Quality Account 2010/2011 Looking after you locally
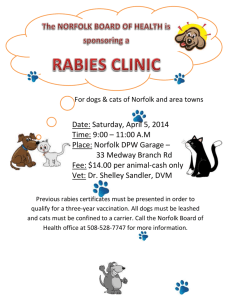
advertisement

Quality Account 2010/2011 Looking after you locally 2 Norfolk Community Health and Care NHS Trust Our Health Visitors see more than 1,000 new families every month We deliver health services to over 400 schools and colleges Our Community Nursing teams have around 108,000 face­to­face contacts with patients every month We have 3,000 We have around 300 members of dedicated NHS staff across the county patient beds in Norfolk NCH&C receives Our School Nurses hold 16,500 1,300 referrals from GPs and other healthcare professionals every month More than 3,000 patients per year are admitted to our community hospitals face­to­face appointments with children each year We deliver more than 70 different services in and around Norfolk Quality Account Norfolk Community Health and Care NHS Trust 3 Contents Part 1 Part 3 1.1 Statement on Quality 4 1.2 Our vision for the future 6 3.1 Review of Quality Achievements in 2010/2011 22 3.1.1 Valuing Our Staff 22 3.1.2 Clinical Leadership 23 8 3.1.3 Quality, Innovation, Productivity and Prevention (QIPP) 25 2.1.1 Quality Goals for 2011/2012 8 3.1.4 Performance Highlights 26 2.1.2 Commissioning for Quality and Innovation (CQuIN) 3.1.5 Patient Safety 30 12 3.1.6 Effectiveness of Care 34 2.1.3 Quality, Innovation, Productivity, Prevention (QIPP) 13 3.1.7 Patient Experience 39 2.1.4 Performance Monitoring 13 3.1.8 Commissioning for Quality and Innovation (CQuIN) 2010/2011 45 Part 2 2.1 2.2 Priorities for quality improvement (2011/2012) Statements of assurance from the Board 14 2.2.1 Review of services 14 2.2.2 Participation in clinical audits 15 2.2.3 Participation in clinical research 18 2.2.4 Goals agreed with commissioners 19 2.2.5 Statement from the Care Quality Commission 19 2.2.6 Statement on relevance of data quality and actions to improve 20 2.2.7 Information Governance Toolkit attainment levels 21 2.2.8 Clinical coding error rate 21 3.2 NCH&C Quality Account 2010/2011: Involvement and Engagement 3.2.1 Third Party Statements 46 46 The content of this Quality Account has been endorsed by the Trust Board and has taken into account feedback from our lead commissioners, and our local population via the representative organisations, LINks and the Health Overview and Scrutiny Committee. We trust that you will find our Quality Account informative and helpful in reviewing our progress against our key priorities for the forthcoming year. If you would like this publication in large print, Braille, alternative format or in a different language, please contact us on 01603 697300 and we will do our best to help. design: woolfdesigns.co.uk 4 Quality Account Norfolk Community Health and Care NHS Trust Statement on Quality Norfolk Community Health and Care NHS Trust (NCH&C) is a provider of generalist and specialist community health services. We have expert staff across a broad range of professional disciplines: district nursing, physiotherapy, occupational therapy, health visiting, medicine, dietetics, psychology, dentistry, speech and language therapy, school nursing, radiography, nursery nursing, specialist services for diabetes, palliative care, stroke, neuro­rehabilitation, respiratory care. We have reorganised our service delivery structure to focus on the delivery of pathway based on quality outcomes. It is the outstanding personal motivation of our staff, their expertise, their experience and their local knowledge, that is at the heart of our Community Foundation Trust application. We cover all of Norfolk, in a wide range of community settings, from over 200 locations. Our 3,000 staff cover a broad range of professional disciplines and have many years experience of working in our communities. We are therefore supremely well placed for supporting the care closer to home agenda, delivering service quality and productivity, in every setting. Our breadth of general community service provision, our experience of specialist service provision and care for vulnerable people, our track record of sustainable delivery and innovation, gives us a strong base for developing new services and in new geographies. 2010/11 has been another outstanding year for NCH&C, with excellent progress in improving quality outcomes, our Community Foundation Trust (CFT) application, significant developments in our service portfolio and organisational structure, and continued improvements in our financial and operational performance. The quality of services we offer our patients, as measured by the Ipsos MORI survey, continues to be of the very highest standard and has improved further, with 91% of patients rating our services as good/very good and over two­thirds of them giving us the highest score possible. This improvement in patient experience has been built upon increased involvement of patients in service delivery and redesign, strengthened clinical leadership and engagement, and robust quality and governance processes, as evidenced by our achieving NHS Litigation Authority level 1 compliance in March 2010. During 2010 the Trust was registered without conditions with the Care Quality Commission under NHS Norfolk, and received its own registration as an independent NHS Trust on 1 April 2011 (with one condition). Our commitment to clinical leadership is evidenced by our Executive Team having over 100 years’ of NHS clinical experience between them. We have strengthened this through the appointment of a Medical Director, who is a practicing GP and is the former Chair of NHS Norfolk’s Clinical Executive. Our management restructure included the identification of 12 key leadership posts and the formation of a Clinical Reference Group has strengthened clinical involvement in key decision­making, starting with the development of our Integrated Business Plan (IBP). We have embraced the Transforming Community Services pathway approach and are working on several pathways with other providers from the local health economy. The establishment of case managers to provide proactive management of the frail and elderly is a central pillar of both the local system Quality Innovation Productivity & Prevention (QIPP) plan and of our IBP. By combining quality, innovation, productivity and prevention as corner stones for the delivery of excellent quality services, we can ensure modern affordable healthcare for all our patients and service users. After successful pilots in North and Central Norfolk, we have Part 1 1.1 Statement on Quality secured funding for over 30 case managers across Norfolk and are close to reaching agreement with the remaining GP practices to complete the roll­out. These roles are critical for helping to reduce local acute activity and have been supported by the re­designation of 11 ‘step­up’ beds in North Norfolk. Other key service developments this year include: 1. Integrated Care Networks (ICN): We are participating in the largest ICN pilot in the country, involving 30 GP practices and a third of our Community Nursing & Therapy staff. The approach has been embraced by our staff and early indications are that the ICNs have reduced local acute admissions by up to 15% as the process becomes embedded. 2. Stroke Rehabilitation Service: The specialist stroke unit at Norwich Community Hospital was opened in early 2010, together with the establishment of an Early Supported Discharge team based within the local community. In its first year, this service has treated over 230 patients, with significant improvements in patients’ quality of life (a 25%, or 11 point, improvement in the Barthel score from admission to discharge) and in the proportion of patients who can continue to live at home. Acute length of stay has also reduced from 14 to eight days. 3. Tilney Ward: NCH&C worked in partnership with the Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust to establish a temporary ward to reduce acute hospital admissions over winter 2010/11. At the insistence of local GPs, the ward was co­staffed but was managed by NCH&C in recognition of our expertise in discharge co­ordination. In the first two months of operation over 250 patients were seen, with the average length of stay at 2.2 days. 5 Store items within seven days at 97.5%. There continue to be pressures around access to Wheelchair Services and Podiatric Surgery. We are working with NHS Norfolk to redesign these services and to address the system­wide issues that underlie underperformance. Improved access to diagnostics has been instrumental in reducing breaches significantly in Podiatric Surgery. Stretched public health targets, notably in Chlamydia Screening and Smoking Cessation have not been met, however, we will end the year with a slight increase in smoking quits, in the context of a significant reduction in expenditure on public health awareness. Continued improvement in those services that underperform against access or public health targets is a key element of our 2011/12 Annual Plan. We are proud to have achieved independent NHS Trust status on 1 November 2010. We are one of eight community services providers who are in the first wave of aspirant Community Foundation Trusts (CFTs). Our CFT programme has continued to maintain good progress against the timetable required for our Trust’s authorisation as a CFT within 2012. We also aim to improve the value given to the taxpayer and, to date, our financial performance has been robust, with a year end surplus £528,000. This has been as a result of tight financial management and controls. In addition to the achievement of mandatory and contractually agreed commissioning targets for access, patient safety and quality, we have taken significant steps in transforming our services. The information supporting the content of this Quality Account is, to my knowledge, accurate and was published by the Board on 30 June 2011. 4. Prisons: From October 2010, NCH&C has acted as the prime sub­contractor to Serco in the delivery of healthcare in three Norfolk prisons. We know we have further improvements to make. Access to our services continues to improve with delivery of 18 weeks Referral to Treatment at 98.3% year to date, and the delivery of Community Equipment Sheila Adams­O’Shea Chief Executive 6 Quality Account Norfolk Community Health and Care NHS Trust Our vision for the future We are part of Norfolk, and we know our community is changing. Our population is getting older and living longer. We want to continue to help keep local people healthy and living independent lives. To do this, we have identified four key strategic priorities for Norfolk Community Health and Care NHS Trust. More joined up personalised care We want to deliver services which are more joined up for all of our patients across Norfolk. Our personalised care approach will help to ensure that our patients and clients receive the care that is right for them, and that we help them to move seamlessly between our services, and other health and social care organisations. The right care close to home More and more people in Norfolk are living with long­ term conditions, like diabetes and heart disease. Our population of frail and elderly people is also growing. We want to help keep our patients well ­ providing care as early as possible, to help people avoid having to stay in an acute hospital and we will support people to return home as quickly and safely as possible. We know that for many people with long­term conditions, keeping well can be hard ­ having to attend regular appointments at hospitals many miles from home or travelling to receive the kind of rehabilitation needed. We believe that patients are better served within the community – having check­ups at clinics run at local GP surgeries or receiving physiotherapy at home. New services for our changing population As our population ages and more people are affected by illnesses caused by lifestyle choices (like obesity, smoking, alcohol or drug problems), the types of services needed by our community will change. We will develop new services, often in partnership with others, to meet these changing needs, from tackling childhood obesity to improving care for older people with dementia. Taking down borders We will continue to offer excellent services to our patients right across Norfolk, but we will also enable more people from outside of Norfolk to benefit from our expert community health and care. We will continue to build services in the towns and villages on the Norfolk border, so patients from neighbouring counties can choose to use our services. Part 1 1.2 Our vision for the future KEY Community Team 7 Community Hospital (includes rehabilitation, step up beds and outpatients) Specialist Rehabilitation & Specialist Palliative Care Wells-next-the-sea Sheringham Hunstanton Children’s Short Breaks and Child Development Units Sure Start and Children’s Centres Hard to Reach Prison Health Centres Cromer High Kelling North Walsham Aylsham Fakenham HMP Bure King’s Lynn Dereham Norwich Brundall Swaffham Acle Great Yarmouth Watton Downham Market Loddon Wymondham HMP Wayland Long Stratton Attleborough Thetford Diss We shall deliver our strategies through: 1 Delivering quality: effective clinical outcomes, providing the highest patient satisfaction in the region and delivering high standards of safety 2 Having the voice of patients, the public and staff at the centre of our organisation 3 Building our reputation: building membership, building GP satisfaction 4 Building sustainability: strengthening financial performance, delivering cost improvements, developing our estates and Information Management and Technology strategies 5 Building our organisation: strengthening clinical leadership and engagement, developing a more flexible workforce, building on our experience of a variety of partnership arrangements. We believe Community Foundation Trust status to be the optimum organisational form for delivering our strategy. Patient experience and outcomes will be improved through: the membership model ‘hard­wiring’ the voice of patients and staff; reinvesting surplus in service redesign; and being able to engage in a wider range of partnership models. A strong and independent community services provider is a catalyst for systemic change within the health economy. 8 Quality Account Norfolk Community Health and Care NHS Trust Priorities for quality improvement (2011/2012) At the heart of our first service development theme ­ ‘Strengthening the core’ ­ is the continual improvement of the quality of our services for patients. Improving quality is at the heart of our strategy and we are committed to sustaining what is already excellent, and making improvements to achieve consistently and sustainably high levels of quality across all areas of our service provision, with regard to patient safety, effectiveness of care and patient and carer experience. Quality Goals for 2011/2012 NCH&C’s Quality Improvement Strategy sets out how we will deliver continuous quality improvement and identifies key quality goals in conjunction with our Annual Plan 2011. In addition, we have negotiated a set of Commissioning for Quality and Innovation (CQuIN) Initiatives for 2011 and all of these improvements are identified under the following quality headings: Patient Safety – protecting people from harm Effectiveness of care – looking at variations in standards of care Patient experience – listening to what our service users think (Extract from Annual Plan 2011) Part 2 2.1 Priorities for quality improvement (2011/2012) 2.1.1 Quality Goals for 2011/2012 9 Patient safety & quality improvement Achieve Care Quality Commission (CQC) Registration without conditions Undertake rolling programme of CQC self­assessments at each location throughout 2011 Produce action plans for any non­compliant areas (monthly) Produce dashboard of results (monthly) Report results to Quality and Risk Assurance Committee (QRAC) (quarterly) Achieve Information Governance (IG) Toolkit level 2 IG Toolkit submission 31/3/11 action plans in place for all requirements which do not meet level 2 standard To reduce levels of pressure ulcers Ref: High Impact Actions (HIAC) 'your skin matters' Achieve 95% compliance for IG e­learning by 31/6/11 Develop policy for the prevention and treatment of pressure ulcers Progress towards level 2 NHS Litigation Authority (NHSLA) (by March 2012) Evaluation and decision on current assessment risk tools for pressure ulcer prevention Set up NHSLA Steering Group (reporting to QRAC quarterly) Implementation of the 'Safety Express' initiative in partnership with acute trusts ­ reviewing the patient pathway and tissue viability and sharing information Review of level 1 requirements Implementation of level 2 standards (monitored by NHSLA Steering Group) To reduce levels of falls resulting in serious harm Q1 – Collect baseline data (2010/11 and Q1 2011/12) and develop action plan Q2 – Implementation of an action plan identified from the Patient Safety First guidance due in Q2 and continue to monitor falls data Q3 – Implement actions due in Q3 and continue to monitor falls data. Revise action plan in November, adding additional actions where necessary Q4 ­ Implement actions due in Q4 and produce report showing comparison of falls data by quarters during 2011/12 10 Quality Account Norfolk Community Health and Care NHS Trust To reduce levels of attributable Clostridium Difficile (C.diff) To reduce levels of medication errors (CQuIN indicator 4) Implement the key recommendation of the NHS Norfolk working group, to change the timeframe of specimen testing Development and implementation of a plan to put in place the actions described in National Patient Safety Agency (NPSA) RRR 009 and reduce harm from omitted and delayed medicines in hospital Staff training is being reviewed and updated in light of the above recommendation More timely specimen testing of newly admitted patients (within 48 hours) To reduce levels of MRSA bacteraemia Implementation of a decolonisation team Proactive treatment of high risk patients within our community caseloads IT alerts placed on any new MRSA isolates (PAS, ICNet) including those in primary care SystmOne local marker for MRSA to be developed Q1 ­ Analysis of Q4 2010/11 incidents relating to missed, omitted, or duplicated medicines or issues in obtaining or supplying medicines in community hospitals to determine the baseline numbers and trends of root causes for previous incidents. Point prevalence audit of the charts in community hospitals to highlight the current issues. Each unit to have all charts present at the time of the audit, assessed using the audit tool. All units to be audited once during the defined week within the quarter. Development of an action plan to put measures in place to reduce the risks due to omitted and delayed medicines Q2 ­ Development of a list of critical medicines, specific to our Trust. Review systems for supplying critical medicines and procedures and guidance for staff who are prescribing, ordering or administering medicines Q3 – Instruct staff on above procedures and systems for supplying critical medicines, including standardisation of prescription charts and other related medicines management paperwork Q4 ­ Review of incident reports in January and February 2012 and re­point prevalence audit of practice Part 2 2.1 Priorities for quality improvement (2011/2012) 2.1.1 Quality Goals for 2011/2012 Patient and carer experience and effectiveness Establishment of a monthly Patient Experience Tracker (PET) Including delivery of CQuIN indicator 5 Patient Experience Procurement of PET tools Staff training and communication Implementation of PET tools Monthly reporting internally Quarterly reporting to NHS Norfolk for CQuIN Implementation of action plans by service leads Delivery of CQuIN indicator 7 Carer satisfaction Implementation of Health Feedback questionnaires Quarterly reporting to NHS Norfolk for CQuIN Implementation of action plans by service leads Patient Experience ­ improve four Ipsos MORI areas < 50% Action plans to be completed by each service pathway Implementation of action plans by service leads 11 12 Quality Account Norfolk Community Health and Care NHS Trust Commissioning for Quality and Innovation (CQuIN) CQuIN requires primary care trusts to improve quality and innovation by discussing, agreeing and monitoring quality indicators with its providers. A CQuIN scheme is the locally agreed package of quality improvement goals and indicators which, if achieved in their totality, enables the provider to earn its full CQuIN payment ­ a quality based payment. A CQuIN scheme should address the three pillars of quality: safety, effectiveness and patient experience; while also reflecting innovation. Indicators need to be realistic to ensure that a provider can reasonably set out to earn the allocated money. The monies to meet the cost of this payment will come from incentivising a proportion of annual contract values (1.5% for 2010/2011 and 1.5% for 2011/2012). The indicators set out in the table below have been agreed and set within the contract as part of the established quality schedule and monitored through the CQuIN Steering Group. Patient CQuIN indicator description Increase number of patients provided with assistive technology (Telehealth) in the community and audit outcomes To improve the care and access to palliative care services within our community hospitals through improved awareness and adherence to Gold Standard Framework To analyse the rationale for admitting patients to the local acute trust (Norfolk and Norwich Hospitals NHS Foundation Trust and Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust) who then die within four days Implementation of a medicines management action plan to reduce harm from omitted and delayed medicines in community hospitals To improve Patient Experience in Adult Services by focusing on orthopaedic triage, musculoskeletal physiotherapy, podiatry and biomechanics To improve Patient Experience in Children’s Services by focusing on outpatient appointments held at Upton Road Children’s Centre Improve outcomes for patients in inpatient units by the reduction of falls, to meet or be below the National Patient Safety Agency level of 8.4 falls per 1,000 occupied bed days (OBD) Improve Carer Experience within community Adult Services by interaction of Case Managers Improve Carer Experience within the Children’s Short Breaks service (residential units ­ Squirrels and Little Acorns) Achieve UNICEF accreditation stage 1 and commence stage 2 Experience Patient Safety Effectiveness Part 2 2.1 Priorities for quality improvement (2011/2012) 2.1.2 Commissioning for Quality and Innovation (CQuIN) 2.1.3 Quality, Innovation, Productivity, Prevention (QIPP) 2.1.4 Performance Monitoring Quality, Innovation, Productivity, Prevention (QIPP) NHS Norfolk has recently established three system­wide QIPP work streams. The intention is that NCH&C’s QIPP Steering Group members will be invited to attend and contribute to workshops over the coming months. As this work progresses we will share the key outputs and any actions we need to develop. Frail Elderly Focus – central and west Norfolk • Single Point of Access – Online vision of all available services, telephone triage offering clinical and pathway advice, clinical responsibility handover, directory of services 13 Performance Monitoring During 2011/12, we will bring together data on several areas of organisational performance to create one integrated performance report. Not only will it include information on waiting times and service productivity, it will also incorporate a range of quality and safety indicators in a dashboard format, supported by a commentary and what actions will be required to address adverse performance. The dashboard will include data against three key quality domains: patient safety, clinical effectiveness and patient experience. The indicators reported on will include: • Complaints, and how quickly we respond to them • Adverse incidents, such as medication errors and pressure ulcers • Serious Incidents Requiring Investigation (SIRIs), and how quickly we investigate and report on them • Reshaping Out of Hospital Care – Management of the frail elderly, assistive technology and diagnostics, end of life care, access to beds, integrated support teams, acute outreach. Dementia care, case management and long term conditions management • Health Care Associated Infection rates • Discharge – Early planning, primary care/integrated team as holder of case, staff rotation, timeliness We will report on this data monthly, to ensure we identify trends over time and take any action necessary to address adverse performance. • Use of technology to help manage patients’ conditions within their own home, improving rehabilitation, and empowering patients Whole Norfolk system – Referral Management and Pathway Development • Referral management and pathway development – developing objective criteria planned for referrals, use of email/Telemed, delivering consistency in quality and reducing unnecessary appointments • Integrated diagnostics; 24/7 electrocardiogram (ECG) • Thresholds – consistent thresholds, de­commissioning • Patient satisfaction levels • Number of ‘never events’ – incidents that can cause significant harm, including death of patient 14 Quality Account Norfolk Community Health and Care NHS Trust Statements of assurance from the Board Review of services During April 2010 ­ March 2011 NCH&C provided and/or sub­contracted 74 services of which around 95% are commissioned by our three main commissioners, NHS Norfolk, NHS Great Yarmouth & Waveney and NHS Suffolk. These include; Learning Disabilities; Prison Healthcare and the Stroke Rehabilitation Service. The income generated by NHS services reviewed during April 2010 ­ March 2011 represents 95% of the total income generated from the provision of NHS services by NCH&C for 2010­2011. NCH&C undertakes an extremely rigorous review of the data available on the quality of care in our NHS services via the monthly contract and clinical quality review meetings with our commissioners. We have also developed a ‘balance scorecard’ through which we can give assurance to the Trust Board, our regulators and commissioners, patients and the public, that we are on track for realising our vision. Our scorecard includes short term targets for years one and two of our five­year plan, and stretching targets for year five. It reflects the following elements: 1 Compliance 2 Quality for patients (safety, effectiveness, experience) 3 Staff 4 GP commissioning 5 Finance In addition to the review of data by the Trust Board, each Non­Executive Director (NED) has been allocated a ‘locality’ area ­ north, south, west, Norwich and central Norfolk ­ which provides an opportunity for them to talk to frontline staff, patients and relatives and gain further insight into the quality of our services. Kelling Hospital North Walsham Community Hospital St Michael’s Hospital Aylsham St James Clinic Kings Lynn Swaffham Community Hospital Dereham Hospital Norwich Community Hospital Ogden Court Community Hospital Wymondham Key Central North South West Various leadership roles have been identified for each of the NEDs, such as safeguarding adults and children; infection control, patient­related issues, and serious incidents. These provide an opportunity for our NEDs to gain experience of our operational services, across the county. Part 2 2.2 Statements of assurance from the Board 2.2.1 Review of services 2.2.2 Participation in clinical audits 15 Participation in clinical audits During April 2010 ­ March 2011, five national clinical audits and one confidential enquiry covered NHS services that NCH&C provides. During that period NCH&C participated in 60% of national clinical audits and 50% national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that NCH&C was eligible to participate in during April 2010 – March 2011 are as follows: National Clinical Audits Audit Lead organisation Participation from NCH&C National Childhood Epilepsy Audit Royal College of Paediatricians and Child Health (RCPH) Yes Diabetes (National Adult Diabetes Audit) National Clinical Audit Support Programme No Parkinson’s Disease (National Parkinson’s Audit) Parkinson’s UK No Falls and non­hip fractures (Falls and Bone Health Audit) Royal College of Physicians Yes Depression and anxiety (National Audit of Psychological Therapies) Royal College of Psychiatrists Yes 16 Quality Account Norfolk Community Health and Care NHS Trust National Confidential Enquiries Title Applicable to NCH&C Participation from NCH&C National Confidential Enquiry into Patient Outcome and Death (NCEPOD) Yes Yes Confidential Enquiry into Maternal and Child Health (CMACH) Yes (in part) No National Confidential Inquiry (NCI) into Suicide and Homicide by people with mental illness No No National Clinical Audits The national clinical audits and national confidential enquiries that NCH&C participated in, and for which data collection was completed during April 2010 – March 2011, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Name Lead organisation Percentage National Childhood Epilepsy Audit Royal College of Paediatricians and Child Health (RCPH) Data collection ongoing (January 2011 – May 2011) Falls and non­hip fractures (Falls and Bone Health Audit) Royal College of Physicians Organisational Audit – 100% Patient Sample Audit – 95% Overall average – 98% Depression and anxiety (National Audit of Psychological Therapies) Royal College of Psychiatrists ‘Service Context’ (Questionnaire 1) – 100% ‘Therapist’ (Questionnaire 2) – 100% ‘Retrospective patient audit’ (Questionnaire 3) – 100% ‘Service Users Survey (Questionnaire 4) – 2% Overall average – 76% National Confidential Enquiry into Patient Outcome and Death (NCEPOD) Cardiac Arrest Procedures NCEPOD No cases occurred during audit two­week period – therefore no data to submit Part 2 2.2 Statements of assurance from the Board 2.2.2 Participation in clinical audits 17 The report of one national clinical audit (Falls and Bone Health Audit) was reviewed by the provider during April 2010 – March 2011 and NCH&C intends to take the following actions to improve the quality of healthcare provided: • All NCH&C Community Falls Teams will provide relevant exercise programmes to patients within their own home • Identify ‘non­conveyed’ fallers with the development of the Ambulance Service pathway which will link into the community teams • NCH&C is to develop a Falls Accident and Emergency Pathway for the Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust. This model is to be standardised with the Norfolk and Norwich University Hospitals NHS Foundation Trust to ensure appropriate referral into NCH&C teams • Use of screening tool, standardised across the county, to define patients at high risk of falling to ensure these patients are referred to the correct clinician or agency • Introduction of a standard assessment tool which is tailored to the individual • Ensure that all patients seen by the NCH&C Falls Prevention Service receive written copies of their agreed action plans to help prevent falls • All NCH&C Community Falls Teams will carry out fracture screening using an agreed tool and process, and will implement health education and lifestyle advice for the patient with onward referral as appropriate • Ensure public representation on the Falls Steering Group. Falls documentation is to include patient satisfaction surveys to evaluate the service • The National Patient Safety Alerts (NPSA) ‘Slips, trips and falls’ documentation will be used as a reference tool to achieve a clear screening and care plan for our community hospitals. Standardised tools (including bone health screening) will be used within all of our community hospitals • Community services will work closely with primary and secondary prevention strategies for falls and bone health, in order to provide a continuous provision of service for patients • All high fracture risk patients will be referred to their GP for either primary or secondary osteoporosis treatment • All NCH&C Community Falls Teams will continue to visit patients in care homes Local clinical audits The reports of 11 local clinical audits were reviewed by NCH&C during April 2010 ­ March 2011 and the Trust intends to take the following actions to improve the quality of healthcare provided: • Training on record keeping to be provided to staff • A review of the Prison Healthcare Discharge Policy to be undertaken and a discharge checklist to be created • Documenting outcome measures within Specialist Rehabilitation and taking part in the UK Rehabilitation Outcomes collaborative data collection which will help us to see the cost benefits of rehabilitation • To ensure our medical and nursing staff are fully aware of, and engaged with, medicines reconciliation process • To explore options for greater pharmacy support 18 Quality Account Norfolk Community Health and Care NHS Trust Participation in clinical research The number of patients receiving NHS services provided or sub­contracted by Norfolk Community Health and Care NHS Trust (NCH&C) in 2010/11 that were recruited during that period to participate in research approved by a research ethics committee, was 289. Participation in clinical research demonstrates NCH&C’s commitment to improving the quality of care we offer and to making our contribution to wider health improvement. Our clinical staff stay abreast of the latest possible treatment possibilities and active participation in research leads to successful patient outcomes. We were involved in conducting 48 research studies during 2010/11, of which 22 were new projects which were given permission to start in 2009/10. The National Institute for Health Research (NIHR) supported 59% of these studies through its research networks, the majority of non­supported studies being student research, which is not eligible for adoption onto the national portfolio. In conjunction with the Comprehensive Local Research Network (CLRN) and Primary Care Research Network (PCRN) we have developed a research support scheme known as the Research Site Initiative Scheme to encourage hosting of research in specified clinical areas. This scheme aims to increase the capacity of our staff to host portfolio studies alongside delivery of care, in order to improve the health of our patients through the delivery of innovative, high quality care. There were 18 clinical staff participating in research (as participants) approved by a research ethics committee at NCH&C during 2010/11. Over the 2010/11 period NCH&C conducted clinical research studies within a number of different healthcare specialties. However, none of these studies map to medical specialties where mortality rate data is available and therefore it is not possible to show any differences in the healthcare/mortality rate from causes preventable in the specialty compared with the 2009/10 reporting period. Within the last year we have been successful collaborators in three NIHR funded projects, including one Health Technology Assessment (HTA) and two ‘Research for Patient Benefit’ (RfPB) projects. We have been awarded five research bursaries through NHS Norfolk to enable our staff to develop their research ideas, with academic partners, into successful funding applications. During 2010/11 NCH&C has not recorded any publications that have arisen as a result of our involvement in NIHR research. We plan to continue to collect such information from the current financial year and onwards and will be able to report on this activity for 2011/12. Part 2 2.2 Statements of assurance from the Board 2.2.3 Participation in clinical research 2.2.4 Goals agreed with commissioners 2.2.5 Statement from Care Quality Commission (CQC) Goals agreed with commissioners Statement from the Care Quality Commission Use of the Commissioning for Quality and Innovation (CQuIN) payment framework NCH&C is required to register with the Care Quality Commission (CQC) and its current registration status is registered with a condition. NCH&C has the following condition on registration: A proportion of NCH&C’s income during April 2010 ­ March 2011 was conditional on achieving quality improvement and innovation goals agreed between NCH&C and any person or body they entered into a contract, agreement or arrangement for the provision of NHS services, through the CQuIN payment framework. Further details of the agreed goals for April 2010 ­ March 2011 are set out in Part 3 of the Quality Account and for the following 12­month period can be found in Part 2.1. 19 The Registered Provider must ensure that the regulated activity of “Accommodation for people who require nursing or personal care” is managed by an individual who is registered as a manager in respect of the activities at or from all locations. This condition has been imposed as the CQC see this regulated activity as having a social care aspect and therefore requires a Registered Manager situated at each of our three Children’s Short Break locations. NCH&C is currently working towards having this condition removed. The CQC did not take enforcement action against NCH&C during April 2010 ­ March 2011. The CQC conducted an unannounced inspection on 27 July 2010 to assess whether NCH&C is adequately protecting patients, workers and others from Healthcare Associated Infections (HCAI). The overall judgement of inspection stated; ‘We found no cause for concern regarding the provider's compliance with the regulation on cleanliness and infection control’. This response supports the ongoing work that is being undertaken with all levels of staff. There were no actions required to be taken. 20 Quality Account Norfolk Community Health and Care NHS Trust Statement on relevance of data quality and actions to improve NCH&C will be taking the following actions to improve data quality: It has established a Data Quality Forum chaired by the Assistant Director of Performance. The purpose of this forum, which meets bi­monthly, is: • To assist NCH&C to work to a common set of principles around data quality issues • To share experience, ideas and examples of good practice in business units and corporate functions in taking forward the data quality agenda • To assist NCH&C in the delivery of the data quality agenda in support of key national initiatives, eg. Transforming Community Services Quality Indicators, Patient Safety, QIPP, and the NHS Outcomes Framework • To action collectively­agreed data quality initiatives • To assist business units and corporate functions in raising the profile of data quality at a local level and making the links with the wider agenda outlined above • To provide a forum for coordination of user issues, support arrangements and developments for data quality reporting • To review, where available, local and national benchmarking resources to identify any issues of data quality, and consider any necessary actions • To review the Data Quality Dashboard against local benchmarks and targets as defined in the Data Quality Improvement Plan, and to monitor trends over time in order to assess progress in improving data quality The Forum is action­oriented in order to effect improvements in data quality. This ensures that when decisions are made, it is clear what tasks are required by Forum members or other staff. This ensures responsibility is appropriately assigned and that achievements can be followed up and monitored to improve data quality. Data quality reports have been designed to monitor a range of key performance indicators on a monthly basis, and the Secondary Uses Service (SUS) dashboards are reviewed regularly in relation to key national indicators. NHS Number and General Medical Practice Code Validity NCH&C submitted records during April ­ October 2010 to the SUS for inclusion in the Hospital Episode Statistics which are included in the latest published data under organisation code 5PQ. The percentage of records in the published data which: • Included the patient’s valid NHS number was: 100% for admitted patient care 100% for outpatient care • Included the patient’s valid General Medical Practice code was: 100% for admitted patient care 100% for outpatient care Following separation from NHS Norfolk and our establishment as an independent NHS Trust, NCH&C submitted records during November 2010 ­ March 2011 to the SUS for inclusion in the Hospital Episode Statistics which are included in the latest published data under organisation code RY3. The percentage of records in the published data which: • Included the patient’s valid NHS number was: 100% for admitted patient care 100% for outpatient care • Included the patient’s valid General Medical Practice code was: 100% for admitted patient care 100% for outpatient care Part 2 2.2 Statements of assurance from the Board 2.2.6 Data quality 2.2.7 Information Governance Toolkit attainment levels 2.2.8 Clinical coding error rate 21 Information Governance Toolkit attainment levels There are robust action plans in place which aim to achieve level 2 compliance of all criteria by the end of June 2011. The Trust declared compliance at level 2 against each of the 21 key requirements, although the 95% training target was not achieved at the time of submission of information to this Quality Account. However, an action plan to achieve compliance by June 2011 was in place to ensure compliance could be declared. Using the NHS Connecting for Health submission scoring, this represented an overall score for April 2010 ­ March 2011 of 63% out of a possible 66% against level 2 requirements. Of the remaining 20 standards, 15 were declared at level 2, with four declared at level 1. Prior to submission, discussion with the support team enabled an exemption to be applied to one of the standards. The four criteria declared at level 1 were: 1 8­309 Business Continuity planning 2 8­324 Pseudonymisation of data 3 8­406 Monitoring the availability and tracing of paper records 4 8­501 National data definitions incorporated into key systems For further information, the Information Governance Toolkit is available on the Connecting for Health website: www.igt.connectingforhealth.nhs.uk Clinical coding error rate NCH&C was not subject to the Payment by Results clinical coding audit during 2010/11 by the Audit Commission. 22 Quality Account Norfolk Community Health and Care NHS Trust Review of Quality Achievements in 2010/2011 It is important to recognise the role that every member of staff plays in order for us to succeed in continuing to provide care high­quality care to our patients. The hard work of our colleagues means we are able to build upon previous successes and offer local people further improved health and care services. Valuing Our Staff NCH&C’s Chief Executive, Sheila Adams­O’Shea recently thanked staff for their ongoing commitment to the development of our Trust and for continuing to deliver excellent services to the people of Norfolk. She said: “I am confident that our Trust will further develop over the coming year and continue to offer patients excellent services, particularly as we have such an array of people with talent, skill and commitment to patient care at all levels of NCH&C. This was especially evident at the recent REACH for the Stars staff awards, which recognised staff members who have especially improved patient care, delivered the highest standards and inspired colleagues. “It was a wonderful event at which I was proud to share in the comments made by patients about the care they have received, as well as colleagues who witnessed the excellent work being delivered by people across our Trust.” Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.1 Valuing Our Staff 3.1.2 Clinical Leadership 23 Clinical Leadership NCH&C’s clinical leadership was promoted in a national journal ­ The Nursing Standard in December 2010. The Trust’s development towards CFT status has been used as an example of both good progress and robust clinical leadership. Mrs Adams­O’Shea said: “Clinicians are at the heart of what our Trust does... when we are developing strategies or considering business opportunities, our clinical leaders work with senior managers to drive it forward.” NCH&C’s Clinical Strategy provides our clinical staff with a clear picture as to how they can ensure continuous quality improvement and innovation in clinical care for our patients and their carers. This can be evidenced by a number of key initiatives and projects which have been undertaken during 2010­11, such as: Norfolk’s Key Worker service for children with disabilities and their families celebrated its first anniversary in September 2010. The Family Nurse Partnership (FNP) scheme which offers support to young, first­time mothers and their babies. The project received praise from the Department of Health (DoH) following its first successful year. Providing support to soon­to­be mums, under the age of 18, from early pregnancy all the way through until their child is two years old, the project aims to improve the health and wellbeing of both parents and babies. Launched in January 2010, the team has already helped over 100 families, reduced the rates of smoking during pregnancy and increased breastfeeding rates. The scheme aims to help and support parents and carers, who often find it overwhelming, confusing or frustrating to deal with the many agencies and individuals necessary to their child’s care and development. “Often the family of a disabled child will deal with a whole range of professionals,” explains Clare Draper, NCH&C’s Key Worker Coordinator. “But they may not be getting all the assistance that’s available, or there may be lots of duplication in terms of filling in forms, arranging appointments or attending meetings. Key Workers help to reduce the number of times families have to ‘tell their story’ to different organisations and provide a link to a whole range of services, making sure they get all the help they need.” 24 Quality Account Norfolk Community Health and Care NHS Trust A ‘trip’ aboard the NCH&C Health Bus In February 2011 NCH&C invited people to hop aboard the big, red double­decker bus to meet healthcare professionals and receive a wealth of advice to improve their quality of life. Aboard the bus people were able to get advice on cervical cancer (HPV) immunisations from an NCH&C school nurse, or to pick up a discreet Chlamydia Screening test pack. People were also able to undertake a simple lung health check with the How Big Are Your Breaths Roadshow Team from NCH&C’s Respiratory Triage Service. The team aims to identify people who are at risk of developing Chronic Obstructive Pulmonary Disease (COPD), a condition commonly associated with smoking, the progression of which can be slowed down by early diagnosis. The NCH&C Smokefree Norfolk team was also on board. The team helped around 2,287 local people quit smoking last year. Department of Health selected our Health Visitors to lead rollout of new­look service NCH&C’s Health Visitor Service was granted ‘Early Implementer’ status by the Department of Health to begin rolling out a redesigned service to Norfolk families. The decision means our health visitors will be one of just 20 services nationally ­ and one of only two in the East of England ­ to start delivering a new­look health visitor service before March 2012. As an Early Implementer, NCH&C’s Health Visitor Service will begin delivering a newly designed service this year – while the national roll out will run until 2015. The new programme will ensure that all families are offered a programme of health and care services to help meet the needs of both the parents/foster parents and their children, with additional care and support for those who especially need it. Families and children will benefit from health visitors providing joined up care in partnership with their colleagues in Sure Start Children’s Centres and GP practices to offer an even more personalised service. There will also be a significant recruitment drive to further increase the number of NCH&C health visitors. In Norfolk, it is expected that over 50 additional health visitors could be recruited by 2015 – an increase of around 50% on existing team numbers. Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.2 Clinical Leadership 3.1.3 Quality, Innovation, Productivity, Prevention (QIPP) Quality, Innovation, Productivity and Prevention (QIPP) NCH&C are delivering across the Quality, Innovation, Productivity and Prevention agenda (QIPP). Among our our recent operational and service achievements are: Quality Tree Tops Day Nursery – Our nursery in Thetford received an ‘outstanding’ report from Ofsted inspectors in September 2010, placing it within the top four per cent of educational settings in the UK. Our staff took over its management just two years before, and raised the quality of provision from ‘satisfactory’ to ‘outstanding’ in a short space of time. End of Life Care – We have become a member of the national Dying Matters Coalition, which aims to make ‘dying well’ a natural part of a good life. One of the primary providers of integrated specialist palliative care services in the country, we also provide a quality service to the prison population through our innovative prison palliative care service. Innovation Integrated Care Organisation pilots – This project is a joint initiative between NCH&C, Norfolk County Council Adult Social Services Department, 30 GP practices and NHS Norfolk to develop more integrated services for the community. It is the largest pilot in England. Our objective has been to establish a series of fully integrated, joined up care pathways, through GP­based health and social care teams across Norfolk. The teams comprise GPs, community health staff and adult social care staff and provide cohesive, proactive and personalised care for older and vulnerable people, transcending the traditional boundaries between the organisations involved. 25 Specialist Stroke Rehabilitation Unit – NHS Norfolk commissioned an £8m purpose­built specialist stroke rehabilitation unit, at Norwich Community Hospital. Services are provided via a partnership project between NCH&C and the Norfolk and Norwich University Hospitals NHS Foundation Trust (NNUH). NNUH subcontracts our Trust to provide services within this new unit. This represents significant partnership working with an acute trust for the benefit of local people. Productivity Releasing Time to Care – Our Productive Community Ward project has improved relationships between staff and patients, and has improved patient experience. A patient at our specialist palliative care rehabilitation centre commented: “You are given respect and dignity, and you are involved in all of the choices around your care.” Better care for patients over winter – Thanks to more joined up working between health and care services, hundreds of patients avoided unnecessary delays over the winter of 2009­10. This improved patient experience, relieved pressure on acute services and reduced costs and waste across the system. There was a 75% reduction in the number of patients experiencing delays in discharge over winter 2009­10. Prevention Kicking the habit – Our Smokefree Norfolk team continues to lead thousands of local people to kick the habit. Team Leader, Katie McGoldrick was recently crowned ‘Stop Smoking Advisor of the Decade’ at the East of England’s 10th anniversary Stop Smoking Awards. Helping more than 1,200 smokers kick the habit, 85% of the people she sees quit the habit for good. Reducing cancer – Our children’s immunisation team surpassed national averages for delivering human papillomavirus (HPV) vaccinations among school girls and young women in 2010. This will protect thousands of women from developing cervical cancer later in life. 26 Quality Account Norfolk Community Health and Care NHS Trust Performance Highlights Infection Prevention and Control Infection control rates remain good with no reported cases of C.diff during March 2011, nor have there been any reported cases of MRSA bacteraemias since June 2010. We had nine reported cases of C.diff during 2010­ 11 against a contractually agreed ceiling of 10 cases. Compared to previous years’ infection control rates, 2010­11 saw the lowest level of C.diff and MRSA occurrences within our patients ­ a testament to the hard work of staff in adhering to strict infection control measures. The ceilings for C.diff and MRSA bacteraemias for 2011­12 is nine cases and one case, respectively. Community Equipment Store (CES) The response times for the delivery of equipment by the Community Equipment Store (CES) continues to exceed the NHS East of England (EoE) target of 95%. Throughout 2010/11, the CES delivered 21,490 items to patients needing equipment, with just 2.3% being delivered seven days after the referral was received. This ensured that the vast majority of our patients were not kept waiting unnecessarily. 18 weeks Referral­to­Treatment (RTT) Most services provided by NCH&C are now compliant with, or close to achieving a maximum wait of 18­weeks from referral­to­treatment (RTT). We have seen particular improvements within our Adult Speech and Language Therapy service, musculoskeletal physiotherapy and Continence Management. All services within our Children’s Services have achieved 18­week wait compliance and of the services which are subject to an 18­week wait pathway, they treated or assessed nearly 5,300 patients. Of these patients, just 22 patients had to wait in excess of 18 weeks, excluding those breached due to patient choice and clinical reasons to delay treatment. Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.4 Performance Highlights Performance tables The following tables show a number of indicators common to community organisations, which are monitored by NCH&C and NHS East of England. These form part of the Provider Management Regime (PMR) to which NCH&C is subject, and a number of these indicators are closely monitored by NHS Norfolk as part of the community services contract. These have been split into separate tables to indicate where NCH&C is achieving its targets, where it is approaching its ceiling/at risk of missing a target, and where we are missing targets. 27 Several indicators reported to NHS East of England have been performing consistently above the required level of performance, and have therefore been removed to make way for three further indicators from Children’s Services, highlighted as ‘New’ in the performance tables ­ breastfeeding, smoking cessation in pregnancy and new birth visits. All three areas are performing above expected levels, which demonstrates the high quality of service that expectant and new mothers in Norfolk are receiving from our staff. Title Indicator Target or upper ceiling March performance Recent trend Year to date performance C.diff No more than 10 cases during 2010/11 0 cases 9 cases year­to­date MRSA bacteraemia No more than one case during 2010/11 0 cases 1 case year­to­date MRSA Screening ­ elective patients 100% of all patients having planned surgery to be screened 100% 100% Delayed transfers of care No more than 6% of beds occupied by patients whose discharge is delayed for non­medical reasons 4.3% 3.6% Community Equipment Store (CES) response within seven days 95% delivered within seven days of receipt of a referral 99.7% 97.7% Breastfeeding success rates NEW Minimum of 21% of new mothers to be fully breastfeeding at six weeks 32.40% 32.96% Health Visiting NEW 95% or more of mothers receiving a New Birth Visit within 28 days of delivering 98.45% 97.74% Smoking cessation in pregnancy NEW 23% or more of women who gave up smoking during pregnancy 35.71% 25.62% 28 Quality Account Norfolk Community Health and Care NHS Trust At risk of breaching target – to end March 2011 Indicator Target or upper ceiling March performance 18­week wait referral to treatment 100% patients receiving definitive treatment within 18 weeks of referral * 97.2% Recent trend Year to date performance 96.7% * 18­week wait key: Green: 100%, Amber: 95­99.9%, Red: Below 95% Target Breach Assurance Below is a list of services which were breaching the 18­week wait target at end of March 2011, with action plans for improvement. For comparison purposes, performance rates from the previous month (February 2011) are also listed in brackets: from 98.0%) Biomechanics – 96.2% ( During 2010/2011, the average 18­week compliance for this service was around 97%. Plans were drawn up to ensure there were no breaches at the end of March, but due to staff sickness these plans could not be fully implemented. Consequently, new steps, such as recruiting more technicians and introducing patient tracking, have now been brought in. from 97.9%) Podiatric Surgery – 69% ( Following significant improvements over the last few months which have seen an improvement in compliance, waiting times are currently increasing due to a backlog of outpatient work which has impacted on waits for first appointments. However, actions are in place to reduce backlog, including recruitment to a vacant post. Wheelchairs – 92% ( from 97.6%) A slight fall in compliance which is partly due to problems with suppliers delivering necessary items. Overall, the service continues to show improvements in compliance compared to previous months. Pulmonary Rehabilitation – 81.5% ( from 86.4%) Changes to the way patients are managed are to be implemented in coming weeks. The service delivery model has previously meant that patients had to wait over eight weeks for the next group if there was more demand than capacity. However, the new model will see a rolling programme brought in with increased capacity, which should enable a reduction in backlog. Continence Management – 99.2% ( from 99.9%) Musculoskeletal Physiotherapy – 99.7% ( from 99.9%) Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.4 Performance Highlights 29 Missing target – to end March 2011 Indicator Target or upper ceiling March performance Recent trend Year to date performance Successful four­week smoking quitters Performance against the contractual trajectory of 2,610 successful quits during 2010/11* 211 2287 Chlamydia Screening Performance against the contractual trajectory of 1,500 successful screens during 2010/11** 51 581 *NCH&C agreed a ‘stretch’ target of 3,557 quits for 2010­11 as part of a Norfolk­wide quit target **We agreed a stretch target of 3,000 in 2010­11 for Chlamydia Screening Target Breach Assurance Smoking ­ Despite strong performance for much of the year, and a new management structure being put in place, the Smokefree Norfolk team was below its contractual trajectory agreed with NHS Norfolk to the end of March 2011. Despite this, the service has raised its profile through various local events and was able to generate an increased number of referrals from our own services, helping 2,287 people give up smoking by end of March. The service is expecting more successful quits to be recorded (June 2011 data release) for the 2010­11 contractual year, following national No Smoking Day events, which traditionally increases quit rates. Chlamydia ­ NCH&C performed 51 successful chlamydia screens in March for young people aged 16­24 years of age. For the whole year the Trust has achieved nearly 600 screens, more than double the number of screens undertaken last year. This is a clear reflection of all the hard work by the Chlamydia Screening Project Team and our staff in getting young people to accept the offer of a screening kit. Quality Account Norfolk Community Health and Care NHS Trust Patient Safety 2010-11 NCH&C cumulative community hospitals MRSA bacteraemia cases against cumulative trajectory Infection Control – Healthcare Associated Infections 8 Care Quality Commission (CQC) inspection success 6 Number of Cases 5 4 3 2 1 Clostridium Difficile (C. diff) and MRSA bacteraemia b11 ar -1 1 M Fe 0 11 n- Ja 0 D ec -1 0 -1 -1 ct ov O N Se p- 0 10 0 -1 ug l-1 A Ju 0 10 n- Ju -1 2010-11 2010-11 Cumulative actual (Please note that the attribution criteria changed between the periods 2009­10 to 2010­11) 2010-11 NCH&C cumulative community hospitals C.diff cases against cumulative trajectory 20 18 16 14 12 10 8 6 4 2 0 pr -1 M 0 ay -1 Ju 0 n10 Ju l-1 0 A ug -1 Se 0 p1 O 0 ct -1 N 0 ov -1 D 0 ec -1 Ja 0 n1 Fe 1 b1 M 1 ar -1 1 The IPC team has worked closely with NHS Norfolk, acute hospitals, microbiologists, the Health Protection Unit and the antibiotic pharmacists to identify trends across Norfolk in relation to C. diff infections. A printed information booklet was produced, mainly for primary care, but it has also been shared with NCH&C, to ensure collaborative working in reducing C. diff infection rates across the health economy. This work has also informed education and practice within NCH&C; issues such as reviewing the timeframe in which a specimen should be sent have been significant in our management of C. diff. 2009-10 Pre 48 Cumulative actual Number of Cases Root cause analysis is undertaken on all cases and examined within the Infection Prevention and Control (IPC) team, and Trust colleagues, to inform learning which is shared across the Trust. This has culminated in the IPC team providing specific education sessions for NCH&C staff. 2010-11 Cumulative trajectory A NHS Norfolk set local ceilings for NCH&C inpatient beds during 2010/2011 against C. diff and MRSA bacteraemia. Both graphs show that NCH&C finished the year either on or below trajectory. ay pr -1 0 0 A CQC conducted an unannounced inspection on 27 July 2010 to assess whether NCH&C is adequately protecting patients, workers and others from healthcare associated infections (HCAI). The overall judgement of inspection stated: ‘We found no cause for concern regarding the provider's compliance with the regulation on cleanliness and infection control.’ This response supports the ongoing work that is being undertaken with all levels of staff. 7 M 30 2010-11 Cumulative trajectory 2009-10 Pre 48 Cumulative actual 2010-11 2010-11 Cumulative actual Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.5 Patient Safety Adverse Incidents All high level incidents reported in NCH&C were analysed and three key areas have been identified for action from the drilled down data: 1) Pressure Ulcers A review of all reported grade 3 and grade 4 pressure ulcers show the following contributory factors which are in line with known risk factors. These include: poor mobility, frail elderly and vulnerable patients, incontinence, excoriated skin and poor nutrition. Following this an internal audit tool was developed to assess the prevalence of pressure ulcers and identify where they were acquired. An audit was undertaken in July 2010 looking at the high risk areas of Inpatient units and Community Nursing & Therapy (CN&T) to identify whether pressure ulcers occurred under the care of NCH&C or prior to admission. 31 Actions are being taken at a local level to prevent ulcers occurring and deteriorating. All inpatients have a tissue viability and Malnutrition Universal Screening Tool (MUST) or specialist palliative care assessment as part of their admission procedure. All high risk patients in the community are identified and assessed and competencies have been devised for staff working in the wider community. Latest incidence data demonstrates that there has been an overall reduction of pressure ulcers acquired while under the care of NCH&C services. Work continues to further reduce the prevalence of pressure ulcers and a pan­Norfolk Pressure Ulcer Steering Group has been established to set a consistent approach across the county. Reporting requirements have recently been updated, in line with the requirements of the National Patient Safety Agency (NPSA) and CQC. 32 Quality Account Norfolk Community Health and Care NHS Trust 2) Falls As a consequence of their rehabilitation some patients experience a slip trip or fall. An action plan has been agreed to reduce the incidence of falls. Data from incidents will be used to measure the number of falls across locations and identify trends. NCH&C recognises that it is vitally important to be able to measure whether interventions to reduce the risk of falls to patients, visitors and the public are effective in keeping people safe while on Trust premises or within our care. The key measures used to assess the frequency and severity of falls are: • All falls reported using the incident reporting system • The number of inpatient falls per 1,000 occupied bed days • The degree of assessed harm For 60% of reported falls, minimal harm occurred. However, for the person who has fallen, even though physical harm may not be apparent, it may cause delays in recovery or loss of confidence and will have an effect on their perception of the care received. Work is being carried out both at ward level and in the community to identify patients at risk of falling and to introduce improvements through a number of initiatives, such as use of risk assessment documentation within care plans and use and monitoring of the post­fall protocol, a National Patient Safety Agency (NPSA) requirement to be implemented by July 2011. In the nine months from April ­ December 2010 our incident data shows that there was a reduction in falls compared with the same period in 2009. There was an average of 8.9 falls per 1,000 occupied bed days set against a national average of 8.4 (NPSA 2007). Assistive technology is in use in our Specialist Neurological Rehabilitation ward to alert staff when patients are out of bed and are at risk of falling. However, such technology is only appropriate in single room settings and for specific client groups. NCH&C Falls Prevention Service will benefit hundreds more Norfolk patients Hundreds more patients across the county will benefit from the expert support of the NCH&C Falls Prevention Service after it won its bid to deliver services throughout the remainder of Norfolk. The expanding service will also develop new pathways of care in partnership with other providers, aimed at reducing the number of admissions to the acute hospitals resulting from falls. Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.5 Patient Safety 33 3) Medication incidents Numbers of incidents Medication is the third most frequently reported category of incident nationally (ref NPSA Safety in Doses). It is therefore important that medication incidents are reviewed and trends identified at both the local ward/unit level and across the organisation. Trends and common themes can then be discussed and actions taken to address the factors contributing to incidents. The reporting of medication incidents within NCH&C appears to be in line with comparable NHS trusts. The organisational medicines management structure has recently been improved by the appointment of a pharmacist to lead this area of work, and the membership and terms of reference of the Medicines Management Group has been updated. The aim is also to ensure that the high level of reporting across our Trust continues to improve, and that the trend shows an increasing number of low risk incidents compared with moderate/high risk incidents. Overall, there has been a reduction in incidents involving medication with 149 incidents being reported during September ­ December 2010 compared to 163 during the previous quarter. However, this will continue to be monitored to ensure that safe systems of working are reducing the number of incidents. There is evidence of a good reporting culture which will ultimately lead to sharing of learning and overall reduction in risk to patients. 34 Quality Account Norfolk Community Health and Care NHS Trust Effectiveness of Care Productive Community Series is enabling more time for patients The Community Nursing & Therapy Teams have been able to re­invest more than 1,000 hours back into patient care by using a new efficiency model. The Productive Community Series provides a system to identify and remove inefficient activities and reinvest that saved time into making care more interactive, stimulating, reliable and safe. The first stage of this model is ‘Well Organised Working Environment’ (WOWE). This has been already implemented across six integrated teams since May 2010 and has saved 1,113 hours which were reinvested into patient care. The WOWE module helps team to transform their working environment, using no cost/low cost techniques, so that they contribute to, and do not hinder, the efficient delivery of care. Examples of time saving activities include: organising office space and stock cupboards; implementing stock control procedures; developing grab­and­go bags for procedures; and relocating commonly used items so they are easily accessible. This approach involves teams designing the way they plan, organise and deliver care. There are multiple other important benefits including improved standards of care, safety, dignity and job satisfaction. Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.6 Effectiveness of Care 35 Clinical Audit 2010 Clinical Audit is defined as: “A quality improvement process that seeks to improve patient care and outcomes through a systematic review of care against explicit criteria and the implantation of change. Aspects of the structure, processes and outcomes of care are selected and systematically evaluated against specific criteria. Where indicated, changes are implemented at an individual, team or service level and further monitoring is used to confirm improvement in healthcare delivery.” (Ref: National Institute for Clinical Excellence (NICE) Principles for Best Practice in Clinical Audit 2002.) Annual Clinical Audit Programme All trusts are required to consider the following areas for inclusion in the Annual Clinical Audit Programme: • National Audits, eg. National Clinical Audit and Patient Outcome Programme (NCAPOP), currently managed by the Health Quality Improvement Partnership (HQIP) • NICE Guidance Technology Appraisals The following are also integral to our clinical audit programme: • Nationally agreed guidance • Commissioning for Quality and Innovation (CQuIN) • National Service Frameworks (NSF) • Audits initiated by other key national bodies, such as the NHS Litigation Authority, Department of Health, National Patient Safety Agency • NCH&C Policies and Procedures • Serious Incidents Requiring Investigation (SIRIs) trends • Risk Assessments • Root Cause Analysis (RCA) • NICE Clinical Guidelines, Interventional Procedures, Public Health Guidance The NCH&C Clinical Audit Programme will be developed by the Clinical Audit and Effectiveness Team (CAET) one year in advance. The programme will be shared with the Clinical Audit and Effectiveness Committee (CAEC) and the Assistant Directors of the operational business units for comment and local agreement. The final version of the Clinical Audit Programme will be ratified by the Quality & Risk Assurance Committee and submitted to commissioners. 36 Quality Account Norfolk Community Health and Care NHS Trust Medicines Reconciliation A new clinical audit tool was devised by the Modern Matron for Development (Community Rehabilitation), and an audit was run in December 2010. In total 196 patient records were reviewed within Community Rehabilitation teams across our Trust. This audit demonstrated an overall achievement target of 74%, which was set by the commissioners. Osteoporosis Staff in the Community Rehabilitation business unit have run a local audit based on the NICE technology appraisal ­ TA160 (osteoporosis). Childrens’ Services Care Plan Audit Local Clinical Audits completed during 2010 Record Keeping – mandatory trust­wide Annual Clinical Audit The Trust­wide Record Keeping Clinical Audit received 483 returns during November­ December 2010. Both paper and electronic records were audited. Trends found within the audit included: • Clinical teams were generally highly successful with effectively capturing patient identifiable information in the health records, as well as documenting clear accounts of their interaction with the patient without involving personal judgement • Religion was not effectively captured within the patient notes: within SystmOne records there is no place to record this • Inconsistent methods for ensuring that when abbreviations or acronyms are used, the first entry in the record is in full with the corresponding abbreviation or acronym in brackets to follow, allowing the shortened form of the term to be used consequently • The audit tool will be revised in summer 2011 to take into account the organisation’s transition from paper to electronically held patient records This audit was developed, taking into account the NICE guidance TA79 (Epilepsy in Children – Newer Drugs) which was released in 2004. Clinicians within Children’s Services carried out the data collection for this audit between February and September 2010, and have asked the Clinical Audit and Effectiveness Team (CAET) to collate, analyse and report on the result, making any necessary recommendations. Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.6 Effectiveness of Care Participation in National Clinical Audits National Service Framework (Diabetes) The Diabetes Specialist Nurse, who is part of our Community Nursing & Therapy team, based in west Norfolk, has confirmed that their team is taking part in this year’s National Service Framework audit which is looking specifically at the treatment of diabetes. Royal College of Physicians Falls and Bone Health Audit Data collection has been completed and all stages of this national audit are now completed in terms of input from NCH&C. The community input has been returned to the two acute trusts ­ Norfolk and Norwich University Hospitals NHS Foundation Trust and the Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust. Final results are expected in 2011. National Access to Psychological Therapies (NAPT), Anxiety and Depression Three of the four stages of this national audit have now been completed for NCH&C. The final outstanding section is the fourth questionnaire the ‘Service Users’ Surveys’ which have been sent directly to patient’s home addresses with a pre­paid, self addressed return envelope directly back to the NAPT team. The deadline for completion and return of these surveys was the end of February 2011. Results are expected to be published in mid 2011. Health Quality Improvement Partnership (HQIP) Children’s/Young People's Epilepsy Audit ‘Epilepsy 12’ (Royal College of Paediatric and Child Health) The CAET received confirmation that one of our Children’s Service leads is currently taking part in this three­year national audit. 2011/12 is due to be the last data collection year for this audit and results are anticipated as being available early in 2012. 37 Implementation of National Institute for Health and Clinical Excellence (NICE) Guidance NICE is the independent organisation responsible for providing guidance for the promotion of good health and the prevention and treatment of ill health. NICE guidance aims to ensure that the promotion of good health and patient care within the NHS are in line with best available evidence and practice of clinical effectiveness and is cost effective. NCH&C has developed a Clinical Quality & Effectiveness Group which reviews all published NICE guidance for relevance to our services prior to it being distributed to the clinical teams for implementation. For clinical interest / service development reasons, clinical teams are enthusiastic in running clinical audits on the following topics with the intention of linking these to applicable NICE guidance. Children’s Services: Clinical Guideline 99 ­ Constipation in children and young people The CAET are in the process of working with key clinicians to develop a suitable audit tool, using this NICE guidance to supply areas of the criterion. Community Nursing & Therapy (CN&T): Clinical Guideline 20 ­ Epilepsy in Adults and Children The CAET is setting up a clinical group to discuss the development of an audit tool for CN&T based on the guidelines and measurable patient outcomes. Prisons and CN&T Clinical Guideline 109 ­ Transient loss of consciousness in adults and young people This guidance was shown to be relevant by both of these teams. CN&T’s action plan was received in October 2010, and found that there needed to be a trigger question in the multi­disciplinary team falls assessment, indicated when a more detailed history is required with onward referral. The aim is to have all documents amended and available on SystmOne. A clinical audit followed on from this and a report was delivered in Q4 of 2010­11. 38 Quality Account Norfolk Community Health and Care NHS Trust Research Achievements NCH&C has increased its research activity by more than a third compared with the previous year’s activity. ‘Portfolio’ research has also increased this year and now makes up more than 50% (53.2) of total research studies which are active in the Trust. This shows that NCH&C is actively engaging in studies that have been developed and funded through open competition, peer­ reviewed and vetted by the National Institute for Health Research (NIHR) to assure the studies deliver quality research outcomes which can benefit patients and the NHS. Research activity and staff engagement is high in the following areas: Learning Disability Services 8 studies Stroke Rehabilitation 7 studies Community Nursing 6 studies Children’s Services 5 studies Prison Healthcare 3 studies Speech and Language Therapy 3 studies Portfolio research studies such as VenUS 1V A Randomised Control Trial (RCT) of compression bandaging versus compression hosiery in the treatment of venous leg ulcers has had an impact on the care and treatment of our patients. Community nurses have commented on the greater compliance by patients with treatments as a result of being part of the study. The study has increased the use of compression hosiery leading to a reduction in cost and staff seeing patients in the trial healing quicker than patients who are not eligible to take part. Research bursaries for staff A total of £30,000 has been awarded to our staff who were successful in bidding for research bursaries. Five members of NCH&C have received £6,000 each to support themselves in a number of ways to develop a research proposal to be submitted to NIHR for nationally­competitive research funds, such as Research for Patient Benefit (RfPB). Some of the applicants use the money to ‘buy themselves out of clinical time’ so that they can devote themselves appropriately to research. Research Site Initiative Scheme Research highlights from 2010­11 include: Stroke Rehabilitation and Early Supported Discharge Service This service has incorporated research into their care they deliver to local patients in a fundamental way since they opened in Beech Ward, at the Mulberry Rehabilitation Unit, Norwich in January 2010. High numbers of patients going through the service are eligible to participate in research studies. NCH&C has a strong collaboration with the University of East Anglia (UEA), Norfolk & Norwich University Hospitals NHS Foundation Trust and Trent Stroke Research Network. Current and new collaborations with academics and clinicians working at the acute end of the Stroke Care Pathway have led to excellent research collaborations which have had a positive impact on patient care in terms of opportunities to receive new and innovative rehabilitation treatments as a result of taking part in locally based research studies. This is a new research initiative being piloted at NCH&C which aims to provide clinical teams the opportunity to increase their research capacity. By signing up to a contract which contains a set of outcomes, the teams should be able to develop an even more skilled research workforce with greater capacity to host NIHR portfolio research. It is designed to assist teams with ‘buying out’ time to complete research skills training and to develop the research infrastructure within their service. Six teams are involved from Children’s Services, Specialist Palliative Care Services, Learning Disability Services, the Stroke Rehabilitation Service and one Integrated Care Team. £20,000 of funding has been provided throughout Norfolk & Suffolk Comprehensive Local Research Network (CLRN) to support the initiative. We hope that it will have an impact on our Trust’s capacity to host more portfolio research over the next 12 months and beyond. Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.6 Effectiveness of Care 3.1.7 Patient experience 39 Loyola Weeks, NCH&C’s Director of Quality and Risk, said: “I am delighted that this feedback has shown that patients continue to benefit from our excellent health and care services. I would like to thank all of our staff whose commitment to delivering these services across Norfolk has made these further improvements possible and I commend them for their efforts. The year­on­year improvements which have been highlighted by patients show that we are continuing to offer excellent health and care provision to our patients.” Patient Experience Ipsos MORI Survey 2010 All teams are being asked to build on the excellent progress made so far and to assess how we can make further improvements in the future. Patients praise NCH&C’s staff and services Patients have highly rated our health and care services in a recent survey. More than 90% of people have expressed their satisfaction with our Trust’s services in a recent Service User Experience Survey, with two­ out­of­three people giving the highest rating possible. The results of the independent survey, managed by Ipsos MORI, have also shown a significant improvement in patient/user satisfaction with our services over the past 12 months with ‘fairly good’ scores having been transformed into ‘very good’ scores in many areas. People were particularly positive about how their care was joined up between services (continuity of care), an increase in choice, how supported they felt by staff in making healthcare decisions, and the helpfulness of staff. Two­out­of­three of the 1,139 people (67%) taking part in the survey said they were ‘very satisfied’ (the highest rating possible) with our services, which is an increase of 2% on the previous year, with a combined score of 91% being either ‘fairly’ or ‘very satisfied’ with our services Three quarters of people (75%) rated the helpfulness of our healthcare staff as ‘very good’ and 62% of people rated the helpfulness of our admin staff as ‘very good’ 86% of those who took part would be ‘likely’ to recommend our services to a friend or relative; two­out­of­three people (66%) were ‘very likely’ to recommend NCH&C and 20% were ‘fairly likely’ 69% of those surveyed felt our services had improved or stayed the same over the past year; with 34% saying things had improved 40 Quality Account Norfolk Community Health and Care NHS Trust Delivering Same­Sex Accommodation Essence of Care: Privacy and Dignity NCH&C is proud to confirm that mixed sex accommodation has been virtually eliminated in all of our community hospitals. Our inpatient units carried out a benchmarking exercise against ‘Essence of Care; Privacy & Dignity’ in the summer of 2009. At the beginning of 2009 we started a programme of work in response to the Department of Health commitment to eradicate mixed sex accommodation (Same Sex Accommodation: Your Privacy, Our Responsibility). In the following year there has been considerable work across the units in relation to privacy and dignity and meeting the same sex agenda. This has included: staff developing unit plans to identify gender allocation for bathrooms and toilets; clear labelling of hygiene facilities; the development of a reporting system for mixed sex occurrences; the creation of a Privacy and Dignity Steering Group which meets regularly; and the roll out of a Privacy and Dignity training package and Personal Care Policy. Since this launch we have delivered this agenda and 2010 has seen the privacy and dignity philosophy embedded into day­to­day practice for patients admitted to our community hospitals. Patients can expect to find the following in relation to same sex accommodation: • The bedded rooms will only have patients of the same sex • Toilets and bathrooms will be just for one gender, and will be near to the bed area While there will be both men and women patients on the ward, they will not share the same sleeping area. Men and women may have to cross a ward corridor to reach their bathroom, but they will not have to walk through opposite­sex bedded areas. A self­assessment has been undertaken focusing on four key areas: 1 Patient experience 2 Estates 3 Systems and processes 4 Staff culture If our care should fall short of the required standard, we will report it. We will also set up an audit mechanism to make sure that we do not misclassify any of our reports and we will publish the results of that audit on our website. The original 2009 benchmarking exercise also required staff to create and work through action plans in response to any identified weaknesses. This benchmarking exercise was repeated in September 2010. Method: Each unit was given a prepared pack and score card. This pack set out the seven ‘Essence of Care’ key factors for the Privacy and Dignity benchmark with supporting statements which enabled the unit staff to consider practice and re­score themselves on a score from A to E. It also included the 2009 results so staff could reflect on the changes made during the year. The scores were entered on a matrix and returned for collating and review. Conclusion: It is clear that all areas have either scored themselves as having stayed at the same high level (two units remained at 85% A scores) or have improved in the year 2009/2010. Across the units the overall percentages of A and B scores have increased and very few factors fall below these high scores. One unit ­ Beech Ward, Mulberry Rehabilitation Unit ­ opened in January 2010 and therefore had not previously been through this process. This team identified areas which could be improved and is creating an action plan to take this improvement work forward. Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.7 Patient Experience The two main issues that have been revealed by this benchmarking are: 1 Communication: Understanding of how to access INTRAN. Action: Contact details have been re­circulated to all Modern Matrons. 2 Availability of an area for privacy: The design of the estate and the inability of the older un­refurbished buildings to provide an environment conducive to maintaining the privacy and dignity of our patients. Action: Estates issues are flagged up at all opportunities and have been built into the capital bids programme. This is monitored via the Patient Environment Action Team (PEAT) inspections and areas are achieving high scores despite the limited nature of the estate. 41 Outstanding Patient Environment Action Team (PEAT) Results Health facilities at NCH&C were assessed by the PEAT programme during 2010. Ten of the healthcare facilities that we manage were assessed and achieved outstanding results in all three categories: environment, food, and privacy and dignity. Every healthcare facility in England with 10 or more inpatient beds is assessed annually and given a rating of excellent, good, acceptable, poor or unacceptable. We obtained six ‘excellent’ scores and the remainder all achieved ‘good’ ratings. Congratulations were passed on to the staff at these sites for aiding in the effort to continuously maintain a high level of standards. This is a vast improvement on last year’s results, as we received no ‘acceptable’ scores. For more information about this year’s PEAT scores, please visit: www.nrls.npsa.nhs.uk/patient­safety­data/peat NCH&C PEAT Scores for 2010/11 Site Name Environmental score Food score Privacy and Dignity score Colman Hospital, Norwich Good Good Good Norwich Community Hospital Good Good Good Dereham Hospital Good Excellent Good North Walsham Hospital Good Good Good St Michael’s Hospital, Aylsham Good Good Good Kelling Hospital Good Good Good Swaffham Community Hospital Good Good Excellent Ogden Court, Wymondham Good Good Excellent Cranmer House, Fakenham Good Good Excellent Benjamin Court, Cromer Good Excellent Excellent 42 Quality Account Norfolk Community Health and Care NHS Trust Real time data collection ­ Patient Experience Tracker (PET) Pilot The three themes of environment, food and privacy and dignity were included in questionnaires developed for the PET pilot, which ran from May ­ December 2010. The questionnaires developed for inpatients also included elements of ‘Essence of Care’ and the Productive Community Ward programme. 1% 4% 4% NCH&C services involved in the pilot were asked to create their own questionnaire for the pilot, however, there were a number of questions common to all. Below are some examples of the results: 2% 3% 2% Key 9% Excellent 14% Very Good Involving you in decisions about your care or treatment 48% The explanations given to you during your appointment Good Average Poor Very Poor 29% 84% 9% 2% 2% 3% 5% 6% 2% 10% 5% The overall experience of your appointment 55% The way the staff communicated with you 24% 77% Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.7 Patient Experience Learning from complaints and incidents From January ­ December 2010 a total of 203 complaints were received by NCH&C. Number of complaints 60 58 56 54 52 50 48 46 44 42 40 43 3 Changes in the procedure for clinical referrals in prison healthcare will ensure timely clinical review. • Changes have also been made in the distribution medication to ensure all prison patients can collect before leaving the landing in the morning • Within the Learning Disabilities Service’s respite care provision, all faxed requests to pharmacy for medication will be confirmed by telephone to ensure prompt dispensing and delivery Learning event ­ 5 October 2010 Q4 2009/10 Q1 2010/11 Q2 2010/11 Q3 2010/11 NCH&C use complaints as a positive means of learning and where necessary, making improvements. Some of the themes or learnings from these are as follows: 1 Various aspects of communication with patients were highlighted, including: • Appointment systems • Clarity of access criteria, pre­access information required and management of patient expectations • Problems were also identified in the way in which clinicians communicate with patients or carers/families Appointment systems and patient information are being reviewed. Clinicians communications are under review through reflective practice. 2 Complaints about failures of community nurses to carry out scheduled home visits has resulted in a review of the methods of logging, allocating and confirming home visits. • Changes in how counselling sessions are managed have resulted from a complaint. The importance of a holistic approach was emphasised with staff involved • It was identified that some community nurses require specialist training in post­operative care for patients and this is being addressed A learning event organised by the Quality and Risk Management Team was attended by 61 members of NCH&C staff. The aim was to enable staff to share the learning from Serious Incidents Requiring Investigation (SIRIs) and complaints. This included a keynote speaker from NHS East of England on the learning from the Mid Staffordshire Inquiry and the commissioning perspective from NHS Norfolk. NCH&C staff presented the root cause analysis information from SIRIs and compaints over the past 12 months. The workshop closed with a session entitled ‘Celebrating Success from Learning’ which all delegates were invited to contribute to. Our internal auditors, PriceWaterhouse Cooper, attended the event and advised that further similar events should be welcomed across the organisation. Staff who attended have brought the information back to their teams. There will also be further local risk and learning events at team level. 44 Quality Account Norfolk Community Health and Care NHS Trust Compliments From April ­ December 2010, 462 compliments were passed to the Complaints and Claims Manager for recording, which demonstrate how the care, treatment, advice and support offered by all NCH&C staff is appreciated by the patients we serve and their relatives, friends and carers. A selection of these include: Physiotherapy, Dereham Hospital: Pineheath Ward, Kelling Hospital: I came here with mixed feelings about what would be achieved. I have been very pleased with the end result... now I have the quality of life I have wanted for a good number of years... I am writing to say what excellent care my husband received on Pineheath Ward. The standard of nursing was very high and done with care and compassion. Nothing was ever too much trouble. The ward was kept very clean which was good to see... Community Nursing & Therapy: I write to thank you and your team for the extraordinary support you gave my late sister during her last few days of life. She was able to say goodbye to all her friends and family in her own surroundings and was truly happy to be able to die peacefully and with dignity, in the comfort of her own home thanks to your wonderful standard of care... The community nurses have looked after my mother for the past eight years and me for the past two weeks. They are all very professional, very kind and friendly. People should appreciate how lucky we are to have them... My husband and I attended the Parkinson’s Disease Education Group at Kelling Hospital. It was very informative and well organised with very friendly staff. We both looked forward to those Monday afternoons... Occupational Therapy: Two nice young ladies came and measured me for two sticks, which have been so useful, and they advised me on walking and exercises. Thank you... Orthopaedic Outreach: Within an hour of contacting my doctor I had received a call from the Orthopaedic Outreach Team, in Wymondham, and within three hours they were at my house providing a whole range of equipment and advice about my surrounds. The service was well beyond my expectation and the team was extremely professional... Rapid Response Team: I would like to offer our thanks to this team which gave such fantastic care and support to us as a family. The service you provide is second to none and we don’t know what we would have done without you all... Part 3 3.1 Review of Quality Achievements in 2010/2011 3.1.7 Patient Experience 3.1.8 Commissioning for Quality and Innovation (CQuIN) 45 Commissioning for Quality and Innovation (CQuIN) 2010/2011 NCH&C and NHS Norfolk agreed a set of quality measures which were assessed as part of the CQuIN initiative, and which focused on the following areas for 2010/11 and represented 1.5% of the contract value: CQuIN indicator description Patient Experience Patient Safety Indicator Effectiveness weighting To improve the recording of referrals to Smokefree Norfolk and increase health promotion in the community 3% Introduction of a health promotion campaign which will improve the sexual health of the local population (15­24 year­olds) 2% Increase the number and use of community ‘step­up beds’ 10% Set up processes to increase the number patients provided with assistive technology support in the community, community hospitals and care homes 10% Review admissions to community hospitals to inform the requirement for increasing or standardising hours 5% To improve the care and access to services for patients with dementia 10% To improve the care and access to palliative care services in the community 5% Improve end of life care by increasing the use of Liverpool Care Pathway (LCP) for those entering the last days of life 5% Improve the discharge planning and referrals to ongoing care organisations for prisoners 5% Utilisation of Quality Outcomes Framework (QOF) to inform and support the care and treatment of prisoners accessing healthcare 5% All inpatients to have their medicines reconciled within 72 hours of admission and discharge policy developed 5% Reduced cancellation rates to community paediatrician 5% Improve Patient Experience based on review of data from Ipsos MORI survey 15% Improve outcomes for patients in the community through active review and analysis of adverse events 10% Improve care and access to services for patients with learning disabilities 5% NCH&C forecast an overall delivery of 70% of the £1.5 million available through the 2010/11 CQuIN scheme 46 Quality Account Norfolk Community Health and Care NHS Trust NCH&C Quality Account 2010/2011: Involvement and Engagement • Presentation of Quality Account process at the Norfolk LINks Strategic meeting on 2 February 2011 • LINks and Public Involvement at Board and other committees, including Quality and Risk Assurance Committee, Patient Experience Steering Group, Patient Environment Action Team and Nutrition Group • Development of the Integrated Business Plan (IBP) by Trust Board members and the Clinical Reference Group • Development of the Annual Plan by Executive Directors and Assistant Directors and their teams • Quality and Risk Assurance Committee provides assurance to the Board and has a LINk representative in attendance • Patient Experience Steering Group’s LINk representative said: “I am already inspired by the innovative work that, in conjunction with Norfolk LINk members, NCH&C are currently doing to identify their own shortcomings and thereby improve their services.” • Third party commentary requested from Norfolk LINk, Health Overview and Scrutiny Committee and NHS Norfolk Third Party Statements Norfolk NHS Norfolk “NHS Norfolk, as lead commissioner for the Trust, notes receipt of Norfolk Community Health and Care NHS Trust’s publication of a Quality Account for 2010/11. We have reviewed the mandatory data required within this account and can confirm that some of the information provided does not meet the national requirements in terms of narrative. NHS Norfolk have shared these areas with you so that amendments can be made. The report presents detailed and comprehensive information relating to quality and safety of care delivered within the prioritised areas identified by the Trust. The quality goals for 2011/12 are relevant and are substantiated by involvement with the clinical quality and patient safety agenda via the Commissioning for Quality & Innovation payment framework (CQuIN) and the Quality, Innovation, Productivity and Prevention (QIPP) initiatives. We commend staff for their work to improve outcomes within these areas. We look forward to the inclusion of an update on achievements in the identified priority areas as part of the reporting within next year’s quality account. The patient satisfaction survey provided valuable feedback for the Trust and identified areas of work required to address the issues raised, building on the progress made so far. We will continue to work with you on all matters relating to the quality of the services that you provide. This includes topics or services not covered by your 2010/11 report.” Andrew Morgan, Chief Executive, NHS Norfolk Part 3 3.2 NCH&C Quality Account 2010/2011: Involvement and Engagement 3.2.1 Third party statements Norfolk LINk “A LINk member has a non voting place on the board. The member is encouraged to voice the opinion of the patients and public. Both Executive and Non Executive members spend time outside these meetings explaining policies and strategies and answering any questions. “A LINk member has a place on the CFT Programme Board and is also involved in the communications work of that board to ensure that Patient and Public involvement will be at the centre of the Community Foundation Trust. A LINk member will sit on the governing board of the new Trust. “LINk recognises the excellent work that NCH&C are undertaking in various parts of the county, however it recognises that some of these services are not available throughout the whole county and will continue to monitor these services to ensure an equality of service throughout Norfolk. “Whilst services in the prisons appear to be improving slowly, LINk will continue to monitor the service to ensure that this improvement is maintained and strengthened. “LINk recognises the value of the NCH&C vision for the future, and hopes that the vision of working in new geographies will not distract from the present workload. “LINk members have been involved in the annual PEAT inspections and can confirm that the standards remain high in all hospitals. Any suggestions made by LINk members have been evaluated and where possible have been accepted. A member sits on the PEAT/PENG working group to ensure that the highest standards are being maintained throughout the service. 47 “LINk members are following progress of the frail elderly focus, including dementia care and palliative care and again want to ensure that this will be a county wide service as soon as possible. “LINk notes the improvement in service delivery for wheelchairs, continuing healthcare and podiatric surgery, but recognises that not all targets have been achieved and will continue to monitor their progress. “A LINk member has contributed to the estates strategy to ensure that needs of the patients and public will be considered. “A Norfolk LINk member sits on the (NCH&C) Patient Experience Steering Group that meets at bi­monthly intervals. We acknowledge the commitment that NCH&C has made to involving their staff in gathering patient feedback and studying and trialling a number of different methods of obtaining this. NCH&C also has a comprehensive complaints system, reports from which discussed regularly at Patient Experience Steering Group meetings.” Norfolk LINk 15th June 2011 Norfolk Health Overview & Scrutiny Committee “The Norfolk Health Overview and Scrutiny Committee has decided not to comment on any of the Norfolk NHS Trusts' Quality Accounts for 2010­11 and would like to stress that this should in no way be taken as a negative statement”. Head Office: Elliot House, 130 Ber Street, Norwich NR1 3FR Online: www.norfolkcommunityhealthandcare.nhs.uk Telephone: 01603 697300