A System Identification Approach to Non-Invasive Central Cardiovascular Monitoring SEP
advertisement

A System Identification Approach to Non-Invasive
Central Cardiovascular Monitoring
MASSACHUSETTS INSi ~TE
OF TEOHNOLOG)
by
SEP 15 2008
Jin-Oh Hahn
r\
1
Bachelor
1
1" rr "
of
Science
"
lr
in
1
Mechanical
Seoul
National
"
lrr
j
•
Design
University,
l
and
1
.°
LIBRARIES
1",
Production
Engineenng
1997
Master of Science in Mechanical Design and Production Engineering
Seoul National University, 1999
Submitted to the Department of Mechanical Engineering
in Partial Fulfillment of the Requirements for the Degree of
Doctor of Philosophy
at the
Massachusetts Institute of Technology
June 2008
© 2008 Massachusetts Institute of Technology
All rights reserved
Signature of Author
-
--
Depaftn\ent of Mechanical Engineering
....
Certified by
-7 /
/
/7
April 24,2008
VH
arry Asada
Ford Professor of Engineering, Departm t of Mechanical Engineering
Thesis Supervisor
Accepted by
Lallit Anand
Chairman, Department Committee on Graduate Students
ARCHIVS
I would like to thank God for making possible everything I have achieved to date. This work is a manifestation of his will and power. I also would like to thank all of those who have guided, supported and prayed for
me up to this point in my life, including my family and my relatives as well as my friends. Especially I dedicate
this thesis to my beloved mother Irene and my lovelywife MJ.
_.
_1_1_~~~
A System Identification Approach to Non-Invasive
Central Cardiovascular Monitoring
by
Jin-Oh Hahn
Submitted to the Department of Mechanical Engineering on April 28, 2008
in Partial Fulfillment of the Requirements for the Degree of
Doctor of Philosophy in Mechanical Engineering
Abstract
This thesis presents a new system identification approach to non-invasive central cardiovascular monitoring problem. For this objective, this thesis will develop and analyze blind system identification and input
signal reconstruction algorithms for a class of 2-channel IIR and Wiener systems. In particular, this thesis will
present blind identifiability conditions for a class of 2-channel IIR and Wiener wave propagation systems and
develop the associated blind identification algorithms. It will be shown that the blind identifiability conditions
can be achieved in many real-world applications by appropriate selection of channel lengths, sensor locations,
and sampling frequency which are the specifications that the system design can exploit for blind identifiability
In addition, this thesis will develop a novel input signal reconstruction algorithm that is applicable to general
class of multi-channel IIR and Wiener systems. Furthermore, this thesis will rigorously analyze and evaluate
three analytic measures for determining the system order and other key parameters of the black-box dynamics as well as for quantifying the quality of the identified gray-box dynamics, without any direct use of unknown input signal: persistent excitation, model identifiability and asymptotic variance.
The blind identification and input signal reconstruction algorithms will first be applied to 2-sensor central cardiovascular monitoring problem using two distinct peripheral blood pressure measurements, where the
cardiovascular wave propagation dynamics is blindly identified and the aortic blood pressure and flow signals
are reconstructed by exploiting black-box and physics-based gray-box model structures of the cardiovascular
system. The validity of the 2-sensor central cardiovascular monitoring methodologywill be illustrated by experimental data from swinie subjects and simulation data from a full-scale human cardiovascular simulator
_~~·~
~__
across diverse physiologic conditions.
The 2-sensor central cardiovascular monitoring methodology will then be extended to address noninvasive, 1-sensor cardiovascular monitoring problem, where the specific challenges involved are 1) identifying the cardiovascular wave propagation dynamics and reconstructing the aortic blood pressure signal by exploiting the measurement from a single peripheral sensor, and 2) identifying the scale for calibrating the blood
pressure signal. In order to address these challenges, this thesis will propose a heuristics-based system order
estimation algorithm and a model-based blood pressure calibration algorithm, which will be combined with
the blind identification of the cardiovascular wave propagation dynamics to realize the non-invasive 1-sensor
central cardiovascular monitoring. The non-invasive 1-sensor central cardiovascular monitoring methodology
will be illustrated by experimental data from swine subjects, simulation data from a full-scale human cardiovascular simulator, and experimental data from human subjects across diverse physiologic conditions.
Thesis Supervisor
H. Harry Asada, PhD
Title:
Ford Professor of Engineering, Department of Mechanical Engineering
Massachusetts Institute of Technology
Thesis Committee
Nicholas M. Patrikalakis, PhD
Title:
Kawasaki Professor of Engineering, Department of Mechanical Engineering
Massachusetts Institute of Technology
Kamal Youcef-Toumi, ScD
Title:
Professor of Mechanical Engineering, Department of Mechanical Engineering
Massachusetts Institute of Technology
Andrew T. Reisner, MD
Title:
Department of Emergency Medicine
Massachusetts General Hospital
__
~1~~1_1_
~_________1~ ____11_~_1____
Acknowledgements
As I look back, the last three and half years I spent at MIT was the most challenging and exciting time in
my life. I would like to thank all of those who have guided and supported me throughout this challenge.
First, I would like to thank my thesis advisor, Professor H. Harry Asada, for his passionate guidance, encouragement and support. By virtue of his enthusiasm and keen insight for cutting-edge research, I could
enjoy plenty of opportunities to explore new and exciting ideas. Especially; his inspiration to break and go
beyond my limit and boundarywill be a life-long lesson that I should carrywith me throughout my career.
I am equally grateful to Professor Nicholas M.Patrikalakis, Professor Kamal Youcef-Toumi and Dr. Andrew T. Reisner for serving on my doctoral thesis committee. This thesis would not be possible without
their technical and intuitive guidance. Especially Professor Patrikalakis offered valuable pieces of knowledge
for the theoretical developments in this thesis, and Professor Youcef-Toumi offered a great deal of physical
insights and unique views to my research. Most importantly, my special thanks should be given to Dr. Reisner for his intensive collaboration and support on my thesis research. His advice and way of thinking as a
clinical physician helped me a lot in shaping myself as a biomedical engineer. I also appreciate his enormous
effort to make possible my human subject testing trials at the Massachusetts General Hospital, which was an
invaluable opportunity for me to learn a lot of real hands-on knowledge.
I also would like to express my gratitude to Dr. Farouc Jaffer, Ms. Sharon McKenna and all the staff in
the Cardiac Catheterization Laboratory at the Massachusetts General Hospital for their collaboration and
support in my human subject testing trials. I have to admit that my doctoral thesis would not be complete if
it were not for the wonderful results and outcomes I obtained from the joint research with the team. Besides,
their kindness and supportiveness always turned the stressful human subject testing trials into a pleasant and
enjoyable experience. I also appreciate the patients in the Cardiac Catheterization Laboratory for their willingness to participate in my human subject testing trails.
I also appreciate the Korean Government as well as the Sharp Corporation for their support on mythesis research. I was able to explore numerous new ideas thanks to them.
It was my great pleasure to have the opportunity to work with many talented people in the d'Arbeloff
Laboratory for Information Systems and Technology Definitely; my life at MIT was enriched by a lot of
I
_
~
__
~~_~I___
__
_~___I
__
__~
__~__
~~~_~_I~___
~__
_
__
__~
work and fun with them, including Kyujin Cho, Binayak Roy Eric Wade, Levi Wood, Manas Menon, Tom
Secord, Jun Ueda, Phillip Shaltis, Devin McCombie, Lael Odhner, Josiah Rosmarin, Chris Brown, Ani Mazumdar, Daniel Cunningham and Devin Neal Especially Kyujin, Binayak and Levi deserve special credit for
uncountable nights and weekends we spent together in the laboratory
I also would like to express many thanks to the Korean Graduate Student Association in Mechanical
Engineering and the Korean Graduate Student Association at MIT as well as Korean Grads '2004 at MIT.
Especially I appreciate Daekeun Kim, Euiheon Chung, Ki-Hean Kim and Hyuk-Sang Kwon for their voluntary help and advice to settle me down in the MIT community I also appreciate all the kind help I got from
KGSAME, including Chulmin Joo, Yeonwoo Cho, Jae Jeen Choi, Hohyun Lee, Hyun Jin In, Do-Nyun Kim,
Jinho Jang and many others. My special thanks should also be given to my precious friends who became an
important asset of my life byvirtue of MIT, including Sang-il Lee, Jaemyung Ahn, Won Yong Lee, Sangwon
Byun, Sangmok Han, Chiwon Kim, Jooeun Ahn, Jaewon Cha, Sangjin Ryu, Wonjae Choi, Taeho Shin, Sungjoong Kim, Han-Lim Choi, Taehee Han, Kang-HyunJi, Tairin Hahn, Youjin Lee and Ryan Lim, to list a few
I would like to wish all the best to their future carrier paths.
I would like to express my special gratitude to Professor Rajesh Rajamani at the University of Minnesota,
Twin Cities. In retrospect, all the critical shifts in my life happened since I encountered him. I learnt the
value of ambition and will in carving out my future from him. In addition to offering many opportunities
for professional growth, he has been willing to provide invaluable advice, suggestions and guidance as well
as encouragement and support at many important points in my life.
I am deeply grateful to my departed parents for their endless inspiration, encouragement and support,
without which I would not have been able to achieve this demanding goal in my life. To my brothers JinBaek and Jin-Seok, I give thanks for their love and encouragement. I would also like to thank all my relatives
for their kind assistance and support throughout my life. Special gratitude should also be given to my parents-in-law for their concern, encouragement and strong support. Finally I would like to thank my wife, MJ,
for her unlimited patience, inspiration and support, which has been the strongest source of thrust for me to
keep moving forward towards my goal as well as to overcome the loss of my beloved mother, who had been
my strong life-long supporter. I would like to express my deepest love and appreciation to her for the numerous challenges that she was willing to go through together with me.
I dedicate this work to my beloved mother Irene and my lovely wife MJ.
__·___I___·_____~
1__1_
Table of Contents
TABLE OF CONTENTS......................................................................................................................
7
LIST OF FIGURES.......................................................................................................................
10
LIST OF TABLES ..........................................................................................................................
13
CHAPTER 1.INTRODUCTI ON..................................................................................................... 14
1.1. CENTRAL CARDIOVASCULAR MONITORING ........................................
1.2. RELATED PREVIOUS WORK
.................................................
14
..........................................................................................................................................
16
1.3. THESIS SCOPE AND ORGANIZATION.................................................................................................... 17
CHAPTER 2. THEORETICAL DEVELOPMENT AND ANALYSIS...................
20
2.1. BLIND IDENTIFICATION OF GENERAL 2-CHANNEL IIR AND WIENER SYSTEMS ............................... 20
2.1.1. IIR Systems .................................................
.............................................. 20
2.1.2. Wiener System s ....................................................................................................
............................. 22
2.2. BLIND IDENTIFICATION OF 2-CHANNEL IIRAND WIENER WAVE PROPAGATION SYSTEMS ........
25
2.2.1. Identifiability Conditions for IIR and Wiener Wave Propagation Systems ........................................ 26
2.2.2. Blind Identification Design: Sensor Locations and Sampling Frequency..........................
...
39
2.2.3. Blind Identification Algorithms for IIR and Wiener Wave Propagation Systems ............................. 40
2.3. INPUT SIGNAL RECONSTRUCTION FOR 2-CHANNEL IIR AND WIENER SYSTEMS .............................. 42
2.3.1. IIR System s ................................. ................................................................................................
42
2.3.2. W iener System s ........................................................................................................................................
45
2.4. PERSISTENT EXCTATION AND MODEL IDENTIFIABILITY ANALYSIS ........
.........................................
46
2.5. ASYMPTOTIC VARIANCE ANALYSIS .......................................................................................................
48
2.6. SUMMARY . ..........
...........
..............
............................................................
50
.............................................
CHAPTER 3. MULTI-CHANNEL CARDIOVASCULAR WAVE PROPAGATION.................... 51
3.1. CARDIOVASCULAR SYSTEM ANATOMY .......................................................................................................
51
3.2. WAVE PROPAGATION IN CARDIOVASCULAR SYSTEM ...............................................................................
52
3.3. BLACK-Box AND GRAY-BOX CARDIOVASCULAR SYSTEM MODELING................................53
3.4. SUM MARY .....................................................................................................
............................................. 54
CHAPTER 4. EVALUATION PLATFORMS .......................................................................
55
4.1. EXPERIMENTAL SWINE SUBJECr DATA...................................................................................................55
4.2. FULL-SCALE HUMAN CARDIOVASCULAR SIMULATOR DATA.....................................
7
.............
57
4.3. EXPERIMENTAL HUMAN SUBJECT DATA..............................................................................................60
4.4. SUMMARY .....................................................................................................................................................
63
CHAPTER 5. TWO-SENSOR BLACK-BOX METHOD ..............................................
65
5.1. CARDIOVASCULAR SYSTEM IDENTIFICATION: DUAL LAGUERRE BASIS FUNCTIONS.......................
65
5.2. AORTIC FLOW SIGNAL RECONSTRUCTION .......................................................................................... 68
5.3. VALIDITY AND QUALITY ASSURANCE ......
........................................
72
5.4. RESULTS AND DISCUSSION............................................................................................................................74
5.4.1. Cardiovascular System Identification and Aortic Signal De-Convolution......................
.... 75
5.4.2. Quality Assurance....................................................................................................................................75
5.5. SUMM ARY .....................................................................................................................................................
81
CHAPTER 6. TWO-SENSOR IIR METHOD.............................................................................. 82
6.1. IIR CARDIOVASCULAR WAVE PROPAGATION DYNAMICS FOR SWINE SUBJECT ...............................
82
6.1.1. Cardiovascular System Modeling: Asymmetric T-Tube Model......................................83
6.1.2. Identifiability A nalysis .........................................................................................
............................. 85
6.1.3. Im plementation Issues ........................................................................................
............................. 87
6.2. RESULTS AND DISCUSSION.....................................................................................................................89
6.2.1. Accuracy of Frequency Responses .................................................................................................
89
6.2.2. Physiologic Relevance of Model Coefficients................................................................................93
6.2.3. Validity and Quality Assurance........................................................................................................99
6.3. SUMMARY .................
..................................................................................................................
CHAPTER 7. TWO-SENSOR WIENER METHOD .....................................
106
109
7.1. WIENER CARDIOVASCULAR WAVE PROPAGATION DYNAMICS FOR HUMAN SUBJECT .................... 109
7.1.1. Cardiovascular System Modeling: Aortic-to-Radial Channel............................................................. 109
7.1.2. Cardiovascular System Modeling: Aortic-to-Femoral Channel ....................................
111
7.1.3. IdentifiabilityAnalysis .............................................................................................................
115
7.1.4. Implementation Issues .............................................................................................................
120
7.2. RESULTS AND DISCUSSION..........................................................................................................................
122
7.3. SUM MARY .................
..................................................................................................................
132
CHAPTER 8. NON-INVASIVE ONE-SENSOR METHOD .....................................
133
8.1. CARDIOVASCULAR SYSTEM IDENTIFICATION USING ANON-INVASIVE PERIPHERAL SENSOR.......... 138
8.1.1. Temporal 2-Channel Blind Identification: Basic Principle..............................................................
138
8.1.2. Temporal 2-Channel Blind Identification of Cardiovascular System ........................................
140
8.1.3. Error Propagation Analysis ..................................................................................................................
142
8
8.2. SYSTEM ORDER ESTIMATION: PULSE TRANSIT TIME ESTIMATION.......................................................
145
8.3. MODEL-BASED SYSTOLIC BLOOD PRESSURE CAIIBRATION ..........................
150
8.4. VALIDITY AND QUALITY ASSURANCE ................................................................................................. 152
8.5. RESULTS AND DISCUSSION...................................................
....................................................
152
8.5.1. Experimental Swine Subject Data ........................................
153
8.5.2. Full-Scale Human Cardiovascular Simulator Data................................
165
8.5.3. Experimental Human Subject Data .....................................................................................................
168
8.6. SUMMARY ......................................................................................................................................................
CHAPTER 9. CONCLUSIONS ........................................
172
173
9.1. SUMMARY OF THESIS CONTRIBUTIONS ..................................................................................................... 173
9.2. FUTURE DIRECTIONS FOR RESEARCH ....................................................................................................... 174
APPENDIX A. EQUIVALENCE BETWEEN SVD AND LEAST-SQUARES ESTIMATES......... 176
APPENDIX B. WIENER TWO-SEGMENT TRANSMISSION LINE REPRESENTATION OF
AORTIC-TO-FEMORAL CARDIOVASCULAR CHANNEL DYNAMICS .................................... 178
REFERENCES .......................................................................................................................
180
List of Figures
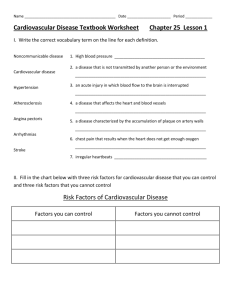
FIG. 1.1. EXAMPLES OF PHYSIOLOGIC MEASURES FOR CENTRAL CARDIOVASCULAR MONITORING................ 15
FIG. 2.1. A 2-CHANNEL INFINITE IMPULSE RESPONSE (IR) SYSTEM ....................................
....... 21
FIG.2.2. A 2-CHANNEL W IENER SYSTEM. ...................................................
23
FIG. 2.3. AN ILLUSTRATIVE WAVE PROPAGATION CHANNEL ..........................
........
27
FIG. 2.4. LINEARREGRESSIONOF z2 (n) FOR FIRAND IIR/WIENER DYNAMICS .................................
29
FIG. 2.5. DECOMPOSITIONOF P (z) INTO D2(z) AND Nl(z) IN THE ABSENCE OF SEPARATION...........30
FIG. 2.6. DIRECT DETERMINATION OF COEFFIQENTS IN D(z) AND N(z) FROM P(z) ........................
33
FIG. 2.7. SEPARATION STRUCTURE OF LOWER DIMENSIONAL DECOMPOSITION PROBLEMS ...........................
34
FIG. 2.8. MATRIX EQUATION FOR DETERMINATION OF bm-_,,--,bo, ak-_•_ l ,- , -ak-_ w N AD ay_...........36
FIG. 2.9. MATRIX EQUATION FOR DETERMINATION OF ak-
k_(,
..........................................
37
FIG. 2.10. MATRIX EQUATION FOR THE DESIGN OF A STABLE DE-CONVOLUTION FILTER...........................44
FIG. 2.11. BLOCK DIAGRAM OF THE DE-CONVOLUTION FILTER (rl ni- m i)..........................
45
FIG. 2.12. ASYMPTOTIC VARIANCE OF PARAMETER ESTIMATION ERROR. ........................................
50
FIG. 3.1. CARDIOVASCULAR SYSTEM ANATOMY...................................................
............................................ 52
FIG. 4.1. TIME HISTORY OF KEY CARDIOVASCULAR PHYSIOLOGIC MEASURES OF SWINE SUBJECT # 1...........
57
FIG. 4.2. BLOOD PRESSURE SIGNALS OBTAINED FROM THE FULL-SCALE CARDIOVASCULAR SIMULATOR......60
FIG. 4.3. DEVICES AND CONNECTIONS FOR HOSPITAL HUMAN SUBJECT TESTING .................................
62
FIG. 4.4. DEVICES AND CONNECIIONS FOR HOSPITAL HUMAN SUBJECT TESTING .................................
63
FIG. 5.1. CARDIOVASCULAR SYSTEM AS A 2-CHANNEL ORTHONORMAL BASIS FUNCTION SYSTEM. ................
66
FIG. 5.2. TYPICAL IMPULSE RESPONSE OF A CARDIOVASCULAR PATH. .....................................
....... 68
FIG. 5.3. MATRIX EQUATION FOR THE DESIGN OF LAGUERRE DE-CONVOLUTION FILTER.........................
70
FIG. 5.4. BLOCK DIAGRAM OF THE LAGUERRE DE-CONVOLUTION FILTER ......................................
... 71
FIG. 5.5. LAGUERRE-FUNCTION-BASED CARDIOVASCULAR SYSTEM ID AND INPUT DE-CONVOLUTION ........
74
FIG. 5.6. PERIPHERAL BLOOD PRESSURES AND TRUE VERSUS RECONSTRUCTED AORTIC FLOW SIGNALS......77
FIG. 5.7. IMPULSE RESPONSES OF IDENTIFIED AORTIG-TO-RADIAL TRANSFER FUNCTIONS .........................
77
FIG. 5.8. ASYMPTOTIC VARIANCE OF LAGUERRE SERIES COEFFICENTS WITH RESPECT TO DATA LENGTH..79
FIG. 5.9. PERCENTAGE ASYMPTOTIC VARIANCE OF DC GAINS WITH RESPECT TO DATA LENGTH. .............. 79
FIG. 6.1. ASYMMETRIC T-TUBE MODEL OF A 2-CHANNEL CARDIOVASCULAR SYSTEM...............................
84
FIG. 6.2. BLOCK DIAGRAM OF ASYMMETRIC T-TUBE CARDIOVASCULAR WAVE PROPAGATION DYNAMICS.....86
FIG. 6.3. IDENTIFIED 2-CAHNNEL FREQUENCY RESPONSES AND RECONSTRUCTED AORTIC SIGNALS. ......... 90
FIG. 6.4. MAGNITUDE FREQUENCY RESPONSES OF 83 CARDIOVASCULAR WAVE PROPAGATION DYNAMICS.. 92
FIG. 6.5. AORTIC BLOOD PRESSURE RECO NSTRUCTION ERRORS. ......................................................................
93
FIG. 6.6. PHYSIOLOGIC RELEVANCE OF IDENTIFIED ASYMMETRIC T-TUBE MODEL ODEFFICIENTS .............
94
FIG. 6.7. TRUE VERSUS IDENTIFIED AORTIGC-TO-RADIAL PULSE TRANSIT TIMES .....................
97
FIG. 6.8. PHYSIOLOGIC RELEVANCE OF PULSE TRANSIT TIME IDENTIFIED FROM BLIND APPROA-
............ 97
FIG. 6.9. THE INFLUENCES OF PULSE TRANSIT TIMES AND POLYNOMIAL COEFFICIENTS ON G, (j)
.......... 98
FIG. 6.10. PERSISTENT EXCITATION AS AFUNCTIONOF IFHR - F, ......................................................... 100
FIG. 6.11. EFFECT OF DATA LENGTH ON ASYMPTOTIC VARIANCE ......................................
102
FIG. 6.12. PARAMETRIC ASYMPTOTIC VARIANCE FOR EXPERIMENTAL SWINE SUBJECT .............................. 103
FIG. 6.13. ASYMPTOTIC VARIANCE FOR EXPERIMENTAL SWINE SUBJECT (N=1,000) ..................................
104
FIG. 6.14. NORMALIZED ASYMPTOTIC VARIANCE FOR EXPERIMENTAL SWINE SUBJECT (N=1,000).......
105
FIG. 6.15. CONSISTENCY OF A AND SN AGAINST DIFFERENT DATA LENGTHS. ....................................... 107
FIG. 6.16. ASYMPTOTIC STANDARD DEVIATION OF G1 (1j)
AND G2 (jw) ATT=710 S WITHN=1,000...108
FIG. 7.1. A SINGLE-SEGMENT TRANSMISSION LINE MODEL FOR AORTIGTO-RADIAL CHANNEL ........
110
FIG. 7.2. RECONSTRUCTED AORTIC BLOOD PRESSURE SIGNALS ......................................
112
FIG. 7.3. PHYSICS-BASED GRAY-BOX MODEL OF HUMAN AORTIG-TO-FEMORAL CHANNEL ........................
113
FIG. 7.4. A NONLINEAR TWO-SEGMENT TRANSMISSION LINE MODEL OF HUMAN LOWER LIMB .........
114
FIG. 7.5. POSSIBLE SEPARATION LOCATIONS IN N 2 1(z)
117
1
(z) ..........................................
.......
FIG. 7.6. BLOCK DIAGRAM OF WIENER CARDIOVASCULAR SYSTEM .....................................
120
FIG. 7.7. TRUE VERSUS IDENTIFIED G,(z) AND TRUE VERSUS RECONSTRUCTED P,(n) AND Ps (n).....127
FIG. 7.8. RECONSTRUCrED AORTIC BLOOD PRESSURE SIGNALS ......................................
131
FIG. 8.1. EXTENSION OPPORTUNITIES FOR 2-SENSOR CENTRAL CARDIOVASCULAR MONITORING. .......... 133
FIG. 8.2. A NON-INVASIVE 1-SENSOR CENTRAL CARDIOVASCULAR MONITORING SET-UP .......................... 134
FIG. 8.3. DYNAMICS FROM AORTIC BLOOD PRESSURE SIGNAL TO NON-INVASIVE SENSOR SIGNAL.......... 135
FIG. 8.4. BLIND IDENTIFICATION AND MODEL-BASED BLOOD PRESSURE CALIBRATION...........................
137
FIG. 8.5. A CLOSED-LOOP DIGITAL CONTROL SYSTEM FOR TEMPORAL 2-CHANNEL BLIND ID..................... 140
FIG. 8.6. STOCHASTIC SECOND MOMENT ANALYSIS OF ERROR PROPAGATION .....................................
143
FIG. 8.7. AN EXAMPLE OF THE INCIDENT AND THE REFLECIING BLOOD PRESSURE WAVES. ....................... 146
FIG. 8.8. SUPERPOSITION OF INCIDENT AND REFLECIING BLOOD PRESSURE WAVES ................................... 148
FIG. 8.9. BLOOD PRESSURE SIGNALS AND THEIR SECOND DERIVATIVE NORMS ........................................
149
FIG. 8.10. 'INDKESSEL THEORY FOR SYSTOLIC BLOOD PRESSURE CALIBRATION .....................................
151
FIG. 8.11. DISCREPANCY BETWEEN TRUE AND APPROXIMATED AORTIC AND RADIAL BLOOD PRESSURES.. 155
FIG. 8.12. TRUE VERSUS ESTIMATED
iil AND
..............................................................................................
158
FIG. 8.13. TRUE VERSUS RECONSTRUCTED AORTIC BLOOD PRESSURES ......................................
159
FIG. 8.14. TRUE VERSUS IDENTIFIED AORTIG-TO-RADIAL PULSE TRANSIT TIMES ........................................
162
FIG. 8.15. TRUE VERSUS CALIBRATED RADIAL SYSTOLIC AND SYSTOLIC MEAN BLOOD PRESSURES........... 162
FIG. 8.16. PERSISTENT EXCITATION AS AFUNCTIONOF IF,H - F
AT 500HZ SAMPLING FREQUENCY. ... 164
FIG. 8.17. TRUE VERSUS RECONSTRUCTED AORTIC BLOOD PRESSURES ......................................
167
FIG. 8.18. TRUE VERSUS ESTIMATED FINGER SYSTOLIC BLOOD PRESSURES FOR 15 HUMAN SUBJECIS. ....... 168
FIG. 8.19. TRUE VERSUS RECONSTRUCTED AORTIC BLOOD PRESSURES .........................................................
171
List of Tables
TABLE 4.1. PHYSIOLOGIC SPAN OF EXPERIMENTAL SWINE DATA. ....................................................................
58
TABLE 4.2. PHYSIOLOGIC CONDITIONS OF SIMULATED HUMAN SUBJE CT MODELS .......................................... 60
TABLE 5.1. ASYMPTOTIC VARIANCE OF LAGUERRE SERIES CDEFFIIENTS (L, = L 2 = 3) ................................ 78
TABLE 5.2. PERCENTAGE ASYMPTOTIC VARIANCE OF DC GAINS (N = 800) ..................................................... 81
TABLE 6.1. FEATURE ESTIMATION STATISTICS: BLIND AND AVERAGED APPROACHEES.........................
92
TABLE 7.1. COMPARISON OF WIENER AND LINEAR 2-SEGMENT TRANSMISSION LINE MODELS ................ 128
TABLE 7.2. IDENTIFIED PULSE TRANSIT TIMES....................................
131
TABLE 8.1. NORMALIZED &, UNDER SAMPLING FREQUENCIES OF 100, 200, 300, 400, AND 500HZ.........
156
TABLE 8.2. LEAST-SQUARES ERROR ASSOCATED WITH (8.26) .................................
160
TABLE 8.3. FEATURE ESTIMATION STATISTICS: BLIND AND AVERAGED APPROACHES...............................
161
TABLE 8.4. SYSTOLIC AND SYSTOLIC MEAN BLOOD PRESSURE ESTIMATION STATISTICS...........................
163
TABLE 8.5. HUMAN NON-INVASIVE-MEASUREMENT-BASED SYSTOLIC BLOOD PRESSURE STATISTICS .......... 169
TABLE 8.6. TRUE VERSUS ESTIMATED AORTIC SYSTOLIC BLOOD PRESSURES...............................
170
Chapter 1. Introduction
The cardiovascular (including heart and blood vessel) disease has no geographic, gender, or socioeconomic boundaries. Especially in the United States, nearly 80 million adults (which amount to approximately
one third of the entire adult population) suffer from one or more types of cardiovascular disease such as hypertension, coronary heart disease, heart failure, stroke, and so forth [1]. Its prevalence is more problematic
among old population; nearly 50% of the cardiovascular disease population are estimated to be age older than
65. Furthermore, the cardiovascular disease has accounted for more death than any other single or group of
causes of death in the United States since the beginning of the 20" century[1]. As such, there are still a lot of
rooms and opportunities to help out the cardiovascular disease population.
In this thesis, the cardiovascular system is viewed as a dynamical system. In particular, with sensors
placed at multiple extremity locations to measure blood pressure and flow waves, it can be viewed as a multichannel wave propagation system. As such, many clinically important signals and phenomena can be monitored and even diagnosed by identifying its dynamics. The goal of this thesis is to develop, analyze and verify
a system identification approach to non-invasive central cardiovascular monitoring, which is able to characterize the health condition of the central cardiovascular system based on minimally invasive and/or even noninvasive biological signals measured at peripheral extremity locations.
1.1. Central Cardiovascular Monitoring
In this thesis, the term "central cardiovascular monitoring" refers to the measurement and/or estimation
of physiologic measures and/or features that are useful to assess the physiologic condition of the central cardiovascular system including the heart and the global circulation. Examples include systolic, mean and diastolic aortic blood pressures, aortic blood flow and cardiac output, arterial compliance, total peripheral resistance and its baro-reflex, characteristic impedance, pulse wave velocity and pulse transit time, systolic time
14
intervals such as ejection duration [2-3], left ventricular elasticity, end-diastolic volume, etc., some of which
are shown in Fig. 1.1.
Fig. 1.1. Examples of physiologic measures for central cardiovascular monitoring.
Up until now, tremendous amount of research efforts has been made to develop algorithms for estimating these physiologic measures by utilizing the central aortic as well as peripheral blood pressure and flow
measurements, which includes, but is not limited to: 1)estimating cardiac output by central aortic or peripheral blood pressure waveform analysis [4-101 2) estimating constant, pressure- and frequency-dependent arterial compliance [11-16] using central aortic blood pressure and/or flow signals, 3) estimating total peripheral
resistance and its baro-reflex using features of a peripheral blood pressure [9,17] as well as central aortic
blood pressure and flow [9,15,18], 4) estimating characteristic impedance by analyzing the systolic portion of
the aortic blood pressure and flow signals [15,19,201 5) estimating maximum left ventricular elasticity and end
15
diastolic volume by analyzing a peripheral blood pressure signal [17]. It can be easily noticed that majority of
the physiologic measure estimation algorithms resort to blood pressure and/or flow signals measured at central aortic and/or peripheral extremity locations.
1.2. Related Previous Work
In terms of the utility in central cardiovascular monitoring, central cardiovascular signals, such as aortic
blood pressure and flow, are generally more informative about cardiac dynamics and global circulation, in
comparison with the peripheral cardiovascular signals. However, standard measurement of these signals, such
as pulmonary artery or central aortic catheterization, entails invasive procedures, which are relatively costly
dangerous, uncomfortable and risky Furthermore, peripheral circulatory measurements, e.g arterial blood
pressure measured at distal extremity locations, cannot be used as a direct surrogate for their central counterparts, because the morphology of the central cardiovascular signals are distorted at distal locations due to the
transmission and reflection effects in the cardiovascular system [21-23]. Therefore, there has been substantial
interest in developing indirect methods to reconstruct the central cardiovascular signals from peripheral cardiovascular measurements by utilizing the dynamic relationship between the two, ie. the cardiovascular wave
propagation dynamics. Most of the methods available to date involve a population-based model, employing
nominal parameter values derived from prior experimentation [24-30]. In many cases, this approach yields
useful estimates [24-26]. In theory, however, the use of a population-based model for different subjects under
diverse physiologic conditions will be invalid to some extent, ie. there will be states when an average relationship between the aortic and peripheral signals is less applicable [27-30]. It would be ideal if the cardiovascular
wave propagation dynamics could be identified without resorting to any a priori knowledge.
Efforts have been made to use multiple peripheral circulatory measurements in order to reduce the reliance on a priori knowledge and other population-based assumptions regarding the relationship between cen-
tral aortic and peripheral cardiovascular signals [8,10,31-38]. Some of the efforts involved measurements rela16
tively close to the central aorta, e.g. the carotid [8,10], and used it as a surrogate for a central cardiovascular
signal. Problems associated with this approach are 1) the carotid blood pressure is not strictly identical to the
aortic blood pressure, and 2) the use of proximal blood pressure signal limits the applicability of the method.
Another approach used the multi-channel blind system identification methodology [39-42], which was shown
capable of reproducing the aortic blood flow [31,36,38] and aortic blood pressure [32-35] signals, as well as
estimating other key cardiovascular physiologic measures [31,37] from a couple of peripheral blood pressure
measurements. However, these earlier attempts have revealed several critical shortcomings:
1. Using these methods, which are based on black-box model structures such as finite impulse response
(FIR) [33,38] and generalized FIR [31,36,37] models, it is difficult to systematically determine the order of each channels' dynamics and other key parameters due to the lack of available analytic measures and guidelines to select appropriate model structures. As a result, it often involves a lot of tuning procedures. Furthermore, interpreting the physical implication of the identified black-box model
and the coefficients therein still remains as a challenge.
2. Extending these methods to physics-based gray-box model structures will resolve the aforementioned issues. However, extending the methods to standard infinite impulse response (IIR) and Wiener systems (to which a class of physics-based gray-box model structures of the cardiovascular dynamics belongs) requires at least three distinct peripheral measurements [38-42], which is difficult to
implement in a clinical setting. Besides, up to the author's knowledge, there has been no unified
methodology developed for reconstructing unknown input signal from the identified dynamics of
general multi-channel IIR and Wiener systems.
1.3. Thesis Scope and Organization
Based upon the author's preliminary work [31,32,34,35,37] as well as motivated by the aforementioned
challenges, this thesis will develop and analyze blind system identification and input signal reconstruction al17
gorithms for a class of 2-channel IIR and Wiener systems. In particular, this thesis will present blind identifiability conditions for a class of 2-channel IIR and Wiener wave propagation systems and develop the associated blind identification algorithms. It will be shown that the blind identifiability conditions can be achieved
in many real-world applications by appropriate selection of channel lengths, sensor locations, and sampling
frequency; which are the specifications that the system design can exploit for blind identifiability In addition,
this thesis will develop a novel input signal reconstruction algorithm that is applicable to general class of
multi-channel IIR and Wiener systems. Furthermore, this thesis will rigorously analyze and evaluate three analytic measures for determining the system order and other key parameters of the black-box dynamics as well
as for quantifying the quality of the identified gray-box dynamics, without any direct use of unknown input
signal: persistent excitation, model identifiability and asymptotic variance.
The blind identification and input signal reconstruction algorithms will first be applied to 2-sensor central cardiovascular monitoring problem using 2 distinct peripheral blood pressure measurements, where the
cardiovascular wave propagation dynamics is blindly identified and the aortic blood pressure and flow signals
are reconstructed by exploiting black-box and physics-based gray-box model structures of the cardiovascular
system. The validity of the 2-sensor central cardiovascular monitoring methodology will be illustrated by experimental data from swine subjects and simulation data from a full-scale human cardiovascular simulator
across diverse physiologic conditions.
The 2-sensor central cardiovascular monitoring methodology will then be extended to address the noninvasive, 1-sensor central cardiovascular monitoring problem, where the specific challenges involved are 1)
identifying the cardiovascular wave propagation dynamics and reconstructing the aortic blood pressure signal
by exploiting the measurement from a single peripheral sensor, and 2) identifying the scale for calibrating the
blood pressure signal. In order to address these challenges, this thesis will propose a heuristics-based system
order estimation algorithm and a model-based blood pressure calibration algorithm, which will be combined
with the blind identification of the cardiovascular wave propagation dynamics to realize the non-invasive 118
sensor central cardiovascular monitoring. The non-invasive 1-sensor central cardiovascular monitoring methodology will be illustrated by experimental data from swine subjects, simulation data from a full-scale human
cardiovascular simulator and experimental data from human subjects across diverse physiologic conditions.
This thesis is organized as follows. In Chapter 2, key algorithmic development and analysis will be presented. Chapter 3 will briefly review the cardiovascular physiology to provide the basis for regarding the cardiovascular system as a multi-channel wave propagation system. In Chapter 4, evaluation platforms used in
this thesis will be discussed. Chapter 5 will deal with the 2-sensor central cardiovascular monitoring using a
black-box model, with emphasis on the use of the analytic measures for effectively determining the system
order and other key parameters. Chapter 6 and Chapter 7 will deal with the 2-sensor central cardiovascular
monitoring using physics-based gray-box models, with emphasis on the use of the analytic measures for
quantifying the quality of the identified cardiovascular wave propagation dynamics. Chapter 8 will extend the
2-sensor central cardiovascular monitoring to non-invasive 1-sensor central cardiovascular monitoring. Chap-
ter 9 will summarize the contributions of this thesis and propose directions for future research.
Chapter 2. Theoretical Development and Analysis
In this chapter, blind system identification and input signal reconstruction algorithms for a class of 2channel IIR and Wiener systems are developed and analyzed. Especially, we consider a class of 2-channel systems that describe the wave propagation dynamics. As we will demonstrate, this class of systems subsumes
the physics-based gray-box models of the cardiovascular dynamics used subsequently in this thesis. For this
specific class of 2-channel IIR and Wiener wave propagation systems, the blind identifiability conditions and
the associated blind identification algorithms, as well as a novel input signal reconstruction filter design algorithm, will be developed.
In addition to the algorithmic developments, this chapter rigorously analyzes persistent excitation, model
identifiability and asymptotic variance as effective analytic measures to determine the system order and other
key parameters of the black-box dynamics as well as to assess the quality of the identified gray-box dynamics
of the 2-channel IIR and Wiener systems, in terms of both accuracy and reliability The development and
analysis in this chapter will be subsequently used throughout this thesis.
2.1. Blind Identification of General 2-Channel IIR and Wiener Systems
2.1.1. IIR Systems
Consider a 2-channel IIR system shown in Fig. 2.1, which creates two distinct output signals yi (n) and
y2 (n) in response to a common input signal u(n). The dynamics of the channels S, and S2 , G,(z) and
G2 (z), are described as follows, which are assumed to be minimal realizations of S1 and S2:
Gi (z)
b zm + b(')
N,(z)
Di(z)
n
z
+anlz
+*--ao
,
i=1, 2.
(2.1)
Since both channels are excited by a common input signal, one of the following functional relationships be20
tween the output signals can be explored to identify the channels S1 and S2 , if G,(z) and G2 (z) possess
no common poles and zeros [38-42]:
G, (z)y 2 (n)= G,(z)[G 2 (z)u(n)] = G2 (z)[G, (z)u(n)] = G2 (z) y (n),
(2.2a)
GI' (z)y, (n)= Gj' (z)[G, (z)u(n)] = G l ' (z)[G2 (z)u(n)] = G-' (z)yl (n).
(2.2b)
Equating the first and the last expressions, we have, in general,
dG (z)y, (n)= G2 (z)Y2 (n)
for proper IIR systems G (z) and
(2.3)
2(z)
and delayed output signals , (n) and 2(n) as follows. Assum-
ing that S, and S2 are causal processes, G,(z) and G2 (z) can be regarded as proper or strictly proper.
Then we can set Gi (z)= Gi (z) and 7 (n)= y, (n), i =1,2 to convert (2.2a) into (2.3). In order to convert
(2.2b) into (2.3), we can set G (z) = G-' (z)z
- (n' - mi)
and j (n) = y, (n+ n -mi),
i = 1,2 . This system identi-
fication technique is called the "blind" system identification [38-42] because it does not involve the use of
input signal for system identification.
yi(n)
u(n)
Y2(n)
Fig. 2.1. A 2-channel infinite impulse response (IIR) system.
Let G (z)=N•(z)DI(z) for i=1,2, where Di(z) is an n,-th order monic polynomial in z and
9, (z) is an mi -th order polynomial in z, respectively Then (2.3) is equivalent to
IP(z)3 l (n) = )2() 1(z)5;(n)= A (z)N 2(z) 5 (n)= P2 (z)Y2 (n),
or alternatively in discrete-time domain,
(2.4)
[Y (n+ n2 +
m
where
I
Y)
[PiP2 , and P
-2(n+nl
+m,+,... Po
2
+nm)2).
(2.5)
Y 2(n)p= 0,
and P2
mnl "...p
]T
2)I
are the vectors consisting of the coef-
ficients of iP(z) , i = 1,2. The challenge in identifying S, and S2 by solving (2.5) arises from the fact that
1) only Yl (n) and Y2 (n), but not u(n), are available for identifying the system, and 2) G,(z) and G2 (z)
have IIR dynamics. In particular, because (2.5) is a homogeneous equation and can only provide the directionality of p, P (z) and P2 (z) can be determined only up to scale. As a result, the gains of G,(z) and
G2 (z) cannot be uniquely determined. In addition, it is well known that identifying a multi-channel IIR sys-
tem requires at least three distinct channels together with the associated output measurements [38-42], in order to uniquely decompose P (z) into 52 (z) and N, (z) as well as P2 (z) into D5(z) and
2(z)
in (2.4).
However, since the class of IIR systems considered in this thesis involves only two channels, it is in general
impossible to uniquely identify S, and s2 solelybysolving (2.5).
Note that a 2-channel FIR system is a special case of a 2-channel IIR system with unity denominators,
that is, Di (z)= 1 for i= 1,2 in (2.1). Then it is obvious from (2.4) that P (z)= Ni(z) for i= 1,2, and
thus a 2-channel FIR system can always be identified up to scale as long as the homogeneous equation (2.5)
yields a non-trivial solution p.
2.1.2. Wiener Systems
Consider a 2-channel Wiener system shown in Fig. 2.2, which creates two distinct output signals yi (n)
and Y2 (n) in response to a common input signal u(n). The dynamics of the i-th channel, S,, for i= 1,2 is
described by a Wiener system, that is, a linear dynamical system G1 (z) followed by a static nonlinear function N, (xi) . The intermediate signals, i.e. the outputs of G,(z) and G2 (z), are denoted by x, (n) and
x2 (n), respectively Note that x, (n) and x2 (n) are not available for blind system identification. The linear
dynamical systems G,(z) and G2 (z) are described by the following IIR representations, which are assumed
22
to be minimal realizations:
Gi (z) A
b()
0 , ...
Ni (z) bz')+0
mi
Di (z)
Zni
+ a0i).Zn-I
,
i=1,2.
(2.6)
-a
Assuming that the nonlinearities involved in the system are sufficiently smooth and invertible, we consider the
following basis function expansion representation for the nonlinear functions N,(x,) and N2 (x 2 ):
=
xiN
(i)
'(Yi)= i)1
,
Li)
()i)=
(2.7)
(Yi), i=1,2.
k=1
System: S,
Gj(z)
N1(xt)
yi(n)
G2(z)
N2(X2)
Y2(n)
u(n)
System: S2
Fig. 2.2. A 2-channel Wiener system.
If x, (n) and x2 (n) as well as Yi (n) and Y2 (n) were available, the identification of the nonlinear
functions would become trivial. In addition, one of the following relationships between x,1 (n) and x2 (n)
could be explored to identify the linear dynamical portion of the channels Si, i = 1,2, based on the fact that
both channels are excited by a common input signal:
G 1'(z)x (n)= G1'(z)[G, (z)u(n)] = G2'(z)[G2 (z)u(n)] = G' (z)x2 (n),
(2.8a)
G, (z)x2 (n)= G, (z)[G 2 (z)u(n)] = G 2 (z)[Gi (z)u(n)] = G 2 (z)x l (n).
(2.8b)
Equating the first and the last expressions, we have, in general,
G,(z) , (n) = G2 (z)Y2 (n)
(2.9)
for proper IIR systems ,(z) and 2(z)and delayed output signals ,(n)and 72 (n)as follows. Assum-
ing that S, and S2 are causal processes, G1 (z) and G2 (z) can be regarded as proper or strictly proper.
Then we can set Gi (z)= Gi(z) and i (n)= xi(n), i=1,2 to convert (2.8a) into (2.9). In order to convert
" -m,)
(2.8b) into (2.9), we can set Gi(z)= GT1(z)z-(n
and i(n)= xi(n+ ni -m) , i =1,2 .
Let G,(z) = Ni (z)bD' (z) for i = 1,2 . Substituting the nonlinear functions (2.7) into (2.9) yields
k,
d,(Z)
k2
=
(yl ())
1)k
G2
(Y2 (n)).
72)k
(z)
(2.10)
k=1
k=1
Multiplying /b (z)D 2 (z) to both sides of (2.10), we get
k,
(z)[
(y, (n))] =P2(
')k
k'
1
(n))
2)k (Y2
(2.11)
Ik=1
Ik=1
where P,(z)- D2 (z)Nl (z) and P2 (z) --D1 (z)KR2 (z), or alternatively in discrete-time domain,
1(l)
p l
(1)
[I Il(yl(n))." pk, (yl(n))
pk2(Y2(n))]
-- l(Y2(n)) ....
r71)P2
(2.12)
=TP =0,
k2 P2
where pi, i = 1,2, are vectors consisting of the coefficients of P.(z), and
(Pk (n)
))
[~k(y (n+n2 +ml ))...
k (Yl (n))],
(pk(Y2(n)) •[
k(y2 (n+nl
M2
))... k(Y2(n))].
(2.13)
Therefore, the 2-cahnnel blind Wiener system identification problem (2.10) can be reformulated into an overparameterized homogeneous equation (2.12), which can be regarded as a multi-variable extension of the 2channel blind IIR system identification problem, with each of the terms in the basis function expansion in
(2.7) viewed as independent output signals; see (2.5). Once (2.12) is solved and P is identified, then
P [Pi
ij
and qA= [
composition:
with 1 A[q•).
]
for i =1,2 can be identified using the singular value de-
(2.14)
[1i)Pi "'17 Pi]=Pi =iU ViT,
where the columns of the unitary matrices Ui and V, corresponding to the maximum singular value are
taken as the estimated values of pi and qii.
The challenge in identifying S, and S2 by solving (2.12) arises from the fact that 1) only y, (n) and
y2 (n), but not u(n), are available for identifying the system, and 2) G1 (z) and G2 (z) have IIR dynamics.
In particular, because (2.12) is a homogeneous equation and can only provide the directionality of P (and
therefore p and q), P (z) and P2(z) as well as N1(x)
and N2 (x 2 ) can be determined only up to
scale. As a result, the gains of G,(z) and G2 (z) cannot be uniquely determined. In addition, since the class
of Wiener systems considered in this thesis involves only two channels, it is in general impossible to identify
S, and S2 solelybysolving(2.12).
2.2. Blind Identification of 2-Channel IIR and Wiener Wave Propagation Systems
For both 2-channel IIR and 2-channel Wiener systems, it is evident that the first issue, the inability to
uniquely determine the gains of S1 and s2 , is an intrinsic shortcoming of the blind system identification
methodology regardless of the model structures (i.e. finite impulse response (FIR) models, generalized FIR
or basis function expansion models, IIR models, Hammerstein and Wiener models, etc.) and the number of
channels involved in the system, unless any additional information on the model and/or the signals relevant
to determine the gains are available [38-42]. However, the second issue of characterizing G1 (z) and G2 (z)
from P (z) and P2 (z), by decomposing i (z) into D2 (z) and
(z) as well as P,2 (z) into D, (z) and
N2 (z) in (2.4) and (2.11), respectively heavily depends on the specifics of the IIR and Wiener dynamics
given for a particular target system, and this issue can be resolved by confining ourselves to a class of IIR and
Wiener dynamics satisfying some structural properties. Especially inspired by a class of physics-based graybox models describing the cardiovascular wave propagation dynamics [10,17,22,23,26,30,43-481 this thesis
will concentrate on analyzing blind identifiability conditions and developing blind identification algorithms
for a class of 2-channel IIR and Wiener wave propagation systems, whose channel dynamics involve the
propagation and the reflection of traveling waves. A unique property of this class of systems is the "sparseness," ie. the existence of zero coefficient terms, of the denominator and/or numerator polynomials, which
is introduced into the system dynamics by nonzero pulse transit time due to finite pulse wave velocity As we
will demonstrate, the sparseness of the denominator and/or numerator polynomials can be exploited to identify a subset of their coefficients directly from their product, which can be subsequently used to obtain a set
of linear equations that can yield the remaining set of the coefficients in the denominator and numerator
polynomials under certain conditions.
2.2.1. Identifiability Conditions for IIR and Wiener Wave Propagation Systems
Fig. 2.3 shows an illustrative 2-channel wave propagation system e.g. two distinct branches of the cardiovascular system, where a common pressure wave (e.g. the aortic blood pressure wave) P0 (n) is fed to the
channel inlets and propagated through the channels to create the distinct pressure waves P (n) and P2 (n)
at the channel outlets. In Fig. 2.3, Zck and Ztk are the characteristic and the terminal load impedances,
rk (z) is the resulting reflection coefficient, and n
An (k)+n k)
is the pulse transit time for k=1,2. The
locations of the sensors are nfk) in pulse transit time away from the inlets of the channels. Note that the
superscripts i and r represent "incident" and "reflecting" components of the pressure wave, respectively
It can be shown that for a uniform and lossless channel, the dynamics between P0 (n), the pressure
wave at the inlet, and Pk (n), the pressure wave at the outlet, is given by [49,50]
Gk
Gk (z)
(z) Po
(n)
Po(n)
+kk
)k(z)
Z"
+z-"rk
k
for k=1,2, where rk(Z) A
sk
z~kDr• k ()+z'-"
(
k• ()
Dkk (ZZ)
(Z)
(2.15)
(2.15)Dk
,) and Dk (z)and Nrk (z)are polynomialsin z.It isnoted that the
(z)
denominator Dk (z) consists of two polynomials, znk Dk (z) and
Z- nk Nrk
(z), due to the incident and the
reflecting pressure waves, which are separated out, leaving zero-coefficient terms in Dk (z). These zerocoefficient terms may also arise in the numerator polynomial Nk (z) if a channel dynamics is made up of a
series and/or parallel connection of multiple wave propagation channels shown in Fig. 2.3.
Po(n)
Fig. 2.3. An illustrative wave propagation channel.
Plugging (2.15) into (2.4) or (2.11) clearly shows that the identifiability conditions and identification algorithms for this class of 2-channel IIR and Wiener wave propagation systems are equivalent to the problem
of when and how to decompose a sparse denominator polynomial from its product with an arbitrary numerator polynomial (since the numerator polynomial may or may not possess zero coefficient terms). In general, it
is impossible to uniquely decompose the two polynomials from their product, because the coefficients are
related by a set of bilinear equations. As we will demonstrate, however, the sparseness of the denominator
and/or numerator polynomials, ie. the zero coefficient terms, can be exploited to identify a subset of their
coefficients directly from their product, which can be subsequently used to obtain a set of linear equations
from the original set of bilinear equations that can yield the remaining set of the coefficients in the denominator and numerator polynomials under certain conditions. We first provide the following definitions:
n-i
Definition 2.1 (Sparse Polynomial): A polynomial D(z)= z"+
akzk is a sparse polynomial if it has at
k=O
least one zero coefficient between its highest-order and lowest-order terms.
E]
Example 2.1: D(z)=z 7 +a z4 +a1z+a isa sparse polynomial since a6 =a5 =a3 =a 2 =0.
n-1
Definition 2.2 (Separation): A sparse polynomial D(z)= zn + Zakzk has a [vk,Wk ] separation at k if
k=O
it satisfies
ak+1
.
. ak+vk = 0 and ak-1...-
ak-wk = 0.1
Example 2.2: D(z)=z 8 +a4z4 +a1z+ao has a [3,2] separation at 4. It is noted that v=oo for the
highest-order term and w= oo for the lowest-order term.
Before rigorously dealing with the blind identifiability conditions and the blind identification algorithms,
we first graphically demonstrate the role of sparseness, i.e. the separations, in securing the identifiability of 2-
channel IIR and Wiener wave propagation systems. Both (2.4) for IIR dynamics and (2.11) for Wiener dynamics yield, generally
P (z)T
ý (n)=D 2 (z)N,(z) (n)= D,(z)N2(z) 2 (n)N= P2
2(z)2 (n),
with 4•(n) •i (n)for IIR dynamics and
(n)(n)
for Wiener dynamics, respectively, where i=1,2.
(z)• (n) to examine the decomposability of
Let z,(n)AP 2 (z)2(n) and uI (n)N
(2.16)
P (z) into D 2(z)
and AF (z), then (2.16) becomes:
n
z2 (n)= D 2(z)ul (n)= u (n)+
(2.17)
a2u(n-k),
k=1
where it is assumed that z2 (n) is available from solving (2.4) for IIR dynamics and (2.11) for Wiener dynamics, which suggests that z2 (n)can be viewed as the output of an FIR filter D2 (z) in response to the input
u,(n). Note that u,(n)depends on
u (n)ý•,(n)+ ,b()
1
(n),...,, (n-m):
,(n-j).
(2.18)
j=1
28
Fig. 2.4 graphically demonstrates the linear regression relationship (2.17) between z2 (n) and ul (n). If,
in particular, the channels are represented by FIR dynamics, Le. N, (z)= 1, then each of the regressors in
(2.17) becomes an impulse, and all the coefficients in D2 (z) can be determined uniquely in a single step by
formulating the input-output relationship between z2 (n) and ul (n) in the linear regression shown in (2.19),
because all the elements in the regressor are independent of each other in time as shown in Fig. 2.4(a):
z2 (n) D(=
D2 z)u,(
--·-·
= - Yýfl
.Z1, II--
D2 (z),
(n)=
1 .. a[2)
a
(2.19)
z2(n)=
Xa
~r\~nl
1
.a.:
i
y,(n-l)
.~
P · I'
IA~rr(
I
+
[(n)
y,(?2)
i
y,(-•)
Xa.
a.
IX i
,.-•.m)
1
ly~a i
-'I
ul(k)
o
4.
yrk
+
+
yl(k-m)
Xak
Soz
X ,
i
i
-
ml Order Dependench
¢
....
ao
4-+
Ye
X oI
(a)FIR: Linear Regresion
(b)IIR &Wiener Regression inthe Absence of Separations
z2(n)=
+
---~m1I
y,(!O)yi(-2-1)
X a.
Xear,,,)
+
X , 2(,. I)
e
Independence
y(k)
±"
I
"
y.(k-m)
X ak
o.-I
IX Ok(.+)
(c) IIR &Wiener: Regression in the Presence of Separations
Fig. 2.4. Linear regression of Z2 (n) for FIR and IIR/Wiener dynamics.
However, if (2.19) is extended to IIR and Wiener dynamics, i.e. N,(z)# 1, then each of the regressors in
29
(2.17) becomes a train of impulses, and the samples of u1 (n) are no longer independent of each other in
time. In fact, since u, (n) depends on 4 (n),--,4,(n -m),
u, (n) is correlated with u, (n ±i) for 1< i m
as shown in Fig. 2.4(b), and in general the input-output relationship between z2 (n) and ul (n) cannot be
expressed as a linear regression shown in (2.19).
akk:1
0100
I
ak
o
t
t-
tt
·
[ !::.±l·,-~t~
-
i
?
i
I
Lnt··1ZLBa
.(A)-inFig. 2.7
.........
. .......
(B) in Fig. 2.7
aA.1
ab.
!
.....""""t
N(z) -0
Z2
as
IKnjtown
bm-lt
t
? ?
?
i
L------------------------------
b's Known
??ttI
Af
I
If
a's &b's Known
LknIown
4~-r?
D(z)
%
0a
0
? I f ft~
t
t ?t
Azblsoko7! J jAW
..
?.k..4?
? ? t
Fig. 2.5. Decomposition of P (z) into D2 (z) and N (z) in the absence of [v, w] separation with v m
and w 2m.
Comparing Fig. 2.4(a) for N, (z) = 1 and Fig. 2.4(b) for N, (z) # 1 suggests that D2 (z) should have
[v, w] separations with v _m and w > m, as shown in Fig 2.4(c), to formulate the input-output relationship
between z2 (n) and ul (n) in a linear regression equivalent to (2.19) and determine all the coefficients in
D2 (z) in a single step, i.e.
)
ul
Z2 (n)= D2 Z)ul(n) = ul n)+1ak(m+
(2.20)
(n-k(m+ )),
k
which shows that the existence of appropriate separations in D2 (z), i.e. D2 (z) being a sparse polynomial,
is indeed crucial to determine the coefficients in D2 (z) and Nl (z) and decompose P (z) into D2 (z)
and N1 (z). In practice, noting that each of the regressor elements e.g. ul (n- k(m+1)) is related to
b,,',,---,b ) which are k-independent as well as a(2) , the existence of at least one [v,w] separation
with v_Žm and w>_m in D2(z) suffices to determine N,(z) in a single step (because b
.,b )
are
determined), and then D2 (z) can be determined from p (z) AD2 (z)NJ (Z) accordingly It can further be
shown that even if D2 (z) has no [v, w] separation with v Ž m and w> m, all the coefficients in D2 (z)
and N, (z) can be determined (although not in a single step) and P,(z) can be decomposed into D2 (z)
and N,• (z) under certain conditions, as shown in Fig. 2.5.
Remark 2.1: The decomposability of P2 (z) into D,(z) and N2 (z) can be examined exactly in the
P(z),J(n)
same waybyusing z (n)
and u2 (n)N
2
(z)
2
(n).U0
Based on the fundamental understanding on the benefit of appropriate separations for identifiability of
2-channel IIR and Wiener wave propagation systems, we are now ready to rigorously analyze blind identifiability conditions and develop blind identification algorithms for this class of systems. Consider a product of
n-1
two polynomials P(z) D(z)N(z), where D(z)= zn +
m-1
az
and N(z)=z m +
k=O
bkzk. Denote the cok=O
efficients of P(z) as pi, O i n+m-1. Then Pk+m is givenby
m
m-1
ak+m-jbj =
Pk+m =
j=0
ak+m-jb
ak+m-
j=j*
where j*
,
k+m<n
(2.21)
k+m 2 n
(2.22)
j=0
m
Pk+m =
+ ak
m-1
j bj
=b . +
ak+m-
j b
+ ak ,
j=j*+1
k +m -n. In general, D(z) and N(z) cannot be uniquely determined from P(z) because its
31
coefficients are bilinear combinations of the coefficients in D(z) and N(z). For a class of wave propagation systems, however, a subset of the coefficients in D(z) and N(z) can be determined from P(z) by
exploiting the separations in D(z). In particular, it is obvious from (2.21) as well as Fig. 2.6 that if
ak+ ... ak+m = 0 , i.e. if D(z) has a [vk,1 ] separation at k with vk 2 m, then ak can be directly determined from Pk+m:
(2.23)
Pk+m = ak ,
where k + m < n . It is also obvious from (2.22) as well as Fig. 2.6 that if ak ...
= a,_~
= 0,i.e. if D(z) has a
[oo,w,]
separation at n with w, = n - k, then bm_(n-k) can be directly determined from pk+m:
(2.24)
Pk+m =bm-(n-k) ,
where k + m n . In fact, referring to Fig. 2.6, it can also be shown that if D(z) has a [oo,wn] separation at
n with w,, = n - k, then bm_, ...
bm-(n-k) can be directly determined from pk+m,'
'
P,,+m-:
m-1
Pm+k+l =bm-(n-k)+ +
I
am+k+l-jbj +ak+l =bm-(n-k)+l,,
j=j'++l1
O
1• n-k-l.
(2.25)
Besides, Fig. 2.6 further suggests that (2.25) is valid at any k having vk > m in addition to n (where
v, = 0o Ž m is automatically satisfied), because the coefficients in D(z) before and after a [vk,wk] separation at k with vk 2 m are not simultaneously involved in any of the coefficients in P(z). Indeed, in the
presence of a [vk,Wk] separation at k with vk > m, P(z) can be divided as follows:
P(z)= D(z)N(z)= [D (z)+D 2 (z)]N(z)= D,(z)N(z)+D 2 (z)N(z),
where DI (z) - zn +...+ak+vk+,Zk+vk+l and D2 (z) akzk +...+a
. It
(2.26)
is obvious that the lowest polynomial
order associated with D, (z)N(z) is k+vk +1, which is greater than k+m, the highest polynomial order
associated with D2 (z)N(z), as long as vk > m. In general, therefore, any [vk,wk] separation at k with
vk _ m essentially divides the original polynomial decomposition problem into two independent subproblems with lower dimensions. Generalizing the above discussion, we have the following lemma:
32
Lemma 2.1: Suppose a polynomial P(z) A D(z)N(z) is given, where D(z) is a sparse monic polynomial of order n and N(z) is a monic polynomial of order m.
1. If D(z) has a [vk, wk ] separation at k with vk
m, then bm_-I
,
b m w,k
as wellas ak can be di-
rectly determined from P(z).
2. If D(z) has a [vk,wk] separation at k with wk _m , then the products akb,,,..., akbo can be di-
rectly determined from P(z).
Proof: The first part of the lemma is obvious from the above discussion. The proof for the second part
of the lemma is nearly identical; it is obvious from Fig. 2.6 that for a given v and
k
Wk
m, pk+j
= bkaj
holds for Oi j5 vk. Q.E.D. •
D(z)= zn + 000o + ak+v+l Zk+ v+ 1 ++ ak k
Orders
-------------------n+m
n+m-1
n+m-2
coo
oo
a0
D(z)=
km-'
K-l+m
k+m+v-1
k-2+m
m
m-1
ooo
m-2
00
k+v+l
n
+ an-k-1Zn-k-1 + an-k-2Zn-k- 2 + coo + ao
Orders
,-----------n+rn-
--------------
t---~-----rn
k+m+v+1
k+m+v
z"
n+m-k-1
n+m-k-2
n+m-k-3
n+m-k-2
n+m-k-3
n+m-k-4
m
m-1
00ooo m-2
0
k
n
0
n-k-2
n-k-1
0
Fig 2.6. Direct determination of-coefficients in D(z)
.-------1
ak+v+l
b.-
b.lak+v+
b1-2
000
I
bo
bf..ak+0 +1
I
b.2ak
r----------_boa+v
J::
boak
~,..,----------
(a) m+k < n
80
o
a:
o
bl
000
an-k-1
b.ao
b000
a
an-m-2
ac
ban-k-z
b0 1aa
b-a0
*00
br 2an-k-1
0
bao
I
be
o
boan-k-2
boa-.1
boao
(b)m+k > n
Fig. 2.6. Direct determination of coefficients in D(z) and N(z) from P(z).
It is evident from Lemma 2.1 that not all the separations are valuable for polynomial decomposition;
only the separations with vk _ m and/or wk > m can be exploited to determine the coefficients in D(z)
and N(z) directly from P(z). Due to the importance of these particular separations, we provide the following definition:
Definition 2.3 (Type-I and Type-II Separations): If a [vk,Wk] separation at k has vk > m, then this
separation is of type-I. If a [vk , wk ] separation at k has wk _ m , then this separation is of type-II. [
TYPE-I
TYPE-II
X=mk-wk
4-Vk>
Z4-L ---wo
Y-.k-wk-N-vy-t
0000
Z'
L -------1
X
'
'
X'(w'wk) ZX (w wk): 000 ZXN
L-------------------------
Z.-1
FVy.r*w
---------.
>m--
·· ~
··
LI
ww vwK
L
N(z)=Z m
m wk
+bm-wkZ +bm-wk-1Z m wk'
+bm-wz"
w
mw
+bm-w.Zz
- -1
+bz'
+boz
Fig. 2.7. Separation structure of lower dimensional decomposition problems.
In general, Lemma 2.1 by itself can determine only a subset of the coefficients in D(z) and N(z),
while the remaining coefficients are subject to a set of bilinear equations shown in (2.21) and (2.22). However,
substituting the set of coefficients determined by Lemma 2.1 into (2.21) and (2.22), some of those bilinear
equations turn out to be linear equations, which can be solved to determine the remaining coefficients in
34
D(z) and N(z) under certain conditions. First note the following lemma:
Lemma 2.2: Everytype-II separation entails a type-I separation.
Proof: Consider a type-II separation at k. Then ak- = ... ak=
0 holds for wk Ž m, which can be
seen as a type-I separation at k- wk -1 with vk-wk- = Wk > m . Q.E.D.[]
Recalling that any [Vk, wk ] separation at k with vk Ž m essentially divides the original polynomial decomposition problem into two independent sub-problems with lower dimensions, Lemma 2.2 essentially suggests that each sub-problem assumes the structure shown in Fig. 2.7, which involves a type-I [vk, wk ] separation at k followed by a type-II [vy-1,Wy 1,] separation at Y -=
k - wk - N- vy- 1 -1 and possibly contains
additional unknown terms ak-,_,_,1,'ak-w-N in D(z) between them. Note that shown at the first row in
Fig. 2.7 is a part of D(z) associated with a sub-problem, while shown at the first column is N(z). The
coefficients a,.b
for Y-l1 il k and 0 5 i2 ! m, resulting from the product of each terms in D(z) and
N(z), are also shown. Then we have the following result on the decomposability of P(z) A D(z)N(z) into
D(z) and N(z):
Theorem 2.1 (Sufficient Conditions for Blind Identifiability): Suppose a polynomial P(z) A D(z)N(z)
is given, where D(z) is a sparse monic polynomial of order n and N(z) is a monic polynomial of order
m, respectively Let
w~= max[w lvk
(2.27)
iT max [vklwk m]
1. If v+i•_m,then P(z) canbe uniquelydecomposedinto D(z) and N(z).
2. If V+ <m,then P(z) can be uniquely decomposed into D(z) and N(z) if,for any k,there
exists a type-I [vk,wk ] separation at k in D(z) followed by a type-II [y_1 , w_,Wy] separation at
Y- 1 = k- wk - N - vy 1 -
with N unknown terms ak-wk l, , ak-,
-N
between them, which sat-
isfies the following two conditions, where p(-) is the rank of a matrix and the matrix A is shown
in Fig. 2.8:
1) i
max [(m+N+wk),l (N+wk + vY)].
(2.28)
2) p(A)=m-2,+wk +N+1.
(2.29)
jl=k-wk-1
j2=k- w
Pk+m-w-1"rajbk+m-w-1-j
1
l
o0
L-I-
E
Pk+m-wk-Najbk+m-wk-N- IZ
12--zv
0
0
---6----h
----0
S=2w-N-wk-Vy-1
Fig. 2.8. Matrix equation for determination of bm-~-1, * ,bo , ak-~_1,,',ak-_k-N and ayr-.
Proof: First of all, Lemma 2.1 guarantees that bm_,, , ,bm_
and ak, as wellas al-, ** ,a_-lbo ,can be
determined directly from P(z). Suppose v+ •_2 m, then ay,_ can be determined from
Pv+y-i =ayti
1 ,
(2.30)
because V _m- i and b~ should be available from bmi,_,,,bm,_. Using ay_1 , the remaining coefficients in
N(z), b_,..--,bo, can be determined by
Pj+-_ = ar-lbj
(2.31)
for o0 j IvF-1i, which determines N(z). Then D(z) is determined bysolving P(z) ' D(z)N(z) .
Now suppose V+ i < m . First, it is obvious from Fig. 2.7 that ak-.1_l,..a
mined from bm_,...,b,_
k-w can be uniquely deter-
by a set of linear equations shown in Fig. 2.9, because i > wk .Then the area (A)
36
in Fig. 2.7 becomes available for constructing a set of linear equations to determine the remaining coefficients
in D(z) and N(z). In particular, Fig. 2.7 shows that totally i+1 linear equations are available for
m+N-2i + wk+l unknowns, i.e. bm_,-l,.. ,bo (m-w unknowns), ak-
l,..",akwN (N-(ik-wk) un-
knowns) and ay_1 (1 unknown). Therefore, we require
ii +12 m+N-2i
+wk ++1=> 2- (m+N+wk),
3
A
t
I
W-Wk
1
0
bm-1
1
(2.32)
p
ax-1
Pm+X-2-akbm-wk-2
0
0
bim-
pm+x-l-akbm-wk-1
00
0a
0
0
0
bm-(w-wk)+l
000
t
aX-(w-wk)
(W-Wk)X(W-Wk)
Fig. 2.9. Matrix equation for determination of ak--l,.
t
Pm+X-(w-wk)-akbm-w
Nonsingular Matrix
, ak-( -wk)"
which implies that the number of linear equations should be greater than or at least equal to the number of
remaining coefficients. Next, we will show by contradiction that at_1 is included as an element of the vector
of unknowns in the set of T+ 1 linear equations. Assume that ay_1 is not included in the set of linear equations. Then it is obvious from Fig. 2.7 that the following inequality should hold:
T< N-(v- wk )+vr_
,
= W < I(N+
2
(2.33)
w, +v,_).
Combining (2.32) and (2.33), we have
2(m+N+ wk) : 6 <3(N+wk +vyl),
(2.34)
which reduces to 2m <(N+wk + vy- 1)+ 2vy- 1. Re-applying (2.33) to this inequality yields m < i+ vy_ 1 , which
is a contradiction because it violates m > w+iT-
+ v,_,1 . Therefore, by,1 is included as an element of the
37
vector of unknowns in the set of ii+
i_ N-(_
-wk)+ vy -
2
linear equations, and we also have, instead of (2.33),
(N+ w +vy_),
(2.35)
which, together with (2.33), constitute the first condition. Then it can be shown that the set of -+ 1 linear
equations can be formulated into the matrix equation shown in Fig. 2.8, where the second condition is derived: A should have full column rank for the matrix equation to have a nontrivial solution. Q.E.D.
]
Remark 2.2: The second blind identifiability condition essentially suggests that there should exist at least
one type-I [vk,Wk] separation at some k other than n in D(z), where wk # wn. Indeed, (2.32) can be
rewritten as
(i- wk)+ [2i -(m + N)] Ž0,
(2.36)
where 2 - (m + N) wk +vy-1 - m from (2.35), which, combined with (2.36), yields
( -wk)+[2iw-(m+N)] _( -wk)+[wk +VY-m]_ 0.
Noting that
k + v,_ 1 < m,
(2.37)
it can be concluded that W> wk. In fact, for a special case where N = 0, the sec-
ond sufficient condition for decomposability ie. when v+ w < m, reduces to
N= 0 implies wk = Vy_ 1 by Fig. 2.7, which reduces (2.32) and (2.35) to wf
3
W> w k
as follows. First,
(m+wk) and 3 Wk ,respec-
tively The first inequality can be rewritten as:
(;-wk)+(2w-m) 0,
while the second inequality, together with
(2.38)
k=
vy_, implies w2 VŽ_1, which, together with w >Wk, yields
2, 2_wk + vy_1 .Since Wk +vy_ 1 < m by assumption, we get 2W <m, which, combined with (2.38), finally re-
sults in w> Wk.]
Example 2.3: Suppose the 2-channel wave propagation system represents two distinct branches of a cardiovascular system with the following terminal load impedance function:
['k (Z)
(2.39)
bk
z+a
k
Then it can be shown that the dynamics between the pressure waves at the channel inlet and at the sensor
locations can be expressed as follows:
(k)
(Z)Zn2 +Fk(Z)
Gk(z)
znk +k
which yields
Dk (Z)
(k)
2
Z -n
(k)
(Z+ak)nk
(z)z-nk
2
n+l+akz
k)
(Z+ak)zn2 +bkZ-n2
2
nk +bk
+bkz
and
-nk
k(z)
(2.40)
, k=,2.
2n
+a
2
+bk,
where, we have V= 2 nk
= 0, and m = 2n k ) +1.Therefore, the following blind identifiability conditions for each of the channels
can be obtained from Theorem 2.1:
2 +1
, 2 n2(2)
(2.41)
l)
n1
2 n~ +I'
which implies that nik) needs to be sufficiently small, or physically the sensors need to be placed close
enough to the outlets of the channels. []
2.2.2. Blind Identification Design: Sensor Locations and Sampling Frequency
Theorem 2.1 can be exploited to design the blind identification procedure, including the selection of
channel lengths, sensor locations and sampling frequency In essence, the blind identifiability of 2-channel IIR
and Wiener wave propagation systems requires high-order separations, i.e. separations having large v's and
w 's. Noting that the separations arise from the nonzero pulse transit time, and their orders (v's and w 's)
depend on the sampling frequency the blind identifiability conditions can be actively met in many real-world
applications by appropriate choice of channel lengths, sensor locations and sampling frequency:
1. It is obvious from Fig. 2.3 that moving the location of the sensors changes the pulse transit times,
k),
which in turn alters the separation structures, i.e. n(
•
k), and
nk in(2.40). In particular, mov-
ing the sensors more distally, i.e. away from the channel inlet, results in the decreased pulse transit
times n k),which reduces the orders of the numerator polynomials and makes it easier to secure
blind identifiability On the other hand, if the sensors are placed at the outlets of the channels, it becomes easier to secure blind identifiability by recruiting longer channels, which increases the pulse
transit times nk, resulting in the increased separation orders in the denominator polynomials.
2.
It is also obvious that adjusting the sampling frequency results in the alternation in the separation
structure even in the absence of sensor relocation, by virtue of the relationship between the discrete
and continuous pulse transit times, i.e. the discrete pulse transit time is the continuous pulse transit
time multiplied by the sampling frequency Therefore, increasing the sampling frequency results in
higher-order separations, since the separation orders (which are nothing but the discrete pulse transit
times) are essentially proportional to the sampling frequency
In fact, blind identification design is closely tied up with the system design itself in the sense that the
length of the channels, the locations of the sensors as well as the sampling frequencies are important system
design specifications.
2.2.3. Blind Identification Algorithms for IIR and Wiener Wave Propagation Systems
Once a 2-channel IIR or Wiener wave system satisfies the blind identifiability conditions in Theorem 2.1,
its dynamics can be identified by following the procedure summarized below:
1. For IIR dynamics, formulate (2.5) into a matrix equation using the time series sequences of Y, and
y2 to form a set of over-constrained linear equations, i.e. N > n, + m i+ n2 +
2:
(2.42)
p [y, -2y]p = O,
where N is the length of the time series sequences used to solve (2.42), and
S(n)-
[y(n+n2
m
,(n)],
2(n)! [y2 (n
40
2)
(n)].
(2.43)
For Wiener dynamics, formulate (2.12) into a matrix equation using the time series sequences of y,
and Y2 to form a set of over-constrained linear equations, i.e. N > n1 + mi + n2
2 +2
=0
:
(2.44)
where N is the length of the time series sequences used to solve (2.44).
2. For IIR dynamics, identify p from (2.42) using singular value decomposition:
V
T
[YI -Y2 ]= U
(2.45)
,
where the column of the unitary matrix V corresponding to the minimum singular value is taken
as the estimated value of p, the unit vector satisfying (2.5). For Wiener dynamics, identify i from
(2.44) using singular value decomposition. Then determine p and 11 using (2.14).
3. If possible, identify
Ilpil
and determine p =Ijplf.
4. Let P(z)= P, (z) , D(z)= D2 (z) and N(z)= N1 (z). Determine i
to determine b0),
5. If
+i
..
b'ý
a~2) and a(2)
,...,1 a
b
and 7. Then use Lemma 2.1
for all k,Y=k- wk-N-v
pairs.
m, then first determine N(z) using (2.30) and (2.31). Then determine D(z) by solving
the equality P(z) - D(z)N(z).
6. If v + w < m but (2.28) and (2.29) are met, then formulate the matrix equation in Fig. 2.8 to determine N(z). Then determine D(z) by solving the equality P(z) - D(z)N(z).
7. Repeat the steps 4, 5 and 6 above for P(z)=P2 (z), D(z)= D (z) and N(z)= N2 (z).
8. Characterize D,(z), D2(z), N (z) and N2 (z) from D1 (z),
9. Characterize G (z)=N (z)D- '(z) and G2 (z)=
2 (z)D21 (z).
2(z),
N1 (z)
and N2 (z).
2.3. Input Signal Reconstruction for 2-Channel IIR and Wiener Systems
Once the dynamics of a 2-channel IIR system or a 2-channel Wiener system is identified, the unknown
input signal can be reconstructed by de-convoluting the output signal measurements from the identified IIR
or Wiener system dynamics. First, if at least one of G,(z) and G2 (z) has a stable inverse, the unknown
input signal may be reconstructed by directly filtering the output signal (for IIR dynamics) or intermediate
signal (for Wiener dynamics) using G;' (z) or G21 (z), whichever is stable. If both G,(z) and G2 (z)
have unstable and/or unacceptable (e.g. damping is too low, dominant time constant is either too fast or too
slow, etc.) zeros, however, an additional step for designing a stable de-convolution filter is needed. In this thesis a novel algorithm for designing a de-convolution filter that is applicable to a general class of multi-channel
IIR and Wiener systems is developed and analyzed. It is shown that the solution to the de-convolution algorithm is guaranteed to exist as long as the identified multi-channel dynamics does not share any common zeros, which is an extremely trivial condition in the sense that the channels determined by the blind system
identification methodology do not share any common poles or zeros.
2.3.1. IIR Systems
lThe de-convolution filter design algorithm developed in this thesis is built upon the concept of coprime
transfer functions [51]:
Lemma 2.3: Two stable, proper, real-rational transfer functions M, (z) and M2 (z) are coprime if they
have no common zeros outside the unit circle and at least one of them has zero relative degree. If M, (z)
and M2 (z) are coprime, there exist stable, proper, real rational transfer functions W, (z) and W2 (z) that
satisfythe following generalized Bezout identity [51]:
M, (z)W, (z)+ M2 (z) W2 (z)= 1.[
(2.46)
Based on the concept of coprime transfer functions and Lemma 2.3, this thesis presents the following
novel de-convolution filter design algorithm:
Theorem 2.2 (De-Convolution Filter Design Algorithm for Multi-Channel IIR Systems): Consider a 2channel IIR system shown in Fig. 2.1. If G,(z) and G2 (z)possess no common zeros, then the unknown
input signal can be reconstructed from the output signal measurements yi(n), i=1,2 using the deconvolution filter shown in (2.47) with the identified multi-channel dynamics G,(z,O) and G2 (z,O), where
o0
-(
l,b,a
•2
2,,b
u(n) =
where
with a a')...ai,-1, and b,
Ab(o,-b
D2 (z,0)
Izo1<1,
(Z--z0 )n- m
l(n)
D (z,
(n),
)n
for i=1,2:
(2.47)
,
2.47)
G2 (z0,o0) 0, and ir,(z) and z7
2(z) are polynomials in z of order n2 and (ni-1), re-
spectively, satisfying
(z-zo)
-m
' N, (z,9)t1 (z)+N 2 (z,0)q2 (z)= D (z,)D
2
(2.48)
(z,O).
Proof: From (2.1), (z- zo)-"'G,
(z,O) isatransfer function with zero relative degree, and therefore,
(Z-z)l n -m l G1 (z,0) and G2 (z,0) are coprime. Hence, from Lemma 2.3, there exist stable proper transfer
functions W,(z) and W 2 (z)satisfying
(2.49)
(z-zo)" m"'G,(z,0)W,(z)+ G2 (z,0)W2 (z)= 1.
Constructing W,(z) and W2 (z)as
W,(z)= 71 (z)D-j'(z,O), W 2 (z)=72()D'I(z,O),
(2.50)
then (2.49) reduces to the polynomial identity (2.48). Multiplying u(n) to both sides of (2.49) yields (2.47).
Since rh (z) and q72(z) together give nl +n2 +1 unknowns and both sides of (2.48) are polynomials
of order nI+ n2 , (2.48) results in a set of n + n2 +1 linear equations with nI+n2 +1 unknowns, Aq = i
shown in Fig. 2.10, where
+...+T') z
zo) NJ (z,o)= -')z"l
(zD,(z,0)D2 (z,0) =",,n+n2 " +...+
o
•
n(2.51)
n4--of
.n2I,
1 L
c
4
r
r;
)r
lani*,/6
D
'Ui/Q/'
1 L
PI
11n2i
W1'
03
Fig. 2.10. Matrix equation for the design of a stable de-convolution filter.
the coefficients of the de-convolution filter.
The matrix A should be nonsingular for the existence of qi,
First, it is evident from the structure of A that the columns of the sub-matrix A2 are linearly independent
of the columns of the sub-matrices A, and A3 as well as of each other, because b(1) 0; otherwise
deg[NI (z,0)] <mi
since b')=b ).It then follows that the sub-matrix [A,
A3 ] should be nonsingular
for non-singularity of A . Noting that [A1 A3] is the Sylvester matrix of (z-zo)"l- m' N1 (z,O) and
N2 (z,0), these two polynomials should be coprime, which is always guaranteed because G1 (z,0) and
G2 (z,0) have no common poles and zeros and zo is chosen such that G2 (z0 ,0) 0.QE.D.]
The block diagram of the de-convolution filter is shown in Fig. 2.11.
Example 2.4: Consider a 2-channel IIR system with G,(z)=
z-2
-2
z2-0.5
and G2 (z)=
1
z-0.8.Then the de-
convolution filter is given by (2.47):
(n)=-1" (
u(n)-
n) + 1"
2 (Z)
(z-y (n)+
z2 (n),
z-0.5 2
z-0.8 ,
(2.52)
where q,(z)A $f')z+ q') and q2 (Z) A 72) satisfies (2.48):
(z-2)+
(I
(2.53)
(+z(')
0.5)(z -0.8),
=(z-
which yields q$') -1,7) -=0.7, and (2)
• 1.8. Therefore, the de-convolution filter becomes
z + 0.7
1.8
u(n)= z
Yl (n)+ -- Y2 (n)
,
z-0.8
(2.54)
z-0.5
which is indeed capable of reconstructing the unknown input signal:
z+0.7
1.8
0yl (n)+
S( -
Y2 (n)
z-0.8
z+ 0.7
z-0.5
-2
1.8
=z+.7 z-2 u(n)+I'8
z-0.8 z-0.5
1
z-0.5 z-0.8
(n)
z2 -1.3z-1.4)+1.8]
z2 -1.3z+0.4
u(n)=u(n)
(2.55)
-yl(k)*
Fig. 2.11. Block diagram of the de-convolution filter (r, n - mi).
2.3.2. Wiener Systems
The above de-convolution filter design algorithm for multi-channel IIR systems is also valid for multichannel Wiener systems without any extension and/or modification, by noting that once a multi-channel
Wiener system is identified, the intermediate signals x, (n) and x2 (n), instead of the output signals yi (n)
and y2 (n), can be used with the above de-convolution filter design algorithm to reconstruct the input signal
for the multi-channel Wiener system.
2.4. Persistent Excitation and Model Identifiability Analysis
For IIR dynamics, solving (2.42) for p hinges upon the rank condition of the matrix [Y
represents the richness of the signals y, (n) and Y2 (n). As the dimension of p increases, [,
-Y2 ],which
-Y2] gets
closer to singular and the resulting p estimated from the blind identification becomes unreliable. Equivalently for Wiener dynamics, solving (2.44) for P hinges upon the rank condition of the matrix [4 1 -(2 ].
As the dimension of P increases, [(D
-42] gets closer to singular and the resulting P becomes unreli-
able. Therefore, care must be taken to determine the model structure (i.e. its complexity), given the output
signal measurements having limited richness. This critical issue can be addressed by examining the persistent
excitation and model identifiability conditions [52,53].
Consider first an IIR system. Let P (z)= p(m)zn2+mI
+...+
p1) and rewrite (2.5) as:
(2.56)
)-(n+n + m )= qTy(n),
where qi
r (Pn2-1
+M-1
)
LPn2 +m,_"
LL
y;(n)=[-5(n+n2+m M -1) ...-
ad
p j, and
(n)
Y 2 (n)] T .
(2.57)
Given the time series sequences of Y, and y2, (2.56) can be formulated into:
Yi(n+n
[yl
2
+m 1 )
q A q,
(2.58)
(n+n
2 +mI -N)
where N > n, + m + n2
+
2 . It can be solved for q using the least-squares method if (DJT4
isnonsingu-
lar, which means that -yand 72 persistently excites the system so that p is determined to scale (see Remark 2.3). Therefore, the persistent excitation condition is given by the positive definiteness of
1
1
N1
N+I
4~:
y(k)y
k=n-N
(k)= N
N+I1-(1 > 0.
(2.59)
Remark 2.3: It is easyto show that p identified from (2.42) and q identified from (2.58) are equivalent
up to scale if the regressor signal y(n) is persistently exciting (see Appendix A). Therefore, the persistent
excitation condition for the original blind system identification problem (2.42) reduces to the persistent excitation condition for the least-squares problem (2.58), which isgiven by (2.59). ]
The above result can be readily extended to a Wiener system. Let P (z)= pl
zn2+m, +...+ p1) and
rewrite (2.12) as:
(2.60)
S(yl (n+n 2 +m,))= qT (n),
where
r
qq"pn(1)
2+m
F
-
PP +m-
P
(1)
(1)
1
2L-- Pp
117
(2)
(1)
1
--(1)
.
p
p2
r7i
(2)
]TT
p
""--2 "
(2.61)
'171
and
q(n) A[-4 (y (n +n2 +m1 -))...--
(y (n))
--P2 (Y
(n))...Pk,(y(n))
4p(Y2(n))...'pk2
(2(n))]T.
(2.62)
Given the time series sequences of Y3;and y2 together with the knowledge of the basis functions, (2.60)
can be formulated into:
FA
(yn+n
+m
22))
1
q cDq,
(2.63)
A(yl(n+n 2 +m -N))
where N >nj +mi +n2 +m2 + 2, which is equivalent to its IIR counterpart (2.58). Therefore, the persistent
excitation condition is given by (2.59) but with the Wiener regressor (2.62) instead of the IIR regressor (2.57):
1
N+1
i (k)ý
k=n-N
T
(k)= -
eDT
> 0O.
(2.64)
N+1
Once the persistent excitation condition is satisfied, the model identifiability condition becomes trivial
both the IIR model structure (2.56) and the Wiener model structure (2.60) are always identifiable, since they
47
are moving-average models [52,53].
2.5. Asymptotic Variance Analysis
Analyzing the parameter estimation error variance is essential in order to judge how confidently and reliably the parameters of an unknown dynamical system can be identified. Although it is hard to compute the
exact variance of the parameter estimation error, var( -00), since 00 (the vector of true model coefficients) is not known in practice, the expected variance can be estimated as the "asymptotic" variance based on
the model structure and the empirical measurements [52,54].
For 2-channel blind IIR system identification, the model coefficients are determined by minimizing the
error associated with (2.3):
n,+ ) Ad, (z,6)i (n)-
2(z,6) 2(n),
(2.65)
which is defined as the empirical measurement error. Following [52,54] it can be shown that, using the time
series sequences of y, and y2 with N > 1, the variance in estimating 0 asymptotically converges to
1
1
NI
tivity of e(n,0) to 0, and SN (0) is the inverse of the sensitivity covariance matrix. The variance is not
computable since it is evaluated at 00. However, the following empirical approximation using the estimate 6
suffices in many applications:
var(6--eo )= -I(6)SN
(6).
(2.67)
The variance var(G(z,6)-Gi(z,e0)), i=1,2, of estimating G,(z) and G2 (z) can then be obtained as
follows [52,54]:
var (G z,0)-G 1(z,0o) ))
dG!z,)
dG (z',)
var 0-0
i=1,2.
(2.68)
From this asymptotic variance we can obtain useful insights as to how reliably the system is identified:
1. The asymptotic variance is inversely proportional to the length of data N used for identifying the
system. This gives a guideline to choose N in order to reduce the parameter estimation error variance to a desired level.
2. If one or more of the model coefficients have very low sensitivity upon the empirical measurement
error (2.65), the inverse of the sensitivity covariance matrix SN (0) blows up, or it becomes extremely large as the sensitivity diminishes. This often happens when the model contains too many
coefficients to estimate. Such low-sensitivity coefficients should be eliminated from the model
3. The reliability of the frequency response identification depends on its sensitivity to 0 as well as
var(6 -0), as suggested by (2.68). In particular, if an element in 0 has large sensitivity on the frequency response at certain frequency range, the reliability of the frequency response identification in
that range hinges upon the quality of that element. Such high-sensitivity model coefficients should be
identified very carefully
4. Too large AN implies that the measurement is noisy and/or the model structure does not fit the data.
In this case, the signal quality must be improved, and/or the model structure should be reconsidered.
Therefore, the asymptotic variance analysis can provide a warning sign and quality measures for the validity of the 2-channel IIR blind system identification.
It is also noted that since a 2-channel FIR system is a special case of a 2-channel IIR system with unity
denominators, and a 2-channel Wiener system is a multi-variable extension of a 2-channel IIR system with
multiple output measurements, the end results on the asymptotic variance analysis, (2.67) and (2.68), can be
applied to 2-channel FIR and Wiener systems with trivial modifications to (2.65).
0-00
I
I
I
I
i
I
I
I
I
I
I
I
I
I
I
e
I
1
N
Fig. 2.12. Asymptotic variance of parameter estimation error.
2.6. Summary
The main theoretical contributions of the thesis were presented in this chapter. Specifically blind identifiability conditions and blind identification algorithms for a class of 2-channel IIR and Wiener wave propagation systems, as well as a novel design algorithm for a stable input de-convolution filter for general class of
multi-channel IIR and Wiener systems, have been developed. In addition to these theoretical contributions,
persistent excitation, model identifiability and asymptotic variance have been analyzed within the context of
2-channel blind system identification as effective measures and tools to determine the system order and other
key parameters of the black-box dynamics as well as to assess the quality of the identified gray-box dynamics
of the 2-channel IIR and Wiener systems, in terms of both accuracy and reliability The theoretical developments and analysis presented in this chapter will be extensively used throughout the remainder of the thesis
for identifying the multi-channel cardiovascular wave propagation dynamics and reconstructing the aortic
blood pressure and flow signals.
Chapter 3. Multi-Channel Cardiovascular Wave Propagation
This chapter concentrates on how the theoretical development and analysis presented in Chapter 2 can
be exploited to identify the cardiovascular wave propagation dynamics. Especially this chapter will demonstrate how a cardiovascular system can be viewed as a multi-channel wave propagation system, by providing a
brief overview on its anatomy and the blood pressure wave propagation.
3.1. Cardiovascular System Anatomy
The main components of a cardiovascular system are the heart, the blood and the blood vessels. The
cardiovascular system includes 1)the pulmonary circulation, a loop through the lungs where blood is oxygenated, and 2) the systemic circulation, a loop through the rest of the body to provide oxygenated blood. In this
thesis, we are interested in identifying the systemic portion of the cardiovascular system.
The systemic cardiovascular circulatory system is made up of a series of multi-branched channels (or
vessels) connected in series and/or parallel, as shown in Fig. 3.1. All the arterial branches arise from the aorta,
which stems from the left ventricle and contains a valve at its origin, the aortic valve, which prevents the
blood flow back into the left ventricle during diastole, i.e. the ventricular relaxation. The aorta is divided into
the aortic root, the ascending aorta, the aortic arch, the thoracic aorta and the abdominal aorta. The blood is
supplied to the upper limb through the major branches of the aortic arch, e.g. the carotid and the subclavian
arteries, and to the lower limb through the bifurcations from the abdominal aorta, e.g. the iliac and the femoral arteries.
Summarizing, a cardiovascular system can be viewed as a multi-channel dynamical system, where the
central cardiovascular dynamics, represented by the aortic blood flow and/or the aortic blood pressure, is
transmitted distally through different arterial paths. If sensors are placed at multiple distinct peripheral locations, e.g. the radial and/or the femoral arteries, then the central cardiovascular wave propagation dynamics
51
can be observed at multiple extremity locations. From a system theoretic point of view, therefore, a systemic
cardiovascular system is a multi-channel system with the heart as a source, the arterial branches as channels,
and the peripheral sensor measurements as outputs.
Fig. 3.1. Cardiovascular system anatomy
3.2. Wave Propagation in Cardiovascular System
As the blood pressure wave travels back and forth in the cardiovascular system, its morphology is distorted due to the wave propagation and reflection phenomena. Specifically there are three major changes as
the blood pressure wave travels towards distal extremity.
1. The pulse transit time, associated with the onset of initial systolic rise in the blood pressure wave,
increases due to the finite pulse wave velocity.
2. The peripheral blood pressure wave has larger systolic blood pressure and lower diastolic blood
52
pressure than the aortic blood pressure.
3. The dicrotic notch, a high-frequency feature of the aortic blood pressure wave, is damped out and
disappears at distal extremities, due to the visco-elastic properties of the arterial wall.
Although the aforementioned distortion of the blood pressure wave in the cardiovascular system is caused by
a variety of factors such as propagation and reflection of blood pressure and flow waves, visco-elasticity of
the arterial wall, vascular tapering and bifurcations, nonlinearity in arterial compliance and so on, it can be
explained to very large extent by the wave propagation phenomena, especially within a short time window
[21]. Therefore, the cardiovascular system can be viewed as a wave propagation system.
3.3. Black-Box and Gray-Box Cardiovascular System Modeling
In this thesis, the cardiovascular dynamics is considered to be an unknown and time-varying process.
However, over short time intervals, it is assumed that the cardiovascular system can be approximated as a linear time-invariant system. It is known that, on a beat-by-beat basis, the cardiovascular wave propagation dynamics is time-invariant and that the effect of nonlinearity is negligibly small [21].
In using a black-box model structure based on an orthogonal basis function expansion to identify the
cardiovascular wave propagation dynamics, it is desirable that the number of basis function coefficients, i.e.
the order of basis function expansion or the system order, to reproduce the true cardiovascular wave propagation dynamics be small, because a large number of basis function coefficients are difficult to identify unless
the system input signal is rich enough to meet persistent excitation conditions [52,53]. For instance, the standard HR representation requires a large number of basis function coefficients, particularly when the system
has a slowly decaying pole. Given that we have no control over the input source (i.e. the heart) for identifying
the cardiovascular system, it is crucial to reduce the system order. As we will demonstrate later in Chapter
5, this can be achieved with an appropriate set of basis functions that can represent the cardiovascular
channel dynamics with fewer terms.
In contrast to its black-box counterpart, a physics-based gray-box model of the cardiovascular system is
much more structured and constrained. Unfortunately however, it is known that there is no unified physicsbased gray-box model structure that can fit all different kinds of cardiovascular system. Rather, the best
model for a given cardiovascular wave propagation dynamics heavily depends on the geometry and size of its
arterial tree [21]. Therefore, we have to employ different cardiovascular system model for different species
having different upper and lower limb geometry Furthermore, even for a single species, we might have to
employ more complicated model as its size gets bigger. As we will demonstrate later in Chapter 6 and Chapter
7, the cardiovascular wave propagation dynamics of the experimental swine subjects used in this thesis is well
described by an existing IIR model called the "asymmetric T-tube" model, whereas the cardiovascular wave
propagation dynamics of the human subjects, especially the lower limb dynamics, requires much more rigorous treatment.
3.4. Summary
Cardiovascular system is a dynamical system. In particular, with sensors placed at multiple extremity lo-
cations to measure blood pressure and flow waves, it can be viewed as a multi-channel wave propagation sys-
tem. As such, many clinically important signals and phenomena can be monitored and even diagnosed by
identifying its dynamics. In the chapters to follow, we will exploit the theoretical development and analysis
presented in Chapter 2 as well as the black-box and the physics-based gray box model representations of the
cardiovascular system to identify its dynamics.
Chapter 4. Evaluation Platforms
Several evaluation platforms are employed to validate the theoretical developments for central cardiovascular monitoring in this thesis. Specifically, we will make extensive use of experimental measurements from
10 swine subjects, simulation-based measurements from 8 human subject models, experimental measurements from 15 human subjects at the Massachusetts Institute of Technology and experimental measurements
from 2 human subjects at the Massachusetts General Hospital, respectively, to illustrate how the multichannel cardiovascular wave propagation dynamics can be characterized and monitored with fidelity
Each of the evaluation platforms has its own merits against the other. First, the experimental swine subjects allow simultaneous measurement of several gold standard blood pressure and flow signals necessary for
this thesis that are not easy to collect from real human subjects, i.e. the blood pressure signals at two distinct
peripheral locations in addition to the aortic blood pressure and flow signals. Therefore, these measurements
are very useful for the initial proof-of-principle. The simulation-based human subject models are versatile in
estimating the efficacy of the central cardiovascular monitoring in this thesis in the sense that the blood pressure and flow signals associated with a variety of physiologic conditions of human subjects can be replicated
with reasonable accuracy Finally the measurements from the real human subjects are crucial in this thesis for
complete and solid validation of the central cardiovascular monitoring in real clinical practice.
4.1. Experimental Swine Subject Data
Under the experimental protocol #01-055 approved by the Massachusetts Institute of Technology
Committee of Animal Care, invasive cardiovascular data were obtained from 10 anesthetized swine subjects at
a sampling rate of 500 Hz.
Physiological transducers were placed as follows. A couple of 7.5 French sheath introducers (Arrow International, Reading, PA) were placed in the bilateral femoral arteries. A micro manometer-tipped catheter
55
(SPC 350, Millar Instruments, Houston, TX) was zeroed in vitro per the manufacturer's instructions, then fed
retrograde to the thoracic aorta from the femoral artery for central aortic blood pressure (this was passed
blindly and it was technically difficult to place the catheter tip with any more precision than somewhere in the
central aorta near the apex of the aortic arch). The second introducer was attached to the stiff fluid-filled
tubing; (Arrow International, Reading, PA) and an external pressure transducer (TSD104A, Biopac Systems,
Santa Barbara, CA) for the femoral arterial blood pressure. The chest was opened with a midline sternotomy
An ultrasonic flow probe was placed around the aortic root for the reference central aortic flow (T206 with
A-series probes, Transonic Systems, Ithaca, NY). Finally, a 25-gauge angiocatheter was placed in the foreleg,
distal to the brachial artery and attached to an external pressure transducer via short, rigid tubing for the radial arterial blood pressure. Each transducer output was interfaced to a microcomputer via an A/D conversion system (MP150WSW,Biopac Systems, Santa Barbara, CA).
The physiologic conditions of the swine subjects were widely altered in order to illustrate how effectively the central cardiovascular monitoring methodology based on the theoretical developments in this thesis
works for a broad range of physiologic conditions. The following interventions were performed to vary the
physiologic conditions of the swine subjects: infusions of crystalloid volume, phenylephrine, dobutamine,
isoproterenol, esmolol, nitroglycerine, and progressive hemorrhage. Several infusion rates were implemented
followed by brief recovery periods. The physiologic conditions of the swine subjects are summarized in Table
4.1. In.
particular, the time history of the key cardiovascular physiologic measures of the swine subject # 1 is
shown, in Fig. 4, where transient, out-of-nominal physiologic condition is followed by nominal physiologic
condition up to t=300s.
Prior to their application to central cardiovascular monitoring, the blood pressure and flow signal measurements were pre-filtered using an FIR digital filter with 30 Hz cut-off frequency and down-sampled to appropriate frequencies.
*~n
**rr
IOU
140
.
120
100
1 U
I
I
I
- ~I----I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I.
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
600
800
1000
Anl
200
400
I
I
E 120
I
I
0. 100
~-
-I-'---'
o 0
c
-- I------
60
--
I
200
r
400
Time [sec]
I
SI
E
I
I
I
I
65
E
o
30
I
I
I
I.........-
I
I
i
E
25
a
20
I
I
I
--------I
I
I
I
1
I
I
I
3
2
I-
800 1000
I
I
I
4
--
600
Ill --
Time [sec]
05
L-
m
'--'-
Il--
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
i-
200
400
600
800
1000
200
Time [sec]
400
600
800 1000
Time [sec]
Fig. 4.1. Time history of key cardiovascular physiologic measures of swine subject # 1.
4.2. Full-Scale Human Cardiovascular Simulator Data
We also used a full-scale cardiovascular simulator to illustrate the efficacy of our methodology for human cardiovascular system. In particular, we used a distributed cardiovascular system model developed by[17]
and [43] in order to create blood pressure data for several human subject models under different physiologic
conditions. This model consists of a distributed arterial system and boundary conditions to simulate the left
ventricle, bifurcations and peripheral vessels. The cardiovascular system model has thirty main arterial vessels.
The proximal boundary condition for the cardiovascular system model is the left ventricle, while the lumped
parameter models for the smaller branching peripheral vessels serve as distal boundary conditions. Given specific parameter values, the one-dimensional fluid dynamic equations are solved numerically to yield estimates
of blood pressure, blood flow velocity as well as cross-sectional area at each location in the cardiovascular
system as a function of time. Details about the modeling and computational methods are described in [17]
and [43]. The physiologic conditions of the subject models used in this thesis are summarized in Table 4.2, in
terms of the following physiologic measures: heart rate (HR), maximum left ventricular elasticity (ELV), end
diastolic volume (VED), total peripheral resistance (TPR), and mean blood pressure (BP). In particular, the
blood pressure signals, obtained from the full-scale cardiovascular simulator, are shown in Fig. 4.2, where the
aortic as well as the brachial and the femoral blood pressure signals are shown together for a single beat.
Table 4.1. Physiologic span of experimental swine data: maximum, minimum and mean values.
Mean HR
Mean BP
Mean CO
Mean TPR
[bpm]
[mmHg]
[lpm]
[mmHg/lpm]
1
173 / 85 (110)
135 / 43 (88)
5.7 / 1.7 (3.5)
34 / 18 (26)
2
193 / 55 (109)
119 / 28 (61)
5.9 / 1.4 (3.5)
26 / 8 (19)
3
293 / 80 (140)
139 / 38 (66)
7.9 / 1.6 (3.5)
53 / 8 (21)
4
195 / 99 (175)
110 / 37 (68)
7.2 / 1.9 (4.4)
24 / 12 (16)
5
180 / 93 (123)
106 / 36 (60)
5.5 / 1.5 (3.3)
37 / 9 (19)
6
207 / 83 (127)
167 / 61 (86)
4.9 / 2.3 (3.2)
57 / 15 (27)
7
159 / 72 (124)
120 / 59 (85)
5.8 / 1.4 (3.8)
43 / 11 (24)
8
201 / 99 (125)
110 / 59 (85)
4.0 / 2.4 (2.9)
51 / 14 (31)
9
204 / 89 (138)
118 / 47 (80)
5.6 / 2.4 (3.7)
35 / 8 (22)
10
200 / 50 (127)
123 / 23 (70)
6.2 / 0.2 (3.4)
117 / 11 (26)
Subject ID
Remark 4.1: The total number of the parameters in the full-scale human cardiovascular simulator that
needs to be tuned to describe a particular physiologic condition is more than 200. In this thesis, however, only
the four key parameters, ie. heart rate, maximum left ventricular elasticity end diastolic volume and total peripheral resistance, were manipulated to realize distinct physiologic conditions [17].[-]
T
130
/
I
-
120
1
T
"
--
IAortic BP
----- Brachial BP
II
.-........Femoral
BP
--
. -
105
I
110
--
I
-
S' • L "•
I
I
I
•
IL
I
Aortic BP
Brachial BP
F..........
emoralBP
•, ..--I
SJ l
E
-
I
I-----
- -- - II
"
'
I
E 100
- - -. go
- - -
--L--
L_ -- --
- -- -L-
-
-
--
-
- - - - '- ---
4
80
I I
80
1.
1
'Y`
4
4.1
I
I
4.2
I
4.4 4.5
4.6
Time[sec]
4.3
4.7
4.8
I
I
4.9
5
4.
4.7 49
4.8 4.9
4.7
S
-
I
I
I
I
-- _ -
-_--- --
-:
5.
5.7
_
--
- Aortic
BP
S-----
... Femoral BP
110
.6
5.6
55
5.5
,
Aortic BP
-- ---- Brachia
BP
--
I
(b) Subject # 2
120
S- -- - - -
I
5.
5.4
.3
.2
5.2 5.3
lime [sec]
51
5.1
5
(a) Subject # 1
115
I
75
I
I
Brachial BP
100
I•
--
E
"
XXI
I.l -- .i
I---
I:
---
---
-
......... FemoralIlBP
iL
•
100
95
I
I
I
I
I
/
70
go
S- - -"--..
85
-
-R
--,-J
-
-
-- -
'
--
I
- ---
I
I
--
I
80
-1
80
4
3.9
4.1
4.2
7
4.3
T,
4.4
I
4.5
4.6
4.7
4.8
4.9
,U
3.8
4
4.2
4.4
4.6
lime [sec]
Time [sec]
(c) Subject # 3
BP
Brachial BP
... Femoral BP
------
I
/
i
,
90
on.
.
85
-
.
I
9
.. -
-
L _
+ 4-
-
ti
.
4.8
5
I
5.2
I
('ef
-L
--L
5.4
Time [sec]
P
Femoral BP
_
I_
_ _I
_ •
i
- - --
-
I
-
I
I
---
-
a. S75
f 70
60
...
I
..... Brachial
_.
"-
85
i
I
80
I
-- -t -
-0--
.
II
-
96-
5
(d) Subject # 4
IAortic
110
4.8
1I
5.6
(e) Subject # 5
5.8
55
I
I
I
__
*"
4
4.1
4.2
4.3
I
I
4.4
I
4.5
4.6
Time [sec]
(f) Subject # 6
I
I
I
4.7
4.8
4.9
-
11U
120
-
Aortic BP
- BrachialBP
--
I
---. - . Femoral
BP
100
/-
I
.4 1-I
t--- Y-i-i-'-"*•---
4.6
-..-
-
--
-I-tr-
I
I
I
-
I
--
V11-- i- •"-'•."•±
AorticBP
..... Brachial BP
Femoral BP
.I
- -.-
I
•
'
4.8
5
I
I
I
4.4
-l
I
I
S
I
i
4.8
5
Time[sec]
5.2
5.4
4
4.2
(g)Subject # 7
4.4
4.6
Time[sec]
5.2
(h) Subject # 8
Fig. 4.2. Blood pressure signals obtained from the full-scale cardiovascular simulator.
Table 4.2. Physiologic conditions of simulated human subject models.
HR
ELV
VED
TPR
BP
[bpm]
[xl0 5Pa]
[x10- 6m3 ]
[xl0 5Pa's]
[mmHg]
1
75
10500
120
1253
98.8
2
64
6723
76
2811
87.4
3
77
5411
108
2031
96.8
4
62
3899
166
1228
81.6
5
62
7436
78
2930
93.9
6
76
943
255
2134
69.4
7
69
3268
151
1417
78.8
8
60
2644
202
1374
84.2
Subject ID
4.3. Experimental Human Subject Data
Under the experimental protocol # 2008-P-000124 approved by the Partners Human Research Committee (PHRC), human subject testing was carried out in the Wearable Sensors Laboratory at the Massachusetts
60
Institute of Technology as well as in the Cardiac Catheterization Laboratory at the Massachusetts General
Hospital.
In the Wearable Sensors Laboratory at the Massachusetts Institute of Technology non-invasive blood
pressure measurements at the middle finger were obtained using a device approved by the Food and Drug
Administration (Finapres, Finapres Medical Systems, Netherlands) from 15 subjects, which include 11 male
subjects, 3 female subject, and 1 female subject with pregnancy For those subjects whose pulse blood pressure were not wide enough, the subjects' arm posture was changed (ie. the arm was moved up and down)
during the measurement to collect wide range of blood pressure values.
In the Cardiac Catheterization Laboratory at the Massachusetts General Hospital, direct blood pressure
measurements near the aortic arch and non-invasive blood pressure measurements at the middle finger were
obtained from 2 subjects, which include a male subject and a female subject. The subjects were non-emergent
cases scheduled for routine diagnostic coronary artery angiography Subjects received low doses of benzodiazepine for anxiolysis, per clinical routine, but remained fully alert and responsive during the procedure. Patients with any form of instability (e.g. arrhythmia, bleeding from the insertion site, coronary ischemia) were
excluded from the investigation. The Apparatus used for the experiment is shown in Fig. 4.3. Per the clinical
routine, a percutaneous sheath introducer (Arrow International, Reading, PA) was placed in a femoral artery
and a diagnostic catheter was fed over a wire to the aortic arch, positioned near the origin of the left subclavian artery The positioning was confirmed by fluoroscopy The catheter was attached to stiff fluid-filled
tubing (Arrow International, Reading, PA) and an external pressure transducer ((TruWave PX, Edwards Life
Sciences, Irvine, CA), which was interfaced to a microcomputer via an interface cable (0395-2281, Fogg System, Aurora, CO), a transducer connector interface (TC[102, Biopac Systems, Santa Barbara, CA) and an
A/D conversion system (MP150WSW, Biopac Systems, Santa Barbara, CA). The non-invasive blood pressure
at the middle finger was measured by a non-invasive blood pressure measurement device (Finapres, Finapres
Medical Systems, The Netherlands), which was directly interfaced to the A/D conversion system. In the
61
course of routine diagnostics, the finger cuff of the Finapres device was placed on the subject's middle finger
for finger blood pressure. The blood pressure signals were recorded simultaneously for less than 5minutes to
minimize the interference with the routine diagnostics.
Aortic Blood Pressure
MGIT800-4
Isolation Transformer
-------
Finger Blood Pressure
Signals
P
Powers
AC Power
Fig. 4.3. Devices and connections for hospital human subject testing
For electrical safety, each device was powered by an isolation transformer (MGIT800-4). In addition, to
completely eliminate the electrical interference with the routine diagnostic set-up of the cardiac catheterization laboratory, a redundant separate pressure transducer was mechanically connected to the diagnostic pressure transducer via tubing with a flow switching valve, as shown in Fig 4.4.
Aortic Blood Pressure
Finger Blood Pressure
FDA APPROVED
~I
A,.
:---·
-I---:--;-~
tion T,.?ý
am
Catheterizat
ubi
Finapres
iiii~i!ii
iiiiii
~iii
o
at
O(D
0
/
nrn
CD
(DW
il:iiiiii
Iii
iiil
'-CD
3_u
Biopac Systems
DA100IC
Biopac Systems
MP150
iii
i!iiii
iii:ii,·/,-iiii!
,·
Cathete/g
r ization La
i'at Arhiin Syte
Cardiac
Catheterization Lab
Cardiac Catheterization
Lab
Routine Diagnostic Set-Up
Investigation Team Data Collection Apparatus
Fig. 4.4. Devices and connections for hospital human subject testing.
4.4. Summary
The evaluation platforms described in this chapter will be extensively used to demonstrate how effectively the theoretical developments in this thesis can deal with the challenges in the central cardiovascular
monitoring problem. Especially the experimental swine subject data will be used in Chapter 5, Chapter 6 and
Chapter 8 for the initial proof-of-principle of the black-box and gray-box 2-sensor central cardiovascular
monitoring as well as its extension to the 1-sensor central cardiovascular monitoring. The simulation-based
human subject data will be used in Chapter 7 and Chapter 8 to investigate the efficacy of the gray-box 2sensor central cardiovascular monitoring and its extension to the 1-sensor central cardiovascular monitoring
for human cardiovascular system in idealized environments. Finally, the experimental human subject data will
be used in Chapter 8 to demonstrate the efficacy of the 1-sensor central cardiovascular monitoring in real
clinical applications.
Chapter 5. Two-Sensor Black-Box Method
In this chapter, we apply the theoretical development and analysis presented in Chapter 2 to the 2-sensor
central cardiovascular monitoring problem based on a black-box model of the cardiovascular wave propagation dynamics. Specifically a data compression technique using dual Laguerre basis functions will be devel-
oped, which assures identifiability and reduces estimation error by enabling compact representation of cardiovascular wave propagation dynamics. The input de-convolution filter design algorithm presented in Chapter 2 will be tailored to the dual Laguerre basis functions to reconstruct the aortic flow signal from two peripheral blood pressure measurements. Determination of system order and other key parameters as well as
data length will be based on a rigorous evaluation of persistent excitation, model identifiability and asymptotic variance, without use of any direct measurement of the aortic flow signal The black-box 2-sensor central cardiovascular monitoring methodology will be evaluated for 7,000 data segments from experimental
swine subjects across diverse physiologic conditions. This analysis will demonstrate that the proposed methodology based on the dual Laguerre basis functions is significantly more reliable and valid than the prior one
that required identical Laguerre basis poles for all channels [36]. A similar analysis might be constructively
applied to a range of contemporary research involving dynamic physiologic models, e.g. [32,33,38].
5.1. Cardiovascular System Identification: Dual Laguerre Basis Functions
Consider two distinct arterial paths connected to the same aortic flow input, as shown in Fig. 5.1. Let
G, (z) and G2 (z) be stable transfer functions from the common input u(n) to the outputs, yi (n) and
y2 (n), observed at the ends of the 1st and the 2nd arterial paths, respectively The impulse response of
each transfer function can be approximated by a finite series expansion:
G
= 4(z)
bk(i),) (z), i = 1,2,
k=I
(5.1)
where IVk(i)
(4))
Ib )
are the associated series co-
= z-k,
which gives the standard finite im-
is a set of orthonormal basis functions, and
efficients of the i-th arterial path, or channel. A special case is Vk'
pulse response (FIR) of each path dynamics. Given a series description of the cardiovascular system, our objective is to identify both the arterial path dynamics (i.e. the series coefficients) and the aortic flow input fed
to them using only the peripheral blood pressure signals, yl (n) and
2(n).
Idws
BP #1; y1 (n)
u(n)
SBP
a
#2; y2(n)
r
r
Fig. 5.1. Cardiovascular system as a 2-channel orthonormal basis function system.
Assume that Gi (p)
, i= 1,2 share no common roots p*. Then substituting (5.1) into (2.3)
i)
k=1
yields:
b)2
k() k2) (n),
(n)
k=1
(5.2)
k=I
where
xk' ) (n)= V( 2)
y),
2)
(n) = Vk) (z) y 2 (n).
(5.3)
This equality can be formulated into a matrix equation given the time series sequences of peripheral blood
pressure signals to form a set of over-constrained linear equations, i.e. N > L + L2 :
I2)
1
) xSQ(n-N) bL
)
x )N
(n-N) b4
,
(2)x
which can be written using a more compact notation for the matrices, Xb
2=
X2bl, or
(5.4)
[X,
(5.5)
=0.
X-21
Then the unknown series coefficients of the two impulse response functions are identified by singular value
decomposition:
[X
-X 2]=UUIV T ,
(5.6)
where the column of the unitary matrix V corresponding to the minimum singular value is taken as the estimated value of the series coefficient vector,
=[i
[
]T.
Remark 5.1: This formulation of blind system identification using an orthonormal basis functions has
distinct features. As mentioned in Chapter 2, if a rational function is used for the transfer function instead of
this series expansion or FIR, at least three output blood pressure signals are needed for identifying both denominator and numerator coefficients of the cardiovascular wave propagation dynamics. In contrast, this series expansion method needs only two blood pressure signals.[]
Of special interest and significance in this chapter is how to choose an appropriate set of basis functions
that can represent the cardiovascular channel dynamics with fewer terms. Investigating typical impulse responses of arterial path dynamics reveals a unique feature of cardiovascular system [38]: as shown in Fig. 5.2,
it consists of a fast decaying dynamics that is branch-specific and a common slowly decaying dynamics, often
referred to as the "Windkessel" response [21,36,38]. The Laguerre basis functions, which are given by (5.7), is
effective for compressing dynamic representation of systems having a predominant slow pole [31,36,37,55]:
1-a2 ITs
Vk(z)=
az
z-a-k=1,2,,
(z-a)
k-1
(5.7)
where a is called the Laguerre basis pole, which is to be set close to the slowly decaying pole of the original
system (0 < a <1), and T, is the sampling interval. Using the Laguerre basis poles a1 for G,(z) and a2 for
G2 (z), (5.3) becomes:
a-
O
A
U
I
Additional Response by Fastly Decaying Dynamics
- Branch-specific
.
ýesponse Dominated by Slowly Decaying Dynamics
Cn
- Common to all arterial branches
E
1-
t/
I
1
2
3
4
5
6
Time [sec]
Fig. 5.2. Typical impulse response of a cardiovascular path.
)
xk(l
(n)1=
1-a-a2T, 1-a2
-a2Z
z - a2 ( -2 )
1Yl (n)
k2
(n) =
1-2al k- Y2 (n).
1-al ,1-)
.( I-alz
(5.8)
As we will demonstrate, the number of terms needed for approximating the original system depends on
the choice of the Laguerre basis pole. An earlier attempt by the author's group required that the same
Laguerre basis pole must be used for both path dynamics [36-38]. Although the use of the Laguerre basis
functions was motivated by the slowly decaying common dynamics of the cardiovascular system, the estimated values of the Laguerre basis poles for different arterial paths are in general different from each other,
since the Laguerre basis poles are determined in such a way that they can reproduce the gross behavior of the
associated arterial paths, including the effects of both common and branch-specific dynamics. Motivated by
this physical intuition, the obligatory use of the same Laguerre basis pole is removed in this thesis, which will
allow us to further reduce the number of terms for both paths' dynamics.
5.2. Aortic Flow Signal Reconstruction
Once the 2-channel cardiovascular wave propagation dynamics is identified, the de-convolution filter de68
sign algorithm developed in Chapter 2 can be tailored to the Laguerre basis functions as follows to recon-
struct the aortic flow signal
Corollary 5.1 (De-Convolution Filter Design Algorithm for Multi-Channel Laguerre Basis Function Sysml4: An unknown input sequence u (n) of a multi-channel Laguerre basis function system can be reconstructed from observed output sequences y, (n) and y2 (n) by using the identified Laguerre series coeffi-
cients 6and the Laguerre basis poles a, and a2 (a, # a2 in general):
u(n)= N,(z)
z
(z-al)yl (n)+ N(_(z)
N2
t-y2 (n),
(z-a2
a,f1
-(Z
(5.9)
where N,(z) and N2 (z) are polynomials of order L, and L,-1, respectively that satisfythe following:
A,(z)N, (z)+ A2(z)
(z)= (z-a,-' (z-a2),
(5.10)
where N2 (0)=1, and
b)
A,(z)=
(1-aiz)k (za,)L-k , i=1,2,
(1-a
(5.11)
k=1
if a1, a2 and 6 satisfy
k=1
bl (- 1 )4-Ik0,
bk(-a )k-1
(5.12)
0,
k=1
and At (z) and A2 (z) are coprime (see Remark 5.3).
Proof: From (5.1) and (5.9), F, (z) t (z - a ) G,(z) is a transfer function with relative degree zero, and
the transfer functions F, (z) and G2 (z) are coprime. Therefore, from Lemma 2.3, there exist stable trans-
fer functions B,(z) and B2 (z) satisfying
F,(z)B, (z)+ G2 (z)B 2 (z)= 1 .
(5.13)
Constructing B,(z) and B2 (z)as:
B (z) = N ()
t
(z-a2) 2
(z,)=
'
N2 ()
(zIal),
(5.14)
- '
I
Then (5.13) reduces to the polynomial identity (5.10). Multiplying u(n) to both sides of (5.13) and using
y,(n)=G,(z)u(n) and y2 (n)=G2 (z)u(n) yield (5.9).
69
Since N2(0)= 1 has been given, N,(z) and N2 (z) together give (L2 +1)+(LI -1)= L +L2 unknown
coefficients. Also, since both sides of (5.13) are polynomials of order L +L2-1, (5.10) results in L, +L
2
linear equations with L,+L2 unknown coefficients, Aq = y (see Fig. 5.3), where
A, (z)= Z bl)(1-az)j - (z-a,)•1J-
ca')zj =ao•+l)+al(z+.+a1)Z4-1
j=1
SA(=2
j=0
b$2) (1
z)(2zj- )
2L
2
La
j=1
(5.15)
(2)z
(2)
A(=E
a
,
2)Z+...+
(2) zL2-1
j=0
and
1+L2-1
(z-a
-a
I )-I (z
L2-1
m_
) 2
m=O
L2+1
m
a[(2) z'j
(5.16)
j=1
-
L1-1---Yo
I-
+t
//
//
/
I-
YL1+L2-1
Fig. 5.3. Matrix equation for the design of Laguerre de-convolution filter.
The matrix A should be nonsingular for the existence of q , the coefficients of the Laguerre deconvolution filter. Fig. 5.3 suggests that A should satisfy two conditions. First, it is obvious from the top
and the bottom rows of A that both a,') and a,(), should be nonzero, which, together with (5.11), (5.15)
70
and (5.16), yields (5.12). If a1') and a')_, are nonzero, the first and the (L2 + 1)th column vectors are linearly
independent of the remaining L, + L 2 - 2 column vectors in A. Thus, A is nonsingular if these remaining
column vectors are linearly independent. Noting that the elimination of the first and the (L2 +1)fh column
vectors as well as the top and the bottom rows from A results in the Sylvester matrix associated with the
polynomials A,(z) and A2 (z), A1 (z) and A2 (z) need be coprime (otherwise the Sylvester matrix becomes rank-deficient). QE.D.[]
The block diagram of the Laguerre de-convolution filter is shown in Fig. 5.4.
CV System
De-Convolution Filter
I
-un- 0
-u(n)-
1
I
0'
(z-a2)
2
1
I
±u(n).,
--y2(n)
I
N,(z) _
tyi(n)
I
N2 (z)
z- )1-1
.....................
.......
Fig. 5.4. Block diagram of the Laguerre de-convolution filter.
Remark 5.2: One might think of inverting either or both of the identified Laguerre series expansions to
reconstruct the aortic blood flow signal. However, this inversion often ends up with instability due to the
non-minimum phase zeros in the arterial path transfer functions, which are often caused by the pulse transit
time associated with the central-to-peripheral transfer of blood pressure and flow waves. An earlier attempt
by the author's group [36] developed a Laguerre de-convolution filtering algorithm to stably reconstruct the
common input signal, but its application was limited to the situation where the Laguerre basis poles of the
two distinct arterial paths are identical. It was a significant limitation since the Laguerre basis poles for differ71
ent arterial paths are typically different. [7
Remark 5.3: The coprime condition can be checked by the following method. Let A(i), i= 1,2 and
Lk-1
j = 1,2,. .Li -1 be the roots of the polynomial equation
bki)
k=I
form z(i)= {z(•)j= 1,2,...Li -
1
(i)1=0. Compute zi) = +
I
and
A +a.
for i =1,2. Then A (z) and A2 (z) are coprime if z( 1) r Z(2)==0.-
5.3. Validity and Quality Assurance
The three analytic measures presented in Chapter 2, i.e. persistent excitation, model identifiability and
asymptotic variance, can be applied to dual Laguerre basis function systems as follows.
Consider (5.2) to analyze the persistent excitation and model identifiability Assuming b(2) • 0, let us
= b(i)/b(2)
0')
and rewrite (5.2) as:
scale the Laguerre series coefficients as
xf') (n)=-
(2)x(I) (n)+
0
1
)x 2) (n)= 0 T(n),
(5.17)
k=1
k=2
where
b(
= [2(2)..b(2)
(.l)
and
-(n)=[-x ) (n)-- x ) (n)
x 2) (n)... (2) (n)T .
(5.18)
Note that given the time series sequences of peripheral blood pressure signals, the equality (5.17) can be formulated into a set of over-constrained linear equations, i.e. N > L + L 2 -1:
1)
X
xI
x (n)
(n)
=
I
=
x')
(n - N)
0 = X0,
i
T
(5.19)
(n - N)
which is equivalent to (2.51). Therefore, the persistent excitation condition is given by the positive definiteness of xTx. Once the persistent excitation condition is met, the model identifiability issue becomes trivial:
the model structure (5.17), which can be viewed as a moving-average model, is always identifiable.
72
Remark 5.4: The usefulness of the above persistent excitation condition is that it can be evaluated using
the time series sequences of the peripheral blood pressure signals alone. Unlike the persistent excitation conditions for blind system identification in the previous literature e.g. [38,41,42], the above persistent excitation
condition does not include the input, ie. the aortic flow, which is inaccessible. []
Remark 5.5: When an FIR model is used for each channel of cardiovascular wave propagation dynamics,
a large number of coefficients must be identified from the observed output signals [38]. This increases the
dimension of the regressor vector i(n) and makes the persistent excitation condition difficult to satisfy
Furthermore, as we will demonstrate, using different Laguerre basis poles, a, and a2 , for the two distinct
channels, allows us to further reduce the dimensionality [31], compared to the single basis pole model [36].
1
Remark 5.6: As long as the Laguerre series expansion accurately represents the original system, the observed signals yl (n) and Y2 (n) and their transformed (filtered) signals x1)(n) and (2)(n) in (5.4) con-
tain the same information. Although the persistent excitation condition isgiven interms of x1) (n)and
x(2) (n)in(5.18), the "richness" of the signals remains the same. The transformed signals are acompressed
representation of the original observed signals. ]
Now consider (5.2) again for asymptotic variance analysis. The empirical measurement error, c(n,i), is
given by
1)4 2)(n),
b=(2)x(1) (n) -
(n,b)
k=l
(5.20)
k=1
whose sensitivityto the Laguerre series coefficients are given by:
v(n)=
=[...x)(n).....
2)(
T
(5.21)
which can be substituted into (2.59) and (2.60) in order to assess the asymptotic variance of the identified
Laguerre series coefficients as well as the resulting cardiovascular wave propagation dynamics.
As we will demonstrate, persistent excitation and asymptotic variance will be extensively utilized to de73
termine the system order and the key parameters, i.e. the Laguerre basis poles.
5.4. Results and Discussion
From the experimental data obtained from the 10 swine subjects (see Chapter 4 for details), we obtained totally 7,000 segments of data, each having approximately 2,000 samples of peripheral blood pressure
and aortic flow signals. The blind system identification and the input de-convolution algorithms were applied
to these data, following the procedure shown in Fig. 5.5. First, initial estimates of the orders of the Laguerre
series expansions and the Laguerre basis poles of the two arterial paths were provided, based upon which the
peripheral blood pressure signals were Laguerre-filtered to generate the intermediate signals x() (n) in (5.4).
Then the matrix [X, -X 2 ] in (5.5) was formed to identify the Laguerre series coefficients, 6. Using this 6
the polynomials A1 (z) and A2 (z) in (5.11) were calculated, which were in turn used to solve the polynomial
identity (5.10) to design the Laguerre de-convolution filter (5.9). The aortic flow signal was reconstructed by
filtering the peripheral blood pressure signals using this de-convolution filter. The performance of the cardiovascular system identification was assessed by comparing the observed outputs to the estimated ones:
2
yi(n)-Gi z,ai,b)t2(n,ai,6)
:=
IlSYi (((5.22)
)ll
(5.22)
Fig. 5.5. Laguerre-function-based cardiovascular system identification and input de-convolution procedure.
The procedure described above isiterated to optimize the metric (5.22). Note that, since the true input signal
is not available in the blind system identification, the reconstructed input U(n) derived from the deconvolution was used for creating the estimated outputs in (5.22).
Remark 5.7: If the Laguerre basis poles a, and a2 in (5.8) are unknown, the Laguerre series becomes
an ARMA model, which requires at least three distinct measurements for identification [38]. In order to avoid
this difficulty the solution procedure first assumes the Laguerre basis pole values and solves (5.4).[]
5.4.1. Cardiovascular System Identification and Aortic Signal De-Convolution
Fig. 5.6 shows a typical result of the blind cardiovascular system identification and aortic flow signal deconvolution using dual Laguerre basis functions. The system order was kept low. L =6, L, = L2 = 3. The left
two plots are the peripheral blood pressure signals used for identification, and the measured versus reconstructed aortic flow signals are shown on the right. Note that, although the system order was kept low, the
reconstructed waveform of the aortic flow accurately reproduced the true aortic flow
The identified transfer functions differ significantly depending on the physiologic conditions of each
swine subject. Fig. 5.7 exemplifies how much variation we observed in the aortic-to-radial transfer functions
even for a single swine subject. It is difficult to average these responses and replace all the diverse transfer
functions by a single transfer function. Our methodology can identify each of these diverse transfer functions.
5.4.2. Quality Assurance
For each data segment, the richness of the data was evaluated by examining the persistent excitation
condition, which guarantees the identifiability of the Laguerre series model with orders 4 and 4. Furthermore, to assess the level of confidence on the identified cardiovascular system dynamics, the asymptotic
variance of the Laguerre series coefficients was evaluated by using (2.59) and (2.60) as well as (5.20) and
(5.21). This whole procedure was repeated for different values of system orders 4 and L, as well as dual
75
Laguerre basis poles a, and a2 . In particular, the proposed method using dual Laguerre basis functions,
a, # a2 , was compared to the single basis pole method [36], a, = a2 . To objectively compare the asymptotic
variance of the Laguerre coefficients 6, (single-pole) and b1 d (dual-pole) identified with and without the
constraint a, = a2 in the absence of any reference scale, fi, and ýd were scaled in such a way that the resulting DC gains of the arterial path dynamics become identical, which, noting that the DC gain of a discrete-
time transfer function G(z) is simply given by G(1), means that i, and 1d were appropriately scaled to
,. and
6d
in order to meet the following equality.
S
=
a= a2
where i) and 0
(5.23)
,d1i)
k=1
aa
2
are the elements of 6, and
d.
These 6i and
6d
associated with the 7,000 seg-
ments of peripheral blood pressure signals were applied to asymptotic variance analysis.
Examination of the persistent excitation condition for the 7,000 segments of peripheral blood pressure
data showed that the persistent excitation condition was met for most data segments when the total number
of system order L = L, + L, was less than 12. For L = 6, L,
= L2
= 3, the persistent excitation condition was
satisfied for all the 7,000 data segments. This reveals a few important points:
1. The observed peripheral blood pressure data contained information rich enough to identify no more
than 12 parameters.
2. Occasionally some data segments were found to be rich enough to satisfy the persistent excitation
condition for high system orders. However, to assure that the cardiovascular wave propagation dynamics is identifiable for all the swine subjects under diverse physiologic conditions, the total system
order should be kept on a conservative side, i.e. 6 or lower, and this needs an effective representation of the cardiovascular system.
Direct BP Measurements
True & Recovered Aortic Flows
E 15
E
I_____-L-_-,_~_l___
1
E
0
aCL
Mr
•0 -5
2 <0
I--
5186
5188
Time [sec]
ill
5190
5186
5188
Time [sec]
5190
5186
5188
Time [sec]
5190
120
15
I
E 100
10
-
80
o
E
60
U-
40
AO
5
0
0
5186
5188
Time [sec]
eC
5190
-5
Fig. 5.6. Peripheral blood pressures and true versus reconstructed aortic flow signals. System order L = 3,
L2 = 3; Laguerre basis poles: a, = 0.79, a2 = 0.94; Normalized squared error: J = 0.0982.
0nn
uuu
I
I
500
-E--- -
400
- ---------
-44--
a,
I
- HR=312.7 [bpm], BP=84.1 [mmHg], CO=5.2 [Ipm]
-*--
HR=129.1
HR=164.8
HR=114.6
HR=106.6
[mmHg],
[mmHg],
[mmHg],
[mmHg],
BP=56.7
BP=41.0
BP=101.
BP=100.
CO=4.4
CO=4.6
CO=2.9
CO=3.6
[Ipm]
[Ipm]
[Ipm]
[Ipm]
-
HR=105.8 [bpm], BP=72.4 [mmHg], CO=3.6 [Ipm]
HR=104.7 [bpm], BP=62.2 [mmHg], CO=3.5 [ipm]
-
S-
[bpm],
[bpm],
[bpm],
[bpm],
-
-L-
-
CL
E
-----
---------
100
l---------r--------7----------
w V
E
I
I
II
_Inn
0
0.05
0.1
0.15
0.2
0.25
Time [sec]
Fig. 5.7. Impulse responses of identified aortic-to-radial transfer functions under diverse physiologic conditions.
The results of asymptotic variance analysis give more insights into accuracy and reliability of the cardiovascular system identification. First, Table 5.1 summarizes the asymptotic variances of the Laguerre series
coefficients for dual-pole and single-pole cardiovascular system models, averaged over the 7,000 segments of
data. The results are also shown in Fig. 5.8. The asymptotic variances for the data length of 400, 800 and
2,000 show that they decrease approximately in proportion to the size of data points N, as predicted by the
analysis. Hence, the confidence of the parameter estimation can be improved by increasing the data length.
Table 5.1 also shows comparisons between the proposed model with dual Laguerre basis functions,
a1 • a2 , and a model with single Laguerre basis pole, a, = a2 , which suggests that the latter does not work
well for L = 6 (see also Fig. 5.8). The single-pole model needs more terms in the Laguerre series expansion,
since constraining the Lguerre basis pole to the same value creates more mismatches with the individual
channel dynamics However, this higher system order incurs poor asymptotic variance, as shown in Table 5.2.
Table 5.1. Asymptotic variance of Laguerre series coefficients (LI = L2 = 3).
a1 = a2
a1 # a2
N=400
N=800
N=2000
N=2000
7.392
5.112
3.732
6.172
7.782
5.652
4.042
5.812
g(')
4.352
3.132
2.292
3.642
1(2)
10.742
5.162
2.732
6.272
522)
14.952
5.972
2.702
7.322
/•3(2)
9.562
4.042
2.112
5.002
gl')
I
I
2
b(1,d
)
--
- - - - - - - - - - - - - - - - - - - - - - - - - - -
b(2 )
Sb
--------------------------
------------- ----------------
(2)
3,d
(
b l)
1,d
Sb
( )
-
2,d
-
b (1 )
3,d
-
(2
b )
-
b(2)
-
)
b(1
2,s
-
1
b (3,s
)
2,s
-- -
--------
----
3,s
-----------F
i ,s
----------- ----------IL-------------~_-- ________________I
200
-
- - -
2000
400
Data Length, N
Fig. 5.8. Asymptotic variance of Laguerre series coefficients for single-pole and dual-pole cardiovascular system models with respect to data length (L1 = L2 = 3).
--------------
L
-------------
- -----
- -
-
----
0--
- -
---
--
|
.....
2-Pole, Upper Limb
-
T
2-Pole, Lower Limb
1-Pole, Upper Limb
---....--------------S--
-- -
1-Pole, Lower Limb
-------------------- L-----------------------------T-----,------f---------'----------- r---------r--------------
-2
10
200
------
I
. ---.
.
..---
....
.
I
800
Data Length, N
2000
Fig. 5.9. Percentage asymptotic variance of DC gains with respect to data length (L, = L2 = 3).
We also investigated how the asymptotic variance analysis can be used for the trade-off between accu-
racy and reliability in cardiovascular system identification. In particular, two different system orders (6 versus
10) and two different model structures (single Laguerre basis function versus dual Laguerre basis function)
were considered in applying the cardiovascular system identification and aortic flow signal de-convolution to
the 7,000 segments of data. In these comparisons, N =800 was used. The resulting empirical measurement
error variance ZN (i), the magnitude of the inverse sensitivity matrix (which is measured by its trace norm)
SN, (6) , and the resultant asymptotic variance given by (2.59) in identifying the individual cardiovascular
path dynamics, averaged over the 7,000 segments of data, are summarized in Table 5.2. Specifically it lists the
percentage asymptotic variances of the DC gain of the 1st and 2nd arterial paths normalized with its own DC
gain as a representative of the asymptotic variance (see also Fig. 5.9). The DC gain of the cardiovascular wave
propagation dynamics G,(1) can be interpreted as the mean blood pressure for a given mean aortic flow, and
its variance includes the aggregate effects of all the variances in estimating the Laguerre series coefficients.
First, the variance of empirical measurement error, N(6), and the magnitude of the inverse sensitivity
matrix for estimating cardiovascular path dynamics were computed for different system orders, L = 6 and
L = 10, respectively As the system order increases, the empirical measurement error decreases. This is be-
cause more parameters can be used to fit the data as the system order increases. However, the overall asymptotic variance increases as the system order increases. The magnitude of the inverse parameter sensitivity matrix SN (i)
increases significantly for L = 10, indicating that some Laguerre series coefficients have low
sensitivities. As a result, the estimates of these series coefficients become unreliable. For N =800, which corresponds to 6.4 seconds of data, the asymptotic variance of the dual-pole model with L =6 decreases to just
a few percent for both arterial paths. On the other hand, the variance is significantly larger for the single-pole
model with L = 10, supporting again that allowing different Laguerre basis poles to different arterial paths
can deliver tremendous benefit in improving the confidence of the cardiovascular system identification. In
summary the persistent excitation and asymptotic variance analyses provide useful insights and design guidelines as to data richness, data length, system order, and model efficiency which allow us to guarantee the accuracy and reliability of identified cardiovascular wave propagation dynamics.
Table 5.2. Percentage asymptotic variance of DC gains (N= 800).
az a2
a,1
a2
L = L2 =3
L =L2 =5
L, = L2 = 3
L, =L2 =5
FN())
57.3
31.7
113
93.3
iSN(0)
0.52
1.10
1.31
3.88
AG1 (1)/G, (1)
5.14%
15.2%
30.5%
188%
AG2 (1)/G
7.93%
28.9%
43.2%
424%
2
(1)
5.5. Summary
In this chapter, the blind system identification and input signal reconstruction algorithms presented in
Chapter 2 were applied to 2-sensor central cardiovascular monitoring based on a black-box model structure.
In particular, an effective data compression technique based on dual Laguerre basis functions was presented,
which allows us to deliver compact and high-fidelity representation of the cardiovascular wave propagation
dynamics. This chapter also described how the analytic measures introduced in Chapter 2 can be used to determine the system order and key parameters as well as to evaluate the richness of the signals and quantify the
parameter sensitivity and estimation error variance. Overall, the methodology presented in this chapter illustrates a systematic way of identifying cardiovascular wave propagation dynamics based on quantitative reliability measures, which may be valuable in many physiologic applications of system identification.
Chapter 6. Two-Sensor IIR Method
In this chapter, we apply the theoretical development and analysis presented in Chapter 2 to the 2-sensor
central cardiovascular monitoring problem based on a physics-based gray-box model of the cardiovascular
wave propagation dynamics. Specifically the "asymmetric T-tube" model [44-47], which is an IIR representation describing the cardiovascular wave propagation dynamics, will be analyzed and explored for 2-sensor
central cardiovascular monitoring methodology in this chapter, based on the compromise between the ability
of a model to reproduce the key features of the cardiovascular system and its simplicity to guarantee the
mathematical tractability Besides, the validity and quality assurance analyses will be presented where persistent
excitation, model identifiability and asymptotic variance will be analyzed to quantify the validity accuracy and
reliability of the methodology without employing direct measurement of the aortic blood pressure and flow
signals. The gray-box 2-sensor central cardiovascular monitoring methodology will be evaluated for 83 data
segments from experimental swine subjects, which will illustrate how the cardiovascular wave propagation
dynamics can be accurately identified, and the aortic blood pressure and flow signals can be reliably reconstructed from two distinct peripheral blood pressure measurements across diverse physiologic conditions.
6.1. IIR Cardiovascular Wave Propagation Dynamics for Swine Subject
The theoretical development, in particular the blind identifiability condition and the blind identification
algorithm for a class of 2-channel IIR systems developed in Chapter 2, is applicable to a class of cardiovascular system models. The "asymmetric T-tube" model [44-47], which satisfies Theorem 2.1, the blind identifiability condition for a class of 2-channel IIR wave propagation systems, is explored as an exemplary case
study in this chapter. It is noted, however, that the theoretical development in Chapter 2 can be easily extended to more complex representations of the cardiovascular system, possibly with additional cardiovascular
signal measurements as well as increased computational cost. Especially, Chapter 7 will demonstrate the de82
velopment and analysis of a more complicated physics-based gray-box representation to describe and identify
human cardiovascular wave propagation dynamics.
6.1.1. Cardiovascular System Modeling: Asymmetric T-Tube Model
The "asymmetric T-tube" model [44-47] represents the dynamics of the cardiovascular system by a parallel connection of two distinct transmission line channels with the associated terminal load impedances, as
shown in Fig. 6.1. The transmission lines describe the proximal vessels, whereas the terminal load impedances
represent the resultant effect of the distal circulation, ie. the small extremity vessels. In Fig. 6.1, Pa (n),
1 (n), P2
(n) and Qa(n), Q(n), Q2 (n) are the
blood pressure and flow signals at the aortic, upper-limb
(e.g. brachial or radial) and lower-limb (e.g. femoral) locations. Note that the subscripts 1 and 2 are used to
designate the upper-limb and lower-limb quantities. The parameters n1 and n2 are the pulse transit times
[56] in terms of the number of samples associated with the blood pressure and flow wave propagation from
aortic to peripheral locations, Zci and zc2 are the characteristic impedances, C1 and C2 are the terminal
compliances, R, and R2 are the terminal resistances, and R01 and R02 are the high-frequency matching
resistances [44-47].
Assuming constant vessel compliance (ie. elasticity) and inertance (i.e. the blood density), the blood
pressure and flow wave propagation in the cardiovascular system can be described by the transmission line
equations (6.1), where x and t are the spatial (along the length of vessel, measured from the terminal location) and the temporal coordinates, and C0')and L4) are the compliance and the intertance per unit length
of vessel i, i =1,2 [44-47,49,50]:
aPi(x,t)
ax
aQ, (x,t)
ax
t)
L) aQ,(x,
at
c()
ai (x,t)
at
which can be solved to yield (6.2) [49,50], where nx - F
,LsOC(
83
x
is the pulse transit times associated with
the blood pressure and flow wave propagation (measured from the terminal location), 5P and Qj are the
incident components of the blood pressure and flow waves [21,44-47,49,50,571 F, isthe sampling frequency
and Fi (z) is the reflection coefficient [21,44-47,49,50,57] of vessel i, i =1,2:
)• P[ePi (z, nx)A
oc:X+Fi(z)ei4z
= P+[z-" +Fi (z)z" ]
T
x]
(6.2)
.
n
Qi(z,nx) A Q+[z-n" -r (z) z ]
Upper Limb
LJ'
Lower Limb
Fig. 6.1. Asymmetric T-tube model of a 2-channel cardiovascular system.
Substituting the modified Windkessel terminal load impedance [44-47] to (6.2), the transfer function Gi (z)
from Pa(n) to P (n)becomes:
N,(z,O)
Gi (z,z) Di(z,
where OA {n,n 2 ,0},
)
'+'+[(ai +bi)/F_1-] zn3
z"
+ +(alF-l1)z2 n,+b,
z2n"
1F
O {al,a 2,b,b
2
}, and
(6.3)
2Rot + R,
R,
.
2RoiCi (Roi + Ri )"
2RiCi (Roi + R i )'
(6.4)
Remark 6.1: In addition to the aortic blood pressure signal, it is often of interest to reconstruct the aortic blood flow signal [4-10,31,36-38]. The asymmetric T-tube model can be exploited for this purpose as follows. The parallel arrangement of the transmission lines in the asymmetric T-tube model suggests that the
root impedance, Z a (z,0)
P (z) , at the aorta
ga (z)
is given by Za (z,0)= Z,(z,0)//Z 2 (z,),
where the root
impedance of vessel i, Zi (z,0) for i= 1,2 are obtained from (6.2):
Si(z,nx)
Qi (Z n )
(6.5)
=.+ 1+Fi(z,0)z 2ni ]/[1-i (z,O)z-2n
with a constraint Z
P - RAiR
Q,+
Ri +RA
] AZci [i+
r'i(z,O)z2ni
i]/[a-r
(z,0)z -2n;
i
due to the zero wave reflection condition in the cardiovascular system
at infinite frequency [44-47]. Then it can be shown that Za (z, e) becomes:
Za (z,)
A
ZZ 2D (,O)D 2 (z,)
ZCD)• (z,O)D 2 (z,
0)+ Zc2b1 (z,O)D 2 (z,O)
2n
where D5(z,O) A z 2n+1 +(al/F
s -1)z i -bil/F,
(6.6)
i =1,2. The aforementioned functional relationship among
the aortic blood flow signal, the aortic blood pressure signal and the peripheral blood pressure signals are
summarized in Fig. 6.2. As we will demonstrate, za (z,O) can be determined up to scale once the 2-channel
wave propagation system from u(n) to yl (n) and y2 (n) in Fig. 6.2 is characterized by blind identification. Then the aortic blood flow signal can be reconstructed byinverse-filtering u(n) using Za (z,O).]
6.1.2. Identifiability Analysis
It is easy to prove that Theorem 2.1, the blind identifiability condition for 2-channel wave propagation
systems, can be satisfied for the asymmetric T-tube model (6.3) of cardiovascular wave propagation dynamics.
First, applying (6.3) to (2.4) and neglecting the pure time delays z"
identifiability analysis) yields
(which does not influence the blind
(6.7a)
PI (z) D2 (z)NJ (z)= {z2n+1 + (a2 /Fs 1)z2n2 +b2 Fs }{z+[(al + b)/Fs -1]},
and
P2 (z)j DI (z)N
v(n)
2
(z)={z2n+1+(al/F s -1)z2n' +b/F }{z+[(a 2 +b2)/F
...................
Impedance
Upper Limb
u(...................................
)
G (z )
.Z.(z)
.
(6.7b)
y (n )
Lower Limb
STEP 2: Impedance Relationship
ft
-1]},
STEP 1: Blind System Identification
Gi(z), G2(z)
4
1
Fig. 6.2. Block diagram of asymmetric T-tube cardiovascular wave propagation dynamics.
which shows that D, (z) has a type-II [2n -1,oo] separation at 0, and D2 (z) has a type-II [2n 2 - ,c ]
separation at 0, respectively Therefore, we have - = 2ni -1,
wi = 0 as well as mi =1 for i =1,2. Then
according to the first blind identifiability condition in Theorem 2.1, we need to satisfy vi +wi = 2ni -1 > 1 for
i = 1,2 , or equivalently
n _1, i=1,2.
(6.8)
To satisfy (6.8), for instance, both the aortic-to-radial and the aortic-to-femoral pulse transit times should be
longer than 10ms if a sampling frequency of 100Hz is used for data recording. It will be demonstrated later
in this chapter that (6.8) is indeed met for all the data segments used in this chapter.
Remark 6.2: It is also noted that the cardiovascular wave propagation dynamics (6.3) indicates that both
N, (z) and N 2 (z), as well as D1 (z) and D2 (z), are monic polynomials, implying that the leading coefficients of both p, and P2 in (2.5) are unity which can be exploited to identify the gains of (6.3) by
=
or p =
(2)
(2)
P2n,+n2+2
(1)
, where j is the unit vector satisfying (2.5).41
P2n2 +n1+2
6.1.3. Implementation Issues
From the experimental data obtained from the swine subject, totally 83 segments of data, each having
2,000 samples of aortic blood pressure and flow signals, as well as radial and femoral blood pressure signals,
were collected. In order to apply the technical developments presented in Chapter 2 to these data, a few implementation issues specific to the asymmetric T-tube model had to be taken care of:
1. In the absence of aortic measurements, the pulse transit times n1 and n2 , which determine the orders of (6.3) are unknown prior to identifying the cardiovascular wave propagation dynamics (see
Remark 6.3). In this chapter, we iteratively applied the 2-channel blind IIR system identification algorithm to (6.3) and optimized the solution over a range of physiologically relevant values of n,,
with n2 restricted to n2 = nI +An. This issue will be discussed in further detail later in this chapter.
2.
By virtue of the physical implications of the coefficients in the asymmetric T-tube model, O parameterizing (6.3) can be constrained as follows [44-47]:
O E D = ({ n,
1 > 0,ai > 0,bi > 0,at > bi,i =1,2),
(6.9)
which, together with the use of An mentioned above, results in the constrained least-squares formulation (6.10):
O=argmin min JG['(z,0)yl(n)-G2'(z,0)y 2 (n
nl DeD L0eDS12o
(6.10)
3. It is evident from (6.4) that the asymmetric T-tube model cannot be uniquely characterized by o,
becasue the asymmetric T-tube model has eight unknowns (ni, Ci , &R and Rot for i = 1,2), while
0 yields only six coefficients pertaining to Gi(z,O), i = 1,2 in (6.3). Obviously this has no influence in identifying the 2-channel cardiovascular wave propagation dynamics (6.3) and reconstructing
the aortic blood pressure signal However, noting from (6.6) that Z. (z,0) cannot be determined
87
completely from
, additional physical information need to be augmented to
. The incompe-
tence to determine the scale ie. the gain of Za (z,O) is inevitable in the absence of any blood flow
measurements; it is an intrinsic problem of the blind system identification methodology However,
the shape of the frequency response of Za (z,0) can be determined by making use of the physical
knowledge that the denominator of Za (z,0) should have the Windkessel pole (the decay rate in
the basic RC circuit representation of the cardiovascular system) [21,36,38] as its root. To identify
Za (z, ), therefore, we estimated the Windkessel pole using the diastolic portion of the two pe-
ripheral blood pressure signals [36] and augmented the following constraint to o, which allows us
to determine the relative magnitudes of Ci, ~. and Roi, i=1,2:
A(
0)D
ZcD 1 (w,
2D (,0o)D 2 (,0)
2 ,0))+ Zc
(6.11)
=0,
where A2 is the Windkessel pole estimated from the peripheral blood pressure signals. Once the 2channel dynamics G, (z,0) and G2 (z,)
as well as the root impedance Za (z,0) are identified,
the aortic blood pressure signal can be reconstructed using the input signal de-convolution algorithm developed in Chapter 2. Then the aortic blood flow signal can be reconstructed by inversefiltering the aortic blood pressure signal using Za (z,o):
,(n)= Z' (z,O)i(n).
(6.12)
4. To guarantee the identifiability of the 2-channel cardiovascular wave propagation dynamics (6.3), the
richness of the peripheral blood pressure measurements was evaluated by examining the persistent
excitation condition (2.59) for all the data segments used in this chapter, where
ip(n) = [-y 1 (n+ 2n1 + 1),-y
l
(n + 2n ),-yl (n+ 1),-y
1
(n),
y2 (n+2n 2 + 2),y 2 (n + 2n2+ 1),y
2
2 (n+2n2),y 2 (n+1) (n)
T
(6.13)
Furthermore, to assess the level of confidence on the identified cardiovascular system, the asymptotic
variance of o and the resulting Gi (z, 0), i=1,2 was evaluated by (2.67) and (2.68).
Remark 6.3: The pulse transit times can be approximately determined by measuring the end-diastolic or
88
foot-to-foot interval between the aortic blood pressure or flow signal and the peripheral blood pressure signals [21].[]
Remark 6.4: In the context of central cardiovascular monitoring, the blind identification and the input
signal reconstruction algorithms are adaptive to the underlying physiologic conditions in the sense that it is
capable of identifying the cardiovascular system solely based on the peripheral blood pressure measurements
within a small time interval, without using any a priori knowledge on the cardiovascular system, e.g. a predetermined transfer function. Hence, the resulting model coefficients represent the physiologic state of the cardiovascular system associated with an individual subject under a specific physiologic condition from which
the peripheral blood pressure signals are taken. []
Remark 6.5: The usefulness of the persistent excitation condition (2.59) based on (6.13) is that it can be
evaluated using the time series sequences of the peripheral blood pressure signals alone; (6.13) does not include the input signal, i.e. the aortic blood pressure signal, which is inaccessible. [
6.2. Results and Discussion
The experimental results will be discussed in terms of the accuracy of the identified frequency responses of the 2-channel cardiovascular wave propagation dynamics, the physiologic relevance of the identified model coefficients, and the quality assurance.
6.2.1. Accuracy of Frequency Responses
The experimental results suggest that the 2-sensor gray-box central cardiovascular monitoring methodology developed in this chapter is able to identify the cardiovascular wave propagation dynamics and reconstruct the aortic blood pressure and flow signals with fidelity and reliability over wide-ranging physiologic
conditions. Fig, 6.3 shows a representative example of the cardiovascular wave propagation dynamics identified and the aortic signals reconstructed, where the upper two plots show the true and the identified fre89
quency responses of G,(z) and G2 (z), and the lower two plots show the true and the reconstructed aortic
blood pressure and flow signals (see Remark 6.6). Using blood pressure signals from two distinct extremity
locations (ie. from the radial and the femoral arteries), the methodology could provide high-fidelity estimates
of the 2-channel cardiovascular wave propagation dynamics as well as accurate aortic blood pressure and flow
signals for all the 83 segments of data used in this chapter.
,1
-IU -
..........TF E
..........
•~
S10
01
0
-- _
,1
-IV
J, t-,TE4 +1-
J-I I- FI-I FI
- I-IT
-1FF
L II t
I-I -I" "tII + l I 7I ý~-j
FFi 5 l
F
- - -
I-- I -I I
-
Ti-i
7IT
1
Frequency [Hz]
l
-17i-
10
E
a-
J-~-
~l&.-I
- EII
u. 10
o
0I
I
I 1 11,1
710.5
709
--
--
•-I-•--
10
I
------
I
I
709.5
710
Time [sec]
i TT I
I-TTT Tq
--
20 ----
100
709
TTITITM
7T
T IT*
T TIT
1
Frequency [Hz]
E
Ir
E
- -
+-+-
041o °
-_1z r t on ==1 1 :1To II
--
--
I-Identified
,l
L0L
LLU-- -
----fHF F II I H H
TFE
---
T
Identified TT'
T:
-i
IN--,
-
I
I
709.5
710
Time [sec]
710.5
Fig. 6.3. Identified 2-cahnnel frequency responses and reconstructed aortic blood pressure and flow signals at
t=710s. Dashed and solid lines are true and identified/reconstructed quantities, respectively
Remark 6.6: Since the true frequency responses of the cardiovascular system are unknown, their nonparametric transfer function estimates G'
(jo) A
()
for i=1,2, which can be readily obtained from
ea (ijO)
the cross- and input power spectra, were used to represent the true frequency responses, where oa, (jo) is
the power spectrum of u(n) and ai((ji
tively [
) is the cross power spectrum of u(n) and yi(n), respec-
To further quantify the accuracy and performance of the methodology to identify the 2-channel cardiovascular wave propagation dynamics and reconstruct the aortic signals, an averaged transfer function, which
represents a nominal upper-limb cardiovascular wave propagation dynamics [24-30], was used as a benchmark
performance (see Remark 6.7). The methodology was compared with the averaged transfer function over the
83 experimental data segments, in terms of the aortic blood pressure reconstruction error, 1u (n)
-
(n) 2, as
well as the accuracy of estimating the ejection duration and the systolic blood pressure, which can be directly
extracted from the reconstructed aortic blood pressure signals [2,3,28]. Table 6.1 summarizes the results using
bias, standard deviation, and R2 values as evaluation metrics, which clearly suggests that the 2-sensor central
cardiovascular monitoring proposed in this thesis far outperforms its averaged alternative: on the average, the
aortic blood pressure reconstruction was improved by 47%; besides, the estimation of ejection duration and
systolic blood pressure was also improved, particularly in terms of the standard deviation (50% for the ejection duration and 71% for the systolic blood pressure).
This significant benefit of the 2-sensor central cardiovascular monitoring suggests that the wide-ranging
physiologic conditions of the cardiovascular system cannot be described by a single predetermined transfer
function, which is widely used in clinical practice [24-30]. Indeed, Fig. 6.4 shows that the identified cardiovascular wave propagation dynamics differ significantly depending on the underlying physiologic condition of
the swine subject; it is extremely difficult to average out these diverse frequency responses and replace all the
diverse cardiovascular wave propagation dynamics by a single, fixed transfer function. The limited accuracy of
the averaged transfer function approach has been rigorously investigated [27-38]. Indeed, it is obvious from
Fig. 6.5 that the accuracy of the averaged transfer function is deteriorated significantly after t-=500s, where the
swine subject starts to experience transient, widely-varying physiologic conditions. The methodology proposed in this thesis allows for identifying each of these diverse cardiovascular wave propagation dynamics.
Table 6.1. Feature estimation statistics: blind and averaged approaches
Blind Approach
Averaged Approach
Improvement
Mean 47%
Aortic Blood Pressure
2.8 +/- 0.8mmHg
5.3 +/- 2.7mmHg
RMSE
(R2 = 0.96)
(R2 = 0.87)
R2 10%
STD 70%
Ejection Duration
0 +/- 0.012s
0 +/- 0.021s
(0.21 +/- 0.07s)
(R2 = 0.91)
(R2 = 0.76)
Systolic Blood Pressure
2.3 +/- 2.4mmHg
6.3 +/- 7.9mmHg
(124 +/- 76mmHg)
(R2 = 0.99)
(R2 = 0.93)
R2 20%
STD 43%
Mean 63%
R2 6%
STD 72%
4- -- I- - 4 - -4 - 44--4-1 4- t
I- -1 -- - 1-1-1---
------
,- I •, ,••-,•-
I
I
----- - -
F7
-1-I
.-4--I---I4-,
I -i-I
I -1I -- 4I-4-4
11
--
I-I
I
-
-I--
1I
-i"
"I
I--I"I1
I
I
I
I
I
I
I
II1 I
II I
4
- 4
-
II II
--T
I
..
4I - -i74I
4 -- 4 -
T
- --- - II-IS----I--
I
I- 4 -
-I-
rl I
I I
I I
I
II
----
I
I
I
I
I
I I
1 1 1I
I I
I
---
-- -. ..-
- -
--
I-
I
I-
I---
-1
10
Frequency [Hz]
Fig. 6.4. Magnitude frequency responses of 83 aortic-to-radial and aortic-to-femoral cardiovascular wave
propagation dynamics.
11
II
I
10
E
I
I
I
I
I
-
I
"
....
II
9
I
S8
w
c)
I
--Adaptive Transfer Function
-- 5E-- Generalized Transfer Function'-
I
S-F ,T
7
---------
c--
~iz---I
I
----
c------
---
.
~---1e---
SI---
I
E
5
m
4
.2
0
<
3
1
200
i-
300
. . .
400
-
500
-
600
700
Time [sec]
I
800
I
900
1000
Fig. 6.5. Aortic blood pressure reconstruction errors for blind and averaged identification approaches.
Remark 6.7: The nominal cardiovascular wave propagation dynamics used in this chapter was obtained
by averaging the 20 aortic-to-radial frequency responses, which were identified using the aortic and the radial
blood pressure signals for the first 20 segments of the experimental data (which correspond to nominal
physiologic conditions, i.e. t <300s in Fig. 4.1).L]
6.2.2. Physiologic Relevance of Model Coefficients
The preceding results established the fidelity of the frequency responses identified from the proposed 2sensor central cardiovascular monitoring methodology It was then necessary to assess the physiologic relevance of the resulting asymmetric T-tube model coefficients thus obtained. To this end, the coefficients Ci ,
Ri and Roi for i = 1,2 were first normalized using the following relationship between the characteristic im-
pedance and the pulse transit times for blood pressure and flow wave propagation [21,49,501 where p is the
blood density and Li is the length of vessel i:
Zci
R i =pF L', i=1,2.
(6.14)
ni
Roi +Ri
Although a rigorous validation was not performed, the findings which are in accordance with our a priori expectations gave evidence that the model coefficients indeed represent important cardiovascular features: as
shown in Fig. 6.6, n, and n2 , as well as C1 and C2 were inversely proportional to mean blood pressure,
while Rol and R02 were proportional to it. In particular, Fig. 6.7 and Fig. 6.8 compare true versus identified
values of n1 associated with 5 swine subjects used in this chapter. The true values of n1 were obtained by
measuring the end-diastolic intervals of the aortic blood flow signal and the radial blood pressure signal. The
results clearlysuggests that the values of n, are physiologicallycorrect.
Remark 6.8: Since the exact values of Li , i = 1,2 are not available, this paper used Li = L2 = 1 for normalization purposes. 1]
---------- ---------
150
EI-
E 100
E 100
---------
#----4-
k
+
II
+
: --- - ----
--
L
a
a.
50
50
I
0
Th
0.05
&Tb [Sec]
150
---WI
I"
E 100
---------- ----------
150
---
S
----
I
0.1
0
5
10
RO & Rb
150
--------
---------- ---------
I
----
++
x x+
I
100
----
+I
E
a.
±1
S50
--
--
----
a 50
0
2
4
Ch & Cb
6
8
0
5
10
Rh & Rb
Fig. 6.6. Physiologic relevance of identified asymmetric T-tube model coefficients: correlation of identified
asymmetric T-tube model coefficients with mean blood pressure.
An
85
80
75
70
E 65
a. 60
55
50
45
40
100
200
300
400
500
600
700
800
900
1000
1100
Time [sec]
(a) Subject # 1
E
H
4600
4700
4800
4900
5000
5100
Time [sec]
(b) Subject # 2
5200
5300
5400
5500
1
^^A
0
Time [sec]
(c)Subject # 5
400
500
600
700
800
900 1000
Time [sec]
(d) Subject # 8
1100
1200
1300
1400
V
a)
U)
1000
1100
1200
1300
1400 1500 1600
Time [sec]
1700
1800
1900
2000
(e) Subject # 9
Fig. 6.7. True versus identified aortic-to-radial pulse transit times in transient physiologic conditions.
18
True PTT [sec]
Fig. 6.8. Physiologic relevance of pulse transit time identified from blind approach.
In fact, the pulse transit time can be accurately identified by the following reasons. First, ni, i = 1,2 are
parameterized in (6.3) in such a way that they affect the magnitude as well as the phase frequency responses
of the cardiovascular wave propagation dynamics (6.3). Second, the effect of ni on the magnitude frequency
responses of G,(z) and G2 (z) is different from the polynomial coefficients, a, and b,. Fig. 6.9 clearly
shows that increasing a, and b, results in the increase in both the location F, and the magnitude
MG
Gi (2rFG j)l of the first peak in the frequency response G,(jo), whereas increasing n, is followed
by the increase in M, but the decrease in F . Furthermore, using the peripheral blood pressure measure-
ments, the "differential" pulse transit time, defined by An
n2 - n, can be estimated as the end-diastolic or
foot-to-foot interval between the peripheral blood pressure signals (see Remark 6.9). This An plays a crucial
role in efficiently identifying (6.3) by imposing a restriction on the orders of G,(z, O) and G2 (z, O). Noting
that n1 and n2 essentially specify the effective lengths of the upper-limb and lower-limb cardiovascular
channels, a physical implication of fixing An to the measured differential pulse transit time is to constrain
the difference between the lengths of the upper-limb and lower-limb cardiovascular channels so as to facilitate the accurate determination of the system orders in (6.3).
IGi(jw)l
IGi(w)l
F
F
Nominal
IGi(aw)jl
aF
-aF
F
Increasing ai and bi
F
Increasing ni
Fig. 6.9. The distinct influences of pulse transit times and polynomial coefficients on the location and the
magnitude of the first peak of G,(jco).
Remark 6.9: Although this notion of An is not strictly true due to the complex effects of the wave re-
flections on the blood pressure signal morphologies, the rising limb of the blood pressure signal retains its
identity reasonably well in the sense that the early part of the blood pressure wave is in general little affected
by the wave reflections [21]. []
Remark 6.10: In fact, the results presented in Fig. 6.7 and Fig. 6.8 provide the initial proof-of-principle
for the feasibility of pulse transit time estimation solely based on extremity signal measurement. Due to its
clinical importance as an indirect indicator of blood pressure as well as a key parameter in aortic blood pressure reconstruction [56,58-60], there have been tremendous amount of previous effort for the estimation of
pulse transit time using a variety of methods [56-64].][
Remark 6.11: It is obvious that the pulse transit times shown in Fig. 6.7 satisfy the blind identifiability
condition (6.8). [
6.2.3. Validity and Quality Assurance
The examination of the persistent excitation condition for the 83 segments of the radial and femoral
blood pressure data showed that the persistent excitation condition was satisfied for all the 83 segments of
data. The persistent excitation analysis also revealed that the well-posedness of the cardiovascular wave
propagation dynamics identification problem (6.10), i.e. the degree of persistent excitation, is closely related
to the heart rate frequency FHR (which represents the characteristics of the excitation signal), and the fre-
quency FG
2 at which IG
2 (jco) attains its maximum (which represents the underlying physiologic condition
of the cardiovascular system): the smaller IFHR - F 2 I, the better the condition number of
a e,
as shown in
Fig. 6.10. This finding can be interpreted as follows. First, scrutinizing Gi (z), i = 1,2 suggests that the location FG and the corresponding magnitude MG of the first peak in Gi (jco), i = 1,2 are the most important features to identify because:
1. The frequency responses G (jco), i = 1,2 are insensitive to 0 at low frequencies due to the
99
unique model structure of Gi (z); in particular, G (jO) = 1 regardless of 0.
2. The high-frequency portion of Gi (jco), i = 1,2 are extremely difficult to identify due to the lack
of high-frequency contents in the blood pressure signals used for identifying the cardiovascular
wave propagation dynamics.
3. FG, and MG are the most salient feature of Gi (jco), i = 1,2 in mid-frequency range that is determined by the interaction between ai, bi and n1 , as demonstrated in Fig. 6.9.
Z
I
I
=1=
-0- -I -0I
I
o
------200
300
400
500
600
700
800
900
1000
i
I
I
I
I
I
I
IFG-F R I
-
'''
-----
-
I
200
I
300
400
I
500
600
700
Time [sec]
I
I
800
900
1000
Fig. 6.10. Persistent excitation as a function of IFHR -FG 1
2
Obviously the frequency range from which the maximal amount of information relevant to identifying the
cardiovascular wave propagation dynamics can be obtained is the neighborhood of FG . Therefore, FHR
needs to be close to FG . It also turns out that FG2 <FG, since n <n 2 , and that FHR < FG
2 in most physiologic conditions; thus, FHR < FG2 < FG . Therefore, the well-posedness of the cardiovascular wave propaga-
100
tion dynamics identification depends on IF,R - FG, rather than IF,, - FG,
, because F, is easier to reach
2
for FHR than FG . Note that once n, is well identified, so is n, by virtue of the differential pulse transit
time measurement, n, = n2 - An. In other words, the quality of identifying the cardiovascular wave propagation dynamics hinges upon how well the frequency range around FG2 is excited by the aortic blood pressure
(or, equivalently the aortic blood flow) signal. This suggests that care must be taken when we interpret the
identified cardiovascular wave propagation dynamics associated with large FR - FG, , in the sense that the
system might have been identified using poorly exciting measurements.
The results of asymptotic variance analysis give additional insights into the reliability of the cardiovascular system identification. First, Table 6.2 summarizes the results of the asymptotic variance analysis for the
data length of 250, 500, 1,000 and 2,000, which show that the asymptotic variance of 0 decreases approximately in proportion to N, as predicted by the analysis; see (2.67) and (2.68). Therefore, the reliability of
parameter estimation can be improved by increasing the amount of the data used for identifying the cardiovascular system. The results are also graphically shown in Fig. 6.11-Fig. 6.13. Table 6.2 as well as Fig. 6.14 also
shows that n2 and a1 have the smallest and the largest asymptotic variance, respectively which accords well
with our eigenstructure analysis of SN: the eigenvectors associated with the smallest and the largest eigenvalues were mostly aligned with the directions of n2 and a1 , suggesting that E(n) is the most and the least
sensitive to n2 and a1 , respectively Since those elements of 0 having large sensitivity on the empirical
measurement error are relatively easier to identify than their small-sensitivity counterparts, n2 and a1 can be
regarded as the easiest and the most difficult coefficients to identify in 0, respectively
Quantifying AN showed that its values were limited within 4% of the associated mean blood pressure
values, with the average of 2.3% (see Table 6.2), indicating that the asymmetric T-tube model is an efficient
representation of the cardiovascular system for the swine subject considered in this chapter.
101
IV
2
t:
---
S-
4------
-
-
- -----
-
-
- -
-
1
-
I
___L
101
()
0
C
--
•
_:""--,,•.
_'--
C----r[~ -~E-IZ
A
4I
--
--
8'-
I I
E
S, - - , •
__
C-r-t
1--
-
------- ---
---- [
I
.
.-.-
-..
-:
- z _-t
-- I_
-.
t :: z z
-I::-.
:: : .- : ..:::z
.
....
b2 -
8a2
•
I
> 10
0.
Z
E
Z-- I --- •••---
-- iT
--
400 -- 6
10,
- - 8--
i
7i"
÷,
100
10T
I
-
-I
-
- ----
~-
--
-----
•
.- -.T
I--
L---....
- --
....
10-2
--
--"I"
I'
400
---
I
- F
----
Il--
600
800
...
,' - --
40
I -
-
10
•2
10
2000----
-----
I---
-----
--
+---
I
-','
-
-
- - - - -T
V
Ir-----I
..
-ps---T-f
T --
1000
..
I--
--
-
r-
1"--
Ir
1200
1400
1600
1800
2000
Data Length, N
(a)Asymptotic variance of asymmetric T-tube model coefficients.
10
-1
"
..
. ..
-
---
--------
--
2
.
-- ---------r----
I------------------
r ----
---- - - - --1 - - --
-
----------
L
r-
0
-
-
0c.
0.
-I-
----------
-
-
r--
-
.e
0"
.
I
.
_
I
• ..
.
-:- -"
II
-
- :Z:
-t...-----r-
------.
I.
I. _
I
I
8bb2
"
-- 6
"
11
-
!----------
------------ -
I
8bv-
'-------------
I~~
+ .....
SI
E
E3
I
-------L
I--------
+
a
- I----I- ---
S _LIw~ici•_.
0. _
10-
--
LI
_ _-
1
IL _
-
I
I
I
S-3
r-
-
r - -- -
_---
--I
-Z- Z-
.
.....
.
-----------•
L ....
-.-- .•I,,
•-.....
.. . --I. I.. ---.
- -..-- ~--- -- -
4
N
z
S_--. L :-------. 4---•
+--- . .I.
..
10
4
.I
.
.-
-
--- I_
-
• ---
400
__
-
600
--I_
800
_ _--'•r••'" -
1000
-•
1200
:.l... _
1400
_
.
..
1600
. T .
1800
..
2000
Data Length, N
(b)Normalized asymptotic variance of asymmetric T-tube model coefficients.
Fig. 6.11. Effect of data length on asymptotic variance of asymmetric T-tube model coefficients.
102
102
10100
--
....... N=250
..........
N=500
----- N=1,000
- -
N=2,000
-
200
400
600
1000
800
....... N=250
..........
N=500
----- N=1,000
1
-
200
400
600
800
1000
---.-.- N=250
..........
N=500
N=1,000
- N=2,000
10
E.
N=2,000
10-4
200
400
600
800
1000
Time [sec]
(a)Parametric asymptotic variance: aortic-to-radial channel
100
_--
-T
-
1
- - - ---
....... N=250
.......... N=500
----- N=1,000
-
200
400
t~~__~===rII
I-E
600
800
rt==_===~=====~-l==
-
E- E
:zzz
10-
--
200
400
600
800
1000
==r==l==_~~
zZ
=I==-
-
-----.- N=250
.......... N=500
----- N=1,000
-
-4
100
200
400
600
Time [sec]
800
N=2,000
1000
- --
- - --?--
....... N=250
.......... N=500
----- N=1,000
-
-
V*-
-3
N=2,000
N=2,000
1000
(b)Parametric asymptotic variance: aortic-to-femoral channel
Fig. 6.12. Parametric asymptotic variance for 83 data segments of experimental swine subject.
103
-----
100
I
100 ---
L
- - --
- - I- -
J
--
r----;--
----
50----
L
,
-- -
---
-
J--
t-
-- ;--
----
---
rk-l--;'
0
200
300
400
500
600
700
800
900
1000
200
300
400
500
600
700
800
900
1000
10
-
5
50
" 40 - - -
L----L
--------
-
30
P20---
---
- - ---
----
--
-
-_
-J---
- ---
-
-
_----
--
-
-
-
--------
-
10
200
300
400
500
600
700
Time [sec]
800
900
1000
(a)Parametric asymptotic variance for N=1,000: aortic-to-radial channel.
15
10
----
20
--
200
- --
-
300
400
I
S
I
5---------------200
300
400
80
S40
S
--•
---
500
I
500
-------
600
104
600
F------
-
-~---
l--'- -
--
-
'
-~----+-
----------
104
--
-
700
800
900
700
800
900
--
-
1--
--
----
1000
1000
--
I-
- -- - - - - -, -
0.04
0.04
'u
N
0.02
'U
0
4
200
x
400
600
I
0.02
0 200
800 1000
10-3
II
-I---H---
4x
400
600
800 1000
10-3
~u 2 I I -- I - - ------+ --
co
.0
x
200 400
I
.ioI
0
600
800 I 1000
I
200
400 600
800 1000
x 10-3
4
2 -.200 -- 400
•
600
+-- 800---1000
2 ---- 40
"lime [sec]
200
4
*-
400 600 800 1000
Time [sec]
Fig. 6.14. Normalized parametric asymptotic variance for 83 data segments of experimental swine subject
(N=I,000).
As a practical matter, accurate estimates of
AN
and SN can be obtained even using very small N, e.g.
250. Indeed, Fig 6.15 shows that both AN and SN are highly consistent against different values of data
lengths. This implies that in the early stage of cardiovascular system identification, the amount of data needed
to achieve a desired level of reliability can be estimated by predicting
AN
and SN using small number of
data samples and evaluating the asymptotic variance using (2.67) and (2.68).
The asymptotic variance analysis also showed that the high-frequency variance of the identified asymmetric T-tube model, G,(jco) and G2 (jc), hinges upon the variance of n, and n2 . This finding is consistent with the previous results on the parametric sensitivity analysis [32,34,35,59,61], which revealed that the
asymmetric T-tube model given by (6.3) is highly sensitive to n, and n2 at high frequencies, whereas it has
zero sensitivity to all of its model coefficients at steady state (ie. zero frequency). This suggests that accurate
identification of n1 and n2 as well as accurate measurement of An is crucial in order to minimize the high105
frequency uncertainty of G,(jco) and G2 (jc). Indeed, Fig. 6.16 shows that their high-frequency variance
can be significantly improved when the variance of n, and n2 is assumed to be zero.
In summary the persistent excitation and asymptotic variance analysis provide validity and quality assurance as well as useful insights and design guidelines as to data richness, data length, and model efficiency,
which allow us to guarantee the accuracy and reliability of 2-sensor gray-box central cardiovascular monitoring methodology
6.3. Summary
In this chapter, the blind system identification and input signal reconstruction algorithms presented in
Chapter 2 were applied to 2-cahnnel central cardiovascular monitoring based on a physics-based gray-box
representation of the cardiovascular wave propagation dynamics. Using the experimental data obtained from
swine subjects, we demonstrated that high-fidelity physiologically relevant representation of cardiovascular
wave propagation dynamics can be identified, from which the aortic blood pressure and flow signals can be
reconstructed from two extremity blood pressure measurements.
In this chapter, we rigorously demonstrated the potential clinical utility of the 2-sensor central cardiovascular monitoring combined with physics-based cardiovascular system representations. For instance, many
important central cardiovascular features e.g. the ejection duration and the aortic systolic blood pressure
(which could be accessed by highly invasive surgical procedures), as well as the cardiovascular wave propagation dynamics itself, have potential clinical applicability for central cardiovascular monitoring,
In this chapter, we also provided an initial proof-of-principle for a new approach to the pulse transit
time estimation problem, which may further be explored to open up a unique opportunity to the pulse transit
time estimation problem using minimally invasive or even non-invasive signal measurements at extremity locations. Further investigation and clinical application of this new approach iswarranted.
106
I
I
I
I
....... N=250
........... N=500
!j
,
i~Am~kI
I
I
I
I
I
I
I
I
I
I
I
I
I
200
300
400
500
600
700
200
300
400
500
600
700
N=1,000
N=2,000
.-...
-..
I
I
800
900
1000
800
900
1000
Time [sec]
2
(a) Consistency of
-I.
------
-------
N=250
against different data lengths.
N
. . .------. . . . .4---. ..
-I----4
I
-- ----
1----------------.
-.
--. I- .
-.. . 4 -.
. . --.
.S-I-- - - .I
- -- ~---4---I--------4
L4
-----------
-
...........
N=500
-- -N=1
-----N ''VV7
-=2,000 /
- I-r-- -- -
- - --r
4, 4
i
E----
---- - --
I
I -- II - -
I
-
T
T-
-
L £T __L
L
-I--I L
_
I
I
I
I
I
I
I
I
I
I
200
-
a-
-
~1
---
I
I-
I
- -
I
---
"!
I--J
I
t
.
-
I
I
I
--
-
-
I
I
I
I
I
I
I
400
500
-r
r --
" __L_
_ J--
i
1-
I-
I
I-- I.
---
II
----1. .I I
- -- -
-
I
-I--4---
-
~
1-
- -I
__I--
_
I
I
I
I
I
I
600
700
-
?
--
-1
J_1
"I-J~
II
II
I
I
I
I
I
900
1000
I
800
(b) Consistency of SN against different data lengths.
N
and SN against different data lengths.
107
--
---
Time [sec]
Fig. 6.15. Consistency of
---
I--
-
-----
I
300
I
II
_I_II
- --
I
-----
r
----
I
.
-
I
I
--
--- ---
I
S
-- - - -- - -- --------
- - -
---
I
I - - - -
4---r
Z--
-4 . -. . .
Uncertain Time Delay
--
I
I
I
II
I
I
I
I
I
---
I
11111I
1 11 III
f
I
II III
I I I I111111
I I
1111
I I I I111111
1111111
II
I I Ill1
111lli
II II 1
11111
I I I I I I II
I I I I IIII
I I I I I III
I
I
I
I I I I I I II
I I 11III
I I 1 1 III
I
1-4I +4-4441I
1IIII
I
I
I 111111
11 11111
I
111111
II I I I11111
II I
I
I
I
I I
IKl.LL
111111
11111I
11111
l
I IIIi
I
I
-I I
I I
I
I
li
t
I
I
I
I
1111
111111
I
I
I 11111I
I lilii
I
I
I I1 I I I
I
I
I I I
I
I I
I I
I
I 11 IIII
I111 IIII
I I IIII
I
I
I
I
I
I
I I I1 1I
I I1111II
I I11111
I
I
I I 11 1l
I
I
I
I I I IIII
I
I
I
I
I
I
I I I 111111
I
I
I
111IIII
I
I
I
I
I
I
I
I
I
I
--
I
I IIIIII
III
II
-
I
111
II 1 II
111111
111111
I
I
IIIII
M I I
I
I
I
I
I
IIII
I 111111
I I 111
I 11111
-I 4-144-I1 I111111H
I11111
IIIi
I I
11111
I
I
I I IIIII
I I I 1 III
I
1
I
I
i llIII
I 1111111
-4-4-4-4-1-14-I-1---1-4-
111111
11111
11111
II I I III
II
L Ir
I II I
I
I 1111
1 11111
l
I
II 1111
1
II '
I
I
I
I
I III
I III
I I ll1
ll
-- I 44-1-1H4-14---.
11111i
I IIIII
I II
I
Accurate Time Delay
I
I
I
1I
I
I
I
I I1 I IIII
I 111111
I I 11 III
-44---4 I I 11111
I I I 11 l
I
IIII
II I
I
I II
I
I
-
1111
I I I
III
III
I 1111111
Frequency [Hz]
Frequency [Hz]
Fig. 6.16. Asymptotic standard deviation of G,(jw) and G2 (jCO) at t=710 s with N=1,000, using uncertain and accurate pulse transit times.
108
Chapter 7. Two-Sensor Wiener Method
In this chapter, we consider the 2-sensor human central cardiovascular monitoring problem, where we
deal with modeling and blind identification as well as aortic blood pressure signal reconstruction in human
cardiovascular system. Especially, we develop an identification-oriented Wiener model of human cardiovascular wave propagation dynamics, to which we apply the theoretical development and analysis developed in
Chapter 2. The Wiener model of human cardiovascular wave propagation dynamics will be validated and the
2-sensor central cardiovascular monitoring methodology will be evaluated for eight different human subject
models presented in Chapter 4. We will demonstrate that the methodology together with the Wiener model
of human cardiovascular wave propagation dynamics, is able to characterize the human cardiovascular system
and stably reconstruct the ascending aortic and abdominal aortic blood pressure signals.
7.1. Wiener Cardiovascular Wave Propagation Dynamics for Human Subject
As in Chapter 6, based on the compromise between the ability of a model to reproduce the important
features of the cardiovascular system and its simplicity to guarantee the mathematical tractability we used the
mechanical analogy of the transmission line theory [49,50] to describe the blood pressure and flow wave
propagation behavior in the cardiovascular system. In fact, the transmission line model has been widely used
in the study of the cardiovascular wave propagation dynamics in human upper limb, and abundant previous
research efforts support the adequacy of single-segment transmission line model to describe the behavior of
the pressure wave propagation in the aortic-to-upper limb cardiovascular channel, e.g. aortic-to-brachial and
aortic-to-radial channels [26,30,55,56].
7.1.1. Cardiovascular System Modeling: Aortic-to-Radial Channel
Consider a single-segment transmission line model for aortic-to-radial blood pressure propagation in the
109
human cardiovascular system shown in Fig. 7.1, which is very similar to Fig. 2.3 but has more details. We will
derive an identification-oriented input-output relationship ie. a transfer function (2.15) specific to blood pressure wave propagation. In Fig. 7.1, Px is the blood pressure at a location X, nx is the pulse transit time
associated with the wave propagation between x and the distal end of the cardiovascular channel, Z, and
z,, are the characteristic and the terminal load impedances, and T, is the resulting reflection coefficient defined by F,
A
z tl
c
. The subscripts 'a' and '1' denote the aorta and the distal end of the cardiovascular
Zel + Zcl
channel, respectively and the superscripts 'i' and 'r' denote the incident and reflecting components of the
blood pressure wave, respectively
Px(n)
Pa(nn)
1
I
Timi erela\
Pa'(n)
par(n)
h;
n,
ny
1
P (n)
Pi
Time Delay ni
P
Fig. 7.1. A single-segment transmission line model for aortic-to-radial blood pressure wave propagation in
human cardiovascular system.
Assuming that the compliance and the inertance of the arterial vessel are constant, and the energy loss
due to the visco-elasticity of the arterial vessel is negligible, the blood pressure wave at a location X in the
aortic-to-radial cardiovascular system can be decomposed into its incident and reflecting components:
Px (t) P' (t)+ P (t),
where t -
(7.1)
and F, is the sampling frequency It is assumed that the morphology of the incident and
reflecting blood pressure waves is not distorted but preserved while traveling back and forth in the aortic-to110
radial cardiovascular channel. Therefore, (7.1) can be rewritten in terms of the blood pressure wave at the
radial extremity
(t)1 (t)+(t)
I
as follows:
X
W(7.2)
(t +rx)+r(t-rx)=e."'sPi (t)+e-r.sPir (t)'
=
n--x. Then the transfer function G1 (s) relating Px (t) and JP (t) becomes
where rx
G,(s)
Pl(s)
f (s)+pr (s)
Px (s)
erXSPli (s)+e-rxsP
(s)
i
=
Pi (s)[1+[I (s)]
, (s)]
(s)[erxs+e-rxS
1+, (s)
+ ,()
ePxs +e-rxS
(s)
(7.3)
Substituting the modified Windkessel terminal load impedance [44-47] shown in Fig. 7.1 into (7.3), we have
(
G, (s) = e-
where a A
s+a 1 +e - 2 r
s + a + bl
2Rol + RI
wI
2R0oC
(Rol + RI)
(7.4)
s
and b1 A
Rl
, and the terminal resistance R , the terminal arterial
2RoC1 (Rol +RI)
compliance C, and the high-frequency matching resistance Rol, respectively are the parameters characterizing the modified Windkessel terminal load impedance. Therefore, with the knowledge of G,(s), the blood
pressure wave P, (t) at a location X in the aortic-to-radial cardiovascular channel can be reconstructed by
inverse-filtering the radial blood pressure measurement P,(t) using G,(s). In particular, the aortic blood
pressure wave P, (t) can be reconstructed by specifying nx = n,, where n, is the pulse transit time associated to the aorta and the radial measurement site (see Fig. 7.1).
Remark 7.1: In fact, (7.1) is the continuous-time equivalent of the discrete-time blood pressure wave
propagation dynamics (6.3). Indeed, substituting t
2nx++)z2nx /Fs
G,
Fs
Fx x -X and z
Fs
e_'=
into (7.5) yields (6.3):
+(7.5)
7.1.2. Cardiovascular System Modeling: Aortic-to-Femoral Channel
In contrast to its aortic-to-radial counterpart, the study on the cardiovascular wave propagation dynam111
ics of human lower limb, e.g. aortic-to-femoral channel, has been relatively rare, and at least to our knowledge
there is no widely-accepted identification-oriented model to describe the blood pressure and flow wave
propagation in the human lower-limb cardiovascular system. In this chapter, we first examine the relevance of
a single-segment transmission line model for the aortic-to-femoral channel in the human cardiovascular sys-
tem, by 1)identifying a single-segment transmission line model (7.5) using the aortic and femoral blood pressure signals as its input and output signals, and 2) reconstructing the aortic blood pressure signal by filtering
femoral blood pressure signal using the identified single-segment transmission line model. A typical result of
aortic blood pressure reconstruction is shown inFig. 7.2, which clearly shows that a single-segment transmission line model has limitation in effectively reproducing the wave propagation behavior of the aortic-to-
femoral channel inthe human cardiovascular system.
120
---- I
115
-
110 S-
-_
120
----True
--.......-1_ _ I
..
Reconstructed, 1-TL,P
1
-
Reconstructed, 1-TL, P2
I
I
I
I
I
110
- --
- -- r-- -----I
I
105
I
I
--
I
I
E 105
I
L
I
I
i
85
-T
I
T
I
II
I
- - - - -
I
-- ' - -- 7tl','-'-'---- ---- '--'------------
S-
'95
----------
-
980
I
---
75
L---------
I
- -- 1--I--I
----
5.5
5.6
I
I-I
5.7
I
-- -I
5.8
-- I
I
I - -I
IrII
I --T--i--- ---- ----I---- -
-+
I
/
5.9
6
6.1
Time[sec]
I
I
6.2
6.3
I
I
6.4
75
75
6.5
80
85
-
- -r -
~I
J,
~
75
80
70
I
115
7- -
I
..,L
r - 1
---------
90
95
100 105
TrueAorticBP [mmHgl
110
---
115
120
Fig. 7.2. Aortic blood pressure signals reconstructed from radial and femoral blood pressure signals of human
cardiovascular system using a single-segment transmission line model
The incompetence of a single-segment transmission line model to describe the human lower limb, ie.
the aortic-to-femoral cardiovascular channel, may arise from a variety of reasons, including:
1. The aortic-to-femoral cardiovascular channel is relatively longer compared with its aortic-to-radial
counterpart. Therefore, the effect of tapering, bifurcations and visco-elasticity may not be negligible.
112
2. Unlike the aortic-to-radial cardiovascular channel, the aortic-to-femoral cardiovascular channel involves significant leakage flow from the abdominal aorta to splanchnic organs.
Motivated by these findings, we will develop a physics-based gray-box model structure for the human
aortic-to-femoral cardiovascular wave propagation dynamics in this chapter, which consists of two distinct
transmission line segments and two terminal load impedances as well as a static nonlinear function, as shown
in Fig. 7.3. In Fig. 7.3, the transmission line segments qualitatively represent the thoracic and abdominal portions of the aorta and the femoral artery respectively and the terminal load impedances approximate the
lumped effects of the splanchnic organs and the distal extremity vessels beyond the femoral artery The role
of the static nonlinear function is to account for the remaining nonlinear effect due to tapering, viscoelasticity etc. In particular, considering that the smaller vessels exhibit more nonlinear behavior than the larger vessels, we used a Wiener model structure (instead of a Hammerstein model structure), i.e. the static
nonlinear function was added at the output of the second transmission line segment.
r
X2
.
pa
-)-
PS
-F
,-
r
IL
I
TL
#2
-rL·.I,~
I_
-Terminal
,
I
.
Impedance
I
.
Leakage to Organs
Fig. 7.3. Physics-based gray-box model of human aortic-to-femoral cardiovascular channeL
Based on the model structure shown in Fig. 7.3, a nonlinear two-segment transmission line model of the human aortic-to-femoral cardiovascular channel shown in Fig. 7.4 can be developed, where (see Appendix B for
113
the details of derivation):
SaP (s)N (s)
(s) D21
(7.6a)
21 (S)
X (S)
s+a,
G22 (s) X 22 s -
s +
X 2 ()
)
N1
(7.6b)
(7.6b)
+ b2
s +a 2 +b 2 2e -Ts
Ps (S)
2)k
[2 ()].
(7.6c)
k=1
Pa(n)
Ps(n)
X2(n)
P2(n)
Fig. 7.4. A nonlinear two-segment transmission line model of human aortic-to-femoral cardiovascular channel.
Finally, in order to apply the theoretical developments as well as the time series sequences of the radial
and femoral blood pressure signals to the 2-channel human cardiovascular system model consisting of (7.4)
and (7.6) developed in this chapter, the continuous-time dynamics (7.4) and (7.6) were converted into the following discrete-time transfer functions using the forward Euler approximation:
G,(z)=
Z
n+
+[(a
+b
+ (,
z2n,+1 +(a1/Fs -1)z2n, +
S
(7.7a)
)/Fs -1]
(7.7a)
/lFs
G2(z)G
N 22 (z)
2 1 (z)
22 (z)N
N 2 1()
D 2 1 (z) D 22 (z)
D 2 1 ()
Zn2
+[(a 22 +b 22 )lFs -1]z
Z2n22+ 1 +(a 22 /Fs
2
n
22
1) Z n22 +b22 /
(7.7bFs
where
N21(
Z2n22+2+'
N21 (z) z'fl
+[-2 + a22 +a 21 +b21 + a 2
+[1
a
2
21
+a21 +b2 1+a 2C21
+
z2n22+1
a22 (a 21 +b21
Fs,
+
b[_
22 b22 (a21 +b21 +a2C21
Fs
Fs
114
221
2n
,
(7.7c)
and
2n22+ 2
D21(z)- 2n2+
a 21 +22 +a
+ -2+
+[
+ a 22 + a2C2 1 a22 (a21 +a 2C21 lz2n2l+2n22
1
Fss
21
+
2c 2 1 ]Z2n21+2n22+1
z2n21+1
++
K
-
lFs
b 2d21 +
Z2n2
2
z2n22+
b21
b
22 21 Z2n22
+[b2 (1- d21)Fs
]
[
(7.7d)
b22(1-d21)b22(2
7.1.3. Identifiability Analysis
Plugging (7.7) into (2.11), we have
P (z)x1 (n)= D 21 (z)D22 (z)N 1 (z)x,(n)==
21 (z)N 22 (z)= D
(z)N
2 1 (z)N 22 (z)x 2 (n)=
(z)[N21(z)N
22 (z)].
P (z)2(n).
(7.8)
It is obvious from (7.7) that D, (z) has
First consider P2 (z)
DA (z)N
V = vo = 2n - I1and
= 0 , while the order of N21 (z)N 22 (z) is m = 2n22 + 3. Therefore, if the radial and
the femoral channel lengths and sensor locations are chosen to satisfy 2n
1 -1 2 2n 22 + 3, or
(7.9)
n I - n22 + 2,
then P2(z) can be decomposed into Dl (z)and Q2(z)- N21(z)N
is
also obvious
22 (z)by Theorem 2.1. It
from (7.7) that N21(z) has a [2n22-3,0] separation at 1,while the order of N22(z)is m=1. Therefore, if
the femoral sensor location is chosen to meet 2n22 -3 _1, or
115
n=22 ý 2,
(7.10)
in addition to (7.9), then b22 can be determined from n(21) = b22
Fs by Lemma 2.1. Now consider the following coefficients in Q2 (z):
q(2)
b22
Fs
F,
2+2
+(a2+ +222C2)
(7.11)
Fs
[a 22 + b22 1]+[ 2+ a22 +(a2 + b2 +a2 c21)]
q(2)
2,from
+2the which
ollowing
Fs
matrix equation can be formulated to yield a
(7.12)
and (a
from which the following matrix equation can be formulated to yield a22 and (a21 + b21 + a2C2 I
[2
a22
[1
1 I (a21
(7.13)
+b21 + a2C21
Then D22 (z) and N 22 (z) can be determined by the availability of both a22 and b22 . Finally N21(z) can
be determined by solving Q2 (z)
N 21(z)N
22
(z) with Q2 (z) and N22 (z) given. Furthermore, noting that
N , (z) can be determined once D, (z) is decomposed from P2 (z), D2 1 (z) can be determined by solving
P (z)
D2 1(z)D
22
(z)N (z) with
P (z), D22 (z) and N, (z) given. Summarizing, the 2-channel Wiener
model of blood pressure wave propagation in human cardiovascular system is identifiable by choosing the
radial and the femoral sensor locations such that (7.14) is satisfied:
nI n22 + 2 > 4.
(7.14)
Remark 7.2: More generally it can be shown that this specific 2-channel Wiener model is identifiable if
1. 2n, 2 3,
(7.15)
2. 2n22 > 3,
(7.16)
3.
(7.17)
n,
n222.
First consider P2 (z)= N 21 (z)N 22 (z)D 1 (z)= [N 21(z)D (z)]N 22 (z). Fig. 7.5 suggests that there are two possible separation locations in P2 (z). In particular,
1. A separation occurs at 1 if both n, 1.5 and n22 2 1.5 hold.
116
2. A separation occurs at 2n, + 2 if n1 > n22 > 2 holds.
3. A separation occurs at 2n22 +2 if n22 > nI 2 holds.
Note that the last two separations (ie. 2 and 3) cannot occur simultaneously Therefore, assuming that the
radial and the femoral channel lengths as well as the sensor locations are chosen such that the conditions in
(7.15)-(7.17) are satisfied, there occur two separations in P2 (z) at 1 and at either 2n
1 + 2 or 2n22 +2.
N21(Z)=
Z2n22+2
Orders
z2n22+1
r -- ýý--i------
--------------------
2n 1+2n 22+2
2n1+2n22+1
2n 1+2n 22+3
2n 1+2n22+2
Z
z2n22
r-------------------------
2n 1+2n22+1
2n1+2n 22
2n 1+2
2n 1+1
2n22+1
2n
22 .1•
I
2n 1+1
2n,
-------------------
----------------------------------
r-------------#
2n22+2
1
----- 1
0
Fig. 7.5. Possible separation locations in N21(z)D (z).
Evaluation of P2 (z) reveals that the coefficients associated with z, z2" +2 and z2"2 +2 are1
b22 and
F2
-,
F2
22
sF
respectively Therefore, determination of b4 and b22 from P2 (z) is guaranteed. Next, the
coefficients associated with z and z2n" +2n22+3 in P2 (z) are given by:
P(2)_ 4b22
P•(
22 +b22
Fs
1
+ 1]+
a2+2n2
F4 b22 +b22
+
Fs
F
(a21 +b21 +a2C21
2
F2
(7.18)
(7.19)
-1,]+[-2 + 22•21+b2 +a2C21
Besides, it can also be verified that the coefficients associated with z2 '+2 and
2n22+ 2
in P2 (z) are given
by:
(2)
b22 [ a22 + b 22
[Fs F
1]+b22 al- ]1[Fs Fs,
b22
F
b22(
21+
b+
F
if n, > n22 ,and
117
]
c21)
,
(7.20)
(2)
P2n2+2
_
b[ a
22b221
FsL 2 Fs
]+ Fs--[-
2 a+22 +21
Fs
+ a12C21
(7.21)
if n22 > n1. Combining (7.18)-(7.21) yields the following matrix equations to uniquely determine a,, a22
and (a21+b +a2c21), depending on the values of n, and n22:
2)
sF Fs2P(
a,
1 b221
2 1
1
1
a22
•
a21 +b21
}2
- b22
+
{P2n,
=
a2C21)
+2
Fs (
2nl+2 +3
F b22
(7.22)
- b22
+
if n > n22 and
1a
1 b22
2
1
2
1 J(a
a22
21 +b2
( 2)·d
p
+2 {2-b22
Fs·(Fs2 Ab~22122)
= F {P+2n22 3 +4}-b22
+a 2c 21)
(2)
3
2n
22+2
FS
(7.23)
b22
Fb
if n22 > n. Therefore, together with b,and b22 ,the polynomials N (z), D1 (z), N22(z), D22(z)and
N21(z)can be determined uniquely Then the remaining polynomial D21(z)
can also be determined as follows, since PI(z)= D 2 1(z)D22)N ()=[D
2
(z)D22()]NI (Z), D 22(z) and N (z) are all given. Evalua-
tion of IP(z)reveals that the coefficients associated with 1, z and
(1)
b22 a+bi
Fs F,
F,
ý2
-1
Fs2
b22 +
(1-d
12
+ -2+ a2 +a
2C21
Fs
Fs
are given by
(7.24)
b22(1-d
21+a2C21)
21)b22(b
1)= b222(1-d21)
Fs2 al +
c
Pi +4n22+4
Z2" 21+ 4 n22+ 4
Fs
21 )
+
b22 (b21 2a 2C21
an
Fs2
.
First, b2, Can be determined from (7.26). Using (7.24) and (7.25), we have
118
(7.25)
(7.26)
(1)= 22(1-d2 [a+
1)
1 [alb
1]
(7.27)
which yields d21. Then c21 can be determined from either (7.24) or (7.25). Finally the knowledge of b2,,
c•21 and (a21 +b21 +a2 C21) yields a21. Therefore, the 2-channel Wiener model of the human cardiovascular
system is identifiable if (7.15)-(7.17) hold. Note that (7.15)-(7.17) are less strict than (7.14). []
The analysis above guarantees that the coefficients of both the dynamic i.e. transfer function portion
and the static nonlinear portion of the Wiener model can be identified up to scale. It can further be shown
that the scale can also be determined for this specific 2-channel Wiener model First, note that all the numerator polynomials N, (z), N2 1(z) and N22 (z) are monic, which can be used to determine the scale of the
transfer functions involved in the Wiener model, as briefly discussed in Chapter 6 for the asymmetric T-tube
model. Furthermore, it is also obvious from (7.7) that both G,(z) and G2 (z) have unity DC gains, that is,
IG1 (jO0) = 1 and IG2 (jO)1= 1, which physically implies that there is no energy loss involved. Therefore, the
loss in the mean blood pressure from the aorta to the radial and the femoral arteries cannot be accommodated by the transmission line portion of the model, and it should be taken care of by the static nonlinear
function, which yields:
I=N- l [ ],
where
.
(7.28)
and 52are the mean blood pressures at the radial and the femoral arteries. Since (7.28) provides a
non-homogeneous relationship among the coefficients in the static nonlinear function, the scale of the static
nonlinear function can be determined accordingly
Remark 7.3: In general, the mean blood pressure drop at the radial artery is negligible (e.g <5mmHg),
while the mean blood pressure drop at the femoral artery is larger (e.g. >10mmHg). This negligible energy
loss on the aortic-to-radial channel is one of the reasons why a single-segment transmission line model suffices for the aortic-to-radial cardiovascular channeL []
Summarizing, the 2-sensor human central cardiovascular monitoring reduces to identifying the coeffi119
cients 0 characterizing the Wiener representation of the human cardiovascular wave propagation dynamics
(7.29)-(7.31), which is also shown in Fig. 7.6:
G,(
(z,)
G,
= 2
+bi)F
- 1] z
Z'
n+) +[(a/n,
-1z2n,
+41
N 21
(7.29)
(z)
D2 1(zz)D 22 (
X 2 (n)
4
N' [P2 (n),o] = ýrk
2
22
-
(7.30)
N 2 1(z) zn 1 + [(a 22 +b22 )Fs -1]
D21 () Z2n22 +(a 22/Fs _)z2n +b22/Fs
)Sk [P2 (n)]
(7.31)
k=1
where 0- {n1,n 21(n,n22 ,0})22 and o 1 4albl,a21,b21,C21,d2122
•2),
. ..
r
)
yl(n)
Y2(n)
x2(n)
Fig. 7.6. Block diagram of Wiener cardiovascular system from aortic to peripheral blood pressures.
7.1.4. Implementation Issues
From the full-scale human cardiovascular simulator described in Chapter 4, blood pressure and flow data
for totally eight different human subject models, each having 1,000 samples of blood pressure and flow signals (which corresponds to the 10s time interval with the sampling frequency of 100Hz), were collected. In
order to apply the blind identification and the input signal reconstruction algorithms developed in Chapter 2
to these data for 2-sensor human central cardiovascular monitoring, the following challenges specific to the
model structure (7.29)-(7.31) had to be taken care of:
1. In the absence of aortic measurements, the pulse transit time parameters n1 , n21 and n22 deter-
120
mining the orders of (7.29) and (7.30) are unknown prior to identifying the cardiovascular system
(see Remark 6.3). Nevertheless, a qualitative discussion can be made as to their identifiability First,
ni, n2 and n22 are parameterized in (7.29) and (7.30) in such a waythat they affect the magnitude
as well as the phase frequency responses of the cardiovascular system given by (7.29) and (7.30).
Second, the influence of nI on the magnitude frequency response of G,(z) is distinct from that
of the polynomial coefficients a, and b,, and the influence of n22 on the magnitude frequency
response of G22 (z) is distinct from that of the polynomial coefficients a, and b22 as well, since
G22 (z) assumes exactly the same form as G,(z) (see Fig. 6.9 for details). Third, scrutinizing
G21 (z) reveals that the magnitude frequency response of N2 1 (z) is affected only by n22 , whereas
the magnitude frequency response of D21 (z) is affected by both n2 1 and n22 . Therefore, once nl
is accurately identified, n2 1 and n22 can be determined accordingly by virtue of their distinct influences on G21 (z) and G22 (z). Furthermore, using the peripheral blood pressure measurements, the
"differential" pulse transit time, defined by An -n2 - nI with n2 An21+ n2 2 , can be measured as the
end-diastolic or foot-to-foot interval between the peripheral blood pressure signals (see Remark 6.9).
This An plays a crucial role in efficiently identifying (7.29) and (7.30) by imposing a restriction on
the orders of G,
1 (z,)
and G2 (z,0). In particular, noting that nI and n2 essentially specify the
effective lengths of the upper-limb and lower-limb cardiovascular paths, a physical implication of
fixing An to the measured differential pulse transit time is to constrain the difference between the
lengths of the upper-limb and lower-limb cardiovascular channels so as to facilitate the accurate determination of the system orders in (7.29) and (7.30). In this thesis, we iteratively applied the blind
identification algorithm to (7.29) and (7.30), and optimized the solution over a range of physiologicallyrelevant values of nl and n22 , with n21 -n -n 22 +An.
2.
By virtue of the physical implications of the coefficients in the Wiener model, O parameterizing
(7.29)-(7.31) can be constrained as follows:
121
SDo={0 ni>, n2 >O,n22 >O, al > 0,, > O,a21 >O,b2 >O,c2 > O,d2 >0,a22 > O,b> 0}.
22
(7.32)
3. Due to the lack of physical implication in the static nonlinear function (7.31) to describe the lumped
nonlinear effects, it is not trivial to choose the basis function and its order of expansion. In this thesis, we used a set of polynomial basis functions, i.e.
[k []k as a preliminary trial, because of
their simplicity as well as their abilityto serve as universal approximators as k2 -> oo. In addition, its
order of expansion was determined to be k2 = 2 by trial and error. It turned out that the expansions with k2 > 2 did not deliver significant improvement over k2 = 2.
which, altogether, results in the constrained least-squares formulation (7.33):
0 =narg,n min
[ miGT' (z,0)y (n)
-G'(z,0)(n
EDO LOEDO
1
.
(7.33)
22
7.2. Results and Discussion
First, true versus identified aortic-to-radial frequency responses of the cardiovascular wave propagation
dynamics are shown in the upper plots in Fig. 7.7 for eight human subject models, which suggests that the 2channel Wiener model of the human cardiovascular wave propagation dynamics can be accurately identified
by using the blind identification algorithm developed in this thesis for a class of 2-channel Wiener wave
propagation systems. Besides, using the 2-channel cardiovascular wave propagation dynamics thus identified,
the aortic and the abdominal aortic blood pressure signals, i.e. P,(n) and P,(n) in Fig. 7.3 and Fig. 7.4,
were reconstructed, which are shown in the lower plots in Fig. 7.7 for eight human subject models. The accuracy of both the aortic and the abdominal aortic blood pressure signals suggests the physiological relevance
of the Wiener two-segment transmission line model structure developed in this thesis for the aortic-tofemoral cardiovascular wave propagation dynamics. Noting that measurement of the descending aortic blood
pressures is extremely difficult in non-invasive clinical settings, the methodology developed in this thesis may
122
open up new possibilities for reliably estimating these hard-to-access internal signals.
The errors associated with the aortic blood pressure reconstruction are summarized in Table 7.1, where
the root mean square errors (RMSE) are shown to be less than 4% of the associated mean aortic blood pressures for all subject models. On the average, RMSE is approximately 2.5% of the mean aortic blood pressure.
In order to quantify the benefit of adding the static nonlinear function N2 (.) to the aortic-to-femoral
cardiovascular wave propagation dynamics shown in Fig. 7.3, the Wiener 2-segment transmission line model
was compared with a linear 2-segment transmission line model (which is identical to its Wiener counterpart
except for the absence of N 2 (.) in Fig. 7.3) by characterizing the cardiovascular wave propagation dynamics
and reconstruct the aortic blood pressure signal using both of them. The aortic blood pressure signals thus
reconstructed are compared in Fig. 7.8 for eight human subject models, which clearly suggest that the static
nonlinear function plays a crucial role in compensating for the blood pressure drop caused by the arterial
visco-elasticity etc. as well as minor morphological distortion. The RMSE are compared in Table 7.1, where
employing the static nonlinear function results in the decreases in the RMSE of aortic blood pressure reconstruction by approximately 39% on the average, from 4.1% to 2.5%.
In order to assess and accommodate the effect caused by the dynamics associated with the arterial viscoelasticity, the following nonlinear function was compared with (7.31) in terms of the accuracy in reconstructing the aortic blood pressure signal:
X2(n)' N'[P2 (n),O] = () [P
2(n)]k +Iq
k,=1
P2(n)1
(7.34)
k2 =1
which essentially resulted in nearly identical results to those shown in Fig. 7.8, suggesting that the viscoelasticity-induced dynamics does not significantly affect the overall response of the cardiovascular system. In
fact, this finding accords with a previous experimental study [64], which showed that the dynamics associated
with the arterial compliance is not crucial and it may be approximated as a static nonlinear function.
123
i I
111111
l lI
I
II;;" ll l
S1111
I 1 11111
n ,l
II lli
I
III l
•
1111111
1111111
I
II
I
__True
II II
'i
- True
-
I
I
I
I
-100
I
id
l
I II
Ienfe•
-
I I I Ii
1 11
1 111111
i l11
I
I
I
-
,
II
IIII
-
------Identified
T
I 1
1l
I
I I I
1
Frequency [Hz]
-
-
- - F-
- -I - -I
-
---
I,
o
<
4.8
5
5.2 5.4
Time [sec]
10
%%
100
m
-II
r--I
•
1
Frequency [Hz]
.E 120
E
110
a.
- ---F
------
-200
10
-
---
-.
-- - -- --
90
80
------
4.,8
r---I-
i-----
5.2 5.4
Time [sec]
5
5.6
(a)Subject # 1
I
I
I I I
1
I I I II
111
I:I!
I II I I II
I I
III1I
11111111
I
-100
I
I I I I II
11111
I I11 III
1111111
,.
_I . I II
I I
II
-True
T
-True
Identified
-\T-
0
I
11111
I III
I
--
I
11111111
II 111111
Identified
-200
101
100
Frequency [Hz]
, .t•
100
Frequency [Hz]
14nf
I gg
I
L
I
A
00-_
--
I
IL
I
I
L
80
-
s
_
__
II
i
7n
4.6 4.8
i
i
-L
-_,- _
g
I
_
I
i
70
-
5 5.2 5.4 5.6
Time [sec]
(b) Subject # 2
124
4.8
5 5.2 5.4 5.6 5.8
Time [sec]
-
A ^f"
I UU
I
I
II I IIII
I I II
l
I ,,I
IIil
C
I
0
I
11111
I
11111
I
I Il iIt
I
I
I
I 11111
1I 11111
I II1 ,
II lilI~t
,I
•t
-100
"Identified
"
100
Frequency [Hz]
I
3 110
E
I
|
10
I
I
I
i
i
i
I
4
F-IL-V I-L
I
i
'
"
-nn
I
I
u
L.
.I
I
•'•%
I
,
I
I
I
E
I
I
101
II
---I
- ----I
I
I
I
,--
I
100
I
I
II
E 110
100
E
90
0
"I
100
Frequency [Hz]
412
I-I
I
I
Identified
-
I
I 1
-- I--
I
--
'-C-
0
I
<
4.6
4.8
5
5.2
Time [sec]
5.4
5.6
4.8
5
5.2 5.4
Time [sec]
(c)Subject # 3
III IIIIII
I
---
IIIIIII
I
r--14. r--W--
100
W4WI
o0
II
li
I
I
l
i
I 1I II11
III I .
IlI
-100
-True
-- Identified
"
I
I
-200
II
Frequency [Hz]
* ---
Frequency [Hz]
41d•
I
I
-
I
I---1
%
II
100 --
90
-- -
I
"----I
5
I
-
I
80
I-
IL
-
--
-II
I
-I-I ---
7
5.2 5.4 5.6
Time [sec]
5.8
-- I-----
i
4.8
4--- -----------
I
r
I
011U
I
r----
5.5
Time [sec]
(d) Subject # 4
125
------
4fll'%
I
~ ~~ 1-4
I I II I
-:4
- I.-I ItI- I. - - f
r
I III I
1.-14
.I-I- i I1
1-
IIIIIII IJill,.Fi/I i• l lll
I
-,,
0
'
II
I
I
I
i i ''ii i
I
I
ii
I
I
III
'i
!
i. I I lilI
Truie
Ident fie
-Identified
I I
I
-100
•
I•,•
I ri
,
,
-200
100
Frequency [Hz]
'
I
110
'
I
I
IIII
'•I
I,
i
101
'
'
I
I
I
I
I
I
90
If -~c--
----..
80
-I
I
I
-
4.8
I
I
5
l
-
I
I
- -
I
-
I
100
-c-
I
I _
5.2 5.4 5.6
Time [sec]
I'~_I___
J
-lr7-------u;-~----
-
I
I
I---r~ft----l-
__~
100
----
101
100
Frequency [Hz]
-.1
- -N-
r
5.8 I
5.5
Time [sec]
(e)Subject # 5
I
11111
11 1111
I
11111
i
Illi iI
il
,i
I
i
I
I
1
I 1 I 1111
I11111
I
I
I
True
Identified
I
I
I
-- I-
---
--
~
I I'
Frequency [Hz]
I
I 80
E
E
m 70
-
-
j
I
II
I
I
I
I
II
-
-
I
r
- I-
0 60
----
I
I
I
r-------.
<
4.8
-h-
101
'
~
1
j
Identified
---
H
-
l
.
True
100
Frequency [Hz]
H--
Ililii
III~:Ijq,
I I
'll/l
1 111,111/1
I II l I I
i I
II
--
I
I
I
5
5.2 5.4
Time [sec]
5.6
4.8
(f) Subject # 6
126
5
5.2 5.4
Time [sec]
5.6
I --II- I I I i-III II
1
I I I
--I
-
II-I
1 I I i
I I
1
ill I I- - 14
III
C
0
I I I II II
I
I I I I II II
I
11111
I
II I IIIII
I
I
IM 1I 4i1iii
111111
I
I II
I
1I I II
I I I II
I
I
I
I IIII
enII•dI I
I
-Ill
I
-100
Identified
-
II
S II
'
Il
100
--
Identified
SIl
I
"'
I
I III
-l200I l
--LU
101
10o
Frequency [Hz]
101
Frequency [Hz]
4/f/fl
I
E
I
SI
-.L-- -
- ---.
-L, -
:4I
-
-
~jh~
1,1
I
i
I
4.4
4.6
I
..
---L
.
i---
-
I
I
I,
L-
innI
%
ft
~~iI
/I
E
. . ..
L'--
i
0
i
I
4.8
5
V
5.2
4.6
4.4
4.8
lime [sec]
5.2
5
5.4
Time [sec]
(g) Subject # 7
I
I I I I IIII
1-14W
--
I
Il
l
I
I
I
III
-- I--
I I
-
I I III
1-
1
W-
,
IIlIl i l I
I
I
I
I I IIII
i-
111
I I dentified
I IIII
I i,II
i
I
-100
-__
-
-
True
'l
Identified
Sit l
1I
it11
""
-200
101
100
Frequency [Hz]
Frequency [Hz]
110
I
100
I
I
-----
90
I
I
I
I
1
I
80
----------
------
II
-
70
I
I
I
-
-
I
--
SL-
60
I
nu
Time [sec]
Time [sec]
(h) Subject # 8
Fig. 7.7. True versus identified G,1 (z) and true versus reconstructed PJ(n) and P,(n).
127
Table 7.1. Comparison of Wiener 2-segment transmission line model and linear 2-segment transmission line
model: RMSE and normalized RMSE in aortic blood pressure reconstruction for eight different human subject models.
2-Sensor, Wiener 2-TL Model
2-Sensor, Linear 2-TL Model
RMSE
Normalized RMSE
RMSE
[mmHg]
[%]
[mmHg]
1
1.83
1.9
4.09
4.1
2
1.42
1.6
2.25
2.6
3
2.58
2.7
3.61
3.7
4
2.91
3.6
4.79
5.9
5
1.55
1.7
2.33
2.5
6
1.92
2.8
2.77
4.0
7
1.92
2.4
3.75
4.8
8
2.95
3.5
4.54
5.4
Subject ID
Normalized RMSE
[%]
2.5
4.1
120
125
-
120
115
'
- Wiener
2-TL
LowerLimb
---
--
r95
---
I
I
--
- --
I
100
I
---
----- I-
,E 105
a.
I
-1-
I
---
- -
-
- -
120
I--
I
I I-I--- ----4--+---
I
'--
I-
l
I
- I4 -
+I--
I
-1- --
r-
I
--
110
--
a.lo
105
-
I
I
--
---
---
I--4+--I---I--"--
2-LI
I
--
fi
I-
-
r--- 2-rL Lower imb
Linear
1--1--l-
+
I
I-1----1---t--rl
I
r - -
I
.
I
I-
Winer
-
115
------
t--l--1--r-------I
110 ----
I
I
- -1
-...-- -Lineer2-'LowarLimb
-I-
--
--
S-
1. 4--+
--
--
I
I,
1--+
--
I
--t-
---
+- -I---
-
-
---
I'
-
- --
-
1
-
-
-I-
-
4
4
C~Y--+XZ--
1~
--
--
-1--
75
--
-
----
-
-- I-
--
-
-
-I-
-
-
-
go
i
- -
5
so
-
4--
I l- --I
--- -- - -------.-I-
~---
I
75
"
I
L
I•--- ------- - -----I--- II
-I
-4 - --
II--k
- --
I--
-I
4
I--C-
I
li i
.I-
I
I
I
I
--I--
---- 85---I-- I--75
I
I
I
105
110
IIi
7IM
)
7
75
80
85
90
True
05
Aoltic
100
BP
70
[mmHg]
(a) Subject # 1
128
75
- -I-- I
I---
80
-
I
-L-
-J
- •----4 I.-- --1 -.-1--L-I-4
-- I
I--
-
I-I--
-
85 90
95 100 105 110 115 120 125
TrueAbdominal
AorticBP [mmHg]
lb
--- Wiener
2-1.
Lower
Limb
- Liner
2-1.LowerLimb
100
I
--
/
---
---
---
•g5
m.2
a.
T
Ii
I
1so
--
75
i^
II
II
--
4
I II -
-
-
II-4I-
--
rou
)
?
75
80
85
True
90
Aartic
BP
M
100
105
Tmr Abdominal AorticBP [mmHg]
[mmHg]
(b) Subject # 2
1•0
Wiener2-L LowerLimb
Linear2-11L
LowerLimb
115 . -.-
I
I.,
II-~110
J -
-
-
--
!
0.
II
II
II
'
'I
I
I
,
-
I
iI
- -
Ig
I
1
1051
-i . ..
U
-=0
-8
--
M
--
90
95
100
True
Aortic
BP
iM
110
115
120
ThoeAbdominal Aortic BP [mmHg]
[mmHg]
(c)Subject # 3
110
lin
I
I
Wiener 2-7L Lower Limb I
- Liner 2-11.
Lower Limb + - I
I
I
I II L
---
105 --
100
I
I
II
I-
----- Wiener2-LLowerUmb
105 Liner2- L LowerLimb
I
I
I
I
- -
-
- -
I
I
-
too
I
900
85
90
85
~80
|75
70
--
-I--
T
-I
70
T••----I-
I S--I
7 !
----I
I- - -I -
I
-------- If-~-t--
I
I
€*/l-I-II,,LLw -I-
-_
•~-------w
-T-W--
I
-I-I"
III
II
--
+-----
I
I
-I
--
85
05
o0D
I
--
5
I
I
70
75
I
I
80
85
00
95
TrueAorticBP [mmHg]
I
I
100
105
110
00
(d)Subject # 4
129
55
70
75
80
85 90
95
TrueAbdominal Aortic BP [nmHg]
00105
110
--"-- Wiener2- LowerLimb
* LUnear
2-L LowerLimb
I
110
105
.
I-Lo-e
-----
I
I
,
110 -
L
*
--- I - - - 4-
5
I
I0
go
-1-- --
L/ I
--
I
I
I
FS105
- -
100
.9
Wiener
2-R Lower
Limb I
*Linear
2-TLLowerLimb
100
T-
I -
I
I
_-
+-I--
I
I
I
go
0,0•"
J85
80
·=-
-5
7
--
80
M
00
The
M
Aartic
BP
---
---
---
100
105
110
· =_
__
75
115
__
80
__
90
95
100
105
TmIeAbdominal AorticBP [mmHg]
85
[mmHg]
110
115
(e) Subject # 5
--
-[--Wiener 2-TLLowerLimb I
- Linear 2-TLLowerLimb
Wiener 2-L LowerLimb I
,--
Linear 2-TL Lower Umb
-- I-- -i
55
80
S
I
-L
- -
. . ..
--
-- I--
85
70
75
ThmiAbdominal AorticBP [mmHg]
TrueAorticBP [mmHg]
(f) Subject # 6
SWlener 2- LwerULimb
95
Limb--
--- Uner2-TL a
I
I
I
L--L-L.
I
Wiener 2-L LowerLiUmb
--- ine2-TL LowerLimb-
05
I
L.
I
L
I
90
I"
---
--
--
I-
- -
•0.
i
8
-
--
S85
---
-I
-J
- -I
I
-a
I
0
75
I
'°
t j70
i
S-I
I
I
--
- -r
-
-•--
r-
-
-
75
I
65
85
60
"
w
55
-
60
..-- L----1L
iSI
05
-
75
80
70
85
ThueAorticBP [mmHg]
90
-
95
on
"
100
3
'"
5
00
65
--
70
75
True
(g)Subject #7
130
.L1
--
Abdominal
-80
Aortic
BP
L ..--7----
--
--
M
90
Z
[mmHg]
100
Wener 2-7 LowerUmb I
105
I
I
I
- -1 - - -
-
-
T
-
Linear 2-1. Lower Limb
.. -
-
.
Wiener 2- LowarUmb I
Linear2-TLowerLimb +
-I-
- -I-
--
- -I-
--
-
1056
I
I
I
100
100
95--
I---I--~-
85
--
I-- -F-I- -----
IL ·-
1~-L---L
go
8
r---- --
lI
I1---w•
~
-----
95
1--LI
I
--
--
I--
I
T
-------
I----
65
O
-
M
70
75
-
-
80
Thus
M
Aortic
00
BP
M
100
105
60
110
i
i
i
ii
65
70
~
-I -
-•-
--
--
I
-
-L- -
I
I
i
i
S
70
05
D
--
-
|75
- -
70
w=
7
_ _ I__ _I_ _
L
7I
-
i
i
~ ~i
I
I-- ---- I- - -I--
-
_ _ I__ _I _ _
I
III
i
i
i
i
i
i
i
i
i
i
i
i
i- i
75
80
85
90
95
100 105
TrueAbdominal
Aortic BP[mmHg]
[mmHg]
-
110
(h) Subject # 8
Fig. 7.8. Aortic blood pressure signals reconstructed by Wiener versus linear 2-segment transmission line
models of aortic-to-femoral cardiovascular wave propagation dynamics.
Table 7.2. Identified pulse transit times.
Radial PTI
Abdominal PTT
Femoral PTI'
2ni-2n22 I
[ms]
[ms]
[ms]
[I]
1
39
91
48
2
2
45
101
48
1
3
45
102
42
1
4
55
95
78
5
5
55
99
58
1
6
57
115
45
2
7
40
103
49
2
8
55
122
43
2
Subject ID
The blind identifiability conditions (7.15)-(7.17) for the 2-channel Wiener human cardiovascular system
(7.29)-(7.31) are satisfied by the identified pulse transit time parameters, as summarized in Table 7.2, which,
131
together with the persistent excitation of the peripheral blood pressure signals, suggests that the 2-channel
Wiener human cardiovascular systems for the eight subject models are correctly characterized.
7.3. Summary
In this chapter, the blind system identification and input signal reconstruction algorithms presented in
Chapter 2 were applied to 2-sensor human central cardiovascular monitoring based on the 2-channel Wiener
representation of the human cardiovascular wave propagation dynamics. In particular, we proposed a physicsbased gray box representation of the aortic-to-femoral cardiovascular channel dynamics to facilitate the blind
identification procedure. Using the eight subject models based on a full-scale human cardiovascular simulator,
we demonstrated that high-fidelity physiologically relevant representation of human cardiovascular wave
propagation dynamics can be achieved, from which the aortic and the abdominal aortic blood pressure signals
can be reconstructed from two extremity blood pressure measurements. In effect, this chapter provides an
initial proof-of-principle for the applicability of the 2-sensor central cardiovascular monitoring methodology
developed in this thesis to human cardiovascular system.
132
Chapter 8. Non-Invasive One-Sensor Method
In Chapter 5-Chapter 7, we have shown the feasibility of 2-sensor central cardiovascular monitoring
methodology based on two distinct blood pressure measurements. However, measuring blood pressures at
two distinct locations is not an easy task in real clinical practice, and it may set limitations on the applicability
of the blind 2-sensor approach to the central cardiovascular monitoring. This led us to identify the following
extension opportunities (see Fig. 8.1):
1. Using non-invasive measurements instead of direct invasive blood pressures will make the blind 2sensor approach more realistic.
2. The blind 2-sensor approach may be applied to wearable as well as hospital practices by reducing the
number of physical measurements, i.e. sensors.
r
Fig. 8.1. Extension opportunities for 2-sensor central cardiovascular monitoring based on two blood pressure
measurements: non-invasive 1-sensor central cardiovascular monitoring.
Given these opportunities, we direct our attention to the non-invasive 1-sensor central cardiovascular
monitoring problem in this chapter. Especially we will demonstrate that the cardiovascular wave propagation
133
dynamics can be identified and monitored even with a single extremity measurement by judicious use of blind
identification methodology In particular, this chapter will develop a methodology to identify the cardiovascular wave propagation dynamics, reconstruct the aortic blood pressure signal, and estimate both peripheral and
aortic systolic blood pressures from a single non-invasive extremity sensor measurement. In contrast to the
previous related efforts on the use of a single physical extremity blood pressure measurement for reconstructing the aortic blood pressure signal, the methodology developed in this chapter solely builds itself upon
the blood pressure signal measurement at a peripheral location itself and it does not require a priori knowledge on the empirical and/or population-based cardiovascular wave propagation dynamics, e.g. a predetermined or a generalized transfer function [24-30].
Aortic BP, P.(t)
y1(t)
Radial BP, Pl(t)
Fig. 8.2. A non-invasive 1-sensor central cardiovascular monitoring set-up.
Fig. 8.2 depicts the set-up for the non-invasive 1-sensor central cardiovascular monitoring problem. The
main difficulties of this set-up, compared with its invasive 2-sensor counterparts that were solved in the pre-
134
vious chapters, are:
1. There is only one physical extremity measurement available for identifying the cardiovascular wave
propagation dynamics, which, from the standard input-output system identification point of view,
turns out to be an ill-posed problem, because both the process dynamics (cardiovascular wave propagation dynamics) and the input signal (aortic blood pressure) need to be identified from a single output signal (a non-invasive extremity measurement).
2. The scale of the blood pressure signal (which was supposed to be available in the previous invasive
2-sensor set-up) is lost due to the existence of the non-invasive sensor. Therefore, blood pressure
calibration becomes necessary in addition to identifying the cardiovascular wave propagation dynamics (which was the only issue that needs to be addressed for 2-sensor central cardiovascular monitoring set-up based on invasive blood pressure measurements).
The dynamic process from the aortic blood pressure signal to the non-invasive sensor signal can be well
described by Fig. 8.3. Throughout the development in this chapter, it is assumed that
1. The major dynamics involved in the process is the cardiovascular wave propagation; the sensor dynamics is relatively fast and is neglected.
2. The sensor is at least locally affine in blood pressure, i.e. for some q, and q2 ,
(8.1)
Y (t)= q-IP (t)+rlq2 .
Aortic BP
Radial BP
Pa(t)
Pl(t)
u(t)
Xi(t)
yl(t)
Fig. 8.3. Dynamic process from aortic blood pressure signal to non-invasive sensor signal.
Remark 8.1: It is noted that the local affine relationship of the non-invasive sensor is not a strict restric-
135
tion. Indeed, many non-invasive blood pressure monitoring devices have approximately affine relationship
locally or even globally For instance, the Finometer and the Finapres finger blood pressure monitoring devices provide voltage recordings that are globally linear in blood pressure [66,67]:
y, (t) = q
1
(8.2)
(t) .
Besides, the tonometry devices, which usually calibrates its measurement using a cuff, provide voltage recordings that are globally affine in blood pressure [68,69]:
(8.3)
y (t)= q, P(t)+q2
Furthermore, even non-invasive optics-based sensors such as photoplethysmographic sensors, which exhibit
globally nonlinear relationship between their voltage readings and blood pressure, have locally affine relationship once they are appropriately placed [70]. Therefore, the range of application of the development in this
chapter is fairly broad.
[
The proposed approach of this thesis is to break the non-invasive 1-sensor central cardiovascular monitoring problem into two sub-problems, which are the cardiovascular system identification problem and the
blood pressure calibration problem, as illustrated in Fig. 8.4, which are addressed independently of each other
as we will demonstrate later in this chapter. Specifically the methodology developed in this chapter builds
itself upon the following three key ingredients: the approximated temporal 2-channel blind identification [401
heuristics-based system order estimation, and model-based blood pressure calibration. First, the approximated
temporal 2-channel blind identification methodology will be exploited to formulate a well-posed blind cardiovascular system identification problem based on a single peripheral sensor measurement. It will be shown that
once the system order i.e. the order of the cardiovascular system model is given, the cardiovascular system
identification problem reduces to a constrained least-squares problem. Next, a heuristics-based system order
estimation algorithm will be developed by exploiting the physics and the physiology of blood pressure propagation and reflection, where it will be shown that the system order can be estimated with reasonable accuracy
by minimizing the error associated with the constrained least-squares problem with respect to the unknown
136
system order, i.e. the aortic-to-peripheral pulse transit time. Finally a model-based blood pressure calibration
algorithm will be developed by exploiting the so-called "Windkessel" theory where the cardiovascular system
is approximated as a lumped parameter model having a capacitance and a resistance, which will be shown to
be able to accurately estimate the systolic blood pressure once the diastolic blood pressure is given [71]. The
non-invasive 1-sensor central cardiovascular monitoring methodology proposed in this thesis will first be
evaluated using the experimental swine subjects as well as the eight different human subject models based on
the full-scale cardiovascular simulator for preliminary validation and assessment. In addition, it will further be
evaluated using the experimental data obtained from real human subjects in order to demonstrate its expected
efficacy in real clinical applications.
Aortic BP, Pa(t)
----------------Aortic-Radial CV System ID
roach
BP Morphology Estimation
Radial BP, Pl(t)
Radial SBP
Model-Based BP Calibration
BP Scale Estimation
heory
Diastolic BP
Y1 (t)
Non-Invasive BP Sensor
Radial
Fig. 8.4. Blind identification and model-based blood pressure calibration for non-invasive 1-sensor central
cardiovascular monitoring.
Remark 8.2: In contrast to the diastolic and mean blood pressures which are to large extent consistent
137
regardless of the measurement locations, the systolic blood pressure assumes drastically different values depending on where it is measured, which is mainly caused by the blood pressure wave propagation and reflection in the aortic-to-peripheral cardiovascular channel. In most cases, the systolic blood pressure close to the
heart e.g. the ascending aorta is much more important than its peripheral counterpart, since the aortic blood
pressure is the actual load acting on the heart. For central cardiovascular monitoring, therefore, this thesis is
interested in estimating the aortic systolic blood pressure as well as the peripheral systolic blood pressure.[]
8.1. Cardiovascular System Identification Using a Non-Invasive Peripheral Sensor
First, we will briefly demonstrate how the blind identification methodology can be used to identify an
unknown dynamic process solely based on a single physical output signal measurement [40]. Then we will
apply this methodology to formulate the 1-sensor central cardiovascular monitoring problem, in which the
aortic-to-radial cardiovascular wave propagation dynamics is identified from a single non-invasive sensor
measurement at an extremity location.
8.1.1. Temporal 2-Channel Blind Identification: Basic Principle
Consider the following class of input-output system dynamics, which can be viewed as a generalized
auto-regressive moving average (ARMA) model:
y(n) = F[y(n-1),...,y(n-nD) ]
+
"•ku(n-k),
(8.4)
k=1
for some fl,"',N
,
, where nD and nN are the orders of the auto-regressive and the moving-average por-
tions of the dynamics, respectively It is assumed that only the output signal sequence y(n) is available for
measurement, whereas the input signal u(n) is not measured. Then after a sampling interval,
nN
y(n+1)= F[y(n),---,y(n-nD +1)]+ j
ku(n-k+1).
(8.5)
k=1
Following [40], it is possible to obtain a relationship that depends only on the output signal by exploiting the
138
difference between the output measurements at distinct sampling intervals. First, ubtracting (8.4) from (8.5)
results in the following:
N
Ay(n) ' y(n+1)-y(n)= AF[y(n),.,y(n-n D )
[u(n-k +1)-u(n-k)],
+
(8.6a)
k=1
where
AF[y(n),-,y(n-nD)]
(8.6b)
F[y(n),.,y(n-n o +1)]-F[y(n-1),'y(n(n-nD)] .
Now if we assume that u (n) is a piecewise constant signal over every (nN + 1) sampling intervals, ie.
u(n)= u(n-1)=... = u(n-nN) ,
(8.7)
then (8.6) reduces to the following relationship:
Ay(n)
(8.8)
y(n +1)- y(n)= AF [y (n),--, y(n-n D)].
Note that (8.8) depends only on y(n + 1),..,y(n - nD ) , which can be measured. Therefore, the differential
auto-regressive dynamics AF[.] can be identified under persistent excitation and model identifiability assumptions. Once AF[.] is identified, the moving-average dynamics i.e. the coefficients p, --
fl,
can be
identified through a procedure similar to the traditional 2-channel blind identification methodology [40]. We
will call this specific blind identification methodology the "temporal" 2-channel blind identification in this
thesis, because it pretends to have 2-channel signals by exploiting the measurement from a single sensor at
distinct sampling intervals.
Remark 8.3: In fact, the temporal 2-channel blind identification methodology was originally devised for
digital control systems where the control input signal passes through a zero order hold (ZOH) before it actually acts upon the physical plant. Consider the set-up shown in Fig. 8.5 depicting a closed-loop digital control
system, where Fs(i) and F( ° ) are the sampling frequencies of the ZOH and the sensor, respectively Note
that hi A
1
1
i) and ho A 1
are the corresponding sampling intervals. Then it is obvious that the piece-
( ) with
wise constant condition (8.7) can be satisfied by choosing F(O) A pFs
p > n, +1, i.e. by over-
139
sampling the output signal than the input signal [40].][
There are two major issues in applying the temporal 2-channel blind identification methodology to the
non-invasive 1-sensor central cardiovascular monitoring. The first issue is the validity of the piecewise constant assumption on the input signal for the cardiovascular system, since the aortic blood pressure signal
(which is regarded as the input signal to the cardiovascular system) is continuous but not piecewise constant.
The second issue is the unknown system order;, the cardiovascular system identification does not allow a direct application of the temporal 2-channel blind identification methodology since the order of the model
describing the cardiovascular wave propagation dynamics (i.e. the aortic-to-peripheral pulse transit time) is
not known a priori. The first issue can be quantitatively investigated by analyzing the propagation of the error
associated with the piecewise constant assumption, and it will be shown later in this chapter that the adverse
effect of the piecewise constant assumption can be effectively suppressed by increasing the sampling frequency In order to resolve the second issue, a system order estimation algorithm, which is capable of estimating the aortic-to-radial pulse transit time based on the physics and the physiology of the blood pressure
wave propagation and reflection, will be developed later in this chapter.
-oto U
• , #'f.\
,.I'.rL "
UML)
r[kho]
-01
ULKHiJ
_40
"1
L
-'
IL\
YtM)
I
01
-9
Fig. 8.5. A closed-loop digital control system for temporal 2-channel blind identification.
8.1.2. Temporal 2-Channel Blind Identification of Cardiovascular System
Now we will demonstrate how the temporal 2-channel blind identification methodology is applied to the
140
non-invasive 1-sensor central cardiovascular monitoring problem. Consider the single-segment transmission
line model (7.5) relating the blood pressure waves at the termination and a location X in the aortic-to-radial
cardiovascular channel (see Fig. 7.1). Using the time series sequence of the radial blood pressure signal, it can
be rewritten in the time domain as follows:
2
Pj (n+ nx +1)=F[PI(n+nx),Pl (n-nx)]+ZLkPx (n+2-k)
k=(8.9a)
F
S['F,
Fs
1
where the order of the moving-average portion of the dynamics is 2, F6- 1, /2
F[ (n+nx ),(n-n)
L -• I P
1,
1- 1 +1a and
(8.9b)
(n+n)-n -nx).
The problem is to identify the model coefficients a, and b, as well as the system order nx solely based
on a single non-invasive peripheral sensor measurement (8.1). Note that after a sampling interval, the dynamics (8.9) becomes
2
JP (n+ nx +2)= F[P(n +
A[
where F[[ (n+n
I
nx
+ I),Pl (n-n
x
kPx (n+3-k)
+1)]+ L
k=1
(n-nx+l)+Px(n+2)- -
(n+nx+1)-y
+l1),4P(n-nx +1)] a
1-
(n+n +n1)-L
P,(n-nx +1).
(8.10)
Px (n+1)
Subtracting (8.9) from
(8.10) and arranging terms, we have
2
AP,(n+ +1)= AF[P (n+nx),AP(n-nx)]+ P •kAPX(n+2-k),
(8.11)
k=1
where AP 1(n)
Jj-P(n+I)-Pi(n), APx(n) A-Px(n+1)-Px(n),and
AF[At (n+nx),AtI (n-nx)] - F[P (n+nx +1),Pl
FsbI
a
(n-nx +1)]-F[P(n+nx),P(n-nx)]
(8.12)
Therefore, if the input signal u(n)APx (n) can be effectively approximated as a piecewise constant signal
over p 2 3 sampling intervals, then the following functional relationship is obtained from (8.11), which de141
pends only on the radial blood pressure signal:
AI (n+nx+1)=[
,M1--- lnx
+ )-
L (n-nx).
(8.13)
Finally, it is obvious to show that in terms of the non-invasive sensor measurement (8.1), (8.13) can be rewritten in the following linear regression:
Ayl (n + n + 1)= 1L
where
e=oI1
02
'
a- 1
&Ay(n
and
+ n )-
AyI (n -n
x )
T
•
p
(n),
(8.14)
(n)A ,[Ay (n+n]x). Therefore, (8.14) reduces to a standard least-squares
y& (n-n,)
problem, once the system order nx is specified.
Remark 8.4: By virtue of the physical implications of the coefficients in the single-segment transmission
line model, a priori knowledge on the model coefficients in (8.14) can be exploited to expedite the blind identification of the cardiovascular wave propagation dynamics. Specifically it can be easily shown, similarly to
(6.9) and (7.32), that
0 e Do = {OI1 <1,92 <0,0, - 02 < 1}.
(8.15)
Combining (8.14) and (8.15), the following constrained least-squares problem can be obtained:
0=arg min JAy, (n+n + )-O'q(n)ll .
(8.16)
8.1.3. Error Propagation Analysis
Consider (8.11) and (8.14). In reality, because u(n), whose physical implication is the blood pressure
signal at the location x, is not piecewise constant, the moving-average portion of the dynamics in (8.11) is
not completely cancelled out in (8.14) and the remaining error acts as a disturbance in identifying 0:
Ay, (n+ nx +1) = 0'q (n)+ e(n),
(8.17)
where
142
Au(n+2-k)
2
L f
e(n)
,S
k=1
2
=
k
771
u(n+3-k)-u(n+2-k)
I A
(8.18)
k=1
is the error signal associated with the piecewise constant assumption on u(n). Therefore, it is of interest to
quantify the effect caused by e(n) on the accuracy of identifying 0. To analyze how e(n) propagates
through the cardiovascular wave propagation dynamics to alter y(n), a stochastic second moment analysis is
employed in this chapter.
Consider the block diagrams shown in Fig. 8.6. The panel (A) shows the real situation, where the radial
blood pressure signal Pj (n) is created in response to the true input signal Px (n). On the other hand, the
panel (B) shows the least squares formulation (8.14), where the true input signal Px (n) is approximated to a
piecewise constant input signal Px (n) by introducing an artificial error signal 3x (n) in order to create an
estimate of the radial blood pressure P (n), i.e. the radial blood pressure signal in response to the approximated input signal
x
(n). Given the panels (A) and (B), the effect of P,(n) on the accuracy of P,(n) can
be assessed by analyzing the propagation of Px(n) through G,(z) to
(n) ~A(n)-P (n) as shown in
the panel (C), by virtue of the linearity of the cardiovascular wave propagation dynamics G,(z).
(A)
CV Dynamics
Px(n)
(n) --
Gx
Gx(z)
PP (n)
CV Dynamics
(
(B)
Px(n)
/ x (n)
p(n)
J (
Piecewise Constant
(n)
G(z)
II
(C)
x
(n)
CV Dynamics
n
Fig. 8.6. Stochastic second moment analysis of error propagation associated with piecewise constant assumption imposed on Px (n).
143
To analyze the error propagation, consider the following state-space representation of G,(z) with
and
A (n)
x (n)
as input and output signals, respectively:
x(n+ 1) = Axx(n)+ BxPx (n)
(8.19)
A (n)= Cxx(n)
Given the mean and the variance of & (n), the resulting steady-state mean and variance of
A (n)
can be
estimated using (8.19) as follows. First, it is obvious that the mean of & (n) can be estimated by
mhI = C x (I-A
Ax)- Bmxhx,
(8.20)
where in and thx are the mean values of P(n)and x (n), respectively and I isan identity matrix having appropriate dimension. Besides, the steady-state variance of
&I E[E
2
(n)] = E[Cxx(n)x
where the covariance matrix
(n)C]= CxEx(n)xT
A (n)
(n)]C/
can be estimated by
C~XXC
(8.21)
:x of x(n) can be obtained by solving the following discrete Lyapunov
equation (see Remark 8.5):
AxExAT -Ix
+Bx&xB T =0,
where &x is the variance of
(8.22)
x (n).
Remark 8.5: Using the state equation in (8.19), we have
E[x(n + 1)xT (n+ 1)] = E [Axx(n)+BxPx (n)} {Axx(n) + BxPx ((8.23)
-
T
AXE[x(n)xT (n)]AT +Bx&'xB
where we assumed that the correlation between P (n)and x(n) issmall, because x(n)can be viewed
as a quantization error of Px (n), which is usually treated as white noise. Then (8.22) can be obtained by
noting that in steady state,
Ex-
E[x(n +1)x T (n+ 1)]= E[x(n)x (n)] .
(8.24)
The stochastic second moment analysis, especially (8.21) together with (8.22), will be used in this chapter
to illustrate how the adverse effect of the piecewise constant assumption on Px (n) can be effectively suppressed by increasing the sampling frequency Specifically since Px (n) is a band-limited low-frequency sig144
nal, it is obvious that increasing the sampling frequency will reduce a x by reducing the quantization error,
which in turn will reduce 8~ because P (n) is nothing but the output of a stable filter G,(z) in response
to P, (n). To demonstrate how effectively the choice of sampling frequency suppresses the error propagation, the stochastic second moment analysis will be carried out upon experimental data obtained from the
swine subjects using a few different sampling frequencies later in this chapter.
8.2. System Order Estimation: Pulse Transit Time Estimation
In order to facilitate the temporal 2-channel formulation of the non-invasive 1-sensor central cardiovascular monitoring problem, we will develop a system order estimation algorithm for the aortic-to-radial cardiovascular wave propagation dynamics by exploiting the physics and the physiology of the blood pressure wave
propagation and reflection.
It has been shown earlier in this chapter that the aortic-to-radial cardiovascular wave propagation dynamics can be characterized by solving the constrained least-squares problem (8.16) if the cardiovascular system order is known. Therefore, a critical issue is howto estimate the value of the system order nx, ie. the
aortic-to-radial pulse transit time. This chapter seeks to resolve this issue heuristically by analyzing the physics
and the physiology behind the superposition of the incident and the reflecting blood pressure waves at the
aortic-to-radial cardiovascular channel as a function of nx.
First, it is known that the effect of the blood pressure wave reflection is to redistribute the blood pressure with the value of the mean blood pressure preserved, since it is totally an oscillatory phenomenon.
Therefore, instantaneous change in the blood pressure due to reflection must average zero throughout the
heart beat, which implies that if the superposition of incident and reflecting blood pressure waves is constructive at some portion of the heart beat, then it should be destructive at some other portion of the heart
beat in such a way that the constructive and the destructive superposition is balanced out [72].
Fig. 8.7 illustrates an example of the incident and the reflecting blood pressure waves at the terminal lo145
cation of the radial artery; ie. nx = 0. The radial blood pressure signal is obtained by superimposing them
with each other. The relationship between PI (n) and Px(n) in (7.2) suggests that as the location x
moves proximally towards the aorta, Le. as nx increases, the incident and the reflecting components of the
blood pressure wave are separated apart by 2nx in time, as shown in Fig. 8.7, before they are superimposed
with each other to yield the blood pressure wave Px (n).
E
a)
0)
0.9
1
1.1
1.2
1.3
1.4
Time [sec]
1.5
1.6
1.7
1.8
Fig. 8.7. An example of the incident and the reflecting blood pressure waves in the aortic-to-radial cardiovascular channeL
Fig. 8.8 shows an example of the blood pressure signals PX (n) and their second derivatives that result
from the incident and the reflecting blood pressure waves in Fig 8.7 for different values of n,, ie.
nx = 0,.--, 6, which corresponds to 0, 10, 20, 30, 40, 50, and 60ms of pulse transit times. In this particular
example, the ascending aorta corresponds to nx =4, and the blood pressures associated with nx >4 are
physically meaningless. Fig 8.8 demonstrates that
146
1. For nx = 0, the incident and the reflecting blood pressure waves superimpose in such a way that
their superposition is highly constructive in systole, resulting in the largest pulse pressure at nx =0 .
2. The systolic superposition of the incident and the reflecting blood pressure waves becomes less
constructive (see '1' in Fig. 8.8) as nx increases, which results in the reduction of the amplitude of
the first peak (i.e. the systolic blood pressure).
3. The dicrotic notch starts to develop as nx further increases so that the peaks of the incident and
the reflecting blood pressure waves are completely separated apart by each other, which also results
in the amplification of the second peak (see '2' in Fig. 8.8).
Fig. 8.8 and Fig. 8.9 also illustrate that the fluctuation in the second derivative of the blood pressure wave
heavily depends on the level of the systolic blood pressure as well as the sharpness of the dicrotic notch. In
fact, it is proportional to both of them. In terms of the second derivative norm of the blood pressure signal,
therefore, it first decreases as the systolic blood pressure is lowered in response to the increase in nx , up to
the value of nx approximately corresponding to the ascending aortic location, where the dicrotic notch
starts to develop. Beyond this value of nx , however, the dicrotic notch cancels out and even overwhelms the
effect of lowering systolic blood pressure as nx further increases, resulting in the increases in the second
derivative norm as nx exceeds the aortic-to-radial pulse transit time.
Based on the analysis, therefore, the optimal estimate of nx ie. the value of nx corresponding to
the aortic-to-radial pulse transit time, can be heuristically determined by identifying the value of n, which
minimizes the second derivative norm of the blood pressure signal. Noting from (8.18) that the error e(n)
associated with the least-squares problem (8.14) converges to the second derivative norm of the blood pressure signal at a location X as the sampling frequency increases, ie.
lim e(n)= lim
AP (n
L, s 7
(1
Fs
APx(n)
)
147
=F
d
2
dt
(8.25)
120
E
E 110
a.
100
90
80
0.7
0.8
0.9
1
1.1
1.2
Time [sec]
1.3
1.4
1.5
1.6
(a) Blood pressure signals for different values of nx.
I
E
E
a.
cL
VO
0.7
0.8
0.9
1
Time [sec]
1.1
1.2
1.3
(b) Second derivative norms of the blood pressure signals for different values of nx.
Fig. 8.8. Superposition of incident and reflecting blood pressure waves in the aortic-to-radial cardiovascular
channel with respect to system order. waveforms and second derivative norms.
148
130
130
120
-- 120 - -L-
L
_- ..
nx=0
i
- I---- -
-- -110 - ,-
110
S-T
--
1--------
100
100
---- '--- -----
90 -
- ----
80
-
-
4--
---
----
---
1
1.4
70
1.6
130
-----
- - -
80
-- -
1.2
--`
90 --
-
7A%
0.8
0.8
1
1.2
1.4
1.6
142_
I.ItJ
S-
-
100
100
---
---------
-
-t
nx=6
--
----
-- -- -------- -- - - - --
90 F - - -
--I4----4-----4------
---
70
T
n2
- --
I-
III
0.8
1
1.2
1.4
Time [sec]
1.6
1
1.2
Time [sec]
0.8
1.4
(a) Blood pressure signals for different values of nx.
-----_
----
J__ L__
--
j-I
-
,
"o
-. . .
N
.
I ~,
1.,'11
----
Il
I
-o
--I
nx=O, Norm=11.2
0.8
-4-
,
I
1
I
nx-2,
--
_
S
I
I_o
Norm=10.2
1.2
1
0.8
0.8
1.2
N
I
1
1.2
.1
"V
Nu
A-1 NL_
I
.
.
.I .
-I
.
-
.
.
---
•'I• *I
llll -
I
I_
_ _L _
%
c0
-nx=4, N,
,, r
I
I
•
.
N.
------V
~
Il
I
I
------
~I
. . -- .•J I
--. I"II-,I,,
I----
Il
S
nx6,
tI
Norm=i1.1
I
nx=4, Norm=9.92
0.8
1
Time [sec]
1.2
0.8
1
Time [sec]
(b) Second derivative norms of the blood pressure signals for different values of nx.
Fig. 8.9. Blood pressure signals and their second derivative norms for different values of nx.
149
the estimation of nx can be combined with the least squares estimation of 0 in (8.14) simply by increasing the sampling frequency, nx can be estimated by minimizing the least squares error of (8.14) as a function of nx, if the sampling frequency is sufficiently high.
Remark 8.6: Combining the system order estimation with the constrained least-squares formulation in
(8.15) and (8.16), it can be finally concluded that 0 is a function of nx; 0= O(nx). Therefore, the noninvasive 1-sensor central cardiovascular monitoring problem can be formulated into the following nonlinear
constrained least-squares problem:
A {nx,} = argmin m
Ayl(n+nx +)-OTp(n)12,
(8.26)
where O8Do=({01 <1,02 <0,01 -92 <1}.1
8.3. Model-Based Systolic Blood Pressure Calibration
The model-based blood pressure calibration algorithm developed in this thesis exploits the so-called
"Wmdkessel" theory where the cardiovascular system is approximated as a lumped parameter model having a
capacitance and a resistance. Consider the simple 2-element Windkessel model of the cardiovascular system
shown in Fig. 8.10. Its governing equation is given by
dt
+-•P(t)=
RC
C
Q(t),
(8.27)
where P(t) and Q(t) are the arterial blood pressure and flow, respectively R is the total peripheral resistance, and C is the total arterial compliance.
The response of a cardiovascular system during the diastole can be viewed as a zero-input response,
since the heart does not provide any blood flow into the arterial tree during the diastole. Furthermore, the
systolic duration of a beat cycle is relatively shorter compared with its diastolic counterpart (i.e. approximately
30%). Therefore, if the phenomena is simplified by approximating the aortic blood flow to an infinite train
of impulses, then the response of a cardiovascular system can be approximated to an impulse response, ie.
150
the response to impulsive aortic flow signal. Then the solution to (8.27) within a beat cycle is given by:
•' , O_<tTT,
P(t)=Pe- A
(8.28)
where P, is the systolic blood pressure, AA I is the time constant of the exponential decay, and T is
RC
the beat cycle period.
Arteries
I
I
r\I/ rirr'
l.ixirna
1-
E
E
Pd= Pse ' T
Time [sec]
Fig. 8.10. Windkessel theory for systolic blood pressure calibration.
Noting that the diastolic blood pressure is the blood pressure at the end of the beat cycle, it can be expressed as follows, where Pd is the diastolic blood pressure:
Pd = P(T)= Pe
'
,
(8.29)
which can alternatively be written as follows:
(8.30)
Ps =Pde .
151
Therefore, the systolic blood pressure can be estimated using (8.30) by measuring A and T from the noninvasive sensor measurement, once the diastolic blood pressure is given [71].
Remark 8.7: The strength of this algorithm is its capability to calibrate the systolic blood pressure solely
by exploiting the time-related quantities that are consistent against the vertical scale of the non-invasive sensor measurement, that is,the quantities 2 and T used in (8.30) are independent of the vertical scale of the
measured signal as long as the non-invasive sensor is affine in the blood pressure.
I]
8.4. Validity and Quality Assurance
Given a time series sequence of the non-invasive sensor signal, the equality (8.14) can be formulated
into a set of over-constrained linear equations:
Ay(n+n x +1)=I Ay(n+nx) Ay,(n-nx) 0 0,
(8.31)
which is equivalent to (2.51). Therefore, the persistent excitation condition is given by the positive definiteness of •T0I*.Once the persistent excitation condition is met, the model identifiability issue becomes trivial:
the model structure (8.14), which is a moving-average model, is always identifiable.
8.5. Results and Discussion
The efficacy of the non-invasive 1-sensor central cardiovascular monitoring methodology will be demonstrated using the experimental swine subject data, the simulation-based human subject data, and the experimental human subject data. Specifically the results from the experimental swine subject data will provide
initial proof-of-principle by illustrating how effectively the system order estimation and the model-based systolic blood pressure calibration algorithms as well as the temporal 2-channel approach to the cardiovascular
system identification work in practice. The results from the simulation-based human subject data will show
that the aortic-to-radial human cardiovascular wave propagation dynamics can be accurately characterized
152
solely based on an upper limb blood pressure measurement. Finally, the results from the experimental human
subject data will demonstrate the efficacy of the non-invasive 1-sensor central cardiovascular monitoring
methodology for human subjects in real clinical practices by showing its capability to reconstruct the aortic
blood pressure signal very accurately from a non-invasive finger blood pressure measurement.
8.5.1. Experimental Swine Subject Data
First, the frequency contents of the aortic blood pressure signals in a total of 83 data segments associated with a swine subject were analyzed, which revealed that across diverse physiologic conditions associated
with the swine subject, 99% of the total energy in the aortic blood pressure signal lies within the low frequency envelop, i.e. below 13Hz. Then the Shanon's sampling theorem suggests that the sampling frequency
for the aortic blood pressure signal needs to be at least 25Hz, which, combined with the piecewise constant
assumption, yields the minimum sampling frequency of 75Hz for the radial blood pressure signal. For the
stochastic second moment error propagation analysis, therefore, we considered the sampling frequencies of
100, 200, 300, 400 and 500Hz for the radial blood pressure signal. The discrepancy between the true and the
approximated aortic and radial blood pressures under these sampling frequencies are shown in Fig. 8.11.
- [-
160
True
BP
j
140 ---
-- -
----- Appmximated
BP
120
120 - - ----
-I
-
0.1
0.2
0.3
100-
I
0.4
I
0.5
0.6
0
4-.
-
I-----. True
BP
Approximated
-BP
-••-
S
----------
0.1
-
---i
i
0.2
0.3
0.4
•
•
03
04
-
I
I
0.5
0.6
-20
,o
----
.20
-10-o--
20
- -
80
20
.10
- -
1 2 0
S10080
0
-
-
L
---.---
l-- 1H
0.1
0.2
0.3
Time [sec]
---
-----I--04
-0------
-A-
--
4
I----
0.5
-10
S0
0.6
I
0.1
I-----------
0.2
Time[sec]
(a) 100Hz
153
05
0.
.
lee,
.
.
r
--
-
142
0
--- rI
1200
100 - j.-i00--80
-
--
.0
(
i
-
a2---------'10 ----
I
0
0
0----
01
0.2
0
0.1
0.2
I
0.3
0.3
Time[sec]
-
0.1
----
------
0.2
0.3
I
0.4
0.6
0.5
ip
I
I
120
0.6
.E
•o
TmeBP
Appmximated
BP
E
--------
0.5
0.4
20
..
----
I
O4
0.3
IDO
--- Approximatd BP
-
--
0.2
.
TrueBP
----
0.1
0
,
.
I
S
I
0.4
------
05
0.4
0.5
I
I
0.6
Time [sec]
(b)200Hz
140 - - -
-I
---
E 120
14 - - -.
_- -
- - - -----
True BP
Appoimated
- - - ---
0
140 - - - -
...
0.2
0.1
I
BP
0.3
0.4
- - -
120----I
-
10
0
0.6
0.5
-
True BP
- --
imate
A
-
I
0.2
0.1
---
I
- -
....
0.4
0.3
0.8
0.5
20
J?20-
-10 -
-!-I
-"-----T ---V
---100
i-- --
-... ----
-10-------2-----------201
80
0
0.3
0.2
0.1
0.5
0.4
0.3
0.2
0.1
0
0.86
0.4
0.6
0.5
Time
[saec]
Time [sec]
(c)300Hz
10
- - - --
- - -
120-----------
- - -
100-- ------
---
Appmximated
P
140 p -
- -
1--e---100---
- - -- - -- - -
-
-
- -- -
-
-
Appoximted BP
:----1-----t----t---
--
80
800
f20
E
20
E
ol - - - . .
10---
.
l--- - ----
1----
SI
0
o.1
0.2
03
0.4
0.5
0
O.
Time [sec]
I
01
02
03
Time[sec]
(d)400Hz
154
-
I
-201 - - -I-
I
-40r
-I.. ,
t-------------
-
----
0.4
I---
0.5
I
0.0
lm.r
-
IM)
•
I
S
140
-
I
-
I
---
-----
-TrBP
Approximat BP
---
Tru BP
ApIted
0.4
0.4
0.5
140
E
0120-------
-------I
120
-
I
CO
100-
--
so0 0
1001
0.1
0.2
0.2
0.3
0.3
0.4
0.4
0.5
0.5
Wo
0.0
0.6
0
0.1
0.1
-
---0.2
0.2
0.3
0.3
0.6
20
W
I,
10----------
20
10
.20
1
-
0.1
I
I
0.2
0:2
p--
I
0.3
0.3
-- ----
I
0,0.44
I
0,--5
0.5
0.I
0.6
0.6
-
-
1
Time [sec]
Time[sec]
(e) 500Hz
Fig. 8.11. Discrepancy between true and approximated aortic and radial blood pressure signals under sampling frequencies of 100, 200, 300, 400, and 500Hz.
To quantify the first and the second moments, A, and &I, of P (n) using (8.20) and (8.21) from
those of Px (n), iAx and &x, the aortic-to-radial cardiovascular wave propagation dynamics (7.5) was identified using the standard input-output system identification for the 83 data segments, with the aortic and the
radial blood pressure measurements used as the input and the output of (7.5), respectively Then the corresponding 83 sets of the matrices Ax, Bx and Cx of the state space representation (8.19) associated with
the identified transfer functions were obtained, from which Ai and &i were calculated using (8.20) and
(8.21), based on the values of ix and ax measured at the aortic location. The values of 6~ (normalized
by the mean blood pressure of the associated data), averaged over the 83 data segments, shown in Table 8.1
suggest that the propagation of error caused bythe piecewise constant assumption on the aortic blood pressure signal can indeed be suppressed by increasing the sampling frequency In particular, &I is reduced from
7.3% at 100Hz to 1.8% at 500Hz. This implies that the radial blood pressure signals P (n) and P (n) created by the original and the approximated (to piecewise constant) aortic blood pressure signals P,(n) and
Pa (n) become closer to each other as the sampling frequency increases, which in turn suggests that the use
of higher sampling frequency is beneficial to improve the accuracy of the cardiovascular system identification
155
in the presence of piecewise constant input signal assumption.
Table 8.1. Normalized &4under sampling frequencies of 100, 200, 300, 400, and 500Hz.
Sampling Frequency
100Hz
200Hz
300Hz
400Hz
500Hz
5
7.3%
4.3%
2.9%
2.2%
1.8%
It is also noted that t5~ and &Iestimated from the analysis were compared with those directly calculated from the radial blood pressure measurements, in order to assess the validity of the stochastic second
moment analysis. Fig. 8.12 shows the true and the estimated ri, and &4 under different sampling frequen-
cies, which strongly supports the validity of the analysis in the sense that both i~ and &4are very close to
their true counterparts regardless of the sampling frequency
...........
True Mean
-.----- Estimated Stochastic Mean --- ~----True STD
-
------ Estimated Stochastic STD
I
I
---- 4i---~--- L-
IJ:.]l
1
I
I
I------
I-T------
_
I
I
I
-
FIl-----.
-
....
I---
I
I
I
I
I
I
I
I
I
200
300
400
500
600
700
800
900
1000
Time [sec]
(a) 100Hz
156
nr
z0
I
I
.......... True Mean
20
p
I
I
I
I
I
I
I
- ------- Estimated Stochastic Mean -----
15
I
True STD
E
E
a 10
0
o 5
----
----
------------------
I
I
-
-I
i
-
i
-
S
I
I
, ----
----- •
------
I
-i-
i,
-
I
-,'L-
-
I
J
i-
I --------
I
---
I ----
II
I
II
I--
I
I--
--
-'-----l---
----
I ----
-'
-
-
.V-- -
-20
200
300
400
500
600 700
Time [sec]
800
900
1000
,
,--
r- ,--r
(b)200Hz
25
I
I
I
I
----- True Mean
20 - -...--Estimated Stochastic Mean --- ----True STD
Tru
E
15 ------ Estimated Stochastic STD
,
E 10
5--
-----
- -- '-1
--
---
----
----
-
,
---------- --
-------, -1o5
T
-
---
- -
-20 ---- ---- T------
F
---
.
-- ,----
--
-25
200
300
400
500
600
Time [sec]
(c)300Hz
157
700
800
900
1000
25
I
I
.........
-.--.-*r-----
20
15
10
I
1
~----c------
---
I
I
True Mean
Estimated Stochastic Mean
True STD
Estimated Stochastic STD
-
I
I
---
--
r
'--
'
l--------~-
--
-------
5
0
----
----
---
---
----
L----I---~---
--
----
---
-5
r-
---
-10 ---- - --- - --
---------
-
----
-l-f1-
-----
---
----
,-- - - -- - --------- -- - - --- - - --- --, - -..
. .. '--.-...,
- -- -
-"--
-
-
-
-
-
--------------
- -
-
- -
-- -
-
-l
-15
-20
-25
200
300
400
500
600
700
800
900
1000
Time [sec]
(d) 400Hz
25
.........
True Mean
--..-Estimated
Stochastic Mean - - -True STD
---.
Estimated Stochastic STD
20
15
10
5 ----
--- -
---
--
- ---- ----
I
---- ----
-- ---
I
0
4-
-5
-
----
I
--
-
--
I--- -
---I--
-------
I
I.I--
-4
4-
-
---
-----
-
I-
----
-10
-15
---
----
F F
--
F
---------F
F
F
1--F
Fi
----
-20
_-2)
200
300
400
500
600
700
Time [sec]
800
900
1000
(e) 500Hz
Fig. 8.12. True versus estimated rhiand &I under sampling frequencies of 100, 200, 300, 400, and 500Hz.
158
The experimental results on a swine subject suggest that the non-invasive 1-sensor central cardiovascular
monitoring methodology developed inthis thesis is indeed able to identify the aortic-to-radial cardiovascular
wave propagation dynamics and reconstruct the aortic blood pressure signal with fidelity and reliability over
wide-ranging physiologic conditions. Fig. 8.13 shows a representative example of the aortic blood pressure
signal reconstructed from the radial blood pressure measurement.
160
......
S-------t
--
+-----•
I
---
----- True Aortic BP
-
Recovered Aortic BP
-
I
.......... True Radial BP
15(
. .I
E 14C
E
,---- "------------
:3
Ca
a.
,,.-
: X
.
,
6
i---
m
110
-
----
-
-~-
----
IL
%-
- - -- - -
- - - - - - I
III
100C
i
i
9.2
- - --
I
9.3
I
1
9.4
II
1
9.5
9.6
lime [sec]
I
i
9.7
9.8
I
9.9
Fig. 8.13. True versus reconstructed aortic blood pressures.
To analyze the effect of sampling frequency selection on the accuracy of cardiovascular system identification, the radial blood pressure signals having different sampling frequencies were used to identify the transfer function (7.5). Table 8.2 summarizes the least squares error associated with (8.26) averaged over the 83
segments of data under different sampling frequencies, which clearly suggests that the accuracy of the identified cardiovascular wave propagation dynamics is improved as higher sampling frequency is employed. Note
from the discussion earlier in this chapter that increasing the sampling frequency has two benefits:
159
1. It helps to identify high-fidelity cardiovascular wave propagation dynamics by suppressing the error
propagation caused by the piecewise constant assumption on the aortic blood pressure signal.
2. It also facilitates the estimation of the system order nx corresponding to the aortic-to-radial pulse
transit time by rendering the error signal e(n) in (8.18) closer to the second derivative of the blood
pressure signal, as shown in (8.25).
Table 8.2. Least-squares error associated with (8.26) under sampling frequencies of 100, 200, 300, 400, and
500Hz.
Sampling Frequency
100Hz
200Hz
300Hz
400Hz
500Hz
Least-squares Error
55.6mmHg
23.4mmHIg
13.2mmHg
8.7mmHg
6.3mmHg
To further quantify the accuracy and performance of the methodology to identify the cardiovascular
wave propagation dynamics and reconstruct the aortic blood pressure signal, it was compared with the averaged transfer function (see Remark 6.7) over the 83 experimental data segments, in terms of the aortic blood
pressure reconstruction error, 1u (n)- ý(n)l1 2 , as well as the accuracy of estimating the ejection duration and
the systolic blood pressure, which can be directly extracted from the reconstructed aortic blood pressure signals. Table 8.3 summarizes the results using bias, standard deviation, and R2 values as evaluation metrics,
which clearly suggests that the methodology proposed in this thesis far outperforms its averaged alternative:
on the average, the aortic blood pressure reconstruction was improved by 30%; besides, the estimation of
ejection duration and systolic blood pressure was also improved, particularly in terms of the standard deviation (25% for the ejection duration and 37% for the systolic blood pressure). It is also noted from Table 8.3
that the methodology could provide nearly unbiased estimate for the systolic blood pressure.
This significant benefit of the 1-sensor central cardiovascular monitoring suggests that the wide-ranging
physiologic conditions of the cardiovascular system cannot be described by a single predetermined transfer
160
function, as pointed out in Chapter 6 (see Fig. 6.4). The methodology proposed in this thesis allows for identifying each of these diverse cardiovascular wave propagation dynamics.
Table 8.3. Feature estimation statistics: blind and averaged approaches.
Blind Approach
Averaged Approach
Improvement
Mean 28%
Aortic Blood Pressure
3.8 +/- 1.OmmHg
5.3 +/- 2.7mmHg
R2 6%
RMSE
(R2 = 0.92)
(R2
0.87)
STD 63%
Ejection Duration
0 +/- 0.016s
0 +/- 0.021s
R2 12%
(0.21 +/- 0.07s)
(R2 = 0.85)
(R2 = 0.76)
STD 24%
Systolic Blood Pressure
0.4 +/- 5.0mmHg
6.3 +/- 7.9mmlIg
(124 +/- 76mmHg)
(R2 = 0.98)
(R2 = 0.93)
Mean 94%
R2 6%
STD 37%
To demonstrate the efficacy of the system order estimation algorithm developed in this chapter, the aortic-to-radial pulse transit times estimated for the 83 segments of data were compared with their true counterparts measured directly from the aortic and the radial blood pressure signals. Fig 8.14 suggests that the true
and the estimated aortic-to-radial pulse transit times are highly correlated with each other, which strongly supports the competence of the system order estimation algorithm to deliver accurate aortic-to-radial pulse tran-
sit time estimates.
Remark 8.8: Fig 8.14 also provides preliminary evidence that the model coefficients identified by the
methodology proposed in this thesis are physiologically relevant and they may represent important cardiovas-
cular features. I
161
V
0)
u)
0
E
200
300
400
500
600
700
800
900
1000
Time [sec]
Fig. 8.14. True versus identified aortic-to-radial pulse transit times.
180
I
-
-
I
-
-
II
----•
140
L
140
------
I-l-----
----
~I TI----
I
I
-
•
7
0"
I
I*~
•
.....
I
II
II
II
..
II.
7" -- I -- I--
~___l----
120
I
gI
•
I
I
180
I
-
I0.
I
I
55I
1I 0.t.5
180
r2=O.g674
+.
I
-"
-
I
"1
- i-
I
_
1-+---
. 100
I
S100
wU 80
I
l
.-. If
I
I
I
I
I
I
I
I
ll'
I
I
I
I
Co
80
----
00
- --
40
60
80
100
120
140
160
180
200
40
TrueRadialSBP [mmHg]
IIII
I
L.
I
I
60
80
I
I
----
--I
I
I
100
120
140
T-
100
Tre RadialSMBP[mmHg]
Fig. 8.15. True versus calibrated radial systolic and systolic mean blood pressures.
Fig. 8.15 shows a representative example on the results of the model-based blood pressure calibration,
where true versus estimated systolic and systolic mean blood pressures are compared with each other. The
systolic blood pressure was calibrated by using (8.30), where the time constant A was identified from the
end-diastolic portion of the radial blood pressure signal and the diastolic blood pressure was assumed to be
162
available. Note that there is an ambiguity in specifying the beat period T in (8.30), because the aortic blood
flow signal is not strictly an impulse. Therefore, a few alternative specifications for T was considered, from
which it was empirically observed that the model-based blood pressure calibration algorithm is able to estimate the systolic blood pressure if T is specified as the beat cycle period (see the left plot in Fig. 8.15),
while it is able to estimate the systolic mean blood pressure (which is defined as the mean blood pressure during the systole) if T is specified as the diastolic period (see the right plot in Fig. 8.15). The systolic blood
pressure estimation statistics based upon 950 distinct beat cycles is summarized in Table 8.4 for the radial and
the aortic blood pressures, which shows that given the diastolic blood pressure, the model-based blood pressure calibration algorithm is capable of providing systolic blood pressure with reasonable accuracy solely
based on the time-related quantities in the upper-limb peripheral blood pressure measurement.
Table 8.4. Systolic and systolic mean blood pressure estimation statistics.
Radial SBP
Radial SMBP
Aortic SBP
Aortic SMBP
Error [mmHg]
3.8 +/- 6.8
1.4 +/- 4.1
1.8 +/- 11.7
4.3 +/- 7.1
Normalized Error [%]
3.1 +/- 5.1
1.3 +/- 3.6
0.6 +/- 9.6
4.7 +/- 6.2
The examination of the persistent excitation condition for the 83 segments of the radial blood pressure
data showed that the persistent excitation condition was satisfied for all the 83 segments of data. The persistent excitation analysis also revealed that the well-posedness of the cardiovascular wave propagation dynamics
identification problem (8.26), ie. the degree of persistent excitation, is closely related to the heart rate frequency, FHR (which represents the characteristics of the excitation signal), and the frequency FG, at which
IG1 (jco)I attains its maximum (which represents the underlying physiologic condition of the cardiovascular
system), where G, (z) is the aortic-to-radial cardiovascular wave propagation dynamics: the smaller
163
F,R -FG I, the better the condition number of *D*,as shown in Fig. 8.16. Note that this finding is the 1sensor equivalent of the 2-sensor persistent excitation analysis shown in Chapter 6 (see Fig. 6.10). Therefore,
the well-posedness of the cardiovascular wave propagation dynamics identification problem hinges upon
FHR - FG, . In other words, the quality of identifying the cardiovascular wave propagation dynamics hinges
upon how well the frequency range around FG is excited by the regressor signal. This suggests that care
must be taken when we interpret the identified cardiovascular wave propagation dynamics associated with
large FR - FG, . It is also important to note that this correlation between the level of persistent excitation
and IFHR - F I is independent of the sampling frequency in the sense that it is consistent over a range of
sampling frequency
52E
2
z
o 1.5
1
I0
4•
200
300
400
500
600
700
800
900
1000
200
300
I
400
I
500
600
I
700
I
800
I
900
1000
I
IF--F,-I
:I 10
C
0- ----
I--
----• .....
-
-
------
-
A_
I
I
I
I
I
I
I
I
I
200
300
400
500
600
700
800
900
1000
Time [sec]
Fig. 8.16. Persistent excitation as a function of IFHR - F
164
I at 500Hz sampling frequency
8.5.2. Full-Scale Human Cardiovascular Simulator Data
Fig. 8.17 shows the results from applying the non-invasive 1-sensor central cardiovascular monitoring
methodology to the simulation-based human subject data, where the reconstructed aortic blood pressure signals are compared with their true counterpart. Throughout the eight human subject models, the aortic blood
pressure signal could be accurately reconstructed. Especially scrutinizing the end-diastolic portion of the true
as well as the reconstructed aortic blood pressure signals illustrates that the system order estimation algorithm
is able to provide reliable estimate of the aortic-to-radial pulse transit time.
125
----- TruAortic BP,
120
S
..-
.--
--
I
, IRecovered Aortic BP
-t--- TrueUlnar BP
_
-
120
-L
I
I
I
I
I
1L
I ,,
L_
115
110
E 110
---
4i-
-1-
-- -
---7-- ----
-
I-
--
--
--
S105
L
E 100
I
1
-'I ,
I
-I
I
-
1
I
"-
'
1 -- - r-
-
I
-
I
I
J
I
I
I
L
-L
I
I
a-
85
2.8
2.9
3
3.1
3.2
3.3
Time [sec]
3.4
3.5
3.86
W)1
3.7
0
8
85
--
--
80^
90
95
True
100
Aortic
105
BP
110
[mmHg]
(a) Subject # 1
----105
- -- -- - - - - 'I
I
----
True Aortic BP
RecoweredAortic BP
True UInarBP
100
_
95
----I--
. I - -_
..
I
I
- -_
- -
I
85
80
- ,T"
lI ,-
- - -- - -
- - -"•
4- - -
- - -I
'1;
:
',--
t
i
i
4.4
4.86
,L.
75
70
3.6
3.8
4
4.2
Time [sec]
True Aortic BP [mmHg]
(b) Subject # 2
165
115
1
120 - - -
- -
--
I
- - 4-
I
-+
S---- True Aortic BP
RecoveredAortic BP
---TrueUnar BP
--I
I
110 ----
I
I
I
I
I
I
t
I
I
I
I
I ,/'
i----±---±-----II
II
I
II
,/
+---+---+---+---+---
115
110
E
105
100
- -
-
- - ---
-
-- -- -
-
--
--
--
T,-- --
,--
--- -E
105-----
--
----
'
E
L
L"
S100
II --
-
I-
0
+---.
I•
"
I•
-+_
--
-
.-
-
85
-T
I
I
,-_--
I
I
--__-II
III
I
I
I
I
i
I
I
._•
85
I-~__
--.-.--
II
I
I''o"
I
i
Soo
+-----------------
---
--
II
f
II
•
II
I
90
--
---
--
i
I
I
I
I-+--
----
II
I
I
4
-
, I
I
I
I
I
I
I
I
I
I
I
I
85
90
105
110
80
2.6
2.7
2.8
2.9
3
3.1
3.2
Time [sec]
3.3
3.4
3.5
3.6
80
95
100
True Aotic BP [mmHg]
115
(c) Subject # 3
011V
I
110-
--
-
I
I True Aortic BP
Recovered Aortic BP
True Ulnar BP
--
I
105
-l-
I
I
i
-I
I
I
-
I
I
I
+---
-
I
I
-----
I
I
- -
I
I
100
100
E
----
L
P95
L.
I
E 90-----
/
S80-
~-- I---
- - ----
-
----
I--~__1
-
-__--__
85
7
-
-
--
---
'so 80
-
-
__J.
-t--L
L..1
------
.
-I-J
I _•__•,•-
I
L
L
I
I
-
L
- --
_L
-
_
I
75
70
-
85
-- I-,"I
2.8
3
3.2
3.4
Time [sec]
3.86
3.8
4
0
65
4-I I
70
75
--
T--
I
I
I
-7
I
80
85
90
95
True Aortic BP [mmHg]
1
I
100
105
110
(d) Subject # 4
010
120lU
----- True Aortic BP
115
-
-L I-
Recovered Aortic BP
True Ulnar BP
- - - I ---
-
105-
-
--
110
Ill105
------------I
I
0
E 100
S95
2.8
I
-
-
J--
-
------
-
T
-
-
--
T---r----1---
'
----- -
----
- ---90
an
--
S05----I-1--l-- I
95
85
1-
E 100---I
--
85I----
-I--
---
-------
-J
I
3
•
II
3.2
I
3.4
Time [sec]
3.8
80
3.8
80
(e) Subject # 5
166
85
0S
100
True Aortic BP [mmHg]
90
10511
110
[
I
I
I",
I-
I
I
I
80
-
-
T I
lcU I
----- True Aortic BP
I
I
I
T
-
--
Recovred Aortic BP
True Ulnar BP
---
1,
---
1
I
I
,--r
.\
I
i,
I - -l
- I - -L - - I - -
---
--
--- 4
I'Iv~
- T
--I ----r --- r,I --
80
I
I
3.5
1,1
-L
.
I.
Xi
-,L.•
---
I
I
I
I
i
T-.-- %
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
3.8
3.7
3.8
3.0
4
4.1
Time [sec]
I
I
1
I1
4.2
4.3
4.4
4.5
TrueAorticBP [mmHg]
(f)Subject # 6
105-
S----
- -
-
--
- -
S
100
--L--
I
I
-- TrueAortic BP
--Recoered Aortic BP
.......
TrueUlnarBP
I
--
--
I
95
-
r-.•
T
T
r-.rr - -r- T -
+T
I
Si
S85 - --
1
.
I
II---I
i
L.
L --I
I
I
- -
-
I
I
T
.
I
I
~CP
I
i75
I
75
--
70
I
I----
80
- - --
3.3
I
-T-I
l
--
-T- - -
TT--
II
-- 4 - -
65
3.2
I
I
-
-
I
3.4
3.5
3.6
3.7
3.8
Time [sec]
3.9
4
4.1
m·
w--
o0
4.2
70
05
75
80
85
True AorticBP [mmHg]
90
95
100
(g) Subject # 7
110
120
----- TrueAorticBP
SI Recored Aortic BP
I
------
L
105 - -I- - -1100
L----.---
- -I
-
- -
- - + - -
-I- -- - -
-
A
so
I f lI
fi
- -
-- -I-
--
--
-
-
- -- -
t I L
--,- - -,- - n - -
L-- -
- -- -
r---
- ---
75
- IV1
I
I
I
3
3.2
3.4
I
I
3.6
Time [sec]
I-
I
I
I
3.8
4
S-
70
85
/
4.2
6
(h) Subject # 8
Fig. 8.17. True versus reconstructed aortic blood pressures.
167
-
--
-
--
- -- '---I-----+---II
865
-i
70
75
i
i
i
80
85
90
95
TrueAorticBP [mmHg]
1---1---
i
100 105 110
8.5.3. Experimental Human Subject Data
Finally the non-invasive 1-sensor central cardiovascular monitoring methodology was applied to the experimental human subject data to assess its efficacy for human subjects in real clinical practices. Specifically
the model-based systolic blood pressure calibration algorithm was tested using the experimental data obtained
in the Wearable Sensors Laboratory at the Massachusetts Institute of Technology while the cardiovascular
system identification algorithm was tested using the experimental data obtained in the Cardiac Catheterization
Laboratory at the Massachusetts General Hospital. Note from Fig. 8.4 that these two algorithms can be assessed independently
L24U
I
220
I
I
------
------
I
200
-
- T------
I
I
l
I
-----
----
1
---------------I
II
I
SI
I
I
I
-180
-
_o-
I-
--------
E
E 160
O 140
t
E
----
II
I
I
I
r
I
----
--------
--
120
----
-
"1 ---
-
f----r----
w 100
----
4----
----
----
f----
----
80
60
,r
An
40
0
I
I
I
60
80
100
I
I
I
120
140
160
180
Measured SBP [mmHg]
I
I
200
220
240
Fig. 8.18. True versus estimated finger systolic blood pressures for 15 human subjects.
First, the true versus the estimated systolic blood pressures at the middle fingers for 15 human subjects
are compared with each other in Fig. 8.18, and the corresponding statistics is summarized in Table 8.5. The
time constant A was identified from the end-diastolic portion of the non-invasive finger blood pressure
168
measurement, the beat cycle period was measured directly from the non-invasive finger blood pressure measurement, and the diastolic blood pressure was assumed to be available. The results strongly suggest that the
model-based systolic blood pressure calibration algorithm can be implemented for clinical practice, using the
non-invasive upper-limb peripheral blood pressure signal (which is, in theory, inaccurate compared with the
invasive intra-arterial blood pressure signal).
Table 8.5. Human non-invasive-measurement-based systolic blood pressure estimation statistics.
Subject
Error [mmHg]
Normalized Error [/o]
Age
1M
4.4 +/- 2.8
2.7 +/- 2.0
3X
2F
5.9 +/- 10.9
5.0 +/- 8.7
3X
3M
0.1 +/- 7.9
0.4 +/- 5.1
3X
4M
7.7 +/- 11.5
4.7 +/- 6.5
2X
5M
2.3 +/- 8.5
2.1 +/- 6.9
2X
6M
7.1 +/- 6.1
6.0 +/- 5.1
3X
7M
17.2 +/- 15.5
11.8 +/- 10.9
3X
8M
9.9 +/- 6.7
9.5 +/- 6.4
2X
9M
0.1 +/- 4.3
0.1 +/- 3.0
3X
10M
10.3 +/- 3.5
8.0 +/- 2.8
3X
11F
0.5 +/- 2.0
0.6 +/- 2.1
3X
12M
1.0 +/- 2.5
0.9 +/- 2.1
3X
13M
9.0 +/- 4.9
6.5 +/- 3.6
3X
14F
12.6 +/- 6.0
10.1 +/- 5.0
6X
15F
0.6 +/- 5.2
0.5 +/- 4.5
5X
169
Remark
Pregnancy
The results of reconstructing the aortic blood pressure signals from non-invasive finger blood pressure
measurements are shown in Fig. 8.19 for the 2 subjects recruited from the Cardiac Catheterization Laboratory
at the Massachusetts General Hospital, which strongly suggests the potential of the non-invasive 1-sensor
central cardiovascular monitoring methodology in real clinical setting First of all, the reconstructed aortic
blood pressure signals are very close in morphology to their true counterparts. Besides, scrutinizing the true
versus the reconstructed aortic blood pressure signals as well as the non-invasive finger blood pressure signals
indicates that the aortic-to-finger pulse transit time can also be reliably estimated, which supports the validity
of the system order estimation algorithm proposed in the thesis for real human subjects under non-invasive
measurement environment.
The experimental results also illustrates that the non-invasive 1-sensor central cardiovascular monitoring
methodology proposed in this thesis can be very effective in estimating the aortic systolic blood pressure. The
results summarized in Table 8.6 shows that the aortic systolic blood pressures offered by the methodology
were highly accurate, compared with their finger counterparts. For subject # 1, the discrepancy between the
true and the reconstructed systolic blood pressures is 2.5mmHg, which is 88% reduction against the
13mmHg discrepancy between the true aortic and the finger systolic blood pressures. For subject # 2, the discrepancy between the true and the reconstructed systolic blood pressures is 7.4mmHg, which is 87% reduction against the 55.6mmHg discrepancy between the true aortic and the finger systolic blood pressures.
Table 8.6. True versus estimated aortic systolic blood pressures.
Subject
Estimated [mmHg]
Finger [mmHg]
(Error [mmHgW
(Error [mmHgl
True [mmHg]
1F
135.0
137.5 (2.5)
148.0 (13)
2M
148.6
156.0 (7.4)
204.2 (55.4)
170
I
I
I
I
I
I
I
L
140
130
-
J
---
' 120
E
E
I 110
--" -
I
I
I
----- True Aortic BP
-I
Recovered Aortic BP
----....... Finapres Finger BP
-
150
--------
---I
r--
Il---C--- I
--
---
II +---
-
---
I --- I,I---
I -4 -" -
-
100
90
I
I
S
80
--
"-t-----I--r----t-t
I
4.7
4.75
4.8
4.85
4.9
4.95
5
Time [sec]
-.--- - - --
I
I
I
5.05
5.1
5.15
I-
5.2
5.25
(a)Subject # 1
L2U
-
S
200
I----- True AorticBP
Recovred Aortic BP
I
I i
-"-*-
I
1
180
U
I
Finapres Finger BP
T
Iiir
I
i
I
I
I"
I
I
I
-- I
I
160
---
E
S140
a120
---
- r-- -
---
--I
I
-
i I!
---
I-
---------I
I--
--
I
I
I
i
-"--
I
I
iI
I
I
L
Ir
I
Ir-
----
II
!
II
100
II
I
I
80
t -----
I
-
LLt-
rfN
1.8
1.85
1.9
1.95
2
2.05 2.1
Time [sec]
(b) Subject #2
Fig. 8.19. True versus reconstructed aortic blood pressures.
171
2.15
2.2
2.25
2.3
2.35
In summary the experimental results from the real human subject testing suggest the proof-of-principle
of the non-invasive 1-sensor central cardiovascular monitoring methodology in real clinical practices.
8.6. Summary
Towards the real clinical applications, this chapter extended the 2-sensor central cardiovascular monitoring based on two distinct, direct invasive blood pressure measurements to the 1-sensor central cardiovascular
monitoring based on a non-invasive blood pressure measurement. Specifically this chapter developed a methodology to identify the cardiovascular wave propagation dynamics, reconstruct the aortic blood pressure signal, and estimate both peripheral and aortic systolic blood pressures from a single non-invasive extremity
measurement. Its rigorous evaluation upon experimental swine subjects, simulation-based human subject
models, and experimental human subjects strongly supports the efficacy of the non-invasive 1-sensor central
cardiovascular monitoring by demonstrating that the cardiovascular wave propagation dynamics can be well
identified, the aortic blood pressure signal can be accurately reconstructed, and the systolic blood pressure
can be calibrated with reasonable accuracy solely based on a single non-invasive upper-limb blood pressure
measurement without any a priori knowledge on the empirical and/or population-based cardiovascular wave
propagation dynamics, e.g. a predetermined or a generalized transfer function.
Despite the promising results obtained in this thesis, its direct comparison with the competing empirical,
population-based approach was not feasible due to the limited amount of data available for this thesis. The
methodology still needs to be investigated and compared with the empirical and/or population-based approach over larger human subject population under wide-ranging physiologic conditions.
172
Chapter 9. Conclusions
This thesis presented a new system identification approach to non-invasive central cardiovascular monitoring, which is capable of identifying the cardiovascular wave propagation dynamics and reconstructing the
aortic blood pressure and flow signals from extremity blood pressure measurements.
9.1. Summary of Thesis Contributions
1. Blind identification methodology for a class of 2-channel IIR and Wiener systems was developed
and analyzed. Specifically blind identifiability conditions and the associated blind identification algorithms for 2-channel wave propagation systems were developed. It was shown that the sparseness
structure e.g. the separations in the wave propagation dynamics can be exploited for identifying this
class of 2-channel systems. It was also shown that the blind identifiability conditions can be
achieved in many real-world applications by appropriate selection of channel lengths, sensor locations and sampling frequency which are the specifications that the system design can exploit for
blind identifiability
2. New input signal de-convolution filter design algorithm for general multi-channel IIR and Wiener
systems was developed and analyzed by exploiting the coprimeness property of the 2-channel dy
namics identified from the blind identification methodology It was shown that the new algorithm
guarantees the existence of a de-convolution filter.
3. The blind identification and input signal de-convolution algorithm for 2-channel IIR/Wiener wave
propagation systems was used to implement the 2-sensor central cardiovascular monitoring, which
was shown to be able to identify the cardiovascular wave propagation dynamics and reconstruct the
aortic signals very accurately from blood pressure measurements at two distinct extremity locations.
4. The 2-sensor central cardiovascular monitoring based on invasive blood pressure measurements was
173
extended to non-invasive 1-sensor central cardiovascular monitoring towards real clinical applications, opening up a new potential direction for wearable central cardiovascular monitoring. It was
shown to be able to identify the aortic-to-radial cardiovascular wave propagation dynamics and reconstruct the aortic blood pressure signal very accurately solely based on a single non-invasive blood
pressure measurement at an upper-limb extremity location.
9.2. Future Directions for Research
1. Developing and analyzing the blind identification methodology for 2-channel Hammerstein systems
is a challenging future direction for technical research. In contrast to their Wiener counterparts, the
blind identification formulation for the 2-channel Hammerstein systems cannot be viewed as the
multi-variable extension of the 2-channel IIR formulation. Furthermore, it generally results in the
explosion of terms that are tough to handle. By virtue of its frequent use in modeling real physical
processes, developing blind identification methodology for 2-channel Hammerstein systems will be
highly rewarded.
2. The 2-sensor central cardiovascular monitoring developed in this thesis is built upon invasive blood
pressure measurements. Noting that many of the sensor modalities which are capable of measuring
the biological signals non-invasively can be mathematically characterized by a combination of linear
dynamic system and static nonlinear function, current invasive 2-sensor central cardiovascular monitoring can further be explored for its extension to non-invasive 2-sensor central cardiovascular
monitoring, by exploiting the blind identification methodology for 2-channel Wiener systems developed in this thesis. In order for this end, research endeavors on the analysis and the parametric
modeling of the existing non-invasive sensor modalities are necessary
3. It is of interest to explore new non-invasive sensor modalities for measuring biological signals that
have potentials for central cardiovascular monitoring, e.g. blood pressure and flow signals at the ex174
tremity locations. In particular, a promising future direction will be the sensor fusion using optical
photoplethysmographic and the ultrasound sensor modalities for estimating the blood pressure signal at an extremity location. Our preliminary investigation suggests that the blood volume and the
blood flow velocity measurements provided by the photoplethysmographic and the ultrasound sensors may be effectively combined to reconstruct the blood pressure signal at the corresponding extremity location, which can then be used for central cardiovascular monitoring
4. There can be plenty of opportunities to improve the non-invasive 1-sensor central cardiovascular
monitoring developed in this thesis. Despite its clinical promise and potential, the methodology developed in this thesis is definitely the first step towards the central cardiovascular monitoring based
on a single peripheral sensor. Especially the system order estimation algorithm developed in this
thesis is built upon a heuristics derived from the physical and the physiologic understanding on the
blood pressure wave propagation and reflection phenomena in the aortic-to-radial cardiovascular
channel, and there should be room for improving its accuracy and reliability via systematic mathematical treatment. Besides, the model-based systolic blood pressure calibration algorithm may be
improved by considering models with added complexity (e.g. transmission line models) to better describe the dynamics of the cardiovascular system.
5. The clinical utility of the new central cardiovascular monitoring methodology needs to be identified
and explored. In essence, the methodology opened up a new possibility of utilizing the aortic blood
pressure and flow signals in trying to assess the cardiovascular health. This thesis demonstrated the
accuracy of some basic physiologic measures directly available from the identified cardiovascular
wave propagation dynamics (e.g. aortic-to-peripheral pulse transit times) and the reconstructed aortic signals (e.g systolic blood pressure and ejection duration). However, potential clinical application
of the methodology for central cardiovascular monitoring and diagnostics still abound, and many of
them are yet to be rigorously explored.
175
Appendix A. Equivalence between SVD and Least-Squares
Estimates
Consider (2.39):
L[,
(A1)
(n) - Y2(-N)2
-P-l
L
where dividing the vector p
iby
,n2+m
yields
(1)
(A-2)
;e[ui -vl;t]o ,
f,-i2][
which isequivalent to
7Y
(n+n
2+M")
I=
i
A
-Oq.
(A3)
y (n+ +m
1 -N)
Using the singular value decomposition [iY - 2]= UVT and (A.1), we have
•
T
I'1)
-Ty41)
4
=
= V-T)
V
T
,
(A.4)
T4
or equivalently
pV = VETE ,
where
(A.5)
T£ can be viewed as a diagonal matrix having the eigenvalues of Y as its diagonal elements. As-
suming q satisfying (A.3) isunique and non-trivial, the null space of [y1) -0] isone dimensional, which
in turn implies that there is only one zero eigenvalue (which is the smallest) associated with T . Therefore, 0
should satisfy
S[1L.T ''
•
T)
'T '
Jl
176
whose solution is identical to the least-squares solution (2.51). Indeed, each of the rows in (A.6) turns out to
be a least-squares equation:
-
=0,
-0
OT0 TO-()
(A.7a)
= 0.
(A.7b)
177
Appendix B. Wiener Two-Segment Transmission Line Representation of Aortic-to-Femoral Cardiovascular Channel
Dynamics
Assume that both the terminal load impedances used in the model (see Fig. 7.3) have the modified
Windkessel representations shown in Fig. 7.1. The blood pressure wave propagation dynamics G22 (s) in the
femoral artery i.e. distal transmission line, which relates abdominal aortic blood pressure Ps (n) and the intermediate signal X2 (n) in Fig. 7.3, is given by:
G1+22
P, (s)
where
a22
where
r22 (S)
eS=' + e-•S
(SS))
(s)
22
,
22
2R0 222RO22
C22 (R+0 R
b22
22 + R22)
22 (S)
-422
Zt22 (s)+•Zc22
e22s
(B.1)
s+a22 +b 22
b22 -2s
s + a 22 +
2R022 C 22 R22
(R22 + R22 )
and
(B.2)
-2,
S+ 22
which is the reflection coefficient associated with the distal transmission line. Similarly, the blood pressure
wave propagation dynamics G21 (s) in the thoracic and the abdominal aorta, ie. proximal transmission line,
which relates the ascending aortic blood pressure Pa (n) and the abdominal aortic blood pressure P,(n), is
given by:
SG21 (s)
1+r21 (s)
Pa()(s)
e"2s +e2s'r2, (S)
where r2 1(s)= Z 2 1(S)-
21
zt21 (S)
+c21
(B.3)
is the reflection coefficient of the proximal transmission line. Therefore, in
order to derive the dynamics of the proximal transmission line i.e. the thoracic and the abdominal aorta, its
terminal load impedance Zt2 1(s) needs to be evaluated. Note that Zt2 1 (S) is given by the parallel contribution of the distal transmission line's input impedance, Zi22 (s), and the terminal load impedance describing
the lumped effects of the splanchnic organs, Z 21(
R2 1(R 21C2 +1 . Zi2 2 (S)i given by[49,50]:
(R21 +R2 1)C21S+1
178
Zi22 (s) &Zc22
er( s
s
+ F22 (s) e-22
-
]F 22 (s)e
er22s
22s
= Zc22
S + a 22 + b 22
e- 2
r22s
2-2
b 22
S + a 22 -
s
R22
=
a 2 2 - b2 2 s +
a 2 2 +b
22 + b22 e
- 2
r22
(B.4)
.
s + a 2 2 - b 22 e r2s
-2
22
Accordingly
a-1
Z211
t21
1
Zsl
Zs21
2
e- 2
a 2 2 +b 2 2 s+a
22
-b22 - 2 r22
22
+ 2 e
1
21
R22 a22 -b 22 st+a 22 +b22-2R22
(B.5)
(Ro21 +R 2 1 )C21S +1
(R 0 2 1C 2 1s+1)
1
and using the physically relevant assumption that the wave reflection coefficient is zero at infinite frequency
i.e.
Zc21 = Zt21 (S = joo),
1
1
a2 2 + b 2 2
R22 a22 - b
22
R02 1 + R21
R 21R02 1
(B.6)
Substituting (B.5) and (B.6) into (B.3) yields the dynamics of the proximal transmission line:
G21 ()
(B.7a)
N 21 (s)
D21 (s)
with
N21 (s) ~e-21S [s2 + (a 22 +a 2 1 + b2
2 C21 )s
+ a22 (a 2 1 +2 + a 2 C21 )+
b22
-2
e r22s + b22 (a 2 1 + b
a2 C21 )e-222],
(B.7b)
D 21 (s)
S2 +(a 22 + a 21
+b2 se
-2
s
2+
2 1)S + a22 (a 21 + a22 21)
+ b22 d 21se
-2
r22s +a 22 b21
e - 2r
s
+ a 2 b 22e - 2 rs +b 22 (1-d 21 )se - 2(
+r)s + 22 (b21+a
2
)
- 2 ( rr +
)
22
(B.7c)
where a 2
a 22 +b 22
a22 -b 22
a21l K, a2
K34
b
+ K4
IC,+/C-)
K[2
,a K3K4
K1 + K2
+ K4 ]
C21
K3
a2
K3K4 + C4
KI +
,d21
2
4
a2
3K4 + K4
KIC+ K2
(B.7d)
with
il
(2R21 + R21) R22
K2
R21R22
K3 A 2RK21R21, K4
179
A 2(R21+R21
21R22C21.
(B.7e)
References
[1] American Heart Association, Heart disease and stroke statistics - 2007 update. Dallas, Texas: American
Heart Association, 2007.
[2] Q. Li and G. Belz, "Systolic time intervals in clinical pharmacology," European Journal of Clinical Pharmacology, voL 44, no. 5, pp. 415-421, 1993.
[3] H.Boudoulas, "Systolic time intervals," European Heart Journal, voL 11, Supplement I, pp. 93-104, 1990.
[4] Z. Lu and R Mukkamala, "Continuous cardiac output monitoring in humans by invasive and noninvasive
peripheral blood pressure waveform analysis," Journal of Applied Physiology voL 101, no. 2,pp. 598-608,
2006.
[5] J.Jansen, J. Schreuder, J.Mulier, N.Smith, J. Settels, and K. Wesseling, "A comparison of cardiac output
derived from the arterial pressure wave against thermodilution in cardiac surgery patients," British Journal of Anesthesia, voL 87, no. 2, pp. 212-222, 2001.
[6] C.Cerutti, M. Gustin, P. Molino, and C paultre, "Beat-to-beat stroke volume estimation from aortic
pressure waveform in conscious rats: comparison of models," American Journal of Physiology vol.281,
no. 3, pp.1148-1155, 2001.
[7] N.Linton and R Linton, "Estimation of changes in cardiac output from the arterial blood pressure
waveform in the upper limb," British Journal of Anesthesia, voL 86, no. 4, pp. 486-496, 2001.
[8] J. Redling, and M.Akay "Noninvasive cardiac output estimation: a preliminary study",' Biological Cybernetics, vol. 77, no. 2, pp. 111-122, 1997.
[9] K. Wesseling, J.Jansen, J.Settels, and J.Schreuder, "Computation of aortic flow from pressure in humans
using a nonlinear, three-element model," Journal of Applied Physiology, voL 74, no. 5, pp. 2566-2573,
1993.
[10] W Welkowitz, Q. Cui, Y Qi, and J. Kostis, "Noninvasive estimation of cardiac output," IEEE Transac180
tions on Biomedical Engineering, vol. 38, no. 11, pp. 1100-1105, 1991.
[11] C. Quick, D. Berger, D. Hettrick, and A. Noordergraaf, "True arterial system compliance estimated from
apparent arterial compliance," Annals of Biomedical Engineering, vol. 28, no. 3, pp. 291-301, 2000.
[12] C. Quick, D. Berger, and A. Noordergraaf, "Apparent arterial compliance," American Journal of Physiology, vol. 274, no. 4, pp. 1393-1403, 1998.
[13] N. Stergiopulos,
J. Meister, and N. Westerhof,
"Evaluation of methods for estimation of total arterial
compliance," American Journal of Physioogy, vol. 268, no. 4, pp. 1540-1548, 1995.
[14] R Marcus, C Korcarz, G. McCray A. Neumann, M. Murphy, K. Borow, L. Weinert, J. Bednarz, D.
Gretler, K. Spencer, P. Sareli, and R. Lang, "Noninvasive method for determination of arterial compliance using Doppler echocardiography and subclavian pulse tracings," Circulation, vol. 89, no. 6, pp.
2688-2699, 1994.
[15] G. Toorop, N. Westerhof, and G. Elzinga, "Beat-to-beat estimation of peripheral resistance and arterial
compliance during pressure transients," American Journal of Physiology vol. 252, no. 6, pp.1275-12 83,
1987.
[16] Z. Liu, K. Brin, and E Yin, "Estimation of total arterial compliance: an improved method and evaluation
of current methods," American Journal of Physiology; vol. 251, no. 3, pp. 588-600, 1986.
[17] X. Xiao, E. Ozawa, Y Huang, and R Kamm, "Model-based assessment of cardiovascular health from
noninvasive measurements," Annals of Biomedical Engineering, vol. 30, no. 5, pp. 612-623, 2002.
[18] R Mukkamala, K. Toska, and R Cohen, "Noninvasive identification of the total peripheral resistance
baroreflex," American Journal of Physiology vol. 284, no. 3, pp. 947-959, 2003.
[19] C Lucas, B. Wilcox, B. Ha, and G. Henry; "Comparison of time domain algorithms for estimating aortic
characteristic impedance in humans," IEEE Transactions on Biomedical Engineering, vol. 35, no. 1, pp.
62-68, 1988.
[20] J. Li, "Time domain resolution of forward and reflected waves in the aorta," IEEE Transactions on
181
Biomedical Engineering, voL 33, no. 8, pp. 783-785, 1986.
[21] W Nichols and M. O'Rourke, McDonald's blood flow in arteries. London, United Kingdom Arnold,
1998.
[22] M. Karamanoglu, D. Gallagher, A. Avolio, and M. O'Rourke, "Pressure wave propagation in a multibranched model of the human upper limb," American Journal of Physiology voL 269, no. 4, pp. 13631369, 1995.
[23] M. Karamanoglu, D. Gallagher, A. Avolio, and M. O'Rourke, "Functional origin of reflected pressure
waves in a multibranched model of the human arterial system," American Journal of Physiology voL 267,
no. 5,pp. 1681-1688, 1994.
[24] D. Gallagher, A. Adji, and M. O'Rourke, "Validation of the transfer function technique for generating
central from peripheral upper limb pressure waveform," American Journal of Hypertension, voL 17, no.
11, pp. 1059-1067, 2004.
[25] B.Fetics, E. Nevo, C-H Chen, and D. Kass, "Parametric model derivation of transfer function for noninvasive estimation of aortic pressure by radial tonometry," IEEE Transactions on Biomedical Engineering, voL 46, no. 6, pp. 698-706, 1999.
[26] M. Karamanoglu and M. Feneley "Derivation of the ascending aortic-carotid pressure transfer function
with an arterial model," American Journal of Physiology, voL 271, no. 6, pp. 2399-2404, 1996.
[27] W Stok, B. Westerhof, and J.Karemaker, "Changes in finger-aorta pressure transfer function during and
after exercise," Journal of Applied Physiology vol 101, no. 4, pp. 1207-1214, 2006.
[28] S. Hope, D. Tay I. Meredith, and J. Cameron, "Use of arterial transfer functions for the derivation of
aortic waveform characteristics," Journal of Hypertension, voL 21, no. 7, pp. 1299-1305, 2003.
[29] S.Millasseau, S.Patel, S.Redwood, J. Ritter, and P.Chowienczyk, "Pressure wave reflection assessed from
the peripheral pulse," Hypertension, vol 41, no. 5,pp. 1016-1020, 2003.
[30] P.Segers, S.Carlier, A. Pasquet, S.Rabben, L. Hellevik, E. Remme, T. De Backer, J. De Sutter, J. Thomas,
182
and V Verdonck, "Individualizing the aorto-radial pressure transfer function: feasibility of a model-based
approach," American Journal of Physiology, voL 279, no. 2, pp. 542-549, 2000.
[31] J.O. Hahn, A. Reisner, H.Asada, "Identification of multi-channel cardiovascular system using dual-pole
Laguerre basis functions for assessment of aortic flow and TPR," Proc. ASME International Mechanical
Engineering Congress and Exposition, Seattle, USA, IMECE2007-41186, 2007.
[32] J.O. Hahn, A. Reisner, and H Asada, "Sensitivity and variance analysis of arterial pressure transfer dynamics estimated from adaptive multi-channel system identification," Proc. American Control Conference, New York, USA, pp. 613-618, 2007.
[33] G. Swamy Q. Ling, T. Li, and R Mukkamala, "Blind identification of the aortic pressure waveform from
multiple peripheral artery pressure waveforms," American Journal of Physiology voL 292, no. 5, pp.
2257-2264, 2007.
[34] J.O. Hahn, A. Reisner, H. Hojman, and H.Asada, "Reconstruction of central aortic pressure waveform
using adaptive multi-channel identification," Proc. IEEE Engineering in Medicine and Biology Conference, New York, USA, pp. 3377-3380, 2006.
Asada, "A blind approach to reconstruction of aortic blood pressure wave[35] JO. Hahn, A.Reisner, and HIform using gray-box identification of multiple pressure transfer channels," Proc. American Control Conference, Minneapolis, USA, pp. 3415 -3420, 2006.
[36] D. McCombie, A. Reisner, and H Asada, "Laguerre model blind system identification: cardiovascular
dynamics estimated from multiple peripheral circulatory signals," IEEE Transactions on Biomedical Engineering, vol 52, no. 11, pp. 1889-1901, 2005.
[37] J.O. Hahn, D. McCombie, A. Reisner, H. Asada, H Hojman, R Mukkamala, "Adaptive left ventricular
ejection time estimation using multiple peripheral pressure waveforms," Proc. IEEE Engineering in
Medicine and Biology Conference, Shanghai, China, pp. 2383-2386, 2005.
[38] Y Zhang and H Asada, "Blind system identification of noncoprime multichannel systems and its appli183
cation to noninvasive cardiovascular monitoring," ASME Journal of Dynamic Systems, Measurement
and Control, vol 126, no. 4, pp. 834-847, 2004.
[39] M. Radenkovic, T. Bose, and Z. Zhang, "Self-tuning blind identification and equalization of IIR channels," EURASIP Journal on Applied Signal Processing, vol. 2003, no. 9, pp. 930-937, 2003.
[40] E. Bai and M. Fu, "Blind system identification and channel equalization of IIR systems without statistical
information," IEEE Transactions on Signal Processing, vol 47, no. 7, pp. 1910-1921, 1999.
[41] G. Xu, H. Liu, L.Tong, and T. Kailath, "A least-squares approach to blind channel identification," IEEE
Transactions on Signal Processing, vol. 43, no. 12, pp. 2982-2993, 1995.
[42] MIGurelli and C Nikias, "EVAMV An eigenvector-based algorithm for multichannel blind deconvolution
of input colored signals," IEEE Transactions on Signal Processing, vol 43, no. 1, pp. 134-149, 1995.
[43] E. Ozawa, K. Bottom, X.Xiao, and R. Kamm, "Numerical simulation of enhanced external counterpulsation," Annals of Biomedical Engineering, vol 29, no. 4, pp. 284 -297 , April 2001.
[44] S.Shroff, D. Berger, C Korcarz, R Lang, R Marcus, and D. Miller, "Physiological relevance of T-tube
model parameters with emphasis on arterial compliance," American Journal of Physiology vol 369, no. 1,
pp. 365-374, July 1995.
[45] K. Campbell, R Burattini, D. Bell, R Kirkpatrick, and G. Knowlen, "Time-domain formulation of
asymmetric T-tube model of arterial system," American Journal of Physiology, vol. 258, no. 6, pp. 17611774, June 1990.
[46] R Burattini and K. Campbell, "Modified asymmetric T-tube model to infer arterial wave reflection at the
aortic root," IEEE Transactions on Biomedical Engineering, vol 36, no. 8,pp. 805-814, August 1989.
[47] Z. Liu, E Shen, and E Yin, "Impedance of arterial system simulated by viscoelastic t tubes terminated in
windkessels," American Journal of Physiology vol 256, no. 4, pp. 1087-1099, April 1989.
[48] A. Avolio, "Multi-branched model of the human arterial system," Medical and Biological Engineering
and Computing, vol 18, no. 6, pp. 709-718, November 1980.
184
[49] D. Blackstock, Fundamentals of physical acoustics. New York, NY: John Wiley & Sons, 2000.
[50] J. Kong, Electromagnetic wave theory Cambridge, MA: EMW Publishing, 2000.
[51] J. Doyle, B.Francis, and A. Tannenbaum, Feedback control theory New York, NY: Macmillan Publishing,
1992.
[52] L. Ljung, System identification theoryfor the user. Le River, NJ: Prentice-Hall, 1999.
[53] L. Ljung, "Convergence analysis of parametric identification methods," IEEE Transactions on Automatic Control, vol. 23, no. 5,pp. 770-783, 1978.
[54] L. Ljung and P. Caines, "Asymptotic normality of prediction error estimators for approximate system
models," Stochastics, voL 3,no. 1-4, pp. 29-46, 1979.
[55] B.Wahlberg, "System identification using Laguerre models," IEEE Transactions on Automatic Control,
vol. 36, no. 5, pp. 551-562, 1991.
[56] K. Hirata, M. kawakami, and M. O'Rourke, "Pulse wave analysis and pulse wave velocity. a review of
blood pressure interpretation 100 years after Korotkov," Circulation Journal, vol. 70, no. 10, pp. 12311239, 2006.
[57] N Stergiopulos, B. Westerhof, and N. Westerhof, "Physical basis of pressure transfer from periphery to
aorta: a model-based study," American Journal of Physiology vol 274, no. 4, pp. 1386-1392, 1998.
[58] J. Williams, and B. Williams, "Arterial pulse wave velocity as a psychophysiological measure," Psychosomatic Medicine, voL 27, no. 5, pp. 408-414, 1965.
[59] B.Westerhof, I. Guelen, W Stok, K. Wesseling, J. Spaam, N. Westerhof, W Jan Bos, and N. Stergiopulos,
"Arterial pressure transfer characteristics: effects of travel time," American Journal of Physiology vol
292, no., 2,pp. 800-807, 2006.
[60] W Chen, T. Kobayashi, S. Ichikawa, Y Takeuchi, and T. Togawa, "Continuous estimation of systolic
blood pressure using the pulse arrival time and intermittent calibration," Medical and Biological Engineering and Computing, voL 38, no. 5, pp. 569-574, 2000.
185
[61] M. Sugimachi, T. Shishido, K. Miyatake, and K. Sunagawa, "A new model-based method of reconstructing central aortic pressure from peripheral arterial pressure," Japanese Journal of Physiology, voL 51, no.
2, pp. 217-222, 2001.
[62] J. Davies, Z. Whinnett, D. Francis, K. Willson, R Foale, I. Malik, A. Hughes, Kim Parker, and J. Mayet,
"Use of simultaneous pressure and velocity measurements to estimate arterial wave speed at a single site
in humans," American Journal of Physiology, vol. 290, no. 2, pp. 878-885, 2005.
[63] J. McLaughlin, M. McNeill, B. Braun, and P. McCormack, "Piezoelectric sensor determination of arterial
pulse wave velocity" Physiological Measurement, vol. 24, no. 3, pp. 693-702, 2003.
[64] A. Harada, T. Okada, K. Niki, D. Chang, and M. Sugawara, "On-line noninvasive one-point measurements of pulse wave velocity" Heart Vessels, vol. 17, no. 2, pp. 61-68, 2002.
[65] Y Tardy J. Meister, E Perret, H. Brunner, and M. Arditi, "Non-invasive estimate of the mechanical
properties of peripheral arteries from ultrasonic and photoplethysmographic measurements," Clinical
Physics and Physiological Measurement, vol. 12, no. 1, pp. 39-54, 1991.
[66] R. Maestri, G. Pinna, E. Robbie, S. Capomolla, and M. La Rovere, "Noninvasive measurement of blood
pressure variability. accuracy of the Finometer monitor and comparison with the Finapres device,"
Physiological Measurement, vol. 26, no. 6, pp. 1125-1136, 2005.
[67] G. Pinna, R Maestri, and A. Mortara, "Estimation of arterial blood pressure variability by spectral analysis: comparison between Finapres and invasive measurements," Physiological Measurements, vol. 17, no.
3, pp. 147-169, 1996.
[68] T. Sato, M. Nishinaga, A. Kawamoto, T. Ozawa, and H. Takatsuji, "Accuracy of a continuous blood pressure monitor based on arterial tonometry" Hypertension, vol. 21, no. 6, pp. 866-874, 1993.
[69] N. Searle, J. Perrault, H Ste-Marie, and C. Dupont, "Assessment of the arterial tonometer (N-CAT) for
the continuous blood pressure measurement in rapid arterial fibrillation," Canadian Journal of Anesthesia, vol. 40, no. 4, pp. 388-393, 1993.
186
[70] P. Shaltis, A. Reisner, and H. Asada, "A hydrostatic pressure approach to cuffless blood pressure monitoring," Proc. IEEE Engineering in Medicine and Biology Conference, San Francisco, USA, pp. 21732176, 2004.
[71] D. McCombie, P. Shaltis, A. Reisner, and H Asada, "Adaptive hydrostatic blood pressure calibration: development of a wearable, autonomous pulse wave velocity blood pressure monitor," Proc. IEEE Engineering in Medicine and Biology Conference, Lyon, France, pp. 370-373, 2007.
[72] C Quick, D. Berger, and A. Noordergraaf, "Constructive and destructive addition of forward and reflected arterial pulse waves," American Journal of Physiology voL 280, no. 4, pp. 1519-1527, 2001.
187