Review into the Quality of Care & Treatment provided by
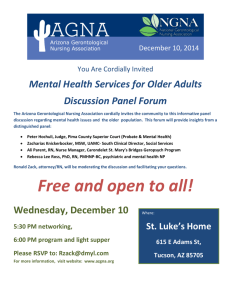
advertisement

United Lincolnshire Hospitals NHS Trust Review into the Quality of Care & Treatment provided by 14 Hospital Trusts in England RAPID RESPONSIVE REVIEW REPORT FOR RISK SUMMIT June 2013 Contents 1. Introduction 3 2. Background to the Trust 7 3. Key Lines of Enquiry 16 4. Findings 18 5. Governance and leadership 22 Clinical and operational effectiveness 30 Patient experience 35 Workforce 40 Safety 48 General Medicine and Elderly Care 52 Urgent Care 56 Obstetrics 61 Critical Care and Surgery 65 Conclusions and support required Appendices Appendix I: Appendix VI: Information available to the RRR panel 81 Appendix VII: Unannounced site visit 84 70 73 SHMI and HSMR definitions 74 Appendix II: Panel Composition 76 Appendix III: 77 Interviews held on announced visit Appendix IV: Observations undertaken 78 Appendix V: 80 Focus groups held 2 1. Introduction Overview of review process On 6th February the Prime Minister asked Professor Sir Bruce Keogh, NHS England Medical Director, to review the quality of the care and treatment being provided by those hospital trusts in England that have been persistent outliers on mortality statistics. The 14 NHS trusts which fall within the scope of this review were selected on the basis that they have been outliers for the last two consecutive years on either the Summary Hospital level Mortality Indicator (SHMI) or the Hospital Standardised Mortality Ratio (HSMR). Definitions of SHMI and HSMR are included at Appendix I. These two measures are intended to be used in the context of this review as a ‘smoke alarm’ for identifying potential problems affecting the quality of patient care and treatment at the trusts which warrant further review. It was intended that these measures should not be reviewed in isolation and no judgements were made at the start of the review about the actual quality of care being provided to patients at the trusts. Key principles of the review The review process applied to all 14 NHS trusts was designed to embed the following principles: 1) Patient and public participation – these individuals have a key role and worked in partnership with clinicians on the reviewing panel. The panel sought the views of the patients in each of the hospitals and also considered independent feedback from stakeholders, related to the Trust, which had been received through the Keogh review website. These themes have been reflected in the reports. 2) Listening to the views of staff – staff were supported to provide frank and honest opinions about the quality of care provided to hospital patients. 3) Openness and transparency – all possible information and intelligence relating to the review and individual investigations will be publicly available. 4) Cooperation between organisations – each review was built around strong cooperation between different organisations that make up the health system, placing the interest of patients first at all times. Terms of reference of the review The review process was designed by a team of clinicians and other key stakeholders identified by NHS England, based on the NHS National Quality Board guidance on rapid responsive reviews and risk summits. The process was designed to: Determine whether there are any sustained failings in the quality of care and treatment being provided to patients at these Trusts. Identify: i. Whether existing action by these Trusts to improve quality is adequate and whether any additional steps should be taken. ii. Any additional external support that should be made available to these Trusts to help them improve. iii. Any areas that may require regulatory action in order to protect patients. 3 The review follows a three stage process: Stage 1 – Information gathering and analysis This stage used information and data held across the NHS and other public bodies to prepare analysis in relation to clinical quality and outcomes as well as patient and staff views and feedback. The indicators for each trust were compared to appropriate benchmarks to identify any outliers for further investigation in the rapid responsive review stage as Key Lines of Enquiry (KLOEs). The data pack for each trust reviewed is published at http://www.nhs.uk/NHSEngland/bruce-keogh-review/Documents/trust-datapacks/ulh-data-packs.pdf Stage 2 – Rapid Responsive Review (RRR) A team of experienced clinicians, patients, managers and regulators (see Appendix II for panel composition), following training, visited each of the 14 hospitals and observed the hospital in action. This involved walking the wards and departments, interviewing patients, trainees, staff and members of the Board. The report from this stage was considered at the risk summit. Stage 3 – Risk summit This brought together a separate group of experts from across health organisations, including the regulatory bodies. They considered the report from the RRR, alongside other hard and soft intelligence, in order to make judgements about the quality of care being provided and agree any necessary actions, including offers of support to the hospitals concerned. A report following each risk summit has been made publically available. Methods of investigation The three day announced RRR visit took place at the Trust’s three acute sites: Grantham Hospital, Lincoln County Hospital and Pilgrim Hospital Boston on Monday 17 June, Tuesday 18 June and Wednesday 19 June 2013. A variety of review methods were used to investigate the KLOEs and enable the panel to consider evidence from multiple sources in making their judgements. The visit included the following methods of investigation: Interviews Nine interviews took place with members of the Board and selected members of staff based on the key lines of enquiry during the visits. See Appendix III for details of the interviews undertaken. Observations Ward observations enabled the panel to see the Trust undergo its day to day operations. They allowed the panel to talk to current patients, and their families where observations took place during visiting hours. They allowed the panel to speak with a range of staff and observe the quality of care and treatment being provided to patients. The panel was able to observe the action by the Trust to improve quality in practice and consider whether any additional steps should be taken. 4 Observations took place in sixty one areas of The Trust split across the three hospitals; Grantham Hospital, Lincoln County Hospital and Pilgrim Hospital, Boston. See Appendix IV for details of the observations undertaken. Focus Groups Focus groups provided an opportunity to talk to staff groups individually to ask each area of staff what they feel is good about patient care in the Trust and what needs improving. They enabled staff to speak up if they felt there was a barrier that was preventing them from providing good quality care to patients and what actions might the Trust need to consider improving, including addressing areas with higher than expected mortality indicators. Focus groups were held with seven staff groups during the announced site visit, with mixed groups being held across the three main hospital sites. See Appendix IV for details of the focus groups held. The panel would like to thank all those attending the focus groups who were open with the sharing of their experiences and balanced in their perceptions of the quality of care and treatment at the Trust. Listening events Public listening events give the public an opportunity to share their personal experiences with the hospital, and to voice their opinion on what they feel works well or needs improving at the Trust in relation to the quality of patient care and treatment. A listening event for the public and patients was held on the evening of 17 June 2013 at The White Hart Hotel in Lincoln and on the evening of 18 June 2013 at The White Hart Hotel in Boston. These were open events, publicised locally, and attended by c.65 members of the public and patients at each event. The panel would like to thank all those attending the listening event who were open in sharing of their experiences and balanced in their perceptions of the quality of care and treatment at the Trust. We would also like to express our thanks to those families and patients who have contacted us through the patient voice website or through ‘Cure the NHS Lincolnshire’. The panel has considered each story in detail and whilst we cannot respond to individual complaints we want you to know that the panel will take on board your comments as part of the review. Review of documentation A number of documents were provided to the panellists at the Trust during the site visit. Whilst not every document was reviewed in detail, they were available to the panellists to validate findings as considered appropriate. See Appendix VI for details of the documents available to the panel Unannounced visit The unannounced out-of-hours visit took place at Lincoln County Hospital and Pilgrim Hospital, Boston on the evening of Thursday 19 June 2013. This focused observations in areas identified from the announced site visit, see Appendix VII. 5 Next steps This report has been produced by Dr Ruth May, Panel Chair, with the full support and input of panel members. It has been shared with the Trust for a factual accuracy check. This report was issued to attendees at the risk summit, which focussed on supporting United Lincolnshire Hospitals NHS Trust (“the Trust”) in addressing the actions identified to improve the quality of care and treatment. Following the risk summit the agreed action plan will be published alongside this report on the Keogh review website. A report summarising the findings and actions arising from the 14 investigations will also be published. 6 2. Background to the Trust This section of the report provides relevant background information for the Trust and highlights the areas identified from the data pack for further investigation. Context United Lincolnshire Hospitals NHS Trust is the principal acute provider of healthcare across the three main hospital sites (Boston, Grantham and Lincoln) for the residents of Lincolnshire. The Trust also provides a number of services within smaller community hospitals (at Louth, Gainsborough, Skegness and Spalding) owned by other organisations. Lincolnshire’s resident population of 700,000 exceeds the Royal College of Surgeons preferred catchment population for an acute general hospital providing a full range of facilities. Lincolnshire is the second largest county in England (2700 square miles), and the Trust provides its services across its three main sites. Transport and road links between the sites are poorly developed compared with many other parts of England, with travelling time between sites of 50 minutes to one hour. To maintain local access the Trust replicates service provision across the county. The Trust and wider health community has recognised the future challenges to sustaining the current service configuration across all services in Lincolnshire, including acute provision. The whole health and social care community is committed to a sustainability review for Lincolnshire. The Trust provides a full range of District General Hospital (DGH) based services with General Medicine and General Surgery being the largest inpatient specialties; and Ophthalmology being the largest for outpatients. Lincoln County is unusual in that it is a DGH providing Radiotherapy Services, normally a tertiary centre function. In 2012 the Trust had 657,315 outpatient’s attendances and 157,391 inpatient attendances. The day case rate over the same period was 82%, that is, patients entering and leaving hospital on the same day. With a total of 1,079 beds it has a market share of 78% for inpatient activity within a 5 mile radius of the Trust sites. The market share falls to 74% within a 10 mile radius and 49% at a 20 miles radius. In the three localities covered by the Trust, 2.4% of Lincolnshire’s population belong to non-white ethnic minorities. The Trust’s HSMR level has been above the expected level for the last 2 years and the Trust was therefore selected for this review. The health profile of the area is generally similar to that of England’s average with some areas that are worse than the national average with several indicators that fall lower than what would be expected. The Trust covers seven district/borough council areas: Boston, East Lindsey, West Lindsey, North Kesteven, South Kesteven, South Holland, the City of Lincoln Council; and one County Council: Lincolnshire. The following matters are pertinent to this review: Long term unemployment in Lincoln is higher than the national average but both Boston and South Kesteven show above average employment 7 The levels of deprivation in Lincoln are worse than the national average together with the proportion of children in poverty in Lincoln being greater than the national average. Both Boston and South Kesteven perform more favourably on these metrics Smoking during pregnancy throughout the county is worse than England’s national average Teenage pregnancy levels (under 18) in Lincoln and Boston are significantly greater than the English national average, although for South Kesteven a lower than average prevalence is noted Alcohol specific hospital stays are significantly greater than the average in Lincoln and Boston although below average for South Kesteven Rates of smoking in adults is above the national average The number of physically active adults is below the national average Hospital stays for self harm are significantly higher in Lincoln than the national average but fall within the national average for Boston and South Kesteven Lincoln and Boston also witnesses a much higher level of drug misuse incidents than the national average Life expectancy for male and females is lower than the national average in Lincoln and Boston with the respective figures Population data indicate that early deaths related to cancer are higher in Lincoln than the national average Population data indicate that early deaths related to heart diseases are also higher in the trust, specifically, Boston and Lincoln Acute sexually transmitted infections are significantly greater in Lincoln than the national average The health profile for the Trust is complex, with some areas being more deprived than others and some facing greater health challenges than others for specific diseases as articulated above. The variety of health needs of the population it serves poses a significant challenge for this Trust. Key messages from the Trust data pack Mortality indicators The Trust has an overall HSMR higher than expected for the past two years; with scores of 113 and 111 for the FY 2011 and FY 2012 respectively; the number of actual deaths in the hospitals within the trust is higher than the expected level and above the statistically expected range. Further analysis of this demonstrates that non-elective admissions are the primary contributing factor to this figure. Elective admissions are within the expected range, with an HSMR of 80. 8 The official SHMI was within the expected range at 110 for the period October 2011 to September 2012 and therefore as the Trust was not an outlier for SHMI for two consecutive periods, it was not selected for review on the basis of its SHMI. It was noted that the Trust has a SHMI of 109 (December 2011 to November 2012), which is statistically above the expected range. There is variation between SHMI and HSMR data across the three sites at which the Trust provides services. Similar to the HSMR, non-elective admissions are seen to be contributing primarily to the overall Trust SHMI. The Trust had nine high mortality alerts for diagnostic groups since 2007 and five requests for investigation relating to mortality from the CQC since 2009. The Trust has provided full responses to each of these and no further action has been required by the CQC. In depth reviews of the Trust by CQC have revealed the following areas as common themes of concern: Fluid balance monitoring Delays in implementing treatment plans Clinical documentation issues Delays in implementation of the Liverpool Care Pathway Failure to escalate the deteriorating patient Risk of falling during stays in hospital Senior review, particularly post operatively Together with the Care Quality Commission (CQC) Healthcare Evaluation Data (HED), Health and Social Care Information Centre and Dr Foster reviews have notified the following 8 mortality indicators out of 13 used nationally, as outside the expected ranges: Overall HSMR Emergency specialty groups much worse than expected (CQC) Emergency specialty groups worse than expected (CQC) Diagnosis group alerts to CQC Diagnosis group alerts followed up by CQC 9 Non-elective mortality (SHMI and HSMR) 30 day mortality following specific surgery / admissions Mortality among patients with diabetes Diagnosis coding depth has an impact on the expected number of deaths. A higher than average diagnosis coding depth is more likely to collect co-morbidity which will influence the expected mortality calculation. For The Trust, it is apparent that for elective admissions, the Trust has been consistently performing below the national average for coding depth. The average diagnosis coding depth for non-elective admissions has also been close to the national average and the most recent quarter shows the trust is above the national average. The Trust make below average use of palliative care coding on admission (using diagnosis codes rather than treatment speciality). This may impact on the mortality indicators. Leadership and governance The Trust has had 9 CEOs in 11 years and has consistently experienced major turnover of directors during this time. In addition to existing substantive directors (Chief Executive, Deputy Chief Executive, Director of Operations) the current Board is also composed of 2 interim directors: the Director of Nursing and the Director of Facilities as well as an Acting Director of Finance. The current Medical Director is working on a part time basis. There is a new Director of HR/Organisational Development who is shared with another local provider. New substantive Medical, Nursing and Facilities Directors have recently been appointed but have not yet commenced in post. The Board also consists of a Chairman and 5 non executives. Two additional non-executives are in the recruitment process. The Governance Committee, a sub-committee of the Board that provides assurance on quality governance is chaired by a Non Executive Director. The Quality & Safety Committee reports to the Governance Committee and is chaired by the Medical Director. Since the departure of the last Medical Director, this has been chaired by a senior member of his team. The Trust set up the pan-Trust Mortality Reduction Board in 2010. In 2012, this was further supported by a new system at site level; site-based mortality reduction committees at main hospital sites, which report into the pan-Trust Mortality Reduction Board. The current Director of Nursing is an interim member of the executive team and the Trust has recently appointed a new Director of Nursing from within the Trust patient services team. Recent reviews by the CQC identified minor concerns in relation to two outcomes: staffing, and the care and welfare of people who use services. This represents a significant improvement on the Trust’s CQC inspections in prior years, which had identified a number of major concerns. The Trust is not currently a Foundation Trust, however in December 2012 the Board conducted a self-assessment of its performance against Monitor quality governance framework. The Board self assessed a score of 14.0 (aspirant trusts must receive a score of 3.5 or lower to be authorised as a foundation trust). This score included two ‘reds’ (indicators of major concern) and did not meet expectation in the following areas: ‘Is the Board sufficiently aware of potential risks to quality?’ ‘Are there clearly defined, well understood processes for escalating and resolving issues and for managing quality performance?’ 10 An independent assessment in March 2013 scored the Trust as 9.5, with an improvement in the area ‘Are there clearly defined, well understood processes for escalating and resolving issues and for managing quality performance?’ The Trust continues to undertake actions to improve its quality governance performance although the panel found little evidence that some of these matters had been addressed. Key self identified risks for the Trust relate to service provision, demand and sustainability, mortality, progress reliability, staffing and skills, lack of whole system provision, patient records and culture. In 2012/13, the Trust achieved cost improvement savings of £14.5m. The Trust plans to save £22.4 million in 2013/14 through cost improvement programmes (CIPs). £20.4 million has been identified as per submission to the Trust Development Authority (TDA) on 24 May 2013. The Trust currently has an ‘amber’ Monitor governance risk rating, although it is not a Foundation Trust, indicating that there is “minor or moderate concerns” in terms of any future authorisation. A high level review of the effectiveness of the Trust’s quality governance arrangements, including the use of mortality information on a local basis, was a key line of enquiry for the review. Clinical and operating effectiveness The Trust was reviewed on its clinical and operational effectiveness based on nationally recognised key performance indicators. The Trust has high rates of severe hypoglycaemic episodes and low rates of patients receiving a foot risk assessment in 2012. They were also an outlier for the percentage of discharged patients who are prescribed beta blockers following a myocardial infarction and for the proportion of patients having surgery within 36 hours following hip fractures. The Trust sees 93.7% of A&E patients within 4 hours which is below the 95% expected level. The achievement of the 95% expected level varies from site to site. For referral to treatment, 90.6% of patients start treatment within the 18 week expected time which is above the target level. This has been a consistent trend from April 2012 to March 2013. The Trust’s crude readmission rate which is the percentage of patients that were discharged and then re-admitted within 30 days is within the expected range when compared against the national average, at 11.3%. The average length of stay is shorter than that of the national average. The Patient Reported Outcome Measures (PROMs) dashboard shows that there has been some decline in performance across the six measures, with one instance (Hip Replacement Oxford Hip Score) of being below the lower 99.8% control limit. The data in this area highlighted some specific key lines of enquiry including, Respiratory Medicine, Stroke and Diabetes, all of which were highlighted as areas to review in the key lines of enquiry under clinical and operating effectiveness. Patient experience Of the 9 measures reviewed with Patient Experience and Complaints there are seven which are rated ‘red’ which means the indicators are outside of the expected range: 11 National Inpatient Survey: The national inpatient survey 2012 measured a wide range of aspects of patient experience. A composite ‘overall measure’ is calculated for use in the Outcomes Framework. This measure uses a pre-defined selection of 20 survey questions to rate the Trust on aspects including access to services, coordination of care, information and choice, relationship with staff and the quality of the clinical environment. The Trust sits below the national average with an overall measure of 73.8 compared with the national average at 76.5 Cancer survey: of the 58 questions, 22 were ranked in the bottom 20% whilst only 2 were in the top 20%. The main negative focus relates to overall care and care and treatment for inpatients Patient Environment Action Team (PEAT - privacy and dignity: The scores for privacy and dignity were shown as ‘acceptable’ across some sites – this is a low rating on this indicator PEAT - environment: The scores for environment are routinely shown as ‘acceptable’ across all sites – this is a low rating on this indicator Friends and family test (FFT): The Trust showed a decline in scores for the Midlands and East FFT to an overall score of 63 placing the Trust in the bottom quartile of the submissions Patient voice comments: In the two years to 31 January 2013, there were 241 comments on The Trust of which 165 were negative (68%). The negative focus includes a lack of professionalism displayed by staff (notes not filled in for example), lack of organisation and too much focus on targets Complaints about clinical aspect: Within the Trust, 704 written complaints were submitted during 2011-12 of which 73% related to clinical aspects of care, compared to the national average of 47%. The Ombudsman currently rates the Trust as A-rated. The Ombudsman investigates complaints escalated to it by complainants who are not satisfied with the Trust's response. It rates Trusts on whether they have implemented the recommendations made at the end of an investigation in a satisfactorily and timely manner, helping to ensure that Trusts learn from mistakes. The Ombudsman rates each Trust’s compliance with recommendations and focuses on monitoring organisations whose compliance history indicates that they present a risk of non-compliance. The complaints process and the appropriateness of language used in front of patients by doctors and the manner by which patients are treated are highlighted as areas to observe in the key lines of enquiry under patient experience. Keogh review patient voice comments The patient voice comments received directly to the Keogh review website (at the time of writing this report) identified the following themes from 33 emails and letters: Positive Patient was happy with services provided by Pilgrim Hospital. Admitted to A&E where care was very good. Appointments are on time. Receptionist was attentive and professional. Nurse was supportive and the operation and physiotherapy went well. All the staff were brilliant and care was excellent. 12 Excellent treatment and attention at orthopaedic ward. Physiotherapy was also very good. Patient had to wait 7 hours for a bed for an operation. Intensive Care ward was very good, staff were brilliant. As an outpatient there is a long wait to see a consultant but the staff are helpful and consultant is informative Negative Lack of communication between patient and staff at all levels. Mistakes in surgery and diagnosis Patient was undressed with the curtains not shut, no respect for dignity Delay in providing treatment and medical forms Buzzers not working and ward overcrowding, concerns about cleanliness Operations cancelled and appointments rearranged, long waits for diagnostic procedures and pain relief Poor attitude of staff with no respect for dignity of the patients, no help with basic tasks or personal hygiene Concerns about controlled drug management not being addressed Too few staff Inappropriate language and lack of sensitivity towards patients, staff being rude to patients Staff raised concerns in the following areas: Issues with staffing including recruitment, retention, use of agency, release of staff for training Poor escalation procedures Lack of stability within the Trust at senior level. Poor communication and engagement with staff and patients Poor communication, poor note taking, discrepancies in notes and communicated issues. Inappropriate use of ‘do not resuscitate’ order, poor communication of test results No response or poor response in relation to a complaint made Poor management of medication being taken by a patient in advance of hospital admission 13 ‘Disregard’ of available treatment due to age of patient, no assistance with eating Poor after care Key lines of enquiry were followed in the review based on what patients say about the quality of care and treatment of patients and what the Trust is doing in response to this feedback. Workforce and safety A review of the workforce data flagged a number of ‘red rated’ indicators: The Trust’s sickness levels across all staff types (medical, nursing, other staff and overall) are rated red. This means that staff sickness rates are above the national average for each of these groups. Turnover rate of staff is also higher than the Midlands and East Region median with a joining rate lower than the average at 5.7% compared to 5.9% and a leaving rate of 7.5% compared with 6.7%. This means that more staff than average are leaving the Trust and fewer staff than average are joining the Trust. The Trust’s spend on agency staff was 5.1% of its total staff costs in 2011/12. This compares to an average in the Midlands and East region of 4.2% In addition to the above, a number of factors were identified from the General Medical Council’s (GMC) National Training Scheme Staff Survey in 2012. These include: Worse than expected staff engagement The number of staff that would recommend the organisation as a place to work is below the national average The number of staff that, if a friend or relative needed treatment they would be happy with the standard of care provided by this organisation is below the national average Staff did not see ‘care of patients’ as the organisation’s top priority Further concerns were raised by the Deanery, when, in October 2011, it considered removal of junior doctors. However the Trust was able to sufficiently demonstrate that doctors in training were no longer working in wards without adequate supervision, and there was a more equitable workload. At Pilgrim Hospital in Boston, the Deanery conducted a full quality review of training in all specialties after student nurses were removed from the site by the Nursing and Midwifery Council in July 2011. The Deanery undertook five further visits in 2012 and confirmed that rotas had been reorganised to ensure appropriate workload and supervision for trainee doctors, who are also now receiving appropriate education. This site was noted as having persistent recruitment issues. The Deanery continues to undertake routine monitoring of arrangements. The NMC temporarily removed student nurses from one site during February 2011 following concerns expressed by the CQC. The situation was investigated and students were returned to the site in July 2011. 14 At Grantham and District Hospital, the Deanery quality management activity indicated that there were issues with handover and clinical supervision in medical and emergency medicine posts. The Deanery met with the Trust in November 2012 to discuss the issues. An action plan dated February 2013 indicated that there is now 24/7 middle grade cover, and the rota has been revised to improve handover. The Deanery continues to closely monitor the site. Key lines of enquiry were included in the review focusing on how the Trust is assured over its workforce in relation to out of hours cover and how it is responding to concerns raised by the Deanery in recent months and years. The Trust is ‘red rated’ in the following two safety indicators: For methicillan resistant staphylococcus aureus (MRSA) infection rates, the Trust was in the bottom third of 143 trusts nationally over the three years from 2010 to 2012. The Trust’s infection rate in relation to other Trusts has improved in 2012, and places ULH close to the average for all Trusts. The Trust has informed us that whilst its MRSA infection rates were above average nationally over the three years from 2010 to 2012, the rate of infection was significantly lower than the highest rates recorded across the country and the Trust has performed at or below the maximum acceptable ceiling for MRSA infection rates for the last 4 years. Clinical Negligence payments have exceeded contributions to the ‘risk sharing scheme’ for two of the last three years. Payout exceeded contributions by a total of £4.9m over this period. The Trust has had 12 ‘never events’ since 2009. ‘Never events’ have potential to cause harm to patients and are judged as easily preventable by Department of Health (DH) guidelines. The Trust is above the average levels for all acute Trusts for pressure ulcers throughout the last 12 months. Between December 2012 and March 2013 there has been an increase in the percentage of ulcers from 1.1% to 2.9%. Key lines of enquiry were included in the review focusing on how the Trust is assured over the safety of care in its hospitals. 15 3. Key Lines of Enquiry The Key Lines of Enquiry (KLOEs) were drafted using the following key inputs: The Trust data pack produced at Stage 1 and made publically available Insights from the Trust’s lead Clinical Commissioning Group (CCG), West Lincolnshire CCG Review of the patient voice feedback received specific to the Trust prior to the site visit These were agreed by the panellists at the panel briefing session prior to the RRR site visit. The KLOEs identified for the Trust were the following: Theme Key Line of Enquiry Governance and leadership Can the Trust clearly articulate its governance processes for assuring the quality of treatment of care? Are the leadership roles and responsibilities clearly defined for the quality processes? Can staff at all levels of the organisation describe the key elements of the quality governance processes Clinical and operational effectiveness What governance arrangements does the Trust have to monitor clinical and operational performance data at a senior level? What processes does the Trust have in place to support monitoring mortality data and clinical effectiveness? Has the Trust data identified any issues? What actions is the Trust taking to address issues noted? Patient experience How does the Trust review patient experience data and engage with patients to seek views about their experience? What are the key themes from patients on their experiences? What action is it taking to address the key themes emerging? What do patients say about the quality of care in the Trust during our observations/interviews? Workforce How is the Trust addressing staffing issues as raised through the Deanery? How is the Trust responding to out of hours staffing issues? How is the Trust responding to issues with qualified nursing ratios, nursing hours to patient day and high sickness rates? 16 Theme Key Line of Enquiry Safety How engaged are staff in the Trust’s quality strategy? What do staff groups interviewed (including trainee groups) say are the main barriers in the Trust to delivering high quality treatment and care for patients? How does the Trust review and monitor its patient safety indicators? What actions are taken to improve patient safety? Trust Specific – General Medicine and Elderly Care What actions is the Trust taking to address issues in general medicine including treating elderly care patients? How is the Trust managing its stroke patients? How is the Trust responding to high mortality flags in oncology, respiratory and thoracic medicine? How does the Trust manage patients with Diabetes and what action is it taking to prevent avoidable deaths? Trust Specific – Urgent Care How does the Trust manage its Urgent Care Pathway? Trust Specific – Obstetrics What actions is the Trust taking to address issue relating to obstetrics and the high number of deaths attributed to perinatal conditions? Trust Specific – Critical Care and Surgery How is the Trust managing its critical care pathway and what actions is it taking to address the higher than expected mortality rates in this area? How is the Trust responding to the contributing factors such as deteriorating EWS score rates, shock cardiac arrest triggers and deteriorating renal function triggers within its crude surgical mortality rate? 17 4. Findings Introduction The following section provides a detailed analysis of the panel’s findings, including good practice noted, outstanding concerns and prioritisation of actions required. Summary of findings A number of areas of good practice were identified as part of our review, notably: We met with some dedicated, committed and loyal staff Monthly mortality reviews have good attendance with good clinical engagement The Interim Director of Nursing has provided strong leadership to the nursing team The Matrons at all sites displayed strong leadership, especially at Grantham Hospital Many wards displayed safety thermometer data sets Plan for Every patient on wards Evidence of innovation e.g. Red Lid Scheme for Hydration/medication; phlebotomy service at weekends which takes pressure off junior doctors The Colorectal team at Lincoln hold an annual patient listening event Patient experience and stories are now part of the Trust Board meetings Safety and quality dashboards displayed on the wards Proactive work around dementia in particular wards GP support within the Grantham A&E Department that enables the most appropriate care to be provided to the patient The Trust is embarking upon a major review of services, with its Health and Social Care partners in Lincolnshire, to address the sustainability challenges for the whole community The Chief Executive, who was fairly recently appointed, is sighted on the complex issues in the organisation of aligning a Board driven strategy into fabric of every part of the organisation 18 During our visit, an issue was identified in relation to inadequate staffing levels within all three hospital sites. The panel formally escalated this to the CQC after the unannounced visit. In addition, concerns around satisfactory completion of ‘do not attempt resuscitation’ (DNAR) forms were also raised. This was escalated to the Trust management team for immediate action. The Trust has completed a review of all patients with DNAR forms across all three hospitals and every DNAR form has now been signed off by a consultant and discussed with both patients and relatives as appropriate. As part of the review process, the panel received a submission from a former Chief Executive of the Trust. As with all evidence received through the public communication channels, the panel has reviewed this and triangulated this with its findings. This submission highlights issues with governance and staffing levels which triangulate with the findings detailed in this report. The main priority areas identified for action in each of the key lines of enquiry themes are below. Leadership and governance: There is a disconnect between leadership at Board level and leadership at clinical levels within the organisation: The Trust should ensure there are clear and active discussion lines between the clinical leaders at ward level, the clinical directors and the Trust Board to ensure that leadership of the organisation is joined up and consistent. The Trust should focus on engaging clinical teams rather than specialties or separate professional groups. Clinical and operational effectiveness: The panel was unable to easily see or understand how escalation worked for both actions taken in managing deteriorating patients and also managing patient flow as there seemed to be no standardised process in operation across the specialties and sites: The Trust should seek to clarify its escalation policy and ensure that it uses the ‘track and trigger’ system effectively across all the Trust sites. Staff should ensure that escalation responses are appropriate and well documented in response to managing deteriorating patients. In addition the Trust should ensure that patient flow is planned and managed appropriately. An IT solution needs to be found to allow the ambulance inbound system to be visible in A&E. Patient experience: The complaints process is confusing and not fit for purpose: The Director of Nursing and the Company Secretary should review the handling of complaints and the processes whereby complaints can be systematically fed back and used by staff teams to improve service delivery. This should include creating a PALs function. Complaints should be seen as everyone’s responsibility – not just the complaints team / board. Patient experience is not seen by patients to be at the heart of the organisation and service improvement: The Trust should implement a patient experience action focussed improvement plan that should include: real time patient feedback, evidence of listening and responding and using and working with patients to codesign service improvement. Workforce: 19 Staffing levels were, in some areas and at certain times of the day, low. The panel formally escalated its concerns to the CQC on 21 June 2013: The Trust should consider urgently the staffing levels and mix throughout the Trust, covering: nursing numbers and appropriate use of agency and bank staff; Matron cover at Pilgrim Hospital, Boston; dependency of patients including 1:1 care, assistance with eating and assistance using toileting facilities, and; middle grade cover and appropriate supervision of junior doctors, especially out of hours. Workforce planning is poor with no recruitment plans and no plans in place to cover maternity leave, sickness and annual leave other than through the use of agency, bank staff or, in the case of medical staffing, locums: The Trust should document and implement a recruitment plan with immediate effect to fill the short term vacancies but also consider its medium term requirements. The Trust should also seek to firm up its strategic plans, including the level of future service provision at all three main hospital sites and the community sites. This should be done in conjunction with stakeholders. Student nurse posts should be advertised earlier. Safety: Quality strategy could not be consistently articulated by all staff and non executive directors: The Trust should confirm the key quality priorities for the Trust and ensure these are widely understood by staff using campaigns and listening events as well as emails, the intranet and Ward to Board initiatives. General Medicine and Elderly Care Lack of awareness of the Mental Capacity and Deprivation of Liberty Act 2005 in relation to the Trust’s responsibilities in allowing patients to leave wards if they are deemed capable and wish to: Staff should ensure that they are fully compliant with mandatory training requirements and adult safeguarding is given clinical engagement as a matter of urgency. Urgent Care There were no urgent actions under this KLOE. Obstetrics There were no urgent actions under this KLOE. Critical Care and Surgery We observed a number of issues with the completion of DNAR forms: The Trust has already undertaken an immediate review of all patients with DNAR forms to ensure they are accurately and adequately completed. This was completed immediately by the Trust. The Trust should review its process and policies for the completion for DNAR forms to ensure they meet best practice and legal requirements. 20 The following definitions are used for the rating of recommendations in this review: Rating Definition Urgent The Trust should take immediate action to respond to these recommendations and ensure improvement in the quality of care High The Trust should develop a response and action plan for these recommendations to ensure improvement in the quality of care Medium The Trust should implement these recommendations to ensure ongoing improvement in the quality of care 21 Governance and leadership Overview The panel’s focus for governance and leadership was on the articulation and understanding of the Trust’s governance processes for assuring the quality of treatment and patient care and how well embedded this was throughout the organisation. Through staff interviews, focus groups and review of governance documentation, the panel tested whether staff at all levels could describe the key elements of the quality governance processes, i.e. policies and procedures, escalation, incident reporting, risk management. The panel also reviewed the Trust’s process to assess the impact of cost savings plans on quality of patient care and its workforce. Summary of findings The following good practice was identified: The Chief Executive, who was fairly recently appointed, is sighted on the complex issues in the organisation of aligning a board driven strategy into the fabric of every part of the organisation. The Non Executive Directors report recent more detailed quality discussions at Trust Board and increased confidence that the work on the integrated dashboard should provide congruence on patient safety and quality, performance and finance. Monthly mortality reviews have good attendance with good clinical engagement. The voicing concerns policy has been reviewed with support from staff and is ready for roll out and adoption. The Interim Director of Nursing has provided strong leadership to the nursing team. The Matrons at all sites displayed strong leadership and many wards displayed safety thermometer data sets. The intensive approach and “ Shop in Shop “ has driven substantial improvements in services where there has been concern. Patient Stories feature at the Trust Board each month. The Trust Board is embracing the need for a Service Sustainability Review to work with health and social care partners to tackle the emerging clinical viability challenges across all health services including acute service providers. This will address the real challenges of providing specialist acute services across geographically distant sites. The following areas of concern were identified: There is disconnect between leadership at Board level and front line clinical teams in the organisation. There is also variation in the levels of medical engagement across the hospital sites with this being strongest at Pilgrim and Grantham Hospitals. 22 The constant change in leadership at the executive level has led staff to feel uncertain and has created cultural problems as identified in the recent organisational diagnostic. Staff feel there is no clear vision and direction for the Trust and subsequently there is a disconnect between individual, team, directorate and corporate objectives. The governance structures and processes reflect the complexity of a large organisation that provides care on three sites that are separated by significant distances. Staff on the ground were unable to articulate the governance processes for quality of treatment and patient care and patient safety or the Trust’s Quality Strategy. It was not clear to the panel where the accountability for quality and patient safety lies between Medical Director/ Director of Nursing. There was some evidence of Board to Ward assurance, however this was not visible to all staff and so there was limited opportunity for the board to evidence to staff that they truly take ownership of governance of quality of care. Serious Incidents and Never Events are received by the board via the committee structure but complex structures build delay into this process. Staff report that they do not receive any feedback on these routinely or in a timely fashion. There is confusion in the organisation as to whether there is a PALs function to support monitoring of quality and patient experience and how the complaints process worked. There is no PALs function at ULH. The engagement of staff and clinicians in the governance processes for assuring the quality of treatment and patient care and the identification and implementation of the Trust extensive Cost Improvement Plans is variable. Not all CIPs have been assessed for impact on patients and the process for monitoring these is not known or owned by staff. Non Executive Directors and the Clinical Commissioning Groups reported that they were not sighted on the QIA of the 2013/14 CIP plans. The Chair of the Audit Committee had seen details about 180 line items but this was not reported at an appropriate level of detail. There was little evidence of strong medical consultant leadership for the patient safety and quality agenda. For some of the above areas of concern, the panel identified a number of improvements already planned or underway at the Trust. Detailed Findings Good practice identified The Chief Executive and Vice Chair recognise the culture is not as conducive as it needs to be to provide good patient care and have recently used their reference group to work with the Execs on a cultural diagnostic and rolling out “ Listening into Action”. There were some areas within the Trust, such as Stroke Unit, where clinical leaders and staff were able to clearly articulate governance processes and knew their individual quality metrics. The established Mortality Review meetings gaining wider clinical support and the proposal to write these into the job plans of the Consultant body. The interim Director of Nursing has a clear understanding and insight into the shortfalls in the current governance processes and has provided strong leadership to the nursing teams to improve and raise standards of care. Wards display patient safety information and the ‘plan for every patient’ methodology is applied to manage care in a coordinated way. 23 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions (i) There is a disconnect between leadership at Board level and leadership at clinical levels within the organisation The Trust accepts that there is more to do to connect Clinical Directors and the Board with clinical leadership at ward level. The Trust should ensure there are clear Urgent and active discussion lines between the clinical leaders at ward level, the clinical directors and the Trust Board to ensure that leadership of the organisation is joined up and consistent. The Trust should focus on engaging clinical teams rather than specialties or separate professional groups. The panel observed strong clinical leadership from the matrons at hospital and ward level but identified there was a disconnect between this clinical leadership at ward level, medical clinical leadership (especially at Lincoln County Hospital) and the clinical directors and the Board (both executive and non executive directors). The panel was informed by the Trust that a number of initiatives are currently in progress however these were not observed by the panel on the review visit. Priority – urgent, high or medium The Executive Team recognise the need to build stronger connections between leadership at Board level and leadership at clinical level. It is critical that this recognition is adopted across the entire Trust, by all staff groups and by the whole Board. (ii) Clarity is required on what the Trust’s Quality Strategy is The panel understand that the Trust is conducting a review which will lead to an integrated dashboard. The panel could not clearly identify what the Trust’s quality strategy is through discussion with staff as staff could not articulate it to us. There was no clear view on who is accountable for quality and the governance process is also unclear. The panel also understands that the following actions are underway: The Trust Board needs to clarify both ‘the High who’ and ‘the what’ in the process for patient safety, quality and governance and to evidence strong visible leadership in this area. Frequent executive-led staff briefings Refined Team Brief process, involving a toolkit 24 Outstanding concerns based on evidence gathered There was little evidence of strong medical leadership for the patient safety and quality agenda. Key planned improvements Recommended actions Priority – urgent, high or medium The Trust Board needs to ensure that there is a systematic approach in place for the collection, reporting and acting upon information on the quality of services, patient and clinician insights and that the processes include feedback and engagement of staff in learning and service improvement High for managers to cascade key issues to staff Regular podcasts by execs and senior clinicians about quality and safety issues These were not observed by the panel on the announced and unannounced visits (iii) The governance structures are complex and staff on the ground were unable to articulate the governance processes for quality of treatment and patient care and patient safety or the Trust’s Quality Strategy The panel saw and heard evidence from frontline staff, including senior clinicians that there was confusion about the governance structures and processes for quality and patient safety. This included a lack of clarity between divisional and Trust level governance arrangements, a lack of clarity on the feedback mechanisms for complaints and reported incidents. Staff in a number of groups, interviews and visits were unable to describe a cross-trust, systematic approach to the collection and reporting of data, its use by the Board to assure itself of quality and patient safety and the feedback mechanisms to support learning and service improvement. The Trust informed us that the Board held a development session on Risk and Governance on 22 May 2013. The outputs of this were not reviewed by the panel during the review process. The Trust should review its risk registers and ensure that all high rated risks are flagged to the Board and addressed appropriately. Staff highlighted issues around the governance process within the Trust. For example staff highlighted that despite logging a number of risks rated at level 20 on the risk register, these had not been escalated to or flagged to the board. Example risks highlighted are those from 19 25 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium The Trust informed that the panel that a number of actions are already underway but these were not observed or reviewed by the panel during the review visit. To undertake a regular programme for all Board members to visit patient care areas and to consider adopting the “15 Steps” approach as implemented at Nottingham University Hospitals or similar schemes. This should include announced, unannounced and out of hours visits. Medium The Trust has informed us that it has a communications plan supporting patient safety campaign however this was not observed or reviewed by the panel during the review visit. To review how the Trust communicates High with its staff and to actively respond to staff views in their preferences for communications. Dec 2012: Risk regarding nurse staffing levels Risk regarding the failure to recruit nurses Risk regarding the failure to resource enough bank staff to cover the escalation beds Risk which highlighted the current nursing gaps on the stroke unit The Trust informs us that all but one of these risks have now been closed. (iv) The constant change in leadership at executive level has led staff to feel there is no clear vision and direction for the Trust and subsequently there is a disconnect between individual, team, directorate and corporate objectives During focus groups, many staff felt that Board Exec and Non-Exec Members did not make themselves available on a regular basis to see the quality of services for themselves. (v) There was some evidence of Board to Ward assurance however this was not visible to all staff and so there was limited opportunity for the board to evidence to staff that they truly take ownership of governance of quality of care During focus groups, many staff groups felt that communications of issues relating to the quality of services relied too heavily on the staff intranet and 26 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium The Director of Nursing and Medical Director review current incident reporting processes and implement new processes High that other methods of communication including face to face with Board members, face to face cascade through team meetings and other methods would be more meaningful and have greater impact on their practice. The Trust executive informed us that the following initiatives take place although these were not widely identified by the staff: Patient Safety Leadership Walkaround programme – every ward visited in the past 18 months by a Board member and the patient safety team Risk, Patient Experience and Patient Safety reports presented and discussed at monthly Quality and Safety committees, chaired by Medical Director and attended by nonexecutive director, director of quality governance Direct Board oversight of mortality steering group (deputy CEO in the chair) and medical directors key attendees Safety and Quality dashboard, reflecting 56 near-real-time indicators of fundamental care processes reviewed at Quality and Safety Committee Internal compliance team in-depth reviews of CQC essential standards (Be Assured programme) reported to Director of Nursing and Medical Director; most wards reviewed in past 12 months. (vi) Serious Incidents and Never Events are The Trust notes a number of actions underway received by the board via the committee however the panel did not observe these during the structure but complex structures build delay into 27 Outstanding concerns based on evidence gathered Key planned improvements this process. Staff report that they do not receive visit. any feedback on these routinely or in a timely fashion Recommended actions Priority – urgent, high or medium that ensure the feedback loop to staff and their active engagement in lessons learnt. There were examples given to the panel where incidents had occurred, staff had reported fully, but had received no feedback or confirmation that the report had been received. Some Junior Doctors told us that they had ceased reporting incidents because they ‘went into a black hole’. (vii) There is confusion in the organisation as to whether there is a PALs function to support monitoring of quality and patient experience and how the complaints process worked The panel is aware that the Trust Board has recognised Complaints/ PALs and patient feedback both PALs and complaints are issues that require mechanisms need reviewing. action. High The panel identified that there were many instances where complaints had not been dealt with to the satisfaction of the complainant and that the complaints process was not feeding adequately into the wider governance of assurance for trend analyses, early warnings and feedback to staff. (viii) The engagement of staff and clinicians in the governance processes for assuring the quality of treatment and patient care and the identification and implementation of the Trust extensive Cost Improvement Plans is variable. Not all CIPs have been assessed for impact on patients and the process for monitoring these is not known or owned by staff. Non Executive Directors reported that they were not sighted on The Trust told us that the Board has agreed, as part of its review of governance arrangements, to establish a QIPP and Transformation Committee and establish a QIPP Executive. The panel did not observe these governance arrangements as part of the review. To review the mechanism for the engagement of all those affected by proposed CIPs in their development and agreement. To ensure the Board is assured that it has strong clinical engagement in the development of all CIPs and that QIAs have been carried out in all cases prior to High 28 Outstanding concerns based on evidence gathered the 2013/14 CIP plans Key planned improvements Recommended actions Priority – urgent, high or medium commencement of any plans. The engagement of staff and clinicians in the development and agreement of CIPs is patchy. Not all schemes have had quality impact assessments as part of process and unclear as to how these are monitored. The Trust executive team told us that 65% of CIPs have been impact assessed with the balance to be finalised in July prior to implementation. 29 Clinical and operational effectiveness Overview The panel’s focus for clinical and operational effectiveness was to explore how the Trust used clinical and operational performance data at a senior level. Looking specifically at what processes the Trust has in place to support monitoring mortality data and clinical effectiveness and what the Trust’s data identified and what action is the Trust taking. Through staff interviews, focus groups and review of documentation, the panel tested whether staff at all levels could describe the key operational data and policies and procedures, escalation, incident reporting, risk management. The panel also reviewed the Trust’s process to assess the impact of cost savings plans on quality of patient care and its workforce. Summary of findings The following good practice was identified: Mortality Reviews are discussed at Clinical Directorate Level monthly underpinned by weekly reviews at ward level. We found some evidence of the shared learning and/or changes to practice but this was not widespread. Good evidence of displaying patient safety thermometer / harm free care metrics on wards. Plan for Every patient on wards. Evidence of innovation e.g. Red Lid Scheme for Hydration/medication; phlebotomy service at weekends which takes pressure off junior doctors. A Trust wide nursing and skill mix review has been undertaken with Board agreement to invest £7 million over 2 years. A recruitment plan is underway to implement this. Achievement of CQUIN 2012-13 regarding the reduction of patient moves. The following areas of concern were identified: The panel was unable to easily see or understand how escalation worked through discussions with staff as there seemed to be no standardised process in operation across the specialities and sites. We understand from discussions with the executive team that the Trust does have a standardised approach which is linked to the track and trigger system at patient level and a standardised escalation processes are a feature of the revised Operations Directorate structure however this did not come across in discussions with staff. Staffing levels are flagged as an area of risk which potentially compromises patient safety and optimal care for patients. The cover at weekends and out of hours is minimal for both medical and the nursing teams. Some wards also expressed concerns that general staffing levels were such that they could not free staff up to escort patients to diagnostics which resulted in extended length of stay. This has been discussed in detail under KLOE5 (Workforce) below. There were a number of concerns flagged with regard to ‘do not attempt resuscitation’ (DNAR) forms and record keeping. This is also discussed under KLOE 10 (Critical Care) below. 30 At individual site level there was lack of knowledge/awareness of the actual operational data such as readmissions and mortality data. Staff raised concerns regarding outliers not getting appropriate care from the right consultant teams and difficulties in getting consultants to review patients. Staff reported that many patients get moved resulting in lack of continuity of care and sub optimal care so there are concerns flagged with regard to flow /surge and capacity planning. Not all CIP projects had quality impact assessments to look at how they would affect patient safety and care and the arrangements for monitoring these projects. Monitoring seemed to focus on achieving the financial targets. This is discussed in more detail under KLOE 1 (Governance and Leadership) above. Detailed Findings Good practice identified The practice of mortality reviews has been well supported by the staff and reported good engagement with this process. There were some areas within the Trust, such as Oncology, Stroke, Maternity and Critical Care where clinical leaders and staff were able to clearly articulate the detailed processes to support the mortality and quality reviews of care for patients. Every ward displayed some safety and quality information on the boards which was open for all staff, patients and visitors to see. This information often included pressure ulcers, falls and VTE assessments; however there was some inconsistency in the information that was displayed and the level of detail available. The use of a plan for every patient was a simple, effective and visible daily record of each patient’s status / actions for that day and for planning discharges. Outstanding concerns based on evidence gathered Key planned improvements (i) The panel was unable to easily see or understand how escalation worked for both actions taken in managing deteriorating patients and also managing patient flow as there seemed to be no standardised process in operation across the specialties and sites The Trust told us that it recognises that the inbound information system is mid-implementation, and not yet fully operational from an ambulance trust perspective. As part of the implementation phase there are a number of issues to be resolved, including IT. These Staff were unable to articulate the escalation policy that was consistent and issues will be resolved as part of the implementation trust wide. We found examples of good escalation processes (such as A&E plan, prior to going live. The Trust hopes that this will at Boston) but other areas where processes were not clear or well reduce the number of inappropriate placement of formulated. patients within the department. There was a Track and Trigger warning score in place which emphasised The Trust tells us that it has already changed the Recommended actions Priority – urgent, high or medium The Trust should seek to clarify its escalation policy and ensure that it uses the ‘track and trigger’ system effectively across all the Trust sites. Staff should ensure that escalation responses are appropriate and well documented in response to managing deteriorating patients. Urgent 31 Outstanding concerns based on evidence gathered Key planned improvements that a score >4 would lead to a newly admitted patient from A&E at Lincoln on the Medical EAU to be brought to the attention of a doctor immediately although it was not clear that this was being used appropriately. working of Bailgate to an ambulatory care facility. Recommended actions Priority – urgent, high or medium In addition the Trust should ensure that patient flow is planned and managed appropriately. There was an escalation policy at Grantham (made available to the review team) for managing an increase in the number of patients from 6 to 9 in CCU, but staff were unable to articulate this or demonstrate actions arising from failure to adhere to this policy. An IT solution needs to be found to allow the ambulance inbound system to be visible in A&E. A&E at Lincoln did not make use of the ambulance inbound information to plan capacity needs due to IT issues. This can lead to inappropriate placement of patients within the department. The panel observed inappropriate use of Bailgate on a frequent basis with patients being transferred to await an appropriate bed. An elderly orthopaedic patient was observed on our unannounced visit who had been transferred to Bailgate. The staff were not familiar with a brace being worn and this was an additional move for this patient. The Trust told us about the achievement of its CQUIN 2012-13 regarding the reduction of patient moves. (ii) At individual site there was lack of knowledge and awareness of the actual operational data such as readmissions and mortality data During visits and focus groups staff were unable to describe the mortality rates/issues and therefore unable to describe what actions the trust had taken. (iii) Staff raised concerns that outliers were not getting appropriate care from the right consultant teams and difficulties in getting consultants to review patients The Trust tells us that the Board has adopted an evidence-based mortality reduction plan. This was not evidenced to the panel as being communicated during the review period. The Board and the CDs need to ensure that this information is made accessible to staff, discussed at team /ward meetings. High The Trust is implementing a virtual hospital framework, which when embedded and fully utilised should ensure good capacity management and escalation. The capacity and surge High plan for the Trust needs to be embedded and there needs to be understood and 32 Outstanding concerns based on evidence gathered There were a large number of concerns raised by staff and indeed patients about inconsistency of care and or sub optimal care as a result of being an outlier and being moved about between wards. The panel attended a bed management meeting at Lincoln County Hospital where the current Trust position was discussed however there was no discussion regarding capacity required for the next 12 hour period and no evidence of forward planning to ensure capacity planning for overnight. Key planned improvements Recommended actions The new build scheme will provide sufficient cubicles to enable earlier review and planning consistently applied actions with particular regard to managing patient flow. Priority – urgent, high or medium The Trust should continue with its implementation of the virtual hospital framework. Details regarding expected admissions and capacity were part of the framework but the Trust did not actively use this in the meeting as a measure for when to escalate. The Trust had a written escalation plan but did not use this at the meeting despite not having enough beds available for the next 12 hour period. At the meeting a decision was made that the Trust would actively outlie patients as there were not enough medical beds. There were no other actions taken. The panel would have expected to see action regarding creation of capacity by the home units. Outlying patients at the meeting attended appeared to be the primary option for managing capacity demands (this approach of course creates a number of problems that are well documented regarding the care of patients outside their home wards and access to clinical expertise appropriate with their condition). Patients being moved or cared for on an outlying ward was a key area of concern raised to the panel at the patient listening events. The Bostonian ward at Pilgrim was aimed at private or mainly urology patients, however some medical patients were on this ward and solely cared for by one stroke consultant who at times of being on leave would get a registrar to review patients. 33 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium Escalation at Lincoln was late and the panel observed patients moved just before the 4 hour threshold, sometimes inappropriately to Bailgate ward. At the unannounced visit, 50% of patients on Bailgate required admission to specialist beds and not a Clinical Decision Unit. This compromised flow from the A&E department. 34 Patient experience Overview The panel focused on how the Trust understands and responds to patient feedback on their experience through discussing this with patients and staff on wards and at the focus groups and listening events, as well as reviewing board and ward level information on patient experience. Summary of findings The following good practice was identified: There were areas of the hospitals visited where Friends and Family Test scores were displayed. The Intensive Treatment Unit (ITU) has a call back service for patients and relatives. The Colorectal team at Lincoln hold an annual patient listening event. Patient experience and stories are now part of the Trust Board meetings. The Trust also informed us that there are a wide range of improvements and projects currently in progress within the Trust in line with the Patient Experience Strategy. Action plans are in place against the national inpatient, outpatient and A&E surveys and a workplan against the strategy. The strategy is aligned to the 14 standards and was widely consulted on (including PCT/CCGs) before being ratified at Quality & Safety Committee. Real time surveys have been in use since June 2012 and are reported on widely including within Board reports and to sites and services. The following main areas of concern were identified for patient experience: The complaints process is confusing and not fit for purpose. Patients told us that they felt that the patient experience is not at the heart of the Trust’s strategy. The Non Executive Directors (NEDs) interviewed could not articulate patient experience vision and actions taken in response to this. There is no triangulation by the Trust of patient experience, staff experience and incident reporting. Pain recognition and treatment in patients with dementia was not well managed. 35 The panel did not identify any improvements already underway or planned at the Trust. Whilst accepting that there were negative stories from patients as part of the review process, the Trust articulated to us that it is committed to listening and learning from these. During 2012 - 2013 the Trust informs us that 113 stories were posted on ‘Patient Opinion’ which use a criticality scale against each story. 74% of these stories were rated as zero, that is, ‘no criticism / positive feedback’. Alongside this, the Trust has been collecting real time surveys for 12 months which includes free text comments. These are included in Trust Board reports as an overview report and sent weekly to all wards. The Trust tells us that on average 25 – 30% of these stories are negative comments. Detailed Findings Good practice identified There were areas of the hospitals visited where Friends and Family Test (FFT) scores were displayed prominently. The panel observed clear actions to address FFT feedback on specific wards however this was not consistent across the Trust. The Intensive Treatment Unit (ITU) has a call back service for patients and relatives which patients told us was valued and of use. The Colorectal team at Lincoln hold an annual patient listening event to hear the views of patients and negotiate agreed actions to take in response. It is disappointing to note that the Executive team do not form part of this listening event. Patient experience and stories are now part of the Trust Board meetings although this is relatively recent therefore it is too soon to comment on any actions that have been taken as a result. Outstanding concerns based on evidence gathered (i) The complaints process is confusing and not fit for purpose Key planned improvements The Trust Chief Executive and Director of Nursing told Recommended actions Priority – urgent, high or medium The Director of Nursing and the Company Secretary should review the handling of complaints and the processes whereby complaints can be systematically fed back and used by staff Urgent The panel observed a number of issues related to the 36 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium us that they are now sighted teams to improve service delivery. This should include: on complaints; a review of Improving understanding and visibility of complaints There were a number of complaints raised at the Patient complaints is underway methods with staff and patients. and Public listening events where patients raised concerns that their complaint had not been responded to however this was not Educate front-line clinical staff to respond more effectively evidenced to the review satisfactorily. to complaints and ensure accountability and ownership. panel during the visit. Patients told the panel that they felt ‘scared’ to complain as they were worried they would be labelled and this Continue to liaise with and meet patients to ensure their would affect the quality of the care they received. concerns are addressed. complaints process: There is confusion as to whether PALs exists at the Trust. Ensure complaints are responded to promptly. All complaints are referred to an administrative function. There is no sign off of complaints by the Chief Executive, Medical Director or Director of Nursing. Review size and structure of complaints team to ensure it is fit for purpose. Creation of a PALs function. Learning from complaints is not systematic or Trust wide. Complaints need to be seen as everyone’s responsibility – not just the complaints team / board. Devolve complaints management to Directorate/specialty level rather than a centralised process to improve ownership. Review the process and person responsible for ensuring a complaint is answered in a timely manner. Complaints are dealt with on a department by department basis and the process is inconsistent. There is a perceived lack of visibility of complaints methods by patients. Based on patient feedback, no one appeared to control or own the complaints process. (ii) Patient experience is not seen by patients to be at the heart of the organisation and service improvement The panel found that patient experience is not integrated into the Trust’s strategy. The approach to patient experience was inconsistent across the Trust and the Trust approach could not be articulated by key staff groups both at focus groups The Trust executive informs us that there are a wide range of improvements and projects currently in progress within the Trust in line with the Patient Experience Strategy. These The Trust should implement a patient experience action focussed improvement plan that should include: real time patient feedback evidence of listening and responding using and working with patients to co-design service improvement Urgent 37 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions and as part of our interviews and observations. were not reviewed by the panel during the visit. The whole trust staff should engage with this process. (iii) The Non Executive Directors (NEDs) interviewed could not articulate patient experience vision, actions, issues None noted The NEDs should ensure they have the appropriate level of awareness in relation to patient experience issues, including performing ‘walk arounds’ of wards and have ‘drop in clinics’ for patients to come and talk to them. The NEDs were unable to articulate to the panel the Trust’s patient experience strategy as well as any patient experience issues that the Trust may be experiencing. (iv) Pain recognition and treatment in patients with dementia was not well managed Priority – urgent, high or medium High In addition, the NEDs should be involved in any development of a patient experience strategy, alongside patient experience group. None noted NHS choices website for the Trust has stories of poor responses to request for analgesia. The Trust should carry out an audit cycle of pain assessment and widely published with a campaign to improve awareness and compliance with appropriate guidelines. High The Trust should introduce a pain assessment tool for people with dementia supported by the necessary training. The panel noted consistent infrequent monitoring of pain documented on the vital signs charts across all 3 sites. The Trust has no standardised pain assessment tool for people with dementia or other patients who cannot express if they are in pain verbally, for example, the Abbey Pain Scale. A patient with severe dementia and bedbound on ward 5 at Grantham had not had a pain assessment; the patient was assessed as being in pain by a clinician on the panel. The staff nurse providing his care was able to articulate how he would know a patient with dementia was in pain however did not respond appropriately to the patient in question. (v) There is no triangulation by the Trust of patient None noted The Trust should triangulate its patient experience data with Medium 38 Outstanding concerns based on evidence gathered experience, staff experience and incident reporting Triangulation of complaints, patient experience, staff experience and incident reporting could help the Trust to identify key themes, training gaps, systematic failures or linkages between events Key planned improvements Recommended actions Priority – urgent, high or medium staff experience and incident reporting to identify key themes arising and cross cutting issues. This should be reported to the Trust Board by the Director of Nursing. 39 Workforce Overview The panel’s focus for workforce was on how the Trust was addressing staffing concerns raised by the Deanery and also the issues noted about out of hours, nurse staffing ratios and high sickness absence. Summary of findings The following good practice was identified: We met some dedicated, committed and loyal staff who often work over and above their shift hours. Matrons showed excellent clinical leadership at ward level. Recruitment of new consultants and middle grade medical staff al sites, especially in emergency medicine. Junior doctors said they gained good experience with easy access to senior supervision in-hours and in most areas. The Trust recognises the clear linkage between recruitment / retention of key clinical staff and service viability. This will be a key issue for the sustainable service review. The following areas of concern were identified for workforce: Staffing levels were, in some areas and at certain times of the day, low. The panel formally escalated its concerns to the CQC on 21 June 2013. Workforce planning is poor with no recruitment plans and no plans in place to cover maternity leave, sickness and annual leave other than through the use of agency, bank staff or, in the case of medical staffing, locums. Supervision was found to be inadequate out of hours. For some of the above areas of concern, the panel identified a number of improvements were planned or already underway at the Trust. Detailed Findings Good practice identified Matrons and band 7 nurses showed some really excellent clinical leadership at ward level, leading by example, with a good presence on the wards. There has been additional recruitment at consultant and middle grade level at all sites which has strengthened the team, in particular in emergency medicine. The staff we spoke to across all three sites and across multiple disciplines came across as committed, dedicated, hard working and loyal to the Trust. We genuinely identified that staff wanted to give the best possible care that they could. 40 Outstanding concerns based on evidence gathered (i) Staffing levels were, in some areas and at certain times of the day, low. The panel formally escalated its concerns to the CQC on 21 June 2013. Key planned improvements The Trust has completed a comprehensive review of nursing numbers and skill mix. The Board has agreed to invest £7 million over 2 years a) Nurse Staffing in the nursing workforce. An Pilgrim Hospital, Boston implementation group is in place and On our unannounced visit at Pilgrim Hospital, Boston we were concerned active recruitment is underway. A about the levels of staffing on a number of wards. Staff also expressed marketing strategy will be developed concerns about the levels of staffing on a number of wards. We recognise that with local partners to promote the staff are generally caring, committed and incredibly loyal, however we note benefits of living in Lincolnshire. that there are simply not enough of them to do the tasks that are required. On ward 8A, we saw that at the time of our unannounced inspection there There is a plan to undertake overseas were two qualified nurses on duty with two HCAs to care for 28 patients. We recruitment and to appoint all new were told that the preferred staffing level would be five nurses and two HCAs nurses qualifying this summer who for that shift. want to work in Lincolnshire. We were informed that the ward never went below 2 qualified nurses but often this number was only achieved by filling with bank and/or agency, or staff from The panel is aware that the Trust’s other wards. recruitment programme for increasing On ward 6A, staff told us that more nurses were required to be sourced from nurse workforce has been agreed. bank, agency or other wards on all shifts. We were told that there were only eight permanent nursing staff to cover three shifts. The staff spoken to flagged that this situation was placing pressure upon those remaining and that gaps The Trust tells us that senior clinical would have to be filled from bank, agency and other wards. staffing out of hours will be specifically Staff on this ward stated that bank and/or agency staff were used every day. considered by the sustainability review. This has the effect of reducing staff morale. The Trust has a policy regarding drug administration and the use of agency nurses to perform such tasks it not The Trust tells us that it does permitted without evidence of IV compliance – this is to maintain patient experience higher unfilled vacancy safety. Agency nurses can monitor blood sugar if they can evidence and feel rates for Doctors, both substantive and competent to do. FR-training. The latter will be a feature of review with the Deanery. Recommended actions Priority – urgent, high or medium The Trust should urgently implement the recommendations of its nurse staffing review, in particular taking account of: nursing numbers and appropriate use of agency and bank staff; Matron cover at Pilgrim Hospital, Boston; dependency of patients including 1:1 care, assistance with eating and assistance using toileting facilities. Urgent The Trust should also consider urgently middle grade cover and appropriate supervision of junior doctors, especially out of hours. As an illustration of the challenges staff face: the panel observed a patient crying out for help over a 30 minute period who was not attended by staff during this time. The panel flagged this to the nursing staff at the time and we were told that the patient was fine and called out a lot due to dementia. We were also 41 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium told that the patient responded well to reassurance by staff but staff could only reassure when they had time to do so. At times there are wards with large numbers of patients who require some assistance with eating. Like all Trusts this can be a challenge. The Trust has recently developed a scheme of dining companions. In addition, on elderly care wards visiting time has been altered to enable relatives who want to assist with mealtimes to be on the ward. Non-clinically based nurses are also encouraged to assist. Ward housekeepers have a system whereby if there are large numbers of patients requiring assistance, the serving of hot food is staggered so that patients’ needs are met. An example of good practice is Stow ward, where all available staff gather together at mealtimes to be involved and this is led by the housekeeper and Sister. A relative of a patient on another ward visited on the unannounced visit identified another patient who had not received timely assistance to eat her food. The panel was also told that those patients that required support when transferring through use of the hoist were not usually supported to use the toilet away from the bay. They usually used a commode or bedpan within their bay area. When asked about the quality of care, a patient on ward 3B noted that "the staff are excellent, they need more [staff] though". Grantham Hospital Overnight cover was the most significant concern and although the Trust assures us that this never happens we were told by some staff that 1 bank worker may be the only member of staff on the wards overnight. Lincoln County Hospital We observed staffing on Stow Ward of 3 registered nurses (2 establishment plus 1 agency) with 1 HCA for 32 patients at night during our unannounced visit. There were insufficient staff available to provide 1 to 1 care for a patient who required this. Poor handover of patients was also identified in this ward and not all nurses questioned could describe how this was managed. 42 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium In A&E during our unannounced visit, staffing numbers matched the established roster however there were four extra patients being cared for in the corridors and the central area. Patients being cared for in the central areas and corridors add pressure to the department’s staffing compliment. Hatton Ward staffing had been increased in recent months so that there was 3 registered nurses and 3 HCAs on the late shift. During our unannounced visit we noted that the Band 7 nurse who had been due to leave at 3pm was still present on the ward (the time of our visit was approximately 7pm). This band 7 nurse had taken the decision to stay on the ward due to a poor nursing skills mix. b) Medical Staffing Our discussions with staff through focus groups and observing wards throughout the trust identified that during weekends and out of hours, medical staffing is not always sufficient to cover the needs of the Trust. Although the clinical teams had raised their concerns with the Deanery, there were often gaps in recruitment and in the subsequent on-call rotas. Gaps were often filled by locum or agency doctors. Pilgrim Hospital, Boston The panel observed a number of wards where consultants were required to work long shifts in order to provide sufficient cover, for example in A&E. In addition, the number of locums was high. During the unannounced visit it was also noticeable that, of all the doctors spoken to, the majority were working beyond their expected shift end time. When asked about this, these staff noted that there was too much to be done to have left earlier. There was only junior doctor covering the medical wards and one doctor covering the surgical wards at night and during the weekend. Consultants told us that they had concerns about the inability to recruit consultants to the following specialties: A&E, Radiology in general and breast and interventional radiology in particular, Health Care of the Elderly physicians and Stroke physicians. 43 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium Grantham Hospital During the days at weekends, and overnight, the only doctor covering the wards is an FY1. There will be a registrar and an SHO covering EAU and they will be making admission and discharge decisions. The concern we note is around supervision although the JDs did note that the consultants were contactable when they needed them and would come to the hospital if required The Trust informed us that that at any one time on the weekends and at night for medicine there will be two junior doctors and a middle grade on site. These are backed up by consultant o/c (non-resident). For Orthopaedics and General Surgery there will be a junior doctor during the day and one during the night (one for each speciality / shift – 4 Doctors in total). These are supported by non-resident on call – a middle grade for surgery and a consultant and a middle grade for orthopaedics. Therefore, the Trust asserts that at any one time during the weekend day or any night there will be at least 4 junior doctors and a middle grade on site, with a non-resident on call team of 2 middle grades and 2 consultants. These rotas are compliant with the working time directive and the Trust covers any gaps with backfill internally or agency. The Trust tells us that it is reliant on the Deanery providing candidates for the posts, which may be a risk from August (as the Deanery may reduce numbers). The Trust informs us that this risk was raised by the Trust with the Deanery on their recent visit. Lincoln County Hospital Similar issues around out of hours cover and weekend cover were observed at Lincoln through our conversations with staff and observations of shift patterns and rotas. 44 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium The Trust has identified a number of initiatives in place however these were not evidenced to the panel during the visit. The Trust should document and implement a recruitment plan with immediate effect to fill the short term vacancies but also consider its medium term requirements. Urgent In addition, the panel told by staff that middle grade doctors were covering for each other while the one slept during the night. Nursing staff were unaware of nd the location of the 2 middle grade doctor during this time which raises serious questions about clinical governance. The Trust confirmed this issue is being investigated by its local counter fraud service (LCFS). Staff told us that changes made to wards i.e. opening more beds were not accompanied by associated staffing increases. This was noted in the Hyper Acute Stroke Unit as in April 2012, capacity was increased from 22 to 28 beds, with no subsequent increase in staff to meet the additional capacity. It was noted that there is a standard ratio for nurses to patients on this ward and that at present this ratio is not being met. This is also the case at Lincoln hospital. The Trust informed us that the staffing establishment at the stroke unit at Pilgrim Hospital was 30.43 WTE prior to the business case investment that increased capacity from 22 to 28 beds. After the business case investment, the staffing establishment rose to 39.90 WTE. The Lincoln 28 bedded stroke unit is similarly staffed. (ii) Workforce planning is poor with no recruitment plans and no plans in place to cover maternity leave, sickness and annual leave other than through the use of agency, bank staff or, in the case of medical staffing, locums. The panel identified a number of gaps in the establishment numbers of various wards and specialities. Most notably, we were informed by staff that there was a 20% vacancy rate for AHPs in Boston and a 10% vacancy rate in Grantham. It should be noted that the above vacancy rates were not recognised by the executive team who state that vacancy rates are proactively managed by Therapy Management and posts are being held vacant to respond to the The Trust should seek to firm up its strategic plan, including the level of service provision at all three main hospital sites and the community sites. Student nurse posts should be 45 Outstanding concerns based on evidence gathered significant reduction in GP-referred MSK patients as a result of an AQP initiative in Lincolnshire. Key planned improvements Recommended actions Priority – urgent, high or medium advertised earlier. The panel felt that gaps had a disproportionate effect on Grantham Hospital due to its relative smaller size. The panel also noted that the uncertainties surrounding the future provision of services at Grantham Hospital could act as a deterrent for applicants. The Shaping Health for Mid Kesteven review which has now been finalised and made public reinforces the future of services at Grantham Hospital. We were told by clinicians and managers throughout the Trust that there were difficulties recruiting into existing vacancies and staff were not hopeful that the additional planned recruitment would be filled. In addition, student nurses told us that posts were advertised by the Trust later than others and this led to many of them applying for and accepting jobs elsewhere when they would like to work at ULH. The panel identified that if effective workforce planning is implemented, this will assist the Trust with its agency spend and also its high levels of sickness absence. When the panel engaged with staff, they opened up and gave us their views, the Trust should build upon this to create a cohesive team across management and the clinical professions. 46 Outstanding concerns based on evidence gathered Key planned improvements The Trust has identified the following initiatives in place: Hospital at Night review to The lack of middle grade and consultants on site over night and at weekends conclude by mid-July 2013, indicated that there was a lack of supervision of junior doctors. Whilst all junior with agreed action plan doctors indicated that they felt they could approach the more senior clinicians Senior clinical staff presence and they were generally available and would come on site if required, the lack out of hours will be a feature of of on-site presence raised questions for the panel about supervision. the sustainability review, with In addition, the reduction in numbers of nursing staff overnight and at consideration given to the weekends raised question about capacity and supervision. viability of services Lincolnshire Sustainable Our review indicated some issues around out of hours and weekend cover at Services Review will explicitly Grantham Hospital but this was the better of the three sites we visited in terms consider the need for senior of staffing. clinical input out of hours and its impact upon site and service Our review identified positive feedback from student nurses in relation to their viability. experiences, support and mentoring (iii) Supervision was found to be inadequate, particularly out of hours Recommended actions Priority – urgent, high or medium The Trust should review its out of High hours and weekend cover and, if necessary, consider an on-site presence of consultants and senior nurses. 47 Safety Overview The key line of enquiry in relation to safety focussed on: How engaged staff are in the Trust’s quality strategy and staff views of the main barriers in the Trust to delivering high quality treatment and care for patients How the Trust reviews and monitors its patient safety indicators and what actions are taken to improve patient safety Summary of findings The following good practice was identified: Safety and quality dashboards displayed on the wards Staff aware of patient safety indicators and net promoter score A number of wards displayed key risks and lessons learnt from incidents Development of ‘A&E staff competency framework’ Proactive work around dementia in particular wards Staff competencies in maternity Pressure ulcer e-learning competencies The following areas of concern were identified: Quality strategy could not been communicated to staff and therefore could not be clearly articulated Staff do not routinely work across sites Lessons learnt from incidents and examples of good practice are not shared across specialties or across sites Staffing numbers described as main barrier to delivering quality of care Equipment management was identified as an issue across all three sites The panel observed a number of issues with the completion of DNAR forms Detailed Findings Good practice identified Every ward displayed some safety and quality information on the boards which was open for all staff, patients and visitors to see. This information includes pressure ulcers, falls, patient observations, VTE, dignity, nutrition, catheter management. Some wards also display more detailed analysis of safety and 48 quality metrics. All the staff were aware of patient safety indicators such as falls and pressure area care as well as their recent friends and family test results. The Waddington Unit at Lincoln County Hospital in particular was highlighted as an area which displayed a wealth of information including the current key risks to their service, any recent complaints and key lessons learnt from recent incidents. This was an excellent example of transparency. At Pilgrim Hospital there has been a development of an A&E staff competency framework which has taken all nurses back to the beginning, ensuring every member of staff is competent in the key areas. The competency assessment process now being introduced by the Matron, Sister and Nurse Consultant at Boston Pilgrim deserve special mention. The base lining of all staff against a new competency framework through demonstration of skills is an excellent tool to assess the abilities of all nursing staff, whilst also providing an evidence base against which Department training needs can be identified and then delivered. Wards 6A and 6B at Pilgrim Hospital in particular had improved the support for their dementia patients with the help of the Alzheimer’s Society. More information is included in KLOE 7. Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium (i) Quality strategy could not be articulated by all staff and non executive directors The Trust tells us that a structured patient safety and quality communication plan has been developed however this was not evidenced to the panel through discussion with staff on the ground. Confirm the key quality priorities for the Trust and communicate these widely to staff using campaigns and listening events as well as emails and the intranet. Urgent The Quality strategy has not been communicated effectively to site staff and therefore this could not be clearly articulated by the staff we spoke to. Without a clear quality strategy and shared goals among staff there are no consistent priorities across the three sites to improve the quality of care provided. A well understood quality strategy would help to engage staff to improve the quality of care. 49 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium (ii) Not all staff routinely work across sites and lessons learnt from incidents and examples of good practice are not shared across specialties or across sites The Trust informs us that it facilitates the cascade of good practice by means of patient safety newsletters and that Trust safety conferences are also specifically arranged to support this work. Develop a plan to rotate staff across the sites where appropriate, in particular where there is a risk of deskilling or where good practice and lessons learnt need to be shared more frequently. High The Trust also informs us that all SUIs are reviewed for quality and content by a group which includes the Medical Director and Director of Nursing. Lessons learned are discussed at the Sharing Lessons Learned forum which in turn informs the content of patient safety newsletters. The Trust should consider how to share across the specialties more regularly through governance processes and subcommittees. Not all staff types routinely work across sites which reduces the sharing of good practice and lessons learnt as well as potentially deskilling the staff that work in quieter areas. The panel noted the practical challenges that this may pose. For example, the nurses that work within paediatrics at Grantham hospital have seen a 50% drop in referrals in the last year and often only have 1 patient in the unit at a time. This significantly reduces the experience and knowledge they can gain compared to a member of staff working in Lincoln with a higher volume and complexity of patients. Lessons learnt from incidents and examples of good practice are also not shared regularly across specialties. (iii) Staffing numbers are described as main barrier to delivering quality of care That being said, these were not found to be embedded into the Trust’s processes through discussion with staff on the ground. See KLOE 5 (Workforce) See KLOE 5 (Workforce) N/A One of the wards where this issue was brought to the attention of the sister has already started to make improvements. Digby ward at Lincoln Hospital now includes the resuscitation trolley check in the handover, and if it has not been completed by the night staff it is A consistent approach to completing the High checklist and monitoring compliance should be determined and rolled out across the three sites. Staffing numbers were described as the main barrier to delivering quality of care in the majority of areas that the panel visited. This has been covered in more detail in KLOE 5 (Workforce). (iv) Equipment management was identified as an issue across all three sites. Equipment management was identified as an issue across all three sites; the majority of resuscitation trolleys that were reviewed had gaps in the daily check without the nurse in charge being aware. It appeared that this safety check was not 50 Outstanding concerns based on evidence gathered Key planned improvements embedded within the organisation or reviewed regularly to ensure compliance. completed first thing in the morning. Recommended actions Priority – urgent, high or medium See KLOE 10 N/A During the unannounced visit, it was identified that the defibrillator had not been checked on Bailgate and the nurse in charge did not know when it had last been done. The panel ensured the check was done before leaving the area. (v) The panel observed a number of issues with the completion of DNAR forms See KLOE 10 The panel observed a number of issues with the completion of DNAR forms. This has been covered further in KLOE 10. 51 General Medicine and Elderly Care Overview General medicine and elderly care were identified as key lines of enquiry based on review of the data pack and the information submitted by the Trust. The data pack identified the following issues in particular; Pneumonia and COPD are flagged as outliers under thoracic, general medicine and critical care for non elective for SHMI and under critical care, thoracic and general medicine for HSMR, The Health and Social Care Information Centre 30-day stroke mortality is high and improving substantially below the national average in the data to 2010-11 and; The Trust was rated “high” for mortality among diabetic patients, in a report published by the Yorkshire and Humber Public Health Observatory (YHPHO) and the National Diabetes Information Service. Summary of findings The following good practice was identified: Forget me not and ‘this is me’ for patients with dementia and cognitive impairments on 6A and 6B at Pilgrim Hospital. Involvement of the Alzheimer’s society. Mortality reviews are being carried out across medicine and junior doctors are involved in the process. Plan for every patient every day Electronic boards for patient location and separate board to use during board rounds (with plans to link these two). Quality metrics on boards to focus discussions and use of the safety cross for pressure ulcers. Stroke consultant had easy access to metrics relating to sinap data and could demonstrate progress – information available for all 3 sites from the governance team and benchmarked against national standards- also good engagement from multidisciplinary team and evidence of good thrombolysis rates. The following areas of concern were identified: Little evidence of care bundles being used effectively, There is clear evidence that whilst the ULHT Dementia programme is still in its early stages there is a clear strategy and action plan in progress which have been developed with commissioners and partner agencies. Pain control was found to be generally poor. Lack of awareness of the Mental Capacity and Deprivation of Liberty Act 2005. 52 Detailed Findings Good practice identified Stroke consultant had easy access to metrics relating to sinap data and could demonstrate progress – information available for all 3 sites from the governance team and benchmarked against national standards- also good engagement from multidisciplinary team and evidence of good thrombolysis rates ( Boston). The panel identified some areas of best practice on wards 6A and 6B at pilgrim hospital in relation to care of elderly patients with cognitive impairments. There were ‘forget me not’ magnets on the patient board to identify patients with dementia, although there did not appear to be as many as expected. Patients also had a ‘this is me’ document in their notes which is a simple and practical tool that people with dementia can use to tell staff about their needs, preferences, likes, dislikes and interests. This work has been supported by the Alzheimer’s society who provides three members of staff to Lincoln Hospital. Mortality reviews are being carried out across medicine; the panel understands that the Trust now review every death in medicine although the robustness of these reviews can vary between the three sites. Junior Doctors are also being included in the process for their learning and development. Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium (i) Lack of awareness of the Mental Capacity and Deprivation of Liberty Act 2005. Concerns were identified by the panel in relation to the Mental Capacity and Deprivation of Liberty Act 2005. The Trust has a Mental Capacity Act policy in place which it tells us is compliant with the necessary legislation and updated to reflect recent rulings in case law via the Court of Protection. This was not referred to by staff at ward level during our visit. Staff should ensure that they are fully compliant with mandatory training requirements and adult safeguarding is given clinical engagement as a matter of urgency. Urgent A particular patient was identified by a nurse consultant on the panel which raised concerns in relation to treatment for delirium. Nursing staff interviewed could not articulate the implications of the actions taken to prevent the patient from leaving the ward in relation to the Mental Capacity and Deprivation of Liberty Act 2005. Having asked for an expert opinion from the mental health nurse, the mental health nurse failed to follow the delirium guidelines, specifically for this patient; assessment of his painful leg, assessment of his 53 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium The Trust tells us that there is a pain prevention role in Grantham Hospital. We did not meet this person during our visit to Grantham. Audit cycle of pain assessment should be carried out and widely published with a campaign to improve awareness and compliance. High capacity and any deprivation of liberty issues. Having asked a number of Matrons, sisters and staff nurses the panel’s observations was that there is a lack of understanding of the Mental Capacity and Deprivation of Liberty Act 2005, the most common response was to ask the Trust safeguarding lead. (ii) Pain control was found to be generally poor There was consistent infrequent monitoring of pain documented on the vital signs charts across all 3 sites. The is no standardised pain assessment tool for people with dementia or other patients who cannot express if they are in pain verbally, for example, the Abbey Pain Scale. A patient with severe dementia and bedbound on ward 5 at Grantham was identified during the announced visit who was grimacing and moaning but had not had a pain assessment, although the staff could articulate how they would identify if a patient was in pain this particular patient had not been identified. The panel was informed that the Trust plans to implement to Abbey Pain Scale during quarter three, 2013-14. Introduction of pain assessment tool for people with dementia supported by the necessary training. The Trust should consider effective use of The panel was informed that the agreed mortality reduction plan care bundles and staff should be trained in There is little evidence of care bundles being used effectively across the has a clear roll out of care bundles order to deliver effective services. three sites. across the Trust. This process is to be overseen by the PMO. Recently the sepsis care bundle has been introduced, although a number of staff felt they had not been trained adequately and evidence suggested that it is not always being used effectively. On one surgical ward, the sister had ensured all her staff were trained in the new bundle – this followed an SUI related to sepsis. A matron reported that the bundle arrived on the wards but only about 30% of staff had been (iii) Little evidence of care bundles being used effectively Medium 54 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium None noted This best practice example should be shared and rolled out to all areas across the three sites which care for elderly patients and those with cognitive impairments. Medium trained in its use. The panel observed the Oncology ward at Lincoln using the sepsis bundle and we did see that a patient had been admitted the previous might because the bundle highlighted the need for admission. However, a relative at one of our patient listening events identified that her father was not admitted in a timely matter when he was septic following chemotherapy. The relative was told by a nurse that there were no beds in the hospital. The panel was told by a ward sister that this would no longer happen because of the sepsis bundle now in place. There is a Pneumonia care bundle being developed as a response to it being identified as an outlier. This has not yet been rolled out; the pace at which these care bundles are introduced is a concern and was highlighted by the Trust Board. (iv) Good practice above for dementia patients is not wide spread across the organisation The best practice identified above on wards 6A and 6B for dementia patients is not wide spread across the organisation. There were no other wards identified which used the ‘forget me not’ magnet to identify patients with dementia or consistent use of the ‘this is me’ leaflet. Support and training is required to ensure it is rolled out and used effectively. An awareness campaign should be considered. 55 Urgent Care Overview The panel’s focus on the management of the urgent care pathway arose from a review of A&E operational effectiveness, evidenced by Trust under performance. Department of Health data reviewed by the panel indicated that less than 95% of patients were seen, treated, discharged or admitted within 4 hours at Trust A&E Departments from January-December 2012. However, the Trust did achieve this target overall for the financial year 2012-13 but this varied between its three sites. Through observation of A&E Departments at 3 Trust sites (Grantham, Lincoln and Boston), associated staff interviews, focus groups and a review of documentation including the Board Integrated Performance Report, the panel reviewed the processes and effectiveness of the urgent care pathway within the Trust. Further investigation of A&E performance against the 4 hour target drawing on evidence provided in the Trust Board Performance Report of 29 April 2013, identified that the Trust overall and the A&E Department at Lincoln achieved the A&E 4 hour target in the period April 12- March 13. Whilst performance was below target at Boston in the same period, it was on an improvement trajectory from the performance seen in 2011. The view of the panel was that whilst the process improvements observed clearly needed to be supported and continued, there was not a systemic problem with A&E operational effectiveness, nor the urgent care pathway within the Trust. . Summary of findings The following good practice was identified: GP support within the Grantham A&E Department that enables the most appropriate care to be provided to the patient. Apart from enabling those patients who need GP care to receive it, the co-location also enables the reinforcement of messages to the public about when treatment within an A&E Department is appropriate. Panel members identified that despite staffing challenges, the engagement of and support provided by nursing staff deserved a positive commendation. The enquiries of panel members were dealt with professionally and courteously no matter what time of the day or shift. The observations of the inherent strength of the nursing leadership (at matron, nurse consultant and sister levels) and junior staff seen across the Trust, were also seen across the Emergency Departments, The competency assessment process now being introduced by the Matron, Sister and Nurse Consultant at Boston Pilgrim deserve special mention. The base lining of all staff against a new competency framework through demonstration of skills is an excellent tool to assess the abilities of all nursing staff, whilst also providing an evidence base against which Department training needs can be identified and then delivered. Strong Hospital at night team at Lincoln with very professional and effective hand over. The following areas of concern were identified: A&E performance trajectory is improving although remains below the 95% expected level Good practice is not routinely shared across the 3 Trust sites Urgent Care Staffing remains challenging Clarification is needed of consultant reviews 56 Escalation is left too late We identified a number of improvements already planned or underway at the Trust: The improvement in overall trust performance against the 95% target (underachievement in 2011/12 and achieved in 2012/13) is commended. The investment in infrastructure, service improvement and Board focus needs to be maintained in order to ensure that all sites exceed the required levels of performance. The A&E Matron at Boston informed panel members of an ‘A&E Strategy’ paper being taken to Board in July 2013. Given the historic underperformance at Boston, this attempt to ‘forward look’ and outline clinical and management strategy in order to ensure the delivery of safe and effective services that meet the needs of patients whilst sustaining minimum standards of performance (such as the A&E 4 Hour target) is commendable. The panel recommend that this work should be included in a clinical services strategy that addresses the needs of the public and how they are met from the sites that the Trust operates from. An Accident & Emergency strategy for Lincoln is in place. The sustainability review will consider as a priority, the clinical sustainability of the three A&E departments operating 24/7, given the national shortage of A&E consultants. Detailed Findings Good practice identified GP support within the Grantham A&E Department that enables the most appropriate care to be provided to the patient. Apart from enabling those patients who need GP care to receive it, the co-location also enables the reinforcement of messages to the public about when treatment within an A&E Department is appropriate. Panel members identified that despite staffing challenges, the engagement of and support provided by nursing staff deserved a positive commendation. The enquiries of panel members were dealt with professionally and courteously no matter what time of the day or shift. The observations of the inherent strength of the nursing leadership (at matron, nurse consultant and sister levels) and junior staff seen across the Trust, where also seen across the Emergency Departments. The competency assessment process now being introduced by the Matron, Sister and Nurse Consultant at Boston Pilgrim deserve special mention. The base lining of all staff against a new competency framework through demonstration of skills is an excellent tool to assess the abilities of all nursing staff, whilst also providing an evidence base against which Department training needs can be identified and then delivered. The multi disciplinary team (MDT) input at Grantham was viewed as very good and enabled rapid patient interventions and discharge within the Emergency Assessment Unit (EAU). The use of Dictaphone handover at Grantham was viewed as a simple but effective means of ensuring a timely and effective handover. 57 The Trusts internal urgent care board coordinates the development of A&E services. Outstanding concerns based on evidence gathered Key planned improvements (i) A&E performance trajectory is improving The Trust tells us that there is an Accident & Emergency although remains below the 95% expected level strategy for Lincoln in place. The panel noted that a Boston ‘A&E Strategy’ paper being Maintaining performance improvement trajectory and then sustaining A&E operational effectiveness. taken to Board in July 2013. The Trust informed us that A&E performance is to be considered by the sustainability review. (ii) Good practice is not routinely shared across the 3 Trust sites or between departments The Trust identified to the panel that urgent care standards are agreed pan-Trust however this did not come out in the review. Good practice is not routinely shared across the 3 Trust sites visited or indeed between departments. There does not appear to be any structure for sharing best practice across what was observed to be 3 distinct departments that had no common management or clinical structure. Recommended actions Priority – urgent, high or medium The panel recommend that this work should be included in a clinical services strategy that addresses the Urgent Care needs of the public and how they are met from the all sites that the Trust operate from. High The Director of Nursing and Director of Operations to review options and implement a process for sharing best practice. High Director of Operations to invite an ECIST review of practice along the Trust urgent care pathway. There is a particular opportunity to share the Nursing Competency framework developed at Boston across all sites. (iii) Urgent Care Staffing remains challenging The Trust identified a number of relevant actions will be undertaken, including: Given the overall and significant shortfall in nursing and clinical support High 58 Outstanding concerns based on evidence gathered Despite new appointments, staffing remains challenging with limited night clinical cover at Lincoln and nursing vacancies at Grantham. (iv) Clarification is needed of consultant reviews Key planned improvements International recruitment (for middle grades) Significantly increased cons numbers since Oct (at LCH from 1 to 6) Increased middle grade cover at nights Recommended actions Priority – urgent, high or medium at the Trust, the Board should continue to monitor recruitment progress and seek assurance on safe levels of staffing through routine reporting and unannounced reviews. Challenging the historic under recruitment to the Trust requires the active monitoring of service viability within an overall clinical services strategy. None noted Trust to review ward round processes and patient discharge policies. Medium The Trust informed the panel that risk assessment tools are active in A&E and MEAU at LCH, which by design lead to early escalation. These were not being fully utilised by staff during the review period. To review patient flow policy and supporting processes on all sites. Medium There appeared to be a general need on all sites for clarity on the daily process of consultant reviews including a programme of early ward rounds that could be repeated in order to assist early patient discharge. At Grantham, there did not appear to be any system of delegation for patient criteria based discharge. The panel notes that ‘daily senior ward round reliability’ and ‘time to senior review’ have been included in the medical process reliability dashboard, as documented within the Trust’s mortality reduction plan. (v) Escalation takes place too late with regard to ensuring patient flow is maintained The sense gained through conversation with staff that escalation within Grantham A&E was left to 59 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium late i.e. reactive once A&E full rather than proactively as demand increases and capacity decreases. Indeed the panel found no evidence of ongoing risk assessment to inform escalation at either the Lincoln or Grantham sites. The panel were told that admissions were, in part, due to inappropriately timed senior review and untimely observations (due to lack of nursing staff) that lead to delayed escalation of care. The panel observed that patients at Lincoln A&E were often moved in the last 15-20 minutes of the 4 hour window. These admission should have a clear plan earlier e.g. after 2 hours in A&E. See also KLOE2. 60 Obstetrics Overview The panel’s focus on obstetric and perinatal mortality was driven by HSMR data which indicated for the period January-December 2012, that perinatal conditions was one area with a greater number of deaths above the expected level. Through observation of the Obstetrics and Gynaecology Departments at 3 Trust sites (Grantham, Lincoln and Boston), associated staff interviews, focus groups and a review of documentation, the panel reviewed the delivery of patient services and the review processes around perinatal mortality. It became clear that the Trust had commenced its own review of the stillbirth rate, triggered by the Dr Foster HSMR data The report reviewed by the Quality and Safety Committee in May 2013 was based on a 2 year audit from January 2010 – January 2012 and showed that the stillbirth rate at Lincoln was below the national still birth rate in 2011 and 2012 (2.05 and 4.62 against the national rate of 5.2 per 1000). At Boston the still birth rate in 2011 was below the national average and just above in 2012 (4.1 and 5.3 against the national rate of 5.2 per 1000). The audit findings were not conclusive of any defining factors or common themes but did highlight the need to improve the accuracy of coding. It is clear that the Trust maintains a monthly focus on perinatal mortality through standing clinical governance arrangements and has action plans in place at both the Lincoln and Boston sites. The panel were assured that there were no underlying issues with respect to perinatal mortality, on the basis of the evidence presented and collected. Summary of findings The following good practice was identified: Completed [perinatal] mortality review and monthly perinatal mortality meetings where the multi disciplinary team (MDT) reviews mortality and morbidity. The development of a new competency development package at Lincoln for all new preceptor Band 5 staff which is being rolled out and will also be used with existing band 6 staff. A good escalation policy within the maternity unit which staff clearly understand. Good understanding of the patient complaints and Serious Incident processes. Early commencement in August 2013 of the Friends and Family Test. The following areas of concern were identified: The Trust has not reviewed mortality from February 2012 onwards. There was no clear information displayed at Grantham on how to provide patient feedback. Midwife driven service with little consultant engagement. 61 Whilst staffing did appear to have moved in line with establishment, the panel was not assured that the specialist staffing requirement was similarly matched nor that staffing levels were resilient. The panel noted the community midwife workload in the coastal area and short staffing of the team. Sensitivity of appointment scheduling of a multi disciplinary obstetrics and gynaecology clinic. Whilst the panel recognised the limitations of space, it was observed that particular care was required in scheduling Gynaecology and Obstetrics outpatient appointments in the women’s outpatient area at Grantham. Even if clinics for infertility, termination of pregnancy, antenatal etc are scheduled so as not to occur alongside each other, there is a need to clearly identify the clinic area, and consider the positioning and content of display board materials. Safety checks of equipment were not made. For all the above areas of concern, we identified a number of improvements already planned or underway at the Trust. The panel noted the recent review of staffing conducted using the Birthrate Plus model and the adjustments made. Staffing numbers need to be updated to include specialist staff. Risk investigation is well established. The panel would encourage the Trust to ensure that the process is owned and conducted by the full multi-disciplinary team. Detailed Findings Good practice identified Monthly MDT review of mortality and morbidity; and the submission of a stillbirth report to the Trust Quality and Safety Committee. The development of a new competency development package at Lincoln which is being rolled out to Band 5 and existing staff. A good escalation policy within the maternity unit which staff clearly understood. Early commencement in August 2013 of the Friends and Family Test. Joint investigation but from separate supervisory and management perspectives of incidents; this makes best use of time and minimises impact on staff. Birth after thought service offered by the Trust to all women. Change in practice in response to a complaint. e.g. Wheelchairs being provided to take Mothers to their transport on discharge following C-Sections. Eye catching and comprehensive Infection Control display board on Lincoln Nettleham ward. Comprehensive introduction to Lincoln ante/post natal ward by the ward sister which commenced with an explanation of staff uniforms. 62 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium (i) The Trust has not reviewed perinatal mortality trends although mortality is reviewed on a monthly basis Ongoing monthly reviews of mortality and morbidity The Trust should continue its review of the trends in perinatal mortality data for 2012 and provide an update to their current stillbirth report (informed by audit from Jan 2010- Jan 2012). High None noted Trust to clarify patient complaints, feedback High and advice arrangements (note this is a wider trust observation and is also included in KLOE 3) None noted To review capacity alongside policy and process to ensure that the requirements for consultant and MDT engagement are clarified to add value. High Birthrate Plus model recently used. Trust to confirm funding decision for additional midwifery staff and to update establishment to include specialist staff requirement. High Our review identified that the Trust had commenced its own review of the stillbirth rate, triggered by the Dr Foster HSMR data The report reviewed by the Quality and Safety Committee in May 2013 was based on a 2 year audit from January 2010 – January 2012. The monthly meetings do not cover trends in the perinatal mortality rates. (ii) There was no specific information displayed at Grantham antenatal clinic on providing feedback about maternity services at Grantham. No information on providing patient feedback was displayed at Grantham. (iii) Midwife driven service with little consultant engagement The service appears to be driven by midwives with little apparent consultant engagement even though the service is officially led by a Clinical Director. Whilst actual practice may be different, it is notable that the guidance flowchart for SI investigation does not include any consultant engagement in the process. (iv) Whilst the clinical component of birthrate plus has been applied, there was less assurance around the specialist staffing requirements and maintenance of resilience of staffing levels out of hours. The day to day challenges of staffing also become more acute when considering the tapering of staff over the day and night e.g. on Lincoln Nettleham Ward the staffing on the night shift is less than 50% of the 63 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium None noted Trust to review outpatient clinic scheduling and layout alongside display board materials High None noted Trust to action in accordance with own Safety and Quality requirements High day shift eg 7 trained and 2 untrained in the morning reducing to 5+2 later, reducing to 2+2 overnight. This ward also covers the transitional care area out the staffing described. The panel noted that whilst the workload of the community midwife team in the coastal area was as expected, the team was short staffed. This was recognised and this community team is currently not part of the on call escalation for supporting the labour ward. (v) Sensitivity of appointment scheduling of a multi disciplinary Obstetrics and Gynaecology clinic Whilst the panel recognised the limitations of space, it was observed that particular care was required in scheduling Gynaecology and Obstetrics outpatient appointments in one clinical area at Grantham. Even if clinics for infertility, termination of pregnancy, antenatal etc are scheduled so as not to occur alongside each other, there is a need to clearly identify the clinic area and consider the positioning and content of display board materials. (vi) Safety checks of equipment were not made There were gaps in daily checking of essential equipment on Lincoln labour ward. 64 Critical Care and Surgery Overview Critical care and surgery were identified as key lines of enquiry based on review of the data pack and the information submitted by the Trust. The data pack identified critical care medicine as a mortality outlier under both SHMI and HSMR. The panel also focussed on how the Trust is responding to the contributing factors such as deteriorating Early Warning Score (EWS) rates, shock cardiac arrest triggers and deteriorating renal function triggers within its crude surgical mortality rate. Summary of findings The following good practice was identified: Clear articulation of the Trust’s ‘track and trigger’ process for early warning of deteriorating patients and escalation. Outreach team and ‘hospital at night’ team. Surgical Emergency Assessment Unit (SEAU) triage and score all patients to prioritise and escalate. The following areas of concern were identified: The panel observed a number of issues with the completion of DNAR forms. There was a lack of understanding around why the Critical care pathway was identified as an outlier. The Trust often has insufficient capacity in its High Dependency Units (HDU) and Critical Care Units (CCU). Patients were in inappropriate clinical areas due to capacity issues. Detailed Findings Good practice identified The majority of staff that the panel spoke to during ward observations could clearly articulate the Trust’s ‘track and trigger’ process for early warning of deteriorating patients and escalation to medical staff although it should be noted that this is not in place at Pilgrim Hospital, Boston. There is an outreach team for critically ill and deteriorating patients; the team try to stop patients from requiring intensive care. The outreach team are covered by a ‘hospital at night’ team out of hours which consists of experienced nurses who support staff with critically ill patients. At Boston, however, the lack of outreach and hospital of night was raised as a problem. 65 SEAU (surgical emergency assessment unit) at Lincoln Hospital triage and score all patients on arrival to prioritise and escalate any who need immediate medical attention. SEAU was also an area where track and trigger was well understood by staff. Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium (i) We observed a number of issues with the completion of DNAR forms Pilgrim Hospital, Boston The panel looked at four DNAR forms on a ward and found the following matters: Only one was completed correctly with a MCA assessment and best interests supporting the decision. IMCAs had not been involved in decisions Lack of evidence of appropriate dialogue with patients There was some evidence of family involvement but not in all cases Consultant sign off had not taken place The Trust undertook an immediate review of DNAR forms in the hospitals and the current policy is going to be updated and matched with best practice from elsewhere. The Trust has already undertaken a review of all patients with DNAR forms to ensure they are accurately and adequately completed. This was completed immediately by the Trust. Urgent In addition, the Trust should review its process and policies for the completion for DNAR forms to ensure they meet best practice and legal requirements. We were present on the ward when a cardiac arrest took place during our unannounced visit and observed comments and discussion about whether a DNAR existed or not during resuscitation. The panel’s view was that staff were not aware of the process around DNAR and that they were not aware of the wishes of individual patients on the ward. On another ward we reviewed one DNAR form that had been completed appropriately and accurately. Lincoln County Hospital The panel looked at two DNAR forms on one ward at Lincoln County Hospital and the following issues were noted: One patient had two different DNAR forms among the notes, one completed in March and one in April Lack of evidence of appropriate dialogue with patients Neither form identified whether the decision not to resuscitate would be reviewed The nurse on the ward was not clear on which DNAR form 66 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium None noted. The Trust should ensure that there are appropriate escalation processes in place for managing deteriorating patients, including the use of outreach services to support the ‘hospital at night’ team. Staff should ensure that there is an appropriate response to escalation. High should apply. The panel was unable to identify any entry in the patient’s notes to suggest that a DNAR form was appropriate/needed Another patient had an active DNAR form dated June The DNAR form noted that the decision not to resuscitate would not be reviewed, the panel noted that the patient records identified the patient as 'MFFD' (medically fit for discharge) although it is recognised that a DNAR may remain appropriate even where patients no longer require acute hospital care. The panel looked at three DNAR forms on another ward and noted the following: One DNAR form did not identify whether the decision not to resuscitate would be reviewed Of the 3 DNAR forms examined by the panel, only 1 was fully completed but this one had not been discussed with the patient or relatives. (ii) The Trust has work to do in relation to its processes for escalating deteriorating patients and responding appropriately. Our review of critical care found that the Trust had undertaken significant work on its ICNARC (intensive care national audit and research centre) data which shows a strong performance in this area. The panel notes that the alert from HSMR and SHMI might reflect a sub group of patients, who were admitted and died within CCU, but when incorporated into the overall ICNARC data, did not result in the Trust being flagged as an outlier. The diagnostic groups included in critical care medicine with higher mortality in this alert are mainly pneumonia and septicaemia. The Trust has undertaken work on septicaemia with the sepsis bundle as discussed under KLOE for General Medicine and Elderly Care and the panel has been informed that some work has commenced on a care bundle for pneumonia. The Trust should move to embed the quality and safety work in a programme of improvement linked to the problems identified and aligning staff engagement to this work. The Trust should plan the medical workforce in the context of the specific problems relating to recruitment and 67 Outstanding concerns based on evidence gathered Key planned improvements Priority – urgent, high or medium engagement with the Local Education and Training Boards (LETB) in this. Whilst the panel had no fundamental concerns in this area, the panel identified that the Trust did not have sufficient outreach services on a 24/7 basis throughout the Trust and that escalation of deteriorating patients was not always well managed. Staff told us that they often felt unable to escalate deteriorating patients due to a lack of capacity. (iii) The Trust often has insufficient capacity in its High Dependency Units (HDU) and Critical Care Units (CCU) Recommended actions The Trust should clarify the quality governance arrangements and communicate arrangements to staff. None noted Review of and adherence to the Trust’s escalation plan, particularly in relation to discharge. High The panel was informed of the joint Review of and adherence to the Trust’s work being undertaken by the Trust escalation plan, particularly in relation to with primary care to minimise discharge. inappropriate admissions, especially end of life care. High The Trust often has insufficient capacity in its High Dependency Units (HDU) and Critical Care Units (CCU). However, the panel notes that HDU capacity is currently being reviewed at Pilgrim Hospital. This can result in some cancellations and holding patients in recovery for longer than usual while they wait for a bed to become free. This is often as a consequence of delayed discharges from the Trust as a whole rather than a capacity issue in HDU/ITU. Staff at Boston stated that patients were often waiting for a bed on the wards well after a decision to discharge. (iv) Patients were in inappropriate clinical areas due to capacity issues During the announced visit a number of patients were identified as being in inappropriate clinical areas with reasons cited by staff as due to capacity issues, particularly with the urgent care pathway. On the unannounced visit, it was recorded that 3 out of the 7 patients on Bailgate (short-stay unit at Lincoln Hospital) should have been in other wards as they required orthopaedic admission for surgery or rehabilitation. There is a risk associated with outliers that the patients do not receive the right quality of care from appropriate nursing and medical staff. 68 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium The Bostonian was used as a mixed ward of surgical and medical patients and there was no clear ‘medical team’ looking after the patients admitted with medical problems. Patients raised concerns at the focus group that they were outliers on surgical wards with infrequent visits by the parent medical team (both Lincoln and Boston patient focus groups), 69 5. Conclusions and support required The review identified a number of good areas of practice across the Trust, with some great examples of excellent care being delivered to patients. Some staff groups and particular individuals at the Trust also received praise. The review also identified a number of areas of outstanding concern across all ten key lines of enquiry which will require urgent or high priority action to address as identified in the detailed findings section. The Trust recognises that there are steps it needs to take to address the concerns raised by the review. Some improvement plans are already in motion, and the review team thinks these should be expedited. Other things may be areas that the Trust has not yet considered and the panel recommends the Trust quickly develops action plans to address these concerns. A number of these areas are recommended for discussion at the risk summit to consider what support may be required from the Trust to address these concerns. Urgent priority actions for consideration at the risk summit Problem identified Recommended Action for discussion Leadership and governance: The Trust should ensure there are clear and active discussion lines between the clinical leaders at ward level, the clinical directors and the Trust Board to ensure that leadership of the organisation is joined up and consistent. The Trust should focus on engaging clinical teams rather than specialties or separate professional groups. There is a disconnect between leadership at Board level and leadership at clinical levels within the organisation (page 24). Support required by the Trust The Executive Team recognise the need to build stronger connections between leadership at Board level and leadership at clinical level. It is critical that this recognition is adopted across the entire Trust, by all staff groups and by the whole Board. Clinical and operational effectiveness: The panel was unable to easily see or understand how escalation worked for both actions taken in managing deteriorating patients and also managing patient flow as there seemed to be no standardised process in operation across the specialties and sites (page 32). The Trust should seek to clarify its escalation policy and ensure that it uses the ‘track and trigger’ system effectively across all the Trust sites. Staff should ensure that escalation responses are appropriate and well documented in response to managing deteriorating patients. In addition the Trust should ensure that patient flow is planned and managed appropriately and there is consistent and early use of existing escalation policy. An IT solution needs to be found to allow the ambulance inbound system to be visible in A&E. 70 Problem identified Recommended Action for discussion Patient experience: The Director of Nursing and the Company Secretary should review the handling of complaints and the processes whereby complaints can be systematically fed back and used by staff teams to improve service delivery. This should include creation of PALs. Complaints should be seen as everyone’s responsibility – not just the complaints team / Board. The complaints process is confusing and not fit for purpose (page 37). Patient experience: Patient experience is not seen by patients to be at the heart of the organisation and service improvement (page 38). Workforce: Staffing levels were, in some areas and at certain times of the day, low. The panel formally escalated its concerns to the CQC (page 41 - 45). Support required by the Trust The Trust should implement a patient experience action focussed improvement plan that should include: real time patient feedback evidence of listening and responding Using and working with patients to co-design service improvement The whole trust staff should engage with this process. The Trust should urgently implement the recommendations of its nurse staffing review, in particular taking account of: nursing numbers and appropriate use of agency and bank staff; Matron cover at Pilgrim Hospital, Boston; dependency of patients including 1:1 care, assistance with eating and assistance using toileting facilities. The Trust should also consider urgently middle grade cover and appropriate supervision of junior doctors, especially out of hours. Workforce: Workforce planning is poor with no recruitment plans and no plans in place to cover maternity leave, sickness and annual leave other than through the use of agency, bank staff or, in the case of medical staffing, locums (page 46 - 47). Safety: The Trust should document and implemented a recruitment plan with immediate effect to fill the short term vacancies but also consider its medium term requirements. The Trust should also seek to firm up its strategic plans, including the level of future service provision at all three main hospital sites and the community sites. This should be done in conjunction with stakeholders. Student nurse posts should be advertised earlier. The Trust should continue to confirm and communicate its key quality priorities for the Trust to staff using campaigns and listening events as well as emails, the 71 Problem identified Recommended Action for discussion Quality strategy has not been communicated effectively and therefore could not be articulated by all staff and non executive directors (page 50). intranet and Ward to Board initiatives. General Medicine and Elderly Care: Staff should ensure that they are fully compliant with mandatory training requirements and adult safeguarding should be given clinical engagement as a matter of urgency. Lack of awareness of the Mental Capacity and Deprivation of Liberty Act 2005 in relation to the Trust’s responsibilities in allowing patients to leave wards if they are deemed capable and wish to (page 54 - 55). Critical Care and Surgery: We observed a number of issues with the completion of DNAR forms (page 67 -68). Support required by the Trust The Trust has already undertaken an immediate review of all patients with DNAR forms to ensure they are accurately and adequately completed. This was completed immediately by the Trust. The Trust should review its process and policies for the completion for DNAR forms to ensure they meet best practice and legal requirements. 72 Appendices 73 Appendix I: SHMI and HSMR definitions HSMR definition What is the Hospital Standardised Mortality Ratio? The Hospital Standardised Mortality Ratio (HSMR) is an indicator of healthcare quality that measures whether the mortality rate at a hospital is higher or lower than you would expect. Like all statistical indicators, HSMR is not perfect. If a hospital has a high HSMR, it cannot be said for certain that this reflects failings in the care provided by the hospital. However, it can be a warning sign that things are going wrong. How does HSMR work? The HSMR is a ratio of the observed number of in-hospital deaths at the end of a continuous inpatient spell to the expected number of in-hospital deaths (multiplied by 100) for 56 specific groups (CCS groups); in a specified patient group. The expected deaths are calculated from logistic regression models taking into account and adjusting for a case-mix of: age band, sex, deprivation, interaction between age band and co-morbidities, month of admission, admission method, source of admission, the presence of palliative care, number of previous emergency admissions and financial year of discharge. How should HSMR be interpreted? Care is needed in interpreting these results. Although a score of 100 indicates that the observed number of deaths matched the expected number; in order to identify if variation from this is significant confidence intervals are calculated. A Poisson distribution model is used to calculate 95% and 99.9% confidence intervals and only when these have been crossed is performance classed as higher or lower than expected. SHMI definition What is the Summary Hospital-level Mortality Indicator? The Summary level Hospital Mortality Indicator (SHMI) is a high level hospital mortality indicator that is published by the Department of Health on a quarterly basis. The SHMI follows a similar principle to the general standardised mortality ratio; a measure based upon a nationally expected value. SHMI can be used as a potential smoke alarm for potential deviations away from regular practice. How does SHMI work? 1) Deaths up to 30 days post acute trust discharge are considered in the mortality indicator, utilising ONS data 2) The SHMI is the ratio of the Observed number of deaths in a Trust vs. Expected number of deaths over a period of time 3) The Indicator will utilise 5 factors to adjust mortality rates by a. b. c. d. e. The primary admitting diagnosis The type of admission A calculation of co-morbid complexity (Charlson Index of co-morbidities) Age Sex 74 4) All inpatient mortalities that occur within a Hospital are considered in the indicator How should SHMI be interpreted? Due to the complexities of hospital care and the high variation in the statistical models all deviations from the expected are highlighted using a Random Effects funnel plot Some key differences between SHMI and HSMR Indicator Are all hospital deaths included? When a patient dies how many times is this counted? HSMR No, around 80% of in hospital deaths are included, which varies significantly dependent upon the services provided by each hospital If a patient is transferred between hospitals within 2 days the death is counted multiple times Does the use of the palliative care code reduce the relative impact of a death on the indicator? Does the indicator consider where deaths occur? Yes Is this applied to all health care providers? Yes Only considers in hospital deaths SHMI Yes all deaths are included 1 death is counted once, and if the patient is transferred the death is attached to the last acute/secondary care provider No Considers in hospital deaths but also those up to 30 days post discharge anywhere too. No, does not apply to specialist hospitals 75 Appendix II: Panel Composition Panel role Panel Chair Name Panel role Name Ruth May Board Level Nurse Marion Collict Lay representative (Patient/public representative) Jackie Wilkinson Board Level Nurse Lynne Wigens Board Level Nurse Pol Toner Lay representative (Patient/public representative) Jean Gallagher Lay representative (Patient/public representative) Howard Naylor Junior Doctor Nassim Parvizi Junior Doctor Saheel Mukhtar Doctor Mike Lambert Doctor Charles Mann Doctor Sonia Swart Doctor Geoff Hunnam Student Nurse Jane Philpott Student Nurse Madalina Veturia Fabian Board Level Nurse Senior Nurse Birte Harlev Lam Senior Nurse Vicki Leah CQC representative Alan Swain Senior Trust Manager Cara Charles Barks Senior Regional Support Mark Driver Senior Regional Support Trish Thompson Senior Regional Support Shelley Bewsher CCG Observer Wendy Martin Area Team Observer Aly Rashid Area Team Observer Manjit Darby Nancy Fontaine 76 Appendix III: Interviews held on announced visit Interviewees Date held Vice Chairman, Chief Executive, Chair and Director of Performance and Improvement 17 June Interim Medical Director, Medical Director (not yet in post), Deputy Director of Nursing, Head of Quality, Interim Director of Quality Governance 17 June Director of Operations, Director of Human Resources and Non Executive Directors 17 June Complaints Team 18 June Interim Director of Nursing 18 June CCGs 18 June Deputy Director of Patient Services 19 June Deputy Director of Operations 19 June Chair of Audit Committee and Vice Chairman and Chair of Governors 19 June 77 Appendix IV: Observations undertaken Observation area Date of observation Grantham Hospital Observation area Date of observation MEAU 18 June Obstetrics and Gynaecology 17 June Oncology 18 June Accident and Emergency 17 June Stroke Ward 18 June CCU 17 June Theatres 18 June Respiratory 17 June Digby Ward 18 June Maternity 17 June SEAU 18 June General Surgery and Theatres 17 June Stow Ward 18 June Outpatients 17 June Shuttleworth Ward 18 June Rehabilitation 17 June Mitchell Ward 18 June EAU 17 June Navenby Ward 18 June MMU 17 June Paediatrics - Rainforest Ward 18 June Stroke – Ward 1 17 June Paediatrics - Safari Ward 18 June SEAU Ward 18 June Lincoln County Hospital EAU 18 June Burton Ward 18 June Accident and Emergency 18 June Johnstone Ward 18 June Maternity 18 June ICU 18 June Obstetrics 18 June Hatton Ward 20 June Gynaecology 18 June Digby Ward 20 June 78 SEAU 20 June CDU 20 June A&E 20 June Ward 5A – General Surgery 20 June Ward 8B – Cardiology Ward 20 June Pilgrim Hospital, Boston Maternity 19 June Ward 7B – Respiratory 20 June Obstetrics 19 June Ward 3A – Elective Orthopaedics/ Ophthalmology 20 June Gynaecology 19 June Ward 3B - Trauma and Orthopaedics 20 June Vascular Ward 19 June A&E 20 June Gastro Ward 19 June CCU 19 June ICU 19 June Bostonian 19 June Accident and Emergency 19 June CDU 19 June 6A and 6B – Elderly Care Wards 19 June Stroke Ward 19 June 7A and 7B 19 June Theatres and Recovery 19 June 2b – Day case Ward 19 June Labour Ward 19 June Ward 6A – Elderly Care 20 June Ward 6B – Elderly Care 20 June 79 Appendix V: Focus groups held Focus group invitees Focus group attendees Date held Trainee Nurses and Junior Doctors - Grantham 18 registered attendees 17 June Senior Doctors and Senior Staff - Grantham 26 registered attendees 17 June Senior Nurses - Grantham 15 registered attendees 17 June Other health professionals and non clinical staff - Grantham 18 registered attendees 17 June Trainee Nurses and Junior Doctors - Lincoln 18 registered attendees 18 June Senior Doctors and Senior Staff - Lincoln 24 registered attendees 18 June Senior Nurses - Lincoln 22 registered attendees 18 June Other health professionals and non clinical staff - Lincoln 29 registered attendees 18 June Trainee Nurses and Junior Doctors - Boston 26 registered attendees 19 June Senior Doctors - Boston Were seen individually 19 June Senior Nurses - Boston 42 registered attendees 19 June Other health professionals and non clinical staff - Boston 26 registered attendees 19 June 80 Appendix VI: Information available to the RRR panel Customer Care Screening Tool Patient Experience (G. Collier) CSAS Incident Report 04/1/2013 Serious Incident Investigation Report Jun-13 CSAS Incident Report 04/06/2013 Serious Incident Investigation Report May-13 CSAS Incident Report Apr-13 Serious Incident Investigation Report Apr-13 CSAS Incident Report Apr-13 Ward Information Pilgrim Hospital Mar-13 Dixon ward info and FFT comments Dixon ward graphs Inpatient care quality audit and patient feedback 02-May-13 Medicine administration competency 2012-2013 Sepsis training Track and Trigger 2012 Track and Trigger 2013 Band 5 time out day agenda/attendance list Medications Management 04-Jul-12 Quality review 25-Apr Quality governance-internal review of compliance (stow, Clayton and Dixon) 23Apr-12 Process product FMEA 03/11/2011 Ward list Process product FMEA 17/01/2012 Process product FMEA 17/01/2012 Process product FMEA 03/11/2011 ULHT Annual Plan 2013-14 ULH - Financial Plan - 2013-14 ULH Future Mgmt Arrangements 08/11/2010 Pilgrim Management Group Meeting Minutes 28Feb-13 Vascular service option appraisal 20-Jun-11 East Midlands Vascular Network - requirements to centralise vascular inpatient services Management of behaviour and psychiatric symptoms of dementia (BPSD) Feb-12 Pilgrim Management Group Meeting Minutes 25-Apr-13 Notes of Vascular Hub Options Appraisal Meeting 27Apr-11 Vascular timeline 2011 Letter from MD and DoN Feb-13 Email re CIPs and QIA 29-Apr-13 CSAS Incident Report Aug-12 ULH org chart ULH In-patient care going home survey (incl Friends and Family test) Alzheimer’s society - 'this is me' leaflet Track and Trigger Step Up chart Midwives day and night checking and cleaning list (13/5/13 18/6/13) 17-Jun-13 ULH Proforma for the management of drug incidents errors 81 Work roster - Digby short stay (June July 2013) Consultant info card template Aug-10 A&E daily activity sheet template May - 13 Managing long waiting patients in A&E through escalation Lincoln A&E patient flow - chart A&E clinical quality indicators 09-Jun-13 1to1 ward sister report for matrons monthly meeting (template) 28.5.12 Patient Experience (Alan Tolley) Jun-13 Work roster - GDH ward 2 (may June 2013) EAU GP Referral Form (template) Grantham Exclusion Protocol 21/09/2012 Grantham Admission Protocol 21/09/2012 Advice sheet - acute back pain Advice sheet - high temperature (child) Advice sheet - chest injury Friends and Family template Perinatal meeting learning points - May 13 07-May13 Perinatal meeting attendance list - May 13 07May-13 Perinatal meeting learning points - March 13 13-Mar-13 Perinatal meeting attendance list - March 13 13Mar-13 Perinatal meeting learning points - March 13 13-Mar-13 Perinatal meeting learning points - Jan 13 10-Jan-13 Perinatal meeting learning points - Dec 13 07Dec-13 Perinatal meeting attendance list - Oct 12 04-Oct-12 Perinatal meeting learning points - Oct 12 04-Oct-12 Perinatal meeting learning points June 12 09Jun-12 Perinatal meeting learning points - June 12 08/06/2012 Perinatal meeting attendance list - April 12 27-Apr-12 Perinatal meeting learning points - April 12 27Apr-12 Perinatal meeting learning points - March 12 06Mar-12 Perinatal meeting learning points - March 12 Mar-12 Paediatric Gov Meeting Dates 2013 2014 V4 Minutes of the Private Trust Board Meeting 07-May-13 Minutes of the Private Extra Trust Board Meeting - 22 May 2013 22-May-13 Alex Ward Admission Criteria Management structure, deputies May-12 Management structure, deputies 3.1A May-12 Dixon ward action plan 06-Jun-13 Handover sheet sdm (7.6.13 8.6.13 - night. SDM= Stephens) Jun-13 Lincoln operational escalation policy 14/11/2012 Opening beds checklist – Clayton 16/03/2013 ULH org chart work roster - Digby short stay (may June 2013) 82 Opening beds checklist - template Lincoln Site Adverse weather plan - 12/13 06.11.12 Lincoln A and E escalation plan Dec-12 Outlier policy for medicine Jan-13 Trust wide outlier policy Reviewed Aug 2012 DRAFT Aug12 SOP for the repatriation of patients Mar-13 SOP for outlying surgical patients 10-Jan-13 SOP for staff support with increased demand in A&E Incident policy final revised Jan 13 (FINAL)[1] 08Jan-13 Clinical Systems Analysis Manual v1.2 Clinical Systems Analysis and contextual risk factors Mortality Reduction - Saving lives in Lincolnshire 11/06/2013 Mortality and Quality of Care - Internal Review 01/05/2013 Mortality reviews carried out and ongoing – June 2013 01/06/2013 SQD data - pressure ulcers - June13 01/06/2013 Pressure Ulcer performance March 2013 17/06/2013 Raw data from PUNT pressure ulcer management tool Cat 3 and 4 March 2013 Mar-13 WHISTLE BLOWING POLICY draft5 2013.03 Lincoln site scorecard Mar-13 Medicine and A&E Lincoln Scorecard March 2013 Mar-13 INTEGRATED PERFORMANCE REPORT PERIOD TO 30th April 2013 28-May-13 UROLOGY BUSINESS IMPROVEMENT PLAN 2013 - project groups - version2 18/04/2013 Urology Business Plan 2013 v9 Shaping Health for Mid Kesteven - Consultation Cure Lincolnshire submission20-Febto review team 13 Letter from Chief Exec of Lincolnshire Partnership NHS Trust to Sir Bruce Keogh Record of PNM&M Attendances 83 Appendix VII: Unannounced site visit Agenda item Lincoln County Hospital Entry into Lincoln County Hospital and announced arrival to site manager Accident & Emergency Observations undertaken of the following: Accident & Emergency Hatton and Digby Wards SEAU Meeting held with site manager to understand current staffing and patient levels Panel left Trust and announced exit Pilgrim Hospital, Boston Entry into Pilgrim Hospital, Boston and announced arrival to site manager Observations undertaken of the following: Accident & Emergency Wards 3A and 3B Wards 6A and 6B Ward 5A Ward 8B Ward 7B Meeting held with site manager to understand current staffing and patient levels Panel left Trust and announced exit 84