E C l i n i c a l ... The rise of moral emotions in neuropsychiatry
advertisement

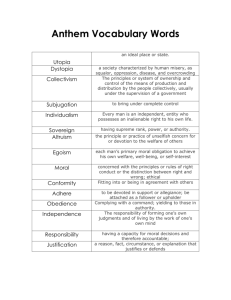
Clinical research The rise of moral emotions in neuropsychiatry Leonardo F. Fontenelle, MD; Ricardo de Oliveira-Souza, MD; Jorge Moll, MD Introduction E arly psychiatrists such as Emil Kraepelin,1 Eugen Bleuler,2 and Kurt Schneider3 have dedicated substantial space in their oeuvres to the discussion of what has been broadly defined as “emotional symptoms.” Clinical (or descriptive) psychopathology, heavily rooted in phenomenological philosophy (as exemplified by Karl Jaspers’ work4), has struggled to provide a conceptual framework to the field for over a century. Broadly speaking, affectivity has been defined as a group of subjective experiences that share transcendence from its own boundaries (for influencing personality and behavior), communicability (for being expressed through verbal and nonverbal means), and polarity (for fluctuating in dual terms, eg, joy and sadness).5 Although concepts such as feelings or sentiments, emotions, mood, and affect have been frequently used in the neuropsychiatric literature, progress in understanding their psychopathological implications has been hindered by: (i) the diver- Clinical psychopathology has largely ignored the developments in the field of social neuroscience. The so-called moral emotions are a group of affective experiences thought to promote cooperation, group cohesion, and reorganization. In this review, we: (i) briefly describe a provisional taxonomy of a limited set of moral emotions and their neural underpinnings; and (ii) discuss how disgust, guilt, anger/indignation, and shame/embarrassment can be conceptualized as key affective experiences in different neuropsychiatric disorders. Based on a concise review of the literature linking moral emotions, psychopathology, and neuropsychiatry, we have devised a simple and preliminary scheme where we conjecture how specific moral emotions can be implicated in some categories of DSM-5 diagnoses, potentially helping to bridge psychopathology and neurobiologically plausible variables, in line with the Research Domain Criteria initiative. We hope this stimulates new empirical work exploring how moral emotional changes and their underlying neurobiology can help elucidating the neural underpinnings of mental disorders. © 2015, AICH – Servier Research Group Author affiliations: D’Or Institute for Research and Education, Rio de Janeiro, Brazil (Leonardo F. Fontenelle, Ricardo Oliveira-Souza, Jorge Moll); Anxiety, Obsessive and Compulsive Spectrum Disorders Program, Institute of Psychiatry of the Federal University of Rio de Janeiro, Brazil (Leonardo F. Fontenelle); Brain and Mental Health Laboratory, School of Psychological Sciences & Monash Institute of Cognitive and Clinical Neurosciences, Monash University, Victoria, Australia (Leonardo F. Fontenelle) Dialogues Clin Neurosci. 2015;17:411-420. Keywords: social cognition; motivation; value; emotion; sentiment; affect; psychiatric disorder; descriptive psychopathology Copyright © 2015 AICH – Servier Research Group. All rights reserved Address for correspondence: Leonardo F. Fontenelle, MD, Anxiety, Obsessive and Compulsive Spectrum Disorders Research Program, Institute of Psychiatry of the Federal University of Rio de Janeiro, Rua Visconde de Pirajá, 547, 617, Ipanema, Rio de Janeiro-RJ, Brazil, CEP: 22410-003 (email: lfontenelle@gmail.com) 411 www.dialogues-cns.org Clinical research sity in their constructs as used by clinicians, social psychologists, and neuroscientists; and (ii) the often tacitly adopted view that the culturally stable “basic emotions” as communicated by facial expressions,6 or that simple two-dimensional valence-arousal models7,8 suffice to capture the complex human emotional make-up. Thus, despite substantial developments in the understanding of human emotions, translation of these advances to the “clinical encounter”9 has been challenging. As thoughtfully put by Keltner and Kring10: “…given the prevalent association between emotion disturbance and psychopathology,11 basic research on emotion and social interaction provides a conceptual framework for considering possible causes and consequences of emotional disturbances as well as potential interventions.” In line with this view, we would like to emphasize that the growing understanding of the psychology and neurobiology of a class of more elaborate emotions (variously called secondary,12 social,13 or moral14) during the last two decades may provide important new insights for psychopathology. Although the importance of this broad class of emotions and their function in regulating social relations and self-evaluation had long been recognized by classical Aristotelian philosophy15 and was elaborated during the Scottish Enlightenment (eg, see Adam Smith’s theory of moral sentiments16), a systematic scientific approach to moral emotions did not begin to be used until quite recently.13,14 The emerging field of moral neuroscience From the psychopathological perspective, early theorists observed that emotions or feelings are often based on “objects” which human beings appraise or refer to, eg, people can love, hate, admire, or disdain something or someone, including themselves. The initial attempts to systematize and classify affectivity on clinical grounds divided evaluative emotions or feelings as negatively or positively valenced, both being potentially referred to (i) self (eg, guilt or pride); or (ii) other people and objects (eg, disgust or affection).3 Thus, it was evident that emotions often assumed social (by involving social information or communication) and often moral (by invoking kinds of social approval or disapproval) contours. Emotions are said to be moral when they reflect the interests or welfare either of society as a whole or at least of persons other than the judge or agent.14 Moral emotions are thought to emerge as neural repre- sentations that rely on the coactivation of brain regions that code for perception of social cues (temporoparietal junction and other posterior cortical regions), social conceptual knowledge (chiefly the anterior temporal cortex), abstract event sequence knowledge (anterior, medial, and lateral sectors of the prefrontal cortex), and basic emotional states (including subcortical structures such as the basal forebrain and hypothalamus).17,18 The ability of moral emotions to aggregate or alienate human beings is often used to categorize such experiences into prosocial and social aversive ones, respectively. Typically, prosocial emotions lead to cooperation, helping, reciprocity, reparative actions, and social conformity, and include guilt, embarrassment, compassion, awe, and gratitude.18,19 Among these, affiliative emotions are those relying on social attachment (ie, parent-infant, filial, and pair-bonding, also known as “proximate” or “basic attachment”) or attachment to nonhuman living beings (eg, nature), cultural symbols, abstract ideas, and beliefs (so-called “extended attachment”), which may explain the remarkable human inclination to cooperate beyond kinship boundaries, even when no reputation gains are at stake.20 Affiliative emotion is a cornerstone for several prosocial emotions that rely on social bonding (ie, guilt, gratitude, and compassion), but less so for those that promote social conformity based on self-interested motivation (eg, embarrassment). In contrast, sentiments linked to interpersonal aversion—the other-critical sentiments (such as disgust, contempt, and anger/indignation)—are experienced when others violate norms or one’s rights or expectations, and endorse aggression, punishment, group dissolution, and social reorganization.14,17 The functional role of moral emotions in regulating social behavior is intrinsically dependent on culture. Culture is the sculptor of moral beliefs and norms, shaping the ways by which elicitors and specifiers lead interpersonal feelings according to contextual elements and social niches. For example, feeling shame when violating some “etiquette” codes in the Victorian era would not apply today in most situations. Similarly, physical violence as a mean to clear one’s honor following a verbal insult (to avoid shame) was commonplace and acceptable not long ago, but is largely rejected today in most Western cultures. Nonetheless, for psychopathology it is important to emphasize that some emotional experiences can be abnormally heightened or blunted after accounting for what is considered to be “normal” in a 412 Dialogues in Clinical Neuroscience - Vol 17 . No. 4 . 2015 Moral emotions in neuropsychiatry - Fontenelle et al given sociocultural niche. Likewise, feelings of blame towards oneself can be heightened in major depression21 and absent in psychopathy.22,23 With this in mind, we believe it is possible to envisage a model of moral emotions that may have heuristic value and allow us to make better predictions regarding psychopathology, behavior dysfunctions, and their neural underpinnings in neuropsychiatric disorders. Moll and colleagues19 proposed a framework for moral emotions, with six main components defined on the basis of their psychological and neurobiological plausibility. In this schematic model, domains of attachment, aggressiveness, and social rank/dominance/selfesteem correspond to basic cognitive and emotional mechanisms that are widely represented across species. In contrast, outcome assessment, agency/intentionality, and norm violation are cognitive capacities readily identifiable in humans that rely more on differentiated integrative systems. It is notably difficult to extrapolate a taxonomy of moral emotions to clinical disorders, however, and any attempt to translate concepts from experimental neuroscience to the “clinical encounter” embedded in the practice of neuropsychiatry should be considered preliminary and taken with a grain of salt. Therefore, much of what will be discussed in this review will require corroboration, correction, and extension from future experimental and theoretical work. In the following sections, we will: (i) briefly describe a provisional taxonomy of a limited set of moral emotions and their putative neural underpinnings19; and (ii) discuss how disgust, guilt, anger/indignation, and shame/embarrassment can be conceptualized as key emotional ingredients in the experiences of patients suffering different neuropsychiatric disorders. A thorough coverage of the emotional space, its neural underpinnings, and psychopathological associations is beyond the scope of the present paper. and experience in humans is often associated with its moral counterparts, including contempt or moral disgust.24 As Haidt14 noted: “In evolution, the function of disgust shifted: a mechanism for avoiding harm to the body became a mechanism for avoiding harm to the soul.” Two dimensions of disgust have been established, one related to the tendency to react with the emotion of disgust (disgust propensity) and the other related to how unpleasant the experience of disgust is to the individual (disgust sensitivity), each thought to be involved in specific forms of psychopathology.25 On an interpersonal level, disgust and contempt sometimes mark distinctions of rank and prestige, especially in hierarchical societies.19 Moral disgust, arguably a more extreme form of contempt that can be a motivational factor for severe antisocial behaviors such as hate crimes and genocides, is evoked by characterological blame to others26 and devaluation of their social status (ie, attribution of lower social value to persons or groups). Contempt and disgust can also be elicited by minor social norm violations in which another person is the agent. Severe social violations will generally trigger indignation instead, and are more associated with behavioral blame. The neural correlates of disgust include the anterior insula, the anterior cingulate, and inferior temporal cortices, the basal ganglia, the amygdala, and the lateral orbitofrontal cortex,19 with preliminary evidence suggesting that more dorsomedial divisions of the prefrontal cortex are recruited by moral disgust.27 Also, there is evidence suggesting that, despite the fact that moral disgust and core disgust share common neural representations, the latter engages the left inferior frontal gyrus more reliably, whereas moral disgust (triggered by taboo stimuli) elicits stronger medial prefrontal cortex and temporoparietal junction cortical responses.28 Psychopathological associations Disgust, contempt, and moral disgust Psychology and neuroscience Disgust has been described as “the revulsion at the prospect of oral incorporation of an offensive contaminating object” in a way that “if they even briefly contact an acceptable food, they tend to render that food unacceptable.” Although disgust is one of the classical “basic emotions” (in this case, “core” disgust), its expression Most work done on the descriptive psychopathology of disgust has been based on its more traditional rather than interpersonal meaning (ie, the so-called “core disgust”). Besides its well-known role in contaminationrelated obsessive-compulsive disorder (OCD), bloodinjection-injury phobia, and small animal phobias,29 abnormal disgust processing is likely to be involved in several other mental disorders, including eating and sexual disorders,29 and other obsessive-compulsive and 413 Clinical research related disorders (OCRDs), such as body dysmorphic disorder (BDD), olfactory reference syndrome (ORS), and hoarding disorder (HD). For instance, in eating disorders, some patients may express disgust for highcalorie foods and overweight body shapes.30 In contrast, women suffering from sexual aversion disorder display a number of sex-related fears, aversion to looking or touching their own or others’ genitalia, and disgust regarding body fluids.31,32 Disgust appears to be an important ingredient of the emotional experience of patients suffering from several “cognitively based” OCRDs. Patients with BDD are preoccupied by and often disgusted by their own appearance,33 while ORS patients believe they emanate obnoxious odors, including “sewage,” “rotten animals” and other fetid smells, which the individual believes generate disgust reactions in other people.34 Some hoarding patients (particularly those who exhibit a severe domestic squalor) may also seem to be insensitive or indifferent to the consequences of hoarding behaviors, including vermin, insects, and extreme filth.35 Lastly, OCD patients may also display a form of selfdisgust for having immoral sexual/religious thoughts.36 Whether increased “interpersonal disgust” or contempt toward others may be found in manic episodes (eg, bipolar disorder), psychotic disorders (eg, delusional disorders, grandiose type), or personality disorders associated with increased self-esteem (eg, narcissistic or other cluster B personality disorders) is an interesting possibility that remains to be investigated. Guilt not required for guilt elicitation, the acknowledgement that a social norm was violated may magnify feelings of guilt,19 suggesting that deontological and altruistic guilt may coexist and have additive effects. Neuroimaging data showed that the experience of guilt is mediated by the anterior prefrontal (frontopolar) cortex, the dorsomedial prefrontal and the lateral orbitofrontal cortex, the anterior temporal cortex, the insula, the amygdala, the anterior cingulate cortex, and the superior temporal sulcus region.19,39,40 In addition, in one study measuring concerns about payoffs to oneself and to others using dictator, ultimatum, and trust games, six patients with ventromedial prefrontal cortex lesions donated significantly less, and were less trustworthy. Mathematical models showed that these patients were abnormally insensitive to guilt, but not to envy.41 The subgenual cortex has been implicated in major depressive disorder (MDD), as well as in individual differences in empathic concern during guilt provocation in normal volunteers.42 In line with these findings, this brain region showed heightened hemodynamic responses in patients with remitted MDD when making altruistic donations,43 which have been previously demonstrated to engage the subgenual cortex in healthy volunteers.44 In addition, evidence obtained in patients with the behavioral variant of frontotemporal dementia suggests that the frontopolar cortex and the septal region are required for guilt.45 Notably, in the later study, impairments of other-critical feelings (anger and disgust) were associated with dorsomedial prefrontal and amygdala dysfunction.45 Psychopathological associations Psychology and neuroscience In contrast to adaptive guilt, “pathological” guilt is motivated by the desire to ensure that the “wrong” is made “right” at the expense of maintaining social norms and mutuality of social relationships.37 Typically, guilt develops when one foresees a bad outcome for another person, recognizes him or herself as the agent of such an outcome, and feels emotionally attached to the damaged person or abstract value (eg, justice, honesty).19 Guilt can derive from the transgression of a moral rule (also termed deontological guilt, eg, “do not play God”) or of a personal altruistic goal (also know as altruistic guilt, eg, feeling guilty for having hurt someone’s feelings).38 Although violations of social norms in themselves are Self-blaming biases, including guilt, have been implicated in MDD (particularly in melancholic forms),21,23,46 post-traumatic stress disorder (PTSD),47 and OCRDs.38 Patients with remitted MDD exhibit an increased selfcontempt bias, ie, less contempt/disgust and indignation towards others despite having unimpaired self-blame (guilt and self-contempt).48 Guilt is thought to play a key role in PTSD, thought it is not clear whether it results from exposure to trauma, depression, shame, or the full-blown clinical syndrome itself.47 There are many OCRDs that have been associated with abnormalities in guilt processing. Studies suggest that OCD is associated with increased sensitivity to deontological, but not altruistic, guilt.38 Also, overscrupulous OCD patients49 414 Dialogues in Clinical Neuroscience - Vol 17 . No. 4 . 2015 Moral emotions in neuropsychiatry - Fontenelle et al and HD patients who find themselves obliged to discard objects to which they are emotionally attached50 may be more prone to manifest increased guilt. In contrast to other OCRD patients, who show heightened experiences of guilt before the execution of their compulsions, trichotillomania, and excoriation (skin picking) disorder, patients tend to display guilt only after they perform their abnormal behaviors and realize the extension of the damage and the social consequences.51 This latter feature is shared by many substance and behavioral addictions (including gambling disorder), disruptive, impulse control, and conduct disorders (ie, intermittent explosive disorder, pyromania, and kleptomania), and paraphilias.52 Psychopathy is a disorder characterized by pronounced emotional deficits, marked by reduction in guilt and remorse, which contribute to their callous and antisocial behaviors. Structural and functional abnormalities have been reported in brain networks implicated in guilt and other prosocial emotions in psychopathy.53,54 For instance, in contrast to individuals characterized by reactive aggressiveness (ie, intermittent explosive disorder), subjects showing psychopathic traits exhibit decreased amygdala and orbitofrontal cortex responses to emotionally provocative stimuli or during emotional learning paradigms (for a review, see Blair55). Anger and indignation Psychology and neuroscience Anger has been defined as a negative affect that arises from the blockage of movement toward a desired goal that “ought to be.”56 Although anger as a basic emotion does not necessarily involve a moral context for its expression (you may get angry at a malfunctioning device or because of a traffic jam), indignation requires the recognition of injustice or other moral violations. It remains unclear, however, whether their emotional experience can be clearly distinguished. Furthermore, anger/indignation and moral disgust share several phenomenological commonalities, but are typically elicited in different contexts: while moral disgust is predominantly felt in response to “bodily moral violations,” such as a lack of respect for sexual or eating taboos,57 anger/indignation is mostly a reaction to violations of sociomoral norms about fairness, harm, or rights in which another person is the agent, especially if the agent acted intentionally.19 Anger/indignation also relies on engagement of aggressiveness, following an observation of bad outcomes to the self or to a third party.19 Typically, anger/indignation evokes activation of the orbitofrontal cortex (especially its lateral division), the dorsomedial prefrontal and frontopolar cortex, the anterior insula, the amygdala, and the anterior cingulate cortex.17,18,28,40 Damage to the amygdala and to the dorsomedial prefrontal cortex in patients with frontotemporal dementia impairs feelings of anger/indignation and disgust.45 Psychopathological associations Anger (and indignation, though seldom mentioned explicitly) is a relatively pervasive emotional experience in everyday life, and prevalent in mental disorders in general. Although it is frequently found in psychosis, mania, and even depression, DSM-5 also lists a number of conditions that exhibit anger or indignation as core diagnostic features, including intermittent explosive disorder, disruptive mood dysregulation disorder, antisocial and borderline personality disorders, and conduct and related disorders, among others.52 Regardless of its etiology, anger can also severely modify the expression of other mental disorders, ie, by increasing the burden on the family, friends, and society as a whole.58 For instance, neurodevelopmental conditions, such as autism spectrum disorders59 and Tourette syndrome,60 are also frequently associated with rage attacks. In OCD, individuals presenting symmetry/ordering symptoms seem particularly prone to exhibit increased anger and aggressiveness.61 As reported above, there is also some evidence showing decreased negative feelings toward the others (especially anger/indignation) among patients with remitted MDD.48 Shame Psychology and neuroscience Shame reflects a concern with a threatened self, which motivates behaviors to restore a positive view of himself or herself.12,62,63 It most probably evolved as an attempt to mitigate the likelihood or costs of reputation-damaging information spreading to others (loss of face).64 In fact, compared with other prosocial emotions, shame uniquely predicts a desire for self- 415 Clinical research Disgust Guilt Anger/indignation Shame Neurodevelopmental disorders Autism spectrum disorders with self-injurious behaviors ↑ Tourette syndrome ↑ ↑ ↑ ↓ Schizophrenia and other psychotic disorders Delusional disorder, grandiose, jealous and persecutory types ↑ Delusional disorder, somatic type ↑ Bipolar and related disorders Manic/hypomanic episode ↓ ↑ ↑ ↓ ↓ Depressive disorders Major depressive episode with melancholic features ↑ Major depressive episode, with atypical features Anxiety disorders ↑ Specific phobia, animal type ↑ Social anxiety disorder Obsessive-compulsive and related disorders Obsessive-compulsive disorder ↑ Concerns about germs and contamination ↑ Concerns about responsibility ↑ Symmetry, completeness, and “just right” ↑ Unacceptable thoughts Body dysmorphic disorder and olfactory reference syndrome ↑ Hoarding disorder ↓ ↑ ↑ ↑ ↑ ↑ ↑ ↑ ↑ ↑ ↑ ↑ ↑ ↑ Trichotillomania and excoriation disorder Trauma- and stressor-related disorders Post-traumatic stress disorder Feeding and eating disorders Eating disorders Sexual dysfunctions Genito-pelvic pain disorder Disruptive, impulse control, and conduct disorders Oppositional defiant disorder ↑ Intermittent explosive disorder ↑ ↑ ↑ ↓ ↓ Conduct disorder ↓↑ Substance-related and addictive disorders ↓↑ Personality disorders ↓ ↑ ↓ Borderline personality disorder ↑ ↓ ↑ ↑ Narcissistic personality disorder ↑ ↓ ↑ ↓ Antisocial personality disorder Table I. Examples of DSM-5 entities and how their predominant moral emotions can help illuminate the pathophysiology of mental disorders. 416 Dialogues in Clinical Neuroscience - Vol 17 . No. 4 . 2015 Moral emotions in neuropsychiatry - Fontenelle et al change.65 It may focus on the body, intimacy and sexuality (bodily shame); on the person’s moral standards, competence, and social exclusion (cognitive shame); or on the person as a whole (existential shame).66 Although shame has been considered a central emotion to the psychopathology of social phobia/social anxiety disorder (SAD), it is probably a much wider concept then merely social anxiety. Similarly, the experience of shame in SAD may be magnified by the expression of particular attitudes by specific groups of patients. For instance, submissive behaviors mediated the relationship between social anxiety and shame in men, but not women, with SAD.67 Shame follows “an action attributed to self-agency that is associated with a violation of a social norm, leading to a bad outcome to oneself (eg, damage to one’s self-image), and reduced self-esteem and social dominance as judged by oneself and others, which is often reliant on the other’s awareness or one’s action.” 19 A similar emotion to shame, embarrassment, follows the violation of less severe social norms or conventions, leading to a non-pervasive or non-characterological reduction of one’s self-image, which is dependent on other’s awareness (being observed).19 Perhaps a milder variation of shame, embarrassment is not thought to be associated with a significant reduction of self-esteem or to a sustained decrease in self-attributed social status.19 In one fMRI study, shame/guilt conditions, as well as pride, activated an emotional circuit including the amygdala, the insula, and the ventral striatum, and the bilateral dorsomedial prefrontal cortex.68 In another study that attempted to disentangle the neural correlates of shame from guilt, both were associated with increased activations in the temporal lobes. However, shame activated most specifically the medial and inferior frontal gyrus, while guilt lead to greater activity in the amygdala and the insula.69 Psychopathological associations While it is difficult to establish the psychopathological significant of embarrassment, an excessive level of shame may be associated with a wide range of psychopathological symptoms. However, a lack of shame may also lead to distress, for instance as it may facilitate violation of social norms and thus may promote interpersonal problems. In one study, SAD patients displayed greater bodily and cognitive shame than community and psychiatric control groups.66 Fortunately, however, shame in SAD seems to be amenable to treatment.70 Increased shame is also often reported in eating disorders,71 PTSD,72 and OCD patients, particularly those with sexual, blasphemous, or hoarding symptoms.73 Finally, the experience of shame may also result from excessive grooming behaviors and their esthetical consequences as in trichotillomania and excoriation disorder, inability to discard items and the resulting clutter in HD, imaginary defects in the appearance in BDD and beliefs about emanating repulsive odors in ORS.74 In the same study reported above,66 while borderline personality disorder patients reported the highest level of “existential” shame (ie, an enduring feeling of shame comprising the person as a whole) as compared with community and other psychiatric control groups, attention deficit/hyperactivity disorder patients exhibited the lowest severity of “bodily” shame. Conclusions It is important for neuropsychiatry to crosstalk with social neurosciences, as research on the neural basis of moral emotions can help inform the pathophysiology of mental disorders and, ultimately, develop innovative diagnostic and treatment targets. Surprisingly, a resurgence of the descriptive psychopathology of emotions, a discipline that has been dormant for more than 50 years, will open up a rich avenue for investigation that has been unduly obliterated by the rise of animal models of emotional processing since the first quarter of the 20th century. Such models, by nature and necessity, largely ignored the uniqueness of human existential and moral feelings.75 Based on a concise review of the literature linking moral emotions, psychopathology, and neuropsychiatry, we have devised a simple and provisional scheme where we conjecture how moral emotions can be disturbed in some categories of DSM-5 diagnoses, potentially helping to bridge psychopathology and neurobiologically plausible variables, in line with the RDoC initiative.76 We hope this stimulates new empirical work exploring how moral emotional changes and their underlying neurobiology can help elucidate the neural underpinnings of mental disorders (Table 1). The identification of neurocircuitries mediating abnormal emotional processing in neuropsychiatric disorders may have implications that transcend the boundaries of neuroanatomy, particularly in terms of cognition, 417 Clinical research neuroendocrinology, and molecular genetics.77 In contrast to more basic psychological constructs such as basic emotions, moral emotions map onto a phenomenological level that is likely to be closer to their neural network, symptomatic and psychological counterparts, thereby representing a very interesting venue for fundamental research and clinical inquiry. This endeavor can also help sharpen ideal targets for different forms of neurostimulation and other neurosurgical procedures, or to better select treatment candidates based on a more personalized approach. While these therapeutic approaches seem relatively aggressive for some of the conditions described in DSM-5, new neuromodulation approaches based on neurotechnological advances, combined with a better knowledge of how distributed brain networks encode specific complex cognitive-emotional states (and traits), such as those associated with moral emotions and different motivations, may help devise effective noninvasive treatments for neuropsychiatric conditions. o REFERENCES 21. O’Connor LE, Berry JW, Weiss J, Gilbert P. Guilt, fear, submission, and empathy in depression. J Affect Disord. 2002;71(1-3):19-27. 22. Hare RD. Psychopathy: a clinical and forensic overview. Psychiatr Clin North Am. 2006;29(3):709-724. 23. O’Connor LE, Berry JB, Lewis T, Mulherin K, Yi, E. Empathy and depression: the moral system on overdrive. In: Farrow TFD, Woodruff PWR, eds. Empathy in Mental Illness. Cambridge, UK: Cambridge University Press; 2007. 24. Rozin P, Lowery L, Imada S, Haidt J. The CAD triad hypothesis: a mapping between three moral emotions (contempt, anger, disgust) and three moral codes (community, autonomy, divinity). J Pers Soc Psychol. 1999;76(4):574-586. 25. van Overveld WJM, de Jong PJ, Peters ML, Cavanagh K, Davey GCL. Disgust propensity and disgust sensitivity: Separate constructs that are differentially related to specific fears. Personal Indiv Diff. 2006;41(7):12411252. 26. Janoff-Bulman R. Characterological versus behavioral self-blame: inquiries into depression and rape. J Pers Soc Psychol. 1979;37(10):1798-1809. 27. Moll J, Zahn R, de Oliveira-Souza R, Krueger F, Grafman J. Opinion: the neural basis of human moral cognition. Nat Rev Neurosci. 2005;6(10):799809. 28. Schaich Borg J, Lieberman D, Kiehl KA. Infection, incest, and iniquity: investigating the neural correlates of disgust and morality. J Cogn Neurosci. 2008;20(9):1529-1546. 29. Davey GC. Disgust: the disease-avoidance emotion and its dysfunctions. Philos Trans R Soc Lond B Biol Sci. 2011;366(1583):3453-3465. 30. Harvey T, Troop NA, Treasure JL, Murphy T. Fear, disgust, and abnormal eating attitudes: a preliminary study. Int J Eat Disord. 2002;32(2):213218. 31. de Jong PJ, van Overveld M, Borg C. Giving in to arousal or staying stuck in disgust? Disgust-based mechanisms in sex and sexual dysfunction. J Sex Res. 2013;50(3-4):247-262. 32. Farnam F, Janghorbani M, Merghati-Khoei E, Raisi F. Vaginismus and its correlates in an Iranian clinical sample. Int J Impot Res. 2014;26(6):230234. 33. Lambrou C, Veale D, Wilson G. The role of aesthetic sensitivity in body dysmorphic disorder. J Abnorm Psychol. 2011;120(2):443-453. 34. Prazeres AM, Fontenelle LF, Mendlowicz MV, et al. Olfactory reference syndrome as a subtype of body dysmorphic disorder. J Clin Psychiatry. 2010;71(1):87-89. 35. Snowdon J, Pertusa A, Mataix-Cols D. On hoarding and squalor: a few considerations for DSM-5. Depress Anxiety. 2012;29(5):417-424. 36. Rachman S. Fear of Contamination: Assessment and Treatment. New York, NY: Oxford University Press; 2006. 37. Shapiro LJ, Stewart ES. Pathological guilt: a persistent yet overlooked treatment factor in obsessive-compulsive disorder. Ann Clin Psychiatry. 2011;23(1):63-70. 38. Mancini F, Gangemi A. Deontological guilt and obsessive compulsive disorder. J Behav Ther Exp Psychiatry. 2015;49(Pt 3):157-163. 39. Wagner U, N’Diaye K, Ethofer T, Vuilleumier P. Guilt-specific processing in the prefrontal cortex. Cereb Cortex. 2011;21(11):2461-2470. 1. Kraepelin E. Lectures on Clinical Psychiatry, by Dr. Emil Kraepelin. New York, NY: Wood; 1917. 2. Bleuler E. Afectividad sugestibilidad, paranoia. Madrid, Spain: Morata; 1942. 3. Schneider K. Clinical Psychopathology. New York, NY: Grune & Stratton; 1959. 4. Jaspers K. General Psychopathology. Baltimore, MD: Johns Hopkins University Press; 1997. 5. Crespo JM. Psicopatología de la afetividad. In: Ruiloba JV, ed. Introducción a la psicopatología y la psiquiatría. Barcelona, Spain: Elsevier Masson; 2006. 6. Ekman P. Are there basic emotions? Psychol Rev. 1992;99(3):550-553. 7. Lang PJ, Bradley MM, Cuthbert BN. International Affective Picture System (IAPS): Affective Ratings of Pictures and Instruction Manual. Gainsville, FL: NIMH, Center for the Study of Emotion & Attention; 2005. 8. Mourao-Miranda J, Volchan E, Moll J, et al. Contributions of stimulus valence and arousal to visual activation during emotional perception. Neuroimage. 2003;20(4):1955-1963. 9. Schattner A. The clinical encounter revisited. Am J Med. 2014;127(4):268-274. 10. Keltner D, Kring AM. Emotion, social function, and psychopathology. Rev Gen Psychol. 1998;2(3):320-342. 11. Thoits PA. The Sociology of Emotions. Ann Rev Sociol. 1989;15(1):317342. 12. Fessler D. Shame in two cultures: implications for evolutionary approaches. J Cogn Culture. 2004;4(2):207-262. 13. Eisenberg N. Emotion, regulation, and moral development. Ann Rev Psychol. 2000;51(1):665-697. 14. Haidt J. The moral emotions. In: Davidson RJ, Scherer KR, Goldsmith HH, eds. Handbook of Affective Sciences. Oxford, UK: Oxford University Press; 2003:852-870. 15. Irwin T. Nicomachean Ethics. 2nd ed. Indianapolis, IN: Hackett Publishing Company; 2000. 16. Haakonssen K. Adam Smith: The Theory of Moral Sentiments. Cambridge, UK: Cambridge University Press; 2002. 17. Moll J, de Oliveira-Souza R, Moll FT, et al. The moral affiliations of disgust: a functional MRI study. Cogn Behav Neurol. 2005;18(1):68-78. 18. Moll J, De Oliveira-Souza R, Zahn R. The neural basis of moral cognition: sentiments, concepts, and values. Ann N Y Acad Sci. 2008;1124:161180. 19. Moll J, De Oliveira-Souza R, Zahn R, Grafman J. The cognitive neuroscience of moral emotions. In: Sinnott-Armstrong W, ed. Moral psychology: The Neuroscience of Morality: Emotion, Brain Disorders, and Development. Vol 3. Cambridge, MA: The MIT Press; 2008:1-17. 20. Moll J, De Oliveira-Souza R. “Extended attachment” and the human brain: internalized cultural values and evolutionary implications.. In: Verplaetse J, de Schrijver J, Vanneste S, Braeckman J, eds. The Moral Brain: Essays on the Evolutionary and Neuroscientific Aspects of Morality: Dordrecht, the Netherlands: Springer; 2009. 418 Dialogues in Clinical Neuroscience - Vol 17 . No. 4 . 2015 Moral emotions in neuropsychiatry - Fontenelle et al El surgimiento de las emociones morales en neuropsiquiatría L’essor des émotions morales en neuropsychiatrie La psicopatología clínica ha ignorado ampliamente los desarrollos en el campo de la neurociencia social. Las así llamadas emociones morales son un grupo de experiencias afectivas que se piensa promueven la cooperación, la cohesión grupal y la reorganización. En esta revisión 1) se describe brevemente una taxonomía provisoria de un conjunto limitado de emociones morales y sus sustratos neurales y 2) se discute cómo el asco, la culpa, la ira/enojo y la vergüenza/bochorno pueden ser conceptualizadas como experiencias afectivas clave en diversos trastornos neuropsiquiátricos. En base a una breve revisión de la literatura que vincula las emociones morales, la psicopatología y la neuropsiquiatría se ha ideado un esquema simple y preliminar donde se supone que las emociones morales específicas se pueden implicar en algunas categorías diagnósticas del DSM-5, ayudando potencialmente a unir las posibles variables psicopatológicas y neurobiológicas, en línea con la iniciativa del Research Domain Criteria. Se espera que esto estimule a nuevos trabajos empíricos que exploren cómo los cambios emocionales morales y su neurobiología subyacente pueden ayudar a dilucidar las bases neurales de los trastornos mentales. La psychopathologie clinique a largement ignoré les développements dans le domaine des neurosciences sociales. Les émotions dites morales sont un groupe d’expériences affectives destinées à promouvoir la coopération, la cohésion de groupe et la réorganisation. Dans cet article, 1) nous décrivons brièvement une taxinomie provisoire d’un ensemble limité d’émotions morales et de leurs fondements neuronaux ; et 2) nous analysons comment il est possible de conceptualiser le dégoût, la culpabilité, la colère/l’indignation et la honte/la gêne comme expériences affectives-clés dans différents troubles neuropsychiatriques. Sur la base d’une revue concise de la littérature associant les émotions morales, la psychopathologie et la neuropsychiatrie, nous avons conçu un projet préalable simple dans lequel nous supposons l’implication des émotions morales spécifiques dans certaines catégories diagnostiques du DSM-5, aidant éventuellement à établir des liens avec des variables psychopathologiques et neurobiologiques crédibles, conformes avec l’initiative des Research Domain Criteria (Critères de domaines de recherche). Nous espérons ainsi stimuler un nouveau travail empirique en étudiant comment les changements moraux émotionnels et leur neurobiologie sous-jacente peuvent permettre de comprendre les fondements neuronaux des troubles mentaux. 40. Kedia G, Berthoz S, Wessa M, Hilton D, Martinot JL. An agent harms a victim: a functional magnetic resonance imaging study on specific moral emotions. J Cogn Neurosci. 2008;20(10):1788-1798. 41. Krajbich I, Adolphs R, Tranel D, Denburg NL, Camerer CF. Economic games quantify diminished sense of guilt in patients with damage to the prefrontal cortex. J Neurosci. 2009;29(7):2188-2192. 42. Zahn R, de Oliveira-Souza R, Bramati I, Garrido G, Moll J. Subgenual cingulate activity reflects individual differences in empathic concern. Neurosci Lett. 2009;457(2):107-110. 43. Pulcu E, Zahn R, Moll J, et al. Enhanced subgenual cingulate response to altruistic decisions in remitted major depressive disorder. Neuroimage Clin. 2014;4:701-710. 44. Moll J, Krueger F, Zahn R, Pardini M, de Oliveira-Souza R, Grafman J. Human fronto-mesolimbic networks guide decisions about charitable donation. Proc Natl Acad Sci U S A. 2006;103(42):15623-15628. 45. Moll J, Zahn R, de Oliveira-Souza R, et al. Impairment of prosocial sentiments is associated with frontopolar and septal damage in frontotemporal dementia. Neuroimage. 2011;54(2):1735-1742. 46. Green S, Lambon Ralph MA, Moll J, Deakin JF, Zahn R. Guilt-selective functional disconnection of anterior temporal and subgenual cortices in major depressive disorder. Arch Gen Psychiatry. 2012;69(10):1014-1021. 47. Pugh LR, Taylor PJ, Berry K. The role of guilt in the development of post-traumatic stress disorder: A systematic review. J Affect Disord. 2015;182:138-150. 48. Green S, Moll J, Deakin JF, Hulleman J, Zahn R. Proneness to decreased negative emotions in major depressive disorder when blaming others rather than oneself. Psychopathology. 2013;46(1):34-44. 49. Miller CH, Hedges DW. Scrupulosity disorder: an overview and introductory analysis. J Anxiety Disord. 2008;22(6):1042-1058. 50. Frost RO, Hartl TL. A cognitive-behavioral model of compulsive hoarding. Behav Res Ther. 1996;34(4):341-350. 51. Arzeno Ferrao Y, Almeida VP, Bedin NR, Rosa R, D’Arrigo Busnello E. Impulsivity and compulsivity in patients with trichotillomania or skin picking compared with patients with obsessive-compulsive disorder. Compr Psychiatry. 2006;47(4):282-288. 52. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington: DC: American Psychiatric Publishing; 2013. 53. de Oliveira-Souza R, Hare RD, Bramati IE, et al. Psychopathy as a disorder of the moral brain: fronto-temporo-limbic grey matter reductions demonstrated by voxel-based morphometry. Neuroimage. 2008;40(3):12021213. 54. Glenn AL, Raine A, Schug RA. The neural correlates of moral decisionmaking in psychopathy. Mol Psychiatry. 2009;14(1):5-6. 55. Blair RJ. Neuroimaging of psychopathy and antisocial behavior: a targeted review. Curr Psychiatry Rep. 2010;12(1):76-82. 56. Carver CS, Harmon-Jones E. Anger is an approach-related affect: evidence and implications. Psychol Bull. 2009;135(2):183-204. 57. Russell PS, Giner-Sorolla R. Bodily moral disgust: what it is, how it is different from anger, and why it is an unreasoned emotion. Psychol Bull. 2013;139(2):328-351. 58. Storch EA, Jones AM, Lack CW, et al. Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry. 2012;51(6):582-592. 419 Clinical research 59. Kanne SM, Mazurek MO. Aggression in children and adolescents with ASD: prevalence and risk factors. J Autism Dev Disord. 2011;41(7):926-937. 60. Chen K, Budman CL, Diego Herrera L, et al. Prevalence and clinical correlates of explosive outbursts in Tourette syndrome. Psychiatry Res. 2013;205(3):269-275. 61. Whiteside SP, Abramowitz JS. The expression of anger and its relationship to symptoms and cognitions in obsessive-compulsive disorder. Depress Anxiety. 2005;21(3):106-111. 62. de Hooge IE, Zeelenberg M, Breugelmans SM. Restore and protect motivations following shame. Cognition Emotion. 2009;24(1):111-127. 63. Tangney JP, Stuewig J, Mashek DJ. Moral emotions and moral behavior. Annu Rev Psychol. 2007;58:345-372. 64. Sznycer D, Takemura K, Delton AW, et al. Cross-cultural differences and similarities in proneness to shame: an adaptationist and ecological approach. Evol Psychol. 2012;10(2):352-370. 65. Lickel B, Kushlev K, Savalei V, Matta S, Schmader T. Shame and the motivation to change the self. Emotion. 2014;14(6):1049-1061. 66. Scheel CN, Bender C, Tuschen-Caffier B, et al. Do patients with different mental disorders show specific aspects of shame? Psychiatry Res. 2014;220(1-2):490-495. 67. Zimmerman J, Morrison AS, Heimberg RG. Social anxiety, submissiveness, and shame in men and women: a moderated mediation analysis. Br J Clin Psychol. 2015;54(1):1-15. 68. Roth L, Kaffenberger T, Herwig U, Bruhl AB. Brain activation associated with pride and shame. Neuropsychobiology. 2014;69(2):95-106. 69. Michl P, Meindl T, Meister F, et al. Neurobiological underpinnings of shame and guilt: a pilot fMRI study. Soc Cogn Affect Neurosci. 2014;9(2):150157. 70. Hedman E, Andersson G, Ljotsson B, et al. Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: a randomized controlled non-inferiority trial. PLoS One. 2011;6(3):e18001. 71. Goss K, Allan S. Shame, pride and eating disorders. Clin Psychol Psychother. 2009;16(4):303-316. 72. Budden A. The role of shame in posttraumatic stress disorder: a proposal for a socio-emotional model for DSM-V. Soc Sci Med. 2009;69(7):10321039. 73. Assuncao MC, Costa DL, de Mathis MA, et al. Social phobia in obsessive-compulsive disorder: prevalence and correlates. J Affect Disord. 2012;143(1-3):138-147. 74. Weingarden H, Renshaw KD. Shame in the obsessive compulsive related disorders: a conceptual review. J Affect Disord. 2015;171:7484. 75. De Oliveira-Souza R, Moll J, Grafman J. Emotion and social cognition: Lessons from contemporary human neuroanatomy. Emotion Rev. 2011;3(3):310-312. 76. Cuthbert BN. Research Domain Criteria: toward future psychiatric nosologies. Dialogues Clin Neurosci. 2015;17(1):89-97. 77. Moll J, Schulkin J. Social attachment and aversion in human moral cognition. Neurosci Biobehav Rev. 2009;33(3):456-465. 420