do staff listen carefully to you? 5. Are you involved as much as you want to be in decisions about your care and treatment? 6. Do you know who your care coordinator/therapist/key worker or lead professional is? 7. Do you have a plan of care/treatment/ therapy? 8. Do you understand what is in your plan of care/treatment/therapy? 9. Have you had a care review meeting to discuss your care/treatment/therapy? 10. Could you bring a friend, relative or advocate to your care review meeting? 11. Are the purposes of medication and treatments explained in a way you can understand? 12. Do you have the telephone number of someone from the Trust that you can phone out of office hours? 13. How would you rate the care/treatment/therapy/ activities you receive? 14. How likely is it that you would recommend this Trust to your friends and family? Table 14: Top 5 scores Questions Are staff polite and approachable? Do you feel you are treated with respect and dignity by our team? Do you have trust and confidence in our staff? Do staff listen carefully to you? Are you involved as much as you want to be in discussions about your care? Q1 Q2 Q3 Q4 Overall 2012/13 99 98 97 97 99 99 98 98 100 99 98 99 99 99 99 99 99 99 98 98 94 95 96 97 96 Examples of comments received from our community patients are shown below. Comments received from (Meridian) patient surveys Staff attitude “There is always someone at the other end of the phone if we need them. All our questions, no matter how silly we think they are, are always answered in a way that we understand. We are treated with respect. There is always somebody available to do a home visit when needed.” “Good rapport with support worker. Helpful and friendly advice.” “They have taken the time to understand who I am and help me understand my condition.” “Very helpful, friendly and understanding. Any concerns and necessary changes have been dealt with immediately. I am treated like a human being.” “Very good that I can talk to my care coordinator as though she is a friend and feel that I am treated as an equal.” “The consistency and professionalism of the service has made me feel valued and accepted and encouraged me to live as fulfilling a life as possible given the limitations of my long term mental health issues.” Care planning “Always given advice on what is more favourable but given the choice of deciding what I personally feel will be better. Very friendly and find it easy to talk to.” “All consultations have been on a regular basis and all disciplines involved Page 46 of 74 Table 15: Bottom 5 scores Questions How likely is it that you would recommend this Trust to your friends and family? Do you have the telephone number of someone from the Trust that you can phone out of office hours? How would you rate the care/treatment/therapy/activities you receive? Have you had a care review meeting to discuss your care/treatment/therapy? Could you bring a friend, relative or advocate to your care review meeting? Q1 Q2 Q3 Q4 Overall 2012/13 53 65 62 60 61 77 77 76 77 77 78 82 83 84 82 87 82 82 82 83 88 89 88 88 88 Four out of the five top scoring items refer to staff attitude and the quality of their relationship with our patients, while the fifth one pertains to the quality of the patient’s involvement in planning their care, treatment and support. These results mirror our national and inpatient survey results and reflects the work that we have done around the 7Cs care planning standards and the improvement in collaborative practice with patients in the care planning process (see section 3.3.1). Our bottom five scores also appear to mirror the results of our inpatient survey results. It is worth noting however that the scores for the Friends and Family test are higher than the Trust target of 30% (see quality priority 1 in section 1.2.1). The introduction of the ARC (Advice and Referral Centre) will address the issue around out of hours contact. Likewise, we expect that the restructuring of our community services and development of Care Pathway teams will have a positive impact on the quality of care provided. Page 47 of 74 3.2 PATIENT SAFETY Our performance in 2012/13 on patient safety quality indicators (i.e., suicide prevention, physical assaults and absconsions, patient safety incidents and mandatory training including safeguarding children and adults training) have been discussed in previous sections of this Quality Report. Additional quality indicators are outlined below. 3.2.1 Reducing Healthcare Associated Infections (HCAIs) The Trust remains committed to ensuring patients receive care in clean and safe environments. During the year we continued to build on the measures put in place in order to support good practice and reduce the risk of infection. Training figures are produced by the Learning and Development team from ESR and LMS (see section 1.2.3), and are reported through our quality dashboard. The e-learning training programme which runs alongside the face-to-face training helps to ensure that staff maintain their knowledge and skills in the control and prevention of infection. We have made significant improvements in training as compared to the previous year as shown in Chart 15. Chart 15: Infection Prevention & Control Training HCAI incidents in 2012/13 1 incident of C Difficile in 2012/13 which is the same as the previous year. This was investigated fully through our SI process 2 closures of wards due to diarrhoea and/or vomiting (3 closures in 2011/12). The protocol was followed thereby ensuring the safest care for our patients and staff One ward had two separate episodes of scabies (none in the previous year) . 3.2.2 MRSA Screening Assessing for MRSA screening is a national requirement for mental health providers since 2011. 100% of patients admitted into our wards need to be assessed for MRSA screening, and those who fit into higher risk categories are offered swabs. We have made huge improvements in 2012/13 and compliance level is much improved as shown in Chart 16. This is monitored through the quarterly Patient Safety Thermometer returns (see CQUIN goal 1, section 2.4) and reported through our quality dashboard. Actions we have taken/are taking to ensure consistent achievement of the target include: continued provision of Infection control training identification of Infection Control leads/link workers in each service monthly reminders to ward managers, link workers and modern matrons Chart 16: MRSA screening Page 48 of 74 3.2.3 Pressure Ulcers (PUs) Chart 17 shows the number of PUs reported in Datix, our electronic incident reporting system, during the year. Of the four reported that were attributable to the Trust, two were grade 2, one was grade 3 and another one was a grade 4 PU. The increase in cases reported is most likely due to improved level of awareness regarding pressure ulcers and care of the skin. Other examples of good practice Chart 17: Incidence of Pressure Ulcers reported via Datix that are in place are listed below. Modern Matron for Infection Prevention & Control identified as dedicated Trust lead for PUs. Use of NICE Guidance (CG29, 2005) and the European Pressure Ulcer Advisory Panel (EPUAP) guidance Information resources available on PU page on the Trust intranet for staff Use of the Waterlow assessment tool as part of the physical examination on admission Reporting and investigation of all PUs through Datix, our incident reporting system. In accordance with national guidance, any pressure ulcers of grades 3 or 4 are treated as a Serious Incident. All actions resulting from investigations have been completed. 3.2.4 NHSLA The NHS Litigation Authority handles negligence claims and works to improve risk management practices in the NHS. The Trust achieved Level 2 accreditation in February 2011. The Level 3 assessment was originally scheduled in February 2014. This has been moved to February 2015 by NHSLA following a review of their standards and assessment process. An action plan is in place to help us prepare for the Level 3 assessment. 3.3 CLINICAL EFFECTIVENESS 3.3.1 Care Planning Care planning is an on-going quality priority of the Trust. In 2010/11, our priority was to ensure that 95% of our patients have a care plan and we consistently met this target over the last three years (see section 1.3). In 2012/13, we shifted our focus on improving the quality of our care plans (see section 1.2.1). We developed the 7Cs standards, which are based on Outcome 4 and 6 of the CQC standards, to clearly define the standards expected of our care plans and implemented a process of monthly self and peer assessments. The scores are reported through our quality dashboards and performance management framework. The 7Cs standards are grouped under the following main headings: Crisis/contingency Comprehensive and cross-checked Carried out Collaborative Carers and care for Clear and concise Choices The standards are used to assess the quality of the care plans and include a section for patients and/or their carers where appropriate to give feedback on their views about their care plan and their involvement in planning and reviewing their care. Page 49 of 74 Our work on improving the quality of our care plans contributed towards achieving compliance with the CQC standards and improvement in our 2012 national patient survey scores, with the section on ‘care plans’ showing the largest improvement. The results for this section in the survey, taken from the CQC website and is presented below, shows we scored higher than the national average around patients understanding their care plan. This was acknowledged by our CQC assessors who praised the improvements we have made in the quality of our care plans during the year. Comparative scores are also shown in Table 16 below. CQC, National Community Patient Survey 2012 Table 16: Comparative scores for care planning (CQC Community patient survey 2011 & 2012) Questions Do you understand what is in your NHS care plan? Do you think your views were taken into account when deciding what was in your NHS care plan? Does your NHS care plan set our your goals? Have the NHS mental health services helped you start achieving these goals? Does your NHS care plan cover what you should do if you have a crisis? Have you been given (or offered) a written or printed copy of your NHS care plan? 2011 2012 6.6 7.7 6.8 7.5 6.0 6.6 6.6 6.8 6.6 6.7 6.9 7.8 Change Actions for further improvement We aim to further improve our practice and monitoring arrangements around care planning in 2013/14. This includes: reviewing the questions around care planning in our inpatient and community patient surveys. We will adapt the questions around the specific needs and requirements of individual services and patient groups. reviewing our guidelines and policy around care planning to strengthen the links with NICE guidelines and recovery principles. rolling out a consistent care plan template through RiO, our electronic patients records system. Page 50 of 74 3.3.2 Breastfeeding Our community children’s services were under their targets for breastfeeding at the end of 2012/13 as shown in Table 17. Data is collected though SystmOne (our electronic clinical records system) and is monitored and reported though our quality dashboard. Table 17: Breastfeeding targets and performance Performance Breast Feeding NI 53 (VSB 11) Prevalence of breastfeeding (totally plus partially) at 6-8 weeks from birth (%) NI 53 (VSB 11) Percentage of infants for whom breastfeeding status is recorded at 6-8 weeks from birth (%) Target 2011/12 Target 2012/13 March 2012 March 2013 48% 48% 44.5% 38.39% No target set 95% 92.0% 93% As a Trust we have strongly disputed the target which has been set in regard to breast feeding prevalence within Peterborough. This is for two principal reasons, firstly the target does not take account of the rapidly changing population and demographics of Peterborough which would indicate reducing prevalence rates given that no new services have been commissioned in this area. Equally, given the service we provide in this area (Health Visiting), we have very limited scope to affect this performance given the dependency that we have from other commissioned services such as community midwifery and maternity services and in the absence of other support services such as baby cafes. However, we remain committed to continually improving the effectiveness of our health visiting services through active participation in a range of programmes such as UNICEF (United Nations Children’s Fund) Baby Friendly Accreditation, but remain in active debate with our commissioners to establish an appropriate measure to indicate the support we provide to new mothers on breast feeding. 3.3.3 Participation in National Quality Improvement Programmes National quality accreditation schemes provide a way of assessing the quality of our services and comparing our performance with other Trusts across the country. They provide assurance that our services are meeting the highest standards set by the professional bodies, and also provides us with a framework for quality improvement. During 2012/13, CPFT participated in the four accreditation schemes run by the Royal College of Psychiatrists. This is shown in Table 18 in the following page. Page 51 of 74 Table 18: Accreditation Schemes by CPFT Accreditation Services Scheme ECTAS (ECT Accreditation Service) AIMS (Accreditation for Inpatient Mental Health Services) QNIC (Quality Network for Inpatient CAMH) PLAN (Psychiatric Liaison Accreditation Network) Current status Addenbrookes ECT Clinic, Cambridge Accredited Cavell Centre, Peterborough Accredited Oak 2 Ward, Cavell Centre, Peterborough (Adults unit) Accredited Oak 1 Ward, Cavell Centre, Peterborough (Adults unit) Accredited Friends Ward, Fulbourn, Cambridge (Adults unit) Deferred (currently closed for refurbishment IASS, Ida Darwin, Cambridge (Learning Disability unit) Accredited Hollies Ward, Cavell Centre, Peterborough (Learning Disability unit) Accredited The Croft, Ida Darwin, Cambridge (Children's unit) Accredited Darwin Centre, Ida Darwin, Cambridge (Children's unit) Accredited Addenbrookes, Cambridge Accredited Page 52 of 74 4.0 PERFORMANCE AGAINST KEY NATIONAL PRIORITIES The Trust is required to achieve a number of key national priorities as outlined within the Department of Health Operating Framework. The Trust continues to perform well against these targets in 2012/13 as shown below. Table 19: Key national priorities Target(%) Target 2011/12 Target 2012/13 2011/12 2012/13 100% 100% 100% 95% 99.60% 95.99% <= 7.5% 1.42% 2.30% 95% 100% 100% 97% 50% 99% 72% 98.81% 86.32% LOCAL TARGET Service users seen within 18 weeks (CPFT target) 100% NATIONAL TARGETS CPA patients having formal review within 12 95% months Minimising delayed transfers of care <= 7.5% Meeting commitment to serve new psychosis 95% cases by early intervention teams Data completeness: identifiers 99% Data completeness: outcomes 50% Data completeness: Community services referral to treatment information Referral information Treatment activity information Patient identifier information Self-certification against compliance with No requirements regarding access to healthcare for threshold people with a learning disability set MRSA Infection rate (per 1000 bed days) 0.60 C.Difficile Infection Rate (per 1000 bed days) 0.70 Data has been sourced from the clinical records system 50% 100% 50% 50% 50% No threshold set 0.00 0.00 98.9% 99.6% 97.6% Met Met 0.00 0.01 0.00 0.0001 Notes: Please note that data for the following have already been presented in section 2.8 under the mandatory core set of quality indicators for 2012/13: Patients on Care Programme Approach who were followed up within 7 days following discharge from psychiatric inpatient care during the reporting period Admissions to acute wards for which the Crisis Resolution Home Treatment Team acted as a gatekeeper during the reporting period. . Page 53 of 74 5.0 HIGH QUALITY WORKFORCE 5.1 Workforce Factors Research evidence from the NHS has shown that higher levels of staff engagement are linked to: overall measures of financial effectiveness lower levels of absence improved levels of patient satisfaction High quality patient care is therefore strongly associated with a highly skilled and motivated workforce. As a consequence, the Trust’s Workforce Strategy is currently being developed around four key themes that will enable effective staff engagement: The four key themes and key performance indicators (KPI’s) for our workforce strategy are as follows: Theme Definition Target Outcome Productivity Maximising the contribution of every CPFT staff members to patient care 75% of our substantive staff productivity deployed at any one time Safe establishments on Ward and Community Teams engAgement Every member of staff will be involved with, committed to and satisfied with their work for CPFT 60% staff to recommend CPFT to family and friends 60% of staff state they have the ability to make the changes necessary for excellent patient care Every CPFT staff member will have the knowledge, skills and attitudes to perform to the required performance standards Vacancy rates across CPFT are less than 5% 95% of staff will receive appropriate training relevant to their job role, including Governance All Band 7 and 8A’s will have completed an appropriate leadership Development Programme 95% of staff receiving appraisal and competency review Our key workforce processes will be slick and efficient Recruitment ‘Time to Fill’ < 12 weeks currently 16 weeks Discipline Cycle Time < 63 days currently 113 days Sickness and Capability cycle time will be reduced by 20% Capability Efficiency Page 54 of 74 5.2 Staff Survey The 2012 National Staff Survey was completed by 1185 members of staff between October – December 2011, a sample of which (441) was used by the Department of Health to report and directly compare our organisation to other Mental Health and Learning Disability organisations. The findings for the 2012 National Staff Survey puts the Trust in the lowest (worst) 20% for overall staff engagement when compared with Trusts of a similar type. The areas the Trust performed well in and are the weakest areas are detailed in Tables 20 and 21 below. Table 20: CPFT’s top 5 ranking scores Key Finding Description % of staff having equality and diversity training in last 12 months % of staff receiving health and safety training in last 12 months 26 10 7 4 % of staff appraised in last 12 months Effective team working % of staff experiencing harassment, bullying or abuse from patients, relatives or the public in last 12 months 18 Threshold 2012 score 77% Higher the better Lower the better 84% 2011 score National Average for MH & LD Trusts (2012) 59% 74% 73% 86% 91% 3.87 82% 3.94 87% 3.83 30% n/a 30% 2012 score 2011 score National Average for MH and LD Trusts (2012) 68% 70% 78% 3.34 3.37 3.52 3.06 3.30 3.54 52% 28% 41% 3.23 n/a 3.02 Table 21: CPFT’s top 5 ranking scores Key Finding 1 15 24 11 3 Description % of staff feeling satisfied with the quality of work and patient care they are able to deliver Fairness and effectiveness of incident reporting procedures Staff recommendation of the Trust as a place to work of receive treatment % of staff suffering work-related stress in last 12 months Work Pressure felt by staff Threshold Higher the better Lower the better The Trust will undertake the following actions in response to the survey findings: Undertake a thorough analysis of questions as well as key findings. Complete analysis for Divisions, Occupational Groups and Demographical Profile of respondents. Review against current objectives and priorities already in place as part of the Trust’s Strategic Objectives. Develop a communications plan around the results and engage with the Trust in developing an action plan to improve staff experience. This phase is called the ‘Big Conversation’. Achieve feedback from the Executive Team around priority focus going forward. Create an Action Plan involving representatives from the whole organisation. Focus on staff engagement. Develop workforce strategy in liaison with staff. Page 55 of 74 5.3 An Effective Healthcare Organisation The Trust has robust workforce policies in place to ensure staff are safely recruited, inducted, supervised and appraised and provide a minimum standard. The policies are monitored to ensure managers and staff are compliant with these standards Mandatory Training compliance is monitored on a monthly basis as well as being included on the monthly Quality Dashboard which is reported corporately to demonstrate compliance. In 2012 the new Performance Management Framework Appraisal System was launched. This includes a competency framework for staff performance, enabling a simpler and consistent approach to individual assessment and a clearer overview of the overall workforce performance. This rates staff performance on a ranking scale of between 1 and 5 and will feed into future Talent Management and Performance Management processes. The system includes a validation process and appeals process, for consistency and fairness. Feedback collected on the new system has enabled further development to take place ready for the 2013 Appraisal launch in May. The Trusts updated governance structure includes the Workforce Executive, which includes Executive Directors and Divisional Managers and reports to the Board on a number of workforce issues. A review of workforce data takes place on a monthly basis at high level performance meetings. This workforce KPI’s are triangulated with patient safety and experience KPI’s to highlight areas of concern for action. Stop the line is an initiative which was launched in February 2013, and is where any member of staff can raise an objection and literally stop something that is happening in order to prevent a mistake from being made. It creates a safe environment for any member of staff to report an unacceptable risk or when a harmful incident happens that seems to go unnoticed or is not being taken seriously enough. From the report the Stop the Line Hub alerts the Senior Manager and Executive Director to take action. In response to the recommendations from the Francis Report (Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry, February 2013) all new job descriptions will include a requirement for staff to be able to demonstrate care and compassion in their work, and this will be monitored through our appraisal system and revised appraisal forms. 5.4 Planning and Developing the Workforce A revised establishment control process has been implemented. Forms are completed, including a risk assessment and final approval is required from Human Resources (HR) before adverts are placed. In response to the recommendations from the Francis Report (Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry, February 2013) all changes to nursing posts and clinical establishments must be signed off by the Director of Nursing and Director of Finance for final approval. , A robust recruitment procedure is in place to ensure new staff are safe to work and this complies with all the national recruitment standards which include appropriate pre employment checks. A co-ordinated approach to filling vacancies is underway, to reduce risks associated with vacant positions and also increase consistency across the Trust. All staff are fully inducted corporately and locally when they commence and this includes ensuring they complete the appropriate mandatory training to ensure they are safe to practice. Robust monitoring is in place to ensure our compliance. Checks are in place to ensure appropriate CRBs (Criminal Records Bureau) are in place and professional registrations are up to date. A robust workforce plan was developed to support the activity plans within the Trust business plans for the last year. This included staff changes affected by service transformation, changes to service provision and subsequent consultations. This will be Page 56 of 74 reviewed annually to ensure it reflects changes to Trust plans and activities. A training needs analysis (TNA) has been completed and this will inform future training plans. The TNA was also commended by NHSLA (NHS Litigation Authority) at the last assessment as an example of good practice nationally. 5.5 Staff Engagement Feedback from All Staff Events supported the Trust in developing four Quality Priorities to support the Trust in achieving our vision. Staff Engagement is one of the four priorities and can be seen on the Quality Diamond Strategy in Section 1.1 and Annex 1. Regular communications are provided to staff via weekly staff news emails and direct emails from the Chief Executive. Staff have opportunities to directly feedback to the Chief Executive and other Directors through the monthly Live ‘Webex’ chat and the ‘Back to the Floor’ initiative. An excerpt from the CQC report below shows that staff value these initiatives. “Staff told us of the many changes that had taken place at the trust recently and of the extra work that implementing the various quality initiatives to improve people's care had entailed. However they clearly appreciated the many benefits this had brought to people and were keen to continue the improvements and incorporate them into their everyday ward routines. One staff member told us about the 'Ask Attila' initiative, whereby staff could email their concerns and questions directly to the trust's chief executive (Attila Vegh) and that they had done so and received a good response from him. Another staff member told us that visits to the ward from the trust's directors had, as this staff member described, "been resurrected", making the directors much more "visible and approachable" for staff. A number of staff told us they felt that there was a lot more openness from senior managers in the trust and that lines of communication with them had improved significantly within recent months. This had resulted in staff feeling more confident that their concerns would be taken seriously. One staff member commented, "There's shorter distance between here and the top" and another reported, "Things get done a lot quicker now". CQC report, July 2012 (pg 14/15)) The Trust’s Guiding Coalition forum which was set up in January 2012 comprised of 80 members of Trust staff from across all areas, bands and disciplines. Meetings on a regular basis in 2012, the forum gathered feedback from staff on Trust direction, actions and plans as well as led various projects around the Trust in improving the patient and staff experience. An increased number of staff responded to the 2012 Staff Survey (60.24%). Whilst the challenges of turning the organisation around have affected staff engagement, with a lower than average score of 3.48 (out of 5) it’s positive that an increased number of staff took the time to feedback. The Trust takes the feedback from staff very seriously and feel strategic action plans already in place will support in achieving increased staff engagement. Staff are being invited to be part of the ‘Big Conversation’ which will look at the draft Workforce Strategy and make improvements. As part of the Trust performance reports we monitor sickness absence (the Trust’s KPI is 4.35%). In 2012, the Trust sickness rate has averaged at 4.17%. Reward and recognition schemes have been developed through 2012, where staff can be nominated and awarded monthly Quality Hero Awards for individuals and teams as well as the annual Staff Awards. The first annual event was held in February 2013 and included 8 awards as well as the long service awards. All nominees and winners were invited to the black tie celebration event. Page 57 of 74 5.6 Health & Wellbeing One of CPFT’s key values is “Our staff matter – we trust, value and develop each other. We build a great place to work, where people are inspired to be the best they can be.” In accordance with CPFT’s vision and values in all our policies and procedures, it is outlined and acknowledged that staff wellbeing is of paramount importance. Wellbeing is an important factor in the job satisfaction of our staff and is therefore a management issue for the organisation. Following feedback from staff at the Town Hall Events in June 2012 and the results of the 2011 Staff Survey, a Health and Wellbeing Strategy has been designed to bring existing staff wellbeing issues to the forefront, whilst seeking to create an organisational culture where negative wellbeing issues are identified, minimised and managed before they affect the wellbeing of staff. We have a clear aim to promote the positive aspects and ideas associated with health and wellbeing at work. The CPFT Health and Wellbeing Strategy aims to embed a positive health and wellbeing culture for all staff and that this is underpinned in the Trust’s policies and procedures, including through appraisal, supervision and learning and development programmes. It aims to: Reduce sickness absence by improving the services available to staff for their mental health Reduce pressure felt by staff and effectively manage stress levels Reduce the number incidents of staff affected by violence and bullying/harassment via a Zero Tolerance Policy Provide better access to health and wellbeing activities and facilities We have also developed a ‘Mindfulness for the Health and Social Care’ course which is based around the widely researched clinical approach to teaching mindfulness – ‘mindfulness based cognitive therapy’ (MBCT). The Trust expect to achieve the East of England’s aSHAWed accreditation in Spring 2013. They have also signed up to the National Responsibility Deal for Health and wellbeing in the workplace. 5.7 Leadership Following the previous changes to the Executive Leadership team and the Trust’s turnaround agenda the leadership development for the Trust has been reviewed. A new Leadership Development programme will be launched in the Summer 2013. As well as the active engagement and hosting of the Festival of Leadership for the 3rd year in 2012, which supported managers and clinical staff build their knowledge and skills around various leadership qualities. HR skills modules are in place to provide managers with the appropriate management skills to support them in their roles and specific leadership and management competencies are included in the performance management framework to support the development of managers and leaders across the Trust. As the Trust’s Academy is developed, further leadership development opportunities will be available in Summer 2013. 5.8 Empowering Staff The Trust’s Staff Consultative forum is the formal mechanism for consulting, liaising and negotiating with staff side colleagues and trade unions. Consultations, staff developments and employment policy development and changes are consulted on with staff side. Page 58 of 74 In 2012 the Trust developed a Guiding Coalition which met regularly and provided a mechanism for discussion and feedback with staff from across the Trust. The Trust also continues to engage with staff and through the all staff meetings which take place biannually. Fed-ex is a scheme which was launched in 2012 to support staff to make change happen, by giving them a full day and £200 budget to work on an initiative which improves patient or staff experience. Much of the engagement strategy is built around empowering staff to make changes, be heard and improve the services they provide. Page 59 of 74 ANNEX 1 SUMMARY OF QUALITY DIAMOND STRATEGY What we will do Rationale Culture of quality We want a culture of quality that goes way beyond the CQC essential standards where regular monitoring against quality and safety standards becomes part of our day to day practice. We will use new systems such as the InCA tool to ensure we keep improving our practice, our systems and process and the environment. . Achieving and maintaining full compliance with the CQC and other quality standards will help us to ensure that we continue to provide the very best care possible that we will be proud of and that we are happy for our friends and family to receive. Stop the line This initiative was launched in February 2013 and will enable CPFT staff to 'stop the line' whenever they see something that poses a risk to patient or staff safety or the quality of care. Immediate action will be taken and reported upon when 'stop the line' incidents are raised. Learning will be disseminated Trust wide and unannounced inspections will take place to ensure identified actions have been put in place. We believe that most serious safety events can be prevented if more decisive actions are taken at the time of or leading up to the event. This aims to create a safe environment for any member of staff to report an unacceptable risk or harmful incident they think is not being taken seriously enough. How are we doing? Every clinical team will have a Quality Dashboard by March 2013 to show how they are doing at giving patients safe, effective treatment; at making sure their experience is a good one, at looking after the needs of staff and at using our resources sensibly. We will also introduce 'risk cards' to report and manage risks openly and efficiently. Providing accurate, relevant, meaningful and timely information about the quality of their practice and service will enable staff and teams to act in a timely manner to improve services. It will also help them to demonstrate how well they are doing as a service to their patients, fellow staff, visitors and other stakeholders. No hotspots OBJECTIVE 1: To be top 5 in patient safety We will reduce the number and severity of adverse events and serious incidents by noticing when there are hotspots of risk, finding out why and putting thing right. We will focus on areas of unacceptable risks and harmful events and improve the process for investigation of serious incidents and dissemination of learning. We acknowledge that there are still areas in our service where risks to patient safety and harmful incidents still exist. By identifying and focusing on hotspots, we can focus our efforts and resources to eradicate these in order to improve the environment of safety in our services. Indicators where available 95% compliance with 7Cs standards 95% compliance with InCA standards No conditions in our CQC registration status Agreed targets in the Quality Dashboard. reduction in adverse events and serious incidents Children’s community services will meet 18 week waiting time targets Clinical Effectiveness OBJECTIVE 2: To be top 5 in patient experience Rationale Put patients first We will reorganise our services and develop diagnosis, problem and need-based pathways that are based on the evidence of best practice to be delivered by specialists in that area. We will create a single point of access by opening our Advice and Referral Centre (ARC) to all GPs, patients and partners. Diagnosis and needs-based services ensures that patients don’t have to move between services when they reach a certain age and eliminates the risk of falling between the gaps. Having staff with the right skills also ensures that the best and clinically effective care is provided with the best possible outcomes of care. Right staff for the right amount of work We will ensure that our staffing levels are based on international research into patient care and staff requirements. Work to determine safe and effective staffing levels was concluded in December 2012, and will take account of patient acuity and referral patterns. We will reduce our bank and agency staff usage to less than 5%. The delivery of good quality care is dependent upon having the right number of appropriately skilled staff. Ensuring adequate staffing levels will help us ensure we provide the best quality care for our patients. Reduce bank and agency staff usage to less than 5% In your shoes We will use new ways to listen to our patients. Initiatives include using iPads to collect feedback about our services. Results will be published and combined with other information to help us shape our services. We will also link with social care and other partner organisations to deliver seamless care. We believe that listening to our patents and their carers and giving them more involvement in decision about their care will help us to change and develop our services. Collecting and sharing meaningful qualitative information from patient feedback in a timely manner will also help teams to keep improving their services. Patient survey scores as reported in Divisional quality dashboards Recovery & integration Indicators where available What we will do We will continue to increase and strengthen the role of peer support workers and maintain our national leading position in this area. We opened our Recovery College East in November 2012 – the first in the region - which will deliver unique peer-led training in recovery. We will deliver a new social care strategy and appoint a new Director of Service Integration to improve the way we provide support, recovery, education, employment and financial advice to our patients. We believe that giving our patients and their carers more control over how their care and treatment will be delivered will help us to shape our services and deliver responsive and personalised care. By empowering them to express their choice and preferences, we can help them to direct their care, maintain their recovery and promote their independence. Clinical Effectiveness Page 61 of 74 Rationale We will implement RiO to help make keeping electronic records more efficient, use of iPads to help community teams access and create patient records remotely, develop standardised and service-specific templates to deliver personalised care, review our record keeping and records management processes to ensure we support patient care in the most effective and efficient way. We will train our staff to become IT literate. Freeing up staff time spent on administrative tasks will create more time to spend with patients. Developing a fit for purpose electronic record keeping system and streamlining our processes around managing health records will help create an efficient and effective service that is aimed towards helping staff to spend more time with patients. Beyond the carrot & CPFT Academy stick The CPFT Academy will provide our staff with decision making and leadership skills to ensure that they have the skills and competencies to do their job as best as they can. It will help staff to deliver good quality care, learn how to understand and investigate risks and problems, plan new innovative services and measure results and outcomes of care competently. By developing our staff and providing them with opportunities for personal and professional development, we will make sure that they have the right and up to date knowledge and are capable of making the right decisions when it comes to managing their teams and their services. We will recognise and reward good performance based on their merits – initiatives include the ‘Quality Heroes’ and ‘Team Champions’. We celebrated our very first Annual Staff Awards in February to recognise the outstanding achievements of our staff. We will strive to attain effective and meaningful staff appraisals that will recognise good practice and also help staff improve areas that need further development. We believe that hard work and success need to be acknowledged and rewarded fairly. This helps to create a motivated and committed workforce which contributes to the success of our organisation. Hence we will reward staff achievement and provide open and honest feedback to developed engaged staff that will help us to meet our objectives and priorities. We will listen to our staff and give them the opportunity to help shape our vision and direction as an organisation. We will continue to have Town Hall events to ensure staff are informed of new developments and enabled to give feedback in a safe environment. We will continue to support the Guiding Coalition to deliver changes to our services. In 2012, we introduced various initiatives to encourage open communication between the management team and our staff. Sharing information with staff in an open and timely manner and providing them with opportunities to ask questions and express their views in a safe environment will encourage engagement and ownership, which are essential ingredients of successful organisations. More time with patients What we will do Taking staff seriously OBJECTIVE 3: To be top 5 in staff engagement Indicators where available Clinical Effectiveness Page 62 of 74 OBJECTIVE 4: To be top 5 in value for money Frontline first Attack waste Reducing the money spent on management and non-clinical overheads will enable us to increase the proportion of money spent on clinical services that will lead to better care and outcomes for the people who use our services. We have reduced the money spent on management by reducing our Clinical Divisions from five to three, and the money spent on non-clinical overheads such as finance, HR and performance. We also commit to reducing the time for recruitment from 94 to 62 days, and we will double the number of volunteers within the Trust. We will reduce the cost of business travel by £400,000 Reducing our overhead costs will mean that a year and our legal fees by a further £100,000. We we are able to spend more money on patient will also reduce our printing costs and find other ways of care and save jobs. saving money. Buy smarter Rationale We will get the best value for our money on products and services and overall, work to save money in all the areas where saving money does not make a negative impact on patient care. We have started this work by asking our suppliers to give us an initial 5% discount on their current charges. The same as above. A workplace fir for work What we will do We will ensure that all of our wards will meet the 5 star environmental standards and ensure that maintenance works are done quickly. We have launched our ‘warm reception’ programme and will improve staff facilities. We will also review and improve all our community facilities and build a workplace that is fit for a top 5 Trust. Improving the working environment will show that we value our staff and our commitment to their wellbeing which will, in turn, improve morale, performance and productivity. Indicators where available Clinical Effectiveness Reduce business travel by £400,00 Reduce legal fees by £100,000 Page 63 of 74 Annex 2 DEFINITIONS OF KEY NATIONAL QUALITY INDICATORS 1. The proportion of those patients on Care Programme Approach (CPA) discharged from inpatient care who are followed up within 7 days. Data definition ‘Patients discharged’ includes all patients discharged to their place of residence, care home, residential accommodation, or to non psychiatric care or to prison. All avenues need to be exploited to ensure patients are followed up within 7 days of discharge. Where a patient has been discharged to prison, contact should be made via the prison in-reach team. CPFT adapted definition The indicator excludes patients who are readmitted within 7 days transferred to other wards (patients transferred to NHS psychiatric inpatient ward when discharged from inpatient care) discharged to other hospitals discharged to Alcohol Service/Bridge Alcohol Team/Drink Sense discharged to GPs discharged to Out of Area Learning Difficulties discharged to Community Alcohol Team CAT/Community Drug Team/Add Action. of no fixed abode discharged to the Prison Service die within 7 days of discharge patients removed from the country as a result of legal precedence: and CAMHS (children and adolescent mental health services), i.e. patients aged under 18. Those that are recorded as followed up receive face to face contact or a telephone conversation (not text or phone messages). The 7 day period is measured in days not hours and starts on the day after discharge Accountability Achieving at least 95% rate of patients followed up after discharge each quarter. 2. The proportion of inpatient admissions gatekept by the crisis resolution home treatment teams. Data definition Gatekeeping: In order to prevent hospital admission and give support to informal carers CRHT are required to gatekeep all admission to psychiatric inpatient wards and facilitate early discharge of service users. An admission has been gatekept by a crisis resolution team if they have assessed the service user before admission and if the crisis resolution team was involved in the decision making-process, which resulted in an admission. CPFT adapted definition The indicator is expressed as proportion of inpatient admissions gatekept by the crisis resolution home treatment teams in the year ended 31 March 2013. The indicator is expressed as a percentage of all admissions to psychiatric inpatient wards. The following patients are excluded from the indicator: patients recalled on Community Treatment Order, patients transferred from another NHS hospital for psychiatric treatment, Internal transfers of patients between wards in the Trust for psychiatric treatment, patients on leave under Section 17 or come under section 136 of the Mental Health Act, patients who are sections under s.2 or s.3 of the MHA Ministry of Defense (MoD) patients, planned admissions to detox beds, and planned admission for psychiatric care from specialist units such as eating disorder unit. An admission is reported as gatekept by a crisis resolution team where they have assessed* the service user before admission and if the crisis resolution team were involved** in the decisionmaking process which resulted in an admission. Notes: 1. An assessment should be recorded if there is direct contact between a member of the team and the referred patient, irrespective of the setting, and an assessment made. The assessment may be made via a phone conversation or by any face-to-face contact with the patient. 2. Involvement is the assessment of all patients thought to be requiring admission other than those detained under the Mental health Act., although seen out of hours between 10.00pm – 08.00am 3. Where the admission is from out of the Trust's area and where the patient was seen by the local crisis team (out of area) and only admitted to this Trust because they had no available beds in the local areas, the admission is recorded as gatekept if the CR team assure themselves that gatekeeping was carried out. 3. Patient safety incidents reported Indicator description Patient safety incidents (PSI), reported to the National Reporting and Learning Service (NRLS), is defined as ‘any unintended or unexpected incident(s) that could or did lead to harm for one of more person(s) receiving NHS funded healthcare’. CPFT adapted definition The Trust also uses the criteria of 'suffered long term harm' to classify an incident as severe, as well as 'permanently harmed'. Indicator construction The number of incidents as described above. Indicator format Whole number. 4. Safety incidents involving severe harm or death Indicator description: Patient safety incidents reported to the National Reporting and Learning Service (NRLS), where degree of harm is recorded as ‘severe harm’ or ‘death’, as a percentage of all patient safety incidents reported. Indicator construction Numerator: The number of patient safety incidents recorded as causing severe harm /death as described above. The ‘degree of harm’ for PSIs is defined as follows; ‘severe’ – the patient has been permanently harmed as a result of the PSI, and ‘death’ – the PSI has resulted in the death of the patient. Denominator: The number of patient safety incidents reported to the National Reporting and Learning Service (NRLS). Indicator format: Standard percentage. Page 65 of 74 5. The number of Delayed Transfers of Care per 100,000 population (all adults – aged 18 plus). Data Definition A delayed transfer of care occurs when a patient is ready for transfer from a hospital bed, but is still occupying such a bed. A patient is ready for transfer when: a clinical decision has been made that the patient is ready for transfer AND a multi-disciplinary team decision has been made that the patient is ready for transfer AND the patient is safe to discharge/transfer. To be effective, the measure must apply to acute beds, and to non-acute and mental health beds. If one category of beds is excluded, the risk is that patients will be relocated to one of the ‘excluded’ beds rather than be discharged. Accountability The ambition is to maintain the lowest possible rate of delayed transfers of care. Good performance is demonstrated by a consistently low rate over time, and/or by a decreasing rate. Poor performance is characterised by a high rate, and/or by an increase in rate. (Monitor 2012/13 Detailed Guidance for External Assurance for External Reports) Page 66 of 74 Annex 3 STATEMENTS FROM CLINICAL COMMISSIONING GROUP, LOCAL HEALTHWATCH and OVERVIEW AND SCRUTINY COMMITTEE Statement for inclusion in 2012/13 Quality Account for CPFT 21 May 2013 Cambridgeshire and Peterborough Clinical Commissioning Group (the CCG) has reviewed the Quality Account produced by Cambridgeshire and Peterborough NHS Foundation Trust (CPFT) for 2012/13. The CCG and CPFT work closely together to review performance against quality indicators and ensure any concerns are addressed. There is a structure of regular meetings in place between the CCG, CPFT and other appropriate stakeholders to ensure the quality of CPFT services is reviewed continuously with the commissioner throughout the year. In addition, the CCG has carried out announced and unannounced visits to CPFT to observe practice and talk to staff and patients about quality of care, feeding back any concerns and actions required by the Trust. The Trust are required to develop annual Cost Improvement Plans (CIPs) focusing on service redesign, whilst maintaining quality of services. The CCG look to review the CIPs so that a quality impact evaluation of the potential effect on front-line service delivery can be made During 2012/13 the commissioners had to use a range of contract mechanisms to obtain information, and a similar situation is now occurring for the 2013/14 CIPs. The lack of financial transparency as to future CIPs and how they might impact on service quality remains a major concern for the CCG and will be pursued through the range of channels available. CPFT has safeguarding systems in place to ensure both children and vulnerable adults are protected from harm. The CCG had concerns about the level of safeguarding training in the Trust in 2012/13, and has worked with all providers to develop a CCG Safeguarding Training Strategy which makes explicit the framework required for safeguarding systems. The CCG will be seeking a higher degree of clarity about safeguarding training delivered to staff in 2013/14 to ensure it is commensurate with their role. The CCG monitor all trusts’ Serious Incident investigation processes to ensure investigations are carried out in a timely and robust way and learning is taken forward and embedded. CPFT has reviewed how clinical risk assessments are undertaken as part of the care planning process and are working through an action plan for improvement. Concerns in relation to understanding of physical health issues and co-morbidities are also being addressed. CPFT commissioned an external review of suicides by Professor Appleby from the Centre for Suicide Prevention at the University of Manchester during 2012/13. The review is due to be published in spring 2013. The Trust has been working with other agencies to develop a health economy suicide prevention strategy, with terms of reference now finalised for the strategy group. A task and finish multiagency group has looked at improving risk assessments in this area. The CCG expect CPFT to play a major role in driving work and learning from thematic analysis forward across the health economy in 2013/14. The Care Quality Commission (CQC) is the national regulator of quality in the NHS and carries out inspections across all health and social care organisations. The CQC inspected CPFT in June 2012 and reported a moderate concern relating to medicines management and a minor concern for assessing and monitoring quality. The Trust addressed all issues raised and the CQC confirmed these areas were no longer concerns after a follow-up review in January 2013. The Trust currently has no CQC concerns. The Quality Account summarises both concerns and actions taken to address these issues. Page 67 of 74 The CQC also has a responsibility to inspect compliance with the Mental Health Act and carried out a visit to CPFT in relation to this area in December 2012. The final report was received in March 2013 and a response is being submitted by CPFT. The report raised issues about advocacy services, facilities, patients’ understanding of their rights and restriction of patients. The Chief Executive reserves special praise for the staff at CPFT who have worked hard to turn the Trust around following a period of significant CQC concerns. However, this pressure has had a detrimental effect on staff morale with the both national and internal staff surveys reflecting the stress staff feel. The percentage of staff who would recommend the Trust as a place to work to family and friends was well below the national average for similar trusts. The Quality Account sets out a range of measures that have been put in place to support and involve staff in decision making and their own health and wellbeing. The CCG will monitor this work closely to ensure it is driving improvement in staff morale. With the emphasis of staff engagement in the Quality Account, the work relating to service user and care experience and engagement has a lower profile. There is limited detail about service user engagement, although the CCG is aware work is being carried out, with involvement in care planning a priority. The CCG are concerned about the slow progress in developing and implementing a Carers Strategy. In 2012/13, all acute providers started to use the Net Promoter / Friends and Family question as part of their patient experience surveys. The question asks ‘Would you recommend the trust to family and friends?’ The requirement to use this question was not extended to Mental Health Trusts. However, CPFT did collect some data and are working with other similar trusts nationally to determine how to use the Friends and Family test for Mental Health providers. Following a year when priorities for improvement for 2012/13 were driven by the improvements required by the CQC, the priorities for 2013/14 reflect a more rounded approach with involvement of all stakeholders, better use of data and information, and a focus on the initiatives in CPFT’s Quality Diamond Strategy. Seven of the nine priorities cover the whole of CPFT, and so will support not only the clinical mental health work of the organisation, but also cover social care and the physical health of adults and children. The CCG expect to see CPFT improve working between the different parts of the Trust in 2013/14. The Quality Account gives detail of the Commissioning for Quality and Innovation (CQUIN) scheme, which rewards trusts for developing and implementing innovative plans for improvement. The Trust did well against most of the 2012/13 CQUIN goals. However, the project to promote public health initiatives by giving advice to service users regarding smoking and alcohol did not progress well and the CCG expect the Trust to ensure this work receives a higher priority in 2013/14. The Quality Account is well set out and fairly easy for the public to understand, although there are some sections which use NHS jargon The report is open about the areas where improvement is needed, and looks at and links all quality priorities from the past three years with those chosen for 2013/14. The Quality Account includes all the nationally mandated sections including a list of services and specialties provided by the Trust. Healthwatch Cambridgeshire 17 May 2013 Healthwatch Cambridgeshire is new organisation and so at this point are not able to constructively comment on the Trust's draft Quality Accounts for 2012/13. Once fully established, Healthwatch Cambridgeshire will be delighted to work together with CPFT on consultations and participation work on matters that are important to the health and social care economy of Cambridgeshire Page 68 of 74 Cambridgeshire Overview & Scrutiny Committee 16 May 2013 Statement from OSC Cambridgeshire Officer As a result of the County Council elections, the Council's Committees were not determined at the time that comments on the draft quality account were required. We are therefore not able to provide a full Overview and Scrutiny Committee response on this occasion. There has been on going liaison and communication between the Committee and the Trust throughout the year During 2012/13 the Adults Wellbeing and Health Overview and Scrutiny Committee Highlighted the need for more timely access to and more co-ordinated provision of child and adolescent mental health services, particularly for young people in the transitional age ranges, including those who are referred for the first time when they are aged 16-18 Raised concerns about timely access to urgent inpatient mental health provision within the County for working age adults and older people. As part of a review of delayed discharge from acute hospitals used by Cambridgeshire residents, identified a need for o Ensuring prompt identification, referral and access to secondary mental health services for patients with mental health problems o Strengthening the provision of liaison psychiatry within the hospitals for working age adults and older people o Developing inter-agency strategies for supporting the discharge of people who have alcohol problems, are homeless, or have other support needs. The Committee worked with Peterborough City Council Scrutiny Commission for Health Issues to follow up the implementation of the changes to CPFT services which were agreed in early 2012. A particular area of focus is ensuring that the Advice and Referral Centre provides a high quality and effective service when it is rolled out across the County. Comments from Scrutiny Commission for Health Issues – Peterborough City Council 20 May 2013 Comment from the Chair I would like to thank the Trust for all of the hard work that has been put into producing this document. A lot of work has been put in to improve the service for patients and I fully support the 2013/14 priorities. Comments from Members of the Commission 5 Star Standard. It is encouraging to see that all 21 wards have achieved at least 4 stars and hope standards will continue to improve so that we see mostly 5 stars in future. I hope the IT response times will continue to improve and that discussions with Serco will address these issues. Priority 3: Clinical Effectiveness, Trust Indicators Numbers 2 and 4 are red and we would look to see improvements in these areas in the future. I was pleased to see that positive steps have been taken to improve patient safety overall. It is reassuring to see that staff ratings have been taken seriously and that training and an improvement in the patient satisfaction rate is expected to raise morale in this respect. Congratulations are due for the phoenix-like rising from the ashes from the position two years ago. I only hope the IT situation improves as this is also crucial in building staff morale in my experience. It may be helpful to see what the position is regarding staffing at all levels in future reports but this one was really easy to read so well done for that too. Page 69 of 74 ANNEX 4 STATEMENT OF DIRECTOR’S RESPONSIBILITIES IN RESPECT OF THE QUALITY REPORT The directors are required under the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010 as amended to prepare Quality Accounts for each financial year. Monitor has issued guidance to NHS Foundation Trust Boards on the form and content of annual quality reports (which incorporate the above legal requirements) and on the arrangements that Foundation Trust Boards should put in place to support the data quality for the preparation of the quality report. In preparing the quality report, directors are required to take steps to satisfy themselves that: the content of the quality report meets the requirements set out in the NHS Foundation Trust Annual Reporting Manual 2012-13; the content of the Quality Report is not inconsistent with internal and external sources of information including: o o o o o o o o o o o Board minutes and papers for the period April 2012 to May 2013; Papers relating to Quality reported to the Board over the period April 2012 to May 2013; Feedback from the Commissioners Cambridgeshire Commissioning Group dated 21/05/2013; Feedback from local Healthwatch organisation Healthwatch Cambridgeshire dated 17/05/2013; Feedback from Cambridgeshire County Council Adults Wellbeing and Health overview and Scrutiny Committee dated 16/05/2013; Feedback from Peterborough City Council Scrutiny Commission for Health Issues dated 20/05/13; The Trust’s complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009, presented in the PALS and Complaints report to the Quality and Performance Committee in April 2013; The 2012 national patient survey; The 2012 national staff survey; The Head of Internal Audit’s annual opinion over the Trust’s control environment for the year ending 31 March 2013 dated 23/05/2013; and CQC quality and risk profiles dated 02/04/13. the Quality Report presents a balanced picture of the NHS foundation trust’s performance over the period covered; the performance information reported in the Quality Report is reliable and accurate; there are proper internal controls over the collection and reporting of the measures of performance included in the Quality Report, and these controls are subject to review to confirm that they are working effectively in practice; the data underpinning the measures of performance reported in the Quality Report is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review; and the Quality Report has been prepared in accordance with Monitor’s annual reporting guidance (which incorporates the Quality Accounts regulations) (published at www.monitornhsft.gov.uk/annualreportingmanual) as well as the standards to support data quality for the preparation of the Quality Report (available at www.monitornhsft.gov.uk/annualreportingmanual)). The directors confirm to the best of their knowledge and belief they have complied with the Page 70 of 74 above requirements in preparing the Quality Report. By order of the Board NB: sign and date in any colour ink except black ................................................ Chairman 24th May 2013 ................................................ Chief Executive 24th May 2013 Page 71 of 74 ANNEX 5 EXTERNAL AUDIT REPORT Independent Auditor’s Limited Assurance Report to the Council of Governors of Cambridgeshire and Peterborough NHS Foundation Trust on the Annual Quality Report We have been engaged by the Council of Governors of Cambridgeshire and Peterborough NHS Foundation Trust to perform an independent assurance engagement in respect of Cambridgeshire and Peterborough NHS Foundation Trust’s Quality Report for the year ended 31 March 2013 (the ‘Quality Report’) and specified performance indicators contained therein. Scope and subject matter The indicators for the year ended 31 March 2013 in the Quality Report that have been subject to limited assurance consist of the following national priority indicators as mandated by Monitor: 100% enhanced CPA patients receiving follow-up contact within seven days of discharge from hospital (“CPA patient follow-ups”) – page 34 of the Quality Report; and Admissions to inpatient services had access to crisis resolution home treatment teams “Gate-keeping” – page 34 of the Quality Report. We refer to these national priority indicators collectively as the “specified indicators”. Respective responsibilities of the Directors and auditors The Directors are responsible for the content and the preparation of the Quality Report in accordance with the assessment criteria referred to on page 70 of the Quality Report (the "Criteria"). The Directors are also responsible for the conformity of their Criteria with the assessment criteria set out in the NHS Foundation Trust Annual Reporting Manual (“FT ARM”) issued by the Independent Regulator of NHS Foundation Trusts (“Monitor”). Our responsibility is to form a conclusion, based on limited assurance procedures, on whether anything has come to our attention that causes us to believe that: The Quality Report does not incorporate the matters required to be reported on as specified in Annex 2 to Chapter 7 of the FT ARM; The Quality Report is not consistent in all material respects with the sources specified below; and The specified indicators have not been prepared in all material respects in accordance with the Criteria. We read the Quality Report and consider whether it addresses the content requirements of the FT ARM, and consider the implications for our report if we become aware of any material omissions. We read the other information contained in the Quality Report and consider whether it is materially inconsistent with the following documents: Board minutes for the period April 2012 to the date of signing this limited assurance report (the period); Papers relating to Quality reported to the Board over the period April 2012 to the date of signing this limited assurance report; Feedback from the Commissioners Cambridgeshire Commissioning Group dated 21 May 2013; Feedback from local Healthwatch organisation Healthwatch Cambridgeshire dated 17 May 2013; Feedback from the Cambridgeshire County Council Adults Wellbeing and Health Overview and Scrutiny Committee dated 16 May 2013; Feedback from Peterborough City Council Scrutiny Commission for Health Issues dated 20 May 2013; Page 72 of 74 The Trust’s complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009, presented in the PALS and Complaints report to the Quality and Performance Committee in April 2013; The CQC national inpatient survey 2011 and 2012; The CQC survey of people who use community mental health services 2012; The NHS national staff survey dated 2011 and 2012; Care Quality Commission quality and risk profiles dated monthly from April 2012 to March 2013; CQC Inspection Reports in respect of: The Cavell Centre - January 2012; and Fulbourn Hospital - January 2012; CQC reviews of compliance in respect of Fulbourn Hospital - July 2012 and October 2012; The Head of Internal Audit’s opinion over the Trust’s control environment for the year ending 31 March 2013 dated 23 May 2013; Quality and Performance Committee minutes dated 13 December 2012, 14 March 2013 and 18 April 2013; Trust Patient Experience Survey 2012, including data from the Trust’s internal inpatient and community patient experience surveys; Staff 'Pulse' survey results March 2013; and Report of the National Audit of Schizophrenia (NAS) 2012. We consider the implications for our report if we become aware of any apparent misstatements or material inconsistencies with those documents (collectively, the “documents”). Our responsibilities do not extend to any other information. We are in compliance with the applicable independence and competency requirements of the Institute of Chartered Accountants in England and Wales (ICAEW) Code of Ethics. Our team comprised assurance practitioners and relevant subject matter experts. This report, including the conclusion, has been prepared solely for the Council of Governors of Cambridge and Peterborough NHS Foundation Trust as a body, to assist the Council of Governors in reporting Cambridge and Peterborough NHS Foundation Trust’s quality agenda, performance and activities. We permit the disclosure of this report within the Annual Report for the year ended 31 March 2013, to enable the Council of Governors to demonstrate they have discharged their governance responsibilities by commissioning an independent assurance report in connection with the indicators. To the fullest extent permitted by law, we do not accept or assume responsibility to anyone other than the Council of Governors as a body and Cambridge and Peterborough NHS Foundation Trust for our work or this report save where terms are expressly agreed and with our prior consent in writing. Assurance work performed We conducted this limited assurance engagement in accordance with International Standard on Assurance Engagements 3000 ‘Assurance Engagements other than Audits or Reviews of Historical Financial Information’ issued by the International Auditing and Assurance Standards Board (‘ISAE 3000’). Our limited assurance procedures included: Evaluating the design and implementation of the key processes and controls for managing and reporting the indicators. Making enquiries of management. Limited testing, on a selective basis, of the data used to calculate the specified indicators back to supporting documentation. Comparing the content requirements of the FT ARM to the categories reported in the Quality Report. Reading the documents. A limited assurance engagement is less in scope than a reasonable assurance engagement. The nature, timing and extent of procedures for gathering sufficient appropriate evidence are deliberately limited relative to a reasonable assurance engagement. Page 73 of 74 Limitations Non-financial performance information is subject to more inherent limitations than financial information, given the characteristics of the subject matter and the methods used for determining such information. The absence of a significant body of established practice on which to draw allows for the selection of different but acceptable measurement techniques which can result in materially different measurements and can impact comparability. The precision of different measurement techniques may also vary. Furthermore, the nature and methods used to determine such information, as well as the measurement criteria and the precision thereof, may change over time. It is important to read the Quality Report in the context of the assessment criteria set out in the FT ARM and the Directors’ interpretation of the Criteria on page 70 of the Quality Report. The nature, form and content required of Quality Reports are determined by Monitor. This may result in the omission of information relevant to other users, for example for the purpose of comparing the results of different NHS Foundation Trusts. In addition, the scope of our assurance work has not included governance over quality or non-mandated indicators in the Quality Report, which have been determined locally by Cambridge and Peterborough NHS Foundation Trust. Basis for Disclaimer of Conclusion – CPA patient follow-ups and Gate-keeping indicators The CPA patient follow-ups indicator, requires patients to be followed up within 7 days of discharge through face to face contact or a phone call. For 3 patients that we tested out of a total of 35, patient files did not contain evidence of the follow-up process performed. As a result, we were not able to conclude that a followup had been performed. The Gate-keeping indicator requires in-patients to be assessed by the crisis resolution home treatment service prior to admission (“gatekeeping”). We identified that the report produced from the Trust’s information systems to calculate this indicator had not been programmed correctly. In our sample of 35 cases, there was insufficient evidence on patient files in respect of 7 cases to substantiate that the patients, as reported by the Trust, had been subject to gatekeeping. As a result, we were not able to conclude that the crisis resolution home treatment service had assessed the patient prior to admission. Conclusion (including disclaimer of conclusion on the specified indicators) Because of the significance of the matters described in the Basis for Disclaimer of Conclusion paragraph, we have not been able to form a conclusion on the specified indicators. Based on the results of our procedures, nothing has come to our attention that causes us to believe that for the year ended 31 March 2013, The Quality Report does not incorporate the matters required to be reported on as specified in annex 2 to Chapter 7 of the FT ARM; and The Quality Report is not consistent in all material respects with the documents specified above. PricewaterhouseCoopers LLP Chartered Accountants Cambridge 29th May 2013 The maintenance and integrity of the Cambridge and Peterborough NHS Foundation Trust’s website is the responsibility of the directors; the work carried out by the assurance providers does not involve consideration of these matters and, accordingly, the assurance providers accept no responsibility for any changes that may have occurred to the reported performance indicators or criteria since they were initially presented on the website. Page 74 of 74