Optical Frequency Domain Imaging of Human Retina... 9
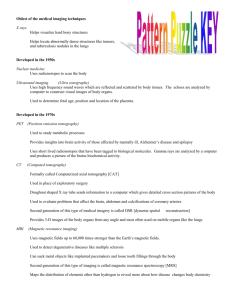
advertisement

Optical Frequency Domain Imaging of Human Retina and Choroid
by
Edward Chin Wang Lee
B.A.Sc. Engineering Physics
University of British Columbia, 2004
SUBMITTED TO THE DEPARTMENT OF ELECTRICAL ENGINEERING AND
COMPUTER SCIENCE IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE
DEGREE OF
MASTER OF SCIENCE IN ELECTRICAL ENGINEERING AND COMPUTER SCIENCE
AT THE
MASSACHUSETTS INSTITUTE OF TECHNOLOGY
JUNE 2006
0 2006 Massachusetts Institute of Technology
/ 9 /All/pights reserved
Signature of Author:
Department of Electrical Engineering and Computer Science
May 20, 2006
Certified by:
Seok-Hyun Yun
Assistant Professor of Dermatology, Harvard Medical School
Thesis Supervisor
Certified by:
Brett E. Bouma
Associate Professor of Dermatology, Harvard Medical School
Member of the Faculty of the Harvard-MIT Divigion of Health Sciences and Technology
Thesis Sunervisor
Accepted by:
Arthtir C. Smith
MASSACHUSETTS NSTITUTE
0 F IECH
LOGY
NOV 0 2 2006
L
IES6
LIBRARIES
Professor of Electrical Engineering and Computer Science
Chairman, Committee for Graduate Students
BARKER
Optical Frequency Domain Imaging of Human Retina and Choroid
by
Edward Chin Wang Lee
Submitted to the Department of Electrical Engineering and Computer Science
on May 20, 2006 in Partial Fulfillment of the
Requirements for the Degree of Master of Science in
Electrical Engineering and Computer Science
ABSTRACT
Optical coherence tomography (OCT) has emerged as a practical noninvasive technology for
imaging the microstructure of the human eye in vivo. Using optical interferometry to spatiallyresolve backreflections from within tissue, this high-resolution technique provides cross-sectional
images of the anterior and posterior eye segments that had previously only been possible with
Current commercially-available OCT systems suffer limitations in speed and
histology.
sensitivity, preventing them from effective screening of the retina and having a larger impact on
the clinical environment. While other technological advances have addressed this problem, they
are inadequate for imaging the choroid, which can be useful for evaluating choroidal disorders as
well as early stages of retinal diseases. The objective of this thesis was to develop a new
ophthalmic imaging method, termed optical frequency domain imaging (OFDI), to overcome
these limitations. Preliminary imaging of the posterior segment of human eyes in vivo was
performed to evaluate the utility of this instrument for comprehensive ophthalmic examination.
The 1050-nm OFDI system developed for this thesis comprised a novel wavelength-swept laser
that delivered 2.7 mW of average power at a sweep rate of 18.8 kHz, representing a two-order-ofmagnitude improvement in speed over previously-demonstrated lasers in the 1050-nm range and
below. The system, with an optical exposure level of 550 gW, achieved resolution of 10 gm in
tissue and sensitivity of >92 dB over a depth range of 2.4 mm. Two healthy volunteers were
imaged with the OFDI system, with 200,000 A-lines over 10.6 seconds in each imaging session.
In comparison to results from a state-of-the-art spectral-domain OCT system, the OFDI system
provided deeper penetration into the choroid.
This thesis demonstrates OFDI's capability for comprehensive imaging of the human retina, optic
disc, and choroid in vivo. The deep penetration power of the system enabled the first
simultaneous visualization of retinal and choroidal vasculature without the exogenous dyes
required by angiography. The combined capability for imaging microstructure and vasculature
using a single instrument may be a significant factor influencing clinical acceptance of
ophthalmic OFDI technology.
Thesis Supervisor: Seok-Hyun Yun
Title: Assistant Professor of Dermatology, Harvard Medical School
Thesis Supervisor: Brett E. Bouma
Title: Associate Professor of Dermatology, Harvard Medical School
Member of the Faculty of the Harvard-MIT Division of Health Sciences and Technology
3
4
Acknowledgements
All I ever wanted to learn about research, I learnt at MIT and Wellman - from tinkering
during rotation, to gaining project ownership, to eventually building a state-of-the-art
imaging system from scratch. Yet, none of this could have been possible without the
tremendous help I received from the incredible people around me. My supervisor Andy
Yun has been an amazing inspiration to me, with his enthusiastic attitude towards science
and seemingly unlimited energy. And how often do you get to shoot a laser into your
boss' eye and get published for it? Brett Bouma, my co-supervisor, is the main reason
behind my finishing this thesis and graduating on time.
I am most grateful for his
guidance and genuine interest in my personal development over the last two years. I
would also like to thank Johannes de Boer and Mircea Mujat for their indispensable roles
in this marvelous collaboration.
Johannes provided his super-stable eye and much-
needed expert opinion on retinal imaging, while Mircea remained extremely courteous
and helpful in spite of my constant harassment. Aside from Andy and myself, Catherine
Bolliet had the honor (misfortune) of spending the most time examining my OFDI
images. I cannot overstate the value of her feedback and artwork for this thesis.
It is rare in life to work in a truly collegial environment, but that is what I have found at
the Wellman Center for Photomedicine. I will definitely miss the marshmallows from
Alyx Chau and her expertise in Word and MATLAB. William Oh and Pilhan Kim have
my gratitude for their patient reception to stupid questions; Jason Motz and Ben Vakoc
have my appreciation for their invaluable technical assistance. I am also indebted to
Gary Tearney and Seemantini Nadkarni for their supervision during my rotation through
mini-projects. Jason Bressner has been a great buddy, and was gracious enough to agree
to be the first person besides my supervisors to read this thesis. And I would like to
extend a big thank-you to everyone else at the lab for their impressive work ethics and
high tolerance for noise.
Like everything else in life, money can be a practical problem for poor graduate students,
even those with high ideals. As someone without the noblest ideals, I fortunately have
5
had the blessing of the Canadian government and education system - I benefited from
Canada's high-quality secondary education and excellent undergraduate training for free.
I would also like to acknowledge the scholarship support for this graduate research from
the Natural Sciences and Engineering Research Council of Canada.
Last but certainly not least, my family and friends have been an inexhaustible source of
love and encouragement. In particular, thank you to Mom and Dad and Susan for your
unwavering support. It means a lot to me to know that, no matter what path I take, I will
always have you on my side.
For one more time, thank you.
Artistic Rendering of Retinal Vasculature by CatherineBolliet
6
Table of Contents
CHA PTER 1: IN TR OD U CTION ..................................................................................
1.1
OPHTHALMIC IMAGING ..............................................................................................
11
12
1.1.1
A Brief History of Inventions and Advances.....................................................................
13
1.1.2
Optical Coherence Tomographyfor Ophthalmic Imaging...............................................
15
THEORY OF OPTICAL COHERENCE TOMOGRAPHY (OCT).........................................
17
1.2 .1
Interferom etry........................................................................................................................
17
1.2.2
From OCDR to OCT .............................................................................................................
20
1.2 .3
SD -O C T .................................................................................................................................
22
1.2
OPTICAL FREQUENCY DOMAIN IMAGING (OFDI).....................................................
24
1.3 .1
B ackground ...........................................................................................................................
24
1.3.2
Sensitivity Advantage ................................................
25
1.3.3
OFDIvs SD-OCT ..................................................................................................................
29
NEW OPPORTUNITY - IMAGING HUMAN RETINA AND CHOROID WITH OFDI ......
31
1.3
1.4
CH A PTER 2: LA SER ....................................................................................................
37
2.1
INTRODUCTION .............................................................................................................
37
2.2
SETUP............................................................................................................................
37
2.2.1
Polygon-BasedFilter............................................................................................................
2.2.2
Design and Operation...........................................................................................................39
RESULTS .......................................................................................................................
2.3
CHA PTER 3: O FD I SY STEM ......................................................................................
37
40
43
3.1
INTRODUCTION ..........................................................................................................
43
3.2
SETUP............................................................................................................................
43
3.2.1
Design and Operation.......................................................................................................
3.2.2
DataAcquisition....................................................................................................................45
43
SIGNAL PROCESSING ....................................................................................................
47
3.3.1
BackgroundSubtraction...................................................................................................
48
3.3.2
Windowing and FourierTransform...................................................................................
49
3.3.3
Interpolationto Linear k-Space..........................................................................................49
3.3.4
DispersionMismatch Compensation.................................................................................
3.3.5
Image Construction...............................................................................................................52
3.3
3.4
RESULTS .......................................................................................................................
51
54
7
CHAPTER 4: IN VIVO IMAGING OF HUMAN RETINA AND CHOROID......... 61
4.1
INTRODUCTION .............................................................................................................
61
4.2
OFDI IMAGING .............................................................................................................
61
4.3
COMPARISON TO AN 840-NM SD-OCT SYSTEM.......................................................
63
CHAPTER 5: VISUALIZING RETINAL AND CHOROIDAL VASCULATURE 67
5.1
INTRODUCTION .............................................................................................................
67
5.2
AUTOMATIC DEPTH-SECTIONING ALGORITHM .........................................................
68
5.3
FUNDUS-TYPE IMAGES ..............................................................................................
72
CHAPTER 6: SUMMARY AND DISCUSSION .........................................................
6.1
SUMMARY.....................................................................................................................
77
6.2
DISCUSSION ..................................................................................................................
79
REFERENCES................................................................................................................
8
77
81
List of Figures
MICHELSON INTERFEROMETER AND DETECTION CURRENT. .......................................................
12
14
16
18
TYPICAL SETUP OF AN OCT SYSTEM. ......................................................................................
20
CREATION OF CROSS-SECTIONAL OCT IMAGE BY SUCCESSIVE AXIAL SCANS. ........................
21
TYPICAL SETUP OF A SD-OCT SYSTEM. ....................................................................................
24
FIGURE I -1. SIDE VIEW OF THE EYE. .............................................................................................................
FIGURE
FIGURE
FIGURE
FIGURE
FIGURE
FIGURE
1-2.
1-3.
1-4.
1-5.
1-6.
1-7.
INDOCYANINE GREEN ANGIOGRAMS. .....................................................................................
COMPARISON OF OCT IMAGE TO HISTOLOGY. ............................................................................
24
FIGURE 1-8. TYPICAL SETUP OF AN OFDI SYSTEM. ......................................................................................
FIGURE
1-9.
WATER ABSORPTION'S WAVELENGTH DEPENDANCE AND ITS IMPLICATIONS ON CLINICAL
A PPLIC ATIO N S. .........................................................................................................................
FIGURE 2-1. WAVELENGTH-SCANNING FILTER. .............................................................................................
31
38
FIGURE 2-2. EXPERIMENTAL SETUP OF WAVELENGTH-SWEPT LASER.........................................................40
FIGURE 2-3. MEASURED LASER OUTPUT CHARACTERISTICS. .....................................................................
41
FIGURE 3-1. EXPERIMENTAL SETUP OF THE OFDI SYSTEM. .........................................................................
44
FIGURE 3-2. TIMING DIAGRAM FOR THE OFDI SYSTEM. ..............................................................................
46
FIGURE 3-3. LABVIEW USER INTERFACE FOR THE OFDI SYSTEM. ................................................................
47
FIGURE 3-4. INITIAL PROCESSING OF DETECTED FRINGES. ........................................................................
48
FIGURE 3-5. NUMERICAL SIMULATION OF ACHIEVABLE RESOLUTION. .......................................................
50
FIGURE 3-6. NUMERICAL MAPPING TO A UNIFORM K-SPACE BY INTERPOLATION. .....................................
50
FIGURE 3-7. MEASURED SNR OF A SAMPLE REFLECTOR AS A FUNCTION OF REFERENCE ARM POWER. ........... 55
FIGURE 3-8. GLASS SLIDE FOR LASER TUNING CALIBRATION. ....................................................................
56
FIGURE 3-9. TREMENDOUS IMPROVEMENT TO REFLECTIVITY PROFILE AFTER INTERPOLATION AND
DISPERSION COMPENSATION. ................................................................................................
57
FIGURE 3-10. RESOLUTION PERFORMANCE ACROSS THE ENTIRE DEPTH RANGE. .......................................
57
FIGURE 3-11. POINT SPREAD FUNCTIONS MEASURED AT VARIOUS DEPTHS. ..................................................
58
FIGURE 3-12. ORIGINAL PLOT OF POINT SPREAD FUNCTIONS BEFORE NOISE FLOOR SUBTRACTION. .............. 59
FIGURE 4-1. REPRESENTATIVE OFDI IMAGE FRAME. ..................................................................................
FIGURE 4-2. COMPARISON OF TWO IMAGING SYSTEMS (OFDI AT 1050 NM AND SD-OCT AT
840 NM).
62
............ 64
FIGURE 5-1. ILLUSTRATION OF AUTOMATIC DEPTH-SECTIONING ALGORITHM. ..........................................
71
FIGURE 5-2. RETINAL AND CHOROIDAL VASCULATURE. ............................................................................
72
FIGURE 5-3. COMPARISON OF OFDI FUNDUS-TYPE IMAGES TO SLO IMAGE. ................................................
74
9
... on eyes ...
You cannot depend on your eyes when your imaginationis out of focus.
-- Mark Twain
10
Chapter 1: Introduction
Humans might have seen the world for ages, but the world has only seen inside the living
human eye for a little over 150 years. Until the invention of the ophthalmoscope by
Helmholtz in 1851, the fine structures inside the living eye had remained an inaccessible
mystery. Since then, there have been many exciting advances in the field of ophthalmic
imaging.
In particular, optical coherence tomography (OCT) has emerged in the last
decade as a practical noninvasive technology that can provide clinically-meaningful
images of the human eye in vivo and in real time. With its unique capability in highresolution cross-sectional imaging, OCT offers a compelling advantage over other
existing technologies for ophthalmic clinical applications.
Current commercially-available OCT systems suffer limitations in speed and sensitivity,
preventing them from effective screening of the retina and having a larger impact on the
clinical environment. While other technological advances have addressed this problem,
they are inadequate for imaging the choroid, which can be useful for evaluating choroidal
disorders as well as early stages of retinal diseases. The objective of this thesis was to
develop a new ophthalmic imaging method, termed optical frequency domain imaging
(OFDI), to overcome these limitations. Preliminary imaging of the posterior segment of
human eyes in vivo was performed to evaluate the utility of this instrument for
comprehensive ophthalmic examination.
The thesis is organized as follows. The rest of this chapter reviews the background for
this thesis, and explores the new opportunity in posterior eye segment imaging with
OFDI at 1050 nm.
Chapter 2 describes the source for the OFDI system - a novel
wavelength-swept laser.
Chapter 3 focuses on system design and operation.
Then
Chapter 4 demonstrates the first OFDI imaging of the human posterior eye and Chapter 5
presents the first simultaneous visualization of both retinal and choroidal vasculature
without the exogenous dyes required by angiography.
Finally, Chapter 6 provides a
summary and discussion of this thesis research.
11
1.1 Ophthalmic Imaging
The human eye is a complex organ of numerous components (Figure 1-1). The posterior
eye segment includes the vitreous, retina, and choroid and is essential to our vision. The
ability to image the posterior segment plays a crucial role in the detection, monitoring,
and treatment of common blinding eye diseases such as glaucoma, diabetic retinopathy,
and macular degeneration.
Vitreous Humor
Ciliary Muscle
Sclera
Body
Aqueous
/Retina
Zonules
Choroid
Cornea-Fovea
Lens
....
.
. ....
ii-Visual Axis--
; ;- Lens Sack
Iris
------- -----....
M acula
Optic Disk-
Canals of
Schlemm
Optic
Conjunctiva
Nerve
Orbital Muscles
Retinal Blood Vessels
Figure 1-1. Side view of the eye.
(reproduced from Charlie Web's website on vision loss and blindness [1])
Light enters the eye through the cornea and is focused by the lens through the vitreous
humor onto the retina, where photoreceptive cells translate optical images into electrical
impulses that the brain understands. Directly opposite the lens, the macular region on the
retina has a dip in its center called the fovea. Densely packed with photoreceptive cone
cells, the fovea provides color vision and enables high acuity.
The optic nerve is
responsible for transmitting electrical signals to the brain, but the nerve cells of the retina
reside inside the multiple layers that absorb excess radiation and supply nutrients. In
order for the optic nerve to connect to nerve cells of the retina, the optic nerve pierces the
retina at a point near the macula called the optic disc. The optic disc is also known as the
blind spot because no photosensitive cells exist there. Beyond the retina lies the choroid,
a vascular layer that supplies retinal cells with oxygen and nourishment.
It is the
reflection of light from the choroidal blood vessels that causes the red eye effect in
photography.
12
1.1.1 A Brief History of Inventions and Advances
The invention of the ophthalmoscope by Helmholtz in 1851 marked the first milestone
towards the goal of imaging the posterior segment. Helmoholtz's design consisted of a
partially-reflecting mirror that directed light from a source onto the retina. The reflected
light transmitted through the partially-reflecting mirror and was magnified to form an
image. With lenses and mirrors, the ophthalmoscope equipped scientists with a tool for
examining the retina. In 1886, Jackman and Webster recorded the first in-vivo human
retinal photograph, showing the optic disc and larger blood vessels [2].
Such en face
retinal photography known as fundus photography was commercialized by Zeiss in 1920.
It was at first limited in clinical use due to the slow speed of film and long exposure time
with the then carbon-arc illumination system, until the invention of the electronic flash in
the 1950s.
Shortly after in 1961, the first successful fluorescein angiography was
administered in humans. Through intravenous injection of the fluorescent fluorescein
dye, fluorescein angiography has become the main diagnostic tool for study of retinal
circulation [3]. The choroid, however, is usually not visible in either fundus photography
or fluorescein angiography, due to the strong scattering and absorption of the retinal
pigment epithelium above it. By the early 1990s, indocyanine green angiography [4] has
gained clinical acceptance for the study of choroidal circulation. The indocyanine green
dye facilitates penetration into the choroid with its infrared emittance and excitation
spectra. Its strong binding to blood proteins also results in slow diffusion out of the
fenestrated choriocapillaris in contrast to the rapid leakage of fluorescein dye, which
prevents visualization of choroidal vascular details.
Webb's invention of the scanning laser ophthalmoscope (SLO) in the early 1980s [5]
thrust the field of fundus imaging into a new era. Instead of capturing the image as a
whole, the SLO samples the retina point by point in a raster-like fashion with its laser
beam. The SLO's high light efficiency allows the laser beam better penetration through
the lens and corneal opacities even at a low light level, resulting in improved spatial
resolution and contrast.
With real-time continuous imaging, the SLO can be used in
conjunction with angiography to monitor dye arrival and leakage (Figure 1-2) [4]. The
SLO is housed in a human interface that uses a high-power condensing lens to image the
13
retina onto a plane within the instrument, which is in turn imaged by another lens to the
eye of the operator or a recording device.
b
a
Figure 1-2. Indocyanine green angiograms for a 48-year-old woman without significant retinal
pathology: (a) 72 seconds and (b) 22 minutes 32 seconds after injection. The choroidal vessels
discernible in Figure (a) are usually not visible in fluorescein angiograms. With the dye exited from
the vasculature in Figure (b), the angiogram is identical to a normal fundus image.
( reproduced from Jozik et al's publication in Retina [4] )
The traditional two-dimensional fundus view from an ophthalmoscope is limited in
clinical diagnostic value and often requires additional techniques such as fluorescein
angiography and visual field testing that are sensitive to the physiologic consequences of
structural abnormalities.
One of the greatest modern developments in ophthalmic
imaging is the ability to evaluate posterior microanatomy in three dimensions.
aforementioned SLO was combined with confocal optics in 1987 [6].
The
In addition to
obtaining a higher contrast by reducing light scatter from other ocular structures, the
confocal SLO is capable of depth-sectioning and enables en face fundus imaging with
micron-scale transverse and -300-im axial resolution. Meanwhile, ultrasound has been
widely used clinically for quantitative measurements of intraocular distances. With its
principle of operation similar to radar detection of aircraft, ultrasound determines
distances within the eye from the echo delay of sound from different boundaries within
the eye. It has the inconvenient requirement of direct contact of the ultrasound measuring
14
device to the cornea or immersion of the eye in a liquid which facilitates transmission of
sound waves into the globe. Standard ultrasound offers axial resolution of 150 pm [7];
although higher-frequency ultrasound can offer higher resolution approaching 20 pm, it
has been limited to use for the anterior segment due to its strong attenuation in biological
tissues [8]. The resolutions of computed tomography and magnetic resonance imaging
are also limited to hundreds of microns [9, 10]. All these current techniques do not have
sufficient depth resolution to provide useful cross-sectional images of retinal structure.
In comparison, optical coherence tomography has emerged as a promising technology for
three-dimensional imaging of the posterior segment, by offering high transverse and axial
resolution (<10 pm) in a noninvasive and non-contact manner.
1.1.2 Optical Coherence Tomography for Ophthalmic Imaging
Optical coherence tomography (OCT) is analogous to ultrasonography in operation.
However, instead of sound waves, OCT measures the echo time delay and intensity of
backscattered light from sites within the eye. Because the high speed of light does not
permit direct detection of echo signals, OCT uses low-coherence
interferometry.
light with
The retina is virtually transparent with extremely low optical
backscattering, but the high sensitivity of OCT enables detection of such weak signals.
In contrast to conventional microscopy, OCT decouples the governing mechanisms for
the axial and transverse resolution, and thus allows for high resolution in all three
dimensions. In short, OCT is a noninvasive, cross-sectional diagnostic imaging modality
that is capable of producing a highly-accurate structural representation of the retina.
OCT was first demonstrated in 1991 for in vitro imaging of the human retina and
atherosclerotic plaque [11]. Then in 1993, the human optic disc and macula were imaged
in vivo [12, 13].
Fortunately for the field of OCT, the rise of the telecommunication
industry brought numerous technological advances in fiber optics, and the industry's
downturn provided sophisticated components at affordable prices.
Hence, it is now
possible to engineer a compact and robust OCT system at low cost. Carl Zeiss Meditec
introduced the first commercial OCT system to the ophthalmic marketplace in 1996. To
15
date, partly due to the ease of optical access to the eye, OCT has made the largest clinical
impact in ophthalmology.
The primary strength of OCT in ophthalmic imaging lies in its high-resolution,
noninvasive imaging of the retina in vivo, as the precise visualization of pathology is
critical for the diagnosis and staging of ocular diseases.
OCT's axial resolution far
exceeds that of ultrasound or confocal SLO, and approaches that of conventional
histology.
Although the imaging depth is limited by the high optical scattering of
biological tissue to a few millimeters, it is on the same scale as histology, sufficient for
imaging the entire thickness of the retina. Figure 1-3 shows the remarkable resemblance
of OCT images to histology. Since excisional biopsy of the retina is unviable, OCT can
serve as an excellent noninvasive tool for diagnosis and monitoring of diseases, as well as
evaluating response to therapeutic intervention. In addition, OCT's ability to examine
posterior microanatomy in three dimensions facilitates detection of diseases in their
earliest stages, when treatment is most effective and irreversible damage can be most
easily prevented or delayed.
a)
b)
Remarkable resemblance of OCT image to histology.
Figure 1-3.
(a) In vivo OCT image of a healthy volunteer near the macular region (obtained
with the system built for this thesis). (b) Histology of a different subject.
( Figure 3b reproduced from Uniformed Services University's website [14])
16
Other advantages of OCT make it a practical tool with significant clinical impact. For
example, the new high-speed OCT systems make real-time diagnosis a reality. Also,
compared to conventional fundus photography, OCT requires no dilation and causes
minimal discomfort to the patient with its low-intensity infrared illumination. Unlike
ultrasound, OCT is a non-contact method that is well tolerated by patients. Moreover,
objective and reproducible quantitative values can be derived from OCT images. For
example, the thickness of a retinal structure is simply the thickness measured from the
OCT image divided by the group refractive index of the retina (n = 1.38 [15, 16]). This is
important, since thickness maps of retinal structures can be useful for detection of
pathology. For instance, a thickness map of the nerve fiber layer is of great diagnostic
value for macular diseases and glaucoma [17, 18].
Last but not least, OCT can be
extended to functional imaging applications such as Doppler blood flow measurements
[15,
19],
blood oxygenation
quantification with spectroscopy
[20],
and tissue
birefringence measurements with a polarization-sensitive system [21].
With its long list of benefits, optical coherence tomography is no longer a research
curiosity. It is gaining acceptance as a clinical diagnostic tool for the three leading causes
of blindness [22] - glaucoma [18], diabetic retinopathy [23], and macular degeneration
[24]. Clinical studies have also been performed to investigate its feasibility for diagnosis
and monitoring of other retinal diseases such as macular edema [17], macular hole [25],
central serous chorioretinopathy [26], epiretinal membranes [27], and optic disc pits [28].
1.2 Theory of Optical Coherence Tomography (OCT)
1.2.1
Interferometry
The heart of optical coherence tomography is the employment of interferometry, a
method with a long history and numerous applications in diverse areas. The Michelson
interferometer commonly used in OCT was invented around 1881. Before its application
in OCT, it provided the famous first evidence against the existence of the aether and
paved the path to modem techniques in optical precision measurements.
17
Figure 1-4(a) illustrates the free-space configuration of a Michelson interferometer. A
collimated light beam is split by a beamsplitter into two arms. Light in the sample arm
probes the sample and its backscattered signal is recombined with light from the
reference arm at the beamsplitter.
Assuming a simplified case where the source is
perfectly coherent (monochromatic) with wavenumber k and the sample is a partial
reflector of reflectance R, the detector current can be expressed as [29]:
idet(t)
oc
(1.1)
2 PrjPRcos(2kzjt))
where Pr is the optical power reflected from the reference arm at the photodetector, P, is
the optical power reflected from the sample arm at the photodetector assuming a perfect
mirror sample, and zo is the sample's position relative to the scanning reference mirror (or
the path length difference between the two arms). In other words, the detector current
varies sinusoidally when the reference mirror is scanned back and forth mechanically
(Figure 1-4b). The DC components of the detector current are neglected in Equation
(1.1), since the desired sample information is contained in the interferometric term.
Reference Mirror
a)
Linht ;nrc
77
liJ
b
)
Detector
c)
Short Coherence Length
Envelope
Long Coherence Length
C
Co
co
t,z
t~z
Figure 1-4. (a) Free-space configuration of a Michelson interferometer. (b) Sinusoidal
detection current with a scanning reference mirror and a perfectly-coherent source.
(c) Detection current with a low-coherence source. The coherence length, 6z, is also shown.
18
Now consider the case of a low-coherence source with finite bandwidth AA. Also assume
that the reflectors are spectrally uniform and that the sample and reference arms consist
of a uniform, linear, and non-dispersive material. The detector current can be expressed
as [29]:
idet(t)
C R -real edJWOATP JS(o - co, )ej(CO)A r d( - wo
2;r
)}
(1.2)
where S(w-wo) is the spectrum of the source with center frequency 0-)o, Azr is the phase
delay mismatch, and Arg is the group delay mismatch. This time, as the reference arm is
scanned, the detector current still oscillates at the carrier frequency (first exponential
term), but is now modulated by an envelope (integral term) that is the inverse Fourier
Transform of the source power spectrum. The envelope is the interferometer's detected
signal of the mirror sample and thus characterizes the system's point spread function
(Figure 1-4c). The width of the envelope (FWHM value), also known as the coherence
length or resolution, is given as follows [29]:
0Z=
22
n 7r AA
(1.3)
assuming a Gaussian source spectral profile of center wavelength AO and bandwidth AA,
and a sample of refractive index n.
This low-coherence interferometry was first applied in the telecommunication industry in
1987 and was called optical coherence domain reflectometry (OCDR). Since interference
is observed only when the lengths of the two arms of the interferometer are matched to
within the coherence length, a short coherence length translates to a high system
resolution. The interferometric approach also offers an extremely high sensitivity. As in
optical heterodyne detection, the weak field from the sample is amplified by the strong
field from the reference beam. Furthermore, the detector current is proportional to the
field of the sample signal rather than its intensity, giving rise to a high dynamic range and
sensitivity.
Therefore, by employing low-coherence light and demodulating the
interference output, OCDR is a nondestructive method used for high-resolution, highsensitivity measurements of optoelectronic devices [30, 31].
19
1.2.2 From OCDR to OCT
It was not long after the development of OCDR when the potential of low-coherence
interferometry for biomedical imaging applications became obvious. Figure 1-5 depicts a
typical OCT system, which has required a few modifications from an OCDR system for
applications in biomedical imaging. First of all, most clinical OCT systems employ fiber
optics for its environmental stability and compactness.
Second, the paramount
importance of resolution in biomedical imaging demands a large source bandwidth, since
the axial resolution is inversely proportion to the bandwidth of the source, as indicated in
Equation (1.3). Short-pulse lasers in laboratories are extremely broadband, but compact
and cost-effective superluminescent diodes or semiconductor-based light sources are
more suitable for building commercial systems. The wavelength of the source also bears
important implications for possible clinical applications with OCT, considering the
absorption curves of tissue constituents (Section 1.4). Third, the requirements for the
mechanical scanning of the reference mirror are different. Higher speed is desired for
imaging to minimize motion artifacts, while the depth for imaging is much less than that
for OCDR due to tissue scattering and absorption.
.. _.-Broadband
Source
Detector
.... .
Mirror
reference arm
(50150)
sample arm
Sample
Figure 1-5. Typical setup of an OCT system. The 50/50 fiberoptic coupler replaces the free-space beam splitter.
OCT is capable of providing three-dimensional information, whereas OCDR operates in
one dimension. With the reference mirror scanning for information in the axial direction,
two orthogonal galvanometer mirrors are used to scan in the transverse directions. The
collimated light in the sample arm reflects off the galvanometer mirrors and is focused by
a lens onto the sample. As the galvanometers change the angles of the mirrors, the beam
focus is scanned across the sample. OCT's trademark cross-sectional 2D image can be
20
created with one galvanometer mirror by successive axial scans at different transverse
locations (Figure 1-6). For 3D data, the second galvanometer mirror also scans slowly in
the other transverse direction for successive cross-sectional images. The compiled 3D
data is often displayed as a movie sequence of cross-sectional images, or used for 3D
rendering of the sample.
....
Scan
Transverse...............................
....................................
Reflectivit
No
Depth
Figure 1-6. OCT's trademark cross-sectional 2D image is created by successive axial scans at
different transverse locations. On the right of the OCT image is a reflectivity versus depth plot for
one axial scan (blue arrow).
For retinal imaging, the galvanometer mirrors are housed in a human interface similar to
that used for the scanning laser ophthalmoscope. The transverse resolution depends on
the imaging optics. Assuming a Gaussian beam at wavelength A, it can be shown [29]
that a lens with a focal lengthf and filled aperture D gives a spot size (1/e
8x
=
Azfcus
=
2
width) of:
(1.4)
rD
and a depth of focus of:
(1.5)
Thus better transverse resolution requires a decrease in the depth of focus, as in
conventional microscopy.
Unlike conventional microscopy or the SLO, OCT's axial
resolution depends only on the temporal coherence properties of the source, and not on
the pupil-limited numerical aperture of the eye or ocular aberrations. In addition, recent
works have shown that adaptive optics can further improve transverse resolution for
retinal imaging [32].
21
Measurements of axial eye length and corneal thickness were some of the first
biomedical applications of low-coherence interferometry [33, 34]. Since then, OCT has
been used to investigate numerous clinically-meaningful physical properties that change
the amplitude, phase, or polarization of backscattered light. It is important to keep in
mind that, despite its accurate description of the retina, OCT reports optical properties of
the tissue and does not necessarily reflect the true histopathologic morphology. As well,
artifacts and other noises can arise when light is strongly attenuated by media opacities
such as corneal edema, significant cataract, and vitreous hemorrhage.
Finally, OCT
images are constructed based on the time delay of reflected light. If the reflected light is
multiply scattered before being collected, it would appear to originate from a site deeper
than the actual location of the reflection. Furthermore, multiple scattering can also cause
speckle, an inherent noise source of coherent imaging.
Fortunately, such multiple
scattering is a minor concern. The retina is a relatively non-turbid tissue, the confocal
configuration of most OCT systems spatially selects singly-scattered light, and multiplyscattered light tends to lose temporal coherence with successive scattering events
preventing detection by OCT.
1.2.3 SD-OCT
As OCT progressed from the research laboratory into the clinical setting, scientists and
clinicians recognized the need to increase acquisition speed without compromising
sensitivity or resolution. This need has been fulfilled by a second-generation technology
called spectral-domain optical coherence tomography (SD-OCT), also known as FourierDomain OCT (FD-OCT) [35, 36]. In the original time-domain method (TD-OCT), the
reference mirror is mechanically scanned to obtain the interference pattern for each
sample depth sequentially in time. In SD-OCT, the entire depth profile is interrogated all
at once, while the reference arm pathlength is kept constant.
The spectrum of the
interference signal is acquired by a spectrometer and then analyzed to yield the desired
depth profile.
22
The spectrometer is often custom-built and consists of a grating, a lens and a CCD array.
The collimated interference light is dispersed by the grating and focused by the lens onto
the CCD array. Assuming a single reflector of reflectance R at depth zo in the sample
arm, the interferometric signal measured by the CCD array is [29]:
ispec(k)
oc
2 PrPRcos(2kzo)
(1.6)
neglecting the DC terms. This means that a single reflector sample induces in the k-space
domain a characteristic
sinusoid, whose frequency and amplitude are directly
proportional to the depth and reflectance of the sample, respectively. Clearly, the depth
and reflectance of the sample can be obtained via the Fourier Transform relation. In the
case of a more complex sample, additional surface reflections simply superimpose
sinusoids of different frequencies corresponding to their depths and reflectances.
Because the Fourier Transform is a linear operation, the complete reflectance profile of
the sample can be reconstructed from the Fourier Transform of ispec(k).
SD-OCT has enabled video-rate imaging at unprecedented speed and resolution. Because
the sensitivity of a SD system does not suffer the same inverse relationship with
resolution as a TD system does [37, 38], ultrahigh resolution is now possible [39, 40].
Also, SD systems can afford to operate at very high speed while maintaining sufficient
sensitivity, owing to their intrinsic sensitivity advantage (Section 1.3.2). Furthermore,
SD-OCT has eliminated inconveniences, such as nonlinearity, associated with the
mechanical scanning of the reference mirror. A TD system is limited in speed due to the
mechanics of its scanning reference mirror, but a SD system is only restrained by the
detection rate of its CCD array. Since affordable broadband sources and spectrometers
are readily available in the 800-nm range, SD-OCT is mostly applied at this wavelength
for ophthalmic applications. Figure 1-7 depicts a typical SD system.
23
J
JLJ
Mirror
,
._.-
!Broadbandi
Source
reference arm
(i 50/50)
Spectrometer
sample armi
Sample
-_ -_._ -_._._._._!
Figure 1-7. Typical setup of a SD-OCT system.
1.3 Optical Frequency Domain Imaging (OFDI)
1.3.1
Background
Optical frequency domain imaging (OFDI), also known as swept-source OCT (SS-OCT),
is another second-generation method for OCT [41]. Like OCT itself, OFDI is based on a
technology
from the telecommunication
industry
-
optical
frequency
domain
reflectometry (OFDR). OFDR is used for characterizing optoelectronic devices [42] as
well as fiber-optic cables [43], and OFDI is its biomedical imaging counterpart. An
OFDI system (Figure 1-8) uses a wavelength-swept laser source and a single
photodetector in place of the broadband source and spectrometer in SD-OCT. Similar to
SD-OCT, OFDI has no scanning reference mirror, and offers the same sensitivity
advantage [37] that makes simultaneous high resolution, speed, and sensitivity feasible.
It enjoys several additional benefits such as reduced susceptibility to motion-induced
signal fading [44], a simple polarization-sensitivity or diversity scheme [45], and a long
ranging depth [41].
Mirror
reference arm
i Tunable
Source
(50/50)
sample arm
Detector !
!1
.
I
Sample
Figure 1-8. Typical setup of an OFDI system.
24
As its name suggests, a wavelength-swept laser sweeps its output wavelength periodically
in time in a monotonic fashion. Assuming a single reflector of reflectance R at depth zo
in the sample arm, the detector current without the DC terms is [41]:
idet(t)
oc
2 PPRcos(2k(t)zo )
(1.7)
where k(t) = 27r / A(t) is the wavenumber of the swept laser at time t. Suppose that the
tuning of the laser obeys the linear relation k(t) = ko + k1 t. Then the linear tuning of the
laser has effectively mapped the k-space into the time domain; the discrete-time detector
current recorded by the data acquisition board can be written as i(t,)=i(k). Equation
(1.7) is thus similar to Equation (1.6) for SD-OCT, with surface reflections inducing
characteristic sinusoids in the detected signal. By analogy, the Fourier Transform will
also yield the reflectance profile of the sample. In reality, the laser does not tune linearly
in k-space, but this can be corrected numerically [41, 46], as explained in Section 3.3.3.
OFDI has been extensively applied in the 1300-nm wavelength range. A main reason for
this is the wide availability of commercial fiber-optic components at 1300 nm and the
lack of a wide-tuning rapidly-swept light source outside this range [47-49]. Besides this,
OFDI can achieve a larger usable imaging depth at 1300 nm as a result of lower tissue
scattering at longer wavelengths. Finally, OFDI is typically preferred over SD-OCT at
1300 nm because affordable high-speed spectrometers are currently unavailable. The
drawback of using long-wavelength sources is the quadratic dependence of resolution on
wavelength (Equation (1.3)): 10-pm resolution requires only 28 nm of bandwidth at 800
nm, but would require 75 nm at 1300 nm.
1.3.2 Sensitivity Advantage
The sensitivity of an OCT system is a measure of the minimum detectable reflectivity R2
in the sample arm. Since the measured signal is proportional to the reflectance R, the
sensitivity is equal to the ratio of the time-averaged signal power to the time-averaged
noise power.
25
1.3.2.1 Noise Sources
There are four main sources of noise in an OCT system: thermal or Johnson noise,
digitization noise, relative intensity noise, and shot noise. Thermal noise arises from
random particle motion in resistors due to their thermal energy. Digitization noise refers
to the excess noise generated in the data acquisition board. Relative intensity noise (RIN)
describes any noise source with a power spectral density that scales linearly with the
mean photocurrent power. Optical source power fluctuation is one example. Shot noise,
on the other hand, is a white-noise process that is a consequence of the quantized nature
of light and charge. The photodetector emits charge at a mean rate that depends on the
detected optical power; however, the time between specific emissions is random. Such
current fluctuations are termed shot noise.
OCT offers extremely high sensitivity for detection of weak reflections from the retina.
Besides utilizing optical heterodyne detection and enjoying the advantage of measuring
optical field rather than intensity, OCT can achieve quantum-limited performance.
Thermal noise and electrical noise can be minimized with a high-gain electrical amplifier
circuit placed before the data acquisition board. RIN can be reduced by appropriately
selecting the reference power and employing dual-balanced detection. When shot noise
becomes the dominant noise source, the OCT system is said to be shot-noise-limited.
1.3.2.2 Sensitivity of TD-OCT
For a shot-noise-limited TD system with detector signal current is and noise current in, the
sensitivity can be shown to be [29]:
SNRTD
-
i (t))
((t)
_
--
_____
(1.8)
2 E, NEB
where q is the quantum efficiency of the photodetector, E. is the energy of a single
photon, NEB is the noise-equivalent-bandwidth of the system, and P, is again the optical
power reflected from the sample arm at the photodetector assuming a perfect mirror
sample. The bracket < > denotes the time average and Equation (1.8) assumes that
26
PsR2<<Pr,which is generally true for retinal imaging. The noise-equivalent-bandwidth is
essentially the electronic detection bandwidth, which is linearly proportional to the
system's axial-line (A-line) rate
fA
and optical bandwidth AAZ.
Since the optical
bandwidth is inversely proportional to the axial resolution 3z, it follows that:
NEB
x
fAAA
oc
fA/z
and
C power -resolution
speed
SNRTD
Equation (1.10) describes the tradeoff in the design of a TD system.
(1.9)
(1.10)
Most retinal
imaging applications require a level of sensitivity close to 100 dB and cannot tolerate a
reduction in sensitivity to achieve a higher frame rate or better resolution. Although the
source is the ultimate limitation on maximum optical power, the maximum power used
for imaging is usually constrained by the safety limit for retinal exposure and is not
considered a design variable. Resolution is critical to identifying retinal structures and
pathologies, while high speed is required to minimize motion artifact and patient
discomfort.
1.3.2.3 Sensitivity of OFDI
For the case of OFDI, recall that the reflectance profile R(z) can be obtained via Fourier
Transform.
This derivation [37, 41] assumes a square-profile spectral envelope and
100% tuning duty cycle for the source, i.e., constant output power in time. A Discrete
Fourier Transform (DFT) of the detector current i(k,) with M samples gives:
M
F(z)
-j2rlm
i(k,)e
=
(1.11)
.
m=1
Parseval's theorem, I F 2
=
MXi2 , holds for both signal and noise [50]. The sampled
noise current can be shown to be mutually uncorrelated in the case of Nyquist sampling
[38, 51]. Hence, the white-noise power adds incoherently, yielding:
(F,
=
I F!
M
=
(f) n
=
M(i).
(1.12)
27
Now consider the signal power in the Fourier domain (reflectivity) for a mirror at depth
zo. It is zero everywhere except for two peaks at zl=±zo, giving
F, (z = +zo
1=1
=
2
- MD,
=
i2
2K~)(.3
S
(1.13)
with the coherent addition of signal power. Therefore,
SNROFDI
-
|Fs((zi
=+Zo
20
M
2
(F2)
SNRTD
(1.14)
and in the shot-noise limit,
SNROFDI
t
s
Ev f
(1.15)
where the A-line ratefA is the tuning speed of the source for OFDI. It can be shown [37,
41] that Equation (1.15) is valid for a more general case where the source spectral
envelope is not square and the tuning duty cycle is less than 100%, if Ps is taken to be the
time-averaged value over one tuning cycle.
In all cases, while the noise power is
distributed across all frequencies, the signal power of a single discrete reflection remains
concentrated in two peaks in the Frequency domain (±zo). Compared to Equation (1.8),
the noise-equivalent-bandwidth for OFDI is equal to only the A-line rate, rather than the
electronic bandwidth which is the A-line rate multiplied by the optical bandwidth. The
significance of this result and the meaning of Equation (1.14) may be better understood
when one considers that M/2 corresponds to the number of spatially-resolvable points in
the ranging depth [41]. For a system of better resolution, M is larger and the sensitivity
gain of OFDI is even more profound. That is because TD-OCT, unlike OFDI, suffers
from the explicit inverse relationship between sensitivity and resolution (Equation
(1.10)).
1.3.2.4 Sensitivity of SD-OCT
The derivation of sensitivity for SD-OCT [37] is straightforward following the above
analysis.
As indicated by Equation (1.6), the SD-OCT signal is also discrete in
wavenumber. While OFDI discretizes its signal by sampling the detected light in time,
SD-OCT performs discretization by dispersing the detected light onto M discrete
28
detectors of the CCD array. The analysis for SD-OCT can be related to that for OFDI by
comparing the integrated signal from one CCD detector,
ispec(km),
to one sample value of
the photodetector current, idet(kd. If the source power is the same for OFDI and SDOCT, the optical power arriving at one CCD detector is reduced by a factor of M. Yet,
the CCD detector's integration time is the entire duration of an axial scan, reducing the
detection bandwidth also by a factor of M. Therefore,
SNRsD
=
E, (f4 IM)
=
SNROFDI
(1.16)
showing that both SD-OCT and OFDI enjoy the same inherent sensitivity advantage in
Fourier-domain techniques.
The resultant higher sensitivity allows higher image
acquisition speed without sacrificing sensitivity.
1.3.3 OFDI vs SD-OCT
This section discusses the two second-generation OCT technologies with respect to key
system performances. Alike in their Fourier-domain analyses, the two technologies differ
in their hardware configurations. OFDI maps k-space to time with a tuning source whilst
SD-OCT maps to spatial location with a spectrometer.
This difference in hardware
contributes to some marked differences in performance.
For both technologies, the reflectance profile is obtained via DFT. As a result, the
highest detectable frequency of the signal corresponds to a reflection at the maximum
depth, which is defined by [41]:
Az
=
4n9A
(1.17)
and depends on the sampling wavelength interval 6A=AA/M according to Nyquist
Theorem. A reflection from outside the depth range will appear in the image by aliasing.
For OFDI, the sampling rate of the data acquisition board limits the sampling wavelength
interval and hence the depth range. For SD-OCT, the limiting factor is the spectral
resolution of the spectrometer. Since a real signal's Fourier Transform is symmetric,
there exists an ambiguity between positive and negative depths.
To avoid the
29
superposition of the positive-depth image upon the negative-depth image, the reference
arm can be adjusted to position the sample entirely on the positive or negative side.
Techniques have also been developed to remove this depth degeneracy [52, 53].
Not the entire depth range is always usable due to sensitivity dropoff. As explained
earlier for TD-OCT, interference occurs only when the pathlength difference is within the
coherence length of the source. In that case, a large bandwidth is desired for a short
coherence length (high resolution). Yet for OFDI, at any instant in time, the laser light is
interrogating the entire depth range simultaneously. A narrow instantaneous linewidth of
the tuning laser enables interference with reflections from large depths, and corresponds
to a slowly-decaying coherence function, a measure of sensitivity dropoff over z. Also
note that the sampling interval should be smaller than the instantaneous linewidth of the
source; otherwise, the coherence function would decay more quickly. For SD-OCT, the
finite width of pixels in the CCD array leads to spatial integration of the interference
spectrum, and causes a strong dependence of sensitivity on depth [51, 54]. In short,
OFDI enjoys a greater ranging depth and a greater usable depth, due to its higher
sampling wavelength interval and narrow linewidth, respectively.
Other qualities of the different hardware lead to further differences in characteristics.
Availability of affordable equipment dictates the operating wavelength range and the
possible clinical applications of each technology accordingly. The A-line rate depends
on the repetition rate of the tuning source and the speed of the CCD array for OFDI and
SD-OCT, respectively. Because an additional photodetector is much more convenient
and economical than an additional spectrometer, polarization diversity, polarization
sensitivity, and dual-balanced detection are more easily implemented in OFDI. Lastly,
SD-OCT's CCD array integrates its signal during the entire A-line acquisition.
Consequently, SD-OCT is more sensitive to phase instabilities [44] induced by motion or
blood flow, with fringe washout resulting in a weaker signal and a smaller dynamic range
for Doppler flow measurements.
30
OFDI and SD-OCT share almost the same relations in terms of resolution. The axial
point-spread function of the system is given by the Fourier Transform of the source
power spectrum, with the axial resolution being inversely proportional to the spectral
width.
For OFDI, the spectrum refers to the time-averaged spectrum of the tuning
source. The transverse resolution is determined by the focusing properties of the optics
and the eye. A high-NA lens in the human interface is desired for a small spot size on the
retina, since a shallow depth of focus can be tolerated with the small retinal thickness.
1.4 New OpportunityImaging Human Retina and Choroid with OFDI
Among the numerous applications of optical coherence tomography (OCT), ophthalmic
imaging is the most clinically-advanced area to date.
Ophthalmic imaging presents
unique challenges in comparison to other imaging applications, because the aqueous and
yitreous humors are 99% water. For this reason, water absorption plays a pivotal role in
any optical imaging system for the posterior eye segment.
Figure 1-9 shows water
absorption's dependence on optical wavelength [55] for roundtrip propagation in a
typical human eye that is modeled as a water volume of 21 -mm length.
4030 -
OFDI
200
10 -
retinal imaging)
SD-OCT
-
retinal imaging
0
700
800
900
1000
1100
0D
OFDI
non-retinal tissue
imaging
1200
1300
Wavelength (nm)
Figure 1-9. Water absorption for roundtrip propagation in a typical human eye that is
modeled as a water volume of 21-mm length. The applications of SD-OCT and OFDI are
also shown at their respective wavelengths of operation. The potential of OFDI for retinal
imaging is investigated in this thesis for the 1 -pm range.
31
The standard spectral range of conventional ophthalmic OCT has been between 700 and
900 nm.
Not only does near-infrared light transmit well through the vitreous, it
minimizes patient discomfort in comparison to visible light.
The availability of
broadband sources was an equally-important incentive that invited the development of
the first-generation time-domain OCT (TD-OCT) systems in the 800-nm range. Spectraldomain OCT (SD-OCT) was also developed at 800 nm to take advantage of the
broadband sources and fast CCD cameras at this wavelength. It has since enabled threedimensional retinal imaging in vivo with superior image acquisition speed and sensitivity
compared to TD-OCT.
Optical frequency domain imaging (OFDI) delivers the same improvements in imaging
speed and sensitivity as SD-OCT and offers several additional advantages. The reduced
scattering at its long operating wavelength (1300 nm) affords greater light penetration
depth, but water absorption at this wavelength becomes a dominator factor for retinal
imaging. Even when assuming a perfectly-reflecting retina, less than 0.5% of incident
light can be measured in reflection. For this reason, only the human anterior eye segment
has been imaged by 1300-nm systems [56, 57]. Until now, however, a clinically-viable
OFDI system has been unavailable outside the 1300-nm range, primarily due to the lack
of a wide-tuning rapidly-swept light source. Therefore, retinal imaging has been out of
reach for OFDI systems.
Recent studies have suggested that the 1-pm region [58-60] could be a viable alternative
operating window for retinal imaging. The zero-dispersion point of water occurs around
1 tm so operation in that range can lead to easier dispersion management. The 1-pm
region could also benefit from less attenuation from scattering in opaque eye media, that
occurs in older patients with cataract lenses and haze in cornea [58]. Most importantly,
there exists a local minimum in water absorption (Figure 1-9) and the small absorption
loss at this wavelength can be compensated with higher incident optical power. The
ANSI (American National Standards Institute) standards govern the maximum limits on
optical power incident on human eyes [61].
With the retina being the main safety
concern, the ANSI standards are concerned with the actual power impinging the retina.
32
Hence, the ANSI power limitations, having taken water absorption into account, are less
restrictive at longer wavelengths.
For continuous exposure up to eight hours, the
maximum power of light into the pupil is 600 ptW at 800 nm.
At 1050 nm where
roundtrip water absorption loss is -3 dB, the maximum power is 1.9 mW. Therefore, the
absorption loss at 1050 nm can be compensated by imaging at a higher power that is still
well below the ANSI safety limit. In contrast, the huge loss of -20 dB at 1300 nm
requires power beyond the capability of existing lasers and the ANSI safety limit, which
does not rise as fast as water absorption beyond 1 pim. It should be noted that the correct
value for maximum power is obtained by multiplying the area of the human pupil by the
maximum power density from the ANSI standards.
Imaging in the 1-pm region could also potentially offer deeper penetration into the
choroid below the retinal pigment epithelium (RPE) [58].
The highly absorbing and
scattering nature of the RPE becomes evident in the case of RPE atrophy, in which
enhanced penetration and visualization of the choroid is observed [58]. Most of the eye
structure is designed to facilitate transmittance of light to the retina, where light is
absorbed by photoreceptors. Melanin, a chromophore in the RPE and choroid, absorbs
any excess radiation to prevent disruptive reflections within the eye that might otherwise
result in the perception of confusing images. In fact, it is the choroid that gives the inner
eye a dark color. Due to melanin's strong absorption, typical 800-nm OCT images show
weak signals from only superficial layers of the choroid. Melanin does have a decreasing
absorption spectrum from 600 nm to 1200 nm and scattering in biological tissue exhibits
a similar trend. Therefore, there exists a window of opportunity in the 1 -pm region for
deeper penetration into the choroid.
The visualization of morphological features in the choroid can offer substantial benefits.
Early stages of retinal pathologies such as age-related macular degeneration and
proliferative diabetic retinopathy are often accompanied by choroidal neovascularization
[62], an extensive growth of new blood vessels in the choroid and retina which
irreversibly impairs vision in the affected regions. Therefore, the ability to image the
choroid and detect the onset of choroidal neovascularization can provide valuable insight
33
to retinal specialists. Many diseases of the retina also have characteristic findings in
choroidal circulation, whose current imaging method requires intravenous injection of
indocyanine green dye.
The visualization of this choroidal vasculature with a non-
contact, non-invasive OCT technology could have a significant clinical impact.
This thesis reports the development of a high-performance wavelength-swept laser with a
center wavelength at 1050 nm. The laser source was incorporated into an OFDI system
and the first OFDI imaging of posterior segments of the human eye in vivo with high
image acquisition speed, sensitivity, and penetration depth was demonstrated. With the
system's enhanced penetration, depth-sectioned fundus-type reflectivity images of the
choroidal capillary and vascular networks were also obtained.
34
35
... on seeing ...
"The trick is to love somebody. Ifyou love one person,
you see everybody else diffkrently
--
36
James Baldwin
Chapter 2: Laser
2.1 Introduction
During the last decade, the development of rapidly scanning, widely tuning laser sources
has been driven by diverse applications in optical reflectometry, sensor interrogation, test
and measurement applications, and biomedical imaging. A commonly-used technique is
to employ an intracavity narrowband wavelength-scanning filter.
Although single-
frequency operation was demonstrated with sophisticated grating filter design [63], it is
not essential for imaging applications and can be compromised to enhance tuning speed.
Sufficiently-narrow linewidths and wide sweep ranges were achieved by the use of
rapidly-tuning elements such as acousto-optic filters and Fabry-Perot filters [64, 65].
Yet, their speed had been less than 1 kHz, inadequate for video-rate biomedical imaging.
In 2003, a novel wavelength-scanning filter based on a polygon scanner and diffraction
grating was developed. The filter was incorporated into a 1300-nm extended-cavity laser
[66] that achieved a variable repetition rate an order of magnitude faster than previously
demonstrated.
The rest of this chapter describes the principles, design, and
characteristics of the rapidly scanning, widely tuning laser - the key enabling element of
the 1050-nm OFDI system for posterior eye imaging.
2.2 Setup
2.2.1
Polygon-Based Filter
As shown in Figure 2-1, the wavelength-scanning filter comprises a diffraction grating, a
telescope with two lenses in an infinite-conjugate configuration, and a polygon mirror
scanner. With the grating at the front focal plane of the first lens and the polygon spin
axis at the back focal plane of the second lens, the telescope serves two distinct roles: the
conversion of diverging angular dispersion into converging angular dispersion, and the
control of the imaged beam size and convergence angle at the polygon. As indicated in
37
Figure 2-1, from all the light converging onto the polygon scanner, only a narrow band
that is normal to the front mirror facet is reflected back at any instant in time. As the
polygon scanner rotates, the filter selects the narrow spectral band of light that is
reflected back through the telescope into the laser cavity, and thus accomplishes
wavelength tuning. The actual direction of wavelength tuning depends on the orientation
of the beam's incidence angle and rotation direction of the polygon. For example, Figure
2-1 illustrates a sweep in increasing wavelength.
fibeir-o
Polyon mirror
r
Figure 2-1. Wavelength-scanning filter. F, and F2 are the focal
lengths of Lens 1 and Lens 2, respectively.
( reproduced from Yun et al's publication in Optics Letters [66] )
The following derivation [66] assumes a collimated Gaussian beam incident on the
grating. By the grating equation, the center wavelength of the filter's tuning range is:
-%
p (sin a+ sin/p)
=
where p is the grating pitch, and a and
p
(2.1)
are the angles of the incident beam and the
optical axis of the telescope, respectively, with respect to the grating normal.
The
instantaneous linewidth of light from the filter's output can be shown to be:
F1FWHM
where A =
=
AAGpm)cos(a/W)
(2.2)
41n2/;r, m is the diffraction order, and W is the l/e 2 width of the Gaussian
beam at the collimator. If the angular range of the spectrum incident upon the polygon is
greater than the facet angle (6 = 2n/N), the N-sided polygon mirror can retroreflect more
than one spectral component at a given time. The spacing of these spectral components is
called the free spectral range:
AAFSR
38
=
p9(F2 /F)cosp8
(2.3)
where F1 and F 2 are the focal lengths of the first and second lens, respectively. Although
the tuning range of the filter is fundamentally limited by the finite numerical aperture of
the first lens, in practice it is the free spectral range that determines the tuning range of
the laser for a homogenously-broadened gain medium. Finally, in order to maintain the
duty cycle of the laser sweep at 100%, all the beams within the spectral tuning range
should fall within a mirror facet without clipping, or equivalently,
(F2 -S)9+W'
<
2L
(F 2 -S)o -W'
>
0
and
(2.4)
(2.5)
where W'= W(cos f/cos aXF2 /FI) is the beam size at the polygon mirror and S is the
distance between the second lens and the front of the polygon mirror.
The filter of the 1050-nm system in this thesis was designed in accordance with the above
equations and in consideration of the bandwidth of the available semiconductor optical
amplifier (SOA).
A laser source with a large bandwidth is desired for high system
resolution, but the limited bandwidth of the SOA presents a tradeoff. If the filter's free
spectral range is too small, the full bandwidth of the SOA would be underutilized; if it is
too large, the laser will operate with a reduced duty cycle. Optical components were
selected with the following optimal parameters: p = 1200 lines/mm, F1 = 100 mm, F2
=
50 mm, N = 40, m = 1, a = 65 deg, and / = 21.5 deg. Corresponding to these design
parameters, the theoretical linewidth was ~0. 1 nm and the free spectral range was 61 nm.
2.2.2 Design and Operation
Figure 2-2 depicts a schematic of the laser source incorporating the wavelength-scanning
filter. The linear-cavity configuration is an attractive alternative to the previous ring
cavity design [66] as low-loss, low-cost circulators and isolators are not readily available
at 1050 nm.
The gain medium was a SOA that was recently introduced to the
commercial market (QPhotonics, Inc., QSOA-1050). It was bi-directional and driven at
an injection current level of 400 mA. One port of the amplifier was coupled to the filter.
The other port was spliced to a Sagnac loop mirror made of a 50/50 coupler. The Sagnac
loop also served as an output coupler [67].
Two counterpropagating waves traveled
39
along identical paths in the loop, but were in different polarization states during different
parts of the loop, depending on the tuning and location of the polarization controller PC,.
Hence the reflectivity and output coupling ratio were complementary and optimized by
adjusting PC, to tune the amount of birefringence-induced non-reciprocity in the loop.
Sweep repetition rates of up to 36 kHz were possible with 100% duty cycle, representing
a significant improvement over previously demonstrated swept lasers that offered tuning
rates of a few hundred Hz in the 1050-nm range and below [47-49]. In order to achieve a
good depth range given the speed limitation of the available data acquisition board, the
laser was operated at a repetition rate of 18.8 kHz in the OFDI system, producing a
polarized output with an average output power of 2.7 mW.
lO"p minrw
PC,
50150
Pc
G
Lens
Lens
Polygon
scanning fter
Figure 2-2. Experimental setup of wavelength-swept laser.
2.3 Results
Figure 2-3(a) depicts the output spectrum measured with an optical spectrum analyzer in
peak-hold mode (resolution = 0.1 nm). The output spectrum spanned from 1019 to 1081
nm over a range of 62 nm determined by the free spectral range of the filter. The spectral
range coincided with a local transparent window of the eye.
The roundtrip optical
absorption in human vitreous and aqueous humors was estimated to be 3 - 4 dB based on
known absorption characteristics of water (Figure 2-3a) [55].
Using a variable-delay
Michelson interferometer, the coherence length of the laser output, defined as the
roundtrip delay resulting in 50% reduction in interference fringe visibility, was measured
to be approximately 4.4 mm in air. This value represented the entire usable depth range,
40
including the positive and negative regions. From this value, the instantaneous linewidth
of laser output was calculated to be 0.11 nm.
(a)
(b)
'
08
6
\
j.
08
s
0.4
4
E
25
2
1020
1040
10
1080
3
0--50
0,111I",.T (nm)
0
Time
50
100
(ps)
Figure 2-3. Measured laser output characteristics. (a) Peak-hold output spectrum (blue
curve) and optical absorption in water (red curve) for 42-mm propagation distance
corresponding to a roundtrip in typical human vitreous. (b) Time-domain output trace.
Figure 2-3(b) depicts an oscilloscope trace of laser output showing 100% tuning duty
cycle at 18.8 kHz (single shot, 5-MHz detection bandwidth).
represents instantaneous optical power.
The y-axis of the trace
When lasing was suppressed by blocking the
intracavity beam in the polygon filter, the total power of amplified spontaneous emission
(ASE) in the output was ~0.5 mW. Since ASE is significantly suppressed during lasing,
it is expected that the ASE level in the laser output should be negligible.
The laser output exhibited significant intensity fluctuation (-8% pp). The fluctuation was
a consequence of an etalon effect originating from relatively large facet reflections at the
SOA chip, with a thickness equivalent to 2.5 mm in air. In the imaging system, the
etalon reflection could cause interference with sample reflections, but due to its low
intensity, no ghost image was observed for retinal imaging.
41
... on life (and science) ...
"Ihear and I target. I see and I remember. I do and1 I understand.
-- Confucius
42
Chapter 3: OFDI System
3.1 Introduction
Optical frequency domain imaging (OFDI) was championed in the 1300-nm region [41],
driven by the development of high-speed wavelength-swept sources based on available
semiconductor optical amplifiers [66, 68].
In addition to delivering improvements in
imaging speed and sensitivity over TD-OCT, OFDI offers several additional advantages,
such as reduced susceptibility to motion-induced signal fading [44], simple polarizationsensitivity or diversity scheme [45], and long ranging depth [41]. The rest of this chapter
describes the setup, operation, and characteristics of a 1050-nm OFDI system developed
for posterior eye imaging.
3.2 Setup
3.2.1
Design and Operation
An OFDI system, comprising a fiber-optic interferometer, a human interface for retinal
imaging, detection electronics and a computer, was constructed using the 1050-nm
wavelength-swept laser as a light source (Figure 3-1).
The single-mode fiber-optic
implementation of the interferometer had the advantages of layout simplicity, alignment
convenience, and portability. It also ensured the mutual spatial coherence of the sample
and reference light incident on the detector. Furthermore, single-mode wideband fiberoptic couplers are commercially available with arbitrary splitting ratios, and have proved
to be excellent replacements of beamsplitters.
The sample arm (30% port) was connected to a human interface. The human interface
was originally designed by Cense et al [21] based on a slit lamp. The slip lamp, an
instrument commonly used by ophthalmologists for routine corneal and retinal exams, is
a bio-microscope on a movable table with a headrest. When adapted with suitable lenses
43
and galvanometer scanners, it became a clinically-applicable human interface for retina
imaging. Aberrations in the eye limited the diameter of the collimated beam to 2.5 mm
and the focal beam size (transverse resolution) to approximately 10 pm in tissue (index =
1.38). The optical power level at the entrance pupil of the eye was measured to be 550
pW, well below the 1.9-mW maximum exposure level at 1050 nm according to the ANSI
laser safety standard for continuous exposure.
XYscannr
swept
laser
Eye
30(70
Computer
90110
NO
arm
Figure 3-1. Experimental setup of the OFDI system.
The reference arm (70% port) employed a transmission-type variable delay line.
A
neutral-density attenuator was used to obtain the optimal reference-arm power. Light
returning from the sample was combined with the reference light at a 50/50 coupler and
the resulting interference signals were measured with an InGaAs dual-balanced detector
(New Focus, Inc., 1811). By using a transmission-type variable delay line instead of the
usual reflection-type, the OFDI system achieved dual-balanced detection without any
circulators. Not only does balanced detection reduce RIN, it also improves the dynamic
range, reduces fixed-pattern noise, and suppresses self-interference noise originating
from multiple reflections within the sample and optical components including the laser
[51, 69]. The balanced detector achieved a common-noise rejection efficiency of -25 dB
in the range between DC and 5 MHz. The detector signal was further amplified (10 dB)
to minimize the effects of excess electrical noise. It was then low-pass filtered and
digitized at 10 MS/s with a 12-bit data acquisition board (National Instruments, Inc., PCI6115).
44
In the reference arm, a 10% tap coupler was used to generate sampling trigger signals for
data acquisition. The tapped laser output was launched into free space from a collimator,
dispersed by a grating, and focused by a lens onto a fast InGaAs photodetector. This
setup acted as a narrowband fixed-wavelength filter; the detector generated a pulse when
the output spectrum of the laser swept through the narrow passband of the filter. The
detector pulse was converted to a TTL pulse train with an electronic circuit and the TTL
pulses were used to generate gating pulses for signal sampling at the data acquisition
board.
3.2.2 Data Acquisition
A complete OFDI imaging system is a complex instrument of many optical and
electronic components. In order to acquire meaningful image data, the dynamic functions
of the system's laser driver, scanning optics, and digitization electronics have to be
coordinated. With the advance of digitization and computer technology, the hardware
comprising the synchronization and image acquisition electronics can be as simple as a
multifunctional data acquisition board (DAQ) residing in a personal computer, with a
LabVIEW user interface.
Figure 3-2 is the timing diagram for the OFDI system. The speed of the polygon scanner
determined the A-line rate and was controlled by a driver that took a 5-Vpp square wave
as its input. For this particular polygon scanner, the A-line rate fA was ten times the
frequency of the input square wave. A function generator generated the square wave, but
the clock output of the DAQ could also be used.
As the polygon scanner rotated, a
triggering signal (Figure 3-2a) was created for each A-line scan by the narrowband filter
and converted into a TTL pulse train by an electronic circuit. Upon reception of each
TTL pulse, the DAQ acquired M samples. Recall that M, the number of samples in each
A-line, is proportional to the imaging depth range. For the purpose of retinal imaging, M
was chosen to be 512 for an imaging depth of 2.44 mm in air (1.77 mm in tissue). This
also means that the maximum A-line rate was 19.5 kHz, limited by the DAQ's maximum
sampling rate of 10 MS/s. At a lower A-line rate, the system could gain a larger depth
45
range with a higher value of M, but a higher A-line rate could only be achieved if the
system sacrificed its depth range or employed a faster DAQ. In the experiment, the
system was operated at 18.8 kHz with 512 samples per A-line (Figure 3-2b).
In this
configuration, the data samples at the very beginning and end of each sweep were
excluded and their discontinuous slopes would not distort the depth profile in the Fourier
domain. Electrical ramp signals were also used to control the galvanometer mirrors of
the human interface for transverse scanning (Figure 3-2c).
a)
fA = 18.8 kHz
b)
Trigger
f= 18.8 kHz M = 512 samples
>*-.
500 A-lines
-Signal
DAQ Sampling
C)
Period~b = 500 A-lines/frame x
200 frames/scant.
pr ..
...cvi
c
ra
e
Periodfast = 500 A-lines/frame
---Fast Transverse Axis
- = = Slow Transverse Axis
Figure 3-2. Timing diagram for the OFDI system. (a) Triggering signal for each A-line.
(b) Sampling with the data acquisition board. (c) Ramp signals for transverse scanning.
The user-friendly LabVIEW interface (Figure 3-3) provided convenient control and realtime feedback of the imaging environment. The window at the top left corner displayed
the acquired samples for each A-line in real time. Although the triggering signal was not
automatically synchronized to the beginning of each sweep, a potentiometer on the TTL
46
triggering circuit could be used for adjustment by monitoring the displayed A-line. The
operator could also use the interface to output a sawtooth waveform from the DAQ to
drive a galvanometer-mirror for transverse scanning. The period corresponded to the
number of A-lines in the cross-sectional frame, which was displayed in real time at the
bottom right corner. Similarly, the interface could be used to synchronize transverse
scanning to the beginning of each frame acquisition.
An external function generator
drove the slower axis of transverse scanning, whose period corresponded to the number
of frames in a scan across the retina. This could also be replaced by using the second
signal output of the DAQ. Finally, the top right window displayed the depth profile, the
Fourier Transform of the acquired A-line in the top left window. With a sample reflector,
the user could optimize the imaging system's reference arm power, polarization
alignment, and dual-balanced detection by monitoring and maximizing the signal in the
depth profile.
Figure 3-3. LabVIEW user interface for the OFDI system.
3.3 Signal Processing
Signal processing involves several steps, including reference subtraction, envelope
apodization (windowing), interpolation into linear k-space, and dispersion mismatch
compensation. The subtleties of image construction are also discussed below.
47
3.3.1 Background Subtraction
At the beginning of every image acquisition, a reference image was obtained by blocking
the sample arm. This reference image consisted of a residual background signal from the
reference light, as a result of the wavelength-dependent splitting ratio of the 50/50
coupler [41] and imperfect symmetry of the balanced detectors. Subtracting the reference
from the interference signal can account for source fluctuations between measurements
and eliminate fixed-pattern artifacts at low frequencies (depths).
The raw data of a
typical A-line after balanced detection is depicted in Figure 3-4(a).
The desired
interference signal is contained in the fringes that are superimposed on the reference. It
should be noted that the reference also fluctuates in optical power. Since this fluctuation
is random in phase, it can be removed by averaging all A-lines in the reference image.
Figure 3-4(b) shows the fringes after subtraction of the averaged reference. The fringes
were then normalized with their envelope, before apodization with a Gaussian window,
as illustrated in Figure 3-4(c,d).
Raw Data
a)
--
b)
----
After Reference Subtraction
C)
--
d)
0
---
100
200
300
Time (samples)
Reference
-
400
Normalized
Gaussian-Windowed
500
600
Figure 3-4. Initial processing of detected fringes. (a) Raw data - fringes superimposed
on the reference. (b) Fringes after subtraction of the averaged reference. (c) Normalized
fringes. (d) Apodized fringes.
48
3.3.2 Windowing and Fourier Transform
Apodizing interference fringes with a proper window function before Fourier
Transform can suppress sideband ripples to avoid image artifacts and realize better image
contrast [70, 71]. On the other hand, by the convolution property of Fourier Transform,
window functions impose a limit on the achievable width of the point spread function.
Consequently, the choice of an appropriate window function represents a tradeoff
between ripple suppression and resolution [72]. Consider a numerical simulation with a
perfect sinusoid as the time-domain data (Figure 3-5a). The use of no windowing,
Gaussian windowing, and Hamming windowing yielded resolutions of 11 ptm, 13 pim,
and 17 pim, respectively.
It is important to realize that, as opposed to the theoretical
value predicted by Equation (1.3), these values were the practical limitations on
achievable resolutions, in the sense that they were the best attainable values even when
assuming perfect raw data and no error sources. As expected, the best resolution was
achieved with no windowing, at the expense of substantial ripples (Figure 3-5b). For this
thesis research, the Gaussian window was chosen for its high resolution and reasonable
ripple suppression. By inspection, the Gaussian window indeed produced the highestquality retinal images, compared to other window functions. Note that windowing can
also impose a penalty on sensitivity if the effective average power is lower after
normalization and windowing. For the experiment in this thesis, this corresponded to a
sensitivity loss of -2 dB, given the envelope of the time-domain data.
3.3.3 Interpolation to Linear k-Space
The Fourier-Transform relationship (Equation (1.11)) between the time-domain fringe
data and the Fourier-domain depth profile assumes a tuning source that sweeps linearly in
k-space. Nonlinearity in the tuning curve of the laser results in chirping of the signal, and
this variation in the characteristic frequency of a given reflection leads to resolution
degradation in z-space.
A solution to this image blurring problem is to sample the
detector signal in nonlinear time intervals to compensate for the frequency chirping of the
source [56]. Alternatively, the existing chirped signal can be numerically mapped to a
uniform k-space by interpolation prior to Fourier Transform (Figure 3-6) [41, 46].
49
Although both methods were previously demonstrated to yield a transform-limited axial
resolution, the second method is preferred for its ease of implementation in software.
a)
Perfect Sinusoid
-C--
---
Gaussian Envelope
Hamming Envelope
'U
Time
b)
Figr 1-.
NNo
Window wGaussian
windowing, -usnw
LeTHamming
0.6 -
-
=0.4 --
w0.2-
0
190
200
z4
210
Depth (pm)
220
230
240
Figure 3-5. Numerical simulation of achievable resolution. (a) Perfect sinusoid
shown with Gaussian and Hamming envelopes. (b) Point-spread functions with no
windowing, Gaussian windowing, and Hamming windowing.
-
onLinear Tuning
Nonlinear Tuning
t
Figure 3-6. Numerical mapping to a uniform k-space by interpolation.
50
The actual tuning curve of the laser is unknown, unless one explicitly measures it.
Alternatively, one can estimate its polynomial expansion by iteratively searching for
parameters that optimize the system's point spread function, in terms of resolution and
symmetry. This procedure can be implemented with an automated algorithm, but it was
carried out manually for this thesis, because it only had to be done once for a given laser
configuration. The use of two parameters was found to be sufficient for this application,
and the duration of the entire procedure was about 5 - 10 minutes. In the laboratory
setting, the laser tuning curve remained stable over time and did not require recalibration.
Sometimes more data points in the z-domain (512 by default) are needed to better
visualize the reflectivity profile or compute a more precise value for resolution. Direct
interpolation (linear, spline, or FFT) from a reflectivity profile is possible, but it is more
accurate to perform an N-point DFT (N>512) of the time-domain data.
3.3.4 Dispersion Mismatch Compensation
Chromatic dispersion arises from the wavelength dependence of the speed of light and
increases linearly with propagation length in a dispersive medium.
In optical
communications and ultrafast measurements, dispersion compensation is essential for
preserving pulse shape and temporal resolution [73]. Fortunately for OCT technologies,
only the dispersion mismatch between the two arms of the interferometer must be
compensated for optimal resolution. Compensation in hardware was demonstrated by
matching the optical materials and path lengths in the two arms [22, 74], and
compensation in software was proved feasible in TD-OCT systems [75, 76]. Recently, a
software compensation method for SD-OCT was introduced by Cense et al [39]. This
flexible method is well suited for retinal imaging, because dispersion compensation needs
to be tailored to individual subjects with different and unknown axial eye lengths. The
method is also directly applicable to OFDI, which has the spectral fringe pattern readily
available in its detected signal.
Dispersion mismatch introduces a phase shift e'o(k) in the detected spectral fringe pattern
i(k). By Taylor series expansion, the phase shift can be expressed as:
51
9(k)
=
0(ko)+
(k) (kO -k)+
ak
I0(
182(k)
aa(2 k (k0-k)2)2 +...+- 1 a"o(k k (k,-k)",
2 Ok
n! ak )
(3.1)
where ko is the wavenumber corresponding to the center wavelength. The third term in
the equation represents group-velocity dispersion, which is largely responsible for
dispersion mismatch. Higher-order dispersion is represented by the higher-order terms.
Multiplying the spectral fringes by a nonlinear phase distorts the depth profile in the
Fourier domain, resulting in a loss of axial resolution.
Therefore, to correct for the
chromatic mismatch, the spectral fringe pattern was multiplied with the inverse phase
shift e~'O(k) [39], upon completing interpolation and prior to Fourier Transform.
Like the tuning curve of the laser, the amount of dispersion mismatch is an unknown
factor. In the case of a single-reflector sample, the phase shift can also be estimated in an
iterative manner, searching for parameters that optimize the resolution and symmetry of
the computed reflectivity profile.
However, in the case of retinal imaging, isolated
reflections are often unavailable, so the sharpness of the image has to be evaluated
instead. For this thesis, the procedure was carried out manually, once for each subject,
with the image sharpness assessed by the operator. A more objective assessment would
require a sharpness metric function [40], which could be used in an automated algorithm.
It should be noted that this numerical dispersion compensation procedure was done after
data acquisition and did not interfere with the imaging session.
3.3.5 Image Construction
The last major step of signal processing is visualization of the OFDI data. The 3D data
set is sometimes visualized with volume rendering using commercially-available
software, but this has not gained wide acceptance. Retinal specialists are used to 2D
histological sections and fundus images, so 3D-rendered visualization is difficult for them
to interpret. Instead, the 3D OFDI data set is usually visualized as a movie sequence of
2D cross-sectional reflectivity plots.
These cross-sectional images can be shown
realistically in a 1:1 scale, but often they are expanded vertically to reveal the
microanatomy of the layered structures. The choice of mapping used to represent data
52
values can have a profound effect on the appearance and interpretability of the images.
Typically, the images display the logarithm of reflectivity in units of decibels (dB),
because the dynamic range of OCT images approaches 50 dB.
Humans can sense
brightness variation of only 3-4 decades and in practice monitors and printers place even
more stringent limitations. Puliafito et al advocated for false color mapping [77], but
false colors may produce image artifacts and lead to incorrect interpretation of physical
structures. With standard grayscale mapping, strong reflections appear white on a black
background. The inverse grayscale, with black structures on a white background, was
primarily motivated by its relative ease in printing and photocopying. As will become
obvious in the next chapter, the two scales lead to significant differences in image
perception, as a result of the nonlinear response of human visual systems.
The dimensions of OCT images, especially in retinal imaging, are computed rather than
directly measured. The transverse dimensions are calculated from the angular deviations
of the scanning mirrors using geometric optics. In the axial dimension, the image depth
range can be calculated by Equation (1.17). The axial scale can also be experimentally
determined by moving a reflector in the sample arm and dividing the distance of
translation in air by that in the image. Both methods require a further division by the
refractive index of tissue to yield correct intraocular distances. Since the local refractive
index usually does not vary over more than a few percent, the error induced by assuming
a constant index over the entire retina is negligible [78]. The value of the index used for
this thesis was 1.38, based on previous studies in the 800-nm region [15, 16], since the
index was not expected to differ much at 1050 nm. Although the refractive index value
might not be highly accurate, OCT enjoys a high degree of repeatability in thickness
measurements, which is the primary consideration for clinical diagnostics. Koozekanani
et al [79] conducted a clinical study with a commercial time-domain system (Humphrey
Instruments) to image twenty-six volunteers (15 images over 3 sessions for each person).
The average retinal thickness was found to be 274 ± 17 ptm for a 1-mm long region 0.75
mm from the fovea.
They obtained a 99% confidence interval that individual scan
averages of the retinal thickness would be within 11.2 pm of the true subject value, and
53
that sessional averages would be within 7.0 pm. These results of high repeatability were
comparable with those of Hee et al [80] and Baumann et al [81].
Image processing was applied extensively in the past for motion correction. Natural and
saccadic patient motion was fast compared to the image acquisition time of the slow TDOCT systems, degrading image resolution and inducing artifacts. The advent of highspeed OFDI technology has in large part alleviated this concern. Even without using any
motion-correction algorithm, the cross-sectional images in this thesis do not exhibit
motion artifacts, although movie sequences do show a slow drift of the eye. The only
image processing tool employed was a median filter for smoothing images and mitigating
speckle noise.
3.4 Results
Now that the theory, practical issues, and optimization tools have been discussed, this
section will describe the characterization of the 1050-nm OFDI system. The test sample
was a partial reflector (-73 dB) that comprised a neutral-density attenuator and a goldcoated mirror. The sensitivity of the system was the measured SNR value of the sample
plus 73 dB.
The operating parameters of the system were first optimized to maximize sensitivity. The
performance of dual-balanced detection was originally suboptimal due to the imperfect
symmetry of the balanced detector and fiber coupling at the two ports. By loosening the
fiber at one port, one could carefully fine-tune the balanced detection. Now consider a
sample at a fixed depth. By measuring the SNR of the sample as a function of the
reference arm power, the optimal reference arm power for maximum sensitivity was
determined to be 2.6 p.W at each detection port of the dual-balanced detector. Figure 3-7
illustrates the relationship between signal and noise. Note that these measurements were
obtained for a previous setup that had a slightly lower optimal power. At high power,
RIN noise dominated; at low power, signal dropped off faster than noise. Sensitivity was
maximized when the shot noise equaled the RIN noise at the optimal power of 2.6 p.W.
54
The relatively low value is attributed to the relatively large intensity noise of the laser
that cannot not be completely suppressed in balanced detection. The system was further
improved by adjusting the polarization controller to align the polarization states of the
two arms, while monitoring the SNR with the LabVIEW interface.
a)
30
20 -
z
&0 100
10 -2
10,
100
10~1
Reference Arm Power (pW)
10 110
2
b)
4030
C,
Signal
Noise
20
100-10
10.
102
10~
100
10
102
Reference Arm Power (pW)
Figure 3-7. (a) Measured SNR of a sample reflector as a function of reference arm
power. (b) Signal and noise power as a function of reference arm power.
The system's tuning curve and dispersion mismatch were determined next. As explained
previously, both nonlinear tuning and dispersion mismatch give rise to peak broadening.
If the partial reflector's reflectivity profile were used for estimating the tuning curve's
polynomial expansion, it would yield an incorrect value by including the effect of
dispersion mismatch. Instead, the sample arm was blocked and a 1 -mm-thick glass slide
was inserted in the reference arm. The air-glass interface reflection generated a delayed
version of the reference beam (Figure 3-8).
In this experiment's configuration of a
transmission-type reference arm and reflection-type sample arm, the delayed reference
beam's beating with the original reference beam appeared as a sample reflection at a
depth equivalent to the optical thickness of the slide (~1.3 mm). Unlike a real reflection
55
...
. .....
.
from the sample arm, this signal did not experience the dispersion mismatch of the two
arms, except for negligible dispersion in the glass slide. Therefore, the use of the glass
slide led to a more accurate estimate of the tuning curve. In this case, balanced detectin
was not used, as balanced detection would have substantially reduced the selfinterference signal from the reference arm.
Figure 3-8. Glass slide in the reference arm and its
self-interference for laser tuning calibration.
Peak broadening that results from nonlinear tuning is strongly dependent on the depth of
the sample, while broadening from dispersion is depth-independent. In order to verify
this, the resolution (width) of the reflectivity profiles of the partial reflector at different
depths was measured by moving the reference mirror. In the case where the resolution
versus depth curve was not flat after interpolation, the polynomial coefficients of the
tuning curve were adjusted accordingly. The reflectivity profile of the partial reflector,
after correction for interpolation, was then used to estimate dispersion mismatch. Given
a flat resolution versus depth curve after interpolation, the curve should remain flat after
dispersion compensation.
Figure 3-9 illustrates the tremendous improvement to the
reflectivity profile of the partial reflector after interpolation and dispersion compensation.
The theoretical curve was obtained from a numerical simulation based on the source
spectrum (Figure 2-3a) and the Gaussian window function. Before applying the Gaussian
window, random noise was added to a perfect sinusoid to match the curve to the system's
theoretical sensitivity. Figure 3-10 highlights the system's resolution performance. The
measured values of axial resolution were 14 - 16 gm in air, slightly increasing with the
depth, while the theoretical value was computed to be 13 pm from the curve in Figure
3-5(b).
Errors in interpolation and dispersion compensation due to higher order terms
probably account for the discrepancy.
56
IIII
I
II
-70
Original
-
- - - After Interpolation
After Dispersion Compensation
- Theoretical
\
-80
a -85
0
0~
Ij
-90
0
-95
-100
I
it
-105
1.45
1.4
1.35
1.5
Depth (mm)
1.6
1.55
1.65
Figure 3-9. Tremendous improvement to the reflectivity profile of the partial reflector
after interpolation and dispersion compensation. The theoretical curve was obtained from
a numerical simulation with a perfect sinusoid plus random noise.
30
28262422-
---- After Interpolation
& After Dispersion Compensation
- --. Theoretical
.2 200
18
16141210
-2.5
I
-2
-1.5
-1
-0.5
.5
0
Depth (mm)
1
1.5
2
2.5
Figure 3-10. System performance in resolution across the entire depth range.
57
..................
Figure 3-11 depicts the point spread functions measured at various depths.
The
maximum SNR was 25 dB, corresponding to a maximum sensitivity of 98 dB.
The
theoretical shot-noise limit of sensitivity, after accounting for Gaussian windowing, was
calculated to be 106 dB; the 8-dB deficiency in sensitivity of our system seems
reasonable, considering that the residual laser intensity noise and imperfect polarization
alignment between the sample and reference light, among many other practical details,
contributed to SNR loss. In addition, due to absorption by water in the eye, the actual
SNR for the human retina would be 3 - 4 dB lower than the values measured with the
mirror sample.
3025-
a 20-
10-
5
-
0
-2.5
-2
-1.5
-1
-0.5
0
0.5
Depth (mm)
1
1.5
2
2.5
Figure 3-11. Point spread functions measured at various depths for a sample reflectivity of -73 dB.
As indicated in Figure 3-11, sensitivity decreased from 98 dB to 92 dB as the path length
increased to a depth of 2.4 mm, due to the finite coherence length of the laser output.
Compared to the previous time-domain system using a broadband source at 1040 nm (50nm bandwidth and 10-pm resolution in air) [58], the OFDI system offers a higher
sensitivity at a 100-fold faster image acquisition speed and using only one sixth of sample
arm power. The high sensitivity and depth range of the OFDI system compare favorably
58
with those of state-of-the-art spectral-domain systems using broadband sources in the 700
- 900 nm spectral range [39, 40].
The above system characterization was performed averaging over 500 A-lines at constant
depth. This way random noises were removed and only systematic noises remained. The
reflectivity profiles were averaged after undergoing all prior processing steps
individually. The noise floor in sensitivity analysis, obtained from reference images,
exhibited variations of -5 dB across the depth range due to the frequency response of the
electronic low-pass filter. Hence, Figure 3-11 was produced from the original plot of
point spread functions (Figure 3-12) after subtraction of the noise floor.
I
I N sI IFI
-.. Noise Floor
30-
-
25
20@1
0
*1
15
ci) 10
5
0
-2.5
-2
-1.5
-1
-0.5
0
.5
1
1.5
2
2.5
Depth (mm)
Figure 3-12. Original plot of point spread functions before noise floor subtraction.
59
... on science (and life) ...
"Genius? Nothing ... Sticking to it is genius. I've failed my wiay to success.
-- Thomas Edison
60
Chapter 4: In Vivo Imaging of Human Retina and Choroid
4.1 Introduction
The compelling advantages of optical frequency domain imaging (OFDI) have already
been shown for imaging skin, coronary artery, esophagus, and anterior eye segments [41,
45, 56, 82-85].
Until now, however, a clinically-viable OFDI system for imaging
posterior eye segments has been unavailable. This chapter presents the results obtained
with the OFDI system developed for this thesis. The first OFDI imaging of posterior
segments of the human eye in vivo with high image acquisition speed, sensitivity, and
penetration depth was demonstrated.
The system's deep penetration power into the
choroid was confirmed by a comparison to a state-of-the-art spectral-domain system.
4.2 OFDI Imaging
OFDI imaging was conducted with two healthy volunteers (A: 36-year-old Asian male,
B: 41-year-old Caucasian male).
With real-time feedback (images) on the LabVIEW
interface, the operator focused light through the human interface onto the retina of each
subject and selected the region of interest. The OFDI system acquired 200,000 A-lines
over 10.6 seconds in each imaging session as the focused sample beam was scanned over
an area of 6 mm (horizontal) by 5.2 mm (vertical) across the macular region. The movie
sequence of images recorded from volunteer A at a frame rate of 18.8 Hz was published
[86] and can be viewed online (http://www.opticsinfobase.org/abstract.cfm?URI=oe-1410-4403). One-hundred-twenty of a total of two-hundred image frames are shown in the
movie.
Each frame was constructed from a thousand A-line scans with an inverse
logarithmic grayscale table mapping to the reflectivity range.
Figure 4-1(a) is a
representative image frame from the movie. The OFDI image allows clear visualization
of the anatomical layers in the retina and provides deep penetration into the choroid up to
the interface with the sclera.
61
a)
2oownL.
Figure 4-1. (a) Representative OFDI image frame from a movie sequence of a healthy volunteer
(movie downloadable from http://www.opticsinfobase.org/abstract.cfm?URI=oe-14-10-4403).
The image allows clear visualization of the anatomical layers in the retina and provides deep
penetration into the choroid up to the interface with the sclera. Each image frame consists of 1000
axial lines, spans over 6.0 mm (horizontal) and 1.8 mm (depth) in tissue, and was produced with
inverse logarithmic grayscale mapping. (b) Same image produced with standard logarithmic
grayscale mapping.
As mentioned previously, the choice of mapping in creating images can have a significant
impact on the viewer's perception. Figure 4-1(b) uses the same data as in Figure 4-1(a)
but applies a standard grayscale. A typical viewer can observe in Figure 4-1(a) more
details of high-reflectivity areas (e.g. capillaries and pigment cells appearing as black
spots in the choriocapillary layer just beneath the RPE); however in Figure 4-1(b), the
low-reflectivity areas (e.g. choroidal vessels appearing as dark ellipsoid regions) are more
noticeable to the eye.
In addition, the mapping range corresponds directly to the
reflectivity dynamic range displayed in the image and thus determines the image contrast.
In this thesis, the mapping range was chosen to match the dynamic range of the detected
signals (-47 dB).
62
Figure 4-2(A) in the next page depicts a vertically-expanded image of the macular region.
The layered structure of the retina visualized in the OFDI image correlates well with
previously published OCT images and histological findings [14, 39, 40, 58]. The center
of the fovea appears as a highly-reflective spot in the center of the image, at the top of the
retina. The thick dark band at the top left and right of the image is the retinal nerve fiber
layer (RNFL), which becomes thinner closer to the fovea. The layer below the RNFL is
the inner plexiform layer (IPL) that grows very thick near the fovea. The two white
bands underneath the IPL are the inner and outer nuclear layers (INL and ONL),
respectively, sandwiching a darker band called the outer plexiform layer (OPL). Further
down, the dark line that rises directly below the center of the fovea is the interface
between the inner and outer segments of the photoreceptor layer (IPRL). The bottom
layer is the retinal pigment epithelium (RPE). Finally, the choroid (C) lies below the
RPE.
4.3 Comparison to an 840-nm SD-OCT System
To assess the penetration power of the OFDI system, three-dimensional imaging was
performed on the two volunteers A and B with both the OFDI system and a state-of-theart SD-OCT system previously developed for video-rate retinal imaging [35]. The SD
system employed a superluminescent diode with a center wavelength of 840 nm and a 3dB spectral bandwidth of 50 nm, offering an axial resolution of 8 - 9 pm in air. At an Aline rate of 29 kHz and a sample arm power level of 600 p.W, the SD system offered a
peak sensitivity of 98 dB at zero delay that decreased to 82 dB at the maximum ranging
depth of 2.4 mm in air. In comparison, the OFDI system offered resolution of 14 - 16 pm
and sensitivity of 89 - 95 dB over a similar depth range, after accounting for the
additional water absorption at 1050 nm.
Figure 4-2 represents side-by-side comparison of OFDI and SD-OCT images near the
fovea and optic disc. Figures Al - A4 were obtained from a 36-year-old Asian male, and
Figures B 1 - B2 were from a 41-year-old Caucasian male. Evidently, the OFDI images
exhibit considerably deeper penetration into the choroid compared to the SD-OCT
63
In particular, penetration into the choroid is generally much shorter in the
images.
macular region than near the optic disc due to the macula's high melanin content [87], a
phenomenon observed in the SD-OCT image (Figure A3). In contrast, the OFDI image
(Figure Al) shows deep penetration across the entire retina. On the other hand, the
higher axial resolution in the SD-OCT images provides better contrast between retinal
layers. The apparently superior penetration of the OFDI system to the SD system is
attributed to the lower absorption and scattering in RPE at 1050 nm than 840 nm [58] as
well as the higher sensitivity of OFDI at large depth. However, verifying this hypothesis
would require detailed analysis involving more human subjects and imaging systems.
B1
B2
Figure 4-2. Comparison of two imaging systems (OFDI at 1050 nm and SD-OCT at 840 nm). Al and
A2: OFDI images at fovea and optic nerve head, respectively, from volunteer A, 36-year-old Asian
male. A3 and A4: SD-OCT images from the same volunteer at similar tissue locations. B1 and B2:
OFDI and SD-OCT images, respectively, obtained from volunteer B, 41-year-old Caucasian male.
OFDI images exhibit considerably deeper penetration in tissue than SD-OCT images in all the data
sets. The OFDI image (Al) shows the anatomical layered structure: RNFL; retinal nerve fiber layer,
IPL; inner plexiform layer, INL; inner nuclear layer, OPL; outer plexiform layer, ONL; outer nuclear
layer, IPRL; interface between the inner and outer segments of the photoreceptor layer, RPE; retinal
pigmented epithelium, and C; choriocapillaris and choroid.
64
65
...
on grad school ...
"A gradstudent in procrastinationtend to stay in procrastination
unless an externalforce is applied to it.
-- phdcomics.com
66
Chapter 5: Visualizing Retinal and Choroidal Vasculature
5.1 Introduction
A primary obstacle to the widespread acceptance of OCT is the difficulty for an
ophthalmologist to follow and interpret video-rate OCT movie sequences of crosssectional images. Ophthalmologists are familiar with transverse fundus images and have
access to large fundus image databases for various diseases. Precise spatial registration
of OCT structures to fundus landmarks can capitalize on this knowledge to facilitate the
analysis of OCT data. For instance, a fundus image can be shown as a still picture beside
an OCT movie, with a line across the fundus image indicating the transverse position of
the OCT cross-sectional scan along the retinal surface [88, 89]. This technique helps
emphasize the relation between the fundus image and the underlying 3D OCT data set.
The problem of spatial registration has been tackled in different ways. A basic approach
is to separately acquire OCT and fundus images, and perform image registration using
prominent features of the fundus image such as the retinal vasculature and the optic disc.
Precision with this approach is unsatisfactory due to its inherent differences in image
acquisition in terms of time and retina orientation. Another method is to combine OCT
with the capability of a scanning laser ophthalmoscope (SLO). A TD-OCT system was
demonstrated that acquired images transversely, one depth at a time [90]. This system
split reflected sample light into two detection channels to produce transverse OCT and
fundus images simultaneously.
The system's pixel-to-pixel correspondence enabled
precise spatial registration, but required a complicated setup and suffered sensitivity loss
due to the splitting of reflected light. A simpler method is to employ a transverse-mode
OCT system and construct a fundus-type image by numerical integration of transverse
images along the depth axis [91]. Recently, Jiao et al [88] developed a technique with
SD-OCT to acquire fundus-type images. Since the fundus-type image was constructed
from the same raw spectra used to generate OCT data, the problem of spatial registration
was solved, and both fundus-type and cross-sectional OCT images could be displayed in
67
real time. Mujat et al [89] demonstrated similar fundus-type images with SD-OCT by
integrating cross-sectional images along the depth profile, which is equivalent to Jiao's
method by Parseval's Theorem. Their comparisons to images from SLO [88, 89] and
fluorescein angiography [89] indicated that these fundus-type images could be used as a
reliable representation of the retinal vasculature.
Jiao et al [88] also showed that image contrast of fundus-type images could be further
enhanced by integrating only selective regions in cross-sectional images, based on
anatomical structures. In this thesis, this technique has been extended to produce depthsectioned fundus images.
For the first time, the choroidal vasculature was clearly
visualized in a noninvasive manner.
5.2 Automatic Depth-Sectioning Algorithm
The study of image segmentation, or partitioning of an image into selective regions, has a
long history in the fields of computer vision and image processing.
With OCT,
segmentation algorithms have been applied to retinal imaging for estimating thicknesses
of various retinal layers [92, 93].
For this thesis, an automatic algorithm similar to
Mujat's method [89] was developed. Utilizing MATLAB's image processing tools [94],
the algorithm can segment retinal layers by boundary detection in cross-sectional frames
and construct depth-sectioned fundus-type images from an OCT movie sequence. The
algorithm was applied to areas away from the optic disc, because the optic disc is difficult
to track and does not provide relevant depth-resolved information of the vasculature.
The algorithm operates as follows:
Image Segmentation:
1. Convert a cross-sectional frame (Figure 5-la) into a binary frame of edges
(Figure 5-1b) with the MA TLAB function edge. This function performs edge
detection by gradient calculation and binary conversion with a threshold value. In
a typical retinal image, the top boundary of the retinal nerve fiber layer (RNFL)
68
and the interface between the inner and outer segments of the photoreceptor layer
(IPRL) appear as two prominent boundaries and serve as a good starting point for
segmentation.
The two boundaries often contain holes due to image noise or
shadow of structures above (e.g. retinal vessels). On the other hand, additional
edges may appear elsewhere.
The threshold in the edge function represents a
tradeoff between holes and additional edges.
2. Remove holes and additional edges (Figure 5-1c) by performing morphological
operations on binary images with MATLAB functions bwmorph('bridge') and
bwareaopen.
The bwmorph('bridge') function removes holes by bridging
continuous boundaries with short broken sections. Then the bwareaopen function
eliminates additional edges by removing short isolated sections.
3. Trace the IPRL by tracking its detected boundary across the image one pixel at
a time. Even after Steps 1 - 2, holes and additional edges are often still present.
They are identified with sharp discontinuities in the boundary, since the IRPL is
slowly-varying in depth. When a hole or an additional edge is detected, the
tracking algorithm corrects for it by referring back to the previous value in the
traced boundary or the value from the last traced frame at the same transverse
location.
4. Smooth the traced boundary with the MATLAB function sgolayfilt.
The
presence of holes and additional edges can sometimes distort some part of the
traced boundary.
The Savitzky-Golay smoothing filter [94, 95] can minimize
such distortion effect with its generalized moving average algorithm.
Selective Integration:
5. Draw a parallel line to the traced IPRL to mark the RPE (Figure 5-1d).
Because the curvatures of retinal layers below the IPRL are similar across the
region of interest, the RPE can be approximated by a parallel line to the IPRL.
The boundaries used for integration in the choroid region are also created this
way.
69
6. Integrate pixel values along the depth in the region defined by the two
boundaries (Figure 5-1d). This projects the 2D region into a ID data set (Figure
5-le) for each frame. The integration is performed in the logarithmic scale to
yield a smoother fundus-type image [89].
Fundus-Type Image Production:
7. Repeat steps 1 - 6for all frames in the movie sequence to produce afundus-type
image (Figure 5-1e). The 1D data set from each frame is displayed as a line in
the 2D fundus-type image of the retinal vasculature. The red line corresponds to
the result of integration (Figure 5-1d) in the selected region shown in Figure 5-1c.
The ditch in Figure 5-1d indeed shows up as a dark segment (vessel) in the
fundus-type image.
8. Correct for motion artifact by correlation.
Discontinuities in the retinal
vasculature, resulting from eye movements between frames, can be readily
observed in the fundus-type image (Figure 5-le).
The prominent retinal
vasculature lends itself to an automatic image realignment procedure.
Each
transverse line of the fundus-type image is compared to the next, and the offset (if
any) can be found from correlation. It should be noted that the offset information
can potentially be used to realign the cross-sectional movie sequence.
The
corrected image (Figure 5-1f) is slightly narrower than Figure 5-le, because
transverse realignment results in the need for removal of part of the image. The
visible intensity gradient in the vertical direction in Figure 5-le has also been
corrected.
9. The depth-sectioned fundus image has been produced (Figure 5-1f).
70
b)
a)
f
d)
C)
-
',~
-~
IPRL
RPE
---
Integrated Signal
Figure 5-1. Automatic depth-sectioning algorithm. (a) Original cross-sectional image frame.
(b) Binary frame of edges (step 1). (c) Binary frame after removal of holes and additional edges (step
2). (d) Original cross-sectional image frame with traced boundaries of IPRL and RPE (steps 3 - 5).
The integrated signal from the selected integration region is also shown (step 6). (e) Resultant fundustype image from repeating steps 1 - 6 for all frames in the movie sequence (step 7). (f) Final fundustype image after correction for motion artifact (step 8). The corrected image is slightly narrower,
because transverse realignment results in the need for removal of part of the image.
71
5.3 Fundus-Type Images
Given three-dimensional tomographic data of the eye's posterior segment, integrating the
pixel values along the entire depth axis readily produces a two-dimensional fundus-type
reflectivity image [88, 89]. Figure 5-2(A) depicts a fundus-type image generated from
the entire OFDI image sequence for volunteer A. The image visualizes the optic nerve
head, fovea, retinal vessels, and the faint outline of the deep choroidal vasculature;
however, the depth information is completely lost. To overcome this limitation of the
conventional method, one can integrate only selective regions based on anatomical
structures.
Seltivo
integradon
_E
Figure 5-2. The retinal and choroidal vasculature extracted from the three-dimensional OFDI data
set of volunteer A. (A) Two-dimensional reflectivity image (5.3 x 5.2 mm 2 ) obtained with the
conventional full-range integration method. Higher (lower) reflectivity is represented by white
(black) in the grayscale. (B) Illustration of the depth-sectioning integration method, with the
different integration regions labeled C, D, E corresponding to the following fundus-type
reflectivity images, respectively: (C) retinal reflectivity image showing the shadow of retinal
vasculature (3.8 x 5.2 mm 2 ), (D) reflectivity image obtained from the upper part of the choroid,
and (E) reflectivity image from the center of the choroid revealing the choroidal vasculature.
Shadows of retinal vasculature are also visible in D and E. Scale bars: 0.5 mm.
72
For example, to visualize the retinal vasculature selectively with improved contrast, the
aforementioned automatic algorithm was applied to integrate reflectivity in a selected
region. A retinal blood vessel produces a large reflection by strong scattering and casts a
shadow in the layers below. Integrating over the entire retina including vessels and their
shadows often results in a lower contrast in the vasculature. Therefore, integration was
performed in the region between IPRL and RPE (marked by red lines and labeled C in
Figure 5-2B), where the shadows created by the retinal vessels above appear most
distinctly [88].
Figure 5-2(C) depicts the fundus-type image (shadow) of the retinal
vessels produced with this method.
In this thesis, this method has been extended to produce depth-sectioned fundus-type
images of the choriocapillary layer and the choroidal vasculature. The choriocapillary
layer contains abundant small blood vessels and pigment cells [62, 96]. It is visualized
(Figure 5-2D) using a thin integration region in the upper part of choroid (labeled D in
Figure 5-2B). To obtain a fundus-type image of the complete choroid region, the bottom
integration region (marked by blue lines and labeled E in Figure 5-2B) was used. In
contrast to retinal vessels, choroidal vessels appear as low-signal (white in inverse
grayscale) regions compared to their surroundings in the cross-sectional image. The
reason for this phenomenon has not been completely understood yet. In the resulting
fundus-type image, the choroidal vasculature (dark from integrating over low-signal
regions) is clearly visualized (Figure 5-2E). Fundus-type images with similar qualities
were obtained for volunteer B.
During the last decade, an increasing number of retinal specialists have adopted
indocyanine green (ICG) angiography [4] to visualize the choroidal vasculature for
disease diagnosis. It is because fundus cameras [2] and scanning laser ophthalmoscopes
(SLOs) [6] do not have access to the choroid otherwise, except for subjects with a low
level of pigmentation.
The above in vivo fundus-type image of human choroidal
vasculature (Figure 5-2E) was created from the three-dimensional data set acquired by
the 1050-nm OFDI system. In Figure 5-3, the choroid image (with selective integration),
along with the image produced from the entire 3D data set (without selective integration),
73
is compared to a fundus image of the same eye obtained with a state-of-the-art
commercial SLO (Heidelberg Engineering - HRA 2; laser wavelength = 820 nm;
resolution ~ 5 pm; power = 46 p.W; speed = 5 Hz). This shows that the OFDI fundustype images are reliable representation of the retinal vasculature.
Furthermore, the
choroidal vasculature, which is not visible in the SLO image, is clearly visualized with
the OFDI depth-sectioning method. The method does not require dilation or intravenous
injection of fluorescent dyes. The entire imaging session took only approximately 10
seconds, while ICG imaging usually required up to 30 minutes, excluding the time for
dilation and angiography.
In addition to offering clinical convenience, the new non-
invasive method would enable clinicians to image the choroidal vasculature of a larger
patient population, some of whom might be allergic to dyes.
The high-speed OFDI
machine, now capable of high-resolution cross-sectional imaging as well as fundus
imaging of retinal and choroidal vasculature, makes an ideal candidate for a one-stop
clinical system for a wide range of ophthalmic applications.
OFDI
SLO
Figure 5-3. A comparison of OFDI fundus-type images (A,B) to a SLO image (C).
Figure A is a reliable representation of the retinal vasculature and Figure B clearly
visualizes the choroidal vasculature, which is not visible in the SLO image. Figures
A and B are Figure 5-2A and Figure 5-2E rescaled to match Figure C.
74
75
... on life after grad school
"WIELL ... we'll see."
--
76
Edward Chin Wang Lee
Chapter 6: Summary and Discussion
This thesis introduces a new ophthalmic technology that allows for comprehensive
imaging of human retina, optic disc, and choroid in vivo. The technology's ability to
produce high-resolution cross-sectional images and visualize retinal and choroidal
vasculatures without angiography has been demonstrated. This final chapter presents a
summary of the thesis and a discussion about the technology's future.
6.1 Summary
From the first retinal photograph with the ophthalmoscope to the invention of the
scanning laser ophthalmoscope (SLO), the field of retinal imaging has seen many
exciting advances. Analogous to ultrasound in operation but based on interferometry for
signal detection, optical coherence tomography (OCT) has emerged as a practical
noninvasive technology that can produce a highly-accurate structural representation of
the human retina in vivo with its high-resolution cross-sectional imaging.
Optical frequency domain imaging (OFDI) is a second-generation method for OCT. It
employs a wavelength-swept laser source to encode depth information into characteristic
frequencies in the detected signal. Like spectral-domain (SD) OCT, OFDI has made
significant improvements in imaging speed and sensitivity. Furthermore, OFDI offers
additional benefits such as a long usable ranging depth and reduced sensitivity to motioninduced signal fading. However, while retinal imaging has been demonstrated for SDOCT with affordable spectrometers in the 800-nm region, this application has been out of
reach for OFDI to date, due to the high water absorption in the 1300-nm region and the
lack of a wide-tuning rapidly-swept light source in a low water-absorption window.
Since the 1-pm region was shown to be a viable alternative window for retinal imaging
and could even potentially offer deeper penetration into the choroid, the recent
introduction of a commercial semiconductor optical amplifier in the 1 -pm region has
opened a window of opportunities for OFDI.
77
Chapter 2 describes in detail the novel wavelength-swept laser developed for this thesis.
The laser adopted a linear-cavity configuration and comprised a custom-built polygonbased intracavity scanning filter. With its output spectrum spanning 62 nm, the laser
delivered 2.7 mW of average power at a sweep rate of 18.8 kHz. Chapter 3 explains the
design and operation of the OFDI system constructed with this light source.
The
resultant system, with a sample arm power of 550 pW, achieved resolution of 10 pm in
tissue and a peak sensitivity of 98 dB that dropped to 92 dB at the maximum depth of 2.4
mm. Compared to the previous time-domain system using a broadband source at 1040
nm [58], this OFDI system offers a higher sensitivity at a 100-fold faster image
acquisition speed and using only one sixth of sample arm power.
In Chapter 4, comprehensive in vivo imaging of human retina and choroid was
demonstrated for two healthy volunteers. The movie sequence of images was recorded at
a frame rate of 18.8 Hz for 10.6 seconds, with a thousand A-lines in each frame and a
reflectivity dynamic range of 47 dB. The important steps in data processing included
background subtraction, windowing, interpolation into linear k-space, and dispersion
mismatch compensation. The resultant images clearly visualize the anatomical layers in
the retina and correlate well with previously-published OCT images and histological
findings. For the first time, posterior eye segment imaging has been realized with OFDI.
Also for the first time, video-rate imaging has been demonstrated in the 1-pm region.
The OFDI system further provides deeper choroid penetration in comparison to a stateof-the-art SD-OCT system at 840 nm. The improved penetration may be clinically useful
for evaluating early stages of retinal pathologies, such as age-related macular
degeneration, that are accompanied by choroidal neovascularization.
The production of fundus-type images was examined next in Chapter 5. Previous studies
showed that fundus-type images could be produced from a 3D OCT data set by
integrating along the depth. These fundus-type images are helpful to retinal specialists,
who can use them for precise spatial registration of OCT structures. It had also been
shown that the prominent retinal vasculature in a fundus-type image could be enhanced in
contrast by integrating only selective regions. This thesis has extended the technique to
78
produce depth-sectioned fundus-type images, with an automatic algorithm that was
developed for selective integration based on anatomical structures. In combination with
the system's enhanced penetration, the choroidal vasculature was, for the first time,
clearly visualized in a noninvasive manner. This approach does not employ angiography
and thus eliminates angiography's associated disadvantages such as a long measuring
time, required dilation, and possible allergic consequences.
6.2 Discussion
The unique characteristics of the 1050-nm OFDI system present challenges as well as
opportunities in the future. Increasing the saturation power of the semiconductor optical
amplifier (SOA) in the source and decreasing its relative intensity noise can drive the
system sensitivity higher. Similarly, increasing the bandwidth of the SOA can result in
higher resolution. However, in the 1-pm region, the increased water absorption away
from the local minimum presents an obstacle to be overcome.
Even in ultrahigh-
resolution SD-OCT in the 800-nm window, the effective bandwidth in the eye can be
limited due to increased absorption above 920 nm in the vitreous [39]. Yet in a positive
light, with this thesis' demonstration of high-speed, high-sensitivity imaging in the 1050nm window and Lim et al's development of another high-speed swept source in the 800nm window [97], it is now possible to conceive a system that has a bandwidth spanning
from the 800-nm window to the 1050-nm window. In such a Fourier-domain system
(OFDI or SD-OCT), the time-domain fringes would be enveloped by the product of the
source spectral shape and the water absorption spectral profile. Even though the fringes
corresponding to the high-absorption region between the two windows would be smaller
and noisier, the fringes could be normalized before Fourier Transform.
The overall
achievable resolution would still be higher than even that of the current ultrahighresolution systems. Nevertheless, all of this is contingent on technological advances in
commercial SOAs. In the immediate future, source development would be the deciding
factor between operation at 1050 nm (deep penetration and demonstrated high-quality
images) and 800 nm (proven wavelength for clinical ophthalmic applications).
79
The powerful features of OFDI have profound implications for applications in posterior
segment imaging.
For example, the system can be readily adapted for polarization
diversity and polarization-sensitive measurements. Polarization-sensitive measurements
can quantify loss of retinal birefringence for early detection of glaucoma, but require two
detection channels for the two different polarization states [21]. Thus, OFDI's use of
simple photodetectors is appealing compared to SD-OCT's spectrometers. Besides this,
OFDI's capability for phase-resolved measurements can enable the imaging of blood
flow dynamics. Its reduced susceptibility to motion-induced fringe washout also allows
measurements of flow rates much higher than possible with SD-OCT [19].
One can
expect that a future phase-resolved OFDI system at 1050 nm can enhance the contrast of
retinal and choroidal vessels in both cross-sectional images and fundus-type images.
Furthermore, while fundus-type images cannot show a dye's filling of or leakage from
vessels as in angiography, a phase-resolved system can produce depth-sectioned fundustype images that illustrate the retinal blood flow dynamics.
With several thousand units of commercial TD-OCT systems in operation, the OFDI
system developed for this thesis offers a glimpse into the future of second-generation
OCT systems that might reside in the majority of ophthalmic clinics worldwide. The
1050-nm OFDI machine, with its high peak sensitivity and slow dropoff in addition to a
deep penetration power, could potentially become the de facto platform for routine eye
examinations.
Compared to the system's current level of retinal exposure, the ANSI
maximum permissible exposure allows for an increase by a factor of three, which would
translate to a three-fold speed improvement at the same high sensitivity. This means that
a complete three-dimensional data set of a patient's retina that includes information on
retinal and choroidal vasculature could be obtained in 3 - 4 seconds without eye dilation
or angiography. OFDI's multifunctional capability such as Doppler blood flow imaging
and polarization-sensitive glaucoma diagnostics could further provide a universal
platform for diverse imaging applications.
With its demonstrated performance and
impressive potential, OFDI is a promising technology for comprehensive ophthalmic
examination.
80
References
[1]
C. Web, "The eye: information about vision loss and blindness," (2005),
http://www.99main.com/~charlief/Blindness.htm.
[2]
P. J. Saine, and M. E. Tyler, Ophthalmic Photography:Retinal Photography,Angiography, and
Electronic Imaging (Butterworth-Heinemann, Woburn, MA, 2002).
[3]
S. Wolf, F. Jung, H. Kiesewetter, N. Korber, and M. Reim, "Video Fluorescein Angiography Method and Clinical-Application," Graefes Archive for Clinical and Experimental Ophthalmology
227, 145-151 (1989).
[4]
J. J. Jorzik, A. Bindewald, S. Dithmar, and F. G. Holz, "Digital simultaneous fluorescein and
indocyanine green angiography, autofluorescence, and red-free imaging with a solid-state laserbased confocal scanning laser ophthalmoscope," Retina-the Journal of Retinal and Vitreous
Diseases 25, 405-416 (2005).
[5]
R. H. Webb, and G. W. Hughes, "Scanning Laser Ophthalmoscope," Ieee Transactions on
Biomedical Engineering 28, 488-492 (1981).
[6]
R. H. Webb, G. W. Hughes, and F. C. Delori, "Confocal Scanning Laser Ophthalmoscope,"
Applied Optics 26, 1492-1499 (1987).
[7]
T. Olsen, "The Accuracy of Ultrasonic Determination of Axial Length in Pseudophakic Eyes,"
Acta Ophthalmologica 67, 141-144 (1989).
[8]
C. J. Pavlin, K. Harasiewicz, M. D. Sherar, and E. S. Foster, "Clinical Use of Ultrasound
Biomicroscopy," Ophthalmology 98, 287-295 (1991).
[9]
D. F. Chang, General Ophthalmology (Appleton & Lange, Norwalk, Conn, 1992).
[10]
T. Seiler, and T. Bende, Noninvasive Diagnostic Techniques in Ophthalmology(Springer-Verlag
NY Inc, New York, NY, 1990).
[11]
D. Huang, E. A. Swanson, C. P. Lin, J. S. Schuman, W. G. Stinson, W. Chang, M. R. Hee, T.
Flotte, K. Gregory, C. A. Puliafito, and J. G. Fujimoto, "Optical Coherence Tomography," Science
254, 1178-1181 (1991).
[12]
A. F. Fercher, C. K. Hitzenberger, W. Drexler, G. Kamp, and H. Sattmann, "In-Vivo Optical
Coherence Tomography," American Journal of Ophthalmology 116, 113-115 (1993).
[13]
E. A. Swanson, J. A. Izatt, M. R. Hee, D. Huang, C. P. Lin, J. S. Schuman, C. A. Puliafito, and J.
G. Fujimoto, "In-Vivo Retinal Imaging by Optical Coherence Tomography," Optics Letters 18,
1864-1866 (1993).
[14]
Uniformed Services University of the Health Sciences, "HistoWeb," (2000),
http://bicmra.usuhs.mi/M RA/Histology/Eye/HTMLdocs/eye05.html.
[15]
S. Yazdanfar, A. M. Rollins, and J. A. Izatt, "Imaging and velocimetry of the human retinal
circulation with color Doppler optical coherence tomography," Optics Letters 25, 1448-1450
(2000).
81
[16]
J. F. de Boer, B. Cense, N. Nassif, B. R. White, B. H. Park, M. C. Pierce, G. J. Tearney, B. E.
Bouma, and T. C. Chen, "Ultra-high speed and ultra-high resolution optical coherence tomography
and optical Doppler tomography," Investigative Ophthalmology & Visual Science 46 (2005).
[17]
M. R. Hee, C. A. Puliafito, C. Wong, J. S. Duker, E. Reichel, B. Rutledge, J. S. Schuman, E. A.
Swanson, and J. G. Fujimoto, "Quantitative Assessment of Macular Edema with Optical
Coherence Tomography," Archives of Ophthalmology 113, 1019-1029 (1995).
[18]
J. S. Schuman, M. R. Hee, C. A. Puliafito, C. Wong, T. Pedutkloizman, C. P. Lin, E. Hertzmark, J.
A. Izatt, E. A. Swanson, and J. G. Fujimoto, "Quantification of Nerve-Fiber Layer Thickness in
Normal and Glaucomatous Eyes Using Optical Coherence Tomography - a Pilot-Study," Archives
of Ophthalmology 113, 586-596 (1995).
[19]
B. J. Vakoc, S. H. Yun, J. F. de Boer, G. J. Tearney, and B. E. Bouma, "Phase-resolved optical
frequency domain imaging," Optics Express 13, 5483-5493 (2005),
http://www.opticsexpress.org/abstract.cfm?id=84914.
[20]
D. J. Faber, E. G. Mik, M. C. G. Aalders, and T. G. van Leeuwen, "Light absorption of (oxy)hemoglobin assessed by spectroscopic optical coherence tomography," Optics Letters 28, 14361438 (2003).
[21]
B. Cense, H. C. Chen, B. H. Park, M. C. Pierce, and J. F. de Boer, "In vivo birefringence and
thickness measurements of the human retinal nerve fiber layer using polarization-sensitive optical
coherence tomography," Journal of Biomedical Optics 9, 121-125 (2004).
[22]
W. Drexler, U. Morgner, R. K. Ghanta, F. X. Kartner, J. S. Schuman, and J. G. Fujimoto,
"Ultrahigh-resolution ophthalmic optical coherence tomography," Nature Medicine 7, 502-507
(2001).
[23]
W. Goebel, and T. Kretzchmar-Gross, "Retinal thickness in diabetic retinopathy - A study using
optical coherence tomography (OCT)," Retina-the Journal of Retinal and Vitreous Diseases 22,
759-767 (2002).
[24]
M. R. Hee, C. R. Baumal, C. A. Puliafito, J. S. Duker, E. Reichel, J. R. Wilkins, J. G. Coker, J. S.
Schuman, E. A. Swanson, and J. G. Fujimoto, "Optical coherence tomography of age-related
macular degeneration and choroidal neovascularization," Ophthalmology 103, 1260-1270 (1996).
[25]
M. R. Hee, C. A. Puliafito, C. Wong, J. S. Duker, E. Reichel, J. S. Schuman, E. A. Swanson, and
J. G. Fujimoto, "Optical Coherence Tomography of Macular Holes," Ophthalmology 102, 748-756
(1995).
[26]
M. R. Hee, C. A. Puliafito, C. Wong, E. Reichel, J. S. Duker, J. S. Schuman, E. A. Swanson, and
J. G. Fujimoto, "Optical Coherence Tomography of Central Serous Chorioretinopathy," American
Journal of Ophthalmology 120, 65-74 (1995).
[27]
J. R. Wilkins, C. A. Puliafito, M. R. Hee, J. S. Duker, E. Reichel, J. G. Coker, J. S. Schuman, E.
A. Swanson, and J. G. Fujimoto, "Characterization of epiretinal membranes using optical
coherence tomography," Ophthalmology 103, 2142-2151 (1996).
[28]
B. K. Rutledge, C. A. Puliafito, J. S. Duker, M. R. Hee, and M. S. Cox, "Optical coherence
tomography of macular lesions associated with optic nerve head pits," Ophthalmology 103, 10471053 (1996).
[29]
B. E. Bouma, and G. J. Tearney, Handbook of Optical Coherence Tomography (Dekker, New
York, NY, 2001).
82
[30]
K. Takada, I. Yokohama, K. Chida, and J. Noda, "New Measurement System for Fault Location in
Optical Wave-Guide Devices Based on an Interferometric-Technique," Applied Optics 26, 16031606 (1987).
[31]
R. C. Youngquist, S. Carr, and D. E. N. Davies, "Optical Coherence-Domain Reflectometry - a
New Optical Evaluation Technique," Optics Letters 12, 158-160 (1987).
[32]
B. Hermann, E. J. Fernandez, A. Unterhuber, H. Sattmann, A. F. Fercher, W. Drexler, P. M.
Prieto, and P. Artal, "Adaptive-optics ultrahigh-resolution optical coherence tomography," Optics
Letters 29, 2142-2144 (2004).
[33]
A. F. Fercher, K. Mengedoht, and W. Werner, "Eye-Length Measurement by Interferometry with
Partially Coherent-Light," Optics Letters 13, 186-188 (1988).
[34]
D. Huang, J. P. Wang, C. P. Lin, C. A. Puliafito, and J. G. Fujimoto, "Micron-Resolution Ranging
of Cornea Anterior-Chamber by Optical Reflectometry," Lasers in Surgery and Medicine 11, 419425 (1991).
[35]
N. A. Nassif, B. Cense, B. H. Park, M. C. Pierce, S. H. Yun, B. E. Bouma, G. J. Tearney, T. C.
Chen, and J. F. de Boer, "In vivo high-resolution video-rate spectral-domain optical coherence
tomography of the human retina and optic nerve," Optics Express 12, 367-376 (2004),
http://www.opticsexpress.org/abstract.cfi?id=78765.
[36]
M. Wojtkowski, R. Leitgeb, A. Kowalczyk, T. Bajraszewski, and A. F. Fercher, "In vivo human
retinal imaging by Fourier domain optical coherence tomography," Journal of Biomedical Optics
7, 457-463 (2002).
[37]
M. A. Choma, M. V. Sarunic, C. H. Yang, and J. A. Izatt, "Sensitivity advantage of swept source
and Fourier domain optical coherence tomography," Optics Express 11, 2183-2189 (2003),
http://www.opticsexpress.orgabstract.cfm?id=78787.
[38]
J. F. de Boer, B. Cense, B. H. Park, M. C. Pierce, G. J. Tearney, and B. E. Bouma, "Improved
signal-to-noise ratio in spectral-domain compared with time-domain optical coherence
tomography," Optics Letters 28, 2067-2069 (2003).
[39]
B. Cense, N. A. Nassif, T. C. Chen, M. C. Pierce, S. H. Yun, B. H. Park, B. E. Bouma, G. J.
Tearney, and J. F. de Boer, "Ultrahigh-resolution high-speed retinal imaging using spectraldomain optical coherence tomography," Optics Express 12, 2435-2447 (2004),
http://www.opticsexpress.org/abstract.cfm?id=80 150.
[40]
M. Wojtkowski, V. J. Srinivasan, T. H. Ko, J. G. Fujimoto, A. Kowalczyk, and J. S. Duker,
"Ultrahigh-resolution, high-speed, Fourier domain optical coherence tomography and methods for
dispersion compensation," Optics Express 12, 2404-2422 (2004),
http://www.opticsexpress.or/abstract.cfm?id=80147.
[41]
S. H. Yun, G. J. Teamey, J. F. de Boer, N. Iftimia, and B. E. Bouma, "High-speed optical
frequency-domain imaging," Optics Express 11, 2953-2963 (2003),
http://www.opticsexpress.org/abstract.cfm?id=77825.
[42]
H. Barfuss, and E. Brinkmeyer, "Modified Optical Frequency-Domain Reflectometry with High
Spatial-Resolution for Components of Integrated Optic Systems," Journal of Lightwave
Technology 7, 3-10 (1989).
[43]
W. Eickhoff, and R. Ulrich, "Optical Frequency-Domain Reflectometry in Single-Mode Fiber,"
Applied Physics Letters 39, 693-695 (1981).
83
[44]
S. H. Yun, G. J. Tearney, J. F. de Boer, and B. E. Bouma, "Motion artifacts in optical coherence
tomography with frequency-domain ranging," Optics Express 12, 2977-2998 (2004),
http://www.opticsexpress.org/abstract.cfmn?id=80320.
[45]
S. H. Yun, G. J. Tearney, J. F. de Boer, M. Shishkov, W. Y. Oh, and B. E. Bouma, "Catheterbased optical frequency domain imaging at 36 frames per second," in Coherence Domain Optical
Methods and Optical Coherence Tomography in Biomedicine IX, 5690-16(San Jose, CA, 2005).
[46]
E. Brinkmeyer, and R. Ulrich, "High-Resolution Ocdr in Dispersive Wave-Guides," Electronics
Letters 26, 413-414 (1990).
[47]
S. R. Chinn, E. A. Swanson, and J. G. Fujimoto, "Optical coherence tomography using a
frequency-tunable optical source," Optics Letters 22, 340-342 (1997).
[48]
F. D. Nielsen, L. Thrane, J. Black, K. Hsu, A. Bjarklev, and P. E. Andersen, "Swept-Wavelength
Source for Optical Coherence Tomography in the 1 pm Range," in European Congress on
Biomedical Optics (ECBO)(Munich,Germany, 12-16 June 2005).
[49]
M. V. Shramenko, E. V. Andreeva, D. S. Mamedov, V. R. Shidlovski, and S. D. Yakubovich,
"NIR semiconductor laser with fast broadband tuning," in Coherence Domain OpticalMethods
and Optical Coherence Tomography in Biomedicine X, 6079-42(2006).
[50]
A. V. Oppenheim, R. W. Schafer, and J. R. Buck, Discrete-Time Signal Processing(Prentice Hall,
New Jersey, 1999).
[51]
R. Leitgeb, C. K. Hitzenberger, and A. F. Fercher, "Performance of fourier domain vs. time
domain optical coherence tomography," Optics Express 11, 889-894 (2003),
http://www.opticsexpress.org/abstract.cfm?id=71990.
[52]
M. Wojtkowski, A. Kowalczyk, R. Leitgeb, and A. F. Fercher, "Full range complex spectral
optical coherence tomography technique in eye imaging," Optics Letters 27, 1415-1417 (2002).
[53]
S. H. Yun, G. J. Tearney, J. F. de Boer, and B. E. Bouma, "Removing the depth-degeneracy in
optical frequency domain imaging with frequency shifting," Optics Express 12, 4822-4828 (2004),
http://www.opticsexpress.org/abstract.cfin?id=81308.
[54]
C. Dorrer, N. Belabas, J. P. Likforman, and M. Joffre, "Spectral resolution and sampling issues in
Fourier-transform spectral interferometry," Journal of the Optical Society of America B-Optical
Physics 17, 1795-1802 (2000).
[55]
D. J. Segelstein, The complex refractive index of water (University of Missouri-Kansas City,
1981).
[56]
M. A. Choma, K. Hsu, and J. A. Izatt, "Swept source optical coherence tomography using an allfiber 1300-nm ring laser source," Journal of Biomedical Optics 10 (2005).
[57]
Y. Yasuno, V. D. Madjarova, S. Makita, M. Akiba, A. Morosawa, C. Chong, T. Sakai, K. P. Chan,
M. Itoh, and T. Yatagai, "Three-dimensional and high-speed swept-source optical coherence
tomography for in vivo investigation of human anterior eye segments," Optics Express 13, 1065210664 (2005), http://www.opticsexpress.org/abstract.cfm?id=86669.
[58]
A. Unterhuber, B. Povazay, B. Hermann, H. Sattmann, A. Chavez-Pirson, and W. Drexler, "In
vivo retinal optical coherence tomography at 1040 nm-enhanced penetration into the choroid,"
Optics Express 13, 3252-3258 (2005), http://www.opticsexpress.org/abstract.cfm?id=83715.
84
[59]
S. Bourquin, A. D. Aguirre, I. Hart, P. Hsiung, T. H. Ko, J. G. Fujimoto, T. A. Birks, W. J.
Wadsworth, U. Bunting, and D. Kopf, "Ultrahigh resolution real time OCT imaging using a
compact femtosecond Nd : Glass laser and nonlinear fiber," Optics Express 11, 3290-3297 (2003),
http://www.opticsexpress.org/abstract.cfm?id=7809 1.
[60]
H. Lim, Y. Jiang, Y. M. Wang, Y. C. Huang, Z. P. Chen, and F. W. Wise, "Ultrahigh-resolution
optical coherence tomography with a fiber laser source at 1 pm," Optics Letters 30, 1171-1173
(2005).
[61]
American National Standards Institute, American nationalstandardforsafe use of lasersz136.1
(American National Standards Institute, Orlando, FL, 2000).
[62]
D. V. Alfaro, P. E. Liggett, W. F. Mieler, H. Quiroz-Mercado, R. D. Jager, and Y. Tano, Agerelatedmacular degneration:a comprehensive textbook (Lippincott Williams & Wilkins,
Philadelphia, PA, 2006).
[63]
K. C. Harvey, and C. J. Myatt, "External-Cavity Diode-Laser Using a Grazing-Incidence
Diffraction Grating," Optics Letters 16, 910-912 (1991).
[64]
B. Golubovic, B. E. Bouma, G. J. Tearney, and J. G. Fujimoto, "Optical frequency-domain
reflectometry using rapid wavelength tuning of a Cr4+:forsterite laser," Optics Letters 22, 17041706 (1997).
[65]
S. H. Yun, D. J. Richardson, and B. Y. Kim, "Interrogation of fiber grating sensor arrays with a
wavelength-swept fiber laser," Optics Letters 23, 843-845 (1998).
[66]
S. H. Yun, C. Boudoux, G. J. Tearney, and B. E. Bouma, "High-speed wavelength-swept
semiconductor laser with a polygon-scanner-based wavelength filter," Optics Letters 28, 19811983 (2003).
[67]
B. Culshaw, "The optical fibre Sagnac interferometer: an overview of its principles and
applications," Measurement Science & Technology 17, Rl-R16 (2006).
[68]
W. Y. Oh, S. H. Yun, B. J. Vakoc, G. J. Tearney, and B. E. Bouma, "Ultrahigh-speed optical
frequency domain imaging and application to laser ablation monitoring," Applied Physics Letters
88, 103902 (2006).
[69]
K. Takada, K. Yukimatsu, M. Kobayashi, and J. Noda, "Rayleigh Backscattering Measurement of
Single-Mode Fibers by Low Coherence Optical Time-Domain Reflectometer with 14-Mu-M
Spatial-Resolution," Applied Physics Letters 59, 143-145 (1991).
[70]
J. A. C. Lee, and D. C. Munson, "Spatially variant apodization for image reconstruction from
partial Fourier data," Ieee Transactions on Image Processing 9, 1914-1925 (2000).
[71]
F. J. Harris, "On the Use of Windows for Harmonic Analysis with the Discrete Fourier
Transform," Proceedings of the IEEE 66, 51-84.
[72]
A. H. Nuttall, "Some Windows with Very Good Sidelobe Behavior," Ieee Transactions on
Acoustics Speech and Signal Processing 29, 84-91 (1981).
[73]
B. E. Lemoff, and C. P. J. Barty, "Cubic-Phase-Free Dispersion Compensation in Solid-State
Ultrashort-Pulse Lasers," Optics Letters 18, 57-59 (1993).
[74]
B. Bouma, G. J. Tearney, S. A. Boppart, M. R. Hee, M. E. Brezinski, and J. G. Fujimoto, "HighResolution Optical Coherence Tomographic Imaging Using a Mode-Locked Ti-Al2o3 Laser
Source," Optics Letters 20, 1486-1488 (1995).
85
[75]
J. F. de Boer, C. E. Saxer, and J. S. Nelson, "Stable carrier generation and phase-resolved digital
data processing in optical coherence tomography," Applied Optics 40, 5787-5790 (2001).
[76]
A. F. Fercher, C. K. Hitzenberger, M. Sticker, R. Zawadzki, B. Karamata, and T. Lasser,
"Dispersion compensation for optical coherence tomography depth-scan signals by a numerical
technique," Optics Communications 204, 67-74 (2002).
[77]
C. A. Puliafito, M. R. Hee, J. S. Schuman, and J. G. Fujimoto, Optical coherence tomography of
ocular diseases (SLACK Incorporated, Thorofare, NJ, 1996).
[78]
M. R. Hee, J. A. Izatt, E. A. Swanson, D. Huang, J. S. Schuman, C. P. Lin, C. A. Puliafito, and J.
G. Fujimoto, "Optical Coherence Tomography of the Human Retina," Archives of Ophthalmology
113, 325-332 (1995).
[79]
D. Koozekanani, C. Roberts, S. E. Katz, and E. E. Herderick, "Intersession repeatability of
macular thickness measurements with the Humphrey 2000 OCT," Investigative Ophthalmology &
Visual Science 41, 1486-1491 (2000).
[80]
M. R. Hee, C. A. Puliafito, J. S. Duker, E. Reichel, J. G. Coker, J. R. Wilkins, J. S. Schuman, E.
A. Swanson, and J. G. Fujimoto, "Topography of diabetic macular edema with optical coherence
tomography," Ophthalmology 105, 360-370 (1998).
[81]
M. Baumann, R. C. Gentile, J. M. Liebmann, and R. Ritch, "Reproducibility of retinal thickness
measurements in normal eyes using optical coherence tomography," Ophthalmic Surgery and
Lasers 29, 280-285 (1998).
[82]
R. Huber, M. Wojtkowski, J. G. Fujimoto, J. Y. Jiang, and A. E. Cable, "Three-dimensional and
C-mode OCT imaging with a compact, frequency swept laser source at 1300 nm," Optics Express
13, 10523-10538 (2005), http://www.opticsexpress.org/abstract.cfm?id=86656.
[83]
R. Huber, M. Wojtkowski, K. Taira, J. G. Fujimoto, and K. Hsu, "Amplified, frequency swept
lasers for frequency domain reflectometry and OCT imaging: design and scaling principles,"
Optics Express 13, 3513-3528 (2005), http://www.opticsexpress.orgy/abstract.cfm?id=83745.
[84]
B. J. Vakoc, S. H. Yun, M. S. Shishkov, W. Oh, J. A. Evans, N. S. Nishioka, B. E. Bouma, and G.
J. Teamey, "Comprehensive microscopy of the esophagus using optical frequency domain
imaging," in Coherence Domain OpticalMethods and Optical Coherence Tomography in
BiomedicineX, 6082-13(San Jose, CA, 2006).
[85]
J. Zhang, and Z. P. Chen, "In vivo blood flow imaging by a swept laser source based Fourier
domain optical Doppler tomography," Optics Express 13, 7449-7457 (2005),
http://www.opticsexpress.org/abstract.cfm?id=85477.
[86]
E. C. Lee, J. F. de Boer, M. Mujat, H. Lim, and S. H. Yun, "In vivo optical frequency domain
imaging of human retina and choroid," Optics Express 14, 4403-4411 (2006),
http://www.opticsinfobase.org/abstract.cfn?URI=oe- 14-10-4403.
[87]
R. Seth, and P. Gouras, "Assessing macular pigment from SLO images," Documenta
Ophthalmologica 108, 197-202 (2004).
[88]
S. L. Jiao, R. Knighton, X. R. Huang, G. Gregori, and C. A. Puliafito, "Simultaneous acquisition
of sectional and fundus ophthalmic images with spectral-domain optical coherence tomography,"
Optics Express 13, 444-452 (2005), http://www.opticsexpress.org/abstract.cfm?id=82381.
86
[89]
M. Mujat, R. C. Chan, B. Cense, B. H. Park, C. Joo, T. Akkin, T. C. Chen, and J. F. de Boer,
"Retinal nerve fiber layer thickness map determined from optical coherence tomography images,"
Optics Express 13, 9480-9491 (2005), http://www.opticsexpress.org/abstract.cfm?id=86235.
[90]
A. G. Podoleanu, G. M. Dobre, R. G. Cucu, R. Rosen, P. Garcia, J. Nieto, D. Will, R. Gentile, T.
Muldoon, J. Walsh, L. A. Yannuzzi, Y. Fisher, D. Orlock, R. Weitz, J. A. Rogers, S. Dunne, and
A. Boxer, "Combined multiplanar optical coherence tomography and confocal scanning
ophthalmoscopy," Journal of Biomedical Optics 9, 86-93 (2004).
[91]
C. K. Hitzenberger, P. Trost, P. W. Lo, and Q. Y. Zhou, "Three-dimensional imaging of the
human retina by high-speed optical coherence tomography," Optics Express 11, 2753-2761
(2003), http://www.opticsexpress.org/abstract.cfm?id=77668.
[92]
H. Ishikawa, D. M. Stein, G. Wollstein, S. Beaton, J. G. Fujimoto, and J. S. Schuman, "Macular
segmentation with optical coherence tomography," Investigative Ophthalmology & Visual Science
46, 2012-2017 (2005).
[93]
D. Koozekanani, K. Boyer, and C. Roberts, "Retinal thickness measurements from optical
coherence tomography using a Markov boundary model," Ieee Transactions on Medical Imaging
20, 900-916 (2001).
[94]
MATLAB, "MATLAB Documentation," (2006),
http://www.mathworks.com/access/helpdesk/help/techdoc/matlab.html.
[95]
S. J. Orfanidis, Introduction to Signal Processing(Prentice-Hall, Englewood Cliffs, NJ, 1996).
[96]
V. Poukens, B. J. Glasgow, and J. L. Demer, "Nonvascular contractile cells in sclera and choroid
of humans and monkeys," Investigative Ophthalmology & Visual Science 39, 1765-1774 (1998).
[97]
H. Lim, J. F. de Boer, B. H. Park, E. C. Lee, R. Yelin, and S. H. Yun, "Optical frequency domain
imaging with a rapidly swept laser in the 815-870 nm range," Optics Express (submitted 2006).
87
Artistic Rendering of Choroidal Vasculature by CatherineBolliet