Protections of Human Subjects in Research: Interface with medical/clinical services

Protections of Human Subjects medical/clinical services
Deepak Kumar, PT, MPT, OCS
Issues
• In BIOMS there are many different recruitment procedures
▫ Recruiting from community
Advertisements
Word of mouth
▫ p
(MD, PT, Hospital)
One contact (eg. surgeon, PT)
10/6/2009
1
Regulations to Consider
• The Common Rule
▫ Protection of Human subjects and Privacy
• Health Information Portability and
Accountability Act of 1996- (HIPAA)
▫ Health Information Privacy Rule
• Recruitment from clinics or medical practices
▫ Retrospective studies
▫ Prospective studies
10/6/2009
The Common Rule
2
“The Common Rule”
• Dept of Health and Human Services- Code of Federal
Regulations
• “Basic HHS Policy for Protection of Human Research
Subjects” (45 CFR 46 Part 102-106)
• Defines:
▫ What is considered “research”
▫ What are considered “Human Subjects”
▫ What is Private information
▫ What is an acceptable level of risk
• Sets guidelines that ensure that researchers comply with
The Belmont Report - Ethical Principles and Guidelines for the protection of human subjects of research http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.102
What is Research?
• Research means a systematic development, testing and evaluation, designed to develop or contribute to generalizable knowledge
10/6/2009
3
10/6/2009
What are Human
Subjects in research?
“Human subject means a living individual about whom an investigator (whether professional or student) conducting research obtains”:
▫ Data through intervention or interaction with the individual
“Intervention includes:
physical procedures by which data are gathered (e.g. strength test)
manipulations of the subject (eg. training)
Manipulation of the subject's environment (eg split belt treadmill training)
“Interaction” includes communication or interpersonal contact between investigator and subject.
▫ Identifiable private information http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.102
4
• Private information includes:
▫ behavior that occurs in a context in which an individual can reasonably expect that no observation or recording is taking place
Eg. Observations in a an educational setting
▫ which has been provided for specific purposes by an individual and which the individual can reasonably expect will not be made public
Eg. a medical record
▫ that can be identified as belonging to a particular individual or information that an investigator could use readily to determine the identity of the person.
Name, Address, Phone Number
Date of birth, diagnosis http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.102
The Common Rule
• Defines Level of Risk of the Research Procedures
• Relates to level of IRB review
• Mi i l Ri k
probability and magnitude of harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life or during the performance of routine physical or psychological examinations or tests.
10/6/2009
5
10/6/2009
Health Information Portability and Accountability Act (HIPAA)
HIPAA Privacy Rule
• The Office for Civil Rights enforces the HIPAA
Privacy Rule, which protects the privacy of individually identifiable health information under different circumstances, including research with human subjects.
▫ 45 CFR 164.501, 164.508,164.512(i)- Private Health
Information from any “HIPAA covered entity”
• Researchers may obtain, create, use, and/or disclose y ways:
▫ without individual authorization
under limited circumstances set forth in the Privacy Rule
▫ with individual authorization
6
• Regardless of need for authorization or not,
ALL Research
Protocols must be submitted to the IRB
•
The IRB determines if the authorization can be waived or not.
10/6/2009
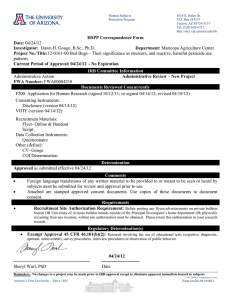
Use of PHI without authorization
• IRB will grant waiver of authorization if the research in whole or in part, satisfies the three criteria in the Rule;
1.
The use or disclosure of protected health information involves no more than a minimal risk to the privacy of individuals presence of the following elements: based on at least the
an adequate plan to protect the identifiers ; an adequate plan to destroy the identifiers at the earliest opportunity , unless there is a health or research justification for retaining the identifiers or such retention is otherwise required by law; and
adequate written assurances that the protected health information will not be reused or disclosed to any other person or entity , except as required by law, for authorized oversight of the research project, or for other research for which the use or disclosure of protected health information would be permitted by this subpart;
2.
The research could not practicably be conducted without the waiver or alteration; and
3.
The research could not practicably be conducted without access to and use of the protected health information .
7
Use of PHI without authorization
• After an IRB has waived the need for authorization, the covered entity (eg. a medical practice) may use or disclose protected health information for research purposes provided it has obtained documentation of all of the following:
An IRB is identified and the date on which the waiver of authorization was approved;
A statement that the IRB has determined that the waiver of authorization, in whole or in part, satisfies the three criteria in the
Rule;
A brief description of the protected health information for which y y
Privacy Board;
A statement that the alteration or waiver of authorization has been reviewed and approved under either normal or expedited review procedures; and
The signature of the chair or other member, as designated by the chair, of the IRB or the Privacy Board, as applicable.
Use of PHI without authorization
▫ Retrospective Study eg: records search
▫ Preparatory to research- eg: feasibility study
▫ Research on decedents
▫ Limited data sets with a data use agreement
De-identified
Signed agreement
10/6/2009
8
Use of PHI with authorization
▫ Eg: clinical trials, records research
▫ Authorization may be valid indefinitely
* UD IRB does not encourage open-ended authorizations. You should specify exactly what private health information is will be used rather than asking to use the whole medical record
* Researcher responsible for confidentiality under HIPAA
10/6/2009
Institutional Review Boards (IRB)
Review Process
9
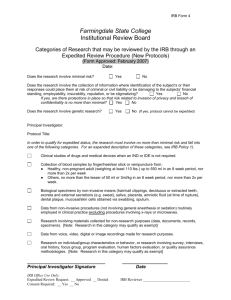
Institutional Review Board
Types of IRB Review
• Exempt from review
• Expedited review
• Full-board review http://www.udel.edu/research/preparing/protocolreview.html
IRB Review - Exemptions
• Determined ONLY by the Chair of the IRB or designee
• Granted under very limited circumstances
• All submissions done online on IRBnet
• Should Include the following:
▫ A completed protocol form
▫ The exemption you request with an explanation of h b li it li t th j t
▫ Your adviser's name, if you are a student
▫ Enclose the following with the letter:
A copy of all survey, test, interview questions, recruitment fliers or letters to be used in the project.
10/6/2009
10
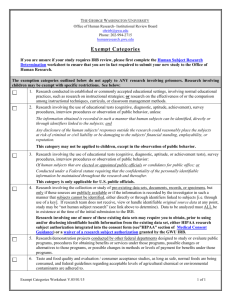
IRB Review - Exemptions
• 6 categories (from Title 45, Code of Federal Regulations, part
46.101(b), 6/18/91)
1 established or commonly accepted educational settings, involving normal educational practices
2.
use of educational tests (cognitive, diagnostic, aptitude, achievement), survey procedures, interview procedures, or observation of public behavior, unless:
subjects can be identified, directly or through identifiers risk of criminal or civil liability or be damaging to the subjects’ financial standing, employability, or reputation
3.
not exempt under category 2 subjects are elected or appointed public officials or candidates for public office
federal statute(s) require(s) without exception that the confidentiality of the personally identifiable information will be maintained throughout the research and thereafter
4.
collection or study of existing data, documents, records, pathological specimens, or diagnostic specimens, if these sources are publicly available or if the information is recorded by the investigator in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects.
10/6/2009
11
IRB Review - Exemptions
• IRB review of a research protocol is necessary when anyone involved in the research (even “key personnel”) has access to the patient identifiers
▫ Eg: therapists, physicians, teachers etc.
▫ If those individuals could link a subject number to a person’s identity then the IRB needs to formally review
10/6/2009
IRB Review- Expedited
• Certain minimal risk research qualifies
• Often amendments to full IRB approved protocols may also qualify
• 9 categories from the Common Rule (Refer to
UD webpage)
▫ Use of routine medical procedures like blood samples, venipuncture
▫ Non invasive collection of biological specimens like hair or nail clippings, saliva, plaque etc.
▫ Routine imaging procedure
▫ Medical records
▫ Behavioral studies http://www.udel.edu/research/preparing/protocolreview.html
12
IRB Review- Full Board
• more than minimal risk
• Investigator required to be present at the meeting
• review begins with a short (maximum of five minutes) summary of the research by the investigator, after which board members ask any questions they have
• h d meeting also.
l h
HSRB, his or her adviser must attend the
• submitted at least ten working days before an
HSRB meeting for review at that meeting
10/6/2009
13
Examples – Retrospective Study
• Use of PHI that has been collected in medical/clinical practices during normal patient care
• Eg. Study the relationship between BMI and radiographic severity of knee OA using data from Christiana Care
▫ d h h b d h l d :
A completed protocol form
Request that the review be exempted and an IRB waiver of consent
Plus why you believe an exempted review is warranted
Your adviser's name, if you are a student
Enclose the following with the letter:
The PHI you intend to use, from whom, etc.
▫ If IRB approves the request:
Representative from the medical/clinical practice can provide a “limited use data-set”
Data set should to be de-identified – can’t include:
Name, Date of birth (age at time of data collection is ok), HIPAA numbers, Address, phone numbers etc.
▫ Exemption from review will NOT be approved if you need information such as patient contact information is needed (eg. if you wanted to know the incidence of
OA in a particular area for which you will need the address of the subjects …)
▫ Instead, an Expedited review will be needed
Examples: Prospective Studies
• You want to study a cardiac rehabilitation interventions and you want to recruit patients who had been admitted to Christiana Care Health Systems
(CCHS) with MI
▫ R i IRB R i (F ll B d E dit d)
Protocol will include information on how subjects will be recruited
Ads, flyers etc. need approval too
• If IRB approves the research protocol:
▫ For patients being admitted after approval, the practitioner (or their representative) tells the patient (in person) about the study and gets the
Now patient name and contact info can be sent to the researchers
▫ For patients who had been admitted in the past,
Letter to be sent to potential subjects by the practitioner or a representative
Those who reply can be contacted by researchers
▫ Need to sign written consent specific for the study before enrolment
10/6/2009
14
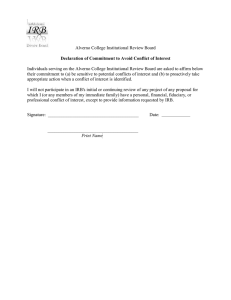
Special Circumstances
• Outside practitioner as co-investigator
▫ Depends on funding agency
▫ Not exempt – needs either expedited or full board review
• Permanent relationship with a medical practice
(eg: if you will be working closely in the future with the Dept. of
Nutrition at Jefferson Hospital for various projects)
▫ Request for authorization from every patient
▫ For any future study
▫ Will include consent to be contacted and consent for data to be used
▫ Need IRB approval
10/6/2009
• Elizabeth Peloso, Director of
Compliance, Research Office
• Dr. Katherine Rudolph,
Associate Professor, Dept. of PT
• Dr. Tara Jo Manal, Director of
Clinical Services, Dept. of PT
15