Edward H. Piepmeier, Jr. for the degree of Doctor of... Pharmacy presented on April 16, 1991.
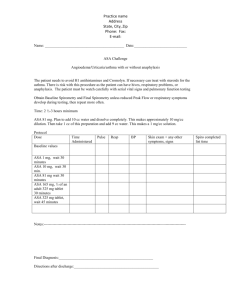
advertisement

AN ABSTRACT OF THE THESIS OF Edward H. Piepmeier, Jr. for the degree of Doctor of Philosophy in Pharmacy presented on April 16, 1991. Title: Formulation of an Oral Acetylsalicylic Acid Suspension and Pharmacokinetics of Parenteral Thrombomodulin Analogues. 1"? Abstract approved: Redacted for Privacy i Mark Christensen, rn. v. Sustained c ncentrations of active compound were maintained in vitro and in vivo for an oral and a parenteral dosage form respectively. The vehicle of a oral dosage form was modified and the molecular structure of a parenteral dosage form was modified. An oral dosage form was tested in vitro using dissolution apparatus. A parenteral dosage form was tested in vivo using rats. A new oral suspension dosage form for acetylsalicylic acid was compared to two controlled release forms and two immediate release dosage forms which are currently commercially available. A parenteral thrombomodulin analogue conjugated to polyethylene glycol was compared to the unconjugated thrombomodulin analogue. In each case the goal was to maintain sustained concentrations of active compound. Formulation of an Oral Acetylsalicylic Acid Suspension and Pharmacokinetics of Parenteral Thrombomodulin Analogues by Edward H. Piepmeier, Jr. A THESIS submitted to Oregon State University in partial fulfillment of the requirements for the degree of Doctor of Philosophy Completed April 16, 1991 Commencement June 1991 APPROVED: 4 , . _ Redacted for Privacy P ofAsOr of Pharmacy in charge of major ,1 Redacted for Privacy - Dean of College of Pharmacy Redacted for Privacy Dean of duate Scho Date thesis presented Presented by April 16, 1991 Edward Piepmeier, Tr. ACKNOWLEDGEMENTS This thesis is dedicated to Heidi and Andrew who make my work worthwhile. I wish to express my sincere gratitude to my major professors, Dr. J. Mark Christensen and Dr. James Ayres for their guidance, support and tireless proofreading. My sincere appreciation goes to my parents for providing moral support to help me attain my goals. The research reported in this thesis was supported in part by a grant from Berlex Biosciences. I would like to thank the people at Berlex Biosciences, especially Dr. John Morser, Dr. David Light and Susan Fink, for providing the thrombomodulin analogue and conjugate, as well as for performing the activated protein C assay. Finally I would like to thank my fellow graduate students for their help and friendship. TABLE OF CONTENTS CHAPTER 1: THREE LAYERED POLYMER COATING OF ASPIRIN IN A SUSPENSION DOSAGE FORM ABSTRACT INTRODUCTION MATERIALS AND METHODS RESULTS AND DISCUSSION REFERENCES CHAPTER 2: HIGH DOSE AND LOW DOSE THROMBOMODULIN ANALOGUE PHARMACOKINETICS IN RATS ABSTRACT INTRODUCTION MATERIALS AND METHODS RESULTS AND DISCUSSION REFERENCES CHAPTER 3: CONJUGATION OF THROMBOMODULIN ANALOGUE WITH POLYETHYLENE GLYCOL TO INCREASE THE HALF LIFE IN THE BLOOD ABSTRACT INTRODUCTION MATERIALS AND METHODS RESULTS AND DISCUSSION REFERENCES 1 2 3 8 17 38 40 41 43 50 56 73 75 76 78 80 86 95 BIBLIOGRAPHY 97 APPENDIX 104 LIST OF FIGURES Figure 1.1 Diagram Describing the Dissolution of an Aspirin Formulation Including the Dissolution of Salicylic Acid Present in the Formulation and the Degradation of ASA to SA in Solution. 20 Figure 1.2 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid U, Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Genuine Bayer Aspirin, Immediate Release Tablets. 23 Figure 1.3 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid II, Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Therapy Bayer Aspirin, Enteric Coated Tablets. 24 Figure 1.4 Milligrams of Acetylsalicylic Acid 0 and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Dissolved in Simulated Gastric Fluid and Simulated Acid Intestinal Fluid Versus Time From Measurin Timed Release Aspirin, Eight Hour Release Tablets. 26 Figure 1.5 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid U, Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Eight Hour Bayer Timed Release Aspirin, Eight Hour Release Tablets. 27 Figure 1.6 Milligrams of Acetylsalicylic Acid Cl, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid U, Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Experimental Beads With Triple Polymer Coating. 28 Figure 1.7 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid U, Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Experimental Beads With Triple Polymer Coating, Incubated in Grape Jelly at 400C for One Week. 29 Figure 1.8 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid , Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Experimental Beads With Triple Polymer Coating, Incubated in Grape Jelly at 400C for Two Weeks. 30 Figure 1.9 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid II, Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Experimental Beads With Triple Polymer Coating, Incubated in Grape Jelly at 400C for Six Weeks. 31 Figure 1.10 Percent of Total Acetylsalicylic Acid and Salicylic Acid Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Genuine Bayer Aspirin, Immediate Release Tablets 0, and Therapy Bayer Aspirin, 33 Enteric Coated Tablets . Figure 1.11 Percent of Total Acetylsalicylic Acid and Salicylic Acid Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Eight Hour Bayer Timed Release Aspirin, Eight Hour Release Tablets 0, and Measurin 34 Timed Release Aspirin, Eight Hour Release Tablets . Figure 1.12 Percent of Total Acetylsalicylic Acid and Salicylic Acid Dissolved in Simulated Gastric Fluid and Simulated Intestinal Fluid Versus Time From Experimental Beads With Triple Polymer Coating, Incubated in Grape Jelly at 35 400C for Zero 0, One , Two 0, and Six Weeks II. Figure 2.1 A schematic model showing the five domains in the structure of endothelial thrombomodulin. 44 Figure 2.2 Schematic representation of the coagulation system which forms crosslinked fibrin, and the fibrinolytic system which breaks the crosslinked fibrin into fibrin degradation products. 45 Figure 2.3 The fraction of initial protein C activation versus time curves for ten rats receiving 10, 20, 50, 100, or 200 micrograms of thrombomodulin with leucine substituted for methionine at the 388th position. 57 Figure 2.4 Average fraction of initial radiolabel remaining from 1251 thrombomodulin analogue for low dose , and high dose administered. 59 Figure 2.5 Fraction of initial protein C activation 0 remaining over time and fraction of initial radiolabel remaining over time for a rat which was administered 200 micrograms of thrombomodulin with leucine substituted for methionine at the 388th position. 61 Figure 2.6 Fraction of radiolabel from 1251 labelled 67 thrombomodulin analogue which appears in the bile at low doses 0, and high doses . Figure 2.7 Fraction of radiolabel from 1251 labelled 69 thrombomodulin analogue found in tissues following sacrifice of high dose rats. Figure 3.1 Fraction of initial protein C activation remaining over time for four doses of thrombomodulin analogue and two different doses of PEG conjugate analogue. 89 Figure 3.2 Average fraction of initial radiolabel remaining from 1251 thrombomodulin analogue for low dose and high dose administered, and PEG conjugated thrombomodulin analogue with 50% of initial activity 0 and 70% of initial activity O. 91 LIST OF APPENDIX FIGURES Figure A.1 The fraction of initial radiolabel administered remaining over time for radiolabelled Bovine Serum Albumin 0, low dose radiolabelled thrombomodulin analogue with radiolabelled BSA , and high dose radiolabelled thrombomodulin analogue with radiolabelled BSA E. 107 108 Figure A.2 This figure shows the result of step #1 when the radiolabel vs. time curves shown in figure A.1 are used to determine the fraction of radiolabelled bovine serum albumen in each of the two thrombomodulin analogue BSA mixtures. 109 Figure A.3 The radiolabelled bovine serum albumen in the high dose thrombomodulin analogue BSA mixture is calculated to be 33.7%. So the BSA curve is multiplied by 0.337 and this resulting curve is subtracted from the thrombomodulin analogue BSA mixture to obtain the radiolabel attributable to the thrombomodulin analogue only 0. 110 Figure A.4 The radiolabelled bovine serum albumen in the low dose thrombomodulin analogue BSA mixture is calculated to be 48.9%. So the BSA curve is multiplied by 0.489 and this resulting curve is subtracted from the thrombomodulin analogue BSA mixture to obtain the radiolabel attributable to the thrombomodulin analogue only Figure A.5 These curves represent the fraction of radiolabel which is attributable only to thrombomodulin analogue relative to the initial amount of radiolabel injected. 111 Figure A.6 The amount of radiolabel remaining due to thrombomodulin analogue relative to the initial radiolabel injected into the rat in the form of thrombomodulin analogue. 112 Figure A.7 High dose and low dose pharmacokinetics of thrombomodulin analogue in rats. The high dose and low dose administered as pure thrombomodulin samples is compared to the mathematically derived curves from the high dose and low dose 0 samples administered with radiolabelled BSA. 113 LIST OF TABLES Table 1. 1 The percent of drug in beads which is acetylsalicylic acid or salicylic acid is compared to what would be expected with the coating procedures carried out in this experiment. 10 Table 1.2 Percent of ASA and SA measured in each dosage form relative to the total weight of each formulation. 12 Table 1.3 Percent of ASA and SA found in the bead and jelly components of beads incubated in jelly at 400C over time relative to the total amount of drug in each formulation. 13 Table 1.4 The rate constants for release of ASA as SA and ASA and the rate constant for conversion of ASA to SA in 18 intestinal fluid in simulated gastric fluid and simulated intestinal fluid. Table 1.5 The time is the amount of time elapsed after beginning dissolution. The dosage form is transferred to the simulated intestinal fluid at 120 minutes. The actual number of mg of ASA determined by HPLC assay in simulated intestinal fluid is listed in the second column. The amount of ASA which would be expected based on the rates of ASA release and rates of ASA to SA conversion found in Table 1.4 is calculated and shown in the third column. The final column shows the percent of theoretical release which was actually observed and the coefficients of variation. 22 Table 2.1 The fraction of initial protein C activation over time + standard deviations for rats receiving thrombomodulin with leucine substituted for methionine at the 388th position. 58 Table 2.2 Average fraction + standard deviations of initial radiolabel remaining in the blood from 1251 thrombomodulin analogue for low dose and high dose. 60 Table 2.3 Fraction of thrombomodulin analogue remaining as determined by 1251 radiolabel and activated protein C assay for a rat which received 200ug of thrombomodulin analogue with leucine substituted for methionine at the 388th position. 62 Table 2.4 Radioactivity half life times in minutes 63 following low dose and high dose of thrombomodulin analogue as determined by monoexponential and biexponential curve fitting. Monoexponential half lives as determined by activated protein C assay. Table 2.5 Fraction of initial radiolabel from 1251 labelled 68 thrombomodulin analogue which appears in the bile at high doses and low doses. Each timepoint represents data from up to four rats. Table 2.6 Each tissue collected represents the following percent of total body weight. 70 Table 2.7 Fraction of radiolabel from 1251 labelled 72 thrombomodulin analogue found in tissues following sacrifice of high dose rats. Four rats were sacrificed one hour apart at 1, 2, 3, and 4 hours. Table 3.1 Half lives in minutes and areas under the curve in mOD/minute versus minutes as determined by protein C activity for thrombomodulin analogue with methionine converted to leucine at the 388th position and for the polyethylene glycol conjugate of the thrombomodulin analogue. 87 Table 3.2 The fraction of initial protein C activation over time ± standard deviations for rats receiving thrombomodulin with leucine substituted for methionine at the 388th (M388L) position conjugated with PEG. 90 Table 3.3 Half lives in minutes, areas under the curve in mOD/minute versus minutes, and mean residence times in minutes (MRT) are calculated for each rat using 92 RSTRIP. Table 3.4 Average fraction ± standard deviations of initial radiolabel remaining in the blood from 1251 thrombomodulin analogue conjugated to PEG. 93 FORMULATION OF AN ORAL ACETYLSALICYLIC ACID SUSPENSION AND PHARMACOKINETICS OF PARENTERAL THROMBOMODULIN ANALOGUES CHAPTER 1 THREE LAYERED POLYMER COATING OF ASPIRIN IN A SUSPENSION DOSAGE FORM 2 ABSTRACT An experimental controlled release aspirin (ASA) suspension dosage form was investigated wherein the ASA was coated with three distinct polymer layers in "sandwich" fashion. The experimental suspension and four commercially available aspirin products were analyzed for acetylsalicylic acid and its primary degradation product, salicylic acid. Dissolution profiles for one immediate release tablet, one enteric coated tablet, two controlled release tablets, and the experimental suspension were compared. The experimental formulation releases all drug over eight hours. Salicylic acid release from the experimental formulation was higher than from commercially available solid dosage forms. INTRODUCTION Controlled release of acetylsalicylic acid (ASA) increases the duration of action and decreases gastrointestinal irritation. A short duration of action from immediate release tablets is due to rapid elimination of ASA through degradation and metabolism in both the gastrointestinal and vascular fluids. The distribution and elimination half lives for ASA in the blood are 2.8 and 15 minutes respectively (1,2). This elimination cannot be countered with increased doses of ASA. When the gastrointestinal tract is exposed to high concentrations of ASA, cell necrosis occurs. Irritation occurs to the Gastrointestinal (GI) tract when rapid dissolution or disintegration causes a large surface area of high concentrations of ASA in liquid, semiliquid or solid forms to come in contact with the GI tract (3). Rapid disintegration of immediate release dosage forms causes high dissolution layer concentrations of ASA with large surface areas of undissolved particles to come in contact with the mucosal membrane of the stomach. Buffers minimize the time for aspirin dissolution and the time the aspirin remains in contact with the stomach and decrease bleeding compared to non buffered tablets (4). An immediate release buffered tablet causes more irritation to the stomach than microencapsulated tablets (3). Enteric 4 coating minimizes gastric irritation (5), however aspirin is absorbed readily in the stomach and so release of low concentrations in the stomach is beneficial if a rapid effect is desired. Additionally, enteric coated tablets cause high concentrations of aspirin to come in contact with the intestinal mucosa where it is degraded rapidly by esterase. The esterase activity in the duodenum is ten times that of the stomach (2). ASA is rapidly metabolized and cleared following absorbtion. In vascular fluids, ASA is deacetylated to form salicylic acid which is then metabolized through the following routes: conjugation of salicylic acid (SA) with glycine to form salicyluric acid, conjugation of SA with glucuronic acid to form salicyl phenolic glucuronide and salicyl acyl glucuronide, and oxidation of SA to gentisic acid. SA is also excreted directly by the kidney (6). In vitro, acetylsalicylic acid degrades to salicylic acid, salicylsalicylic acid, acetylsalicylsalicylicacid, acetylsalicylic anhydrate, acetylsalicylsalicylsalicylic acid, acetylsalicylsalicylsalicylsalicylic acid, salicylsalicylsalicylic acid, and salicylsalicylsalicylsalicylic acid (7). The primary degradation product is salicylic acid (SA) which was monitored along with ASA in this study. Products containing ASA lose much of their activity when ASA is degraded to SA. ASA, unlike SA, has both antiinflammatory and antipyretic effects. ASA has greater 5 analgesic affects than SA (8). ASA is an inhibitor of cyclooxygenase. PGE2, a precursor to cyclooxygenase, is inhibited by ASA but not by SA (9). Aspirin tolerance in asthmatics occurs when SA binds to the cyclooxygenase supplementary binding site. Therefore, SA inhibits some activity of ASA. Complete thromboxane inhibition can occur from the amount of ASA released from one immediate release tablet per day but collagen induced platelet aggregation can occur shortly after the ASA levels decline. Induction of platelet aggregation increases the risk for myocardial infarction the morning after an ASA tablet has been taken, when ASA has not been present in the blood for hours (10). By releasing ASA from a dosage form over a sustained period of time, a sustained level of ASA may be maintained in the blood. The controlled release property of the experimental dosage form has the potential to reduce the risk of myocardial infarction associated with immediate release dosage forms. Because the new formulation is a suspension, it will pass through a nasal gastric tube and still provide sustained release, unlike crushed solid dosage forms. The only non-tablet, solid, sustained release product currently available is Theo-Dur Sprinkle Sustained Action Capsules (ScheringPlough, New Jersey). The contents of the capsule, microencapsulated 6 theophylline beads, are intended to be sprinkled on or mixed in with food prior to ingestion. If microencapsulated beads are chewed or crushed, however, all sustained release properties are lost. The only sustained release suspension currently available is the Pennkinetic system (ion exchange system). Suspensions are typically messy to administer and may not enjoy a high acceptance rate among consumers. A suspension of very high viscosity, however, may be easier to administer and therefore more acceptable. Geriatric patients may have chewing or swallowing difficulties (11). In this case, traditional oral dosage forms are not ideal and alternate drug delivery systems are needed. Therefore a goal in the development of the experimental dosage form was to formulate a dosage form that is easily administered to and readily accepted by geriatric consumers. The experimental product is a controlled release suspension consisting of beads coated with three distinct membrane coats and presuspended in a grape jelly type vehicle. In the experimental product, the enteric coat prevents ASA release in the stomach, while the controlled release polymer coat prevents high concentrations of aspirin from being released upon entering the intestine. The stomach will be protected from irritation and the aspirin continuously released in the intestine. The purpose of this research is to track ASA and SA in dissolution tests and to formulate and evaluate a sustained release 7 ASA suspension as well as commercially available ASA preparations. 8 MATERIALS AND METHODS Nonpareil sugar beads (25 mesh) were coated with ASA to a final mesh of 18-20. Polyvinylpyrrolidone and hydroxypropylmethylcellulose were dissolved in 95% ethanol for use as binders. Acetylsalicylic Acid (Sigma) was dissolved in the ethanol solution, and loaded onto sugar beads at 300C. The ASA beads were then coated with Aquacoat 7%, by weight theoretical, followed by Eudragit 5%, followed by Aquacoat 7%. The sugar cores were loaded with acetylsalicylic acid using a STREA-1 laboratory scale spray coater (Aeromatic, Towaco, NJ) equipped with a 6-inch Wurster column and Lab-Line/P.R.L. Hi-Speed Fluid Bed Dryer (Lab-Line Instruments, Inc., Melrose Park, IL). Ethanolic drug solution was applied to freely moving sugar beads through a 1.2mm orifice diameter spray nozzle. Atomization air pressure was 10-12 psi. A medium perforated plate was placed below the nozzle of the Wurster column and fluidization air was applied with a blower speed of 50-80% of capacity. The fluidization air kept the beads moving freely throughout the drug loading. A peristaltic pump (Minipuls 2, Gilson Medical Electronics, Middleton, WI) introduced drug suspension into the coating chamber at a rate of 10m1/minute. Freshly prepared acetylsalicylic acid beads were transferred to a sieve 9 and oven dried at 400C for one day to remove residual moisture. Dried acetylsalicylic acid beads were then sieved and the ten mesh fraction was coated with a triple layer of polymers, using the same spray coating equipment. The drug load of acetylsalicylic acid and salicylic acid were determined using high pressure liquid chromatography. Two commercially available latex dispersions, Aquacoat and Eudragit L-30D, were used for polymer film application. Coating formulations containing these materials were applied only to 10 mesh fractions of acetylsalicylic acid cores to minimize variability in release behavior due to drug core size variations (12). During the application of Aquacoat, bed temperature was kept at 400C and the blower speed and delivery rate varied to maintain a fluidized circulation because of differences in the stickiness of the developing film. Blower speed ranged from 50 to 100% and delivery rate ranged from 0-10 milliliters per minute. An 0.8 millimeter orifice diameter spray nozzle was used. Eudragit L-30D was applied under identical conditions. After each coating, three samples of beads were pulverized, dissolved and analyzed for drug content with high pressure liquid chromatography. The expected and actual results following each coating procedure are shown in Table 1.1. The beads (16g) were mixed in with grape jelly (Danish Orchards, 30g) and carbopol (BF Goodrich, 0.4g). The jelly was divided into jars containing 10 Table 1. 1 The percent of drug in beads which is acetylsalicylic acid or salicylic acid is compared to what would be expected with the coating procedures carried out in this experiment. Higher assayed values than expected may be attributable to loss of beads during the coating procedure and lower assayed values than expected may be attributable to loss of coating material during the coating procedure. HPLC assay was used until three values were obtained within 1% of each other. BEADS FIRST COAT SECOND COAT THIRD COAT ASSAYED 92% 83 78 72 EXPECT ED 83% 77 73 69 11 1.6g of suspension equivalent to 556mg of beads or 400mg of ASA. All commercial and experimental products were assayed for ASA and SA content relative to their total formulation weight (Table 1.2). The experimental beads were tested both in a suspension and out of suspension (dry). Stability studies were performed for the ASA suspension. The jelly suspension was incubated at 400C. This temperature was chosen to increase the rate of aging over the rate of aging found at room temperature. The jelly and beads were separated and assayed using the high pressure liquid chromatography method described below for ASA and SA content after incubation for one, two, and six weeks (Table 1.3). HIGH PRESSURE LIQUID CHROMATOGRAPHY Acetylsalicylic acid and salicylic acid were measured quantitatively in each sample by a modification of a previously reported HPLC procedure (13). The mobile phase was prepared by mixing acetonitrile, methanol and 0.1M Potassium Phosphate Dibasic (10:34:56 by volume). The final pH was adjusted to 2.5 + 0.1 with phosphoric acid. Solvent was filtered (0.4 microns) and degassed prior to use. Flow rate was set to 1.0m1/minute. Effluent from the column was monitored by UV absorption at 229nm. 3-hydroxybenzoic acid was used as an internal standard. Peak height ratios were used for 12 Table 1.2 Percent of ASA and SA measured in each dosage form relative to the total weight of each formulation. Each formulation is within one standard deviation of the labelled value. All are analyzed in triplicate. DOSAGE FORM Eight Hour Immediate Release Coated Beads Measurin Enteric Coat *less than 0.25% ASA% (SD) 89.5(0.815) 79.9(2.91) 72.0(1.66) 91.4(3.16) 73.7(8.80) SA% (SD) 0.479(0.0199) 1.69(0.113) 2.19(0.0543) 0* 1.65(0.301) 13 Table 1.3 Percent of ASA and SA found in the bead and jelly components of beads incubated in jelly at 400C over time relative to the total amount of drug in each formulation. n=3 1week ASA% mean(sd) SA% mean(sd) 93.49(4.683) 1.240(1.157) 3.510(0.0543) 1.780(1.585) jelly 60.46(2.697) 8.404(1.812) 6.475(0.812) 24.65(4.693) beads jelly 41.16(1.513) 22.15(6.978) 13.51(2.205) 23.18(6.330) beads jelly 2 weeks 6 weeks beads 14 quantitation based on standard curves established on the same day. All chromatographic separations were carried out at ambient temperature. An HPLC solvent delivery system Model M-45, an Automatic Injector Model 712-WISP, a 30cm X 3.9mm ID microBondapak C18 Column, and a Model 441 Absorbance detector, all from Waters Associates (Milford, Mass., U.S.A.), were used in this study. A Shimadzu CR3A Integrator was used to record the peaks measured at 229nm. The United States Pharmacopeia dissolution Apparatus 2 (paddle) was used in all experiments. The paddle was rotated at 50rpm. Studies were carried out in simulated enzyme free gastric and intestinal fluid. Simulated enzyme free gastric fluid was prepared by dissolving 6g of NaC1 in 21 ml of concentrated HC1 and sufficient deionized water to make 3L; the pH was adjusted to 1.4 ± 0.1 with hydrochloric acid. Simulated enzyme free intestinal fluid was prepared by dissolving 20.4g of potassium phosphate monobasic (EM Industries, Inc., Gibbstown, N.J) in 750m1 of deionized water. To this was added 4.56g of NaOH and 1.2L of water. The pH was adjusted to 7.4 ± 0.1 with 2N NaOH before the volume was made up to 3L with water. Dissolution was performed in quadruplicate for each dosage form. Three of the same dosage form were analyzed on the same day and a fourth was analyzed on a different day to insure that day to day 15 variability was not significant. The dosage form was added to 900m1 of gastric fluid at 37 + 0.50C in a water bath. This temperature was maintained throughout the study. All dosage forms were tested first in simulated gastric fluid and then changed to simulated intestinal fluid after 2 hours to simulate passage of the residual dosage form from the stomach into the upper intestine. The simulated intestinal fluid was prepared fresh and brought to 370C just prior to the actual dissolution test. Transfer of dosage forms from gastric to intestinal fluid was carried out by filtering the gastric fluid and then placing the filter paper in 900m1 of simulated intestinal fluid in the vessel. Rotation of the paddle then resumed for the duration of the test. The change in fluids took 10 to 15 minutes. Fifty microliter samples were taken at 15, 30, 60, 90, 120 (before transfer to intestinal fluid), 180, 240, 300, 360, 720, and 1440 minutes. Samples, 50u1, were run on HPLC within one hour following sampling using 3hydroxybenzoic acid, 1mg/ml, 950u1, as an internal standard. When drug concentrations were low, equal volumes of sample and internal standard were combined and analyzed. Standard curves were run for both methods of analysis. The first five samples were taken from the simulated gastric fluid and the remaining samples were taken from the simulated intestinal fluid. The following dosage forms were purchased commercially; Measurin Timed Release Aspirin (Winthrop, 650mg), 16 Therapy Bayer Aspirin (Bayer, 325mg), Genuine Bayer Aspirin (Bayer, 325mg), and Eight Hour Bayer Timed Release Aspirin (Bayer, 650mg). Quattro was used to calculate peak height ratios and conversion of peak height ratios to concentration in mg/ml. Standard deviations and regression of all linear fits were also calculated using Quattro. First order linear release rates and conversion rates were assumed due to the high solubility of ASA, 1g/100m1 at 370C. The highest content of ASA in a formulation was 650mg and the dissolution beaker contained 900m1. 17 RESULTS AND DISCUSSION Each of the commercial formulations in this experiment were tested for ASA and SA content (Table 1.2). In each case the labelled content was within one standard deviation of the assayed amount. All commercial products met USP requirements. The experimental formulation did not meet USP requirements for an extended release aspirin formulation. USP requires that immediate release aspirin formulations be between 90% and 110% of the labeled dose and that both delayed release and extended release aspirin formulations be between 95% and 105% of the labelled dose. The ASA and SA content of the experimental formulation changed while it incubated in the jelly suspension at 400C (Table 1.3). The dissolution rate constants are calculated from the amount of drug undissolved at each timepoint (Table 1.4). The dissolution rate constants in simulated intestinal fluid are calculated based on the undissolved drug which remains after the simulated gastric fluid is removed. After all of the ASA has been released from the tablet as ASA or SA then it is possible to calculate the rate constant for conversion from ASA to SA. This value is 0.021hour-1 based on calculations from immediate release and enteric coated tablets. The other formulations continued to release ASA over most of the sampling period and so accurate ASA to SA conversion values were 18 Table 1.4 The rate constants (hour-I) for release of ASA as SA and ASA and the rate constant for conversion of ASA to SA in intestinal fluid in simulated gastric fluid and simulated intestinal fluid. Standard deviations are shown in parentheses. Gastric Fluid total release Immediate Enteric 8-hour Measurin Dry Beads One Week Two Weeks Six Weeks 1.1(0.11) b 0.32(0.045) 0.45(0.033) 0.034(0.0041) 0.052(0.0027) 0.097(0.071) 0.13(0.016) Intestinal Fluid SA conversion total release 0.11a 1.2(0.16) 0.42(0.070) 0.048(0.0024) 0.067(0.0074) 0.062(0.00064) 0.23(0.019) 0.30(0.073) 0.020(0.0017) 0.021(0.00062) 0.016(0.0016)c alower limit (calculated based on total amount released in < one hour) bless than 0.5% total dose released c some ASA continues to be released and so this value is an estimate 19 not obtainable. The model depicted in Figure 1.1 was used to calculated the concentration of ASA and SA in solution. The conversion of SA to ASA was assumed to be negligible. The conversion of ASA to SA was negligible in simulated gastric fluid at low pH (1.5), and 0.021hourl in simulated intestinal fluid. The release of SA from the dosage forms was very small and assumed to be complete after two hours in gastric fluid. The rate constants that were calculated were based on the total release of ASA and SA in both simulated gastric fluid and simulated intestinal fluid. In addition the rate constant for conversion of ASA to SA in intestinal fluid was used to compare estimated ASA concentrations in the intestinal fluid with actual concentrations in intestinal fluid for the controlled release suspension. The equation used in simulated gastric fluid to determine the amount of dose remaining to be released was C.Ae-ki ( 0 A represents the total amount of drug remaining to be dissolved in gastric fluid, k1 represents the rate constant found in Table 1.4 and t represents the time in hours. The equation used to determine the amount of drug remaining to be released in simulated intestinal fluid was C =Be-k2(t) - De-k3(t). B represents the total amount of drug which remains to be dissolved in simulated intestinal fluid D represents the total amount of ASA degraded to SA in simulated intestinal fluid, k2 and k3 represent rate constants found in Table 1.4 and t represents to the time in hours. This 20 Figure 1.1 Diagram Describing the Dissolution of an AspirM (ASA) Formulation Including the Dissolution of Salicylic Acid (SA) Present in the Formulation and the Degradation of ASA to SA in Solution. Kl, K2, and K3 are the rate constants which are listed in Table 1.4. ASA solid K1 ASA dissolved K3 SA solid SA dissolved 21 fit gave coefficients of variation of less than 10% for all samples (Table 1.5). The immediate release tablets release 260mg of ASA as ASA and 8.7mg of ASA as SA in the first two hours (Figure 1.2). This is 89% of the drug released in the gastric fluid, without much of the ASA being hydrolyzed to SA. The remaining ASA is released within the first hour in the intestinal fluid. The SA content does not increase noticeably post 120 minutes in the intestinal fluid because only 11% of the ASA remains in the dissolution flask after disposing of the ASA which was dissolved in the gastric fluid. The remaining ASA degrades to SA with a half life of 33 hours in simulated intestinal fluid. The half life of approximately 33 hours for degradation of ASA to SA in simulated intestinal fluid was calculated for enteric coated tablets and Bayer eight hour controlled release tablets (Table 1.4). The enteric coated tablets do not release any ASA until after they are transferred into the intestinal fluid (Figure 1.3). In intestinal fluid (pH 7.4) nearly all of the ASA dissolves in the first hour. The ASA then degrades to SA over the next 22 hours until SA almost equals ASA in concentration. This conversion of ASA to SA will not be as great in vivo in the gastrointestinal tract as in in vitro intestinal fluid since the dissolved ASA would be absorbed. For the measurin formulation 58% of drug was dissolved in the 22 Table 1.5 The time is the amount of time elapsed after beginning dissolution. The dosage form is transferred to the simulated intestinal fluid at 120 minutes. The actual number of mg of ASA determined by HPLC assay in simulated intestinal fluid is listed in the second column. The amount of ASA which would be expected based on the rates of ASA release and rates of ASA to SA conversion found in Table 1.4 is calculated and shown in the third column. The final column shows the percent of theoretical release which was actually observed and the coefficients of variation. DRY BEADS time ASA ACTUAL 63 240 86 360 139 480 167 540 183 720 208 840 252 1080 215 1440 CALCULATED 72.5 99.1 151 174 179 202 244 208 % THEORETICAL 86.9 86.8 92.1 96.0 102 103 103 103 CV=6.23 BEADS INCUBATED IN SUSPENSION FOR ONE WEEK CALCULATED % THEORETICAL time ASA ACTUAL 89.7 100 89.7 240 300 360 420 540 720 1080 1440 104 117 129 144 170 171 156 114 156 140 157 179 184 177 91.2 75.0 92.1 91.7 95.0 92.9 88.1 CV=6.92 BEADS INCUBATED IN SUSPENSION FOR TWO WEEKS CALCULATED % THEORETICAL ASA ACTUAL time 240 300 360 480 1440 125 148 159 202 149 89.8 116 132 182 124 139 128 120 111 120 CV=8.50 BEADS INCUBATED IN SUSPENSION FOR SIX WEEKS CALCULATED % THEORETICAL time ASA ACTUAL 240 300 360 420 720 1080 1440 197 233 244 251 230 203 176 186 223 237 246 228 209 186 106 104 103 102 101 97.1 94.6 CV=3.94 23 Figure 1.2 Milligrams of Acetylsalicylic Acid El, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid III, Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Genuine Bayer Aspirin, Immediate Release Tablets. 400 - 300 - -.0- ASA ---*- SA 200 - ASA & SA 100 - 416.1r.-1"--r-1 0 240 480 I 720 TIME(MINUTES) 960 1 1200 1 440 24 Figure 1.3 Milligrams of Acetylsalicylic Acid CI, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid W Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Therapy Bayer Aspirin, Enteric Coated Tablets. 400 ASA SA ASA+SA 0 240 480 720 TIME (MINUTES) 960 1200 1440 25 first two hours in gastric fluid but the remaining drug did not dissolve entirely until after an additional 46 hours in intestinal fluid (Figure 1.4). The SA increases along with the ASA content in intestinal fluid due to ASA to SA conversion. The Bayer Eight Hour tablets released 44% of drug in the first two hours with the remainder dissolving over the next six hours (Figure 1.5). The salicylic acid increased slowly over the twelve hours. After 24 hours, 78% of the ASA from the dry experimental dosage form is released (Figure 1.6). There is a gradual increase in SA, in solution, comparable to that seen in measurin. 93% of the drug was released after 48 hours total elapsed time. The experimental dosage form (beads) incubated in jelly for one week release 58% of total after 12 hours and 69% of total drug after 24 hours (Figure 1.7). The beads incubated in jelly for two weeks released 80% of drug after twelve hours with the remainder being released within 24 hours (Figure 1.8). After six weeks of incubation the beads release the entire amount of drug within eight hours (Figure 1.9). The drug released as SA increased, the longer the beads were incubated in jelly (Table 1.3). The percent of total labelled salicylate released over time curves show release from each formulation without regard for ASA degradation (Figures 9-11). The enteric and immediate release dosage forms have released their entire contents within one hour of reaching 26 Figure 1.4 Milligrams of Acetylsalicylic Acid 0 and Salicylic Acid 11, and Combination of Acetylsalicylic Acid and Salicylic Acid III, Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Measurin Timed Release Aspirin, Eight Hour Release Tablets. 700 600 0 500 w ta 0-- ASA 1,-- SA < 400 w 1 w cc 300 ASA+SA 0 2 200 100 0 0 1000 2000 TIME (MINUTES) 3000 27 Figure 1.5 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid 0, and Combination of Acetylsalicylic Acid and Salicylic Acid MI, Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Eight Hour Bayer Timed Release Aspirin, Eight Hour Release Tablets. 700 600 w 500 - < 400 w ASA -4-- SA -J cc 300 - ASA+SA 0 2 200 100 0 240 480 720 960 TIME (MINUTES) 1200 1440 28 Figure 1.6 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid III, Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Experimental Beads With Triple Polymer Coating. 400 G 300 - w ASA 10-- SA _1 200 - ASA+SA cc 0 2 100 - 0 240 480 720 960 TIME(MINUTES) 1200 1 440 29 Figure 1.7 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid III, and Combination of Acetylsalicylic Acid and Salicylic Acid III, Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Experimental Beads With Triple Polymer Coating, Incubated in Grape Jelly at 400C for One Week. 350 300 - 0 ASA 250 w Cl) <I 200 - w 12""".....,1 1 ul 150 ce 10-- SA (5 2 100 50 0 0 240 i I I 1 480 720 960 1200 TIME (MINUTES) 1 440 ASA+SA 30 Figure 1.8 Milligrams of Acetylsalicylic Acid CI, and Salicylic Acid , and Combination of Acetylsalicylic Acid and Salicylic Acid II, Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Experimental Beads With Triple Polymer Coating, Incubated in Grape Jelly at 400C for Two Weeks. 400 300 -0-- ASA ---e- SA 200 ASA+SA 100 0 0 240 480 720 960 TIME (MINUTES) 1200 1 440 31 Figure 1.9 Milligrams of Acetylsalicylic Acid 0, and Salicylic Acid 0, and Combination of Acetylsalicylic Acid and Salicylic Acid IS, Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Experimental Beads With Triple Polymer Coating, Incubated in Grape Jelly at 400C for Six Weeks. 500 -0- ASA --*-- SA ASA&SA . 0 1 240 . 1 480 - I 1 720 960 TIME (MINUTES) . 1 1200 1440 32 the intestinal fluid (Figure 1.10). The dissolution of Bayer eight hour tablets give release rates of 0.32 hour-1 in simulated gastric fluid and 0.42 hour-1 in simulated intestinal fluid. The dissolution of measurin displayed much less consistent release rates 0.45-1 in gastric fluid and 0.048 hour-1 in intestinal fluid (Figure 1.11). The experimental formulation approximates a zero order release over the first eight hours or longer depending on the amount of time it has been aged in jelly although first order release rate constants provided better fits (Figure 1.12, Table 1.5). For the experimental formulation, the outer coat protects the enteric coat from becoming damaged while in suspension (11). The enteric coat prevents rapid release in the stomach and the inner coat prevents rapid release in the intestine. This dosage form provides controlled release comparable to the two commercially available solid dosage forms. Chemical degradation of acetylsalicylic acid beads suspended in jelly is retarded, but not sufficiently to allow the beads to be used commercially. For the experimental formulation, 8% of the ASA is released in the first two hours in gastric fluid, which is an improvement in bioavailability to the stomach over enteric coated tablets. ASA is readily absorbed in the stomach compared to the intestines (2). This 8% release may provide immediate beneficial effects of ASA while minimizing the effects of high ASA 33 Figure 1.10 Percent of Total Acetylsalicylic Acid and Salicylic Acid Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Genuine Bayer Aspirin, Immediate Release Tablets 0, and Therapy Bayer Aspirin, Enteric Coated Tablets . -0-- IMMEDIATE -*-- ENTERIC i 0 240 1 i 480 720 960 TIME (MINUTES) i I 1200 1440 34 Figure 1.11 Percent of Total Acetylsalicylic Acid and Salicylic Acid Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Eight Hour Bayer Timed Release Aspirin, Eight Hour Release Tablets 0, and Measurin Timed Release Aspirin, Eight Hour Release Tablets . 120 -0- 8 HOUR -*-- MEASURIN 240 480 720 960 TIME (MINUTES) 1200 1440 35 Figure 1.12 Percent of Total Acetylsalicylic Acid and Salicylic Acid Dissolved in Simulated Gastric Fluid (0-2 hours) and Simulated Intestinal Fluid (2-24 hours) Versus Time From Experimental Beads With Triple Polymer Coating, Incubated in Grape Jelly at 400C for Zero 0, One , Two 0, and Six Weeks U. 120 100 - 80 DRY BEADS ONE WEEK 60 - TWO WEEKS SIX WEEKS I 0 240 .I.I .1.1. 480 720 TIME (MINUTES) 960 1200 1440 36 concentrations in the stomach. The problem of ASA to SA conversion must be addressed in future work to develop a sustained release suspension of ASA. The amount of drug dissolved in gastric fluid is added to the dissolution data in the intestinal fluid. Dissolved ASA in simulated gastric fluid is not transferred to the simulated intestinal fluid. Since the degradation of ASA to SA is not recorded from the gastric fluid after two hours, there is no apparent SA formation for the immediate release tablets which do not release much ASA after two hours. The controlled release formulations which release most of the ASA in the first two hours have little SA formation compared to the enteric coated formulation. The enteric coated tablets show a large amount of SA formation in intestinal fluid as the ASA remains in the intestinal fluid throughout sampling. This may mimic in vivo ASA and SA concentrations in the GI tract since ASA is absorbed rapidly in the stomach. ASA is absorbed relatively slower in the intestines where ASA is degraded to SA at the high intestinal pH. As stated previously some of the ASA would be absorbed in the intestines and so there may not be as much SA present in the intestines as there is in the intestinal fluid during dissolution. The percent of ASA released as SA increases for the experimental formulation, the longer it incubates (40C, 1-6 weeks) in its 37 jelly suspension (Table 1.3). The rate of release from the jelly suspension also increases as the suspension is incubated over longer periods of time (Table 1.4). Future formulations may minimize the amount of SA formation in the beads and transfer of the drug into the jelly through improvements in decreasing the permeability of the enteric coat. 38 REFERENCES Rowland, M., and S. Riegelman. Pharmacokinetics of acetylsalicylic acid and salicylic acid after intravenous administration in man. The Journal of Pharmaceutical Sciences 57(8):1313-1319 (1968). (1) Kergueris, M. F., Bourin, M., Larousse, C., Lasserre, M. P., and A. Ortega. Effects of administration route on pharmacokinetics of aspirin in the rabbit. Methods and Findings in Experimental and Clinical Pharmacology 10(3):171-175 (1988). (2) (3) Alcorn, G., Lucker, P. W., Procaccini, R. L., and W. A. Ritschel. In vivo-in vitro correlations with various aspirin formulations. Methods and Findings in Experimental Clinical Pharmacology 9(11):761-767 (1987). Leonards, J., and G. Levy. Biopharmaceutical aspects of aspirininduced gastrointestinal blood loss in man. The Journal of (4) Pharmaceutical Sciences 58(10):1277-1279 (1969). (5) Frenkel, E. P., McCall, M. S., Douglass, C. C., and S. Eisenberg. Fecal blood loss following aspirin and coated aspirin microspherule administration. The Journal of Clinical Pharmacology Nov-Dec:347-351 (1968). (6) Day, R., Furst, D. E., Dromgoole, S. H., and H. E. Paulus. Changes in salicylate serum concentrations and metabolism during chronic dosing in normal volunteers. Biopharmaceutics & Drug Disposition 9:273-283 (1988). Verstraeten, A., Roets, E., and J Hoogmartens. Quantitative determination by high-performance liquid chromatography of acetylsalicylic acid and related substances in tablets. Journal of (7) Chromatography 388:201-216 (1987). Bell, S., M. Berdick, M. and W. Holliday. Drug blood levels as (8) indices in evaluation of a sustained-release aspirin. The Journal of New Drugs Sep-Oct:284-293 (1966). Tashjian, Jr., A. H., Voelkel. E. F., Lazzaro, M., Goad, D., Bosma, T., and L. Levine. Tumor necrosis factor-alpha (cachectin) stimulates (9) bone resorption in mouse calvaria via a prostaglandin-mediated mechanism. Endocrinology 120(5):2029-2036 (1987). 39 Anti lla, M., P. Kahela, and P. Uotila. The absorption of acetylsalicylic acid from an enteric-coated formulation and the inhibition of thromboxane formation. International Journal of Clinical (10) Pharmacology, Therapy and Toxicology 26(2):88-92 (1988). Mansell, L. New acetaminophen products: formulation development and bioavailability. Ph.D. Thesis, Oregon State (11) University, 11-12 (1990). Hossain, M. and J. W. Ayres. Variables that influence coat integrity in a laboratory spray coater. Pharmaceutical Technology Oct:72(12) 82 (1990). Aarons, L., Hopkins, K., Rowland, M., Brossel, S., and J. F. Thiercelin. Route of administration and sex differences in the pharmacokinetics of aspirin, administered as its lysine salt. Pharmaceutical Research 6(8):660-666 (1989). (13) 40 FORMULATION OF AN ORAL ACETYLSALICYLIC ACID SUSPENSION AND PHARMACOKINETICS OF PARENTERAL THROMBOMODULIN ANALOGUES CHAPTER 2 HIGH DOSE AND LOW DOSE THROMBOMODULIN ANALOGUE PHARMACOKINETICS IN RATS 41 ABSTRACT Pharmacokinetics were determined for a thrombomodulin analogue produced in insect cells through recombinant DNA technology. Anticoagulant activity of the thrombomodulin analogue is a result of inactivation of thrombin in the presence of protein C, protein S, and phospholipid surfaces. The activity of thrombomodulin analogue was measured by the amount of protein C which is activated through an activated protein C assay (APCA). The elimination half life for thrombomodulin analogue activity as determined by APCA ranged from 2.5 minutes to 5.2 minutes for low dose, and high dose respectively. Thrombomodulin analogue pharmacokinetics were also followed using 1251 radiolabel. The curves obtain by following radiolabel were best fit by a biexponential equation. The half life as determined by radiolabel for the initial elimination phase following intravenous administration of 1251 labelled thrombomodulin analogue in rats was 1.5+0.76 and 2.1+0.48 minutes, for low dose and high dose respectively and the 1251 terminal elimination phase tin was approximately 360+130 minutes. Rat bile and urine samples were collected along with the following tissues; heart, lungs, liver, kidney, spleen, brain, and muscle. Less than 1% of the radiolabel appeared in the urine. Radio label in bile indicates that vesicular mediated 42 transcellular transport is occurring. The peak bile concentration of radiolabel occurs at 30 to 45 minutes. Approximately 10% of the radioactivity appeared in the bile. Less than 10% of the radioactivity is found in the remaining tissues which were sampled. 43 INTRODUCTION Thrombomodulin (TM) exists in a soluble form which circulates through the vasculature, and an insoluble form which remains on the vascular endothelium. The entire amino acid sequence of endothelial TM has been determined (1). The structure of soluble TM is unknown although it is presumed to be a cleaved form of endothelial TM (Figure 2.1) (2). TM has been purified from rabbit and human lung, as well as rabbit, bovine, and human placenta (3,4). Human TM has been expressed in COS-1 cells (4). It was initially proposed that there is a difference in activity of rabbit TM (5), bovine TM (6) and human TM (7). The difference in activity may be due to difficulties in removing high molecular weight cationic compounds during purification (8). TM is an endogenous protein which has both anticoagulant and fibrinolytic activity (Figure 2.2). This activity of thrombomodulin is carried out in part by its ability to activate protein C. The fibrinolytic activity of TM is due to activated protein C's direct enzymatic action which lyses fibrin clots. There are three anticoagulant activities of TM; protein C activation, inhibition of thrombin indirectly through antithrombin III, and direct inhibition of thrombin. TM forms a 1:1 complex with thrombin which activates protein C a thousand times faster than thrombin alone (9). TM activates protein C in the presence 44 Figure 2.1 A schematic model showing the five domains in the structure of endothelial thrombomodulin. The amino terminus is followed by a domain which is not homologous with any other known protein. The second domain consists of six repeating epithelial growth factor (EGF) like sequences. The third domain consist of a region with sites for potential glycosylation. The final domain prior to the carboxy terminus is a lipophilic transmembrane domain. NH2 i ( Domains ) ) ) ( ( ) H---' 71L--) c-0---: NH2-terminal EGF-like structures r---*--; 0-glycosylation site-rich transmembrane cytoplasmic COOH (Suzuki, 1987) 45 Figure 2.2 Schematic representation of the coagulation system which forms crosslinked fibrin, and the fibrinolytic system which breaks the crosslinked fibrin into fibrin degradation products. Thrombomodulin acts on the extrinsic pathway, the Xa-Va complex, and thrombin to exhibit anticoagulant activity. Thrombomodulin acts directly on crosslinked fibrin to exhibit fibrinolytic activity. extrinsic intrinsic XIII Val thrombin prothrombin fibrinogen fibrin monomers Xllta fib in polymers Ca"1 fibrin degradation products crosslinked fibrin plasminogen plasmin--a2-anti-plasmin plasminogen activator inhibitor plasminogen activator (Bertina, 1988) 46 of a phospholipid surface, Ca2+, and protein S, providing anticoagulant activity by degrading factors Va and VIIIa. Therefore the TM-thrombin complex does not inhibit clot formation outside blood vessels, while it maintains blood fluidity through anticoagulant and fibrinolytic activity within blood vessels where it is in the presence of cofactor proteins (2). Sustained levels of TM are beneficial to continuously prevent clotting within the vasculature. Unlike other anticoagulants, TM's activity is decreased outside of the vasculature where clotting may be necessary to prevent blood loss. TM provides prophylactic anticoagulant activity while it lyses clots. TM's continuous fibrinolytic and anticoagulant activity in the vasculature is desired since the blood's ability to coagulate is not entirely inhibited by TM and the risk of hemorrhage may be minimized relative to dosing with other anticoagulants. Coagulation problems are a leading cause of acute morbidity. Abnormalities in coagulation can be a result of obstetrical conditions, infections, neoplastic diseases, tissue trauma, and congenital defects. Two classes of drugs are commonly used for coagulation therapy; anticoagulants such as heparin and warfarin which prevent clotting, and fibrinolytic agents such as tissue plasminogen activator and streptokinase which lyse clots. Thrombomodulin provides a novel approach to coagulation therapy because it has both anticoagulant and 47 fibrinolytic activity. Endogenous TM may not be sufficient to regulate the coagulation and fibrinolytic system. Purified TM may be used to diagnose and correct for abnormal levels of endogenous protein C and TM. Protein C abnormalities in a patient may be detected by use of anticoagulant activation with thrombin, TM, or Protac (snake venom). Patients showing lack of anticoagulant activation have an increased risk of thrombosis after surgical procedures (10). TM is also currently being investigated to counteract coagulation problems which occur as a result of tissue trauma. TM may be useful to prevent blood clot formation when used in conjunction with heparin in cardiac bypass surgery (11). Human TM inhibits coagulation by a different mechanism than heparin. Heparin only activates antithrombin III to inhibit thrombin and does not completely inhibit the formation of thrombin. Protein C, protein S, and TM levels decrease during cardiopulmonary bypass surgery. Increase in thrombin is responsible for depletion of the TM induced protein C anticoagulant activity. This decrease promotes clotting. TM and tissue plasminogen activator are both absent in obstructed coronary artery bypass grafts (12). TM is suppressed in bovine aortic endothelium when it is under hypoxic conditions (14). Endothelial cell injury, depletion due to excessive deposition of thrombin, or local proteolysis following 48 endothelial cell damage all may cause a decrease in TM and tissue plasminogen activator levels. TM's activation of protein C is an important regulator of the coagulofibrinolytic system. Presence of excess TM is less likely to result in adverse affects because the presence of other cofactors and enzymes in the coagulation cascade regulate the activity of TM. The active portion of TM consists of six loops, each with a sequence similar to epithelial growth factor (EGF) (Figure 2.1). The fourth, fifth, and six loops of the EGF like structures of TM were suggested to be the minimally active fragment for anticoagulant activity (9). However the same authors show that the first, second, and third loops are also as active as native TM. Therefore the six similar EGF like loops appear to have similar activity. The TM analogue used in this study exhibits anticoagulant and fibrinolytic activity by the same mechanism as native TM as determined by activated protein C assay (APCA). The TM analogue is structurally different than native TM in three ways (Figure 2.1). The TM analogue (M388L) is made with leucine substituted for methionine at the 388th position to prevent loss of activity which occurs if methionine is oxidized. M388L is missing the lipophilic transmembrane portion that attaches native endothelial thrombomodulin to the vasculature. Finally, glycosylation of M388L is 49 different than native TM because M388L is produced through recombinant techniques. The purpose of this research was to evaluate M388L pharmacokinetics including determination of the routes of distribution and elimination for M388L. This is accomplished through 1251 radiolabelling and the use of APCA. Understanding the pharmacokinetics of this M388L will increase the therapeutic options available for prevention of thrombosis and for dealing with emboli. 50 MATERIALS AND METHODS PREPARATION OF THROMBOMODULIN. Human thrombomodulin (TM) analogue (M388L) with leucine substituted for methionine at the 388th amino acid position was prepared using an insect cell line to prevent oxidation and loss of activity. Since the recombinant M388L was produced in insect cells, glycosylation of the protein is different than native human thrombomodulin. M388L is missing the lipophilic portion which is found in native endothelial TM. M388L was analyzed by gel electrophoresis to ensure that there were no contaminating compounds. RADIOIODINATION OF THROMBOMODULIN. M388L was radiolabelled with 1251 to give a specific activity of 2 to lOuCi/ug. Purity was determined by polyacrylamide gel electrophoresis. Pharmacological activity was measured as the ability of M388L to activate Protein C as determined by the activated protein C assay described later. ANIMAL EXPERIMENTS. Male Sprague Dawley Rats 280-300g, 65-75 days old, were 51 maintained on Wayne Rodent Blocks (Harlan Sprague Dawley). The rats were anesthetized with an interperitoneal (IP) injection of sodium pentobarbital, 6-7.5mg/100g body weight. Maintenance doses were given IP, 1mg/100g body weight, as needed to insure full anesthesia during all procedures. Euthanasia was by exsanguination without the rat ever regaining consciousness. Surgery began each morning between 9AM and 12PM. A polyethylene cannula (PE-10, Clay Adams) was inserted into the bile duct through a 3-4cm abdominal incision. The incision was then clamped and kept moist throughout the procedure with gauze soaked in normal saline. Another cannula (PE50) was placed in the right femoral artery. One hundred units of heparin were injected into rats where protein C activation by M388L was not measured. Non-radiolabelled M388L was sampled without the use of heparin. A rapid 0.1m1 burst of saline into the cannula was usually all that was necessary to clear the cannula. The cannula was gradually inserted further into the artery to break clotting when necessary in unheparinized rats where protein C activation by M388L was measured. The rat was placed in a supine position on a heating pad under a heating lamp to maintain 380C body temperature. The M388L dose was administered through the arterial cannula followed by 1m1 of 0.9% saline. M388L was injected into four rats at a low dose (0.2ug/rat) or at a 52 high dose (10Oughat). The M388L was stored in phosphate buffered saline with 0.1% bovine serum albumin. For low dose samples, 0.2ug of radiolabelled M388L was diluted with 0.5m1 0.9% saline immediately prior to injection. For high dose an additional 10Oug of unlabeled M388L (1mg/m1) was added to 0.2ug of radioactive M388L immediately prior to injection. For samples where protein C activity of M388L was measured, 500, 250, 100, 50, 25, or bug total M388L was injected was injected into four rats for each dose. Bile was collected continuously and blood was sampled at -1, 1, 2, 4, 5, 6,10, 20, 30, 45, 60, 75, 90, 105, 120, 150, 180, 210, and 240 minutes for all doses. The volume of blood sampled was replaced with 0.9% normal saline. Upon completion of bile and blood collection the rat was exsanguinated. One rat each was sacrificed at one, two, three, or four hours of elapsed time after dosing M388L. Urine and tissue samples were collected upon completion of the 1-4 hour study period. Liver and kidneys were weighed and portions of each were collected for sampling. Spleen, heart, lung, brain, and urine were collected in their entirety and a small weighed portion of thigh muscle was sampled. Sacrificing animals one hour apart allowed observation of distribution of radiolabel in tissues over time. 53 ASSAY METHOD, RADIOLABELLED THROMBOMODULIN 1251 radioactivity in blood, bile, urine, and tissues was measured using an automated gamma counter (Beckman Gamma 4000, 74.9% efficiency). Each sample was counted for one minute. Counts per minute for each sample were compared to counts per minute for the initial M388L dose injected, after subtracting the background in each case. This resulting fraction of the dose was then corrected for the weight of the tissue or fluid sample. Radio labelled bovine serum albumin (BSA) was found in early M388L preparations and pharmacokinetic curves obtained from these radiolabelled M388L samples were mathematically corrected for radiolabelled BSA (Appendix). These data are compared to M388L pharmacokinetics determined from doses free of BSA. BSA presence was necessary in M388L solutions to prevent adsorption of M388L onto the container walls. In early studies, BSA was inadvertently radiolabelled along with the M388L. Later, M388L was radiolabelled separately, and gel electrophoresis was used to show that M388L is the only source of radiolabel in all M388L pharmacokinetics reported outside of the Appendix. 54 THROMBOMODULIN ACTIVITY (ACTIVATED PROTEIN C ASSAY). Heparin was not administered to rats providing samples for activated protein C assay (APCA) because heparin interferes with measurement of thrombomodulin activity through the APCA. Blood samples were diluted 1:20 in phosphate buffered saline containing 0.5% bovine serum albumin and centrifuged immediately following collection. Supernatant liquids of blood and the entire bile samples were frozen in dry ice acetone and packed in dry ice for later analysis. Activation of protein C by M388L is measured according to the following assay. Thrombin and protein C are dissolved in 20mM Tris HCL, 0.1M NaC1, 2.5mM CaC12, and BSA (5mg/m1) at pH 7.4. Twenty microliters each of sample, thrombin, 3nM (Sigma), and protein C, 0.5uM (Genzyme) are mixed and incubated for 60 minutes at 37°C. Hirudin, 20u1, 0.16units/m1 (American Diagnostica) is then added and the mixture is incubated at 37°C for 15 minutes to stop the protein C activation. Chromogenic substrate 52266,100u1, 1.0mM (Kabi Vitrum) is then added and absorbance measured every sixty seconds at 405nm for 15 minutes. The change in absorbance per minute is proportional to the concentration of activated protein C. Standard protein C activation rates are determined from a single batch of insect cell line M388L (64units/m1) manufactured on site. 55 CALCULATIONS The number of micrograms of each dose administered was determined by APCA. The activity was compared to the activity per microgram of a single batch of insect cell line M388L. The fraction of radioactivity or protein C activity at each timepoint is compared to the activity of the dose injected. The activity of the dose injected, in each rat, is determined by taking a small sample of blood from each rat prior to dosing and mixing the blood with an amount of M388L which is proportional to the entire dose administered in 20m1 of blood. The activity of the single batch of insect cell line M388L in each rats blood was not determined and so the amount of M388L remaining in the blood over time is not able to be calculated. Background radioactivity and protein C activity for each rat's serum is subtracted from the activity of that rat's samples. The parameters for protein C activity pharmacokinetics of the thrombomodulin analogue were calculated using PCNONLIN (Modified Newton-Gauss method). 56 RESULTS AND DISCUSSION The pharmacokinetics of M388L are evaluated via the 1251 label pharmacokinetics and the ability of M388L to activate protein C. The volume of blood in each rat is estimated at approximately 20m1 based on body weight. This volume is used to calculate the total radiolabel remaining in blood over time. The pharmacokinetics of M388L's protein C activation over time (Figure 2.3, Table 2.1) at five doses in the blood (10, 20, 50, 100, and 200ug) can be compared to radiolabelled thrombomodulin analogue over time (Figure 2.4, Table 2.2). Figure 2.5 and Table 2.3 show the APCA activity relative to the counts per minute of 1251 in the blood after M388L was administered to a single rat. 1251 radioactivity clearance from rat plasma lags the clearance of activation of protein C after 5-10 minutes. This may be due to radiolabel becoming detached from M388L or the M388L becoming inactivated. The M388L half lives as determined by following the radiolabel or protein C activation assay of the initial elimination phase and the terminal elimination phase are listed in Table 2.4. There is a single exponential fit for the M388L's profile as assayed by protein C activation. After 60 minutes the activity approaches 1% of the initial activity (Figure 2.3, Table 2.1). The M388L's ability to cause protein C 57 Figure 2.3 The fraction of initial protein C activation versus time curves for ten rats receiving 10, 20, 50, 100, or 200 micrograms of thrombomodulin with leucine substituted for methionine at the 388th position. Protein C activation before dosing is subtracted from protein C activation after dosing and the differences are used in calculating the fraction of initial protein C activation at each timepoint. M388L bug M388L bug -CI- M388L 2Oug M388L 2Oug M388L 5Oug M388L 5Oug M388L 10Oug M388L 10Oug M388L 100ug M388L 200ug 17. z .001 0 20 40 60 80 TIME (MINUTES) 100 120 140 58 Table 2.1 The fraction of initial protein C activation over time + standard deviations for rats receiving thrombomodulin with leucine substituted for methionine at the 388th position (M388L). Time (minutes) 0 200ug n=1 10Oug 5Oug 2Oug n=3 n=2 n=2 10ug n=2 1.00 1.00 1.00 1.00 1.00 2 5 0.54 7 10 Dose Administered 0.096 15 0.91+0.33 0.78+0.09 0.71+0.08 0.72+0.12 0.65+0.11 0.60+0.09 0.54+0.00 0.65+0.09 0.51+0.16 0.40+0.04 0.36+0.02 0.37+0.04 0.24+0.19 0.33+0.01 0.28+0.04 0.21+0.07 0.28+0.07 0.30+0.09 0.16+0.07 0.17+0.11 20 0.033 0.11+0.06 0.15+0.01 0.16+0.09 0.05+0.00 30 0.015 0.03+0.02 0.04+0.02 0.04+0.00 0.05+0.00 45 0.008 0.01+0.01 0.02+0.02 0.03 0.05+0.00 60 0.006 0.01+0.00 0.01+0.01 0.01 0.05+0.00 59 Figure 2.4 Average fraction of initial radiolabel remaining from 1251 thrombomodulin analogue for low dose (0.2ug) , and high dose administered. (n=4 for each dose) (10Oug) 1 CO LL OJ Z- LOW DOSE 17:a CC HIGH DOSE O0 - -I .< UCC .1 0 10 20 30 TIME(MINUTES) 40 50 60 60 Table 2.2 Average fraction + standard deviations of initial radiolabel remaining in the blood from 1251 thrombomodulin analogue (M388L) for low dose and high dose. Time (minutes) 2 Dose Administered High Dose (10Oug) n=4 0.62+0.10 Low Dose (0.2ug) n=4 0.42+0.08 5 0.32+0.03 0.21+0.03 10 0.16+0.03 0.12+0.02 20 0.15+0.01 0.15+0.01 30 0.15+0.01 0.14+0.01 45 0.14+0.01 0.12+0.01 60 0.13+0.01 0.12+0.01 61 Figure 2.5 Fraction of initial protein C activation CI remaining over time and fraction of initial radiolabel remaining over time for a rat which was administered 200 micrograms of thrombomodulin with leucine substituted for methionine at the 388th position. CI . l i 20 40 - protein C activation radiolabel 1 1 60 80 TIME(MINUTES) . 1 100 120 62 Table 2.3 Fraction of thrombomodulin analogue (M388L) remaining as determined by 1251 radiolabel and activated protein C assay (APCA) for a rat which received 200ug of thrombomodulin analogue with leucine substituted for methionine at the 388th position. Time (minutes) 1251 Radio label APCA 0 1.00 1.00 5 0.46 0.54 10 0.20 0.10 20 0.15 0.03 30 0.15 0.01 45 0.13 0.01 60 0.11 0.01 90 0.09 0.00 120 0.10 0.01 63 Table 2.4 Radioactivity (1251) half life times in minutes following low dose (0.2ug, n=4) and high dose (10Oug, n=4) of thrombomodulin analogue as determined by monoexponential and biexponential curve fitting. Monoexponential half lives as determined by activated protein C assay (APCA). The APCA half lives are the range. Standard deviations are given in parentheses. Calculated using RSTRIP. MONOEXPONENTIAL (minutes) 1251 HIGH LOW APCA HIGH LOW Average 33(12) 39(10) 5.2 2.5 3.3(0.80) BIEXPONENTIAL (minutes) 2.1(0.48) 1.5(0.76) 700(140) 360(130) * * * * 64 activity fluctuates between 0.5% and 1% of the initial activation for hours after the dose is administered. The standard deviation for most points include the baseline however the difference between the protein C activation and baseline is statistically significant (p<0.01) when performing a rank sum test. For the radiolabelled low dose M388L, the half life of the initial elimination phase was 1.5+0.76 minutes and the half life of the terminal elimination phase was 360+130 minutes when fitted to a biexponential curve (r2=0.987). For the radiolabelled high dose TM analogue the initial elimination phase was 2.1+0.48 minutes and the terminal elimination phase was 700+140 minutes when fitted to a biexponential curve (r2=0.998). The radioactivity elimination half lives vary greatly among rats, 220 to 530 minutes for low dose rats, and 410 to 870 minutes for high dose rats. The radioactivity is different at 2 minutes (p<0.01) and at 5 minutes (p<0.05) for low dose and high dose radiolabelled M388L. There is no significant difference between low dose and high dose pharmacokinetics of radioactivity for points after 60 minutes (p<0.5). The M388L half life as assayed by protein C activation also increases slightly with increased TM analogue concentration administered. This curve is best fit by a single exponential. The elimination half life of TM analogue as assayed by protein C activation is 2.5 minutes for 10ug administered and increases gradually with increasing dose administered to 5.2 minutes for 10Oug with the average 65 r2 value equal to 0.979. These initial elimination phase half lives are shorter than those reported by Erlich (3) who administered thrombomodulin to rabbits. Erlich reported a 18 minute half life for the radiolabel and 20 and 12 minutes half lives for the thrombin clotting time and activated partial thromboplastin time respectively. This discrepancy may be due to the different number of timepoints sampled by Erlich, 5 and 30 minutes compared to 1, 2, 4, 5, 6, 10, 20, and 30 minutes sampled in this experiment. Alternatively this difference may be due to use of rabbits instead of rats or a difference in the TM used. Erlich administered 200ug/kg which would be equivalent to 6Oug for the rats used in this experiment. The elimination phase half lives are approximately the same for M388L in rats (360 minutes) and thrombomodulin in rabbits (385 minutes) when measuring radiolabel. When measuring TM analogue by activation of protein C it is difficult to detect a decrease in activity in rats after 60 minutes post dose. The half life of mouse tissue thrombomodulin in mice is nine minutes. The elimination in mice was largely due to hepatic clearance as indicated by its initial distribution in the liver and then accumulation in the intestine (14). Figure 2.4 and Table 2.2 show that 80-90% of circulating radiolabel in the blood has disappeared after 10 minutes. There is an initial elimination phase with a one to two minute half life followed 66 by a long terminal elimination phase with a half live of 360 to 700 minutes for the radiolabel. The terminal elimination of low dose M388L is the same as elimination of high dose M388L (the r squared value increases when combining the two elimination phases) even though the terminal elimination rates when calculated for individual rats vary from 220 to 880 minutes. This variation in calculated elimination half life is due to the low number of timepoints between one and four hours and the lack of sampling after four hours. Figure 2.6 and Table 2.5 show that peak bile concentration of radiolabelled M388L occurs at 30-45 minutes. This time to peak is consistent with vesicular mediated transcellular transport (VMTT) in the liver (15). The observed rapid alpha elimination phase is partially due to VMTT clearing the radiolabel on the first pass. This is also consistent with the levels of radiolabel found in the liver (Figure 2.7). The only non passive way for the liver to clear the radiolabel more rapidly is by receptor mediated transport (13). Each point on the bile curve represents the fraction of the initial dose released in bile per hour. Only 30% of M388L radioactivity was accounted for in the blood, bile, urine and tissues sampled after the first 60 minutes. The weights of tissue collected relative to body weight are in Table 2.6. The tissues collected include the liver, spleen, kidney, brain, heart, lung, brain, and muscle. Approximately 10% of the radiolabel is 67 Figure 2.6 Fraction of radiolabel from 1251 labelled thrombomodulin analogue which appears in the bile at low doses (0.2ug) 0, and high doses (1 0Oug) O. Each point represents data from up to four rats. 0.02 0.01 - 0.00 0 1 1 30 60 1 1 120 150 1 90 TIME(MINUTES) 180 68 Table 2.5 Fraction of initial radiolabel from 1251 labelled thrombomodulin analogue (M388L) which appears in the bile at high doses (10Oug) and low doses (0.2ug). Each timepoint represents data from up to four rats. Time (minutes) Dose Administered High Dose (10Oug) Low Dose (0.2ug) 5 0.0014+0.0002 0.0015+0.0005 15 0.0089+0.0013 0.0090+0.0053 25 0.0158+0.0025 0.0154+0.0027 37 0.0163+0.0025 0.0148+0.0018 52 0.0141+0.0027 0.0183+0.0108 75 0.0120+0.0012 0.0109+0.0002 97 0.0112+0.0009 112 0.0098+0.0004 127 0.0093+0.0002 142 0.0088+0.0000 157 0.0086+0.0000 172 0.0084+0.0005 69 Figure 2.7 Fraction of radiolabel from 1251 labelled thrombomodulin analogue found in tissues following sacrifice of high dose rats (10Oug). Four rats were sacrificed one hour apart at 1, 2, 3, or 4 hours. 0.05 -J w u- 0 0.04 co -1 Z 0 0.03 0g 0 cc cc I u- < E 60 minute M 120 minute M 180 minute ta 240 minute 0.02 0.01 0.00 liver kidney spleen heart TIME(MI MUTES) lung brain urine muscle 70 Table 2.6 Each tissue collected represents the following percent of total body weight. TISSUES COLLECTED TISSUE % BODY WEIGHT* LIVER KIDNEY SPLEEN HEART LUNG 2.3 3.6 0.63 - 0.89 0.13 0.20 0.26 - 0.37 0.27 0.40 0.32 0.43 BRAIN *tissue weight divided by total body weight of rat 71 recovered in the tissues, 5% is removed while sampling blood, less than 10% is found in the bile, 1% is found in the urine, and 10% remains in the blood after two to four hours. Nearly two thirds of the radiolabel remains in the unsampled tissues of the rat. Results from the tissues sampled over time are shown in Figure 2.7 and Table 2.7. M388L is rapidly eliminated within the first ten minutes after IV administration. Future research may enable TM analogues to become clinically useful by modification of the molecule to increase the duration of protein C activation. 72 Table 2.7 Fraction of radiolabel from 1251 labelled thrombomodulin analogue (M388L) found in tissues following sacrifice of high dose rats (10Oug). Four rats were sacrificed one hour apart at 1, 2, 3, and 4 hours. Time of sacrifice Tissue 1 hour 2 hours 3 hours 4 hours liver 0.048 0.041 0.025 0.031 kidney 0.026 0.016 0.013 0.013 spleen 0.003 0.002 0.001 0.001 heart 0.002 0.002 0.001 0.001 lung 0.004 0.004 0.003 0.003 brain 0.001 0.001 0.000 0.000 urine 0.000 0.001 0.008 0.009 muscle 0.001 0.001 0.001 0.001 73 REFERENCES Suzuki, K., Hayashi, T., Nishioka, J., Kosaka, Y., Zushi, M., Honda, G., and S. Yamamoto. Structure and expression of human (1) thrombomodulin, a thrombin receptor on endothelium acting as a cofactor for protein C activation. The EMBO Journal 6(7):1891-1897 (1987). Dittman, W., and P. Majerus. Structure and function of thrombomodulin: a natural anticoagulant. Blood 75(2):329-336 (1990). (2) Erlich, H., Esmon, N., and N. Bang. In vivo behavior of detergent-solubilized purified rabbit thrombomodulin on intravenous (3) injection into rabbits. T. Lab. Clin. Med. 115(2):182-189 (1990). Zushi, M., Gomi, K., Yamamoto, Maruyama, I., Hayashi, T., and (4) K. Suzuki. The last three consecutive epidermal growth factor-like structures of human thrombomodulin comprise the minimum functional domain for protein C-activating cofactor activity and anticoagulant activity. The 'journal of Biological Chemistry 264(18):10351-10353 (1989). (5) Bourin, M., Oh lin, A. K., Lane, D. A., Stenflo, J., and U. Lindahl. Relationship between anticoagulant activities and polyanionic properties of rabbit thrombomodulin. The Journal of Biological Chemistry 263(17):8044 -8052 (1986). Jakubowski, H., and W. Owen. Macromolecular specificity (6) determinants on thrombin for fibrinogen and thrombomodulin. The Journal of Biological Chemistry 264(19):11117-11121 (1989). (7) Esposito, C., Gerlach, H., Brett, J. Stern, D., and H. Vlassara. Endothelial receptor-mediated binding of glucose-modified albumin is associated with increased monolayer permeability and modulation of cell surface coagulant properties. T. Exp. Med. 170:1387-1407 (1989). (8) Preissner, K. T., Koyama, T., Muller, D. Tschopp, J., and G. Muller-Berghaus. Domain structure of the endothelial cell receptor thrombomodulin as deduced from modulation of its anticoagulant functions. The Journal of Biological Chemistry 265(9):4915-4922 (1990). 74 Gomi, K., Zushi, M., Honda, G., Kawahara, S., Matsuzaki, 0., Kanabayashi, T., Yamamoto, S., Maruyama, I., and K. Suzuki. (9) Antithrombic effect of recombinant human thrombomodulin on thrombin-induced thromboembolism in mice. Blood 75(7):1396-1399 (1990). Vasse, M., J. Borg, and M. Monconduit. Protein C: Rouen, a new hereditary protein C abnormality with low anticoagulant but normal (10) amidiolytic activities. Thrombosis Research 56:387-398 (1989). Tanaka, K., Wada, K., Morimoto, T., Shomura, S., Satoh, T., Yada, I., Yuasa, H., Kusagawa, M., and K. Deguchi. The role of the (11) protein C-thrombomodulin system in physiologic anticoagulation during cardiopulmonary bypass. Trans. Am. Soc. Artif. Intern. Organs 35:373-375 (1989). (12) Brody, J., N. Pickering, and G. Fink. Abnormalities of thrombomodulin and tissue plasminogen activator in occluded aortocoronary grafts detected by immunohistochemistry. Trans-Assoc- Am-Physicians 101:79-87 (1988). (13) Ogawa, S., H. Gerlach, C. Esposito, A. Pasagian-Macaulay, J. Brett, and D. Stern. Hypoxia modulates the barrier and coagulant function of cultured bovine endothelium. I. Clin. Invest. 85:1090-1098 (1990). Kumada, T., Dittman, W. A., and P. W. Majerus. A role for thrombomodulin in the pathogenesis of thrombin-induced thromboembolism in mice. Blood 71(3):728-733. (14) Ashwell, G. and J. Harford. Carbohydrate specific receptors of the liver gluconeogenesis and related aspects of glycolysis. Ann. Rev. (15) Biochem. 51:531-554 (1982). 75 FORMULATION OF AN ORAL ACETYLSALICYLIC ACID SUSPENSION AND PHARMACOKINETICS OF PARENTERAL THROMBOMODULIN ANALOGUES CHAPTER 3 CONJUGATION OF THROMBOMODULIN ANALOGUE WITH POLYETHYLENE GLYCOL TO INCREASE THE HALF LIFE IN THE BLOOD 76 ABSTRACT Thrombomodulin analogue activities were monitored by measuring radiolabel 1251 and activation of protein C in the blood. Thrombomodulin analogue exhibits a rapid initial elimination phase of 1-2 minutes when following the radiolabel of 1251 labelled thrombomodulin analogue, and 5-7 minutes when following protein C activation. The thrombomodulin analogue was conjugated to polyethylene glycol (PEG). The PEG conjugation resulted in conjugates with three different activities relative to the unconjugated thrombomodulin analogue. The different change in activity may be due to PEG blocking the active site of the thrombomodulin analogue. The difference in activities between the thrombomodulin analogue conjugates may be due to different amounts of PEG conjugation. Two PEG conjugates with 50% and 70% of initial thrombomodulin analogue activity were monitored using radiolabel. The conjugate with the larger decrease in activity relative to unconjugated thrombomodulin analogue exhibited the longer half life. For the PEG conjugate with 70% of initial thrombomodulin activity, as determined by 1251, had a half life for the initial elimination phase of 3.76+1.96 and the terminal elimination 77 phase half life was 90.7+28.0. For the PEG conjugate with 50% of initial thrombomodulin activity, as determined by 1251, had a half life for the initial elimination phase of 3.45+1.79 and the terminal elimination phase half life was 139+33.2. The elimination of the conjugate with 50% of thrombomodulin analogue activity was best fit by a single exponential with a half life of 60+1.1 and 80+6.2 minutes as determined by protein C activation assay for the two doses administered, 2Oug and 5Oug respectively. 78 INTRODUCTION Polyethylene glycol conjugation has been used successfully to increase the half lives of many proteins. The conjugation of PEG to proteins has the additional benefit of decreasing the immunogenicity of proteins however a decrease in the activity in many proteins is also observed. Bovine liver catalase (1), superoxide dismutase, lactoferrin and alpha macrogloblin (2), urate oxidase (3), adenosine deaminase (4), interleukin 2 (5), alpha proteinase inhibitor (6), and superoxide dismutase (7) have apparent increased plasma concentrations over time when conjugated with polyethylene glycol compared to that of the native protein. Decreased immunogenicity was demonstrated for urate oxidase (3), adenosine deaminase (4), bovine liver catalase (1), phenylalanine ammonia lyase (8), bovine liver arginase (9), bovine serum albumin (10), and superoxide dismutase (7) when conjugated to polyethylene glycol. Decreased activity was reported for urate oxidase (3), interleukin 2 (5), and alpha proteinase inhibitor (6) when conjugated with PEG. Sufficient activity remains with some PEG conjugates so that the protein remains clinically effective (7,8). A successful method of increasing half life of thrombomodulin analogue was found by conjugation of polyethylene glycol (PEG) to the analogue at lysine, tyrosine and the terminal amine positions. Two 79 different radiolabelled PEG linked thrombomodulin analogue (PEGM388L) samples with different unquantified numbers of PEG attachment and quantified anticoagulant activity were tested. One PEG conjugate was monitored through its activation of protein C. The purpose of this research was to evaluate PEG-M388L pharmacokinetics to detemine if clearance of M388L could be decreased through conjugation with PEG. Sustained protein C activity in the blood will increase the duration of fibrinolytic and anticoagulant activity thereby decreasing thrombosis. By increasing the half life in the blood of a M388L through conjugation with PEG a thrombomodulin analogue may be found that is therapeutically more useful than co-administration of both an anticoagulant and a fibrinolytic agent. 80 MATERIALS AND METHODS PREPARATION OF THROMBOMODULIN. Human thrombomodulin (TM) analogue (M388L) with leucine substituted for methionine at the 388th amino acid position was prepared using an insect cell line to prevent oxidation and loss of activity. Since the recombinant M388L was produced in insect cells, glycosylation of the protein is different than native human thrombomodulin. M388L is missing the lipophilic portion which is found in native endothelial TM. M388L was analyzed by gel electrophoresis to ensure that there were no contaminating compounds. PREPARATION OF THROMBOMODULIN CONJUGATES M388L was conjugated to polyethylene glycol by incubation of the TM analogue with paranitrophenol polyethylene glycol (Sigma, 4000MW). Two conjugates were used one conjugate had 50% of M388L activity (PEG-M388L-50) and the other conjugate had 70% of M388L activity (PEG-M388L-70). RADIOIODINATION OF THROMBOMODULIN. Thrombomodulin analogue was radiolabelled with 1-125 to give 81 a measurable specific activity of at least ten times background at 1/10,000th of the dose. Purity was determined by gel electrophoresis. Pharmacological activity was measured by the ability of the thrombomodulin in the sample to activate Protein C as determined by the activated protein C assay described later. ANIMAL EXPERIMENTS Male Sprague Dawley Rats 280-300g, 65-75 days old, were maintained on Wayne Rodent Blocks (Harlan Sprague Dawley). The rats were anesthetized with an interperitoneal (IP) injection of sodium pentobarbital, 6-7.5mg/100g body weight. Maintenance doses were given, 1mg/100g body weight, as needed to insure full anesthesia during all procedures. Euthanasia was by exsanguination without the rat ever regaining consciousness. Surgery began each morning between 9AM and 12PM. A polyethylene cannula (PE-10, Clay Adams) was inserted into the bile duct. Another cannula (PE-50) was placed in the right femoral artery. One hundred units of heparin were injected into rats when protein C activation by M388L or PEG-M388L was not measured. Non-radiolabelled blood samples of the M388L or PEG- M388L were taken from animals without the use of heparin. A rapid 0.1m1 burst of saline into the cannula was usually all that was necessary to clear the cannula. The cannula was gradually inserted 82 further into the artery to break clotting when necessary in unheparinized rats where M388L or PEG-M388L was measured by protein C activation. The rat was placed in a supine position on a heating pad under a heating lamp to maintain 380C body temperature. The M388L or PEG-M388L dose was administered through the arterial cannula followed by 1m1 of 0.9% saline. M388L or PEG-M388L were injected into four rats at a low dose (0.2ug) or at a high dose (10Oug). The M388L or PEG-M388L was stored in phosphate buffered saline with 0.1% bovine serum albumin. For low dose samples, 0.2ug of radiolabelled M388L or PEG-M388L was diluted with 0.5m1 0.9% saline immediately prior to injection. For high dose an additional 10Oug of unlabeled M388L or PEG-M388L was added immediately prior to injection. For samples where protein C activity of M388L or PEG-M388L was measured, 100, 50, 20, or 10ug total M388L or PEG-M388L was injected. For the protein C activation assay (APCA) two rats were used for each of four doses. Bile was collected continuously and blood was sampled at -1, 1, 2, 4, 5, 6, 10, 20, 30, 45, 60, 75, 90, 105, 120, 150, 180, 210, and 240 minutes for all doses. The volume of blood sampled was replaced with 0.9% normal saline. Upon completion of bile and blood collection the rat was exsanguinated. One rat each was sacrificed at one, two, three, or four hours of elapsed time for each M388L or PEG-M388L dosing. Urine and 83 tissue samples were collected upon completion of the 1-4 hour study period. Liver and kidneys were weighed and portions of each were collected for sampling. Spleen, heart, lung, brain, and urine were collected in their entirety and a small portion of thigh muscle was sampled. Sacrificing animals one hour apart allowed observation of distribution of radiolabel in tissues over time. ASSAY METHOD FOR RADIOLABELLED THROMBOMODULIN 1251 radioactivity in blood, bile, urine, and tissues were measured using an automated gamma counter (Beckman Gamma 4000, 74.9% efficiency). Each sample was counted for one minute. Counts per minute for each sample were compared to counts per minute for the initial M388L or PEG-M388L dose injected, after subtracting the background in each case. This resulting fraction of the dose was then corrected for the different weight of the tissue or fluid sample. THROMBOMODULIN ACTIVITY (ACTIVATED PROTEIN C ASSAY) Heparin was not administered to rats providing samples for the activated protein C assay (APCA) because of heparin interference with the measurement of thrombomodulin (TM) activity through the APCA activation. Blood samples were diluted 1:20 in phosphate buffered saline containing 0.5% bovine serum albumin and 84 centrifuged immediately following collection. Supernatant liquids of blood and the entire bile samples were frozen in dry ice acetone and packed in dry ice for later analysis. Activation of protein C by M388L or PEG-M388L is measured according to the following APCA. Thrombin and protein C are dissolved in 20mM Tris HCL, 0.1M NaC1, 2.5mM CaC12, and BSA (5mg/m1) at pH 7.4. Twenty microliters each of sample, thrombin, 3nM (Sigma), and protein C, 0.5uM (Genzyme) are mixed and incubated for 60 minutes at 37°C. Hirudin, 20u1, 0.16units/m1 (American Diagnostica) is then added and the mixture is incubated at 37°C for 15 minutes to stop the protein C activation. Chromogenic substrate S2266,100u1, 1.0mM (Kabi Vitrum) is then added and absorbance measured every sixty seconds at 405nm for 15 minutes. The change in absorbance per minute is proportional to the concentration of activated protein C. The results are reported in change in mOD per minute as well as the fraction of the change in initial mOD per minute over time. Standard protein C activation rates are determined from a single batch of insect cell line M388L (64units /ml) manufactured on site. CALCULATIONS The number of micrograms of each dose administered was determined by APCA. The activity was compared to the activity per 85 microgram of a single batch of insect cell line M388L. The fraction of radioactivity or protein C activity at each timepoint is compared to the activity of the dose injected. The activity of the dose injected is confirmed by taking a small sample of blood from each rat prior to dosing and mixing the blood with an amount of M388L or PEG-M388L which is proportional to the entire dose administered in 20m1 of blood. The activity of the single batch of insect cell line M388L in each rats blood was not determined and so the amount of M388L PEG-M388L remaining in the blood over time is not able to be calculated. Background radioactivity and protein C activity for each rat's serum is subtracted from the activity of that rat's samples. The parameters for protein C activity pharmacokinetics of the thrombomodulin analogue were calculated using PCNONLIN (Modified Newton-Gauss method). 86 RESULTS AND DISCUSSION Paranitrophenol polyethylene glycol 4000 was conjugated to M388L produced in insect cells. Conjugation of PEG to M388L may occur with the lysine and tyrosine residues as well as the amino terminus of proteins. The seven tyrosine residues found in soluble thrombomodulin are located at the 288 and 296 positions of the second loop, at the 334 and 337 position of the third loop, at the 358 and 368 position of the fourth loop and at the 413 position of the fifth loop. There are no tyrosine residues in the first or sixth loop. Following optimization of the procedure for conjugation of the PEG, 30-50% of the M388L activity is lost. Treatment of the PEG conjugated M388L with hydroxylamine to remove the PEG groups restored the anticoagulant activity, demonstrating that no irreversible damage to the active fragment occurred. The conjugate which retained 70% activity (PEG-M388L-70) was used in radiolabel studies only. The conjugate which retained 50% activity (PEG-M388L-50) was followed both with 1251 radiolabel and activated protein C assay (APCA). The half lives for M388L and PEG-M388L are listed in Table 3.1. PEG-M388L-50 was administered in four replicates of two doses and the M388L was administered in two replicates of four doses. The half lives decrease with decreasing dose. Thrombomodulin activity may 87 Table 3.1 Half lives in minutes (T1/2) and areas under the curve in mOD/minute versus minutes (AUC) as determined by protein C activity for thrombomodulin analogue with methionine converted to leucine at the 388th position and for the polyethylene glycol conjugate of the thrombomodulin analogue. Standard deviations are in parentheses. The parameters were calculated using PCNONLIN (Modified Newton-Gauss Method). M388L PEGM388L-50 T1/2 10 7.21(0.242) 6.79(1.09) 5.68(0.294) 5.39(0.0241) AUC* 200(8) 80(3) 40(3) 20(1) 50 20 82.5(6.22) 61.2(1.06) 4000(400) 2000(100) DOSE 100ug 50 20 *based on mOD/min which is proportional to activity 88 measured by the activation of protein C through use of an APCA. The mOD/minute values are proportional to activation of protein C. Activated protein C cleaves a substrate used in the assay to cause a change in absorbance which provides mOD/minute values which are proportional to the concentration of activated protein C. Figure 3.1 shows the average values at each time point for each dose of M388L and PEG-M388L administered. Table 3.2 shows the average values at each timepoint for each dose of PEG-M388L and Table 2.1 shows the average values at each timepoint for each dose of M388L. Figure 3.2 shows the fraction of the initial radiolabel remaining in the blood over time for 1251 radiolabelled M388L and PEG-M388L. The parameters calculated from radiolabelled M388L and PEG-M388L are shown in Table 3.3. The data used to calculate the parameters in Table 3.3 are given in Table 3.4 and Table 2.2. The radiolabel in the blood over time curve is best fit by a biexponential equation. The terminal elimination phase of the biexponential equation does not represent active M388L in the case of unconjugated M388L as shown by the APCA. This terminal elimination phase levels off at approximately 10% of the initial injected radiolabel. The terminal elimination phase of the PEG-M388L remains above 50% of the initial radiolabel injected for over four hours. This terminal elimination phase is reflected in the APCAs. 89 Figure 3.1 Fraction of initial protein C activation remaining over time for four doses of thrombomodulin analogue (n=2) and two different doses of PEG conjugate analogue (n=4). Thrombomodulin analogue is administered at 10ug 0, 2Oug , 5Oug II, and 10Oug 0. PEG conjugated thrombomodulin analogue is administered at 2Oug , and 5Oug A. 100 PEG 2OUG PEG 5OUG M388L 1OUG M388L 2OUG M388L 5OUG M388L 100UG .01 0 20 40 60 TIME (MINUTES) 80 90 Table 3.2 The fraction of initial protein C activation over time + standard deviations for rats receiving thrombomodulin with leucine substituted for methionine at the 388th (M388L) position conjugated with PEG. The conjugate retained 50% of the initial M388L activity. (n=4) Time (minutes) Dose Administered 1 5Oug 0.910+0.127 2Oug 0.809+0.128 2 0.807+0.121 0.948+0.073 4 0.627+0.280 0.784+0.205 5 0.575+0.208 0.853+0.202 6 0.723+0.179 0.711+0.370 10 0.742+0.211 1.007+0.417 20 0.677+0.231 0.784+0.345 30 0.758+0.416 0.558+0.218 45 0.571+0.132 0.438+0.184 60 0.468+0.141 0.498+0.232 75 0.458+0.096 0.342+0.191 90 0.388+0.223 0.312+0.222 105 0.457+0.110 0.369+0.130 120 0.308+0.158 0.259+0.071 91 Figure 3.2 Average fraction of initial radiolabel remaining from 1251 thrombomodulin analogue for low dose (0.2ug) and high dose administered, and PEG conjugated thrombomodulin (1 0Oug) analogue with 50% of initial activity 0 and 70% of initial activity a (n=4 for each dose) 10? 0 peg#1 0 peg#2 111 LOW DOSE HIGH DOSE .01 0 I I 30 60 f"""-120 150 180 210 240 1 90 time (minutes) 1 1 92 Table 3.3 Half lives in minutes (T1/2), areas under the curve in mOD/minute versus minutes (AUC), and mean residence times in minutes (MRT) are calculated for each rat using RSTRIP. Radio labelled low (0.2ug) and high (10Oug) doses of thrombomodulin analogue, and radiolabelled PEG conjugates of the thrombomodulin analogue are depicted. All values are calculated based on the amount of 125I radiolabel remaining over time. Standard deviations for the average values are given in parentheses. PARAMETERS CALCULATED USING RSTRIP (biexponential) PEG 50% activity* Average PEG 70% activity* Average M388L LOW Average M388L HIGH Average T1(1 /2) T2(1/2) AUC MRT 2.59 5.85 1.69 3.66 3.45(1.79) 97.7 140 138 100 200 100 200 100 200 200 300 0.737 58.4 78.2 135 91.4 90.7(28.0) 60 60 80 60 70 100 200 100 3.61 6.08 4.63 3.76(1.96) 179 139(33.2) 0.735 1.24 1.25 2.55 1.5(0.76) 2.80 1.84 1.75 2.02 2.1(0.48) * relative to unconjugated thrombomodulin analogue 93 Table 3.4 Average fraction + standard deviations of initial radiolabel remaining in the blood from 1251 thrombomodulin analogue (M388L) conjugated to PEG. One conjugate had 50% of M388L activity (PEGM388L-50) and the other conjugate had 70% of M388L activity (PEGM388L-70). Time (minutes) PEG-M388L-50 n=4 PEG-M388L-70 n=4. 2 0.957+0.087 1.254+0.710 5 0.841+0.064 0.676+0.043 10 0.756+0.056 0.524+0.031 20 0.712+0.039 0.449+0.039 30 0.647+0.038 0.381+0.028 45 0.592+0.041 0.327+0.023 60 0.543+0.034 0.290+0.028 90 0.480+0.035 0.224+0.030 120 0.416+0.042 0.190+0.024 180 0.358+0.040 0.149+0.047 240 0.335 0.099 94 The area under the curves (AUC) are measured in mOD/minute versus minute rather than concentration versus time as determined by protein C activation assay. For both M388L and PEG- M388L, AUC are linear with respect to dose. This indicates that linear pharmacokinetics are occurring for the doses administered. The AUC data as determined by APCA for the PEG-M388L are higher for conjugates which exhibit lower activity per unit mass relative to the M388L. The decrease in activity is more than offset by the increase in half life in the blood as shown by Figure 3.1. Thus a 2Oug or 5Oug dose of PEG-M388L maintained higher amounts of protein C activation, as measured by APCA, over time than the respective doses of unconjugated M388L. AUC is calculated for 1251 radiolabel which reflects concentration in terms of the fraction of the radiolabel remaining. The values obtained for the AUC indicate that linear pharmacokinetics are occurring for the doses administered and that higher values are obtained for the conjugated TM analogue. Conjugation of TM analogue with polyethylene glycol increases the half life of TM analogue in the blood of rats. Further research is necessary to find the amount of conjugation which increases the half life and does not decrease the activity. 95 REFERENCES Abuchowski, A., McCoy, J. R., Palczuk, N. C., Van Es, T., and F. F. Davis. Effect of covalent attachment of polyethylene glycol on immunogenicity and circulating life of bovine life of bovine liver catalase. The Journal of Biological Chemistry 252(11):3582-3586 (1977). (1) Beauchamp, C. 0., Gonias, S. L., Menapace, D. P., and S. V. Pizzo. A new procedure for the synthesis of polyethylene glycol-protein adducts; effects on function, receptor recognition, and clearance of superoxide dismutase, lactoferrin, and alpha-macroglobulin. Analytical Biochemistry 131:25-33 (1983). (2) Chen, R. H., Abuchowski, A., Van Es, T., Palczuk, N. C., F. F. Davis. Properties of two urate oxidases modified by the covalent attachment of poly(ethylene glycol). Biochimica et Biophysica Acta (3) 660:293-298 (1981). (4) Davis. S., Abuchowski, A., Park Y. K., and F. F. Davis. Alteration of the circulating life and antigenic properties of bovine adenosine deaminase in mice by attachment of polyethylene glycol. Clin. Exp. Immunol. 46:649-652 (1981). (5) Katre, N. V. , M. J. Knauf , and W. J. Laird. Chemical modification of recombinant interleukin 2 by polyethylene glycol increases its potency in the murine Meth A sarcoma model. Proc. Natl. Acad. Sci. 84:1487-1491 (1987). (6) Mast, A. E., Salvesen, G., Schnebli, H., and S. V. Pizzo. Evaluation of the rapid plasma elimination of recombinant alphaiproteinase inhibitor: synthesis of polyethylene glycol conjugates with improved therapeutic potential. J. Lab. Clin. Med. 116(1):58-65 (1990). Pyatak, P. S., A. Abuchowski and F. F. Davis. Preparation of a polyethylene glycol: superoxide dismutase adduct, and an examination of its blood circulating life and anti-inflammatory activity. Res. Comm. (7) Chem. Path. Pharm. 29(1):113-127 (1980). (8) Wieder, K. J., Palczuk, N. C., Van Es, T., F. F. Davis. Some properties of polyethylene glycol: phenylalanine ammonia-lyase adducts. The Journal of Biological Chemistry 254(24):12579-12587 (1979). 96 Savoca, K. V., Abuchowski, A., Van Es, T., Davis, F. F., and N. C. Palczuk. Preparation of non-immunogenic arginase by the covalent attachment of polyethylene glycol. Biochimica and Biophysica Acta (9) 578:47-53 (1979). (10) Abuchowski, A. Van Es, T., Palczuk, N. C., and F. Davis. Alteration of immunological properties of bovine serum albumin by covalent attachment of polyethylene glycol. The Journal of Biological Chemistry 252(11):3578-3581 (1977). 97 BIBLIOGRAPHY Aarons, L., Hopkins, K., Rowland, M., Brossel, S., and J. F. Thiercelin. Route of administration and sex differences in the pharmacokinetics of aspirin, administered as its lysine salt. Pharmaceutical Research 6(8):660-666 (1989). Abuchowski, A., McCoy, J. R., Palczuk, N. C., Van Es, T., and F. F. Davis. Effect of covalent attachment of polyethylene glycol on immunogenicity and circulating life of bovine liver catalase. The Journal of Biological Chemistry 252(11):3582-3586 (1977). Abuchowski, A. Van Es, T., Palczuk, N. C., and F. Davis. Alteration of immunological properties of bovine serum albumin by covalent attachment of polyethylene glycol. The Journal of Biological Chemistry 252(11):3578-3581 (1977). Ahern, T. J., Morris, G. E., Barone, K. M., Horgan, P. G., Timony, G. A., Angus, L. B., Henson, K. S., Stoudemire, J. B., Langer-Safer, P. R., and G. R. Larsen. Site-directed mutagenesis in human tissueplasminogen activator. The Journal of Biological Chemistry 265(10):5540-5545 (1990). Alcorn, G., Lucker, P. W., Procaccini, R. L., and W. A. Ritschel. In vivo- in vitro correlations with various aspirin formulations. Methods and Findings in Experimental Clinical Pharmacology. 9(11):761-767 (1987). Antilla, M., P. Kahela, and P. Uotila. The absorption of acetylsalicylic acid from an enteric-coated formulation and the inhibition of thromboxane formation. International Journal of Clinical Pharmacology, Therapy and Toxicology 26(2):88-92 (1988). Ashwell, G. and J. Harford. Carbohydrate specific receptors of the liver gluconeogenesis and related aspects of glycolysis. Ann. Rev. Biochem. 51:531-554 (1982). Beauchamp, C. 0., Gonias, S. L., Menapace, D. P., and S. V. Pizzo. A new procedure for the synthesis of polyethylene glycol-protein adducts; effects on function, receptor recognition, and clearance of superoxide dismutase, lactoferrin, and alpha-macroglobulin. Analytical Biochemistry 131:25-33 (1983). 98 Bell, S., M. Berdick, M. and W. Holliday. Drug blood levels as indices in evaluation of a sustained-release aspirin. The journal of New Drugs Sep-Oct:284-293 (1966). Bertina, R. M., ed., Protein C and Related Proteins, Churchill Livingston, Edinburgh, 1988. Bourin, M., Oh lin, A. K., Lane, D. A., Stenflo, J., and U. Lindahl. Relationship between anticoagulant activities and polyanionic properties of rabbit thrombomodulin. The Journal of Biological Chemistry 263(17):8044-8052 (1986). Brody, J., N. Pickering, and G. Fink. Abnormalities of thrombomodulin and tissue plasminogen activator in occluded aortocoronary grafts detected by immunohistochemistry. Trans-Assoc-AmPhysicians 101:79-87 (1988). Chen, R. H., Abuchowski, A., Van Es, T., Palczuk, N. C., F. F. Davis. Properties of two urate oxidases modified by the covalent attachment of poly(ethylene glycol). Biochimica et Biophysica Acta 660:293-298 (1981). Davis. S., Abuchowski, A., Park Y. K., and F. F. Davis. Alteration of the circulating life and antigenic properties of bovine adenosine deaminase in mice by attachment of polyethylene glycol. Clin. Exp. Immunol. 46:649-652 (1981). Day, R., Furst, D. E., Dromgoole, S. H., and H. E. Paulus. Changes in salicylate serum concentrations and metabolism during chronic dosing in normal volunteers. Biopharmaceutics & Drug Disposition. 9:273-283 (1988). Dittman, W., and P. Majerus. Structure and function of thrombomodulin: a natural anticoagulant. Blood 75(2):329-336 (1990). Erlich, H., Esmon, N., and N. Bang. In vivo behavior of detergentsolubilized purified rabbit thrombomodulin on intravenous injection into rabbits. T. Lab. Clin. Med. 115(2):182-189 (1990). 99 Esposito, C., Gerlach, H., Brett, J. Stern, D., and H. Vlassara. Endothelial receptor-mediated binding of glucose-modified albumin is associated with increased monolayer permeability and modulation of cell surface coagulant properties. J. Exp. Med. 170:1387-1407 (1989). Frenkel, E. P., McCall, M. S., Douglass, C. C., and S. Eisenberg. Fecal blood loss following aspirin and coated aspirin microspherule administration. The Journal of Clinical Pharmacology NovDec:347-351 (1968). Gomi, K., Zushi, M., Honda, G., Kawahara, S., Matsuzaki, 0., Kanabayashi, T., Yamamoto, S., Maruyama, I., and K. Suzuki. Antithrombic effect of recombinant human thrombomodulin on thrombin-induced thromboembolism in mice. Blood, 75(7): 1396-1399 (1990). Hirahara, K., M. Koyama, T. Matsuishi, and M. Kurata. The effect of human thrombomodulin on the inactivation of thrombin by human antithrombin III. Thrombosis Research, 57:117-126 (1990). Hossain, M. and J. W. Ayres. Variables that influence coat integrity in a laboratory spray coater. Pharmaceutical Technology, Oct:72-82 (1990). Iwashima, Y., Sato, T., Watanabe, K., Ooshima, E., Hiraishi, S., Ishii, H. Kazama, M., and I. Makino. Elevation of plasma thrombomodulin level in diabetic patients with early diabetic nephropathy. Diabetes 39:983-988 (1990). Jakubowski, H., and W. Owen. Macromolecular specificity determinants on thrombin for fibrinogen and thrombomodulin. The Journal of Biological Chemistry 264(19):11117-11121 (1989). Katre, N. V. , M. J. Knauf , and W. J. Laird. Chemical modification of recombinant interleukin 2 by polyethylene glycol increases its potency in the murine Meth A sarcoma model. Proc. Natl. Acad. Sci. 84:1487-1491 (1987). Kergueris, M. F., Bourin, M., Larousse, C., Lasserre, M. P., and A. Ortega. Effects of administration route on pharmacokinetics of aspirin in the rabbit. Methods and Findings in Experimental and Clinical Pharmacology 10(3):171-175 (1988). 100 Kumada, T., Dittman, W. A., and P. W. Majerus. A role for thrombomodulin in the pathogenesis of thrombin-induced thromboembolism in mice. Blood 71(3):728-733 (1987). Kurosawa, S., J. Galvin, N. Esmon, and C. Esmon. Proteolytic formation and properties of functional domains of thrombomodulin. The Journal of Biological Chemistry 262(5):2206-2212 (1987). Leonards, J., and G. Levy. Biopharmaceutical aspects of aspirin-induced gastrointestinal blood loss in man. The Journal of Pharmaceutical Sciences 58(10):1277-1279 (1969). Lucore, C. L., Fry, E. T. A., Nachowiak, D. A., and B. E. Sobel. Biochemical determinants of clearance of tissue-type plasminogen activator from the circulation. Circulation 77(4):906-914 (1988). Mansell, L. New acetaminophen products: formulation development and bioavailability. Ph.D. Thesis, Oregon State University, 11-12 (1990). Mast, A. E., Salvesen, G., Schnebli, H., and S. V. Pizzo. Evaluation of the rapid plasma elimination of recombinant alpharproteinase inhibitor: synthesis of polyethylene glycol conjugates with improved therapeutic potential. I. Lab. Clin. Med., 116(1):58-65 (1990). Melton, R. G., Wiblin, C. N., Foster, R. L., and R. F. Sherwood. Covalent linkage of carboxypeptidase G2 to soluble dextrans - I properties of conjugates and effects on plasma persistence in mice. Biochemical Pharmacology 36(1):105-112 (1987). Melton, R. G., Wiblin, C. N., Baskerville, A., Foster, R. L., and R. F. Sherwood. Covalent linkage of carboxypeptidase G2 to soluble dextrans II in vivo distribution and fate of conjugates. Biochemical Pharmacology 36(1):113-121 (1987). Mencke, A. J. and F. Wold. Neoglycoproteins. The Journal of Biological Chemistry 257(24):14799-14805 (1982). 101 Ogawa, S., H. Gerlach, C. Esposito, A. Pasagian-Macaulay, J. Brett, and D. Stern. Hypoxia modulates the barrier and coagulant function of cultured bovine endothelium. T. Clin. Invest. 85:10901098 (1990). Pizzo, S. V. Serpin receptor 1: a hepatic receptor that mediates the clearance of antithrombin III-proteinase complexes. The American Journal of Medicine 87(suppl. 3B):3B10S-3B14S (1989). Preissner, K. T., Koyama, T., Muller, D. Tschopp, J., and G. MullerBerghaus. Domain structure of the endothelial cell receptor thrombomodulin as deduced from modulation of its anticoagulant functions. The Journal of Biological Chemistry 265(9):4915-4922 (1990). Pyatak, P. S., A. Abuchowski and F. F. Davis. Preparation of a polyethylene glycol: superoxide dismutase adduct, and an examination of its blood circulating life and anti-inflammatory activity. Res. Comm. Chem. Path. Pharm. 29(1):113-127 (1980). Rowland, M., and S. Riegelman. Pharmacokinetics of acetylsalicylic acid and salicylic acid after intravenous administration in man. The Journal of Pharmaceutical Sciences 57(8):1313-1319 (1968). Savoca, K. V., Abuchowski, A., Van Es, T., Davis, F. F., and N. C. Palczuk. Preparation of a non-immunogenic arginase by the covalent attachment of polyethylene glycol. Biochimica and Biophysica Acta 578:47-53 (1979). Seppala, I. and 0. Makela. Antigenicity of dextran-protein conjugates in mice. The Journal of Immunology 143:1259-1264 (1989). Simrock, R., Rehders, K., Spahn, H., Mutschler, E., and H. K.Breddin. Plasma drug and antiplatelet profiles of the original acetylsalicylic acid preparations used in the AMIS, PARIS and German-Austrian trials for secondary prevention of myocardial infarction. European journal of Clinical Pharmacology 33: 541547 (1988). 102 Suzuki, K., Kusumoto, H., Deyashiki, Y., Nishioka, J., Maruyama, I., Zushi, M., Kawahara., S., Honda, G., Yamamoto, S., and S. Horiguchi. A domain composed of epidermal growth factor-like structures of human thrombomodulin is essential for thrombin binding and for protein C activation. The Journal of Biological Chemistry 264(9):4872-4440 (1989). Suzuki, K., Hayashi, T., Nishioka, J., Kosaka, Y., Zushi, M., Honda, G., and S. Yamamoto. Structure and expression of human thrombomodulin, a thrombin receptor on endothelium acting as a cofactor for protein C activation. The EMBO Journal 6(7):1891-1897 (1987). Szmidt, M., Grzelewska-Rzymowska, I., Kowalski, M. L., and J. Rozniecki. Tolerance to acetylsalicylic acid (ASA) induced in ASA-sensitive asthmatics does not depend on initial adverse reaction. Allergy 42:182-185 (1987). Tashjian, Jr., A. H., Voelkel. E. F., Lazzaro, M., Goad, D., Bosma, T., and L. Levine. Tumor necrosis factor-alpha (cachectin) stimulates bone resorption in mouse calvaria via a prostaglandin-mediated mechanism. Endocrinology 120(5):2029-2036 (1987). Tanaka, K., Wada, K., Morimoto, T., Shomura, S., Satoh, T., Yada, I., Yuasa, H., Kusagawa, M., and K. Deguchi. The role of the protein C-thrombomodulin system in physiologic anticoagulation during cardiopulmonary bypass. Trans. Am. Soc. Artif. Intern. Organs 35:373-375 (1989). Vasse, M., J. Borg, and M. Monconduit. Protein C : Rouen, a new hereditary protein C abnormality with low anticoagulant but normal amidiolytic activities. Thrombosis Research 56:387-398 (1989). Veronese, F. M., Largajolli, R., Boccu, E., Benassi, C. A., and 0. Schiavon. Surface modification of proteins. Applied Biochemistry and Biotechnology 11:141-152 (1985). Verstraeten, A., Roets, E., and J. Hoogmartens. Quantitative determination by high-performance liquid chromatography of acetylsalicylic acid and related substances in tablets. Journal of Chromatography 388:201-216 (1987). 103 Wieder, K. J., Palczuk, N. C., Van Es, T., F. F. Davis. Some properties of polyethylene glycol: phenylalanine ammonia-lyase adducts. The Tournal of Biological Chemistry 254(24):12579-12587 (1979). Wilkinson C. J., Jackson, J. C., Lang, G. M., Strevens, V.H., and A. H. Sehon. Tolerogenic polyethylene glycol derivatives of xenogeneic monoclonal immunoglobulins. Immunology Letters 15:17-22 (1987). Wilson, J. T., Brown, R. D., Bocchini, Jr., J. A., and G. L. Kearns. Efficacy, disposition and pharmacodynamics of aspirin acetaminophen and choline salicylate in young febrile children. Therapeutic Drug Monitoring 4:147-180 (1982). Zushi, M., Gomi, K., Yamamoto, Maruyama, I., Hayashi, T., and K. Suzuki. The last three consecutive epidermal growth factor-like structures of human thrombomodulin comprise the minimum functional domain for protein C-activating cofactor activity and anticoagulant activity. The Journal of Biological Chemistry 264(18):10351-10353 (1989). APPENDIX 104 APPENDIX In early experiments radiolabelling thrombomodulin (TM) analogue resulted in some of the BSA in the sample also being radiolabelled. Radio labelled BSA content was detected, but not quantified using gel electrophoresis. In these cases radiolabelled BSA present in each of the TM analogue samples was calculated based on radioactivity in the blood 90 minutes post dosing. It is assumed that no radiolabel from the TM analogue remains in the blood 90 minutes after dosing. The radioactivity contributed by BSA in early experiments was subtracted assuming linear pharmacokinetics and no 1251 TM analogue remaining after 90 minutes. The resulting curve, Figure 2.6, gives a good approximation of the alpha distribution phase of pure TM analogue but the beta elimination phase is not accurate because the assumption that no radiolabel from TM analogue remains after 90 minutes is false. The low dose elimination curve gives negative values after 2 minutes due to error in estimation of the radiolabelled BSA in the dose. The adequacy of this method was determined by administering TM analogue without the presence of radiolabelled BSA as determined by gel electrophoresis. The calculated pharmacokinetic curves of TM analogue when administered with radiolabelled BSA are similar to that for pure TM analogue (Figure 2.6). The underestimation in calculated values is due to the 10% radiolabel that remains in the pure TM curve. CORRECTION PROCEDURE Radio labelled thrombomodulin containing radiolabelled BSA and pure radiolabelled BSA samples were injected according to the same protocol as the radiolabelled thrombomodulin to determine the elimination rates of thrombomodulin with BSA versus pure BSA in rats. This was necessary to determine how radiolabelled BSA affects the radiolabel versus time curves for radiolabelled thrombomodulin. 105 To correct for bovine serum albumin interference the following procedure is used: Assumptions BSA is assumed to be eliminated at a rate independent of dose. There is a systematic error if there is thrombomodulin (TM) analogue remaining after 60 minutes since that TM analogue is assumed to be BSA. Therefore if the half life of the TM analogue is too long then it appears that the half life of the TM analogue is shorter than it actually is. The half life of the TM analogue is at least as long as the calculated half life found by this correction method. The fraction of administered sample in the blood was calculated as described above for all rats. Calculations are performed on the average data from four rats for each of the doses administered. Data from the low dose M388L, high dose M388L, rats were individually analyzed as follows: Step1 The value at each timepoint (fraction of dose administered in 20m1 of blood based on average counts per minute data) was divided by the value at the corresponding timepoint for the 100% BSA. Step 2 The resulting fraction did not become constant until after ninety minutes. The average of the resulting fractions between ninety and two hundred and forty minutes was calculated (average of four points). This average fraction is the fraction of BSA in the data set of interest. Step 3 The timepoints in the 100% BSA data set are multiplied by the fraction of BSA in the data point of interest and then these numbers are subtracted from the corresponding time points in the data set to be analyzed. This resulting value is the fraction of total radioactivity at a particular timepoint which is attributable only to thrombomodulin analogue. Step 4 The fraction of BSA is subtracted from one (1.0) to give the fraction of thrombomodulin in the sample. Step 5 The fraction of initial thrombomodulin which this represents is then calculated as follows. The fraction of radioactivity attributable to 106 thrombomodulin analogue is divided by the fraction of thrombomodulin analogue in the sample. 107 Figure A.1 The fraction of initial radiolabel administered remaining over time for radiolabelled Bovine Serum Albumin (BSA) -0, low dose radiolabelled thrombomodulin analogue with radiolabelled BSA , and high dose radiolabelled thrombomodulin analogue with radiolabelled BSA M. These are how the curves appear before step 1 of the mathematical manipulation. 0.5 w 0.4 u. ,.., 0.3 - -0- BSA Oa< < LL LOW DOSE HIGH DOSE 0.2 C.) < i= 2. 0.1 0.0 0 30 60 90 120 150 180 210 240 TIME (MINUTES) 108 Figure A.2 This figure shows the result of step #1 when the radiolabel vs. time curves shown in figure A.1 are used to determine the fraction of radiolabelled bovine serum albumen (BSA) in each of the two thrombomodulin analogue BSA mixtures. The mixture curves are divided by the BSA curve and the average of the points in the boxed area are used to calculate the percent of BSA in each of the two mixtures. Step 2 is performed based on these curves. 1.0 -0- LOW DOSE/BSA 0.8 HIGH DOSE/BSA 0.6 Z 0.4 < E 0.2 0 H 0 0 100 200 TIME (MINUTES) 300 109 Figure A.3 The radiolabelled bovine serum albumen (BSA) in the high dose thrombomodulin analogue BSA mixture is calculated to be 33.7%. So the BSA curve is multiplied by 0.337 and this resulting curve is subtracted from the thrombomodulin analogue BSA mixture to obtain the radiolabel attributable to the thrombomodulin analogue only 0. Step 3 is depicted in this figure. 0.35 -J U. CO O -J 0.25 - go-- HIGH DOSE 0--- BSA*0.337 HIGH DOSE - (BSA*0.337) Z 0 O0 17: O CC 0.15 cc -I LI- I 0.05 - -0.05 0 30 60 90 III 1. 120 1 50 180 2 1 0 240 TIME (MINUTES) 110 Figure A.4 The radiolabelled bovine serum albumen (BSA) in the low dose thrombomodulin analogue BSA mixture is calculated to be 48.9%. So the BSA curve is multiplied by 0.489 and this resulting curve is subtracted from the thrombomodulin analogue BSA mixture to obtain the radiolabel attributable to the thrombomodulin analogue only O. Step 3 is depicted in this figure. -0.05 I 0 30 60 I 90 I 120 150 180 210 240 TIME (MINUTES) 111 Figure A.5 These curves represent the fraction of radiolabel which is attributable only to thrombomodulin analogue relative to the initial amount of radiolabel injected. These curves are found as the calculated difference in figure 3a and 3b. 0.3 LOW DOSE HIGH DOSE m 0.2 LL < O -I z2 O e P. 0.1 - 0 cc cc - -I < F.: 0.0 -- -0.1 0 30 TIME (MINUTES) 6'0 90 112 Figure A.6 The amount of radiolabel remaining due to thrombomodulin analogue relative to the initial radiolabel injected into the rat in the form of thrombomodulin analogue. Step 5 is depicted in this figure. w xI- 0.4 I'Ll D 0 (.5 ...1 I.4 P 0 _1 0.3 IP-- LOW DOSE HIGH DOSE U9 Z4C Z c.) =< u_ < z O rn O _1 za0 I= LLI 0 2 o co C < co cc 400 3 CC 4CCX I-- 0.2 0.1 0.0 -0.1 . 0 30 TIME (MINUTES) 60 90 113 Figure A.7 High dose (10Oug) and low dose (0.2ug) pharmacokinetics of thrombomodulin analogue in rats. The high dose and Iciw dose administered as pure thrombomodulin samples is compared to the mathematically derived curves from the high dose and low dose 0 samples administered with radiolabelled BSA. The fraction of radiolabel in the low dose sample which is attributable to BSA is 49% and the fraction of radiolabel in the high dose sample which is attributable to BSA is 34%. 0.8 low dose high dose co w 0.6 u. < O1 zo 2a low dose containing BSA high dose containing BSA 0.4 - cc< szt cc -1 u. 0.2 - z I 0.0 10 I I 20 30 TIME(MINUTES) 4 40 50 60