Review into the Quality of Care & Treatment provided by
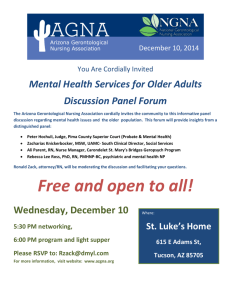
advertisement

Report for Basildon and Thurrock University Hospitals NHS Foundation Trust Review into the Quality of Care & Treatment provided by 14 Hospital Trusts in England RAPID RESPONSIVE REVIEW REPORT FOR RISK SUMMIT July 2013 Contents 1. Introduction 3 2. Background to the Trust 7 3. Key Lines of Enquiry 11 4. Review findings 13 5. Governance and leadership 15 Clinical and operational effectiveness 21 Patient experience 30 Workforce and safety 35 Pharmacy support 41 Conclusions and support required Appendices 42 46 Appendix I: SHMI and HSMR definitions 47 Appendix II: Panel composition 49 Appendix III: Interviews held 50 Appendix IV: Observations undertaken 51 Appendix V: 52 Focus groups held Appendix VI: Information available to the RRR panel 53 Appendix VII: Unannounced site visit 57 2 1. Introduction This section of the report provides background to the review process and details of the key stages of the review. Overview of review process On 6th February the Prime Minister asked Professor Sir Bruce Keogh, NHS England Medical Director, to review the quality of the care and treatment being provided by those hospital trusts in England that have been persistent outliers on mortality statistics. The 14 NHS trusts which fall within the scope of this review were selected on the basis that they have been outliers for the last two consecutive years on either the Summary Hospital level Mortality Indicator (SHMI) or the Hospital Standardised Mortality Ratio (HSMR). Definitions of SHMI and HSMR are included at Appendix I. These two measures are intended to be used in the context of this review as a ‘smoke alarm’ for identifying potential problems affecting the quality of patient care and treatment at the trusts which warrant further review. It was intended that these measures should not be reviewed in isolation and no judgements were made at the start of the review about the actual quality of care being provided to patients at the trusts. Key principles of the review The review process applied to all 14 NHS trusts was designed to embed the following principles: 1) Patient and public participation – these individuals have a key role and worked in partnership with clinicians on the reviewing panel. The panel sought the views of the patients in each of the hospitals and also considered independent feedback from stakeholders, related to the Trust, which had been received through the Keogh review website. These themes have been reflected in the reports. 2) Listening to the views of staff – staff were supported to provide frank and honest opinions about the quality of care provided to hospital patients. 3) Openness and transparency – all possible information and intelligence relating to the review and individual investigations will be publicly available. 4) Cooperation between organisations – each review was built around strong cooperation between different organisations that make up the health system, placing the interest of patients first at all times. Terms of reference of the review The review process was designed by a team of clinicians and other key stakeholders identified by NHS England, based on the NHS National Quality Board guidance on rapid responsive reviews and risk summits. The process was designed to: Determine whether there are any sustained failings in the quality of care and treatment being provided to patients at these Trusts. 3 Identify: i. Whether existing action by these Trusts to improve quality is adequate and whether any additional steps should be taken. ii. Any additional external support that should be made available to these Trusts to help them improve. iii. Any areas that may require regulatory action in order to protect patients. The review follows a three stage process: Stage 1 – Information gathering and analysis This stage used information and data held across the NHS and other public bodies to prepare analysis in relation to clinical quality and outcomes as well as patient and staff views and feedback. The indicators for each trust were compared to appropriate benchmarks to identify any outliers for further investigation in the rapid responsive review stage as Key Lines of Enquiry (KLOEs). The data pack for the trust reviewed is published at http://www.nhs.uk/NHSEngland/bruce-keogh-review/Documents/trust-datapacks/data-pack-basildon-and-thurrock.pdf. Stage 2 – Rapid Responsive Review (RRR) A team of experienced clinicians, patients, managers and regulators (see Appendix II for panel composition), following training, visited each of the 14 hospitals and observed the hospital in action. This involved walking the wards and interviewing patients, trainees, staff and the Senior Executive Team. The report from this stage will be considered at the risk summit. Stage 3 – Risk summit This will bring together a separate group of experts from across health organisations, including the regulatory bodies. They will consider the report from the RRR, alongside other hard and soft intelligence, in order to make judgements about the quality of care being provided and agree any necessary actions, including offers of support to the hospitals concerned. A report following each risk summit will be made publically available. Methods of Investigation The two day announced RRR visit took place at the Trust’s main site on Tuesday 7 and Wednesday 8 May 2013. A variety of review methods were used to investigate the KLOEs and enable the panel to consider evidence from multiple sources in making their judgements. The visit included the following methods of investigation: Listening events Public listening events give the public an opportunity to share their personal experiences with the hospital, and to voice their opinion on what they feel works well or needs improving at the Trust. A listening event for the public and patients was held on the evening of 7 May 2013 at the Education Centre on the Basildon Hospital site. This was an open event, publicised locally, and attended by approximately 30 members of the public, patients and staff. 4 The panel would like to thank all those who attended the listening event and were open with the sharing of their experiences and balanced in their perceptions of the quality of care and treatment at the Trust. The panel found the listening event extremely useful as it identified a number of positive themes around patient experiences, along with highlighting a number of areas for further investigation. Information obtained about the quality of care and treatment at the Trust from the listening event was used to drive the panel's agenda for the second day of the announced site visit and for the unannounced site visit. Relevant areas emerging have been included within this report. Interviews Twelve interviews took place with key members of the Executive Team, Non Executive Directors and selective members of staff based on the KLOEs during the visits. See Appendix III for details of the interviews undertaken. Observations Ward observations enabled the panel to see the Trust undergo its day to day operations. They allowed the panel to talk to current patients, and their families where observations took placed during visiting hours. They allowed the panel to speak with a range of staff and enabled the panel to analyse any observed handover processes within wards, to ensure that the staff that are coming on duty are appropriately briefed on patients. During the RRR announced visit, observations took place in 17 areas of the Basildon Hospital and an additional observation took place at Orsett Hospital. See Appendix IV for details of the observations undertaken. Focus Groups Focus groups provide an opportunity to talk to staff groups individually and to ask each area of staff what they feel is the contributing factor to the Trust’s high mortality scores. They enable staff to speak up if they feel there is a barrier that is preventing them from providing quality care to patients. Focus groups were held with six staff groups, including a focus group open to all staff, during the announced site visit. See Appendix V for details of the focus groups held. The panel would like to thank all those who attended the focus groups. The groups were open and balanced in sharing their experiences, as well as in their perceptions of the quality of care and treatment at the Trust. Review of documentation A number of documents were provided to the panellists through a copy being available in the panel’s ‘base location’ at the Trust during the site visit. Whilst the documents were not reviewed in detail, they were available to the panellists to validate findings. See Appendix VI for details of the documents available to the panel. 5 Unannounced visit The unannounced site visit took place on the evening of Sunday 12 May 2013. This focused observations in identified areas from the announced site visit, see Appendix VII. Next steps This report has been produced by Dr David Levy, Panel Chair, with the full support and input of panel members. The RRR findings contained in this report have been agreed with the Trust for factual accuracy. This report was issued to attendees at the risk summit, which focussed on supporting Basildon and Thurrock University Hospitals NHS Foundation Trust (“the Trust”) in addressing the actions identified to improve the quality of care and treatment. Following the risk summit the agreed action plan will be published alongside this report on the Keogh review website. A report summarising the findings and actions arising from the 14 investigations will also be published 16 July 2013. 6 2. Background to the Trust This section of the report provides background information on the Trust. Introduction The Trust became one of the first ten Foundation Trusts in the country in 2004 and has a total of 667 beds. Prior to this, in 2002, the Trust had gained University Hospital status. The Trust services a population of approximately 400,000 and has more than 10,000 public members as well as 3,700 staff. 1 The Trust’s SHMI has been above the expected level for the last two years (112 ) and was therefore selected for this review. The Trust’s HSMR is within the expected range (106). Trust size and focus The Trust is a medium sized Trust, relative to the rest of England, for both inpatient and outpatient activity. The Trust provides an extensive range of acute medical services with overnight beds. Regulated services provided by the Trust are: diagnostic and screening procedures; management of supply of blood and blood derived products; maternity and midwifery services; surgical procedures; termination of pregnancies; and treatment of disease, disorder or injury. Nephrology and Gynaecology are the largest inpatient specialties while Trauma & Orthopaedics and Dermatology are the largest specialties for Outpatients. The Trust has 66% market share of inpatient activity within a 5 mile radius of the Trust sites. However, the Trust’s market share falls to 31% within a radius of 10 miles and 8% within a radius of 20 miles. The main competitors in the local area are Southend University Hospitals NHS Trust, Mid Essex Hospital Service NHS Trust, Barking, Havering and Redbridge University Hospitals NHS Trust and Colchester Hospital University NHS Foundation Trust. The Trust has two hospital sites – Basildon Hospital and Orsett Hospital – with the Essex Cardiothoracic Centre (CTC) also located within the grounds of Basildon Hospital. The CTC opened in 2007 and is one of the most modern centres of its kind in the country. Heart attack victims from across the county are brought directly to the CTC to have stents fitted to repair constricted coronary arteries. It also has 24 haemodialysis stations; this is the largest renal unit in Essex. The unit currently has over 150 patients receiving haemodialysis daily, six days a week. Basildon and Thurrock’s population Basildon and Thurrock is not a particularly deprived region of England. Over 65s constitute a lower proportion of the population in this region, compared to their proportion of the English population as a whole. However, obesity is a particular health concern in this region, just as postnatal care is below the national average on some measures. The ethnic composition of the population varies significantly between the two unitary authorities that comprise the region, with Thurrock being home to a higher percentage of Black African, Indian and other ethnic minorities than Basildon. 7% of Basildon’s population belong to non-White ethnic minorities. Childhood obesity is significantly more common, whilst breastfeeding is significantly less common than in the rest of England. Basildon and Thurrock’s health profile outlines that there are a number of aspects for which children’s and young people’s and adult’s health is significantly lower than the national average. It also shows that in Basildon and Thurrock male life expectancy is slightly lower than the national average. 1 Source: Healthcare Evaluation Data (HED) 7 Key messages from the data analysis 2 The Trust data pack identified a number of key concerns that were used to inform the KLOEs, which are outlined below . Mortality The Trust has an overall SHMI of 112 for the last twelve months, meaning that the number of actual deaths is higher than the expected level. Deeper analysis of this demonstrates that non-elective admissions are the primary contributing area to this figure, with a SHMI of 112 compared to a level of 92 for elective admissions. Specialty-level analysis of SHMI results highlighted some key diagnostic groups for further review: cancer of colon; general surgery; general medicine; palliative medicine and geriatric medicine. The Trust has an overall HSMR of 106 for the period 1 January 2012 to 31 December 2012 and which, though above 100, is still within the expected range. As with SHMI non-elective admissions are seen to be contributing primarily to the overall Trust HSMR with 107, against 84 for elective admissions. In addition, the Trust is an outlier for weekend mortality based on HED mortality; this shows mortality is not flat across weekdays and weekends. The data shows changes by small increments but the trend is consistent and weekend mortality a statistical outlier. It is noted that the Trust’s analysis of the data suggests that its death rate is flat across the full week and the weekend mortality is made to look higher due to the rate of discharge fluctuating between weekday and weekend. It is agreed that a reduction in discharge rates could potentially affect the HSMR. Specialty-level analysis highlighted areas for further review in non-elective admissions: Coronary atherosclerosis (blocked arteries) and other heart disease and senility and organic mental disorders. Review of diagnostic groups revealed further areas for analysis including cancer of bronchus, lung; cancer of colon and chronic obstructive pulmonary disease and bronchiectasis. The KLOEs for the RRR informed the panel’s observations and interviews to include a review of the specialities in the Trust with higher mortality indicators. Governance and leadership The Trust was deemed to be in significant breach by Monitor in 2009 as a result of concerns raised by the Care Quality Commission (CQC). These concerns included high mortality indicators, poor infection control and concerns regarding clinical leadership. Since this period the Trust continues to have a 'red' governance rating. There have been a number of changes to the Board over the last 18 months including the appointment of a new Chief Executive in September 2012 and a new Medical Director in February 2013. All executive roles are permanent, except for the current Director of Estates (interim) and the current Finance Director (acting up). The Trust established a new Clinical Director role on 1 April 2013, as part of the new clinically-led operational management structure which has five clinical divisions, instead of the previous three. The Trust has established a Hospital Mortality Review Group (HMRG) which meets fortnightly and is chaired by the Medical Director. It also has a Quality & Patient Safety subcommittee, which provides the Board with assurance on quality and has a non-executive chair. The Board governance structure is currently being revised following a review by the Good Governance Institute. A high level review of the effectiveness of the Trust’s quality governance arrangements was a standard key line of enquiry for the review. 2 For further information and explanations on the data analysis used please see the published data packs please at http://www.nhs.uk/NHSEngland/bruce-keogh-review/Documents/trust-data-packs/data-pack-basildonand-thurrock.pdf. 8 Clinical and operating effectiveness The Trust saw 92.3% of patients attending accident and emergency (A&E) within 4 hours in 2012. This is below the 95% target level and performance has been dropping in recent years. In the year to February 2013, 89% of patients referred to the Trust were seen and treated within the 18 week target time (RTT) which is lower than the target level. 3 The Trust’s readmission rates are lower than average and it has a shorter than national mean average length of stay for the period January 2012 to December 2012 , which is generally considered to be an indicator of efficiency. It is noted that the Trust benchmarked analysis has identified their length of stay to be above average. Patient Reported Outcome Measures (PROMs) assess the quality of care delivered to NHS patients from the patient perspective, currently covering four clinical procedures (hip replacements, knee replacements, hernia and varicose veins). PROMs calculate the health gains after surgical treatment using pre and post-operative surveys. The Trust is in line with the average outcomes across the procedures covered but the average health gain from hip replacement declined in each of the last two years, and is now close to the lower control limit (outcomes less good than average). High level reviews of clinical and operating effectiveness measures were standard KLOEs. Patient experience Of the nine measures reviewed within Patient Experience and Complaints there are three which are rated ‘red’: ‘Cancer Survey’, ‘Patient Voice Comments’ and ‘Complaints about Clinical Aspects’. Particular areas of concern from the ‘Cancer Survey’ were diagnostic tests, deciding best treatment and hospital doctors. The Care Quality Commission’s Patient Voice helpline received 144 individual comments from patients and public for the Trust in the two years to 31 January 2013. 66 of these comments were negative (46%) and 62% of complaints related to clinical treatment (the average is 47%). The Trust is A-rated by the Ombudsman for satisfactory remedies which indicates a low risk for non-compliance with its recommendations. The Ombudsman investigates complaints escalated to it by complainants who are not satisfied with the Trust's response. It rates Trusts on whether they have implemented the recommendations made at the end of an investigation in a satisfactorily and timely manner, helping to ensure that Trusts learn from mistakes. The Ombudsman rates each Trust’s compliance with recommendations and focuses on monitoring organisations whose compliance history indicates that they present a risk of non-compliance. The patient voice comments received directly to the Keogh review website (at the time of writing this report) identified the following themes from 29 emails and letters: Positive Negative Good care in intensive care unit Lack of communication Excellent after-care and treatment received after surgery Lack of basic patient care No follow up or change of medication 3 Source: HED. Data source listed as Hospital Episode Statistics. 9 Positive Negative Lack of respect for family members Neglect to inform family of illness prior to death The patient listening event also identified a number of themes for further investigation, including: Frequent bed moves for inpatients Inappropriate discharge arrangements Examples of a lack of compassion from some staff PALS appearing to serve the hospital rather than the patient. KLOEs were included in the review focusing on what patients say about the quality of care and treatment and what the Trust was doing in response to this feedback. Workforce and safety The NHS Safety Thermometer monitors trust incidents and measures rates of harm. The Trust is ‘red rated’ in four of the safety indicators: rate of “serious harm”, “harm” for all four safety thermometer indicators, pressure ulcers and clinical negligence scheme payments. The Trust is higher than average terms of the percentage of patients that develop new pressure ulcers once admitted. The Trust’s Clinical Negligence scheme payments have exceeded contributions to the ‘risk’ sharing scheme’ in each of the last 3 years. A review of the Coroners rule 43 reports flagged two items: Review of risk assessment Record keeping A review of the workforce data flagged eight ‘red rated’ indicators. Most notably the Trust’s response rate to the staff survey rate has fallen since 2011 and is below national average rate for both years on almost all indicators. The Trust’s staff engagement is below average when compared with trusts of a similar type in the 2012 National Staff Survey Results. The Trust is below the national average on all but one - care of patients/service users in my organisation’s top priority - of the organisational questions. KLOEs were included in the review focusing on pressure ulcers, workforce measures and what staff say about the quality of care and treatment. 10 3. Key Lines of Enquiry The Key Lines of Enquiry (KLOEs) were drafted using the following key inputs: The KLOEs which were included expected areas of focus for all 14 trusts building on the RRR guidance and design work. The Trust data pack produced at Stage 1 and made publicly available to tailor the KLOEs to address any areas the Trust was an outlier in (see section 3 for more details). Insights from the Trust’s lead Clinical Commissioning Group (CCG), Basildon and Brentwood CCG. Review of the patient voice feedback received via the Keogh review website specific to the Trust prior to the site visit. These were agreed by the panellists at the panel briefing session prior to the RRR visit. The KLOEs identified for the Trust were as follows: Theme Key Line of Enquiry Governance and leadership 1. Can the Trust clearly articulate its new governance processes for assuring the quality of treatment of care? Can staff at all levels of the organisation describe the key elements of the quality governance processes? Clinical and operational effectiveness 2. What actions are the Trust taking to improve mortality performance, particularly having had an ongoing issue with mortality over a number of years and a significant difference between weekday and weekend mortality? How does the Trust manage deteriorating patients? 3. What actions are the Trust taking to reduce pressure ulcers and falls? 4. What processes does the Trust have to manage bed occupancy? How does the Trust manage beds? How does the Trust manage patient moves during their time in hospital including between the main hospital and the Cardiothoracic Centre? Patient experience 5. How does the Trust seek views from patients about their experience? What are the key themes from patients on their experiences? What action is the Trust taking to address the key themes emerging? In particular, what actions have been taken to improve cancer care? 6. How does the Trust ensure adequate quality of care to patients with learning disabilities? Workforce and safety 7. What do staff groups interviewed (including trainee groups) say are the main barriers in the Trust to delivering high quality treatment and care for patients? 11 Theme Key Line of Enquiry 8. How does the Trust approach workforce planning to ensure that patient safety is managed effectively including skill mix? How is clinical cover managed out of hours particularly at weekends for patients on the emergency pathway? 9. How does the Trust support its staff with adequate training, including safeguarding training? Trust specific – pharmacy support 10. How does the Trust ensure that there is adequate pharmacy support to the wards, including out of hours? 12 4. Review findings Introduction The following section provides a detailed analysis of the panel’s findings, including good practice noted, outstanding concerns and prioritisation of actions required. A high level summary of the areas identified for urgent action are as follows: Leadership and governance: Prioritisation of improvement plans – the panel noted a significant numbers of plans for improving quality of care and services currently in place at the Trust, in response to the many reviews undertaken in recent years. The Trust needs to develop a single, prioritised action plan to focus on the key improvement areas noted in this report Developing quality focus - the Trust needs to evidence a clearer focus on quality through its improvement and delivery plans Clarity of governance – the Trust needs to ensure that its new governance structure is embedded and well communicated to its staff Clinical and operational effectiveness: Bed management – the systems for bed management and patient flows need to be urgently reviewed and improved Infection control – the Trust needs to ensure its infection control procedures are consistently applied in the organisation and undertake audits to gain assurance on this area Patient experience: Action on patient experience themes – the Board needs to urgently review and understand what their patients’ views are and address key complaints themes. Workforce and safety: Staffing and skill mix – the Trust needs to review its current staffing levels for nursing and medical staff and action any changes required for improving quality and safety of care. 13 The following definitions are used for the rating of recommendations in this review: Rating Definition Urgent The Trust should take immediate action to respond to these recommendations and ensure improvement in the quality of care High The Trust should develop a response and action plan for these recommendations to ensure improvement in the quality of care Medium The Trust should implement these recommendations to ensure ongoing improvement in the quality of care 14 Governance and leadership Overview The review into governance and leadership focused on the articulation and understanding of the new governance processes for assuring the quality of treatment of care. The following good practice was identified: The Trust has recognised that the previous governance processes were not fit for purpose and has reorganised its structure. Recognition by the Trust that it needs to improve quality of care and treatment. The visibility and positive impact of the new Chief Executive (CEO). A good working relationship between the Director of Nursing and new Medical Director. The following areas of concern were identified: An absence of organisational stability and frequent external reviews have led to a lack of clear prioritisation on improvement plans. There is a lack of clarity of governance. A focus on quality is still being developed. There is a gap between ward level and Board level in terms of understanding of quality governance arrangements. For all the above areas of concern the panel identified a number of improvements already underway at the Trust or planned improvements demonstrating the Trust’s continued progress and improvement. Many of these are in the process of implementation and are not yet embedded. 15 Detailed Findings Understanding of the new governance processes for assuring the quality of treatment of care KLOE 1: Can the Trust clearly articulate its new governance processes for assuring the quality of treatment of care? Can staff at all levels of the organisation describe the key elements of the quality governance processes? Good practice identified During interviews, the Trust Chief Executive noted that the previous governance processes were not fit for purpose and that changes were required. At the time of the visit she had started to implement these changes including introduction of a Director of Transformation, appointment of a new Medical Director and a restructuring of the clinical divisions from three to five. The changes to the Board of Directors, since the appointment of the new CEO, have been communicated to staff by the CEO through a number of ways including the CEO blog. During interviews, the Trust Executive Team acknowledged that there were issues with the quality of care and treatment at the Trust. For example, the Chief Executive recognised that prior to her appointment the Trust had achieved its financial targets but quality and safety were not considered such a high priority. The Trust had not prioritised care of its emergency patients and sickest patients. Furthermore, the Executives interviewed recognised the significant levels of work needing to be done at the Trust to change the culture and focus on quality and patient experience. The CEO had appointed a Director of Transformation to ensure a focus on the transformational work, to prioritise actions and clearly focused on long term sustainable solutions. Throughout the visit during focus groups, one to one interviews and ward observations the staff throughout the Trust noted the visibility and positive impact of the new CEO, citing the CEO blog as one such example. We observed a good working relationship between the Director of Nursing and new Medical Director, further demonstrated by the joint chairing role of the Clinical Quality Board. Patients, staff and the Trust Board interviewed consistently spoke of a changing culture at the Trust, albeit slowly, to one of improvement and forward planning. The Trust recognises the significant amount of work still to be done. 16 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium i. Absence of stability and clear prioritisation The Trust is now demonstrating a desire to review current practices, understand issues and design solutions in a more proactive way so as to sustain the required improvements. The Trust should put in place a single clinical strategy for the Trust. High The Board should approve a single, prioritised action plan for the Trust showing clearly the priorities by time period, e.g. for the next six months, six months to a year and so on. This should be clearly communicated to staff. Urgent The Trust has been under scrutiny for an ongoing period and has undergone a number of reviews; including a number commissioned by the new Chief Executive to gain an in-depth understanding of the issues at the Trust. Historically the Trust has generally been viewed as a reactive organisation rather than a proactive one when dealing with issues and concerns. A number of staff members talked of the number of reviews that the Trust has undergone in recent years and the tendency of the Trust Executive to react with significant change in response to the reviews. Staff members referred to “knee jerk reactions” and spoke of not being able to see initiatives through and evaluate their impact, moving onto the next thing before completing the last. Staff expressed concern that they did not know whether initiatives had been completed, for example ‘right patient, right place’, which some thought had been abandoned. In January 2013, the Trust appointed the Director of Finance as Deputy Chief Executive and gave him the responsibility of leading the Trust’s transformation programme. Interviews with the Chief Executive identified that this role will include prioritisation of actions for the Trust. The Chief Executive and Chair have stated that they will ensure that they will regularly review, through the board development programme, that the Trust has the necessary skills, background and experience to lead the organisation on an ongoing basis. Whilst the Executives interviewed referred us to a number of action plans in place, we observed an absence of prioritisation of the actions. Staff, including some of the Executive Team, were unable to clearly articulate the key priorities for the Trust. 17 Outstanding concerns based on evidence gathered ii. Lack of clarity of governance arrangements Key planned improvements The restructuring of clinical governance is underway and the Whilst Board members interviewed could articulate members of the Executive interviewed the governance restructuring, this was still in the stated the implementation date as 1 implementation stage. A number of actions will not be June 2013. in place until 1 June 2013 so it was not possible for the panel to understand the new arrangements fully. An improvement plan in place is using the Hub, the Trust’s intranet The majority of staff members interviewed had a communication tool, as a mechanism limited understanding of the new structure and lines of of communication. accountability going forward. Recommended actions Priority – urgent, high or medium Communication of the revised structure to all staff, clearly detailing the new structure, and the policies and processes to be used, so there is clarity of how the new system works. Urgent Middle management should be engaged to ensure that communication is effective throughout the Trust. Medium 18 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium iii. Quality focus still being developed The Chief Executive stated that a NED with a clinical background will be sought as part of the next rotation of NEDs. The Trust will need to consider how it develops a clearer focus on quality, based on transparent information and a tone from the top. This should include implementation of the planned improvements and recommended actions in this report. Urgent The Trust has a Quality and Patient Safety Committee, which is a subcommittee of the Board. It was clear from our interviews with the Chief Executive, Medical Director and Director of Nursing that they recognised the need for a quality and safety focus to be developed at the Trust. The Trust governors attending the focus group stated that they had appointed Non Executive Directors (NEDs) with the background and skills to address the issues faced by the Trust. We noted the following issues: The Trust does not have a NED with a clinical background. The Board agenda has not had a Nursing Report presented for over a year. The Board does not hear patient stories (see also KLOE 5). The Board only receives details of numbers of complaints and response times, not the detail of the complaints (see also KLOE 5). The panel could not clearly see quality risks recorded on the Board Assurance Framework. The Governors did not appear to take a fully active role on quality, receiving information rather than actively requesting it and using it to challenge the Trust. We were informed that a Nursing Report was to be received by the May 2013 Board meeting. Governors should be more active in their role of holding the Board to account on all aspects of We were informed that a patient story quality. The Trust has 50 governors and should would be heard by the May 2013 consider a reduction in numbers of governors and Quality and Patient Safety offer them further development so they can Committee. undertake their role more effectively. High The recent appointment of a new Medical Director in January 2013 along with the new Chief Executive alongside the Director of Nursing was cited by a number of staff spoken to as increasing the quality focus at the Trust. Governors commented they now considered the Trust engages with them and responses to their concerns. 19 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions iv. Gap between ward level and Board level A number of staff interviewed provided positive feedback on actions underway by the Chief Executive in particular, including reference to increased visibility and the CEO blog. The Trust Board should consider how it can High strengthen their visibility, accessibility and listening mechanisms with staff (also with patients and the public, see KLOE 5). This could include visiting areas of the hospital, including at night and during weekends, to understand the current position and any concerns. The panel considered that processes and actions articulated by the Board members interviewed were not consistently understood by ward level staff interviewed. Whilst staff interviewed spoke positively of the Board, the majority of comments were specific to the Chief Executive rather than the Board as a whole and very limited reference was made to the NEDs. A number of staff interviewed spoke of the Executive Team open door policy in a positive manner, although comments were made that this was seen as an open door to more senior staff rather than all staff. It was also noted that the open door policy was unrealistic in practice, as the management offices were separately located at a distance from operations. Comments were made that the Board only visited the staff to perform checks and audits. Continued executive open door policy. Priority – urgent, high or medium These visits should be clearly distinguished from audits and checks performed by the Board throughout the Trust. These should involve all Board members and the Trust should consider including NED only events. High Board to review the BAF and ensure that it captures significant risks to the quality of care and treatment, including workforce issues, considering patient and staff feedback and concerns. High It was clear that the changes being implemented were closing the gap and the panel observed a positive movement in this area. Staffing issues are not included within the Board Assurance Framework, (BAF) despite there being poor morale amongst some staff and concern about staffing levels. 20 Clinical and operational effectiveness Overview The three KLOEs in the clinical and operational effectiveness area focused on the following: Actions to improve mortality performance, particularly having had an ongoing issue with mortality over a number of years and weekend mortality being a statistical outlier based on HED mortality. Actions to reduce pressure ulcers and falls. Management of beds. The following good practice was identified: The Patient at Risk Support (PARS) escalation process and team. Development of a real time measure of SHMI (crude) for ongoing monitoring, as well as detailed mortality reviews. Examples of good levels of cleanliness. The use of sepsis care bundles. Good assessment practices and incident reporting for both pressure ulcers and falls. Regular bed management meetings to manage capacity challenges. The following areas of concern were identified: Understanding of mortality issues throughout the Trust. Dissemination of lessons learned throughout the Trust. Out of hours staff cover. Examples of areas where the panel observed that infection control management still needed to be improved. An effective ambulatory care operating model was not clearly in place. Quality impact assessing of cost improvement plans (CIPs). The need for wider and consistent use of care bundles. 21 Inconsistent use of Trust policy for pressure ulcer grading. Bed flows and management. For the majority of the areas of concern, above, we identified a number of improvements planned or already underway at the Trust evidencing continued progress. Detailed Findings Improvement of mortality performance KLOE 2: What actions are the Trust taking to improve mortality performance, particularly having had an ongoing issue with mortality over a number of years and a significant difference between weekday and weekend mortality? How does the Trust manage deteriorating patients? Good practice identified Staff interviewed were consistently very supportive of the PARS team for management of deteriorating patients and their support and visibility on the wards. Escalation of concerns was evidenced through review of a sample of patient notes and speaking with members of the PARS team who confirmed that sicker patients were referred to them throughout the Trust. The Trust has developed a real-time crude SHMI to monitor mortality performance on an ongoing basis. One key consultant was found to be undertaking 100% death reviews and findings were being discussed with peers at mortality review meetings, evidencing a sharing of lessons learned. In addition 20% of mortality reviews are independently assessed. The Trust is participating in the national cardiac arrest audit. During the visit, examples of good practice were observed and staff and patients provided further examples, including: Bulphan ward – good practice and good level of care observed. Caring assistance provided to elderly people with eating. Lionel Cosins ward – observers impressed with the level of care given to elderly patients. Kingswood ward – good levels of care observed. Orsett ward – able to demonstrate evidence through the nearest set of patient notes to the observation team indicating a consistent approach to care. Pre-assessment service for surgical elective patients. In-patient risk and assessment documentation. Fracture of the femur service including excellent multi professional orthopaedic team and theatre capacity. During the visit, examples of good levels of cleanliness observed, including: Patient observations that A&E is cleaner than previously. Examples of clean wards observed throughout the Trust. 22 Good practice identified Elsdon ward out of hours observation found the ward to be clean and tidy and infection control was considered by the observers to be very good. The discharge lounge and refurbished clinical decision unit were observed to be well designed clinical areas, including being in close proximity to A&E. The Trust’s use of sepsis care bundles. Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium i. Understanding of mortality issues throughout the Trust The governance restructure includes the Quality and Patient Safety Committee responsible for the review of the Trust developed crude SHMI. The Trust should consider ways to increase understanding and ownership of mortality performance throughout the organisation. This should include mortality reviews undertaken through multidisciplinary speciality groups so that these groups take ownership of mortality performance. High Mortality performance is an agenda item at Board meetings. This agenda item is led by the Medical Director and Director of Nursing with support from a NED. When interviewed, a number of staff and governors within the organisation stated that the Trust’s mortality performance was due to sicker patients being admitted (which is to some extent already taken into account in calculating mortality rates). The Trust Executive Team and staff did not demonstrate that they had reviewed mortality data in detail to understand the root causes and identify improvement actions that could be taken. ii. Dissemination of lessons learnt There was limited evidence of systematic mortality and other clinical reviews being undertaken, lessons being learnt and dissemination of these themes across the whole Trust. The Trust has a mortality reduction programme that has three strands – improving information, focus on outlier pathways and mortality review. The Board has an explicit prioritised objective to reduce crude mortality to less than 2%. The panel obtained evidence of good practices throughout the Trust and reviews were being undertaken to learn lessons from them. For instance cross-ward senior nurse meetings were being held See the single prioritised action plan recommended High in KLOE 1(i) – to contain reference to improvement of mortality performance and actions that the Trust own to manage performance. This should be clearly communicated to all staff. The Trust should evaluate the performance of the new Quality and Patient Safety Committee by the Board in six months to assess its effectiveness in monitoring and managing mortality performance. Medium The Trust should consider further investment in High learning from reviews and ensure that lessons learnt and key themes are clearly disseminated throughout the organisation. Medical staff job planning should be reviewed to High 23 Outstanding concerns based on evidence gathered From discussion with medical staff, it appeared that they have very little protected time to undertake clinical audit. The panel observed that many board clinical audit reports were incomplete. iii. Out of hours staff cover Key planned improvements Recommended actions Priority – urgent, high or medium periodically, enabling good practice to be shared and nurses to learn from each other. ensure all medical staff have protected time that is appropriately used to undertake clinical audit and attend clinical audit meetings. See KLOE 8(ii) for details. See KLOE 8(ii) for details. The Director of Nursing states that the Trust has an infection control action plan. Immediate improved infection control using policies consistently across the Trust through ownership at divisional and ward level. Urgent Use of processes that incentivise the staff to comply with infection control policies, for example publication of infection data by ward. High Board to review infection control plan and to seek assurance that leadership is in place at all levels to deliver the action plan. High Ambulatory care should be further reviewed and developed at the Trust, working with the CCG to agree protocols for common ambulatory conditions. High We identified issues with staff cover, including junior doctor workload, particularly out of hours and at weekends. This will impact performance and effectiveness. See KLOE 8(ii) for details. iv. Examples of infection control concerns Whilst the panel observed examples of good practice in infection control during the site visit, issues were also noted in some areas: A member of staff entering an isolation area without using universal precautions. Observation of the Surgical Referral Unit, out of hours, found a number of infection control concerns on the ward including empty drip bags, IV lines with no covering on the end and no evidence of IV line labelling. Concerns raised by staff about the building work in the Cardiothoracic theatres proceeding without infection control input. v. Ambulatory care model not evidenced The panel did not obtain evidence that the ambulatory care model was sufficiently well defined at the Trust. None identified 24 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium The Trust was only using ambulatory care for one clinical indication and examples were noted of unnecessary admissions. vi. Quality impact assessment of CIPs The Trust has a £15 million CIP target for 2013/14. Whilst interviews with Executives evidenced some clinical sign off of CIPs, the panel did not identify a clearly articulated and consistent response as to how CIPs are Quality Impact Assessed (QIA) before approval, or monitored once implemented. Whilst some interviewees stated that the Medical and Nursing Directors are involved in all CIP sign off, the Medical and Nursing Director themselves said they were involved only where there was a patient impact. The Medical Director and Director of The Medical Director and Director of Nursing’s Nursing are involved in some CIP involvement in all CIP sign-off should be understood sign off. and clearly and consistently articulated by all Executives with Board sign-off of the full CIP programme for each year. The QIAs should be regularly reviewed and monitored. Where a concern over quality is identified, this risk should be properly mitigated before the plan is allowed to go ahead / continue. In future years, the full CIP programme with QIA should be completed and signed off by the Trust Board before the start of the financial year. High High There was a wide variation in the value of CIPs considered to be signed off and approved by different members of the Executive Team ranging from £6m to almost all of the full £15m. Executives were unable to give strong examples of where the Board had stopped a proposed plan being implemented or subsequently paused or changed due to quality concerns. The Trust state that this is due to 2012/13 CIPs largely consisting of additional income due for extra activity from the PCTs rather than being quality related. There appeared to be no quality monitoring process for CIPs. Executives were unable to clearly articulate triggers that would be used by the Board to identify if 25 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium The Trust states that it is actively reviewing care against care bundles and leads have dedicated time allotted for pneumonia, sepsis, COPD, AMI (acute myocardial infarction) and senility. Regular planned audits of the use of all care bundles High should take place and the results shared with clinical teams and at Board level. delivery of a CIP is leading to a quality issue and the need to consider pausing, stopping or changing a CIP. The Trust state that the root cause of this issue is not a weakness in process but one of articulation in part caused by the timing of the review falling at the start of the financial year and an issue articulating the differences between 2012/13 and 2013/14. vii. Use of care bundles Care bundles for the management of patients with some common conditions such as pneumonia and sepsis were available in the Trust. However, the panel noted that these were not always used by clinical staff on wards observed. Pressure ulcers and falls KLOE 3: What actions are the Trust taking to reduce pressure ulcers and falls? Good practice identified The panel observed good assessment practices in place for both pressure ulcers and falls, with the Trust tools for these areas seen to be being used by staff. Good use of systems was evidenced for both skin assessment and the falls process, with appropriate access to equipment. The panel observed actions taken by staff to reduce pressure ulcers including observing good use of slide sheets and air mattresses. The panel’s review of the Hub and discussion with staff concluded that it was a straightforward process to order equipment to reduce pressure ulcers such as mattresses. Review of a sample of patient notes provided evidence of comfort rounds taking place. Review of incidents reported provided evidence of good reporting of both falls and pressure ulcers as incidents. 26 Good practice identified Staffing structures were seen to include pressure ulcers and falls nurses in post. Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium i. Inconsistent use of Trust policy Verita, an external consultancy, has reviewed all serious incidents including falls and pressure ulcers for any learning. Ensure that the latest pressure ulcer policy is communicated to all staff and that staff understand and apply it across the organisation. High Whilst the Trust provided evidence of a pressure ulcer grading policy, we did not see evidence of an embedded, owned policy or guidance at the Trust. Discussions with staff on Orsett ward identified that staff had developed their own policy. Staff interviewed explained this was due to the Trust policy being too complex. The Trust changed its policy in line with all of the East of England trusts last year as part of Learning from Verita work to be shared with the ‘Stop the Pressure’ campaign. staff Medium Bed management KLOE 4: What processes does the Trust have to manage bed occupancy? How does the Trust manage beds? How does the Trust manage patient moves during their time in hospital including between the main hospital and the Cardiothoracic Centre? Good practice identified The Trust staff detailed in interviews the regular bed management meetings held at the start of the day, midday, mid afternoon and an optional fourth meeting depending on the need for it. The staffing structure was seen to include a discharge doctor at weekends to support bed management. The Trust has an elderly care strategy including the use of medi-home. The Chief Executive stated that she had implemented increased consultant presence during week days and weekends. Staff interviewed spoke positively of 27 Good practice identified this for leadership decisions and support. Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium i. Bed flows and management A single patient tracking system is being implemented and was observed by the panel on Katherine Monk ward. Full implementation of real time patient tracking to manage flow rather than record issues post event. Urgent The Trust has high activity levels as evidenced by performance data and the panel’s observations. Also staff and patients interviewed consistently spoke of how busy the hospital was. Whilst the Trust Board members interviewed recognised the issue, we did not obtain evidence of a clear and prioritised plan to address the issues with bed management. Throughout our visit we identified evidence of poor bed management and flows including the following: Use of escalation areas over extended periods, including the use of the Surgical Referral Unit and Cardiac Suite to bed patients down. A high number of outliers which did not appear to be managed. A high number of patient moves during in-patient stays. Observation of ambulances stacked outside A&E. The panel also reviewed: A&E waiting times through the system and by speaking to patients and staff. This process identified patients regularly breaching the four hour target. Acute Medical Unit (AMU) stays through discussion with a number of patients. Patients stated that their stay exceeded the 48 hours for which the AMU was designed and some patients stated that they had been in the unit up to 14 days. Improved bed flows and management through: Urgent Review of systems to enable best use of beds at all times including ensuring staff have access to, and are making effective use of, patient flow IT systems. A move to seven day working, with Senior doctors reviewing in-patients every day on all wards. Improved end of life care planning and application, discharge planning. To review use of the PARS team and ward rounds to provide assurances that the policies are being consistently applied. Better use of the discharge lounge To systematically review discharge planning at all stages of a patient’s journey to enable safe and effective discharge. High Bed flow and management should be underpinned by quality of care and treatment and making effective use of the service. Additional beds should be considered as a last resort and only in agreement with commissioners. 28 Outstanding concerns based on evidence gathered Other issues noted included: A number of patients interviewed stated that they had been inappropriately discharged and required readmission (this could not be investigated by the panel further). Whilst patients with dementia were confirmed to be transferred to wards on ground level to reduce the risk of harm, the panel identified a number of dementia patients not being cared for on appropriate wards. Temporary areas being used for patients were observed to not be consistently fit for purpose. For example there were no showers for inpatients in AMU where patients were staying for period for up to 14 days. Observation of the discharge lounge identified poor use of a good facility with one patient and four staff. Staff interviewed, particularly junior doctors, spoke of the pressure to discharge patients due to the shortage of available beds. Some staff spoke of an overuse of the PARS team and we observed the use of the PARS team on a palliative care ward. A number of staff also noted the reluctance of some medical staff to discuss end of life care and discuss the application of Do Not Resuscitate agreements. Observation of the operations room identified that staff did not have access to the relevant patient flow IT systems without IT support. Absence of real time patient tracking and multiple systems in place to monitor patient location – A&E list, AMU list (manual), PAS (reliant on a ward clerk to update) and the doctor list. Key planned improvements Recommended actions Further staff training on dementia including appropriate wards for dementia patients to be transferred to for care. Priority – urgent, high or medium High A strategy should be developed through joint engagement with the CCG to make increased use of High other facilities. This could include reviewing use of the minor injuries unit at Orsett Hospital. Also this should include wider health system engagement to make better use of hospital beds including using out of hospital care, preventative strategies and community care. 29 Patient experience Overview The two KLOEs in the patient experience area focused on how the Trust understands and responds to patient feedback and adequate quality of care to patients with learning disabilities. The following good practice was identified: Examples of good levels of patient care and treatment and good experiences from the patients. Feedback leaflets within wards and electronic feedback points around the Trust. A learning disabilities nurse was identified as being in post. Interviews with staff confirmed that staff were aware of how to contact her if necessary. The following areas of concern were identified for patient experience: Systematic Board understanding of patient experience. Clarity over actions taken in response to concerns and complaints. Patient communication and engagement. For the majority of the areas of concern above, we identified a number of improvements planned or already underway at the Trust evidencing continued progress. 30 Detailed Findings Patient involvement and experience KLOE 5: How does the Trust seek views from patients about their experience? What are the key themes from patients on their experiences? What action is the Trust taking to address the key themes emerging? In particular, what actions have been taken to improve cancer care? Good practice identified During the visit examples of good practice were observed and staff and patients provided further examples, including: Bulphan ward – good practice and good standard of care observed. Caring feeding of the elderly observed. Lionel Cosins ward – observers were impressed with the level of care given to elderly patients. Pre-assessment service for surgical elective patients was noted by the panel to be good practice. Evidence of in-patient risk and assessment documentation. Existence of fracture of the femur service, including excellent multi-professional orthopaedic team and theatre capacity. Examples of good experiences of care and treatment at the Trust provided to a number of patients spoken with. Leaflets observed within wards detailing how to provide feedback to the Trust as well as electronic feedback points had been installed at the Trust. There were protocols in place for Individual Care Plans. Outstanding concerns based on evidence gathered Key planned improvements i. Systematic Board understanding of patient experience We were informed that a patient story Patient stories to be regularly heard by Urgent would be heard by the 2013 May the Board with lessons learned from the Quality and Patient Safety Committee story and any action required as a result. Whilst Board members interviewed spoke of knowing about patient experiences, issues were noted with the lack of processes in place to ensure they monitor it regularly, including: The Board does not hear patient stories. Whilst the Trust states that is has a monthly Patient Experience data report, providing analysis of all areas of patient experience feedback including complaints received, the Board only receives details of numbers of complaints and Recommended actions Priority – urgent, high or medium The Board should receive a summary Urgent of the substance of complaints, trends and themes as a minimum. This should be reviewed and an action plan agreed to respond to key themes. 31 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium The complaints process needs to be quickly reviewed to ensure there is clarity of the role of PALS. High response times, not the detail of the complaints. The panel did not see evidence of action being taken in response to these complaints. ii. Clarity over concerns and complaints The Trust states that considerable work is underway in the management The Trust has policies for incidents and complaints and these are of complaints including: under review. Introduction of a Senior Nurse to provide specialist support to Interviews with staff identified a lack of clarity, from the majority patients and their carers / interviewed, as to what constituted a Patient Advice Liaison relatives. Service (PALS) concern and how this was differentiated from a Development of focused KPIs complaint. Staff also struggled to articulate the complaints process (key performance indicators) and definition of “serious” consistently. regarding the quality of service provision and data indicating Some comments were received from patients that the perception themes and trends within quality was that the PALS service was there to serve the Trust and not measures. patients. Patient information is being developed with new leaflets Some staff interviewed indicated they did not feel they could raise regarding PALS and complaints. concerns and that action will be taken. Planned move of the Patient Experience Team alongside PALS to strengthen routes of referrals between the teams. Links are being developed between chaplaincy and bereavement teams, which will also include counselling services. Creation of a new post of Patient Experience Lead commencing 1 July 2013. Definitions of and policies for concerns, High complaints and serious incidents should be reviewed and clarified, so that the terminology and processes are understood by all staff. Executive Team should take action to: - Remind staff of their responsibility to raise concerns as per the whistle blowing policy, - Promote a positive culture towards complaints, including consideration of a complaints forum for patients and relatives, supported by the Governors. High 32 Outstanding concerns based on evidence gathered Key planned improvements Recommended actions iii. Patient communication and engagement The Trust has installed electronic feedback points around Basildon Hospital. Real patient communication and High engagement through: Report patient stories at Board. Actions taken in response to patient feedback communicated to patients. A culture of openness to issues to be further developed. Consideration to be given to moving PALS from the CTC to front of house to make finding it easier. Increased communication of accurate expected discharge dates consistently to all patients. Involvement of patients and carers in their care plans. Actively seeking feedback from patients and relatives. Whilst we observed leaflets within wards on how to provide treatment and the electronic feedback points, interviews with patients identified that the majority had not noticed either of them and were unaware of how to provide feedback to the Trust. Further issues were noted with patients including: The majority of patients interviewed out of hours in A&E cited communication as the one area that the Trust could improve in. Examples provided included the provision of better signposting towards the assessment nurse on arrival, as well as better communication of the A&E waiting times and process. Significant numbers of in patients interviewed were unaware of their expected discharge date (EDD). There were examples of the EDDs showing on ward boards in a number of wards being inaccurate. More than one patient stated that they would not provide feedback to the Trust or make a complaint either due to an assumption that nothing would be done, or due to fear that they would not receive good treatment if they complained. The panel found the location of PALS difficult to find. Furthermore when panel members spoke to PALS they were not able to provide evidence that the team were working for patients rather than the Trust (as per concerns raised above). The panel identified only limited evidence of patient and family involvement in the design or application of care plans and treatment. PALS is located in the hospital. Leaflets on the complaints procedure were observed within wards. The recent appointment of a new Medical Director in January 2013, along with the new Chief Executive and the Director of Nursing, was cited by a number of staff spoken to as increasing the patient focus at the Trust. Better signage is planned for PALS. Priority – urgent, high or medium See also ii above 33 Patients with learning disabilities KLOE 6: How does the Trust ensure adequate quality of care to patients with learning disabilities? Good practice identified A learning disabilities nurse was identified as in post and interviews with staff confirmed that staff were aware of how to contact her if necessary. Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium No significant outstanding concerns. 34 Workforce and safety Overview The three KLOEs in the workforce and safety area focused on staff views of the main barriers in the Trust to delivering high quality treatment and care for patients, workforce planning and staff training. The following good practice was identified: Workforce is generally committed, loyal, passionate, caring and motivated. Orthopaedics was cited by a range of staff as a general exemplar of effective rotas and ward systems. The surgical handover room was observed as well set up. The following areas of concern were identified within workforce and safety: Staffing levels and skill mix need urgent further review. Implementation of NHS Professionals (NHSP) did not appear to have been well managed. Consistency and comprehensiveness of training, including adult safeguarding training. For the majority of the above areas of concern, we identified a number of improvements planned or already underway at the Trust evidencing continued progress. 35 Detailed Findings Staff issues KLOE 7: What do staff groups interviewed (including trainee groups) say are the main barriers in the Trust to delivering high quality treatment and care for patients? Good practice identified From interviews with the staff, the panel found the workforce to be committed and loyal to the Trust. The vast majority of student nurses interviewed stated that they would like a job at the Trust. The panel observed passionate and caring staff including a number of staff attending the listening event as they wanted an awareness of the patient feedback. A large number of staff observed appeared to genuinely care and want the best for their patients despite the high level of negative press and local criticism of the Trust. Good care was observed within the Trust. Nursing teams and junior doctors were noted as being particularly motivated and driven; despite a high workload they were found to be putting in the energy and effort to meet demand. Friendly, receptive and open staff, welcomed the review panel. Some staff said that they felt they were able to be open about concerns and could provide examples of the Trust Board acting upon feedback. Outstanding concerns based on evidence gathered Key planned improvements A number of issues raised by staff have See KLOE 8 been included in the relevant KLOE. For instance staff observed were clearly under a high work load and pressure due to staffing levels and skill mix - see KLOE 8 Recommended actions Priority – urgent, high or medium See KLOE 8 36 Workforce planning KLOE 8: How does the Trust approach workforce planning to ensure that patient safety is managed effectively including skill mix? How is clinical cover managed out of hours particularly at weekends for patients on the emergency pathway? Good practice identified Orthopaedics was cited by a range of staff as a good example of an effective staff rota and ward systems. Observation of the surgical handover identified good practice with six PCs and a proper PACS (picture archiving communication system) screen supporting a handover process. The process included the detail of the patient condition, what had been done and what needed to be done. Staff commented on improvements made by recent increases in senior medical presence in some parts of the Trust into extended hours Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium i. Staffing levels and skill mix An additional overnight registrar has been in place over the last three months. Noted this post is being filled on a temporary basis through locum support. Full staffing levels and staff mix reviews to be completed across nursing and medical staff. Urgent Relieving clinicians care time through initiatives such as: Advanced nursing roles. A review of numbers of Cannula and phlebotomy support. nursing has been Nursing sister triaging calls. completed and a paper is Greater use of administration staff. due to go to the May 2013 Electronic booking system. Trust Board. Real time patient tracking. Additional overnight registrar post to A similar review of medical be made permanent. numbers is planned. Urgent The Trust activity levels are high and Basildon Hospital is very busy as observed by the panel and cited consistently by staff and patients. A number of issues were noted by the panel with staffing levels and skill mix: Junior doctor workload, particularly overnight, was pressured. A recent junior doctor audit had identified the work required for a 12 hour shift was an average of 19 hours. Panellists particularly noted concerns around obstetrics and gynaecology cover and the majority of staff, from throughout the Trust, highlighted concerns over junior doctor workload and welfare. Due to the use of escalation wards and high number of outliers, we identified a number of areas where the ward skill mix was not appropriate to the patients on the ward at that time. The staffing levels were observed to not be consistently sufficient, for example we observed a nurse in charge responsible for caring for 10 Review of recruitment processes to ensure that there is interaction with the ward managers for staff who are being High 37 Outstanding concerns based on evidence gathered Key planned improvements patients during an overnight shift. We also observed long wait times in A&E, paediatric A&E and the fracture clinic. Discussion with staff during interviews identified a number of vacancies on all shifts dependent on agency and bank staff. A number of staff further commented on the recruitment process as being disengaged with operations and for having issues with communications, for example staff arriving to commence work without this being communicated to the ward. A number of staff interviewed felt that there was an increase in paperwork that took away from hands on care. Health Care Assistants (HCAs) stated that they felt they were doing more observations and bed baths that expected. ii. Implementation of NHS Professional (NHSP) At the time of our visit, the Trust had recently implemented NHSP and a Steering Group had been in place to govern its implementation. Discussions with a number of staff identified issues with the implementation including operational deployment, management and payment of temporary staff. This was observed to be a significant risk to quality of care for patients during the visit and escalated to the Trust. Recommended actions Priority – urgent, high or medium recruited. None identified The Trust should demonstrate implementation issues have been addressed. Urgent The Steering Group should continue to meet post implementation to closely monitor and manage NHSP. Urgent It was also identified that the Trust did not plan for the Steering Group to meet following implementation. This issue was escalated to the Director of Nursing on 8 May 2013 when it was identified by the panel as it was felt it could be a significant risk to the quality of care and treatment. 38 Staff support and training KLOE 9: How does the Trust support its staff with adequate training, including safeguarding training? Good practice identified The feedback provided by the junior doctors who attended the focus group was that training and support was generally good. This was consistent with interviews with junior doctors during observations. Interviews with staff in paediatrics concluded that staff in paediatrics had a strong understanding of safeguarding processes. During the observation of the paediatric A&E out of hours, the sister in charge was able to clearly articulate the safeguarding process to a level of detail that impressed the panel members interviewing her. Outstanding concerns based on evidence gathered Key planned improvements Recommended actions Priority – urgent, high or medium i. Consistency and comprehensiveness of training The Trust has rolled out increased e-learning to address mandatory training completion issues. Student nurses to be consistently provided with appropriate training including ward training. High The Trust has rolled out increased e-learning replacing face-to-face training. Staff interviewed were mixed in their response to this, with a significant number responding negatively due to the decreased networking opportunities and opportunities to share lessons learned as well as the reliance on computer literacy and confidence. To review the use of e-learning based High on staff feedback. Staff to be provided with opportunities to network and share ideas. From interviews with nurses and the Executive, the panel identified that the nursing development strategy was not clear. Strategy for advanced nursing roles and nursing development. Medium Student nurses interviewed stated that they were provided training through the university but were not involved in ward training. See also KLOE 4(i) regarding dementia training. Furthermore it was identified that the Qualification and Credit Framework (replacing NVQ) for students has been stopped and the panel observed inconsistent practices by student nurses. See also KLOE 4(i) regarding dementia training ii. Consistency of safeguarding training, particularly for adults The Trust is currently recruiting to The safeguarding training provided to Medium 39 Outstanding concerns based on evidence gathered While staff members in paediatrics interviewed were able to clearly articulate paediatric safeguarding processes, this was not consistent for all staff interviewed. Panel members were provided with vague details on the escalation route for adult safeguarding issues. Key planned improvements Recommended actions the post of an adult safeguarding lead. be sufficient so that staff can clearly articulate the safeguarding processes, particularly for adults. Priority – urgent, high or medium The panel noted that the post of Nurse Advisor for safeguarding and disabilities is vacant and that this role is being covered by the Deputy Director of Nursing. 40 Pharmacy support Overview Due to the issues identified in the data pack related to use of out of date drugs, a specific KLOE for pharmacy support to the wards was included. The following good practice was identified: Daily ward visits by pharmacy technicians who review all drug charts and drug trolleys. The following area of concern was identified: Risk of incorrect drugs being prescribed due to inadequate labelling. Detailed Findings KLOE 10: How does the Trust ensure that there is adequate pharmacy support to the wards, including out of hours? Good practice identified Staff informed the panel that wards have daily visits by pharmacy technicians who review all drug charts and drug trolleys. Outstanding concerns based on evidence gathered i. Risk of incorrect drugs being prescribed Key planned improvements The Trust states that a review of this process is During interviews with staff the panel identified that, for efficiency, the list of drugs already underway and is a for discharge uses coding for drugs of alphabetic lettering (i.e. A, B, C rather than key element of the newly either specific codes for specific drugs or the full name of the drugs along with the developed Strategy for dose). Pharmacy Services and Medicines Management. Whilst the panel recognise the efficiency from the process, there is a risk of incorrect drugs being issued. Interviews with staff identified that incorrect prescriptions were not uncommon. Members of the public also spoke of concerns with this issue. Recommended actions Priority – urgent, high or medium Consideration to be given to the full details to be seen by the pharmacy to enable a check to be made. High 41 5. Conclusions and support required Conclusions The Executive Team and staff recognise that the historical culture of the Trust was focused on financial targets and that finances were prioritised over quality. This is now a Trust undergoing significant transformation with a new Chief Executive, Medical Director and Chair. The Chief Executive and Chair have stated that they will regularly review the board to ensure, through its development programme, that the Trust has the necessary skills, background and experience to lead the organisation on an ongoing basis. The Executive Team interviewed recognised both the issues at the Trust and the need for change. The Chief Executive and Chair are clear that the tone at the top should be one of long term sustainability and not short term solutions. As a result a transformation programme is underway. There is a lot to do within that and many priorities, for which there needs to be an explicit plan (with timelines) to ensure all staff are aware of what is important and the pace of change. Although the Trust is on a transformation journey members of the Board need to ensure that they close the gap between ward level and Board level, communicating and engaging with the staff throughout. This should include being clear as a Board on the quality priorities and in communications with staff on transformation plans. The Trust also needs to ensure that the effectiveness of the transformation is regularly evaluated, ensuring that patients remain at the heart of this improvement journey. The Trust is currently delivering financial targets but under extreme service pressure with high activity levels evidenced throughout our visit. It is noted that the 2012/13 surplus was delivered due to the commissioners funding the increased activity and that the Trust is yet to fully identify the £15m CIP target for 2013/14 despite being two months into the financial year. During interviews the Executive Team were unable to clearly articulate the process for quality impact assessing cost improvement plans and the Trust must ensure that costs are managed without compromising patient care and treatment. The Trust has been under scrutiny for some time and has undergone a number of reviews, including a number commissioned by the new Chief Executive, to gain an in-depth understanding of the issues at the Trust. Historically the Trust has generally been viewed as a reactive organisation rather than proactive one when dealing with issues and concerns. The Trust leadership now want to review current practices, understand issues and design solutions in a more proactive way so as to sustain the required improvements. They are on an improvement journey and the next stage is, perhaps, the most challenging, requiring implementation and embedding changes in practice - a period of stability is required to enable the Trust to deliver this challenging programme of transformation. Until this implementation and embedding is complete, the effect of the changes cannot be assessed as appropriate. Our review identified a number of areas of good practice, although these generally related to specific areas, wards or specialities. Therefore there is more for the Trust to do in ensuring good practices are in evidence across the organisation, all of the time. Our review also identified a number of areas of outstanding concerns across all ten KLOEs. For the majority of areas we identified a number of improvements either already underway at the Trust or planned actions. However we have included further recommended actions for each area including a number of areas of concern outstanding from the July 2012 Silverman report. These include, for example, the presence of medical outliers and examples of infection control issues. 42 Urgent priority actions for consideration at the risk summit Problem identified Recommended action for discussion Support required by the Trust 1. Stability and prioritisation (see detailed finding at A single, prioritised action plan for the Trust showing clearly the priorities for the Trust by time period, e.g. for the next six months, six months to a year and so on. This should be clearly communicated to staff. Support from external stakeholders for a period of stability for the Trust. A clear focus on quality based on transparent information and a tone from the top. Quality governance support. Communication of the revised structure to staff, clearly detailing the new structure. The policies and processes to be used also need to be shared at the same time. Communication and supporting policies and processes. Improved infection control practises need to be applied consistently across the Trust, all of the time. Infection control support. page 16) Absence of stability in governance and clear prioritisation of actions. 2. Quality focus (see detailed finding at page 18) Quality focus of the Trust is still being developed. 3. Governance structures (see detailed finding at page17) Lack of clarity of governance structures. 4. Infection control (see detailed finding at page 23) Whilst the panel observed examples of good practice in infection control during the site visit, the panel also observed examples of infection control issues. 43 Problem identified Recommended action for discussion Support required by the Trust 5. Bed management and flows (see detailed finding Full implementation of real time patient tracking, either through a single system or automated links between those systems used to track patients. Support for implementation of a real time patient tracking system. at pages 27 to 29) Throughout our visit we identified evidence of poor bed management and flows. 6. Systematic Board understanding of patient experience (see detailed finding at page 30) There is no systematic Board understanding of patient experiences and evidence of action being taken to respond to issues raised in them. 7. Staffing (see detailed finding at pages 23 and 37 to 38) A number of issues were noted by the panel with staffing levels and skill mix. 8. Implementation of NHSP (see detailed finding at page 37) Improved bed flows and management through: Review of systems to enable best use of beds at all times including ensuring staff have access to, and are making effective use of, patient flow IT systems. A move to seven day working, with senior doctors reviewing in-patients every day on all wards. Improved end of life care planning and application, discharge planning. To review use of the PARS team and ward rounds to provide assurances that the policies are being consistently applied. Better use of the discharge lounge To systematically review discharge planning at all stages of a patient’s journey to enable safe and effective discharge. Patient stories should be regularly heard by the Board with lessons learned from those discussed and any action required as a result agreed upon. Recommended action provided to enable the Trust to address the problem identified. The Board to receive a summary of the substance of complaints, trends and themes and debate the actions required to address these. Full staffing levels and staff mix reviews to be completed across nursing and medical staff. Staff review support. Relieving clinicians care time through initiatives. Support for implementation of appropriate initiatives. Action plan to address implementation issues to be presented. Recommended action provided to enable the Trust to address the problem identified. 44 Problem identified Recommended action for discussion Discussions with a number of staff identified a number of issues with the implementation of NHSP affecting the management of temporary staffing. Steering Group to continue to meet post-implementation to closely monitor and manage NHSP. Support required by the Trust 45 Appendices 46 Appendix I: SHMI and HSMR definitions HSMR definition What is the Hospital Standardised Mortality Ratio? The Hospital Standardised Mortality Ratio (HSMR) is an indicator of healthcare quality that measures whether the mortality rate at a hospital is higher or lower than you would expect. Like all statistical indicators, HSMR is not perfect. If a hospital has a high HSMR, it cannot be said for certain that this reflects failings in the care provided by the hospital. However, it can be a warning sign that things are going wrong. How does HSMR work? The HSMR is a ratio of the observed number of in-hospital deaths at the end of a continuous inpatient spell to the expected number of in-hospital deaths (multiplied by 100) for 56 specific groups (CCS groups); in a specified patient group. The expected deaths are calculated from logistic regression models taking into account and adjusting for a case-mix of: age band, sex, deprivation, interaction between age band and co-morbidities, month of admission, admission method, source of admission, the presence of palliative care, number of previous emergency admissions and financial year of discharge. How should HSMR be interpreted? Care is needed in interpreting these results. Although a score of 100 indicates that the observed number of deaths matched the expected number; in order to identify if variation from this is significant confidence intervals are calculated. A Poisson distribution model is used to calculate 95% and 99.9% confidence intervals and only when these have been crossed is performance classed as higher or lower than expected. SHMI definition What is the Summary Hospital-level Mortality Indicator? The Summary level Hospital Mortality Indicator (SHMI) is a high level hospital mortality indicator that is published by the Department of Health on a quarterly basis. The SHMI follows a similar principle to the general standardised mortality ratio; a measure based upon a nationally expected value. SHMI can be used as a potential smoke alarm for potential deviations away from regular practice. How does SHMI work? 1) Deaths up to 30 days post acute trust discharge are considered in the mortality indicator, utilising ONS data. 2) The SHMI is the ratio of the Observed number of deaths in a Trust vs. Expected number of deaths over a period of time. 47 3) The Indicator will utilise 5 factors to adjust mortality rates by: a. The primary admitting diagnosis b. The type of admission c. A calculation of co-morbid complexity (Charlson Index of co-morbidities) d. Age e. Sex. 4) All inpatient mortalities that occur within a Hospital are considered in the indicator. How should SHMI be interpreted? Due to the complexities of hospital care and the high variation in the statistical models all deviations from the expected are highlighted using a Random Effects funnel plot. Some key differences between SHMI and HSMR Indicator Are all hospital deaths included? When a patient dies how many times is this counted? HSMR No, around 80% of in hospital deaths are included, which varies significantly dependent upon the services provided by each hospital. If a patient is transferred between hospitals within 2 days the death is counted multiple times. Does the use of the palliative care code reduce the relative impact of a death on the indicator? Does the indicator consider where deaths occur? Yes Is this applied to all health care providers? Yes Only considers in-hospital deaths SHMI Yes all deaths are included. 1 death is counted once, and if the patient is transferred the death is attached to the last acute/secondary care provider. No Considers in-hospital deaths but also those up to 30 days post discharge anywhere too. No, does not apply to specialist hospitals 48 Appendix II: Panel composition Panel role Name Panel Chair David Levy Lay representative (Patient/public representative) Fiona Loud Lay representative (Patient/public representative) Asa’ah Nkohkwo Lay representative (Patient/public representative) Jenny Robinson Junior Doctor Lola Loewenthal Doctor Gillian Derrick Doctor Jane McCue Student Nurse Board Level Nurse Senior Nurse CQC representative Elizabeth McKerrow Fay Baillie Clare Beattie Margaret McGlynn Senior Trust Manager Rebecca Brown Senior Regional Support Graeme Jones Senior Regional Support Finola Muir 49 Appendix III: Interviews held Interviewee Date held Claire Panniker, Chief Executive 7 May Celia Skinner, Medical Director, and Diane Sarker, Director of Nursing 7 May Celia Skinner and Diane Sarker, joint chairs of Quality and Patient Safety Committee 7 May David Hulbert (Non Executive Director), Chair of Clinical Quality Board 7 May Diane Sarkar, Director of Nursing 8 May Andy Ray, Acting Director of Finance, and Adam Sewell-Jones, previous Director of Finance 8 May Hannah Coffey, Chief Operating Officer 8 May Nigel Taylor, Director of Personnel & Organisational Development 8 May Michael Catling, General Manager, Medicine 8 May Dr Tayyab Haider, Divisional Clinical Director for Medicine, Stuart Harris, Divisional Clinical Director for CTC, and Celia Skinner, Medical Director 8 May Liz Seale, Associate Director of Clinical Governance & Risk (Head of Quality) 8 May Julie Hickman, Deputy Director of Nursing (Safeguarding lead) 8 May 50 Appendix IV: Observations undertaken Observation area Date of observation Care of the elderly wards 7 May Accident and emergency (A&E) 7 May Paediatrics ward 7 May William Harvey ward 7 May Acute Medical Unit (AMU) 7 May Cedar ward 8 May Maternity 8 May Cardiothoracic Centre (CTC) 8 May Elizabeth Fry ward, Renal 8 May Orsett ward, palliative care 8 May Katherine Monk ward, endocrine and general medicine 8 May PALS 8 May Discharge lounge 8 May Florence Nightingale, respiratory 8 May Operations room 8 May Lionel Cosins ward, care of the elderly 8 May Pasteur ward 8 May Orsett Hospital 8 May Further observations were undertaken as part of the unannounced site visit, see Appendix VII. 51 Appendix V: Focus groups held Focus group invitees Focus group attendees Date held Doctors 12 registered attendees; attendees included consultants, clinical leads, a CSU lead and radiologist. 7 May Patients and public 15 registered attendees; attendees included patients, relatives of patients, visitors and ex-patients. 7 May All staff 18 registered attendees; attendees were primarily nurses and health care assistants; also staff from radiology, health and safety, administration and a porter. 7 May Governors 8 registered attendees; attendees included staff and public governors. 8 May Junior doctors 11 registered attendees; attendees included junior doctors from acute medicine, surgery, orthopaedics, renal, and CTC; attendees included FY1, FY2, CT1, CT2, CT3 and SPRs. 8 May Trainee nurses 14 registered attendees; all attendees were student nurses. 8 May Nurses 12 registered attendees; attendees included sisters, lead nurses and HCAs. 8 May 52 Appendix VI: Information available to the RRR panel Quality Strategy Quality Strategy Overview Patient Safety Steering Group and combined TOR v4 June 2012 BAF 2012/13 updated 16.04.2013 Revised significant risk report April 2013 Corporate Clinical Audit report and Plan for April 2013 QPSC Clinical Audit and Effectiveness Q4 2012-13 Acute Medicine Clinical Audit and Effectiveness Q4 2012-13 Critical Care Clinical Audit and Effectiveness Q4 2012-13 Cardiology Clinical Audit and Effectiveness Q4 2012-13 CTC Surgery & Anesthetics Clinical Audit and Effectiveness Q4 2012-13 DMOP & Stroke Clinical Audit and Effectiveness Q4 2012-13 General Medicine Clinical Audit and Effectiveness Q4 2012-13 General Surgery & Urology Clinical Audit and Effectiveness Q4 2012-13 Head & Neck Clinical Audit and Effectiveness Q4 2012-13 Imaging Clinical Audit and Effectiveness Q4 2012-13 Obs & Gynae Clinical Audit and Effectiveness Q4 2012-13 Paediatrics Clinical Audit and Effectiveness Q4 2012-13 Pathology Clinical Audit and Effectiveness Q4 2012-13 Pharmacy Clinical Audit and Effectiveness Q4 2012-13 Specialist Medicine Clinical Audit and Effectiveness Q4 2012-13 T&O Clinical Audit and Effectiveness Q4 2012-13 Therapies 2012/13 CIPs CIP process document (Quality Impact Document) March 2012 2013/14 CIPs GGI Basildon RapidReviewReport 290113 GGI BTUH Gov Review Maturity Matrix Jan2013 Final Executive Team CVs (collated from applications) Operational Management Structure Committee Structure August 2012 (in process of being updated for 2013-2014) ToR - Audit and Risk Committee ToR Quality and Patient Safety Committee ToR Finance Committee ToR Investment Committee ToR Health and Safety Committee Trust committee Structure 2013 including reporting 53 committees Public BoD 27.02.2013 Private BoD 25.02.2013 Public BoD 27.03.2013 QPSC 11.03.2013 QPSC 08.04.2013 Quality Contract Meeting Minutes 7.03.2013 (DRAFT - for approval at the April meeting) Quality Contract Meeting action log 7.03.2013 Quality Contract Meeting Minutes 11.02.2013 Quality Contract Meeting action log 11.02.2013 Quality Contract Meeting Minutes 03.01.2013 Quality Contract Meeting action log 03.01.2013 Risk Steering Group minutes 14.03.2013 Risk Steering Group minutes 13.02.2013 Health and Safety Committee minutes March 2013 Health and Safety Committee minutes Feb 2013 HMRG - 18.03.2013 HMRG - 08.04.2013 HMRG ToR v3 July 2012 Performance Report for BoD 2012/13 Performance Report appendix Annual Plan 2012-13 with guidance removed DRAFT Annual Plan 2013 - 2014 (Draft annual plan to be submitted to Board of Directors 24.04.2013) Mortality Alert AMI March 2011 AMI Medical Directors report July 11 CQC AMI mortality Report – update AMI - Mr Chris Sherlaw letter May 2012 AMI - Mr Chris Sherlaw letter August 2011 AMI - Mr Chris Sherlaw letter September 2011 AMI - Mr Chris Sherlaw letter October 2011 AMI outlier closure Email re outlier - 25.05.2012 Email re AMI - 31 May 2012 Email re mortality figures - 31.05.2013 Email re AMI and continued actions - 14.01.2013 Closure letter AMI - 8.12.2013 20120503 BTUH alert letter for pneumonia Letter to Mr Chris Sherlaw - response to alert 01.06.2012 Pneumonia review Mortality - audit tool Paediatric Service Review BTUH CQC final report 180113 Pharmacy Basildon peer review final report 11.12.2012 GGI risk management system at BTUH FT 03012013 West Midlands SHA review in to mortality 09072012 (Stan Silverman) 54 Legionella Hydrop Review July 2012 IST cancer summary visit March 2012 IST pressure ulcer South Essex Review Letter CQC Jan 2013 NMC Review December 2012 IST Emergency Care Review November 2012 Report of PCT visit to BTUH on Wednesday 16th January 2013 PCT visit to Paediatric Unit 16.01.2013 PCT visit 8.01.2013 Radiology Review 19.03.2012 Infection control review (Steve Barratt) OHI results & OHI Board Report Elderly care strategy development - 11th April v4 Elderly Care Steering Group outline pack Elderly Care Strategy - Week 2 update Elderly Care Strategy - Week 3 update Elderly Care Strategy - Week 4 update Elderly Care Strategy - Week 5 update 130315 Elderly Care Strategy workstreams 130403 Elderly Care Strategy Progress Report 20130311 elderly care steering group charts 5 20130312 Elderly Care Strategy data summery V4 Complex discharge pathway (MDT assessment) Draft SLA pharmacy 040412 Social Care Timelines in regards to the community care act 2003 NMC Strategy Risk Strategy Quality Account (2011/12) Generic CQC Action Plan Feb 2013 CQC action plan - outcome 4 & 8 March 2013 Real-time feedback Quality and Patient Safety Committee agenda Monthly Serious Incidents report Analysis of mortality by day of the week Cardiac arrest national data Parent survey – Acute Children’s Services A&E Patient feedback survey WHO (World Health Organisation) Checklist Tissue Viability Referral Form Adult in-patient risk and assessment documentation CIP (Cost Improvement Schemes) listing, detailed summary and key instructions for reporting CLIP (Complaints, Litigation, Incidents and PALS) report HSMR colorectal data Complaints policy Patient experience and engagement strategy 55 Increased nursing supervision trigger Letters of responses complaints from patients and Community Acquired Pneumonia Care Bundle Leaflet provided by hospital summarising complaints / compliments policy Hospital newsletter CPR booklet Medical on call rota CQC/OFSTED Action Plan Safeguarding policies (adults and children) Operational Policy for the Surgical Referrals Unit 56 Appendix VII: Unannounced site visit Agenda item Panel pre-meet Entry into Basildon Hospital and announced arrival to site manager Observations undertaken of the following: Accident and emergency Paediatric accident and emergency Katherine Monk ward Kingswood ward Elsdon ward Surgical Referral Unit Doctors on call - surgical and general medical teams. Meeting held with site manager to understand current staffing and patient levels Panel left Trust and announced exit 57