UW-Stout Biological Safety Program Policy Manual
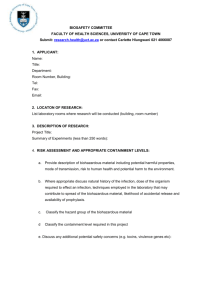
advertisement

UW-Stout Biological Safety Program Policy Manual Table of Contents 1. Introduction ................................................................................................................................1 2. Terminology ................................................................................................................................1 3. Biosafety Subcommittee of the Research Safety Committee ...........................................................4 4. Review and approval of biohazardous materials studies and instruction ..........................................5 5. Roles and responsibilities .............................................................................................................8 6. Practices and procedures ........................................................................................................... 10 7. Biohazardous waste disposal ...................................................................................................... 14 8. Biohazardous spill cleanup .......................................................................................................... 14 9. Transportation and shipping of infectious agents ......................................................................... 16 10. Select agents (Health and Human Services and US Department of Agriculture) .......................... 17 11. Controlled substances (Drug Enforcement Agency) .................................................................. 18 12. Forbidden agents ................................................................................................................... 18 APPENDIX A KEY CONTACTS ............................................................................................................. 19 APPENDIX B PROJECT REGISTRATION AND APPROVAL ...................................................................... 20 APPENDIX C PROJECT REGISTRATION FORMS AND SIGNS ................................................................. 21 APPENDIX D STANDARD PRACTICES AND PROCEDURES..................................................................... 32 Autoclave procedures and safety .................................................................................................... 32 Biological safety cabinets (BSCs) .................................................................................................... 33 Blenders, ultrasonic disrupters, grinders and lyophilizers .................................................................. 35 Bloodborne pathogens ................................................................................................................... 36 Centrifuge equipment .................................................................................................................... 36 Cryostats ...................................................................................................................................... 37 Decontamination ........................................................................................................................... 38 Housekeeping ............................................................................................................................... 40 Labeling ........................................................................................................................................ 40 Loop sterilizers and Bunsen burners ............................................................................................... 41 Personal protective equipment (PPE) .............................................................................................. 41 Pipettes and pipetting aids ............................................................................................................. 42 Sharps safety ................................................................................................................................ 43 APPENDIX E TRAINING ..................................................................................................................... 46 APPENDIX E-1 BIOSAFETY LEVEL 1 (BSL-1) LABORATORY WORKER TRAINING ................................ 47 APPENDIX E-2 BIOSAFETY LEVEL 2 (BSL-2) LABORATORY WORKER TRAINING ................................ 50 APPENDIX E-3 ............................................................................................................................... 54 APPENDIX F TREATMENT, HANDLING AND DISPOSAL OF BIOLOGICAL MATERIALS ............................. 55 APPENDIX G SELECT AGENTS AND TOXINS........................................................................................ 59 APPENDIX H ACRONYMS ................................................................................................................... 60 1. Introduction 1.1. This manual, in conjunction with the latest editions of the U.S. Department of Health and Human Services Publication Number (CDC) 21-1112, Biosafety in Microbiological and Biomedical Laboratories (the BMBL) (http://www.cdc.gov/biosafety/publications/index.htm) and the National Institutes of Health (NIH) Guidelines for Research Involving Recombinant or Synthetic Nucleic Acid Molecules (NIH Guidelines) (http://oba.od.nih.gov/rdna/nih_guidelines_oba.html), outlines the requirements for safely working with biohazardous materials at the University of Wisconsin - Stout. The Research Safety Committee (RSC) is responsible for the regulation of biohazardous materials on the UW-Stout campus. Registration with the RSC is required for all instructional, research, and outreach projects involving potentially pathogenic microorganisms, etiologic agents of Risk Group 2/biosafety level 2 or higher, infectious agents, oncogenic viruses, human tissue and bloodborne pathogens, and in-vitro construction or propagation of recombinant nucleic acid molecules and synthetic nucleic acid molecules. The RSC may be contacted through Safety and Risk Management at 232-1793. 1.2. The concern with all biohazardous material is the safety of University employees and students working with the material and the prevention of release of that material. 1.3. An integral component of the UW-Stout Biosafety Program is a group of generally accepted standard practices and procedures, included in Appendix D. Anyone working with a biohazardous agent or biohazardous material at any facility at UW-Stout is expected to follow these practices and procedures. 1.4. Investigators may work with vertebrate animals in conjunction with their work with some biohazardous materials. All vertebrate animal work conducted at UW-Stout must be approved by the Institutional Animal Care and Use Committee (IACUC), which can be contacted through Research Services at 232-1126. 1.5. Any work with biohazardous materials that involves human subjects must also be approved by the Institutional Review Board (IRB), which can be contacted through Research Services at 2321126. 1.6. Inevitably there are special situations that the existing program is not designed to accommodate. In those situations, consult with the RSC before initiation of the work to prevent misunderstandings after work begins, whether the work is research, teaching or outreach. 1.7. The principal investigator (PI) or instructor involved in teaching, research, and/or outreach activities involving biohazardous materials has the primary ethical and legal responsibility to ensure the safety of students, faculty, staff, visitors and the environment. For that reason PIs are urged to carefully read this manual and understand its contents. If there are specific questions concerning this manual or the UW-Stout Biological Safety Program please contact Safety and Risk Management at 232-1793. 2. Terminology 2.1. Traditionally, microorganisms have been classified according to the biological containment they require. Four levels of containment have been defined and termed biosafety levels (BSLs 1-4); thus an organism requiring, for example, BSL-2 containment is termed a BSL-2 or a Class 2 1 agent or organism. More recently, NIH has introduced classification of agents into four risk groups based on their relative pathogenicity for healthy adult humans. The following table lists the four groups and the basis for classification. Risk Group 1 (RG1) Risk Group 2 (RG2) Risk Group 3 (RG3) Risk Group 4 (RG4) Agents that are not associated with disease in healthy adult humans Agents that are associated with human disease that is rarely serious and for which preventive or therapeutic interventions are often available Agents that are associated with serious or lethal human disease for which preventive or therapeutic interventions may be available (high individual risk but low community risk) Agents that are likely to cause serious or lethal human disease for which preventive or therapeutic interventions are not usually available (high individual risk and high community risk) 2.1.1. Risk group classifications correlate with but do not equate to biosafety levels. A risk assessment performed by the PI will determine the degree of correlation between an agent’s risk group classification and the required biosafety level. Under some circumstances, the containment level required may be raised or lowered as a result of a comprehensive risk assessment as detailed in Section II-A-3 of the NIH Guidelines. If you have any concerns regarding the risk group or appropriate level of containment for an organism, consult the NIH Guidelines. 2.1.2. There are several references for assistance with classification of organisms by risk group: 2.1.2.1. Appendix B of the NIH Guidelines lists biological agents by risk group and includes those agents known to infect humans as well as selected animal agents that may pose theoretical risks if inoculated into humans. Included are lists of representative genera and species known to be pathogenic. Mutated, recombined, and nonpathogenic species and strains are not considered. Non-infectious life cycle stages of parasites are excluded. The list includes the more commonly encountered agents and is not meant to be all-inclusive. 2.1.2.2. The American Biological Safety Association maintains a searchable database (http://www.absa.org/riskgroups/index.html) of international risk group classifications for bacteria, viruses, fungi, and parasites that provides information to be used as a starting point for the risk assessment and the determination of the biosafety level to be used when working in the laboratory. 2.1.2.3. The Public Health Agency of Canada has produced Pathogen Safety Data Sheets for common human pathogens (http://www.phac-aspc.gc.ca/lab-bio/res/psdsftss/index-eng.php) that include a section on recommended exposure controls/precautions, including risk group/biosafety level. 2 2.1.3. All PIs using human organ or cell cultures (primary cultures, cell strains, cell lines) must handle all such cultures under BSL-2 conditions and in accordance with the Bloodborne Pathogen Standard (29 CFR 1910.1030) unless the RSC has specifically approved a lower standard of containment. 2.2. For the purposes of this policy, a biohazardous material is any biological material capable of causing harm to humans, animals or plants, including both biohazardous agents and nonreplicating materials such as toxins. In addition, this term may also be used to refer to material that harbors a biohazardous agent. A biohazardous agent is a pathogen capable of replication and is a disease-causing microorganism capable of causing diseases in humans, animals, or plants. Toxic, mutagenic, and teratogenic chemicals are not considered biohazards for the purpose of this policy. 2.2.1. There are several categories of biohazards or potentially infectious materials, including: 2.2.1.1. Human, animal and plant pathogens: bacteria (including those with drug resistance plasmids), rickettsiae, fungi, viruses (including oncogenic viruses and viroids), parasites, and prions. 2.2.1.2. All human and/or non-human primate blood, blood products, tissues and certain body fluids. Researchers or instructors contemplating use of human blood, blood products, tissues and body fluids should also contact the IRB through Research Services at 232-1126; more information is available at http://www.uwstout.edu/rs/humansubjects.cfm. 2.2.1.3. Cultured cells (all human and certain animal species) and potentially infectious agents these cells may contain. 2.2.1.4. Biological toxins (bacterial, fungal, botanical, etc.). 2.2.1.5. Certain recombinant nucleic acid molecules and synthetic nucleic acid molecules, and cells, organisms and viruses containing such molecules. 2.2.1.6. Infected animals and animal tissues. 2.3. Research involving experimentation and manipulation of various types of potentially infectious systems can be divided into four general categories. They are those that expose the worker or the environment to (1) blood, bodily fluids, and organs/tissues of human origin; (2) infectious agents and their potentially infectious products; (3) recombinant or synthetic nucleic acid molecules and their products; and (4) miscellaneous biohazardous materials. 2.3.1. Experimentation or manipulations of human blood or other materials of human origin, including, but not limited to excreta, secreta, blood and its components, unfixed tissue, and tissue fluids, all of which may or may not contain an infectious agent, may place the worker at risk of exposure to bloodborne pathogens. Examples that could result in exposure would be clinical sciences laboratories performing tests or analyses on human blood or other potentially infectious materials or research labs performing experiments and/or manipulations with human blood or unfixed tissues or organs. 3 2.3.2. Infectious agents, pathogens or substances are defined as those substances containing viable microorganisms or their toxins that are known or suspected to cause disease in animals, plants or humans. Pathogens are classified as bacteria, fungi, rickettsiae, viruses, parasites, oncogenic viruses, and prions. Any materials that come in contact with infectious agents or their byproducts must be handled and disposed of in the same manner appropriate for disposing of the infectious agents themselves. 2.3.3. In the context of the NIH Guidelines, recombinant and synthetic nucleic acid molecules are defined as: 2.3.3.1. Molecules that a) are constructed by joining nucleic acid molecules and b) that can replicate in a living cell (i.e., recombinant nucleic acids); 2.3.3.2. Nucleic acid molecules that are chemically or by other means synthesized or amplified, including those that are chemically or otherwise modified but can base pair with naturally occurring nucleic acid molecules (i.e., synthetic nucleic acids); or 2.3.3.3. Molecules that result from the replication of those described in 2.3.3.1 and 2.3.3.2. 2.3.4. Miscellaneous biohazardous materials include materials not directly covered by the above definitions, such as allergens, cultured animal cells and their potentially infectious agents, tissues from experimental animals (including animal dander), plant viruses, bacteria and fungi, toxins (bacterial, plant, etc.), and those as yet unnamed elements or agents that may produce disease. In regard to allergens, it is not the intent of the RSC to require the registration of research projects involving only allergens (i.e. projects involving allergens not listed as biohazardous agents or materials). Allergens are almost ubiquitous in the environment. However, it is important that PIs consider the hazard associated with allergens because manipulations of these allergens or materials containing allergens may result in human exposures to allergens at concentrations orders of magnitude greater than would normally occur. Because severe allergenic reactions may be life-threatening, the control of allergens in any teaching, research or outreach project must be an important consideration in experimental/procedural design. 3. Biosafety Subcommittee of the Research Safety Committee 3.1. The RSC is charged by the University Chancellor to formulate policy and procedures related to biosafety, chemical hygiene and radiation safety. The Biosafety Subcommittee of the RSC (referred to as the Biosafety Subcommittee for the remainder of this document) functions to approve experiments involving human gene therapy, formation of transgenic animals or plants, and the generation and/or use of recombinant or synthetic nucleic acid molecules in accordance with the requirements of the NIH Guidelines. UW-Stout also requires Biosafety Subcommittee registration and approval for use of RG2 biohazardous agents and toxins. 3.2. Structure and responsibilities 3.2.1. Members of the Biosafety Subcommittee will be selected from the general RSC membership based on their experience with and expertise in biohazardous materials and their capability to assess the safety of work with these materials and to identify any potential risk to public health or the environment. 4 3.2.2. The Biosafety Subcommittee has the responsibility of assessing risks and potential environmental impacts associated with investigations involving biological agents and making recommendations for safe conduct of such studies. It also functions on behalf of the institution to ensure that the experimental work is performed in compliance with current policies and guidelines promulgated by government granting and regulatory agencies. 3.2.3. Registrations approved by the Biosafety Subcommittee will be active for three years from the date of approval. Written notification that the registration will expire will be sent out at least 30 days prior to the expiration date. The PI will then be required to submit a new registration application for review and approval by the Biosafety Subcommittee. 3.2.4. The Biosafety Subcommittee will meet as necessary to conduct business. 4. Review and approval of biohazardous materials studies and instruction 4.1. The Biosafety Subcommittee and RSC can effectively carry out their designated functions only if they have adequate prior knowledge of potentially hazardous research projects and instruction. Therefore, all instructional, research, and outreach projects involving potentially pathogenic microorganisms, etiologic agents of RG1 or higher, infectious agents, oncogenic viruses, human tissue and bloodborne pathogens, and work with recombinant or synthetic nucleic acid molecules must be registered with and approved in writing by the Biosafety Subcommittee. 4.2. It is not the purpose of the Biosafety Subcommittee to pass judgment on scientific merits or even to consider "risk" versus "expected benefits" of potentially hazardous research projects involving an organism of RG1 or RG2 to be undertaken on the University’s premises. Rather, it is the concern of this Committee to know whether or not the safety precautions proposed for the experimental work are adequate for protection of personnel and the environment. In general, the review process will focus on (1) qualifications of the investigator, (2) agents to be employed, (3) risks presented by experimental procedures, (4) adequacy of containment equipment and facilities, (5) training level of persons directly associated with the work, and (6) other factors relevant to safe conduct of the study. 4.3. Due to a lack of facilities designed to contain them, UW-Stout does not allow RG3 or RG4 organisms or biohazardous materials requiring BSL-3 or BSL-4 containment or facilities on the campus or at any of its outlying units or off-campus locations. There are a limited number of approved and certified BSL-4 facilities within the U.S., such as those at the Centers for Disease Control and Prevention (CDC) in Atlanta, GA and the U.S. Army Medical Research Institute for Infectious Diseases in Fort Detrick, MD. 4.4. The PI and the Biosafety Subcommittee must concur on all matters relating to containment requirements, safe practices, and handling and disposal procedures for biohazardous materials. In the event of non-concurrence, the recommendations of the Biosafety Subcommittee shall prevail until such time as they are modified or rescinded by appellate decision of an administrative review that may include outside reviewers. Questions relating to recombinant or synthetic nucleic acid molecule studies that are not covered by the NIH Guidelines will be referred to the NIH Office of Biotechnology Activities (OBA) for resolution. 5 4.5. Some laboratories maintain cultures and/or archival samples of biohazardous materials. In these instances, a “generic” registration for maintenance and storage of reference or other samples/cultures shall be submitted to the Biosafety Subcommittee. An inventory of agents should be attached and updated whenever significant changes are made, either additions or deletions. Significant changes include additional species or additional strains of inventoried agents that demonstrate a need for more stringent containment. 4.6. All projects involving recombinant or synthetic nucleic acid molecules must comply with the NIH Guidelines, regardless of the source of funds supporting the research. It is the definitive reference for this research in the United States. 4.6.1. UW-Stout requires that all experiments involving the generation and/or use of recombinant or synthetic nucleic acid molecules be registered with the Biosafety Subcommittee, EVEN IF THEY ARE EXEMPT from the NIH Guidelines. There may be recombinant or synthetic nucleic acid molecule experiments that are not covered by the NIH Guidelines that require review and approval by outside agencies before initiation or funding. These experiments are most common in the environmental sciences. If you have specific questions about a particular host-vector system not covered by the guidelines, please call the OBA, National Institutes of Health at (301) 496-9838 or FAX (301) 496-9839. 4.6.2. Experiments involving recombinant or synthetic nucleic acid molecules are divided into categories denoted as classes. Presently there are six classes (III-A, III-B, III-C, III-D, III-E and III-F). It is the responsibility of the PI to read the NIH Guidelines in order to determine which class is applicable to the work conducted. 4.6.3. Exempt experiments are listed in the NIH Guidelines. To register exempt recombinant or synthetic nucleic acid molecule research complete the “Registration Cover Sheet,” noting the reason the research is exempt, and a “Registration Form for Exempt Research” and send both to the Biosafety Subcommittee. Forms are found in Appendix C. The Biosafety Subcommittee review will certify the project as exempt. All such research must be conducted using BSL-1 practices. Exempt experiments include: 4.6.3.1. Those that are not in organisms or viruses. 4.6.3.2. Those that consist entirely of DNA segments from a single nonchromosomal or viral DNA source, though one or more of the segments may be a synthetic equivalent. 4.6.3.3. Those that consist entirely of DNA from a prokaryotic host including its indigenous plasmids or viruses when propagated only in that host (or a closely related strain of the same species), or when transferred to another host by well-established physiological means. 4.6.3.4. Those that consist entirely of DNA from a eukaryotic host including its chloroplasts, mitochondria, or plasmids (but excluding viruses) when propagated only in that host (or a closely related strain of the same species). 4.6.3.5. Those that consist entirely of DNA segments from different species that exchange DNA by known physiological processes, though one or more of the segments may 6 be a synthetic equivalent. A list of such exchangers will be prepared and periodically revised by the NIH Director with advice of the Recombinant DNA Advisory Committee (RAC) after appropriate notice and opportunity for public comment. See the NIH Guidelines, Appendices A-I through A-VI, Exemptions Under Section III-F-5-Sublists of Natural Exchangers, for a list of natural exchangers that are exempt. 4.6.3.6. Those that do not present a significant risk to health or the environment as determined by the NIH Director, with the advice of the RAC, and following appropriate notice and opportunity for public comment. See the NIH Guidelines, Appendix C, Exemptions under Section III-F-6 for other classes of experiments that are exempt. 4.6.4. The following experiments require Biosafety Subcommittee review and approval simultaneous with initiation (prior approval is not required); see the NIH Guidelines, Section III-E. To register non-exempt recombinant or synthetic nucleic acid molecule research, complete “Registration Cover Sheet” and a “Recombinant DNA Registration Form for Non-Exempt Research” and send to the RSC. 4.6.4.1. Experiments involving the formation of recombinant or synthetic nucleic acid molecules containing no more than two-thirds of the genome of any eukaryotic virus. 4.6.4.2. Experiments involving nucleic acid modified-whole plants, and/or experiments involving recombinant or synthetic nucleic acid molecule-modified organisms associated with whole plants, except those that fall under Section III-A, III-B, III-D, or III-F of the NIH Guidelines (as described in the NIH Guidelines, Section III-E-2). 4.6.4.3. Experiments involving transgenic rodents in which the animal’s genome has been altered by stable introduction of recombinant or synthetic nucleic acid molecule, or nucleic acids derived therefrom, into the germ line (transgenic rodents). 4.6.5. The following experiments require approval from the Biosafety Subcommittee prior to initiation; see the NIH Guidelines, Section III-D. To register these projects, complete “Registration Cover Sheet” and a “Registration Form for Non-Exempt Research” and send to the Biosafety Subcommittee with the applicable supporting documentation. 4.6.5.1. Experiments using RG2 (or higher) or restricted agents as host-vector systems. 4.6.5.2. Experiments in which DNA from RG2 (or higher) or restricted agents is cloned into nonpathogenic prokaryotic or lower eukaryotic host-vector systems. 4.6.5.3. Experiments involving the use of infectious DNA or RNA viruses or defective DNA or RNA viruses in the presence of a helper virus in tissue culture systems. 4.6.5.4. Experiments involving whole animals. 4.6.5.5. Experiments involving whole plants. 4.6.5.6. Experiments involving more than 10 liters of culture. 7 4.6.5.7. Experiments involving influenza viruses. 4.6.6. The use of any campus greenhouse facility for research with transgenic plants must be approved by the Biosafety Subcommittee and greenhouse management personnel. 4.7. Research and instruction involving infectious biological agents (RG2 organisms or above) and biologically-derived toxins must be registered with and approved by the Biosafety Subcommittee prior to the start of work. Additional information and forms are found in Appendices B and C. 4.8. All animal protocols involving the use of recombinant or synthetic nucleic acid molecules; infectious or transmissible agents; human blood, body fluids or tissues; or toxins must be submitted to the Biosafety Subcommittee for registration and approval prior to final approval by the IACUC. The PI must notify the IACUC in writing prior to initiation of experimentation. IACUC guidelines are available online (http://www.uwstout.edu/rs/iacuc.cfm). Investigators who are uncertain how to categorize agents should contact the Biosafety Subcommittee. 5. Roles and responsibilities 5.1. The Biosafety Officer (BSO) is primarily responsible for implementation and the day-to-day management of the biological safety program. Major duties or activities of the BSO include the following: 5.1.1. Monitor compliance with University safety practices and procedures regarding potentially infectious and biohazardous materials. 5.1.2. Assist in the preparation and periodic updating of a biosafety manual that is in accordance with University policy and consistent with government regulatory guidelines. 5.1.3. Provide consultation to investigators and instructors on matters relating to laboratory safety, appropriate handling and containment of biohazardous materials, decontamination, and disposal of biohazardous wastes. 5.1.4. Aid investigators and instructors in the development of appropriate emergency measures for dealing with accidental spills and contamination. 5.1.5. Conduct surveillance of laboratories in which biohazardous materials are employed to ensure compliance with the approved protocol, prescribed safety guidelines, prescribed safety training and rectification of any deficiencies. 5.1.6. Monitor all intra-campus transport to ensure compliance with the rigorous containment procedures described herein. Provide information for off-campus shipment of biohazardous materials. 5.1.7. Develop and conduct training programs for laboratory personnel using biohazardous materials, specifically to promote techniques for safe handling and disposal. 5.1.8. Serve as liaison between the University and outside regulatory agencies concerned with the use of biohazardous materials. 8 5.1.9. The BSO, with concurrence from the Co-chairs of the RSC, or with concurrence of three members of the RSC if the Chairs are unavailable, may stop any work with microbial agents or any hazardous research project that creates an unreasonable hazard to personnel or involves experiments prohibited by the University. The entire RSC then will review the problem and will complete the review within a working week. Written recommendation(s) will be forwarded from the RSC to the Vice Chancellor for Academic and Student Affairs for final action. 5.1.10. In the event of a mechanical malfunction, systems breakdown or shutdown of any nature, or preventive maintenance of primary containment equipment or components, the BSO must be notified immediately. In the case of an unplanned event and if Physical Plant mechanical staff is not already on the scene, the BSO will notify appropriate Physical Plant staff. Proper precautions must be taken immediately. All experiments must be halted and the biological agents secured (e.g. containers sealed or placed in freezer or refrigerator). The area must be cordoned off during the entire time of the shutdown. No further activities will be allowed until the BSO certifies that the facility is safe to use. 5.2. Principal investigators (PIs) and Laboratory Instructors: 5.2.1. The PI is expected to know and understand all relevant safety guidelines described in this manual, to personally monitor day-to-day operation of the laboratory, and to take all necessary steps for protection of staff, students, and the general public against undesirable consequences of experimental work conducted within UW-Stout facilities. Ultimate responsibility for the safe conduct of research involving biohazardous materials rests with the PI. The PI is aware of the complexities of the research and its associated hazards and must adequately inform all who are working in the research laboratory or otherwise involved in the research of the hazards involved. Because working with biohazardous materials may pose special risks, the PI must assure compliance with the biohazardous materials standard policies and procedures. 5.2.2. File a registration form with and obtain written approval of the Biosafety Subcommittee before performing work involving the use of oncogenic viruses, infectious agents, recombinant or synthetic nucleic acid molecules or experiments involving the use of human blood, bloodborne pathogens or other potentially infectious materials such as unfixed human tissues, primary human cell lines, and certain bodily fluids. See Section 4 and Appendix B of this manual for the registration and approval process. 5.2.3. Thoroughly inform and train all persons (including research personnel such as graduate students, undergraduate students, technicians and laboratory researchers) directly involved in potentially hazardous experiments on the biohazardous materials and harmful chemicals, the potential health risk presented and the safety procedures necessary to minimize exposure. Training requirements are outlined in Appendix E. Each laboratory must maintain a current inventory book of biohazardous material, maintain a current record of personnel training, post safety standards for the required biosafety level and maintain safety information for each human pathogen in the inventory. 5.2.4. Establish emergency procedures to be followed in the event of an overt spill or contamination with potentially hazardous biological material. These procedures should be 9 posted in a prominent place in the laboratory. Moreover, it is recommended that a responsible member of the laboratory staff be designated to handle emergency situations whenever the PI is absent from the premises. Section 9 of this manual provides guidelines for spill cleanup. 5.2.5. Immediately report any unusual incident, such as spill, break in containment, or overt contamination to the BSO or Safety and Risk Management. 5.2.6. Post working areas and facilities with biohazard warning signs. Standardized signs will be provided by the BSO, and are included in Appendix C. The PI should consult the BSO if assistance is required in placement of signs. 5.3. Laboratory personnel and students 5.3.1. All research personnel (researchers, graduate students and undergraduate students) and teaching lab students under the direction of the PI are expected to participate in the safety training and to use safety procedures established by the PI. 5.3.2. Perform all tasks using established safety practices and shall comply with the safety guidelines for the work being performed. 5.3.3. Keep themselves informed of the risks in the laboratory and ask for and participate in training that increases their knowledge and ability to deal safely with the risks. 5.3.4. Report all unsafe practices, accidents and injuries to the PI/instructor (or the laboratory manager or BSO if the PI/instructor is unavailable). 6. Practices and procedures 6.1. Standard microbiological practices will be followed when working with all biohazardous materials, regardless of BSL or risk group. 6.1.1. The laboratory supervisor must enforce UW-Stout policies that control access to the laboratory (e.g. granting key card access only to authorized students and staff, keeping doors closed). 6.1.2. Persons must wash their hands after working with potentially hazardous materials and before leaving the laboratory. 6.1.3. Eating, drinking, smoking, handling contact lenses, applying cosmetics, and storing food for human consumption must not be permitted in laboratory areas. Food must be stored outside the laboratory area in cabinets or refrigerators designated and used for this purpose. 6.1.4. Mouth pipetting is prohibited; mechanical pipetting devices must be used. 6.1.5. Policies for the safe handling of sharps, such as needles, scalpels, pipettes, and broken glassware must be developed and implemented; see Appendix D for recommended practices. Whenever practical, laboratory supervisors should adopt improved engineering 10 and work practice controls that reduce risk of sharps injuries. Precautions, including those listed below, must always be taken with sharp items. These include: 6.1.5.1. Careful management of needles and other sharps are of primary importance. Needles must not be bent, sheared, broken, recapped, removed from disposable syringes, or otherwise manipulated by hand before disposal. 6.1.5.2. Used disposable needles and syringes must be carefully placed in conveniently located puncture-resistant containers used for sharps disposal. 6.1.5.3. Non-disposable sharps must be placed in a hard walled container for transport to a processing area for decontamination, preferably by autoclaving. 6.1.5.4. Broken glassware must not be handled directly. Instead, it must be removed using a brush and dustpan, tongs, or forceps. Plastic ware should be substituted for glassware whenever possible. 6.1.6. Perform all procedures to minimize the creation of splashes and/or aerosols. 6.1.7. Decontaminate work surfaces after completion of work and after any spill or splash of potentially infectious material with appropriate disinfectant. 6.1.8. Decontaminate all cultures, stocks, and other potentially infectious materials before disposal using an effective method. Depending on where the decontamination will be performed, the following methods should be used prior to transport. 6.1.8.1. Materials to be decontaminated outside of the immediate laboratory must be placed in a durable, leak proof container and secured for transport. 6.1.8.2. Materials to be removed from the facility for decontamination must be packed in accordance with applicable local, state, and federal regulations. 6.1.9. A sign incorporating the universal biohazard symbol must be posted at the entrance to the laboratory or classroom when infectious agents are present. The sign should include the name of the agent(s) in use, and the name and phone number of the laboratory supervisor or other responsible personnel. For BSL-2 agents, the sign should also include the procedure required for entry and exit (e.g. PPE) and special practices (e.g. use of BSC, immunizations). Signs are available in Appendix C, or from the BSO. 6.1.10. An effective integrated pest management program is required (see Appendix G of the BMBL). 6.1.11. The laboratory supervisor must ensure that laboratory personnel receive appropriate training regarding their duties, the necessary precautions to prevent exposures, and exposure evaluation procedures. Personnel must receive annual updates or additional training when procedural or policy changes occur. Personal health status may impact an individual’s susceptibility to infection, ability to receive immunizations or prophylactic interventions. Therefore, all laboratory personnel and particularly women of childbearing age should be provided with information regarding immune competence and conditions that may predispose them to infection. Individuals having these conditions should be 11 encouraged to self-identify to their healthcare provider for appropriate counseling and guidance. 6.2. Work with BSL-2 agents requires special practices: 6.2.1. Access to the laboratory must be restricted when work is being conducted. 6.2.2. All persons entering the laboratory must be advised of the potential hazards. This can be accomplished by posting the BSL-2 Point Paper (Appendix E-3) along with a sign-in sheet to record the names of people who have reviewed the paper. The paper can also be reviewed with classes or groups as a whole. 6.2.3. Laboratory personnel must be provided medical surveillance, as appropriate, and offered available immunizations for agents handled or potentially present in the laboratory. 6.2.4. A laboratory-specific biosafety manual must be prepared and adopted as policy. The biosafety manual must be available and accessible. 6.2.5. The laboratory supervisor must ensure that laboratory personnel demonstrate proficiency in standard and special microbiological practices before working with BSL-2 agents. 6.2.6. Potentially infectious materials must be placed in a durable, leak proof container during collection, handling, processing, storage, or transport within a facility. 6.2.7. Laboratory equipment should be routinely decontaminated, as well as after spills, splashes, or other potential contamination. 6.2.8. Spills involving infectious materials must be contained, decontaminated, and cleaned up by staff properly trained and equipped to work with infectious material. 6.2.9. Equipment must be decontaminated before repair, maintenance, or removal from the laboratory. 6.2.10. Incidents that may result in exposure to infectious materials must be immediately evaluated and treated according to procedures described in the laboratory biosafety manual. All such incidents must be reported to the laboratory supervisor. Medical evaluation, surveillance, and treatment should be provided and appropriate records maintained. 6.2.11. Animal and plants not associated with the work being performed must not be permitted in the laboratory. 6.2.12. All procedures involving the manipulation of infectious materials that may generate an aerosol should be conducted within a biological safety cabinet (BSC) or other physical containment devices. 12 6.3. The following safety equipment should be used when working with biohazardous materials: 6.3.1. For BSL-1 agents, special containment devices or equipment, such as BSCs, are not generally required. For BSL-2 agents, properly maintained BSCs, other appropriate personal protective equipment, or other physical containment devices must be used whenever: 6.3.1.1. Procedures with a potential for creating infectious aerosols or splashes are conducted. These may include pipetting, centrifuging, grinding, blending, shaking, mixing, sonicating, opening containers of infectious materials, inoculating animals intranasally, and harvesting infected tissues from animals or eggs. 6.3.1.2. High concentrations or large volumes of infectious agents are used. Such materials may be centrifuged in the open laboratory using sealed rotor heads or centrifuge safety cups. 6.3.2. Protective laboratory coats, gowns, smocks, or uniforms designated for laboratory use are recommended for work with BSL-1 agents and required for BSL-2 agents. Remove protective clothing before leaving the laboratory. Dispose of protective clothing appropriately, or deposit it for laundering. BSL-2 laboratory clothing should not be taken home. 6.3.3. Safety glasses are required to be worn by everyone in the laboratory if anyone is working with a liquid chemical or biohazardous material. Splash goggles (and mask, face shield or other splatter guard as needed) should be used for anticipated splashes or sprays of infectious or other hazardous materials when the microorganisms must be handled outside the BSC or containment device. Eye and face protection must be disposed of with other contaminated laboratory waste or decontaminated before reuse. Persons who wear contact lenses in laboratories should also wear eye protection. 6.3.4. Gloves must be worn to protect hands from exposure to hazardous materials. Glove selection should be based on an appropriate risk assessment. Alternatives to latex gloves should be available. Gloves must not be worn outside the laboratory. In addition, laboratory workers should: 6.3.4.1. Change gloves when contaminated, glove integrity is compromised, or when otherwise necessary. 6.3.4.2. Remove gloves and wash hands when work with hazardous materials has been completed and before leaving the laboratory. 6.3.4.3. Do not wash or reuse disposable gloves. Dispose of used gloves with other contaminated laboratory waste. Hand washing protocols must be rigorously followed. 6.3.5. For work with BSL-2 agents and animals, a risk assessment should be used to determine if eye, face and/or respiratory protection is needed in rooms containing infected animals. 13 6.4. Emergency procedures: 6.4.1. All injuries and accidental autoinoculation, ingestion or inhalation of infectious agents must be reported immediately to the lab director or supervisor and the BSO. Affected employees should be sent to their primary care physician for evaluation, possible treatment and/or possible referral. Dial 911 immediately for any medical emergency. 6.4.2. In case of natural disasters, fires, or power failure the following precautions must be taken: 6.4.2.1. In power failures, immediately discontinue all work until power is restored. If a BSC is being used, all open containers and the hood sash must be closed. 6.4.2.2. In case of fire, personnel must immediately follow standard emergency procedures (evacuate area, call 911). Temperatures sufficient to ignite materials will inactivate infectious agents used in the laboratory. However, emergency personnel should don PPE before entering the lab and follow disinfecting procedures described in Section 8 for decontaminating any released infectious materials not involved in the fire. 6.4.2.3. In natural disasters, personnel must immediately follow standard emergency procedures (take shelter, wait for further instructions). Upon return to the facility, PPE must be used when entering a lab to decontaminate any disaster-related release of infectious material. Contain released material and decontaminate using spill procedures outlined in Section 8. Emergency personnel should don PPE before entering lab and/or areas housing infected animals. 7. Biohazardous waste disposal 7.1. All disposal of infectious waste, autoclave bags, pipettes, sharps and biological waste must be performed in accordance with Wisconsin Department of Natural Resources medical waste regulations. UW-Stout has developed procedures for the proper disposal of biological waste materials. Specific information on the disposal of biological materials and biological waste management is found in Appendix F. 8. Biohazardous spill cleanup 8.1. If a small or moderate spill (<100 mL) occurs inside the BSC: 8.1.1. Wear lab coat, safety goggles and gloves during cleanup. 8.1.2. Allow BSC to run during spill cleanup. 8.1.3. Apply disinfectant and allow a minimum of 30 minutes contact time. 8.1.4. Wipe up spillage with disposable disinfectant-soaked cloth. 8.1.5. Wipe the walls, work surface and any equipment in the cabinet with a disinfectantsoaked cloth. 8.1.6. Discard contaminated disposable materials in an appropriate autoclavable waste container(s) and autoclave before discarding. 14 8.1.7. Place contaminated reusable items in autoclave bags, autoclavable pans with lids or wrap in newspaper before autoclaving and cleanup. 8.1.8. Expose non-autoclavable materials to disinfectant for a minimum of 20 minutes of contact time before removal from the BSC. 8.1.9. Remove protective clothing used during cleanup and place in an autoclave bag for autoclaving. Wash hands whenever gloves are removed. 8.1.10. Allow the BSC to run for 10 minutes after cleanup before resuming work or turning cabinet off. 8.2. If a small or moderate spill (<100 mL) occurs in the lab, outside of the BSC: 8.2.1. Clear the area of all personnel. Wait for aerosol to settle before entering the spill area. The time required will depend on ventilation within the area but a general rule of thumb is to wait approximately 30 minutes. 8.2.2. Remove any contaminated clothing and place in an autoclave bag to be autoclaved. 8.2.3. Don a lab coat, safety goggles and gloves. 8.2.4. Soak paper towels in disinfectant and place over the spill. 8.2.5. Encircle the spill with additional disinfectant, being careful to minimize aerosolization while assuring adequate contact. 8.2.6. Decontaminate all items within the spill area. 8.2.7. Allow a minimum of 30 minutes of contact time to ensure germicidal action of disinfectant. 8.2.8. Wipe equipment with a 1:10 bleach solution, followed by water and 70% alcohol. 8.2.9. Place disposable contaminated spill materials in appropriate autoclavable container(s) for autoclaving. 8.2.10. Place contaminated reusable items in autoclave bags, autoclavable pans with lids or wrap in newspaper before autoclaving and cleanup. 8.2.11. Remove protective clothing used during cleanup and place in an autoclave bag for autoclaving. Wash hands whenever gloves are removed. 8.3. If a large spill (>100 mL) occurs inside or out of the BSC: 8.3.1. Evacuate the room, close the doors, prevent others from entering, and wait 30 minutes for aerosols to settle. 8.3.2. Follow procedures for small and moderate spills. If it is not safe for staff to perform the cleanup, call 911. 15 8.3.3. 8.4. 8.5. For large spills in the BSC, contact the BSO for assistance in determining if professional decontamination of the BSC is indicated. If a spill occurs outside of the lab, during transport: 8.4.1. Should a spill occur in a public area, do not attempt to clean it up without appropriate PPE (gloves, safety goggles, lab coat). 8.4.2. As an interim measure, wear gloves and place paper towels, preferably soaked in disinfectant, directly on spilled materials to prevent spread of contamination. To assure adequate contact, surround the spill with disinfectant, if available, taking care to minimize aerosols. 8.4.3. Call 911 to report the spill and request outside assistance. Also call the BSO and/or Safety and Risk Management for assistance in managing the situation. If a centrifuge tube breaks while the centrifuge is running: 8.5.1. Turn off the motor. Allow the machine to be at rest for 30 minutes before opening. Or, if breakage is discovered after the machine has stopped, re-close the lid immediately and allow the unit to be at rest for 30 minutes. 8.5.2. Unplug the centrifuge before initiating clean-up. 8.5.3. Don strong, thick rubber gloves, safety goggles and a lab coat. 8.5.4. Flood the centrifuge bowl with a germicidal disinfectant. Place paper towels soaked in a disinfectant over the entire spill area. Allow a minimum of 30 minutes of contact time. 8.5.5. Use mechanical means (such as forceps) to remove broken tubes and glass fragments. Place them in a sharps container for autoclaving and disposal as infectious waste. 8.5.6. Remove buckets, trunnions and the rotor and place in disinfectant for 24 hours or autoclave. Place paper towels soaked in a disinfectant over the equipment if transport is necessary. 8.5.7. Unbroken, capped tubes may be placed in disinfectant and recovered after 30 minute contact time or autoclaved. 8.5.8. Use mechanical means to remove remaining disinfectant soaked materials from centrifuge bowl and discard as infectious waste. 8.5.9. Place paper towels soaked in a disinfectant in the centrifuge bowl and allow it to soak overnight, wipe down again with disinfectant, wash with water and dry. Discard disinfectant soaked materials as infectious waste. 8.5.10. Remove protective clothing used during cleanup and place in a biohazard bag for autoclaving. Wash hands whenever gloves are removed. 9. Transportation and shipping of infectious agents 16 9.1. All shippers of hazardous materials (biological, chemical, radioisotopes) must have documented, U.S. Department of Transportation-mandated training. There are significant fines associated with improper packaging and shipping of hazardous materials. Please contact Safety and Risk Management for further information. 9.2. Regulations on the transportation of biological agents are aimed at ensuring that the public and the workers in the transportation chain are protected from exposure to any agent that might be in the package. Protection is achieved through (a) the requirements for rigorous packaging that will withstand rough handling and contain all liquid material within the package without leakage to the outside, (b) appropriate labeling of the package with the biohazard symbol and other labels to alert the workers in the transportation chain to the hazardous contents of the package, (c) documentation of the hazardous contents of the package should such information be necessary in an emergency situation, and d) training of workers in the transportation chain to familiarize them with the hazardous contents so as to be able to respond to emergency situations. 9.3. For transportation within and between buildings on campus biohazardous materials need to be packaged in a sealed, leak-proof primary container that is securely positioned in a secondary leak-proof and closable container (e.g. cooler, ice chest) containing a clearly visible biohazard symbol on the outside. Please contact Safety and Risk Management regarding the transport of biohazardous materials over public highways utilizing a state of Wisconsin vehicle. The use of private vehicles for the transportation of such materials on or off campus is prohibited. 9.4. Receiving and sending animals, animal-derived materials, infectious or biohazardous agents, biological toxins, and genetically modified organisms require the approval of federal agencies such as the CDC, the U.S. Department of Agriculture (USDA), or the U.S. Fish and Wildlife Service. Regulations that govern the transfer of biological materials help to minimize or eliminate the possible threats to public health and agriculture. Current resources regarding the transportation of infectious substances are found in Appendix C of the BMBL. 10. Select agents (Health and Human Services and US Department of Agriculture) 10.1. The U.S. Department of Health and Human Services (HHS) and the USDA have developed a list of select biological agents and toxins that have the potential to pose a severe biosecurity threat to public health, animals, and agricultural crops. A list of those materials currently classified as a select agent is on a joint USDA Animal and Plant Health Inspection Service (APHIS)/CDC website (http://www.selectagents.gov) and in Appendix G. HHS and USDA have adopted strict regulations for the obtaining, possession, use, or transfer of any of these selected agents. Failure to comply with the established regulations can result in significant civil and criminal penalties. Therefore, any plans for obtaining such materials must approved by the Biosafety Subcommittee well in advance of any planned use. Anyone contemplating select agent use should understand that a decision to do so means accepting a significant level of personal responsibility for meeting all aspects of the requirements mandated by the federal rules. At the time this manual was developed there were no select agents on campus. 10.2. HHS regulations in 42 CFR Part 73 and the companion USDA regulations in 7 CFR Part 331 and 9 CFR Part 121 require federal registration and a security risk assessment; safe handling; provisions for securing the agents against unauthorized access, theft, loss or release; and 17 restricted laboratory access. 11. Controlled substances (Drug Enforcement Agency) 11.1. A controlled substance is a drug that is regulated by state and federal laws that aim to control the danger of addiction, abuse, harm and illegal trafficking. They may be illegal for sale or use, but can be permitted for legitimate use in research. 11.2. When planning for research that involves drugs, the PI shall identify whether the drug is a controlled substance and act accordingly. The U.S. Drug Enforcement Agency (DEA) publishes schedules of controlled substances: http://www.deadiversion.usdoj.gov/schedules/. 11.3. The use of controlled substances for research requires obtaining both state (Wisconsin Controlled Substances Board Special Use Authorization) and federal (DEA) registration. The state registration must be obtained first. Penalties for using controlled substances without proper registration can be severe. The regulations strictly limit who can handle or administer the drugs and imposes physical security and inventory requirements. 11.4. The permitting process is between and individual researcher and the state and DEA. Registrants cannot share controlled substances with non-registered users who are not under their supervision. 11.5. Possession of expired substances can bring additional scrutiny from the U.S. Department of Agriculture since administration of expired substances is not allowed. 11.6. Disposal is strictly regulated by the DEA. 11.7. Neither the BSO nor Safety and Risk Management play a role in the permitting process, although the BSO can provide limited guidance. 11.8. The UW-Madison Research Animal Resources Center has very good guidance on the use of controlled substances: https://www.rarc.wisc.edu/documents/printable_lab_notebook.pdf. 12. Forbidden agents 12.1. UW-Stout policy prohibits the use or possession of RG3 or RG4 organisms on campus or at any off-campus locations. The only exclusion to this policy is reference material necessary for identification purposes. Reference material must be labeled as such and stored in an inactive state, either frozen or lyophilized. All freezers and storage cabinets must be clearly labeled with signs that include the biohazard symbol, the name of the organism, and emergency contact information. A list of all such viable reference material must be provided to the Biosafety Subcommittee. 18 APPENDIX A KEY CONTACTS Position Research Safety Committee Co-Chair Chemical Hygiene Officer, Research Safety Committee Co-Chair Biological Safety Officer Executive Director, Health and Safety Research Administrator IACUC Administrative Assistant Institutional Review Board (Human Subjects) University Police Name John Kirk Rebecca Hoeft Phone number 232-2209 232-2151 Jim Burritt Jim Uhlir Elizabeth Buchanan Landon Kafka 232-5048 232-2188 232-2477 232-1126 232-1126 232-2222 19 APPENDIX B PROJECT REGISTRATION AND APPROVAL University Researchers are required to obtain Biosafety Subcommittee of the Research Safety Committee (RSC) review and approval for work involving: Recombinant or synthetic nucleic acid molecules. All work must be registered with the Biosafety Subcommittee. Submit: “Registration Cover Sheet for All Recombinant or Synthetic Nucleic Acid Molecule Research” and “Recombinant or Synthetic Nucleic Acid Molecule Registration Form” (either exempt or non-exempt) (see Appendix C). Infectious Biological Agents (organisms in Risk Group 2 or above). This includes a broad spectrum of organisms able to cause human disease. Submit: “Biological Agent Registration Form” (see Appendix C). Biologically Derived Toxins. Examples include endotoxins, staphlococcus, entertoxins, saxitoxin, cholera toxin, botulinum toxin, etc. Submit: “Biological Toxin Registration Form” (see Appendix C). To initiate the review process, University researchers must submit a Biosafety Subcommittee registration form. Forms are in Appendix C. Project protocols that include the following items must accompany the completed form: Identification of potential hazards during sample preparation and experimental manipulations (e.g. aerosol generation, use of sharps, excretion of animals). Staff training and investigator experience. Safety procedures that will be employed to minimize risks and prevent release (e.g. protective clothing, use of biological safety cabinets, sharps disposal). Accidental spill and/or exposure procedures specific to the project. Send the documents to the BSO, who will process the forms for Biosafety Subcommittee review. The principal investigator will be invited to attend the review to summarize the project and answer questions. The Biosafety Subcommittee and/or RSC may request modification of the procedures or request that the BSO inspect labs or other facilities before granting approval. A copy of the approved form will be sent to the principal investigator. 20 APPENDIX C PROJECT REGISTRATION FORMS AND SIGNS 21 UNIVERSITY OF WISCONSIN – STOUT RESEARCH SAFETY COMMITTEE REGISTRATION COVER SHEET FOR ALL RECOMBINANT OR SYNTHETIC NUCLEIC ACID MOLECULE RESEARCH Principal Investigator: Project Title: Click here to enter text. Click here to enter text. PROTOCOL # Click here to enter text. APPROVAL – SUBCOMMITTEE APPROVAL – FULL COMMITTEE Click here to enter text. WITH MODIFICATION Click here to enter text. Department: Click here to enter text. Click here to enter text. UW-Stout adheres to the NIH Guidelines for Research Involving Recombinant or Synthetic Nucleic Acid Molecules (http://oba.od.nih.gov/rdna/nih_guidelines_oba.html) with regard to all uses of recombinant or synthetic nucleic acid molecules. Experiments involving recombinant or synthetic nucleic acid molecules are divided into six classes listed below; it is the responsibility of the PI to read the NIH Guidelines in order to determine which class is applicable to the work. UW-Stout requires that all recombinant or synthetic nucleic acid molecule work done at the University be registered with the Research Safety Committee EVEN IF IT IS EXEMPT from the NIH Guidelines. Registration is accomplished by completion of this cover sheet and the appropriate registration form for either exempt or non-exempt research. III-F. Experiments that are exempt from the NIH Guidelines. ☐ Those synthetic nucleic acids that (1) can neither replicate nor generate nucleic acids that can replicate in any living cell, and (2) are not designed to integrate into DNA, and (3) do not produce a toxin that is lethal for vertebrates at an LD 50 of less than 100 nanograms/kilogram body weight. ☐ Those that are not in organisms, cells or viruses and that have not been modified or manipulated to render them capable of penetrating cellular membranes. ☐ Those that consist solely of the exact recombinant or synthetic nucleic acid sequence from a single source that exists contemporaneously in nature. ☐ Those that consist entirely of nucleic acids from a prokaryotic host, including its indigenous plasmids or viruses when propagated only in that host (or a closely related strain of the same species), or when transferred to another host by well-established physiological means. ☐ Those that consist entirely of nucleic acids from a eukaryotic host including its chloroplasts, mitochondria or plasmids (but excluding viruses) when propagated only in that host (or a closely related strain of the same species). ☐ Those that consist entirely of DNA segments from different species that exchange DNA by known physiological processes, though one or more of the segments may be a synthetic equivalent. ☐ Those genomic DNA molecules that have acquired a transposable element, provided the transposable element does not contain any recombinant and/or synthetic DNA. ☐ Those that do not present a significant risk to health or the environment, as determined by the NIH Director. III-E. Experiments that require RSC registration simultaneous with initiation. ☐ Those involving the formation of recombinant or synthetic nucleic acid molecules containing no more than two-thirds of the genome of any eukaryotic virus. ☐ Those involving recombinant or synthetic nucleic acid molecule-modified whole plants, and/or those involving recombinant or synthetic nucleic acid molecule-modified organisms associated with whole plants. ☐ Those involving transgenic rodents. III-D. Experiments that require RSC approval before initiation. ☐ Those using RG2 (or higher) or restricted agents as host-vector systems. ☐ Those in which DNA from RG2 (or higher) or restricted agents is cloned into nonpathogenic prokaryotic or lower eukaryotic hostvector systems. ☐ Those involving the use of infectious/defective DNA/RNA viruses in the presence of helper virus tissue culture systems. ☐ Those involving whole animals. ☐ Those to genetically engineer plants by recombinant or synthetic nucleic acid molecule methods, to use such plants for other experimental purposes, to propagate such plants, or to use plants together with microorganisms or insects containing recombinant or synthetic nucleic acid molecules. ☐ Those involving more than 10 liters of culture. ☐ Those involving influenza viruses. III-C. Experiments that require RSC and IRB approvals and NIH RAC review before participant enrollment. ☐ Those involving the deliberate transfer of recombinant or synthetic nucleic acid molecules, or DNA/RNA derived from recombinant or synthetic nucleic acid molecules, into one or more human research participants. III-B. Experiments that require NIH/OBA and RSC approval before initiation. ☐ Those involving the cloning of toxin molecules with LD50 of less than 100 nanograms/kilogram body weight. III-A. Experiments that require RSC approval, NIH RAC review and NIH Director approval before initiation. ☐ Those considered as Major Actions under the NIH Guidelines. Oct 13 UNIVERSITY OF WISCONSIN – STOUT RESEARCH SAFETY COMMITTEE PROTOCOL # Click here to enter text. REVIEW – SUBCOMMITTEE Click here to enter text. WITH MODIFICATION Click here to enter text. REGISTRATION FORM FOR EXEMPT RESEARCH RECOMBINANT OR SYNTHETIC NUCLEIC ACID MOLECULES Principal Investigator: Campus Mailing Address: ☐New Submission Project Title: Funding Agency: Phone No.: Click here to enter text. E-mail: Click here to enter text. ☐Grant Renewal of RSC# Click here to ☐Revision/Resubmission of RSC#Click here to Click here to enter text. Click here to enter text. enter text. Click here to enter text. Click here to enter text. enter text. Project Dates: Click here to enter text. to Click here to enter text. 1. Attach a project summary describing your research in such a way that a scientist from another field will understand. 2. Location. Provide information regarding the research facilities and type of use. Building Room No. Type of Use (e.g. Procedure room, animal housing, cold room) Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 3. Assurance by Principal Investigator. Electronic submission of this form from the principal investigator’s UW-Stout email address confirms his/her agreement that all work on this project will be conducted according to the National Institutes of Health (NIH) "Guidelines for Research Involving Recombinant or Synthetic Nucleic Acid Molecules" and using Biosafety Level 1 practices as described in the most current version of the Centers for Disease Control and Prevention/NIH publication entitled "Biosafety in Microbiological and Biomedical Laboratories." Additional stipulations required by the Research Safety Committee on behalf of UW-Stout will also be followed. Date of submission: Click here to enter a date. Save an electronic copy of this completed form and submit it to burrittj@uwstout.edu along with required attachments (including the Registration Cover Sheet). The email must come from the principal investigator’s/instructor’s UW-Stout email address. You will receive an email within 2-3 days acknowledging receipt of your submission. Oct 13 UNIVERSITY OF WISCONSIN – STOUT RESEARCH SAFETY COMMITTEE REGISTRATION FORM FOR NON-EXEMPT RESEARCH RECOMBINANT OR SYNTHETIC NUCLEIC ACID MOLECULES Principal Investigator: Campus Mailing Address: ☐New Submission Click here to enter text. APPROVAL – SUBCOMMITTEE APPROVAL – FULL COMMITTEE Click here to enter text. WITH MODIFICATION Click here to enter text. Click here to enter text. Phone No.: Click here to enter text. E-mail: Click here to enter text. ☐Grant Renewal of RSC# Click here to ☐Revision/Resubmission of RSC#Click here to Click here to enter text. Click here to enter text. enter text. Click here to enter text. Click here to enter text. Project Title: Funding Agency: PROTOCOL # enter text. Project Dates: Click here to enter text. to Click here to enter text. 1. Attach a project summary describing your research in such a way that a scientist from another field will understand. 2. Recombinant or Synthetic Nucleic Acid Molecules Source(s) (Gene, species, strain) Name (Spell out acronyms) Name of Insert or Protein Expressed Use on Construct (e.g. toxin, marker train, virulence factor, DNA repair gene, oncogene, transcription factor) (Cloning for sequencing; PCR expression in a microbe; expression in Organ, Tissue or Cell Culture; expression assoc. w/ organism) Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 3. Vector Description(s). Attach a construct map if available. Please indicate any regions that increase the safety of this construct. Gene Transfer Method (e.g. conjugation, liposome, viral, infection, electroporation, CaPO4, polyplexes, naked DNA uptake) Vector Backbone Source (e.g. bacterial plasmid, cosmid, phage, virus synthetic, transposition, YAC, BAC) Risk Attenuation Vector Technical Name (Include commercial vendor if applicable) (Replication defective? Helper dependent? Disarmed? K-12 derivative? Restricted to prokaryotic expression?) Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 4. Toxic Molecules. Do the DNA clones contain genes for the biosynthesis of toxic molecules lethal for vertebrates? ☐Yes Oct 13 ☐No If yes, provide LD50 information: Click here to enter text. UW-Stout Registration Form for Non-Exempt Research 5. Scale. Does an individual experiment involve more than 10 liters of culture? ☐Yes ☐No 6. Location. Please provide information regarding the research facilities, type of use and the biosafety level (BSL-1 or BSL-2) that will be used during this project. Building Room No. Type of Use (e.g. procedure room, animal housing, cold room) Biosafety Level Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 7. Provide laboratory protocols specific to this research. Be sure to include the following: a. Identification of potential exposure hazards during sample preparation and experimental manipulations (e.g. aerosol generation when transferring, mixing or centrifuging; use of sharps; excretion by animals). b. Staff training. c. Safety procedures that will be employed to minimize risk and prevent release of the agent (e.g. protective clothing, use of biological safety cabinet, sharps handling and disposal) d. Accidental spill/exposure procedures. 8. Research Personnel. Identify personnel conducting the experiments (including students). Specify degree, applicable training and experience including duration, and project responsibilities. Name Degree Training/Experience Project Responsibilities Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 9. Assurance by Principal Investigator. Electronic submission of this form from the principal investigator’s UW-Stout email address confirms his/her agreement that all work on this project will be conducted according to the National Institutes of Health (NIH) "Guidelines for Research Involving Recombinant or Synthetic Nucleic Acid Molecules" and using appropriate biosafety practices as described in the most current version of the Centers for Disease Control and Prevention/NIH publication entitled "Biosafety in Microbiological and Biomedical Laboratories." Additional stipulations required by the Research Safety Committee on behalf of UW-Stout will also be followed. Date of submission: Click here to enter a date. Save an electronic copy of this completed form and submit it to glenztr@uwstout.edu and burrittj@uwstout.edu along with required attachments (including the Registration Cover Sheet). The email must come from the principal investigator’s/instructor’s UW-Stout email address. You will receive an email within 2-3 days acknowledging receipt of your submission. Oct 13 UW-Stout Registration Form for Non-Exempt Research UNIVERSITY OF WISCONSIN – STOUT RESEARCH SAFETY COMMITTEE BIOLOGICAL AGENT REGISTRATION FORM PROTOCOL # Click here to enter text. APPROVAL – SUBCOMMITTEE APPROVAL – FULL COMMITTEE Click here to enter text. WITH MODIFICATION Click here to enter text. Click here to enter text. Principal Investigator/Instructor: Phone No.: Click here to enter text. Click here to enter text. Campus Mailing Address: Click here to enter text. E-mail: Click here to enter text. ☐New Submission ☐Grant Renewal of RSC# Click here to ☐Revision/Resubmission of RSC#Click here to enter text. enter text. Project Title/Course Number: Click here to enter text. Funding Agency: Click here to enter text. Project/Course Dates: Click here to enter text. to Click here to enter text. 1. Attach a project summary describing your research or instruction in such a way that a scientist from another field will understand. Include in detail all methods that will be used that are directly involved with the biological agent, including the experimental/instructional design and goals, the source of the agent, assessment of the biohazardous potential and containment methods. 2. Biological Agents. Identify the agent(s), biosafety level and check the applicable categories*. Microorganism Biosafety Level (Gene, species, strain) Human Pathogen* Animal Pathogen* Plant Pathogen* Click here to enter text. Choose an item. ☐ ☐ ☐ Click here to enter text. Choose an item. ☐ ☐ ☐ Click here to enter text. Choose an item. ☐ ☐ ☐ 3. Source. How will the agent be acquired? ☐Laboratory stock ☐Off-campus collection ☐Directly from animal/plant tissues ☐Off-campus researcher ☐Other (describe): Click here to enter text. 4. Storage. How will the agent be maintained? ☐Lypholized ☐Chemical-fixation ☐Frozen ☐Refrigerated ☐Incubator ☐Room Temperature ☐Other (describe): Click here to enter text. 5. Location. Where will experiments be performed? Building and room number: Click here to enter text. 6. Animals. Does the experiment involve infection of animals? All research involving animals must also be submitted to the IACUC. If yes, can the organism be released from the animal to the environment? 7. Scale. Does an individual experiment involve more than one liter of culture? Oct 13 ☐Yes ☐No ☐Yes ☐No ☐Yes ☐No UW-Stout Biological Agent Registration Form 8. Safety Equipment. Identify equipment to be used. Biosafety cabinet? ☐Yes Autoclave available? ☐No ☐Yes ☐No Model: Click here to enter text. Location: Click here to enter text. Location: Click here to enter text. Monitored? ☐Yes ☐No Certification date: Click here to enter text. 9. Disposal. How are the compound and/or other materials containing biological agents (e.g. animal excrement, blood, bedding, carcasses) inactivated or disposed of? If a chemical disinfectant is used, state the type and concentration. Material to be Disposed Of Method/Procedure for Inactivation/Disposal Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 10. Provide laboratory protocols specific to this research/instruction. Be sure to include the following: a. Identification of potential exposure hazards during sample preparation and experimental manipulations (e.g. aerosol generation when transferring, mixing or centrifuging; use of sharps; excretion by animals). b. Staff and/or student training. c. Safety procedures that will be employed to minimize risk and prevent release of the agent (e.g. protective clothing, use of biological safety cabinet, sharps handling and disposal). d. Accidental spill/exposure procedures. Include information on vaccines available and their recommended use for persons handling the agent. 11. Research/Instruction Personnel. Identify personnel conducting the experiments or assisting with the instruction (including students). Specify degree, applicable training and experience including duration, and project responsibilities. Name Click here to enter text. Click here to enter text. Click here to enter text. Degree Click here to enter text. Click here to enter text. Click here to enter text. Training/Experience Project Responsibilities Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 12. Assurance by Principal Investigator/Instructor. Electronic submission of this form from the principal investigator’s/instructor’s UW-Stout email address confirms his/her agreement to perform all work using appropriate biosafety practices as described in the most current version of the Centers for Disease Control and Prevention/NIH publication entitled "Biosafety in Microbiological and Biomedical Laboratories." Additional stipulations required by the Research Safety Committee on behalf of UW-Stout will also be followed. Date of submission: Click here to enter a date. Save an electronic copy of this completed form and submit it to glenztr@uwstout.edu and burrittj@uwstout.edu along with required attachments. The email must come from the principal investigator’s/instructor’s UW-Stout email address. You will receive an email within 2-3 days acknowledging receipt of your submission. Oct 13 UW-Stout Biological Agent Registration Form UNIVERSITY OF WISCONSIN – STOUT RESEARCH SAFETY COMMITTEE BIOLOGICAL TOXIN REGISTRATION FORM PROTOCOL # Click here to enter text. APPROVAL – SUBCOMMITTEE APPROVAL – FULL COMMITTEE Click here to enter text. WITH MODIFICATION Click here to enter text. Click here to enter text. Principal Investigator/Instructor: Phone No.: Click here to enter text. Click here to enter text. Campus Mailing Address: Click here to enter text. E-mail: Click here to enter text. ☐New Submission ☐Grant Renewal of RSC# Click here to ☐Revision/Resubmission of RSC#Click here to enter text. Project Title/Course Number: Click here to enter text. Funding Agency: Click here to enter text. enter text. Project/Course Dates: Click here to enter text. to Click here to enter text. 1. Attach a project summary describing your research or instruction in such a way that a scientist from another field will understand. Include in detail all methods that will be used in the project that are directly involved with the biological toxin, including the experimental/instructional design and goals, the source of the agent, assessment of the biohazardous potential and containment methods. 2. Biological Toxins. Identify the toxin(s), biosafety level, LD50 and source of the LD50 data (e.g. mouse, rat). Biological Toxin Biosafety Level LD50 LD50 Source Click here to enter text. Choose an item. Click here to enter text. Click here to enter text. Click here to enter text. Choose an item. Click here to enter text. Click here to enter text. Click here to enter text. Choose an item. Click here to enter text. Click here to enter text. 3. Quantity. What quantity of the biotoxin will be kept on hand? Please note method used to inventory or account for quantity. Describe: Click here to enter text. 4. Security. How will the security of the toxin be maintained? ☐Locked cabinet ☐Locked refrigerator/freezer ☐Other (describe): Click here to enter text. 5. Location. Provide information regarding the facilities where the biotoxin will be produced, stored and/or used in experiments. Building Room No. Produced, Stored, and/or Used for Experiments? Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 6. Animals. Does the experiment involve infection of animals? If yes, can the organism be released from the animal to the environment? ☐Yes ☐Yes ☐No ☐No All research involving animals must also be submitted to the IACUC. Oct 13 UW-Stout Biological Toxin Registration Form 7. Safety Equipment. Identify equipment to be used. Biosafety cabinet? ☐Yes Autoclave available? ☐No ☐Yes ☐No Model: Click here to enter text. Location: Click here to enter text. Location: Click here to enter text. Monitored? ☐Yes ☐No Certification date: Click here to enter text. 8. Disposal. How are the compound and/or other materials containing biotoxins (e.g. animal excrement, blood, bedding, carcasses) inactivated or disposed of? If a chemical disinfectant is used, state the type and concentration. Material to be Disposed Of Method/Procedure for Inactivation/Disposal Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 9. Provide laboratory protocols specific to this research. Be sure to include the following: a. Identification of potential exposure hazards during sample preparation and experimental manipulations (e.g. aerosol generation when transferring, mixing or centrifuging; use of sharps; excretion by animals). b. Staff training. c. Safety procedures that will be employed to minimize risk and prevent release of the toxin (e.g. protective clothing, use of biological safety cabinet, sharps handling and disposal) d. Accidental spill/exposure procedures. Include information on the availability of antidotes for persons exposed to the toxin. 10. Research Personnel. Identify personnel conducting the experiments (including students). Specify degree, applicable training and experience including duration, and project responsibilities. Name Degree Training/Experience Project Responsibilities Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. 11. Assurance by Principal Investigator/Instructor. Electronic submission of this form from the principal investigator’s/instructor’s UW-Stout email address confirms his/her agreement to perform all work using appropriate biosafety practices as described in the most current version of the Centers for Disease Control and Prevention/NIH publication entitled "Biosafety in Microbiological and Biomedical Laboratories." Additional stipulations required by the Research Safety Committee on behalf of UW-Stout will also be followed. Date of submission: Click here to enter a date. Save an electronic copy of this completed form and submit it to glenztr@uwstout.edu and burrittj@uwstout.edu along with required attachments. The email must come from the principal investigator’s/instructor’s UW-Stout email address. You will receive an email within 2-3 days acknowledging receipt of your submission. Oct 13 UW-Stout Biological Toxin Registration Form BIOSAFETY 1 Standard Microbiological Practices Apply LEVEL Biohazardous material(s): Click here to enter text. Notice Call or See Building Room Entry or Information Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Emergency Emergency Building: Click here to enter text. Campus Phone Emergency Phone Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Room: Click here to enter text. Date posted: Click here to enter a date. Additional copies of this sign available from the UW-Stout Laboratory Safety intranet website: https://www.uwstout.edu/healthandsafety/safety/intranet/laboratory-safety.cfm BIOSAFETY Limited Access LEVEL For work with: Biohazardous material(s) Procedure required for entry/exit (e.g. PPE) Special practices (e.g. use of BSC, immunizations) Click here to enter text. Click here to enter text. Click here to enter text. Notice Call or See Building Room Entry or Information Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Emergency Emergency Building: Click here to enter text. 2 Room: Click here to enter text. Campus Phone Emergency Phone Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Click here to enter text. Date posted: Click here to enter a date. Additional copies of this sign available from the UW-Stout Laboratory Safety intranet website: https://www.uwstout.edu/healthandsafety/safety/intranet/laboratory-safety.cfm APPENDIX D STANDARD PRACTICES AND PROCEDURES Autoclave procedures and safety 1. All users must undergo and document training for operation of the autoclave. 2. Studies have shown that the processing time necessary to achieve decontamination of biological material depends on load size, type of container, and moisture content. A 60 minute autoclave cycle (excluding exhaust time) is recommended to allow enough time for the center of the load to come up to temperature and have sufficient steam penetration. This will insure that the temperature in ALL parts of the load has reached 121°C (250°F) for at least 20 minutes. 3. In order to standardize the autoclaving of wastes and to assure that all loads, regardless of size or content, are properly decontaminated, the following procedures must be followed. a. Place materials in an autoclavable container. Plastics must be labeled as autoclavable or they may melt. i. Autoclave bags should be loosely packed and not more than 3/4 full. Add water to a bag if the load is dry. Do not seal the bag shut; steam must be able to penetrate the bag to decontaminate the contents. If using the supplied rubber bands place on loosely, do not twist. ii. The caps or lids on containers of liquids should be loosened to avoid dangerous pressure build-up and possible explosion. iii. Do not put sharp or pointed contaminated objects directly into an autoclave bag. Place them in an appropriate rigid disposal container (such as a sharps container) first. b. Use autoclave indicator tape as a check that the correct temperature has been reached. To validate adequate steam penetration to the center of a load, tape can be buried in the load. Tape does not prove decontamination effectiveness; see “Autoclave testing” below. c. Load the autoclave according to the manufacturer’s instructions. i. Place containers in a tray and load the tray into the autoclave; this is easier to load and unload and will catch spills. Do not place items directly on the autoclave chamber floor. ii. Do not overload the autoclave; an over-packed autoclave chamber does not allow sufficient steam distribution. Be sure there is ample room between bags so steam circulation is not impaired. d. Autoclave at 121°C for 45-60 minutes. e. After autoclaving, any bag displaying the biohazard symbol should be placed in a nontransparent plastic bag or other secondary non-transparent container (e.g. closed cardboard box, dark colored trash bag) prior to disposal into the normal trash. Bags with 32 the biohazard symbol, regardless of use, must not be placed into the regular waste stream without defacing the symbol or over-bagging. f. Autoclaved liquid culture waste can be sewered unless hazardous chemical waste is present, in which case it must be disposed of in accordance with hazardous waste regulations. Do not sewer melted agar as it will congeal and clog plumbing. 4. Autoclave testing: All autoclaves used for waste decontamination should be regularly tested for effectiveness. Autoclave indicator tape is used to verify that an adequate temperature was reached during the autoclaving cycle, but it does not prove decontamination effectiveness. a. Integrator strips (e.g. B. stearothermophilus spore strips) provide immediate test results. The spores, which can survive 121ºC for five minutes but are killed at 121ºC in 13 minutes, are more resistant to heat than most, thereby providing an adequate safety margin when validating decontamination procedures. Each type of container employed should be individually tested with these spores because efficacy varies with the load, fluid volume, etc. i. Attach the indicator strip to a stick or string and put in the center of the load and place strips at locations throughout the autoclave. ii. Retrieve after autoclaving for confirmation that the entire load has been exposed to the conditions necessary for decontamination. iii. If the indicator reads unsafe, autoclave again. b. An autoclave testing log must be kept for two years. 5. Personal safety precautions: a. Do not autoclave materials containing solvents, volatile or corrosive chemicals (such as phenol, chloroform, bleach, etc.) or radioactive materials. b. When unloading an autoclave, wear heat resistant gloves, eye protection, and lab coat. c. To prevent steam burns, make sure that the autoclave pressure is near zero before opening the door. d. Allow steam to escape gradually by slowly cracking open the autoclave door. Allow load to cool for 10 minutes before removing. e. Do not autoclave sealed containers or full bottles with narrow necks as they may explode. Biological safety cabinets (BSCs) 1. BSCs are often referred to as “tissue culture hoods” or “laminar flow hoods.” “Biological safety cabinet” is the correct term. All BSCs use high efficiency particulate air (HEPA) filters to treat exhaust air. a. Class I and II cabinets are designed for work involving low to moderate risk biological 33 agents (BSL-1, BSL-2 and BSL-3). Class I cabinets provide worker and environmental protection, but no product protection, while Class II cabinets provide worker, environmental and product protection. Class III cabinets are fully enclosed and are used for work with high risk biological agents (BSL-4). b. All BSCs in Jarvis Science Addition are Class II, Type A2; they recirculate 70% of the air and exhaust 30% and provide intake air velocity of 100 feet per minute. Both room air and interior cabinet air are drawn into a front grille creating an air barrier that provides personnel protection. In addition, downward laminar flow of HEPA-filtered air provides product protection. Air exhaust passes through a certified exhaust HEPA filter and may be recirculated back into the laboratory or exhausted out of the building, providing environmental protection. All UW-Stout BSCs exhaust back into the laboratory and therefore cannot be used for applications involving volatile chemicals, cytotoxic drugs or radionuclides. 2. Laminar flow clean benches are not BSCs and they offer no worker or environmental protection. Clean benches must never be substituted for BSCs. Air is discharged across the work surface to protect product on the bench from contamination, but the worker is exposed to whatever is being used on the bench. Clean benches should not be used for work involving cell cultures, toxins, volatile chemicals, infectious materials or materials that may cause hypersensitivity to the worker (e.g. animal dander). 3. To ensure safe use: a. Make sure the BSC is certified when it is installed or after it is moved, and annually thereafter (there is a sticker on the front of the BSC indicating when it was last certified). Do not use a BSC that is marked or signed as “Failed.” Check the blower gauge or LCD screen regularly for an indication of a problem. b. Do not disrupt the protective airflow pattern of the BSC. Rapidly moving your arms in and out of the cabinet, people walking rapidly behind you, and open lab doors may disrupt the airflow pattern and reduce the effectiveness of the BSC. c. Only one person at a time should work in the BSC to minimize air disturbance. d. Minimize the storage of materials in and around the BSC. e. It is not necessary to flame items in the near microbe-free environment of a BSC. This creates turbulence in airflow and will compromise sterility; heat buildup may damage the filters. See Appendix A of the BMBL; the CDC instead recommends, when deemed necessary, touch-plate micro burners equipped with a pilot light to provide a flame on demand, small electric furnaces for decontamination of bacteriological loops and needles, or disposable or recyclable sterile loops. Alcohol lamps should not be used in BSCs. 4. Operational directions: a. Remove all unnecessary equipment and supplies from the cabinet; clutter alters air flow. Do not place objects over the front air intake grille or block the rear exhaust grille. 34 b. Plan your experiment. Gather all required materials, think through the steps and lay out materials in a logical manner that will prevent excessive movements while the BSC is in use. c. Turn on the blower at least 15 minutes before starting work to remove particulates in the cabinet. d. Before using, wipe work surfaces with an appropriate disinfectant. Wipe off each item you need for your procedures with the disinfectant and place in cabinet. e. Place a pan with disinfectant and/or a sharps container inside the BSC for pipette discard. Collect waste materials inside the cabinet to avoid excessive movement inside and outside the BSC. Do not use vertical pipette discard canisters on the floor outside cabinet. Be sure to seal bags and cover open containers before removing them from them from the BSC. f. Delay work for approximately one minute after placing hands/arms inside the cabinet. Do not rest arms on the front grille; raising arms slightly will lessen disruption of air flow. g. Work as far back in the cabinet as practical (at least four inches inside the front grille edge). h. Segregate contaminated and clean items; as a general rule of thumb, keep clean materials at least one foot away from aerosol-generating activities to minimize crosscontamination. Work from “clean” (left) to “dirty” (right). i. If you use a piece of equipment that creates air turbulence in the BSC (such as a centrifuge, blender) place equipment in the back third of the cabinet; stop other work while equipment is operating. j. Protect the building vacuum system from biohazards by placing a HEPA cartridge filter or its equivalent between the vacuum trap and the source valve in the cabinet. k. Clean up all spills in the cabinet immediately. Wait 10 minutes before resuming work. l. When work is finished, wipe down the surfaces of containers and equipment with an appropriate disinfectant and remove from the BSC. m. Leave the blower on for 15 minutes with no activity so that airborne contaminants are purged from the work area. n. Wipe all interior surfaces with disinfectant. o. Remove lab coat and gloves and wash hands thoroughly before leaving laboratory. Blenders, ultrasonic disrupters, grinders and lyophilizers 1. The use of any of these devices results in considerable aerosol production. Blenders, grinders and cell-disruption equipment should be used in a BSC when working with biohazardous materials. 2. Safety blenders, although expensive, are designed to prevent leakage from the bottom of the 35 blender jar, provide a cooling jacket to avoid biological inactivation and withstand sterilization by autoclaving. If blender rotors are not leak-proof, they should be tested with sterile saline or dye solution prior to use with biohazardous material. The use of glass blender jars is not recommended because of the breakage potential. If they must be used, glass jars should be covered with a polypropylene jar to prevent spraying of glass and contents in the event the blender jar breaks. A towel moistened with disinfectant should be placed over the top of the blender during use. Before opening the blender jar allow the unit to rest for at least one minute to allow the aerosol to settle. The device should be decontaminated promptly after use. 3. Depending on the lyophilizer design, aerosol production may occur when material is loaded or removed from the lyophilizer unit. If possible, sample material should be loaded in a BSC. The vacuum pump exhaust should be filtered to remove any hazardous agents or, alternatively, the pump can be vented into a BSC. After lyophilization is completed, all surfaces of the unit that have been exposed to the agent should be disinfected. If the lyophilizer is equipped with a removable chamber, it should be closed off and moved to a BSC for unloading and decontamination. Handling of cultures should be minimized and vapor traps should be used wherever possible. 4. Opening an ampoule containing liquid or lyophilized culture material should be performed in a BSC to control the aerosol produced. Gloves must be worn. a. To open, nick the neck of the ampoule with a file, wrap it in disinfectant soaked towel, hold the ampoule upright and snap it open at the nick. b. Reconstitute the contents of the ampoule by slowly adding liquid to avoid aerosolization of the dried material. c. Mix the contents without bubbling and withdraw it into a fresh container. d. Discard the towel and ampoule top and bottom as infectious waste. 5. Ampoules used to store biohazardous material in liquid nitrogen have exploded causing eye injuries. The use of polypropylene tubes eliminates this hazard. These tubes are available dustfree or pre-sterilized and are fitted with polyethylene caps with silicone washers. Heat sealable polypropylene tubes are also available. Bloodborne pathogens 1. All principal investigators using human or non-human primate blood or blood products, unfixed tissue, body fluids, or organ or cell cultures of human or non-human primate origin must follow the procedures outlined in the UW-Stout Bloodborne Pathogens Exposure Control Plan. 2. Bloodborne pathogens training is required for employees and students working with the abovelisted products and can be provided by Safety and Risk Management or numerous other online providers. Centrifuge equipment 1. Hazards associated with centrifuging include mechanical failure and the creation of aerosols. To minimize the risk of mechanical failure, centrifuges must be maintained and used according to 36 the manufacturer’s instructions. Users should be properly trained, and operating instructions that include safety precautions should be prominently posted on the unit. 2. Aerosols are created by practices such as filling centrifuge tubes, removing plugs or caps from tubes after centrifugation, removing supernatant, and re-suspending sedimented pellets. The greatest aerosol hazard is created if a tube breaks during centrifugation. To minimize the generation of aerosols when centrifuging biohazardous material, the following procedures should be followed: a. Use sealed tubes and safety buckets that seal with O-rings. Before use, inspect tubes, Orings and buckets for cracks, chips, erosions, bits of broken glass, etc. Do not use aluminum foil to cap centrifuge tubes because it may detach or rupture during centrifugation. b. Fill and open centrifuge tubes, rotors and accessories in a biological safety cabinet. Avoid overfilling of centrifuge tubes so that closures do not become wet. After tubes are filled and sealed, wipe them down with disinfectant. c. Add disinfectant to the space between the tube and the bucket to disinfect material in the event of breakage during centrifugation. d. Always balance buckets, tubes and rotors properly before centrifugation. e. Do not decant or pour off supernatant. Use a vacuum system with appropriate in-line reservoirs and filters. f. Work in a BSC when re-suspending sedimented material. Use a swirling rotary motion as necessary, wait a few minutes to permit the aerosol to settle before opening the tube. 3. Small low-speed centrifuges may be placed in a BSC during use to reduce the aerosol escape. High-speed centrifuges pose additional hazards. Precautions should be taken to filter the exhaust air from vacuum lines, to avoid metal fatigue resulting in disintegration of rotors and to use proper cleaning techniques and centrifuge components. Manufacturers’ recommendations must be meticulously followed to avoid metal fatigue, distortion and corrosion. 4. Avoid the use of celluloid (cellulose nitrate) tubes with biohazardous materials. Celluloid centrifuge tubes are highly flammable and prone to shrinkage with age. They distort on boiling and can be highly explosive in an autoclave. If celluloid tubes must be used, an appropriate chemical disinfectant must be used to disinfect them. Cryostats 1. Frozen sections of unfixed tissue infected with an etiologic agent pose a risk because accidents can occur. Freezing tissue does not necessarily inactivate infectious agents. Freezing propellants under pressure should not be used for frozen sections as they may cause spattering of droplets of infectious materials. Gloves should be worn during preparation of frozen sections. When working with biohazardous material in a cryostat, the following is recommended: a. Consider the contents of the cryostat to be contaminated and decontaminate it frequently with disinfectant. 37 b. Consider trimmings and sections of tissue that accumulate in the cryostat to be potentially infectious and remove them during decontamination. c. Defrost and decontaminate the cryostat with a tuberculocidal hospital disinfectant once a week and immediately after tissue known to contain bloodborne pathogens, M. tuberculosis or other infectious agents is cut. d. Handle microtome knives with extreme care. Stainless steel mesh gloves should be worn when changing knife blades. 2. Consider solutions for staining potentially infected frozen sections to be contaminated. Decontamination 1. Decontamination is a term used to describe a process or treatment that renders a medical device, instrument, or environmental surface safe to handle. A decontamination procedure can range from sterilization to simple cleaning with soap and water. Sterilization, disinfection and antisepsis are all forms of decontamination. a. Sterilization is the use of a physical or chemical procedure to destroy all microbial life, including highly resistant bacterial endospores. b. Disinfection eliminates virtually all pathogenic non-spore forming microorganisms but not necessarily all microbial forms on inanimate objects (e.g. work surfaces, equipment). Effectiveness is influenced by the kinds and numbers of organisms, the amount of organic matter, the object to be disinfected and chemical exposure time, temperature and concentration. c. Antisepsis is the application of a liquid antimicrobial chemical to skin or living tissue to inhibit or destroy microorganisms. It includes swabbing an injection site on a person or animal and hand washing with germicidal solutions. Although some chemicals may be utilized as either a disinfectant or an antiseptic, adequacy for one application does not guarantee adequacy for the other. Manufacturers’ recommendations for appropriate use of germicides should always be followed. 2. There are four main categories of physical and chemical means of decontamination. They are heat (wet, dry and incineration), liquid disinfection, vapors and gases, and radiation. Each category is discussed briefly below. a. Wet heat is the most dependable method of sterilization. Autoclaving (saturated steam under pressure of approximately 15 psi to achieve a chamber temperature of at least 121ºC for a prescribed time) is the most convenient method of rapidly achieving destruction of all forms of microbial life. In addition to proper temperature and time, prevention of entrapment of air is critical to achieving sterility. See “Autoclave procedures and safety” in this Appendix. b. Dry Heat is less efficient than wet heat and requires longer times and/or higher temperatures to achieve sterilization. It is suitable for the destruction of viable organisms on impermeable non-organic surfaces such as glass, but it is not reliable in the presence 38 of shallow layers of organic or inorganic materials that may act as insulation. Sterilization of glassware by dry heat can usually be accomplished at 160 - 170º C for periods of two to four hours. Dry heat sterilizers should be monitored on a regular basis using appropriate biological indicators (e.g. B. subtilis [globigii] spore strips). c. Incineration is another effective means of decontamination by heat. As a disposal method incineration has the advantage of reducing the volume of the material prior to its final disposal. d. Liquid disinfection is most practical for surface decontamination and, when used in sufficient concentration, as a decontaminate for liquid wastes prior to final disposal in the sanitary sewer. If liquid disinfectants are used, they must have been shown to be effective against the organism(s) present. Liquid disinfectants are available under a wide variety of trade names. In general, these can be classified as halogens, acids, alkalis, heavy metal salts, quaternary ammonium compounds, phenolic compounds, aldehydes, ketones, alcohols and amines. The more active a compound is, the more likely it is to have undesirable characteristics such as corrosivity. No liquid disinfectant is equally useful or effective under all conditions and for all viable agents. A 0.5% sodium hypochlorite solution (1:10 dilution of household bleach) is effective for decontamination of equipment and work surfaces. In locations where bleach would cause corrosion, an iodophor (e.g. Wescodyne) should be used. e. Vapors and gases are primarily used to decontaminate BSCs and associated systems, bulky or stationary equipment not suited to liquid disinfectants, instruments or optics that might be damaged by other decontamination methods, and rooms, buildings and associated air-handling systems. Agents included in this category are glutaraldehyde and formaldehyde vapor, ethylene oxide gas, peracetic acid and hydrogen peroxide vapor. When used in closed systems and under controlled conditions of temperature and humidity, excellent disinfection can be obtained. Great care must be taken during use because of the hazardous nature of many of these compounds. Contact Safety and Risk Management for monitoring requirements if these compounds are to be used. f. Although ionizing radiation will destroy microorganisms, it is not a practical tool for laboratory use. Non-ionizing radiation in the form of ultraviolet (UV) radiation is used for inactivating viruses, bacteria and fungi. It will destroy airborne microorganisms and inactivate microorganisms on exposed surfaces or in the presence of products of unstable composition that cannot be treated by conventional means. UV lamps are not recommended for decontamination unless they are properly maintained. Because UV lamp intensity or destructive power decreases with time, it should be checked with a UV meter yearly. Frequent lamp cleaning (at least every few weeks) is necessary to prevent accumulation of dust and dirt that drastically reduces its effectiveness. If UV must be used, it should be used when areas are not occupied. 3. All infectious materials and all contaminated equipment or apparatus should be decontaminated before being washed, stored or discarded. Autoclaving is the preferred method. Each individual working with biohazardous material should be responsible for its proper handling. 39 Housekeeping 1. Good housekeeping in laboratories is essential to reduce risks and protect the integrity of biological experiments. Routine housekeeping must be relied upon to provide work areas free of significant sources of contamination. Housekeeping procedures should be based on the highest degree of risk to which personnel and experimental integrity may be subjected. 2. Laboratory personnel are responsible for cleaning laboratory benches, equipment and areas that require specialized technical knowledge. Additional laboratory housekeeping concerns include: a. Keeping the laboratory neat and free of clutter; surfaces should be clean and free of infrequently used chemicals, glassware and equipment. b. Maintaining access to sinks, eyewashes, emergency showers and fire extinguishers; they should not be blocked. c. Proper disposal of chemicals and waste; old and unused chemicals should be disposed of promptly and properly. Contact Safety and Risk Management for instructions. d. Providing a workplace that is free of physical hazards; aisles and corridors should be free of tripping hazards. Attention should be paid to electrical safety, especially as it relates to the use of extension cords, proper grounding of equipment, avoidance of overloaded electrical circuits and avoidance of the creation of electrical hazards in wet areas. e. Removing unnecessary items on floors, under benches or in corners. f. Properly securing all compressed gas cylinders. g. Never using BSCs or chemical fume hoods for storage of chemicals or other materials. 3. Practical custodial concerns include: a. Dry sweeping and dusting that may lead to the formation of aerosols is not permitted. b. The usual wet or dry industrial type vacuum cleaner is a potent aerosol generator and, unless equipped with a HEPA filter, must not be used in the biological research laboratory. Labeling 1. All containers of biohazardous material should be labeled with the scientific name of the contents, the date stored and the name of the individual who stored them. Unlabeled and obsolete material should be autoclaved and disposed of. 2. Bottles with alcohol-containing solutions should be clearly labeled to avoid autoclaving. 3. Refrigerators and freezers that are used to store biohazardous materials should be labeled with “Biohazard: No Food Or Drink” or similar wording and the universal biohazard symbol on the exterior of the door. 4. A sign incorporating the universal biohazard symbol must be posted at the entrance to the 40 laboratory or classroom when infectious agents are present. The sign should include the name of the agent(s) in use, and the name and phone number of the laboratory supervisor or other responsible personnel. For BSL-2 agents, the sign should also include the procedure required for entry and exit (e.g. PPE) and special practices (e.g. use of BSC, immunizations). Signs are available in Appendix C, online (http://www.uwstout.edu/healthandsafety/safety/intranet/Biosafety.cfm), or from the BSO. Loop sterilizers and Bunsen burners 1. Sterilization of inoculation loops or needles in an open flame generates small-particle aerosols that may contain viable microorganisms. The use of a shielded electric incinerator minimizes aerosol production during loop sterilization. Alternatively, disposable plastic loops and needles may be used for culture work where electric incinerators or gas flames are not available. The loops are semi-quantitative and can be used for counting bacteria. 2. Continuous flame gas burners should not be used in BSCs. These burners can produce turbulence that disturbs the protective airflow patterns of the cabinet. Additionally, the heat produced by the continuous flame may damage the HEPA filter. If a gas burner must be used, one with a pilot light should be selected. Personal protective equipment (PPE) 1. PPE is used to protect personnel from contact with hazardous materials and infectious agents. Appropriate clothing may also protect the experiment from contamination. The following PPE is recommended for regular use: a. Eye and face protection: Goggles, in combination with masks or chin length face shields or other splatter guards, are required whenever there is the possibility of splashes, sprays or splatters of infectious or other hazardous materials to the face. b. Laboratory clothing: This category includes laboratory coats, smocks, scrub suits, and gowns. Long sleeved garments should be used to minimize the contamination of skin or street clothes and to reduce shedding of microorganisms from the arms. In circumstances where it is anticipated that splashes may occur, the garment must be resistant to liquid penetration (in order to protect clothing from contamination). If the garment is not disposable, it must be capable of withstanding sterilization in the event it becomes contaminated. Additional criteria for selecting clothing are comfort, appearance, closure types and location, anti-static properties and durability. Protective clothing must be removed before leaving the laboratory. Disposables should be available for visitors, maintenance and service workers in the event it is required. 41 c. All protective clothing should be either discarded in the laboratory or laundered by the facility. Employees and students must not launder laboratory clothing at home. Gloves: Gloves must be selected based on the hazards involved and the activity to be conducted. Gloves must be worn when working with biohazards, toxic substances and other physically hazardous agents. Temperature-resistant gloves must be worn when handling hot material or dry ice. Delicate work requiring a high degree of precision dictates the use of thin walled gloves. Protection from contact with toxic or corrosive chemicals may also be required. More information on glove selection when working with chemicals is available in the UW-Stout Chemical Hygiene Plan. When working with hazardous materials, the lower sleeve and the cuff of the laboratory garment should be overlapped by the glove. A long sleeved glove or disposable arm-shield may be worn for further protection of the garment. In some instances “double gloving” may be appropriate. If a spill occurs, hands will be protected after the contaminated outer gloves are removed. Gloves must be disposed of when contaminated, removed when work with infectious material is completed, and not worn outside the laboratory. Disposable gloves must not be washed or reused. d. Respirators: In certain instances BSCs or other controls may not be sufficient to control exposure to airborne hazards and a respirator is required. Respirator selection is based on the hazard and the protection factor required. Employees and/or students who require respiratory protection must contact Safety and Risk Management for inclusion in the UWStout Respiratory Protection Program. The program provides a medical examination to ensure no health conditions exist that would be exacerbated by respirator usage, annual fit testing to ensure proper respirator size and type and training to ensure proper respirator use and maintenance. Under no circumstances shall anyone wear a respirator unless he/she is a participant in the program. 2. Contact the BSO or Safety and Risk Management for assistance in selection of other PPE. Pipettes and pipetting aids 1. Pipettes are used for volumetric measurements and transfer of fluids that may contain infectious, toxic, corrosive or radioactive agents. Laboratory-associated infections have occurred from oral aspiration of infectious materials, mouth transfer via a contaminated finger and inhalation of aerosols. 2. Exposures to aerosols may occur when liquid from a pipette is dropped onto the work surface, 42 when cultures are mixed by pipetting or when the last drop of an inoculum is blown out. A pipette may become a hazardous piece of equipment if improperly used. The safe pipetting techniques outlined below are required to minimize the potential for exposure to hazardous materials: a. Never mouth pipette. Always use a pipetting aid. b. If working with biohazardous or toxic fluid, confine pipetting operations to a BSC. c. Always use cotton plugged pipettes when pipetting biohazardous or toxic materials, even when safety pipetting aids are used. d. Do not prepare biohazardous materials by bubbling expiratory air through a liquid with a pipette. e. Do not forcibly expel biohazardous material out of a pipette. f. Never mix biohazardous or toxic material by suction and expulsion through a pipette. g. When pipetting, avoid accidental release of infectious droplets. Place a disinfectant soaked towel on the work surface and autoclave the towel after use. h. Use "to deliver" pipettes rather than those requiring "blowout." i. Do not discharge material from a pipette at a height. Whenever possible allow the discharge to run down the container wall. j. Place contaminated, reusable pipettes horizontally in a pan containing enough liquid disinfectant to completely cover them. Do not place pipettes vertically into a cylinder. k. Discard contaminated disposable pipettes in an appropriate sharps container. See Appendix F for more information on the disposal of pipettes or sharps. l. Pans or sharps containers for contaminated pipettes should be placed inside the BSC, if possible. Sharps safety 1. A high degree of precaution must always be taken with any sharp items used in the laboratory, including needles, glass slides and cover slips, Pasteur pipettes, capillary tubes, and scalpels or other blades. Two of the most common causes of needle sticks are re-capping needles and improper disposal of needles. All needle sticks, and other sharps injuries, carry the risk of secondary infections as well as exposure to the needle's content and/or contamination on the outside of the needle or other sharp instrument. a. Plastic ware should be substituted for glassware whenever possible. b. Safety engineered sharps should always be considered first. The University of Virginia has a website devoted to safety-engineered sharp devices at http://www.healthsystem.virginia.edu/pub/epinet/new/safetydevice.html. 43 c. Do not pick up broken glass with hands. Use mechanical means such as a brush and dustpan, tongs or forceps. 2. Syringes and hypodermic needles are dangerous instruments. The use of needles and syringes should be restricted to procedures for which there is no alternative. Blunt cannulas should be used as alternatives to needles wherever possible (i.e. for procedures such as oral or intranasal animal inoculations). Needles and syringes should never be used as a substitute for pipettes. When needles and syringes must be used with biohazardous or potentially infectious agents, the following procedures are recommended: a. Use syringes that re-sheath the needle, needleless systems, or other safety engineered syringes when possible. b. Use needle-locking syringes to prevent exposure to infectious agents or other hazardous materials via sprays or aerosols (and to prevent the loss of valuable samples). c. Work in a BSC whenever possible. d. Wear gloves. e. Fill the syringe carefully to minimize air bubbles. f. Expel air, liquid and bubbles from the syringe vertically into a cotton pledget moistened with disinfectant. g. Do not use a syringe to mix infectious fluid forcefully. h. Do not contaminate the needle hub when filling the syringe in order to avoid transfer of infectious material to fingers. i. Wrap the needle and stopper in a cotton pledget moistened with disinfectant when removing a needle from a rubber-stoppered bottle. j. Bending, recapping, clipping or removal of needles from syringes is prohibited. If it is essential that a contaminated needle be recapped or removed from a syringe, a resheathing needle, mechanical device or the one handed scoop method (in order of preference) must be used. The use of needle nipping devices is prohibited. NOTE: the BMBL does not permit recapping of needles used for BSL-2 agents for any reason. k. Use a separate pan of disinfectant for reusable syringes and needles. Do not place them in pans containing pipettes or other glassware to eliminate sorting later. 3. Only “contaminated” broken glass, plastic vials, laboratory slides, etc. are considered infectious waste. However, all discarded sharps (contaminated or not) such as hypodermic needles, scalpel blades, lancets and syringes with needles attached are considered infectious waste. See Appendix F and/or contact the BSO or Safety and Risk Management for more information on the disposal of sharps. 4. Sharps usage should be reviewed annually. Can a procedure be modified so that a sharp is not needed? Is there a safety engineered sharp available? 44 45 APPENDIX E TRAINING The principal investigator (PI) is responsible for the training of everyone working in his/her laboratory. Training is possibly the single most important action a PI can take to promote a safe and healthy laboratory. Laboratory-specific biosafety training 1. Laboratory specific biosafety training shall be provided by the PI and will include generalized training for the biosafety level at which the laboratory operates and specialized training for specific hazards present in that laboratory. For workers in laboratories operating at Biosafety Level 1 (BSL-1), it is suggested that information included as Appendix E-1 be reviewed with each worker. The document should be signed by both the laboratory worker and the PI. This training shall be reviewed annually. If the suggested training form is not used, an equivalent document shall be developed to document that training in all standard and special practices, safety equipment and facilities related to work at BSL-1 has been provided. 2. For workers in laboratories operating at BSL-2, it is suggested that information included as Appendix E-2 be reviewed with each worker. The document should be signed by both the laboratory worker and the PI. Note that if CDC select agents are used in the laboratory their presence should be noted on training documentation. This training shall be reviewed annually. If the suggested training form is not used, an equivalent document shall be developed to document that training in all standard and special practices, safety equipment and facilities related to work at BSL-2 has been provided. 3. The signed training document should be retained by the PI as record of appropriate laboratory worker training. Bloodborne pathogens training 1. UW-Stout has developed a bloodborne pathogens exposure control plan that should be reviewed by all laboratory workers. 2. Bloodborne pathogens training is necessary for any laboratory worker who works with human blood, human blood components, products made from human blood, human organs or human body fluids. Training can be provided by Safety and Risk Management or other providers. Teaching laboratories: Instructors in teaching laboratories should provide specific training for the hazards expected to be encountered in the laboratory procedures utilized. Because of the brevity of courses and the large number of students involved it is recommended that each instructor develop a streamlined training form emphasizing the particular elements required for their course. Both the instructor and student should sign the training form. General BSL-1 and -2 entry training: The point paper in Appendix E-3 is intended to provide general awareness training to anyone who needs access to the BSL-2 labs. It is posted on the doors to all BSL-2 labs along with a sign-in sheet, and can be used by instructors to inform students enrolled in courses in the BSL-2 labs that are not doing BSL-2 work. It is not intended to be complete training for employees and students who will be working with agents that require BSL-2 containment. 46 APPENDIX E-1 BIOSAFETY LEVEL 1 (BSL-1) LABORATORY WORKER TRAINING BSL-1 is suitable for work involving well-characterized agents not known to consistently cause disease in healthy adult humans, and of minimal potential hazard to laboratory personnel and the environment. The laboratory is not necessarily separated from the general traffic patterns in the building. Work is generally conducted on open bench tops using standard microbiological practices. Special containment equipment or facility design is neither required nor generally used. Laboratory personnel have specific training in the procedures conducted in the laboratory and are supervised by a scientist with general training in microbiology or a related science. The following standard and special practices, safety equipment and facilities apply to agents assigned to BSL-1: Standard microbiological practices 1. The laboratory supervisor must enforce UW-Stout policies that control access to the laboratory (e.g. granting key card access only to authorized students and staff, keeping doors closed). 2. Persons must wash their hands after working with potentially hazardous materials and before leaving the laboratory. 3. Eating, drinking, smoking, handling contact lenses, applying cosmetics, and storing food for human consumption must not be permitted in laboratory areas. Food must be stored outside the laboratory area in cabinets or refrigerators designated and used for this purpose. 4. Mouth pipetting is prohibited; mechanical pipetting devices must be used. 5. Policies for the safe handling of sharps, such as needles, scalpels, pipettes, and broken glassware must be developed and implemented. Whenever practical, laboratory supervisors should adopt improved engineering and work practice controls that reduce risk of sharps injuries. Precautions, including those listed below, must always be taken with sharp items. These include: a. Careful management of needles and other sharps are of primary importance. Needles must not be bent, sheared, broken, recapped, removed from disposable syringes, or otherwise manipulated by hand before disposal. b. Used disposable needles and syringes must be carefully placed in conveniently located puncture-resistant containers used for sharps disposal. c. Non-disposable sharps must be placed in a hard walled container for transport to a processing area for decontamination, preferably by autoclaving. d. Broken glassware must not be handled directly. Instead, it must be removed using a brush and dustpan, tongs, or forceps. Plastic ware should be substituted for glassware whenever possible. 6. Perform all procedures to minimize the creation of splashes and/or aerosols. 47 7. Decontaminate work surfaces after completion of work and after any spill or splash of potentially infectious material with appropriate disinfectant. 8. Decontaminate all cultures, stocks, and other potentially infectious materials before disposal using an effective method. Depending on where the decontamination will be performed, the following methods should be used prior to transport. a. Materials to be decontaminated outside of the immediate laboratory must be placed in a durable, leak proof container and secured for transport. b. Materials to be removed from the facility for decontamination must be packed in accordance with applicable local, state, and federal regulations. 9. A sign incorporating the universal biohazard symbol must be posted at the entrance to the laboratory or classroom when infectious agents are present. The sign should include the name of the agent(s) in use, and the name and phone number of the laboratory supervisor or other responsible personnel. 10. An effective integrated pest management program is required (see Appendix G of the BMBL). 11. The laboratory supervisor must ensure that laboratory personnel receive appropriate training regarding their duties, the necessary precautions to prevent exposures, and exposure evaluation procedures. Personnel must receive annual updates or additional training when procedural or policy changes occur. Personal health status may impact an individual’s susceptibility to infection, ability to receive immunizations or prophylactic interventions. Therefore, all laboratory personnel and particularly women of childbearing age should be provided with information regarding immune competence and conditions that may predispose them to infection. Individuals having these conditions should be encouraged to self-identify to their healthcare provider for appropriate counseling and guidance. Special practices: None Safety equipment (primary barriers and personal protective equipment) 1. For BSL-1 agents, special containment devices or equipment, such as BSCs, are not generally required. 2. Protective laboratory coats, gowns, smocks, or uniforms designated for laboratory use are recommended for work with BSL-1 agents. Remove protective clothing before leaving the laboratory. Dispose of protective clothing appropriately, or deposit it for laundering. It is recommended that laboratory clothing not be taken home. 3. Safety glasses are required in the laboratory whenever anyone in the lab is working with chemical or biological agents that present a splash hazard, or when there is the potential for flying glass. Splash goggles (and mask, face shield or other splatter guard as needed) should be used for anticipated splashes or sprays of infectious or other hazardous materials. Eye and face protection must be disposed of with other contaminated laboratory waste or decontaminated before reuse. Persons who wear contact lenses in laboratories should also wear eye protection. 48 4. Gloves should be worn to protect hands from exposure to hazardous materials. Glove selection should be based on an appropriate risk assessment. Alternatives to latex gloves should be available. Gloves must not be worn outside the laboratory. In addition, laboratory workers should: a. Change gloves when contaminated, glove integrity is compromised, or when otherwise necessary. b. Remove gloves and wash hands when work with hazardous materials has been completed and before leaving the laboratory. c. Do not wash or reuse disposable gloves. Dispose of used gloves with other contaminated laboratory waste. Hand washing protocols must be rigorously followed. Laboratory facilities (secondary barriers) 1. Laboratory doors must remain closed for access control when biohazardous material is being used. 2. Each laboratory must contain at least one sink for handwashing. 3. The laboratory is designed so that it can be easily cleaned. Carpets, rugs and cloth chairs are not appropriate in laboratories. 4. Bench tops are impervious to water and are resistant to moderate heat and the organic solvents, acids, alkalis, and chemicals used to decontaminate the work surface and equipment. 5. Laboratory furniture is capable of supporting anticipated loading and uses. Spaces between benches, cabinets, and equipment are accessible for cleaning. I have received and understand the biological safety training as outlined in this document. WORKER SIGNATURE: DATE: PI SIGNATURE: DATE: LABORATORY LOCATION: 49 APPENDIX E-2 BIOSAFETY LEVEL 2 (BSL-2) LABORATORY WORKER TRAINING BSL-2 is similar to BSL-1 and is suitable for work involving agents of moderate potential hazard to personnel and the environment. It differs from BSL-1 in that (1) laboratory personnel have specific training in handling pathogenic agents and are directed by competent scientists; (2) access to the laboratory is limited when work is being conducted; (3) extreme precautions are taken with contaminated sharp items; and (4) certain procedures in which infectious aerosols or splashes may be created are conducted in biological safety cabinets (BSCs) or other physical containment equipment. The following standard and special practices, safety equipment and facilities apply to agents assigned to BSL- 2: Standard microbiological practices 1. The laboratory supervisor must enforce UW-Stout policies that control access to the laboratory (e.g. granting key card access only to authorized students and staff, keeping doors closed). 2. Persons must wash their hands after working with potentially hazardous materials and before leaving the laboratory. 3. Eating, drinking, smoking, handling contact lenses, applying cosmetics, and storing food for human consumption must not be permitted in laboratory areas. Food must be stored outside the laboratory area in cabinets or refrigerators designated and used for this purpose. 4. Mouth pipetting is prohibited; mechanical pipetting devices must be used. 5. Policies for the safe handling of sharps, such as needles, scalpels, pipettes, and broken glassware must be developed and implemented. Whenever practical, laboratory supervisors should adopt improved engineering and work practice controls that reduce risk of sharps injuries. Precautions, including those listed below, must always be taken with sharp items. These include: a. Careful management of needles and other sharps are of primary importance. Needles must not be bent, sheared, broken, recapped (without specific training), removed from disposable syringes, or otherwise manipulated by hand before disposal. b. Used disposable needles and syringes must be carefully placed in conveniently located puncture-resistant containers used for sharps disposal. c. Non-disposable sharps must be placed in a hard walled container for transport to a processing area for decontamination, preferably by autoclaving. d. Broken glassware must not be handled directly. Instead, it must be removed using a brush and dustpan, tongs, or forceps. Plastic ware should be substituted for glassware whenever possible. 6. Perform all procedures to minimize the creation of splashes and/or aerosols. 7. Decontaminate work surfaces after completion of work and after any spill or splash of potentially infectious material with appropriate disinfectant. 50 8. Decontaminate all cultures, stocks, and other potentially infectious materials before disposal using an effective method. Depending on where the decontamination will be performed, the following methods should be used prior to transport. a. Materials to be decontaminated outside of the immediate laboratory must be placed in a durable, leak proof container and secured for transport. b. Materials to be removed from the facility for decontamination must be packed in accordance with applicable local, state, and federal regulations. 9. A sign incorporating the universal biohazard symbol must be posted at the entrance to the laboratory or classroom when infectious agents are present. The sign should include the name of the agent(s) in use, the procedure required for entry and exit (e.g. PPE), special practices (e.g. use of BSC, immunizations) and the name and phone number of the laboratory supervisor or other responsible personnel. 10. An effective integrated pest management program is required (see Appendix G of the BMBL). 11. The laboratory supervisor must ensure that laboratory personnel receive appropriate training regarding their duties, the necessary precautions to prevent exposures, and exposure evaluation procedures. Personnel must receive annual updates or additional training when procedural or policy changes occur. Personal health status may impact an individual’s susceptibility to infection, ability to receive immunizations or prophylactic interventions. Therefore, all laboratory personnel and particularly women of childbearing age should be provided with information regarding immune competence and conditions that may predispose them to infection. Individuals having these conditions should be encouraged to self-identify to their healthcare provider for appropriate counseling and guidance. Special practices 1. Access to the laboratory must be restricted when work is being conducted. 2. All persons entering the laboratory must be advised of the potential hazards. 3. Laboratory personnel must be provided medical surveillance, as appropriate, and offered available immunizations for agents handled or potentially present in the laboratory. 4. A laboratory-specific biosafety manual must be prepared and adopted as policy. The biosafety manual must be available and accessible. 5. The laboratory supervisor must ensure that laboratory personnel demonstrate proficiency in standard and special microbiological practices before working with BSL-2 agents. 6. Potentially infectious materials must be placed in a durable, leak proof container during collection, handling, processing, storage, or transport within a facility. 7. Laboratory equipment should be routinely decontaminated, as well as, after spills, splashes, or other potential contamination. 51 8. Spills involving infectious materials must be contained, decontaminated, and cleaned up by staff properly trained and equipped to work with infectious material. 9. Equipment must be decontaminated before repair, maintenance, or removal from the laboratory. 10. Incidents that may result in exposure to infectious materials must be immediately evaluated and treated according to procedures described in the laboratory biosafety manual. All such incidents must be reported to the laboratory supervisor. Medical evaluation, surveillance, and treatment should be provided and appropriate records maintained. 11. Animals and plants not associated with the work being performed must not be permitted in the laboratory. 12. All procedures involving the manipulation of infectious materials that may generate an aerosol should be conducted within a BSC or other physical containment devices. Safety equipment (primary barriers and personal protective equipment) 1. For BSL-2 agents, properly maintained BSCs, other appropriate personal protective equipment, or other physical containment devices must be used whenever: a. Procedures with a potential for creating infectious aerosols or splashes are conducted. These may include pipetting, centrifuging, grinding, blending, shaking, mixing, sonicating, opening containers of infectious materials, inoculating animals intranasally, and harvesting infected tissues from animals or eggs. b. High concentrations or large volumes of infectious agents are used. Such materials may be centrifuged in the open laboratory using sealed rotor heads or centrifuge safety cups. 2. Protective laboratory coats, gowns, smocks, or uniforms designated for laboratory use are required for BSL-2 agents. Remove protective clothing before leaving the laboratory. Dispose of protective clothing appropriately, or deposit it for laundering. It is recommended that laboratory clothing not be taken home. 3. Safety glasses are required in the laboratory whenever anyone in the lab is working with chemical or biological agents that present a splash hazard, or when there is the potential for flying glass. Splash goggles (and mask, face shield or other splatter guard as needed) are used for anticipated splashes or sprays of infectious or other hazardous materials when the microorganisms must be handled outside the BSC or containment device. Eye and face protection must be disposed of with other contaminated laboratory waste or decontaminated before reuse. Persons who wear contact lenses in laboratories should also wear eye protection. 4. Gloves should be worn to protect hands from exposure to hazardous materials. Glove selection should be based on an appropriate risk assessment. Alternatives to latex gloves should be available. Gloves must not be worn outside the laboratory. In addition, laboratory workers should: a. Change gloves when contaminated, glove integrity is compromised, or when otherwise necessary. 52 b. Remove gloves and wash hands when work with hazardous materials has been completed and before leaving the laboratory. c. Do not wash or reuse disposable gloves. Dispose of used gloves with other contaminated laboratory waste. Hand washing protocols must be rigorously followed. 5. A risk assessment should be used to determine if eye, face and/or respiratory protection is needed in rooms containing infected animals. Laboratory facilities (secondary barriers) 1. Laboratory doors must remain closed for access control. 2. Each laboratory contains at least one sink for handwashing. 3. The laboratory is designed so that it can be easily cleaned. Carpets, rugs and cloth chairs are not appropriate in laboratories. 4. Bench tops are impervious to water and are resistant to moderate heat and the organic solvents, acids, alkalis, and chemicals used to decontaminate the work surface and equipment. 5. Laboratory furniture is capable of supporting anticipated loading and uses. Spaces between benches, cabinets, and equipment are accessible for cleaning. 6. An eyewash station must be readily available. 7. HEPA-filtered exhaust air from a Class II BSC can be safety recirculated back into the laboratory environment if the cabinet is tested and certified at least annually and operated according to manufacturer’s recommendations. 8. A method for decontaminating all laboratory waste is available. I have received and understand the biological safety training as outlined in this document. WORKER SIGNATURE: DATE: PI SIGNATURE: DATE: LABORATORY LOCATION: 53 APPENDIX E-3 BIOSAFETY LEVEL 2 (BSL-2) LAB TRAINING This training provides a basic understanding of biosafety hazards and practices required to enter UWStout’s designated BSL-2 laboratory spaces. If you will be working with biological agents that require BSL-2 containment, you must receive additional training (such as bloodborne pathogens training, safe use of biosafety cabinets, standard microbiological practices) from your instructor/laboratory supervisor. The “biosafety level” defines the laboratory practices and techniques, safety equipment and laboratory facilities recommended for work with biohazardous materials. Biohazardous materials are infectious agents or hazardous biological materials that present a potential risk to the health of humans, animals or the environment. BSL-2 is for work with moderate-risk agents that are associated with human disease of varying severity. All doors to laboratory or classroom spaces designated as BSL-2 labs have a sign with a large orange “biohazard” symbol and entry and exit requirements for everyone who enters the space. What are the potential hazards? o Exposure is most likely to occur via accidental needle stick; splash into the eyes, nose or mouth; or accidental ingestion people working with the material. o The risk of exposure by being in the room and inhaling the material is extremely low. What are the rules? o Lab coats are mandatory for everyone who enters. o No open-toed shoes. o Safety glasses must be worn by everyone who enters if anyone in the room is working with a liquid chemical or biohazardous material that presents a splash hazard. o Doors must not be propped open. o No eating, drinking, applying cosmetics or storing food for human consumption at any time. o Wash hands with soap and water before leaving the room. 54 APPENDIX F TREATMENT, HANDLING AND DISPOSAL OF BIOLOGICAL MATERIALS Proper treatment, handling and disposal of cultures and items contaminated by potentially biohazardous materials are a vital step toward protection of laboratory and hazardous waste personnel from infectious disease. This waste handling process is also necessary to prevent the release of potentially infectious agents into the community at large. Treatment and disposal of biological waste is regulated by several federal and state agencies. An exposure occurs when potentially infectious materials are permitted to enter a person’s bloodstream through a break in the skin or contact with the eyes, nose, or mouth. Examples of exposure related to biohazardous waste handling include incidents such as: Splashing liquid biological waste into the eye during pour-off for disposal Puncturing the skin with a biologically contaminated needle Spilling liquids from a ruptured biohazardous bag onto broken, unprotected skin. In the event of an exposure to potentially infectious materials, take the following actions: Wash the exposed skin or flush the mucous membrane for 10-15 minutes. Notify your lab director or supervisor and the Biological Safety Officer or Safety and Risk Management.. Contact your health care provider to determine the need for evaluation and/or possible treatment. A waste is considered to be an infectious waste if it falls in one of the following categories: 1. Sharps are potentially the most hazardous items in the infectious waste stream. A high degree of caution should always be used when handling any sharp object, contaminated or not. a. Contaminated sharps (contacted blood or a potentially infectious material) that are both infectious and may easily cause punctures or cuts in the skin, including but not limited to hypodermic needles, syringes with needles attached, scalpel blades, lancets, broken glass vials, broken rigid plastic vials and laboratory slides, must be disposed of as infectious waste. b. Unused or disinfected sharps that are being discarded, including hypodermic needles, scalpel blades, lancets and syringes with needles attached must also be disposed of as infectious waste. c. Note: Only "contaminated" broken glass, plastic vials, laboratory slides, etc. are considered infectious waste. However, all discarded sharps (contaminated or not) such as hypodermic needles, scalpel blades, lancets and syringes with needles attached are considered infectious waste. 55 2. Bulk blood and body fluids from humans means drippable or pourable quantities or items saturated with blood or other potentially infectious materials. In making this determination ask whether blood or other potentially infectious materials are dripping from the item or can be squeezed, poured or flaked from the item. 3. Human tissue. 4. Microbiological laboratory waste means cultures derived from clinical specimens or laboratory equipment that has come in contact with these cultures. 5. Tissue (including whole carcasses), bulk blood or body fluids from an animal that is carrying an infectious agent or has been used in recombinant or synthetic nucleic acid molecule research. 6. Mixed wastes are potentially infectious waste contaminated with other types of waste (e.g. radioisotopes or toxic/carcinogenic compounds). Because of the difficulty in disposal of wastes regulated by more than one set of requirements and regulatory agencies, it is critical that provision be made for proper management prior to the initiation of any research that might result in mixed waste. Mixed wastes may require special containers, labeling, storage, etc. Contact Safety and Risk Management prior to initiation of any research that might result in potentially infectious waste with multiple hazards. 7. Microorganism cultures should be inactivated, using appropriate procedures, before disposal. This includes cultures of Risk Group 1 and 2 organisms. This is considered good laboratory practice. Items that generally are not considered infectious waste include the following: 1. Items soiled but not saturated with blood of body fluids from humans (application of the drippable, squeezable, pourable, flakeable rule). 2. Tissue, blood, body fluids or cultures from an animal that is not known to be carrying or experimentally infected with a zoonotic infectious agent. 3. Animal manure and bedding from uninfected animals. More than one treatment option is available for infectious waste. Sharps are collected and sent off campus for incineration. The remaining infectious waste is autoclaved (steam sterilization) and then disposed of as normal trash. 1. All non-sharp laboratory materials utilized in experiments with biological materials (e.g. microorganisms, recombinant or synthetic nucleic acid molecules, cell cultures) must be treated prior to disposal by an approved decontamination method such as autoclaving. These wastes should be stored in bags bearing the biohazard symbol prior to decontamination. While in use for waste storage, biohazard bags must be secured in a manner that will eliminate spillage. If a bag is used primarily for disposal items that are not likely to release liquids (e.g. contaminated pipette tips or kim wipes), a wire bag rack or rigid container is an acceptable means of securing the bag to eliminate spillage. If the bag is used for storage of items that are likely to release liquids and possible result in leakage, the bag should be stored in a leak proof container such as a trash can with a lid that is also labeled with the biohazard symbol. 56 2. When transporting waste bags to the autoclave for treatment, secure the bags closed with a rubber band, twist tie or other closure device that can be easily removed and place the bags in secondary container such as a pan or bucket. Always use a cart to move the bags if possible. 3. After autoclaving, any bag displaying the biohazard symbol should be placed in a non-transparent plastic bag or other secondary non-transparent container (e.g. closed cardboard box, dark colored trash bag) prior to disposal into the normal trash. Bags with the biohazard symbol, regardless of use, must not be placed into the regular waste stream without defacing the symbol or over-bagging. Collection and handling: 1. Infectious waste should be segregated and contained in an enclosed area until it is treated. 2. Sharps should be placed in a puncture-proof and leak-proof container with a sealable lid. The outside container must be labeled with a visible biohazard emblem (fluorescent orange background with contrasting color - typically black - biohazard symbol). Red sharps containers are commercially available. 3. Other infectious waste should be placed in an infectious waste bag (leak proof) with a biohazard label. 4. Uncontaminated plastic pipette tips and uncontaminated glass are not restricted waste and can be disposed in the regular waste stream after placement in a container, such as a designated cardboard box, that will eliminate the potential of punctures and cuts to solid waste handlers or the public. When it is time to dispose of the box, tape it shut and label it with “uncontaminated plastic pipette tips” or “uncontaminated glass.” 5. Contact University Police (x2222) for the transportation of infectious waste to Student Health Services. Type of Waste Animal bedding from infected animals Animal carcasses and tissue Liquid infectious waste including all recombinant or synthetic nucleic acid molecule material Container for Disposal or Treatment Place cage, water bottle and bedding in an autoclave bag Red biohazard bag; store carcasses in freezer Local Treatment Suitable liquid handling container Disinfect with 1 part bleach to 10 parts liquid, or other appropriate disinfectant per an RSC-approved protocol, and sewer. Can also autoclave and sewer. (Do not sewer agar; handle as solid waste.) Autoclave None Who to Call for Disposal Place autoclaved bedding in regular trash Safety & Risk Management (contractor incineration) N/A 57 Type of Waste Contaminated nonsharps (including recombinant or synthetic nucleic acid molecules) Glass or other non-sharps (e.g. pipette tips) not contaminated with hazardous material Sharps, contaminated or not Biological toxins Container for Disposal or Treatment Autoclave bag Local Treatment Autoclave Who to Call for Disposal Place autoclaved materials in regular trash Dedicated box closed and taped shut None required Regular trash Sharps container None Suitable treatment container Treat with 2N NaOH for at least 1 hr, neutralize the NaOH solution with acid until the pH is between 5 and 8, sewer if toxin is not in a hazardous chemical mixture Campus Police (x2222) for transport to Student Health If toxin in a hazardous chemical mixture, place in hazardous waste container (no longer a toxin hazard) and call Safety & Risk Management 58 APPENDIX G SELECT AGENTS AND TOXINS The following list is taken from the joint APHIS/CDC National Select Agent Registry website (http://www.selectagents.gov) and is dated September 10, 2013. Select agents and toxins are agents that HHS considers to have the potential to pose a severe threat to human health. High Consequence Livestock Pathogens and Toxins are agents that the USDA considers to have the potential to pose a severe threat to animal or plant health, or to animal or plant products. The plant pathogens listed by USDA have been deemed a threat to plant health or products. Agents that pose a severe threat to animal health, animal products, and public health are referred to as “overlap agents.” HHS Select Agents And Toxins Abrin Botulinum neurotoxins Botulinum neurotoxin producing species of Clostridium Conotoxins Coxiella burnetii Crimean-Congo haemorrhagic fever virus Diacetoxyscirpenol Eastern Equine Encephalitis virus Ebola virus Overlap Select Agents And Toxins Bacillus anthracis Bacillus anthracis Pasteur strain Brucella abortus Brucella melitensis Brucella suis Burkholderia mallei Burkholderia pseudomallei Francisella tularensis Hendra virus Nipah virus Rift Valley fever virus Venezuelan Equine Encephalitis virus Rickettsia prowazekii USDA Select Agents And Toxins African horse sickness virus African swine fever virus Avian influenza virus Classical swine fever virus Foot-and-mouth disease virus Goat pox virus Lumpy skin disease virus Lassa fever virus Marburg virus Monkeypox virus Reconstructed replication competent forms of the 1918 pandemic influenza virus containing any portion of the coding regions of all eight gene segments (Reconstructed 1918 Influenza virus) Ricin SARS-associated corona virus (SARS-CoV) Saxitoxin Shiga-like ribosome inactivating proteins Shigatoxin South American Haemorrhagic Fever viruses (Chapare, Guanarito, Junin, Machupo, Sabia) Staphylococcal enterotoxins A,B,C,D, E subtypes T-2 toxin Tetrodotoxin Tick-borne encephalitis complex (flavi) viruses (Far Eastern subtype, Siberian subtype) Kyasanur Forest disease virus Omsk Hemorrhagic fever virus Variola major virus (Smallpox virus) Variola minor virus (Alastrim) Yersinia pestis Mycoplasma capricolum Mycoplasma mycoides Newcastle disease virus Peste des petits ruminants virus Rinderpest virus Sheep pox virus Swine vesicular disease virus USDA Plant Protection and Quarantine (PPQ) Select Agents And Toxins Peronosclerospora philippinensis (Peronosclerospora sacchari) Phoma glycinicola (formerly Pyrenochaeta glycines) Ralstonia solanacearum Rathayibacter toxicus Sclerophthora rayssiae var zeae Synchytrium endobioticum Xanthomonas oryzae 59 APPENDIX H ACRONYMS APHIS Animal and Plant Health Inspection Service (USDA) BMBL Biosafety in Microbiological and Biomedical Laboratories BSC Biological safety cabinet BSL Biosafety level BSO Biological Safety Officer CDC Centers for Disease Control and Prevention HEPA High efficiency particulate air HHS U.S. Department of Health and Human Services IACUC Institutional Animal Care and Use Committee IRB Institutional Review Board NIH National Institutes of Health OBA Office of Biotechnology Activities (NIH) PI Principal investigator PPE Personal protective equipment RAC Recombinant DNA Advisory Committee (NIH) RG Risk Group RSC Research Safety Committee USDA U.S. Department of Agriculture UV Ultraviolet 60