Review into the Quality of Care and Treatment provided by
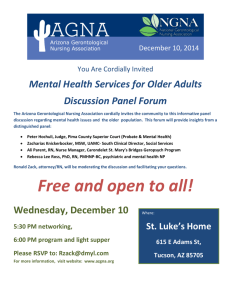
advertisement

Tameside Hospital NHS Foundation Trust Review into the Quality of Care and Treatment provided by 14 Hospital Trusts in England RAPID RESPONSIVE REVIEW REPORT FOR RISK SUMMIT July 2013 Contents 1. Introduction 3 2. Background to the Trust 7 3. Key Lines of Enquiry 11 4. Review findings 12 5. Governance and leadership 16 Clinical and operational effectiveness 25 Patient experience 31 Workforce and safety 39 Conclusions and support required Appendices 44 46 Appendix I: SHMI and HSMR definitions 47 Appendix II: Panel composition 49 Appendix III: Interviews held on announced visit 50 Appendix IV: Observations undertaken 51 Appendix V: Focus groups held 52 Appendix VI: Information made available to the panel by the Trust 53 Appendix VII: Unannounced site visit 55 2 1. Introduction Overview of review process On 6 February 2013 the Prime Minister asked Professor Sir Bruce Keogh, NHS England Medical Director, to review the quality of the care and treatment being provided by those hospital trusts in England that have been persistent outliers on mortality statistics. The 14 NHS trusts which fall within the scope of this review were selected on the basis that they have been outliers for the last two consecutive years on either the Summary Hospital level Mortality Indicator (SHMI) or the Hospital Standardised Mortality Ratio (HSMR). Definitions of SHMI and HSMR are included at Appendix I. These two measures are intended to be used in the context of this review as a ‘smoke alarm’ for identifying potential problems affecting the quality of patient care and treatment at the trusts which warrant further review. It was intended that these measures should not be reviewed in isolation and no judgements were made at the start of the review about the actual quality of care being provided to patients at the trusts. Key principles of the review The review process applied to all 14 NHS trusts was designed to embed the following principles: 1) Patient and public participation – public representatives played a key role and worked in partnership with clinicians on the reviewing panel. The panel sought the views of the patients in each of the hospitals and also considered independent feedback from stakeholders, related to the Trust, which had been received through the Keogh review website. These themes have been reflected in the reports. 2) Listening to the views of staff – staff were supported to provide frank and honest opinions about the quality of care provided to hospital patients. 3) Openness and transparency – all possible information and intelligence relating to the review and individual investigations will be publicly available. 4) Cooperation between organisations – each review was built around strong cooperation between different organisations that make up the health system, placing the interests of patients first at all times. Terms of reference of the review The review process was designed by a team of clinicians and other key stakeholders identified by NHS England, based on the NHS National Quality Board guidance on rapid responsive reviews and risk summits. The process was designed to: Determine whether there are any sustained failings in the quality of care and treatment being provided to patients at these Trusts. Identify: i. Whether existing action by these Trusts to improve quality is adequate and whether any additional steps should be taken. ii. Any additional external support that should be made available to these Trusts to help them improve. 3 iii. Any areas that may require regulatory action in order to protect patients. The review follows a three stage process: Stage 1 – Information gathering and analysis This stage used information and data held across the NHS and other public bodies to prepare analysis in relation to clinical quality and outcomes as well as patient and staff views and feedback. The indicators for each trust were compared to appropriate benchmarks to identify any outliers for further investigation in the rapid responsive review stage as Key Lines of Enquiry (KLOEs). The data pack for each trust reviewed is published at http://www.nhs.uk/NHSEngland/bruce-keogh-review/Documents/trust-datapacks/tamside-data-packs-PUBLISH.pdf. Stage 2 – Rapid Responsive Review (RRR) A team of experienced clinicians, patients, managers and regulators (see Appendix II for panel composition), following training, visited each of the 14 hospitals and observed the hospital in action. This involved walking the wards and departments, interviewing patients, trainees, staff and members of the Board. The report from this stage was considered at the risk summit. Stage 3 – Risk Summit This brought together a separate group of experts from across health organisations, including the regulatory bodies. They considered the report from the RRR, alongside other hard and soft intelligence, in order to make judgements about the quality of care being provided and agree any necessary actions, including offers of support to the hospitals concerned. A report following each risk summit has been made publicly available. Methods of investigation The two day announced RRR visit took place at the Trust’s main hospital, Tameside Hospital on Thursday 23 and Friday 24 May 2013. A variety of review methods were used to investigate the KLOEs and this enabled the panel to consider evidence from multiple sources in making their judgements. The visit included the following methods of investigation: Interviews Nineteen interviews took place with members of the Board and selected members of staff based on the key lines of enquiry during the announced visit. See Appendix III for details of the interviews undertaken. An interview was also held with the Trust’s Governors attended by three members of the Council of Governors. 4 Observations Ward observations enabled the panel to see the Trust undergo its day to day operations. They allowed the panel to talk to current patients, and their families where observations took placed during visiting hours. They allowed the panel to speak with a range of staff and observe the quality of care and treatment being provided to patients. The panel was able to observe the action by the Trust to improve quality in practice and consider whether any additional steps should be taken. Observations took place in eleven areas of Tameside hospital. See Appendix IV for details of the observations undertaken. Focus groups Focus groups provided an opportunity to talk to staff groups individually to ask each area of staff what they feel is good about patient care in the Trust and what needs improving. They enabled staff to speak up if they feel there is a barrier that is preventing them from providing good quality care to patients and what actions the Trust might need to consider improving, including addressing areas with higher than expected mortality indicators. Focus groups were held with four staff groups during the announced site visit. See Appendix V for details of the focus groups held. The panel would like to thank all those attending the focus groups who were open with the sharing of their experiences and balanced in their perceptions of the quality of care and treatment at the Trust. Listening event Public listening events give the public an opportunity to share their personal experiences with the hospital, and to voice their opinion on what they feel works well or needs improving at the Trust in relation to the quality of patient care and treatment. A listening event for the public and patients was held on the evening of 23 May 2013 at Dukinfield Town Hall. This was an open event, publicised locally, and attended by more than 200 members of the public and patients. The panel would like to thank all those attending the listening event who were open in sharing of their experiences and balanced in their perceptions of the quality of care and treatment at the Trust. Review of documentation A number of documents were provided to the panellists through a copy being available in the panel’s ‘base location’ at the Trust during the site visit. Whilst not all the documents were reviewed in detail, they were available to the panellists to validate findings as considered appropriate by the panellists. See Appendix VI for details of the documents available to the panel. Unannounced visit The unannounced out-of-hours visit took place at Tameside Hospital on the evening of Sunday 2 June and morning of Monday 3 June 2013. This focused observations in areas identified from the announced site visit, see Appendix VII. Follow-up discussions were held with a few members of staff already interviewed during the announced visit. 5 Next steps This report has been produced by Gill Harris, Panel Chair, with the full support and input of panel members. It has been shared with the Trust for a factual accuracy check. This report was issued to attendees at the risk summit, which focussed on supporting Tameside Hospital NHS Foundation Trust (“the Trust”) in addressing the actions identified to improve the quality of care and treatment. Following the risk summit the agreed action plan will be published alongside this report on the Keogh review website. A report summarising the findings and actions arising from the 14 investigations will also be published. 6 2. Background to the Trust This section of the report provides relevant background information for the Trust and highlights the areas identified from the data pack for further investigation. Context Tameside Hospital NHS Foundation Trust is the principal provider of acute hospital services for the residents of Tameside in Greater Manchester and the town of Glossop in Derbyshire. The Trust operates from the Tameside General Hospital site which is situated in Ashton-under-Lyne, and serves a population of approximately 250,000 people residing in Tameside and surrounding areas. It has a total of 502 beds and is a small Trust for both inpatient and outpatient activity relative to the rest of England. Tameside became a Foundation Trust on 1 February 2008. The hospital has four divisions: Emergency Services and Critical Care, Elective Services, Diagnostic and Therapeutic, and the Women and Children’s Division. General Medicine and General Surgery are the largest inpatient specialties, while Trauma and Orthopaedics and General Medicine are the largest for outpatients. Tameside falls within the most deprived quartile of counties in England. Teenage pregnancy and alcohol-related hospital stays for under-18 year olds are particularly common in this region, and violent crime and long-term unemployment are relatively more common than in England as a whole. The age distribution in Tameside is fairly similar to the national age distribution. Tameside’s health profile outlines that there are a number of aspects for which children’s and young people’s and adults’ health is significantly lower than the national average. The profile also shows that in Tameside life expectancy for both men and women is significantly lower than the national average. Key messages from the Trust data pack Mortality indicators The Trust was selected for this review as a result of its SHMI for 2011 and 2012 which were above the expected level. The Trust also reported an HSMR of 107 over the period January to December 2012, meaning that the number of actual deaths is higher than the expected level, but this was statistically still within the expected range. The Trust had an overall SHMI of 116 for the period between December 2011 to November 2012, meaning that the number of actual deaths is above the expected range. For both the SHMI and HSMR, the Trust’s non elective admissions were the main contributing factors for higher than expected mortality. Elective admissions were also above the expected range for SHMI, with a value of 166. The main diagnoses contributing to the SHMI and HSMR indicators were noted in general medicine (in particular, pneumonia, acute myocardial infarction (heart attack) and acute cerebrovascular disease (stroke)), so these were a focus identified for the review. The RRR visit included observations of the general medicine wards, specifically those caring for patients with these conditions, and interviews with patients and staff within these areas. 7 Governance and leadership The Trust Board has three main subcommittees, including the Quality and Clinical Governance Committee, which is chaired by a Non-Executive Director and provides assurance to the Board on quality. The Clinical Audit, Patient Safety and Effectiveness Committee is a subgroup of the Quality and Clinical Governance Committee and considers mortality each month. Board responsibility for clinical governance and quality is split between the Medical Director and Director of Nursing. Key risks identified by the Trust in the corporate risk register and other Board papers include ensuring that authorisation and registration requirements are maintained for key regulatory bodies; ensuring that factors impacting on mortality are understood, addressed and managed; capacity issues and their impact on patients; horizontal and vertical strategic partnership implementation in order to ensure critical mass of clinical services and 24/7 consultant cover to support non-elective emergency pathways. The Trust currently has a ‘red’ Monitor governance risk rating as it has been in significant breach of two of its terms of authorisation since 2011. The two areas of concern were; an unplanned financial risk rating of 2 and concerns raised in relation to safety and quality by a Care Quality Commission (CQC) review in 2011. The latest rating against CQC Outcomes is ‘green’ which represents “No concerns”. A high level review of the effectiveness of the Trust’s quality governance arrangements was a standard key line of enquiry for the review. Clinical and operating effectiveness In 2012, the Trust’s accident and emergency department (A&E) assessed and then treated, admitted or discharged as appropriate 95.8% of its patients within 4 hours, which is above the 95% national standard level. The Trust’s referral to treatment (RTT) within 18 weeks for admitted patients is 90.1% in the year to February 2013 which is higher than the national standard level. The data showed that the Trust has been performing above the target level throughout the last 12 months, although this has dropped in recent months. The Trust’s crude readmission rate, which is the percentage of patients that were discharged and then re-admitted within 30 days, is high when compared with trusts nationally at 13.10%. However, the standardised readmission rate, which accounts for the Trust’s case mix, shows that it is within the expected range. The average length of stay is 4.77 days which is shorter than the national mean average of 5.2 days. The only red flag for clinical and operational effectiveness is that relating to hip fracture mortality. In the National Hip Fracture Database, a key measure of effectiveness is the percentage of patients undergoing surgery within 36 hours of admission. On this measure, the Trust is an outlier, being some way outside the lower controls limits. The data in this area did not highlight any further Trust-specific key lines of enquiry. Patient experience Of the nine measures reviewed within Patient Experience and Complaints there are two which are rated ‘red’: The Inpatient survey: There were several areas of concern across the national inpatient survey 2012 results, including delays in being admitted to a ward, weaknesses in information given to patients on discharge, lack of patient involvement in decisions and being treated with respect and dignity. 8 Comments collected through CQC’s patient voice system: Whilst the majority of the comments recorded were positive, the negative comments included noteworthy allegations including those of ignoring formal whistle-blowing from a senior doctor, lack of healthcare worker professionalism, poor or disrespectful communication to patients and patients being bullied or shouted at. The Trust is A-rated by the Ombudsman which indicates a low risk of non-compliance with its recommendations. The Ombudsman investigates complaints escalated to it by complainants who are not satisfied with the Trust's response. It rates Trusts on whether they have implemented the recommendations made at the end of an investigation in a satisfactorily and timely manner, helping to ensure that Trusts learn from mistakes. The Ombudsman rates each Trust’s compliance with recommendations and focuses on monitoring organisations whose compliance history indicates that they present a risk of non-compliance. Keogh review patient voice comments The patient voice comments received directly via the contact details on the Keogh review website (at the time of writing this report) identified the following positive and negative themes from 57 e-mails and letters. Roughly 45% of comments were positive and 55% negative. Positive Negative Positive experience of hospital stay Poor quality of care Professional, caring and helpful staff Poor communication from staff Good treatment received; bed changed daily Misdiagnosis and follow-up treatment slow Caring nurses Poor standard of surgery Good care received in Cardiology Perception of negative impact of Chief Executive Lack of care for elderly – spoken to in unprofessional manner Poor cleanliness and hygiene of staff Poor level of patient safety as an inpatient Inadequate staffing Poor administration of outpatient appointments Key lines of enquiry were followed in the review based on what patients say about the quality of care and treatment and what the Trust is doing in response to this feedback. 9 Workforce and safety The Trust is ‘red rated’ in the following safety indicators: th For MRSA, the Trust has the 7 highest rate of infection of 141 trusts nationally over the three years from 2010 to 2012. For Clostridium difficile, the Trust had the second highest infection rates in the country over the same period. This highlighted infection prevention and control as a potential area for review. The Trust has the 35 highest percentage of patients harmed for the four safety thermometer indicators out of 141 non-specialist trusts. It experienced a harm rate of 10%, compared with the national average of 8.9%. However, it must be noted that due to potential differences in case mix and data collection practices at different organisations, definitive conclusions about differences in the burden of harm between organisations cannot be made. The Trust’s clinical negligence payments have significantly exceeded contributions to the ‘risk sharing scheme’ over the last three years, by a total of £21m over this period. This highlighted incident reporting and learning from incidents as an area for review. A review of the Coroner’s rule 43 reports highlighted a number of areas for potential review, including arrangements for transfer of patients between hospitals, communication procedures between staff, senior house officer and house officer staffing levels, staffing levels within A&E and the medical admissions unit (MAU), written procedures for handling incident reports, arrangements for nurses to summon help if required and record-keeping. th A review of the workforce data flagged five ‘red rated’ indicators: The Trust had a high agency spend over 2011/12 (9.4% of total staff costs) compared to the region median (3.5%). The data also shows that the three month vacancy rate for medical staff is over 50% higher than the national average rate and that the sickness absence rate for medical staff is nearly twice the national average. Whole Time Equivalent (WTE) nurses per bed day were 1.31 which was low compared with a national average of 1.96. Fifteen doctors in training commented on patient safety concerns in the National Training Scheme (NTS) survey 2012, representing 13.99% of respondents. This was nearly three times the national average of 4.7% and included concerns over supervision at the weekend, bed shortages and locum cover. Key lines of enquiry were included in the review focusing on how the Trust plans its workforce and its arrangements for patient safety. 10 3. Key Lines of Enquiry The Key Lines of Enquiry (KLOEs) were drafted using the following key inputs: The Trust data pack produced during the first stage and made publicly available. Documentation submitted by the Trust. Insights from the Trust’s lead Clinical Commissioning Group (CCG). Review of the patient voice feedback received specific to the Trust prior to the site visit. The KLOEs were agreed by the panellists during the panel briefing session held prior to the RRR site visit. The KLOEs identified for the Trust were the following: Theme Key Line of Enquiry Governance and leadership 1. Can the Trust clearly articulate its governance process for assuring the quality of treatment and care? 2. How does the Trust use information locally? Clinical and operational effectiveness 3. What governance arrangements does the Trust have to monitor and address clinical and operational performance data at a senior level? Patient experience 4. How does the Trust engage with stakeholders? 5. How is the Trust assured that its mission statement and values are achieved within its clinical pathways? Workforce and safety 6. In the context of this review, can the Trust describe its workforce strategy? 7. How is the Board assured that it has the necessary workforce deployed to deliver its quality objectives? 8. What assurance does the Board have that the organisation is safe? 11 4. Review findings Introduction This section provides a detailed analysis of the panel’s findings based on the evidence gathered from the Trust data pack, interviews, observations, staff focus groups and patient and public listening events. Overview of findings The panel found committed staff at the Trust and examples of good practice, but there were a number of areas of concern identified. The Trust should focus on urgently addressing these issues to improve the quality of care, patient safety and experience. 1. The clinical safety and experience of care for medical and elderly patients admitted via Accident and Emergency needs further review and urgent action to address operational issues The panel considered that external review recommendations to review and improve the acute medical pathway had not been sufficiently progressed by management. This has led to a number of systematic issues identified by the panel to be impacting on quality and patient safety. The most urgent requiring action are: Inadequate consultant supervision of junior doctors and patients, particularly at night Inadequate patient handover Inappropriate use of escalation areas and medical assessment unit beds to resolve capacity challenges Insufficient access to critical care beds for patients who may require them Insufficient nurse staffing levels and the use of nurses in escalation wards who are not regular staff on the wards Poor infection control practice for patients admitted with Clostridium difficile. Insufficient senior clinical cover, particularly out of hours, is leading to a lack of timely investigations and poor management of deteriorating patients in some areas, particularly the Medical Assessment Unit and Women’s Health Unit. The Trust urgently needs to ensure all acute patients receive a daily ward round review by senior medical staff. The Trust also needs to review its staffing levels and skill mix to improve medical cover arrangements and reduce the use of bank and agency, and locum cover. 2. The Board is not effectively leading the Trust in delivering quality care and the governance and leadership has not delivered the improvements in quality of care required The Board needs to improve its focus on quality improvement in the organisation as the panel considered that it has undertaken insufficient scrutiny and challenge of the executive team to establish how well the Trust is delivering in this area. It was recognised that the Board has received limited performance information to enable it to obtain 12 assurance on quality of care and treatment, but it has also not sought to effectively use all available information in the Trust to do so. This includes limited evidence of taking on board fully the views of its patients and staff. The Chairman was not able to confirm that he was fully assured of the quality of services provided in the hospital – during his interview he described being 60% assured and 40% reassured. Furthermore there appeared to be gaps in communication between the Chairman and Senior Independent Director. The Senior Independent Director could not describe what was on the Chairman’s worry list. From interviews, the panel considered that the Chief Executive’s approach to leading the organisation was overly operational and that the Chairman had not fully considered the impact of this leadership style on the executive team’s ability to fulfil their functions. In interviews with the Non-Executive Directors, it appeared that not all felt they could always effectively challenge at Board meetings because of a perception that the Chief Executive’s response would be unpredictable. As a consequence of these issues the strategic approach to improving care is not adequate and the panel was not convinced that the Board has the capability currently to fully address the cultural change required in the Trust. The Chairman should consider how the Board can address its overall leadership style urgently to drive quality improvement within the organisation. 3. The Quality Strategy and performance management information needs significant improvement Board members were not able to share a consistent view of what the Trust’s quality and safety priorities are because there is no single, cohesive quality strategy. Staff were equally unable to state what their priorities for improvement were or the progress that was being made in achieving these. The Trust has a number of action plans relating to quality and patient safety that must urgently be brought together into a quality strategy which can be effectively monitored at Board level. The recommendations of the Quality Governance Follow Up Review 2012 and other high priority action plans need to be implemented and the role of the Clinical Audit and Patient Safety Committee and Mortality Working Group clarified as part of the quality strategy. The Board does not receive on a monthly basis a comprehensive quality dashboard including performance information relating to CQUIN and quality account objectives. This would limit opportunities for the Board to address deviations in performance. Although the Trust has quality impact assessments of CIPs, these do not include selection of quality indicators for monitoring improvement or deterioration in care quality. The Board is also not receiving adequate information on mortality, for example on SHMI or escalated information from the Quality and Clinical Governance Committee, and therefore has insufficient focus on improving care in the relevant specialties. The Board must urgently agree a management information dashboard to underpin the quality strategy, to provide a mechanism for the Board to hold directorates to account for implementing improvements and to enable the Non Executive Directors to challenge the Board. Accountability for delivering patient quality needs to be embedded at every level of the organisation and individuals need to be held to account for delivering improvements. This will require ward level dissemination of quality priorities and monitoring arrangements so that all staff are clear on their role in delivery. 13 4. There is a need to develop the organisational culture to remove tolerance of sub-optimal care and engage more effectively with staff at all levels to improve quality and patient experience The Trust needs to review how it can improve its organisational culture to focus more on quality and patient experience. The panel did consider that the staff that were interviewed and observed were committed and loyal to the Trust and genuinely believed that they were providing good care, though they could not easily describe what good looked like or how they knew that care compared well to other providers. The frequent external reviews of the Trust and what was seen as constant criticism from the media is affecting the morale of staff. The Board should consider how it can listen more effectively to its staff to engage them further in its vision and improve the clinical leadership from both nurses and medical staff to further enable this. The panel observed acceptance of sub optimal standards of care across the organisation which the Trust needs to review and address, including: The response to patient complaints has been slow, brief, lacking in compassion, candour and accountability and learning from the complaints appears limited. Care bundle compliance was around 50% and although the Patient Safety Strategy includes an aspirational target of 75% (which the panel still considers to be low), no evidence of urgent action to increase compliance was provided. Low compliance undermines the purpose of care bundles to improve consistency of treatment and care. There was evidence of an acceptance of bed moves for non-clinical reasons (for example, a patient will undergo four bed moves before an incident is reported and investigated), poor discharge planning and other operational drivers overriding the ability of staff to provide good patient experience. Poor quality mortality reviews and clinical audits with limited evidence of lessons learnt from when things went wrong. 5. There is a need to improve patient and public engagement The Panel did not see clear evidence that the Board is listening to patients and families to improve the quality of patients’ experience. This is essential to set a cultural tone for staff that is in line with the stated objectives of initiatives, such as Everyone Matters, and provide development to ensure staff are sensitive to patients needs and learn from complaints. Immediate focus is needed on the following issues: Improve timeliness of responding to complaints and articulate how complaints inform improvement. Develop a patient and public engagement strategy in collaboration with stakeholders, including patients and staff. 14 The following definitions are used for the rating of recommendations in this review: Rating Definition Urgent The Trust should take immediate action to respond to these recommendations and ensure improvement in the quality of care High The Trust should develop a response and action plan for these recommendations to ensure improvement in the quality of care Medium The Trust should implement these recommendations to ensure ongoing improvement in the quality of care 15 Governance and leadership Overview The two KLOEs in the area of governance and leadership were focused on the governance processes for assuring the quality of treatment and care. The panel sought to address the effectiveness of governance and leadership through reviewing documentation supporting key governance processes and interviews with Board members and senior staff, including Non-Executive Directors and Governors. We also spoke to staff in different settings and observed conditions in clinical areas to understand whether there was effective Board to ward level communication on quality assurance. Detailed findings KLOE 1: Can the Trust clearly articulate its governance process for assuring the quality of treatment and care? Good practice identified A new Director of Nursing was appointed in October 2012, and two new deputies were recruited following his appointment. The Chairman, other directors and many clinical staff in multiple areas recognise the positive impact which has been made by the Director of Nursing and his two deputies, including improved visibility in the organisation. At the focus group, nurses told us that they are feeling more empowered and more able to challenge than they did in the past, for example on staffing levels. They feel that nursing now has a higher profile and is much stronger in the organisation. Our interviews with the nurse leaders revealed a commitment to raising standards in the hospital. The PATHway initiative (intentional rounding) was identified as good practice, introduced in May 2013, to ensure nurses on all wards are regularly assessing patients for pressure ulcer risk and falls risk (performed hourly from 8am until 8pm, and then two-hourly overnight). All forms observed had been completed, but it was noted that staff interviewed were not fully aware of its main aims, with a view that it is just another piece of paper to fill in. Other good practice examples were identified including improvements with patient flow management, patient and public involvement, and improved safeguarding arrangements and care for dementia patients. The Trust sought external support to review and improve its approach to Quality Governance in September 2011. A number of recommendations were made and developed into an action plan by the Trust which was led by the Medical Director and Director of Nursing. A further review in November 2012 identified that the Trust has made progress in a number of important areas for ensuring more effective monitoring and assurance of quality, particularly at Divisional level. The report identified that the new Director of Nursing had provided fresh insight into where further refinements can be made, for example, in relation to Care Quality Commission (CQC) compliance assurance. The improvements were still in the process of being embedded and when compared to best practice there remained scope to deliver further improvements particularly in relation to reporting and use of quality performance information for monitoring. The report further noted that the Quality and Clinical Governance Committee (QCGC) received information from the specialties only after the three month red escalation rule had been triggered. The report made recommendations that will allow committee members to identify earlier deterioration in performance and obtain assurance over specialty level performance on behalf of the Board. 16 Good practice identified There were examples of areas which seemed to be benefiting from good medical leadership. In particular, the Women’s Health Unit and trauma and orthopedics. The Trust Board, including Executive and Non Executive Directors could describe the clinical governance committee structures and reporting to the Trust Board. A Non-Executive Director confirmed that the Board had debated vacancy rates, healthcare associated infections, staff sickness, the GMC trainee survey responses and mortality figures. Board members were aware that there was a Joint Health Economy mortality action plan. The Trust Risk Register dated April 2013 identified five corporate risks rated as red, which the panel considered demonstrated appropriate focus on quality risks: Failure to meet authorisation and requirements for CQC or Monitor Failure to meet financial and contractual /demand targets including Cost Improvement Plan (CIP) delivery SHMI being higher than expected Failure to reduce healthcare-associated infections (HCAI) Clinical Services become unsustainable due to operational pressures/staffing The Trust informed us that they were submitting their annual statement of compliance with Monitor’s Quality Governance Framework. Non-Executive Directors undertake ward-walkarounds and those interviewed could describe checking if handwash gels are full, checks observations charts and that the patients have had their drugs, and asks patients if the nurses are attentive to their needs. Concerns had been raised with the Executive team following these including use of an escalation ward for day case and in-patients and doctors doing ward rounds without nurses. The NEDs followed up to ensure appropriate action was taken to address this. The Medical Director confirmed that he and the Director of Nursing were required to sign off a quality impact assessment of each CIP. There was also evidence of Board challenge of CIP delivery at meetings. Outstanding concerns including evidence Priority – urgent, high or medium Planned improvements Recommended action Quality Governance Review Report 2012 recommendations The Board should review how it can introduce more challenge to the “assurance process” including seeking independent corroboration of statements on outcomes and processes which are reported to them. Urgent The Trust should continue to High Board assurance processes Interviews with Board members identified that they did not appear to be obtaining the necessary levels of assurance on quality. In an interview, the Chair acknowledged that he was not fully assured. He described being only 60% assured and 40% reassured. Furthermore there appeared to be gaps in communication between the Chairman and Senior Independent Director. The Senior Independent Director could not describe what was on the Chairman’s worry list. The panel was told that the Board has gained assurance through numerous external reviews commissioned. However, it was not clear how these had provided assurance and there is evidence of inadequate learning from 17 Outstanding concerns including evidence Planned improvements these reviews (more detail on this is provided in the section on evidence of gaps in learning from recommendations below). The Board also appears to also have received limited performance information to enable it to do to effectively challenge on quality of services (more detail on this is provided in clinical and operational effectiveness section). Recommended action Priority – urgent, high or medium implement the recommendations in the Quality Governance Follow Up Review Report 2012. Review the development support required for the Governors so they can perform their assurance role effectively. In interviews with the Non Executive Directors it was revealed that not all felt that challenge at Board could take place effectively as the response from the Chief Executive to challenge was viewed as not always being positive or responsive. The Board also appears to also have received limited performance information to enable it to effectively challenge on quality of services (more detail on this is provided in clinical and operational effectiveness section). High Governors who the panel spoke to appeared to be disengaged and have only limited information about the Trust’s quality and safety priorities. One reported not receiving training that had been requested a year earlier. Some Governors were unable to articulate the Trust’s position in relation to adjusted mortality. This raised the question about how informed they were about the major issues facing the Trust. Governors described that they were not yet able to hold the Non-Executive Directors to account. Quality strategy and priorities Although the Trust has a quality strategy, it is lacking detail of the specific areas for improvement and metrics to measure progress. The Trust submitted a Patient Safety strategy. However, this was more in the form of an action plan, rather than a strategy, and targets were not specific. The Trust has a number of action plans in place. However, they do not appear to be linked to an overarching quality strategy and the Board does not have a single, coherent overview of the current quality of care in the Trust. During interviews, not all Board members and senior managers could articulate the organisation’s key quality and safety priorities in a consistent manner. Whilst they could articulate the main challenges, including poor community care, capacity and bed management issues, Board members did not always share a common understanding of how clinical pathways operated within the Trust and consequently did not have an accurate appreciation of the quality of care that patients receive. For example, they could not describe the Trust’s approach to medical supervision of patients and junior medical The Nursing Director indicated that he had written a draft of a quality strategy for nursing which was fairly comprehensive, but as yet unpublished. The panel noted that the Trust had refreshed a document called the “Quality Governance Modus Operandi” in 2013. It included an action plan, clinical governance reporting framework and a number of key improvements. Develop an updated, single, High cohesive quality strategy that takes account of external reports, mortality concerns, feedback from patients and staff, clinical audit recommendations, current identified risks and current Trust performance. As part of this, agree quantifiable and measurable improvements Develop a single improvement plan High relating to quality and outcomes as set out in the quality strategy. Be clear how any actions link to a reduction in mortality and improvement in quality. 18 Outstanding concerns including evidence Priority – urgent, high or medium Planned improvements Recommended action None identified by the panel. Review the Board's leadership style and optimise the effectiveness of this on organisational culture and quality improvement. This should include enhancing the visibility and impact of all Directors. Refer to planned improvements described under the findings for KLOE 5: How is the Trust assured that its mission statement and values are achieved within its clinical pathways The Trust needs to review its out of Urgent hours clinical cover to ensure there is appropriate clinical leadership and supervision. Input from the Deanery should be sought where necessary. The Trust has an action plan in response to the Deanery report. The Trust needs to create a culture of enhanced clinical leadership amongst consultants. High Review the Deanery Action Plan and ensure an effective monitoring programme is put in place. High Review the approach to improving Infection Control to address effective medical engagement and establish effective monitoring mechanisms. High staffing and supervision at the week-ends. Impact of Board leadership style on organisational culture The panel observed that the Chief Executive was seen by staff and Board members interviewed as being heavily involved in the day to day operations of the Trust, which was seen to impact adversely on the ability of other Executive Directors to deliver their functions. The panel considered that the Chairman had not fully considered the impact of the Chief Executive’s leadership style on the executive team’s ability to fulfill their functions. Urgent Feedback from the Governors was mixed. Staff interviewed highlighted limited visibility of the Executive Board members. The Board needs to consider visibility in the organisation to improve the overall leadership culture. Evidence of a lack of impactful leadership from medical staff, especially out of hours On the unannounced visit, the panel was told that out of hours the wards on the Ladysmith site rely on nurse practitioners to provide medical cover. The panel was shown lists of jobs that had been referred to the medical teams and had not been completed. The list included prescribing duties such as for warfarin, referring patients to the Liverpool Care Pathway and assessing a patient for potential aspiration. This was also evidenced in the nursing notes where entries had been made requesting a medical review and there had been no corresponding entry in the medical notes to suggest that the review had been made. Similarly, medical outliers on the trauma ward had not been reviewed on a daily basis and requests for medical review had either taken too long to be performed or not been done at all. The most senior surgical doctor in the hospital was a Foundation Year 2 doctor. This doctor described that the registrar was on-call at home. When asked about supervision, the doctor described being supervised during the day, but not at night. The Deanery recommended in their August 2012 report after their visit in May that “handovers should be supervised by a Consultant”. The Trust response action plan however recommends that MAU handovers in the morning require senior medical presence (either a consultant or a middle grade) and in the evening handovers require a 19 Outstanding concerns including evidence Planned improvements Recommended action Priority – urgent, high or medium senior nurse and a middle grade. It was not clear to the panel why the recommendations had not been implemented. Commitment of all clinicians to the Infection Prevention Committee was not evident. In the Clinical Governance Accountability Committee minutes from 7/12/12 (page 5 item 320/2012) on the matter of the Infection Prevention Committee, it states “It was agreed that medical membership needs to be reviewed. [Medical Director] to request clinical attendance”. Evidence of limited connectivity from the Board to ward level staff The review panel identified clear gaps in Board to ward communication including assurance of quality and safety. Evidence of this included: Staff members interviewed at ward level could not provide a comprehensive explanation of what the Trust’s quality and safety priorities are. Several qualified staff at all grades on both the announced and unannounced visits discussed the “6 C’s” and about providing good, safe care, but were not more specific. Staff were unaware of common themes of incidents, for example the top three harms / incidents reported at ward / division / Trust level. Senior nursing staff interviewed could not articulate the Trust’s nursing strategy and targets, for example, pressure ulcer reduction targets. Staff could not describe the key performance indicators relevant to their areas of the hospital, e.g. hand washing audit rates, stroke performance data, pressure ulcers and infection rates at ward level. It was noted that ward performance data on key indicators such as pressure ulcers and falls was seen at the entrance to some wards but nursing and medical staff interviewed on the wards were still unable to describe their performance. Staff found it difficult to identify improvements following complaints or incident reports. Despite management describing use of the 15 steps, awareness of staff at the unannounced visit was poor. Management mentioned Accelerate the ward level and improvements to address concerns senior leadership development, with ward-level nursing leadership. including nurses and consultants. Develop a clinical effectiveness programme to improve the staff knowledge of evidence based care including infection control, clinical audit, leading and managing quality improvement change. High High Enhance staff communication, High including ward performance and audit results and incident reporting. This maybe more effective through better use of directorate and ward level meetings and direct email newsletters The night staff in particular seem disconnected from the day-time hospital and it is important that they are included in any strategy to improve communication. Board visibility and engagement Director and Non-Executive Director walk-arounds take place monthly, but Non-Executive None identified by the panel. Undertake a Safety Culture Audit to inform a refreshed quality strategy and improvement High 20 Outstanding concerns including evidence Planned improvements Directors perform ward rounds on their own in an unstructured manner. Some staff interviewed did know of the Board walkabouts and were aware of the Board, but generally the panel noted limited awareness amongst staff on the wards of the incumbent directors and the ward walk-arounds. Staff in different settings referred to a monthly briefing session led by the Chief Executive, but they did not feel they could ask questions in the sessions. The panel was also told about apprehension amongst many other staff around speaking out and not really feeling listened to. For example, recent Francis listening events were described as staff having to do the listening, rather than their views being invited. The panel considered that the Trust was reliant on external reviews, but does not have a history of delivering improvements based on them. Priority – urgent, high or medium programme. Although staff described good visibility of the Director of Nursing and his deputies, there appears to be less exposure of other executive directors. Front-line staff described being unaware of what happened following ward walk-arounds as they did not receive feedback. Evidence of gaps in learning from recommendations Recommended action The ECIST report had been discussed with all A&E and medical consultants. The Invited Services Review of the Royal College of Physicians performed in 2008 includes recommendations which do not appear to have been implemented. “Medical staff need to complete a short discharge proforma before any patient leaves the hospital” and discharge summaries “at present are not being sent to the primary care teams with sufficient urgency”. However, the discharge summaries are still being flagged as red on the performance dashboard. In an interview with the Director of Nursing and a Non-Executive Director, panel members were told that the Board had been made aware of the concerns of trainees, these having been highlighted in recent Deanery reports to the Trust. The Royal College of Physicians Invited Services Review in 2008 also produced recommendations that “more senior time will need to be apportioned to the MAU and acute care which should become less dependent on trainees”. A mortality review was undertaken by Dr M Mohammed and Professor R J Lilford, Birmingham University, June 2012 that made recommendations regarding the monitoring of mortality related data e.g. example run charts. Issues have been flagged in the Urgent & Emergency Care Intensive Support Team (ECIST) review in April 2013, ”the acute physicians were not managing acute medicine patients” and “we identified only one ward where a consultant-led ward round was undertaken every day Monday to Friday.” The Medial Director told the panel members that an action plan had previously been sent to the Deanery to address their concerns. It was not clear how this statement fitted with the Deanery’s recent letter of concern to the Trust. Establish a systematic programme for Board safety walkabouts, in line with best practice. High As part of an effective approach to staff engagement, agree a programme of development and listening events, such that there can be effective cultural change where staff, including trainees, feel heard, valued and cared for. High The Trust should review how it is responding to recommendations from external reviews, ensuring these are aligned with its overall quality strategy and action plan. High Improvements in receiving and acting on trainee feedback should be implemented and its effectiveness measured by the Trust. High Management stated that the Trust 21 Outstanding concerns including evidence Planned improvements The panel was told that the Trust now puts on staff listening events and the Board believed they are identifying feedback themes. However, in a letter sent to the Trust in April 2013 by the Dean of Postgraduate Medical Studies, it is clear that the Deanery outlined concerns regarding the Trust not having adequate systems to address issues raised by trainees. The letter states: “The Trust still does not hear about everything that is concerning trainees. Further reflection on why this continues to be the case is a priority for the Trust”. The panel therefore did not gain assurance that trainee concerns were being captured. has been working to improve the timely delivery of discharge letters, but acknowledge that 20% are still not going out on time. Outstanding concerns over the Quality Impact Assessments (QIA) for the latest Cost Improvement Plan (CIP) The panel noted that the Trust had sought an external review of its QIA process for CIPs. The PwC Report “Review of FY 13/14 CIPs and scaling of further opportunities”, dated 22 April 2013, cites that 25% of CIPs had yet to have a QIA completed. Of these, 44% were partially completed and were populated with insufficient detail. In an interview with the panel to follow up on this, the Director of Finance described further progress that had been made since the drafting of the report. In total 37 QIAs were provided for our review – these had been signed off between 16 May and 31 May. Two separate QIA templates were used, with one not requiring the Medical Director’s signature. In total, 21 had not been signed by the Medical Director and two were missing signatures from both the Medical Director and the Director of Nursing. A number were poorly populated and did not contain indicators for monitoring quality. Recommended action Priority – urgent, high or medium All CIPs should have a quality High impact assessment which follows the Trust’s process consistently but also identifies key indicators to allow ongoing monitoring post implementation The Trust should review its arrangements to monitor CIPs post implementation and provide assurance to the Board on the ongoing quality impact High Interviews with the Board indicated that there was not a shared understanding of how the QIAs would provide assurance to the Board. The panel had some concerns that the quality governance system may be insufficiently sensitive and agile to detect deterioration in care quality particularly in relation to CIPs, as it is unclear how the QIA indicators are being selected and monitored. The quality impact assessments did not contain quality indicators for monitoring of either an improvement or deterioration in care quality. A template exists to record a post-CIP implementation quality review, though it is not clear from the policy if the business as usual quality governance systems will be used to monitor the impact of the CIP or whether reliance is being placed on the Finance Recovery Programme Governance. 22 Outstanding concerns including evidence Clarity of responsibility and accountability for clinical outcomes The panel noted that clinical governance responsibility at Board was a shared responsibility between the Medical Director and Director of Nursing. However, it was unclear who was accountable for the delivery of specific actions. An example of where ambiguity was documented is in the Quality and Clinical Governance Committee minutes of February 2013, where four agenda items had action points with the action lead being named as both the Medical Director and the Director of Nursing. The panel could not see who would be held accountable for delivery in this scenario. The Medical Director had been identified as the lead for mortality and it was unclear to the panel why the mortality reports and the mortality case review process were submitted to the CAPSEC committee, which is chaired by the Director of Nursing, rather than a Board scrutiny committee chaired by a Non Executive Director. Planned improvements Recommended action Board level accountability for specific aspects of quality and clinical governance should reviewed and made more explicit Priority – urgent, high or medium Medium KLOE 2: How does the Trust use information locally? Good practice identified The Medical Director described work being done to engage hospital consultants, local GPs and the Clinical Commissioning Group (CCG) to address key areas of risk for the Trust. The Trust is engaging the local health economy to ensure that patients are in the right place, first time. Senior nurse managers described working in partnership with care homes to try to reduce hospital admission of elderly and dying patients, but highlighted that training could be offered to facilitate this. An integrated transfer team was set up October 2012 with Social Services. Management stated that communication with Social Services had improved, but staff had been TUPE (Transfer of Undertakings (Protection of Employment))transferred and it was “not quite working” yet. The Trust is also working with GPs to promote end of life care in the community as opposed to in hospital and the CCG is being engaged to find alternatives. 23 Priority – urgent, high or medium Outstanding concerns including evidence Planned improvements Recommended action Impact of imbalances in the local health economy Noted improvements in good practice above. It is important that the Trust performs and Medium communicates the results of robust analysis to identify true external factors before attributing to the “Shipman effect”. From numerous interviews and discussions, there appears to be a commonly held belief in Trust management that responsibility for excess mortality lies with the wider health economy, in particular: The “Shipman effect”, caused by a reluctance to allow very ill patients to stay in the community Poor community care Deprivation and high prevalence of multiple co-morbidities Compared to surrounding areas, Tameside has the lowest community death rates. The community death rates are lower than those in the Stockport area which would be the other Trust potentially affected by the “Shipman effect”. This provides some support to the theory that more patients come into hospital to die in Tameside. As mentioned above, work is underway to engage GP’s and care homes to reduce end of life care in the hospital. However, there is a risk that the emphasis on the “Shipman effect” and other external factors could reduce focus on improvements within the Trust that may also reduce excess mortality. There is also local GP involvement in the mortality review panel and the CCG has commissioned at a level sufficient to enable the Trust to invest in additional nursing and medical staff. There is regular engagement with the Medical Director, so it is hoped that care in the community can be addressed. A whole health economy approach to performance improvement is to be continued and emphasised, but should include all stakeholders, including community and social services provision. The Trust should work with local GPs and the CCGs to ensure good practice is followed when referring patients to hospital. Similarly, adequate facilities need to exist to support early discharge into the community with adequate medical follow up to prevent unplanned admissions. 24 Clinical and operational effectiveness Overview The panel explored one Key Line of Enquiry for clinical and operational effectiveness, covering the processes the Trust uses to monitor and address clinical and operational performance data. As for our review of other aspects of governance and leadership, we used a combination of documentation and data review, interviews and observations to review the effectiveness of these arrangements. Detailed findings KLOE 3: What governance arrangements does the Trust have to monitor and address clinical and operational performance data at a senior level? Good practice identified Management told the panel that the Trust has used mortality data to focus improvements in care, for example care bundles have been introduced, staff cover increased in A&E and MAU, nurse to bed ratios increased and work done to improve clinical documentation. An example of a new care bundle being used was on the Trauma Unit, which is using a new fractured neck of femur care bundle/enhanced recovery pathway. A&E staff told the panel that they had identified their optimum staffing levels of 13 qualified staff during a day shift and the new Director of Nursing had agreed this. They now worked to this level, although not all staff were contracted. Some were regular bank staff and would be until ongoing recruitment was completed. The new e-rostering team (see section on Workforce and safety) acknowledged the current staffing gaps in A&E and MAU, but stated that they were improving. The panel’s review of the Trust’s staffing and medical cover is documented in Workforce and safety. On the wards, we observed that a new integrated prescription chart has been introduced (Medicines Prescription and Administration Record), which appears to be well designed, covering venous thromboembolism (VTE) prophylaxis, antibiotics, anticoagulant prophylaxis, IV fluids and oxygen. However, the panel noted that the observation charts are poorly designed in that it is unclear which actions need to be taken based on the early warning score. There is also duplication within the charts. 25 Priority – urgent, high or medium Outstanding concerns including evidence Planned improvements Recommended action Governance arrangements for monitoring mortality indicators None identified by the panel. Review the governance of mortality High improvement to bring rigour and pace to a comprehensive and coherent programme of work ensuring multi-professional specialty input to the review of all deaths and to take account of previous review recommendations. SHMI is not included in the Board performance dashboard and from a review of other meeting minutes does not appear to be discussed at key performance meetings. According to the Mortality Reduction Hospital Action Plan, no clinical lead has yet been assigned to investigate SHMI. Although it was noted that there is a health economy group looking at how to address the SHMI, management acknowledged that the drivers of the SHMI are not well understood at the Trust and are unclear what the best actions are to address it. Ensure that there are clear lead responsibilities in particular with regard to any joint health economy strategies and actions. As part of this work the Trust needs to pay greater attention to the SHMI and ensure that it fully understands the issues which are driving higher than expected mortality. The Medical Director explained that mortality is monitored in several ways, but principally that there is a random choice of 8 – 10 patient deaths per week whose case notes are reviewed by a pediatrician. The process therefore could miss about 6 deaths per week. The pediatrician writes a report and where a case is identified with improvements required, it is referred to a Mortality Review Panel. This process appears to rely on one individual’s judgement and has no external scrutiny, as the panel considered that the summaries provided to the CAPSEC did provide enough depth to provide a useful learning exercise and enable scrutiny. For example, if a patient died from sepsis a reviewer would want to know when blood cultures were taken, when antibiotics were administered, whether the correct antibiotics were used, whether an arterial blood gas sample was taken and from this, whether it was possible to identify any emergent themes from poor practice. A number of senior clinicians set up their own Mortality Working Group, and wrote a separate report outside of clinical governance committee processes, which is unusual. This group supplied an undated narrative commentary to the Medical Director, who submitted the comments to the Clinical Audit and Patient Safety Committee (CAPSEC) in April 2013. The minutes show that the Medical Director is to ask the Mortality Working Group to consider making a formal action plan. It is not clear how this will fit with the overall Trust strategy, and to which action plan the clinicians would then be working. On balance, it was not clear who was providing clinical leadership on this issue. Evidence of inadequate progress in addressing mortality issues The current joint health economy mortality action plan is non-specific and does not always The action plan makes a number of recommendations on issues which we identified at ward level: targeting Review the governance of mortality High improvement to bring rigour and pace to a comprehensive and 26 Outstanding concerns including evidence Planned improvements Recommended action identify the impact of an action or the responsible lead. It does not include all possible stakeholders and instead focuses on the Trust and CCGs. Accountability for delivery and where this sits was not clear to the Panel. senior cover to peak admission times, patients needing to be seen within 24 hours by a senior clinician (but preferably within 4 hours) and a medical-led service out of hours. coherent programme of work such that mortality reviews are of adequate depth to produce recommendations. Ensure that there are clear lead responsibilities in particular with regard to any joint health economy strategies and actions. The Trust’s own hospital mortality action plan is clearer and seems to now be considering the specifics around adjusted mortality risks. The hospital mortality action plan (“Mortality Reduction Hospital Action Plan”) refers to nine care bundles which have recently been introduced, but refers to compliance as being “better, but variable” which does not provide assurance on compliance. The Health Economy Action plan is to be revised and updated for 2013/14. See also recommendations above in relation to whole health economy working. The plan seems to address issues such as lack of understanding of SHMI, but it is unclear what progress is being made by the hospital. According to the Mortality Review Group paper presented to the Clinical Audit and Patient Safety Committee (CAPSEC) in April, Critical Care capacity has been reviewed, but action is not being taken given uncertainty over the potential impact of moving emergency surgery to partner hospitals. Limitations in performance monitoring The approach to quality and safety performance reporting is fragmented and could be better integrated. Board papers recognise general themes, but lack SMART objectives on which to judge performance. A Non-Executive Director interviewed could not articulate the measures being used to monitor progress on the quality strategy. Commissioning for Quality and Innovation (CQUIN) targets are being used to address four sources of harm (pressure ulcers, VTE, falls and UTI), but these are not currently reported to monthly Board meetings. The North West Care (NWC) Indicators, which summarise audit information collected by nurses at ward level, showed unexpectedly high performance (all rated “green”) in February in the paper presented to the Board in March. The indicators cover areas such as infection control, but the panel were made aware of poor performance in March and April, with high numbers of Clostridium difficile cases being experienced. By the time the panel were on-site for the unannounced visit at the beginning of June, 10 cases had been experienced in the Priority – urgent, high or medium The Trust needs to satisfy itself that measurable progress is being made with effective, transparent monitoring which affords accountability to the public. None noted by the panel. Review performance management reporting to the Board to make it more responsive and comprehensive to achieve best practice standards. High Assess performance against the upper quartile of national care. High Address the recommendations of the Quality Governance report as previously stated. High 27 Outstanding concerns including evidence Priority – urgent, high or medium Planned improvements Recommended action None noted by the panel. High The Trust should review its approach to mortality reviews to ensure they are appropriately robust. In addition, the Trust should consider external scrutiny to care audits and mortality reviews. year-to-date (vs. a target of no more than 31 for the year). Observations during ward visits which included random notes audits showed other areas that were inconsistent with the currently reported “green” rating on NWC indicators. This included gaps in patient assessments, observation completion, actions taken and responses to treatment. Other gaps were in relation to infection prevention and control care and management. This raised questions over the relevance and usefulness of the information. At the unannounced visit, 8 out of 14 sets of notes viewed did not have the basic patient details on each chart. 5 out of 10 did not record appropriate monitoring of fluid input and output, even in a patient who had undergone transfusion. There were also gaps with regard to nutritional assessments and plans, weighing of patients and monitoring of stools. However, all patients had received their twice daily observations and appropriate escalation had taken place in the case of elevated scores. Apart from a DNAR form that appeared to be missing, the panel noted generally good practice on ward 45 (the stroke unit). CAPSEC receives “verbal reports” from specialty governance reports. There was no clear process demonstrated as to how quality issues identified at the Board and sub-committee levels are transmitted to and owned by the Specialty Governance Groups to make them responsible and thereby accountable. The Quality Governance Follow-up Review Report November 2012 identified a number of these issues. “The QCGC receives minutes from the CGAC which are verbally presented by the Medical Director. In addition, three members of the CGAC (the Medical Director, Director of Nursing and the Chief Pharmacist) sit on the QCGC. However, as a subcommittee to the Board, it is essential that the Non Executive members of the QCGC can obtain assurance over Specialty level quality governance from the CGAC. Currently, based on the verbal report given it would be difficult for the subcommittee members to challenge under-performance in a specific Division.” Poor quality of mortality reviews Mortality reviews and clinical audits reviewed by the panel were weak. Audits submitted to CAPSEC, produced by clinicians in response to alerts about high mortality rates in acute myocardial infarction and acute cerebrovascular disease, are of poor quality. The audits are of insufficient detail and too superficial to identify the causative factors and produce recommendations that would reduce the unexpectedly high death rates in these patient groups. The Board should satisfy itself that the approach to clinical audit and Medium 28 Outstanding concerns including evidence Planned improvements Recommended action Priority – urgent, high or medium effectiveness meets an acceptable standard of practice. The stroke audit performed following the Dr. Foster mortality alert for stroke patients between February 2011 and January 2012 identified poor compliance with national monitoring guidelines with some standards only being achieved in 40% of patients. These low rates were accepted as being adequate when reported to the relevant committee. Specifically, it identified significant deficiencies in monitoring and nutrition, but concluded that “no substandard care that would have made a difference to the outcome was identified on medical review.” The cases selected for review by CAPSEC were studied in insufficient detail to provide a useful learning exercise and promote discussion. For example, in cases of sepsis little consideration had been given to the application of the care bundle and the recommendations of the surviving sepsis campaign. Acceptance of substandard or variable practice, and a paucity of high aspirations for excellence The panel identified evidence that substandard or variable practice is frequently accepted in the Trust. The culture appeared to be one of managing to targets rather than ensuring overall quality and patient experience. The Mortality Reduction Hospital Action Plan for May 2013 includes the implementation of nine key care bundles expected to reduce death rates. An update on progress described “better but variable compliance, particularly in MAU” and when asked, the Medical Director estimated compliance with care bundles only at around 50%, but 60% in A&E based on spot checks. The Panel noted meeting minutes stating that care bundle compliance would be measured only once compliance had improved. The Patient Safety Strategy includes an aspirational target of 75% which the panel still considers to be low and there are no clear timeframes or milestones. The aspiration for managing the right patient, right bed policy is set at a target of only 75%– 80%, and there is an allowance of four bed moves for non-clinical reasons before an incident and root cause analysis (RCA) is triggered. It was not considered to be unusual practice to ensure that the four-hour target was met for surgical patients to be transferred to MAU even though this added an unnecessary non clinical move to their journey. This None noted The Board should satisfy themselves that there are effective mitigation plans in place to ensure a safe and dignified patient experience. Urgent In order to regain the confidence of High the local community, and so that all internal and external stakeholders believe in the “Everyone Matters” campaign the Board needs to revise its approach to creating a culture of excellence. There needs to be a clear alignment between the Boards strategy and its operational practice for example the Panel would expect to see: Compliance rate targets for the application of clinical care 29 Outstanding concerns including evidence practice was highlighted in the Deanery, May 2012, which stated that "all trainees said that there were surgical patients being admitted to MAU to avoid the 4 hour wait target" and that they were "not always informed that patients had been transferred to MAU". Staffing levels in acute medical wards were found to be at 1 registered nurse to 10 beds during the day and 1 registered nurse to 15 beds at night. This is potentially resulting in a poor experience of care for patients as the staff had to create work arounds to prevent falls. This included patients being cared for at the central nurses station or remain in their bed side chairs until there is sufficient nursing time available to assist them to bed. It was noted that it is common practice for the nursing charts, including the intentional rounding charts, to be gathered at the central nurses’ station overnight. This would not meet CQC’s standards and increases the risk of suboptimal care being delivered. Staff shared that they could not always provide basic care at all times because of capacity issues. Planned improvements Recommended action Priority – urgent, high or medium bundles should be set at 90% to encourage excellence. There needs to be a lower tolerance for moving patients and for medical outliers. Out of hours clinical cover needs to be led by senior doctors rather than by nurse practitioners. The panel also talked to staff on wards who understood targets for infection control but did not seem to relate them to the effect on patients, accepting that a few cases were allowable. Other findings It was noted from the data pack that the percentage of deaths with a palliative care coding increased significantly over the past financial year. The Trust provided an audit report from an external party which did not raise any concerns regarding the depth of coding or the accuracy of coding per the national PbR and local clinical coding audit standards, but coding was not investigated further by the panel. 30 Patient experience Overview The panel focused on how the Trust responds to patient and family feedback and reviewed the effectiveness of the Trust in delivering an appropriate patient experience through its clinical pathways. According to its website, “the Trust's mission statement is to gain and retain the status of Hospital of Choice for local people. Dignity, Respect, Trust and Partnership are the themes which underpin our mission and values.” The panel sought to understand whether the values are being achieved through discussions with patients and staff on wards and at the focus groups and listening events. Detailed findings KLOE 4: How does the Trust engage with stakeholders? Good practice identified The panel heard from several patients who were very satisfied with the level of care at the Trust. Patient satisfaction with the care provided in the surgical wards in the new building was one theme that emerged. Staff from a surgical ward that we spoke to said that they would not mind their family or friends being treated at the Trust. A staff nurse on a medical ward also said she would have her family and friends treated on that ward. Through observations, the panel noted instances of high patient satisfaction on some wards, including on ward 45 (in relation to nursing staff, physiotherapy and food) and ward 5 (in relation to nursing care, and the answering of the buzzer very quickly). Patients interviewed on wards 5, 40, 43 and 45 described nursing staff as hard-working. Staff the panel met were very kind, approachable, hard-working and open and described wanting to do what is best for patients and their local hospital. In interviews, including with the Chairman, a Non-Executive Director, the Medical Director, and Deputy Director of Quality and Governance, it was acknowledged that improvements are needed to the Trust’s complaints process. The Medical Director reported that the 25 days response to complaints has already improved from 40% to 75%. 31 Outstanding concerns including evidence Responding to concerns and complaints The public event was well attended and a consistent theme from patient stories was communication following incidents and the complaints process, including slow, cold, brief responses and a lack of candour and accountability. The public attending felt that their complaints are not dealt with seriously or that there is no appreciation of how much patients and their relatives have been affected by poor quality care. The public considered that the Trust responses lacked compassion and often down played the seriousness and personal impact of the incident which has made it difficult for families to gain closure. Whilst some of the stories were some years old, the themes remained contemporary and a Non-Executive Director confirmed that the complaints process “could be improved”, “possibly not all responses are transparent” and “responses can seem standard”. Planned improvements The new Deputy Director of Nursing responsible for complaints had only been in post for around seven weeks, but highlighted improvements he plans to make to the complaints process and to evidence greater learning and improvement. The public also told the Panel of feedback on nursing staff who they considered were brusque when complaints were made about important issues relating to their treatment. On the ward visits the Panel learnt that the ward managers were seen to ‘deal’ with complaints and staff were not able to describe any learning or changes to practice that had occurred as a result. Recommended action Priority – urgent, high or lower Review the complaints management Urgent process so that the ethos to reflect the Everyone Matters espoused principles so that public expectations and the required duty of candour and standards are met. The impact of changes to the complaints process will need to be evidenced so that the Trust Board can be assured that full and proper learning takes place. Respond to more complaints face to face. The Panel did not see clear evidence despites the programme of work that the Board is “hearing the voices of patients and families” to improve the quality of patients experience and setting a strategy to improve the cultural tone in line with the stated objectives of initiatives such as Everyone Matters. Staff will require development support to enable them to engage with patients on their treatment and care needs effectively. Communication with patients and families The panel heard numerous stories from the public highlighting instances where staff have not responded to immediate family or patient concerns or provided inadequate information. A number of recent examples were shared with the Panel including not being listened to, even where they held critical technical information directly relevant to their care or being kept informed of progress. Care was not always felt to be safe for example where a patient had been given penicillin, despite telling staff that they were allergic to this drug or caring for example being left with inadequate bed clothes and family members having to provide essential hygiene following episode of faecal incontinence. None noted. The Trust needs to provide further development for its staff on responding to patients’ and carers’ concerns. High Review and improve the administration of outpatient appointments ensure patient involvement in the redesign. High Patients and members of the public spoke about the distress particularly for the older members of the public about the erratic issuing of outpatient appointments and of receiving a Did Not Attend letter before receiving an appointment letter. 32 Outstanding concerns including evidence Planned improvements Recommended action Priority – urgent, high or lower The Trust has recently introduced the ‘Friends and Family Test’ in April 2013. It was widely advertised on each ward visited, but no meaningful feedback has yet been received as it is too recent. KLOE 5: How is the Trust assured that its mission statement and values are achieved within its clinical pathways? Good practice identified Generally, good practice was found to be implemented in the surgical pathways, which seems to be achieving good outcomes. This was evidenced through observations and interviews with patients both on the wards and at the public listening event. We heard at the listening event that the “surgical wards are good, but the medical wards are struggling”. Areas of good practice observed include (on the elective orthopedics and elective surgery wards): use of enhanced recovery, meticulously clean wards, strict antibiotic prescribing and venous thromboembolism (VTE) prophylaxis for all patients. On the elective orthopedics ward, the panel also observed a dedicated consultant-led trauma list, well-managed orthopedic pathway (the pre-op, post-op, intermediate care and rehabilitation pathways were clear), pro-active bed management, a fully populated ward board (all patients had VTE prophylaxis and antibiotics recorded) and good rapport with allied specialties (physiotherapy and occupational therapy). The consultant-led trauma service has had a positive impact on the elective service. A member of theatre staff confirmed the use of the World Health Organisation (WHO) surgical check-list protocol in theatres, as well as timeout before and after surgical procedures. There is also a daily emergency surgery list. Surgical mortality is discussed at CEPOD meetings. There was some evidence of good practice for stroke pathway patients. Multiple therapists review patients within the 24 and 72 hour time frames and note keeping made by the therapists and nursing staff was of a high standard. It was clear to panel members that on the two visits made to ward 45, the nursing staff were highly dedicated, caring and professional. On stroke ward 5, other points of good practice noted include close working with the stroke association which provides information packs and discharge plans, having outreach from the community stroke team and use of the MOOD screen which is done on all patients. The panel was given the impression that chronic obstructive pulmonary disease (COPD) (in particular asbestos-related lung disease) is common in Tameside, with a large pool of patients having repeated admissions because of it. The respiratory department has introduced non-invasive ventilator support for such patients. Despite the Trust’s challenges with capacity and bed management, the Deputy Director of Nursing and Patient Experience described some good practice and recent improvements in bed management. There are three bed meetings per day (the panel attended one of these meetings, which was well-attended and well-managed), fit for transfer meetings now receive greater challenge and scrutiny, patient movements are documented and reported to the executive group and there is a monthly Strategy Group. Bed managers are more aware and patient experience is a priority for the executive group. The panel observed good predictor tools for assessing bed availability. In general, the hospital estate was in reasonable condition and the wards and A&E department were tidy, clean and organised. 33 Good practice identified At the unannounced visit, staff explained that there was easy access to CT scanning at night. If an urgent MRI was needed, it could be obtained at Salford. Priority – urgent, high or medium Outstanding concerns including evidence Planned improvements Recommended action Failure to deliver a high quality patient experience through the emergency and acute medical pathway The Trust accepts that its surgical footprint is not large enough to support complex and emergency surgery. Management described an option being investigated to transfer emergency and complex elective surgeries to partner hospitals, to ensure on-going safe and effective clinical services. The Board should assure itself that no patients are at immediate risk of unsafe in the acute medical pathway care including ensuring appropriate clinical cover and improving the management of escalation areas and bed management protocols immediately. Urgent Agree a plan of action for improving the acute medical pathway in line with the recommendations from the reports already commissioned by the Board. High The Trust appears to be struggling to cope with a rising non-elective demand, which is contributing significantly to the clinical risks facing the Trust. Patients also told the Panel of long waits in waiting rooms and on trolleys, a lack of attentiveness, lack of monitoring and observations whilst on trolleys and of some staff not showing basic compassion and that “consultants talk down to you”. This is subject to regulatory review and no formal agreement has been signed with competing local Trusts for the distribution of Patients are potentially subject to a high numbers of patient transfers between elective day case work. There are no guarantees wards, frequent escalation into sub-optimal areas such as the Women’s Health that the Trust will receive this extra work – it is Unit, Gynaecology Day Unit and Endoscopy Unit, as well as non-specialty areas dependent on patient choice, GP referrals and such as Trauma. Staff told the panel that patients are frequently held on responses from other Trusts. The timeframe for trolleys in the Endoscopy Unit and the Gynecology Day Unit when escalation is reconfiguration was suggested by the Finance required as a result of an overload of admissions. At a visit to the MAU it was Director as October 2014. confirmed that moving patients to the ward is often delayed and patients are often moved to an inappropriate specialty or to escalation beds, for example the The Trust is looking at swapping wards 39 and Endoscopy Unit. This was reported as often taking place after 10pm. 31 – trauma and cardiology –so as to free up beds and so that cardiology will be next to the The Endoscopy Unit offers a poor patient experience as it is not designed as a critical care unit (CCU). The panel was told by medical ward in terms of privacy, washing and toilet facilities. Patients due to staff that a paper has been written on this have elective endoscopic procedures are at risk of having their treatment proposal. delayed or postponed because of the medical outliers blocking beds. Whilst the Endoscopy Unit is actually a recovery area with high levels of monitoring Following the panel’s announced visit, management indicated that the Standard equipment, the panel were told this would not be used to monitor the medical Operating Procedure had been strengthened in outliers and the nursing staff who looked after the escalation beds were response to feedback from the panel regarding unfamiliar with the endoscopy environment and would bring in equipment and staffing of the endoscopy area and that the documentation packs from other areas of the hospital for these patients. 34 Outstanding concerns including evidence The Panel observed that patients who are moved into the Women’s Health Unit (WHU) are not subject to the same escalation risk assessment, the Panel noted that one patient in the WHU had been there for her fourth night over the weekend. The Panel also noted that the WHU was being managed by a nurse who described herself as an agency nurse. The panel’s understanding was that this was violation of the Trust’s policy. In the panel’s view, this would lead to inadequate staff familiarity of the escalation area. Planned improvements Recommended action requirement for risk assessment of patients had been reinforced. Priority – urgent, high or medium A risk assessment needs to be done for all patients who are not in The Trust is considering trying to create a Clinical the appropriate specialty, including Decision Unit to improve patient flow in A&E. in all escalation areas, and appropriate monitoring arrangements need to be in place. Urgent The Board should assure itself that no patients are at immediate risk of unsafe care and improve the management of deteriorating patient protocols and practice immediately. Urgent The number of critical care beds required should be benchmarked against population (currently ~3.5/100,000 average UK) and used to inform a mid to long term plan. High There was insufficient or locum-based medical cover out of hours and weekends and poor documentation of handover between teams. A junior doctor raised concerns with the panel that bed managers are not always complying with the written policy to require appropriate medical sign-off of moves which puts patients at risk. Concerns were also raised over compliance with the discharge policy. The current approach to managing the emergency and acute medical pathway is placing patients at risk the Panel observed that a patient had been admitted to a six-bedded bay in MAU with suspected Clostridium difficile, which was a breach of the Trust’s own policy and placed the remaining five patients at risk. Management of deteriorating patients and adequacy of critical care facilities The Panel observed during their unannounced visit that the management of the deteriorating patient is sub optimal due to the out of hours medical management is mostly delegated to junior medical staff and a critical care outreach nurse. Patients are transferred back to MAU when escalation of care is required as there may not be sufficient critical care beds in the Trust to cater for the demand which would mean that seriously ill patients could be managed on the ward inappropriately. This is contrary to a recommendation made in an Invited Service Review by the Royal College of Physicians. It was not clear whether the inadequacy of critical care beds alters decision-making regarding escalation of care for some patients, but the perception that this could happen is real. The Panel were provided with data that stated that 19 patients were transferred out because of capacity issues (not for clinical reasons) to other Trusts and 32 patients were cared for in recovery as a result of a lack of critical care beds The Trust stated that there had been a review, but does not believe that any action is required. 35 Outstanding concerns including evidence Planned improvements Recommended action There needs to be an urgent process and pathway design session with all consultants involved with the acute medical pathway. The solutions may need changes in the organisational model of departments / directorates. Priority – urgent, high or medium between April 2012 and April 2013, with an average length of stay of 6 hours 45 minutes. Concerns have also been raised by the consultant body that there are not enough High Dependency Unit beds for general surgical patients but no improvements had been made. Inadequate medical supervision and junior medical staff supervision and cover, and other instances of poor management of the emergency pathway The need to address supervision of junior medical staff is a longstanding issue and is well known to the executive team. There has been a long standing vacancy for additional medical consultant cover. The Royal College of Physicians 2008 review stated that on MAU “two consultant ward rounds must take place every day including weekends”. However, the ECIST report stated that “over the weekends we understand that the on-call consultant sees new patients only”. A junior doctor and middle grade in general medicine both described the A&E and MAU as being overworked and this affected the middle grade doctor’s ability to manage on-call. A consultant physician described the medical supervision of patients in the MAU as independent of specialty. An Incident Investigation Report dated February 2013 highlights inadequate and infrequent consultant review of patients, inadequate cover for consultants on leave, inadequate registrar cover, junior medical staff caring for patients unsupported by senior colleague review for many days, and dysfunctional ward rounds with junior doctors rounding without nursing staff. From the panel’s observations, there appears to have been little progress with acting on previous reports findings. Consultant cover appears to be poorly managed including on two separate medical wards (a general medicine and a respiratory ward) where the panel noted three consultant ward rounds on the same three days, and no full ward rounds on other days. There is a significant reduction of medical cover over the weekend. A consultant ward round on a Saturday and Sunday has been introduced, but is not part of the formal job plan. The Medical Director recognised the need to improve the interface between MAU and A&E and to improve pathways between surgical, orthopaedics and A&E, including recruiting more MAU physicians, defining responsibilities of consultants, establishing roles and leadership, pathways, quality and governance. He indicated that this was agreed by the Board. He referred to actions resulting from the ECIST report, and four meetings that have already taken place between A&E and medicine, which has improved working together with nurses. Some nursing staff told the panel that better engagement with medical staff is being driven by the Medical Director, but this message was not heard consistently. The Medical Director acknowledged that consultants need to do ward rounds on a daily basis, and is working on job plans to increase 3 and 4 ward rounds up to 5 in a week and also to make training mandatory per job rotas. He explained that the Trust needed to recruit two more physicians in MAU (1 replacement currently filled by a locum and 1 newly created post), two in A&E (both of which are established posts currently filled by locums) and two in elderly medicine, reflecting the conversion of current Urgent High The leadership responsibilities of consultants on MAU need to be clearer. High All acute patients need to receive daily ward round review by senior medical staff. High The Trust needs to create a culture of enhanced clinical leadership amongst consultants. 36 Outstanding concerns including evidence Planned improvements Management informed the panel that board rounds are performed by consultants on the remaining weekdays. However, the panel considered that full ward rounds should take place daily. It was noted from comments made to the panel that “there is lack of acute medical leadership at this hospital” and that the structure is “disjointed”, specifically, that there are three consultants covering the MAU, but each has another specialty in which they are based. Consultant cover being located in A&E could help prevent inappropriate admissions to MAU. Other feedback from junior doctors on senior support was mixed. Ease of access to consultants and registrars even out of hours was reported to be good (excluding in medicine), others considered that support whilst on call is poor, that the middle grade is too busy and that junior trainees have to take decisions. It was reported that the consultant (who does a ward round everyday) is available for help all the time and “very dedicated”. At the unannounced visit, the most senior surgical doctor in the hospital was a Foundation Year 2 doctor. This doctor described that her registrar was on-call at home. When asked about supervision, this doctor described being supervised during the day but not at night. Recommended action Priority – urgent, high or medium enhanced payments into new posts. The Trust confirmed that they are in the process of recruiting two additional substantive acute physicians to the MAU. One position will be a Director of Urgent Care, who will address interface issues between the Emergency Department and MAU in addition to formulating enhanced pathways of care. When questioned around the difference between mortality on weekdays and at week-ends, the Medical Director stated that he is in the process of writing a paper to address middle grade out of hours service (there is a plan to increase the rota from 10 to 12). He stated that there is an additional consultant in adult medicine at the weekends who supervises discharges with midgrades or SHOs and that pharmacy hours have been extended. A Respiratory physician job plan showed only 2PAs out of 12.5PAs devoted to ward rounds. A consultant physician described to the panel his likelihood of attendance out of hours as low yet the job plan has 2PAs for this activity. It is hospital policy not to directly admit patients from A&E to the surgical wards without prior surgical review. There is no resident surgical SpR out of hours so the FY2 is responsible for reviewing patients. The FY2 on site out of hours had to assess a patient on MAU (who had already waited for nearly four hours in A&E) before the patient was transferred to a surgical ward. The panel noted other examples of where this policy was affecting admission and discharge processes for the patients observed on the unannounced visit. Sign-off of “Do Not Resuscitate” (DNAR) forms On ward 45 and the MAU, the panel saw DNAR forms which did not contain the None noted The Board needs to assure its self Medium that patient’s choice and dignity is respected at the end of life and that 37 Outstanding concerns including evidence consultant’s name or sign-off. The Trust’s policy, as described by a staff member, is that the DNAR decision has to be made by a consultant or his/her representative at the hospital when the consultant is not present. That representative cannot be below the rank of “SHO”, but juniors can complete the form. During the unannounced visit, one of the forms examined was signed off by an FY2, one by a CT1 and one by SpR. None of them had a consultant signature. Planned improvements Recommended action Priority – urgent, high or medium vulnerable people are safeguarded. The panel would see that this action goes beyond a simple audit, and the plan to improve DNAR documentation needs to reflect creating an ethos that places listening to patients at the centre of care. 38 Workforce and safety Overview The three KLOEs on workforce and safety focused on: The Trust’s workforce strategy Assurance that the Board has the necessary workforce deployed to deliver its quality objectives Assurance that the organisation is safe Detailed findings KLOEs 6 and 7: In the context of this review, can the Trust describe its workforce strategy? How is the Board assured that it has the necessary workforce deployed to deliver its quality objectives? Good practice identified A new electronic system for rostering (e-rostering) has recently been introduced – only the theatres had yet to be put on the system. The e-rostering team explained that it allows fairer allocation to rotas, each ward can tailor the skill mix needed and it ensures that there is always one senior and one junior nurse on duty. Mandatory training is built in automatically. Staff can see their own rota and when training is planned. It helps flag gaps in staffing, thereby aiding recruitment. Twelve hour shifts have also recently been implemented. Surgery staff commented positively on the implementation of e-rostering and 12 hour shifts, saying that it is better for patients as it provides better continuity of care. However, medical staff argued that one size does not fit all and that the subject needs further thinking through. Some staff were concerned that the change has been purely finance-driven. From what staff have told us, there appears to be a good induction programme, supported by the Director of Nursing. A nurse on ward 45 described good mandatory training / induction, good professional development and funding and good communication with medical staff. In response to negative comments from the Deanery report for junior doctors, the Medical Director stated that action plans had been developed and that the Deanery will conduct an interim review against action plans. The Medical Director described one example of where feedback from the Deanery had resulted in positive changes in Endoscopy, ensuring that there is now consultant support for each trainee. The Medical Director explained that more medical staff now receive appraisals and it is his intention to link this with pay progression. The Director of Human Resources said appraisal was at 84% for medical staff. 39 Good practice identified A quarterly Board report on workforce is given to the Board which covers recruitment, pay expenditure, sickness absence and mandatory training. During interview, a Non-Executive Director stated that Board gets “a comprehensive HR report”. During separate interviews, both the Medical Director and Director of Human Resources identified that the strategy was to enhance permanent staffing and to reduce locum spend. Nurses at a focus group described how the Trust had won the Midwife of the Year Award. Priority – urgent, high or medium Outstanding concerns including evidence Planned improvements Recommended action Staffing levels and quality of training experience As described above, the strategy is to enhance permanent staffing and to reduce locum spend. The Board needs to assure its self that staffing skill Urgent mix and levels does not present any immediate risk to patient care or staff welfare. The Board had agreed to establish additional nursing posts using expenditure connected with bank costs to fund them, pending the CCG’s agreement to recurrently fund contracted activity in 2013/14. A CCG funding increase followed in 2013/14. Develop a workforce strategy to support the clinical High strategy and as part of this undertake a nurse staffing review to ensure safe standards of care and dignified patient experience is achieved. Focus on reducing locum spend, vacancy rates and staff moves. Ensure that the e roster templates reflect staffing standards guidance and effective deployment practice. The Panel identified a number of concerns on staffing including: An increase in nurse bank spend in the last year linked to staffing escalation wards. The Trust is failing to meet its 10% target for nursing understaffing levels which is reported to the Board. The April Board paper showed that the target had been breached from November to March 2013, with 14.8% of nursing shifts having less staff than planned in March. Long-term sickness was highlighted as an issue by Directors and the biggest challenges seem to be faced by nursing staff for whom the sickness rate is as high as 6.5%. Elderly care wards, A&E and MAU staffing appeared the most significant areas of concern. In interview the Director of Human Resources stated that locum medical and nursing spending is on the increase because of demand when there is bed escalation. Concerns were raised by both consultants and junior doctors that nursing levels were in their view dangerously low with a high dependency on agency staff. This was considered by staff to be affecting patient experience and care. The 40 Outstanding concerns including evidence Planned improvements Recommended action Priority – urgent, high or medium quality of care is also being impacted when nurses are moved from as it depletes the ward of staff with specialty expertise. The panel heard of a number of concerns from nurses relating to both poor staffing levels and skill mix, including, little opportunity to take entitled breaks in 12 hour shift, poor supervision of newly qualified staff and having to attend mandatory training in their own time. Staff interviewed on one ward described themselves as de-motivated, they attended training in their own time because they cared about patients and their own professionalism and accountability. 41 KLOE 8: What assurance does the Board have that the organisation is safe? Good practice identified The antibiotic prescribing policy is strict. No more than three days of antibiotics are prescribed at one time and the treatment chart has been designed in such a way that no one can prescribe more than three days’ antibiotics at a time. The microbiologist was widely praised and it was stated that he engaged staff and regularly reviewed guidance. According to staff on a stroke ward, intensive teaching of GPs about antibiotic prescribing led to a decrease in the incidence of Clostridium difficile and MRSA. Junior doctors at a focus group were all aware of the antimicrobial policy. They explained that the Trust has been rolling out credit card-sized antibiotic prescribing guides to slide in behind ID badges. The Medical Director described a new online system for incidence reports which has recently been established, as well as an incident reporting hotline, but explained that it would still take 6 – 8 weeks to be embedded. In a focus group, of the 6 to 8 of the doctors which had reported incidents, only 2 or 3 had had any feedback. However, these doctors noted that under the new system they had been receiving feedback. Nurses on the wards also told us that they did not receive feedback on critical incidents from the forms they had submitted, but this may be improved by the implementation of the new electronic recording system. The screen saver message on Trust PC’s seen by the panel advises staff of the infection control targets and the achievement against the target. Priority – urgent, high or medium Outstanding concerns including evidence Planned improvements Recommended action It was not clear how the Trust was using serious incident reporting and learning to improve care. None noted. As previously stated the Board should undertake a Safety Culture Audit to inform a refreshed quality strategy and improvement programme. High The Trust should review its incident reporting process and the wider safety culture to ensure learning is disseminated effectively. High Whilst the Trust has roughly average levels of incident reporting, it has higher than average levels of patient accident and clinical assessment-related incidents. A report on serious incidents 01/04/2012 – 31/03/2013 describes a never event (defined by the NHS as serious, largely preventable patient safety incidents that should not occur if the available preventative measures have been implemented), but it has not been classified as such. It also logs an incident which took place on 11/6/11, which is still awaiting a final investigation report in June 2013. The ward and / or clinical teams do not appear to be closely involved with the process of incident management based on the panel’s observations. There did not appear to be team meetings or root cause analysis following serious incidents in some areas and staff could not give examples of feedback they had received on general themes or specific incidents. Staff perception was that if there is a Clostridium difficile or MRSA episode, the 42 Outstanding concerns including evidence Planned improvements Recommended action Priority – urgent, high or medium Infection Control Team takes over the management rather than supporting the clinical teams to do so. 43 5. Conclusions and support required Urgent and high priority actions for consideration at the risk summit Problem identified Recommended action for discussion Support required by the Trust Care risks associated with the emergency and medical pathway, including capacity and staff planning, clinical cover and out of hours clinical leadership. The Board should assure itself immediately that no patients are at immediate risk of unsafe care due to the issues raised in this report and improve key safety processes, including management of deteriorating patients. The Trust needs to work with the CCG and the Deanery to address the whole system and workforce challenges. The Trust should review operational planning in the emergency and medical pathway to support appropriate care, including improving clinical cover and leadership, particularly at night. The Trust should agree a plan of action for improving the acute medical pathway including the management of escalation areas and bed management protocols immediately. The Trust should agree a plan of action for improving the acute medical pathway in line with the recommendations from the reports already commissioned by the Board. The Trust should develop a workforce strategy to support the clinical strategy and as part of this undertake a medical and nurse staffing review to ensure safe standards of care and dignified patient experience is achieved. The review should focus on reducing locum spend, vacancy rates and staff moves and ensure that the e roster templates reflect staffing standards guidance and effective deployment practice. The Board is not effectively leading quality improvement in the Trust and the leadership and governance arrangements need urgent review to improve assurance and accountability at all levels. Urgently review the Board's leadership style and optimise the effectiveness of this on organisational To be discussed with the Trust and included in the culture and quality improvement, including enhancing the visibility of all of the Directors. risk summit action plan. The Board should consider how it can introduce more challenge to the “assurance process” including seeking independent corroboration of statements on outcomes and processes which are reported to them. The Trust should accelerate the ward and senior leadership development programme and focus on improving clinical leadership (both medical and nursing) in the organisation. Enhance staff communication, including ward performance, audit results, incident reporting and learning from reviews. This maybe more effective through better use of directorate and ward level meetings and direct email newsletters. 44 Problem identified Recommended action for discussion Support required by the Trust Absence of an updated and effective quality strategy, a single cohesive implementation plan and supporting performance information to focus on key risks and drive improvement. Develop an updated, single, cohesive quality strategy that takes account of external reports, mortality concerns, feedback from patients and staff, clinical audit recommendations, current identified risks and current Trust performance. As part of this, agree quantifiable and measurable improvements The Trust needs to work with the CCG to ensure that whole system challenges are addressed consistently. Develop a single improvement plan relating to quality and outcomes as set out in the quality strategy. Undertake a Safety Culture Audit to inform this and prioritise actions that link to a reduction in mortality and improvement in quality and patient experience. A whole health economy approach to performance improvement is to be continued and emphasised, but should include all stakeholders, including community and social services provision. Review reporting to the Board to ensure that performance against the quality strategy and action plan can be monitored and challenged effectively. Reporting should be more responsive and comprehensive, including improvements identified in Board level review of quality accounts, mortality data and the ongoing quality impact of CIPs. Assess performance against the upper quartile of national care. Review the governance of mortality improvement to bring rigour and pace to a comprehensive and coherent programme of work such that mortality reviews are of adequate depth to produce recommendations. Ensure that there are clear lead responsibilities in particular with regard to any joint health economy strategies and actions. In addition, the Trust should consider external scrutiny to care audits and mortality reviews. The organisational culture accepts sub-optimal care and does not engage staff effectively in improving quality and patient experience. Develop a clinical effectiveness programme to improve the staff knowledge of evidence based care including infection control, clinical audit, leading and managing quality improvement change. Lack of meaningful patient and public engagement and transparency. Develop a programme to improve listening to patients including training staff to respond to concerns in line with the Trust’s vision of “Everybody Counts” and "treat you and your family as partners in care". To be discussed with the Trust and included in the risk summit action plan. Agree a programme of development support such that there can be effective cultural change where patients and staff, including trainees, feel heard, valued and cared for. To be discussed with the Trust and included in the risk summit action plan. Review the complaints management ethos and process to ensure that public expectations and the required duty of candour and standards are met. The impact of changes to the complaints process will need to be evidenced so that the Trust Board can be assured that full and proper learning takes place. 45 Appendices 46 Appendix I: SHMI and HSMR definitions HSMR definition What is the Hospital Standardised Mortality Ratio? The Hospital Standardised Mortality Ratio (HSMR) is an indicator of healthcare quality that measures whether the mortality rate at a hospital is higher or lower than you would expect. Like all statistical indicators, HSMR is not perfect. If a hospital has a high HSMR, it cannot be said for certain that this reflects failings in the care provided by the hospital. However, it can be a warning sign that things are going wrong. How does HSMR work? The HSMR is a ratio of the observed number of in-hospital deaths at the end of a continuous inpatient spell to the expected number of in-hospital deaths (multiplied by 100) for 56 specific groups (CCS groups); in a specified patient group. The expected deaths are calculated from logistic regression models taking into account and adjusting for a case-mix of: age band, sex, deprivation, interaction between age band and co-morbidities, month of admission, admission method, source of admission, the presence of palliative care, number of previous emergency admissions and financial year of discharge. How should HSMR be interpreted? Care is needed in interpreting these results. Although a score of 100 indicates that the observed number of deaths matched the expected number; in order to identify if variation from this is significant confidence intervals are calculated. A Poisson distribution model is used to calculate 95% and 99.9% confidence intervals and only when these have been crossed is performance classed as higher or lower than expected. SHMI definition What is the Summary Hospital-level Mortality Indicator? The Summary level Hospital Mortality Indicator (SHMI) is a high level hospital mortality indicator that is published by the Department of Health on a quarterly basis. The SHMI follows a similar principle to the general standardised mortality ratio; a measure based upon a nationally expected value. SHMI can be used as a potential smoke alarm for potential deviations away from regular practice. How does SHMI work? 1) Deaths up to 30 days post acute trust discharge are considered in the mortality indicator, utilising ONS data 2) The SHMI is the ratio of the Observed number of deaths in a Trust vs. Expected number of deaths over a period of time 3) The Indicator will utilise 5 factors to adjust mortality rates by a. b. c. d. e. The primary admitting diagnosis The type of admission A calculation of co-morbid complexity (Charlson Index of co-morbidities) Age Sex 47 4) All inpatient mortalities that occur within a Hospital are considered in the indicator How should SHMI be interpreted? Due to the complexities of hospital care and the high variation in the statistical models all deviations from the expected are highlighted using a Random Effects funnel plot Some key differences between SHMI and HSMR Indicator Are all hospital deaths included? When a patient dies how many times is this counted? HSMR No, around 80% of in hospital deaths are included, which varies significantly dependent upon the services provided by each hospital If a patient is transferred between hospitals within 2 days the death is counted multiple times Does the use of the palliative care code reduce the relative impact of a death on the indicator? Does the indicator consider where deaths occur? Yes Is this applied to all health care providers? Yes Only considers in hospital deaths SHMI Yes all deaths are included 1 death is counted once, and if the patient is transferred the death is attached to the last acute/secondary care provider No Considers in hospital deaths but also those up to 30 days post discharge anywhere too. No, does not apply to specialist hospitals 48 Appendix II: Panel composition Panel role Name Panel Chair Gill Harris Senior Regional Support Damien Riley Lay representative (Patient/public representative) Steve McNeice Lay representative (Patient/public representative) David Tompkins Lay representative (Patient/public representative) Margaret Hughes Lay representative (Patient/public representative) Jackie Wilkinson Junior Doctor Tom Foley Doctor Gulzar Mufti Doctor Gavin Nicol Doctor Roger Hall Student Nurse Sarah Weight Senior Nurse Helen Carter Board Level Nurse Mike Wright CQC representative Jeanette Berry Senior Trust Manager Chris Harrop Local Area Team Observer Trish Bennett Clinical Commissioning Group Observer Steve Allinson 49 Appendix III: Interviews held on announced visit Interviewees Date held Chief Executive (Christine Green) 23 May Chair of Quality and Clinical Governance Committee (Tricia Kalloo), Director of Nursing (and DIPC) (John Goodenough) and Patient Safety Lead (R Kitson) 23 May Deputy Director of Nursing and Patient Experience (Beverley Tabernacle) and Senior Nurse Safeguarding Adults (Naz Khadim) 23 May Director of Nursing (and DIPC) – John Goodenough 23 May Medical Director – Tariq Mahmood 23 May Director of Finance – Barbara Herring 23 May Director of Clinical Services – Paul Williams 23 May Director of Human Resources – David Wilkinson 24 May Associate Director of Planning and Performance – Melissa Laskey 24 May Deputy Director of Quality and Governance – Peter Weller 24 May Individual interviews/calls with each Non-Executive Director 24 May Staff and Patient Governors 24 May Divisional Nurse Manager 24 May Medical Staffing Officer 24 May E-rostering Team 24 May Trust Secretary – Tom Neve 24 May Chairman – Paul Connellan 30 May (held offsite due to availability) 50 Appendix IV: Observations undertaken Observation area Date of observation Ward 43 – General medicine 23 May Ward 41 – General medicine/Diabetes 23 May Ward 30 – General Medicine 23 May Surgical Unit 23 May Ward 40 – Respiratory 23 May Ward 42 – Gastroenterology 23 May Accident and Emergency 23 May Medical Assessment Unit 23 May Ward 31 – Cardiology 23 May Ward 5 – Acute Stroke 23 May Ward 45 – Acute Stroke 23 May Ward 44 – Dementia 23 May Ward 27 – Maternity 23 May DSEC Unit – Endoscopy 24 May Trauma and Orthopaedics 24 May Renal Unit 24 May Women’s Health Unit 24 May 51 Appendix V: Focus groups held Focus group invitees Focus group attendees Date held Band 5 and 6 nurses 12 nurses 23 May Doctors below registrar 16 doctors 23 May Senior nurses (band 7 and above) 17 nurses 24 May Consultants 12 doctors 24 May 52 Appendix VI: Information made available to the panel by the Trust Urgent & Emergency Care Intensive Support Team (ECIST) report, April 2013 SEPSIS bundle AQuA report, April 2013 Payment By Results Assurance Framework Letter from Chief Executive to Jacky Hayden from NHS, April 2013 Tameside PATHway Accreditation Strategy Board Quality Strategy Adult Safeguarding Internal Self Assessment Board Assurance Framework and Trust Risk Register Tameside Journey – Our Experience Clinical Audit plans for 2013/14 and latest Clinical Audit Annual Report Reflect and Review Case Studies Cost Improvement Programmes for 2012/13 and 2013/14 and details of the process for assessing the quality impact of these Mortality rates on a daily basis Most recent self assessment or external assessment of quality governance (against Monitor’s Quality Governance Framework or equivalent) Graphs for improved survival for pneumonia, stroke and cardiac Organisation structure and CVs of executive team 18 Week RTT performance Governance and committee structures and terms of reference for assuring quality including mortality governance structure chart Waiting list payments report Trust Board (private and public) papers and minutes for the most recent four months (excluding minutes for May) BREACH analysis Board sub-committee with delegated responsibility for assuring quality and safety. Papers and minutes for last two months (public and private) Metrics for bed movements Mortality review group papers and minutes for the last two months (CAPSEC papers and minutes were provided for the four months) Maintenance log for Equipment in Surgical, Medical, MAU, A&E Summary of key performance measures for 2012/13 including finance, performance, quality and patient experience Clinical Coding Audit Annual plan submission to Monitor or equivalent for NTDA for 2013/14 ITU Flow – OCC rate for Level 1 & 2 CQC mortality alert action plan and implementation Paper on the surgical collaboration with Stockport and USM Various independent reviews and self-assessments of quality performed within the last year Respiratory and General Medicine Consultant Job Plans 53 Background Information regarding supporting services and service specification Junior medical staff rota for the medical wards for w/c 20th May SUIs (never events and serious harm) – report on serious harm over last year Junior and senior medical rota for ICU for w/c 20th May Board Annual Report Mortality strategy Risk Plans at BU level Escalation policy Deanery reports (May 2012, October 2012, April 2013) Completed Quality Impact Assessments (QIA)’s Antibiotic policy Birmingham report Whistle-blowing policy, intranet screen shots Director of Infection Prevention and Control (DIPC) report Minutes from Patient’s Group and Minutes from Everyone Matters 2012/13 Tameside Hospital Contractual Performance Measures Nursing Strategy Quality Accounts Council of Governors – minutes of meetings 54 Appendix VII: Unannounced site visit Agenda item Panel pre-meeting Entry into Accident and Emergency and announced arrival to site manager Observations undertaken of the following: Accident and Emergency Medical Assessment Unit Medical wards Stroke wards Women’s Health Unit Trauma ward Discussions held with senior nursing staff to understand current staffing and patient levels, as well as details of outliers Follow up meeting with Director of Clinical Services Follow up meeting with Director of Nursing Follow up meeting with Medical Director 55