Sociology of Health & Illness Vol. 35 No. 1 2013... doi: 10.1111/j.1467-9566.2012.01481.x
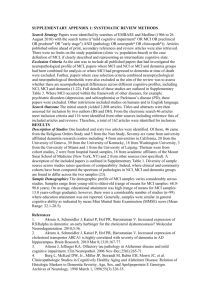
advertisement

Sociology of Health & Illness Vol. 35 No. 1 2013 ISSN 0141–9889, pp. 130–146 doi: 10.1111/j.1467-9566.2012.01481.x Making sense of nonsense: experiences of mild cognitive impairment Renée L. Beard and Tara M. Neary Department of Sociology and Anthropology, College of the Holy Cross, Worcester MA, United States Abstract Alzheimer’s disease (AD) is a stigmatised condition popularly assumed to be a death sentence for diagnosed individuals. Consequently, people with AD are often deemed incapable (and perhaps unworthy) of contributing to the social discourse surrounding their illness experience. Data from qualitative interviews with 18 people diagnosed with the potential precursor of AD known as mild cognitive impairment (MCI) are examined. Using grounded theory methods, analysis revealed overarching themes of uncertainty concerning definitions of memory loss, MCI, and AD as well as distinctions between normal ageing and dementia. While this confusion over the terminology and prognosis mirrors the lack of scientific consensus about nosology and appropriate treatment regimens, such ambiguity creates social and psychological tensions for diagnosed individuals. Arguably, participants’ unequivocal fear of and subsequent desire to differentiate their experiences from Alzheimer’s, however, stems from the exclusively negative social constructions of AD. Drawing from Goffman, these findings demonstrate the psychosocial impact of ‘framing contests’ and how ‘courtesy stigma’ can apply not only to associated persons but also associated conditions, such as MCI to AD. Given the underlying nosological creep – or medicalisation – of the recent diagnostic guidelines proposing two new predementia stages, understanding the illness narratives of MCI is critical. Keywords: mild cognitive impairment, Alzheimer’s, illness narratives, clinical uncertainty Introduction In April 2011 the US National Institute of Aging and Alzheimer’s Association released new diagnostic guidelines for Alzheimer’s disease (AD). In contrast to the original criteria developed over a quarter of a century ago, the revised diagnostic and research standards posit a continuum of AD that extends the medical gaze to include two new phases prior to Alzheimer’s. Clinically, the new classification includes the dementia phase (AD), the symptomatic, pre-dementia phase known as mild cognitive impairment (MCI) and an asymptomatic, preclinical phase (Jack et al. 2011). For the past 20 years MCI was considered merely a potential precursor and while diagnosed individuals scored below average for their age and education on neuropsychological tests, they did not have an impairment in daily living and were not necessarily expected to convert to AD. The new criteria inflate the already soaring numbers of seniors experiencing ‘memory problems’ in a ‘hypercognitive’ 2012 The Authors. Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd. Published by Blackwell Publishing Ltd., 9600 Garsington Road, Oxford OX4 2DQ, UK and 350 Main Street, Malden, MA 02148, USA Sense-making in mild cognitive impairment experiences 131 society where cognition and rational thinking are ascribed paramount importance (Post 1995, 2000). Furthermore, highly medicalised and narrow depictions of Alzheimer’s lead to stigmatisation as the condition is assumed to be a death sentence. Despite empirical documentation that individuals so diagnosed remain engaged in life (Cohen-Mansfield et al. 2000, Li and Orleans 2002, Wilkinson 2001) and, indeed, report positive aspects to living with dementia (Beard 2004a, Beard and Fox 2008, Harris 2009, Holst and Hallberg 2003, Kramer 1997), people with Alzheimer’s are often deemed incapable (and perhaps unworthy) of contributing to the social discourse on their condition or even narrating their own experience of illness. Constructions of individuals with Alzheimer’s as ‘the living dead’ (Aquilina and Hughes 2006) and ‘zombies’ (Behuniak 2011) both reflect and reinforce this marginalisation. The new diagnostic guidelines expand dementia to include cognitive disorders previously defined as typical of ageing and a potentially very lengthy asymptomatic phase (Gaines and Whitehouse 2006, Purser et al. 2006, Whitehouse and Moody 2006). The origin of MCI has been traced to Kral’s (1962) term ‘benign senescent forgetfulness’. In 1993 the International Classification of Diseases (World Health Organization 1993) listed ‘mild cognitive disorder’ and a year later the Diagnostic and Statistical Manual (American Psychiatric Association 1994) cited ‘mild neurocognitive decline’. In 1997 both ‘cognitive impairment no dementia’ and ‘mild cognitive impairment’ entered the discourse in psychiatry and neurology (Graham et al. 1997, Petersen et al. 1997, respectively). Currently, MCI is most widely accepted among medical practitioners to describe the decline in cognitive function that is detected in nondemented people. Clinicians have also identified numerous subtypes of MCI, with amnestic MCI (impairment based predominantly on memory-related symptoms) deemed to be most likely to progress to Alzheimer’s (Petersen 2004). Significant dissent, however, regarding the conceptual basis, the diagnostic algorithms and the relationship between MCI and similar concepts persists (Corner and Bond 2006, Graham and Ritchie 2006, Ritchie and Touchon 2000). This is in part because rates of conversion from MCI to AD vary drastically, with studies reporting as little as 9.6 per cent over 22 years (Elias et al. 2001) and as much as 100 per cent in 4.5 years (Krasuski et al. 1998). Furthermore, research suggests that the same number of MCI cases convert back to normal as they do to AD (Daly et al. 2001) and a general instability across time, with as much as 40 per cent reverting to normal (Ritchie and Touchon 2000). The potential implication of such predictive imprecision for MCI (Corner and Bond 2006) includes direct psychosocial costs to individuals diagnosed with MCI and their family members as well as the indirect consequences for all of us as we age. Despite these controversies, an enormous amount of scientific attention and federal funds have been directed to the recent discovery of this Alzheimer’s prodrome. Although many consider it a potential precursor to AD, others argue that it has clinical utility only and warn of the possible psychosocial consequences of diagnosing the condition. As a result, how to diagnosis MCI – if at all – remains heavily debated among neurologists, geriatricians, neuropsychiatrists, general practitioners and bioethicists (Corner and Bond 2006, Gaines and Whitehouse 2006, Graham and Ritchie 2006). Some critical scholars suggest that the condition demonstrates a ‘hardening of the categories’ (Whitehouse and Moody 2006) and threatens a spoiled identity (Goffman 1963) for those diagnosed (Corner and Bond 2006), resulting in the further medicalisation of ageing. Framed in this way, dementia becomes a spectrum disorder representing an incisive example of diagnostic expansion (Conrad 2007). Like attention-deficit hyperactivity disorder, erectile dysfunction and, most recently, autism, the clinical constructions of Alzheimer’s create an ‘us ⁄ them’ dynamic between the everincreasing ranks of forgetful seniors and everyone else. 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd 132 Renée L. Beard and Tara M. Neary In practice, distinguishing between normal cognitive ageing, MCI and the early stages of degenerative dementias such as Alzheimer’s remains an enormous challenge (Graham and Ritchie 2006, Whitehouse and Moody 2006). Since neuropsychological testing is a poor indicator of MCI, clinical judgment plays a central role in diagnosis (Corner and Bond 2006). The clinical and aetiological heterogeneity of MCI is further complicated by a lack of evidence supporting the notion that early treatment or intervention is beneficial for managing decline or even for improving quality of life (Whitehouse and George 2008, Whitehouse and Moody 2006, Winbald et al. 2004). While early detection and diagnosis may allow planning for the future or starting a specific drug regimen, the potential consequences of research endeavours to identify the criteria and underlying neuropathology of this medical entity include the risk of clinically or socially conflating MCI and Alzheimer’s. Although evidence suggests that some seniors presenting with subclinical cognitive deficit show quantitative anatomical and structural changes distinct from either normal ageing or Alzheimer’s, the magnitude of these changes is difficult to calculate due to the lack of consensus regarding the selection criteria employed and samples that are not representative. This lack of cohesion has implications not only for bench science but also for clinical practice aiming to identify and treat memory loss. Social implications of MCI diagnoses Institutions such as modern medicine are powerful social forces in the lives of citizens of the western world. When clinical diagnoses are assigned, everyday words such as MCI become social labels with the power to differentiate between and discriminate against people. It is well established that not all diagnoses are alike; that is, some come with a stigma relegating those so labelled to second-class or even ‘subhuman’ status. That modern medicine, as an institution of social control, has influenced the perception or social construction of ageing as a negative phenomenon was long ago documented in the social sciences (Estes 1979, Gubrium 1986, Kaufman 1994, Zola 1972). Accordingly, pejorative views of ageing reflect and reinforce its (bio)medicalisation (Beard and Estes 2002, Estes and Binney 1989, Kaufman et al. 2004) rather than a celebration of ageing or even the acceptance of gradual, ‘normal’ decline, which clearly extends to dementia (Bond 1992, Lyman 1989). The medicalisation of dementia involves framings of AD in the public media, advocacy arena and scientific outlets that are predominantly disparaging. Such depictions include ‘narratives of tragedy’ (Basting 2009), often using the ‘zombie trope’ (Behuniak 2011), focused on a loss of self rhetoric, end-stage issues and perceptions of caregivers as the real victims of the condition, which are simplistic and overly reductionist. Scientific efforts emphasise cause and cure and clinical practice focuses on identifying the condition as early as possible (preferably preclinically and now asymptomatically) as reflected in the steadfast focus on biomarkers, including imaging technologies (positron imaging tomography), cerebrospinal fluid and genetic testing. Until recently there has also been scant attention to the diagnostic imprecision that some provocatively claim created ‘the myth of Alzheimer’s’ (Whitehouse and George 2008) and contributes ‘to premature and speculative hype’ (Graham and Ritchie 2006: 32). Yet there has been little discussion of the social or interactional consequences and bioethical implications of predicting Alzheimer’s decades before symptoms are experienced. In exploring the subjective experiences of individuals diagnosed with MCI, our data are among the first to begin asking how individuals make sense of this diagnosis and its potential psychosocial impact. Given the inefficacy of diagnostic and treatment regimens, the social implications of the label are profound yet almost no data on the subjective experience of this condition exist (Corner and Bond 2006). Only recently have scholars begun to examine the experiences of individuals with MCI or their families, and the potential difficulties as well as the unique 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd Sense-making in mild cognitive impairment experiences 133 attributes of the label (Joosten-Weyn Banningh et al. 2008, Lingler et al. 2006) and associated changes in familial roles (Blieszner and Roberto 2009, Garand et al. 2005, 2007) have been demonstrated. Practical, social and psychological consequences of the diagnosis are reported (Joosten-Weyn Banningh et al. 2008). Emotional and cognitive dimensions of assigning meaning to a diagnosis of MCI are also said to be influenced by contextual variables such as previous views about normal ageing, past exposure to dementia and comorbidities (Lingler et al. 2006). Individuals report confusion and misinformation about their diagnosis (for example, whether to take medication and where to seek help and find information). As a result, those diagnosed engage in various coping strategies when faced with the uncertain label of MCI (Joosten-Weyn Banningh et al. 2008) and the condition presents ‘new and complex challenges’ (Blieszner and Roberto 2009) for families and care partners alike. What people with MCI1 do have in common with those diagnosed with AD, sociologically speaking, is a threatened personal and interpersonal wellbeing, including a sense of being devalued (Beard and Fox 2008, MacQuarrie 2005, Werezak and Stewart 2002). Along with epilepsy and schizophrenia, individuals diagnosed with Alzheimer’s risk being conflated with the thing that they are labelled; thus becoming ‘epileptics’, ‘schizophrenics’, and ‘Alzheimer patients’ (Estroff 1989, Link and Phelan 2001). Accordingly, unlike persons who have cancer or even AIDS, the connotation of being ‘no longer there’ or ‘dead before death’ risks throwing individuals with AD into a social wastebasket, which bioethicist Stephen Post (1995) long ago termed ‘The moral challenge of Alzheimer’s disease’. Diagnostic expansion escalates the threat. While MCI diagnoses are likely to increase, given the new guidelines, its aetiological and clinical heterogeneity have prompted questions about whether a diagnosis of MCI can be accurately differentiated from normal ageing and whether the potential consequences of being associated with Alzheimer’s are worth the questionable benefits offered by the current pharmacological treatment options and social services available (Gaines and Whitehouse 2006, Whitehouse and Moody 2006). Although the lack of consistent evidence supporting the hypothesis that MCI may progress to dementia or AD brings to light the relatively arbitrary nature of this clinical entity, biomedical constructions dominate the framing of forgetfulness. Given population ageing and the new diagnostic criteria, the social significance of this illness identity cannot be overstated; a diagnosis of any ‘memory problem’ indeed creates social problems for affected individuals. Understanding the social aspects of MCI diagnoses was the basis for our analysis. We found that respondents were confused and misinformed about definitions of memory loss, MCI and AD as well as the distinctions between normal ageing and dementia. While respondents’ confusion over terminology and prognosis mirrors the lack of scientific consensus about the nosology and appropriate treatment regimen for MCI, their resoundingly negative perceptions of AD and associated fears also reflect the dismal portrayal of the condition in the media, advocacy arena and biomedical realms. We hypothesise that in the framing (Goffman 1974) contest over Alzheimer’s a deficit model of modern medicine prevails, based on America’s decline ideology (Gullette 2011). Since frame analysis sheds light on how people interpret situations and activities, we speculated that individuals diagnosed with MCI would perform interactional work to employ coping strategies similar to those reported by individuals with Alzheimer’s (Beard 2004a, Beard and Fox 2008, Beard et al. 2009, Clare 2002, 2003, Clare et al. 2005, Sabat 2001) in an effort to minimise their subsequent social disenfranchisement or the associated stigma. We suspected that such efforts to avoid the master status of ‘Alzheimer patient’ would reflect an internalised ageism in our respondents based on what has been called the American cultural construction of decline (Gullette 2011). We posit that the interactional tensions resulting 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd 134 Renée L. Beard and Tara M. Neary from this label, which necessitate management strategies, are based on the courtesy stigma (Goffman 1963) from the presumed association with Alzheimer’s. Thus, the diagnosis comes with considerable social baggage; that is, the confusion and fear surrounding the condition causes a threat to the social identity of those labelled with MCI. While stigma as a sociological concept has been widely applied to various illnesses, disabilities and characteristics, ‘courtesy stigma’ is most often used to analyse the social and psychological impact, on the individual level, of associating with a discredited person. We suggest that the term can be extended to various related conditions, here MCI. Applying courtesy stigma to associated conditions adds to the reconceptualising of stigma (Link and Phelan 2001) and the general theoretical discourse on this core sociological concept. Methods These data are a subset of a larger study, entitled ACCESS (Assessing the Cultural Characteristics of Elders and the Support Systems), exploring first-hand and second-hand narratives of AD. The purpose of the subset analysis reported here was to examine the specific experiences of memory loss for individuals diagnosed with MCI. The larger project was an exploratory study utilising mixed methods, including in-depth interviews, focus groups and survey data. Multiple forms of data collection were used to allow participation in either personal or group discussions, depending on the respondents’ preference. Furthermore, triangulation of in-person interviews with focus groups increases the validity of the findings since group conversations remove the potential pressure of direct recall required during in-person interviews. The research was based on a nonprobability sample using convenience, snowball and theoretical sampling. Given the paucity of previous studies on the topic and exploratory nature of this research, grounded theory methods were deemed well-suited to the project. These techniques were employed in collecting, coding and analysing data to inductively generate theory grounded in the data themselves rather than testing hypotheses or existing theories. Recruitment All study participants were recruited from a research registry at an Alzheimer’s Disease Center in a large Midwestern US city. The respondents had sought cognitive evaluation of their own accord because they suspected that something was wrong with their memory, had been given a diagnosis of amnestic MCI within the previous three years and were community-dwelling. They had agreed to be contacted about future research studies and thus, at least implicitly, self-identified with the label they had been given. Sample The subset sample reported on here included in-depth individual interviews (n = 10) and two focus groups (n = 8) with individuals diagnosed with MCI (N = 18). Among our informants, two-thirds (n = 12) were women and one-third (n = 6) were men. Most were either widowed (50%) or married (33%), with one each being single and divorced. Their average age was 76 years old. The sample was divided between respondents who stated their race was Caucasian (56%) and those who self-identified as African American (44%). Almost three-quarters (n = 13; 72%) of the participants had at least ‘some college’, with seven (39%) reporting 16 + years of education and another third (n = 6) who had graduated from high school. Half (n = 9) of our respondents reported income levels between $20,000–39,000 (adjusted per person), with 22% (n = 2 each) below $20,000 and above $65,000. What these 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd Sense-making in mild cognitive impairment experiences 135 characteristics reveal is a group of respondents who are disproportionately middle-class widows of higher than average education living alone in the community. Given the paucity of previous samples to compare with and the lack of consensus on inclusion criteria (amnestic versus other MCI, age, comorbidities, etc.) used in prior studies, meaningful comparisons cannot be made. The social location of these study participants is, however, important to keep in mind when interpreting the findings outlined below. See Table 1 for complete sample characteristics. Qualitative analysis The first author and principal investigator (RB) conducted all interviews in person using an interview guide. The guide was utilised as a probe to generate conversation without following a standardised format and questions were added on if and when new areas of inquiry were discovered. Respondents, as the experts on the subjective experiences of MCI, were generally encouraged to lead the conversation according to what they deemed important. Table 1 Sample characteristics Women (n = 12) Diagnosis Mild cognitive impairment Age 65–74 years 75–84 years 85 + years Race ⁄ ethnicity African Americans White, not Hispanic Marital status Married Widowed Single Divorced Highest education completed High school graduate or general education diploma Some college, technical or vocational College degree At least some graduate education Annual income per person < $20,000 $20,000–39,999 $40,000–64,999 $65,000–99,999 Time since diagnosis < 1 year 2 year 3 years Percentage of total sample Men (%) (n = 6) (%) (N = 18) 12 100 6 100 100 8 3 1 67 25 8 2 1 3 33 17 50 56 22 22 8 4 67 33 0 6 0 100 47 53 1 9 1 1 8 75 8 8 6 0 0 0 100 0 0 0 39 50 6 6 5 42 0 2 1 4 17 8 33 2 2 2 33 33 33 22 17 33 2 7 3 0 17 58 25 0 0 2 2 2 0 33 33 33 11 50 28 11 10 2 0 83 17 0 1 4 1 16.5 67 16.5 61 33 6 28 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd 136 Renée L. Beard and Tara M. Neary All interviews were audio-taped, transcribed and then analysed using the constant comparative method and coding paradigm of grounded theory (Corbin and Strauss 1998, Glaser and Strauss 1967). Since this method aims to generate overarching themes, the ongoing process of taking notes, writing memos and (re)reading data lends itself to emergent categories for simplifying and articulating data. As line-by-line coding occurs, themes are generated. Detailed notes were dictated immediately following all interviews. Paid assistants transcribed each taped interview verbatim, yielding 311 pages of narrative transcript data. The interviewer verified the transcript accuracy by reading each one upon receipt. Additional quality control measures (i.e., reading transcripts while playing the data files) were performed on 100 per cent of the subsample used for the present analysis. In the larger study all interview transcripts were read prior to scheduling the next one to encourage the incremental development of theory and the categorisation of ideas and themes. The present analysis began with open coding, which involved identification of the dimensions and properties of the themes in the margins of textual data line-by-line. Next, themes were consolidated by using an explanatory matrix to identify core variables. Themes were not deemed representative of the subsample unless they occurred in most of the cases or interviews. To ensure reliability of the findings in this sub-study analysis, three research assistants from the larger ACCESS project read all the textual interview files, provided detailed analysis notes and line-by-line coded each transcript. The themes identified in their analyses were consistent with the major core variables identified by the co-authors. The common themes for the subset of individuals diagnosed with MCI will be reported here. Findings The data reveal that the study participants in fact perform various types of interactional work, on abstract as well as concrete levels, to manage their memory difficulties. The four common themes include: questioning whether or not their condition was a disease, struggling to define MCI, distancing their experiences from Alzheimer’s and, at least implicitly, grappling with the social implications of the diagnosis vis á vis Alzheimer’s. In the extracts the abbreviation ‘R’ with a number indicates a respondent, ‘INT’ indicates the setting was an interview and ‘FG’ indicates the setting is a focus group. The interviewer’s questions are in italics. Is what we are experiencing a disease? In support of previous studies (Joosten-Weyn Banningh et al. 2008, Lingler et al. 2006), most respondents identified their forgetfulness as a consequence of the normal ageing process rather than a brain-based disorder. While they reported occasional difficulty with remembering names or places, individuals with MCI did not consider their experiences to be a significant problem. This led them to ascribe their memory problems to their ageing identity: R1: R2: R3: What do you think is going on? Other than getting old? I don’t know. Getting old. I think that’s what it is. Getting older, you forget certain types of things. You’re not as quick as you used to be. (FG, African American women) I think the problem I have today is a mild problem. It is not a severe problem for me. (INT, Caucasian man) 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd Sense-making in mild cognitive impairment experiences 137 Similar views were cited, to varying degrees, by nearly every respondent in our study. As Lingler et al. (2006) suggest, individuals with MCI perceive their diagnosis to be an expected aspect of the ageing process, and our findings demonstrate that those with MCI normalise their memory difficulties accordingly. That is, memory loss was yet another obstacle to be overcome, like hearing loss, reduced mobility or social isolation. Furthermore, several respondents identified the need to slow down in general as they grew older and the importance of accepting the changes in their memory: It’s time to slow down ... I’m not Superwoman. I have to realise that and stop. That’s what I realise is going on with me. (FG, African American woman) I guess another thing that you have to realise is that as you age your whole body changes and things change in your life and you have to accept it. (INT, African American woman) Yes, we all laugh about it. You know, ‘Oh, we’re getting old!’ (INT, African American woman) As the last quote shows, some respondents actively used humour to help them manage their memory lapses. Our findings also support the notion that individuals with MCI engage in various coping strategies when dealing with their diagnosis (Joosten-Weyn Banningh et al. 2008). Such strategies include emotion-oriented coping in which individuals express acceptance and resignation as a way to normalise their forgetfulness rather than fight it. Problem-focused coping, such as keeping notes to remind them of important dates and information, were also reported. Unlike the participants in the Joosten-Weyn Banningh et al. (2008) study, however, our respondents did not explicitly deny their forgetfulness or demonstrate avoidance-oriented coping strategies. On the contrary, most participants contended that their memory problems were not unique and that nearly everyone their age experiences similar difficulties: So do you think you have the same amount of forgetfulness as others your age? Oh, I think we all go through times where we can’t remember something and we just skip and we forget what we’re looking for but it will come back to us. I don’t think it’s a serious problem. All of us go through those things. (INT, African American woman) It’s not early stage Alzheimer’s. It’s not MCI. I have a situation where I can’t remember something. But, I don’t think that is different than other people my age. (INT, Caucasian man) Ultimately, our respondents identified their forgetfulness as a normal and common feature of growing older. As such, they did not consider their difficulties to be a serious problem or something that required routine medical attention. Instead, they normalised their experiences as part of the ageing process. What is MCI? When asked specifically about their diagnosis, respondents reported a resounding lack of clarity about what constitutes MCI despite the predominance of perceptions connecting it to normal ageing processes: 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd 138 Renée L. Beard and Tara M. Neary What does MCI mean to you? [laughs] You forget things. You’re not always doing the right thing 100% of the time … Something’s going on in the brain. Do you think that’s what’s going on for you? Is this mild cognitive impairment? I’m not sure. I don’t know … It means I forget. It could be the first stages of Alzheimer’s. Was your impression that mild cognitive impairment is a disease or forgetfulness? I don’t know about a disease, more of a … Well I don’t believe it was ever discussed. I think it was at least in my mind a consequence of getting older. (INT, Caucasian woman) How would you define mild cognitive impairment? I’m not sure that it was defined. I would say that it is the inability to function the way you should. I don’t necessarily find that is the case with me. (INT, Caucasian man) Have you ever heard the words mild cognitive impairment? I’ve heard those terms, but I’m not sure what they mean. (INT, African American woman) As these quotes demonstrate, study participants generally did not know how to describe MCI. In fact, many were not sure that the term had ever been defined for them by doctors. Perhaps this general ambiguity reflects the scientific literature and clinical practices based on it. Nonetheless, there were a few respondents who defined MCI as a memory-related disorder, if vaguely: Some kind of disorder in … the brain? Mild disorder. That’s what I think. (FG, African American woman) Do you think it might mean you’re on your way to Alzheimer’s? You’re on your way to something … it’s a disorder. (FG, African American woman) While the new guidelines suggest that MCI is undergoing a medicalisation process, narrative accounts of the condition do not support this.2 In fact, study respondents demonstrate a resistance to such labelling. Despite advances in diagnostic criteria and practice parameters, perhaps this is due to the fact that the MCI label is used inconsistently by clinicians and researchers (as the need for new diagnostic guidelines suggest; see Whitehouse et al. 2004). Accordingly, its arbitrary location on a continuum of ageassociated cognitive challenges can be a source of great confusion and uncertainty for individuals with MCI. For example: I don’t have any idea … a precursor? My feeling is there is a lot of guesswork involved and that people don’t really know. Do you have early stage Alzheimer’s? Do you have MCI? Is there a difference? [It’s] a gray area. It’s like trying to make sense of nonsense. (INT, Caucasian man) Such ambiguity about terminology and prognosis reflects the lack of scientific consensus about the nosology and appropriate treatment regimen for MCI. At least it isn’t AD Despite their confusion, participants vehemently denied any association between their experiences and Alzheimer’s. Consequently, many respondents reported that the awareness 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd Sense-making in mild cognitive impairment experiences 139 of one’s own forgetfulness distinguishes MCI from AD. The following quotes demonstrate this differentiation: We acknowledge that we forgot this or forgot that. And do you think that is what makes it different from, say, Alzheimer’s disease? Right. Or it’s just one step behind. (INT, Caucasian woman) I would say that if my memory begins to get worse, then I would know. I would know that something is worse. (INT, African American woman) Previous studies have shown considerable variability in the level of awareness of cognitive deficits among individuals with MCI. While some people have quite limited awareness, others overestimate their dysfunction which may signify a hyper-awareness (Roberts et al. 2009). The ability to recognise their memory difficulties was interpreted by our respondents as evidence of normal ageing rather than a serious problem like Alzheimer’s. Perhaps the apparent need to distinguish their experiences from AD is an example of efforts to maintain a normal identity, as reported in relation to other health conditions (Gray 2002). Although many respondents talked about this, one woman specifically stated that not being able to do what she normally does would signify that her condition was more significant: If it gets to the point where I cannot do a straight tax and I don’t know where to begin with a client, then there’s something wrong. And [if] I’m going to church and Sunday school and I can’t get through a lesson, and I don’t understand what it’s saying to me, then there’s something wrong. (INT, African American woman) This quote demonstrates the assumption most respondents held that crossing some predetermined threshold would signal a ‘real’ problem. Implications of association with Alzheimer’s When discussing Alzheimer’s, there was general consensus among our respondents that it is a medical condition. Despite the vague definitions provided below, respondents relied mainly on medical explanations to define AD. I do think of it as a disease, as a loss of not just function but actual tissue. It is not a normal thing. (INT, Caucasian man) In your impression what is Alzheimer’s, a disease? Okay … I would say it’s a disease. But there’s no cure. But it’s a disease like anything else. (INT, African American woman) Upon further probing, however, most respondents were unsure of its aetiology: R1: R2: R3: R4: So how do you think people get Alzheimer’s? What causes Alzheimer’s? I don’t know. I don’t know. I have no idea. Some people say maybe a lick on the head you incurred earlier. Some people, age just doesn’t affect them the way it affects other people. (FG, African 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd 140 Renée L. Beard and Tara M. Neary American women) What do you think causes that [AD]? I have no idea. Is it something in the brain or something in the body chemistry or something that changes with aging or what? I don’t know. (INT, African American woman) What was unanimously and most commonly expressed, however, was the fear associated with Alzheimer’s – the ‘death sentence’ diagnosis – and their determination not to ‘get it’: It’s feared just like cancer is. It’s a death sentence … Means a loss of function, of essential function. To function as a human being. A loss of the capacity to be one’s self. And it’s frightening. It’s the worst of all insults. Why? Because I suppose above all things we prize ourselves, who we are, who we have come to be, what we have been and what we can be and if we lose all that we’ve lost everything. And as you see it the disease that is Alzheimer’s does that? As it progresses, yes. (INT, Caucasian woman) Because they would rather be crazy than have Alzheimer’s … It’s a death sentence. It’s over. (FG, African American woman) [Alzheimer’s is a] lack of life. Lack of recognition. Lack of knowledge. (INT, Caucasian woman) Perhaps as a result of their determination not to have their experiences conflated with Alzheimer’s, some respondents reflected a lay understanding of what Goffman might have called a courtesy stigma potentially resulting from associating MCI with Alzheimer’s: And when you get something like Alzheimer’s you feel you’re no longer in charge … I don’t think any of us like the idea of having to give over to somebody else. (INT, African American woman) [With Alzheimer’s] you are not able to do what you need to do psychologically and mentally. That’s what I think and I don’t think I have early stage Alzheimer’s. Probably because it is a terrible disease and I don’t want to be a part of that. (INT, Caucasian man) The transparency of their fears related to Alzheimer’s demonstrates the assumptions our respondents held about the futility of life with AD. Given that depictions of memory loss have typically been framed within what has been called a biomedical discourse of loss (Beard and Fox 2008), in which a diagnosis of Alzheimer’s signifies the never-ending funeral, a slow unravelling of the self and a complete loss of one’s self (Basting 2009, Beard et al. 2009, Fox 1989, Gubrium 1986), the views of our participants are not surprising. Empirical studies of memory loss are most often based on biomedical or psychological models of disease pathology and symptom reduction. Our respondents’ views reflect the general public’s negative perception of AD based on media and advocacy representations of this disease as the slow death of the mind and the biomedical emphasis on cause and cure rather than living with Alzheimer’s. 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd Sense-making in mild cognitive impairment experiences 141 Contemporary public perceptions and media portrayals of Alzheimer’s are almost exclusively pejorative despite the now vast literature demonstrating the meaningful lives such individuals continue to live (Basting 2009, Beard et al. 2009, Harris 2009), including numerous autobiographies countering such generalisations (Bryden 2005, DeBaggio 2007, Fisher 2007) and explicit efforts by those so diagnosed to combat these assumptions (Knauss and Moyer 2006, Sterin 2002, Taylor 2006). Attempts to normalise experiences of forgetfulness, or manage their social identities to avoid the master status of Alzheimer patient are commonly reported by individuals who have AD as well (Beard and Fox 2008, Clare 2003, Clare et al. 2005). Although it is likely that our respondents are indeed aware of the vast differences between Alzheimer’s and their own experiences of forgetfulness, it is important to understand the social context within which they were medically evaluated and ultimately diagnosed with MCI. Previous studies have discussed how individuals diagnosed with AD (must) negotiate threats to self (Clare 2003) and a tangled veil (Sabat 2001) in order to preserve their identities (Beard 2004a). Arguably, the respondents’ unequivocally negative perceptions of life with Alzheimer’s encourage them to perform stigma avoidance by differentiating their experiences from those with AD. The social consequences of being associated with individuals who are stigmatised, or courtesy stigma, perhaps leads individuals diagnosed with MCI to (need to) actively resist the stigma of Alzheimer’s. Given the overwhelmingly negative constructions of AD in modern western societies, it is perhaps strategic to at least try to avoid such association. Discussion We argue that Alzheimer’s can be added to the long list of stigmatised medical labels that ascribe a master status to recipients. Perhaps most significantly, the diagnostic creep of Alzheimer’s extends the threat to preclinical states like MCI. The seemingly endless diagnostic expansion (Conrad 2007) demonstrated by the new guidelines for AD has the potential to apply this devalued status to individuals in the asymptomatic phase as well. The study participants expressed considerable uncertainty regarding what MCI is and how it differs from AD. Although they mostly considered their forgetfulness to be ageingrelated or normal, they vacillated on this. Furthermore, they were unclear even about the definition and cause of Alzheimer’s, despite the steady stream of media attention and outpouring of research funding. What is quite clear, however, is their resounding fear of Alzheimer’s – according to them it is a ‘death sentence’ the ‘loss of function as a human being’ and ‘a loss of capacity to be one’s self’. Perhaps the study participants fear AD not as a result of their direct experiences but rather because of their uniformly negative perceptions of the condition. This loss of self rhetoric reflects the contemporary pejorative views portrayed in the public media and basic sciences generally. This projection homogenises all individuals so diagnosed and universalises all ‘stages’ of the condition (to the ‘end stage’). Although advocacy organisations could go a long way to help refute this discourse of loss they have been slow to do so (Beard 2004b). Since social identities are constructed and precarious in nature, people devise strategies to make the unmanageable manageable (Birenbaum 1992, 1970). If the social attribution of stigma creates distinctions – moral and otherwise – then individuals diagnosed with MCI strive to distinguish their experiences from Alzheimer’s to avoid being ascribed the associated spoiled identity (Goffman 1963). Stigma is deeply social and for those adversely labelled, medical conditions become social problems to be managed. 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd 142 Renée L. Beard and Tara M. Neary The ever-expanding medical gaze arguably generates courtesy stigma (Goffman 1963) not only for those associated with individuals who have problematic conditions – as discussed in relation to the significant others of people with various health conditions, including Alzheimer’s (Holston 2005, Jolley and Benbow 2000, MacRae 1999, Werner and Heinik 2008) but also for associated conditions, such as MCI. Accordingly, critical social theorists (Armstrong 1995, Arney and Bergen 1984, Foucault 1973) might position Alzheimer’s as a quintessential case of contemporary surveillance medicine. By reifying everyday words such as MCI into a bona fide medical label, the new guidelines simultaneously socially construct the perception of a need for increased self-surveillance by current and future older individuals alike. Given the relatively recent interest in and now established diagnosis of MCI, the diagnostic shift underway in dementia care reveals a compelling example of postmodern social problems. Since diagnostic labels can influence emotional responses, symptom perceptions, attributions and coping skills (Wadley and Haley 2001), even a ‘pre-dementia’ diagnosis can generate interactional tensions. Thus, more and different information is needed as a result of the prognostic uncertainty of an MCI label than the existing practice geared toward individuals with AD provides. In particular, qualitative, narrative accounts of MCI are missing. Including the perspectives of individuals diagnosed with MCI makes a substantial contribution to the research on subjective experiences of AD and reveals the existential angst present in what has been called a health-obsessed or risk society. Furthermore, since dementia and AD do not exist in all cultures, the heightened sense of value imposed on brains, minds and sentience in western societies positions Alzheimer’s as a distinctly postmodern phenomenon as well as a powerful example of how social constructions and processes of medicalisation can be socially and interactionally troublesome for even potentially diagnosed individuals. In addition to expanding existing theoretical debates, these findings also have implications for future research and clinical practice. It is crucial to understand the perspectives of those most intimately affected in order to trace the effects of medical labels on social interactions and everyday lives. In order to address bioethical concerns, inform interventions and improve clinical encounters and quality of life for diagnosed individuals, as well as to provide appropriate services and treatment options, narratives of MCI must be explored further. Given the recent redefinition of MCI as the symptomatic, pre-dementia phase of Alzheimer’s, which is technically the middle stage of the continuum for what is now a spectrum disorder, experiences of the condition should also be tracked longitudinally as this reconceptualisation infiltrates lay understandings of the condition or is resisted by them. Address for correspondence: Rene´e L. Beard, Department of Sociology and Anthropology, College of the Holy Cross, One College Street, Beaven Hall 218, Worcester, MA 01610, USA e-mail: rbeard@holycross.edu Notes 1 Despite the fact that we use the term ‘people’, the lack of consensus on the terminology prevents an accurate reading of the characteristics, or social location, or the kinds of people who are diagnosed with MCI. It is impossible, therefore, to address variables such as race and ethnicity, social class, gender or even age of diagnosed individuals: issues of central importance to sociology. 2 Perhaps this is related to the fact that the official designation of MCI as a stage of AD had not been made at the time this research was conducted. 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd Sense-making in mild cognitive impairment experiences 143 Acknowledgements The findings from this project were presented at the Gerontological Society of America and Society for the Study of Symbolic Interaction meetings in 2010. We want to thank all the individuals who took the time to share their stories with us. The insightful comments of the journal editors and anonymous reviewers were also very helpful. This research was funded by the Midwest Roybal Center for Health Promotion and Behavior Change (2005-E7651) and the Illinois Department of Public Health’s Alzheimer’s Disease Research Fund (No. 83280014). Thank you also to the Northwestern Alzheimer’s Disease Center (grant AG13854) Clinical Core and the National Chapter of the Alzheimer’s Association, both in Chicago, for kindly helping us recruit participants. The Richard and Sarah Greisch Summer Research Fellowship in Sociology at the College of the Holy Cross, awarded to the second author, supported this sub-set analysis. References American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV), available at http://www.psych.org/mainmenu/research/dsmiv/dsmivtr.aspx (last accessed 19March 2012). Aquilina, C. and Hughes, J.C. (2006) The return of the living dead: agency lost and found? In Hughes, J.C., Louw, S.J. and Sabat, S.R. (eds) Dementia: Mind, Meaning, and the Person. Oxford: Oxford University Press. Armstrong, D. (1995) The rise of surveillance medicine, Sociology of Health & Illness, 17, 3, 393– 404. Arney, W.R. and Bergen, B.J. (1984) Medicine and the Management of Living: Taming the Last Great Beast. Chicago: University of Chicago Press. Basting, A.D. (2009) Forget Memory: Creating Better Lives for People with Dementia. Baltimore: Johns Hopkins University Press. Beard, R.L. (2004a) In their voices: identity preservation and experiences of Alzheimer’s disease, Journal of Aging Studies, 18, 4, 415–28. Beard, R.L. (2004b) Advocating voice: organisational, historical and social milieux of the Alzheimer’s disease movement, Sociology of Health & Illness, 26, 6, 797–819. Beard, R.L. and Estes, C. L. (2002) Medicalization of aging. In Ekerdt, D.J. (ed.) Macmillan Encyclopedia of Aging. London: Macmillan. Beard, R.L. and Fox, P.J. (2008) Resisting social disenfranchisement: negotiating collective identities and everyday life with memory loss, Social Science & Medicine, 66, 7, 1509–20. Beard, R.L., Knauss, J. and Moyer, D. (2009) Managing disability and enjoying life: how we reframe dementia through personal narratives, Journal of Aging Studies, 23, 4, 237–45. Behuniak, S.M. (2011) The living dead? The construction of people with Alzheimer’s disease as zombies, Ageing & Society, 31, 1, 70–92. Birenbaum, A. (1970) On managing courtesy stigma, Journal of Health and Social Behavior, 11, 3, 196–206. Birenbaum, A. (1992) Courtesy stigma revisited, Mental Retardation, 30, 5, 265–8. Blieszner, R. and Roberto, K.A. (2009) Care partner responses to the onset of mild cognitive impairment, The Gerontologist, 50, 1, 11–21. Bond, J. (1992) The medicalization of dementia, Journal of Aging Studies, 6, 4, 397–403. Bryden, C. (2005) Dancing with Dementia: My Story of Living Positively With Dementia. London: Jessica Kingsley. 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd 144 Renée L. Beard and Tara M. Neary Clare, L. (2002) We’ll fight it as long as we can: coping with the onset of Alzheimer’s disease, Aging & Mental Health, 6, 2, 139–48. Clare, L. (2003) Managing threats to self: awareness in early stage Alzheimer’s disease, Social Science & Medicine, 57, 6, 1017–29. Clare, L., Roth, I. and Pratt, R. (2005) Perceptions of change over time in ES Alzheimer’s Disease: implications for understanding awareness and coping style, Dementia: The International Journal of Social Research and Practice, 4, 4, 487–520. Cohen-Mansfield, J., Golander, H. and Arnheim, G. (2000) Self-identity in older persons suffering from dementia: preliminary results, Social Science & Medicine, 51, 3, 381–94. Conrad, P. (2007) The Medicalization of Society: On the Transformation of Human Conditions into Treatable Disorders. Baltimore: Johns Hopkins University Press. Corbin, J. and Strauss, A. (1998) Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. New York: Sage. Corner, L. and Bond, J. (2006) The impact of the label of mild cognitive impairment on individual’s sense of self, Philosophy, Psychiatry, and Psychology, 13, 1, 3–12. Daly, E., Zaitchik, D., Copeland, M., Schmahmann, J.D., et al. (2001) Clinical predictors of conversion to Alzheimer’s. In Vellas, B. and Fitten, L.J. (eds) Research and Practice in Alzheimer’s Disease. Vol 5. Paris: Springer. DeBaggio, T. (2007) When It Gets Dark: An Enlightened Reflection on Life with Alzheimer’s. New York: Free Press. Elias, M.F., Beiser, A. Wolf P.A., Au, R., et al. (2001) 22-years of prospective study of the preclinical phase of Alzheimer’s Disease: the Framingham Cohort. In Vellas, B. and Fitten, L.J. (eds) Research and Practice in Alzheimer’s Disease, Vol. 5. Paris: Springer. Estes, C.L. (1979) The Aging Enterprise: A Critical Examination of Social Policies and Services for the Aged. San Francisco: Jossey-Bass. Estes, C.L. and Binney, E. (1989) The biomedicalization of aging: dangers and dilemmas, The Gerontologist, 29, 5, 587–96. Estroff, S.E. (1989) Self, identity and subjective experiences of schizophrenia: in search of the subject, Schizophrenia Bulletin, 15, 2, 189–96. Fisher, L.S. (2007) Alzheimer’s Anthology of Unconditional Love: The 110,000 Missourians with Alzheimer’s. Columbia: L.S. Fisher. Foucault, M. (1973) The Birth of the Clinic: An Archeology of Medical Perception. London: Tavistock. Fox, P.J. (1989) From senility to Alzheimer’s disease: the rise of the Alzheimer’s disease movement, Milbank Quarterly, 67, 1, 58–102. Gaines, A.D. and Whitehouse, P.J. (2006) Building a mystery: Alzheimer’s disease, mild cognitive impairment, and beyond, Philosophy, Psychiatry, and Psychology, 13161–74. Garand, L., Dew, M.A., Eazor, L.R., DeKosky, S.T., et al. (2005) Caregiving burden and psychiatric morbidity in spouses with mild cognitive impairment, International Journal of Geriatric Psychiatry, 20, 6, 512–22. Garand, L., Dew, M.A., Urda, B., Lingler, J.H., et al. (2007) Marital quality in the context of mild cognitive impairment, Western Journal of Nursing Research, 29, 8, 976–92. Glaser, B.G. and Strauss, A.L. (1967) Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine de Gruyter. Goffman, E. (1974) Frame Analysis: an Essay on the Organization of Experience. New York: Harper Colophon. Goffman, E. (1963) Stigma: Notes on the Management of Spoiled Identity. Engelwood Cliffs: Prentice-Hall. Graham, J.E. and Ritchie, K. (2006) Mild cognitive impairment: ethical considerations for nosological flexibility in human kinds, Philosophy, Psychiatry, and Psychology, 13, 1, 31–43. Graham, J.E., Rockwood, K., Beattie, E.L., Eastwood, R., et al. (1997) Prevalence and severity of cognitive impairment with and without dementia in an elderly population, The Lancet, 349, 9068, 1793–6. 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd Sense-making in mild cognitive impairment experiences 145 Gray, D.E. (2002) ‘Everybody just freezes. Everybody is just embarrassed’: felt and enacted stigma among parents of children with high functioning autism, Sociology of Health & Illness, 24, 6, 734–49. Gubrium, J.F. (1986) Oldtimers and Alzheimer’s: The Descriptive Organization of Senility. London: JAI Press. Gullette, M.M. (2011) Agewise: Fighting the New Ageism in America. Chicago: University of Chicago Press. Harris, P.B. (2009) Intimacy, sexuality, and early-stage dementia: the changing marital relationship, Alzheimer’s Care Today, 19, 2, 63–77. Holst, G. and Hallberg, I.R. (2003) Exploring the meaning of everyday life for those suffering from dementia, American Journal of Alzheimer’s Disease and Other Dementias, 18, 6, 359–65. Holston, E.C. (2005) Stigmatization in Alzheimer’s disease research on African American elders, Issues in Mental Health Nursing, 26, 10, 1103–27. Jack, C.R. Jr, Albert, M.S., Knopman, D.S., McKhann, G.S., et al. (2011) Introduction to the recommendations from the National Institute on Aging and the Alzheimer’s Association Workgroups on diagnostic guidelines for Alzheimer’s Disease, Alzheimer’s & Dementia, 7, 3, 257–62. Jolley, D.J. and Benbow, S.M. (2000) Stigma and Alzheimer’s disease: causes, consequences and a constructive approach, International Journal of Clinical Practice, 54, 2, 117–9. Joosten-Weyn Banningh, L. J.-W., Vernooij-Dassen, M., Rikkert, M. O. and Teunisse, J.-P. (2008) Mild cognitive impairment: coping with an uncertain label, International Journal of Geriatric Psychiatry, 23, 2, 148–54. Kaufman, S.K., Shim, J.K. and Russ, A.J. (2004) Revisiting the biomedicalization of aging: clinical trends and ethical challenges, The Gerontologist, 44, 6, 731–8. Kaufman, S.R. (1994) The social construction of frailty: an anthropological perspective, Journal of Aging Studies, 8, 1, 45–58. Knauss, J. and Moyer, D. (2006) The role of advocacy in our adventure with Alzheimer’s, Dementia: The International Journal of Social Research and Practice, 5, 1, 67–72. Kral, V.A. (1962) Senescent forgetfulness: benign and malignant, Canadian Medical Association Journal, 86, 6, 256–70. Kramer, B.J. (1997) Differential predictors of strain and gain among husbands caring for wives with dementia, The Gerontologist, 37, 2, 239–49. Krasuski, J.S., Alexander, G.E., Horowitz, B., Daly, E.M., et al. (1998) Volume of medial temporal lobe structures in patients with Alzheimer’s disease and mild cognitive impairment (and in healthy controls), Biological Psychiatry, 43, 1, 60–8. Li, R. and Orleans, M. (2002) Personhood in a world of forgetfulness: an ethnography of the selfprocess among Alzheimer’s patients, Journal of Aging and Identity, 7, 4, 227–44. Lingler, J.H., Nightingale, M.C., Erlin, J.A., Kane, A.L., et al. (2006) Making sense of mild cognitive impairment: a qualitative exploration of the patient’s experience, The Gerontologist, 46, 6, 791–800. Link, B.G. and Phelan, J.C. (2001) Conceptualizing stigma, Annual Review of Sociology, 27, 363–85. Lyman, K. (1989) Bringing the social back in: a critique of the biomedicalization of dementia, The Gerontologist, 29, 5, 597–605. MacQuarrie, C.R. (2005) Experiences in early stage AD: Understanding the paradox of acceptance and denial, Aging and Mental Health, 9, 5, 430–41. MacRae, H. (1999) Managing courtesy stigma: the case of Alzheimer’s disease, Sociology of Health & Illness, 21, 1, 54–70. Petersen, R.C., Smith, G.E., Waring, S.C., Ivnik, R.J., et al. (1997) Aging, memory, and mild cognitive impairment, International Psychogeriatrics, 9, 1, 65–9. Petersen, R.J. (2004) Mild cognitive impairment as a diagnostic entity, Journal of Internal Medicine, 256, 183–94. Post, S.G. (1995) The Moral Challenge of Alzheimer’s Disease. Baltimore: Johns Hopkins University Press. 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd 146 Renée L. Beard and Tara M. Neary Post, S.G. (2000) Concepts of Alzheimer’s disease in a hypercognitive society. In Whitehouse, P., Maurer, K. and Ballenger, J.F. (eds) Concepts of Alzheimer’s Disease: Biological, Clinical and Cultural Perspectives. Baltimore: Johns Hopkins University Press. Purser, J.L., Fillenbaum, G.G. and Wallace, R.B. (2006) Memory complaint is not necessary for diagnosis of mild cognitive impairment and does not predict 10-year trajectories of functional disability, word recall, or short portable mental status questionnaire limitations, Journal of the American Geriatrics Society, 54, 2, 335–8. Ritchie, K. and Touchon, J. (2000) Mild cognitive impairment: conceptual basis and current nosological status, The Lancet, 355, 9199, 225–8. Roberts, J.L., Clare, L. and Woods, R.T. (2009) Subjective memory complaints and awareness of memory functioning in mild cognitive impairment: a systematic review, Dementia and Geriatric Cognitive Disorders, 28, 95–109. Sabat, S.R. (2001) The Experience of Alzheimer’s Disease: Life Through a Tangled Veil. Oxford: Blackwell. Sterin, G. (2002) Essay on a word: a lived experience of Alzheimer’s disease, Dementia: The International Journal of Social Research and Practice, 1, 1, 7–10. Taylor, R. (2006) Alzheimer’s from the Inside Out. Baltimore: Health Professions Press. Wadley, V.G. and Haley, W.E. (2001) Diagnostic attributions versus labeling: impact of Alzheimer’s Disease and major depression diagnoses on emotions, beliefs, and helping intentions of family members, Journal of Gerontology: Psychological Sciences, 56, 4, 244–52. Werezak, L. and Stewart, N. (2002) Learning to live with early dementia, Canadian Journal of Nursing Research, 34, 1, 67–85. Werner, P. and Heinik, J. (2008) Stigma by association and Alzheimer’s disease, Aging & Mental Health, 12, 1, 92–9. Whitehouse, P.J. and George, D. (2008) The Myth of Alzheimer’s: What You Aren’t Being Told About Today’s Most Dreaded Diagnosis. New York: St Martin’s Press. Whitehouse, P.J. and Moody, H.R. (2006) Mild cognitive impairment, Dementia: The International Journal of Social Research and Practice, 5, 1, 11–25. Whitehouse, P.J., Frisoni, G.B. and Post, S. (2004) Breaking the diagnosis of dementia, The Lancet Neurology, 3, 2, 124–8. Wilkinson, H., (ed.) (2001) The Perspectives of People with Dementia: Research Methods and Motivations. London: Jessica Kingsley. Winbald, B., Palmer, K., Kivipelto, M., Jelic, V., et al. (2004) Mild cognitive impairment: beyond controversies, towards a consensus: report to the International Working Groups on mild cognitive impairment, Journal of Internal Medicine, 256, 3, 240–6. World Health Organization (1993) International Statistical Classification of Diseases and Related Health Problems (ICD-10). Geneva: WHO. Zola, I.K. (1972) Medicine as an institution of social control, Sociological Review, 20, 4, 487–504. 2012 The Authors Sociology of Health & Illness 2012 Foundation for the Sociology of Health & Illness/Blackwell Publishing Ltd