Health Complaints and Outcome Assessment in Coronary Heart Disease
advertisement

Health Complaints and Outcome Assessment in Coronary Heart Disease
JOHAN DENOLLET, PH.D.
Research on coronary heart disease (CHD) lacks sensitive outcome measures. Health complaints, although
subjective in nature, may provide information on the degree of recovery from CHD. The purpose of Study 1
was to identify common health complaints in a group of 535 men (mean age, 57.5 years) with CHD. In the
weeks after a coronary event, they frequently reported somatic (e.g., chest pain, dyspnea, fatigue, sleep
problems) and cognitive (e.g., concern about health and functional status) health complaints. Statistical
analyses produced the Health CompJaints Scale (HCS), which comprises 12 somatic and 12 cognitive
complaints. Confirmatory factor analysis provided evidence for the model undergirding the HCS, and the
somatic and cognitive scales of the HCS were found to have high internal consistency (a > .89), adequate
test-retest reliability (r > .69), and good construct validity. Study 2 provided evidence for the idea that the
HCS can be distinguished from standard scales of psychopathology. Statistical analyses in 266 men with CHD
indicated that, compared to symptoms of psychopathology, the HCS scales displayed discrete factor loadings
as well as higher scores at baseline and a normal clustering of scores. Important to note, HCS scores decreased
in 60 subjects participating in cardiac rehabilitation (p < .0001) but not in 60 control subjects. Although
research should not disregard psychological biases on symptom reporting, it is argued that health complaints
need to be accurately assessed in CHD patients.
Key words: coronary heart disease, health complaints, outcome assessment, quality of life, cardiac rehabilitation.
INTRODUCTION
Outcome assessment in medical settings is a matter that will receive considerable attention in the
coming years (1). It is important that health care
professionals have finely tuned, sensitive measures
in order to keep track of the impact of chronic
disease on functional status and well being and to
monitor the effects of their care on these outcomes
(2). Research on recovery from coronary heart disease (CHD), however, lacks standardized instruments for measuring psychological constructs that
match the theoretically prescribed effect of treatment in this population (3). That is, standard distress
scales predominantly measure the stable disposition
to experience negative emotions (i.e., negative affectivity) in patients with CHD (4) and thus are less
sensitive to change. Scales that were specifically
designed for patients with CHD may be more appropriate to assess psychological effects of treatment (5).
Of note, findings from the Medical Outcomes
Study indicate that CHD is a medical condition that
has a significant impact on the patient's perceived
health status (2). Decrements in perceived health, in
From the University Hospital of Antwerp, Antwerp, Belgium.
Address reprint requests to: Johan Denollet, Ph.D., UZA —
Cardiale Revalidatie, Wilrijkstraat, 10, B-2650 Edegem, Belgium.
Received for publication March 26, 1993; revision received
October 25, 1993.
Psychosomatic Medicine 56:463-474 (1994)
0033-3174/94/5605-0463S03.00/0
Copyright © 1994 by (he American Psychosomatic Society
turn, are intimately linked to psychosocial morbidity associated with CHD, including the likelihood of
seeking medical care (6) and failure to return to
work (7). In fact, one of the primary goals of health
care for these patients is to enhance daily functioning (8). It follows that health complaints, although
not always paralleling the seriousness of CHD, may
provide information on the degree of psychosociaJ
recovery from CHD. Therefore, this paper addresses
the assessment of health complaints in the context
of CHD. Study 1 focused on the prevalence of health
complaints and the construction of a new scale.
Study 2 focused on the rationale for using health
complaints as an outcome measure in CHD.
STUDY 1: ASSESSMENT OF HEALTH
COMPLAINTS
First, the assessment of health complaints should
be relevant from a theoretical point of view. Accordingly, a limited number of somatic and cognitive
symptom clusters, rather than a heterogeneous conglomerate of symptoms, were studied. Somatic
health complaints focused on "cardiopulmonary
problems," "fatigue," and "sleep problems" symptom
clusters. These health complaints have been associated with myocardial infarction and cardiac death
(9-13) and with coronary risk factors, such as hypercholesterolemia (14). Cognitive health complaints focused on the "health worry" (i.e., anxious
concern about health) and "illness disruption" (i.e.,
463
J. DENOLLET
concern about the extent to which illness interferes
with one's life) symptom clusters that were identified in the psychometric analysis of the illness behavior concept (15). Self-ratings of poor health (16)
and functional status (17) have been associated with
mortality.
Second, the assessment of health complaints
should also be relevant from the patient's point of
view. Accordingly, research needs to identify health
complaints that occur frequently in patients with
CHD. Traditional psychometric measures may be
burdensome for nonclinical (with respect to mental
health) populations to complete on a frequent basis
(18). The more burdensome the scale, the greater
likelihood of poor response rate or quality of data
(19). Health complaints with a high frequency of
endorsement, however, are likely to comprise a
measure that may be perceived as being immediately relevant to patients with CHD. The purposes
of Study 1 were to: a) identify somatic and cognitive
health complaints that occur frequently in patients
recovering from a coronary event; and b) devise, on
this basis, a psychometrically sound scale of selfreported health complaints in CHD. Specifically, the
focus was on the primary factors (i.e., the a priori
defined symptom clusters) and their relationship to
the second-order construct of self-rated health in
the context of CHD.
METHOD
Subjects
Subjects were 535 men with CHD drawn from four hospitals
in the Dutch-speaking part of Belgium: the University (N = 341),
Middelheim (N = 105) and Saint Jozef (N = 16) hospitals in
Antwerp, and the Maria's Voorzienigheid Hospital (N = 73) in
Kortrijk. Subjects of the University Hospital were referred by
their attending physician to an outpatient rehabilitation program;
subjects from the other hospitals either participated in homebased cardiac rehabilitation or received standard medical care.
The mean age was 57.5 years (SD = 8.6). All subjects agreed to
participate in the study and filled out questionnaires at 3 to 6
weeks after the incidence of myocardial infarction {MI, N = 126),
coronary artery bypass surgery (CABG, N = 324), or percutaneous
transluminal coronary angioplasty (PTCA, N = 85).
Assessment of Health Complaints
An initial item pool of 20 somatic and 20 cognitive health
complaints was based on: a) items that were derived from the
Illness Behavior Questionnaire (20), the Heart Patients Psychological Questionnaire (21), and the SCL-90 (22); and b) items that
were specifically written for the purpose of this study. The Illness
Behavior Questionnaire predominantly taps cognitive modes of
responding to one's state of health (15). The Heart Patients Psy-
464
chological Questionnaire comprises items that address the discrepancy between the time before and after onset of an acute
coronary event. The SCL-90 contains a number of cardiopulmonary complaints and one item that reflects concern with global
health.
Subjects were asked to rate how much they had been bothered
lately by each health complaint on a 5-point scale of distress
ranging from 0 (not at all) to 4 (extremely). In order to provide a
representative picture of relatively enduring changes in subjective health, "lately" was used as a temporal reference. The time
frame depends on the researcher's interest. If one wishes to assess
rapid changes in a patient's condition that are associated with
particular events (e.g., CABG) a more specific time frame (e.g.,
past week) may be used. Statistical analyses in a subset of 205
subjects were used to reduce the initial item pool; health complaints with a high endorsement frequency, factor loading, and
corrected item-scale correlation were retained. Health complaints
with too much redundancy were deleted. An intermediate 30item scale was administered to a second subsample, and further
analyses produced 12 somatic and 12 cognitive items, each describing a common health complaint.
Construct Validity
The following scales were used to examine the construct
validity of the self-reported health complaints. The disability
scale of the Heart Patients Psychological Questionnaire (21) was
predicted to correlate positively, and the well being scale to
correlate negatively with health complaints. Health complaints
were also validated against three broad and stable personality
traits: negative affectivity, self-deception, and social inhibition.
Negative affectivity is the tendency to experience somatic and
emotional distress (23) and is assessed well by the trait scale of
State-Trait Anxiety Inventory. The Dutch adaptation of this scale
(24) was predicted to correlate positively with self-reported health
complaints. Self-deception and social inhibition are two traits
that are distinctly different from negative affectivity. Self-deception is the tendency to remain unaware of unpleasant emotional
realities and is assessed well by the Marlowe-Crowne scale (25).
Social inhibition is the tendency to inhibit one's feelings and
behaviors and is assessed well by the social inhibition scale of
the Heart Patients Psychological Questionnaire (21). Importantly,
these self-deception and social inhibition measures were predicted to be largely unrelated to self-reported health complaints.
Procedure and Statistical Analysis
All subjects filled out a questionnaire comprising the somatic
and cognitive symptom clusters that were devised on theoretical
grounds. In order to isolate items with a high frequency of
endorsement, the frequency distribution of each health complaint
was calculated. The self-reported health complaints were analyzed on two levels in the hierarchy of constructs: the first-order
level where each item is more or less an alternate form of each
other item and the second-order level that is defined by the
intercorrelations among symptom clusters (26). Confirmatory factor analysis was used to examine the accuracy of both the firstorder (i.e., specific symptom clusters) and second-order (i.e., general construct of self-rated health as defined by intercorrelations
among symptom clusters) a priori model. Important to note, one
can develop a test of the model's fit with this statistical method.
LISREL VI was used for this purpose (27). Exploratory factor
Psychosomatic Medicine 56:463-474 (1994)
HEALTH COMPLAINTS IN CHD
analysis was used to examine the intercorrelations among somatic
and cognitive health complaints. Scree plot and eigenvalue criteria were used to decide on the optimum number of factors to
retain. Cronbach's a was used to obtain internal-consistency
estimates of reliability of the scales that emerged from these
analyses. Pearson's correlations and exploratory factor analysis
were used to examine the construct validity of the self-reported
health complaints.
RESULTS AND DISCUSSION
Assessment of Health Complaints
The majority of somatic health complaints were
marked positively (i.e., score > 0) in at least 50% of
the cases (Table 1). A confirmatory 3-factor solution
indicated that of the 12 somatic health complaints,
five were related to the "cardiopulmonary," four to
the "fatigue," and three to the "sleep problems" a
priori symptom clusters. The goodness of fit index
for this first-order model of somatic complaints was
.92. Cronbach's a indicated an adequate level of
internal consistency for each of these symptom clusters (a = .80, .91, and .89, respectively). Exploratory
factor analysis of the 24 somatic and cognitive health
complaints yielded two factors that accounted for
56% of the total variance. Scree plot indicated that
eigenvalues tended to level after the second factor.
All of the somatic health complaints had their highest loading on Factor II. Accordingly, corrected itemtotal correlations indicated that cardiopulmonary
complaints, fatigue, and sleep problems tended to go
together in this population of coronary patients (a =
.89).
Eleven cognitive health complaints were marked
positively (i.e., score > 0) in at least 50% of the cases
(Table 2). A confirmatory two-factor solution indicated that six cognitive complaints were related to
the "health worry" and six to the "illness disruption"
a priori cluster. The goodness of fit index for this
first-order model of cognitive complaints was .90.
Cronbach's a indicated an adequate level of internal
consistency for both the "health worry" and "illness
disruption" symptom clusters (a = .92 and .91, respectively). Further, exploratory factor analysis of
the 24 health complaints showed that all of the
cognitive health complaints had their highest loading on Factor I. Cronbach's a indicated a high level
of internal consistency (a — .95), and 11 cognitive
complaints had corrected item-total correlations
greater than .70. In general, these findings suggest
the psychometric soundness of the a priori symptom
clusters that were conceptualized for the assessment
of health complaints at the first-order level.
Consistent with the higher order model of perceived health, the somatic and cognitive symptom
clusters were found to be highly intercorrelated, and
confirmatory factor analysis indicated the existence
of one, single second-order construct (Table 3). The
goodness of fit index for this second-order model
was .92. Corrected item-total correlations and Cronbach's a (.84) provided further evidence for the
existence of a general, broad, second-order factor.
TABLE 1. Frequency of Endorsement, Factor Loading, and Internal Consistency of Somatic Health Complaints [N = 535)
Item
N
A Priori Symptom Clusters
Frequency of
Endorsement1
Confirmatory
Factor Analysis*
L1
A10.
A9.
A2.
A6.
A7.
Pain in heart or chest
Shortness of breath
Tightness of the chest
Inability to take a deep breath
Stabbing pain in heart or chest
52%
51%
50%
43%
36%
A4.
A11.
A3.
A8.
Fatigue
Feeling weak
Feeling that you are not rested
Feeling exhausted without any reason
69%
66%
57%
49%
A1.
A5.
A12.
Sleep that is restless or disturbed
Trouble falling asleep
Feeling you can't sleep
64%
60%
49%
L2
L3
.67
.72
.70
.67
..56
.87
.81
.82
.88
.76
.88
.93
Exploratory
Factor
Analysis*
Internal
Consistency*
I
II
.21
.22
.22
.16
.21
.60
.61
.58
.59
.50
.55
.56
.55
.51
.47
.45
.46
.38
.38
.64
.61
.68
.69
.69
.67
.71
.73
.12
.07
.08
.63
.67
.66
.55
.57
.57
' Mean = 54%.
•Analysis of the 12 somatic health complaints; L1-L3, Lisrel estimates (maximum likelihood).
' Analysis of the 24 somatic and cognitive health complaints; l-ll, extracted factors; items assigned to a factor are in boldface; eigenvalue
1 = 2.33.
* Corrected item-total correlations for the Somatic Complaints scale; Cronbach's a = .89.
Psychosomatic Medicine 56:463-474 (1994)
465
J. DENOLLET
TABLE 2. Frequency of Endorsement, Factor Loading, and Internal Consistency of Cognitive Health Complaints [N = 535)
Confirmatory
Item
..
N
* D• •c
.
r-,
A Priori Symptom Clusters
Frequency of
,
' ,
c
Endorsement"
Exploratory
Factor
Factor
B11.
B3.
B8.
B6.
B12.
B1.
Worrying about health
Being afraid of illness
Something serious is wrong with body
The idea that you have a serious illness
All worries over if physically healthy
Bad health is the biggest problem in life
71%
59%
56%
52%
52%
51%
Analysis*
/Midiys.1;.
L2
L1
.83
.77
.88
.84
.76
.83
B4.
B9.
B5.
B7.
B2.
B10.
Able to take on much more work formerly
No longer worth as much as used to be
Feeling blocked in getting things done
Feeling you are not able to do much
Not being able to work fluently
Feeling despondent
78%
76%
75%
70%
66%
49%
.82
.82
.84
.78
.76
.74
Analysis'
""d'"bl:>
I
II
.79
.22
.76
.16
.84
.17
.82
.16
.75
.22
.80
.17
.73
.79
.70
.63
.61
.63
.29
.25
.39
.47
.45
.48
Internal
rJ
Consistency'
.78
.71
.81
.77
.74
.76
.74
.79
.77
.72
.69
.72
8
Mean = 63%.
'Analysis of the 12 cognitive health complaints; L1-L2, Lisrel estimates (maximum likelihood).
' Analysis of the 24 somatic and cognitive health complaints; l-ll, extracted factors; items assigned to a factor are in boldface; eigenvalue
= 11.03.
* Corrected item-total correlations for the Cognitive Complaints scale; Cronbach's a = .95.
TABLE 3. Intercorrelation Matrix and Secondary Factor Analysis of the Five A Priori Symptom Clusters (N = 535)
IntercomNation Matrix*
2.
3.
4.
5.
Confirmatory
Factor Analysis1
Internal
Consistency*
.60
.34
.43
.43
.54
.35
.55
.73
.37
60
.77
.41
.59
.73
.44
.78
.80
.96
.70
.83
A Priori Symptom Clusters
Somatic
1. Cardiopulmonary problems
2. Fatigue
3. Sleep problems
Cognitive
4. Health worry
5. Illness disruption
* All correlations, p < .001.
' Lisrel estimates (maximum likelihood).
' Corrected item-total correlations for the second-order factor of perceived illness; Cronbach's a = .84.
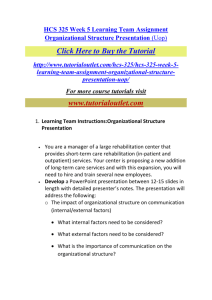
Because the five a priori symptom clusters were
found to measure a common dimension of perceived
health, this list of items was termed the Health
Complaints Scale (HCS) (Fig. 1). In further analyses,
HCS items were summed to obtain somatic and
cognitive health complaint scores that are situated
on the intermediate level of assessment that spans
the hierarchical levels of first-order and secondorder constructs (26).
Construct Validity of the Health Complaints
Scale
Correlations in the range of .54 to .66 indicated
that the somatic and cognitive health complaints
scores (range, 0-48) of the HCS shared 30 to 50%
variance with the disability and well being scales of
466
the Heart Patients Psychological Questionnaire
(Table 4). The HCS scales were also associated with
the tendency to experience distress as measured by
the negative affectivity scale (r = .53 and .60, respectively). Furthermore, the HCS was largely unre lated to measures of self-deception and social inh i b i t i o n (i.e., correlations in the range of .15 to .20).
I n k e e p i n g w i t h t h e s e findingS( exploratory factor
analysis yielded somatopsychic distress, self-deception, and social inhibition dimensions. In general,
these findings revealed a remarkably consistent pattern of convergent and discriminant validity of the
somatic and cognitive health complaints scales.
Clearly, male patients frequently experience
health complaints in the weeks after MI, CABG, or
PTCA. Patients with a spontaneous coronary event
(e.g., MI) reported less somatic complaints (M = 9.4,
Psychosomatic Medicine 56:463-474 (1994)
HEALTH COMPLAINTS IN CHD
HCS
Name:
Sex:
Date:
Age:
Below are a number of problems and complaints that ill people often have. Please read e a c h item
carefully and then circle the a p p r o p r i a t e n u m b e r next to that problem. Indicate how much
each problem has b o t h e r e d you lately. Please use the following scale to record your answers.
0
SOI \ l M l
1
\ I II I I I - l;ll
2
M O D I |{ \ l l
Lately, how much were you bothered
by the following specific problems :
3 .H
III
\ lill
Lately, how much were you bothered
by the following general problems :
Sleep that is restless or
disturbed
0
1 2
3
Dl
The idea that your bad
health is the biggest
problem in your life
1 2
3
Tightness of the chest
0
1 2
3 4
02
Not being able to work
fluently, also with hobbies
1 2
2
Feeling that you are not
rested
0
1 2
3 4
Fatigue
0
1 2
3 4
m
The idea that you were able
to take on much more work
formerly
Trouble falling asleep
0
1 2
3 4
D5
Feeling blocked in getting
things done
-» 0
1 2
3 4
Inability to take a deep
breath
0
1 2
3
06
The idea that you have a
serious illness
0
1 2
3
Stabbing pain in heart or
chest
0
1 2
3 4
Feeling you are not able to
do much
1 2
3
A8
Feeling exhausted without
any reason
0
1 2
3 4
The 'idea that something
serious is wrong with
your body
1 2
3 4
A9
Shortness of breath
0
1 2
3 4
Feeling you are no longer
worth as much as you used
to be
12
3
'° Pain in heart or chest
0
1 2
3 4
Feeling despondent
0
1 2
3 4
Feeling weak
0
1 2
3 4
Worrying about your
health
0 1 2
3 4
Feeling you can't sleep
0
1 2
3 4
Thinking that all your
worries would be over if you
were physically healthy
0
3
A
Being afraid of illness
1)12
- ^ • 0 1 2 3 4
- ^ 0 1 2 3 4
0
1 2
4
4
Fig. 1. The Health Complaints Scale.
Psychosomatic Medicine 56:463-474 (1994)
467
J. DENOLLET
TABLE 4.
Intercorrelation Matrix and Factor Loading of the HCS, HPPQ, STAI, and MC Scales [N = 535)
Intercorrelation Matrix *
HCS
1. Somatic complaints
2. Cognitive complaints
HPPQ
3. Disability
4. Well being
STAI
5. Negative affectivity
MC
6. Self-deception
HPPQ
7. Social inhibition
5.
Exploratory Factor Analysis'
Factor 1
Factor II
.15
.20
.82
.87
-.03
-.05
.02
.08
-.11
.23
.27
-.13
.75
-.83
.07
.21
.24
.00
-.29
.21
.72
-.37
.12
.00
-.10
.96
.01
.12
-.01
.98
3.46
1.05
0.89
2.
3.
4.
.67
.54
.59
-.55
-.66
.53
.60
-.15
-.15
-.54
.41
-.67
Eigenvalue
6.
7.
Factor III
HCS, Health Complaints Scale; HPPQ, Heart Patients Psychological Questionnaire; STAI, State-Trait Anxiety Inventory (Dutch adaptation
of the trait form); MC, Marlowe-Crowne scale.
* All correlations: p < .01, except r = .00: not significant.
f
Loadings of scales that are assigned to a factor are in boldface.
SD = 8.6) than patients who underwent CABG or
PTCA (M = 11.8, SD = 8.8, F(l,533) = 7.12, p < .01).
On a cognitive level, however, neither group of
patients experienced significant differences in subjective health status (F(l,533) = 0.27, p = .60). Consistent with the findings of Study 1, by far the most
common problem reported by the subjects in the
Ischemic Heart Disease Life Stress Monitoring Program was concern about the impact of CHD on their
life (28). Not surprisingly, 80% of the interventions
in this trial focused on the implications of chest
pain, dyspnea, and fatigue. Factor analytic techniques in the present study clearly identified the
somatic and cognitive symptom clusters of cardiopulmonary problems, fatigue, sleep problems, health
worry, and illness disruption.
With reference to this issue, the variables measured by the HCS can be situated on different levels
in the hierarchy of constructs (26). At the lowest
level of this hierarchy (i.e., the level of the a priori
defined symptom clusters) each item is more or less
an alternate form of each other item. At the intermediate level of the hierarchy (i.e., the level of
somatic vs. cognitive health complaints) some of the
defining items for the factor are alternate-forms
types of items, but there are other items with substantial loadings that are not. At the highest level
(i.e., the level of intercorrelations among the various
symptom clusters) the five variables that define the
second-order construct of perceived health are correlated, but they are not alternate forms of one
another in their apparent logical content. Depending
on the researcher's interest, the symptom clusters of
468
the HCS can either be scored separately (assessment
of specific first-order constructs) or can be aggregated to obtain somatic and cognitive scores (assessment of more global constructs) or one single score
that reflects perceived health status (assessment of
one global second-order construct). In this study,
perceived health was measured at the intermediate
level of somatic and cognitive health complaints. On
the whole, the HCS appeared to be a reliable and
valid measure of health complaints in men with
CHD. However, given the fact that there already
exist a large number of widely used distress scales,
it is important to answer the question why a new
scale is needed. The purpose of Study 2 was to
address this central issue somewhat more in detail.
STUDY 2: HEALTH COMPLAINTS VS.
PSYCHOPATHOLOGY
There appears to be a tendency to use familiar
instruments, even if these instruments are less appropriate for the target population or the therapeutic
intervention under investigation. However, the
quality of outcome assessment depends heavily on
the theoretical relevance, the appropriateness, and
the responsiveness of the instruments used. Problems with standard distress scales in the context of
CHD may include measurement of wrong constructs
(3), lack of cover of relevant aspects (29), and a
limited range resulting in floor/ceiling effects (30).
For example, previous research suggests that
Psychosomatic Medicine 56:463-474 (1994)
HEALTH COMPLAINTS IN CHD
standard measures of psychopathology may be less
appropriate to assess change in coronary patients
(target population) as a function of rehabilitation
(therapeutic intervention) (3). Measures that match
the theoretically prescribed effect of cardiac rehabilitation (i.e., enhancement of subjective health and
well being) are more appropriate to assess change in
this context. In other words, identifying appropriate
measures of key constructs is an important factor in
outcome assessment. Considerable difficulties may
also arise because many instruments are based on
what health care professionals regard as important
and take little account of the patient's view about
what is important (29). Items that are perceived as
being relevant to the patient's situation may comprise a measure that is appealing to complete. The
more burdensome the instrument, the greater likelihood of it not being completed. Finally, responsiveness (i.e., sensitivity to changes in what is being
measured) is a crucial requirement in quality of life
research (31).
The major flaw with the method of defining quality of life by the absence of psychopathology is that
this approach does not provide for supranormal levels of functioning and therefore can lead to underestimates of actual changes in quality of life. Therefore, evidence should be provided for the notion that
the HCS can be distinguished from standard scales
of psychopathology. Because the HCS and SCL-90
have the same item-format (a list of symptoms) and
response-format (a 5-point scale of distress), differences in construct validity, distribution of scores,
and responsiveness among these measures are likely
to reflect differences in content: health complaints
vs psychopathology. It is important to note that
research has shown that the SCL-90 is not sufficiently sensitive in the context of cardiac rehabilitation (3). The purpose of Study 2 was to examine:
a) the construct validity of health complaints vs.
symptoms of psychopathology; b) differences in
baseline scores of health complaints and psychopathology; and c) changes in health complaints as a
function of cardiac rehabilitation.
METHOD
Subjects and Measures
The study population consisted of two groups of men with
CHD. The first group was a subset of 266 subjects of Study 1 who
completed the Dutch adaptation of the SCL-90 (32). This adaptation of the SCL-90 comprises seven symptom dimensions that
closely resemble those of the original version (22): somatization,
obsessive-compulsive behavior, interpersonal sensitivity, depres-
Psychosomatic Medicine 56:463-474 (1994)
sion, anxiety, hostility, and phobic anxiety. The second group
consisted of 120 men [mean age, 56.3 years) with CHD (MI N =
55, CABG N = 48, PTCA N = 17) who participated in an ongoing
trial of cardiac rehabilitation (3, 5). In brief, 60 of these 120
subjects received standard medical care at the Maria's Voorzienigheid Hospital of Kortrijk, and 60 subjects completed the rehabilitation program of the University Hospital of Antwerp between
July 1989 and December 1990. This 3-month program included
exercise training, health education, and individual psychosocial
counseling. The second group of subjects was used to examine
the responsiveness of the HCS because previous research indicated that rehabilitation subjects, but not control subjects, experienced significant improvements in perceived health status (3)
and subjective well being (3, 5). Because the cardiac rehabilitation
program is doing what it is claiming, the HCS scales should be
sensitive to changes in perceived health status that are associated
with this program.
Procedure and Statistical Analysis
Pearson's correlations and exploratory factor analysis were
used to examine the relationship between the HCS and SCL-90
scales (N = 266). Next, descriptive characteristics (mean, median,
quartiles, kurtosis, skewness) of both measures were examined.
In this analysis, a median split on the Trait Anxiety Scale (24)
classified subjects as being high (N = 131) or low (N = 135) in
their tendency to experience distress. The 120 subjects that
participated in the rehabilitation trial filled out the HCS scales
again at 3 months after the initial assessment (i.e., at the end of
rehabilitation in the experimental group). Repeated measures
MANOVA, with rehabilitation as between-subjects factor and
time as within-subjects factor, was used to analyze changes in
HCS scores. Finally, test-retest reliability was examined in the 60
control subjects receiving standard medical care alone.
RESULTS AND DISCUSSION
Correlations that were mostly in the range of .50
to .70 indicated that the HCS and SCL-90 scales
shared 25 to 55% of variance (Table 5). Exploratory
factor analysis yielded two dimensions (eigenvalues
> 1.0) of subjective distress. Factor I was largely
defined by the SCL-90 scales, whereas Factor II was
defined by scales that were specifically designed for
cardiac patients. Of note, the SCL-90 scales predominantly reflected a general and broad dimension of
psychological distress in this population of coronary
patients. Despite the fact that both distress measures
have the same format, the HCS and SCL-90 appeared
to have a related, but not an identical, scope. This
finding corroborates the idea that the health complaints of the HCS can be distinguished jrom symptoms of psychopathoJogy in patients with CHD. The
strong factor loadings of the HCS and the Heart
Patients Psychological Questionnaire indicated that
these instruments were measuring a similar construct.
469
J. DENOLLET
TABLE 5.
Intercorrelation Matrix and Factor Loading of the HCS, HPPQ, and SCL-90 scales (N = 266)
Exploratory Factor
Analysis1
Intercorrelation Matrix*
HCS
1. Somatic Complaints
2. Cognitive Complaints
HPPQ
3. Disability
4. Well-Being
SCL-90
5. Somatization
6. Obsessive-Compulsive
7. Interpersonal Sensitivity
8. Depression
9. Anxiety
10. Hostility
11. Phobic Anxiety
5.
6.
7.
8.
9.
-.63
-.69
.74
.68
.63
.66
.51
.58
.61
.71
.66
.74
.39
.39
.44
.60
.40
.50
.74
.71
-.67
.56
-.57
.50
-.52
.32
-.43
.47
-.63
.45
-.64
.30
-.35
.35
-.48
.11
-.29
.86
-.82
.74
.62
.74
.74
.70
.77
.74
.69
.69
.86
.48
.54
.60
.54
.55
.60
.62
.55
.71
.71
.36
.62
.71
.87
.79
.77
.74
.68
.60
.46
.20
.46
.49
.10
.35
6.95
1.09
2.
3.
4.
.73
.57
.58
10.
11.
Eigenvalue
Factor 1
Factor II
HCS, Health Complaints Scale; HPPQ, Heart Patients Psychological Questionnaire; SCL-90, Symptom Check List (Dutch adaptation).
* All correlations: p < .001.
' Loadings of scales that are assigned to a factor are in boldface.
TABLE 6.
Descriptive Characteristics of the HCS and SCL-90 Instruments [N = 266)*
Total Croup
High Distress (N = 131)
Low Distress (N = 135)
Descriptive Characteristics
Mean
Standard deviation
Median
Frequency distribution of scores
(quartiles)
0-24
25-49
50-74
75-100
HCS
SCL-90
HCS
SCL-90
HCS
25.1
20.8
19
12.8
11.9
10
35.8
21.7
33
19.5
12.9
16
14.7
13.4
10
6.4
57
5
57%
28%
12%
3%
85%
14%
1%
0%
35%
39%
21%
5%
70%
28%
2%
0%
80%
16%
4%
0%
100%
0%
0%
0%
SCL-90
* HCL denotes extrapolated total score (range 0-100) of the Health Complaints Scale; SCL-90 denotes extrapolated General Severity
Index (range 0-100) of the Symptom Check List.
Apart from construct validity (or theoretical relevance), a major point in the development of the HCS
is its appropriateness (or relevance from the patient's
point of view). Undoubtedly, the Global Severity
Index of the SCL-90 is a good marker of psychopathology. This implies that the distribution of SCL-90
scores reflects the actual self-report of psychiatric
symptoms in CHD populations. However, the present research did not focus on psychopathology but
on self-rated health. If the notion that coronary
patients may perceive HCS items as being more
relevant to their situation than SCL-90 items is correct, then HCS scores should be significantly higher
than SCL-90 scores. To test this hypothesis, differencesin the frequency distribution of the mean HCS
and SCL-90 scores at baseline were examined.
470
It is important to note that evidence suggests that
an instrument with a less skewed distribution may
sensitively reflect subclinical improvements in selfrated health as a function of cardiac rehabilitation
(3). Because the HCS was specifically designed to
have less extreme response categories than the SCL90, the HCS should be less skewed toward severe
pathology than the SCL-90. Because both instruments have a different range of scores, baseline
scores with a range of 0 to 100 were first extrapolated
in the following manner: HCS = total score/24 x 25;
SCL-90 = total score/90 X 25. Next, the distribution
of these scores was examined (Table 6).
The mean HCS score was twice as high than the
mean SCL-90 score (p < .0001). This difference in
HCS and SCL-90 baseline scores was found in both
Psychosomatic Medicine 56:463-474 (1994)
HEALTH COMPLAINTS IN CHD
TABLE 7.
Mean HCS Entry and End Scores, and Analyses of Variance Results for Rehabilitation and Control Subjects (A' = 120)*
HCS Scale
Somatic complaints
Rehabilitation (N = 60)
Entry Score
End Score
Change
10.1 (7 3)
6.1 (7.5)
-4.0]
10.4 (8.8)
11.1 (8.9)
+0.7J
13.6(10.5)
8.9 (8.3)
-4.7]
14.4 (10.5)
16.0(11.2)
+ 1.6J
Rehabilitation x Time
Interaction Effect
F(1,118) = 19.32,
Control (N = 60)
Cognitive complaints
Rehabilitation (N = 60)
\
Control (N = 60)
p<.0001
F(1,118) = 24.16, p < . 0 0 0 1
* HCS denotes Health Complaints Scale; entry score, mean score within 6 weeks after the coronary event; end score, mean score 3
months after the initial assessment; standard deviations appear in parentheses.
high-distress and low-distress subjects (p < .0001).
Furthermore, the SCL-90 scores were largely restricted to the lower quartiles, whereas the HCL
scores could be found in the higher quartiles as well.
The HCS scores also displayed a normal clustering
around a central point (kurtosis = 0.09), whereas the
SCL-90 clearly displayed a peaked distribution of
low scores (kurtosis = 1.63). Both scales were skewed
to the right, but the HCS (skewness = 0.96) to a lesser
extent than the SCL-90 (skewness = 1.43). The fact
that standard distress scales are usually skewed toward more severe disability makes it difficult to
measure improvement after treatment (29). In general, these findings are consistent with the notion
that patients with CHD may perceive the items of
the HCS as being more reJevant to their situation
than the items of the SCL-90.
A final point in the development of the HCS concerns its sensitivity to change as a function of treatment. In a previous study, the differential sensitivity
to change of the SCL-90 and the Heart Patients
Psychological Questionnaire was examined in a
sample of 162 men with CHD who completed the
Antwerp cardiac rehabilitation program (3). The results of this study indicated that the SCL-90 was
significantly less sensitive to change than the Heart
Patients Psychological Questionnaire. Furthermore,
the anxiety, depression, and hostility subscales of
the SCL-90 were not sensitive enough to detect
actual changes in quality of life in patients who
report a low level of emotional distress at baseline.
By contrast, the HCS items may mirror one of the
primary goals of cardiac rehabilitation, i.e. enhancing functional status and perceived health. This
hypothesis was tested in a sample of 120 patients
with CHD, 60 of which participated in the Antwerp
rehabilitation program. Previous research in this
sample of patients indicated that the 60 rehabilitation subjects, but not the 60 control subjects, rePsychosomatic Medicine 56:463-474 (1994)
ported a significant increase in well being and positive affect and a significant decrease in disability
and negative affect as measured by the Heart Patients Psychological Questionnaire and the Global
Mood Scale (3, 5). There also was significantly less
tranquilizer use in the rehabilitation group than in
the control group.
In the present study, there was no significant
difference between the rehabilitation and control
subjects with reference to age, medical category, or
HCS scores at baseline. Repeated measures MANOVA indicated a significant rehabilitation x time
interaction effect for somatic as well as cognitive
health complaints (Table 7). In other words, changes
in HCS scores differed as a function of treatment.
Three months after the initial assessment, rehabilitation subjects, but not control subjects, reported a
significant decrease in somatic and cognitive health
complaints (p < .0001). This finding suggests that
the HCS reflected the changes in perceived health
that occur during cardiac rehabilitation. Test-retest
reliability (3-month period) of the HCS scales in the
control group was r = .73 and r = .69, respectively
(N = 60).
In general, the findings of Study 2 were consistent
with the notion that the HCS measures a construct
that is not tapped by standard scales of psychopathology. First, factor analysis yielded a distinct distress
factor that had its highest loadings on the HCS and
the Heart Patients Psychological Questionnaire but
not on any of the SCL-90 symptom dimensions.
Second, the HCS had a higher mean score than the
SCL-90, despite the fact that both scales have the
same format. It should be remembered that theoretical relevance and frequency of endorsement were
used as criteria for the selection of items comprising
the HCS. Accordingly, the HCS displayed a normal
clustering of scores. By contrast, the narrow range
of SCL-90 scores indicates that most patients with
471
J. DENOLLET
CHD affirm only a small number of items. Third,
the HCS reflected the clinical changes that occur
during cardiac rehabilitation, whereas previous research found the SCL-90 to be less sensitive to assess
change in this context (3). Hence, the HCS did meet
the criteria of content validity, appropriateness, and
responsiveness.
The nonrandom assignment of subjects to rehabilitation and control groups, however, requires a
conservative interpretation of some findings, and
more research is needed to examine the notion that
health complaints are more than mere markers of
psychopathology in this setting. With reference to
this issue, I do not suggest that research should
ignore the coronary patient's level of psychopathology. On the contrary, evidence indicates that symptoms of psychopathology are associated with an adverse prognosis in patients with CHD (e.g., reference
33). Measures such as the SCL-90 may serve as a
screen to detect patients that are more vulnerable
to serious health problems in the years after a coronary event. However, in addition to assessing
where the patient is in terms of psychopathology, it
is also important to assess other psychological constructs that are relevant in the context of CHD. That
is, the strategy of defining quality of life by the
absence of psychopathology leads to underestimates
of actual changes in quality of life (3). The findings
of Study 2 suggest that an instrument that is sensitive to common problems of patients with CHD (such
as the HCS) better mirrors the changes in perceived
health status in the weeks and months after a coronary event.
GENERAL DISCUSSION
Validation is an ongoing process of obtaining multiple sources of empirical evidence to assess whether
the instrument actually measures what it purports
to (31). It is important to note that this paper does
not provide evidence for the predictive validity of
the HCS. More research is needed to examine the
utility of this new instrument for the prediction of
disease outcome or treatment effects. With reference
to this issue, it is not clear whether the HCS is
superior to other, more general instruments. The
present research only examined the superiority of
the HCS over the SCL-90 for assessing the effect of
cardiac rehabilitation on quality of life.
However, the contribution of this research is
mostly methodological in that it describes the rational development of a potentially useful instrument. Three major principles undergird the devel472
opment of the HCS: a) the HCS is based on a clear a
priori model. The accuracy of this model was tested
with the use of appropriate multivariate statistical
procedures (27); b) the items of the HCS are relevant
from the patient's point of view. The patient was
considered to be the best informant on the way in
which illness affects well being (29); and c) the HCS
is responsive to a clinical intervention. Responsiveness to change was considered to be a dimension of
validity that incorporates longitudinal information
(i.e., change) (31). These methodological issues apply
equally well to other health-related outcome measures.
On the assumption that validity should be built
into a scale from the outset, this paper describes a
new measure of health complaints that are relevant
to patients with CHD. Ideally, the HCS had to be
psychometrically sound, sensitive to change, and
easy to administer. The HCS demonstrated a sound
factor structure that accounted for a large proportion
of variance at both the first- and second-order level
of assessment and was found to have high internal
consistency (a > .80) and adequate test-retest reliability over a 3-month period (r > .69). Significant
correlations with widely used distress measures
(STAI and SCL-90) and with a measure that was
designed for cardiac patients (Heart Patients Psychological Questionnaire) provided evidence for its construct validity. Furthermore, the HCS was largely
unrelated to self-deception or social inhibition, and
sensitively reflected changes in perceived health
that occur frequently in patients with CHD. In addition to psychometric soundness and sensitivity,
the HCS is appealing in its practicality; the scale is
brief and easy to use in a medical setting.
With reference to this issue, the HCS appears to
have broad applicability. Apart from the cardiopulmonary complaints, the items of the HCS may monitor outcomes for other chronic medical conditions
as well. As a matter of fact, the majority of health
complaints of the HCS are symptoms that would be
associated with any serious health or psychiatric
problem. However, cross-validation in other patient
groups is needed. Although both instruments are
closely related, the HCS is distinctive from the Heart
Patients Psychological Questionnaire. The Heart Patients Psychological Questionnaire comprises a mixture of 24 health-related items (i.e., disability and
well-being scales), 16 personality items (i.e., neuroticism and social inhibition scales), and 12 filler
items. As a consequence, the HCS is shorter (24 vs.
52 items) and more straightforward than the Heart
Patients Psychological Questionnaire. Moreover, the
Psychosomatic Medicine 56:463-474 (1994)
HEALTH COMPLAINTS IN CHD
Heart Patients Psychological Questionnaire does not
comprise somatic health complaints.
An unsolved problem, however, concerns the degree to which the present results would generalize
to female patients with CHD. Furthermore, the convergent validity of the HCS was examined by direct
comparison to only one measure of perceived health
in cardiac patients. Another important issue is the
meaning of health complaints per se in patients with
CHD. That is, the reporting of health complaints is
not only dependent on physiological factors, but also
on psychological factors (34). It is by now well established that symptom reporting is influenced by common beliefs about disease (35), the amplification of
bodily sensations (36), and the tendency to interpret
bodily sensations as signs of disease (23). Accordingly, complaints of chest pain (37), dyspnea (38),
fatigue (5), and sleep problems (39) are often a function of psychological distress. Although some individuals tend to overperceive symptoms, others may
fail to report significant bodily sensations (40).
Clearly, self-reported health complaints are error
prone and do not always parallel the objectively
assessed health status. Nonetheless, I believe health
complaints should not be ignored in the context of
CHD.
First, the assessment of health complaints may
serve as a rough screen to identify a subset of patients that are more liable to long-term health complications. Self-report health scales are likely to have
two distinct components: one that is psychological
and another that is health related (23). In other
words, the fact that symptom reporting is biased
does not mean that health complaints cannot also
play a true role in CHD (9-13). In fact, symptom
reporting (41) and poor self-rated health (42) have
been associated with a poor prognosis in patients
with documented CHD. Research also suggests that
coronary spasm may be an organic source of chest
pain in the absence of angiographically documented
CHD (43). Of course, it is unfortunate that most
health complaints, such as discomfort in the chest
or undue fatigue, are not specific of CHD. Nonspecific symptoms do not help a clinician make decisions concerning prognosis and therapy, but they do
warrant further examination of the patient in question. Dismissing measures of perceived health as
merely indicating the illegitimacy of symptom reports may result in the delay of much needed treatment in some coronary patients.
Second, a finely tuned assessment of health complaints may help to evaluate the treatment of patients with CHD. Mortality is not the only outcome
worth studying (1). In fact, a primary goal of health
Psychosomatic Medicine 56:463-474 (1994)
care for coronary patients is to enhance daily functioning and well being (44). Among other things, this
implies the identification of coronary patients at risk
of "medically unnecessary" disability as early as
possible so that they may be given extra help (29).
Another important issue concerns the effect of drug
therapy on quality of life (45).
Unquestionably, the pervasive influence of psychological biases, such as the tendency to experience distress, is a factor with which to be reckoned
in the context of CHD (4). I merely want to stress
that health complaints, albeit subjective in nature,
should be accurately assessed in patients with CHD.
As pointed out by Goodwin (46): " All too often,
excellent papers describing results of sophisticated
research techniques in groups of patients pay little
attention to the clinical aspects studied or to the
patients and their symptoms.. . " Evidence suggests
that quality of life can best be evaluated by patients
themselves (47). The findings of this paper suggest
that the HCS may be of benefit in this area of
research.
This research was supported by a grant of the
National Fund for Scientific Research, Brussels, Belgium.
1 thank Hugo Pauwels at UFSIA for his help in
analyzing the data. I am also indebted to three anonymous reviewers for their helpful comments on an
earlier draft of this article.
REFERENCES
1. Schroeder SA: Outcome assessment 70 years later: Are we
ready? N Engl J Med 316:160-162, 1987
2. Stewart AL, Greenfield S, Hays RD, et al: Functional status
and well-being of patients with chronic conditions: Results
from the Medical Outcomes Study. JAMA 262:907-913, 1989
3. Denollet J: Sensitivity of outcome assessment in cardiac rehabilitation. J Consult Clin Psychol 61:686-695, 1993
4. Denollet J: Negative affectivity and repressive coping: Pervasive influence on self-reported mood, health, and coronaryprone behavior. Psychosom Med 53:538-556, 1991
5. Denollet J: Emotional distress and fatigue in coronary heart
disease: The Global Mood Scale (GMS). Psychol Med 23:111121,1993
6. Manning WG, Wells KB: The effects of psychological distress
and psychological well-being on use of medical services. Med
Care 30:541-553, 1992
7. Smith GR, O'Rourke DF: Return to work after a first myocardial infarction. A test of multiple hypotheses. JAMA 259:
1673-1677, 1988
8. Mulcahy R: Twenty years of cardiac rehabilitation in Europe:
A reappraisal. Eur Heart J 12:92-93, 1991
9. Alonzo AA, Simon AB, Feinleib M: Prodromata of myocardial
infarction and sudden death. Circulation 52:1056-1062,1975
10. Cook DG, Shaper AG. Breathlessness, angina pectoris, and
coronary artery disease. Am J Cardiol 63:921-924, 1989
11. Appels A, Mulder P: Excess fatigue as a precursor of myocardial infarction. Eur Heart ] 9:758-764, 1988
473
J. DENOLLET
12. Carney RM, Freedland KE, Jaffe AS: Insomnia and depression
prior to myocardial infarction. Psychosom Med 52:603-609,
1990
13. Wingard DL, Berkman LF: Mortality risk associated with
sleeping patterns among adults. Sleep 6:102-107,1983
14. Mattiasson I, Lindgarde F, Nilsson JA, Theorell T: Threat of
unemployment and cardio-vascular risk factors: Longitudinal
study of quality of sleep and serum cholesterol concentrations
in men threatened with redundancy. Brit Med J 301:461-466,
1990
15. Zonderman AB, Heft MW, Costa PT: Does the Illness Behavior
Questionnaire measure abnormal illness behavior? Health
Psychol 4:425-436, 1985
16. Kaplan GA, Camacho T: Perceived health and mortality: A
nine-year follow-up of the Human Population Laboratory
cohort. Am J Epidemiol 117:292-304,1983
17. Reuben DB, Rubenstein LV, Hirsch SH, Hays RD: Value of
functional status as a predictor of mortality: Results of a
prospective study. Am ] Med 93:663-669, 1992
18. King AC, Taylor CB, Haskell WL, DeBusk RF: Influence of
regular aerobic exercise on psychological health: A randomized, controlled trial of healthy middle-aged adults. Health
Psychol 8:305-324, 1989
19. Gallacher JE, Smith GD: A framework for the adaptation of
psychological questionnaires for epidemiological use: An example of the Bortner Type A scale. Psychol Med 19:709-717,
1989
20. Pilowsky I, Spence ND, Waddy JL: Illness behaviour and
coronary artery bypass surgery. ] Psychosom Res 23:39-44,
1979
21. Erdman RA, Duivenvoorden HJ, Verhage F, Kazemier M,
Hugenholtz PG: Predictability of beneficial effects in cardiac
rehabilitation: A randomized clinical trial of psychosocial
variables. J Cardiopulm Rehabil 6:206-213,1986
22. Derogatis LR, Lipman RS, Covi L: SCL-90: An outpatient
psychiatric rating scale - Preliminary report. Psychopharmacol Bull 9:13-27, 1973
23. Watson D, Pennebaker JW: Health complaints, stress, and
distress: Exploring the central role of negative affectivity.
Psychol Rev 96:234-254,1989
24. Van Der Ploeg HM, Defares PB, Spielberger CD: ZBV. Een
Nederlandstalige Bewerking van de Spielberger State-Trait
Anxiety Inventory. [ZBV. A Dutch-language adaptation of the
State-Trait Anxiety Inventory]. Lisse, The Netherlands, Swets
and Zeitlinger, 1980
25. Crowne DP, Marlowe D: A new scale of social desirability
independent of psychopathology. J Consult Psychol 24:349354,1960
26. Comrey AL. Factor-analytic methods of scale development in
personality and clinical psychology. J Consult Clin Psychol
56:754-761, 1988
27. Joreskog KG, Sorbom D. LISREL VI: Analysis of linear structural relationships by the method of maximum likelihood.
Chicago, International Educational Services, 1985
474
28. Frasure-Smith N, Prince R. The Ischemic Heart Disease Life
Stress Monitoring Program: Impact on mortality. Psychosom
Med 47:431-445, 1985
29. Mayou R, Bryant B: Quality of life in cardiovascular disease.
Br Heart J 69:460-466,1993
30. Bindman AB, Keane D, Lurie N: Measuring health changes
among severely ill patients: The floor phenomenon. Med Care
28:1142-1152, 1990
31. Hays RD, Hadorn D: Responsiveness to change: An aspect of
validity, not a seperate dimension. Qual Life Res 1:73-75,
1992
32. Arrindell WA, Ettema JH: SCL-90 Handleiding. [SCL-90 Manual]. Lisse, The Netherlands, Swets and Zeitlinger, 1986
33. Ahem DK, Gorkin L, Anderson JL, et al: Biobehavioral variables and mortality or cardiac arrest in the Cardiac Arrhythmia Pilot Study (CAPS). Am J Cardiol 66:59-62,1990
34. Pennebaker JW: The Psychology of Physical Symptoms. New
York, Springer-Verlag, 1982
35. Pennebaker JW, Epstein D: Implicit psychophysiology: Effects
of common beliefs and idiosyncratic physiological responses
on symptom reporting. J Pers 51:468-496,1983
36. Barsky AJ, Goodson JD, Lane RS, Cleary PD: The amplification
of somatic symptoms. Psychosom Med 50:510-519,1988
37. Costa PT, Zonderman AB, Engel BT, Baile WF, Brimlow DL,
Brinker J: The relation of chest pain symptoms to angiographic findings of coronary artery stenosis and neuroticism.
Psychosom Med 47:285-293,1985
38. Bass C, Gardner W: Emotional influences on breathing and
breathlessness. J Psychosom Res 29:599-609,1985
39. Ford DE, Kamerow DB: Epidemiologic study of sleep disturbances and psychiatric disorders: An opportunity for prevention? JAMA 262:1479-1484, 1989
40. Barsky AJ, Hochstrasser B, Coles NA, Zisfein J, O'Donnell C,
Eagle KA: Silent myocardial ischemia. Is the person or the
event silent? JAMA 264:1132-1135, 1990
41. Shekelle RB, Vernon SW, Ostfeld AM: Personality and coronary heart disease. Psychosom Med 53:176-184. 1991
42. Orth-Gomer K, Unden A, Edwards M: Social isolation and
mortality in ischemic heart disease: A 10-year follow-up
study of 150 middle-aged men. Acta Med Scand 224:205-215,
1988
43. Maseri A: Coronary vasoconstriction: Visible and invisible. N
Engl J Med 325:1579-1580, 1991
44. Denollet J: The psychological effect of cardiac rehabilitation
(abstract). Psychosom Med 55:120-121, 1993
45. Dimsdale JE: Reflections on the impact of antihypertensive
medications on mood, sedation, and neuropsychologic functioning. Arch Intern Med 152:35-39, 1992
46. Goodwin JF: The clinical approach - Cui bono ? Eur Heart J
12:751-752, 1991
47. Slevin ML, Plant H, Lynch D, Drinkwater J, Gregory WM:
Who should measure quality of life, the doctor or the patient?
Br J Cancer 57:109-112, 1988.
Psychosomatic Medicine 56:463-474 (1994)