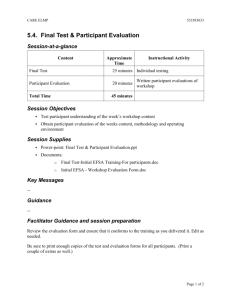
Supplementary appendix
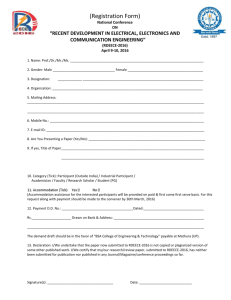
advertisement

Supplementary appendix This appendix formed part of the original submission and has been peer reviewed. We post it as supplied by the authors. Supplement to: Michaleff ZA, Maher CG, Lin C-WC, et al. Comprehensive physiotherapy exercise programme or advice for chronic whiplash (PROMISE): a pragmatic randomised controlled trial. Lancet 2014; published online April 4. http://dx.doi.org/10.1016/ S0140-6736(14)60457-8. CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL Web appendix 1: Trial protocol Chronic Whiplash Exercise Trial A randomised controlled trial of a comprehensive exercise program for chronic whiplash The University of Sydney HREC reference number: 03-2009/11509 The University of Queensland project number: 2008002059 Study Protocol (Draft 7 dated 14/05/2010) Lancet_Web_appendix Draft 7 Page 1 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL Chronic Whiplash Exercise Trial Summary Sheet Name of Sponsors: The George Institute For International Health The University of Queensland Title of Study: A randomised controlled trial of a comprehensive exercise program for chronic whiplash. Principal Investigators: Professor Chris Maher, The George Institute for International Health, Australia. Associate Professor Michele Sterling, Centre for National Research on Disability and Rehabilitation Medicine (CONROD), University of Queensland, Australia. Study Sites: The study will recruit participants from Sydney and Brisbane. Study Period (years): January 2009 to May 2012 Phase of Development: Phase III Duration: 3 years Objectives: 1. The primary aim of this randomised controlled trial is to establish the effectiveness of a comprehensive exercise program for people with chronic (symptoms > 3 months < 5 years duration) whiplash. 2. The second aim is to conduct an economic evaluation of the exercise program. 3. The third aim is to investigate if sensory hypersensitivity and symptoms of posttraumatic stress modify the effect of the program. Methodology: The study will be a randomised controlled trial comparing a comprehensive exercise program, consisting of 20 one-hour supervised exercise sessions over a twelve-week period, to an educational booklet for people with chronic whiplash. Outcomes measures will be assessed at baseline, 14 weeks, 6 and 12 months. Participants will be recruited through written contact to claimants who are registered with the Motor Accidents Authority of New South Wales and through advertisements in Sydney and Brisbane print media. Planned number of participants: - Total: 172 participants (i.e. 86 participants from Sydney and 86 participants from Brisbane) - Comprehensive exercise program: 86 participants - Advice and booklet: 86 participants Diagnosis and main criteria for inclusion: - Grade I or II whiplash of at least 3 months duration but less than 5 years duration. - Currently experiencing at least moderate pain or moderate activity limitation due to pain (modified items 7 & 8 of SF36). - Not currently receiving care for whiplash. Duration of follow-up: One year Statistical methods Treatment efficacy variables: We will analyse the effect of treatment separately for each outcome using linear mixed models with time as a repeated factor. The model will account for correlation over time within participants, correlation within clinics and potential confounders (e.g. important prognostic factors). Effect modifiers: Effect modification will be assessed by including a predictor-by-treatment group-by-time interaction term to the mixed models analyses. Effect modification will only be assessed for the primary outcome of average pain intensity over the last week. Economic analysis: The cost-effectiveness of each mode of care will be assessed using the cost and health preference data (the latter of which will be used to generate QALYs). Lancet_Web_appendix Draft 7 Page 2 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL Chronic Whiplash Exercise Trial Summary Sheet (continued) Name of Sponsors: The George Institute For International Health The University of Queensland Contractual signatories I confirm that I have read and agreed to the Chronic Whiplash Exercise Trial Draft 6, dated 4/09/2009 for the study titled ‘A randomised controlled trial of a comprehensive exercise program for chronic whiplash’ Principal Investigator (NSW) Principle Investigator (QLD) Name Date Signature Professor Chris Maher Associate Professor Michele Sterling The George Institute For International Health The University of Queensland Motor Accidents Authority NSW David Andrews Motor Accidents Insurance Commission Queensland Lancet_Web_appendix Draft 7 Page 3 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL TABLE OF CONTENTS 1. 2. 3. 4. 4.1 5. 5.1 5.2 ETHICS AND CONFIDENTIALITY .......................................................................................................................... 5 ADMINISTRATIVE STRUCTURE ............................................................................................................................ 6 INTRODUCTION.................................................................................................................................................... 7 OBJECTIVES....................................................................................................................................................... 11 Aims and hypotheses of the study ................................................................................................................. 11 STUDY DESIGN ................................................................................................................................................... 12 Design ........................................................................................................................................................... 12 Participants .................................................................................................................................................... 14 5.2.1 Participant recruitment .............................................................................................................................. 14 5.2.2 Inclusion criteria ....................................................................................................................................... 14 5.2.3 Exclusion criteria ...................................................................................................................................... 14 5.3 Study Interventions ....................................................................................................................................... 16 5.3.1 Baseline assessment .................................................................................................................................. 16 5.3.2 Randomisation .......................................................................................................................................... 16 5.3.3 Educational booklet................................................................................................................................... 16 5.3.4 Comprehensive exercise program ............................................................................................................. 16 5.3.5 Treatment sites .......................................................................................................................................... 18 5.3.6 Follow up .................................................................................................................................................. 18 5.3.7 Premature discontinuation of randomised intervention ............................................................................. 18 5.4 Study Outcomes ............................................................................................................................................ 18 5.4.1 Outcomes Assessments ............................................................................................................................. 18 5.4.2 Primary outcome ....................................................................................................................................... 18 5.4.3 Secondary outcomes ................................................................................................................................. 18 5.4.4 Participant diary ........................................................................................................................................ 19 5.4.5 Economic evaluation ................................................................................................................................. 19 5.4.6 Reporting of adverse events ...................................................................................................................... 19 5.5 Study Sequence ............................................................................................................................................. 20 5.5.1 Telephone screening.................................................................................................................................. 20 5.5.2 Baseline Assessment ................................................................................................................................. 20 5.5.3 Randomisation .......................................................................................................................................... 20 5.5.4 Physiotherapy treatment clinic .................................................................................................................. 21 5.5.5 14 weeks, 6 and 12 month follow up assessments .................................................................................... 21 5.6 Quality Assurance ......................................................................................................................................... 22 5.6.1 Monitoring of study sites .......................................................................................................................... 22 5.6.2 Data integrity............................................................................................................................................. 22 5.7 Statistical Issues ............................................................................................................................................ 22 5.7.1 Statistical analysis and methodological considerations ............................................................................. 22 5.7.2 Sample size ............................................................................................................................................... 22 5.8 Indemnity ...................................................................................................................................................... 23 5.9 Publications and reports ................................................................................................................................ 23 5.10 Funding ......................................................................................................................................................... 23 5.11 Timeline ........................................................................................................................................................ 23 6. REFERENCES: .................................................................................................................................................... 24 7. APPENDICES ...................................................................................................................................................... 26 Appendix 1 – Promise advertisement .......................................................................................................................... 26 Appendix 3 – Phone screening..................................................................................................................................... 30 Appendix 6 – Telephone script to arrange follow-up assessments .............................................................................. 34 Appendix 9 – Outcome assessments ............................................................................................................................ 41 Appendix 10 – Measuring cervical spine range of movement: inclinometer method .................................................. 57 Appendix 11– Measuring cold pain threshold over the cervical spine......................................................................... 58 Appendix 12 – Measuring pressure pain threshold over the cervical spine and the tibialis anterior ........................... 59 Appendix 13 – Utility weights: instruction and recording sheet .................................................................................. 59 Lancet_Web_appendix Draft 7 Page 4 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 1. Ethics and confidentiality Approval for the Chronic Whiplash Exercise Trial has been obtained from the University of Sydney Human Research Ethics Committee (03-2009/11509) and the University of Queensland Human Research Ethics Committee (2008002059). Written informed consent, complying with local requirements, will be obtained from all participants prior to entry into the study. The study will not commence in any centre until all the necessary documentation has been completed. In obtaining informed consent, the study staff will provide the potential participant with information about the purposes, methods, possible risks and benefits of participating in the study. All potential participants will have an opportunity to discuss the trial with study staff. The participant and the person obtaining informed consent will each sign and date two copies of the consent form, one copy of which will be provided to the participant and the other copy of which will be stored in the participant’s case record folder. Involvement in the study will be voluntary and all participants will have the opportunity to withdraw from the study at any time without prejudice to their current or future medical management. In the event of a participant wishing to withdraw from the study, they will be required to verbally contact study staff and notify them of their decision. Modifications to the protocol, participant information sheet or consent form will be submitted to the ethics committee for approval and appended to this document. Such modifications will only be implemented once ethics committee approval has been obtained, unless an amendment is being made to eliminate immediate hazards to study participants. All data generated by the study will remain strictly confidential and no report will contain any information that would allow an individual participant in the study to be identified. However, in order to facilitate complete data collection and follow-up individual contact details will be collected at registration and secured in locked filing cabinets with limited access. These details will be stored separate from other data. Participant records at treatment provider clinics will be identified by participant name or initials and their unique randomisation number. Lancet_Web_appendix Draft 7 Page 5 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 2. Administrative structure This investigator-initiated study is sponsored by The George Institute For International Health and The University of Queensland. The study is funded by the Motor Accidents Authority of New South Wales, Motor Accidents Insurance Commission Queensland and the National Health and Medical Research Council. The principle investigators and coinvestigators will be responsible for overseeing all aspects of the trial and they will be responsible for the preparation and publication of the principal results of the study. The study will be conducted in Sydney and Brisbane. Each site will be responsible for participant recruitment, follow up and coordination of the trial. PRINCIPLE INVESTIGATORS Professor Chris Maher The George Institute For International Health and University of Sydney Tel: (02) 9657 0382 Fax: (02) 9657 0301 Email: cmaher@george.org.au Associate Professor Michele Sterling Centre for National Research on Disability and Rehabilitation Medicine (CONROD) University of Queensland Tel:(07) 3365 5344 Fax: (07) 3346 4603 Email: m.sterling@uq.edu.au CO-INVESTIGATORS Professor Gwendolen Jull School of Health and Rehabilitation Sciences University of Queensland Tel: (07) 3365 1114 Fax: (07) 3365 1622 Email: g.jull@uq.edu.au Dr Trudy Rebbeck Specialist Musculoskeletal Physiotherapist Discipline of Physiotherapy University of Sydney Tel: (02) 9363 0490 Fax: (02) 9326 2203 Email: T.Rebbeck@usyd.edu.au Associate Professor Jane Latimer The George Institute For International Health and University of Sydney Tel: (02) 96570 384 Fax: (02) 9657 0301 Email: jlatimer@george.org Matt Roodveldt Centre for National Research on Disability and Rehabilitation Medicine (CONROD) University of Queensland Professor Luke Connelly University of Queensland Tel: (02) 9926 7351 Fax: (02) 99061859 Email: l.connelly@uq.edu.au Miss Zoe Michaleff The George Institute For International Health and University of Sydney Tel: (02) 9657 0321 Fax: (02) 9657 0301 Email: zmichaleff@george.org.au Dr Christine Lin The George Institute For International Health and University of Sydney Tel: (02) 8238 2437 Fax: (02) 9657 0301 Email: clin@george.org.au Stephanie Valentin Centre for National Research on Disability and Rehabilitation Medicine (CONROD) University of Queensland Research assistant Email: s.valentin@uq.edu.au Lancet_Web_appendix Draft 7 Email: m.roodveldt@uq.edu.au Page 6 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 3. Introduction 3.1 Background 3.1.1 The problem of chronic whiplash The most common injury following a motor vehicle accident is a whiplash injury to the neck and this injury is of particular concern because it usually results in persisting pain and disability in an otherwise healthy young adult2 3. At present, there is no known effective treatment for those who suffer persistent pain following a whiplash injury. In our view part of the reason for the lack of attention to whiplash is that many people under-estimate the significance of this health problem. The media has likely contributed to this misconception as it has often trivialised whiplash by commonly depicting people who feign an injury. The reality is quite different. In Australia and abroad the personal and economic burden of whiplash is enormous. For example, in New South Wales in the period 1989-1998 there were 50,000 whiplash claims costing ~$1.5billion4. Whiplash is also notoriously difficult to manage with the most frequent outcome following a whiplash injury being persisting pain and disability. Our research in NSW2 and in Queensland3 revealed that ~60% of people are still in pain and disabled 6 months after the original accident. The ongoing symptoms affect quality of life with our data showing SF36 scores markedly lower than Australian norms2. Our recent systematic review of the prognosis of acute whiplash revealed similar health outcomes in other countries around the World5. With the number of cars in the World to double over the next 30 years there is an urgent need for effective and affordable treatments for chronic whiplash. 3.1.2 Limited treatment options for chronic whiplash The 2007 Cochrane review6 concluded that there are no clearly effective non-surgical treatments for chronic whiplash. The few trials published subsequent to the review do not change this conclusion. The reality is that available treatments have at best very small effects. There is however one surgical technique where there is clear evidence of efficacy: radiofrequency neurotomy7. With this surgical procedure a needle is used to burn, and so destroy, the nerves that transmit pain from the damaged zygapophyseal joints in the lower cervical spine. This treatment is only indicated for the sub-group of patients whose symptoms arise from these joints. Moreover there are major limitations to this treatment. The procedure is technically difficult surgery and offers only temporary relief of symptoms and needs to be repeated when the nerves recover and pain returns. Because of these limitations radiofrequency neurotomy, on its own, cannot provide a solution to the problem of chronic whiplash. For the majority of sufferers with chronic whiplash there are currently no proven effective therapies. 3.1.3 Developing an effective exercise program for chronic whiplash Over the last five years the chief investigators have been working to develop an effective treatment for chronic whiplash that avoided the limitations of neurotomy. The first developments were two different exercise programs: graded activity and specific exercise. The programs were evaluated in separate randomised controlled trials8 9 with each trial demonstrating that the program was effective. While these results were very promising, and have been published in the leading journal Pain, it was apparent that only 10-20% of participants had a completely successful outcome (see Figure 1). In the investigators’ opinion this success rate was too low to represent a solution to the problem of chronic whiplash. Further development was necessary. The features of an exercise program such as the type of exercise, intensity and duration are key determinants of the effects of exercise10. By varying these parameters it could be possible to increase the success rates of the previous exercise programs. We chose not to increase the intensity or dose of exercise because this would increase the risk of side-effects such as exacerbation of symptoms. Instead we opted to combine both treatments. We reasoned that because the two forms of exercise address different impairments seen with whiplash, it is likely that a program that combined both approaches would provide Lancet_Web_appendix Draft 7 Page 7 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL greater results. Accordingly we developed a comprehensive exercise program that combined both approaches yet could still be readily implemented by any physiotherapist. The principle investigators conducted a small uncontrolled phase I/II trial that provided results which confirmed our hypothesis (see Figure 2). This comprehensive program had a much higher success rate with 56% of subjects having minimal or no disability at the end of the program. This success rate approximates that of radiofrequency neurotomy (58%) but importantly avoids the serious limitations of this treatment. probablity of a successful outcome 100% Figure 1. Superior results of the comprehensive exercise program. Figure shows % of subjects with minimal or no disability following graded activity, specific exercise and the new comprehensive exercise program. 80% 60% 40% 20% 0% Graded activity Specific exercise New program 3.1.4 Why the better effect with both treatments combined? We believe that there are sound theoretical reasons to explain why the comprehensive exercise program would provide a substantially greater probability of success. The initial specific neck exercise program restores the functions of the muscles that control and support the neck. The graded activity program improves the patient’s general fitness and teaches the patient how to successfully undertake activities of daily living that they find problematic. Without first ensuring that the neck musculature is able to control and support the neck a graded activity program could potentially exacerbate a patient’s symptoms. Similarly unless a specific exercise program is followed by a graded activity program the improved support and control of the neck may not translate into improved ability to participate in activities of daily living. It is only when both treatments are combined in an integrated package that the foundations for success are provided. Based upon the exciting results of the pilot study and its strong biological rationale, we now propose to definitively establish the effectiveness of this comprehensive program in a large phase III randomised controlled trial. 3.1.5 Predicting response to treatment: effect modifiers In our pilot trial we found that ~60% of subjects responded to the comprehensive exercise program. It would obviously be of great value to be able to identify people with a high likelihood of success so that treatment resources are not wasted on people who will not respond to this program. We believe that we may be able to identify this group based upon clinical characteristics. Our research has demonstrated that whiplash is not a homogeneous condition. Rather sub-groups can be identified that display varying degrees of physical and psychological disturbance11 12. Most patients demonstrate a fairly uncomplicated clinical presentation of mild to moderate levels of pain and disability, mild psychological distress and motor dysfunction. At the other end of the spectrum, there is a group of whiplash patients (approx 25%) who demonstrate a complex clinical picture including moderate/severe levels of pain and disability associated with marked sensory disturbance (widespread hyperalgesia, Lancet_Web_appendix Draft 7 Page 8 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL sympathetic nervous system dysfunction) indicative of central nervous system hypersensitivity13 14. In association with sensory disturbance these patients also display symptoms of a moderate posttraumatic stress reaction15. We have shown that the presence of sensory hypersensitivity and/or symptoms of posttraumatic stress are strongly predictive of poor long-term outcome3 15. Additionally the presence of sensory changes in chronic whiplash moderated the effects of our specific exercise treatment intervention9. The influence of posttraumatic stress on the effects of exercise intervention in whiplash has never been investigated. It is likely that these factors will also influence the effects of a combined exercise therapy approach and for this reason we believe their evaluation as potential treatment effect modifiers is mandatory. 3.2 Summary The aim of the proposed research is to determine the effectiveness of a comprehensive exercise program for chronic whiplash. Currently, for the majority of sufferers with chronic whiplash there are no proven therapies available to manage this personal and financially costly condition. Promising results have been identified in randomised controlled trials evaluating the effects of different exercise programs, graded activity and specific exercise. However, success rates from these studies were too low to represent a solution to the problem of chronic whiplash and further development was necessary. A comprehensive exercise program that combined both specific exercises and graded activity was developed. A small uncontrolled phase I/II trial provided evidence that this new exercise program had a much higher success rate with 56% of subjects having minimal or no disability at the end of the program. This success rate approximates that of radiofrequency neurotomy (58%) but avoids such invasive surgical techniques. Based upon the exciting results of the pilot study and the strong biological rationale for the superior results with the combined program we now propose to definitively establish the effectiveness of the new program in a large phase III randomised controlled trial. 3.2.1 Planned outcomes Our choice of outcomes is consistent with the recommendations of the Cochrane Back Review Group16 and our previous study of the responsiveness of these measures17. Measures of symptoms, global recovery, functional status, quality of life and side effects will be taken. We have chosen a patient-specific measure of functional status because there is evidence that this is more responsive than a condition-specific measure18. We have included the most widely used whiplash-specific (Whiplash Disability Questionnaire) and neck-specific (Neck Disability Index) measures of functional status to allow comparison of our results with those from other studies. The main study results will be submitted for publication in a prominent journal with all actively collaborating investigators acknowledged. The George Institute Marketing and Communication staff will ensure that both the conduct and the results of this study are widely and reliably publicised in the general media, including newspaper, radio talk-back program and TV news items. 3.2.2 Potential Significance This study will provide a definitive evaluation of the effectiveness and cost-effectiveness of a comprehensive exercise program for chronic whiplash. The evaluation of this treatment is critical because for most people with chronic whiplash there are no known effective treatments. Based upon the results of our pilot study we believe we have developed a simple, cost effective, nonsurgical treatment that will decrease pain and disability associated with chronic whiplash and will be available for use by any physiotherapist. The pilot data suggest it would benefit most people with chronic whiplash. Lancet_Web_appendix Draft 7 Page 9 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL The new therapy has resulted from collaboration between Australia’s leading whiplash researchers from The George Institute For International Health and The University of Queensland. This collaboration has allowed us to successfully combine two philosophically and procedurally disparate interventions into a new, simple procedure. The two components have been tested in separate clinical trials and the comprehensive program in a small phase I/II trial. This rigorous scientific approach to developing new treatments is rare in the field of spinal pain and represents a major advance. A search of the WHO International Clinical Trials Registry Platform Search Portal on 28/07/09 revealed no planned or completed trial that would duplicate our work. Lancet_Web_appendix Draft 7 Page 10 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 4. Objectives 4.1 AIMS AND HYPOTHESES OF THE STUDY • The primary aim of this project is to establish the effectiveness of a comprehensive exercise program for chronic whiplash. This program integrates specific motor relearning and graded activity exercises and will be assessed in terms of pain, disability, patient’s global impression of recovery and quality of life. • The second aim is to conduct an economic evaluation of this comprehensive exercise program. • The third aim is to investigate if sensory hypersensitivity and symptoms of posttraumatic stress modify the effect of the comprehensive program. It is hypothesised that: • The effect of the comprehensive exercise program will be greater than that of an educational booklet where effect is measured in terms of pain, disability, patient’s global impression of recovery and quality of life. • The comprehensive exercise program will be more cost-effective than an educational booklet. • The presence of sensory hypersensitivity and/or symptoms of posttraumatic stress modify the effect of the comprehensive program. Lancet_Web_appendix Draft 7 Page 11 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 5. Study design 5.1 DESIGN The study will be a randomised controlled trial evaluating the comprehensive exercise program (specific motor relearning and graded activity exercise) for people with chronic whiplash. A total of 172 voluntary participants with chronic (symptoms > 3 months <5 years duration) whiplash will be randomly allocated to receive either 20 one hour sessions of the comprehensive exercise program over 12 weeks in conjunction with the educational booklet or the educational booklet alone (86 participants per group). Outcomes will be measured at 14 weeks, 6 and 5 years. Results of the treatment program will be supplemented by an economic evaluation of the direct and indirect costs incurred by both the comprehensive exercise program participants and those receiving the educational booklet only. The overall design is illustrated in Figure 5.1. Lancet_Web_appendix Draft 7 Page 12 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL Figure 5.1 Study design Invitation to participate in the study from list of claimants registered with MAA or through print media. Volunteers respond. Participants screened for eligibility via phone call. Inclusion criteria: • Grade I or II whiplash (duration > 3 months < 5 years). • Moderate pain OR moderate activity limitation due to pain. • Not currently receiving care for whiplash. • Aged between 18 and 65 years old. • Proficient in written and spoken English • Able to attend 4 assessment sessions at the trial centre Exclusion criteria: • Serious spinal pathology (e.g. metastatic disease of the spine, spinal fracture). • Nerve root compromise. • Spinal surgery in the past 12 months. • Co-existing medical condition which would severely restrict participation in the exercise program. • Any of the contraindications to exercise listed in the ACSM guideline1. Trial centre screening + baseline measures - Age, gender, level of education - Outcomes - Effect modifiers Concealed random allocation at the trial centre. Referral and initial appointment organised for participant at Physiotherapy treatment site. COMPREHENSIVE EXERCISE PROGRAM + EDUCATIONAL BOOKLET Week 1 – 4: Specific exercise program assessment and prescription (2 sessions per week for 4 weeks) ADVICE AND EDUCATIONAL BOOKLET Participants are allowed to contact the physiotherapist by phone (up to two times only) to clarify information/exercises contained in the educational booklet Week 5 – 12: Graded activity program assessment and prescription (12 sessions over 8 weeks) 14 week assessment (outcomes, side effects, other pain-related treatments and costs) 6 month assessment (outcomes, other pain-related treatments and costs) 12 month assessment (outcomes, other pain-related treatments and costs) Lancet_Web_appendix Draft 7 Page 13 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 5.2 PARTICIPANTS 5.2.1 Participant recruitment A total of 172 participants with chronic (symptoms > 3 months <5 years duration) whiplash will be recruited from the Brisbane and Sydney sites. Participants will be identified through advertisements (Appendix 1) in local and larger metropolitan print media. In NSW participants will also be recruited with the assistance of the Motor Accidents Authority (MAA). The MAA will identify claimants from their database who have sustained a whiplash injury in a motor vehicle accident between two and eleven months previously, this allows time for people to respond and be assessed. These claimants will have a letter sent to them courtesy of the MAA (Appendix 2) informing them of the study and inviting them to participate. People who respond to the invitation to participate in the study will subsequently be screened via a telephone call to identify their eligibility to participate in the trial (Appendix 3). Screening will include a Physical Readiness Questionnaire (PAR-Q) and questions assessing for “red flags”. A positive response to questions in these two screening tools will result in either further review at the trial centre to clarify the response or exclusion from participating in the trial. Volunteers who meet the phone screening criteria will be asked to attend the trial centre where written consent (Appendix 4), and baseline measures will be obtained. A neurological examination will be completed if indicated by the screening procedures (Appendix 5). Immediately following baseline assessment, participants will be randomised and allocated to either the treatment (comprehensive exercise program and educational booklet) or the control group (educational booklet only). A record will be kept of the number of invitations sent out by the MAA (NSW only), the number of potential participants who volunteer to participate, the number of people screened and their eligibility status, if ineligible the reason for their ineligibility will also be documented. The researchers will only have access to the number of invitations, and not to the original records to ensure confidentiality. Therefore, researchers will not have any information about potential participants unless they are recruited into the study. 5.2.2 Inclusion criteria Participants will be included if they meet all of the following inclusion criteria: • Grade I or II whiplash of at least 3 months duration but less than 5 years duration (Figure 5.2). • Currently experiencing at least moderate pain OR moderate activity limitation due to pain (modified items 7 & 8 of SF36). • Not currently receiving care for whiplash. • Aged between 18 years and 65 years old. • Proficient in written and spoke English. 5.2.3 Exclusion criteria Participants will be excluded if they have any of the following: Known or suspected serious spinal pathology (e.g. metastatic disease of the spine). Confirmed fracture or dislocation at time of injury. Nerve root compromise. Spinal surgery in the past 12 months. Any coexisting medical condition which would severely restrict participation in the exercise program e.g. traumatic brain injury. • Any of the contraindications to exercise listed in the ACSM guideline1 as assessed using the PAR-Q and listed below: • • • • • Lancet_Web_appendix Draft 7 Page 14 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Absolute Contraindications to exercise A recent significant change in the resting ECG suggesting infarction or other acute cardiac events. Recent complicated myocardial infarction. Unstable angina. Uncontrolled ventricular dysrhythmia. Uncontrolled atrial dysrhythmia that compromises cardiac function. 3rd degree A-V block. Acute congestive heart failure. Severe aortic stenosis. Suspected or known dissecting aneurysm. Active or suspected myocarditis or pericarditis. Thrombophlebitis or intracardiac thrombi. Recent systemic or pulmonary embolus. Acute infection. Significant emotional distress (psychosis). 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Relative Contraindications Resting diastolic blood pressure > 120 mmHg or resting systolic blood pressure >200 mmHg. Moderate valvular heart disease. Known electrolyte abnormalities (hypokalemia, hypomagnesemia). Fixed-rate pacemaker (rarely used). Frequent or complex ventricular ectopy. Ventricular aneurysm. Cardiomyopathy, including hypertrophic cardiomyopathy. Uncontrolled metabolic disease (e.g. diabetes, thyrotoxicosis, or myxedema). Chronic infectious disease (e.g. mononucleosis, hepatitis, AIDS). Neuromuscular, musculoskeletal, or rheumatoid disorders that are exacerbated by exercise. Advanced or complicated pregnancy. Figure 5.2 – Clinical Classification of Grades of WAD WAD CLASSIFICATION 0 I II III IV No complaint about the neck. No physical sign(s). Neck complaint of pain, stiffness or tenderness only. No physical sign(s). Neck complaint AND musculoskeletal sign(s). Musculoskeletal signs include decreased range of motion and point tenderness. Neck complaint AND neurological sign(s). Neurological signs include decreased or absent tendon reflexes, weakness and sensory deficits. Neck complaint AND fracture or dislocation. Lancet_Web_appendix Draft 7 Page 15 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 5.3 STUDY INTERVENTIONS 5.3.1 Baseline assessment Participants who meet the inclusion criteria will attend the trial centre where all of the primary, secondary baseline measures as well as the effect modifiers will be obtained by a blinded investigator. 5.3.2 Randomisation Participants will be randomly allocated to treatment group. The randomisation schedule will be generated by an independent investigator using a computer program prior to the commencement of the trial. Randomisation will be stratified for each of the trial centres (NSW and QLD) however not for each individual treatment clinics. Consecutively numbered, sealed, opaque envelopes will be used to conceal randomisation. Allocation will occur immediately following the baseline assessment. At this time, an independent (unblinded) researcher will select the next envelope in the box, record the participant’s randomisation number and then open the envelope. In this way concealment of allocation and blinding of baseline measures is ensured. Participants will be considered to have entered the study at the time that the envelope is opened. The independent researcher who randomised the participant will then arrange the initial appointment with the treatment provider site within one week of randomisation. The participant proforma and randomisation envelope will be sent to the treatment clinic prior to the participant’s initial appointment. Those randomised to receive the comprehensive exercise program and educational booklet will have one hour allocated to the initial consultation whilst those in the booklet only group will have a half hour consultation. Participants in both groups will be asked not to seek other treatments and where possible not to change current medications for the twelve-week trial period. Furthermore, the insurance company handling the participant’s claim and the nominated general practitioner will be notified in writing of the individual’s participation in the trial. They will be asked within reason to refrain from referring or suggesting additional or alternative treatments to the individual for the initial twelve weeks after randomisation. 5.3.3 Educational booklet All participants will be provided with the educational booklet ‘Whiplash injury recovery: a self management guide’ written by Professor Gwen Jull and published by the Motor Accident Insurance Commission of Queensland19 The booklet provides information about whiplash, provides advice on how to manage symptoms of whiplash and explains and illustrates an exercise program for whiplash. Participants randomised to receive the educational booklet alone will have one, half-hour physiotherapy consultation where the participant will have time to read the booklet provided, have any questions clarified and be shown the exercises. Participants in this group will, if required, be able to contact the physiotherapist by phone on two occasions to clarify the information/exercise contained in the educational booklet. These participants will subsequently be followed up at the trial centre at 14 weeks, 6 and 12 months after the baseline assessment. 5.3.4 Comprehensive exercise program Participants in the exercise group will in addition to the educational booklet receive the comprehensive exercise program outlined below. Twenty, one-hour treatment session will be delivered by physiotherapists trained specifically to implement the trial treatment over a 12 week period (Table 5.3.4). Please refer to the ‘Therapists Protocol’ for more detail. Lancet_Web_appendix Draft 7 Page 16 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL Table 5.3.4 Outline of the Comprehensive Exercise Program Week Sessions per Components week 1 2 Specific motor relearning exercise component: Baseline & follow-up assessments to guide initial prescription & progression of 2 2 program Exercises to improve cervical and scapular muscle control, kinaesthesia & balance 3 2 Manual therapy if indicated Education and advice 4 2 Progressive home exercise program, aerobic exercise program TRANSITION 5 2 6 2 7 2 8 2 9 1 10 1 11 1 12 1 Graded activity component: Baseline & follow-up assessments to guide initial prescription & progression of program Supervised gym-based exercise to improve the participant’s functional abilities – progress aerobic, range of motion, strength, endurance, coordination and functional exercises. Daily home program including exercise & graded increase of physical activities Graded activity program using Cognitive Behavioural Therapy (CBT) principles Discharge session to reinforce progress and plan for continued activity Specific motor relearning exercise component (8 sessions over 4 weeks) The program begins with a clinical examination of the cervical muscles and the axio-scapular-girdle muscles and includes tests that assess ability to recruit the muscles in a coordinated manner, tests of balance, cervical kinaesthesia and eye movement control and tests of muscle endurance at low levels of maximum voluntary contraction. The specific impairments that are identified are then addressed with an exercise program that is supervised and progressed by the physiotherapist with cognitive behaviour principles (e.g. positive reinforcement and encouragement of skill acquisition by modelling) implemented as required. This specific treatment program has been described in detail20 and focuses on activating and improving the co-ordination and endurance capacity of the neck flexor, extensor and scapular muscles in specific exercises and functional tasks, and a graded program directed to the postural control system, including balance exercises, head relocation exercises and exercises for eye movement control. Manual therapy and/or general whole body aerobic exercise will be prescribed as required by the treating physiotherapist. Participants are expected to practise at home the motor skills they are learning in the therapy sessions. These exercises will be outlined in a home exercise diary which will also be used to monitor participant’s compliance with the program. Graded activity component (12 sessions over 8 weeks) Transition to the graded activity program is flexible and is dependant on the individual’s progress through the earlier stage. The graded activity program can therefore commence between weeks four to six. At the first graded activity exercise session, baseline measures of upper and lower body mobility, coordination, strength and aerobic fitness are taken. From these measures an individualised, sub-maximal, progressive activity program will be developed to train those functions found to be inadequate for performance of preinjury work and home activities. The physiotherapist will guide the participant's return to normal activities using the principles of cognitive-behavioural therapy21 specifically: the encouragement of skill acquisition by modelling, setting progressive goals, self-monitoring of progress, and positive reinforcement of progress. Self-reliance will be fostered by encouraging participants to engage in problem-solving to deal with difficulties rather than seeking reassurance and advice, by encouraging relevant and realistic activity Lancet_Web_appendix Draft 7 Page 17 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL goals, and by encouraging self-reinforcement. Daily physical activity at home will be encouraged and monitored using a diary. Written and illustrated exercise instructions will be provided. 5.3.5 Treatment sites Treatment sites in Sydney and Brisbane will be located in areas easily accessible by public transport. Prior to the commencement of the trial physiotherapists at each treatment site will be provided with a trial and a therapist protocol, they will also be trained to implement the comprehensive exercise program by senior investigators at a one day workshop. 5.3.6 Follow up Measures of outcomes will be taken at 14 weeks, 6 and 12 months after randomisation. To maximise attendance at these follow-ups, appointments will be made by phone (Appendix 6) and then a letter (Appendix 7) will be sent confirming appointment and a phone call 24hours before. Every attempt (within ethical constraints) will be made to obtain outcome data, regardless of the participant’s compliance with the trial protocol. Assessments will be conducted by a blinded investigator. At each follow up, information on the use of other pain-related treatments e.g. health services or medications will be obtained through the economic cost diary. Only at the 14 week follow up will information about side effects be collected from all participants using open-ended questioning. 5.3.7 Premature discontinuation of randomised intervention Participants will have the opportunity to withdraw from the study at any time without prejudice to their current or future medical management. In the event of a participant wishing to withdraw from the study, they will be required to verbally contact study staff and notify them of their decision. Regardless of whether the participant continues to adhere to one or both of the intervention arms, the follow-up schedule should continue unchanged for all randomised participants. If any participant is not able to attend all of the scheduled visits then as far as possible, follow-up should be completed by other means (e.g. alternate visits or telephone follow-up), unless the participant states that he/she also wishes to withdraw from the followup assessments. 5.4 STUDY OUTCOMES 5.4.1 Outcomes Assessments At the baseline assessment, personal characteristics (age, gender, level of education) and information about symptoms of whiplash will be collected (Appendix 8). The following outcome measures will be assessed at baseline, 14 weeks, 6 months and 12 months (Appendix 9). 5.4.2 Primary outcome 1. Average pain intensity over last week (numerical rating 0-10 scale)22 5.4.3 Secondary outcomes 1. Average pain intensity over last 24 hours (numerical 0 to 10 scale)22 2. Patient’s global impression of recovery (-5 to +5 scale)22 3. Patient-generated measure of disability (Patient-Specific Functional Scale)23 4. Neck-specific measure of disability (Neck Disability Index)24 5. Generic measure of health status (SF-36)25 6. Whiplash-specific measure of disability (Whiplash Disability Questionnaire)26 7. Measures of physical impairment (Cervical range of movement – Appendix 10)27 5.4.3 Effect modifiers 1. Cold pain threshold measured over the cervical spine3 (Appendix 11). 2. Pressure pain threshold measured over the cervical spine and the tibialis anterior3 (Appendix 12). 3. Posttraumatic stress symptoms using the Impact of Events Scale (IES)3. 4. Pain Catastrophising Scale (PCS) 5. Post Traumatic Stress Diagnostic Scale (PDS) Lancet_Web_appendix Draft 7 Page 18 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 6. Self-report Leeds Assessment of Neuropathic Symptoms and Signs pain scale (S-LANSS). 5.4.4 Participant diary All participants will be assisted to complete an economic cost diary, in addition to this those randomised to the exercise group will be required to complete a home exercise diary to monitor their compliance with the exercise program. Economic cost diary The economic cost diary (Appendix 14) will be used to identify all the direct and indirect costs associated with the individual’s whiplash injury as they arise. Direct costs can include healthcare costs, transportation costs, medication costs and time spent by family members or volunteers providing care. Indirect costs primarily involve the participant’s lost economic productivity due to poor health. The collection of economic information will coincide with the 14 week, 6 and 12 month follow up assessments. At this time, participants will be asked to recall all direct and indirect costs incurred over the previous two weeks, as a result of their whiplash injury. This method of economic data collection is consistent with Australian Bureau of Statistics National Health Survey. The home exercise diary Those randomised to receive the comprehensive exercise program are expected to complete a home exercise diary (Appendix 15). The home exercise diary will be used to outline the prescribed exercises as well as to monitor the compliance with the exercises as the participant will tick the days on which they complete their program. The treating therapist will assist in the collecting of this data by transposing a copy of the participant’s compliance into the therapist proforma. 5.4.5 Economic evaluation Direct costs (e.g. general practitioner, physiotherapy, chiropractor and pharmaceutical services) will be calculated using schedule consultation fees taken from the Medicare Benefits Schedule, worker’s compensation schemes and the Pharmaceutical Benefits Scheme. Direct health-care and non-health care costs which are not captured by these formal schemes will be identified in participant cost diaries. Participants’ will be assisted to complete cost diaries in order to capture the direct costs; for example, other professional care, transportation costs and time spent by family members or volunteers providing care. The indirect costs associated with their injury include the participant’s lost economic productivity due to poor health. A shadow wage rate will be used to identify the opportunity cost of time spent away from work due to their injury. These costs will be calculated using income and employment data collected at the baseline assessment. Using utility weights derived from participant preferences to health states, the Quality Adjusted Life Years (QALYs) for each participant will be measured. The two widely used techniques to measure directly the preferences of individuals are the visual analogue scale and the standard gamble (Appendix 13). These techniques will be applied to derive upper- and lower-bound estimates of QALYs. These three techniques for eliciting health preferences – or “utility” weights as they are usually called – have different theoretical foundations and are also known to be subject to biases of various kinds 28-30. Using more than one of these methods to derive upper- and lower-bound estimates of QALYs provides an empirical capacity to conduct sensitivity analyses on the QALY denominator of the Cost-utility Analysis ratio. 5.4.6 Reporting of adverse events An adverse event (AE) is any untoward medical occurrence in a participant temporally associated with the trial intervention, whether or not considered related to the trial intervention. Examples of an AE include: • Exacerbation of a pre-existing condition. • New conditions detected or diagnosed after enrolment in the trial. Lancet_Web_appendix Draft 7 Page 19 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL Examples of an AE do not include anticipated day-to-day fluctuations of pre-existing disease(s) or condition(s) present or detected at the start of the study that do not worsen. A serious adverse event (SAE) is one that is life threatening requires inpatient hospitalisation or will result in persistent or significant disability or incapacity. All adverse events will be reported to the Adverse Events Committee for the trial (Chris Maher, Michele Sterling). In NSW, concerns will be addressed to Chris via phone on (02) 9657 0382. In Qld, contact Michele on (07) 3365 5344. In the unlikely event of a SAE, trial recruitment and treatment should be put on hold pending advice from the Adverse Events Committee. The Adverse Events Committee will report all AE and SAE to the relevant ethics committee. STUDY SEQUENCE 5.5 5.5.1 Telephone screening • Assess the participants’ eligibility, willingness and ability to participate • Complete the phone screening assessment forms (Appendix 3) 5.5.2 Baseline Assessment At the baseline assessment the trial coordinator will ensure the following is completed: • Participant informed consent form (Appendix 4) • Contact detail form • Baseline demographic form • Questionnaires – Average pain over the last week (0-10 scale) – Average pain over the last 24 hours (0-10 scale) – Global perceived effect (GPE -5 to + 5 scale) – Neck disability index (NDI) – SF-36 – Whiplash disability questionnaire (WDQ) – Impact of Events Scale (IES) – Pain Catastrophising Scale (PCS) – Post Traumatic Stress Diagnostic Scale (PDS) – Self-report Leeds Assessment of Neuropathic Symptoms and Signs pain scale (SLANSS) – Patient specific functional scale (PSFS) • • • Cervical spine range of movement assessment (Appendix 10) Cold pain threshold over the cervical spine (Appendix 11) Pressure pain threshold measured over the cervical spine and the tibialis anterior (Appendix 12) 5.5.3 Randomisation Immediately following the baseline assessment participants will be randomised. For all participants an independent researcher will: - Select the next envelope in the box and attach it to the competed participant proforma. - Use the randomisation schedule to allocate the next available participant number. - Arrange an initial physiotherapy appointment within one week of randomisation. For participants randomised to receive the educational booklet the initial appointment will be halfhour in duration, for those randomised to receive the comprehensive exercise program the initial appointment will be one hour in duration. - The sealed randomisation envelope and the participant proforma will then be sent to the physiotherapy clinic. The envelope will be opened by the treating physiotherapist and will serve as a confirmation of group allocation. Lancet_Web_appendix Draft 7 Page 20 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 5.5.4 Physiotherapy treatment clinic Participants assigned to the educational booklet The initial consultation for participants randomised to receive the educational booklet will be a maximum of half hour duration. During which the physiotherapist will: - Provide the participant with the educational booklet - Give the participant a short period of time to review the booklet - Discuss and clarify the concepts raised in the booklet - Show the participant the exercises Participants in this group will also be able to contact the physiotherapist by phone on two occasions to clarify the information/exercise contained in the educational booklet. - Remind the participant of the 14 week, 6 month and 12 month follow up assessments to be completed at the trial centre. For participants assigned to the comprehensive exercise program: The initial consultation for participants randomised to comprehensive exercise program will be a maximum of one hour duration. During which the physiotherapist will: - Complete the initial assessment as per the ‘Participant proforma’ - Outline exercises to be completed as part of their home exercise program, making sure a copy of the exercise prescribed are also recorded in the participant proforma. - Arrange a follow up appointment, as per frequency set out in the table under 5.3.4. 5.5.5 14 weeks, 6 and 12 month follow up assessments To be completed by all participants at 14 weeks, 6 and 12 months: • Questionnaires – Average pain over the last week (0-10 scale) – Average pain over the last 24 hours (0-10 scale) – Global perceived effect (GPE -5 to + 5 scale) – Neck disability index (NDI) – SF-36 – Whiplash disability questionnaire (WDQ) – Impact of Events Scale (IES) – Pain Catastrophising Scale (PCS) – Post Traumatic Stress Diagnostic Scale (PDS) – Self-report Leeds Assessment of Neuropathic Symptoms and Signs pain scale (SLANSS) – Patient specific functional scale (PSFS) • Adverse effects of treatment (14 week assessment only Lancet_Web_appendix Draft 7 Page 21 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 5.6 QUALITY ASSURANCE The study will be conducted in accordance with the protocol, Manual of Procedures, ICH Guidelines for Good Clinical Research Practice and with all relevant local ethical regulations. 5.6.1 Monitoring of study sites Prior to commencement of the study, treatment provider sites will be provided with a copy of the Trial and Treatment Protocols. Further, the physiotherapists delivering the trial treatments will be trained to deliver the interventions by experts in the Physiotherapy field. Therapists will be required to sign a clinical trial agreement form which specifies trial obligations, requirements and payments. During the trial, regular contact will be made with the treatment provider sites to ensure that the trial is being conducted according to the protocol and any concerns regarding the implementation of treatment can be addressed in a timely manner. All Physiotherapists will have an advice and treatment session audited by one of the investigators (MS, GJ, TR) to ensure that the therapy is of high quality and in accordance with the protocol. 5.6.2 Data integrity The integrity of trial data will be monitored by regularly scrutinising data sheets for omissions and errors. Data will be double entered and the source of any inconsistencies will be explored and resolved. 5.7 STATISTICAL ISSUES 5.7.1 Statistical analysis and methodological considerations Treatment efficacy variables: We will analyse the effect of treatment separately for each outcome using linear mixed models with time as a repeated factor. The model will account for correlation over time within participants, correlation within clinics and potential confounders (e.g. important prognostic factors). Confounding will be assessed by examining the effect of the potential confounders on the results obtained from the analyses. Any potential confounder whose inclusion changes the estimated treatment effects by a clinically relevant amount will be retained as a confounder. We will obtain estimates of the effect of the intervention by constructing linear contrasts to compare the mean change in outcome from baseline to each time point between the treatment and control groups, with adjustment for the other variables. Effect modifiers: Only those variables listed as effect modifiers in Section 5.4.3 will be assessed for effect modification. This will be done by including a predictor-by-treatment group-by-time interaction term to the mixed models analyses. Effect modification will only be assessed for the primary outcome of average pain intensity over the last week. 5.7.2 Sample size Brookes and colleague’s31 simulations demonstrate that when testing for effect modification, trials have the same power to detect an interaction effect that is twice the size of the main effect. We argue that small interaction effects are not clinically significant and we have planned the study with sufficient power to detect the following clinically important interaction effects: (NB the study can detect main effects half this size) • 2.0 units on the 0-10 Pain intensity scale (estimate for SD= 2.0), • 1.5 units on the 0-10 Patient Specific Functional Scale (estimate for SD = 1.5), • 30 units on the 0-130 Whiplash Disability Questionnaire (estimate for SD = 30), • 2.0 units on the -5 to +5 Global perceived effect impression of recovery scale (estimate for SD 2.0), Lancet_Web_appendix Draft 7 Page 22 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL • • • 6 units on the 0-50 Neck Disability Index (estimate for SD =5.6) 15 points on the 0-100 SF36 physical summary score (estimate for SD =10.0) 15 points on the 0-100 SF36 mental summary score (estimate for SD = 11.0). We have taken the SD estimates from the previous trials we completed that recruited a similar patient cohort8 9 and a published study of the Whiplash Disability Questionnaire26. With specifications of alpha =0.05, power =0.80 and allowing for up to 10% loss to follow-up and 10% treatment non-compliance, a sample size of 86 participants per group will allow us to detect an interaction effect size equal to 1.0 times the SD (the smallest interaction effect size we have specified above) and a treatment main effect of 0.5SD. We understand the study is somewhat overpowered for the main effect of treatment but it is crucial to adequately power the study for the interaction effect 5.8 INDEMNITY The George Institute For International Health and the University of Queensland shall at all times indemnify their study investigators and their staff from claims that may be made against them for any injury sustained by a study participant as a consequence of effects of the interventions used in the study in accordance with this protocol provided the ‘Medicines Australia form of Indemnity for Clinical Trials’ has been signed. 5.9 PUBLICATIONS AND REPORTS The main study results will be submitted for publication in a prominent journal with all actively collaborating investigators acknowledged. The George Institute Public Affairs and Marketing staff will ensure that both the conduct and the results of this study are widely and reliably publicised in the general media, including newspaper, radio talk-back program and TV news items. Individuals meeting the International Committee of Medical Journal Editors (ICMJE) authorship requirements1 are eligible for authorship on study publications. Provision of trial treatment does not meet ICMJE authorship requirements; however trial physiotherapists can elect to be acknowledged in trial publications. 5.10 FUNDING The Chronic Whiplash Exercise Trial is funded by a grant from the University of Sydney, University of Queensland, Motor Accidents Authority New South Wales, Motor Accidents Insurance Commission Queensland and National Health and Medical Research Council. The study was initiated and designed by the investigators, independently of The George Institute For International Health, University of Queensland, Motor Accidents Authority NSW and Motor Accidents Insurance Commission Queensland, and the data will be collected, analysed and published independently of these parties. 5.11 TIMELINE 1. All participating personnel will be trained for the trial by July 2009. 2. Recruitment of participants will commence at the end of August 2009. 3. 100% of participants will be recruited and treatment completed by December 2010. 4. 100% of 12 month follow-up data collected and entered by December 2011. 5. Data analysis and manuscript completed by May 2012. 1 1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; 2) drafting the article or revising it critically for important intellectual content; and 3) final approval of the version to be published. Authors should meet conditions 1, 2, and 3. Lancet_Web_appendix Draft 7 Page 23 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 6. References: 1. Dwyer G, Davis S, editors. ACSM's health-related physical fitness assessment manual / American College of Sports Medicine. Philadelphia: Lippincott Williams & Wilkins, 2005. 2. Rebbeck T, Sindhusake D, Cameron I, Rubin G, Feyer A-M, Walsh J, et al. A prospective cohort study of health outcomes following whiplash associated disorders in an Australian population. Injury Prevention 2006; 12:93-86. 3. Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R. Physical and psychological factors predict outcome following whiplash injury. Pain 2005; 114(1-2):141-8. 4. Motor Accidents Authority of NSW. Whiplash and the NSW Motor Accidents Scheme. Statistical Information Paper No 7. Sydney: Motor Accidents Authority of NSW, 1999. 5. Kamper S, Rebbeck T, Maher C, McAuley J, Sterling M. Course and prognostic factors of whiplash: a systematic review and meta-analysis. Pain 2008; 138: 617-629. 6. Verhagen AP, Scholten-Peeters G, van Wijngaarden S, de Bie RA, Bierma-Zeinstra SMA. Conservative treatments for whiplash [Systematic Review]. Cochrane Database of Systematic Reviews 2007; 4:4. 7. Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. New England Journal of Medicine 1996; 335(23):1721-6. 8. Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Bogduk N, Nicholas M. Randomized controlled trial of exercise for chronic whiplash-associated disorders. Pain 2007; 128(1-2):59-68. 9. Jull G, Sterling M, Kenardy J, Beller E. Does the presence of sensory hypersensitivity influence outcomes of physical rehabilitation for chronic whiplash? - A preliminary RCT. Pain 2007; 129(1-2):28-34. 10. Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Annals of Internal Medicine 2005; 142(9):776-85. 11. Sterling M, Jull G, Vicenzino B, Kenardy J. Characterization of acute whiplash-associated disorders. Spine 2004; 29(2):182-8. 12. Sterling M. A proposed new classification system for whiplash associated disorders--implications for assessment and management. Manual Therapy 2004; 9(2):60-70. 13. Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R. Development of motor system dysfunction following whiplash injury. Pain 2003; 103(1-2):65-73. 14. Sterling M, Jull G, Vicenzino B, Kenardy J. Sensory hypersensitivity occurs soon after whiplash injury and is associated with poor recovery. Pain 2003; 104(3):509-17. 15. Sterling M, Jull G, Kenardy J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain 2006; 122(1-2):102-108. 16. van Tulder MW, Furlan A, Bombardier C, Bouter L, and the Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003; 28(12):1290-1299. 17. Stewart M, Maher CG, Refshauge KM, Bogduk N, Nicholas M. Responsiveness of pain and disability measures for chronic whiplash. Spine 2007; 32(5):580-5. 18. Westaway M, Stratford P, Binkley J. The patient-specific functional scale: validation of its use in persons with neck dysfunction. Journal of Orthopaedic and Sports Physical Therapy 1998; 27(5):331-338. 19. Jull G. Whiplash injury recovery a self-management guide. http://www.maic.qld.gov.au/formspublications-stats/pdfs/whiplash-injury-recovery-booklet.pdf, 2005. 20. Jull G, Treleaven J, Falla D, Sterling M, O'Leary S. A therapeutic exercise approach for cervical disorders. In: Boyling J, Jull G, editors. Grieves' Modern Manual Therapy of the Vertebral Column. 3 ed. Edinburgh: Elsevier Churchill Livingstone, 2004:451-470. 21. Nicholas M, Tonkin L. Persisting pain: using cognitive-behavioural principles for activity-based pain management. In: Refshauge K, Gass E, editors. Musculoskeletal Physiotherapy. Clinical science and evidence-based practice. 2nd ed. Oxford: Butterworth Heinneman, 2004. 22. Pengel L, Maher C, Refshauge K. Responsiveness of pain, disability and physical impairment outcomes in subjects with low back pain. Spine 2004; 29:879-883. 23. Westaway MD, Stratford PW, Binkley JM. The patient-specific functional scale: validation of its use in persons with neck dysfunction. Journal of Orthopaedic and Sports Physical Therapy 1998; 27(5):3318. Lancet_Web_appendix Draft 7 Page 24 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 24. Vernon H, Mior S. The neck disability index: A study of reliability and validity. Journal of Manipulative and Physiological Therapeutics 1991; 14(7):409-415. 25. Ware J, Sherbourne C. The MOS 36-item short-form health survey (SF-36). 1. Conceptual framework and item selection. Med Care 1992; 30:473-483. 26. Willis C, Niere KR, Hoving JL, Green S, O'Leary EF, Buchbinder R. Reproducibility and responsiveness of the Whiplash Disability Questionnaire. Pain 2004; 110(3):681-8. 27. Hole D, Cook J, Bolton J. Reliability and concurrent validity of two instruments for measuring cervical range of motion: effects of age and gender. Manual Therapy 1995; 1:36-42. 28. Bleichrodt H. A new explanation for the difference between Time Trade-Off Utilities and Standard Gamble Utilities. Health Economics 2002; 11(5):447-456. 29. Brazier J. Use of visual analogue scales in economics evaluation. Expert Review of Pharmacoeconomics and Outcomes Research 2003; 3(3):293-302. 30. Oliver A. The internal consistency of the Standard Gamble tests after adjusting for prospect theory. Health Economics 2003; 22(4):659-674. 31. Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G. Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives. Health Technology Assessment 2001; 5(33):1-56. Lancet_Web_appendix Draft 7 Page 25 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL 7. Appendices APPENDIX 1 – PROMISE ADVERTISEMENT Lancet_Web_appendix Draft 7 Page 26 of 102 APPENDIX 2 – MOTOR ACCIDENTS AUTHORITY LETTER OF INVITATION PARTICIPANT INFORMATION SHEET Insert Name Insert Address Re: A randomised controlled trial of a comprehensive exercise program for chronic whiplash I am writing on behalf of the Motor Accidents Authority (MAA) of NSW to invite you to participate in a physiotherapy research study for the treatment of whiplash. The MAA is the NSW Government department that oversees all aspects of the Compulsory Third Party (Green Slips) scheme including the number and type of claims. You have been invited to participate in the research because the MAA claims information indicates that you have had a whiplash injury in the last 5 years. The MAA and National Health and Medical Research Council are funding this important research to find out about the best treatment for chronic whiplash. While there is no clear agreement about what treatments work best for chronic whiplash, we do know that long term neck pain has many negative effects on people’s enjoyment of life. This research will be conducted by experts at the George Institute for International Health, The University of Sydney, and The University of Queensland. The study consists of a 12-week program that begins with exercises for the neck and then progresses to exercise for the whole body. The treatments offered by the study are free. Your participation in this trial is purely voluntary and be assured that your details will remain confidential at all times. Participation in the study will not affect your ongoing medical treatment or relationship with medical staff. If you are interested in participating or would like further details please contact the George Institute study coordinator Zoe Michaleff. For your information, we have attached a detailed information sheet about the study. Phone: (02) 9657 0321 Fax: (02) 9657 0301 Email: zmichaleff@george.org.au Yours Sincerely Carmel Donnelly A/ General Manager Lancet_Web_appendix Draft 7 Page 27 of 102 Musculoskeletal Division George Institute for International Health Level 7, 341 George St, Sydney, NSW Sydney Medical School ABN 15 211 513 464 Prof Christopher Maher, PhD Director, Musculoskeletal Division The George Institute for International Health Professor, Sydney Medical School The University of Sydney PO Box M201, Missenden Rd Sydney, NSW 2050 AUSTRALIA Telephone: +61 2 9657 0382 Facsimile: +61 2 9657 0301 Email: cmaher@george.org.au A randomised controlled trial of a comprehensive exercise program for chronic whiplash Sydney Investigators Prof Chris Maher, A/Prof Jane Latimer, Dr Christine Lin, Dr Trudy Rebbeck, Miss Zoe Michaleff PARTICIPANT INFORMATION STATEMENT This study is funded by the Motor Accidents Authority of New South Wales, Motor Accidents Insurance Commission of Queensland and the National Health and Medical Research Council. Data is being collected in Sydney and Brisbane. The Sydney site is led by Professor Chris Maher and Associate Professor Jane Latimer of the George Institute for International Health. The Brisbane site is led by Associate Professor Michele Sterling and Professor Gwen Jull from the University of Queensland. There are no medical treatments that have been shown to be effective for chronic or persistent whiplash. You are invited to take part in a research study evaluating physiotherapy treatment of chronic or persistent whiplash. The aim is to investigate the effectiveness and cost-effectiveness of a comprehensive exercise program for chronic whiplash. The exercise program begins with exercises for the neck and then progresses to exercise for the whole body. At present we do not know if this program is helpful for people with chronic whiplash. The only way to find this out is to conduct a randomised controlled trial. If you agree to participate in this study, you will be requested to complete assessments at enrolment and then 14 weeks, 6 and 12 months later. The assessments comprise of some questionnaires and a physical examination. The first assessment will take one hour and the follow-ups 30 minutes. You will also need to complete a diary to record your health care costs for whiplash. Questionnaires You will be asked to complete a series of questionnaires seeking information on the accident history, current symptoms, any treatment received to date, compensation status, employment status and weekly income along with time lost from paid employment and unpaid duties (e.g. home duties). You will also be asked to complete questionnaires relating to how your neck pain is affecting your daily activities and in what way your neck pain is affecting you personally. Page 1 of 2 Lancet_Web_appendix Draft 7 Page 28 of 102 Physical Examination The physical examination will provide information about how the joints, muscles and nerves in your neck and upper body are working. Throughout the physical testing procedures, any pain experienced will be constantly monitored and you will be asked to record its level on a scale of 1 to 10. All testing procedures will be explained to you in greater detail just prior to being performed. A summary is provided below. The following physical tests will be performed: • Your neck movements will be tested and this simply requires you to move your head through its normal range of movement. We will place an inclinometer next to your head to measure the range of movement. • Pressure algometry will be performed. This involves the application of a small pressure sensor to various regions on your neck and limbs. The pressure is gradually increased until the moment you first perceive it to be painful, upon which you press a button and the test will cease. No tissue damage will occur at this low intensity. Any local soreness should ease rapidly. • Cold pain thresholds will be measured. This involves the application of a small thermode (element) to various regions on your neck and limbs. The temperature of the thermode will decrease until the moment when you perceive it to be painful, upon which you will press a button and the test will cease. The test will be then repeated three times, and then will be done using a heat stimulus instead of cold. The thermode has both upper and lower safety cut-off points to ensure that no tissue damage will occur. An occasional side effect of such a thorough examination could be a temporary flare-up of your usual symptoms, but this should settle. Don’t hesitate to take your normal medication if warranted after the assessment. All participants will be provided with an educational booklet on whiplash. The booklet provides information about whiplash, provides advice on how to manage symptoms of whiplash and explains and illustrates an exercise program for whiplash. This is the standard way people with chronic whiplash are managed. You will then be randomly assigned to either the exercise or booklet group. Participants in the exercise group will be asked to attend 20 one-hour treatments over a 12-week period delivered at physiotherapy clinics by trained personnel. Participants in the booklet group will receive one physiotherapy consultation and up to two telephone calls to the physiotherapist to review the educational booklet, you do not need to attend for additional treatment. All aspects of the study, including results, will be strictly confidential and only the investigators named above will have access to information on participants. Should documents be subpoenaed, researchers are bound by law to produce them. A report of the study may be submitted for publication, but individual participants will not be identifiable in such a report. Participation in this study is entirely voluntary: you are not obliged to participate and - if you do participate - you can withdraw at any time without prejudice or penalty. Whatever your decision, it will not affect your medical treatment or your relationship with medical staff. When you have read this information, the research assistant will discuss it with you further and answer any questions you may have. If you would like to know more at any stage, please feel free to contact Dr Christine Lin (8238 2437). This information sheet is for you to keep. Any person with concerns or complaints about the conduct of a research study can contact the Senior Ethics Officer, Ethics Administration, University of Sydney on (02) 9351 4811 (Telephone); (02) 9351 6706 (Facsimile) or gbriody@usyd.edu.au (Email). Page 2 of 2 Lancet_Web_appendix Draft 7 Page 29 of 102 CHRONIC WHIPLASH EXERCISE TRIAL APPENDIX 3 – PHONE SCREENING TELEPHONE SCREENING FORM NAME: _________________________________ DATE OF CONTACT: __________________________ INCLUSION (must respond YES to the following) • Is your neck pain a result of a MVA? Y/N • Was the MVA 3 – 5 years ago? Y/N Date of injury: ______________________________ • Are you aged between 18 and 65 years? Y/N • Are you able to attend 4 assessment sessions at the trial centre over 12 months? (Sydney: The George Institute For International Health; Brisbane: UQ RBWH Lab) • Y/N Are you fluent in spoken and written English? Y/N Ask the participant the most appropriate response to the following questions relating to their neck pain. • How much neck pain have you had during the past four weeks? no neck pain very mild mild moderate severe very severe • During the past four weeks, how much did your neck pain interfere with your normal work (including both work outside the home and housework)? not at all a little bit moderately quite a bit extremely (**NB participants must rate their pain as moderate to high in one or both questions) • Numerical rating scale: 0 = no pain, 10 = worst imaginable pain. ___/10 EXCLUSION (must respond NO to all) • Are you currently receiving any other care for whiplash besides seeing the GP? • Did you suffer a head injury, fractures or dislocations at the time of the injury (WAD IV)? Y / N • Do you have any other medical condition affecting your spine (e.g. metastatic, inflammatory or infective disease of the spine)? • Y/N Y/N Do you have any weakness or altered sensation in the arm(s) beyond the shoulder? If yes, the participant will require a neurological examination at the lab assessment (tick) • Y/N Have you had spinal surgery in the past 12 months? Lancet_Web_appendix Draft 7 Y/N Page 30 of 102 CHRONIC WHIPLASH EXERCISE TRIAL Physical Activity Readiness Questionaire (PAR-Q) • Has your doctor ever said that you have a heart condition or that you should only do physical activity recommended by a doctor? Y/N • Do you feel pain in your chest when you do physical activity? Y/N • In the past month, have you had chest pain when you were not doing physical activity? Y/N • Do you lose your balance because of dizziness or do you ever lose consciousness? Y/N • Do you have a bone or joint problem that could be made worse by a change in physical activity? Y/N • Is you doctor currently prescribing drugs (for example water pills) for your blood pressure or heart condition? Y/N • Do you know of any other reason why you should NOT do physical activity? Y/N (Yes in response to any of the above questions may result in either exclusion OR a review at the trial centre to clarify responses) Make the patient aware that: All participants will receive evidence-based physiotherapy exercise treatment, but they will receive either: 1) The educational booklet in addition to one advice session with a physiotherapist. Exercises will self managed and guided by the educational booklet. You will have access to contact the physiotherapist on two occasions if required. OR 2) The educational booklet in addition to 20 sessions with a physiotherapist over 12 weeks and be guided through the exercises. (Encourage the participants to appreciate that group 1 are not ‘hard-done by’, there are benefits to being in both groups!) The study runs for twelve months and involves: • Attending the trial centre for an initial assessment (Sydney: The George Institute For International Health; Brisbane: UQ RBWH Lab). This will involve sensory tests ROM and questionnaires, under the guidance of a physiotherapist. None of the tests are painful. • Follow up assessments completed at 14 weeks, 6 and 12 months after randomisation and will include the same measures as the initial assessment. • Maintaining a diary for the 12 month period of health related costs (practitioner costs, medication) related to the whiplash injury. • No personal financial cost for the participant, however they will be reimbursed for travelling costs (up to $60) each time they attend the laboratory for assessment. Has the participant agreed to participate? Y/N If yes, initial appointment date/time: ___________________ Contact details: Address: ______________________________________________________________________________ Phone: _________________________________ DOB: ____/____/____ Mobile: _______________________________ Gender: M / F E-mail: ________________________________________________________________________________ Lancet_Web_appendix Draft 7 Page 31 of 102 APPENDIX 4 – PARTICIPANT WRITTEN CONSENT FORM Musculoskeletal Division George Institute for International Health Level 7, 341 George St, Sydney, NSW Sydney Medical School ABN 15 211 513 464 Prof Christopher Maher, PhD Director, Musculoskeletal Division The George Institute for International Health Professor, Sydney Medical School The University of Sydney PO Box M201, Missenden Rd Sydney, NSW 2050 AUSTRALIA Telephone: +61 2 9657 0382 Facsimile: +61 2 9657 0301 Email: cmaher@george.org.au A randomised controlled trial of a comprehensive exercise program for chronic whiplash PARTICIPANT CONSENT FORM I, ............................................................................................................................................................... [name] have read and understood the information for participants on the above named research study and have discussed it with the researcher/s. I am aware of the procedures involved in the study, including any inconvenience, risk, discomfort or side effect, and of their implications. I freely choose to participate in this study and understand that I can withdraw without compromise at any time. I also understand that the research study is strictly confidential however should documents be subpoenaed, researchers are bound by law to produce them. I hereby agree to participate in this research study. Signature: ........................................................................................................................................................... Name:.................................................................................................................................................................. Date:.................................................................................................................................................................... Investigator’s signature: ...................................................................................................... Investigator’s name: .......................................................................................................................................... Date:.................................................................................................................................................................... Page 1 of 1 Lancet_Web_appendix Draft 7 Page 32 of 102 APPENDIX 5 – NEUROLOGICAL EXAMINATION CHRONIC WHIPLASH EXERCISE TRIAL TRIAL CENTRE SCREENING Review PHONE SCREENING Neurological examination required? YES Participant name ___________________ Date: ___________________ NO NEUROLOGICAL EXAMINATION MUSCLE STRENGTH LEFT RIGHT C4 (sh. elevation) C5 (sh. abd) C6 (elbow flexors) C7 (elbow extensors) C8 (wrist extensors) T1 (finger abd) SENSATION Light touch L=R L<R Sharp/blunt discrimination (if req) : Dermatomal distribution YES L>R NO REFLEXES L=R L=R Biceps Triceps ELIGIBLE SIGNED CONSENT obtained Proceed to baseline questionnaires INELIGIBLE Lancet_Web_appendix Draft 7 Page 33 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL APPENDIX 6 – TELEPHONE SCRIPT TO ARRANGE FOLLOW-UP ASSESSMENTS Script for phone call to set date and time for follow-ups • Phone participant • Ask to speak to participant • Greet participant and thank them for their participation to date • State that their next follow-up is due and offer them some times to choose from Once a mutually convenient time is agreed thank the participant and state that you will send them a letter confirming details and will make a reminder telephone call to them 24hrs prior to the appointment Script for 24hour phone call reminder • Phone participant • Ask to speak to participant • Greet participant and thank them for their participation to date • Remind them of their agreed appointment and confirm that they are still able to attend. • If appointment confirmed thank them and conclude call • If unable to attend organise an alternate time. Thank the participant and state that you will send them a letter confirming details and will ring them 24hrs prior to appointment. Lancet_Web_appendix Draft 7 Page 34 of 102 APPENDIX 7 – LETTER CONFIRMING APPOINTMENT Musculoskeletal Division George Institute for International Health Level 7, 341 George St, Sydney, NSW Sydney Medical School ABN 15 211 513 464 Prof Christopher Maher, PhD Director, Musculoskeletal Division The George Institute for International Health Professor, Sydney Medical School The University of Sydney PO Box M201, Missenden Rd Sydney, NSW 2050 AUSTRALIA Telephone: +61 2 9657 0382 Facsimile: +61 2 9657 0301 Email: cmaher@george.org.au A randomised controlled trial of a comprehensive exercise program for chronic whiplash <Participants name> <Participants address> CONFIRMATION OF FOLLOW UP APPOINTMENT Dear <name>, Thank you for your contribution to the Chronic Whiplash Exercise Trial. As discussed by phone your next follow-up appointment is <insert date & time> at The George Institute For International Health, Level 7, 341 George St, Sydney. If you have a change of circumstances and cannot make this appointment please contact me immediately and I will reschedule the appointment. Regards Zoe Michaleff Trial Coordinator Ph: (02) 9657 0321 Mob: 0400 369 348 Email: zmichaleff@george.org.au Lancet_Web_appendix Draft 7 Page 35 of 102 APPENDIX 8 – BASELINE DEMOGRAPHIC DETAILS FORM Chronic Whiplash Exercise Trial - Initial Assessment Participant’s Initials Participant Number Date _____/_____/_____ CONFIDENTIAL INFORMATION Please be assured that the information asked on this form will remain confidential at all times. It is collected for statistical purposes only. 1. Working Status: Employed (Occupation _______________________) Self Employed (Occupation ____________________) Home Duties Unemployed Retired Entitled leave (long service, maternity, sick leave) Student 2. If employed/self employed, are you: Currently working usual hours Working reduced hours due to whiplash injury IF REDUCED, indicate percentage of usual hours ______% Not working due to whiplash injury 3. Please indicate your gross (i.e., pre-tax) income by ticking a box. Your income may be entered as either ‘gross annual income’ or ‘gross weekly income’. Gross Annual Income Nil Income $1 - $9,999 $10,000 - $19,999 $20,000 - $29,999 $30,000 - $39,999 $40,000 - $49,999 $50,000 - $59,999 $60,000 - $69,999 $70,000 - $79,999 $80,000 - $89,999 $90,000 - $99,999 $100,000 - $109,999 $110,000 - $119,999 $120,000 - $129,999 $130,00 - $139,999 $140,000 - $149,999 ≥ $150,000 Lancet_Web_appendix Draft 7 Gross Weekly Income $1 - $191 per week $192 - $384 $385 - $577 $578 - $768 $769 - $961 $962 - $1,153 $1,154 - $1,345 $1,346 - $1,537 $1,538 - $1,730 $1,731 - $1,922 $1,923 - $2,114 $2,115 - $2,307 $2,308 - $2,499 $2,500 - $2,691 $2,692 - $2,884 ≥ $2,885 Page 36 of 102 APPENDIX 8 – BASELINE DEMOGRAPHIC DETAILS FORM Chronic Whiplash Exercise Trial - Initial Assessment 4. Participant’s Initials Participant Number _____/_____/_____ Date Education: Please indicate the highest grade you completed at school: _____________________ Please list any further qualifications and/or trades you have gained since leaving school, including their full-time duration: 5. Qualification 1: Length of course Qualification 2: Length of course Qualification 3: Length of course Qualification 4: Length of course Have you lodged a compensation claim for this injury: Yes No If yes Please select what type of compensation claim: CTP Workers Compensation Other (please list) ______________________ Has your claim been settled? 6. Yes No Have you engaged the services of a solicitor with respect to your whiplash injury? Yes Lancet_Web_appendix Draft 7 No Page 37 of 102 APPENDIX 8 – BASELINE DEMOGRAPHIC DETAILS FORM Chronic Whiplash Exercise Trial - Initial Assessment Participant’s Initials Participant Number Date _____/_____/_____ PERSONAL DETAILS Title: Name: D.O.B.: Gender: M / F (Please circle) Address: Postcode: Phone (H): Phone (W): Mobile: Email: Please fill in the contact details for 2 people (a relative, and a friend) who are not living with you. This information is only to be used to help us to find you if we lose contact. Name: Relationship: Address: Postcode: Phone (H): Phone (W): Mobile: Email: Name: Relationship: Address: Postcode: Phone (H): Phone (W): Mobile: Email: Please fill in the contact details for your regular GP below: GP Name: Phone Address: Postcode: Lancet_Web_appendix Draft 7 Page 38 of 102 APPENDIX 8 – BASELINE DEMOGRAPHIC DETAILS FORM Participant’s Initials Chronic Whiplash Exercise Trial - Initial Assessment Participant Number _____/_____/_____ Date ACCIDENT HISTORY Date of Accident: _____/_____/_____ 1. At the time of the accident were you: The driver The front seat passenger A back seat passenger Riding a motorbike 2. Did you know the accident was coming? Yes 3. For the vehicle you were in was the collision: Rear end Rear and front end Front end Side impact 4. Was the vehicle you were in stationary at the time of impact? Yes No EVENTS FOLLOWING ACCIDENT 1. Following the car accident, did your neck pain start: No Immediately Within 24 hours After 24 hours 2. Was your neck movement restricted following the accident? Not at all Mildly Moderately Severely 3. Did the restriction in movement start: Immediately Within 24 hours After 24 hours 4. Did you lose consciousness immediately after the accident? 5. Were you admitted to hospital after the accident? Yes Yes No Yes No No MEDICAL HISTORY 1. Have you had any major surgery or other injuries? If YES – Please give details: __________________________________________________ __________________________________________________________________________________ __________________________________________________________________ 2. Do you suffer from any other medical conditions? Yes No If YES – Please give details: __________________________________________________ __________________________________________________________________________________ __________________________________________________________________ Lancet_Web_appendix Draft 7 Page 39 of 102 APPENDIX 8 – BASELINE DEMOGRAPHIC DETAILS FORM Chronic Whiplash Exercise Trial - Initial Assessment 3. Participant’s Initials Participant Number Date _____/_____/_____ Have any of the following investigations been performed for your neck pain? Yes, please indicate the investigations you have had and any significant findings below No, please proceed to question 4 X-ray – Significant findings NO YES Please give details: ______________________________________________________________________________________ ___________________________________________________________________ CT – Significant findings NO YES Please give details: ______________________________________________________________________________________ ____________________________________________________________________ MRI – Significant findings NO YES Please give details: ______________________________________________________________________________________ ____________________________________________________________________ 4. What treatments have you received for your neck pain since your accident? Type of treatment Number of sessions (Approximately) Physiotherapy _______ Chiropractic _______ Massage _______ Acupuncture _______ Other: _____________________ _______ Other: _____________________ _______ Surgical procedures SYMPTOMS Please mark on the body chart below where you feel pain or any other symptoms e.g. pins and needles or numbness. Lancet_Web_appendix Draft 7 Page 40 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL APPENDIX 9 – OUTCOME ASSESSMENTS PRIMARY OUTCOME MEASURE AVERAGE PAIN INTENSITY OVER THE LAST WEEK Rate your pain on a scale from 0 to 10 where 0 represents no pain and 10 is the worst pain possible. Please circle the number which best describes your average pain over the past week. 0 No Pain 1 2 3 4 5 6 7 8 9 10 Worst possible pain SECONDARY OUTCOME MEASURES AVERAGE PAIN INTENSITY OVER THE LAST 24 HOURS Rate your pain on a scale from 0 to 10 where 0 represents no pain and 10 is the worst pain possible. Please circle the number which best describes your average pain over the past 24 hours. 0 No Pain 1 2 3 4 5 6 7 8 9 10 Worst possible pain GLOBAL PERSEVERD EFFECT (GPE) With respect to your whiplash injury, compared to when you entered the study, how would you describe yourself these days? (circle the most appropriate) -5 Vastly Worse -4 -3 Lancet_Web_appendix Draft 7 -2 -1 0 Unchanged 1 2 3 4 5 Completely Recovered Page 41 of 102 NECK DISABILITY INDEX (NDI) INSTRUCTIONS: This questionnaire is designed to enable us to understand how much your neck pain has affected your ability to manage everyday activities. Please answer each question by ticking () ONE CHOICE that most applies to you. We realise that you may feel that more than one statement may relate to you, but PLEASE JUST TICK () THE ONE CHOICE, WHICH CLOSELY DESCRIBES YOUR PROBLEM RIGHT NOW. 4. READING 8. DRIVING (omit this question if you never drive a I can read as much as I want to with no pain in my car when in good health) neck. 1. PAIN INTENSITY I can drive my car without neck pain. I can read as much as I want with slight pain in my I have no pain at the moment. I can drive my car as long as I want with slight pain neck. The pain is mild at the moment. in my neck. I can read as much as I want with moderate pain in I can drive my car as long as I want with moderate The pain comes and goes and is moderate. my neck. pain in my neck. The pain is moderate and does not vary much. I cannot read as much as I want because of I cannot drive my car as long as I want because of moderate pain in my neck. The pain is severe but comes and goes. moderate pain in my neck. I cannot read as much as I want because of severe The pain is severe and does not vary much. I can hardly drive my car at all because of severe pain in my neck. pain in my neck. I cannot read at all. I cannot drive my car at all. 5. HEADACHE I have no headaches at all. 2. PERSONAL CARE 9. NECK PAIN AND SLEEPING I have slight headaches which come infrequently. I can look after myself without causing extra pain. I have no trouble sleeping. I have moderate headaches which come I can look after myself normally but it causes extra My sleep is slightly disturbed (less than 1 hour infrequently. pain. sleepless). I have moderate headaches which come frequently. It is painful to look after myself and I am slow and My sleep is mildly disturbed (1-2 hours sleepless). I have severe headaches which come frequently. careful. My sleep is moderately disturbed (2-3 hours I have headaches almost all the time. I need some help, but manage most of my personal sleepless). care. My sleep is greatly disturbed (3-5 hours sleepless). 6. CONCENTRATION I need help every day in most aspects of self-care. My sleep is completely disturbed (5-7 hours I can concentrate fully when I want to with no sleepless). I do not get dressed, I wash with difficulty and stay difficulty. in bed. I can concentrate fully when I want to with slight 3. LIFTING 10. RECREATION difficulty. I can lift heavy objects without extra pain I am able to engage in all recreational activities with I have a fair degree of difficulty concentrating when I can lift heavy objects but it causes extra pain no pain in my neck at all. I want to. Pain prevents me from lifting heavy objects off the I am able to engage in all recreational activities with I have a lot of difficulty concentrating when I want floor, but I can if they are conveniently positioned, for some pain in my neck. to. example on a table. I am able to engage in most, but not all recreational I have a great deal of difficulty concentrating when Pain prevents me from lifting heavy objects, but I activities because of pain in my neck. I want to. can manage light to medium weights if they are I am able to engage in a few of my usual I cannot concentrate at all. conveniently positioned. recreational activities because of pain in my neck. I can lift very light weights. I can hardly do any recreational activities because Lancet_Web_appendix Draft 7 Page 42 of 102 I cannot lift or carry anything at all. Lancet_Web_appendix Draft 7 of pain in my neck. I cannot do any recreational activities at all. Page 43 of 102 SF-36 (Generic measure of health status) This questionnaire asks for your views about your health, how you feel and how well you are able to do your usual activities. Answer each question by marking the answer as indicated. If you are unsure about how to answer a question, please give the best answer you can. 1. 2. 3. In general, would you say your health is: Excellent Very good Good Fair Poor Compared to one year ago, how would you rate your health in general now? Much better than one year ago Somewhat better than one year ago About the same as one year ago Somewhat worse than one year ago Much worse than one year ago. The following are about activities you might do during a typical day. Does your health limit you in these activities? If so, how much? Yes, limited a lot Yes, limited a little No, not limited at all Vigorous activities, such as running, lifting heavy objects, participating in strenuous sports Moderate activities, such as moving a table, pushing a vacuum cleaner, bowling or playing golf Lifting or carrying groceries Climbing several flights of stairs Climbing one flight of stairs Bending, kneeling or stooping Walking more than one kilometre Walking half a kilometre Walking 100 metres Bathing or dressing yourself Lancet_Web_appendix Draft 7 Page 44 of 102 4. During the past 4 weeks, have you had any of the following problems with your work or other regular daily activities as a result of your physical health? Yes No Cut down the amount of time you spent on work or other activities Accomplished less than you would like Were limited in the kind of work or other activities Had difficulty performing the work or other activities (for example, it took extra effort) 5. During the past 4 weeks, have you had any of the following problems with your work or other regular daily activities as a result of any emotional problems (such as feeling depressed or anxious)? Yes No Cut down the amount of time you spent on work or other activities Accomplished less than you would like Didn't do work or other activities as carefully as usual 6. 7. 8. During the past 4 weeks, to what extent has your physical health or emotional problems interfered with normal social activities with family, friends, neighbours, or groups? Not at all Slightly Moderately Quite a bit Extremely How much bodily pain have you had during the past 4 weeks? No bodily pain Very mild Mild Moderate Severe Very severe During the past 4 weeks, how much did pain interfere with your normal work (including both work outside the home and housework)? Not at all A little bit Moderately Quite a bit Extremely Lancet_Web_appendix Draft 7 Page 45 of 102 9. These questions are about how you feel and how things have been with you during the past 4 weeks. For each question, please give the one answer that comes closest to the way you have been feeling. How much of the time during the past 4 weeks: All of the time Most of the time A good bit of the time Some of the time A little of the time None of the time Did you feel full of life? Have you been a very nervous person? Have you felt so down in the dumps that nothing could cheer you up? Have you felt calm and peaceful? Did you have a lot of energy? Have you felt down? Did you feel worn out? Have you been a happy person? Did you feel tired? 10. During the past 4 weeks, how much of the time has your physical health or emotional problems interfered with your social activities (like visiting friends, relatives, etc.)? All of the time Most of the time Some of the time A little of the time None of the time. 11. How TRUE or FALSE is each of the following statements for you? Definitely true Mostly true Don't know Mostly false Definitely false I seem to get sick a little easier than other people I am as healthy as anybody I know I expect my health to get worse My health is excellent Lancet_Web_appendix Draft 7 Page 46 of 102 WHIPLASH DISABILITY QUESTIONNAIRE (WDQ) This questionnaire has been designed to provide information on the impact that your whiplash injury and symptoms have upon your lifestyle. Please circle a number in each section to indicate how you have been affected by the whiplash injury and symptoms. If one or more questions are not relevant to you (e.g. you don’t participate in sporting activities), please indicate this by writing N/A next to the question. 1. 0 No Pain How much pain do you have today? 1 2. 0 Not at all 3. 0 Not at all 4. 0 Not at all 5. 0 Not at all 6. 0 Not at all 7. 0 Not at all 2 3 4 5 6 7 8 9 10 Worst possible pain Do your whiplash symptoms interfere with your personal care (washing, dressing etc.)? 1 2 3 4 5 6 7 8 9 10 Unable to perform 8 9 10 Unable to perform Do your whiplash symptoms interfere with your work/home/study duties? 1 2 3 4 5 6 7 Do your whiplash symptoms interfere with driving or using public transport? 1 2 3 4 5 6 7 8 9 10 Unable to travel in car/use public transport perform 6 7 8 9 10 Cannot sleep 7 8 9 10 Always 7 8 9 10 Unable to socialise Do your whiplash symptoms interfere with sleep? 1 2 3 4 5 Do you feel more tired/fatigued than usual since your injury? 1 2 3 4 5 6 Do your whiplash symptoms interfere with social activity? 1 2 Lancet_Web_appendix Draft 7 3 4 5 6 Page 47 of 102 8. 0 Not at all 9. 0 Not at all Do your whiplash symptoms interfere with sporting activity? 1 2 3 4 5 6 7 8 9 10 Unable to participate 8 9 10 Unable to participate 8 9 10 Always 8 9 10 Always 8 9 10 Always 9 10 Unable to concentrate Do your whiplash symptoms interfere with non-sporting leisure activity? 1 2 3 4 5 6 7 10. Do you experience sadness/depression as a result of your whiplash injury/symptoms? 0 Not at all 1 2 3 4 5 6 7 11. Do you experience anger as a result of your whiplash injury/symptoms? 0 Not at all 1 2 3 4 5 6 7 12. Do you experience anxiety as a result of your whiplash injury/symptoms? 0 Not at all 1 2 3 4 5 6 7 13. Do you have difficulty concentrating as a result of your whiplash injury/symptoms? 0 Not at all 1 2 Lancet_Web_appendix Draft 7 3 4 5 6 7 8 Page 48 of 102 IMPACT OF EVENTS SCALE (IES) On ____________________________________ you experienced a motor vehicle accident. Below is a list of comments made by people after stressful life events. Please check each item, indicating how frequently these comments were true for you DURING THE PAST SEVEN DAYS. If they did not occur during that time please mark the ‘NOT AT ALL ‘column. 1. I thought about it when I didn’t mean to. Not at all Rarely Sometimes Often 2. I avoided letting myself get upset when I thought about it or was reminded of it. Not at all Rarely Sometimes Often 3. I tried to remove it from memory. Not at all Rarely Sometimes Often 4. I had trouble falling asleep or staying asleep because pictures or thoughts about it came into my mind. Not at all Rarely Sometimes Often 5. I had waves of strong feelings about it. Not at all Rarely Sometimes Often 6. I had dreams about it. Not at all Rarely Sometimes Often 7. I stayed away from reminders about it. Not at all Rarely Sometimes Often 8. I felt as if it hadn’t happened or it wasn’t real. Not at all Rarely Sometimes Often 9. I tried not to talk about it. Not at all Rarely Sometimes Often 10. Pictures about it popped into my mind. Not at all Rarely Sometimes Often 11. Other things kept making me think about it. Not at all Rarely Sometimes Often 12. I was aware that I still had a lot of feelings about it but I didn’t deal with them. Not at all Rarely Sometimes Often 13. I tried not to think about it. Not at all Rarely Sometimes Often 14. Any reminder brought back feelings about it. Not at all Rarely Sometimes Often 15. My feelings were kind of numb. Not at all Rarely Sometimes Often Lancet_Web_appendix Draft 7 Page 49 of 102 PAIN CATASTROPHISING SCALE (PCS) Everyone experiences painful situations at some point in their lives. Such experiences may include headaches, tooth pain, joint or muscle pain. People are often exposed to situations that may cause pain such as illness, injury dental procedures or surgery. We are interested in the types of thoughts and feelings that you have when you are in pain. Listed below are thirteen statements describing different thoughts and feelings that may be associated with pain. Using the following scale, please indicate the degree to which you have these thoughts and feelings when you are experiencing pain. RATING 0 1 2 3 4 MEANING Not at all To a slight degree To a moderate degree To a great degree All the time Number Statement Rating 1 I worry all the time about whether the pain will end. 2 I feel I can’t go on. 3 It’s terrible and I think it’s never going to get any better. 4 It’s awful and I feel that it overwhelms me. 5 I feel I can’t stand it anymore. 6 I become afraid that the pain will get worse. 7 I keep thinking of other painful events. 8 I anxiously want the pain to go away. 9 I can’t seem to keep it out of my mind. Lancet_Web_appendix Draft 7 Page 50 of 102 10 I keep thinking about how much it hurts. 11 I keep thinking about how badly I want the pain to stop. 12 There’s nothing I can do to reduce the intensity of the pain. 13 I wonder whether something serious may happen. Lancet_Web_appendix Draft 7 Page 51 of 102 POST TRAUMATIC STRESS DIAGNOSTIC SCALE (PDS) PART 1 Below are several questions about your motor vehicle accident. How long ago did the accident happen? 15 Less than 1 month 1 to 3 months 3 to 6 months 6 months to 3 years 3 to 5 years More than 5 years During the accident: Were you physically injured? 16 Y N Was someone else physically injured? 17 Y N Did you think your life was in danger? 18 Y N Did you think that someone else’s life was in danger? 19 Y N Did you feel helpless? 20 Y N Did you feel terrified? 21 Y N PART 2 Below is a list of problems that people sometimes have after experiencing a traumatic event. Read each one carefully and choose the answer (0-3) that best describes how often that problem has bothered you IN THE PAST MONTH. Rate each problem with respect to the motor-vehicle accident (the ‘traumatic event’). O = Not at all or only one time 1 = Once a week of less/once in a while 2 = 2 to 4 times a week/half the time 3 = 5 or more times a week/almost always Having upsetting thoughts or images about the traumatic event that came into your head when you didn’t want them to 22 0 1 2 3 Having bad dreams or nightmares about the traumatic event 23 0 1 2 3 Reliving the traumatic event, acting or feeling as if it was happening again 24 0 1 2 3 Feeling emotionally upset when you were reminded of the traumatic event (for example, feeling scared, angry, sad, guilty, etc.) 25 0 1 2 3 Experiencing physical reactions when you were reminded of the traumatic event (for example, breaking out in a sweat, heart beating fast) 26 0 1 2 3 Trying not to think about, talk about, or have feelings about the traumatic event 27 0 1 2 3 Trying to avoid activities, people, or places that remind you of the traumatic event 0 1 2 3 Not being able to remember an important part of the traumatic event 29 0 1 2 3 Having much less interest or participating much less often in important activities 30 0 1 2 3 Feeling distant or cut off from people around you 31 0 1 2 3 Lancet_Web_appendix Draft 7 Page 52 of 102 Feeling emotionally numb (for example, being unable to cry or unable to have loving feelings) 32 0 1 2 3 Feeling as if your future plans or hopes will not come true (for example, you will not have a career, marriage, children, or a long life) 33 0 1 2 3 Having trouble falling asleep 34 0 1 2 3 Feeling irritable or having fits of anger 35 0 1 2 3 Having trouble concentrating (for example, drifting in and out of conversations, losing track of a story on television, forgetting what you read) 36 0 1 2 3 Being overly alert (for example, checking to see who is around you, being uncomfortable with your back to a door, etc.) 37 0 1 2 3 Being jumpy or easily startled (for example, when someone walks up behind you) 0 1 2 3 How long have you experienced the problem that you reported above? (Mark only ONE) 39 Less than 1 month 1 to 3 months More than 3 months How long after the accident did these problems begin? (Mark only ONE) 40 Less than 6 months 6 or more months PART 3 Indicate if the problems you rated in Part 2, above, have interfered with any of the following areas of your life DURING THE PAST MONTH. Select either Yes or No. Work 41 Y N Household chores and duties42 Y N Relationships with friends43 Y N Fun and leisure activities44 Y N Schoolwork45 Y N Relationships with your family46 Sex life47 Y N Y N General satisfaction with life48 Y N Overall level of functioning in all areas of your life49 Y N Lancet_Web_appendix Draft 7 Page 53 of 102 SELF-REPORT LEEDS ASSESSMENT OF NEUROPATHIC SYMPTOMS AND SIGNS PAIN SCALE (S-LANSS) Leeds Assessment of Neuropathic Symptoms and Sign (self complete) Think about how your pain that you showed in the diagram has felt over the last week. Please tick the descriptions that best match your pain. These descriptions may, or may not, match your pain no matter how severe it feels. 1. In the area where you have pain, do you also have ‘pin and needles’, tingling or prickling sensations? NO – I don’t get the sensations YES – I do get these sensations 2. Does the painful area change colour (perhaps looks mottled or more red) when the pain is particularly bad? NO – The pain does not affect the colour of my skin YES – I have noticed that the pain does make my skin look different from normal 3. Does your pain make the affected skin abnormally sensitive to touch? Getting unpleasant sensations or pain when lightly stroking the skin might describe this. NO – The pain does not make my skin in that area abnormally sensitive to touch YES – My skin in that area is particularly sensitive to touch 4. Does your pain come on suddenly and in bursts for no apparent reason when you are completely still? Words like ‘electric shocks’, jumping and bursting might describe this. NO – My pain doesn’t really feel like this YES – I get these sensations often 5. In the area where you have pain, does your skin feel unusually hot like a burning pain? NO – I don’t have burning pain YES – I get these sensations often Gently rub the painful area with your index finger and then rub a non-painful area (for example, an area of skin further away or on the opposite side from the painful area). How does this rubbing feel in the painful area? The pain area feels no different from the non-painful area. I feel discomfort, like pins and needle, tingling or burning in the painful area that is different from the non-painful area. 6. 7. Gently press on the painful area with your finger then gently press in the same way onto a nonpainful area (the same non-painful area that you chose in the last question). How does this feel in the painful area? The pain area feels no different from the non-painful area. I feel numbness or tenderness in the painful area that is different from the non-painful area. Lancet_Web_appendix Draft 7 Page 54 of 102 PATIENT SPECIFIC FUNCTIONAL SCALE (PSFS) In the spaces provided below, please identify three important activities that you are unable to do or are having difficulty with as a result of your whiplash injury. The activities you choose should be of varying difficulty, that is, try and identify an activity that you have a small amount of difficulty doing as a result of your whiplash injury, moderate amount of difficulty and finally an activity you are finding quite difficult to do as a result of you whiplash injury. Below each activity that you have chosen, please circle a number to indicate how well you feel you are able to perform that activity at this time. Please try and provide as much information as possible when describing your pre-injury activity e.g. include the duration or distance you were able to do an activity for prior to your whiplash injury. Activity 1: _____________________________________________________________________________ _____________________________________________________________________________ 0 Unable to perform the activity 1 2 3 4 5 6 7 8 9 10 Able to perform activity at pre-injury level Activity 2: _____________________________________________________________________________ _____________________________________________________________________________ 0 Unable to perform the activity 1 2 3 4 5 6 7 8 9 10 Able to perform activity at pre-injury level Activity 3: _____________________________________________________________________________ _____________________________________________________________________________ 0 Unable to perform the activity 1 2 Lancet_Web_appendix Draft 7 3 4 5 6 7 8 9 10 Able to perform activity at pre-injury level Page 55 of 102 PHYSICAL EXAMINATION – RANGE OF MOTION Cervical Range of Motion Movement Range Flexion Extension Rotation Right Rotation Left Comments: ________________________________________________________________________________________ ______________________________________________________________________ Pressure Pain Thresholds Left 1 2 Right 3 1 2 3 Tibialis Anterior Spinous Process 1 2 3 C5 Cold Pain Threshold Cervical - Left Cervical - Right Cold Pain (6-14) Comments: ________________________________________________________________________________________ ______________________________________________________________________ Lancet_Web_appendix Draft 7 Page 56 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL APPENDIX 10 – MEASURING CERVICAL SPINE RANGE OF MOVEMENT: INCLINOMETER METHOD CERVICAL RANGE OF MOVEMENT – INCLONOMETER METHOD Modified Hole et al (1995) protocol Description Measurement of active cervical range of motion using an inclinometer. Instruments required Analogue or digital inclinometer Participant’s starting position Flexion and extension For flexion and extension the participant sits in a chair, trunk erect, looking straight ahead. To minimise trunk and shoulder movement the participant should be encouraged to press their thoracic and lumbar spine against the back rest and to lightly grasp the seat with their hands. Rotation For rotation the participant lies supine on a plinth. To minimise trunk and shoulder movement the participant is asked to keep their shoulders in close contact with the plinth. Starting position of examiner Standing beside the patient for flexion/extension, at the front of the patient for lateral flexion and behind the patient for rotation. Procedure Flexion and extension The inclinometer is positioned on the centre of the skull aligned to read movement in the sagittal plane (i.e. mid-sagittal plane (line of nose) with the centre of the inclinometer in line with the external auditory meatus). Participants are requested to keep their shoulders and trunk still by pressing against the chair back and holding onto the seat base with their hands and to then slowly flex or extend the neck. Rotation The inclinometer is positioned on the forehead with the axis in line with the nose. The participant is then asked to maintain their shoulders pressed against the plinth and to then turn their head slowly to the side. Common errors to avoid Failure to fixate the inclinometer, allowing the participant to move their trunk. Reliability Hole and colleagues27 evaluated the inter-rater reliability of the protocol using two student chiropractors as raters and 84 healthy volunteers as targets. They reported excellent inter-rater reliability with ICC values in the range 0.76-0.86. Typical values Approximate values for asymptomatic participants are given below. Direction Rotation Flexion Extension Lancet_Web_appendix Draft 7 20 year old 75deg 65deg 80deg 60 year old 60deg 50deg 60deg Page 57 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL APPENDIX 11– MEASURING COLD PAIN THRESHOLD OVER THE CERVICAL SPINE Description Measurement of cold pain threshold over the cervical spine using the Thermotest system. Instruments required Thermotest system. Plinth. Participant’s starting position The participant lies on a plinth in prone. Starting position of examiner Standing beside the participant/plinth. Procedure • The thermode is applied, either to the left or right of the cervical spine. • The participant is asked to depress a switch the first instant that the sensation changes from one of cold to one of cold and pain • The value at switch press is automatically recorded and transposed to the appropriate site on the ‘Examination Data collection sheet’. • Three cold threshold measures are taken. • Altered thermal thresholds provide indication of sensory hypersensitivity (≥ 13ºC – outside confidence intervals found for asymptomatic controls) Lancet_Web_appendix Draft 7 Page 58 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL APPENDIX 12 – MEASURING PRESSURE PAIN THRESHOLD OVER THE CERVICAL SPINE AND THE TIBIALIS ANTERIOR Description Measurement of pressure pain threshold over the cervical spine (C5 spinous process) and tibialis anterior using Pressure Algometry at a rate of 40kilopascals/sec. Instruments required Pressure Algometer. Plinth. Participant’s starting position Cervical spine – C5 spinous process The participant lies prone on a plinth. Tibialis anterior The participant lies supine on a plinth. Starting position of examiner Standing beside the participant/plinth. Procedure • The thermode is applied to the assessment area – C5 spinous process and muscle belly of tibialis anterior - left and right. • The participant is asked to press an electronic switch when their pain threshold is reached, that is “the moment the pressure sensation becomes one of pressure and pain” • The pressure at the time of the switch press is automatically recorded on the algometer and it is then transposed to the appropriate site on the Examination Data collection sheet. • Three measures of PPT are taken at each of the three assessment sites. • Lower pain thresholds provide indication of mechanical hypersensitivity. The values below represent those outside confidence intervals for asymptomatic controls Tib Ant: < 410 kPa (males); 304 kPa (females) C5: < 210 kPa (males); < 185 kPa (females) APPENDIX 13 – UTILITY WEIGHTS: INSTRUCTION AND RECORDING SHEET Lancet_Web_appendix Draft 7 Page 59 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL INTRODUCTION TO STANDARD GAMBLE “Thank you. Now I’d like to run through some hypothetical questions with you. These questions will help us understand the choices that patients make. Your answers are confidential; so they won’t influence the treatment you receive in the trial or elsewhere.” STANDARD GAMBLE “Now I am going to ask you consider two possible choices, about treatment and your neck symptoms, and ask you which choice you would take. “ “One choice involves a treatment that cures your neck symptoms and you will be healthy for 30 years. However the treatment also carries a risk of death. We use this device here, called a “probability wheel”, to illustrate the chances of death and the chances of cure. The wheel is divided into two sectors: a blue or healthy sector and a red sector for death. At the moment the wheel is three-quarters blue and one-quarter red. So if you select treatment there is a 75% chance of a cure and a 25% chance of death. “ “The other choice you have is not to have the treatment; but the neck symptoms you have right now persist for the next 30 years. “ “I will use the probability wheel to show you different chances of cure or death with treatment and then ask you if you would choose to have the treatment or not. Do you understand? “ Allow the patient to ask questions. If they do not ask any questions ask them to explain in their own words what the task involves. Clarify any misunderstandings. Start with the probability wheel showing 25% risk of death “At the moment the probability wheel shows a 25% risk of death and a 75% chance of cure with treatment. Would you choose to have the treatment or not?” If the subject chooses not to have treatment, decrease the death probability 5% and ask the subject to choose again. “OK the wheel now says the probability of death has dropped to 20% and the probability of cure is 80%. Now would you have the treatment? “ If the subject chooses treatment, increase the death probability 5% and ask the subject to choose again. “OK the probability wheel now shows a probability of death of 30% and of cure of 70% if you choose treatment. What would your choice be?” Repeat this exercise until the choice changes If the subject chooses not to have treatment at 5% risk of death, then decrease the probability in increments of 1% until the choice changes or you reach 0%. We are testing for the respondent’s point of indifference between treatment with a risk of death and no treatment. This will generally by an increment of 2.5 unless the value is between 0 and 5% in which case it should be an in increment of 0.5 Record the “indifferent probability” (usually the two boundary probabilities) at the end of the exercise. Lancet_Web_appendix Draft 7 Page 60 of 102 CHRONIC WHIPLASH EXERCISE TRIAL PROTOCOL Utility weights record sheet Assessor to complete this section Standard Gamble Probability 1 Probability 2 Indifferent probability Lancet_Web_appendix Draft 7 Page 61 of 102 APPENDIX 14 – HOME EXERCISE DIARY Participant’s Initials Chronic Whiplash Exercise Trial Participant Number COST DIARY Date – 14 week follow up _____/_____/_____ One part of this trial involves an economic analysis to look at the costs people with whiplash incur as a result of their condition. 1. In the last two weeks have you attended any appointments as a result of your whiplash symptoms, e.g. medical specialist, GP, Physiotherapist, Psychologist, massage, acupuncture? YES please provide details below; NO Appointment type Est. total travel distance (private vehicle, km) Lancet_Web_appendix Draft 7 Est of total travel time and waiting time (min) Duration of visit (min) Visit was initiated by (e.g. self, GP, insurer, specialist) Total price charged Page 62 of 102 Out of pocket price (i.e. how much you paid) Parking costs or public transport costs Number of visits APPENDIX 14 – HOME EXERCISE DIARY Participant’s Initials Chronic Whiplash Exercise Trial Participant Number COST DIARY Date – 14 week follow up 2. In the last 2 weeks have you PAID someone to assist you with daily activities as a direct result of your whiplash symptoms? below; _____/_____/_____ YES please provide details NO Home help (e.g. Nursing Care) Domestic help (e.g. Cleaners) Other (please specify) Office Use Only Type Type Type Hours Hours Hours Cost Cost Cost Type Type Type Hours Hours Hours Cost Cost Cost Type Type Type Hours Hours Hours Cost Cost Cost Hours Cost 3. In the last 2 weeks have you needed to call on unpaid assistance e.g. from friends or family to assist you with daily activities or attend appointments as a direct result of your whiplash symptoms? YES please provide details below; NO Family/friends in their own time (total hours): _________________________________ Family/friends requiring them to take time off work (total hours) _________________________________ Lancet_Web_appendix Draft 7 Page 63 of 102 APPENDIX 14 – HOME EXERCISE DIARY Participant’s Initials Chronic Whiplash Exercise Trial Participant Number COST DIARY Date – 14 week follow up _____/_____/_____ 4. In the last 2 weeks have you taken time off work due to your whiplash injury or have there been any activities you have been unable to do as a result of your injury, if so please give details? YES please provide details below; NO Time away from work (egg sick leave) because of Whiplash Injury (total hours) _________________________________ Time unable to perform usual activities because of injury (total hours) _________________________________ 5. In the last 2 weeks have purchased any medication to be taken specifically for your whiplash symptoms? YES please provide details below; Medication (Name and dose) NO Prescribed Non-prescribed No. of doses consumed/week ____________ Cost ____________ No. of doses consumed/week ____________ Cost ____________ No. of doses consumed/week ____________ Cost ____________ No. of doses consumed/week ____________ Cost ____________ No. of doses consumed/week ____________ Cost ____________ 6. In the last two weeks have you been required to cover any other costs as a direct result of your whiplash symptoms e.g. pillow, ergonomic devices, please provide details and an approximate cost. YES please provide details below; NO ___________________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________ Lancet_Web_appendix Draft 7 Page 64 of 102 APPENDIX 14 – HOME EXERCISE DIARY Participant’s Initials Chronic Whiplash Exercise Trial Participant Number COST DIARY Exercise week Date: Aerobic EXAMPLE ONLY 20 min walk Posture training RPE: 9 H/W Cue email pop up Neck flexors (CCF training) Train pattern, 5s hold if applic Neck extensors Scapular training 10s Sensorimotor 30s tandem eyes open _ Range of movement Exercise week Date: Aerobic R S Every 15 mins 10 2 5 2 10 2 _____/_____/_____ Date – 14 week follow up Week 1 …./…./…. Week 2 …./…./…. Week 3 …./…./…. Week 4 …./…./…. H/W R S H/W R S H/W R S H/W R S H/W R S 5 5 3 sets a day Week 5 …./…./…. Week 6 …./…./…. Week 7 …./…./…. Week 8 …./…./…. Week 9 …./…./…. Week 10 …./…./…. H = hold; W = weight; R = repetitions; S = sets; = Tick for each day you complete each exercise (e.g. do exercises 4 times in a week = four ticks) exercises 4 times in a week = four ticks) Page 65 of 102 APPENDIX 14 – HOME EXERCISE DIARY Participant’s Initials Chronic Whiplash Exercise Trial Participant Number COST DIARY H/W R S H/W _____/_____/_____ Date – 14 week follow up R S H/W R S H/W R S H/W R S H/W Neck strength and endurance Upper limb Lower limb Sensorimotor Functional activity H = hold; W = weight; R = repetitions; S = sets; = Tick for each day you complete each exercise (e.g. do exercises 4 times in a week = four ticks) Page 66 of 102 R S APPENDIX 14 – HOME EXERCISE DIARY Participant’s Initials Chronic Whiplash Exercise Trial Participant Number COST DIARY Exercise week Date: Aerobic Week 11 …./…./…. H/W R S Week 12 …./…./…. H/W _____/_____/_____ Date – 14 week follow up R S H/W R S H/W R S H/W R S Neck strength and endurance Upper limb Lower limb Sensorimotor Functional activity H = hold; W = weight; R = repetitions; S = sets; = Tick for each day you complete each exercise (e.g. do exercises 4 times in a week = four ticks) Page 67 of 102 H/W R S APPENDIX 14 – HOME EXERCISE DIARY Chronic Whiplash Exercise Trial COST DIARY Participant’s Initials Participant Number Date – 14 week follow up _____/_____/_____ Rate of Perceived Exertion (RPE) scale (Borg 1970) RPE Scale 6 7 8 9 10 11 12 13 Effort % 20% effort 30% effort 40% effort 50% effort 55% effort 60% effort 65% effort 70% effort 14 75% effort 15 16 17 18 19 20 80% effort 85% effort 90% effort 95% effort 100% effort Exhaustion Descriptor Target intensity Very, very light (Rest) Very light gentle walking Fairly light Somewhat hard steady pace Hard Very hard Very, very hard Page 68 of 102 Moderate level of intensity Talk test: exercising at an intensity that allows for comfortable speech Web appendix 2: Therapist manual A randomised controlled trial of a comprehensive exercise program for chronic whiplash C Maher, M Sterling, G Jull, J Latimer, L Connelly The University of Sydney; The University of Queensland Physiotherapy Management Protocol Introduction The management program under investigation combines sequentially, motor relearning and graded exercise, for individuals with a chronic whiplash associated disorder and aims to relieve the individual’s pain, improve their function and return them to their pre-injury work or home activity status. It is conducted over a 12 week period with the participant attending the physiotherapist twice per week for the first eight (8) weeks and once per week for the final four (4) weeks. An important element of the program is that participants need to be involved in setting goals and also complete their activity charts so that they can monitor their progress. This protocol provides an outline of our requirements of you as a trial physiotherapist as well as a comprehensive guide to assessment requirements and exercise prescription. The assessment required throughout the management period underpins the exercise prescription and progression. The physiotherapist can tailor the management program to the individual participant’s presentation and functional goals. Nevertheless, the physiotherapist must prescribe exercises as per the intent of the research protocol, which focuses on motor relearning elements in the first 4 weeks and the graded activity program in the next 8 weeks. In the first four weeks manual therapy (excluding cervical spine manipulation) can be provided as required in a multimodal context, to assist achievement of the goals of the motor relearning program. There can be some flexibility in the transition period (weeks 4 and 5). For example, one participant may be ready for progression to higher load exercise a little earlier and another a little later. We are reliant on your skill as a physiotherapist to guide this transition appropriately on the basis of your continuous reassessment. Aerobic exercise should be introduced from the outset of the management program. An overall view of the program is presented below. The delivery of the exercise program should follow the principles of: positive reinforcement by participant and physiotherapist, goal setting and self monitoring of progress (through diaries), continuous reassessment, addressing unhelpful beliefs and encouraging skill acquisition by modelling. Once the transition to graded activity has occurred, the principles of pacing and exercise quotas should also be incorporated. An extract of a book chapter by Nicholas et al (2004) has been included in Appendix 7 which provides detailed information on application of these principles in a CBT context. It is written for low back pain, but the principles can be applied to the management of whiplash associated disorders. Page 69 of 102 General Procedures 1. The trial centre will contact your practice to arrange a suitable time for the participant’s first appointment. You will be provided with a participant record proforma and a brief overview of the participant’s history and summary of baseline measures taken at the trial centre. 2. Participant record proforma (Appendix 8). Please use this proforma to record: • Dates of attendance • Initial assessment • Outcome measures (PSFS; physical measures relevant to the exercise intervention) • Initial management and exercise program • Details of progressive assessment and management in the 20 sessions • A record of participant compliance with the exercise program • The total duration of each treatment session as well as a breakdown of each session into minutes of 1:1 contact with participant and separately the time required to complete trial paperwork. 3. Keep a copy of the home exercise program that is developed with the participant and its progressions at each management session. Please check participants are completing their diaries. We are using diary entries as a measure of compliance so this is important for the study. 4. What to do if there is an adverse event Minor fluctuations in whiplash symptoms are not an adverse event and do not need to be reported. These could be expected when the participant is embarking on an exercise program. If this occurs: • Check performance and design of the exercise, modify if necessary • Provide assurance • Retain the emphasis on an active and graded approach An adverse event (AE) is any untoward medical occurrence in a participant temporally associated with the trial intervention, whether or not considered related to the trial intervention. Examples of an AE include: • Exacerbation of a pre-existing condition • New conditions detected or diagnosed after enrolment in the trial Examples of an AE do not include anticipated day-to-day fluctuations of pre-existing disease(s) or condition(s) present or detected at the start of the study that do not worsen. A serious adverse event (SAE) is one that is life threatening requires inpatient hospitalisation or will result in persistent or significant disability or incapacity. All adverse events need to be immediately reported to the Adverse Events Committee for the trial (Chris Maher, Michele Sterling). In NSW, concerns should be addressed to Chris via phone on (02) 9657 0382. In Qld, contact Michele on (07) 3365 5344. Please do not contact other trial personnel for ‘blinding’ reasons. In the unlikely event of a SAE trial recruitment and treatment should be put on hold pending advice from the Adverse Events Committee. The Adverse Events Committee will report all AE and SAE to the relevant ethics committee. 5. Cancellation Policy. Each participant should receive 20 exercise sessions. A participant is able to cancel up to 2 sessions without penalty (i.e., these 2 sessions may be made up within the 12 week period). If a participant cancels or fails to attend on more than 2 occasions, these sessions will not be made up. Each participant will receive a sheet outlining the procedure to be followed for cancellations. Please notify the trial centre if a participant has failed to attend on more than two occasions NSW Contact: QLD Contact: Dr Christine Lin Tel: 02 8238 2437 Email: clin@george.org.au Ms Stephanie Valentin Tel: 07 3636 4214 Email: s.valentin@uq.edu.au Page 70 of 102 Management Protocol at a Glance This section provides guidelines at a glance for the Specific Motor Relearning Exercise and the Graded Exercise Components of the trial management program. Please refer to the following appendices for further details: Appendix 1: Initial and progressive assessment to direct specific exercise prescription Appendix 2: Guide to the Motor Relearning Program (Weeks 1-4) Appendix 3: Technical notes for the motor relearning program Appendix 4: Overview of Graded Exercise Program (Weeks 5-12) Appendix 5: Examples of activity tests Appendix 6: Borg Rating of Perceived Exertion (RPE) Scale Week Sessions per week Overview of Components 1 2 2 2 3 2 4 2 Baseline & follow-up assessments to guide initial prescription & progression of program Exercises to improve cervical and scapular muscle control, kinaesthesia & balance Manual therapy if indicated (excluding cervical spine manipulation) Education and advice Progressive home exercise program; aerobic exercise program Transition 5 2 6 2 7 2 8 2 9 2 10 1 11 1 12 1 Baseline & follow-up assessments to guide initial prescription & progression of program Supervised exercise program to improve the participant’s functional abilities progress aerobic, range of motion, expand strength, endurance, coordination and functional exercises. Daily home program including exercise & graded increase of physical activities Graded activity program using CBT principles Discharge session to reinforce progress and plan for continued activity Reminder: We require the following information to be recorded on participant record proforma at each session of attendance. • Date of attendance • Follow-up assessment findings, additional progressive assessments; participant’s achievements and compliance with exercise • Follow-up of PSFS – complete every 2 weeks – Establish new functional goals once the participant has indicated a score of 9 or 10 for any function • Details of management and exercise progression and breakdown of treatment duration • Record the home exercises in a diary for the participant and keep a copy of the exercise diary. Check that the participant is completing the diary and ensure they know how to record their adherence to the program. Page 71 of 102 Weeks 1-4: Specific Motor Relearning Exercise Component Session 1: (week 1) Complete the initial participant interview and physical assessment (Appendix 1) on the proforma provided and establish participant-centred goals based on the PSFS. The management session should contain the following elements: 1. Participant education regarding the nature of their whiplash injury and based on assessment findings, the nature of associated muscle dysfunction and the rationale behind the specific motor relearning exercises. The physiotherapist should ensure the participant has an understanding of their pain and help shape beliefs incorporating CBT principles. 2. Therapeutic exercise: Based on their analysis, the physiotherapist facilitates correct muscle activation for the cervical region and shoulder girdle with specific training exercises as well as functional training in posture. The participant is taught the specific motor relearning strategies (Appendix 2; 3). 3. Any relevant manual therapy (excluding cervical spine manipulation) can be performed, but should not detract from the active approach to management. 4. Prescribe and teach home exercise program – ensure participant has correct strategies and understands how to complete the exercise diaries. 5. Commence aerobic exercise program (see Appendix 4; 6). 6. Record the home exercise program for the participant, including exercise dosage. 7. Book the next follow up session. Sessions 2-8 1. Perform a follow-up assessment of the participant and record findings on the participant record proforma, document achievements. Formally complete the PSFS every 2 weeks and modify as participant progresses. Check exercise diary and participant’s activity chart. 2. Continually progress the specific motor relearning tasks, movement re-education and functional training guided by assessment outcomes (Appendix 2, 3). 3. Monitor and progress the aerobic exercise program as indicated (Appendix 4). 4. Clearly document exercise and management progressions. 5. Reinforce CBT principles as required. 6. Record the home exercise program for the participant, including exercise dosage. 7. The exercise program may have an earlier transition to the graded exercise program and this will be based on participant achievement of goals in motor relearning. 8. Book the next follow-up session. Weeks 5-12: The Graded Activity Program Note: the emphasis in this phase of the management program, which begins in week 5, changes from specific motor relearning exercises to more general whole body functional exercises. The physiotherapist should aim for a seamless transition between the motor relearning phase and the graded exercise phase. Depending on the particular participant, the graded exercise or components of it may begin earlier, that is, in week 4 and for others it may begin a little later that is, in week 6. However this should be the outer limit to commence the graded exercise program. For example: the motor relearning program begins the elements of strengthening for the neck muscles and in a seamless transition, these should be progressed into the principles adopted for the graded exercise program in week 5; the full progression of the exercises for cervical somatosensory function (e.g. balance), may not have been fully achieved in the 4 week period and the progressions can continue into the graded exercise program in a seamless way. Session 9: (week 5) 1. Perform a follow-up assessment of the participant and record findings on the participant record proforma, document participant achievements. Check exercise diary and participant’s activity chart. 2. Review current PSFS goals and identify the participant’s current ability to complete the specific functional goals. 3. Perform a tailored physical and functional assessment to focus on components which are essential for the participant to be able to achieve their specific functional goals as identified in the PSFS. 4. Gain baseline measures of strength/endurance/functional capabilities (Appendix 4; 5). Page 72 of 102 5. Identify reasons for the participant’s inability to complete the specific functional activity, specifically in terms of duration, intensity and factors limiting continuation of the activity (e.g. fatigue, pain) to develop the graded exercise program. 6. Prescribe exercises on CBT principles using the formula: - Reduce the duration or intensity to 80% of the participant’s current ability. This is the starting exercise intensity. 7. Review the goals listed and discuss with the participant an appropriate timeframe to achieve the goals with reference to the nominated PSFS measures. 8. Prescribe and record 6-8 exercises for the participant to continue at the next session at the above exercise intensity. 9. Record a home exercise program, comprising of up to 4 exercises, in the exercise diary. 10. Book the next follow up exercise session. Sessions 10-20 1. Perform a follow-up assessment of the participant and record findings on the participant record proforma, document achievements. Formally complete the PSFS every 2 weeks and modify as participant progresses. Check exercise diary and participant’s activity chart. 2. Continually progress the program components of aerobic capacity/strength/endurance /functional capabilities (Appendix 4, 5). 3. Clearly document exercise and management progressions. 4. Reinforce CBT principles as required. 5. Record the home exercise program, including exercise dosage. 6. Book the next follow up session. At the last session – discuss the follow-up assessment at the trial centre and ensure that the participant has a time booked by the trial centre. Ensure the participant has mapped a program of continuing activity and exercise Page 73 of 102 Appendix 1: Initial assessment to direct specific exercise prescription Analysis of participant’s provocative postures, functions or movements (i) Directed by the participant interview, analyse the participant’s main postures, functions or movements that are provocative of pain. (ii) Analyse the reasons why these manoeuvres might be provocative in terms of postural attitudes, muscle or movement dysfunctions. (iii) Attempt to alter postures or positions so that the task/position is less painful. This serves as a powerful treatment and educational directives. Analysis of Posture: perform in sitting Analysis of spinal posture (i) Analyse the participant’s habitual sitting posture (i.e. ideal is a neutral lumbo-pelvic (L/P), thoracic (T), cervical and shoulder girdle position; observe for too much flexion or too much extension in the L/P and T regions). (ii) Check range and pain response and range of cervical rotation in each direction in their habitual posture (baseline). (iii) Analyse their attempt to assume an ideal sitting posture. (iv) Observe any poor pattern e.g. predominant use of thoraco-lumbar erector spinae with an inability to assume a neutral lumbo-pelvic position; over extension of thoracic region, alternately - too much flexion of thoracic region. (v) Facilitate the correct L/P postural position and thoracic region if necessary. (vi) Assess effect of change in posture on: cervical range of movement and pain response (Treatment and education directives). (vii) Can the participant replicate an ideal sitting posture once taught and if not what is the reason - kinaesthetic ability, poor active control, loss of passive mobility (Treatment directives). Analysis of scapular posture (i) Observe and analyse any positional fault of the scapulae in habitual posture. (ii) Repeat baseline cervical ROM test in each direction. (iii) Facilitate correct sitting posture and then manually position the scapula in a neutral posture on thorax (do separately and choose most deviated scapula first; analyse components of correction). (iv) Check cervical rotation ROM and pain response (treatment and education directives). Scapular muscle assessment (initial) Analysis of scapulae under light load (i) Gently resist each of shoulder flexion, abduction and external rotation. (ii) Reveals where specific weaknesses lie. Analysis of scapular control during arm flexion and abduction (i) Assess control during concentric and eccentric phases as per an examination of the glenohumeral joint. Scapular holding test in prone (i) Modified grade 3 test of the lower trapezius (arm rests by side to eliminate arm load). (ii) Perform after manual examination of the cervical spine – obtain baseline VAS of most symptomatic segment. (iii) Passively place scapula in a neutral position on the chest wall and require the participant to hold the position. Outcome a) Balanced use of scapular synergists or predominant use of one muscle group e.g. lat dorsi; b) Observe for fatigue tremor or movement of scapula indicting a loss of holding capacity. (iv) Re-assess manual examination and determine change in quality of joint feel and VAS score (Treatment and education directives). Cranio-cervical flexion test (CCFT) Test of pattern of cranio-cervical flexion Preparation (i) Test for neural tissue mechanosensitivity: supine lying, assess passive CCF range and resistance and retest in sensitising positions of SLR and BPTT. (NB, the presence of NT mechanosensitivity will modify how CCF is trained). Also gauge ROM of CCF. (ii) Prepare participant, supine, crook lying, ensure cranio-cervical and cervical regions are in a neutral position (support with a folded towel if necessary). (iii) Prepare PBU and insert behind neck and draw up to the sub-occipital region. Inflate to baseline of 20mmHg; stabilise air and re-inflate to achieve 30mmHg. (iv) Teach the CCF action. Use instructions of ‘feel the back of your head slide up the bed as you nod your chin’. (v) Explain dial of PBU and requirements of the task. Page 74 of 102 Stage 1 CCFT (i) Request participant to nod to target sequentially 22, 24, 26, 28, 30 mmHg. They hold each position for a couple of seconds before relaxing. Use the instruction to slide back of head up the bed and nod to target pressure. Ensure that the participant performs the movement slowly. (ii) Analyse: pattern of movement - Does participant perform sagittal rotation (correct) or a rotation/retraction action/retraction action (incorrect) Note retraction is seen when there is a direct descent of the head, or when they are using almost the same range of CCF to attain each target pressure. - Is there unwarranted activity in the sternocleidomastoid (SCM), anterior scalene (AS) muscles. - Is there over-activity of hyoids? – retest with mandible in relaxed position - Is there breath holding? ensure the participant nods with exhalation Outcome: pressure level participant can achieve with correct movement and nil to little use of SCM/AS Stage 2 CCF low level endurance or holding capacity Stage 2 of the test is only performed when the participant has a correct CCF pattern. Often this stage of the test has to be performed on the second treatment as first aim in rehabilitation is to train the participant to achieve the correct movement pattern. (i) Set up participant and PBU as above. (ii) Test holding capacity at each progressive pressure level. (iii) Ensure correct pattern is used at all times. (iv) In testing the participant is required to hold for about 5 secs and a decision should be able to be made for a particular pressure target after 3 or 4 attempts. (v) An inability to perform a tonic hold at the respective level is evident when: - The pressure cannot be maintained on the target. - The participant reverts to a retraction pattern to hold the pressure. - There is phasic activity of the superficial flexors (pressure is not held steadily). Outcome: determine the level the participant can hold and that will be the starting point in training. Assessment of craniocervical and cervical extensors The test exercise is performed either prone on elbows or in four point kneeling. This is not a test with absolute outcomes, but more a pre-exercise assessment/instruction, that will lead into an exercise protocol. In the test position, all extensor muscles will work to hold the head against gravity. However we know from research that the suboccipital muscles and the deep cervical muscles (multifidus and semispinalis cervicus) atrophy or may have fatty infiltrate. Therefore the movement strategies are designed to be biased towards those muscles. (i) Sub-occipital muscles: Focus on a neutral neck position - require the participant to perform cranio-cervical extension (chin down). - require the participant to perform cranio-cervical rotation (the saying ‘no’ action). Assess quality of movement and for smooth co-ordination. (ii) Deep cervical extensors: the cranio-cervical region remains in neutral and the axis of motion is now at C7. - instruct the participant to curl their neck first into flexion and then to curl their neck back to extension. The participant will often require manual facilitation to achieve the correct action. To assist in maintaining the cranio-cervical neutral position, let the participant imagine they have a book between their hands and they must keep their eyes on the book as they lift their head. Check that muscles such as splenius capitis are not overactive. Outcome: many participants cannot extend much beyond neutral to begin with (not a pain protection response). Others will fatigue quite quickly. Progressive assessment Scapular function (i) Assess control of serratus anterior in prone on elbows or 4 point kneeling. (ii) Assess scapular control in functional tasks pertinent to the participant’s work activities. Observe or palpate pattern of use, their maybe underactivity of the trapezius on the dominant side, or there can be overactivity. Observe control of scapular position during the task. Can take task to fatigue. (iii) Test fatigability of the upper trapezius – repeated bilateral arm abduction to overhead height. Outcome: fatigue is often readily displayed. Pattern of cervical flexor eccentric-concentric control (should be holding at least 26-28mmHg in CCF training). (i) Examine pattern in available range of cervical extension in sitting. (ii) Examine holding ability in progressively increasing ranges of cervical extension (obtain baseline for progression of endurance exercises). Page 75 of 102 Cervical somatosensory function The three elements tested are: • Cervical reposition sense, cervical movement sense • Eye movement control • Balance Cervical reposition sense Use prepared target and a laser light. Position participant in sitting, one meter from target. Attach target to wall once the participant is in the relaxed sitting and ‘neutral’ position. Test with eyes closed or use eye mask. (i) Test relocation from each of rotation (L), (R) and extension. (ii) The participant should repeat the movement 3-5 times. Between repetition, participant keeps their eyes closed, the therapist repositions the head to neutral between each repetition. Outcome: mark the average reposition error on target >4.5 mm is abnormal. Cervical movement sense Use prepared target and a laser light. Position participant in sitting, one meter from target. (i) Require participant to trace the laser light within the boundaries of the target. Require to go from left to right and from right to left. Outcome: abnormal if 4-5mm outside central line. Also assess whether the participant can perform with a reasonable speed. Eye movement control Gaze Stability- (Eyes still - head moves) (i) Fixate Gaze - Rotation of head - Vertical movement of head Outcome: - Difficulty maintaining focus - Symptoms reproduction - Marked decrease in ROM Smooth pursuit neck torsion test (Head still eyes move) Sit participant on a swivel chair. (i) Participant focuses on target (e.g. a pen) and therapist moves the target through visual angle of 40 degrees crossing the midline left to right at a speed of 20 degrees per second. (ii) Perform at least 5 times to make a judgement. Observe for saccades, especially observed around the mid line (not like nystagmus which is observed at the periphery). Make baseline judgment. (iii) Keep participant’s head still and rotate trunk to the left approximately 45 degrees. Repeat test of eye follow. (iv) Keep participant’s head still and rotate trunk to the right approximately 45 degrees. Repeat test of eye follow. Outcome: There is a difference in saccadic movement between the trunk neutral and trunk torsioned positions. Eye head co-ordination (iv) Eyes move first to 30 degrees and then head to 30 degrees keeping focused- return to neutral. (v) Perform to both sides, repeat 3 or 4 times. Outcome: - Difficulty controlling co-ordination. - Ability to move head and eyes independently. - Symptom reproduction. Saccadic Movements Head is kept still (vi) Participant’s fix gaze on and follow a target (e.g. a pen) that the therapist moves quickly and then holds still. (vii) The target is moved in several different directions – pure planes, diagonals. Outcome: - Difficulty controlling the task. - Inability to move eyes independently of head. - Symptoms reproduction. Balance Test balance to determine the level the participant is capable of performing (i) Foot position: Comfortable Page 76 of 102 Narrow Tandem Single leg (ii) Eyes open vs closed (shown that conditions with eyes closed have more discrimination for WAD) (iii) Surface- firm; progressing to soft, progressing to unstable Outcome: Ability to maintain the stance position for 30 secs Check for increased sway, rigidity, dizziness Reference text Jull G, Sterling M, Falla D, Treleaven J, O’Leary S. Whiplash, Headache and Neck Pain: research based directions for physical therapies. Churchill Livingstone, Edinburgh, Elsevier UK, 2008. This text can be used to obtain more details of the assessment procedures and the management strategies described in the following two appendices. Page 77 of 102 Appendix 2: Guide to the Motor Relearning Program (Weeks 1-4) Introductory notes The following is a guide only and provides the components of the exercise program for the first 4 weeks of management. The program must be individualised to the particular participant you are treating. There should be a transition between the motor relearning and graded activity program. If the participant has not achieved all the stages of motor relearning, then these can be continued into the following 6 weeks until targets are reached. • • • • • • • • • The assessment will provide baselines at which the participant can commence the various exercise protocols. The rate at which exercises can be introduced will depend on the participant’s pain and disability level. A fundamental rule is that the exercises must not produce pain, especially in those participants with evidence of augmented central pain processing. It is likely that it will take 2-3 treatments to introduce all basic components of the exercise program. However the rate is variable and will be in response to the participant’s state. Do not become overzealous and exacerbate the participant’s condition. Teach, recheck and progress exercise program before performing any manual therapy in a treatment session. This will ensure that the exercises are a predominant feature of the rehabilitation. The exercises also relax the deep neck muscles such as the segmental multifidus which allows more effective performance of manual therapy techniques. Joint mobilising exercises are also included in the program. The home exercise program will replicate that performed in the treatment session. The participants should be provided with some equipment to practise with at home (e.g. laser light, PBU at later stages). Participants are required to practise exercises formally twice per day (once in the morning and once in the evening). There is a particular emphasis on correcting to the upright neutral posture repeated during the day (every 15-20 mins) as this is facilitatory of deep muscles, serves the need for multiple repetitions in the motor relearning process and has the mechanical benefit of taking cervical joints away from their end of range. The following tables provide a guide to the introduction and progression of the exercises over the 4 weeks, but progression will always be individual to the participant, their starting point and their progress. Successful motor relearning is reliant on the physiotherapist’s skill in movement and motor analysis and in teaching. Participant compliance is also required. If participants are non compliant, reflect on find the reason why and correct. - Deficits in the physiotherapist’s communication skills? - Importance of exercises not understood by participant. - Program not tailored to participant’s other daily demands. - Exercise program not clearly written out for participant. Page 78 of 102 Guide to the motor relearning program Week 1 Session 1 Session 2 Posture re-education Posture re-education - facilitate the upright lumbo-pelvic posture and correct - Re-check ability to assume an upright neutral posture, any thoracic deviation if required (leave head/neck at may need to re-teach - Re-check/teach scapular postural correction this stage) - teach participant a self correction strategy - if the participant is able to correct spinal posture with ease, teach scapular postural correction Cranio-cervical flexion training Cranio-cervical flexion training - facilitate and teach the correct pattern of CCF - Re-check the correct pattern of CCF movement movement - Perform formal tests of holding capacity, begin formal retraining of low level endurance of CCF, starting at - if nerve tissue mechanosensitivity is present, practice from extension to neutral in supine lying, use gentle self level participant can achieve (e.g. 22mmHg) resistance Cervical extensors - teach and train the CCE and CE actions Scapular muscle training - train in side lying, facilitate as required - emphasise correct pattern and train to hold the contraction for 10 secs - teach participant a home program strategy in side lying with pillow support, 10x10 sec holds Home Program - posture training – emphasise every 15-20 mins, discuss ‘cue to practise’ with participant - CCF training – practice pattern with facilitation strategies. Encourage to perform 3 sets of 10 movements - Cervical extensors – perform one to two sets of 5 reps for each of the three tasks - Scapular training – side lying, 3 sets of 10 sec holds of lower trap. Cervical extensors - teach and train the CCE and CE actions, progress repetition to 2 or 3 sets of 5 reps of each exercise Scapular muscle training - recheck and train in side lying and check home program strategy - add in exercise for serratus anterior (preferably in prone on elbows or 4 point kneeling to gain effect on neck extensors) Somatosensory function - Commence retraining as indicated from the examination. - Kinaesthetic sense – relocation practice - Balance - Eye movement control – start with one exercise as relevant to the participant Mobilising exercises - Depending on the participant, perform segmental or ROM exercises - Exercises for C/Th region often required Home Program - posture training – including scapular posture - CCF training – ensure correct pattern. Practise 3 sets of 10 x 10 sec holds - Cervical extensors – perform two sets of 5 reps for each of the three tasks - Scapular training – side lying, 3 sets of 10 sec holds of lower trap. - Kinaesthetic, balance, eye movement as developed from treatment program - Active mobilising exercises as developed in treatment Page 79 of 102 Session 3 Posture re-education - Add the ‘occipital lift’ to postural exercise to ensure good facilitation of the CCF Cranio-cervical flexion training - Progress training of the holding capacity. Target is 10x10 sec holds at 30mmHg - Progress only as participant can maintain a good patterns without excess activity of the superficial flexors Cervical extensors - Train the CCE and CE actions, progress repetition to 3 sets of 5 reps of each exercise Scapular muscle training - Continue to train in side lying, 10x10 sec holds each side in home program - Assess and train control in posture and with arm movements to 30 degrees - Progress serratus anterior exercise to 3 sets of 5 reps of ‘thoracic push ups’ Somatosensory function - Kinaesthetic sense – relocation practice; add in movement sense task - Progress balance exercises - Progress exercises for eye movement control – train at least two tasks Mobilising exercises - Progress cervical segmental exercises - Exercises for C/Th region Home Program - posture training – continues as a lifetime event - Posture training with arm load - CCF training – ensure correct pattern Practice 3 sets of 10 x 10 sec holds at variable pressure levels - Cervical extensors – perform three sets of 5 reps for each of the three tasks - Scapular training – continue side lying exercise. Add SA exercise - Progress kinaesthetic, balance, eye movement as developed from treatment program - Active mobilising exercises as developed in treatment Week 2 Session 4 Posture re-education - Begin gentle loading of the postural position, via arm movement <30 degrees Cranio-cervical flexion training - Progress training of the holding capacity. Target is 10x10 sec holds at 30mmHg Cervical extensors - Train the CCE and CE actions, progress repetition 3 sets of 5 reps of each exercise Scapular muscle training - Continue to train in side lying - Serratus anterior - 3 sets of 5 reps - Train control in posture and with arm movements to 30 degrees - Re-educate scapular control through range of GH abduction and flexion Somatosensory function - Kinaesthetic sense – relocation practice, increase the complexity of movement sense tasks - Progress balance exercises - Eye movement control – perform the three tasks, increase speed, change body position Mobilising exercises - Progress cervical segmental exercises; possibly add MWMs - Exercises for C/Th region Home Program - posture training – and include arm load exercises - CCF training –Practise 3 sets of 10 x 10 sec holds at variable levels. - Cervical extensors – perform 3 sets of 8 reps for each of the three tasks - Scapular training – side lying, 3 sets of 10 sec holds of lower trap. Continue SA exercise - Progress kinaesthetic, balance, eye movement as developed from treatment program - Active mobilising exercises as developed in treatment Page 80 of 102 Week 3 Session 5 Session 6 Posture re-education Posture re-education - Add the ‘occipital lift’ to postural exercise to ensure - Check correction of spinal and scapular posture good facilitation of the CCF - Progress gentle loading of the postural position, via arm - Begin gentle loading of the postural position, via arm movement <30 degrees with resistance 0.5 Kg movement <30 degrees with resistance e.g. 0.5Kg Cranio-cervical flexion training Cranio-cervical flexion training - Progress training of the holding capacity. Target is 10x10 - Progress training of the holding capacity. Target is sec holds at 30mmHg 10x10 sec holds at 30mmHg - Progress but maintain a good pattern - Try to increase range of control of cervical extension - Once participant can perform at 26mmHg, practice controlled eccentric and concentric work through available range of extension Cervical extensors Cervical extensors - Train the CCE and CE actions, progress repetition to 3 - Train the CCE and CE actions, progress repetition 3 sets sets of 8 reps of each exercise, ensure that participant is of 8 reps of each exercise, ensure that participant is gaining full cervical extension range gaining full extension range Scapular muscle training Scapular muscle training - Train control in posture and with arm movements to 30 - Progress serratus anterior to 3 sets of 8 reps degrees with load (0.5Kg) - Re-educate scapular control through range of GH abduction and flexion - Progress serratus anterior exercise to 3 sets of 8 reps of ‘thoracic push ups’ - Address fatigability of upper trapezius – start with 3 sets - Continue to re-educate scapular control through range of of 5 reps of full Abd ROM –with control GH abduction and flexion - Task specific training e.g. typing with balanced scapular - Begin task specific training e.g. typing with balanced muscle control scapular muscle control Somatosensory function Somatosensory function - Kinaesthetic sense – relocation practice, increase - Kinaesthetic sense – relocation practice, ↑ complexity of complexity of movement sense tasks movement sense tasks - Progress balance exercises - Progress balance exercises - Eye movement control – perform the three tasks, - Eye movement control – perform the three tasks, increase speed, change body position increase speed, change body position - Integrate eye movement and balance exercise Mobilising exercises Mobilising exercises - Progress cervical segmental exercises; possibly add - Progress cervical segmental exercises; possibly add MWMs MWMs - Exercises for C/Th region - Exercises for C/Th region Home Program Home Program - posture training – and include arm load exercises with - posture training – and include arm load exercises with 0.5Kg resistance 0.5Kg resistance - CCF training – 3 sets of 10 x 10 sec holds at variable - CCF training –Practice 3 sets of 10 x 10 sec holds at variable levels. Practice eccentric control levels. Practice eccentric control, full ROM abd, 3 sets of - Cervical extensors – perform 3 sets of 8 reps for each of 5 reps the three tasks - Cervical extensors – perform 3 sets of 8 reps for each of - Scapular training – side lying, 3 sets of 10 sec holds of the three tasks - Scapular training – side lying, 3 sets of 10 sec holds of lower trap. Continue SA exercise - Progress kinaesthetic, balance, eye movement as lower trap. Continue SA exercise developed from treatment program - Progress kinaesthetic, balance, eye movement as developed from treatment program - Active mobilising exercises - Active mobilising exercises Week 4 Session 7 Session 8 Posture re-education Posture re-education - Check correction of posture, all components - Check correction of spinal and scapular posture - Increase loading of the postural position, via arm - Progress loading of the postural position, via arm movement <30 degrees with resistance e.g. 1Kg movement <30 degrees with resistance 1kg Cranio-cervical flexion training Cranio-cervical flexion training - Holding capacity. Target is 10x10 sec holds at 30mmHg - Holding capacity. Target is 10x10 sec holds at 30mmHg - Once participant can perform at 28-30 mmHg, practice - Once participant can perform at 28-30 mmHg, practice Page 81 of 102 controlled eccentric holds through different ranges of extension Cervical extensors - Train the CCE and CE actions, progress repetition to 3 sets of 10 reps of each exercise, ensure that participant is gaining full cervical extension range Scapular muscle training - Assess and train control in posture and with arm movements to 30 degrees with load - Progress serratus anterior exercise to 3 sets of 10 reps of ‘thoracic push ups’ - Fatigability of upper trapezius –3 sets of 10 reps of full Abd ROM –with control - Progress task specific training Somatosensory function - Kinaesthetic sense – relocation practice, increase the complexity of movement sense tasks - Progress balance exercises - Eye movement control – challenge change body position, do with walking Mobilising exercises - Cervical segmental exercises; add MWMs - Exercises for C/Th region Home Program - posture training – and include arm load exercises with 1Kg resistance - CCF training –Practise 3 sets of 10 x 10 sec holds at variable levels. Practice eccentric holding in extension - Cervical extensors – perform 3 sets of 10 reps for each of the three tasks - Scapular training – side lying, 3 sets of 10 sec holds of lower trap. Continue SA exercise - Bilateral shoulder abduction, 3 sets of 10 rep - Progress kinaesthetic, balance, eye movement as developed from treatment program - Active mobilising exercises controlled eccentric holds through different ranges of extension Cervical extensors - Train the CCE and CE actions, progress repetition 3 sets of 10 reps of each exercise, ensure that participant is gaining full extension range Scapular muscle training - Continue to train in side lying - Progress serratus anterior to 3 sets of 10 reps - Re-educate scapular control through range of GH abduction and flexion - Address fatigability of upper trapezius – start with 3 sets of 10 reps of Abd –with 0.5Kg - Progress task specific training Somatosensory function - Kinaesthetic sense – relocation practice, ↑ the complexity of movement sense tasks - Progress balance exercises - Eye movement control – challenge change body position, do with walking Mobilising exercises - Cervical segmental exercises; add MWMs - Exercises for C/Th region Home Program - posture training – and include arm load exercises with 0.5Kg resistance - CCF training –Practise 3 sets of 10 x 10 sec holds at variable levels. Practise eccentric holding in increasing extension - Cervical extensors – perform 3 sets of 10 reps for each of the three tasks - Scapular training – side lying, 3 sets of 10 sec holds of lower trap. Continue SA exercise - Bilateral shoulder abduction, 3 sets of 10 rep with 1 Kg resistance - Progress kinaesthetic, balance, eye movement as developed from treatment program - Active mobilising exercises Page 82 of 102 Appendix 3 Technical notes Facilitation of posture There must be special and specific attention placed on retaining the upright postural position. The upright postural position takes the joints of the neck off end range positions but importantly, when facilitated at the lumbopelvic region, it has been shown to facilitate multifidus and longus colli/capitis. The repeated correction of posture during the day is important in retraining the deep cervical flexors in their functional role. Pointers - Some participants have extremely poor kinaesthetic awareness and struggle initially to learn the neutral lumbo-pelvic position. If this is so, delay any teaching of scapular posture to the next session to give them the opportunity to master the first phase. Trying too much too soon will lead to loss of one position. - Ensure that you teach simple self facilitation strategies. For example: Use their own thumb as a proprioceptive cue to regain a neutral L/P position; Try simple strategies to improve scapular position – the 5% stretch of the diagonal rubber band on their chest for a downwardly rotated, anteriorly tilted and protracted scapular, the 5% stretch of a rubber band placed horizontally across their upper chest for protracted scapulae. - Add in correction of head position as a third stage of posture correct. Teach as a gentle manoeuvre to lengthen the back of the neck. This has been shown to strongly facilitate the longus colli. Facilitation and re-education of the craniocervical flexion action - Teach the action of head slide, this is the easiest form of feedback for the participant to learn the correct action. - Utilise eye movement in facilitation. - Use a spot on the ceiling to ensure participants can return to a neutral posture. - Encourage relaxed breathing during the action. - Instruct in the neutral mandibular position if there is a tendency to jaw clench or to substitute with the hyoids. - Teach participant to self palpate superficial muscles. They must understand what a contracted and relaxed muscle feels like. - Even when training the CCF movement, emphasise the hold in CCF. - Be very watchful of this exercise and do not underestimate the skill and attention required to have the participant training their deep neck flexors effectively. Training CCF holding capacity The PBU is required in training the low level endurance of the CCF as neither the physio nor the participant can assess holding accuracy without the feedback. The potential error with using the PBU is that the participant (and physio) can fixate on the pressure dial and not on the CCF action to achieve and hold the pressure. They can revert back to an incorrect pattern as their concentration is now distracted to the dial. This results in totally ineffectual training as has been repeatedly observed in our whiplash research unit. This can be avoided with the following strategies. - In the first week (or a little longer if required), it is advised that the participant practise the holding action with feedback from the PBU in the rooms only under the physios observation and they concentrate on performing the action and feeling the correct sensation of the holding contraction with superficial muscles relaxed. They practise the 10 repetitions of holding concentrating on the CCF action and feel of the holding contraction in the home program. - Once the participant has mastered the correct pattern they practise with the biofeedback and progress up the stages of the action until they can hold 30mmHg for 10secs and do this 10 times. They must be repeated checked by the physiotherapist to determine the maintenance of the correct action and the rate of progression. - Some participants find it difficult to concentrate on the CCF action and the dial simultaneously. In these cases, the physio/participant turns the dial away from the participant and the participant performs CCF to the desired level and then they view the dial to give them feedback on the maintenance of the holding contraction. - This strategy can eventually be used with all participants to train relocation accuracy and is a kinaesthetic training strategy. CCF training in the presence of nerve tissue mechanosensitivity - If participants report increased pain with CCF training, the most likely reason is nerve tissue mechanosensitivity. Always assess before commencing exercises. - In these cases, train in supine initially from extension to neutral. The participant can use eye movement facilitation and also use their thumb to provide gentle resistance and an isometric hold. As tolerated, increase the times and repetitions of the holds in the neutral position, so that they too are doing 10x10sec holds. Page 83 of 102 - If possible, progress into some CCF range, if not possible in the 4 week time frame, stay with the isometrics. Determine if there are other ways you can treat the nerve tissue sensitivity, e.g. sliding exercises. Training the cervical extensors - The CCE and C1-2 rotation are familiar movements and usually present no challenge to train. Ensure a good trunk and scapular position. - The CE is an unfamiliar movement and may require manual guidance when first training. The strategy of ‘keep reading a book’ while curling the neck into extension usually keeps their CC region in neutral. - Beware that participants will substitute an unwanted retraction action. - Keep watching the superficial extensors, these should not predominate with the cervical extension exercise. - Ensure that the physio can perform the correct action in standing, as demonstration is an effective teaching tool. Training the interaction of the deep and superficial flexors (i) This first part of training is re-teaching the action of cervical extension and return from extension in the sitting position. To ensure appropriate balanced work between the muscle groups, the action focuses on initiating neck extension with the chin, ensuring the head is gradually taken posterior to the shoulders and the return is led by cranio-cervical flexion. This training commences once the participant can achieve at least 10x10 sec holds at 26 mmHg. Only move to extension ranges that are pain-free. (ii) The training is progressed to holding the extension position with an emphasis on control of the CCF position. These exercises are performed in predetermined positions of extension as tolerated by the participant and the head is just lifted off a wall or the therapist’s/participant’s hand. (iii) The training is further progressed to head lifts from a resting position on two pillows with all concentration on maintaining the CCF position and not allowing it to move into extension, which signals that the superficial flexors have taken over all work. Task specific training Training scapular muscle control is a very important component oft the motor relearning program. Poor scapular control can overload cervical joints as well as cause local discomfort in the axio-scapular muscles. The low level endurance of the scapular stabilizers is often poor, and they need to be trained out of function (side lying), in function (re-education of postural position), under light load (arm movements without and with light weights) and importantly scapular posture and control must be trained in the tasks in which the participant reports pain. This is often sitting and computer work, though it can be any function. It is necessary to train the participant in their nominated adverse work condition so that they can perform it painlessly. Training somatosensory function - Base selection of exercises on findings of physical examination and relate exercises to level of dysfunction. - If JPE, balance, oculomotor function are all impaired there is a need to address each individual impairment. - Exercise 2-3 times per day, there is a need to take exercises to a point where they might provoke dizziness but they should never exacerbate neck pain or headache. - In progression consider combinations of eye and balance exercises. Kinaesthetic sense - repositioning to neutral with laser feedback (add to home program). - repositioning to points in range with laser feedback. - Movement position sense: follow patterns with laser, progress complexity of patterns. - DNF retraining eyes open-closed. Eye movement control: Gaze stability - Perform with neck rotation, flexion and extension. - Progressions:- Body position, Supine, sitting, standing, walking - Speed - Focus point; pen, spot, complex background - Imaginary - perform with eyes closed - open to check accuracy Eye follow - Directions: rotation, flexion/extension/diagonals; Neck torsion - Progress Positions - lying, sitting, standing (increase difficulty of stance position) Page 84 of 102 - Progress speed Saccades - Directions: rotation, flexion/extension/diagonals Balance Progressions: - Hard surface to foam to unstable - Vision to no vision - Wide to narrow base of support - Two legs to one leg - Functional- stairs, stepping Page 85 of 102 Appendix 4 Graded Exercise Component Overview The graded activity program incorporates four (4) categories of exercise, with each category addressing the different components or elements required to compete everyday tasks. 1. 2. 3. 4. Aerobic exercise (began at the commencement of the exercise program however is being continued and progressed) Range of motion exercise Muscle strength and endurance exercises; Higher level sensorimotor exercises Functional exercise There are a number of different exercises in each category that the therapist can prescribe and progress on an individual basis depending on the participant’s functional goals (identified from PSFS which is progressively monitored throughout the program. Each participant will be prescribed an exercise program to be conducted under the supervision of the physiotherapist which will include 6 – 8 exercises, with at least one exercise from each exercise category. Participants will also be prescribed a home exercise program, which will consist of up to 6 exercises (one exercise from each category). These exercises should be modified to suit the participant’s individual functional goals. Use baseline tests to establish where to start the participant in the series. In each case the participant should record their accomplishments. The physiotherapist will select the exercises to perform and implement them considering the CBT principles. Where prescription of exercise considering physiological principles conflicts with a CBT principles please follow the CBT approach. For example if you decide to prescribe a walking program and the participants baseline walking tolerance is 1 kilometre then you would start them training at 80% of 1 kilometre rather than follow the American College of Sports Medicine’s (ACSM) guidelines and get them to walk for 20-30 minutes three times per week at 60-90% of max heart-rate. It is not essential that participant’s achieve a level of function which is in accordance with the ACSM guidelines. However, these guidelines can be used in participants who have a higher level of baseline function. It is more important that the focus is on participant’s achieving their functional goals and being increasingly self reliant, able to apply the CBT skills to set and progress their own exercise goals. The following sections describe the baseline assessments and suggest a progressive program for each element. Page 86 of 102 1. Aerobic • Walking - progression – increasing speed, time, incline, carrying objects • Cycling (if participant has access to an exercise bike) All participants need to perform aerobic training and the mode of aerobic training selected (e.g. walking, bike) must be able to be continued in the home program. This aerobic training should be commenced in week 1 of the program. Establish the baseline performance with the participant, in accordance with the Borg RPE scale and assist the participant develop the progressive aerobic exercise plan. Borg Rating of Perceived Exertion (RPE) Scale RPE Scale 6 7 8 9 10 11 12 13 14 Effort % 20% effort 30% effort 40% effort 50% effort 55% effort 60% effort 65% effort 70% effort 75% effort 15 16 17 18 19 20 80% effort 85% effort 90% effort 95% effort 100% effort Exhaustion Descriptor Target intensity Very, very light (Rest) Very light gentle walking Fairly light Moderate level of intensity Somewhat hard steady pace Talk test: exercising at an intensity that allows for comfortable speech Hard Very hard Very, very hard FOR REFERENCE: American College of Sports Medicine (ACSM) guided targets: AEROBIC: Type Duration Intensity Speed Frequency Walking, cycling (any activity which employs large muscle groups in activities that are rhythmic or dynamic in nature) 20 to 60 minutes of continuous or intermittent activity NB: aerobic exercise can be broken down into intervals, minimum of 10 minute bouts accumulated throughout the day 11 and 15 on the RPE scale Participant dependant 4 -5 times per week Page 87 of 102 Guide to Exercise Progression WEEK 1-2 AEROBIC: Type Walking, bike Duration 75% 80% of time achieved at initial assessment. NB: aerobic exercise can be broken down into intervals, e.g. 20 minutes achieved in assessment training early minimum of 10 min bouts accumulated throughout the day stage = 15-17 mins. Intensity 11 and 13 on the RPE scale Speed Comfortable walk/cycle Frequency 4 -5 times per week WEEK 3-4 AEROBIC: Type Walking, bike Duration 90% of time achieved at initial assessment NB: aerobic exercise can be broken down into intervals, minimum of 10 min bouts accumulated throughout the day Intensity 11 and 13 on the RPE scale Speed Comfortable walk/cycle Frequency 4 -5 times per week WEEK 5-6 AEROBIC: Type Walking, bike Duration 110% of time achieved at initial assessment aiming for NB: aerobic exercise can be broken down into intervals, 30mins (20-60 mins) continuous exercise minimum of 10 min bouts accumulated throughout the day Intensity 11 and 13 on the RPE scale Speed Comfortable walk/cycle Frequency 4 -5 times per week WEEK 7-8 AEROBIC: Type Walking, bike Duration 120 – 140%% of time achieved at initial assessment NB: aerobic exercise can be broken down into intervals, aiming for 30mins (20-60 mins) continuous exercise minimum of 10 min bouts accumulated throughout the day Intensity 11 and 13 on the RPE scale Speed Comfortable walk/cycle Frequency 4 -5 times per week WEEK 9-10 AEROBIC: Type Walking, bike Duration 160% - 180% of time achieved at initial assessment NB: aerobic exercise can be broken down into intervals, aiming for 30mins (20-60 mins) continuous exercise minimum of 10 min bouts accumulated throughout the day Intensity 11 and 13 on the RPE scale Speed Comfortable walk/cycle Frequency 4 -5 times per week WEEK 11-12 AEROBIC: Type Walking, bike Duration 180% - 200% of time achieved at initial assessment NB: aerobic exercise can be broken down into intervals, aiming for 30mins (20-60 mins) continuous exercise minimum of 10 min bouts accumulated throughout the day Intensity 11 and 13 on the RPE scale Speed Comfortable walk/cycle Frequency 4 -5 times per week Page 88 of 102 1. Range of motion exercises Active range of motion exercises are continued on from motor relearning phase of training • Cervical AROM spine exercises should include active exercises for the cranio-cervical, cervical and cervico-thoracic regions • Muscle stretching exercises (e.g.. pecs) • AROM upper limb exercises emphasising scapular stability. 2. Muscle strength and endurance exercises, higher level sensorimotor exercises These exercises progress from the motor relearning phase and incorporate general strengthening exercises for other body regions. In all upper and lower limb exercises, the participant concentrates on maintaining a neutral spinal position and in upper limb exercises, focuses on scapular control. • Neck flexor and extensor strengthening. • Rotator cuff, Biceps, triceps, trapezius (all three parts) strengthening exercises. • Glut med exercises, squats, calf raises (emphasis on whole body). • Balance / coordination /kinaesthetic training. Baseline assessment for strength and endurance exercises Modify the test position or cease test if the participant complains of excessive discomfort or pain (≥ 2 on 0-10 VAS) in any test. (i) Cervical flexor strength and endurance assessment Determine the head flexion load that the participant can perform 12 times. Protocol - Participant supine in crook lying position with the head on two pillows. - Hands resting on their abdomen. - In performing head and neck flexion, the participant should be instructed to flex the cranio-cervical region to a comfortable range and maintain the chin position while they lift their head attempting 12 repetitions. - Loss of cranio-cervical position is failure in the test. - If the participant cannot perform 12 head lifts on two pillows, position them in reclined lying position, such that they can achieve 12 repetitions. - If the participant can achieve 12 repetitions on 2 pillows, progress test to one pillow and then to no pillow (do tests of other muscles in between repeated tests to gain baseline for cervical flexor exercise) (ii) Cervical extensor strength and endurance assessment Determine the head extension load that the participant can perform 12 times. Protocol - Participant lies prone on the therapy table with their head and cervical spine unsupported. Arms are by the participant’s side with their hands by their hips. - Test range is from 20º flexion to maximum achievable extension. Cranio-cervical region is maintained in a neutral position and the action is a curl into flexion and a curl into extension. The position of the cranio-cervical region can be maintained in neutral by instructing the participant to keep their eyes focussed on an imaginary book on the floor. - Perform test with no added load in the first instance. - For added load suspend weights on a helmet and progress in increments of 0.5Kg to determine baseline. (iii) Upper and lower limb strength and endurance exercises • • Rotator cuff, Biceps, triceps, trapezius (all three parts) strengthening exercises. Glut med exercises, squats, calf raises. Determine the load that the participant can perform 12 times for the respective exercise/muscle group. - Set the participant up in the starting position. Emphasise correct spinal posture and scapular control (as per specific exercise protocol). - Select an approximate weight or theraband that would equate to approximately 12RM for upper limb exercises. - Increase or decrease the load as required. - Establish the weight that the participant can lift 12 times and fatigues for the baseline. - Determine repetitions for lower limb exercises. Page 89 of 102 (iv) Higher level sensorimotor exercises Document level the participant has achieved at week 4 and progress from this point to higher level of exercise e.g. increased complexity of task, combinations. Page 90 of 102 Guide to Graded Exercise Program Progression The graded exercise program is to be performed 4-5 times per week. WEEK 5-6 NECK MUSCLE ENDURANCE AND STRENGTH: Position: on 2 pillows (or position achieved at Neck flexor strength and endurance (head lift exercise) baseline) Repetitions: 10 reps (building to 15 reps over first two weeks Position: prone head off end of plinth Neck strength and extensor endurance Repetitions: 10 reps (building to 15 reps over first two weeks with the baseline load UPPER LIMB ENDURANCE focus on scapular stability and spinal posture during activity Sh Abduction Week 5: Biceps Load: 80% of baseline 15RM Triceps (weights or push downs) Repetitions: 15 Sets: 1-2 Week 6: Load: increase by 10% Repetitions: 15; Sets: 2-3 Rot cuff - ER in sitting Using theraband Load: 80% baseline 15RM Sets: 1-2 Position: side lying set scapula Rot cuff - ER in side lie Weights: Load: 80% baseline 15RM Movt: ER from inner range to neutral Sets 1-2 Week 6 Load: increase by 10% Repetitions: 15; Sets: 2-3 Push ups Load: Begin with scapula control in closed chain under low load (e.g. push ups on wall) Reps: 15; Sets: 1-2 LOWER LIMB ENDURANCE focus on maintenance of trunk stability during activity Calf raises Week 5: Load: 80% of baseline repetitions Squats (to depth achievable) Sets: 1-2 Week 6: Increase by 10% Sets: 2-3 Glut medius (clam in side lie) Load: 80% of baseline repetitions Sets: 1-2 Glut medius (hip hitch in stand) Position: 80% of baseline repetitions Sets: 1-2 Sensorimotor training: refer to progressions described in the motor relearning program. Increase complexity of exercises for balance, eye follow and kinaesthetic sense. Do combinations of exercises WEEK 7-8 NECK MUSCLE ENDURANCE AND STRENGTH: Position: on 2 pillows (or position achieved at Neck flexor strength and endurance (head lift exercise) baseline) Repetitions: progress to 2 then 3 sets of 15 repetitions of the initial 12 repetitions maximum load. Neck strength and extensor endurance Position: prone head off end of plinth Repetitions: progress to 2 then 3 sets of 15 repetitions with load as per weeks 5-6 Page 91 of 102 UPPER LIMB ENDURANCE focus on scapular stability and spinal posture during activity Sh Abduction Load: Load: increase to 20%-30% above starting Biceps load, increase theraband colour Triceps (weights or push downs) Repetitions: 12-15; Sets: 3 Rot cuff - ER in sitting Rot cuff - ER in side lie Push ups LOWER LIMB ENDURANCE focus on maintenance of trunk stability during activity Calf raises Squats (to depth achievable) Glut medius (clam in side lie) Load: Load: increase to 20%-30% above starting load, increase theraband colour Repetitions: 12-15; Sets: 3 Load: Load: increase to 20%-30% above starting load, increase theraband colour Repetitions: 12-15; Sets: 3 Load: Increase to moderate load (e.g. push ups on an incline) Reps: 15; Sets: 3 Repetitions: 15; Sets: 3 Repetitions: 15; Sets: 3 Glut medius (hip hitch in stand) Sensorimotor training: refer to progressions described in the motor relearning program. Increase complexity of exercises for balance, eye follow and kinaesthetic sense. Do combinations of exercises. WEEKS 9-10 NECK MUSCLE ENDURANCE AND STRENGTH: Position: progress to 1 pillows (or progress position Neck flexor strength and endurance (head lift exercise) achieved at baseline) Repetitions: 2 then 3 sets of 15 repetitions Position: prone head off end of plinth Neck strength and extensor endurance Repetitions: increase load by 20-30% Repetitions: 3 sets of 15 repetitions UPPER LIMB ENDURANCE focus on scapular stability and spinal posture during activity Sh Abduction Load: Load: increase by 20%-30%, increase Biceps theraband colour Triceps (weights or push downs) Repetitions: 12-15 Sets: 3 Rot cuff - ER in sitting Rot cuff - ER in side lie Push ups Load: Load: increase to 20%-30% above starting load, increase theraband colour Repetitions: 12-15 Sets: 3 Load: Load: increase to 20%-30% above starting load, increase theraband colour Repetitions: 12-15 Sets: 3 Load: Increase to high load (e.g. push ups or half push-ups on the floor) Reps: 10-15reps Sets: 3 Page 92 of 102 LOWER LIMB ENDURANCE focus on maintenance of trunk stability during activity Calf raises Progress to single leg calf raises Repetitions: 15 Sets: 3 Squats (to depth achievable) Repetitions: 15 Sets: 3 Glut medius (clam in side lie) Place further into ¾ prone Repetitions: 15 Sets: 3 Glut medius (hip hitch in stand) Repetitions: 15 Sets: 3 Sensorimotor training: refer to progressions described in the motor relearning program. Increase complexity of exercises for balance, eye follow and kinaesthetic sense. Do combinations of exercises. WEEKS 11-12 NECK MUSCLE ENDURANCE AND STRENGTH: Position: progress to no pillows (or progress position Neck flexor strength and endurance (head lift exercise) achieved) Repetitions: 2 then 3 sets of 15 repetitions Neck strength and extensor endurance Position: prone head off end of plinth Repetitions: increase load by 20-30% Repetitions: 3 sets of 15 repetitions UPPER LIMB ENDURANCE focus on scapular stability and spinal posture during activity Sh Abduction Load: Load: increase by 20%-30%, increase Biceps theraband colour Triceps (weights or push downs) Repetitions: 12-15; Sets: 3 Rot cuff - ER in sitting Rot cuff - ER in side lie Push ups LOWER LIMB ENDURANCE focus on maintenance of trunk stability during activity Calf raises Squats (to depth achievable) Glut medius (clam in side lie) Load: Load: increase to 20%-30% above starting load, increase theraband colour Repetitions: 12-15; Sets: 3 Load: Load: increase to 20%-30% above starting load, increase theraband colour Repetitions: 12-15; Sets: 3 Load: Increase to high load (e.g. push ups or half push-ups on the floor) Reps: 10-15reps; Sets: 3 Progress to single leg calf raises Repetitions: 15; Sets: 3 Repetitions: 15; Sets: 3 Place further into ¾ prone Repetitions: 15; Sets: 3 Repetitions: 15; Sets: 3 Glut medius (hip hitch in stand) Sensorimotor training: refer to progressions described in the motor relearning program. Page 93 of 102 4. Functional exercises Guiding principles to functional exercises: 1. These exercises should be functional and participant specific - identified from the PSFS. The manner in which the functional exercises are trained will depend on the treating physiotherapist’s own clinical judgement and may involve part practice or whole task practice. The emphasis is on achieving the functional goal and assisting the participant in completing these activities in everyday life. The exercise program should be compatible with and reflect their functional goals and their current abilities. 2. Functional exercises that may be relevant to the participant could include: - Computer work - Driving - Overhead work - Carrying - Lifting - Pushing/pulling - Sport specific activities 3. Ergonomic advice and rehabilitation of the functional tasks that the participant has identified will have likely begun in the initial 4 weeks of training. At this stage of training, emphasis is placed on further improving their functional capacity. 4. As the participant’s exercise capacity improves it is important to gradually increase the complexity of the training activity until eventually the participant is able to perform the goal ADL activity. Complexity of a training exercise may be increased by: - Increasing endurance for the task - Increasing the load - Increasing the number of repetitions - Increasing the speed of movement - Increasing balance requirements - Performing concurrent tasks; linking tasks 5. Training of functional capacity is commenced at 80% of the participant’s capacity and the principles of pacing and exercise quotas are used for progression of exercise. Progressions should be in 10% to 20% increments every 2 weeks of training. Examples of baseline assessment for lifting and carrying tasks • Horizontal lift - Lift milk crate from waist level shelf, move horizontally 4 feet put crate down again. Repeat five times. Scored as maximum safe lifted weight. • Front carry - Lift milk crate off floor or waist height bench, carry milk crate 25 feet forward and then return back to floor or bench. Recorded as maximum safe lift. • (R) or (L)-handed carry - Lift container with handle off waist height bench, carry container 25 feet forward and then return back to bench. Recorded as maximum safe lift. • Loaded reach - Participants stand next to a wall on which a meter rule was mounted at shoulder height. They reached forward at shoulder height, holding a weight that does not exceed 5% of body weight or 4.5kg. The maximum reach distance recorded in cm. • Dynamic push/pull - Ability to push a weighted trolley 25 feet and then reverse and pull 25 feet back to the start position. Scored as maximum weight safely moved. Page 94 of 102 SAFETY CONSIDERATIONS INDICATORS TO CEASE EXERCISE Adapted from the ACSM general indications for stopping an exercise test in low-risk adults: - Onset of angina or angina-like symptoms. - Signs of poor perfusion: light headedness, confusion, ataxia, pallor, cyanosis, nausea or cold and clammy skin. - Failure of heart rate to increase with increased exercise intensity. - Physical or verbal manifestations of severe fatigue. - Participant requests to stop (ascertain reason for discontinuation i.e. psychophysical end point (voluntary test termination due to excessive fatigue or discomfort), aerobic end point (85% of age determined ‘maximum heart rate’) or pain (increase in pain intensity by 2 or more points on 10 point scale). - Significant drop (20mmHg) in systolic blood pressure or failure of the systolic blood pressure to rise with an increase in exercise intensity. - Excessive rise in blood pressure: systolic pressure > 260mmHg or diastolic > 115mmHg. - Failure of the testing equipment. Page 95 of 102 Appendix 7 Cognitive – Behavioural Principles Summary Individuals learn most effectively by doing. Providing information or simply telling someone what to do is a much less effective method of training. During the implementation of these principles it is envisaged that individuals are taught the exercises and become increasingly self reliant and motivated. Shaping is a technique which can assist an individual in achieving a specific activity or behaviour that they currently do not exhibit. It is a gradual process, where initially the individual approximates the target activity/behaviour to the best of their ability. Repetition of the activity allows for it to be refined and reinforced until the target activity/behaviour can be performed. Thus, a perfect performance is not expected or required initially however is expected to be developed over time. Reinforcement occurs when an event following an activity or behaviour increases the likelihood that that activity or behaviour will be repeated in the future. Reinforcers can be thought of as a reward, something that the individual wants to achieve and will therefore work towards. They can be external (e.g. charting progress, praise or feedback) or internal (e.g., sense of personal achievement) and they do not need to occur every time the activity or behaviour (or a similar activity or behaviour) occurs however just often enough that the individual continues the desired behaviour. For reinforcements to be effective it is important that they are: - Consistent i.e. the same activity or task is reinforced in a consistent manner. - Reinforced by the individual themselves i.e. the individual is able to acknowledge what they have done and take credit for their achievements. The ultimate aim is to increase the individual’s self-reliance and ability to implement the principles in order to achieve the goals which are important to them. - Considered to be important to the individual and are potent enough to be a meaningful reward. It is important the individual plays an active role when identifying possible reinforcers for themselves as no-one is likely to work for something they don’t really want to achieve. - Provided as soon as possible following the behaviour e.g., immediate feedback after a performance is more effective than delayed feedback. - Achievable. Short term reinforcers can be used to monitor and reward progress which is required to achieve the longer term goals. Long-term reinforcers will usually be the goal(s) aiming to be achieved. - Progressive i.e. initially it is useful to make the reinforcers or goals easy to achieve as this will assist to encourage and motivate the individual to continue the behaviour. Then as the individual regularly achieves the goal then the task can be made more difficult. Completion of a task can act as a reinforcer itself however it is good to augment this with an external or internal reinforcer. Goal setting: Goals can also act as reinforcers as there is a sense of achievement associated with goal attainment and the individual’s behaviour is reinforced and they can further act as a motivator to achieve more. Ideally, clearly defined goals are of most use i.e. specific, measurable, achievable, realistic and time-based goals. Quotas and pacing When setting an exercise quota it is vital that it is set below the individual’s current activity tolerance and therefore achievable while also not aggravating their symptoms. Fordyce (1976) suggest starting setting the initial quota 20% below what the individual can achieve during the baseline assessment. Once the quota and progressive increments (pacing) are determined it is important that the individual adheres to the program and does not under or overdo the amount of activity prescribed e.g., on a day when their pain in worse it is important that the prescribed amount of exercise is completed despite the extra pain however other pacing strategies can be applied e.g. increasing the number of rest periods between exercises or changing task frequently. However, this does not apply to the motor relearning program of the first 4 weeks, where it is important that these exercises are pain free (see Motor Relearning Program section). If the individual reports that the program is difficult and exacerbates their pain, the set quota may have been too ambitious and should be reviewed and re-set if necessary. If the program continues to be difficult and the individual repeatedly stops short of the quota then the quota may have to be re-set. By setting quotas for exercise the participant has an external goal to aim for taking the focus away from their pain. It is important that the individual understands that the amount of activity is progressed in a time-contingent manner and they do no more on a good day and no less on a bad day. Association effects (Reminders): an exercise program is more likely to be completed if it can be tied to (associate the exercises) with specific times or places. Prior to the individual leaving the clinic it is advised that they have a specific plan for when they will do their exercises and how best they can fit their exercises into their current routine. Reminders or Page 96 of 102 triggers such as a note on the fridge or sticker on a wrist watch can be useful to improve our memory of when to do exercise. Overcoming fear avoidance responses through graded exposure and addressing individual’s thoughts/beliefs/expectations. A key element in managing an individual’s fear or avoidance of activity is identifying the specific factors or thought processes limiting them from participating in the activity/exercise and correcting or clarifying these thoughts. It is important that education and reassurance is given as factual and specific as possible and vague or anxiety-inducing responses such as ‘let pain be your guide’ are avoided. It is important to encourage the individual to resume feared activities and when approached in a gradual and paced manner, exacerbations of symptoms are minimised and functional goals can be achieved. Adapted from: Chapter by MK Nicholas and L. Tonkin in Musculoskeletal Physiotherapy: Clinical Science and Evidence-based Practice. K. Refshauge and E. Gass (eds). Butterworth Heinemann, Oxford, 2nd ed. 2004 Page 97 of 102 Appendix 8 Participant Proforma Please see the separate attachment Page 98 of 102 CHRONIC WHIPLASH EXERCISE TRIAL SENSORIMOTOR EXERCISES 1. HEAD REPOSITIONING TO NEUTRALEXERCISE: ROTATION Place the headband with laser attached on your head. Place the target pattern on the wall one metre away in line with the laser. Sit and focus on the bullseye point on the wall straight in front of you. Close your eyes and rotate your head as far as you can to the left/right. Try and return to the starting position as accurately as you can, open your eyes to see how accurate you have been. 4. Repeat ____ times up to 5 2. HEAD REPOSITIONING TO NEUTRAL EXERCISE: FLEXION AND EXTENSION Sit and focus on the bullseye point on the wall straight in front of you. Close your eyes and take you head as far as you can forwards /backwards. Try and return to the starting position as accurately as you can, open your eyes to see how accurate you have been. Repeat ____ times up to 5 3. HEAD REPOSITIONING TO POINTS IN RANGE EXERCISE: ROTATION Place dots 20 centimetres apart across the wall. Place the headband with laser attached on your head. Sit, close your eyes and rotate your head to find each dot as accurately as you can, open your eyes to see how accurate you have been. Repeat ____ times up to 5 Page 99 of 102 CHRONIC WHIPLASH EXERCISE TRIAL SENSORIMOTOR EXERCISES 4. HEAD REPOSITIONING TO POINTS IN RANGE: FLEXION AND EXTENSION Place dots 20 centimetres apart vertically on a wall. Place the headband with laser attached on your head. Sit, close your eyes and move your head forward or backwards to find each dot as accurately as you can, open your eyes to see how accurate you have been. Repeat ____ times up to 5 5. HEAD TRACKING ACTIVITY Sit and place the headband with laser attached on your head. Place the figure of eight pattern on the wall in line with the laser. With your eyes open, move your head to trace the pattern with the light. Try to be as accurate as possible. Repeat ____ times up to 5 You can make these more difficult by • • • Increasing the speed of movements Performing the activities while sitting on an unstable surface such as a therapy ball Performing the activities while standing with feet in an unstable base of support e.g. heel toe 6. GAZE FIXATION WITH HEAD MOVEMENT Sit on a chair and fixate your gaze on a dot straight in front of you. Keep the target in focus, while you move your head to the left, right, back and forwards. Repeat each movement ____ times, twice a day You can make this more difficult by Increasing the speed and range of movements Adding a busy pattern (e.g. stripes or checks) to the background of the visual target or making the target a word/business card to keep in focus rather than just a spot. • Performing the activities while sitting on an unstable surface such as a therapy ball Performing the activities while standing with feet in an unstable base of support e.g. heel toe, or while walking. • • Page 100 of 102 CHRONIC WHIPLASH EXERCISE TRIAL SENSORIMOTOR EXERCISES 7. EYE/HEAD CO-ORDINATION Sit and rotate the eyes and head to the same side, left and right. Sit and move your eyes first to 30 degrees to the left or right keeping your head still, keep focused and then move your head to that point. Bring eyes back to centre (head still) and then move head back. Sit and rotate your eyes and head to the opposite side, left and right. Repeat each exercise 5 times, twice a day. Move hand, arm, head and trunk following with the eyes 8. EYE FOLLOW WITH THE HEAD STILL Keep your head still and follow a moving target with your eyes, side to side and up and down. Keep your head still and then rotate your trunk to the left/ right. Keep the head still and repeat following the moving target with the eyes, side to side/ up and down Repeat each exercise 5 times, twice a day. To make a moving target, you can shine a laser light onto the wall in front of you and move the laser with your hand. 9. BALANCE Standing with your feet in comfortable, narrow, tandem, single leg stance Maintain your balance for 30 seconds with your eyes open/closed firm/ soft surface You can progress the exercises by • • • • • Comfortable/Narrow/Tandem Changing your foot position Eyes closed Soft surface Walking with head movements (rotation, flexion and extension) while maintaining direction and speed of walking Performing your eye and head exercises whilst balance training Exercise progressions: eyes closed/ soft surface Page 101 of 102 Web appendix 3: Sensitivity analysis using imputed values. Treatment effects, mean (95%CI) at 3, 6 & 12 months Clinically worthwhile effect PRIMARY OUTCOME Pain over previous weeka Replace missing values in both groups with “0” Replace missing values in both groups with “10” Replace advice missing value with ‘0’ and exercise missing value with ‘10’ Replace advice missing value with ‘10’ and exercise missing value with ‘0’ 2.0 14 weeks 6 months 12 months 0.0 (-0.7 to 0.7) p = 0.97 0.2 (-0.5 to 1.0) p =0.544 -0.4 (-1.3 to 0.6) p = 0.456 -0.8 (-1.7 to 0.0) p = 0.057 0.7 (-0.1 to 1.6) p = 0.094 0.2 (-0.5 to 1.0) p = 0.537 0.5 (-0.3 to 1.3) p= 0.237 0.1 (-0.8 to 1.2) p = 0.784 -1.2 (-2.1 to -0.3) p = 0.006 1.8 (1.0 to 2.7) p =0.000 -0.1 (-0.8 to 0.6) p = 0.967 0.0 (0.8 to 0.8) p = 0.967 -0.2 (-1.1 to 0.7) p =0.655 -1.3 (-2.2 to -0.4) p = 0.003 1.1 (0.3 to 2.0) p = 0.011 Page 102 of 102