Account 2012/13 Looking after you locally
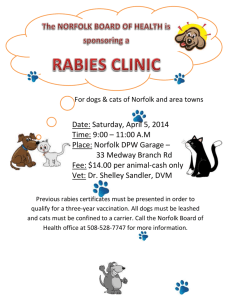
advertisement

Account 2012/13 Looking after you locally 2 Quality Account 2012/13 Our Health Visitors see more than 1,000 new families every month We deliver health services to over 400 schools and colleges Our Community Nursing teams have around 108,000 face-to-face contacts with patients every month We have 3,000 members of dedicated NHS staff across the county NCH&C receives 16,500 referrals from GPs and other healthcare professionals every month More than 3,000 patients per year are admitted to our community hospitals We have around 300 patient beds in Norfolk Our School Nurses hold 1,300 face-to-face appointments with children each year We deliver more than 70 different services in and around Norfolk Norfolk Community Health and Care NHS Trust 3 Contents 1.1 Message from the Chairman 4 3.8.5 Local surveys 1.2 Statement from the Chief Executive 5 1.3Statement from the Director of Nursing, Quality & Operations 3.8.6Patient Environment Action Team (PEAT) Assessment 2012 52 7 3.9Patient Safety – learning from incidents and complaints 54 3.9.1Introduction 54 2.1 Priorities for Quality Improvement (2013/2014) 10 3.9.2Complaints, claims and compliments 54 2.2 Quality Goals for 2013/14 3.9.3Serious Incidents Requiring Investigation (SIRIs) 55 1.4 Introduction to Norfolk Community Health and Care NHS Trust (NCH&C) 8 11 2.3 Health & Social Care Integration 50 2.4Transformation Programme for 2013/14 15 3.9.4 Never Events 57 2.5Statements of Assurance from the Board 16 2.5.1 Review of services 16 3.9.5National Patient Safety Agency Report (NPSA) 57 2.5.2 Participation in clinical audit 18 3.9.6 Safety Alerts 58 2.5.3 Participation in clinical research 21 2.5.4 Goals agreed with commissioners 22 3.9.7Reducing the level of harm of medication incidents 58 2.5.5 Statement from the Care Quality Commission (CQC) 3.9.8 Patient falls 60 23 3.9.9Infection prevention and control 61 2.5.6 Data quality 25 2.5.7 Information Governance Toolkit attainment levels 3.9.10 P atient safety and quality benchmarking data 62 26 2.5.8 Clinical coding error rate 26 3.9.11 S afeguarding vulnerable adults and children 63 2.5.9National Quality Indicators 27 3.10Effectiveness of Care 64 3.10.1Introduction 64 3.10.2National Institute for Health and Clinical Excellence (NICE) 64 3.10.3The Colman Centre for Specialist Rehabilitation (CCSRS) 66 3.10.4Podiatric Surgery – PASCOM 10 audit system 67 3.10.5Research and Development 68 34 3.10.6Clinical Audit Plan 2012/13 69 35 4Explanation of who has been involved and engaged with 3.1 Review of Quality Performance in 2012/13 29 3.2 Our Workforce 30 3.2.1National Staff Survey 2012 31 3.2.2 Mandatory training 32 3.2.3Appraisals 32 3.2.4Staff achievements and awards 33 3.2.5A selection of compliments and ‘thank yous’ 3.3Performance Highlights over 2012/13 3.4Commissioning for Quality and Innovation (CQuIN) Scheme 2012/13 38 4.1Comments from Norfolk Healthwatch (previously Norfolk LINk) 70 4.2Comments from Norfolk Health Overview and Scrutiny Committee 3.5Clinical Quality and Quality Goals for 2012/13 40 3.6Monitor’s Quality Governance Framework 44 3.7 Quality Assessment Visits 46 3.8 Patient Experience 47 3.8.1Introduction 47 3.8.2 The ‘Friends and Family Test’ 48 3.8.3 Patient Stories 49 3.8.4 Patient Opinion 50 70 70 4.3Comments from South Norfolk Clinical Commissioning Group 71 5 Declaration by all Directors 72 4 Quality Account 2012/13 1.1 Message from the Chairman It is with confidence and pride that NCH&C presents its Quality Account for 2012/13. The coming year will see a number of transformational changes in the way that we deliver our community based services. Building on the great work that has been completed in 2012/13, improving the quality of our services, we now look towards getting even better through our transformation programme. The recent report of the Mid Staffordshire NHS Foundation Trust Public Inquiry chaired by Robert Francis QC (herein referred to as the Francis Report) offers a timely reminder of those things each and every one of us within the NHS needs to remember in everything we do. We need to make sure that patients are and continue to be our first and foremost consideration. We need to continue to listen to our patients and staff, encouraging openness and honesty, and monitoring our performance carefully. Our approach to transformation and further improvements to quality are, and will always be, delivered in the framework for delivery as set out by Francis. High quality patient care continues to be at the centre of all we do. A major challenge will be finding new ways of working to help us meet increasing demand, within a constrained funding envelope. Our Transformation Programme will enable us to be fit for the future and help us to keep people in their homes, and cared for in the community by embracing technology; empowering our people; and reviewing our systems. We, the Board of NCH&C, with and on behalf of all our staff, commit ourselves to continuing to deliver high quality patient care, in order to realise our vision, ‘Looking after you locally’. Ken Applegate Norfolk Community Health and Care NHS Trust 5 1.2 Statement from the Chief Executive NCH&C will deliver against its vision of improving the quality of people’s lives through the best in integrated health and care... The vision of Norfolk Community Health and Care NHS Trust (NCH&C) is to improve the quality of people’s lives, in their homes and community by providing the best in integrated health and social care. This is summarised by the Trust’s strapline “Looking after you locally”. The golden thread running through 2012/13 has been the measurable improvement in quality across the portfolio of our services. In summary we have: • Been building strong relationships with the emerging Clinical Commissioning Groups (CCGs) and Norfolk County Council (NCC) • Performed very well against our quality goals • Implemented newly defined services, such as a new CCG led specification for community nursing and therapy • Engaged our partner local providers • Delivered a cost improvement programme of £7.44m recurrent savings • Achieved financial balance and delivered our planned surplus • Worked hard to engage our staff, as is evidenced by improved staff survey results • Successfully addressed areas of service underperformance • Been an active partner in the development of system-wide plans for quality, innovation, productivity and prevention (QIPP) Our improvements have resulted in us progressing on the journey to foundation trust (FT) status, and in the strengthening of our governance arrangements. The themes of the recent Francis Report will form the cornerstone of our work this year. Patients are the first and foremost consideration of NCH&C. We will continue to listen to our patients and staff, encouraging openness, transparency and candour. We will ensure senior and professional accountability through the measurement and understanding of performance, addressing any issues immediately. We will continue on our journey to FT status, not as an end in itself, but as a key enabler to the continued delivery of high quality, safe patient care. 6 NCH&C will be a strong, independent and expert community provider that offers competitive services, in an increasingly challenging and changing environment. This will help us deliver our vision of ‘improving the quality of people’s lives through the best in integrated health and care’. The result will be to support us and our GP, social care and secondary care partners in the development of integrated care pathways and integrated services. We will have a secure platform for exploring opportunities to extend into the delivery of Continuing Care. NCH&C has been making good progress on discussions with Norfolk County Council (NCC) in relation to the integration of adult health and social care. This builds on our existing Integrated Care Organisation (ICO) work and pilot work in the west of the county. We are exploring what the next stage may look like and are going to be considering a range of options. NCH&C staff are being encouraged to feedback their early views. Transformation and further improving quality will be the familiar day-to-day experience of our patients, carers, customers and staff in 2013/14. I hope you will find our Quality Account for 2012/13 informative and helpful in reviewing our progress against our key priorities for the forthcoming year. Declaration and endorsement The content of this Quality Account has been endorsed by the Trust Board and has taken into account feedback, where provided, from our lead commissioners, our local population via Norfolk Healthwatch and Norfolk County Council’s Health Overview and Scrutiny Committee. In line with recommendations made in the Francis Report, this Quality Account is accompanied by a declaration signed by all directors in office at the date of the account certifying that they believe the contents to be true or, alternatively, a statement of explanation as to the reason any such director is unable, or has refused to, sign such a declaration. Michael Scott Quality Account 2012/13 Norfolk Community Health and Care NHS Trust 7 1.3 Statement from the Director of Nursing, Quality & Operations We are committed to high quality care... High Quality Care is about ensuring that those who use our services get the right care, when they need it, by the right person and that it is delivered with compassion. The recently published Francis Report into Mid Staffordshire Hospital has sent shockwaves throughout the NHS. We have taken the report very seriously and although we are confident that we do provide high quality care, we are not complacent. We are in the process of holding a number of staff engagement workshops to discuss the Francis Report and hear directly from our staff what we can do to continue to develop our quality culture. We have already undertaken a significant amount of work to identify our organisational values and have made a concerted effort to recruit people who share those values. We also know that recruiting people for their values on its own isn’t enough - we need to support them to live those values by creating the culture for safe and compassionate care – enabling staff to do the right thing. We believe that there is an inextricable link between quality, values and behaviour – where these are aligned, then patients will have better outcomes and a better experience and perspective of the care they received. In order to achieve this, we are investing in staff training, supervision and development and using a behavioural competency framework to support this. We are raising the awareness of the importance of providing compassionate care and promoting a safety culture - looking beneath the surface to identify and learn from ‘near misses’ as well as learning from things when they go wrong. Part of our learning from incidents is to share information ‘when things go wrong’ with our patients to gain their experience of care. Francis highlights the need for doctors and nurses to be transparent about the care they give and this is being formalised in a new ‘duty of candour’. We are also promoting the importance of being proactive and considering what could potentially go wrong, so that we can plan for and mitigate any risks. In order to achieve a high quality culture we also recognise the need to embrace a continuous improvement mindset – this means actively seeking out best practice and identifying new and improved ways of providing care. By investing in the wellbeing and professional development of our staff, they can then fulfil their calling by providing outstanding care for patients. Anna Morgan 8 Quality Account 2012/13 1.4 Introduction to Norfolk Community Health and Care NHS Trust (NCH&C) The vision of Norfolk Community Health and Care NHS Trust (NCH&C) is to improve the quality of people’s lives, in their homes and community by providing the best in integrated health and social care. This is summarised in the Trust’s strap-line “Looking after you locally”. Our business units provide: 1.Children’s Services, which includes prevention and health promotion services 2.Specialist Services, such as neurological rehabilitation or re-ablement services 3.Adult community services delivered on a locality basis coterminous with the areas covered by Clinical Commissioning Groups (CCGs) and working in an integrated way with social care NCH&C in summary: 1.Serves 750,000 people, across Norfolk and Waveney 2.Provides services for West Norfolk, North Norfolk, South Norfolk and Norwich CCGs and Norfolk County Council 3.Employs 2,201.26 whole time equivalent staff 4.Delivers care in people’s homes, as well as from over 200 different locations, and through over 400 schools 5.Manages 11 community hospitals, with12 wards and 223 beds (this increases with winter pressure beds) 6.Shows results for the Net Promoter test of NCH&C in the top quartile (71 or over) consistently with the exception of one month 7.Our income in 2012/13 was £124.8m The starting point for NCH&C is always the patient – providing individualised care and focusing on maintaining independence. This means that quality is at the heart of everything NCH&C does. The Trust’s services are built up around the patient working closely with GPs as partners, whether as commissioners and thereby customers, or as fellow providers. The unique role of a community trust provides continuity of care on an ongoing basis, treats people at the earliest intervention possible, close to or in their own homes and place of their choosing. As a community trust we aim to lead out of hospital community healthcare, giving children a better start and adults greater independence. We will typically do so in their own home or place of choosing. This, combined with the fact that we are a major employer and operate from multiple sites, means that we are both ‘in’ and ‘of’ the community. The Trust and its commissioners believe that a strong and independent community services provider can be a catalyst for systemic change, enabling commissioners to drive improvements in productivity, quality and outcomes, yet in the context of financial constraint. Becoming a foundation trust is a means of accelerating and embedding the Trust’s values and its aspiration for a highly engaged workforce, proud of the services it delivers, their local presence and local delivery. The Trust’s approach to Membership and Governors enables a stronger involvement of patients and the public. Norfolk Community Health and Care NHS Trust Highlights from 2012/13 include 18 week wait – referral to treatment target During 2012/13 the Trust had a number of important targets to achieve or maintain. One of the key performance targets to be achieved was the 18 week wait for Referral to Treatment (RTT), where 95% of admitted and non-admitted patients had to receive a definitive treatment or intervention within 18 weeks of referral. Throughout the year, NCH&C made significant improvements with most services either exceeding the target on a consistent basis, or achieving 100%. Infection prevention and control In 2012/13, there were three reported cases of Clostridium Difficile against an annual ceiling of nine cases. All reported cases have been subject to Root Cause Analysis (RCA) to review lessons learned. Despite high levels of Norovirus within the general community, NCH&C has only suffered one cluster of Norovirus. This was quickly and efficiently contained with only four patients affected. The ward did not need to close and their patients were managed within side rooms and a bay. Ultimately it is staff vigilance that has kept NCH&C levels of Norovirus so low over the season. 9 Patient safety – Falls causing harm The Trust agreed an annual ceiling of no more than 4.0 injurious falls per 1,000 Occupied Bed Days (OBDs). Despite in-month variation across the Trust’s inpatient units, the number of falls per 1,000 OBDs was 3.41, a clear improvement on the previous year’s rate of 4.03. Patient safety – Venousthromboembolism (VTE) assessments All community service providers are required to report the level of Venous-Thromboembolism (VTE) assessments for patients admitted to its community hospitals who are at risk of developing a VTE. The Trust established a locally agreed trajectory for 2012/13, against which it would be monitored, and to then achieve the national target of 95% compliance by December 2012. By August 2012, the 95% target had been achieved and since maintained across the Trust. 10 Quality Account 2012/13 2.1 Priorities for Quality Improvement (2013/2014) A range of different methods will be used to support delivery of our Integrated Business Plan’s (IBP) aspiration of ‘attaining the best patient experience in the East of England’. We will continue to use the ‘Friends and Family’ test in our inpatient units, asking patients if they would recommend the service to their friends and family and asking for their comments. This process will be rolled out across our community services during 2013/14. Patient Opinion is a website: www.patientopinion.org. uk where the public can publish their experiences (good or bad) of local health services. The website allows health service staff to interact with these patients to help improve care. There is also the option of giving patients a hard copy feedback card or they can call a freephone number and tell their story over the phone. NCH&C commenced a small pilot in early March 2013 in four services to trial Patient Opinion. 23 stories were posted on the website during April and these stories had been viewed 820 times. There has been some excellent feedback about all of the services included in the pilot and service leads are being encouraged to respond to comments regardless of content to demonstrate that we are actively engaging with their feedback to improve care. Our responses to the Winterbourne and Francis reports will be enacted with a particular focus on patient safety during 2013/14. For example, a series of Francis Report workshops have been scheduled during May and June 2013 in light of the Robert Francis Inquiry into the care provided to patients at Mid Staffordshire Hospital and will be led by members of the Executive Director team. These workshops aim to identify actions we can take to continue to ensure the quality and safety of our services in the future. Norfolk Community Health and Care NHS Trust 11 2.2 Quality Goals for 2013/14 To realise our vision of ‘Improving the quality of people’s lives by providing the best in integrated health and social care’, we will focus on a number of priorities which include our quality goals. High quality care means care that is as safe and effective as possible, where patients are in control and are treated with compassion, dignity and respect; their experience of care being as important as the outcomes of care. High quality care also means focusing on the prevention of illness. Within NCH&C, we believe that everyone within the organisation has a role to play in supporting this ethos – this is not just about clinical staff and how they care for patients. Administrative and support staff are also able to contribute in a number of ways – simple things like answering a phone for a colleague can make a real difference. The three domains of high quality care have been defined as being: • P atient Safety: The first dimension of quality must be that we do no harm to patients. This means ensuring that the environment is safe and clean, and reducing avoidable harm, such as excessive drug errors • P atient Experience: Quality of care includes the quality of caring. This means how personal care is delivered, the compassion, dignity and respect with which patients are treated. It can only be improved by analysing and understanding patient satisfaction levels and experience • Effectiveness of Care: This means understanding the success rates of different treatments for different conditions. Assessing this will include clinical measures, such as mortality or survival rates, complication rates and measures of clinical improvement. Just as important is the effectiveness of care from the patient’s own perspective. Examples include, improvement in pain scores or returning to work after treatment. Clinical effectiveness may also extend to people’s wellbeing and ability to live independent lives In order to support high quality care, each year we focus on key Quality Goals. These goals are intended to inform the practice of each member of staff across all three domains of quality. After consultation with staff, we have developed the following goals for 2013/14. At this stage, the goals are of a strategic nature, but it is expected that local teams will identify what each goal means for them and their practice. Our Quality Goals will help us deliver excellent and harm free care and are also designed to reflect the learning from the Francis Report and include the Chief Nursing Officer’s 6 C’s (care, compassion, competence, communication, courage and commitment). These six fundamental values are underpinned by the following key actions to support healthcare professionals deliver excellent care and include: 1.Helping people to stay independent, maximising wellbeing and improving health outcomes 2.Working with people to provide a positive experience of care 3.Delivering high quality care and measuring the impact of care 4.Building and strengthening leadership 5.Ensuring we have the right staff, with the right skills, in the right place 6.Supporting positive staff experience The quality goals also include meeting our commissioner’s quality indicators as set out in the CQuIN schedule and together will build on improvements made during 2012/13. 12 Quality Account 2012/13 1. To continue to embed a culture of compassionate care (the 6 Cs) and act on learning from the Francis Report We will continue to demonstrate this by: a. Treating all our patients with care and compassion Experience b. Ensuring that every patient is treated with respect, privacy and dignity Experience c. Ensuring the safety of patients / service users in our care Experience / Safety d. Raise the organisational visibility of all our vulnerable adults and children to improve their safety Safety e. Being open and transparent Safety / Experience f. Implementing regular mortality reviews Safety / Effectiveness 2. Developing and promoting our approach to clinical effectiveness This year we want to engage with clinicians across NCH&C so that every service has an agreed and shared set of clinical effectiveness measures they can use to demonstrate improved patient care and drive improvement. We will achieve this by attaining goals that our patients want by reducing length of stay and preventing admission to hospital Effectiveness We will also be reviewing the programme of clinical audit 3. Meeting our Commissioning for Quality and Innovation (CQuIN) goals a. Friends and Family Test – To improve the experience of patients in line with Domain 4 of the NHS Outcomes Framework. The Friends and Family Test will provide timely, granular feedback from patients about their experience. To roll-out to community services Experience b. NHS Safety Thermometer – Data collection of the 4 harms: pressure ulcers, falls, catheter acquired urinary tract infections and venous thromboembolism assessments Safety c. Dementia – To incentivise the identification of patients with dementia and other causes of cognitive impairment alongside their other medical conditions, to prompt appropriate referral and follow up after they leave hospital and to ensure that hospitals deliver high quality care to people with dementia and support their carers. Continuation of the care pathway and clinical leadership Safety / Experience d. Venous Thromboembolism (VTE) – To reduce avoidable death, disability and chronic ill health from VTE through assessments of patients at risk Safety / Effectiveness e. System-wide assurance process – Regarding admission avoidance NHS England Local Area Team f. Breastfeeding initiative – NCH&C’s contribution across Norfolk to help increase the numbers of women initiating breastfeeding in line with the Department of Health target of 2% increase per annum NHS England Local Area Team g. Lymphoedema – Roll out of specialist service to include pre-assessment dopplers in the west locality. This will improve patient experience bringing care closer to home to reduce unnecessary admissions Partnership working h. Neurology – Expansion of existing service to provide specialist nurse for patients with Multiple Sclerosis. This service will support patients experiencing problems with relapse, ongoing symptoms and worsening of their condition who would otherwise be admitted to hospital Safety / Experience i. Continuing Healthcare – Exploration of expansion of the Community Nursing Team in the south to cover the social care element for new continuing healthcare patients. This would provide seamless and uninterrupted care for those patients Safety / Experience Norfolk Community Health and Care NHS Trust 13 2.3 Health & Social Care Integration “People shouldn’t have to worry about how their health and social care is delivered; they just need to know where to get the help that they need, when they need it. Making sure that’s as easy as possible is our job...” Why do we need joined up services? Delivering what patients want We know that people are living longer than ever before, that there has been a rise in the number of people with life-long conditions, such as diabetes, and that people often have a number of different conditions or health issues. Our patients tell us that joined up health and social care is important to them, saying: This means that you may need to receive care from a range of different experts, including nurses, therapists, social workers, GPs, or other professional staff. • They want one person to act as their key worker and know their story So by joining up different services, wherever possible, we can ensure that the patient only has to tell their story once to get the right support from different health and social care experts. • They want clear easy to use information, such as a single telephone number How does joined up care work? Staff from NCH&C and NCC are working side-by-side so we can be more informed about exactly what our patients need. This means we can make sure that they receive precisely the right care and enjoy a better experience when accessing our health and social care services. • They want better co-ordination of services • Use their General Practice as the natural focus for local care • They do not want to have repeat assessments • Be treated with courtesy and respect Our joined up approach will increasingly make this a reality. 14 Building on recent success NCH&C and NCC already have a very good record of joined up working. Along with GPs and a number of other local organisations, we took part in a national pilot which was run by the Department of Health. This saw us all working together to create innovative ways of improving the care provided to local people. These were so successful that many of the initiatives are still in place today. Offering patients more choice Health and social care staff work closely together to help prevent the need for separate visits and assessments. This also enables the care professionals to work in partnership with their patients to ensure that services continue to meet individual people’s needs and are delivered in their preferred place of care, which may be at home. Plans for 2013/14 Currently NCH&C and Norfolk County Council are seeking to agree the next stage of adult health and social care provision. They are exploring what the next stage may look like and are going to be considering a range of options. The options appraisal will look at the benefits and risks of moving further on integration or continuing with our current joint management arrangements across the county. Quality Account 2012/13 Norfolk Community Health and Care NHS Trust 15 2.4 Transformation Programme for 2013/14 During 2012 clinical and managerial teams worked together to develop a three year programme of transformational change. In 2013/14 we will deliver our transformation programme in support of further improving quality. Transformation with strong quality achievement will make NCH&C well placed to continue to deliver against commissioner expectations and respond to new business opportunities. Our membership of the Aspiring Community Foundation Trust Network facilitates a deeper understanding of variation across our community services portfolio and learning from best practice to make further quality improvements. Like all NHS organisations we have a number of challenges, such as reducing costs, safeguarding the quality of patient care and working to continually improve the quality of our services. Whilst we have had cost improvement programmes in previous years, we recognise that delivery year on year becomes more challenging and the nature of the change moves from incremental to more transformational, which will come together to achieve our service development objectives for the year. Our Transformation Programme, which has been internally developed, but is being externally validated, covers improvements, such as workforce productivity through new roles and mobile working, supply chain management and planned Estate Rationalisation, which form the basis of our Cost Improvement Programme. But they are also the basis for improving quality through releasing clinicians to have more face-to-face time to care. They draw on clinical engagement in their design and implementation with a view to increasing overall staff engagement. • Mobile working The Programme is sponsored by the Executive Team, with Senior Managers from the operational services as the programme owners. Cost Improvement Plans for 2013/14 are subject to a current validation process externally validated by PricewaterhouseCoopers and culminated in formal Board sign off in March 2013. These plans will have been reviewed and approved by the Trust’s medical and nursing directors as part of the quality impact assessment process. Our transformational programme comes under the following themes: • Streamlined systems • Workforce planning • Supply chain management • Travel / Estates 16 Quality Account 2012/13 2.5 Statements of Assurance from the Board 2.5.1 Review of services During the period April 2012 to March 2013 Norfolk Community Health & Care NHS Trust (NCH&C) provided and/or sub-contracted 31 NHS services. Since September 2011 staff across community teams and the inpatient units assess their areas against a checklist with weighted scores, which resulted in an overall RAG-rated score and an indication of what action is required. NCH&C has reviewed all the data available to them on the quality of the care in all 31 of these NHS services. Green rating – (score 0-10) No action required, re-assess area next month The income generated by the NHS services reviewed in 2012/2013 represents 100% per cent of the total income generated from the provision of NHS services by NCH&C for 2012/2013. Amber rating – (score 11-15) Undertake full risk assessment and agree action plan for red items within one month. Add to local risk register All clinical services are subject to monthly risk assessment through the use of an Early Warning Trigger Tool (EWTT). The implementation of the tool was intended reduce the number of Serious Incidents Requiring Investigation (SIRIs), reduce the risk of an unfavourable CQC report and prevent services going into crisis. The original tool was produced by the National Patient Safety Agency (NPSA) in response to the quality of care at Mid Staffordshire NHS Foundation Trust and has been adapted locally to better reflect community services. Red rating – (score 16 or more) Inform line manager immediately and undertake full risk assessment within one week. Produce action plan for red items within one week. Escalate to Executive Director Team The data from the tool is reviewed monthly to identify services with potential issues, as well as identifying key themes common to a number of teams or departments. Several teams which have flagged as ‘Red’ have been subject to visits and action plans, which have helped to address specific operational issues and reduce the level of risk accordingly. The Trust Board receives a monthly Integrated Performance Report (IPR), which focuses on a number of domains, including patient experience, safety, quality and risk. The data is presented in a dashboard format, using Red-Amber-Green (RAG) ratings to highlight any areas of adverse performance against agreed targets, standards and thresholds and is supported by a narrative explaining the reason for the variance, and actions being taken to mitigate future risks impacting on performance. Norfolk Community Health and Care NHS Trust The Board also receives a monthly Quality and Risk report which provides more operational detail on those areas reported in the IPR. This report is also presented to the Quality and Risk Assurance Committee, and includes the following areas: • Serious Incidents Requiring Investigation (SIRIs) • Medication incidents • Falls causing harm • Pressure Ulcers • Infection rates • Clinical audit and effectiveness • Patient Experience surveys (including the Friends & Family Test and Patient Opinion) • Complaints and compliments • Results of external scrutiny (eg, Care Quality Commission, NHS Litigation Authority, National Patient Safety Agency) Information is given over time, where available, to enable comparisons in reporting levels, improved analysis and identification of themes, trends and learning to improve the safety and quality of care delivery. 17 Quality Account 2012/13 18 2.5.2 Participation in clinical audit During April 2012 – March 2013, three national clinical audits and one confidential enquiry covered NHS services that NCH&C provides. During that period NCH&C participated in 33% of national clinical audits and 0% of national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that NCH&C was eligible to participate in during April 2012 – March 2013 are as follows: Name of National Audit Lead Organisation Included participation from NCH&C? Diabetes (Adult) ND(A), includes National Diabetes Inpatient Audit (NADIA) Health and Social Care Information Centre Yes, joint collection of data with GP surgeries Sentinel Stroke Royal College of Physicians, London No – due to capacity The stroke unit is registering NCH&C for 2013/14 Child Health Programme (CHR-UK) Royal College of Paediatrics and Child Health This audit was registered and led by the Norfolk and Norwich University Hospitals NHS Foundation Trust (NNUH) Title of National Confidential Enquiry Applicable to NCH&C? Included participation from NCH&C? National Review of Asthma Deaths (NRAD) Yes No. There were no asthma deaths recorded from within NCH&C care during 2012/13 National Audit Programme (SSNAP) – (combining the Sentinel stroke audit (2010/11, 2012/13), and the Stroke improvement national audit project (2011/12, 2012/13) Norfolk Community Health and Care NHS Trust The national clinical audits and national confidential enquiries that NCH&C participated in, and for which data collection was completed during April 2012 – March 2013, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Name Lead Organisation Percentage Diabetes (Adult) ND(A), includes National Diabetes Inpatient Audit (NADIA) Health and Social Care Information Centre Information is not currently available 19 The report of two national clinical audits National (Adult) Diabetes Audit, and the National Falls and Bone Health in Older People were reviewed by the provider in April 2011 – March 2012 and NCH&C intends to take the following actions to improve the quality of healthcare provided: (Diabetes) Description of actions: Our Diabetes Practice Educator holds quarterly meetings with our Link Nurses and Community Matrons across the Trust and within these sessions learning from this national report (primary care based) is shared. Where training needs are identified, this is provided to our community staff in order to continue to provide the best possible care for our diabetic patients with the long term goal of them achieving improved HbA1C results (long term blood glucose stability). (Falls) Description of actions: A gap analysis of patient need versus staff capacity was undertaken following publication of the 2011/12 National Falls audit report, and this was included in a business case to our commissioners, to support the development of a robust and sustainable ‘Falls pathway’ between primary, community, acute, and social care services. Part of the funding bid was outlining the need to make the community integrated team’s ‘Falls champion’s’ substantive roles within our Trust. Following this bid for funding, ongoing work was designed to further develop and establish the ‘Falls pathway’. 20 Local clinical audits The reports of 74 local clinical audits were reviewed by the provider during the period from April 2012 to March 2013 and NCH&C intends to take the following actions to improve the quality of healthcare provided. The following is a description of a selection of actions and assurances provided. These assurances are in line with the Clinical Audit Policy; (‘high assurance’ over 85% compliance, ‘moderate’ between 60% - 84% compliance, and ‘low’ as below 59% compliance against clinical audit standards). See section 3.10.6 for more information. a. Record Keeping/Management, Trust-wide, annual, mandatory clinical audit (High assurance achieved) Good record keeping is an integral part of clinical practice, and is essential to the provision of safe and effective care. This audit has been designed to measure compliance with best practice standards and to identify areas where practice should be shared or improved. Following overall achievement of ‘high Trust-wide assurance’ in this audit, next year re-audits will focus locally on any areas of moderate or low compliance. Quality Account 2012/13 b. Resuscitation (policy monitoring) clinical audit (High assurance achieved) This audit was conducted because NCH&C recognises and accepts its responsibility to patients, employees, families, carers and the general public to ensure that the requirements for resuscitation (HSC 2000/28) are satisfied and that best practice is maintained. Actions include: 1.A nominated training lead to monitor compliance with resuscitation training at Ogden Court 2.Learning, Education And Development (LEAD) to provide a resuscitation training session on-site to capture majority of staff members, to maintain up-to-date training for staff c. Auditing attendance at Priscilla Bacon Lodge (PBL) inpatient, community and day unit – multi-disciplinary team (MDT) meetings (Moderate assurance achieved) The aim of this audit was to ensure that in line with the ‘Manual for Cancer Services: Specialist Palliative Care Measures version 1.0 May 2012’, weekly meeting were held recording core member attendance. This manual states that core members should attend at least 66% of MDT meetings. 1.Move to adopting an electronic MDT attendance record to avoid data collection errors 2.Identify a dedicated MDT Co-ordinator and cover 3.Move to a combined weekly MDT meeting to enable core members to attend more easily 4.Repeat audit 1 year (June 2013) Norfolk Community Health and Care NHS Trust d. Administration of Buccal Midazalam and rectal diazepam (Low assurance achieved) The aim of this audit was to monitor our Trust’s epilepsy service compliance with this element of the NICE epilepsy pathway. A confidence level and margin of error for this report’s results were unable to be determined due to it not being possible to estimate the total patient population, but with the development of the Epilepsy Care Plan template on SystmOne, this should be available for future use. An action from this audit is to continue to monitor whether care plans have been signed by the relevant Doctor or manager. e. Audit of medical summaries produced for the adoption unit (Moderate assurance achieved) The aims of this audit were to: 1.Ensure guidelines for producing child permanence reports are being followed 2.To assess the quality of information provided 3.To assess the appropriateness of investigations for children whose parents were known substance mis-users The main recommendations were to include any negatives in the reports and to follow a guideline to encourage medical staff to include as much information as possible. 1.The letter template was changed to ensure recording of which forms had been received or not 2.This needs re-auditing within the next year to see if we have improved 3.The audit tool needs revising for next year to look at a narrower scope of standards in greater detail 21 2.5.3 Participation in clinical research The number of patients receiving NHS services provided or sub-contracted by NCH&C in 2012/13 that were recruited during that period to participate in research approved by a research ethics committee, was 773 (compared with 690 in 2011/12). Participation in clinical research demonstrates NCH&C’s commitment to improving the quality of care we offer and to making our contribution to wider health improvement. Our clinical staff stay abreast of the latest possible treatment possibilities and active participation in research leads to successful patient outcomes. We were involved in 59 research studies during 2012/13, an increase of 20% on 2011/12 figures, this includes 19 studies that were new in 2012/13 and 40 studies ongoing from previous years. The National Institute for Health Research (NIHR) supported 70% of these studies through its research networks, an increase of 5% on 2011/12. The median approval time for achieving NHS permission for studies new to NCH&C in 2012/13 was 26 days, well within the national target of 30 days, and showing a significant improvement over the median of 36 days achieved in 2011/12. Throughout 2012/13 we have taken steps to embed research as core Trust activity and encourage staff to engage with the local clinical research networks. In line with this we are developing a Trust research strategy aligned with the NIHR high level objectives; successfully applied for a second year of funding to continue our Research Site Initiation (RSI) Scheme in 2012/13; and embedded research in our key clinical forums. The RSI funding has helped teams to develop their research capability and capacity to host NIHR supported research across a number of different clinical areas including stroke, paediatrics, specialist palliative care and adult learning disabilities and almost half of all new studies hosted by NCH&C were in these areas. 22 Quality Account 2012/13 A new clinical forum recently set-up for musculoskeletal staff successfully engaged with the local Primary Care Research Network to identify and maximise on research opportunities in the area of musculo-skeletal therapies, resulting in the set up of a new NIHR funded study in this area, which is just starting to recruit. 2.5.4 Goals agreed with commissioners We have continued to work with partner organisations to help develop research ideas and questions of interest to community care. Three NCH&C staff are currently in receipt of research bursaries, and we continue to support these staff to develop their research ideas into fully funded research proposals. A proportion of NCH&C’s income during April 2012 and March 2013 was conditional on achieving quality improvement and innovation goals agreed between NCH&C and any person or body they entered into a contract, agreement or arrangement with for the provision of NHS services, through the CQuIN payment framework. Details of NCH&C’s achievements against the agreed CQuIN indicators for April 2012 to March 2013 are set out in Part 3 of this Quality Account. A further seven NCH&C staff were also involved as co-applicants on five separate research grants that were submitted to the NIHR for funding in 12/13, and NCH&C are collaborators on two ‘Research for Patient Benefit’ grants held by partner organisations in the areas of stroke rehabilitation and social anxiety and stuttering. Use of the Commissioning for Quality and Innovation (CQuIN) payment framework. The CQuIN indicators agreed with our commissioners for the forthcoming year, (April 2013 to March 2014) can be found in Part 2 under ‘Quality Goals’. Norfolk Community Health and Care NHS Trust 23 2.5.5 Statement from the Care Quality Commission (CQC) Norfolk Community Health & Care NHS Trust is required to register with the CQC and its current registration certificate issued on October 12, 2012, confirms that the Trust is registered to provide the following Regulated Activities: 1.Assessment or medical treatment for persons detained under the Mental Health Act 1983 2.Diagnostic and screening procedures 3.Family planning 4.Surgical procedures 5.Treatment of disease, disorder or injury The only conditions of registration are that these regulated activities may only be provided from the following registered locations: Registered Locations Regulated Activity No. (see above) Cranmer House 1, 2, 5 Little Acorns 5 Adult Learning Disabilities, Mill Close 5 Provider Services HQ 1, 2, 3, 5 Squirrels 5 Benjamin Court 1, 2, 5 Colman Hospital 1, 2, 5 This community hospital was found to have met the following essential standards of quality and safety as listed below: Dereham Hospital 1, 2, 5 Outcome 2 Kelling Hospital 1, 2, 5 North Walsham Hospital 1, 2, 5 Outcome 4Care and welfare of people who use services Norwich Community Hospital 1, 2, 4, 5 Outcome 7Safeguarding people who use services from abuse Ogden Court 1, 2, 5 Outcome 14 Supporting staff Swaffham Community Hospital 1, 2, 5 Outcome 16Assessing and monitoring the quality of service provision The Care Quality Commission has not taken enforcement action against NCH&C during the period April 2012 and March 2013. NCH&C has participated in five routine inspections undertaken by the Care Quality Commission relating to the following areas during April 2012 and March 2013: One routine inspection was carried out at Benjamin Court, Community Hospital, Cromer, Norfolk (RY330) in November 2012. Consent to care and treatment 24 Quality Account 2012/13 Routine inspections were undertaken at four of our Joint Community Learning Disability Teams (which are all registered by Norfolk County Council) during the period April 2012 and March 2013 as follows: 1. Eastern Learning Disability Team, Ferry House, Great Yarmouth (November 2012) This LD team were found to have met the following essential standards of quality and safety as listed below and the formal report was sent to Norfolk County Council: Outcome 1Respecting and involving people who use services 3. West Norfolk Learning Disability Service, King’s Lynn (March 2013) This LD team were found to have met the following essential standards of quality and safety as listed below and the formal report was sent to Norfolk County Council: Outcome 2 Consent to care and treatment Outcome 4Care and welfare of people who use services Outcome 6 Cooperating with other providers Outcome 10 Safety and suitability of premises Outcome 4Care and welfare of people who use services Outcome 14 Supporting staff Outcome 7Safeguarding people who use services from abuse 4. Northern Learning Disability Service, Blickling (March 2013) Outcome 14 Supporting staff Outcome 16Assessing and monitoring the quality of service provision This LD team were found to have met the following essential standards of quality and safety as listed below and the formal report was sent to Norfolk County Council: 2. South Norfolk Learning Disability Service, Attleborough (January 2013) Outcome 1 Respecting and involving people who use services This LD team were found to have met the following essential standards of quality and safety as listed below and the formal report was sent to Norfolk County Council: Outcome 4 Care and welfare of people who use services Outcome10 Safety and suitability of premises Outcome 2 Outcome 12 Requirements relating to workers Consent to care and treatment Outcome 4Care and welfare of people who use services Outcome 7Safeguarding people who use services from abuse Outcome 14 Supporting staff Outcome 16Assessing and monitoring the quality of service provision Outcome 17Complaints Outcome 16 Assessing and monitoring the quality of service provision Norfolk Community Health and Care NHS Trust 2.5.6 Data quality High quality information underpins the effective and safe delivery of patient care and is key if improvements in quality of care are to be made. Improving data quality, which includes the quality of demographic, ethnicity and other equality data, should improve patient care and improve value for money. NCH&C will be taking the following actions to improve data quality: • A range of data quality reports have been designed to monitor a range of key performance indicators on a weekly and monthly basis • The Secondary Uses Service (SUS) dashboards are reviewed regularly in relation to a number of national key indicators 25 The Trust has a Data Quality Strategy which will be critical to a number of the Trust’s priorities and objectives, including improving the quality of patient care, compliance with the Information Governance Toolkit version 10 for 2013/14 and the need to introduce and monitor the Community Information Data Set (CIDS). This strategy is underpinned by a Data Quality Policy which is subject to annual review. The purpose of this policy is to ensure the highest standards of data quality throughout NCH&C are achieved and maintained. This policy is for all staff collecting and using data and they must adhere to the local and national standards as laid out in this policy. The Trust is also reviewing its formal structures for monitoring data quality ensuring its Data Quality Forum has the necessary membership and coverage to continue to drive improvements in data quality. • A selection of these indicators are also reported to monthly business unit performance meetings where operational services are held to account for the quality of data held on the Patient Administration System (PAS) and SystmOne NHS Number and General Medical Practice Code Validity • These reports are held on a networked drive and can also be viewed on an Intranet portal to ensure they are accessible to key staff involved in the monitoring and reporting of performance and activity data NCH&C submitted records during 2012/13 to the SUS for inclusion in the Hospital Episode Statistics (HES) which are included in the latest published data under the organisation code RY3. The percentage of records in the published data which: 1.Included the patient’s valid NHS Number was: 100% for admitted patient care (APC) 100% for out patient care 2.Included the patient’s valid General Medical Practice Code was: 100% for (APC) 100% for out-patient care Quality Account 2012/13 26 2.5.7 Information Governance Toolkit attainment levels NCH&C Information Governance Assessment Report overall score for 2012/2013 was 66% at Level 2 and was graded green: Assessment Level 2 Exempt Total Req’ts Overall Score Grade Version 10 (2012-13) 38 1 39 66% Satisfactory The Information Governance toolkit is available on the Connecting for Health website: www.igt.connectingforhealth.nhs.uk The Information Quality and Records Management attainment levels assessed within the Information Governance Toolkit provide an overall measure of the quality of data systems, standards and processes within an organisation. 2.5.8 Clinical coding error rate NCH&C was not subject to the Payment by Results (PbR) clinical coding audit during 2012/2013 by the Audit Commission. Norfolk Community Health and Care NHS Trust 27 2.5.9 National Quality Indicators All trusts requirement: The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the number and, where available, rate of patient safety incidents reported within the trust during the reporting period, and the numbers and percentage of such patient safety incidents that resulted avoidable harm in severe harm or death. All trusts requirement: The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of patients aged (i) 0 to 14 and (ii) 15 or over, readmitted to a hospital which forms part of the trust within 28 days of being discharged from a hospital which forms part of the trust during the reporting period. The Trust considers that this data is as described for the following reasons: It represents the rate of incidents reported against the number of face-to-face contacts with patients, expressed as a rate per 1,000. NCH&C does not re-admit patients aged 15 or over following discharge. All admissions to the Trust’s beds are received from acute trusts or from the patient’s usual place of residence. The Trust has taken the following actions to improve this number and rate, and so the quality of its services, by actively reporting all incidents through its DATIX incident reporting database, whether they result in harm or otherwise, ensuring that appropriate staff are suitably trained to report and record all incidents, and identifying trends, patterns and risk factors, in order to use this information to improve the quality and safety of our services. Number of incidents (total NCH&C) Apr 2012 May 2012 Jun 2012 Jul 2012 Aug 2012 Sep 2012 Oct 2012 Nov 2012 Dec 2012 Jan 2013 Feb 2013 Mar 2013 No harm 243 314 253 297 333 324 285 266 315 322 319 379 Low harm 289 359 303 432 390 348 402 387 337 434 364 396 Moderate harm 58 67 41 81 85 54 72 77 80 92 82 86 Severe harm 9 4 10 10 6 4 10 1 4 6 3 7 Death 3 0 1 2 3 3 4 6 1 3 4 0 Total 602 744 608 822 817 733 773 737 737 857 772 868 6.86 6.23 7.08 8.87 8.82 8.83 6.58 Total incidents in clinical areas per 1,000 contacts 5.96 7.29 5.90 8.46 7.21 28 All trusts requirement: The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of staff employed by, or under contract to, the trust during the reporting period who would recommend the trust as a provider of care to their family or friends. KF24. Staff recommendation of the trust as a place to work or receive treatment On a scale of 0 – 5 (the higher the score the better) 2011 Results: 3.22 2012 Results: 3.39 Showing that staff experience has improved within NCH&C (although worse than average when compared with other community trusts - 0.2%). NCH&C are encouraged that this score has improved this year and is much closer to the average score for community trusts. The Trust now has a process in place to survey all staff twice a year by location on a rolling basis so that a survey happens to one of our business units each month to compliment the national staff survey. The focus is on generating locally responsive actions. The KF24 question is also asked within this process, and where local issues are highlighted, they are addressed. Following this year’s national survey we ran a series of sessions with staff to obtain more information regarding this issue and are currently reviewing the results. This information will continue to inform our staff engagement plan. Quality Account 2012/13 Norfolk Community Health and Care NHS Trust 29 3.1 Review of Quality Performance in 2012/13 Chief Executive hails staff for “Trust’s best ever year” Michael Scott thanked NCH&C’s staff for helping the Trust to make significant progress over the last financial year... 2012/13 has been a year of really focusing on patient quality. We have measurably improved the quality of our services in 2012/13, delivering better health outcomes, high standards of safety, leading to excellent patient experience. A key objective for our Trust was to reduce levels of patient harm and we are delighted to report that we have seen a drastic reduction in the level of pressure ulcers seen locally. Whilst we did not completely eliminate avoidable pressure ulcers, we have only had one in our inpatient units in the last four months. Similarly, we have had very low levels of falls and health care acquired infections, which all contribute to our goal of delivering harm-free care. Central to this success, as well as so many of our others, is the hard work and dedication of our excellent staff. Many of our colleagues have been recognised for their exemplary work over the last year, such as those given the title of “Queen’s Nurse’ and ‘NHS Hero’. Enabling our Trust to take ‘temperature checks’ from our staff about what is working well and what needs to be addressed has also been improved thanks to our new Short Staff Surveys. Recent feedback from colleagues shows that things are improving, with seven of the questions consistently scoring at least 5% higher than in the 2011 NHS Staff survey. We know that things are still not perfect, but we are confident that progress is being made and that we can continue to improve together. Receiving prompt feedback from our staff is key to our ongoing success, so we will keep this dialogue going to see how we can further improve in the coming year. As a community-based Trust, Community Nursing and Therapy (CN&T) is one of our flagship services and a key local NHS provision. It is also highly rated by our patients, with nine out of ten CN&T patients saying they are satisfied with the care they receive. It is therefore important that GPs see the value of this service too. Accessibility of our services has also greatly improved this year. For example our Podiatric Surgery Service has become compliant with our 18 weeks referral to treatment targets thanks to much hard work from the service’s staff. Similarly, our MSK Physiotherapy Service and our Wheelchairs Service have also greatly improved their accessibility. Today, almost every single patient, across each of our services, is seen within the 18 week target. 30 Quality Account 2012/13 3.2 Our Workforce Our overarching view is that an engaged, empowered and compassionate workforce will have a direct impact on the quality of care received by our patients. The Francis Report highlights the importance of listening to the workforce and addressing concerns and issues raised in a timely and effective manner. They are the eyes and ears of the organisation and passionate about patient care, driven by a desire to continuously improve the quality of care provided. With this in mind, increasing staff engagement, summed up as an annual priority for 2012/13 as ‘To truly inspire our staff’ has been a major focus for the year. Our engagement score increased from 3.5 in 2011 to 3.61 in 2012 which is close to the national average of 3.69 for community trusts and the 4th highest improvement compared to 21 community trusts. The Directors have provided a series of roadshows giving up to date information on strategic direction and performance. In 2011, 60% of staff said they knew who the senior managers in the Trust were. In 2012, that figure had risen to 80%. The Trust remodelled some of its services during the year to ensure that they remain efficient and cost effective. In this year we have redesigned our IM&T service, reviewed administrative and clerical roles and restructured corporate management functions. Our voluntary turnover rate for the 12 months to February 2013 is 9.2% which sits within our target of 12% (plus or minus 5%), and is under our annual plan target of 10%. This indicates a good retention of experienced staff and is within the tolerances for a healthy turnover of workforce. The Trust sees effective leadership as an important enabler in delivering this annual plan. The Trust has a number of internal leadership and management programmes that are formally evaluated and highly valued by staff. 89% of participant managers, surveyed three months after completing our REAL programme say it had a significantly positive impact on the participants behaviour. The Trust also draws on training provided by the Norfolk and Suffolk Leadership Academy as well as SHA provided leadership programmes for the national Top Leaders. Development programmes are also in place for the Executive Directors as well as the whole Board, incorporating externally facilitated 360 degree feedback. Absence management within NCH&C has continued to be a challenge against the back drop of increasing demand and capacity. We have increased the uptake of flu vaccinations in 2012/13 but will want to see further uptake in 2013/14. 25% of staff receiving flu vaccinations: an increase from 20% in 2011/12, whilst falling short of the internally agreed target of 50%. We set our sickness target at April 2012 to be 4.5%, decreasing to 4.0% by March 2013. Our actual rolling 12 month sickness rate for the Trust stands at 5.02% at February 2013. We have focussed on complex sickness cases in an effort to meet our target: long term sicknesses (eg, musculo-skeletal conditions, stress, anxiety) account for approximately 60% of our current sickness. Norfolk Community Health and Care NHS Trust 31 3.2.1 National Staff Survey 2012 The National Staff Survey 2012 shows NCH&C as one of the most improving community trusts, albeit with further work to do in 2013. Engagement and satisfaction scores are up as is recommendation of the Trust as a place to work or receive treatment. The 2012 full staff survey was carried out from October to December 2012 and sent to a sample of 778 staff. Our 59% response rate was a 6% improvement on 2011 and compares favourably with the top national response rate of 60%. We improved by a statistically significant amount in five of the 21 Key Findings that could be compared with the 2011 survey. They included the recommendation for the Trust as a place to work or receive treatment from 3.22 out of 5 to 3.39 although this is still below the average of 3.58; effective team working 3.71 to 3.85; number of staff having had appraisals 87 to 92%; contribution to improvements at work from 62% to 72% and the staff experiencing discrimination at work decreased from 11% to 5%. We deteriorated in three key findings. Of the three Key Findings since 2011 we are better than average in one and average in two compared with other community trusts. Two of the areas in which our scores deteriorated related to training in the last 12 months. Health and safety and equality training are specifically mentioned in the national survey, but are only refreshed in the Trust every three years. As a result we would expect fluctuations in this result The overall engagement score for NCH&C improved from 3.5 in 2011 to 3.61 in 2012. The most recent short staff survey in the south shows an engagement score of 3.65. Staff satisfaction improved from 3.38 in 2011 to 3.55 in 2012. The most recent short staff survey in the south shows satisfaction of 3.60 showing a continuing rise in engagement and satisfaction across NCH&C. Only three of 21 community trusts improved their engagement score compared to 2011 by more than we did and only three had a higher number of improved significant key findings compared to 2011. Including improvements in staff satisfaction and the increase in the proportion of staff who would recommend the Trust as a place to work or receive treatment, we are on these measures, arguably in the top five most improving community trusts. We set ourselves an annual objective to half the number of below average scores. We did not meet this goal. Last year we had 23 below average scores. This year we had 15, a reduction by 8/23. Of those below average measures, four were within 1% of the average of the 21 community trust scores. During the year we introduced a short staff survey. This includes themes from the annual national staff survey and builds on research from the Gallop organisation. Following each survey, the relevant business area is then tasked with creating an action plan to address issues raised. 32 Quality Account 2012/13 3.2.2 Mandatory training 3.2.3 Appraisals We remain committed to mandatory training in order to ensure that new and existing staff are equipped for delivering patient centred care. We are aiming for 90% uptake. We are similarly committed to ensuring that all our staff have appraisal completion. We are taking a variety of approaches to achieving our target of 90%. The Trust has reviewed how it delivers mandatory training to staff to ensure that it is accessible and meaningful to them. We have developed a patient centric approach to training for inpatient areas, which is now bring remodelled to make it appropriate for community based staff as well. This involves setting up of training over a two day period covering a range of topics, delivered in the ward environment based around a figurative ‘patient in a bed’. We have also added it to induction to make sure that staff are fully skilled at the point that they join the organisation. In addition, we are creating a number of distance learning training courses to be used locally by staff and managers. Due to these improved delivery methods, mandatory training compliance has remained strong and currently stands at 80% against a target of 90%. This is an increase from 74% at the same point last year The Trust has improved the way that it collects information on appraisal rates and has seen significant improvement in compliance as demonstrated in the accompanying chart. The current appraisal completion rate is at 80% against a target of 90% although our survey results show a higher achievement. The last national staff survey reported a higher rate of 93%. At the equivalent point last year appraisal compliance stood at 61%. Norfolk Community Health and Care NHS Trust 3.2.4 Staff achievements and awards Queen’s Honours – Childrens expert Sian Larrington, one of our Children’s Centre Service Managers will receive an MBE from Her Majesty the Queen after being included in this year’s Birthday Honours list. The honours aim to recognise people who have dedicated their lives to improving those of others. The list of latest recipients was announced in June and Sian received acknowledgment for services to children. She said: “I am absolutely delighted and really proud to accept the honour.” 33 Becky receives ‘Queen’s Nurse’ Award A community neurology Specialist Nurse has been awarded the title of ‘Queen’s Nurse’ in recognition of her long-standing commitment to delivering excellent community-based care to local patients. Rebecca ‘Becky’ Hipkin works in our Community Neurology Team, based at St James’ Clinic, King’s Lynn. The title was awarded by the Queen’s Nursing Institute, a community nurses’ charity which aims to recognise nurses who have shown high standards of care and to encourage them to champion new ways of delivering innovative support to patients. Becky has cared for people in Norfolk since 1980, when she started her career as a ward nurse at the Queen Elizabeth Hospital, King’s Lynn. She has also worked in the evening nursing service team, as a palliative care nurse, and a community nurse. In her current role, which she has held since 2004, Becky provides care to patients in west Norfolk who have Parkinson’s Disease, multiple sclerosis, and motor neurone disease. She visits patients in their own homes, as well as seeing them within community-based clinics in King’s Lynn and Downham Market, where she helps them to manage their symptoms. 34 Quality Account 2012/13 3.2.5 A selection of compliments and ‘thank yous’ Compliments and thanks received from patients are also measured and this year the Trust has received in excess of 955 compliments and thank you’s. The dedication and commitment of our frontline staff is a recurring theme of the compliments received City 2 Integrated Team I would like to compliment the nurse for the excellent way she looked after my wife. She was very pleased to be treated in this way. She is a first class person and a credit to your department... Grimston District Nurses, King’s Lynn I do not take such sterling high standards for granted, I would like to hope, that this summary of a job well done goes some way to officially recognising their critical role in my recovery, and their contribution to the community at large... Priscilla Bacon Lodge, Norwich We could not have wished for better end of life care that you all gave so freely... Thank you for all the kindness you have shown and give me. I didn’t really want to leave... We really appreciated being allowed to stay and shall never forget the care and compassion shown to us all... Thank you all for the love and dedication given. We know he felt safe and well looked after. He never lost his smile with you... Beech Ward, Norwich Community Hospital Excellent service... Well looked after... King’s Lynn South Integrated Team We cannot thank you for all that you have done for mum/wife. You have all went beyond the call of duty. We were very happy that she was in safe hands... Swaffham District Nursing Thank you for all the care that you gave my father. He had the very best of everything from you all... Four individuals and teams from our Trust have been recognised by members of the public, patients, and fellow NHS Colleagues. They have each shown exceptional compassion, kindness, and skill above and beyond the call of everyday duty. The NHS Winter Heroes scheme was a chance for people to nominate the NHS staff who ‘ploughed through’ this winter, despite adverse weather and winter pressures. The scheme celebrates the role that all staff - whether they be doctors, nurses, therapists, support staff, managers, receptionists, or porters - play in improving the lives of patients. The winter campaign follows the NHS Heroes campaign, which was held last summer and saw a number of colleagues from our Trust nominated. Our NHS Winter Heroes were invited to receive a certificate and congratulations at a Board meeting and are: • Integrated Nursing Team, City One, Norwich • Integrated Nursing Team, St James’, King’s Lynn • Kevin Rix, Gardener, Colman Hospital, Norwich Norfolk Community Health and Care NHS Trust 35 3.3 Performance Highlights over 2012/13 Areas of achievement During 2012/13 the Trust had a number of important targets to achieve or maintain. One of the key performance targets to be achieved was the 18 week wait Referral to Treatment (RTT) target, where 95% of admitted and non-admitted patients had to receive a definitive treatment or intervention within 18 weeks of referral. Throughout the year, NCH&C made significant improvements with most services either exceeding the target on a consistent basis, or achieving 100%. However, in year, four services experienced short periods of below expected performance, and in each case, robust action plans and calculated trajectories were established in order to correct performance and return service performance above target. These services were: • Consultant-led community paediatric services • Musculoskeletal physiotherapy • Adult Speech and Language Therapy • Wheelchair services In 2012/13, there were three reported cases of Clostridium Difficile against an annual ceiling of nine cases. All reported cases have been subject to Root Cause Analysis (RCA) to review lessons learned. Despite high levels of Norovirus within the general community, NCH&C only suffered one cluster of Norovirus. This was quickly and efficiently contained with only four patients affected. The ward did not need to close and their patients were managed within side rooms and a bay. Ultimately it is staff vigilance that has kept NCH&C levels of Norovirus so low over the season. The Trust agreed an annual ceiling of no more than 4.0 injurious falls per 1,000 Occupied Bed Days (OBDs). Despite in-month variation across the Trust’s inpatient units, the number of falls per 1,000 OBDs was 3.41, a clear improvement on the previous year’s rate of 4.03. All community service providers are required to report the level of Venous-Thromboembolism (VTE) assessments for patients admitted to its community hospitals who are at risk of developing a VTE. The Trust established a locally agreed trajectory for 2012/13, against which it would be monitored, and to then achieve the national target of 95% compliance by December 2012. By August 2012, the 95% target had been achieved and since maintained across the Trust. 36 Quality Account 2012/13 Meeting targets Indicator Target or upper ceiling Annual performance Trend MRSA Screening – elective patients 100% of patients having planned surgery screened for MRSA 100% Stable Clostridium difficile Nine cases or less during 2012/13 (cumulative) 3 Decreasing Injurious falls Number of falls resulting in harm per 1,000 Occupied Bed Days to be less than 4.0 3.41 Decreasing Venous Thromboembolism (VTE) assessments At least 95% of admissions have a VTE assessment 96.7% Stable 18 week wait referral to treatment 95% patients receiving definitive treatment within 18 weeks of referral 98.4% Increasing Health visiting Over 95% of mothers receiving a New Birth Visit within 28 days 97.9% Stable Norfolk Community Health and Care NHS Trust Areas of non-delivery In the early part of 2012/13, the Trust reported two cases of MRSA bacteraemias, against an annual ceiling of one case. Both were subject to robust RCAs to identify lessons learned, particularly as the Trust had no cases the previous year, (see section 3 for more information). Throughout the year, the number of patients whose discharge was delayed for non-medical reasons occupied an increasing number of the Trust’s community hospital beds. Over the period of the year, 5.4% of beds were occupied by patients whose discharge was delayed, compared to 4.1% the previous year. Whilst there are no contractual targets in place for this performance measure, analysis of the data has shown delays have been attributable to both health service related reasons (including patient and family choice), as well as social care delays. 37 The Smoking Cessation service agreed an annual target for 2012/13 of 2,000 quits with NHS Norfolk and Waveney. Despite a comprehensive restructure of the service the previous year and the engagement with the Smoking Cessation service in Great Yarmouth & Waveney to deliver the quit target, achieving the necessary level of referrals supported by a strong conversion rate, again, proved challenging. It became apparent during the autumn that the Trust was starting to negatively deviate from its trajectory and a number of actions were established to improve referrals rates. However, the number of subsequent referrals generated were not sufficient to recover the level of quits required, and as such the Trust failed this target, with a forecast outturn of 1,600 quits. Missing targets 2012/13 Indicator Target or upper ceiling Annual performance Trend MRSA Bacteraemia Annual ceiling of no more than one case 2 cases Stable Delayed transfers of care No more than 3.7% of beds occupied by patients whose discharge is delayed for non-medical reasons 5.4% Increasing Smoking cessation To achieve 2,000 successful quits during 2012/13 1,606 Decreasing 38 Quality Account 2012/13 3.4 Commissioning for Quality and Innovation (CQuIN) Scheme 2012/13 NCH&C has made excellent progress against is CQuIN Scheme in 2012/13 bringing our total CQuIN earnings for the last financial year to £1.597million. CQuIN are contractual commitments, some are nationally mandated and some are developed in partnership with our commissioners. They are intended to encourage progress to be made within key areas of local services. As a reward to meeting these commitments our Trust will now receive significant investment from our commissioners which is additional funding that can be used to make further improvements in the future. Norfolk Community Health and Care NHS Trust 39 CQUiN indicators and achievements for 2012/13 No Description of Indicator Quality domain % Achievement 1 To reduce avoidable death, disability and chronic ill health from Venous-thromboembolism (VTE) Safety 100% 2 To improve responsiveness to personal needs of patients/carers Patient experience 100% 3 Improve collection of data in relation to pressure ulcers, falls, urinary tract infection in those with a catheter, and VTE Patient safety 100% 4 Development of the care pathway for patients risk assessed as having dementia within the north locality inpatients units Patient safety Effectiveness Experience 100% 5 Patient satisfaction; “How likely is it that you would recommend this service to friends and family? Patient experience 100% 6 Partnership working As part of the health system-wide drive to reduce the rate of avoidable emergency admissions (EMAs) 1% of the total value of CQUIN for 2012/13 has been allocated to system-wide initiatives designed to reduce EMAs. Patient Safety 100% 7 Provision of a dedicated community nurse for each GP practice to support admission avoidance Patient experience Effectiveness 100% 8 Pharmaceutical care plans for “at risk” patients Safety 100% 9 EoL – For NCH&C care home facilitators to roll out training for ACP/PPoC and ensuring PPoC is utilised where clinically appropriate. 15 Care homes will be targeted and supported Patient experience 100% 10 Improve the care of paediatric patients in the community through scoping of activities to be transferred into a community setting from the acute sector and producing a model of community paediatric care to include IV Patient experience Effectiveness 100% 11 Achieve improved outcomes for patients of the community nursing and therapy service in five key areas Effectiveness 58% 12 Avoid acute hospital admissions through effective case management of those at greater risk of admission Effectiveness 100% 40 Quality Account 2012/13 3.5 Clinical Quality and Quality Goals for 2012/13 Quality remained top of our agenda in 2012/13, with a focus on delivering an ambitious set of planned quality goals. Our Quality Goals for 2012/13 were developed through the annual planning process and a series of workshops with clinical staff. They are reported in the forwardlooking section of last year’s Quality Account for 2011/12 and are listed as follows: This section outlines the Trust’s progress against national and regional quality improvement priorities as well as the Trust’s own priorities and Quality Goals from 2012/13 under the following headings: 1.Implement safety thermometer targets in four key areas • Patient experience – listening to what our service users think • Achieve 95% Venous Thromboembolism assessment (VTE) for inpatients by December 2012 • Patient safety – protecting people from harm • 50% reduction in catheter acquired urinary tract infections by December 2012 • Effectiveness of care – promoting a culture of continuous improvement through audit and research projects and implementing NICE guidance • Reduction in the levels of injurious falls in our inpatient units to 4.0 per 1,000 occupied bed days • Eradication of avoidable pressure ulcers (as detailed in 2 below) 2.Deliver zero avoidable pressure ulcer target by December 2012 (Grades 2-4) 3.Improve patient satisfaction to 70% very satisfied and no area < 50% 4.Implement the net promoter score system and meeting target set for inpatients 5.To achieve ‘you’re welcome’ accreditation in school nursing service 6.To achieve UNICEF ‘baby friendly’ accreditation at level 2 Norfolk Community Health and Care NHS Trust Quality Goal 1 Implement safety thermometer targets in four key areas The Safety Thermometer data collection tool is now in place, showing a level of ‘no harm’ of 89.9% at March 2013. To achieve 95% Venous Thromboembolism assessment for inpatients by December 2012 Performance over the year is demonstrated in the graph below showing that we have been ahead of the 95% of patients assessed for VTE consistently since August 2012. GRAPH % Assessed for VTE Ward level monitoring is carried out and an escalation process is in place to the Medical Director. A report 99% which calculates compliance, is being pre-empted by 98% a review each month of Patient data on the Inpatient 97% spreadsheet by Ward Clerks with a view to validating 96% figures before they are calculated. 100% 95% For the forthcoming year we will be undertaking 94% clinical 93% audits to ensure that assessments and treatments were effective. 92% A pr -1 M 2 ay -1 Ju 2 n1 Ju 2 l-1 A 2 ug -1 Se 2 p1 O 2 ct -1 N 2 ov -1 D 2 ec -1 Ja 2 n1 Fe 3 b1 M 3 ar -1 3 91% % Assessed Linear (% Assessed) 41 50% reduction in catheter acquired urinary tract infections (CAUTI) An analysis of all laboratory positive catheter urine specimens has helped to establish a baseline and trajectory for NCH&C, which will be monitored internally via the CAUTI Steering Group. For November and December we met the target reduction and were well ahead of schedule and remained ahead of trajectory for the remainder of the year, (see section 3.9.9 for more details). Reduction in the level of injurious falls in our inpatient units (4.0 per 1,000 occupied bed days) Injurious patient falls have been below 4.0 per 1,000 occupied bed days since April 2012 our average over the year is 3.41 per 1000 occupied bed days, (see section 3.9.8 for more details). 42 Quality Account 2012/13 Quality Goal 2 Deliver zero avoidable pressure ulcers by December 2012 There were no avoidable pressure ulcers within our inpatient settings at the end of December 2012 as a result of our staff’s effort to reduce patient harm. This achievement means our inpatient areas successfully met our ambition to eliminate avoidable pressure ulcers by the end of 2012. However, we reported eight avoidable pressure ulcers within our community settings, though the trajectory continues on a downward trend. Over the last year, we have worked closely with staff to tackle pressure ulcers, developed a best practice policy, and introduced new tools, documentation, and support materials. Key activities during 2012/13 to train staff and prevent the incidence of pressure ulcers were: • 40 pressure ulcer champions identified across NCH&C • A quarter of our staff attended dedicated pressure ulcer prevention and management training events • We delivered 35% more pressure relieving equipment in October 12, than we had done six months earlier • Transfer of care protocol agreed with our main acute partner Quality Goals 3 and 4 Improve patient satisfaction We continue to show steady progress in eradicating avoidable pressure ulcers in both our inpatient units and in the community of which at least 50% occur in care homes. Our latest position for March 2013 shows a total of four avoidable pressure ulcers all occurring in the community, (including care homes). In service specific surveys carried out during 2012/13, we achieved very high patient satisfaction levels, eg, 86% users of Community Nursing and Therapy service ‘very satisfied’ and 87% of our Wheelchair Services users, (see section 3.8 for more details). Our aims for the year 2013/14 are to maintain zero avoidable pressure ulcers across all our inpatient units and to eliminate avoidable pressure ulcers in the community by quarter 4. As part of this objective, we will be working with our ‘top 10’ care homes to improve prevention interventions. The Net Promoter score system has been implemented. These results remain in the top quartile of 71 or more with the exception of December (58). Results were lower in December than all previous months due to a higher number of neutral/passive scores being received. By March 2013 the score had risen again to 75, (see section 3.8 for more details). Norfolk Community Health and Care NHS Trust Quality Goals 5 and 6 Children Services You’re Welcome accreditation A self-assessment against the ‘You’re Welcome’ accreditation in the school nursing service has taken place in 2012/13 Q4, but the method for accreditation remains unclear due to the recent changes in commissioner responsibilities. An action plan will be produced and implemented in 2013/14. UNICEF Baby Friendly accreditation We have not yet achieved UNICEF Baby Friendly accreditation at level 2, but will be reassessing against the standard in 2013/14. Two out of thirteen indicators require further assessment. An action plan is in place. Staff are also being encouraged to make use of the latest breastfeeding resources, which are now available to download from our intranet. The breastfeeding page includes mandatory annual practical skills review paperwork, supplementary materials to support this process, and links to best practice information and video clips. This new information and resources will support staff, particularly our health visitors, nursery nurses and children’s centre staff, to deliver the very best care to local families. This will also help us to achieve Stage Two Baby Friendly status. 43 Quality Account 2012/13 44 3.6 Monitor’s Quality Governance Framework Monitor describes quality governance as the combination of structures and processes at and below board level to lead on Trust-wide quality performance, including: • Ensuring required standards are achieved (or exceeded) • Investigation and taking action on sub-standard performance • Planning and driving continuous improvement • Identifying, sharing and ensuring delivery of best-practice • Identifying and managing risks to quality of care The arrangements for quality governance will complement and be fully integrated with all the other governance arrangements in place to ensure the Board is competent in fulfilling all of its statutory responsibilities. Ultimately, the Trust Board is responsible for the quality of care delivered across all services provided by NCH&C; however, responsibility will be delegated right through to individual staff members ensuring that quality improvement is at the heart of everything that the organisation does. The Board will create a culture of openness and transparency from the operational services to the board. All Managers will be expected to continuously improve care by listening to service users and learning from incidents. Engagement and involvement of staff and patients at all levels will ensure that areas for improvement are continuously identified. The Trust has undertaken a robust self-assessment against the 10 quality questions (see below) using Monitor’s risk rating and scoring matrix as follows: Risk Rating Scoring Definition Evidence Green 0.0 Meets or exceeds expectations Many elements of good practice and there are no major omissions Amber/Green 0.5 Partially meets expectations but confident in management’s capacity to deliver green performance within a reasonable timeframe Some elements of good practice, has no major omissions and robust action plans to address perceived shortfalls with proven track record of delivery Amber/Red 1.0 Partially meets expectations but with some concerns on capacity to deliver within a reasonable timeframe Some elements of good practice, has no major omissions. Action plans to address perceived shortfalls are in early stage of development with limited evidence of track record of delivery Red 4.0 Does not meet expectations Major omission in quality governance identified. Significant volume of action plans required and concerns as to management capacity to deliver Norfolk Community Health and Care NHS Trust 45 A review by KPMG, an external auditor, in March 2012, confirmed our self-assessment rating as 3.5 which is within Monitor’s compliance framework threshold of 4.0. Our Executive Director Team (EDT) has reviewed the QGF each quarter during 2012/13, prior to discussion and approval by the Trust Board and during this time we have moved from a 3.5 rating in Q1 to 1.5 rating in Q4. Following the publication of the Francis review and the increased focus on quality we have decided to refresh this work with a series of Board seminars to review our current position. KPMG will undertake a further review in June 2013. Monitor’s 10 Quality Questions: Strategy Capabilities Processes and structures Measurement 1a Does quality drive the Trust’s strategy? 2a Does the Board have the necessary leadership, skills and knowledge to ensure delivery of the quality agenda 3a Are there clear roles and accountabilities in relation to quality governance? 4a Is appropriate quality information being analysed and challenged? 1b Is the Board sufficiently aware of potential risk to quality? 2b Does the Board promote a quality-focused culture throughout the Trust? 3b Are there clearly defined, well understood processes for escalating and resolving issues and managing quality performance? 4b Is the Board assured of the robustness of the quality information? 3c Does the Board actively engage patients, staff and other key stakeholders on quality? 4c Is quality information used effectively? 46 Quality Account 2012/13 3.7 Quality Assessment Visits A series of visits to assess the quality of services in all our Community Rehabilitation Units and compliance with CQC outcomes was introduced in February 2013 and undertaken by the Deputy Director of Nursing, together with our Quality Assurance Managers. The assessment visits are focusing on five of the CQC standards and outcomes: • Involvement and information Outcome 2: Consent to care and treatment • Personalised care, treatment and support Outcome 4: Care and welfare of people who use services Outcome 5: Meeting nutritional needs • Suitability of staffing Outcome 14: Supporting workers • Quality and management Outcome 16: Assessing and monitoring the quality of service provision • Safeguarding and Safety Outcome 7: Safeguarding people who use services from abuse Overall the assessors have been impressed by the quality of care offered to patients by the Community Rehabilitation Units. The patients and relatives who were spoken to said they were extremely pleased with the care they or their relatives received. One patient said: “staff are always eager to please and I couldn’t fault them”. Staff report they are proud of their wards and value the support provided by their colleagues and managers. The assessors have observed effective multi-disciplinary and multi-agency working to ensure the best outcomes for our patients throughout their care pathway. The quality assessment visits have produced baseline evidence against CQC outcomes. The assessors have identified factors which could make the outcomes for patients even better. There have been two key themes emerging; visibility of name badges and concerns about the effectiveness and volume of documentation which will require addressing from an organisational perspective and will be linked to a transformation project. The assessment reports have been finalised and shared with the Assistant Directors. The Assistant Directors will work with their staff to review the reports and develop action plans which will be monitored on a monthly basis by the Quality Assurance Managers for each locality. Any moderate or major concerns will be escalated appropriately for action and reported to the Quality and Risk Assurance Committee (QRAC). Plans are in place to roll-out these quality assessment visits to our community teams during the summer and will form the basis of the work of the new posts of Quality Assurance Managers. Norfolk Community Health and Care NHS Trust 47 3.8 Patient Experience 3.8.1 Introduction As a healthcare organisation we have the privilege of serving people at their most vulnerable. We know it is important that the care they receive is safe and helps them to get better or effectively maintain their condition. It’s also important that in receiving that care our patients are treated with care and compassion by skilled people and in those circumstances we are committed to delivering the best experience of care that we can. To help us do that we ask our patients what they think of the care we deliver and in response celebrate things that go well as well as put right things that haven’t gone as we would like. We learn from patients in a variety ways, for example we asked our patients on discharge from our community rehabilitation units “how likely is it that you would recommend this service to friends and family”, surveyed patients accessing other services and listened to a ‘patient’s voice’ at our Board meetings. 48 Quality Account 2012/13 3.8.2 The ‘Friends and Family Test’ Overall the comments being received by patients through NPS are very positive, although there are some areas for action, improvement or monitoring. Quality Goal and CQuIN: Implement Friends and Family test using the (NPS) Net Promoter Score, results to be above 63 Top 4 Themes from ‘promoters’ comments (Score of 9 or 10 out of 10) The Friends and Family test, asking all inpatients on discharge from our community hospitals, “How likely is it that you would recommend this service to friends and family?” went live during May 2012. Patients have been given a feedback card on the day of discharge to rate their score between 1 and 10 and leave any comments as to why they gave that score. A minimum survey size of 10% of all inpatients discharged was set and this has been achieved and exceeded every month to date. • Very clean Results from July 2012 – March 2013 are as follows NPS Scores • High standard of care and treatment • Caring, kind and compassionate staff • Good food Top 3 Themes from ‘detractors’ (score of 6 out of 10 or less) (although often the comments are fairly positive) • I received good care • I was satisfied with the services • I was refused meals on wheels just because I could put stuff in the microwave, a good thing because I felt much better going private 90 Top 5 Themes from ‘neutral/passives’ comments (Score of 7 or 8 out of 10) 80 • Positive experience 70 • More staff needed, visit too brief 60 • Food needs improving - general flavouring 50 • Comfortable and clean 40 • Treated well by staff 30 20 10 3 M ar -1 13 bFe 13 n- 2 Ja 2 ec -1 D ov -1 12 No of responses N ct - 2 12 O pSe -1 ug A Ju l-1 2 0 NPS score These results remain in the top quartile of 71 or more (the target set for acute hospitals for 2012/13) with the exception of December. Results were lower in December than all previous months due to a higher number of neutral/passive scores being received (patients scoring 7 or 8 out of 10) although the majority of comments were still very positive. Norfolk Community Health and Care NHS Trust 3.8.3 Patient stories Patient Feedback Challenge NCH&C continues to be involved in a joint project with the NNUH in collecting patient and carer feedback throughout the stroke pathway through the use of Patient Stories. The cohort of six stories have been collected and next steps will be to bring staff from both NCH&C and NNUH together to review the finding from the stories and develop any actions as a result. Patient Voice at the Board Patient stories are a key feature of the ambition to ‘Revolutionise Patient and Customer Experience’, whereby Boards are being asked to capture, use and triangulate intelligence pertaining to patient and carer experience from a variety of different sources. Patient Stories provide a focus on how through listening and learning from the patient voice. NCH&C’s Board confirmed that as part of its commitment to strengthen the patient voice it wished to receive and consider a patient story at each of its Board meetings. The stories heard so far have mostly been told by a member of staff from the relevant service used by the patient to give a ‘case study’ style story. There have been a couple of occasions when the patient has attended and told their story personally. 49 For example, a member of staff from Sure Start Children’s Centre, Thetford and a Norfolk LINk Volunteer attended NCH&C Board meeting in December 2012 describing how they have used Patient Stories to collect feedback from the parents attending a “Babystart” group. Using Patient Stories has been a positive experience for the team, reinforcing they are “getting it right” , boosting morale and understanding what parents and their children really benefit from but also finding out what could be improved. The team are already working on actions as a result of doing the stories which include: • Increase publicity about the Children’s Centre and groups offered through liaison with health visitors, midwives and local libraries • Rotation of a range of toys and play equipment both inside and outside groups A programme of using Patient Stories to improve care in targeted areas has been developed, allocating a trained volunteer or member of staff to work with the following services: • Podiatric surgery • Wheelchair services • North Norfolk Older People • Stroke pathway (as part of the NHS Patient Feedback Challenge project with NNUH) 50 Quality Account 2012/13 3.8.4 Patient Opinion 3.8.5 Local surveys Patient Opinion is a website: www.patientopinion.org. uk where the public can publish their experiences (good or bad) of local health services. The website allows health service staff to interact with these patients to help improve care. There is also the option of giving patients a hard copy feedback card or they can call a freephone number and tell their story over the phone. Quality Goal: Improve patient satisfaction to 70% ‘very satisfied’ no area <50% NCH&C commenced a small pilot in early March 2013 in four services to trial Patient Opinion. 23 stories were posted on the website during April and these stories had been viewed 820 times. There has been some excellent feedback about all of the services included in the pilot and service leads are being encouraged to respond to comments regardless of content to demonstrate that we are actively engaging with their feedback to improve care. Service leads are also being encouraged to link into an online training session offered by Patient Opinion to support raising awareness with patients, responding to comments and how to use reports within the service and organisation. During this pilot phase, work is ongoing to develop processes ensuring Patient Opinion is monitored, reviewed and linked in to other patient feedback systems. a) Cardiac Assessment Service The ‘Cardiac Assessment Service’ was set up as a new initiative in 2004, with the aim to promote efficiency of the pathway delivering care to patients with Acute Coronary Syndrome (Heart Attack and Unstable Angina). This efficiency translated into reduction of length of stay (LOS) in the acute trust with reduction in re-admission rates. One of the aims of the service is to educate and support patients and their relatives to equip them to take responsibility for their long term condition, so helping to promote, improve their quality of life and reduce acute events requiring admission to hospital. In the Cardiac Assessment Service (CAS), patients are often seen as a ‘one off’ acute assessment within the acute admissions area. Questionnaires were distributed to each patient with the instruction to complete and place in the clearly marked NCH&C official collection box. The box was then collected later in the day to allow private consideration of the questionnaire, confidential completion and return to the box. All 30 questionnaires were returned. The feedback was very positive and overall demonstrates that the CAS is highly valued by patients and their relatives. 100% of respondents felt they understood the role of the service/ felt they were treated with dignity and respect/ felt the service helped them to understand their condition and allowed them the opportunity to have questions answered, with the conclusion that they all benefited from improved understanding of their long term condition. Norfolk Community Health and Care NHS Trust Issues Arising 87% said that the assessment helped them make lifestyle changes to manage their condition; however, 13% did feel they needed some on going advice, one mentioning the access of written information. These patients do, however, receive a referral on to an outpatient Cardiac Rehabilitation Service or CVD Specialist Nurse for advice and support. ACTION: • Issue British Heart Foundation (BHF) booklets in addition to those which will be given in a pack by the Cardiac Rehabilitation Nurses where appropriate • Issue BHF booklets to those patients not falling under the remit of the Cardiac Rehabilitation Nurses • Refer on to the Community CVD Specialist Nurse for further support and advice on risk factors as appropriate 97% felt re-assured by the cardiac assessment nurse, however surprisingly low (only one patient) still had concerns about what is a life threatening condition. ACTION: 51 c) Wheelchair Services Patient Experience Survey A patient experience survey was carried out to gather feedback from patients on Wheelchair Services from September 1 to October 31, 2012. All patients who attended the centre for an appointment between September 1 to October 31, 2012 were given a hard copy of the survey to complete. Boxes were also provided in the waiting area for patients to post their completed surveys. 104 surveys were completed by patients, approximately 50% of all patients attending an appointment during that period. Conclusions: Overall, the feedback from patients is very positive on the service they received with 94.2% of patients saying they were very satisfied (86.5%) or fairly satisfied (7.7%). Similar levels of satisfaction were received on the helpfulness of reception staff and clinical staff. • Inpatients requiring ongoing support, refer to CVD Specialist Nurse in the Community for follow-up telephone call, as appropriate 100% of patients who answered the three environment questions agreed that they had enough privacy, felt physically safe and were satisfied with the cleanliness of the centre. b) Community Nursing & Therapy Service Patient Satisfaction Survey 99% felt involved as much as they wanted to be in decisions about their care. As part of CQuIN indicator 11, the Trust has carried out a patient satisfaction survey within Community Nursing and Therapy. The results from the survey indicated 94% of patients were satisfied overall with the service provided by the CN&T Teams. Specifically 86% very satisfied and 8% were fairly satisfied. NCH&C intend to survey again using the same survey and methodology during quarter 4 and although no specific target has been set by commissioners, NCH&C have set an internal target to maintain satisfaction levels at 94%. 22 patients have expressed an interest in potentially being part of a patient user group and 31 expressed an interest in undertaking a one to one patient story. Further comments were received from 35 patients. There were two comments around waiting times but no other common themes emerging from these. Recommendations: 1. Look in more detail at waiting times (two comments received) 2.Contact patients regarding joining a Patient User Group 3.Contact patients regarding undertaking a Patient Story 52 Quality Account 2012/13 d) Catering Survey within the community hospitals The purpose of the patient satisfaction survey is to measure the quality and standards of the catering service within the community hospitals setting, to identify issues that occur within it and where possible, rectify them. The survey is divided into five sections, Menu options, Food, Beverages, Environment and Support. Each subsection has three or more questions that require answering. Measurements range from Very Poor to Excellent on the Food and Environment sections, while the remaining three sections range from Never to All the Time. Patients indicate their preference by ticking the appropriate box they feel meets their perception and level of satisfaction. From the results of the surveys, it shows that standards have increased slightly from the survey conducted in July 2012 from a satisfaction rate of 84% to 89.3% of ‘Excellent’ and ‘Good’ responses. The fair responses have remained the same at 8.3%, with ‘Poor’ and ‘Very Poor’ making up the rest with 2.5%. The overall completion rate has decreased from 63% in July 2012 to 48% in November 2012. Some units continue to have low completion rates; this could be due to the types of patients and the nature and number of questions of the new survey. Several surveys were incomplete. One unit was also closed for refurbishment during the time of the survey. Having reviewed the results per section, the standout areas are: • Improvement in virtually all aspects of the service from the last survey in July, for example, in the Food section: taste up to 78% from 71%, appearance up to 88% from 75%, and helpfulness of staff up to 98% from 91% • The overall satisfaction rate increased significantly from 77% in July, to 84% in November, considerably higher than the 73% recorded in the Picker Institute survey undertaken in May 2011 • Where negative feedback has been received, these will be incorporated into an action plan for the appropriate Housekeeper to follow up and implement, within a specific time frame 3.8.6 Patient Environment Action Team (PEAT) Assessment 2012 The NHS Information Centre (NHS IC) requires trusts to self-assess their patient environment annually using an assessment tool which reflects the needs of its various stakeholders and the policy priorities of Ministers and the Care Quality Commission (CQC). As a result of feedback from users, the Department of Health, CQC and other organisations, changes were made to the assessment for 2012. Changes included questions on laundry services, security arrangements for the storage of drugs and additional questions on the Infection Control section. The assessments took place across our nine inpatient services between January and March 2012 with formal reporting to the NHS IC by 14th March 2012 and the Trust Board on 29th August 2012. The PEAT assessment team was led by the Estates and Facilities Officer and included representation from Estates, Infection Control, Norfolk LINk and a Matron or site representative for each site. The table below provides an overview of the ratings achieved by each unit in 2012, these have been confirmed in a letter to the CEO. Ratings for 2011 are given in brackets. The final ratings produced by the NHS IC have been calculated using the scores committed by the Trust, weighted against the National Standards of Cleanliness scores for each unit. Norfolk Community Health and Care NHS Trust 53 Site Name Environment score Food Score Privacy and Dignity Score Colman Hospital Good (G) Good (G) Good (G) Norwich Community Hospital Good (g) Excellent (G) Good (G) Dereham Hospital Good (A) Excellent (E) Good (G) St. Michaels Hospital Acceptable (G) Good (G) Good (E) Kelling Hospital Good (A) Good (G) Good (G) Swaffham Community Hospital Good (A) Excellent (E) Good (G) Ogden Court, Wymondham Good (G) Good (G) Good (E) Cranmer House, Fakenham Good (G) Excellent (E) Excellent (E) Benjamin Court, Cromer Good (G) Good (G) Good (E) Key: (G) Good (E) Excellent (A) Acceptable Overall, there was an improvement in four out of the 27 scores with 19 remaining the same (of which four were excellent), a drop in 1 from good to acceptable under environment and 3 from excellent to good under privacy and dignity. A progress report was provided to the Board in February 2013 together with a comprehensive action plan arising from the assessment. The improvement works required were conducted either as part of the 2012/13 capital programme or minor works programme. In accordance with the Prime Minister’s commitment to give patients a real voice in assessing the quality of healthcare, including the environment for care, the Department of Health and NHS Commissioning Board have reviewed the efficacy and value of PEAT assessments and from 2013 have introduced a more patient-led assessment called PLACE. The outcome of the assessments will be published as Official Statistics and will be shared with the following organisations: • Care Quality Commission • Department of Health • NHS Commissioning Board • Clinical Commissioning Groups • National Audit Office 54 Quality Account 2012/13 3.9 Patient Safety – learning from incidents and complaints 3.9.1 Introduction NCH&C aims to provide harm free care for all its patients and is committed to learn when things go wrong. We use complaints and incidents to positively identify where changes need to be made and improvements implemented in a culture that is both supportive and open. 3.9.2 Complaints, claims and compliments During the period April 2012 to March 2013, 170 complaints were received from service users or their relatives. This represents a 15% decrease on last year’s figure of 202. 94 of these complaints were partially or wholly upheld following investigation. MPs were involved in 10 complaints this year and GPs were involved in 11 complaints. 14 complaints were investigated jointly with other agencies (eg, NHS Norfolk & Waveney, Norfolk & Norwich University Hospital and Norfolk County Council Social Services) under the agreed Joint Protocol for Norfolk. Complainants who are unhappy with the Trust’s response may ask the Parliamentary and Health Service Ombudsman to review their case. We were notified of three such requests this year; however, the Ombudsman declined to review any of these cases. Complaints by subject 15% 1% 14% 62% 4% 22% 12% 13% 27% Care and Treatment Personal Records Appointment Policy Aids / Equipment Discharge Other Communication Staff Attitude Norfolk Community Health and Care NHS Trust a) Complainant feedback 15 complainants returned feedback questionnaires during the year. 10 of these stated they were satisfied or mainly satisfied with the complaints process and the outcome of their complaint. All stated that their aim in making the complaint was to prevent others suffering the same problem and/or to receive an apology or explanation. Three complainants (less than 2%) expressed a wish that staff should be disciplined. b) Summary of learning and actions taken Learning from complaints is collated from the service managers following an investigation and communicated across the organisation via the Quality and Risk monthly report (seen at the Quality and Risk Assurance Committee and the Trust Board) which is published on the Trust’s website and through the monthly staff newsletter. Themes from complaints are discussed by senior management and, where appropriate, are included in the clinical audit forward plan. c) Clinical claims Notification was received of seven possible claims for clinical negligence during the year. Formal letters of claim have been received for two of these; one concerned the death of a patient in an inpatient unit and the other a delay in family being advised of a diagnosis in respect of a child. Two claims were settled – one in respect of podiatric surgery and one settled jointly with the Medical Defence Union (representing the GP) respect of late diagnosis of hip displacement of a child. Two claims were discontinued because of a lack of response from the claimant or their solicitor. d) Compliments Compliments and thanks received from patients are also measured and this year the Trust has received in excess of 955 compliments. The dedication and commitment of our frontline staff is a recurring theme of the compliments received, (see section 3.2.5 for a summary of quotations) 55 3.9.3 Serious Incidents Requiring Investigation (SIRIs) Serious incidents are reported into a central team, with information being collected via a SIRI log and DATIX a web-based risk management tool. The Executive Team are made aware of serious incidents as they occur and are able to ensure that support for investigations is given to operational teams where required. The Trust Board are informed on a monthly basis of all new SIRIs occurring and the resulting recommendations / actions identified as part of the full investigations into SIRIs. In addition, a quarterly SIRI meeting is held with the Non-Executive Directors of the Board where each of the SIRIs is discussed in more detail. Themes from serious incidents inform learning events, which are attended by a wide range of staff. The topics for learning events held within the last year: • Enabling people to die with dignity (including do not resuscitate orders) • Information Governance – Negotiating the minefield of social networking • Record keeping – if it isn’t documented – it didn’t happen From 1 April 2012 to 31 March 2013, NCH&C reported 349 SIRIs. During this time, there were two changes to the SIRI reporting requirements: • May 2012 – all Grade 3 & 4 Pressure Ulcers became SIRI reportable irrespective of whether they were acquired within the care of NCH&C or outside the care of NCH&C • October 2012 – Grade 3 & 4 Pressure Ulcers acquired outside the care of NCH&C no longer SIRI reportable Quality Account 2012/13 56 The following table identifies the type of SIRI reporting from April 2012 to March 2013: SIRI - Type Number reported Pressure Ulcer - Acquired whilst patient under the care of NCH&C – Grade 3 215 Pressure Ulcer - Acquired whilst patient under the care of NCH&C – Grade 4 24 Pressure Ulcer - Acquired outside the care of NCH&C – Grade 3 & 4 70 Unexpected death 15 Information Governance 6 Infection Control 3 Accident 13 Clinical assessment & treatment 1 Missing patient 1 Staff competence 1 Medication 1 Allegation of abuse 1 Total 349 Learning from a review of unexpected deaths in community hospitals During a four month period from June to September 2012 NCH&C reported and reviewed five patients who died unexpectedly within a community hospital. The aim was to understand the root cause of the incidents, and to review all aspects of quality assurance within the particular inpatient unit. The review also considered in depth, the current clinical practice across all of the Trust’s inpatient units and identified the continuous programme and systems of audit and assurance. Following root cause analysis investigations into each of the deaths, a further clinical review was undertaken by two senior medical consultants who reviewed each of the cases and concluded that of the five deaths only one was, in their opinion, ‘unexpected’. A summary of each case was provided which identified key themes, learning and some notable practice. One of the key findings included the increasing complexity of patients admitted both from the community and the acute units. We are therefore expediting our current plan to introduce an enhanced medical and nursing model of care. An analysis of the workforce was also included which looked at the potential impact of staff absence, turnover, training and appraisal levels and included the medical input. This investigation confirmed that these deaths do not represent a failure of service delivery nor of patient safety. However, the incidents have identified areas of service delivery which can be improved. A further strategic review to consider the findings from the report more broadly across other similar units within NCH&C has been completed and the report was taken to the public Trust Board meeting in February 2013 (see our website for the full report in our Board papers: www.norfolkcommunityhealthandcare.nhs.uk) A strategic action plan has been developed and approved by the Board and a steering group has been formed to ensure the delivery of the agreed actions. Implementation of the action plan is being monitored by the Quality and Risk Assurance Committee and the Norfolk Clinical Commissioning Groups. Norfolk Community Health and Care NHS Trust 57 3.9.5 National Patient Safety Agency Report (NPSA) The latest report in respect of incidents reported to the NPSA between 1 April 2012 and 31 September 2012 was published in March 2013. This report shows that NCH&C has slipped from being within the highest 25% of reporters to the middle 50% of reporters. The number of incidents reported to NPSA during this period equated to 58.3 incidents per 1000 beds days (compared to 147.3 incidents per 1000 bed days in the previous report). This reduction was expected due to the delays in the final incident approval process and backlog of incidents awaiting final approval which has delayed incidents being forwarded to NPSA. 3.9.4 Never Events The Department of Health (DH) published a Never Events Policy Framework in October 2012 which is an update to the Never Events policy and provides greater clarity around never events and how to respond to them. The DH said, “Protecting patients from avoidable harm is something on which there is universal agreement. How we achieve this is often more complex. With ‘Never Events’ there are clearly defined processes and procedures to follow to help ensure that these incidents never happen.” Never Events are serious, largely preventable patient safety incidents that should not occur if the available preventative measures have been implemented by healthcare providers and result in severe harm or death (or have the potential to result in severe harm or death). NCH&C has undertaken a review of the Never Events which could occur within this organisation and has asked staff to provide assurance that there are adequate controls in place to mitigate them. The Trust is pleased to report that it has had no ‘Never Events’ during 2012/13. It is important to note that the reduction in the number of incidents reported to NPSA is not reflective of the number of incidents that we report within the Trust, as our incident reporting continues to grow. It is difficult to analyse and make comparisons within the latest report. For example, we have given priority to final approval of severe incidents, pressure ulcers and slips / trips and falls, and therefore the breadth of incidents that we have reported to NPSA has been limited, it therefore appears that a high percentage (69%) of NCH&C incidents are reported as “implementation of care and ongoing monitoring / review” which is the category pressure ulcers are reported within, compared to the average of 29%; however, as we have not reported to NPSA many other incident types this is not an appropriate comparison. As with the previous NPSA report, it was noted that there is a delay in NCH&C reporting incidents to NPSA, 50% of all incidents where submitted to NPSA more than 30 days after the incident occurred with 50% being submitted more than 45 days after the incident occurred. It has been agreed to allocate a member of staff to specifically tackle the backlog of incidents awaiting final approval, while the new posts of Quality Assurance Manager, (who will work alongside operational teams) will maintain the approval of current incidents. 58 Quality Account 2012/13 3.9.6 Safety alerts 3.9.7 Reducing the level of harm of medication incidents Alerts originating from the Medicines and Healthcare Products Regulatory Agency (MHRA), National Patient Safety Agency (NPSA), Chief Medical Officer (CMO) and Department of Health Estates are broadcast via the Central Alert System (CAS) in England. These alerts must be disseminated in a timely manner throughout NHS Trusts to ensure all staff affected by the safety alert have timely access to relevant information. Continuing the success of work done the previous year the Trust reported 8 moderate harm or above incidents in 2012/13, compared to 13 the year before. The graph below show the trend of no harm, low harm and moderate harm incidents during 2012/13. The reporting data was complicated by NCH&C ceasing to provide healthcare services into the three Norfolk Prisons in April, re-opening of North Walsham Hospital in May and the closure of Dereham Hospital for improvements from October 2012 to January 2013. It is therefore difficult to compare month to month due to these variations. The Health, Safety and Fire Officer is the nominated recipient of CAS alerts and employs an electronic system of dissemination of alerts to all NCH&C localities and business units and other relevant departments. NCH&C also employs an electronic response system which tracks the acknowledgement of alerts and informs the Health Safety and Fire Officer whether action by the locality, business unit or department is required in response to the alert. 60 50 40 30 20 10 -1 2 Ju n12 Ju l-1 2 A ug -1 2 Se p12 O ct -1 2 N ov -1 2 D ec -1 2 Ja n13 Fe b1 M 3 ar -1 3 M ay pr -1 2 0 A Number The Health and Safety Committee monitors the implementation of all relevant alerts and the Executive Director team receives a monthly report on all open or overdue alerts supporting remedial actions, where required, to achieve closure. Breakdown of number of incidents by severity, with trends No harm Moderate harm Low harm Norfolk Community Health and Care NHS Trust Controlled drug incidents There were 80 controlled drug incidents reported in 2012/13 which, after accounting for the exit of prison services, is in line with previous years. The graph below shows the trend for controlled drug incident reporting. These incidents covered a range of issues, such as missed doses, syringe driver incidents, difficulty in obtaining stocks, stock balance issues and administration incidents. Number of controlled drug incidents by month and severity 25 Number 25 20 15 10 5 No harm Low harm 2 -1 12 M ar 12 b- b- Fe Fe 1 12 n- Ja -1 1 D ec 1 -1 ov N 11 -1 O ct 1 Se p- 1 -1 l-1 ug Ju A 1 11 n- Ju -1 ay A M pr -1 1 0 Moderate harm CQUIN Indicator 8 Pharmaceutical care plans The aim of this project was to use a patient-led pharmaceutical care plan to improve medicines adherence and the transfer of information on discharge (and potentially on any subsequent readmission) from NCH&C inpatient units. The care plan was successfully introduced into all Trust inpatient units and 76% of the patients in the target group were discharged with a “My Medicines” booklet, which detailed their medicines and how and why they take them. 59 60 Quality Account 2012/13 3.9.8 Patient falls Inpatient - Patient falls reported by Degree of Harm Quality Goal: Reduction in the levels of injurious falls in our inpatient units to 4.0 per 1,000 occupied bed days 80 40 Number The second graph shows the level of falls causing harm per 1000 occupied bed days (target being 4.0). 40 40 20 Actions currently underway include, regular monitoring of the data and targeted interventions, eg, intentional rounding. Falls representatives from each unit report Root Cause Analysis (RCA) to improve learning and access the locality. Regular Falls meetings led by a dedicated lead clinician. 12 l-1 2 A ug -1 Se 2 p1 O 2 ct -1 N 2 ov -1 D 2 ec -1 Ja 2 n1 Fe 3 b1 M 3 ar -1 3 2 Ju n- Ju -1 ay M A pr -1 2 0 No harm Moderate harm Low harm Severe harm Falls/OBD performance - inpatient units Ju 2 n12 Ju l-1 2 A ug -1 Se 2 p1 O 2 ct -1 N 2 ov -1 D 2 ec -1 Ja 2 n1 Fe 3 b1 M 3 ar -1 3 M ay -1 2 5.0 4.5 4.0 3.5 3.0 2.5 2.0 1.5 1.0 0.5 0.0 pr -1 Falls/1,000 OBD Matrons have reported an increasing number of patients being admitted to the units either with a diagnosis of dementia or with symptoms of confusion during February and March 2013. More equipment for falls prevention including use of ‘Hi-Lo’ beds and crash mats were also in place in this period. We will be undertaking an analysis of the rehabilitation complexity score to better understand this trend. 60 A The graph right shows all categories of patient falls over the past year. 100 2012/13 Performance 2012/13 Target Norfolk Community Health and Care NHS Trust 3.9.9 Infection prevention and control a) Reduction in Healthcare Acquired Infections i) Norovirus The Infection Prevention and Control (IPAC) team have continued to work with the Norfolk health economy throughout 2012/13 to improve communication regarding incidence of Norovirus in order to reduce the issues it causes across the system. All acute, community and mental health providers in the county now populate a shared database detailing clusters/outbreaks of Norovirus across the county. The Health Protection Unit host this database and input details of clusters/ outbreaks in any private healthcare facility or school thereby ensuring all information is shared throughout. This provides us with the best opportunity to manage and contain any episodes of Norovirus in our settings. Despite high levels of Norovirus within the general community, NCH&C have only suffered one cluster of Norovirus. This was quickly and efficiently contained with only four patients affected. The ward did not need to close and their patients were managed within side rooms and a bay. Ultimately it is staff vigilance that has kept NCH&C levels of Norovirus so low over the season. The role of IPAC liaison has now been developed in conjunction with Public Health and this will see further investigation of cases of infection within the wider community along with assistance for Primary Care in the management of their patients with either MRSA or Clostridium difficile. The aim of this post is to identify trends in the wider community and bridge the gap in IPAC which currently exists between acute/community providers and Primary Care. 61 ii) Catheter Acquired Urinary Tract Infection (CAUTI) Avoiding CAUTI is of great importance to maintain the health and independence of our patients. The Trust’s aim throughout 2012-13 was to reduce CAUTI by 50% by December 2012. Through the work of a clinical task force including IPAC and continence teams this ambition was achieved earlier than planned. iii) To reduce levels of attributable Clostridium difficile (C. diff) NCH&C saw a period of seven months without a case of C. diff at which point a case was reported in September 2012. The total reportable for 2012/13 was three cases against an annual ceiling of 9. This compares to 5 cases in 2011/12 and 9 cases in 2010/11. iv) To reduce levels of MRSA bacteraemia There were two cases of MRSA bacteraemia in 2012/13, which compares to no cases in 2011/12 and 1 case in 2010/11. As a result of these cases the IPAC team have prepared documentation for all wards to ensure a patient with any history of MRSA will receive octenisan antimicrobial wash throughout their inpatient admission. The IPAC team are working with all ward areas to ensure they are able to identify these patients quickly and easily. The IPAC team continue to monitor and review all results of hand hygiene and cleaning audits. The focus of the IPAC teams auditing programme is due to alter to concentrate on clinical practice on a more regular basis. This will ensure NCH&C staff have the assistance and support to work safely within the constraints of their environments. 62 Quality Account 2012/13 3.9.10 Patient safety and quality benchmarking data Aspirant community foundation trust benchmarking report – period August 2012 to January 2013 NCH&C are part of a group of community trusts on a journey to achieve foundation trust status in the future and 11 trusts have agreed to share data in order to benchmark performance against one another to stimulate debate and identify opportunities for sharing best practice. This benchmarking report covering the period August 2012 to January 2013 presents data on quality, financial and workforce indicators and includes a benchmark figure and an average score for each indicator. The following results are taken from the Patient Safety and Quality section: Description Benchmark Average NCH&C New Serious Incidents Requiring Investigation (SIRIs) reported per month (excluding pressure ulcers which are reported separately) 4.0 4.2 2.8 4.5% 4.1% Percentage of deaths compared to all discharges (excluding end of life and palliative care units and specialties) Rate of injurious falls per 1,000 occupied bed days 4.0 7.05 3.36 Rate of incidents (injurious and non-injurious) per 1,000 contacts 3.46 3.92 7.27 Rate of complaints per 1,000 contacts 0.16 0.16 0.14 Rate of compliments per 1,000 contacts 0.50 1.35 0.80 Net Promoter Score (NPS) 62 62.6 68.9 Safety Thermometer – Harm free care 82% 90.3% 89.54% Reported Clostridium difficile cases per 1,000 occupied bed days 0.135 0.063 0.026 New Grade 3 or above Pressure Ulcers reported per month whether or not acquired under the care of the provider 12 13 25 Norfolk Community Health and Care NHS Trust 3.9.11 Safeguarding vulnerable adults and children NCH&C has designated leads for safeguarding adults and children who liaise with their counterparts at Norfolk County Council (NCC) who are the lead organisation on safeguarding and who chair the safeguarding adults and children Boards in Norfolk. A quarterly progress report against the various work plans is provided to the Quality and Risk Assurance Committee and a strategic quarterly report is provided to the Board. The following items are some of the issues arising over the past year. Response to the Savile Allegations Following a letter from the Chief Executive of the NHS, David Nicholson, a number of areas were specified for review including: • Safeguarding arrangements and practices • Access to patients, including that afforded to volunteers or celebrities • Listening to and acting on patient concerns MASH (multi-agency safeguarding hub) This group disbanded on 31/12/12 with the project becoming part of usual business for NCC. The childrens’ aspect of the service had been the most successful. Child Sexual Exploitation – the Norfolk Safeguarding Children Board is leading local multiagency work in addressing this growing area of concern. 63 Safeguarding adults Recent referrals have lead to a number of outcomes: • Sessions held on mental capacity • Financial seminars available to identify fraud management of this type of abuse • Domestic abuse awareness campaign • Update on DOLS with Specialist Services • Agreement on health specific DOLS training from Social Services Safeguarding training • There has been a consistent rise in the uptake of safeguarding adults training and we are now achieving above 80% • A programme of advanced Mental Capacity Act training for clinical staff has been offered for the next three months • Safeguarding Children training is currently at 79.5% with plans to improve this further • Prevent - training has now commenced. A six month training schedule is in place with three members of staff having undertaken two-days of training to support the rollout of the programme OFSTED report Following the recent Ofsted report into the multi-agency arrangements for safeguarding children, the Director of Nursing, Quality and Operations and the Safeguarding Team are working closely with the local authority’s children services to implement the recommendations. Summary The safeguarding team continues to demonstrate assurance through the quarterly board report, evidencing that policies are adhered to and national and local recommendations and campaigns are supported and implemented. 64 Quality Account 2012/13 3.10 Effectiveness of Care 3.10.1 Introduction Quality care can be described as care which is delivered according to the best evidence as to what is clinically effective in improving an individual’s health outcomes. NICE provides advice and support on putting NICE guidance and standards into practice through its implementation programme, and it collates and accredits high quality health guidance, research and information to help health and social care professionals deliver the best patient care through NHS Evidence. 3.10.2 National Institute for Health and Clinical Excellence (NICE) All NICE guidance is received by the Clinical Audit and Effectiveness committee on a monthly basis in order to ensure that appropriate action is taken, where necessary, to implement the guidance. The Clinical Audit Committee proposed an update to the NICE implementation process, essentially adapting the process to take into account the multiplicity of services in localities. The key stages are: • Assessment of new NICE guidance for applicability to the Trust • Dissemination of relevant guidance for an assessment of impact on the Trust by the services affected • Collation of the localities assessments and decision of implementation strategy / actions and risks by the clinical audit committee • Delegation of monitoring to relevant committees (eg, locality governance meeting if only local applicability, or medicines management, infection control etc) and nomination of Trust lead for key relevant guidance Norfolk Community Health and Care NHS Trust 65 CG142 – Autism in adults Learning Disability (LD) services have provided a trust wide action plan for LD services The following are examples of NICE guidance that has resulted in a clinical audit (or re-audit) a) NICE guidance TA98 and CG72 – Attention deficit hyperactivity disorder (ADHD) management in the community A re-audit working with the Norfolk and Norwich University Hospital to review whether best practice National Institute for Health and Clinical Excellence (NICE) guidelines for management of ADHD are being followed in terms of medication; namely – methylphenidate, atomoxetine and dexamfetamine. CG145 – Spasticity in children and young people This guidance was assessed jointly by services in NCH&C and the Norfolk and Norwich University Hospital in December 2012 as partially compliant – requiring work in developing networks and pathway of care, upper limb spasticity service, transition programme, occupational therapy services. Proposed actions: • Development of network arrangements • Development of pathways - Children with spasticity/cerebral palsy without other medical or developmental disorders - Medically complex children with spasticity as one of a number of related problems - Hip surveillance - Upper Limb assessment and treatment - Transition to adult services • Upper limb assessment and treatment service • Occupational therapy services for children with spasticity SystmOne template needs to plot blood pressure of the patient as well as height and weight. For hand held notes – Ensure clinic stickers are in notes, add heart rate to the proforma, print observational graph and highlight if patient is out of normal limits. For clinician – document compliance and considerations to misuse of drugs, and record medication change rational. b) NICE guidance, CG 137 – Epilepsy Care Plan Audit Adult Services The aim of the audit was to measure against a quality standard (NICE), in order to identify the minimum standards required for Epilepsy Care Plans, ensuring that the service was significantly exceeding these. This service is currently undergoing a commissioning review due to a large increase in demand. An action from this audit was to liaise with the SystmOne team in order to establish Epilepsy Care Plan templates for use by staff, and ease of access, for medical/therapy/nursing and future clinical audit needs. 66 3.10.3 T he Colman Centre for Specialist Rehabilitation (CCSRS) The Colman Centre for Specialist Rehabilitation (CCSRS), which is a specialist rehabilitation service in NCH&C, works towards providing an environment to enable, educate and support service users and their families, who have complex disabilities following an acquired brain injury or amputations of limbs to achieve an optimal level of physical, psychological and social wellbeing. The CCSRS provides an interdisciplinary rehabilitation focused on patient and family centred goals through the world health organisations (WHO), international classification of functioning (ICF) framework as well as the ethical framework. They have a workforce that is competent, committed, caring, compassionate and well-motivated to enable a culture of empowerment to the service user and their family. The team deliver a clearly defined goal oriented holistic interdisciplinary rehabilitation programme, which empower service users and their family to make positive health and lifestyle choices that will help to improve the quality of their lives. The CCSRS team strives to develop integrated pathways of care with existing and new partners which helps with supporting the ongoing rehabilitation needs of service users. They try to access a comprehensive range of assistive technologies, orthotics, specialist wheelchair, augmentive communication aids and other equipments to enhance the patients care and support the rehabilitation process. The team ensure the service adheres to CQC and NICE quality standards and to demonstrate continuous quality improvements through audits and learning from incident reports. Quality Account 2012/13 The outcome tools used are matched to the NHS outcome framework are: • Enhancing quality of life for people following an injury and supporting patients and families to manage their condition (domain 2): Use of goal attainment scale for all admissions • Helping people to recover their independence and functional ability following an injury (domain 3): Changes in UK FIM/FAM and Northwick park dependency scores from admission to discharge • Ensuring that people have a positive experience of care (domain 4): The friends and family test • Treating and caring for people in a safe environment (domain 5): Patient safety incident reports, incidence of medication errors, NHS thermometer Norfolk Community Health and Care NHS Trust 3.10.4 Podiatric Surgery – PASCOM 10 audit system This is a national audit tool that podiatric surgery departments have access to that enables each department to monitor their activity and check their results against other departments around the country. The audit tool is used to record key points within the patient’s pathway from referral to discharge; measurable criteria can be used to make an objective judgement on the treatment strategy deployed. The Consultant Podiatric Surgeon at the centre has designed a retrospective admin-controlled data entry system that attempts to reduce variability and improve validity of the data for the whole department. Currently the team use the system to monitor data, such as change in patient reported outcome measures (MOXFQ), patient satisfaction scores (PATSAT), postoperative complications and surgical activity. There are many other facets of the audit tool that will enable the department to audit data, such as usage of specific medicines, type of local anaesthetic block used, type of tourniquet used and duration of use, etc. 67 In a review of 507 cases of data entered at six months post-operation the following results were noted for the Norfolk Foot Surgery Centre: • PSQ-10 score - 86.53/100 (a score of patient satisfaction based on 10 questions, with the national benchmark being set at 75/100) • MOXFQ scores (3 domains, the first being a score of a patient’s functional outcomes/ improved mobility, the second being an improvement in pain level, and the third being an improvement in the patient’s social activities associated with their foot problem): 35.8, 35.69 and 34.06. Each of these improvements is above the minimal clinically important difference level as described in the research/ validation studies for the associated outcome tool • Of the 507 cases, 61 post operative complications were noted. These ranged from five cases of prolonged swelling following foot surgery to one case of a confirmed deep vein thrombosis Along with benchmarking, the tool can be used to provide data, such as success rates and percentage of post-op complications per specific surgical procedure for patient information leaflets. This can also be used on an individual basis (per surgeon), if desired. Along with real world patient reported outcomes, such as direct compliments and complaints, PASCOM provides an objective data set that goes some way towards monitoring activity, providing assurance and directing reflection on practice in the podiatric surgery centre. Although there are only approximately 500 cases on the system so far, the data for the centre so far show that the whole unit has favourable results when compared to two other similar centres elsewhere in England. It is hoped that the podiatric surgeons will build upon this recent success as the tool continues to provide this important data. Quality Account 2012/13 68 3.10.5 Research and Development The following are a summary of a selection of studies that have patients actively recruited to and are underway. Study Title Aim A randomised controlled trial of self-help materials for the prevention of smoking relapse- 2011GC01 To investigate the effect of a set of self-help educational materials for the prevention of smoking relapse in the NHS Stop Smoking Service. This is a national portfolio study running from the UEA, but has had involvement in the design of the study from both NHS Norfolk and Norfolk Community Health & Care. The stop smoking service will recruit 1400 participants between August 2011 and April 2013, and each participant will be in the study for one year. Supported Communication to Improve Participation in Rehabilitation of people with moderate-severe aphasia after a first stroke: a pilot study (SCIP-R) - 2010GC11 To examine the feasibility and provide initial evidence of clinical efficacy and value of a supported communication intervention for people with moderate-severe aphasia after a first stroke, in order to strengthen the design of a subsequent Phase III trial. Clinical efficacy of functional strength training for upper limb motor recovery early after stroke: neural correlates and prognostic indicators – FAST INDICATE– 2012GC11 Does functional strength training in addition to conventional physical therapy (FST+CPT) commenced early after stroke produce greater improvements in upper limb (arm and hand) motor recovery than CPT+CPT? T. Clinical efficacy of the Soft-Scotch Walking Initial Foot (SWIFT) cast on walking recovery early after stroke and the neuralbiomechanical correlates of response 2009MFE07 Revised Feb11 Does the use of a SWIFT CAST provided as an adjunct to Conventional Physical Therapy enhance walking recovery early after stroke more than CPT given alone? Keeping Children Safe at Home from Accidents – 2009PAED05 – Revised Nov09 To find out whether a range of safety behaviours, safety equipment use and home hazards affect the risk of falls, poisonings and scalds in children under five years of age. This is a national portfolio study which is being sponsored by NHS Norfolk, has been developed and will run in Norfolk Community Health & Care. 100 participants are hoped to be recruited across the two centres (the 2nd centre is in Cambridge), of which about half will be from NCH&C (Beech ward, Norwich Community Hospital). The Cambridge centre will be the control centre (standard care only), whereas NCH&C will be the experimental centre (standard care plus intervention). This is a national portfolio study which will be run at three sites in the UK and is looking for a total of 288 participants. Locally, this study will happen at Beech ward and in the Early Supported Discharge Team (ESD) in NCH, and the study team are looking for 5 recruits per month for 20 months (total of 96 participants in NCH). This is a national portfolio study which will be happening at Norfolk Community Health & Care (NCH&C) and the Norfolk and Norwich University Hospital (NNUH), as well as two sites in Scotland. There will be 120 participants in this study, with 60 coming from Norfolk sites and 60 from Scotland. Around 30 participants can be expected to be recruited from NCH&C hospitals, although there may be more if patients are discharged into NCH&C from NNUH. The results of this study will inform the need for a larger scale study. This is a national portfolio study consisting of one main study (study A), and three nested studies (Studies B, C and G). Nationally it is hoped to recruit 3794 case participants and 15176 control participants (4 controls per case) across four centres in the UK (Norfolk, Suffolk and Great Yarmouth & Waveney is classed as one centre). Norfolk Community Health and Care NHS Trust 3.10.6 Clinical Audit Plan 2012/13 69 30% 33% High 85 of the 143 (59%) audits on the audit plan were clinical audits. Of the 85 clinical audits proposed in 2012/13, 27 were completed in full (32%). The clinical audit plan subdivides audits by priority status aligning priority 1 and 2 to the Board Assurance Framework in terms of ‘risk’ and assigning priority 3 and 4 to locality based risk register priorities, and exact division of these responsibilities is demonstrated in the table below: Types of project Examples No. % of total clinical audits Priority 1 – Internal ‘must do’ audits NICE Technology Appraisals (TAs), Commissioning (eg, CQUIN audits), Internal service evaluation 12 44% Priority 2 – External ‘must do’ audits National Audits, National Service Frameworks 1 4% Priority 3 – Operational locality audits Service specific, baseline audits for business cases etc 8 30% Priority 4 – Clinical interest audits Clinical specialty audits (other than technology appraisals – TAs) 6 22% The completed clinical audits reports in line with the clinical audit policy recognise ‘high assurance’ as over 85% compliance, ‘moderate’ as between 60% – 84% compliance, and ‘low’ as below 59% compliance against clinical audit standards. Moderate Low 37% 30% gave high assurance, including: clinical record keeping/management, Essence of Care – bowel and bladder management, reducing avoidable death, disability and chronic ill health from Venousthromboembolism, administration of Beccal Midazalam and rectal diazepam, UNICEF Baby friendly initiative (stage 2), resuscitation (policy monitoring), service response times (Priscilla Bacon Lodge – Palliative Care). 37% gave moderate assurance, including, Community Intra-venous re-audit (west locality), re-audit to demonstrate attendance at multi-disciplinary team meetings (Priscilla Bacon Lodge), management of constipation, Methadone – to review adherence to service guidelines, attention deficit hyperactivity disorder (ADHD) management in the community, SystmOne record keeping in respect of child protection records (Safeguarding team), preferred place of death, timing of consultant review following inpatient admission to Priscilla Bacon Lodge (PBL). 33% gave low assurance, including, re-audit of pain management at Priscilla Bacon Lodge, cuffed tracheostomy care audit to assess if a training programme needs to be organized at Caroline House, auditing operational compliance with the National Institute for Health and Clinical Excellence (NICE) policy, auditing operational compliance with the Clinical Audit policy. 70 Quality Account 2012/13 4. Explanation of who has been involved and engaged with Norfolk LINk and Public involvement at Trust Board meetings and other committees, including Quality and Risk Assurance Committee, Patient Experience Steering Group and PEAT inspections. Development of the annual plan and quality goals by Executive Directors, Assistant Directors, heads of service and clinicians through workshops and management fora. Third party commentary received from Norfolk Healthwatch, Norfolk County Council Health Overview and Scrutiny Committee and South Norfolk Clinical Commissioning Group (our main commissioners) is presented below. 4.1 Comments from Norfolk Healthwatch (previously Norfolk LINk) Norfolk Healthwatch can confirm that it has reviewed the Quality Accounts for 2012-13. However, due to Norfolk Healthwatch only becoming operational from April 1, 2013 we do not believe it is appropriate for us to provide any detailed observations at this time but we will be working closely with Norfolk Community Health and Care NHS Trust and therefore will provide detailed and constructive comments on the Quality Accounts for 2013-14. 4.2 Comments from Norfolk Health Overview and Scrutiny Committee The Norfolk Health Overview and Scrutiny Committee has decided not to comment on any of the Norfolk provider Trusts’ Quality Accounts for 2012-13 and would like to stress that this should in no way be taken as a negative comment. Norfolk Community Health and Care NHS Trust 4.3 Comments from South Norfolk Clinical Commissioning Group Statement of Information Verification within the Quality Account submitted to South Norfolk Clinical Commissioning Group (SNCCG) by Norfolk Community Health & Care NHS Trust May 2013. South Norfolk Clinical Commissioning Group, as lead commissioner for the Trust, acknowledges Norfolk Community Health & Care NHS Trust in it’s publication of a Quality Account for 2012/13. We have reviewed the mandatory data elements required within this account and can confirm that those included are consistent with that known to SNCCG. The report presents detailed and comprehensive information relating to quality and safety of care delivered within the prioritised areas identified by the Trust. The quality goals for 2013/14 are relevant and are substantiated by involvement with the clinical quality and patient safety agenda via the Commissioning for Quality and Innovation payment framework (CQuIN). We commend staff for their work to improve outcomes within these areas and we look forward to the inclusion of an update on achievements in these areas in next year’s Quality Account. SNCCG have appreciated the continued support of the clinical quality review meetings which are vital in assuring the local population that services contracted from the Trust are safe and of good quality. They enable discussions to take place concerning new initiatives and current thinking and practice. They also facilitate challenges regarding current performance. 71 Work continues with the ambition of reducing avoidable pressure ulcers. This has been achieved in the inpatient setting in December 2012, with additional work on-going for the community settings. The Trust acknowledges the learning that arose from the review of the series of unexpected deaths in a community hospital. The Trust outlines where the learning has led to changes in organisational processes in order to assure that the failures described will not be repeated. This has been a year in which the Trust has demonstrated commitment to working with and building strong relationships with the five Norfolk CCG’s as well as Norfolk County Council as a part of the health and social care integration agenda. We look forward to working alongside our providers in supporting quality initiatives in the coming year. Yours sincerely, Ann Donkin Chief Officer South Norfolk Clinical Commissioning Group 72 Quality Account 2012/13 5.Declaration by all Directors The following is a declaration; signed by all directors in office at the date of the account, certifying that they believe the contents to be true, or a statement of explanation as to the reasons any such Director is unable or has refused to sign such a declaration. I believe the contents of this Quality Account 2012/13 to be true: Executive Directors Name: Michael Scott Designation: Chief Executive Name: Roy Clarke Designation: Director of Finance Name: Dr Rosalyn Proops Designation: Medical Director Name: Anna Morgan Designation: Director of Nursing, Quality and Operations Name: Paul Cracknell Designation: Director of Strategy and Transformation Name: Matt Colmer Designation: Director of Performance and Information Non-Executive Directors Name: Ken Applegate Designation: Chairman Name: James Ross Designation: Non-Executive Director Name: Alex Robinson Designation: Non-Executive Director Name: Vivienne Clifford-Jackson Designation: Non-Executive Director Name: Lisa Gamble Designation: Non-Executive Director Name: Neil Harrison Designation: Non-Executive Director Head Office: Elliot House, 130 Ber Street, Norwich NR1 3FR Online: www.norfolkcommunityhealthandcare.nhs.uk Telephone: 01603 697300