Speaker: Megan Wenner Dissertation Defense Date: Wed Jan 7th
advertisement
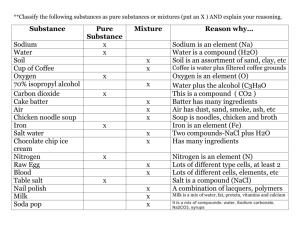
Speaker: Megan Wenner Dissertation Defense Date: Wed Jan 7th Time: 2:00 pm Place: Townsend 132. Title: The Role of COX-2 Inhibition in Salt Sensitivity of Blood Pressure. Committee:Dr. William Farquhar (Chair), Dr. David Edwards, Dr. William Rose, Dr. Darcy Reisman, Dr. Michael Stillabower, and Dr. Timothy Gardner. Abstract:Salt-sensitivity can occur in both normotensive and hypertensive individuals, and may be clinically relevant in determining future cardiovascular events. The literature suggests nonselective cyclooxygenase inhibitors may be associated with sodium and water retention along with an increase in blood pressure; thus the effects of non-selective cyclooxygenase inhibitors on blood pressure and renal sodium handling have been well established. However, data regarding the blood pressure response during selective cyclooxygenase-2 (COX-2) inhibition are conflicting. Recent data in experimental animals suggests that COX-2 inhibition causes salt sensitivity of blood pressure, yet data are lacking in humans. Therefore, the purpose of this study was to determine if COX-2 inhibition increases salt sensitivity of blood pressure in humans. We hypothesized that increases in blood pressure would be greater during selective COX-2 inhibition compared to placebo after dietary sodium manipulation, indicating a link between COX-2 inhibition and salt sensitivity. A secondary aim of this study was to determine the renal and vascular effects of COX-2 inhibition under well-controlled dietary sodium intake. We hypothesized that COX-2 inhibition would decrease sodium excretion during salt loading conditions. Twelve human subjects completed two separate 17-day dietary trials (once under placebo conditions, once under celecoxib conditions; 100mg twice per day). The 17-day dietary trial consisted of 3-days of a normal salt diet, one week of a high salt diet and one week of a low salt diet. Data were collected on the last day of each sodium condition. By design, sodium intake was greater on the high salt diet compared to the low salt diet (HS: 7987 ± 12 mg, LS: 480 ± 12 mg; p < 0.001). Urinary sodium excretion (24-hour) was greater on the high salt diet (p < 0.001) with no differences between placebo and celecoxib (p=0.26). There were no differences in 24-hour mean arterial pressure (MAP) between salt (p=0.89) or drug (p=0.85) conditions. The change in MAP from low to high sodium conditions was used to assess salt sensitivity of blood pressure. The change in MAP was not different during placebo (0.25 ±1.4 mmHg) compared to celecoxib (-0.58 ± 0.4 mmHg). Therefore, there were no differences in salt sensitivity between celecoxib and placebo (p=0.3). Urine flow rate and free water clearance were not different between celecoxib and placebo (p>0.5 for both). Several indices of vascular stiffness were not different between placebo and celecoxib (augmentation index p=0.35; pulse wave velocity p=0.49; flow mediated dilation p=0.82; total peripheral resistance p=0.41), nor was there a main effect of salt (augmentation index p=0.23; pulse wave velocity p=0.22; flow mediated dilation p=0.49; total peripheral resistance p=0.86). In conclusion, celecoxib did not induce salt sensitivity of blood pressure in this group of healthy subjects. There was no effect of celecoxib on renal or vascular function. Additional studies are needed to determine if chronic use of COX-2 inhibitors (ie, more than 17 days, or at higher doses) contribute to salt sensitivity, and whether these findings translate to hypertensives.