The American Journal of Sports Medicine
advertisement
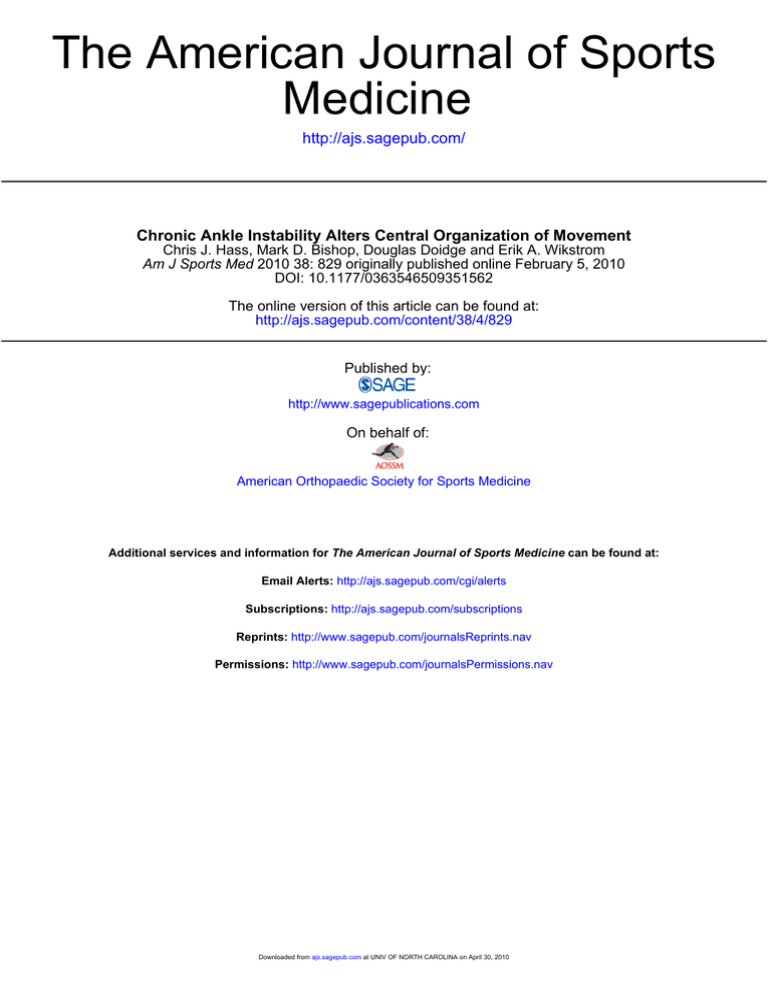
The American Journal of Sports Medicine http://ajs.sagepub.com/ Chronic Ankle Instability Alters Central Organization of Movement Chris J. Hass, Mark D. Bishop, Douglas Doidge and Erik A. Wikstrom Am J Sports Med 2010 38: 829 originally published online February 5, 2010 DOI: 10.1177/0363546509351562 The online version of this article can be found at: http://ajs.sagepub.com/content/38/4/829 Published by: http://www.sagepublications.com On behalf of: American Orthopaedic Society for Sports Medicine Additional services and information for The American Journal of Sports Medicine can be found at: Email Alerts: http://ajs.sagepub.com/cgi/alerts Subscriptions: http://ajs.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav Downloaded from ajs.sagepub.com at UNIV OF NORTH CAROLINA on April 30, 2010 Chronic Ankle Instability Alters Central Organization of Movement Chris J. Hass,* PhD, Mark D. Bishop,y PhD, PT, Douglas Doidge,* and Erik A. Wikstrom,z§ PhD, ATC From the *Center for Exercise Science, Department of Applied Physiology and Kinesiology, University of Florida, Gainesville, Florida, yDepartment of Physical Therapy, University of Florida, Gainesville, Florida, and the §Biodynamics Research Laboratory, Department of Kinesiology, and Center for Biomedical Engineering Systems, University of North Carolina at Charlotte, Charlotte, North Carolina Background: Chronic ankle instability alters spinal level sensorimotor function and is hypothesized to alter supraspinal motor control mechanisms. Gait initiation is a functional task modulated by supraspinal pathways, but the effect of chronic ankle instability, a peripheral musculoskeletal impairment, on gait initiation and thus supraspinal motor control mechanisms remains unknown. Purpose: This study was conducted to determine if supraspinal aspects of motor control are altered in subjects with chronic ankle instability. Study Design: Controlled laboratory study. Methods: Subjects with chronic ankle instability (5 males, 15 females; age, 20.5 6 1.0 years; height, 169.8 6 9.8 cm; weight, 74.2 6 20.2 kg) and uninjured controls (4 males, 16 females; age, 20.85 6 1.6 years; height, 164.3 6 7.9 cm; weight, 64.2 6 10.62 kg) completed 5 gait initiation trials for each leg at a self-selected pace. The resulting trajectory of the center of pressure trace was investigated and peak center of pressure excursions in the anteroposterior and mediolateral directions, peak resultant center of pressure excursions, and average direction-specific velocities were calculated. Results: Significant group 3 limb interactions were noted during the first (resultant center of pressure displacement [F1,37 5 4.60, P 5 .04]) and second (mediolateral center of pressure displacement [F1,37 5 3.82, P 5 .05]) period of gait initiation. Center of pressure displacement was reduced (impaired) in the involved limb of the chronic ankle instability group (resultant, 0.29 6 0.02; mediolateral, 0.72 6 0.02) relative to the uninvolved limb of the chronic ankle instability group (resultant, 0.32 6 0.02; mediolateral, 0.76 6 0.02) and both limbs of the control group (resultant, 0.32 6 0.02; mediolateral, 0.74 6 0.02) when the involved limb of the chronic ankle instability group served as the initial stance limb. Conclusion: These interactions suggest that supraspinal motor control mechanisms are altered in subjects with chronic ankle instability to place a greater emphasis on reducing the postural demands on the involved limb. Clinical Relevance: These changes suggest that supraspinal adaptations to motor control may be an important contributor to the underlying neurophysiologic mechanism of chronic ankle instability. The presence of supraspinal adaptations in subjects with chronic ankle instability also indicates that health care providers and rehabilitation specialists treat chronic ankle instability as a global/central and not just a local/peripheral injury. Keywords: dynamic postural control; center of pressure; supraspinal motor control; lateral ankle sprains Lateral ankle sprains, resulting from a combination of sudden inversion and plantar flexion of the foot/ankle complex, are the most common injury suffered by both high school and collegiate athletes.6,18 These injuries most commonly exceed the maximum load to failure of the anterior talofibular and calcaneofibular ligaments5 and are often believed to have no lasting consequences. However, the sequela of a lateral ankle sprain, commonly referred to as chronic ankle instability (CAI), which includes residual symptoms,1 recurrent injury,36 and decreased physical activity,32 have been reported for months and years after the initial trauma. Impairments in feedback sensorimotor function (ie, proprioception) have long been thought to be a consequence z Address correspondence to Erik A. Wikstrom, PhD, ATC, Department of Kinesiology, University of North Carolina at Charlotte, 9201 University City Blvd, Charlotte, NC 28223 (e-mail: ewikstrom@uncc.edu). One or more authors has declared a potential conflict of interest: This study was funded in part by the Southeastern Athletic Trainers’ Association. The American Journal of Sports Medicine, Vol. 38, No. 4 DOI: 10.1177/0363546509351562 Ó 2010 The Author(s) 829 Downloaded from ajs.sagepub.com at UNIV OF NORTH CAROLINA on April 30, 2010 830 Hass et al The American Journal of Sports Medicine of an initial lateral ankle sprain and a mechanism of CAI.7,8 However, there is little empirical evidence to support this theory. Recent research has indicated that central changes in sensorimotor function are present in subjects with CAI, most notably alterations in gait3,27,29 and altered alpha motoneuron pool excitability,28 which suggests that spinal-level motor control mechanisms have changed. Furthermore, because in vivo measures of sensorimotor function require conscious perception of peripheral joint and muscle information, it has been hypothesized that supraspinal aspects of motor control are also altered.15 Gait initiation (GI) requires effective balance control as one transitions from quiet stance to continuous gait.12-14 Specifically, anticipatory postural adjustments, via a series of muscle contractions prior to initiation of the locomotor pattern (preparatory phase), move the net center of pressure (COP) backward and toward the initial swing limb to move the body’s center of mass forward over the stance limb.21 Execution of the first step (stepping phase) begins when the body’s center of mass has been transferred to the stance limb.19 Most importantly, GI is proposed to be modulated via supraspinal pathways because secondary motor areas control the preparatory phase of GI, while the primary motor cortex controls the stepping phase.21 Previous research has demonstrated inefficient anticipatory postural adjustments as evidenced by decreased velocity and magnitude of COP displacement during GI in patients with impairment of the central nervous system.12-14 Indeed, these GI deficits may be caused by compromised motor programming in the premotor and secondary motor areas of the cortex.24 In contrast, little is known about the effect of peripheral musculoskeletal impairments of the nervous system. Therefore, the purpose of this investigation was to determine if supraspinal aspects of motor control are altered in subjects with CAI. Specifically we used a GI task to test the hypothesis that CAI causes alterations in the organization of movement (ie, alters supraspinal motor control mechanisms). METHODS Experimental Design and Participants This single-session, mixed-model design was part of a larger project that investigated the influence of CAI on locomotion. Twenty participants with CAI (5 males, 15 females; age, 20.5 6 1.0 years; height, 169.8 6 9.8 cm; weight, 74.2 6 20.2 kg) and 20 uninjured controls (4 males, 16 females; age, 20.85 6 1.6 years; height, 164.3 6 7.9 cm; weight, 64.2 6 10.62 kg) volunteered in response to flyers posted on campus and/or classroom presentations made by the investigative team. Additionally, all participants read and signed the University Institutional Review Board–approved informed consent form before data collection. All participants were recreationally active, which was operationally defined as performing 3 aerobic exercise sessions per week for a total of 90 minutes. Those with CAI met specific criteria, including (1) a history of at least 1 unilateral lateral ankle sprain that required immobilization for at least 3 days (11.5 6 9.2 days); (2) at least 1 episode of giving way within the past year (8.5 6 6.7 episodes); (3) at least 1 recurrent ankle sprain between 3 and 6 months before study participation (2.9 6 1.8 recurrent sprains); (4) report of pain, instability, and/or weakness in the involved ankle; (5) attribution of these signs to the initial ankle injury; (6) failure to resume all preinjury level of activities; (7) no previous ankle fractures; (8) no previous head and acute lower extremity injury within the past 3 months; and (9) no formal rehabilitation of the involved ankle. These requirements have been used previously as inclusion criteria for individuals with CAI.34,35 An episode of reinjury between 3 and 6 months before enrollment in this investigation was required to ensure that subjects still had physical manifestations of CAI but that acute symptoms were resolved. Uninjured controls were excluded if they were not free from acute lower extremity or head injuries for the previous 3 months or if they suffered from any equilibrium disorders or chronic lower extremity disorders. Protocol Testing was completed in the Applied Neuromechanics Laboratory at the University of Florida. Before data collection, demographic and anthropometric measurements were taken and participants were tested barefoot in form-fitting clothing. All trials of GI were performed along a 12-m walkway surrounded by an 8-camera optical motion capture system (Vicon Peak, Lake Forest, California). Ground-reaction forces were collected at 1200 Hz using 2 force platforms (Bertec Corporation, Columbus, Ohio) mounted flush with the surrounding floor. Once orientated, participants were instructed on and familiarized with the GI protocol and allowed to practice. Participants began each trial by standing quietly with a foot on each of the 2 adjacent force platforms in a relaxed position. Stance width was self-selected for each trial and was not constrained in any way. In response to an auditory cue, participants began walking and continued along the length of the walkway. The auditory cue triggered an electronic event marker that identified the beginning of the trial. For each participant, 10 trials (5 for the involved limb and 5 for the uninvolved limb) performed at a selfselected pace were collected. For this investigation, the dominant limb of uninjured controls, defined as the limb the individual would use to kick a ball, served as their involved limb while the nondominant limb of uninjured controls served as their uninvolved limb for statistical analyses. Data Reduction The COP trace was divided into 3 periods by identifying 2 landmark events as previously reported.12-14 Briefly, the first section (S1) begins with the auditory cue and ends with the COP located in its most posterior and lateral position toward the initial stepping foot (landmark 1). This posterolateral shift requires bilateral soleus inhibition, followed closely by bilateral tibialis anterior activation.2 The second section (S2) represents the movement of the COP Downloaded from ajs.sagepub.com at UNIV OF NORTH CAROLINA on April 30, 2010 Vol. 38, No. 4, 2010 Chronic Ankle Instability 831 TABLE 1 Normalized COP Excursions During the S1, S2, and S3 Phases of Gait Initiationa S1 ML AP Resultant S2 ML AP Resultant S3 MLd,e AP Resultant CAI Involved CAI Uninvolved Control Involvedb Control Uninvolvedb 0.20 6 0.02 0.21 6 0.02 0.29 6 0.02c 0.22 6 0.01 0.22 6 0.02 0.32 6 0.02 0.22 6 0.02 0.23 6 0.02 0.33 6 0.02 0.21 6 0.01 0.21 6 0.02 0.31 6 0.02 0.72 6 0.02c 0.07 6 0.01 0.73 6 0.02 0.76 6 0.02 0.04 6 0.01 0.75 6 0.02 0.75 6 0.02 0.05 6 0.01 0.76 6 0.02 0.73 6 0.02 0.06 6 0.01 0.73 6 0.02 0.13 6 0.03 0.96 6 0.06 0.97 6 0.06 0.11 6 0.02 0.99 6 0.07 1.00 6 0.07 0.12 6 0.03 0.97 6 0.06 1.01 6 0.06 0.12 6 0.02 1.06 6 0.07 1.08 6 0.07 a Data are reported as mean 6 standard deviation. COP, center of pressure; S1, S2, and S3 are the 3 sections/phases of the COP trace; ML, mediolateral; AP, anteroposterior. b For the control group, involved is the dominant lower extremity and uninvolved is the nondominant lower extremity. c Indicates a statistical difference (P \ .05) from the CAI uninvolved limb and both the involved and uninvolved limbs of the uninjured controls. d Indicates that the CAI was significantly larger than the control group (P \ .05). e Indicates that the involved limb was significantly larger than the uninvolved limb (P \ .05). toward the initial stance foot and ends at landmark 2, which is the position under the initial stance foot on which the COP begins to move forward. The abductors and adductors of the hip contribute to this movement.20 The third section (S3) extends from landmark 2 until toe-off of the initial stance foot as the COP translates forward. During S3, the stance limb gluteus medius maintains control of the center of mass in the frontal plane while the ipsilateral tibialis anterior and soleus activate to pull the center of mass forward while also controlling forward motion, respectively.2,23 During each of these 3 sections, the following outcome measures were calculated: (1) peak COP excursions in the anteroposterior and mediolateral directions, (2) peak resultant COP excursions, and (3) average anteroposterior and mediolateral velocities.12,14 Because stance width was not constrained, a statistical trend (t385 –1.92, P 5 .06) was noted between groups (control, 17.0 6 3.97 cm; CAI, 19.7 6 5.18cm). Therefore, the decision was made to normalize the COP excursions and average velocities to the self-selected stance width of the corresponding trial for each participant. The normalized averages were then used for further analysis. Statistical Analysis Several preliminary analyses were conducted to ensure appropriate analysis of the dependent variables. Group demographics were compared with independent-sample t tests and no significant differences were noted between participants with CAI and uninjured controls with regard to their age, height, or weight. Additionally, weight distribution during quiet stance and over-ground gait velocity was compared between groups using an independentsample t test to ensure that the groups had comparable standing and temporal-spatial gait characteristics. Over-ground gait velocity did not differ [t38 5 –0.52, P 5 .60] between the control (1.22 6 0.09 m/s) and CAI (1.24 6 0.12 m/s) groups. Similarly, the distribution of weight under both limbs was statistically similar for both groups (control [involved, 320 6 62 N; uninvolved, 322 6 58 N) and CAI [involved, 365 6 86 N; uninvolved, 374 6 79 N]), regardless of whether the injured limb was to be the stance or swing limb. This finding indicates that between-group and between-limb differences observed in COP displacements during GI are not attributed to differences in a priori weight distributions. Separate 2 3 2 (group 3 limb) analyses of variances were used to test for overall group differences during each period of the COP trace during GI. A traditional level of significance (a 5 .05) was used on all statistical tests and Bonferonni post hoc analyses were performed when necessary. RESULTS A significant group 3 limb interaction (F1,37 5 4.60, P 5 .04] was noted for the resultant displacement of the COP trace during the S1 phase of GI (Table 1). This interaction was strongly influenced by the mediolateral component of the shift (F1,37 5 3.23, P 5 .08). Post hoc analysis indicated that in participants with CAI, the resultant posterolateral shift was decreased when the involved limb served as the initial stance limb, suggesting impaired motor performance. During the S2 period of GI (Table 1), a significant group 3 limb interaction (F1,37 5 3.82, P 5 .05) was also observed in the mediolateral component of the COP displacement shift. Similarly, post hoc testing indicated that when the involved limb of participants with CAI served as the initial stance limb, the mediolateral COP displacement was reduced, suggesting a more constrained Downloaded from ajs.sagepub.com at UNIV OF NORTH CAROLINA on April 30, 2010 Hass et al The American Journal of Sports Medicine sensorimotor system. During the final phase of gait initiation (S3), limb main effects revealed that mediolateral displacement (F1,37 5 4.47, P 5 .04) and mediolateral COP velocity (F1,37 5 4.80, P 5 .03) were greater on the involved limb (Table 1). Additionally, a group main effect was revealed for mediolateral displacement (F1,37 5 3.86, P 5 .05) and a statistical trend toward a group main effect was illustrated for the mediolateral COP velocity (F1,37 5 3.67, P 5 .06), both indicating that the healthy control group had greater mediolateral displacement during S3, suggesting a less constrained sensorimotor system or greater tolerance to mediolateral COP movement. AP Position 832 Uninjured Control CAI DISCUSSION ML Position Deficits in feedback sensorimotor function (ie, proprioception) have long been hypothesized as the causal mechanism of CAI,7,8 but this theory is largely unsupported. Recent research has identified altered spinal-level motor control mechanisms in persons with CAI.3,27-29,33 However, some aspects of supraspinal motor control have also been hypothesized to be altered in individuals with CAI because in vivo measures of sensorimotor function require conscious perception of joint and muscle information.15 The principal finding of the current investigation (ie, decreased normalized COP excursion magnitudes during the S1 and S2 phases of GI) clearly demonstrates that chronic peripheral joint injury, CAI, negatively alters supraspinal aspects of motor control. The initiation of gait is preceded by several anticipatory postural adjustments that shift the COP in a posterolateral direction (S1) to achieve 2 distinct goals: (1) the generation of forward momentum (posterior shift) and (2) the propulsion of the center of mass toward the initial stance limb (lateral shift).26 The magnitude of the S1 posterior shift naturally declines with age and disability,13,14,26 which is hypothesized to be caused by a deterioration of centrally mediated anticipatory postural adjustments such as the failure to inhibit the soleus muscles prior to the activation of the tibialis anterior muscles. This nonstereotypical pattern of muscle activation limits posterior COP excursions during S1 and subsequent forward momentum.26 Because older adults and patient populations are highly susceptible to falls, these individuals may purposefully limit the posterior COP excursion to minimize mechanical and postural challenges during GI and their risk of falls.10 However, falls do not appear to be a concern of individuals with CAI and it is highly unlikely that age-related declines in the effectiveness of the posterior-directed anticipatory postural adjustments were present in the current CAI study participants. For example, uninjured controls (3.7 cm) and CAI participants (3.8 cm) produced smaller but similar raw posterior COP excursions as those reported in the literature for young adults (4.7 cm).11 Despite the similar raw displacements, deviations from a ‘‘normal’’ COP trace similar to those seen in older adults and Parkinson disease patients were seen in subjects with CAI when the data were normalized to an individual’s stance width. Specifically, participants with CAI reduced the magnitude Figure 1. Representative normalized center of pressure (COP) trace for the uninjured control and chronic ankle instability (CAI) groups when the involved limb served as the initial stance limb. AP, anteroposterior; ML, mediolateral. of their normalized posterolateral COP excursion when their involved limb (ie, unstable ankle) served as the initial stance limb, which is suggestive of decreased postural control (Figure 1). Participants with CAI also reduced stance-side momentum when the involved limb (ie, unstable ankle) served as the initial stance limb, possibly to minimize postural demands while transitioning from double- to single-limb stance. Lateral COP displacement during S1 has significant effects on center of mass displacement, the preservation of lateral stability,37 and stance-side momentum (S2 mediolateral displacement). Both controls (3.7 cm) and CAI participants (3.8 cm) produced similar raw excursions to previously reported means for young adults (3.6 cm).11 Additionally, postural instability during static stance16,22 and when exposed to internal33 and external perturbations25 has been shown in individuals with CAI. Thus, it appears that the altered supraspinal motor control mechanisms used by individuals with CAI serve to (1) reduce anticipatory postural forces and (2) place a greater emphasis on reducing the postural demands on the involved limb. Previously, altered lower extremity muscle activation patterns have also been reported in individuals with CAI during gait,3,27 jump landings,4,9,29 and when transitioning from double- to single-limb stance,31 so it is possible that deviations from the stereotypical pattern of lower limb muscle activation also occurred during GI. However, this is speculative as muscle activity was not recorded in the current investigation. Regardless of the lower extremity muscle activation pattern, these data suggest that supraspinal aspects of motor control are susceptible to chronic peripheral joint injury, specifically CAI. Despite the apparent advantage the identified alterations in GI demonstrated by participants with CAI have for preserving lateral stability, these individuals were still experiencing recurrent episodes of giving way and recurrent injury, which are both important clinical symptoms Downloaded from ajs.sagepub.com at UNIV OF NORTH CAROLINA on April 30, 2010 Vol. 38, No. 4, 2010 Chronic Ankle Instability of CAI. Thus, the supraspinal alterations observed in the current investigation should be considered either maladaptive or ineffective changes to the organization of movement. We speculate that centrally mediated decreases in COP excursion during GI represents a more constrained sensorimotor system that will decrease the individual’s ability to cope with changing task demands,16,22,33 thus contributing to the major clinical symptoms of CAI (ie, episodes of giving way and recurrent injury). Currently, the long-term mechanical and neurologic consequences of a constrained sensorimotor system remain unknown, but recent evidence illustrates that CAI leads to diminished activity levels32 and is a leading cause of posttraumatic osteoarthritis in the ankle.17,30 While our results are important, this study was not without its limitations. We are inferring that alterations in the behavioral performance during GI are reflective of differences in supraspinal control. Future studies should evaluate lower extremity muscle activity and central mediated processes more directly (eg, transcranial magnetic stimulation studies or electroencephalography). For the current investigation, no level of self-reported ankle function was assessed and no validated questionnaire was used to categorize participants. Previously, our laboratory group correlated the current inclusionary criteria to validated instruments for a group of controls, ankle copers, and CAI patients, and noted significant negative correlations. Thus, we are confident that the current inclusionary criteria properly identify functionally impaired CAI individuals and also appropriately categorized CAI participants. Finally, the control group in the current investigation was about 10 kg lighter than those with CAI, but this difference was not statistically significant. Our primary outcome variables were peak excursion (cm) and average velocity (cm/s), which are not influenced by participant weight; thus, we are confident that the average weight of the groups did not affect our results. However, future investigations should consider matching CAI participants and controls by weight if they will be using variables such as peak forces that can be influenced by patient weight. CONCLUSION The results of the current investigation provide evidence that chronic peripheral joint injury, specifically CAI, negatively alters supraspinal aspects of motor control during an internally mediated postural destabilization (GI). The COP excursions during the preparatory phase of GI (S1 and S2), modulated by secondary motor areas,21 were reduced (impaired) in participants with CAI. Similarly, the stepping phase (S3) of GI, modulated by the primary motor cortex,21 was also reduced (limited) in CAI participants. These changes strongly suggest that centrally mediated changes to motor control may be an important contributor to the underlying neurophysiologic mechanism of CAI. Further, and more importantly, these data indicate the need for rehabilitation specialists to conduct global coordination/training programs for both the 833 involved and uninvolved limbs of patients with acute lateral ankle sprains and CAI to prevent motor control alterations and restore proper motor control following a peripheral joint injury. ACKNOWLEDGMENT This study was funded in part by the Southeastern Athletic Trainers’ Association. REFERENCES 1. Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. 2. Brunt D, Lafferty MJ, McKeon A, Goode B, Mulhausen C, Polk P. Invariant characteristics of gait initiation. Am J Phys Med Rehabil. 1991;70:206-212. 3. Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional ankle instability of the ankle joint. Am J Sports Med. 2006;34(12): 1070-1976. 4. Delahunt E, Monaghan K, Caulfield B. Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. J Orthop Res. 2006;24(10):1991-2000. 5. Fallat L, Grimm DJ, Saracco JA. Sprained ankle syndrome: prevalence and analysis of 639 acute injuries. J Foot Ankle Surg. 1998;37(4):280-285. 6. Fernandez WG, Yard EE, Comstock RD. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14(7):641-645. 7. Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):669-677. 8. Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47: 678-685. 9. Fu SN, Hui-Chan CW. Modulation of prelanding lower-limb muscle responses in athletes with multiple ankle sprains. Med Sci Sports Exerc. 2007;39(10):1774-1783. 10. Hahn ME, Chou LS. Age-related reduction in sagittal plane center of mass motion during obstacle crossing. J Biomech. 2004;37:837-844. 11. Halliday SE, Winter DA, Frank JS, Patla AE, Prince F. The initiation of gait in young, elderly, and Parkinson’s disease subjects. Gait Posture. 1988;8(1):8-14. 12. Hass CJ, Gregor RJ, Waddell DE, et al. The influence of Tai Chi training on the center of pressure trajectory during gait initiation in older adults. Arch Phys Med Rehabil. 2004;85:1593-1598. 13. Hass CJ, Waddell DE, Fleming RP, Juncos JL, Gregor RJ. Gait initiation and dynamic balance control in Parkinson’s disease. Arch Phys Med Rehabil. 2005;86:2172-2176. 14. Hass CJ, Waddell DE, Wolf SL, Juncos JL, Gregor RJ. Gait initiation in older adults with postural instability. Clin Biomech. 2008;23: 743-753. 15. Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353-370, vii. 16. Hertel J, Olmsted-Kramer LC. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture. 2007;25(1):33-39. 17. Hirose K, Murakami G, Minowa T, Kura H, Yamashita T. Lateral ligament injury of the ankle and associated articular cartilage degeneration in the talocrural joint: anatomic study using elderly cadavers. J Orthop Sci. 2004;9(1):37-43. 18. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319. Downloaded from ajs.sagepub.com at UNIV OF NORTH CAROLINA on April 30, 2010 834 Hass et al The American Journal of Sports Medicine 19. Ito T, Azuma T, Yamashita N. Anticipatory control of the initiation of a single step under biomechanical constraints in humans. Neurosci Lett. 2003;352:207-210. 20. Kirker SGB, Simpson DS, Jenner JR, Wing AM. Stepping before standing: hip muscle function in stepping and standing balance after stroke. J Neurol Neurosurg Psychiatry. 2000;68:458-464. 21. Massion J. Movement, posture, and equilibrium: interaction and coordination. Prog Neurobiol. 1992;38:35-36. 22. McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. 23. Mickelborough J, Van der Linden ML, Tallis RC, Ennos AR. Muscle activity during gait initiation in normal elderly people. Gait Posture. 2004;19:50-57. 24. Pahapill PA, Lozano AM. The pedunculopontine nucleus and Parkinson’s disease. Brain. 2000;123(Pt 9):1767-1783. 25. Pintsaar A, Brynhildsen J, Tropp H. Postural corrections after standardized pertubations of single limb stance: effect of training and orthotic devices in patients with ankle instability. Br J Sports Med. 1996;30(2):151-155. 26. Polcyn AF, Lipsitz LA, Kerrigan DC, Collins JJ. Age-related changes in the initiation of gait: degradation of central mechanisms for momentum generation. Arch Phys Med Rehabil. 1998;79:1582-1589. 27. Santilli V, Franscarelli MA, Paoloni M, et al. Peroneus longus muscle activation pattern during gait cycle in athletes affected by functional ankle instability: a surface electromyographic study. Am J Sports Med. 2005;33(8):1183-1187. 28. Sedory EJ, McVey ED, Cross KM, Ingersoll CD, Hertel J. Arthrogenic muscle response of the quadriceps and hamstrings with chronic ankle instability. J Athl Train. 2007;42(3):355-360. 29. Suda EY, Amorim CF, Sacco Ide C. Influence of ankle functional instability on the ankle electromyography during landing after volleyball blocking. J Electromyogr Kinesiol. 2009;19(2):e84-e93. 30. Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006; 34(4):612-620. 31. Van Deun S, Staes FF, Stappaerts KH, Janssens L, Levin O, Peers KK. Relationship of chronic ankle instability to muscle activation patterns during the transition from double-leg to single-leg stance. Am J Sports Med. 2007;35(2):274-281. 32. Verhagen RA, de Keizer G, Van Dijk CN. Long-term follow-up of inversion trauma of the ankle. Arch Orthop Trauma Surg. 1995;114: 92-96. 33. Wikstrom EA, Bishop MD, Inamdar AD, Hass CJ. Gait termination control strategies are altered in chronic ankle instability subjects. Med Sci Sports Exerc. 2010;42(1):197-205. 34. Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Naugle KE, Borsa PA. Self-assessed disability and functional performance in individuals with and without ankle instability: a case control study. J Orthop Sports Phys Ther. 2009;39(6):458-467. 35. Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Naugle KE, Borsa PA. Dynamic postural control but not mechanical stability differns among those with and without chronic ankle instability. Scand J Med Sci Sports. 2009 Apr 20. [Epub ahead of print]. 36. Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28(2):112-116. 37. Zettel JL, McIlroy WE, Maki BE. Environmental constraints on foot trajectory reveal the capacity for modulation of anticipatory postural adjustments during rapid triggered stepping reactions. Exp Brain Res. 2002;146:38-47. For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav Downloaded from ajs.sagepub.com at UNIV OF NORTH CAROLINA on April 30, 2010