Health Skills I Unit 102 Vital Signs
advertisement

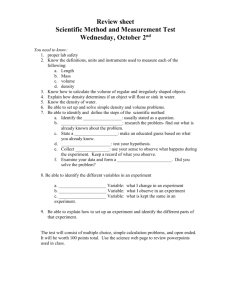
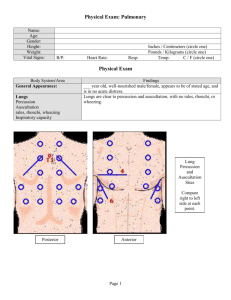
Health Skills I Unit 102 Vital Signs Objectives • Identify observational techniques for determining the health status of a patient. Unit 102.1 Observational Techniques • Observation of Patient – observe physical signs and alertness – listen to patient and ask questions Objective Data • can be observed or tested by healthcare provider • overt, not concealed • Examples: – observe that a patient refused to eat – measure an increased temperature – observe drainage from a wound – skin is warm to the touch – vomited 300 cc Subjective Data • information perceived only by the affected person • Examples: – feels nervous – pain in the abdomen – nauseated – feels chilled Senses to Collect Data • Look – observe visible signs that indicate a problem • Listen – patient’s complaints, description of the problem in their words • Feel – degree’s in body temperature, pulse quality • Smell – unusual odors Collecting Data Inspection • visual examination – signs of movement and posture – skin color signs of distress – ability to maintain health practices (hygiene, dress) – gait Collecting Data Auscultation • listening with use of a stethoscope – – – – – blood pressure heart sounds and/or rate lung sounds bowel sounds detecting bruits Collecting Data Palpation • examination of body parts through feeling with fingertips and hands to – assess skin temperature – determine pulse rate, quality,rhythm, absence or presence – lumps/masses – abdominal tenderness/distention Collecting Data Percussion • tapping body parts with your fingers and listening to sounds produced to – detect presence of air – evaluate amount of fluid in a body cavity – determine size, borders and consistency of body organs or masses Purpose of Systematic Physical Assessment • to determine physical and emotional changes through step by step observation • NOTE: – apparent state of health, does patient seem acutely ill? Signs of Distress • • • • • • • NOTE: dyspnea (difficulty breathing) vomiting pallor pain crying evidence of nervousness Skin Color • NOTE: – pink • indicates adequate oxygen levels – pallor (pale) • major organs being challenged with fluid or blood loss, peripheral blood is being shunted to the core of the body to self protect them – ashen (gray) • body systems begin to suffer due to decreasing oxygen level in blood Skin Color • NOTE: – cyanotic (blue) • indicates that body systems are in critical state due to an excessive amount of blood not carrying oxygen – flushed (pink/red) • harmful levels of carbon monoxide or increased carbon dioxide levels are present • Ketoacidosis (high blood glucose levels) will cause flushing, as will hypertension (high blood pressure) Stature & Build • NOTE: – large/small body frame – obesity – congenital anomalies (changes from normal at birth) Posture, Motor Activity and Gait • NOTE: – deformities – spine curvature – gait • shuffling • stable Dress, Grooming and Hygiene • NOTE: – if appropriate – clean – neat Odors Body and Breath • NOTE: – breath for acetone odor (may be diabetic) – alcohol odor (may be cause of problem) – urine odor (incontinence) – poor hygiene (emotional disturbances or social issues) Relationships, Manner and Mood • NOTE are they: – – – – – – pleasant smiling making eye contact initiating conversation crying appropriate conversation – following directions – – – – – depressed anxious agitated elated flat Speech • NOTE: – clarity – slurring State of Awareness and Consciousness • NOTE, are they: – alert – oriented to: • person • place • time and significant others – drowsy – is response time appropriate Support or Monitoring Devices • NOTE, does the patient use a: – walker – wheelchair – prosthesis – hearing aid – glasses – dentures – are these supports and devices working properly and is the patient knowledgeable in using them? Facial Expressions • NOTE: – tension – grimacing – affect • happy • sad • flat Reporting Observed Data – reporting should be done promptly, accurately, and objectively – identify need for emergency care – may play role in treatment plan by others – may indicate a need for medication changes – to know if patient is improving or not – documentation important for 3rd party payment (Insurance) Knowledge Assessment • Compare and contrast objective and subjective data and give examples of each. • Define and give examples of when inspection, auscultation, palpitation, and percussion are used. • Describe items of a physical assessment. (Example skin color, stature and build)