The Anatomy & Physiology of The Take a Closer Look… Testes
The Anatomy & Physiology of The
Testes
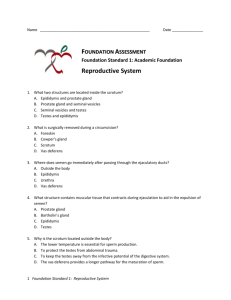
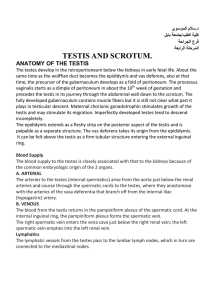
The testes are located within the scrotum. Within the scrotum contains two separate chambers, one for each individual testis. The raphe, a superficial ridge, marks the line of demarcation between the chambers.
A muscle known as the dartos muscle, gives the scrotum a wrinkled façade. The cremaster muscle pulls the testes nearer to the body. The movement towards or away the body keeps the testes temperature several degrees below core body temperature.
The testes develop inside the body cavity and pass along the inguinal canal while they descend into the scrotum. The testes continue to be connected with internal structures via the spermatic cord.
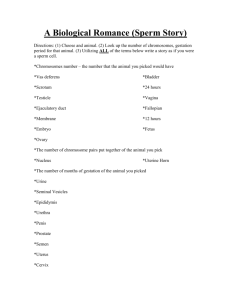
Spermatozoon
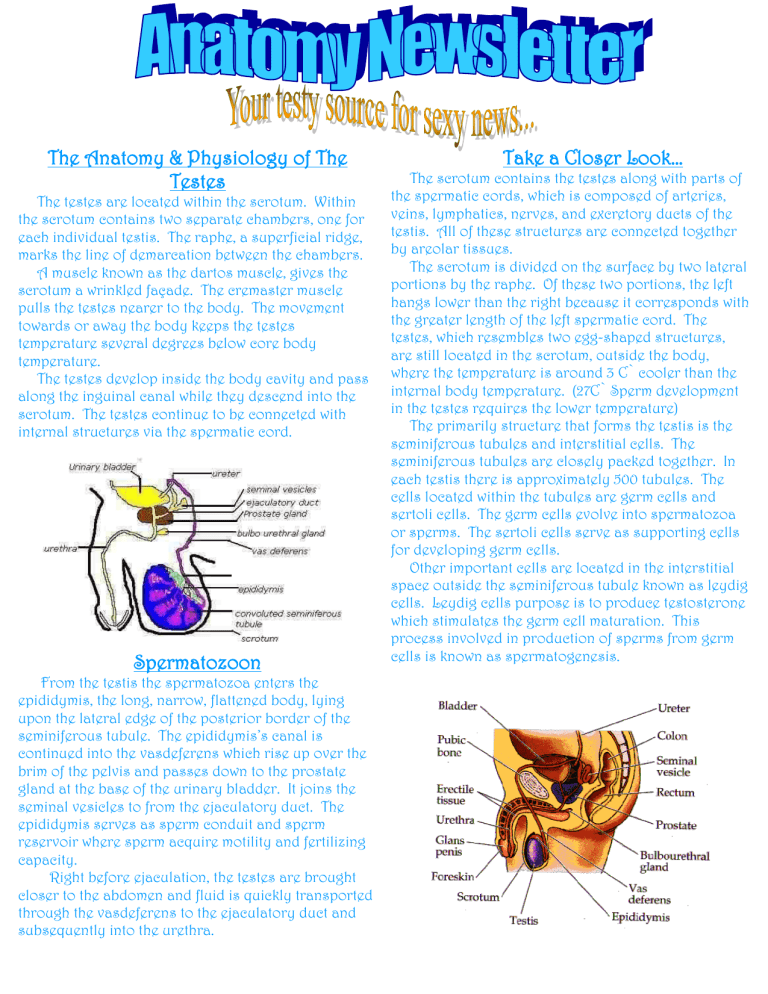
From the testis the spermatozoa enters the epididymis, the long, narrow, flattened body, lying upon the lateral edge of the posterior border of the seminiferous tubule. The epididymis’s canal is continued into the vasdeferens which rise up over the brim of the pelvis and passes down to the prostate gland at the base of the urinary bladder. It joins the seminal vesicles to from the ejaculatory duct. The epididymis serves as sperm conduit and sperm reservoir where sperm acquire motility and fertilizing capacity.
Right before ejaculation, the testes are brought closer to the abdomen and fluid is quickly transported through the vasdeferens to the ejaculatory duct and subsequently into the urethra.
Take a Closer Look…
The scrotum contains the testes along with parts of the spermatic cords, which is composed of arteries, veins, lymphatics, nerves, and excretory ducts of the testis. All of these structures are connected together by areolar tissues.
The scrotum is divided on the surface by two lateral portions by the raphe. Of these two portions, the left hangs lower than the right because it corresponds with the greater length of the left spermatic cord. The testes, which resembles two egg-shaped structures, are still located in the scrotum, outside the body, where the temperature is around 3 C` cooler than the internal body temperature. (27C` Sperm development in the testes requires the lower temperature)
The primarily structure that forms the testis is the seminiferous tubules and interstitial cells. The seminiferous tubules are closely packed together. In each testis there is approximately 500 tubules. The cells located within the tubules are germ cells and sertoli cells. The germ cells evolve into spermatozoa or sperms. The sertoli cells serve as supporting cells for developing germ cells.
Other important cells are located in the interstitial space outside the seminiferous tubule known as leydig cells. Leydig cells purpose is to produce testosterone which stimulates the germ cell maturation. This process involved in production of sperms from germ cells is known as spermatogenesis.
Hormones that Play an Important Role
When young males hit the stage of puberty, they begin to produce sperm. The male hormone,
Androgen, testosterone produced by testes, stimulate the sperm production. ICSH triggers the release of testosterone from the interstitial cells of the testes.
Testosterone promotes the maturation of spermatozoa, maintains the accessory glands, and produces male secondary sexual characteristics and behaviors. The pituitary gland releases FSH (follicle-stimulating hormone) and LH (luteinizing hormone). These hormones incite the testes to make testosterone. FSH casue an increase in the rate of spermatogenesis.
Active sustentacular cells release nhibin, a hormone that suppresses the production of FSH.
Testicular Cancer
WHAT IS TESTICULAR CANCER? ~ AKA Germ cell tumor; Begins when cells within the testicle become cancerous and begin to grow out of control.
Testicular cancer is classified as one of two types, seminoma (30%-40% of all testicular cancers), or nonseminoma, which includes 4 subtypes. These are choriocarcinoma, embryonal carcinoma, teratoma, and yolk sac tumors. A tumor can consist of both cell types; these are called mixed germ-cell tumors. The types have different prognoses and treatments.
ARE YOU AT RISK FOR TESTICULAR CANCER? ~ The cause of this cancer is still unkown. However, there are some known things that leave some at risk for developing this cancer. An undescended testicle
(cryptorchidism) is a condition where the testicle did not move into the scrotum before birth. Surgery can be performed, but it does not lower the risk. Men whose testicles did not develop normally are also at higher risk. Klinefelter’s Syndrome is a disorder characterized by low levels of male hormones, sterility, breast enlargement, and small testes, which carries with it increased risk of testicular cancer. Men who have already had testicular cancer have a two to fiver percent chance of developing cancer in the opposite testicle during the 25 years following the diagnosis.
HOW CAN YOU PREVENT TESTICULAR CANCER?
~Unfortunately this cannot be prevented. The best outcome for patients with testicular cancer occur when the disease is found early, so early detection is important. This is best done by testicular self-exam.
WHAT SCREENING TESTS ARE AVAILABLE ~ The best method of examination is known as testicular selfexam or TSE. TSE includes regular inspection and palpation of the testicles. Men (and boys) should be familiar with the normal weight, texture, and consistency of their testicles. Examination should be done once a month after a warm shower or bath.
WHAT ARE THE SIGNS? ~
*Painless lump or swelling in either testicle, or a change in the way it feels
*A feeling of heaviness in the scrotum
*A sudden collection of fluid in the scrotum
*Pain or discomfort in the scrotum