Effect of Taping on Actual and Perceived Dynamic Postural
advertisement

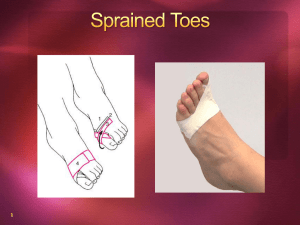
1383 ORIGINAL ARTICLE Effect of Taping on Actual and Perceived Dynamic Postural Stability in Persons With Chronic Ankle Instability Eamonn Delahunt, PhD, Angela McGrath, BSc, Naoise Doran, BSc, Garrett F. Coughlan, PhD ABSTRACT. Delahunt E, McGrath A, Doran N, Coughlan GF. Effect of taping on actual and perceived dynamic postural stability in persons with chronic ankle instability. Arch Phys Med Rehabil 2010;91:1383-9. Objective: To investigate whether 2 different mechanisms of ankle joint taping ([1] lateral subtalar sling or [2] fibular repositioning) can enhance actual and perceived dynamic postural stability in participants with chronic ankle instability (CAI). Design: Laboratory-based repeated-measures study. Setting: University biomechanics laboratory. Participants: Participants (n⫽16) with CAI. Interventions: Participants performed the Star Excursion Balance Test (SEBT) under 3 different conditions: (1) no tape, (2) lateral subtalar sling taping and (3) fibular repositioning taping. Main Outcome Measures: Reach distances in the anterior, posteromedial, and posterolateral directions on the SEBT. Participants’ perceptions of stability, confidence, and reassurance when performing the SEBT under 2 different taping conditions. Results: Taping did not improve reach distance on the SEBT (P⬎.05). Feelings of confidence increased for 56% of participants (P⫽.002) under both tape conditions. Feelings of stability increased for 87.5% of participants (P⬍.001) using condition 2 (lateral subtalar sling taping) and 75% of participants (P⫽.001) using condition 3 (fibular repositioning taping). Feelings of reassurance increased for 68.75% of participants (P⫽.001) using condition 2 (lateral subtalar sling taping) and 50% of participants (P⫽.005) using condition 3 (fibular repositioning taping). Conclusions: No significant change in dynamic postural stability was observed after application of either taping mechanism; however, participants’ perceptions of confidence, stability, and reassurance were significantly improved. Further research is necessary to fully elucidate the exact mechanisms by which taping may help reduce the incidence of repeated injury in subjects with CAI. Key Words: Ankle joint; Ankle sprain; Rehabilitation. © 2010 by the American Congress of Rehabilitation Medicine From the School of Public Health, Physiotherapy and Population Science (Delahunt, McGrath, Doran, Coughlan) and Institute for Sport and Health (Delahunt, Coughlan), University College Dublin, Dublin, Republic of Ireland. No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated. Reprint requests to Eamonn Delahunt, PhD, School of Public Health, Physiotherapy and Population Science, University College Dublin, Health Science Centre, Belfield, Dublin 4, Republic of Ireland, e-mail: eamonn.delahunt@ucd.ie. 0003-9993/10/9109-00185$36.00/0 doi:10.1016/j.apmr.2010.06.023 NJURY TO THE LATERAL ligament complex of the ankle Isports joint is 1 of the most frequently encountered injuries in medicine. After the initial injury, the potential devel1 opment of CAI is of primary concern to clinicians involved in the treatment and rehabilitation of musculoskeletal injuries.2 CAI is dependent on the interaction of various mechanical and functional insufficiencies, which give rise to the 2 frequently encountered clinical phenomena of subjective reporting of “giving way” of the ankle joint and subjective reporting of “feelings” of ankle joint instability.2 Mechanical insufficiencies proposed to be associated with the development of CAI include pathologic laxity, articular synovial changes, degenerative changes, and arthrokinematic restrictions.2 Functional insufficiencies proposed to contribute to the development of CAI include impaired proprioception, impaired neuromuscular control, impaired postural control, and deficits in strength.2 Of those functional insufficiencies believed to contribute to the development of CAI, postural stability has received much attention. Previous prospective research has indicated that decreased postural stability is a predictor of lower-limb injury and, in particular, ankle sprain.3,4 A recently published metaanalysis has comprehensively concluded that subjects with CAI exhibit postural stability deficits in both static and dynamic situations.5 One measure of dynamic postural stability is the SEBT. The SEBT involves moving from a start position of bilateral stance to a single-leg stance while maximally reaching along set multidirectional lines with the opposite leg without compromising equilibrium. It has good intra- and intertester reliability.4,6,7 Olmsted et al8 were the first to investigate the efficacy of the SEBT in detecting postural stability impairments in a population of patients with CAI. Compared with healthy controls and the subject’s own uninjured side, decreased mean reach distances in all directions in the CAI group were observed, suggesting that the SEBT is a functional test capable of detecting impairment in CAI. Other studies have described similar deficits in a CAI population.9,10 Recently, McKeon and Hertel11 indicated that instrumented forceplate testing is more appropriate for assessing those at risk for ankle joint injury and postural stability deficits immediately after an acute injury episode than for detecting deficits associated with CAI. However, readers also must be cognizant of the fact that static testing, especially with eyes open, may not optimally test postural control strategies of subjects with CAI, and perhaps more dynamic measures are needed to address this issue. Therefore, the SEBT may be an applicable clinical tool for assessing postural stability deficits in subjects with CAI. Prevention of injury and repeated injury have become an increasingly important focus of practice and rehabilitation, especially in relation to the ankle joint.12 One successful List of Abbreviations CAI CAIT SEBT chronic ankle instability Cumberland Ankle Instability Tool Star Excursion Balance Test Arch Phys Med Rehabil Vol 91, September 2010 1384 TAPE AND ANKLE INSTABILITY, Delahunt method of reducing the occurrence of ankle joint injury is through the use of external prophylactic ankle supports, such as tape. Previous research has shown that ankle joint taping is most effective in reducing the incidence of repeated injury in subjects with a history of ankle joint injury.12,13 Two methods of ankle joint taping that have received little attention in the literature are the lateral subtalar sling14 and fibular repositioning taping mechanisms.15 The lateral subtalar sling taping mechanism is based on the fact that severe damage to the lateral ligament complex of the ankle joint has been associated with an increased talar tilt.14 This taping technique aims to resist subtalar inversion. We chose to use this technique because it has been noted that subjects with CAI show increased inversion of the rear foot during walking and jump landing.16-19 Fibular repositioning tape works on the premise that after an acute ankle sprain, there is an anterior positional fault at the inferior tibiofibular joint.15 This premise has recently been supported by Hubbard et al.20 Furthermore, a recent study by Moiler et al21 has shown that the use of fibular repositioning tape significantly reduced the incidence of ankle joint injury in a group of basketball players. However, the exact mechanism underlying this reduced incidence of ankle joint injury could not be elucidated. Two recently published articles have reported on ankle joint taping and postural stability in subjects with CAI. In a study by Sawkins et al,22 the investigators aimed to study the effect of 2 different taping techniques (real vs placebo vs no tape) on functional performance measured by using a hopping drill and dynamic postural stability measured by means of performance on the SEBT in a group of subjects with CAI. Results of the study did not show a statistically significant effect across conditions for SEBT reach distance performance or functional performance. However, a secondary analysis indicated that both taping mechanisms resulted in increased subject perceptions of stability, confidence, and reassurance when performing both the functional hopping drill and SEBT. The real taping technique used involved a combination of 3 stirrups, a figure of 6, and a heel lock, whereas the placebo taping technique involved application of a 10-cm long inelastic strip placed above the lateral malleolus in line with the lateral aspect of the shank. Furthermore, a study by Hopper et al23 investigated the effect of fibular repositioning tape on parameters of static and dynamic postural stability, with no positive enhancement of these parameters observed. However, 1 limitation of this study was that all outcome measures used were instrumented forceplate measures, which McKeon and Hertel11 previously have suggested may not be the most sensitive for the measurement of postural stability in subjects with CAI. Owing to the potential effects of taping on reducing the incidence of ankle injury and with decreased postural stability being reported as a risk factor for ankle joint injury, further investigations into the effects of taping on a dynamic measure of postural stability, as well as participants’ perceptions of the benefits of taping, is warranted. The aim of the present study was to investigate the effects of 2 different ankle joint taping mechanisms on participant actual and perceived dynamic postural stability in a group of subjects with CAI. We chose to use 2 mechanisms of taping that have received little attention in the literature. The first mechanism of taping was the lateral subtalar sling because this mechanism of taping is purported to restrict rear-foot inversion,14 which has previously been shown to be a functional deficiency in subjects with CAI. 16-19 To our knowledge, only 1 previously published study has used the lateral subtalar sling mechanism of taping.24 The second mechanism of taping was the fibular repositioning technique because this has previously been shown to reduce the Arch Phys Med Rehabil Vol 91, September 2010 incidence of ankle joint injury.21 However, the exact mechanism of action could not be elucidated. Furthermore, only 1 previous study has reported on the effects of this mechanism of ankle joint taping on postural stability, and the outcome measures may not have been the most sensitive measures for identifying postural stability effects in subjects with CAI. We hypothesized that both taping mechanisms would be accompanied by an increase in reach distance on the SEBT compared with the control untaped trials. Furthermore, we hypothesized that participants would report increased feelings of confidence, stability, and reassurance when performing the SEBT with both mechanisms of ankle joint taping compared with the control untaped trials. Participants Subject recruitment was undertaken by placing notices on the university sports center and school notice boards. Nineteen potentially suitable candidates contacted the investigators, expressing an interest in participation in the study. Potentially interested subjects were interviewed by a member of the research team regarding their ankle joint injury history, and all interested candidates were also required to complete the CAIT for their left and right ankle joints.25 Specific inclusion criteria were a history of 2 or more inversion sprains to the same ankle joint, a subjective history of episodes of giving way of the ankle joint, a subjective reporting of feelings of ankle joint instability during sporting participation, and a CAIT score of 24 or lower. A history of eversion sprain or distal tibiofibular joint (high ankle sprain) injury precluded a subject from inclusion in the present study. Of 19 potentially suitable candidates, 16 meet the full inclusion criteria. Two subjects were excluded because they did not score 24 or loweron the CAIT, whereas another candidate was excluded because of a recent ankle joint sprain (1 week before the start of the study). After the initial interview with the research team, 16 participants were included in the study (10 women, 6 men; age, 21.32⫾1.35y; height, 1.76⫾.08m; mass, 74.94⫾10.43kg; sports participation as follows: 6 participated ⬎6 hours a week, 2 participated 5– 6 hours a week, 4 participated 4 –5 hours a week, 1 participated 3– 4 hours a week, 1 participated 2 to 3 hours a week, and 3 participated 1 to 2 hours a week; sports played: 3 played basketball, 3 played GAA (indigenous Irish field sport), 1 played rugby union, 3 played hockey, 6 attended the gym). Ten participants had bilateral CAI, and the remaining 6 had unilateral CAI. For those with bilateral CAI, the ankle with the lowest CAIT score was tested. Of 16 participants, 8 had left ankle instability and 8 had right ankle instability. The mean CAIT score for left instability was 16.63, and the mean CAIT score for right instability was 17.38. All participants were evaluated for mechanical instability using the anterior drawer test (9 scored 1, 5 scored 2, and 2 scored 3) and talar tilt test (10 negative and 6 positive results) as described by Lynch.26 Mechanical instability was defined as “excessive inversion laxity of the rear foot or excessive anterior laxity of the talocrural joint as assessed using instrumented (arthrometry or stress radiography) or manual stress testing” according to the definition of Delahunt et al.27 The tests of mechanical instability did not form part of the formal inclusion criteria, but were used to assess the amount of ankle joint laxity present in each participant. Performance of these tests was carried out by the principal investigator, who is a qualified physiotherapist with 6 years of post qualification clinical experience. Talar tilt was scored as positive or negative. Laxity on the anterior drawer test was scored on a scale of 0 to 3: 0 represented no instability with a firm end feel, 1 represented mild instability, 2 indicated TAPE AND ANKLE INSTABILITY, Delahunt 1385 position. The vertical component of ground reaction force data was used to determine the onset and termination of each trial. During each trial, participants were required to place their hands on their hips while reaching in the specified direction. Furthermore, participants were required to maintain contact between the forceplate and heel during each trial. A trial was deemed invalid if participants failed to keep their hands on their hips, lifted or moved their stance foot, transferred weight onto the reach foot when touching the measuring tape, failed to touch the tape, failed to return the reach foot to the starting position, or lost their balance and failed to maintain a unilateral stance position during performance of the trial. Invalid trials were discarded and additional trials were completed. A mark was made by 1 of the investigators on the directional component of the SEBT. For ease of quantification of each reach distance, the line of the SEBT directional component was simulated by a 1.5-m measuring tape (see fig 1). Reaching distances were read from the center of the grid to the marked point of maximum reach. Reach distances were divided by leg length and multiplied by 100 to calculate a dependent variable that represents reach distance as a percentage of leg length. This method has been used previously by Gribble et al.30 Both the order of performance of each test condition and the order of reaching directions were randomized using a method of concealed envelopes. The order of reaching directions was kept consistent between each test condition (ie, no tape, subtalar sling taping, fibular repositioning taping). Fig 1. SEBT setup on forceplates. moderate instability, and 3 was characterized by gross instability with a positive sulcus sign. Ethical approval was received from the university ethical review board. All participants signed a university-approved informed consent form on the day of testing. SEBT Performance The SEBT was performed with the participant standing barefoot bilaterally on 2 forceplates.a The anterior, posteromedial, and posterolateral directions of the SEBT were chosen as per previous studies (fig 1). Before the start of each test session, each participant was informed how to perform the test and allowed 4 practice trials in each direction, as recommended by Robinson and Gribble.28 Three consecutive trials in each direction were performed after a short rest period. During performance of the test, each participant initially stood at the center of a grid laid on the laboratory floor and extending from the forceplate directly under the test leg. Similar to the protocol explained by Hertel et al,29 a “crosshairs” was drawn at the center of the grid. The length and width of the test foot were measured, and the foot was placed such that the geometric center of the foot was aligned with the intersection of the crosshairs for each individual trial. Participants were required to reach as far as possible along the directional component of the SEBT (ie, anterior, posteromedial, or posterolateral direction) and make a light touch with the most distal part of the foot. Each trial was initiated when participants transitioned from double- to single-leg stance, with the trial ending when subjects returned to a double-leg stance Forceplate Data Ground reaction forces were measured at 100Hz while participants performed the SEBT trials. The vertical component of ground reaction force data was used to determine the onset and termination of each trial. A threshold of 2.5N was used for identification of the transition from double- to single-leg stance and also for the transition from single- to double-leg stance. Taping Techniques For consistency, all taping techniques were applied by the principal investigator. The tape was applied with the participant in a supine position on a plinth. The techniques are as follows below: Condition 1: no tape. During condition 1 (no tape), participants performed the SEBT trials without tape applied to their test ankle joint. Condition 2: lateral subtalar sling. During condition 2 (lateral subtalar sling), each participant performed the SEBT trials after application of 2 lateral subtalar slings by the principal investigator. For the first strip, Leukotape P tapeb was applied from the base of the first metatarsal head on the plantar aspect of the foot diagonally toward the fifth metatarsal head, then angled at 45° toward the lateral malleolus around the posterior Achilles’ tendon and brought anteriorly to finish at the lower one-third of the tibia above the malleoli, similar to the technique used by Wilkerson.14 A second reinforcing strip was applied in the same manner overlapping by half the width of the first strip. The lateral subtalar sling is shown in fig 2. Condition 3: fibular repositioning tape. During condition 3 (fibular repositioning tape), each participant performed the SEBT trials after fibular repositioning tape application applied by the principal investigator. The initial strip of Leukotape P started at the distal end of the lateral malleolus. The tape then was orientated obliquely while a painfree posterolateral glide was applied to the distal fibula with the tape finishing on the lower one-third of the tibia above the malleoli. A second reinforcing strip was applied in the same manner overlapping Arch Phys Med Rehabil Vol 91, September 2010 1386 TAPE AND ANKLE INSTABILITY, Delahunt effect sizes for reach differences in an uninjured group and a CAI group. Using an alpha of .05 and a power of 0.8 with a correlation of 0.8 among our dependent variables, we computed a sample size of 15 subjects.32 Repeated-measures analysis of variance was used to test the effects of taping on parameters of postural stability (SEBT performance). Descriptive statistics were used to summarize participants’ responses to the question of perceptions of stability, confidence, and reassurance. Furthermore, we used Wilcoxon signed-rank test to determine participants’ responses to questions relating to perceptions of stability, confidence, and reassurance. An alpha level of .05 was chosen. All statistical analyses were performed using SPSS.c RESULTS SEBT Performance There were no statistically significant differences in reach distance among the 3 conditions on the SEBT (F6,56⫽1.30; P⫽.273). Results are listed in table 1. Fig 2. Lateral subtalar sling. by half the width of the first. The fibular repositioning tape application is shown in fig 3 and further detailed in an article published by Moiler et al.21 Perceptions of Stability, Confidence, and Reassurance After the completion of each set of SEBT directional trials under each condition, participants were questioned regarding their perceived levels of stability, confidence, and reassurance when performing the test compared with the practice trials.22 Each participant was required to answer with 1 of the following options: (1) no change, (2) more than the practice trial, or (3) less than the practice trial. Stability referred to how steady and controlled the participant felt; confidence referred to how well the participant believed he/she could perform the test, and reassurance referred to how confident the participant was that he/she would not sprain their ankle while performing the test. For example, after completion of the SEBT with either taping condition, participants were asked “when performing the test, how stable/confident/reassured did you feel compared to the practice trials?” All questions were presented in written format to the participant, who was asked to read the questions and tick the appropriate answer. Questions were presented in written format with the aim of negating any bias that verbal questioning from the investigators could introduce (fig 4). Statistical Analysis Sample size was computed using data previously published by Hale et al,31 who showed low (eg, .41) to moderate (eg, .55) Arch Phys Med Rehabil Vol 91, September 2010 Perceptions of Stability, Confidence, and Reassurance Participants’ perceptions of stability, confidence, and reassurance on the SEBT as a result of application of the taping techniques are detailed next and shown in fig 5. Feelings of confidence increased for 56% of participants (n⫽9; P⫽.002) under both tape conditions. Feelings of stability increased for 87.5% of participants (n⫽14; P⬍.001) using condition 2 (lateral subtalar sling taping) and 75% of participants (n⫽12; P⫽.001) using condition 3 (fibular repositioning taping). Feelings of reassurance increased for 68.75% of participants (n⫽11; P⫽.001) using condition 2 (lateral subtalar sling taping) and 50% of participants (n⫽8; P⫽.005) using condition 3 (fibular repositioning taping). No statistically significant differences were noted for participants’ responses comparing the 2 taping conditions (P⬎.05). DISCUSSION Our primary hypothesis, that both taping mechanisms would be accompanied by an increase in reach distance on the SEBT compared with the control untaped trials, was not confirmed by results of the present study. Our secondary hypothesis, that participants would report increased feelings of confidence, stability, and reas- Fig 3. Fibular repositioning tape. TAPE AND ANKLE INSTABILITY, Delahunt 1387 Fig 4. Quantification of perceptions of stability, confidence, and reassurance. surance when performing the SEBT trials with both mechanisms of ankle joint taping compared with the control untaped trials, was confirmed by results of the present study. Results of the present study indicate that the 2 different taping techniques used did not positively or negatively affect dynamic postural stability measured using the SEBT. Results of the present study concur with those observed by Sawkins et al22 and more recently by Hopper et al.23 In the study by Sawkins,22 the authors aimed to investigate the effect of 2 different taping techniques (real vs placebo vs no tape) on functional performance and dynamic postural stability in a group of Table 1: Reach Distance in Each Direction Direction Condition 1: No Tape Condition 2: Lateral Subtalar Sling Condition 3: Fibular Repositioning Tape Anterior Posteromedial Posterolateral 76.26⫾3.99 79.78⫾8.97 71.38⫾10.19 77.42⫾3.57 81.44⫾8.96 73.57⫾10.10 77.35⫾3.48 81.49⫾10.39 74.98⫾10.16 NOTE. Values are percentage of leg length (n⫽16 in each condition). subjects with CAI. Results of the study did not show a statistically significant effect across conditions for SEBT reach distance performance. The real taping technique used involved a combination of 3 stirrups, a figure of 6, and a heel lock, whereas the placebo taping technique involved application of a 10-cm long inelastic strip placed above the lateral malleolus in line with the lateral aspect of the shank. Thus, the mechanism of taping used differed considerably from those in the present study, in which we used a lateral subtalar sling and fibular repositioning technique. The recent publication by Hopper23 investigated the effect of fibular repositioning tape on parameters of static and dynamic postural stability, with no positive enhancement of these parameters observed. However, the postural stability measures used by these investigators all involved instrumented forceplate measures, which may not be the most sensitive for detecting postural stability deficits in subjects with CAI.11 Taken together, results of the present study along with those of Sawkins,22 and Hopper,23 and colleagues suggest that taping may not enhance postural stability in subjects with CAI. Taping has reduced the incidence of recurrent ankle sprain in subjects with CAI.12,13 One possible mechanism of action of ankle joint taping is through a placebo effect; the athlete believes that the taping technique will reduce their risk of injury.22 In the present Arch Phys Med Rehabil Vol 91, September 2010 1388 TAPE AND ANKLE INSTABILITY, Delahunt could provide new insights into how ankle joint taping could influence functional performance in sports. The use of taping by clinicians for subjects with CAI requires due consideration and may not be appropriate for all athletes. It is the responsibility of clinicians to complete a rigorous physical and sensorimotor evaluation of the specific functional and mechanical insufficiencies present and then decide whether taping is likely to be an appropriate prophylactic measure. Particular emphasis should be given to the perception of comfort of the taping technique applied and also to the particular demands of the sport. Fig 5. Participants’ perceptions of confidence, stability, and reassurance. The y-axis values represent the number of participants reporting an increase in confidence, stability, and reassurance. Abbreviations: FRP, fibular repositioning taping mechanism; LSS, lateral subtalar sling taping mechanism. study, participants were given an explanation of the believed mechanisms of action of the 2 taping techniques used. Several participants remarked at how little tape was used for these techniques compared with the more robust traditional ankle-taping techniques. This may have negatively influenced their perceptions of the techniques. However, statistical analysis of participants’ responses showed that lateral subtalar sling and fibular repositioning taping improved most participants’ perceptions of stability, confidence, and reassurance while performing the SEBT. However, these increased feelings of confidence, reassurance, and stability did not reflect in increased reach distances on the SEBT. Despite this observation, we believe that every effort should be made by clinicians to emphasize the potential benefits of ankle joint taping because this is likely to enhance feelings of confidence, stability, and reassurance. A recent systematic review has shown that ankle joint taping can reduce the incidence of ankle joint repeated injury in subjects with a history of ankle joint sprain.12 Further research is necessary to fully elucidate the exact mechanisms by which taping may help reduce the incidence of repeated injury in subjects with CAI. The seminal work of Hertel2 suggests that the development of CAI is dependent on the interaction of various mechanical and functional insufficiencies. Potential mechanical insufficiencies that ankle joint taping could influence include arthrokinematic restriction and pathologic laxity, whereas the functional insufficiencies that ankle joint taping could influence include proprioceptive and neuromuscular control deficits. Results of a recently published study24 suggest that taping may provide a more mechanical effect on the ankle joint by restricting touchdown plantar flexion and thus reducing vulnerability to ankle sprain, hence influencing any presence of mechanical laxity and potentially improving neuromuscular control strategies. In a more recent publication, Hertel33 has outlined the spectrum of sensorimotor measures that have been used to investigate deficits in subjects with CAI. These sensorimotor measures range from purely passive measures, such as measures of proprioception, to more dynamic measures replicating normal activities of daily living and athletic participation, such as walking, running, landing, and cutting. We believe that further research into the mechanisms of action of ankle joint taping is warranted and suggest that researchers concentrate on the mechanical and functional insufficiencies proposed to manifest in the presence of CAI. Furthermore, research should be undertaken at the dynamic end of the sensorimotor spectrum because this Arch Phys Med Rehabil Vol 91, September 2010 CONCLUSIONS Results of the present study suggest that the 2 mechanisms of ankle joint taping used (lateral subtalar sling and fibular repositioning) do not positively influence dynamic postural stability in subjects with CAI. However, taping seems to positively influence subjects’ perceptions of stability, reassurance, and confidence when performing a dynamic postural stability task. This suggests that ankle joint taping can be used in subjects with CAI, and that every effort should be made by clinicians to emphasize the potential benefits of taping. References 1. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med 2007;37:73-94. 2. Hertel J. Functional anatomy, pathomechanics and pathophysiology of lateral ankle instability. J Athl Train 2002;37:364-75. 3. McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med 2000;10:239-44. 4. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther 2006;36:911-9. 5. Arnold BL, De La Motte S, Linens S, Ross SE. Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc 2009;41:1048-62. 6. Hertel J, Miller SJ, Denegar CR. Intratester and intertester reliability during the star excursion balance tests. J Sports Rehabil 2000;9:104-16. 7. Kinzey SJ, Armstrong CW. The reliability of the star-excursion test in assessing dynamic balance. J Orthop Sports Phys Ther 1998;27356-60. 8. Olmstead LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the star excursion balance tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train 2002;37:501-6. 9. Gribble PA, Hertel J. Considerations for normalizing measures of the star excursion balance test. Meas Phys Ed Ex Sci 2003;7:89-100. 10. Sefton JM, Hicks-Little CA, et al. Sensorimotor function as a predictor of chronic ankle instability. Clin Biomech 2009;24:451-8. 11. McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part I: can deficits be detected with instrumented testing. J Athl Train 2008;43:293-304. 12. Dizon JMR, Reyes JJB. A systematic review on the effectiveness of external ankle supports in the prevention of inversion ankle sprains among elite and recreational players. J Sci Med Sport 2010;13:309-17. 13. Mickel TJ, Bottoni CR, Tsuji G, Chang K, Baum L, Tokushige KA. Prophylactic bracing versus taping for the prevention of ankle sprains in high school athletes: a prospective, randomized trial. J Foot Ankle Surg 2006;45:360-5. 14. Wilkerson GB. Biomechanical and neuromuscular effects of ankle taping and bracing. J Athl Train 2002;37:436-45. 15. Mulligan BR. Self treatments for backs, necks, limbs: a new approach. Wellington (New Zealand): Plane View Services; 2003. TAPE AND ANKLE INSTABILITY, Delahunt 16. Delahunt E, Monaghan K, Caulfield B. Ankle function during hopping in subjects with functional instability of the ankle joint. Scand J Med Sci Sports. 2007;17:641-8. 17. Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med 2006; 34:1970-6. 18. Delahunt E, Monaghan K, Caulfield B. Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. J Orthop Res 2006;24:1991-2000. 19. Monaghan K, Delahunt E, Caulfield B. Ankle function during gait in patients with chronic ankle instability compared to controls. Clin Biomech (Bristol, Avon). 2006;21:168-74. 20. Hubbard TJ, Hertel J, Sherbondy P. Fibular positioning in individuals with self-reported chronic ankle instability. J Orthop Sports Phys Ther 2006;36:3-9. 21. Moiler K, Hall T, Robinson K. The role of fibular tape in the prevention of ankle injury in basketball: A pilot study. J Orthop Sports Phys Ther 2006;36:661-8. 22. Sawkins K, Refshauge K, Kilbreath S, Raymond J. The placebo effect of ankle taping in ankle instability. Med Sci Sports Exerc 2007;39:781-7. 23. Hopper D, Samsson K, Hulenik CN, Hall T, Robinson K. The influence of Mulligan ankle taping during balance performance in subjects with unilateral chronic ankle instability. Phys Ther Sport 2009;10:125-30. 24. Delahunt E, O’Driscoll J, Moran K. Effects of taping and exercise on ankle joint movement in subjects with chronic ankle instability: a preliminary investigation. Arch Phys Med Rehabil 2009;90: 1418-22. 25. Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil 2006;87:1235-41. 1389 26. Lynch SA. Assessment of the injured ankle in the athlete. J Athl Train 2002;37:406-12. 27. Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin CW, Hiller CE. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc 2010; In press. 28. Robinson RH, Gribble PA. Support for the reduction in the number of trials needed for the Star Excursion Balance Test. Arch Phys Med Rehabil 2008;89:364-70. 29. Hertel J, Braham RA, Hale SA, Olmstead-Kramer LC. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther 2005;36:131-7. 30. Gribble PA, Hertel J, Denegar CR. Chronic ankle instability and fatigue create proximal joint alterations during performance of the star excursion balance test. Int J Sports Med 2007;28:236-42. 31. Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther 2007;37:303-11. 32. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioural, and biomedical sciences. Behav Res Methods 2007; 39:175-91. 33. Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med 2008;27:353-70. Suppliers a. AMTI, 176 Waltham St, Watertown, MA 02472. b. BSN Medical Ltd, Willerby, Hull, East Yorkshire HU10 6WT, UK. c. Version 15; SPSS Inc, 233 S Wacker Dr, 11th Fl, Chicago, IL 60606. Arch Phys Med Rehabil Vol 91, September 2010