Resistance training is accompanied by increases in hip strength and... in lower extremity biomechanics during running
advertisement

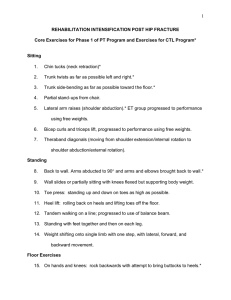
Clinical Biomechanics 24 (2009) 26–34 Contents lists available at ScienceDirect Clinical Biomechanics journal homepage: www.elsevier.com/locate/clinbiomech Resistance training is accompanied by increases in hip strength and changes in lower extremity biomechanics during running Kelli R. Snyder a, Jennifer E. Earl b,*, Kristian M. O’Connor b, Kyle T. Ebersole b a b University of Northern Iowa, Waterloo, IW, USA Neuromechanics Laboratory, Department of Human Movement Sciences, University of Wisconsin–Milwaukee, Pavilion 350, ATEP, P.O. Box 413, Milwaukee, WI 53201, USA a r t i c l e i n f o Article history: Received 8 August 2007 Accepted 23 September 2008 Keywords: Pronation Abductors Injury Alignment a b s t r a c t Background: Movement and muscle activity of the hip have been shown to affect movement of the lower extremity, and been related to injury. The purpose of this study was to determine if increased hip strength affects lower extremity mechanics during running. Methods: Within subject, repeated measures design. Fifteen healthy women volunteered. Hip abduction and external rotation strength were measured using a hand-held dynamometer. Three-dimensional biomechanical data of the lower extremity were collected during running using a high-speed motion capture system. Measurements were made before, at the mid-point, and after a 6-week strengthening program using closed-chain hip rotation exercises. Joint range of motion (rearfoot eversion, knee abduction, hip adduction, and internal rotation), eversion velocity, eversion angle at heel strike, and peak joint moments (rearfoot inversion, knee abduction, hip abduction, and external rotation) were analyzed using repeated measures analysis of variance (P 6 0.05). The independent variable was time (pre-, week 3, and week 6). A separate analysis of variance was conducted with the dependent variables of peak hip abduction and external rotation strength. Findings: Hip abduction (P = 0.009) and external rotation strength (P < 0.0005) increased by 13% and 23%, respectively. Eversion range of motion decreased (P = 0.05), hip adduction range of motion increased (P = 0.05), and a trend of decreased hip internal rotation range of motion (P = 0.08) were found. Rearfoot inversion moment (P = 0.02) and knee abduction moment (P = 0.05) decreased by 57% and 10%, respectively. Interpretation: The hip abductors and external rotators were strengthened, leading to an alteration of lower extremity joint loading which may reduce injury risk. These exercises could be used in the rehabilitation, or prevention, of lower extremity injuries. Ó 2008 Elsevier Ltd. All rights reserved. 1. Introduction It has been estimated that 30 million people in the United States choose running as their mode of exercise and that 10 million of these people run regularly (Kaufman et al., 1999). Estimations from a compilation of studies report that approximately 50–75% of these runners will suffer an injury, typically an overuse injury, which will remove them from activity for at least one week (Kaufman et al., 1999; van Mechelen, 1992; Taunton et al., 2002). It is thought that a contributing factor to lower extremity injury may be an inability to control the motion of the lower extremity segments in the frontal and transverse planes. Specifically, excessive hip adduction and internal rotation, knee abduction (valgus), tibial internal rotation, and foot pronation have been related to lower extremity overuse * Corresponding author. E-mail addresses: kelli.snyder@uni.edu (K.R. Snyder), jearl@uwm.edu (J.E. Earl), krisocon@uwm.edu (K.M. O’Connor), ebersole@uwm.edu (K.T. Ebersole). 0268-0033/$ - see front matter Ó 2008 Elsevier Ltd. All rights reserved. doi:10.1016/j.clinbiomech.2008.09.009 injury (Ireland, 2002; Powers, 2003). Attempts to reduce frontal and transverse plane movement can occur at the distal end of the lower extremity, using methods such as footwear, orthoses, and ankle strengthening. More recently, the importance of adequate hip strength has been discussed in relation to the prevention and rehabilitation of many lower extremity injuries (Ireland et al., 2003; Leetun et al., 2004; Nadler et al., 2000). The idea that improving hip strength may reduce excessive frontal and transverse plane lower extremity motion has not yet been explored. Several studies have reported that hip muscle dysfunction is related to distal movement patterns and is a possible cause of injuries such as ankle sprain, patellofemoral pain syndrome, and non-contact anterior cruciate ligament injury (Beckman and Buchanan, 1995; Nadler et al., 2000; Ferber et al., 2003; Hreljac et al., 2000; Knutzen and Price, 1994; Leetun et al., 2004; Niemuth et al., 2005; Cichanowski et al., 2007; Stefanyshyn et al., 2006). It is thought that the poor dynamic alignment pattern of hip adduction and internal rotation, knee abduction, tibial internal rotation, and K.R. Snyder et al. / Clinical Biomechanics 24 (2009) 26–34 excessive pronation may lead to injury (Bullock-Saxton, 1993; Ireland et al., 2003; Leetun et al., 2004; Powers, 2003). In a group of healthy subjects, movements of the hip were identified as the most important contributors to rearfoot motion (Knutzen and Price, 1994). This is supported by the finding that energy flow in the lower extremity during walking originated proximally and traveled distally, suggesting that the kinematics of proximal joints may affect those of distal joints (Bellchamber and van den Bogert, 2000). These biomechanical studies support the theory that the hip abductors and external rotators play a critical role in controlling the position of the entire lower extremity in the frontal and transverse planes during single-leg stance. Recent research has related hip weakness to lower extremity injury in both retrospective (Nadler et al., 2000; Ireland et al., 2003; Cichanowski et al., 2007) and prospective studies (Leetun et al., 2004; Stefanyshyn et al., 2006). Furthermore, hip strengthening programs seem to be effective in allowing patients to return to pain-free activity (Boling et al., 2006; Cibulka and Threlkeld-Watkins, 2005; Crossley et al., 2005; Frederiscon et al., 2000; Mascal et al., 2003; Tyler et al., 2006). Therefore, it is possible that increased hip muscle strength may effect lower extremity biomechanics in the frontal and transverse planes, and therefore reduce the risk of lower extremity overuse injury. A study directly examining the mechanical effects of hip strengthening on lower extremity movement could not be found in the literature. Traditionally, attempts to control frontal and transverse plane movement of the lower extremity have occurred via interventions directed at the foot, such as orthoses and ankle muscle strengthening. While some studies have shown that excessive pronation is reduced when using foot orthoses (Baitch et al., 1991; Bates et al., 1979; Smith et al., 1986), other studies have reported no effect (Nawoczenski et al., 1995; Stackhouse et al., 2004; Stacoff et al., 2000). An isokinetic training program of the ankle invertors and evertors was shown to reduce rearfoot eversion during running in uninjured subjects, however, the same effect was not seen following a more functional strengthening program (Feltner et al., 1994). While changing foot and ankle mechanics may be one way to reduce overall lower extremity frontal and transverse plane movement, addressing hip mechanics may be an alternative. A closed-chain hip rotation exercise that provides resistance to hip abduction and rotation in a single-leg stance position has been described in the literature to produce a high amount of gluteus medius activity (Earl, 2005). This exercise is beneficial because it challenges the stability of the lower extremity in the frontal and transverse planes in a functional position. Therefore, the purposes of this study were to (1) determine if a closed-chain hip rotation exercise program would increase hip abduction and external rotation strength and (2) to determine if motions and moments that have been related to lower extremity injury (rearfoot eversion, knee abduction, hip adduction, and internal rotation) would be changed following hip strengthening. We hypothesized that 6 weeks of training with the closed-chain hip rotation exercise would result in increased isometric hip abduction and external rotation strength. Furthermore, we hypothesized that the motions and moments that have been related to lower extremity injury (rearfoot eversion, knee abduction, hip adduction, and internal rotation) would be reduced following the training. 2. Methods 2.1. Participants Fifteen women volunteered for this study (mean age (standard deviation): 21.9 (1.2) years, height: 1.54 (.05) m, mass: 63.6 (6.4) kg). Inclusion criteria were an activity level that met the 27 American College of Sports Medicine requirements for moderately active (30 min of moderate intensity activity on most days of the week), and a regular menstrual cycle. Participants having greater than 10 mm of navicular drop (Brody, 1982) were excluded from the study, as this criterion has previously been used to classify participants as having excessive pronation (Menz, 1998; Mueller et al., 1993). Participants with a previous history of lower extremity orthopaedic surgery, injury to the lower extremity within the previous 6 months, neurological impairments, or who used orthoses were also excluded. Each participant provided written informed consent prior to data collection, in accordance to the university’s Institutional Review Board. Based on data from previous studies with a moderate effect size, and alpha set a priori at P < 0.05, a sample size of n = 10 was determined to be needed to achieve adequate statistical power of 0.80 (O’Connor and Hamill, 2004). 2.2. Instrumentation and equipment A hand-held Lafayette Manual Muscle Testing System (model #01163, Lafayette Instrument, Lafayette, IN, USA) was used to measure hip abduction and external rotation strength. The dynamometer was calibrated using weights according to the manufacturer instructions. Kinematic data of the lower extremity were collected during running using the seven-camera Motion Analysis Eagle System (Motion Analysis Systems, Santa Rosa, CA, USA) at a sampling rate of 200 Hz. Kinetic data were collected using a force plate that was calibrated by the manufacturer (SGA6-4, Advanced Mechanical Technology, Inc., Watertown, MA, USA) at a sampling rate of 1000 Hz. Each participant wore standard shoes and tight-fitting shorts provided by the laboratory during the three testing sessions. The shoes exposed the calcaneus (NBA-801 New Balance Slide, New Balance Athletic Shoe Inc. Boston, MA.), allowing the marker cluster to be attached directly to the skin to improve movement accuracy (O’Connor and Hamill, 2004). A cable-column system (Therapy Systems, Roseville, CA, USA) was used during hip strengthening exercises. 2.3. Strength testing protocol The dominant lower extremity (defined as the lower extremity with which a participant would kick a ball as far as possible) was used as the test extremity, and was the right extremity for all participants. Hip abductor strength was assessed using methods described by Ireland et al. (2003) which have been reported as highly reliable. Participants assumed a side-lying position with the test leg facing upward and were stabilized with a strap around the trunk and the table. The test leg was placed in a neutral position, placing pillows between the lower extremities to maintain this position. A handheld dynamometer was placed 5 cm proximal to the lateral knee joint line secured to the leg using a rigid strap that surrounded the leg and table (Ireland et al., 2003). Stabilizing the participant and dynamometer using immovable straps removed the potential for tester strength or experience to influence the results (Fig. 1). Hip external rotation strength was measured with participants seated with their hips and knees in 90° of flexion (Ireland et al., 2003) (Fig. 1). The dynamometer was placed 5 cm above the medial malleolus and secured by a strap around the ankle that was anchored to a table leg. The participants were asked to maximally push against the dynamometer by externally rotating the hip for 5 s. One practice trial and three experimental trials were performed, with 15 s of rest in between. The peak force (kg) of the three experimental trials was recorded and normalized to body mass for analysis. Strength was measured for both the trained and the untrained sides to describe any cross-over training effect that might have occurred. 28 K.R. Snyder et al. / Clinical Biomechanics 24 (2009) 26–34 2.5. Strengthening protocol Each participant was required to attend three supervised training sessions per week for 6 weeks in order to assume uniform performance of the training exercises across all participants and sessions (Abe et al., 2000; Mascal et al., 2003). Most training sessions were separated by at least 48 h, but could vary depending on participant availability. The strengthening program utilized a series of closed-chain hip abduction and rotation exercises. These exercises were chosen because they apply loads to the hip in a position that is more functional than traditional side-lying hip abduction exercises. Furthermore, the exercises can be easily adapted from using a cable column for resistance to using an elastic band for home use. The cable-column method was chosen in order to better standardize the resistance throughout the training. These exercises have been examined and shown to produce high levels of electromyographic activity in the gluteus medius (Earl, 2005). Three training exercises were implemented to train the hip abductors and external rotators: TOWARD, AWAY (based on if the participant was facing towards or away from the cable column), and HIP HIKE exercises. A picture and description of each exercise can be found in Figs. 2–4. A belt was placed around the participant’s waist with a loop on the left side of the hip to which the cable was connected Fig. 1. Participant position for isometric hip strength evaluation: (A) abduction and (B) external rotation. A pilot study of this method using 10 participants was conducted to determine the reliability (using a between-session intraclass correlation coefficient (ICC)) and precision of the measurement (using the standard error of measurement (SEM)) (Denegar and Ball, 1993). Results produced an ICC of 0.88, with a SEM of 0.48 kg for the hip abduction measure, and a betweensession ICC of 0.90, and a SEM of 0.99 kg for the hip external rotation measure. These values indicated strong reliability between testing sessions and a precise measurement. 2.4. Movement analysis For the kinematic data collection, single reflective markers were placed bilaterally over the anterior superior iliac spine (ASIS), iliac crest, and greater trochanter, and unilaterally over the right posterior superior iliac spine (PSIS), lateral femoral condyle, medial femoral condyle, lateral malleolus, medial malleolus, fifth metatarsal head, and first metatarsal head. Plastic clusters of four markers were attached to the lateral aspects of the thigh and shank with a Velcro strap. A three-marker cluster was placed directly on the calcaneus to track rearfoot motion (O’Connor and Hamill, 2004). Following a standing calibration trial all single markers except the ASIS and PSIS were removed. The speed during the running trials was 3.5–4.5 m/s and was monitored with photocells (Model 2T35, Radio Shack Corporation, Fort Worth, TX). Participants were allowed to practice until they were able to perform the task correctly, and five subsequent running trials were recorded. Fig. 2. The TOWARD exercise. Participants began by standing on the right leg facing TOWARD the weights (A) and extending the left leg while rotating the trunk counterclockwise. They reached as far as possible down the white line, lightly touched the floor (B), and returned to the starting position (A). K.R. Snyder et al. / Clinical Biomechanics 24 (2009) 26–34 29 Fig. 3. The AWAY exercise. Participants began by standing on the right leg facing AWAY from the weights (A) and extending the left leg while rotating the trunk counterclockwise. They reached as far as possible down the white line, lightly touched the floor (B), and returned to the starting position (A). for all exercises. The pulley of the cable column was in the lowest position near the floor. Tape marks on the floor provided a guide for the participant’s position during the exercises. Verbal feedback was provided by the investigator to ensure that the shoulders, torso, and hips remained in an upright position with respect to the sagittal and frontal planes. The initial loads used for the strengthening program were based on the one repetition maximum of the HIP HIKE and AWAY exercises. The participant’s one repetition maximum for the AWAY exercise was also used as an initial load for the TOWARD exercise. The initial weight was set at 60% of the participant’s one repetition maximum, and the progression of the load was based on published work on resistance training (Abe et al., 2000). During each training session participants were asked to perform as many repetitions as they could while maintaining proper posture and form. Upon completion of 12 repetitions, the weight for the next session was increased by 1.13 kg (2.5 lbs). If 30 or more repetitions were completed, the weight was increased by 2.27 kg (5 lbs). This was done to ensure that the muscles were being sufficiently overloaded in order to facilitate a strengthening effect. One repetition maximum tests were performed every 2 weeks throughout the training program to monitor progression (Abe et al., 2000). The load and number of repetitions were recorded after each training session. Fig. 4. The HIP-HIKE exercise. Participants began by standing on the right leg with the weights beside the left leg (A) and raising the left side of the pelvis toward the ceiling (B), then returned to the starting position (A). 2.6. Follow-up data collection Strength testing and movement analysis were repeated at the mid-point (week 3) and after the completion of the training program (week 6) using the same procedures as in the initial testing session. 2.7. Data reduction Three-dimensional coordinate data were low-pass filtered using a 4th order, zero-lag, recursive Butterworth filter with a cut-off frequency of 12 Hz (O’Connor and Hamill, 2004). Hip, knee, and ankle joint angles were calculated using a joint coordinate system approach (Grood and Suntay, 1983). Eversion velocity was calculated 30 K.R. Snyder et al. / Clinical Biomechanics 24 (2009) 26–34 using a first central difference approximation. Net joint moments were estimated using a Newton–Euler inverse dynamics analysis (Bresler and Frankel, 1950), and are reported as internal joint moments (those created by the body in response to externally applied moments). All data were time normalized to 101 data points. The kinematic dependent variables were joint range of motion (RoM; defined from heel strike to peak angle) of eversion, knee abduction, hip adduction, and hip internal rotation, eversion angle at heel strike, and maximum eversion velocity. Joint RoM was chosen as the dependent variable because it has been shown to be more reliable between days than peak angles (Ferber et al., 2002). The kinetic dependent variables were peak ankle inversion, knee abduction, and hip abduction and external rotation moments. which expresses differences relative to the pre-test standard deviation (Cohen, 1992). 3. Results Of the initial 15 participants, data from 13 of them were used for statistical analysis. One participant voluntarily withdrew from the study due to medical reasons and another was removed from kinematic analyses (n = 13) because it was discovered during data analysis that she was a forefoot striker. However, this individual’s data remained a part of the strength analyses (n = 14), as foot strike pattern would not affect these outcomes. Results indicated that the training program was successful in strengthening the hip abductors and external rotators. As a result of the training protocol, both isometric abduction (F (2,26) = 5.68, P = 0.009) and external rotation (F(2,26) = 11.23, P < 0.0005) strength increased on the trained side (Table 1). Both the abductors and external rotators were significantly stronger at the mid- and post-intervention testing sessions than at the pre-intervention testing (Tukey’s P 6 0.05). There was no additional strength gain between the mid- and post-intervention testing session for either muscle group. Eversion RoM (F(2,24) = 3.38, P = 0.05) was significantly reduced, and there was a trend of reduced hip internal rotation RoM (F(2,24) = 2.86, P = 0.08). Hip adduction RoM (F(2,24) = 3.29, P = 0.05) significantly increased. There were no statistically significant differences in eversion angle at heel strike, eversion velocity, or knee abduction RoM (Table 2, Fig. 5). Ankle inversion moment (F(2,26) = 8.16, P = 0.02) and knee abduction moment (F(2,26) = 3.24, 2.8. Statistical design and analysis This study utilized a within subject, repeated measures design. Repeated measures analysis of variance (ANOVA) were used to identify changes in peak isometric hip external rotation force and isometric hip abduction force, as they were the dependent variables. A separate ANOVA was performed using the six joint angle dependent variables (eversion RoM, knee abduction RoM, hip adduction RoM, hip internal rotation RoM, eversion angle at heel strike, and maximum eversion velocity). A final ANOVA was used to identify changes in the four joint moment dependent variables (hip abduction, hip external rotation, knee abduction, rearfoot inversion). The independent variable was time with three levels (pre-, mid-, and post-intervention). Tukey’s post-hoc test was performed to determine significant differences. The alpha was set at P 6 0.05 for all analyses. Effect size was reported using Cohen’s d, Table 1 Group means (standard deviations) of hip isometric abduction and external rotation strength across the training intervention. Effect sizes are calculated from the initial to the final session. N = 14. Measure Side Abduction Trained Untrained External rotation Trained Untrained Initial Mid-protocol Final kg %BW kg %BW 18.7 (3.5) 30% (6) 19.5 (3.8) 31% (7) 20.6 (3.8) 32% (6) 19.6 (3.4) 31% (6) 21.1 (3.4) 33% (6) 19.8 (4.4) 31% (8) kg %BW kg %BW 6.5 (1.5) 10% (2) 6.8 (2.4) 11% (4) 7.6 (1.4) 12% (2) 6.7 (1.9) 11% (3) 8.0 (1.6) 13% (2) 7.5 (2.6) 12% (4) P Power ES 0.01 0.82 0.68 0.94 0.06 0.08 <0.000 0.99 1.0 0.06 0.56 0.29 kg = kilograms, %BW = percentage of body weight. ES = effect size, Cohen’s d. Table 2 Group means (standard deviation) of the kinematic and kinetic variables at the three testing sessions. Effect sizes were calculated from initial to final session. N = 13. Measure Initial Mid-protocol Final P Power ES Joint range of motion Eversion RoM (deg) Eversion angle at heel strike (deg) Max eversion velocity (deg/s) Knee abduction RoM (deg) Hip adduction RoM (deg) Hip internal rotation RoM (deg) 9.8 (3.3) 5.0 (4.5) 206.7 (88.6) 3.5 (2.1) 8.1 (4.1) 5.5 (3.7) 8.8 (3.2) 4.4 (4.0) 179.1 (59.9) 3.1 (1.4) 9.5 (4.8) 4.2 (2.9) 8.1 (3.9) 4.6 (2.6) 189.1 (49.9) 3.9 (2.1) 9.5 (4.8) 3.9 (2.9) 0.05 0.83 0.28 0.30 0.05 0.08 0.58 0.07 0.26 0.25 0.57 0.51 0.53 0.05 0.20 0.19 0.33 0.43 Joint moments Rearfoot inversion (N m) Knee abduction (N m) Hip abduction (N m) Hip external rotation (N m) 8.5 (5.8) 82.8 (17.4) 128.5 (28.1) 3.8 (1.8) 7.3 (5.5) 74.9 (16.1)a 132.4 (25.5) 3.8 (1.2) 3.6 (3.8)b 74.6 (13.0)a 127.6 (25.5) 3.9 (1.8) 0.01 0.05 0.38 0.89 0.91 0.56 0.21 0.07 0.83 0.48 0.03 0.10 RoM = range of motion. ES = effect size, Cohen’s d. a Indicates mean significantly different from the initial testing session, P 6 0.05. b Indicates mean significantly different from the initial and mid-protocol testing sessions, P 6 0.05. 31 K.R. Snyder et al. / Clinical Biomechanics 24 (2009) 26–34 B. Eversion(-)/inversion(+) velocity 10 8 6 4 2 0 -2 0 -4 -6 200 10 20 30 40 50 60 70 80 90 100 Velocity (degrees/sec) Angle (degrees) A. Foot eversion(-)/inversion(+) 100 0 0 -200 -300 D. Hip abduction (-)/adduction(+) C. Knee valgus(-)/varus(+) 20 Angle (degrees) 6 Angle (degrees) 10 20 30 40 50 60 70 80 90 100 -100 4 2 0 0 10 20 30 40 50 60 70 80 15 10 5 0 90 100 0 10 20 30 40 50 60 70 80 90 100 Angle (degrees) -5 E. Hip internal rotation(+)/external rotation (-) Initial 8 6 Mid-Protocol 4 2 0 Final 0 10 20 30 40 50 60 70 80 90 100 Percent Stance Fig. 5. Group ensemble averages of joint angles and velocities during the stance phase of running for the three testing sessions. P = 0.05) were significantly reduced following the training program (Table 2, Fig. 6). 4. Discussion 4.1. Hip strength changes Our training protocol targeted the proximal muscles that control frontal and transverse plane motion of the lower extremity. Our rationale for training the hip muscles was that these larger muscles have the potential to cause a greater effect on frontal and transverse plane motion, and that hip motion is a strong predictor of rearfoot motion (Knutzen and Price, 1994). The significant increase in hip strength resulted in a significant reduction in eversion RoM, a trend toward reduced hip internal RoM, and significant decreases in ankle inversion and knee abduction moment, supporting our hypotheses. Isometric hip strength measures reported in the present study as percent body weight were similar to those previously reported by Ireland et al. (2003) (31.4%) and Leetun et al. (2004) (29.2%). The principle of specificity states that the greatest strength enhancements are elicited when the modes of muscular training and testing are the same (McComas, 1996). The strengthening exercises were dynamic and isotonic and performed at relatively slow speeds. The running task was dynamic, but performed at a much faster speed, and the strength assessment technique was isometric. Although the modes of strength training and testing were different, the significant strength increase demonstrates the large effect that the strengthening program had. Our results support previous studies documenting changes in isometric strength following isotonic or functional training (Frederiscon et al., 2000; Starkey and Ryan, 1996). In a previous study, Feltner et al. (1994) implemented both isokinetic and functional training programs and measured isokinetic strength of the ankle invertors and evertors, and rearfoot motion in individuals with excessive pronation. The functional program included exercises such as balance boards, step-ups, toe raises, one- and two-leg jumping, and zig-zag courses. The isokinetic strengthening group trained the invertors and evertors at three velocities (20 deg/s, 90 deg/s, and 180 deg/s), and both groups trained three times per week for 8 weeks. While both groups had significant strength gains, only the isokinetic group demonstrated a reduction in inversion/eversion angle at heel strike and eversion RoM. Our results supported the previous finding that rearfoot eversion RoM was reduced following strength training. While Feltner et al. (1994) strengthened the muscles that directly controlled foot and ankle motion, our results demonstrate that a similar reduction in rearfoot motion can be achieved by strengthening the hip musculature. The strengthening exercises were chosen because they train the hip muscles in a functional position, and have been shown to activate the gluteus medius (Earl, 2005; Schmitz et al., 2002). Due to the functional position it was not possible to isolate specific muscles; therefore muscles in addition to the hip abductors and external rotators may have experienced strength enhancements. This was the first study to use these exercises as part of a strengthening intervention, and several things were learned. It was necessary to 32 K.R. Snyder et al. / Clinical Biomechanics 24 (2009) 26–34 A. Ankle Moment: Inversion (+)/Eversion (-) B. Knee Moment: Adduction (+) / Abduction (-) 5 20 -5 0 0 10 20 30 40 50 60 70 80 90 100 -20 Nm Nm 0 -10 -15 0 10 20 30 40 50 60 70 80 90 100 -40 -60 -20 -80 % of stance % of stance C. Hip Moment: Adduction (+) / Abduction (-) D. Hip Moment: Internal rotation (+) / External rotation (-) 35 10 0 10 20 30 40 50 60 70 80 90 25 100 Nm Nm -40 -90 15 5 -5 0 -140 10 20 30 40 50 60 70 80 90 100 % of stance % of stance Initial Mid-Protocol Final Fig. 6. Group ensemble averages of internal joint moments during the stance phase of running for the three testing sessions. increase the resistance in order to continually overload the muscles to elicit a strength adaptation. However, as the resistance increased during the intervention, it became more difficult for the participants to maintain proper posture. Although the participants were provided immediate feedback on their posture, and reminded that the motion was to occur at their hip only, it is likely that the compromised posture necessitated substitution from muscles other than the abductors and external rotators. 4.2. Biomechanical changes It was hypothesized that increased strength of the hip abductors and external rotators would result in decreased frontal and transverse plane motion of the lower extremity during running. This was based on previous literature that hypothesized that strength at the hip is related to the incidence of lower extremity injury (Bullock-Saxton, 1993; Ireland et al., 2003; Knutzen and Price, 1994; Leetun et al., 2004). Significant decreases in eversion RoM, hip internal rotation (trend), rearfoot inversion moment and knee abduction moment support our hypotheses that strengthening the hip musculature can affect lower extremity mechanics. The small increase in hip adduction RoM is contradictory to our original hypothesis. Our hip adduction angle represented the position of the thigh segment relative to the pelvis. As a post-hoc analysis, we have analyzed the pelvic segment angle data relative to the global coordinate system. No significant changes in pelvic segment RoM in the frontal plane between pre- and post-test were found (P = 0.81). To further explore the apparent contradiction between increased hip adduction RoM and decreased knee abduction moment, we evaluated the angle of the ground reaction force (GRF) vector in the frontal plane. A lateral shift in the center of mass would act to increase hip adduction angle, while decreasing knee abduction moment (as the GRF would pass closer to the knee joint), and decrease rearfoot inversion moment (as the GRF would pass closer to the ankle joint). Results indicated no significant change in either the angle between the GRF and vertical in the frontal plane at heel strike (P = 0.90), or the location of the center of pressure at heel strike (P = 0.26). Based on these analyses, a mechanical explanation for the contradiction in findings has not been found. However, the magnitude of the change in hip adduction RoM is very small (1.5°), with a very small effect size (0.33). Therefore it is quite possible that this difference, while statistically significant, has minimal clinical significance. Further research on this topic is necessary and will continue. Previous research indicated that the movements and forces at the hip are important contributors to rearfoot motion (Bellchamber and van den Bogert, 2000; Knutzen and Price, 1994). Knutzen and Price (1994) demonstrated that movements of the hip are the most important predictors of rearfoot motion. From a clinical perspective, several studies have shown that injury to the foot or ankle is related to dysfunction of the hip musculature (Beckman and Buchanan, 1995; Bullock-Saxton, 1993; Hreljac et al., 2000; Knutzen and Price, 1994; Leetun et al., 2004). Our findings support the concept that strengthening the hip muscles can have a significant impact on knee and rearfoot mechanics and should not be overlooked in the prevention and/or rehabilitation of those injuries. Another important finding was the reduction in knee abduction moment that occurred with increased hip strength. Stefanyshyn et al. (2006) recently reported that patients with patellofemoral pain syndrome had significantly greater knee abduction impulse than controls, and increased knee abduction impulse was predictive of developing patellofemoral pain syndrome. Impulse was the integrated area of the moment-time curve, and chosen to represent the cumulative loading during the entire stance phase. The authors explained that movement of the hip and pelvis in the frontal plane has a large impact on the knee abduction moment arm, and could K.R. Snyder et al. / Clinical Biomechanics 24 (2009) 26–34 therefore impact knee abduction moments. Specifically, Stefanyshyn et al. (2006) stated that a position of increased hip adduction increases the knee abduction moment arm, and therefore the knee abduction moment. Our results partially support this as increasing hip strength did reduce the knee abduction moment, but we did not find the associated reduction in hip adduction angle. Our finding that knee abduction moment was reduced suggests that this hip strengthening intervention can alter knee joint loading, and may be useful for treating patients with patellofemoral pain syndrome or other lower extremity injuries. Further research is needed to fully understand the mechanisms by which hip strength and hip and knee mechanics are related during functional tasks. In an analysis of lower extremity kinematics during running, O’Connor and Hamill (2004) reported inversion angle at heel strike (5.0°), eversion RoM (11.1°), peak eversion angle ( 6.1°), and peak eversion velocity ( 294.8 deg/s). Each of these values are similar to those found in the present study, except for peak eversion velocity, which was lower in the present study ( 227.27 deg/s). Values for knee abduction, hip adduction and internal rotation angles are similar to those previously reported during running (Ferber et al., 2003; Malinzak et al., 2001). There are several factors that could account for why the kinetic changes seen following the strength training were larger than the kinematic changes. Nigg (2001) proposed that the locomotor system chooses a neuromuscular strategy that maintains skeletal movement in an optimal path. Interventions such as shoes, orthoses, or strengthening may alter the neuromuscular activation of muscles and therefore joint moments, in an attempt to maintain the movement pattern that is most efficient (Nigg, 2001). Our result seems to support this paradigm. The changes in joint moments and small changes in joint angles could also be the results of changes in trunk motion not measured in this study. Another explanation for not finding large kinematic differences is that we chose to study individuals with a normal foot type in order to create a more homogenous sample, and minimize the variability associated with foot type. There are a variety of methods to classify foot type, and there is not yet a consensus on what criteria should be used to classify someone as having excessive rearfoot motion. We chose to categorize participants as ‘‘normal foot type” based on the navicular drop measurement because this method is commonly used, and has been validated as predictive of rearfoot motion (Menz, 1998). We also wanted to determine the mechanical effects of strengthening the hip muscles in ‘‘normal” participants before the intervention is applied to those with pathology. Participants who have excessive rearfoot motion to begin with might be more likely to have a greater change in lower extremity motion following this strengthening program. 4.3. Limitations and directions for future research This investigation is an important contribution to the current body of literature as it is the first study attempting to identify a relationship between hip external rotator and abductor muscle strength and lower extremity motion. However, there were several limitations. Although a priori power analysis indicated that 10 subjects would provide adequate power for the variables selected, there were a few analyses with low power values. A larger sample size would be suggested in future studies in this area of research. Secondly, the participants all had a normal foot type, which might have limited the magnitude of kinematic changes following the strengthening program. Our goal was to determine the basic biomechanical changes that may occur following hip strengthening. Future studies should be conducted using participants with ‘‘excessive pronation”. The use of more of an endurance type training protocol, with lower resistance and higher repetition should be 33 investigated to correct the limitation of poor posture with high weight. Finally, studies examining changes in lower extremity kinematics during a variety of tasks following fatigue of the hip muscles, or using a group of patients with hip weakness, should be conducted. 5. Conclusions It can be concluded that the strengthening program effectively strengthened the hip abductors and external rotators which led to an alteration of lower extremity joint loading. This study found rearfoot eversion RoM, hip internal rotation RoM, knee abduction and rearfoot inversion joint moments were reduced following 6 weeks of hip muscle strengthening. These exercises could be used by clinicians in the rehabilitation, or prevention, of lower extremity injuries. Acknowledgements Funding for this project was provided by the University of Wisconsin–Milwaukee College of Health Sciences Graduate Student Research Award. The authors would like to thank David BazettJones, MS, LAT for his assistance in data analysis. References Abe, T., Dehoyos, D.V., Pollock, M.L., Garzarella, L., 2000. Time course for strength and muscle thickness changes following upper and lower body resistance training in men and women. Eur. J. Appl. Physiol. 81, 174–180. Baitch, S.P., Blake, R.L., Fineagan, P.L., Senatore, J., 1991. Biomechanical analysis of running with 25 degrees inverted orthotic devices. J. Am. Pod. Med. Assoc. 81, 647–652. Bates, B.T., Osternig, L.R., Mason, B., James, L.S., 1979. Foot orthotic devices to modify selected aspects of lower extremity mechanics. Am. J. Sports Med. 7, 338–342. Beckman, S., Buchanan, T., 1995. Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Arch. Phys. Med. Rehabil. 76, 1138–1143. Bellchamber, T.L., van den Bogert, A.J., 2000. Contributions of proximal and distal moments to axial tibial rotation during walking and running. J. Biomech. 33, 1397–1403. Boling, M.C., Bolgla, L.A., Mattacola, C.G., Uhl, T.L., Hosey, R.G., 2006. Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch. Phys. Med. Rehabil. 87, 1428–1435. Bresler, B., Frankel, J., 1950. The forces and moments in the leg during level walking. Trans. ASME 72, 27–36. Brody, D., 1982. Techniques in the evaluation and treatment of the injured runner. Orthop. Clin. North Am. 13, 541–558. Bullock-Saxton, J., 1993. Changes in hip and knee muscle strength associated with ankle injury. NZ J. Physiother. 21, 10–14. Cibulka, M., Threlkeld-Watkins, J., 2005. Patellofemoral pain and asymmetrical hip rotation. Phys. Ther. 85, 1201–1207. Cichanowski, H.R., Schmitt, J.S., Johnson, R.J., Niemuth, P.E., 2007. Hip strength in collegiate female athletes with patellofemoral pain. Med. Sci. Sports Exerc. 39, 1227–1232. Cohen, J., 1992. A power primer. Psych. Bull. 112, 155–159. Crossley, K.M., Cowan, S.M., Mcconnell, J., Bennell, K.L., 2005. Physical therapy improves knee flexion during stair ambulation in patellofemoral pain. Med. Sci. Sports Exerc. 37, 176–183. Denegar, C., Ball, D., 1993. Assessing reliability and precision of measurement: an introduction to intraclass correlation and standard errors of measurement. J. Sport Rehabil. 2, 35–42. Earl, J., 2005. Gluteus medius activity during three variations of isometric single leg stance. J. Sport Rehabil. 14, 1–11. Feltner, M., Macrae, H., Macrae, P., Turner, N., Hartman, C., Summers, M., Welch, M., 1994. Strength training effects on rearfoot motion in running. Med. Sci. Sports Exerc. 26, 1021–1027. Ferber, R., Davis, I., Williams, D., 2003. Gender differences in lower extremity mechanics during running. Clin. Biomech. 18, 350–357. Ferber, R., Mcclay Davis, I., Williams 3rd, D.S., Laughton, C., 2002. A comparison of within- and between-day reliability of discrete 3D lower extremity variables in runners. J. Orthop. Res. 20, 1139–1145. Frederiscon, M., Cookingham, C., Chaudhari, A., Dowdell, B., Oestreicher, N., Sahrmann, S., 2000. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin. J. Sports Med. 10, 169–175. Grood, E., Suntay, M., 1983. A joint coordinate system for the clinical description of three-dimensional motions: applications to the knee. J. Biomech. Eng. 105, 136– 144. 34 K.R. Snyder et al. / Clinical Biomechanics 24 (2009) 26–34 Hreljac, A., Marshall, R.N., Hume, P.A., 2000. Evaluation of lower extremity overuse injury potential in runners. Med. Sci. Sports Exerc. 32, 1635–1641. Ireland, M., 2002. The female ACL: why is it more prone to injury? Orthop. Clin. North Am. 33, 637–651. Ireland, M., Willson, J., Ballantyne, B., Davis, I., 2003. Hip strength in females with and without patellofemoral pain. J. Orthop. Sports Phys. Ther. 33, 671–676. Kaufman, K.R., Brodine, S.K., Shaffer, R.A., Johnson, C.W., Cullison, T.R., 1999. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am. J. Sports Med. 27, 585–593. Knutzen, K., Price, A., 1994. Lower extremity static and dynamic relationships with rearfoot motion in gait. J. Am. Pod. Med. Assoc. 84, 171–180. Leetun, D., Ireland, M., Willson, J., Ballantyne, B., Davis, I., 2004. Core stability measures as risk factors for lower extremity in athletes. Med. Sci. Sports Exerc. 36, 926–934. Malinzak, R., Colby, S., Kirkendall, D., Yu, B., Garrett, W., 2001. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin. Biomech. 16, 438–445. Mascal, C., Landel, R., Powers, C., 2003. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J. Orthop. Sports Phys. Ther. 33, 642–660. Mccomas, A., 1996. Skeletal Muscle Form and Function. Human Kinetics, Champaign, IL. Menz, H., 1998. Alternative techniques for the clinical assessment of foot pronation. J. Am. Pod. Med. Assoc. 88, 119–129. Mueller, M., Host, J., Norton, B., 1993. Navicular drop as a composite measure of excessive pronation. J. Am. Pod. Med. Assoc. 83, 198–202. Nadler, S., Malanga, G., Deprince, M., Stitik, T., Feinberg, J., 2000. The relationship between lower extremity injury, low back pain, and hip strength in male and female collegiate athletes. Clin. J. Sports Med. 10, 89–97. Nawoczenski, D.A., Cook, T.M., Saltzman, C.L., 1995. The effect of foot orthoses on three-dimensional kinematics of the leg and rearfoot during running. J. Orthop. Sports Phys. Ther. 21, 317–327. Niemuth, P., Johnson, R., Myers, M., Thielman, T., 2005. Hip muscle weakness and overuse injuries in recreational runners. Clin. J. Sports Med. 15, 14–21. Nigg, B.M., 2001. The role of impact forces and foot pronation: a new paradigm. Clin. J. Sports Med., 2–9. O’Connor, K., Hamill, J., 2004. The role of selected extrinsic foot muscles during running. Clin. Biomech. 19, 71–77. Powers, C., 2003. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J. Orthop. Sports Phys. Ther. 33, 639–646. Schmitz, R., Riemann, B., Thompson, T., 2002. Gluteus medius activity during isometric closed-chain hip rotation. J. Sport Rehabil. 11, 179–188. Smith, L.S., Clarke, T.E., Hamill, C.L., Santopietro, F., 1986. The effects of soft and semi-rigid orthoses upon rearfoot movement in running. J. Am. Pod. Med. Assoc. 76, 227–233. Stackhouse, C.L., Davis, I.M., Hamill, J., 2004. Orthotic intervention in forefoot and rearfoot strike running patterns. Clin. Biomech. 19, 64–70. Stacoff, A., Reinschmidt, C., Nigg, B.M., van den Bogert, A.J., Lundberg, A., Denoth, J., Stussi, E., 2000. Effects of foot orthoses on skeletal motion during running. Clin. Biomech. 15, 54–64. Starkey, C., Ryan, J., 1996. Evaluation of Orthopedic and Athletic Injuries. F.A. Davis Company, Philadelphia, PA. Stefanyshyn, D., Stergiou, P., Lun, V., Meeuwisse, W., Worobets, J., 2006. Knee angular impulse as a predictor of patellofemoral pain in runners. Am. J. Sports Med. 34, 1844–1851. Taunton, J., Ryan, M., Clement, D., Mckenzie, D., Lloyd-Smith, D., Zumbo, B., 2002. A retrospective case-control analysis of 2002 running injuries. Br. J. Sports Med. 36, 95–101. Tyler, T., Nicholas, S., Mullaney, M., Mchugh, M., 2006. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am. J. Sports Med. 34, 630–636. van Mechelen, W., 1992. Running injuries. A review of the epidemiological literature. Sports Med. 14, 320–335.