Multiple Sclerosis
advertisement

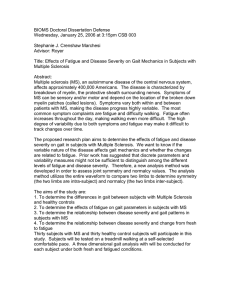
Multiple Sclerosis http://msj.sagepub.com/ Can aerobic treadmill training reduce the effort of walking and fatigue in people with multiple sclerosis: a pilot study M A Newman, H Dawes, M van den Berg, D T Wade, J Burridge and H Izadi Mult Scler 2007 13: 113 DOI: 10.1177/1352458506071169 The online version of this article can be found at: http://msj.sagepub.com/content/13/1/113 Published by: http://www.sagepublications.com Additional services and information for Multiple Sclerosis can be found at: Email Alerts: http://msj.sagepub.com/cgi/alerts Subscriptions: http://msj.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav Citations: http://msj.sagepub.com/content/13/1/113.refs.html Downloaded from msj.sagepub.com at UNIV OF DELAWARE LIB on February 4, 2011 ARTICLE Multiple Sclerosis 2007; 13: 113119 Can aerobic treadmill training reduce the effort of walking and fatigue in people with multiple sclerosis: a pilot study MA Newman1, H Dawes2, M van den Berg3, DT Wade4, J Burridge5 and H Izadi6 Impaired mobility in multiple sclerosis (MS) is associated with high-energy costs and effort when walking, gait abnormalities, poor endurance and fatigue. This repeated measures trial with blinded assessments investigated the effect of treadmill walking at an aerobic training intensity in 16 adults with MS. The intervention consisted of 12 sessions of up to 30 minutes treadmill training (TT), at 55 85% of age-predicted maximum heart rate. The primary outcome measure was walking effort, measured by oxygen consumption (mL/kg per metre), during treadmill walking at comfortable walking speed (CWS). Associated changes in gait parameters using the ‘Gait-Rite’ mat, 10-m time and 2-minute distance, and Fatigue Severity Scale were examined. Following training, oxygen consumption decreased at rest (P/0.008), CWS increased (P /0.002), and 10-m times (P/0.032) and walking endurance (P/0.020) increased. At increased CWS, oxygen consumption decreased (P/0.020), with a decreased time spent in stance in the weaker leg (P /0.034), and a greater stride distance with the stronger leg (P/0.044). Reported fatigue levels remained the same. Aerobic TT presents the opportunity to alter a motor skill and reduce the effort of walking, whilst addressing cardiovascular de-conditioning, thereby, potentially reducing effort and fatigue for some people with MS. Multiple Sclerosis 2007; 13: 113 119. http://msj.sagepub.com Key words: energy cost; gait; multiple sclerosis; oxygen consumption; treadmill training Introduction The performance of everyday movements, motor skills, appears to be influenced by the drive to minimize metabolic energy expenditure. This is observed during normal walking, with individuals selecting comfortable walking speeds (CWS) that coincide with the lowest energy (oxygen) cost on the oxygen cost-walking speed curve [1,2]. Gaits altered by disease are mainly linked to increased costs, fatigue and restricted capacity [1]. People with multiple sclerosis (MS) present with a range of symptoms, but reduced mobility and fatigue are key problems, with up to 85% of people with MS reporting difficulty walking [3,4]. In individuals with MS, walking effort as measured by oxygen cost (CW: mL/kg per metre), has been shown to be up to four times greater than in healthy individuals [5,6]. Even mildly-impaired people with MS are found to have sedentary lifestyles, low cardiovascular fitness and muscle characteristics typical of disuse [3,7 9]. These problems are likely to 1 Physiotherapy Research Unit, NOC NHS Trust, Oxford, OX3 7LD, UK Department of Clinical Neurology, University of Oxford Movement Science Group, School of Biological and Molecular Sciences, Oxford Brookes University, Headington, Oxford, OX3 0BP, UK 3 School of Health Sciences, University of Birmingham, Birmingham, B15 2TT, UK 4 Oxford Centre for Enablement, Windmill Road, Oxford, OX3 7LD, UK 5 School of Health Professions and Rehabilitation Sciences, University of Southampton, Southampton, SO17 1BJ, UK 6 Department of Mathematical Sciences, Oxford Brookes University, Oxford, OX33 1HX, UK Author for correspondence: Dr H Dawes, Senior Lecturer and Associate Research Fellow, Department of Clinical Neurology, Movement Science Group, School of Biological and Molecular Sciences, Oxford Brookes University; Headington, Oxford, OX3 0BP, UK. E-mail: hdawes@brookes.ac.uk Received 9 February 2006; accepted 30 May 2006 2 – 2007 SAGE Publications 10.1177/1352458506071169 Downloaded from msj.sagepub.com at UNIV OF DELAWARE LIB on February 4, 2011 114 MA Newman et al. increase the relative effort of energy expensive activities, such as walking, and compound limitations [1,3]. More recent evidence suggests that exercise, such as cycling, aquatic and strength training, may be helpful to individuals with MS [10 17]. Current consensus is that exercise does no harm and may benefit an individual’s fitness, well-being and strength, whilst reducing their pain and fatigue [10 17]. Treadmill training (TT) has provoked interest as an intervention for neurological conditions because it is a highly repetitive form of gait training that promotes both specific practice and use of systems concerned with walking [18], and can provide an aerobic training stimulus. Aerobic TT following stroke has been associated with improved walking speed, endurance and energy efficiency [19 22], and in a pilot RCT for people with MS, was well tolerated and improved walking speed without increasing fatigue [23]. Whether exercise can reduce the effort required to walk, as well as induce cardiovascular changes in people with MS, has not been established, although a single study that included four minimally-impaired people with MS reported no change in oxygen cost after hydrotherapy [24]. We set out to investigate whether four weeks of TT, which trains the motor skill of walking and is designed to improve aerobic fitness, could reduce the effort, as measured by oxygen consumption of walking CW: (mL/kg per metre), for people with MS with mild to moderate disability, and secondarily, to investigate the associated affects on temporo-spatial gait parameters, endurance and levels of fatigue. Methods and materials Ethical approval for this study was granted by the Local Applied Research and Ethics Committee. From March to June 2003, 19 participants were recruited in a non-consecutive manner, from a regional neurological rehabilitation centre, community physiotherapists, and the local MS Society. Participants were recruited if they had a confirmed diagnosis of MS and could walk 10 m (using aids if required) in B/60 seconds, could walk safely on the treadmill without support from a therapist or partial body weight support harness, and could follow any safety or training instructions. Participants were excluded if they had a MS exacerbation within the preceding eight weeks (determined by interview and medical note review) or had comorbidities, such as unstable cardiovascular disease, diabetes or lower limb arthritis, that might prevent them safely participating in aerobic TT. Procedures This was a prospective, single-centre trial, with a repeated measures design and blinded assessments. Prior to any testing, participants were asked to refrain from consumption of alcohol, cigarettes, food and caffeine, and to avoid strenuous exercise for 2 hours. After giving signed informed consent, each potential participant completed a screening assessment; details of medical history, therapy and exercise routines were taken, they were asked to identify their stronger leg and then completed the Guy’s Neurological Disability Scale (GNDS) and the Rivermead Mobility Index (RMI) to indicate levels of disability and functional mobility [25,26]. Those who fulfilled all of the selection criteria were recruited and then familiarized to all protocols. All participants were then assessed immediately prior to (baseline) and following the four-week training intervention. Expired air and heart rate (HR) were collected to describe energy demands at rest and when walking. Participants sat resting in a chair with arms while a HR chest strap transmitter (Polar-Vantage 2000) and facemask were applied. Expired air was gathered via light-weight respiratory valves and plastic hoses into a 100-L Douglas Bag for 6 minutes, and HR (beats/minute) was monitored every minute until the last minute when three records were made at 15, 30 and 45 seconds [27,28]. A submaximal treadmill test (Power jog 600) was then completed at a self-selected comfortable walking speed (CWS) for 4 minutes. To determine their CWS [29], individuals walked at a range of speeds with the treadmill display covered. To obtain steadystate conditions, participants walked for 3 minutes before expired air and HR were collected for the final minute [27]. For each test, gas analysers were calibrated, then the temperature and volume of expired air collected was measured using a dry gas meter (Harvard Apparatus Ltd, Edenbridge, UK) and gas compositions determined by oxygen and carbon dioxide analysers (Servomex 1400B4 O2/CO2 analyser, Crowborough, East Sussex, UK) with values expressed in standard conditions (standard correction for temperature, air pressure, humidity; STPD). From these, measures were made of minute ventilation: V̇E (L/min) at rest, the rate of oxygen used per unit of body weight over a given time at rest and when walking: V̇O2 (L/min, mL/kg per minute), of net (walking minus resting) V̇O2 (L/min, mL/kg per minute), and of the oxygen cost of walking or the net oxygen consumption per metre walked: Cw (mL/kg per metre) [1,2]. On re-assessment after training, physiological measures were completed again with one addition, a sub-maximal treadmill test completed at the Multiple Sclerosis 2007; 13: 113 119 Downloaded from msj.sagepub.com at UNIV OF DELAWARE LIB on February 4, 2011 http://msj.sagepub.com Treadmill training and the effect of walking and fatigue original CWS to permit direct comparison of effort of moving at the same speed. After a short rest, participants were asked to select their current CWS [29]. If the speed was different from their original CWS, participants then completed a second treadmill test at this new speed. At all assessments, fatigue levels were monitored using the Fatigue Severity Scale (FSS), and the 10-m timed walk and 2-minute walk evaluated walking speed and endurance [30,31]. Participants completed the FSS independently following a standardized explanation by the researcher [30]. The time taken to walk 10 m over a straight track, and the distance completed walking for 2 minutes around a shuttle corridor track were recorded [31]. During the first half of the 2-minute walk, participants walked over a thin pressure-sensitive mat (GAITRite, SMS) and the following gait parameters were recorded: cadence (steps/min), gait cycle (GC) time, duty factor (foot contact time, calculated as a percentage of time in swing and stance (%GC)), and stride length (cm) [32,33]. In all walking tests, participants were asked to walk at their usual CWS; testers walked behind to avoid pacing and walking aids were used if required [34]. All participants received 12 sessions of supervised TT in a physiotherapy gymnasium, for up to 30 minutes on each occasion. As maximal exercise testing was not practical, intensities were calculated using age predicted maximal heart rate (APMHR). Participants were encouraged to train above 55% APMHR, but prevented from training above 85% of APMHR [35]. Initial speed was based on baseline CWS, and during training, participants were allowed to rest when they wished, with a maximum of three rests before stopping. Speed was increased as directed by participants once they were able to walk for 30 minutes continuously. To monitor exercise intensity, HR, time, speed and ratings of perceived exertion using the CR10-RPE scale, were recorded [35]. Study sample characteristics were analysed using descriptive statistics. Before undertaking repeated measures analysis, one-tailed data was tested for normality. Parametric paired sample t -tests were used for measures of walking speed and endurance, and all other measures were analysed using Wilcoxon’s signed rank test. Scores from familiarization were not included in the analysis as this period was designed to decrease learning effects on the dependent variable, but the stability of measures was checked from familiarization to baseline. All pre-training measures were compared with all post-training measures. Data was analysed with SPSS version 11.0, using a significance level of P/0.05. http://msj.sagepub.com 115 Results Of the 19 participants, three dropped out for reasons unrelated to training or to their MS, leaving 16 to complete training (Table 1 provides demographic data). All but two participants used a walking aid, most used a single stick (43.7%). No participant received other physiotherapy during the study or in the four weeks before recruitment. Nine did no exercise, but three attended a weekly MS exercise class, two went swimming and two swam and visited the gymnasium weekly. None had used a treadmill in the past two years. During training, participants spent a mean 310 minutes (SD: 50.8, range: 207 360 minutes) walking on the treadmill. Of this time, a mean 180 minutes (SD: 104, range 2 330 minutes) or 58.5% of possible time was spent at aerobic intensities, as defined by 55 85% of APMHR. Over-ground speed and endurance improved significantly post-training. Mean 10-m time reduced from 15.6 seconds (SD: 5.6, range: 7.8 28.1 seconds) to 13.9 seconds (SD: 5.3, range: 7.5 27.0 seconds), P/0.016, and 2-minute walk distance increased from a mean 88.2 m (SD: 32.2, range: 44.6 154.0 m) to 94.3 m (SD: 32.2, range: 55.2 156.1 m), P/0.020. The median FSS score reduced from 30 points (IQR: 22 37) to 27.5 points (IQR: 12 32), but this change was not significant (P/ 0.178). Physiological measures All metabolic and HR measures (resting and walking), from familiarization to baseline, were checked for stability and no differences were found (P / 0.05). Pre- and post-training measures are presented in Table 2. Expired air measures for one participant at baseline were discarded due to a bag leak, and one participant was unable to complete the second treadmill test post-training, reducing sample sizes. At baseline, a significant decrease in oxygen consumption (mL/kg per minute) and minute ventilation (L/min) was observed at rest without a Table 1 Participants (n/16; 13 female and three male) demographic and disability measures Mean9/SD Age (years) 53.69/8.67 Time since first symptoms 17.39/8.3 (years) Height (cm) 168.29/9.49 GDNS (0 55) RMI (0 15)** Range 30 65 7 37 Median 54.5 16 154 185 167.2 7 19 13 7 14 12 GNDS, Guy’s Neurological Disability Scale; RMI, Rivermead Mobility Index. Multiple Sclerosis 2007; 13: 113 119 Downloaded from msj.sagepub.com at UNIV OF DELAWARE LIB on February 4, 2011 116 MA Newman et al. Table 2 Oxygen costs, oxygen consumption and heart rate pre- and post-training n At rest Weight (kg) RER /V̇O2 (mL/kg per minute) /V̇E (L/min) HR (bpm) Walking: original CWS Gross V̇O2 (mL/kg per minute) Nett V̇O2 (mL/kg per minute) Cw (mL/kg per metre) HR (bpm) Walking: new CWS Cw (mL/kg per minute) Pre-training mean9/SD (range) Post-training mean9/SD (range) 95% Confidence P value interval Difference 16 70.889/13.30 (47.80 92.10) 70.589/12.82 (48.60 91.60) /0.39/1.22 0.969/0.07 (0.85 1.15) 0.009/0.09 15 0.969/0.09 (0.79 1.20) 15 2.109/0.58 (1.19 3.03) 1.549/0.85 (0.58 3.89) /0.539/4.80 0.34 0.89 0.01 15 16 5.699/1.29 (3.40 7.79) 749/8 (59 84) 4.619/1.74 (1.69 8.40) 719/10 (55 85) /1.089/1.47 /2.399/4.80 0.01 0.06 /0.3 to 1.9 15 6.309/2.01 (3.66 10.14) 4.979/2.17 (1.94 11.38) /1.319/1.96 0.03 /0.1 to /2.5 15 4.209/1.99 (1.15 7.11) 3.439/2.03 (1.36 9.79) /-0.789/2.08 0.21 /0.2 to /0.9 15 0.3009/0.215 (0.10 0.79) 16 919/11 (72 107) 0.2619/0.183 (0.05 0.75) 869/12 (68 110) /0.0449/0.131 0.23 /5.39/6.6 0.01 /1.5 to /9.1 14 0.3009/0.215 (0.10 0.79) 0.1479/0.831 (0.02/0.29) /0.0959/0.133 0.02 0.0 to /0.2 Gross oxygen consumption: V̇O2 (mL/kg per minute); Nett (walking resting) oxygen consumption: V̇O2 (mL/kg per minute). Oxygen cost of walking: nett oxygen consumption per metre walked: Cw (mL/kg per metre). Wilcoxon’s signed rank test, P/0.05 significance level. Discussion We observed that four-weeks of aerobic TT resulted in a reduction in resting metabolism, an increase in walking endurance, a more normal temporo-spatial gait pattern, increased self-selected walking speed and a decrease in walking effort. Self-reported fatigue was not significantly different. Training appears to have benefited individuals by making walking less energy expensive, as a result of both lower resting metabolism and an ability to achieve faster walking speeds. Even small savings in energy for those with more restricted mobility could be functionally important, eg, allowing activity for a longer. In summary, our findings suggest that aerobic TT could improve the motor skill of walking and address cardiovascular de-conditioning, thereby potentially reducing effort and fatigue for some people with MS. The significant improvement in walking speed agrees with the findings of increased speed and Oxygen Cost of Walking Self - Selected Speed 1.0 Oxygen Cost (ml/kg/m) significant change in resting HR. When walking at original CWS, gross oxygen consumption (mL/kg per minute) also decreased significantly. However, when resting values of oxygen consumption were considered (walking resting oxygen consumption), no change in nett oxygen consumption (mL/kg per minute) was noted. The mean pre-training original CWS was 0.62 mph (SD: 0.31, range: 0.3 1.30 mph). After training, the new self-selected CWS was significantly faster (P/0.002) at a mean 1.05 mph (SD: 0.45, range: 0.50 2.10 mph). There was no change in oxygen cost (mL/kg per minute) at original CWS, but a reduction at the new CWS (P /0.019); Figure 1 shows the CW (mL/kg per minute) pre- and post-training in relation to comfortable walking speed and movement of individual participants along the oxygen cost-walking speed curve. Table 3 shows the results of the gait parameters examined, with significant differences seen in all measures except cadence, duty factor as represented by swing and stance of the stronger leg, and stride length of the weaker leg. Pre and Post Training .8 .6 .4 .2 0.0 0.0 .2 .4 .6 .8 1.0 Speed m/sec Pre training Post training Figure 1 Oxygen costs walking at self-selected CWS preand post-training. Multiple Sclerosis 2007; 13: 113 119 Downloaded from msj.sagepub.com at UNIV OF DELAWARE LIB on February 4, 2011 http://msj.sagepub.com Treadmill training and the effect of walking and fatigue 117 Table 3 Temporal-spatial gait parameters pre/post-training Gait measure Pre-training mean9/SD (range) Post-training mean9/SD (range) P value Duty factor % Time in swing (wk) % Time in stance (wk) % Time in swing (st) % Time in stance (st) Stride length (str) Stride length (wk) Cadence 339/9.3 (1.7 42.7) 679/9.3 (57.3 98.3) 33.59/5.1 (25.9 46.1) 66.59/5.1 (53.9 74.1) 98.79/21 (65.5 135.0) 98.69/21.9 (62 136) 929/21 (63 132) 369/4.5 (26.7 41.7) 63.89/4.5 (58.3 73.4) 33.39/7.1 (12.2 42.6) 66.69/7.1 (57.4 87.7) 104.09/21 (75.4 146.0) 103.29/21.5 (74.7 143.8) 919/17 (62 119) 0.03 0.03 0.90 0.10 0.04 0.06 0.76 endurance following TT after stroke [18 22], and demonstrates a transfer of the training on a treadmill to improvements in over ground walking performance. Faster walking and increased endurance are certainly clinically relevant, being associated with increased function and independence. Improvements in endurance were relatively greater, probably reflecting our training emphasis on walking for 30 minutes. Even though the training protocol did not emphasize speed, mean 10-m times reduced by 12%, a level equal to the reduction in mean 7.62 m walk time observed by Rhomberg et al . [16], after six months aquatic and strengthening exercise. As TT achieved this improvement after only one month it may be that TT, being more task specific, prompted more rapid changes. Further ongoing investigations are needed to clarify optimal training protocols. TT regimes emphasizing speed following stroke have reported particular improvements, but the suitability of these for people with MS is uncertain. Fatigue levels remained unchanged in common with other research into exercise and MS [11 15], and suggest the training regime was well tolerated. The small, but statistically significant, reductions in ventilation [/V̇E (L/min)] and gross oxygen consumption [/V̇O2 (mL/kg per minute)] at rest is an intriguing and potentially important finding, with implications for overall fatigue levels in this group. With resting metabolic rate normally constant, significant reduction post-training of such a short duration was unexpected from the literature. Ongoing test familiarization is a possible extraneous factor that may have shown such an effect, although with pre-training values in V̇E and V̇O2 not significantly changing from familiarization to baseline testing, ongoing familiarization changes are unlikely. Examining oxygen cost when individuals were walking at post-training, self-selected speeds showed significant reductions in walking effort, even when resting changes were considered. When individuals were made to walk at their pretraining self-selected speed, there was no reduction in walking effort after training. Reductions in oxygen cost were linked to participants walking http://msj.sagepub.com faster in a more optimal (lower oxygen cost) part of the oxygen cost-walking speed curve, as CWS was significantly faster post-training at a mean of 0.43 mph (Figure 1). Individuals were able to walk faster and further after training, with no increases in fatigue associated with this increased activity. Our findings agree with observations in chronic stroke patients with aerobic TT reducing sub-maximal oxygen consumption [19]. Although our sample was small and the evidence from a repeated measures analysis is less powerful than that of a RCT, this study of 16 participants is larger than any other investigations about the impact of exercise on CW in MS identified in the literature [24]. We also recruited a sample of participants that were on average older at 53.6 years and reported symptoms longer at 17.3 years compared to Romberg et al . (43.8 and 9.7 years) and other studies about exercise and MS [10 17]. Although no systematic analysis was made, higher mean age and disease duration per se did not appear to be barriers to exercise, supporting proposals that exercise is also useful for older adults with MS [36]. A convenience sample was used, necessarily as participants needed to be able to walk on a treadmill, but as such it may be unrepresentative of other MS populations, eg, perhaps participants were more motivated to exercise. However, no participant reported changing their exercise routine or receiving any therapy during the study. The outcome measures that were used have been demonstrated to be reliable and were applied in the standardized format, but no investigation of inter-rater reliability was made. Further work would ideally use consecutive sampling and establish inter-rater reliability. We did not measure actual mobility at home or in the community, and the impact of TT on daily life requires further investigation. Participants spent a mean 58% of time training above aerobic thresholds, but their ability to achieve these intensities varied widely. For some, weakness and peripheral muscle fatigue may have limited training before demand reached aerobic levels, for others the training duration may have been insufficient. A larger trial with a sample stratified by mobility level could evaluate these aspects. Additionally, the Multiple Sclerosis 2007; 13: 113 119 Downloaded from msj.sagepub.com at UNIV OF DELAWARE LIB on February 4, 2011 118 MA Newman et al. presence of a physiotherapist and monitoring during training may have increased confidence and motivation to exercise. This could particularly influence factors, such as fatigue, that have links to mood. Conclusions We found the exercise programme feasible and well-tolerated in people with mild to moderate MS. Such a programme is practical and could be easily implemented in community fitness centres where treadmills are freely available. Further investigation of optimal prescription and implementation in a more representative sample is warranted. Acknowledgements The authors would like to thank the Oxford Centre for Enablement staff, the patients who volunteered to take part in the study, and the Oxford MS group. References 1. Waters RL, Mulroy S. The energy expenditure of normal and pathologic gait. Gait Posture 1999; 9: 207 31. 2. Rose J, Ralston H, Gamble J. Energetics of walking. In Human walking . Williams & Wilkins, 1994: 45 72. 3. White LJ, Dressendorfer RH. Exercise and multiple sclerosis. Sports Med 2004; 34: 1077 100. 4. Morris ME, Vowels L, Dodd K. Changes in gait and fatigue from morning to afternoon in people with multiple sclerosis. J Neurol Neurosurg Psychiatry 2002; 72: 361 65. 5. Olgiati R, Burgunder JM, Mumenthaler M. Increased energy cost of walking in multiple sclerosis: effect of spasticity, ataxia, and weakness. Arch Phys Med Rehabil 1988; 69: 846 49. 6. Olgiati R, Jacquet J, Di Prampero PE. Energy cost of walking and exertional dyspnea in multiple sclerosis. Am Rev Respir Dis 1986; 134: 1005 10. 7. Ng AV, Miller RG, KentBraun JA. Central motor drive is increased during voluntary muscle contractions in multiple sclerosis. Muscle Nerve 1997; 20: 1213 18. 8. KentBraun JA, Ng AV, Castro M, Weiner MW, Gelinas D, Dudley GA et al . Strength, skeletal muscle composition, and enzyme activity in multiple sclerosis. J Appl Physiol 1997; 83: 1998 2004. 9. Tantucci C, Massucci M, Piperno R, Grassi V, Sorbini C. Energy cost of exercise in multiple sclerosis patients with a low degree of disability. Mult Scler 1996; 2: 161 67. 10. Gehlsen G, Assmann N, Winant D, Seidle M. Gait characteristics in multiple sclerosis: progressive changes and effects of exercise on parameters. Arch Phys Med Rehabil 1986; 67: 536 39. 11. Petajan JH, Gappmaier E, White AT, Spencer MK, Mino L, Hicks RW et al . Impact of aerobic training on fitness and quality of life in multiple sclerosis. Ann Neurol 1996; 39: 432 41. 12. Mostert S, Kesselring J. Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Mult Scler 2002; 8: 161 68. 13. Rodgers MM, Mulcare JA, King DL, Mathews T, Gupta SC, Glaser RM et al . Gait characteristics of individuals with multiple sclerosis before and after a 6-month aerobic training program. J Rehabil Res Dev 1999; 36: 183 88. 14. Sutherland G, Andersen MB. Exercise and multiple sclerosis: physiological, psychological, and quality of life issues. J Sports Med Phys Fit 2001; 41: 421 32. 15. Surakka J, Romberg A, Ruutiainen J, Surakka J, Aunola S, Karppi SL et al . Effects of aerobic and strength exercise on motor fatigue in men and women with multiple sclerosis: a randomized controlled trial. Clin Rehabil 2004; 18: 737 46. 16. Romberg A, Virtanen A, Ruutiainen J, Aunola J, Karppi S, Vaara SL et al . Effects of a 6-month exercise program on patients with multiple sclerosis a randomized study. Neurology 2004; 63: 2034 38. 17. Gehlsen G, Grigsby S, Winant D. Effects of an aquatic fitness program on the muscular strength and endurance of patients with multiple sclerosis. Phys Ther 1984; 64: 653 57. 18. Manning CD, Pomeroy VM. Effectiveness of treadmill retraining on gait of hemiparetic stroke patients. Systematic review of current evidence. Physiotherapy 2003; 89: 337 49. 19. Macko RF, Smith GV, Dobrovolny CL, Sorkin JO, Goldberg AP, Silver KH et al . Treadmill training improves fitness reserve in chronic stroke patients. Arch Phys Med Rehabil 2001; 82: 879 84. 20. Pohl M, Mehrholz J, Ritschel C, Rückriem S. Speeddependent treadmill training in ambulatory hemiparetic stroke patients: a randomized controlled trial. Stroke 2002; 33: 553 58. 21. Visintin M, Barbeau H, Korner-Bitensky N, Mayo NE. A new approach to retrain gait in stroke patients through body weight support and treadmill stimulation. Stroke 1998; 29: 1122 28. 22. Sullivan KJ, Knowlton BJ, Dobkin BH. Step training with body weight support: effect of treadmill speed and practice paradigms on poststroke locomotor recovery. Arch Phys Med Rehabil 2002; 83: 683 91. 23. Van den Berg M, Dawes H, Wade DT, Newman M, Burridge J, Izadi H. Treadmill training for people with multiple sclerosis; a pilot randomised trial. J Neurol Neurosurg Psychiatry 2006; 77: 531 533. 24. Zamparo P, Pagliaro P. The energy cost of level walking before and after hydro-kinesi therapy in patients with spastic paresis. Scand J Med Sci Sports 1998; 8: 222 28. 25. Rossier P, Wade DT. The Guy’s Neurological Disability Scale in patients with multiple sclerosis: a clinical evaluation of its reliability and validity. Clin Rehabil 2002; 16: 75. 26. Vaney C. Assessing mobility in multiple sclerosis using the Rivermead Mobility Index and gait speed. Clin Rehabil 1996; 10: 216 26. 27. Linnarsson DE, Mattsson L, Eklof, Broman L, Broman M, Brostrom LA et al . Determination of the oxygen cost of level walking. Clin Physiol 1989; 9: 1 10. 28. Waters RL, Lunsford BR, Perry J, Byrd R. Energyspeed relationship of walking: standard tables. J Orthop Res 1988; 6: 215 22. 29. Holt KG, Hamill J, Andres RO. Predicting the minimal energy costs of human walking. Med Sci Sports Exer 1991; 23: 491 98. Multiple Sclerosis 2007; 13: 113 119 Downloaded from msj.sagepub.com at UNIV OF DELAWARE LIB on February 4, 2011 http://msj.sagepub.com Treadmill training and the effect of walking and fatigue 30. Rossier P, Wade DT. Validity and reliability comparison of 4 mobility measures in patients presenting with neurologic impairment. Arch Phys Med Rehabil 2001; 82: 9 13. 31. Krupp LB, La Rocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 1989; 46: 1121 23. 32. Menz HB, Latt MD, Tiedemann A, Mun San Kwan M and Lord SR. Reliability of the GAITRite walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait Posture 2004; 20: 20 25. 33. McDonough AL, Batavia M, Chen FC, Kwon S and Ziai J. The validity and reliability of the GAITRite http://msj.sagepub.com 119 system’s measurements: a preliminary evaluation. Arch Phys Med Rehabil 2001; 82: 419 25. 34. Guyatt GH, Pugsley SO, Sullivan MJ, Thompson P, Berman LB, Jones NL et al . Effect of encouragement on walking test performance. Thorax 1984; 39: 818 22. 35. American College of Sports Medicine. Guidelines for graded exercise testing and training. In Franklin BA, Whaley MH, Howley ET eds. ACSM’s guidelines for exercise testing and prescription , sixth edition. Lippincott Williams & Wilkins, 2002: 368. 36. Eldar R, Marincek C. Physical activity for elderly persons with neurological impairment: a review. Scand J Rehabil Med 2000; 32: 99 103. Multiple Sclerosis 2007; 13: 113 119 Downloaded from msj.sagepub.com at UNIV OF DELAWARE LIB on February 4, 2011