The road to financiallly sustainable health care in an aging society?
advertisement

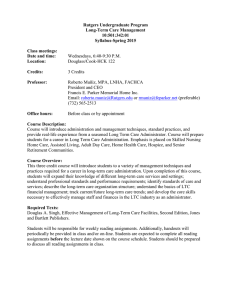
The road to financiallly sustainable health care in an aging society? March 2012 Marc Koopmanschap (Claudine de Meijer/Johan Polder/ Bram Wouterse) koopmanschap@bmg.eur.nl Outline • • • • Overview determinants of HCE Explanation HCE 1995-2009 Determinants of LTC expenditures Decomposition of acute care expenditures • Impact of determinants on HCE • The role of aging in perspective Public health policy Socioeconomic status Demography Age, sex, Household composition Health behavior, living and working conditions Health Status Incidence/preva lence disease Mortality (TTD) Medical technology Consumer preferences, income Medical consumption Acute care Long term care Informal care Disability Health care costs (acute care /LTC) Informal care costs ADL, IADL, mobility Health care system Organisation of supply and insurance, Financial incentives Informal care supply Wages prices Model Anderson and Newman (2005) Determinants Individual level Predisposing Age Gender Household composition (Socio-economic status) Enabling Informal care supply Individual income Consumer preferences Illness/need Health (incl. mortality) Disability Societal Societal level National income Medical technology Wages/prices Organisation health care Fact: HCE and Age 20000 15000 Men Wome n 10000 5000 0 10 30 50 Age (ye ars) 70 90 Fact: (Yearly) HCE at End of Life 25000 20000 Men 15000 Wome n 10000 5000 0 60 50 40 30 20 Time to death in months 10 0 Results 1995-2009 on aging and costs (1) • Naive projections of ageing, not taking into account time to death overestimate cost of aging in acute care by 10-20%. (as most extra elderly will not be in their expensive last year(s) of life) • Consensus: time to death important in acute care sector, calender age per se is not! • However, is time to death really an explanatory variable or more a proxy for health/disability? LTC determinants of consumption • Disability – but not general health – main determinant of LTC use (age has a small impact) • iADL disabilities had a greater effect on homecare, ADL disabilities more on institutional LTC • The number of disabilities matters, but first disability has a larger effect on use than any additional disability Probability of LTC use as a function of disability Aging & LTC expenditures The effect of age on LTC expenditures Old age coincides with more disability and a higher probability to live alone. After controlling for disability and coresidence status, age hardly influences the level of LTC expenditures. De Meijer, Koopmanschap, Bago d’ Uva, Van Doorslaer (2011) Co-residence status and LTC spending The effect of co-residence status Co-residence status approximates informal care availability. Informal care substitutes and postpones the use of formal LTC LTC expenditure determinants The effect of TTD when controlling for additional covariates Homecare (population model) Homecare (ext. homecare model) LTC projections – various scenario’s Scenario Index per capita LTC expenditures (55+) in 2040 (2004=100) “Naïve” (age only) 150 (institutional care = 154; home care = 141) Age plus trend in co-residence 153 status “proximity-to-death” (constant 128 (institutional LTC = 129; home care = proximity-to-death of disability) 124) Extrapolated recent decrease in severe disability 117 (homecare) De Meijer, Koopmanschap, Bago d’ Uva, Van Doorslaer (2011) Living Longer in Good Health? Life expectancy by disability status 35,0 30,0 Life expectancy at age 55 2,0 25,0 20,0 2,0 2,0 5,2 2,0 5,3 5,7 3,6 3,6 8,9 9,1 3,5 3,4 6,1 10,3 11,5 LE with severe disability LE with mild disability DFLE 15,0 10,0 17,8 18,0 19,1 20,2 16,1 16,1 15,9 15,7 5,0 0,0 0 2008 2010 2020 2030 Males 2008 2010 2020 2030 Females Forecast of lifetime LTC spending Forecast LTC spending (2008-2030) Individual life proximity spending on LTC • Future longevity gains coinciding with a compression of severe disability are not very costly per person. Aggregate population spending on LTC • Accounts for growing number of elderly • Increase 56.0% in 2008-2030, from €10.7 to €16.8 bln Acute care: decomposition HCE growth the Netherlands • Decomposition of spending on total acute care and separate analyses for hospital care and pharmaceuticals • Analysis of changes in full marginal expenditure distribution relevant as HCE are heavily skewed • 1998-2004: real spending growth of 28%, but not uniform across the spending distribution Acute care spending growth (19982004) Full distribution .4 .2 -.5 0 0 .5 Change in log expenditure .6 1 Positive expenditures 0 .2 .4 .6 .8 1 0 .2 Quantile Total acute care .4 .6 Quantile Hospital and other secondary acute care Pharmaceuticals .8 1 Decomposition of growth (1998-2004) Hospital care • Growth concentrated at centre distribution • Increased admission rates due to relaxation of hospital budgets • Decrease LOS and shift towards more day care and policlinic care constraint spending at higher quantiles Pharmaceuticals • Growth concentrated at top of distribution • More intensive/expensive drug use • Technological progress dominates growth, especially at higher percentiles (monopolistic prices new drugs) • Moderate contribution of shift towards less intensive hospital treatment (substitution to outpatient drugs) Overview results of determinants of health care expenditures Predisposing determinants Age and gender • age composition of population has a limited (< 1% growth py) role in growth HCE. • For LTC expenditures, age has some impact, might be proxy for frailty not measured by disability/health; • Elderly females depend more on LTC services than males; a longer life expectancy (but less in good health) -> need more formal LTC and have less informal care. Household composition • Singles are substantially more likely to use LTC, and their expenditures are much higher (less informal care). Illness/need determinants Health and disability Acute care: • Time to Death (TTD) important; • Differences in effect of TTD on disease specific HCE -> TTD vs HCE depends on epidemiology (Wong; de Meijer). Long term care: • when controlling for health and esp. disability, effect of both age and TTD is substantially lower Health status vs disability: dynamics: given disease, less disability -> less LTC costs?? As result of acute care investments? Enabling determinants Informal care • informal care lowers LTC use; • supply of informal care depends on household composition and (future) female labor participation. Income • Macro-income major determinant of HCE; • In case of comprehensive insurance, individual income limited role in determining HCE. Consumer preferences • changing preferences important driver of rising HCE? evidence is scarce; difficult to separate from shifts in health care needs and supply. Societal determinants Medical technology • Very important, exact contribution of medical technology hard to estimate; • The impact of technology on HCE strong for prescription drugs and hospital care; • medical technology value for money? Very broad range costeffectiveness; Organization of health care • might clearly affect HCE, but evidence on the link between institutional aspects, ageing and HCE limited. • Cost sharing lowers HCE, managed competition lowered prices, but HC-utilisation increased considerably Wages/prices • Baumol effect (for NL estimated as 0.8% p.a.); • serious labour shortages to come, will raise wages. The role of aging in perspective (1) • Health care costs related to interplay of: – Demography (age, household composition) – Epidemiology/health/disability – Technology (plus demand attitude) • Mechanisms different for acute care vs LTC • Self assessed health, chronic conditions, TTD and cause of death -> acute care costs; • Disability & household composition -> LTC costs • Medical technology major role in boosting HCE in acute care, but might limit disability and lower LTC demand; The role of aging in perspective (2) • Häkkinen (2008): “.. future expenditure is more likely to be determined by health policy than inevitable trends in demography”. – Calls for policies that lower disability further.. • Evans et al. (2001): there is nothing fixed or clinically imperative about current age-specific health care spending, nor do countries need to accept as an unalterable fact that age-specific per capita HCE in the future must necessarily go up for all groups, and especially for the elderly. The role of aging in perspective (3) • From a broader policy perspective: when further advances in medical technology are allowed to be introduced swiftly (for elderly) and growing expectations of future elderly regarding service levels are accommodated, all researchers expect that HCE as % of GDP will increase considerably, probably together with healthy life expectancy. – Calls for choices in medical technology…. • Hence, the policy question is: (how much) are we willing to pay for all these “advances” in care?