Apoptosis in Breast Cancer Cell by
advertisement
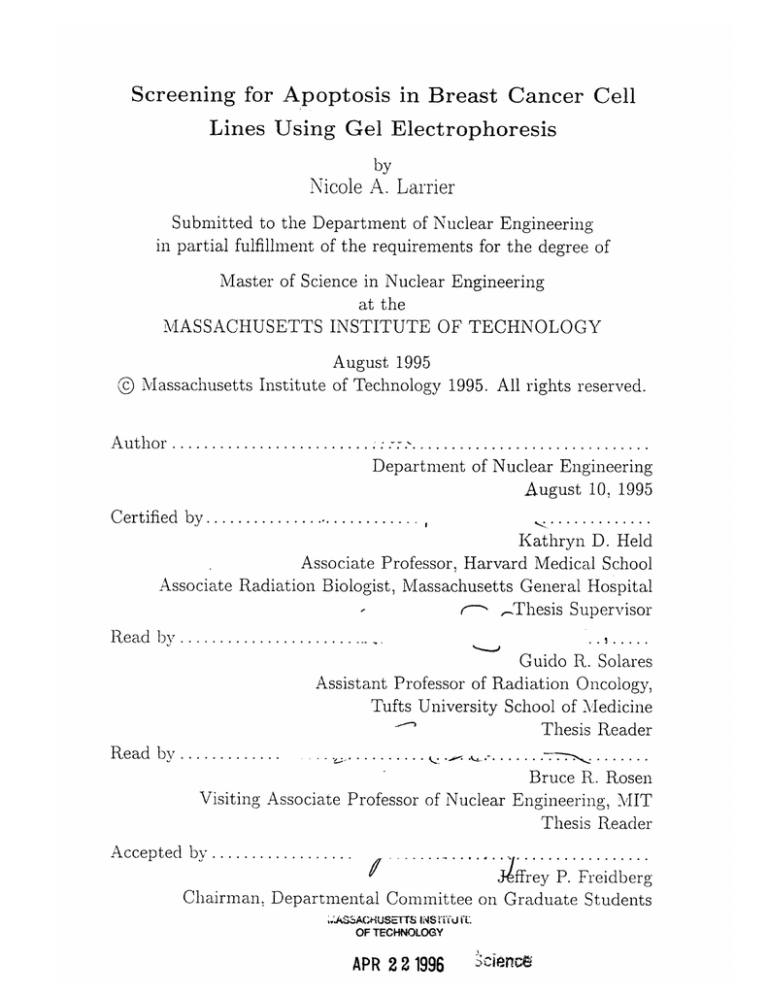
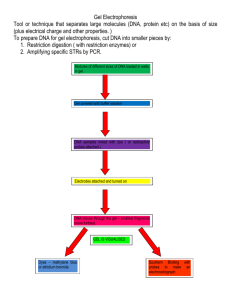
Screening for Apoptosis in Breast Cancer Cell Lines Using Gel Electrophoresis by Nicole A. Larrier Submitted to the Department of Nuclear Engineering in partial fulfillment of the requirements for the degree of Master of Science in Nuclear Engineering at the MASSACHUSETTS INSTITUTE OF TECHNOLOGY © August 1995 Massachusetts Institute of Technology 1995. All rights reserved. Author ................. .............................. Department of Nuclear Engineering August 10, 1995 Certified by ............................ , ......... Kathryn D. Held Associate Professor, Harvard Medical School Associate Radiation Biologist, Massachusetts General Hospital SThesis Supervisor Read by .................. ....... ,.... Guido R. Solares Assistant Professor of Radiation Oncology, Tufts University School of Medicine Thesis Reader Read by ......... . . ...... . . .. . .........- " ....... Bruce R. Rosen Visiting Associate Professor of Nuclear Engineering, MIT Thesis Reader Accepted by....... ffJkrey P. Freidberg Chairman. Departmental Committee on Graduate Students ,.ASSACHUSETTS INSTi'U i OF TECHNOLOGY APR 22 1996 'citence Screening for Apoptosis in Breast Cancer Cell Lines Using Gel Electrophoresis by Nicole A. Larrier Submitted to the Department of Nuclear Engineering on August 10, 1995, in partial fulfillment of the requirements for the degree of Master of Science in Nuclear Engineering Abstract Apoptosis in breast cancer cell lines has not been comprehensively investigated. This study screens for radiation- and tamoxifen-induced apoptosis in five human breast cancer cell lines: BT20, BT549, Hs578T, HTB26 and MCF7. Conventional and Pulsed Field Gel Electrophoresis were used to analyse the DNA and look for any fragmentation that had occured. The results showed no evidence of radiation- or tamoxifen-induced apoptosis. However, the irradiated cells did show significant detatchment from the plates at 25 Gy. In addition, the MCF7 cell line showed a growth delay in response to 10 pM tamoxifen. Thesis Supervisor: Kathryn D. Held Title: Associate Professor, Harvard Medical School Associate Radiation Biologist, Massachusetts General Hospital Acknowledgments I wish to thank the Lord for seeing me through this work. May everything I do contribute to the furthering of Your work. Thank you Dr. Held for allowing me to work in your laboratory over the last two years. The experience has been invaluable. Karen Hopcia, Yvonne McCarey and Craig Sylvester also contributed greatly to my understanding of the subject and helped immensely with the large volumes of tissue culture required to do this work. MIT people who contributed to this endeavor (and maybe didn't even know it) are Professor Jacquelyn C. Yanch and Dr. Guido Solares, who always took my ambitions seriously and encouraged me; the folks in the UAA office, who taught me how to deal with the MIT Firehose and come out a better person for it; and friends such as, Ali Alavi, Emanuela Binello, John de Souza, Anne Kohnen, Jacquin Niles and Olapeju Popoola, who called, emailed, visited and made this a far more pleasant experience than most people have! Finally, there are the wonderful people from Barbados - Mom and Deidre, Brian Pollard, John Skinner and Marcus St. John. You guys are awesome. Even youths shall faint and be weary, and young men shall fall exhausted; but they who wait for the Lord shall renew their strength, they shall mount up with wings like eagles, they shall run and not be weary, they shall walk and not faint. Isiah 40:30-31 Contents 1 Introduction 1.1 1.2 2 9 Mechanisms of Apoptosis .......... .. ... ...... ... . 10 .. ... ..... .... . 10 1.1.1 Apoptosis versus Necrosis 1.1.2 Apoptosis in Breast Cells...... .. .... ..... .... 11 1.1.3 Role of bcl-2 and p-53 in Apoptosis . . . . . . . . . . . . . . . 11 1.1.4 Radiation-Induced Apoptosis . . . . . . . . . . . . . . . . . . 12 1.1.5 Tamoxifen-Induced Apoptosis . . . . . . . . . . . . . . . . . . 13 ..... Endpoints of Apoptosis ........... .. .... ...... ... 15 Gel Electrophoresis 2.1 Conventional Electrophoresis 2.2 Pulsed Field Gel Electrophoresis . . . . . . . . . . . . . ....... 2.3 Description of the CHEF-DR II System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 Materials and Methods 22 3.1 M aterials 3.2 Tissue Culture . . .. . 22 3.3 Treatment of Cells used in Conventional Gel Electrophoresis . . . . . 23 3.3.1 Screening of Cell Lines for Radiation-Induced Apoptosis . . . 25 3.3.2 Screening of Cell Lines for Tamoxifen-Induced Apoptosis . . . 25 3.3.3 DNA Isolation ........................ .. . 25 3.3.4 Conventional Gel Electrophoresis . . . . . . . . . . . . . . . . 26 3.4 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . .. . . . . . . . . . . . . . . . . .. Treatment of Cells used in Pulsed Field Gel Electrophoresis . . . . . 22 26 3.4.1 3.4.2 Pulsed Field Gel Electrophoresis . Experiment 1: Establishing PFGE Run Conditions Using HL60 cells 3.4.3 ............... . . . . . . . . . . . . . . . . . . . . . . . Experiment 2: Analysis of Radiation-Induced Apoptosis in Breast Cancer Cell Lines . . . . . . . . . . . . . . ....... 4 Results 4.1 4.2 4.3 29 Screening on Conventional Gels . . . . . . . . . . . . . . . . . . . . . 29 4.1.1 Effect of Irradiation ........................ 29 4.1.2 Effect of Tamoxifen ........... Screening on Pulsed Field Gels .............. 29 ..................... 33 4.2.1 Setting Conditions Using HL60 cells . . . . . . . . . . . . . . . 33 4.2.2 Screening of Irradiated Breast Cancer Cell Lines . . . . . . . . 33 Cell Counts after Irradiation and Tamoxifen Treatment . . . . . . . . 33 5 Analysis and Conclusions 5.1 5.2 41 Improvements in the Screening Technique . . . . . . . . . . . . . 43 5.1.1 Radiation-Induced Apoptosis . . . . . . . . . . . . . . . . 43 5.1.2 Tamoxifen-Induced Apoptosis . . . . . . . . . . . . . . . . 43 .. .... 43 Future Work ..... ............... A Schematic of the CHEF-DR II System .... 45 List of Figures 1-1 Proposed pathways that lead to Radiation and Tamoxifeninduced apoptosis [54, 40, 13, 33] . 2-1 14 ................. Diagrams of some PFGE systems. (a) The original PFGE system developed by Schwartz and Cantor. (b) Field Inversion Gel Electrophoresis (FIGE). (c) Rotating Gel Electrophoresis. Homogeneous Electric Field Electrophoresis. 4-1 [7] (d) Clamped 20 . .......... Conventional gel electrophoresis of DNA extracted from BT549 cells. The cells grown on 100 mm plates showed very faint apoptotic ladders. When the same number of cells (106) cells were grown on 150 mm plates, no ladders are observed. The horizontal axis is time m easured in days .................... 4-2 .......... 30 Conventional gel electrophoresis of DNA extracted from BT20 and Hs578T cells following irradiation with 25 Gy. The hori31 zontal axis is measured in days. ..................... 4-3 Conventional gel electrophoresis of DNA extracted from MCF7, HTB26 and BT549 cells following treatment with 10 yM Tamoxifen. 4-4 The horizontal axis is time measured in days. . ...... 32 HL60 cells following 25 Gy of irradiation. The top panel shows a conventional agarose gel, where the horizontal axis is time measured in hours. The bottom panels show pulsed field gels run for 22 hours (left) and 32 hours (right). The samples were take at 6 hours after treatment. 34 4-5 PFGE of HTB26 cells following 25 Gy of irradiation. The bottom panel shows conventional electrophoresis of the plug wash. The horizontal axis is time measured in days. . .............. 4-6 . PFGE of MCF7 cells following 25 Gy of irradiation. 35 The bottom panel shows conventional electrophoresis of the plug wash. The horizontal axis is time measured in days. . .............. . 36 4-7 Normalised Cell Counts for the BT20 and BT549 cell lines. The Normalised Cell Count is the number of cells counted on Day 0 divided by the cell count on a particular day. Squares = Untreated cells. Circles = 25 Gy. Triangles = 10 pM Tamoxifen. 4-8 . ........ 38 Normalised Cell Counts for the HTB26 and MCF7 cell lines. The Normalised Cell Count is the number of cells counted on Day 0 divided by the cell count on a particular day. Squares = Untreated cells. Circles = 25 Gy. Triangles = 10 pM Tamoxifen. 4-9 . ........ 39 Normalised Cell Counts for the Hs578T cell line. The Normalised Cell Count is the number of cells counted on Day 0 divided by the cell count on a particular day. Squares = Untreated cells. Circles = 25 Gy. Triangles = 10 pM Tamoxifen. . ................ 40 A-1 A schematic showing the set-up of Biorad's CHEF-DR II Pulsed Field Gel Electrophoresis System [6]. . .......... 45 List of Tables 3.1 Characteristics of Cell Lines ................... 3.2 Maintenance of Cell Lines ................... .... ..... 23 24 Chapter 1 Introduction Studies indicate that one in nine women in the United States will develop breast cancer [26]. Twenty-seven percent of all malignancies in women are breast cancers [26]. The major treatments are surgery and radiation therapy. Adjuvant therapy in the form of hormonal therapy, chemotherapy or radiation therapy is used to prevent or delay the recurrence of the cancer [52]. Understanding the processes involved in tumor cell kill by these agents will help improve the survival of patients. Apoptosis is one of the two defined types of cell death. It was first defined in 1972 when observations distinguished it as a morphologically distinct form of cell death [30]. Many tissue types, both normal and neoplastic, undergo apoptosis [69]. Normal development of vertebrates depends on apoptosis for the shaping of organs and cavities [1]. In mammals apoptosis, coupled with mitosis, serves to keep a constant number of intestinal crypt epithelial cells [63, 29, 1]. Apoptosis also occurs in liver epithelium, prostate and the adrenal cortex. In pathological conditions, apoptosis has been associated with toxin-induced liver disease, neurodegenerative disorders and aplastic anemia [57]. Spontaneous apoptosis also occurs in most tumors [69, 29]. The agents that cause apoptosis are diverse. They include radiation(X-rays [41] and UV [37]) in thymocytes and leukemia cells, hormonal alteration in the prostate, dithiothreitol (DTT) in leukemia cells, ethanol in leukemia and various chemotheraputic drugs such as cisplatin [1]. The pathway that each of these agents uses to induce apoptosis, may be different. For example, it is known that ionizing radiation damage may induce apoptosis via a pathway that includes the p53 tumor suppressor gene, while glucocorticoids induce a p53 independent pathway to apoptosis [13, 67]. With breast cells, estrogen may be involved in the pathway to apoptosis. These multiple pathways probably converge at some point downstream to give the changes that are identified as apoptosis [21]. 1.1 1.1.1 Mechanisms of Apoptosis Apoptosis versus Necrosis Apoptosis and necrosis are morphologically and biochemically distinct modes of cell death. They are observed in both normal and pathological conditions. Necrosis is characterised by swelling of the cell and rupturing of the cell membranes [69]. The cellular organelles disintegrate, and the DNA is randomly degraded. This is accompanied by inflammation of the surrounding tissue. The morphological changes associated with apoptosis are shrinking of cell size, condensation of the chromatin and the appearance of membrane bound "apoptotic bodies" [69, 29]. The first change that is observed in apoptotic cells is the con- densation of the chromatin and a decrease in the size of the nucleus and the cell. Subsequently, nuclear and cytoplasmic materials are packaged in membrane-bound sacs called apoptotic bodies which appear on the surface of the cell. The apoptotic bodies vary in size and content. They may contain intact organelles, DNA fragments or simply contain cytoplasm. In vivo, the apoptotic bodies are phagocytosed by surrounding normal tissue, engulfed by macrophages, or in the case of epithelial cells disposed of by emptying them into the suface of the organ's lumen. Since the remains of apoptosis are quickly disposed of, there is no inflammatory response as in the case of necrosis. In cultured cells, the apoptotic bodies may detach from the plate and float in the media. One of the earliest biochemical events associated with apoptosis was the double stranded internucleosomal cleavage of the DNA [2, 68]. This results in DNA fragments that are multiples of 180 - 200 base pairs. (This fragmentation is postulated to be caused by a calcium dependent endonuclease.) However, the absence of these DNA fragments has been noted in some cells that exhibit morphological features of apoptosis [14, 15]. It has been shown that the DNA is first cleaved to 50 or 300 kbp fragments before proceeding to the smaller 200 bp fragments [9, 45]. Cohen used zinc to show that in thymocytes the morphological changes associated with apoptosis could occur in the absence of DNA cleavage to 200 bp fragments [14]. Subsequently, they showed that even though there were no 200 bp fragments, there was DNA fragmentation to large molecular weights (30-50 kbp and 200-250 kbp) [9]. Thus, it is inferred that morphological changes precede cleavage to 50 or 300 kbp fragments, and subsequently cleavage to 200 bp pieces occurs. 1.1.2 Apoptosis in Breast Cells Like many tissues, breast tissue is susceptible to apoptosis in both normal and pathological situations [3]. Normal breast tissue undergoes apoptosis in a cyclic fashion that patterns the menstrual cycle [51]. In addition, the involution of the lactating breast after weaning is caused by apoptosis [63, 62]. One of the drugs used to treat estrogen receptor positive breast cancer, has been shown to induce apoptosis in breast cancer cell lines [4]. In these experiments, the drug tamoxifen caused estrogen receptor positive MCF7 cells to undergo apoptosis while the estrogen receptor negative HTB26 and BT20 cells did not. This suggests that it might be possible to exploit this property of chemically (or radiation) induced apoptosis in the treatment of breast cancer. 1.1.3 Role of bcl-2 and p-53 in Apoptosis Since the number of cells in a tissue at any time is dependent on the balance between cell proliferation and cell death, it is reasonable to suggest that one of the relevant modes of cell death is apoptosis [21, 49]. This means that apoptosis is likely to be affected by the presence or absence of oncogenes and tumor suppressor genes in the cell [46]. An oncogene is a gene that produces net cell growth when it is mutated. Tumor suppressors act as negative regulators of cell proliferation. When they are mutated a cell will proliferate rapidly, while an unmutated gene keeps cell growth in check. The bcl-2 oncogene is intimately involved in the control of apoptosis [54, 11, 40]. The 26 kDa bcl-2 protein is located on the inner and outer membrane of mitochondria and on the nuclear membrane. Expression of the bcl-2 product does not promote cell proliferation, but instead enhances cell survival by preventing apoptosis [46]. Bcl-2 expression is present in both normal and cancerous tissue, and it is generally found in tissues which contain cells undergoing apoptosis [46]. In particular, bcl-2 expression has been observed in both normal breast tissue and in a breast cancer cell line [65]. It has also been noted that within the same cell line there may exist pathways to apoptotsis that depend on and are independent of bcl-2 expression. In addition, the overexpression of bcl-2 does not prevent apoptosis in response to hydrogen peroxide [40]. Thus the necessity of bcl-2 to the induction of apoptosis is not clear. Alternately, the overexpression of the p53 tumor suppressor gene can lead to cell death by apoptosis. The p53 gene is frequently mutated in human cancers including lung, colorectal, brain and breast [25, 64]. It is located on chromosome 17p and produces a 53 kDa nuclear phosphoprotein that can bind to DNA [35]. It is present at very low levels in normal cells. Its role in the apoptotic pathway is unclear. It seems likely that it is involved in some, but not all, apoptotic pathways [13]. In cases where p53 levels are influential, high levels are associated with apoptosis [47]. When thymocytes from p53 knock-out mice are subjected to radiation, the cells do not undergo apoptosis [38]. However, thymocytes from mice with normal p53 genes readily apoptose. 1.1.4 Radiation-Induced Apoptosis Apoptosis can be induced in tissues and cell lines in response to ionizing radiation [42, 66, 59]. In tumor cells, radiation-induced apoptosis is seen in murine mammary and ovarian adenocarcinomas, sarcomas and squamous cell carcinomas subjected to 2.5 to 25 Gy of y-irradiation [39]. The HL60 human leukemia cell line also readily undergoes radiation-induced apoptosis 3-5 hours after treatment although doses greater than 10 Gy were needed [37, 34]. It has also been observed that a radiosensitive murine ovarian carcinoma is susceptible to radiation-induced apoptosis, while a radioresistant hepatocellular carcinoma is not [58]. This suggests that the tumors natural radioresistance may affect its ability to apoptose. The p53 status of a cell may affect its sensitivity to radiation [33, 32]. This is believed to be a result of p53 levels being elevated in response to the DNA damage resulting from the radiation [33]. The presence of mutant p53 is associated with an increased resistance to i-irradiation. Lee and Bernstein showed that mouse p53 mutations increased the resistance of bone marrow and spleen cells to i-radiation [33]. The effect of p53 on the cell cycle may also affect apoptotic pathways. It is suggested that wild-type p53 acts a cell cycle checkpoint. This can lead to DNA repair or possibly to apoptosis (see Figure 1-1). This would suggest that cells that are going to apoptose would not undergo any cell divisions. However, this is not always observed. Cell death has been observed shortly after radiation and after one or more cell divisions [50]. 1.1.5 Tamoxifen-Induced Apoptosis Tamoxifen is a non-steroidal antiestrogen that is often used in the treatment of estrogen receptor positive breast cancer [27]. One of its main features is that it is a competitive inhibitor of estrogen. There are some data that suggest that high exposure to estrogen increases susceptibility to breast cancer [44] and that estrogen ablation induces apoptosis in the MCF7 breast cancer cell line [31]. There maybe an association between the presence of estrogen receptors and bcl-2 protein levels [65]. In addition, the level of bcl-2 in beast tissue changes during the menstrual cycle [51]. Therefore it is possible that binding of tamoxifen to estrogen receptors leads to lower levels of bcl-2 and hence, to apoptosis (see Figure 1-1). The presence of the wildtype p53 gene is also associated with estrogen receptor positive cancers [10]. However, how (or if) this correlates with apoptosis is not known. Ionizing Radiation Tamoxifen Estro gen Receptors I Radiation Damage bc 1-2 p53 k - G1 Cell Cycl e Arrest DNA Repair Cell Division and Proliferation APOPTOSIS Morphologic Changes 50 & 300 kbp fragments Internucleosomal cleavage (multiples of 200 bp) Figure 1-1: Proposed pathways that lead to Radiation and Tamoxifeninduced apoptosis [54, 40, 13, 33]. 1.2 Endpoints of Apoptosis Given that the apoptotic pathway involves many steps, there are several places that can be used to define a cell that has undergone apoptosis. On a philosophical level the pertinent question is, is there a lowest common denominator in the converging pathways to apoptosis that can be used to identify a cell's commitment to apoptose. From a practical standpoint, criteria for defining and identifying apoptosis depend on the development of assays that can detect changes that occur during the process. The earliest definition of apoptosis was based on morphological observations [63]. This method continues to be very popular as an end point. It is considered to be a reliable "lowest common denominator". The characteristic changes such as cell chromatin condensation, cell blebbing and decreased cell volume can be seen using electron or light microscopy. The percent of apoptosis in a population can be estimated by counting the fraction of apoptotic cells in a sample. However, since this is only at one time point, the total number of cells undergoing apoptosis cannot be counted. In addition, counting the apoptotic bodies in a sample is a tedious, somewhat subjective procedure. The DNA fragmentation that occurs in apoptosis is another useful endpoint. The DNA fragments can be separated and visualised by gel electrophoresis. The 200 bp fragments and multiples thereof appear as a characteristic ladder pattern on conventional agarose gels. (Necrosis is shown as a smear due to the random degredation of the DNA.) The larger 50 or 300 kbp pieces can be seen as bands on pulsed field gels [45]. DNA end labelling techniques may also be used to analyse the DNA fragmentation quantitatively. In tissue culture, the detatchment of apoptotic cells from the plate has been used as an assay for apoptosis [36]. This method is based on the correlation between apoptotic ladders being found in the floating cells and intact DNA being observed in the cells that are still attatched. However, to be a satisfactory technique, this correlation must be performed on every cell line under consideration. In addition, no attempt has been made to identify large molecular weight DNA fragments. The presence of these fragments in the floating or attached cells could change the conclusions. There is also the possibility that necrotic cells are detatching and floating with the apoptotic cells. In this study, apoptosis is screened for by using electrophoresis techniques. The presence of apoptosis should yield "ladders" and/or large molecular weight bands on agarose gels. Identifying apoptosis by these methods will be an efficient, conclusive indicator of its occurrence. Chapter 2 Gel Electrophoresis Electrophoresis refers to the separation of molecules, such as DNA or protein, by the application of an electric field across the sample under investigation. In the system used for these studies, the DNA samples are run through an agarose matrix. The negatively charged DNA molecules migrate towards the positive electrode, called the anode. The mobility and resolution of the DNA depends on many factors including the characteristics of the agarose gel, the type of voltage gradient applied across the gel, the temperature, the size of DNA to be separated and the running buffer. In this analysis of DNA, two electrophoretic techniques are utilized: conventional electrophoresis and pulsed field gel electrophoresis. Conventional electrophoresis is used to separate the low molecular weight DNA ladders, and pulsed field gel electrophoresis is used for separation of the larger (>50 kb) molecular weight DNA [42]. The main difference between the two methods is the applied electric field. In conventional electrophoresis the electric field is static, that is, the voltage is fixed in one direction. However, in pulsed field electrophoresis the electric field changes direction at prescribed times that depend on the size of DNA to be separated. 2.1 Conventional Electrophoresis In conventional electrophoresis, DNA molecules move in a straight line from the cathode towards the anode. The agarose gel is made by pouring an agarose solution into a mold and allowing it harden. As it solidifies, a series of interconnected channels form. The density of the pores (and hence, how the DNA moves through the gel) depends on the concentration of agarose used. (The empirically derived mathematical relationship that describes this is: logpi = logplo - K7T; where p is the mobility of the DNA and 7 is the agarose concentration [55] .) The DNA is loaded onto the gel, and the current turned on. The DNA moves through the gel by a process called reptation. The reptation model was proposed by de Gennes in 1971 [18]. It suggests that a molecule moves through the matrix in a head-on fashion. That is, the DNA can slither back and forth in the channels formed by the agarose. Since the electric field is static, the molecules only move in one direction (towards the anode). It is easier for small molecules to move through the channels, and therefore they move the greatest distance on the gel. Linear DNA migrates through the gel matrix at a rate inversely proportional to the log of its molecular weight. Practically, this empirical relationship means that all DNA fragments greater than about 50 kb move about the same distance in a gel and cannot be resolved. 2.2 Pulsed Field Gel Electrophoresis Pulsed field gel electrophoresis (PFGE) is used to separate the DNA that is larger than 50 kb and up to megabase lengths. This large DNA encounters three problems when moving through gel matrices. These are formation of kinks, chain pinning and formation of knots [19]. Since the agarose channels are not exactly straight lines between the top and bottom of the gel, parts of long DNA, in effect, become trapped in different channels, and thus the forward motion of the DNA is hindered. These formations are known as kinks. Chain pinning refers to the situation where a DNA molecule becomes hooked over one of the fibers in the gel. Since the DNA molecule is large, it takes a lot of energy to get it moving again. It is possible for DNA to become knotted with itself or with other molecules. Longer molecules are more likely to have intra- and inter-chain knots. Again, these knots can hinder the passage of the molecules through the agarose matrix. Pulsed field electrophoresis solves some of these problems by varying the direction of the electric field and giving the DNA time to relax to an equilibrium state, before moving again under the influence of an electric field again [53]. The time required for the DNA to relax depends on the length of the molecule, with larger molecules taking longer to relax. Usually, an electric field is applied in one direction and then the field is switched to another direction. During electric field switching, the DNA uses the first part of the time in that interval to relax, before beginning to move in the new direction. This means that larger moleules spend less time moving than smaller molecules. As the time the DNA spends under each electric field increases, the larger molecules are more effectively separated. When running these gels, it is common to continually increase this switch time so that a range of molecules will be separated. If very large molecules are to be resolved, the electric field can be turned off between the switch in the direction of the electric field. Since its introduction, many variations of PFGE have emerged. The original system developed by Schwartz and Cantor consisted of subjecting an agarose gel to one homogenous and one non-homogenous electic field (Figure 2-1) [53, 7]. Now, variations include changing the angle between the two electric fields, using only homogenous or non-homogenous fields, and periodically rotating the gel while keeping the electric field stationary (Figure 2-1). The most commonly used systems are field inversion gel electrophoresis (FIGE) and clamped homogeneous electric field electrophoresis (CHEF). In FIGE only one electric field is switched, but the anode and cathode are interchanged periodically. The ratio of the time spent in each direction determines the ultimate movement of the DNA. The CHEF system contains twentyfour electrodes arranged in an hexagon. The two homogenous electric fields operate in the northwest to southeast and the northeast to southwest directions relative to the gel. A- B- (a)PFGE (b) FIGE -V (c) Rotating Gel (d) CHEF Figure 2-1: Diagrams of some PFGE systems. (a) The original PFGE system developed by Schwartz and Cantor. (b) Field Inversion Gel Electrophoresis (FIGE). (c) Rotating Gel Electrophoresis. (d) Clamped Homogeneous Electric Field Elec- trophoresis. [7] 2.3 Description of the CHEF-DR II System The commercially available CHEF-DR II System (Biorad) was used for PFGE. This system creates highly uniform electric fields which result in clearer gels. It consists of six components. They are a pump, the electrophoresis chamber, a cooling apparatus, the Drive Module, the Pulsewave 760 switcher and the Model 200/2.0 Constant Voltage Power Supply. The electrophoresis chamber has platinum wire electrodes fixed at 1200. The gel is placed in the middle of the chamber and held in place by two gel stops. The running buffer is pumped through the chamber in the direction that the DNA moves, into the chiller and then back into the chamber. The power supply applies a constant voltage across opposing electrodes, and the switcher is used to determine how quickly the voltage switches between the electrodes and the length of the run. (See Figure A-1.) Chapter 3 Materials and Methods 3.1 Materials The human breast cancer cell lines BT20, BT549, HTB26, Hs578T and MCF7 were obtained from the American Tissue Culture Collection (ATCC). The HL60 cell line, a human myeloid leukemia cell line, was also obtained from the ATCC. The breast cancer cell lines grew attached to the petri plates, and the HL60 cells grew in suspension. The estrogen receptor and p53 gene status of the cell lines were obtained from the ATCC and a review of current literature. A summary of this information is given in Table 3.1. 3.2 Tissue Culture Cells were grown in media as given in Table 3.2. The cells were kept in exponential growth by passaging twice weekly. The cells were trypsinized and plated at a low enough concentration to ensure that they were in exponential growth and did not reach plateau phase. In addition, cell counts were done to determine the doubling time of each line. With the exception of the HTB26 cell line, the cells were maintained in an incubator at 37°C with 5% CO 2 . The HTB26 cells were grown at 37 0 C with no ()CO2 Table 3.1: Characteristics of Cell Lines Estrogen receptor information and the status of the p53 and bcl-2 genes were obtained from the ATCC catalogue and a review of the current literature. II I bcl-2 Status jReferences Cell Line I Estrogen Receptors Ip53 Status [17] normal null yes HL60 [16, 5] point mutation unknown BT20 no [5] point mutation unknown no BT549 unknown ATCC, [20, 23] mutant no Hs578T [43, 56, 5] HTB26 no point mutation unknown MCF7 yes normal normal [3, 48, 23, 61] 3.3 Treatment of Cells used in Conventional Gel Electrophoresis The breast cancer cell lines were treated with either X-rays or the drug Tamoxifen Citrate, and the DNA analysed on an agarose gel. Since these gels only run for three to six hours, the presence of a DNA ladder is a quick indication of death by apoptosis. The cells were treated when they were in exponential growth, and daily samples were taken for six to eight days. The possibility of apoptotic bodies in the media that did not form part of the pellet during centrifugation was examined in previous experiments. In those experiments, the media was collected after centrifugation, and any DNA present was isolated. In the cases where there were no DNA ladders present in the DNA from the cell pellet, there was no evidence of ladders in the media. In the one case where there was a DNA ladder from the cell pellet, there was a faint ladder in the DNA isolated from the media. Thus it was inferred that analysing the media was not a necessary procedure. Table 3.2: Maintenance of Cell Lines Doubling time (DT) information was determined for each cell line from regular maintenance of the cells. Fetal calf serum, bovine insulin, sodium pyruvate, non-essential amino acids and L-glutamine were obtained from Sigma Chemical Company, St.Louis, MO. PenicillinStreptomycin (100 U/ml penicillin, 100 ig/ml streptomycin) was obtained from Gibco/BRL, Grand Island, NY. Cell Line Growth Medium D HL60 BT20 24 hours 2 days BT549 RPMI 1640; 15% FCS; 10 mM Hepes; P/S MEM; 20% FCS; 10 mM Hepes; 1 mM Non-essential Amino Acids; P/S RPMI 1640; 20% FCS; 10 mM Hepes; 1 1.5 days P/S Hs578T HTB26 DMEM; 20% FCS; 10 mM Hepes; 10 pg/ml insulin; P/S Leiboweitz-15; 20% FCS; 10 mM Hepes; L-glutamine; 2.5 days 2 days P/S MCF7 MEM; 20% FCS; 10 mM Hepes; 1 mM Non-essential Amino Acids; 1 mM Sodium Pyruvate; 10 Mg/ml insulin; P/S 2 days 3.3.1 Screening of Cell Lines for Radiation-Induced Apoptosis One to two million cells were plated onto 100 or 150 mm plates and grown in standard media conditions. The cells were treated the next day with 25 Gy (1.95 Gy/min) Xrays in air, using a Siemens Stabilipan 2 X-ray generator operated at 250 kVp, 12 mA, effective HVL 0.5 mm Cu. Daily counts were done using a hemocytometer and confluency conditions noted. (It has been reported that confluent conditions may induce apoptosis [29].) The cells were then collected, and the DNA examined for any evidence of apoptotic ladders on an agarose gel. 3.3.2 Screening of Cell Lines for Tamoxifen-Induced Apoptosis The cells were plated as in radiation experiments and allowed to attach overnight. Tamoxifen Citrate (Sigma Chemical Company, St. Louis, MO) in EDTA was then added to the media to give a final concentration of 10 pM and left on the cells for the duration of the experiment. The cells were observed and counted daily. DNA was isolated from the cells at the desired time points and visualized on an agarose gel. 3.3.3 DNA Isolation The cells were detached from the plate by trypsin or scraping, and the cells and media spun at 1000 - 1500 rpm for five minutes. The supernatent was discarded and the cell pellet resuspended in 500 pl of 1X lysis buffer (10 mM Tris; 1 mM EDTA; 0.2% TritonX -100; pH to 7.5). The cells and lysis buffer were then incubated at 37 0 C with 50 pg/ml of Ribonuclease A for one hour. Subsequently, 50 pg/ml of Proteinase K was added, and the suspension incubated for another hour. The DNA was precipitated by adding 500 pl of 100% isopropanol and 100 pl of 5 M NaC1, and leaving samples in the -200 C freezer overnight. Afterwards, the mixture was spun at 13 000g for 10 minutes at 40 C, the supernatent discarded and the pellet allowed to air dry. The DNA pellet was resuspended in 1X TE buffer (10 mM Tris: pH 7.4; 1 mM EDTA: pH 8.0) to a concentration of 106 cells/100 pl. 3.3.4 Conventional Gel Electrophoresis To observe the DNA, the samples were run on 1% agarose gels with a running buffer of 1X TBE (0.0445 M Tris; 0.0445 M Boric Acid; 0.01 M EDTA, pH 8.0). A 1 kb (Gibco/BRL) DNA ladder was used to estimate the sizes of the DNA in the samples. Gel loading buffer was added to the DNA, and the samples heated to 650 C for ten minutes. The samples were then loaded into the gel and run at either 130V for 34 hours (15 cm X 25 cm gel) or 160V for 3.5-6 hours (20 cm X 40 cm gel). Gels were stained for 30 minutes in ethidium bromide and destained for 12-18 hours in water. The DNA was observed by ultraviolet light, and photographs were taken with a Polaroid MP-4 Land Camera with 667 Poloroid film under UV illumination. 3.4 Treatment of Cells used in Pulsed Field Gel Electrophoresis The cells were treated with X-rays and collected in a manner similar to that used for conventional electrophoresis. Once a pellet of cells was obtained, the pellet was resuspended in 1% low melt agarose (Biorad) in 1X lysis buffer. The agarose mixture was then cast into the plug molds and placed at 4oC for 30 minutes to harden. Each plug holds about 200 pl and can be used for two gels. The agarose solution was added to the pellet so that 106 cells would be loaded onto each gel. The plugs were placed in 1 ml of 1X lysis buffer with Proteinase K (50 pg/ml) and incubated at 37°C for 18 - 24 hours. At the end of this incubation period the agarose plugs were rinsed twice in 1 ml of TE for 15 minutes. The plugs were stored in 1 ml of 1X TE until they were needed for electrophoresis. In some instances, the plug wash was kept so that it could be analysed by conventional electrophoresis. To isolate the DNA, the plug wash was placed in the freezer overnight with 500 pl of 100% isopropanol and 100 p1 5M NaC1. The isolated DNA was run on a conventional gel at the conditions described above. In addition, in certain experiments the agarose plugs were also run on conventional gels. 3.4.1 Pulsed Field Gel Electrophoresis The agarose plugs were run on a 1% agarose gel (Pulsed Field Certified Agarose from Biorad) made with 0.5X TBE and a running buffer of 0.5X TBE. The plugs were cut to fit the size of the wells on the gel using a clean, sharp spatula. They were then placed in the well, being careful to make sure that the plug made contact with the front of the well and that all bubbles were eliminated from the wells. The wells were then sealed along the back, the sides and the top with 0.8% low melt agarose. The agarose hardened for half an hour at room temperature or 10 minutes in the cold room. In addition, MegaBaseII (Gibco/BRL) and 1 kb (Gibco/BRL) DNA ladders were loaded to determine the approximate size of the DNA fragments. (The ladders were suspended in 0.8% low melt agarose plugs and loaded in the same manner as the samples.) The CHEF-DR II Electrophoresis System was filled with 2 liters of the 0.5X TBE, the running buffer. The pump was turned on and the circulating buffer cooled to 140 C using a Model 1000 Mini-Chiller, and then the buffer was further circulated at 140 C for half an hour. The gel was then placed in the gel box, and the flow of the buffer was adjusted so that it did not float away or trap bubbles under the gel. The running buffer was drained out of the system until it was 3-4 mm above the level of the gel. The run conditions were set with a Pulsewave 760 switcher and a Model 200/2.0 Constant Voltage Power Supply. When the gel was run for a long time, the running buffer was changed every 48 hours. At the end of the run, the DNA was stained with ethidium bromide, visualized with ultraviolet light and photographed. 3.4.2 Experiment 1: Establishing PFGE Run Conditions Using HL60 cells The HL60 cell line is known to undergo radiation-induced apoptosis starting at about 3 hours after irradiation. The cells are treated according to the method described above, and the DNA separated by conventional and pulsed field gels. The conditions that show large (50kb) fragments are 100V, 60s - 60s switching, for 0.3 hr, followed by 200V, ls-60s, for 22 hr. At this point the gel was stained, destained and photographed. The gel was then run for another 19 hours at 200V, 50s-80s. 3.4.3 Experiment 2: Analysis of Radiation-Induced Apoptosis in Breast Cancer Cell Lines The five breast cancer cell lines were treated with 25 Gy as described above. For each cell line daily samples were collected and made into plugs. The agarose plugs were analysed by PFGE, and the plug wash was run on a conventional agarose gel. The pulsed field run conditions were similar to those used with HL60 samples. Chapter 4 Results 4.1 4.1.1 Screening on Conventional Gels Effect of Irradiation None of the five breast cancer cell lines showed any DNA fragmentation patterns that would indicate apoptosis in response to radiation. The BT549 cell line showed very faint DNA ladders in both the control and radiation experiments. However, this was likely a result of the large number of cells present. (The plates were 90% confluent by day 2 of the experiment.) When the experiment was repeated with larger plates (150 mm), there was no ladder except in the case of day 7 on the untreated samples. At early time points, all cell lines showed large molecular weight DNA. This DNA was larger than the largest size marker (12 kb) (Figure 4-1). In many cases, there was a large fraction of DNA in the area between the wells on the gel and the largest marker (Figure 4-2). As the time increased, the smears of low molecular weight DNA became more prominent. This type of smearing is indicative of necrosis. 4.1.2 Effect of Tamoxifen No tamoxifen-induced apoptosis was detected by the formation of apoptotic DNA ladders. The DNA smears obtained on the gels were similar to those obtained from the radiation experiments (Figure 4-3). BT549 (grown on 100 mm plates) Tamoxifen Untreated 01 2 3 456 7 8 0123 45 Radiation MW 1 234 56 7 b(p) 2216 072 054 036 636 018 06,517 BT549 (grown on 150 mm plates) Untreated 01 2 3 4 56 Radiation 0 1 23 4 56 7 MW (bp) 12216 4072 3054 2036 1 636 1 018 506,517 Figure 4-1: Conventional gel electrophoresis of DNA extracted from BT549 cells. The cells grown on 100 mm plates showed very faint apoptotic ladders. When the same number of cells (106) cells were grown on 150 mm plates, no ladders are observed. The horizontal axis is time measured in days. BT20 Tamoxifen Control 1 3456 7 012 •4 Radiation 5 MW (bp) 1 234567 12216 4072 3 054 2036 1 636 1 018 Hs578T Control 0123 Radiation 4 0 1 2 34 5 MW (bp) 2216 072 054 036 636 Figure 4-2: Conventional gel electrophoresis of DNA extracted from BT20 and Hs578T cells following irradiation with 25 Gy. The horizontal axis is measured in days. MCF7 Control 0 1 23 4 5 6 Tamoxifen 0 2 4 5 6 MW (bp) 12216 S072 3054 2036 1636 HTB26 BT549 Tamoxifen S1 Tamoxifen [w "34 A S 6 bp) 2216 072 054 036 636 018 ~r_____~_ A~ r(-____-IL~-l-l -- 1 -1--I- r igure 4-3: .onvenuional get electropnoreis or u"tIN j extracteu from IMvIr t, HTB26 and BT549 cells following treatment with 10 pM Tamoxifen. The horizontal axis is time measured in days. 4.2 Screening on Pulsed Field Gels 4.2.1 Setting Conditions Using HL60 cells Treating HL60 cells with 25 Gy of radiation produced the expected result of apoptotic ladders on conventional electrophoresis gels. When this experiment was ananlysed on pulsed field gels, two molecular weight DNA bands were observed (see Figure 4-4). The run conditions were set according to the movement of the MegaBaseII and 1 kb DNA ladders.. 4.2.2 Screening of Irradiated Breast Cancer Cell Lines Observing the DNA of the breast cancer cells on pulsed field gels generally did not distinguish any significant bands of large molecular weight DNA. The smears of DNA observed in conventional electrophoresis were also observed on pulsed field gels during the first half of the run (200V; 1-60s; 22 hours). These smears were obtained on controls, as well as on the treated samples (see Figure 4-5). During the second half of the run, no significant DNA staining occurred with the ethidium bromide. The exception was with the MCF7 control experiment which showed a band at 291-485 kb, which decreased as time increased (see Figure 4-6). Otherwise, there were faint DNA smears and no particular DNA bands could be identified. 4.3 Cell Counts after Irradiation and Tamoxifen Treatment The irradiated cells, generally decreased in number after treatment (Figures 4-7, 48, 4-9). The decreased cell count was accompanied by increasing numbers of cells floating in the media. This was observed in all cell lines after day 3 and was particluarly noticible in BT549 cells which detatched in small clumps. Cell lines that were treated with tamoxifen varied in their cell counts. The BT20, BT549, Hs578t and HTB26 cell lines grew at a comparable rate to untereated controls. HL60 Conventional Gel 0123456 M Ell1 bp) 1216 054 036 636 018 )6,517 Pulsed Field Gel 22 hours MW (Kbp) 0 25 Gv -J 32 hours XMWlI 0 25 Gv (Kbp) 291485 48.5 48.5 Figure 4-4: HL60 cells following 25 Gy of irradiation. The top panel shows a conventional agarose gel, where the horizontal axis is time measured in hours. The bottom panels show pulsed field gels run for 22 hours (left) and 32 hours (right). The samples were take at 6 hours after treatment. Pulsed Field Gels HTB26 - Untreated HTB26- 25 G y 0 1 0123456 34 6 7 MW (khn) 48.5 Conventional Gels of Plug Wash HTB26 - Untreated 01234567 HTB26- 25 Gy 1234567 Figure 4-5: PFGE of HTB26 cells following 25 Gy of irradiation. The bottom panel shows conventional electrophoresis of the plug wash. The horizontal axis is time measured in days. Pulsed Field Gels MCF7 -Untreated MW MCF7 - 25Gy 012345 01234567 6 7 (kbp) 194.0 145.5 48. 5 Conventional Gel of Plug Wash MCF7 - Untreated 01234567 MCF7 - 25 Gy 1234567 Figure 4-6: PFGE of MCF7 cells following 25 Gy of irradiation. The bottom panel shows conventional electrophoresis of the plug wash. The horizontal axis is time measured in days. The tamoxifen treated MCF7 cells grew at a slower rate than the control cells ( 4-8. Graph of Normalised Cell Count vs. Time for BT20 Cell Line 100.0 10.0 1.0 0.1 0 4 Time/Days 2 6 Graph of Cell Count vs. Time for BT549 Cell Line 100.00 10.00 1.00 0.10 0.01 0 2 4 Time/Days Figure 4-7: Normalised Cell Counts for the BT20 and BT549 cell lines. The Normalised Cell Count is the number of cells counted on Day 0 divided by the cell count on a particular day. Squares = Untreated cells. Circles = 25 Gy. Triangles = 10 IiM Tamoxifen. Graph of Normalised Cell Count vs. Time for HTB26 Cell Line 10.00 5.00 2.00 1.00 0.50 0.20 0.10 0.05 0 2 4 Time/Days 6 Graph of Normalised Cell Count vs. Time for MCF7 Cell Line 50.0 20.0 010.0 5.0 c 2.0 E 1.0 zo 0.5 0.2 0 2 4 Time/Days Figure 4-8: Normalised Cell Counts for the HTB26 and MCF7 cell lines. The Normalised Cell Count is the number of cells counted on Day 0 divided by the cell count on a particular day. Squares = Untreated cells. Circles = 25 Gy. Triangles = 10 pM Tamoxifen. Graph of Normalised Cell Count vs. Time for Hs578T Cell Line 10.0 5.0 2.0 1.0 0.5 0.2 0.1 0 2 4 Time/Days Figure 4-9: Normalised Cell Counts for the Hs578T cell line. The Normalised Cell Count is the number of cells counted on Day 0 divided by the cell count on a particular day. Squares = Untreated cells. Circles = 25 Gy. Triangles = 10 pM Tamoxifen. Chapter 5 Analysis and Conclusions Screening the five breast cancer cell lines showed that they did not produce radiationor tamoxifen-induced apoptosis as revealed by DNA ladders on conventional electrophoresis gels or large molecular weight bands on pulsed field gels. The DNA that was observed on both electrophoresis and conventional gels is indicitive of intact chromosomal DNA and necrosis. However, the ability of at least one of the cell lines to apoptose was demonstrated when it appeared that highly confluent conditions induced a faint DNA ladder in BT549 cells. This appeared on day 5, and the pertri plates had been 100% confluent since day 3. The pulsed field gels were equally elusive in producing evidence of apoptosis. Both the control and radiation experiments produced DNA around the 50 kb mark. However, this appeared to be the top of the smears that show up as necrosis on the conventional gels, as opposed to being distinct bands of DNA. In the MCF7 cell line it is clear that on the controls the intensity of the bands decreases as the time increases. This corresponds with the analysis that the cells are becoming more necrotic and the DNA being degraded as time progresses. In the radiation experiment, the high molecular weight bands decrease after day 2, and definite smears are visible on later days. This correlates with the observation that the cells are detatching (and presumably dying) on day 3 and later. Similar results were obtained with the other cell lines. The lack of DNA fragmentation in response to radiation is interesting. Four out of the five breast cancer cell lines have p53 mutations. This might suggest an explanation for their resistance to a p53 pathway to apoptosis. However, the MCF7 cell line has two copies of wildtype p53 genes and still does not undergo apoptosis. This is consistent with suggestions that MCF7 cells and more generally solid tumor cell line are resistant to p53-mediated radiation-induced apoptosis [22, 8]. In addition, the possible involvement of the bcl-2 gene in the apoptotic pathway in breast cell lines is unknown. The expression of the p53 and bcl-2 protein products in breast cell lines was studied by Haldar et al. [24]. This work showed that in the BT20 and Hs578T lines there were high levels of p53 and no bcl-2 present; in the MCF7 cell line, bcl-2 was present, but very little p53; and in the HTB26 line comparable levels of both proteins were present. However, the status of bcl-2 gene mutations in the cell lines was not reported. If wildtype bcl-2 is present in these cell lines, its expression after radiation may serve as an inhibitor of apoptosis. Any effects of tamoxifen on the breast cancer cell lines, if present, are more subtle than with the radiation treatment. While the irradiated cells detatched from the plates after a couple of days, the tamoxifen-treated cells continued to divide. Only in the MCF7 cell line was there a slight growth delay. In both situations, the tamoxifen did not appear to be contributing to cell death. These results do not agree with other work which shows tamoxifen-induced apoptosis in MCF7 cells [4] and tamoxifeninduced growth delays in MCF7 and BT20 cells [12, 60]. In the study that found apoptosis in MCF7 cells, the lack of apopotsis in BT20 and HTB26 cells was also demonstrated [4]. The MCF7 cell line is the only one that has estrogen receptors and the BT20 line has high affinity antiestrogen receptors [12]. This might explain the ability of these cell lines to experience growth delays. 5.1 5.1.1 Improvements in the Screening Technique Radiation-Induced Apoptosis Since the irradiated cells showed a propensity to detatch from the plates, further study of them versus the attatched cells would be useful. Isolating the media and detatched cells and subjecting them to conventinal and pulsed field electrophoresis, will help determine if it is purely necrotic cells that are detatching. In addition, if there is any apoptosis that is being masked by the more dominant levels of necrosis, it is more likely to be seen in this analysis. Another change would be to perform the screening at different radiation doses. Since apooptosis is seen in a wide range of doses (2.5 - 25 Gy), it is possible that the high dose used here overrode the apoptosis mechanism and induced necrosis. 5.1.2 Tamoxifen-Induced Apoptosis The effect of different concentrations of tamoxifen needs to be investigated. It may also be useful to use hydroxy-tamoxifen which has much higher affinity (30 -100X) for estrogen receptors than tamoxifen [28]. The effect of phenol red in the media on the results should also be characterised. Phenol red is a weak estrogen and would therefore compete with tamoxifen for receptor cites. However, on experiments done with BT20 cell line, this effect was not major [12]. The concentration of fetal calf serum used in the media could also affect the response to tamoxifen. Chouvet et al. show that high serum concentration reduced the growth inhibitory effects of tamoxifen [12]. One possibility is that there there is estrogen in the serum that competes with tamoxifen for the estrogen receptor sites. 5.2 Future Work Since gel electrophoresis techniques did not provide any evidence of apoptosis, it is necessary to employ morphological techniques to screen for apoptosis. DNA end labelling techniques could be used to identify any fragmentation that occurs. However, since DNA fragmentation does not show up on agarose gels, the efficacy of the technique is questionable. The other option is to observe the cells directly for changes in chromatin and membrane structure. Further investigations of apoptosis in breast cancer cell lines will require the use of molecular biology techniques. Manipulating the expression of wildtype or mutant forms of the p53 and bcl-2 genes will answer the question of whether their state affects the cell death pathway in these cell lines. Investigating the status of other genes that are involved with cell proliferation or death may also be useful in establishing the ability of breast cells to apoptose. Discovering mechanisms to induce or enhance apoptosis by the methods used in the treatment of breast cancer will lead to the improvement of these treatments and survival of the patient. Therefore work to establish the mechanisms and pathways leading to apoptosis warrants further investigation. Appendix A Schematic of the CHEF-DR II System Model 200/2.0 Pulsewave 760 Switcher Power Supply Figure A-1: A schematic showing the set-up of Biorad's CHEF-DR II Pulsed Field Gel Electrophoresis System [6]. Bibliography [1] T. V. Anilkumar, C. E. Sarraf, and M. R. Alison. The biology and pathology of programmed cell death (Apoptosis). Vet Hum Toxicology, 34(3):251-254, 1992. [2] M. J. Arends, R. G. Morris, and A. H. Wyllie. Apoptosis: The role of the endonuclease. American Journal of Pathology, 136(3):593-608, 1990. [3] D. K. Armstrong, J. T. Issacs, Y. L. Ottaviano, and N. E. Davidson. Programmed cell death in an estrogen-independent human breast cancer cell line, MDA-MB 468. Cancer Research, 52:3418-3424, 1992. [4] S. Bardon, F. Vignon, P. Montcourrier, and H. Rochefort. Steroid receptormediated Cytotoxicity of an antiestrogen and an antiprogestin in breast cancer cells. Cancer Research, 47:1441-1448, 1987. [5] J. Bartek, J. Bartkova, B. Vojtesek, Z. Staskova, A. Rejthar. J. Kovarik, and D. P. Lane. Patterns of expression of the p53 tumour suppressor in human breast tissues and tumorus in situ and in vitro. Oncogene, 46(5):839-844, 1990. [6] Biorad. CHEF-DR II: Pulsed Field Gel Electrophoresis System, Instruction Manual and Applications Guide. Bio-Rad Laboratories, Richmond, California, 1988. [7] Bruce Birren and Eric Lai. Pulsed Field Gel Electrophoresis:A Practical Guide. Academic Press, Inc., San Diego, California, 1993. [8] D. G. Brachman, M. Beckett, D. Graves, D. Haraf, E. Vokes, and R. R. Veichselbaum. p53 mutation does not correlate with radiosensitivity in head and neck cancer cell lines. Cancer Research, 53:3666-3669, 1993. [9] D. G. Brown, X-M. Sun, and G. M. Cohen. Dexamethasone-induced apoptosis involves cleavage of DNA to large fragments prior to internucleosomal fragmentation. Journal of Biological Chemistry, 268(5):3037-3039, 1993. [10] M. Caleffi, M. W. Teague, R. A. Jensen, C. L. Vnencak-Jones, W. D. Dupont, and F. F. Parl. p53 gene mutations and steroid receptor status in breast cancer: Clincopathological correlations and prognostic assessment. Cancer, 73(8):21472156, 1994. [11] S-K Chiou, L. Rao, and E. White. Bcl-2 blocks p53-dependent apoptosis. Molecular and Cell Biology, 14(4):2556-2563, 1994. [12] C. Chouvet, E. Vicard, L. Frappart, N. Falette, M. F. Lefebvre, and S. Saez. Growth inhibitory effect of 4-Hydroxy-Tamoxifen on the BT-20 mammary cancer cell line. Journal of Steroid Biochemistry, 31(4B):655-663, 1988. [13] A. R. Clarke, C. A. Purdie, D. J. Harrison, R. G. Morris, C. C. Bird, M. L. Hooper, and A. H. Wyllie. Thymocyte apoptosis induced by p53-dependent and independent pathways . Nature, 362:849-852, 1993. [14] G. M. Cohen, X-M. Sun, R. T. Snowden andD. Dinsdale, and D. N. Skilleter. Key morphological features of apoptosis may occur in the absence of internucleosomal DNA fragmentation. Biochemistry Journal,286:331-334, 1992. [15] R. J. Collins, B. V. Harmon, G. C. Gobe, and J. F. R. Kerr. Internucleosomal DNA cleavage should not be the sole criterion for identifying apoptosis. International Journal of Radiation Biology, 61:451-453, 1992. [16] B. Cypriani, C. Tabacik, B. Descomps, and A. Crastes de Paulet. Role of estrogen receptors and antiestrogen binding sites in an early effect of antiestrogens, the inhibition of cholesterol biosynthesis. Journalof Steroid Biochemistry, 31(5):763771, 1988. [17] L. Danel. Distribution of androgen and estrogen receptors among lymphoid and haemopoietic cell line. Leukemia Research, 9(11):1373-1378, 1985. [18] P. G. deGennes. Reptation of a polymer chain in the presence of fixed obstacles. Journal of Chemical Physics, 55:272, 1971. [19] J. M. Deutsch. Theoretical aspects of electrophoresis. In Eric Lai and Bruce W. Birren, editors, Electrophoresis of Large DNA Molecules: Theory and Applications, number 1 in Current Communications in Cell and Molecular Biology, chapter 3. Cold Spring Harbor Laboratory Press, Plainview, New York, 1990. [20] D. Eliyahu, S. Evans, N. Rosen, S. Elihayu, J. Zwiebel, S. Paik, and M. Lippman. p53Val135 temperature sensitive mutant suppresses growth of human breast cancer cells. Breast Cancer Research Treatment, 30(2):167-177, 1994. [21] V. G. Evans. Multiple pathways to apoptosis. Cell Biology International, 17(5):461-476, 1993. [22] S. Fan, M. L. Smith, D. J. Rivet, D. Duba, Q. Zhan, K. W. Kohn, A. J. Fornace, and P. M. O'Conner. Disruption of p53 function sensitizes breast cancer MCF-7 cells to Cisplatin and Pentoxifylline. Cancer Research, 55:1649-1654, 1995. [23] D. Goldstein, S. M. Bushmeyer, P. L. Witt, V. C. Jordan, and E. C. Borden. Effects of type I and II interferons on cultured human breast cells: interaction with estrogen receptors and with tamoxifen. CancerResearch, 49(10):2698-2702, 1989. [24] S. Haldar, M. Negrini, M. Monne, S. Sabbioni, and C. Croce. Down-regulation of bcl-2 by p53 in breast cancer cells. Cancer Research, 54:2095-2097, 1994. [25] A. L. Harris. p53 expression in human breast cancer. Advances in Cancer Research, 59:69-88, 1992. [26] I. C. Henderson, J. R. Harris, D. W. Kinne, and S. Hellman. Cancer of the breast. In V. T. DeVita, S. Hellman, and S. A. Rosenberg, editors, Cancer. Principles & Practice of Oncology. Lippincott, Philadelphia, 1989. [27] V. C. Jordan. Long-term adjuvant tamoxifen therapy for breast cancer. Breast Cancer Research and Treatment, 15:125-136, 1990. [28] B. S. Katzenellenbogen, M. J. Norman, R. L. Eckert, S. W. Peltz, and W. F. Mangel. Bioactivities, estrogen receptor interactions, and plasminogen activatorinducing activities of tamoxifen and hydroxy-tamoxifen isomers in MCF-7 human breast cancer cells. Cancer Research, 44:112-119, 1984. [29] J. F. R. Kerr, C. M. Winterford, and B. V. Harmon. Apoptosis: Its significance in cancer and cancer therapy. Cancer,73:2013-2026, 1994. [30] J. F. R. Kerr, A. H. Wyllie, and A. R. Currie. Apoptosis: A basic biological phenomenon with wide-ranging implications in tissue kinetics. British Journal of Cancer, 26:239-257, 1972. [31] N. Kyprianou, H. F. English, N. E. Davidson, and J. T. Isaacs. Programmed cell death during regression of the MCF-7 human breast cancer following estrogen ablation. Cancer Research, 51:162-166, 1991. [32] J. M. Lee, J. L. A. Abrahamson, and A. Bernstein. DNA damage, oncogenesis and the p53 tumour-suppressor gene. Mutation Research, 307:573-581, 1994. [33] J. M. Lee and A. Berstein. p53 mutations increase resistance to ionizing radiation. Proceedings of the National Academy of Science USA, 90:5742-5746, 1993. [34] S. V. Lennon, S. J. Martin, and T. G. Cotter. Dose-dependent induction of apoptosis in human tumour cell lines by widely diverging stimuli. Cell Prolif., 24:203-214, 1991. [35] A. J. Levine, J. Momand, and C. A. Finlay. The p53 tumour suppressor gene. Nature, 351:453-456, 1991. [36] C. C. Ling, C. H. Chen, and W. X. Li. Apoptosis induced at different dose rates: implication for the shoulder region of cell survival curves. Radiotherapy and Oncology, 32:129-136, 1994. [37] S. J. Martin and T. G. Cotter. Ultraviolet B irradiation of human leukaemia HL60 cells in vitro induces apoptosis. International Journal of Radiation Biology, 59:1001-1016, 1991. [38] A. J. Merritt, C. S. Potten, C. J. Kemp, J. A. Hickman, A. Balmain, D. P. Lane, and P. A. Hall. The role of p53 in spontaneous and radiation-induced apoptosis in the gastrointestinal tract of normal and p53 deficient mice. Cancer Research, 54:614-617, 1994. [39] R. E. Meyn, L. C. Stephens, K. K. Ang, N. R. Hunter, W. A. Brock, L. Milas, and L. J. Peters. Heterogeneity in the development of apoptosis in irradiated murine tumours of different histologies. InternationalJournal of Radiation Biology, 64(5):583-591, 1993. [40] T. Miyashita and J. C. Creed. bcl-2 gene transfer increases relative resistance of S49.1 and WEH17.2 lymphoid cells to cell death and DNA fragmentation induced by glucocorticoids and multiple chemotheraputic drugs. Cancer Research, 52:5407-5411, 1992. [41] N. Mori, M. Okumoto, J. Morimoto, S. Imai, T. Matsuyama, Y. Takamori, and O. Yagasaki. Genetic analysis of susceptibility to radiation-induced apoptosis of thymocytes in mice. InternationalJournal of Radiation Biology, 62:153-159, 1992. [42] H. Nakano and K. Shinohara. X-Ray-induced cell death: Apoptosis and necrosis. Radiation Research, 140:1-9, 1994. [43] M. Negrini, S. Sabbioni, S. Haldar, L. Possati, A. Castagnoli, A. Corallini nad G. Barbanti-Brodano, and C. M. Croce. Tumor and growth suppression of breast cancer cells by chromosome 17-associated functions. Cancer Research, 54(7):18181-1824, 1994. [44] I. Nenci, E. Marchetti, and P. Querzoli. Commentary on human mammary preneoplasia. The estrogen receptor-promotion hypothesis. JournalSteroid Biochemistry, 30:105-106, 1988. [45] F. Oberhammer, J. W. Wilson, C. Dive, I. D. Morris, J. A. Hickman, A. E. Wakeling, P. R. Walker, and M. Sikorska. Apoptotic death in epithelial cells: cleavage of DNA to 300 and/or 50 kb fragments prior to or in the absence of internucleosomal fragmentation. The EMBO Journal, 12(9):3679-3684, 1993. [46] M. Oren. The involvement of oncogenes and tumor suppressor genes in the control of apoptosis. Cancer and Metastasis, 11:141-148, 1992. [47] M. Oren. Relationship of p53 to the control of apoptotic cell death. Seminars in Cell Biology, 5:221-227, 1994. [48] M. C. Pagliacci, R. Tognellini, F. Grignani, and I. Nicoletti. Inhibition of human breast cancer cell (MCF-7) Growth in Vitro by the Somatostatin Analog SMS 201-995: Effects on cell cycle parameters and apoptotic cell death. Endocrinology, 129(5):2555-2562, 1991. [49] C. S. Potten. The significance of spontaneous and induced apoptosis in the gastrointestinal tract of mice. Canc. Met. Rev., 11:179-195, 1992. [50] I. R. Radford and T. K. Murphy. Radiation response of mouse lymphoid and myeloid cell lines. Part III. Different signals can lead to apoptosis and may influence sensitivity to killing by DNA double-strand breakage. InternationalJournal of Radiation Biology, 65(2):229-239, 1994. [51] J. C. Sabourin, A. Martin, J. Baruch, J. B. Truc, A. Gompel, and P. Poitout. Immunocytochemical localization of bcl-2 protein in human breast cancers and its relationship to a series of prognostic markers and response to endocrine therapy. InternationalJournal of Cancer, 59:619-628, 1994. [52] E. F. Scanlon. Breast cancer. In A. I. Holleb, D. J. Fink, and G. P. Murphy, editors, American Cancer Society Textbook of Clinical Oncology. American Cancer Society, Atlanta, Georgia, 1991. [53] D. C. Schwartz and C. R. Cantor. Separation of yeast chromosome-size DNAs by pulsed field gradient gel electrophoresis. Cell, 37:67-75, 1984. [54] C. L. Sentman, J. R. Shutter, D. Hockenbery, O. Kanagawa, and S. J. Korsmeyer. Bcl-2 inhibits multiple forms of apoptosis but not negative selection in thymocytes. Cell, 67:879-888, 1991. [55] P. Serwer and J. L. Allen. Confirmation of double-stranded DNA during gel electrophoresis: fractionation of linear and circular molecules with molecular weights between 3x10 6 and 26x10 6 . Biochemistry, 23:922-927, 1984. [56] M. S. Sheikh, Z. M. Shao, J. C. Chen, X.S. Li, A. Hussain, and J. A. Fontana. Expression of estrogen receptors in estrogen receptor-negative human breast carcinoma clls: modulation of epidermal growth factor-receptor (EGF-R) and transforming growth factor alpha (TGF-a) gene expression. Journal of Cell Biochemistry, 54(3):289 - 298, 1994. [57] H. Steller. Mechanisms and genes of cellular suicide. Science, 267:1445-1462, 1995. [58] L. C. Stephens, K. K. Ang, T. E. Schultheiss, L. Milas, and R. E. Meyn. Apoptosis in irradiated murine tumors. Radiation Research, 127:308-316, 1991. [59] L. C. Stephens, N. R. Hunter, K. K. Ang, and R. E. Meyn. Development of apoptosis in irradiated murine tumors as a function of time and dose. Radiation Research, 135:75-80, 1993. [60] R. L. Sutherland, R. E. Hall, and I. W. Taylor. Cell proliferation kinetics of MCF-7 human mammary carcinoma cells in culture and effects of tamoxifen on exponentially growing and plateu-phase cells. Cancer Research, 43:3998-4006, 1983. [61] B. Vanhaesebroeck, J. C. Reed, D. De Valck, J. Grooten, T. Miyashita, S. Tanaka, R. Beyaert, F. Van Roy, and W. Fiers. Effect of bcl -2 proto-oncogene expression on cellular sensitivity to tumor necrosis factor mediated cytotoxicity. Oncogene, 8(4):1075-1081, 1993. [62] N. I. Walker, R. E. Bennett, and J. F. R. Kerr. Cell death by apoptosis during involution of the lactating breast in mice and rats. The American Journal of Anatomy, 185:19-32, 1989. [63] N. I. Walker, B. V. Harmon, G. C. Gobe, and J. F. R. Kerr. Patterns of cell death. Meth. Achiev. Exp. Pathol., 13:18-54, 1988. [64] N. P. Wang, H. To, W-H. Lee, and E. Y-H. P. Lee. Tumor suppressor activity of RB and p53 genes in human breast carcinoma cells. Oncogene, 8(2):279-288, 1993. [65] T. T. Y. Wang and J. M. Phang. Effects of estrogen on apoptotic pathways in human breast cacner cell line MCF-7. Cancer Research, 55:2487-2489, 1995. [66] R. L. Warters. Radiation-induced apoptosis in a murine T-cell hybridoma. Cancer Research, 52:883-890, 1992. [67] G. T. Williams and C. A. Smith. Molecular regulation of apoptosis: Genetic controls on cell death. Cell, 74:777-779, 1993. [68] A. H. Wyllie. Glucocorticoid-induced thymocyte apoptosis is associated with endogenous endonuclease activation. Nature, 284:555-556, 1980. [69] A. H. Wyllie, J. F. R. Kerr, and A. R. Currie. Cell death: The significance of apoptosis. InternationalReview of Cutology, 68:251-306, 1980.