Delayed vasoconstrictor response to venous pooling in the calf is... with high orthostatic tolerance to LBNP
advertisement

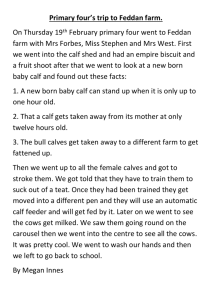
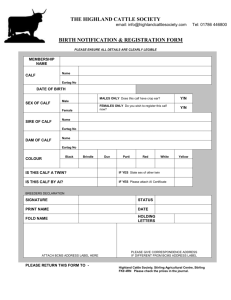
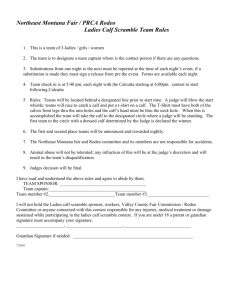
J Appl Physiol 109: 996–1001, 2010. First published July 22, 2010; doi:10.1152/japplphysiol.00593.2009. Delayed vasoconstrictor response to venous pooling in the calf is associated with high orthostatic tolerance to LBNP T. Hachiya,1 M. L. Walsh,1 M. Saito,2 and A. P. Blaber1 1 Aerospace Physiology Laboratory, Department of Biomedical Physiology and Kinesiology, Simon Fraser University, Burnaby, British Columbia, Canada; and 2Laboratory of Applied Physiology, Toyota Technological Institute, Nagoya, Japan Submitted 2 June 2009; accepted in final form 16 July 2010 Hachiya T, Walsh ML, Saito M, Blaber AP. Delayed vasoconstrictor response to venous pooling in the calf is associated with high orthostatic tolerance to LBNP. J Appl Physiol 109: 996–1001, 2010. First published July 22, 2010; doi:10.1152/japplphysiol.00593.2009.—Central blood volume loss to venous pooling in the lower extremities and vasoconstrictor response are commonly viewed as key factors to distinguish between individuals with high and low tolerance to orthostatic stress. In this study, we analyzed calf vasoconstriction as a function of venous pooling during simulated orthostatic stress. We hypothesized that high orthostatic tolerance (OT) would be associated with greater vasoconstrictor responses to venous pooling compared with low OT. Nineteen participants underwent continuous stepped lower body negative pressure at ⫺10, ⫺20, ⫺30, ⫺40, ⫺50, and ⫺60 mmHg each for 5 min or until exhibiting signs of presyncope. Ten participants completed the lower body negative pressure procedure without presyncope and were categorized with high OT; the remaining nine were categorized as having low OT. Near-infrared spectroscopy measurements of vasoconstriction (Hachiya T, Blaber A, Saito M. Acta Physiologica 193: 117–127, 2008) in calf muscles, along with heart rate (HR) responses for each participant, were evaluated in relation to calf blood volume, estimated by plethysmography. The slopes of this relationship between vasoconstriction and blood volume were not different between the high- and low-tolerance groups. However, the onset of vasoconstriction in the high-tolerance group was delayed. Greater HR increments in the low-tolerance group were also observed as a function of lower limb blood pooling. The delayed vasoconstriction and slower HR increments in the high-tolerance group to similar venous pooling in the low group may suggest a greater vascular reserve and possible delayed reduction in venous return. lower body negative pressure; near-infrared spectroscopy; straingauge plethysmography; blood pressure; syncope A PATIENT WITH POSTURAL ORTHOSTATIC tachycardia syndrome or with heart failure has difficulty transitioning from the supine to upright position. Even some healthy people exhibit presyncopal symptoms, such as nausea and dizziness during continuous standing. It is well known that vasoconstriction is a key factor in the regulation of blood pressure (BP) during orthostatic stress. Total peripheral resistance calculated with cardiac output and mean arterial pressure (MAP) has been shown to be greater with high orthostatic tolerance compared with low tolerance (6). Hormonal agents, such as norepinephrine, vasopressin, and renin-angiotensin II, are involved in vasomotor control during lower body negative pressure (LBNP) (4, 9) and consistently greater plasma angiotensin II concentration with high orthostatic tolerance has been reported (4, 9). Furthermore, it has Address for reprint requests and other correspondence: A. P. Blaber, Dept. of Biomedical Physiology and Kinesiology, Simon Fraser Univ., 8888 Univ. Dr., Burnaby, BC, Canada V5A 1S6 (e-mail: ablaber@sfu.ca). 996 been documented that muscle sympathetic nervous activity (MSNA), which modulates skin and muscle vasomotor tone, is augmented with increments in negative pressure (27). Brown and Hainsworth (3) found that increases in forearm vascular resistance were greater in normal control subjects than in orthostatic-intolerant patients during combined head-up tilt (HUT) and LBNP. Although weak vasoconstriction of vascular smooth muscles in the forearm has often been considered to be associated with reduced orthostatic intolerance, it has been documented that the vasoconstrictor rate in the calf is greater than that in the forearm (28), mainly due to greater myogenic responses and increased ␣-adrenergic receptor sensitivity (15). Vascular beds in the lower limbs are considered to play a critical role in regulating BP during orthostatic stress due to their large muscle mass and to their constant exposure to orthostatic blood accumulation (21). An examination of vascular responses in the calf would, therefore, provide more relevant information on the relationship between vascular resistance and orthostatic tolerance. However, there is some controversy with respect to the importance of blood pooling vasoconstriction on orthostatic tolerance (8, 15). The purpose of this study was to examine vasoconstriction in the calf as a function of orthostatic stress and tolerance. Unlike previous studies, in which responses have been characterized as either a function of LBNP or HUT, we chose to examine vasoconstriction in the calf as a function of venous accumulation in the calf. We chose this comparison to venous pooling to normalize the reflex responses to the inducer of a common physiological stress. We hypothesized that participants with low orthostatic tolerance would have a reduced vasoconstrictor response to venous pooling compared with participants with high tolerance. To measure vasoconstriction in the calf we used nearinfrared spectroscopy (NIRS). The degree of oxygenated Hb in muscle can be used to estimate the arterial vascular responses of muscle tissue during orthostatic stress (10) and can be considered an indicator of sympathetically mediated muscle vasoconstriction during graded LBNP. Since high orthostatic tolerance has been associated with greater vasoconstrictor response (9), we hypothesized that a larger oxygenated Hb reduction as a function of venous blood volume (BV) accumulation would be observed in high-tolerant vs. low-tolerant participants during graded LBNP. METHODS Participants. Nineteen healthy male participants volunteered for this investigation. The room was kept quiet, and its temperature was maintained between 22 and 24°C during the experiment. Informed, written consent was obtained from the participants before each experiment. The study conformed to the standard set by the Declaration 8750-7587/10 Copyright © 2010 the American Physiological Society http://www.jap.org CALF VASOCONSTRICTION WITH VENOUS POOLING DURING LBNP of Helsinki, and the experimental protocols were approved by the Human Subjects Ethics Committee for the Toyota Technological Institute and by the office of Research and Ethics for Simon Fraser University. BV (plethysmography). To evaluate lower limb BV changes, the calf belly volume was monitored by mercury strain-gauge plethysmography (EC6, Hokanson Bellevue, WA) (29). The strain gauge was placed at the point of the greatest girth. The change in calf circumference was expressed as a change in voltage values, which reflected BV alterations. The BV change was expressed as percent change (ml/100 ml calf volume). NIRS. NIRS devices were used to monitor oxygenated and deoxygenated Hb changes, yielding total Hb by summing the two Hb values. The basic principle of NIRS is explained elsewhere (18). Briefly, the near-infrared light (700 –900 nm) penetrates skin, subcutaneous, and muscle tissues and is scattered. The scattered light is detected on the surface. Our system (Omegawave, BOM-L1W, Tokyo, Japan) used two laser wavelengths, 780 and 810 nm. Hb and myoglobin molecules absorb the light at the specified wavelengths. However, it can be assumed that oxygenated states of myoglobin should not be affected by LBNP in the current study, because muscle movements were not observed through the LBNP observation window, and previous research has indicated lack of movement with this protocol (11). The NIRS device should mainly detect Hb changes in muscle tissue sites, such as arterioles, capillaries, and venules, since the high amount of Hb molecules will absorb all of the available light passing through these blood vessels (20). To evaluate changes in Hb oxygenated states in a selective deep portion of the calf muscle vasculature, the NIRS model (BOM-L1W) with two photodetectors and one emitter was used. Due to technical difficulties during experimentation, only 15 participants had deep NIRS measurements. The set of probes was positioned on the skin surface of the medial soleus area just below the maximum circumference of the left calf. Soleus muscle is a slow-twitch muscle, with a large degree of vascularization, and is involved in postural control. The photodetectors were placed parallel to the calf 2.0 and 3.0 cm from the emitter. The selective deep NIRS evaluations were provided by subtracting the superficial portion, obtained by the detector 2.0 cm from the emitter, from the total portion assessed by the detector at 3.0 cm (16). The remaining signal from ⬃2.0 to 3.0 cm in depth enabled us to monitor Hb changes primarily from the muscle tissue vasculature. In the previous study (10), our laboratory compared oxygenated Hb changes in calf with MSNA responses and with blood flow evaluated plethysmography during graded LBNP, finding that both variables were significantly correlated. It is believed that oxygenated Hb responses can reflect vasoconstrictor activities accompanying blood flow reduction during LBNP. Heart rate and BP. Heart rate (HR) was recorded continuously by chest electrocardiography. BP was measured in the right arm every minute by a noninvasive automated electrosphygmomanometry (Nippon Colin BP 203, Tokyo, Japan). Finger photoplethysmography (Finapres; Ohmeda, Englewood, CO) was used to monitor instantaneous BP so that a sudden reduction in BP indicating presyncope symptom could be detected. LBNP. Participants were placed in the supine position with their lower body enclosed in a wooden negative-pressure chamber at the level of the iliac crest. The participants straddled a padded seat with their legs horizontal at heart level and their feet placed against a foot plate, which did not hinder blood pooling in the legs. The box was airtight, and a window allowed the experimenter to monitor mercury strain-gauge and NIRS probes. The participants were rested in the supine position for ⬃15 min before the LBNP protocol. Then each participant underwent 35 min of continuous stepped decompression from baseline (0 mmHg) to ⫺10-, ⫺20-, ⫺30-, ⫺40-, ⫺50-, and ⫺60-mmHg LBNP each for 5 min or until exhibiting signs of presyncope [decreased BP (Fig. 1), nausea, or light headedness]. After completion of the LBNP, there was a 5-min recovery at 0 mmHg. J Appl Physiol • VOL 997 Fig. 1. An example of the original data from one presyncopal participant. AU, arbitrary unit; LBNP, lower body negative pressure; Oxy, oxygenated; Deoxy, deoxygenated. Plethysmography, NIRS, BP, and HR data were averaged from the last 3 min of each 5-min pressure stage. The NIRS and plethysmography data were displayed as relative changes from the baseline set as zero. All data were monitored simultaneously and stored on the personal computer for later analysis. Analog-to-digital conversion software (Acqknowledge, Biopac systems, Goleta, CA) was used to acquire the data. Statistical analysis. Participants’ data were divided into two groups [low (Low) and high tolerance (High)], based on their ability to complete an LBNP test up to ⫺60 mmHg. One-way repeated-measures ANOVA for each Hb value in the calf, and for cardiovascular parameters (HR and BP), including blood pooling in response to negative pressure for each group, were performed independently. When the effects were significant, Student-Newman-Keuls post hoc analysis was applied. The GraphPad InStat statistical package (GraphPad Software, San Diego, CA) was used for the one-way ANOVA analysis. Two-way repeated-measures ANOVA was carried out to examine the main effect of the parameters between High and Low groups and stage of LBNP (SPSS, Chicago, IL). Inspection of the data revealed the following linear relations: oxygenated Hb and calf BV, deoxygenated Hb and calf BV, and oxygenated Hb and deoxygenated Hb. However, the physiological responses did not always occur in phase with BV accumulation. For each participant, progressive linear regression analysis was performed. An initial regression was performed with the last three data points (highest calf BV changes). Data points were then sequentially added toward baseline with the regression recalculated for an additional point. At each step, the r2 value was compared with the previous step. If r2 was ⬍0.85, the previous regression was deemed be represent the response. The slope was recorded, and the x-intercept was calculated to determine the “threshold” for the response. The response between HR and BV was observed to be nonlinear without a threshold delay. Further analysis with a lack of fit test revealed that the relationship between HR and calf BV was not linear and that a quadratic provided the best regression. Therefore, a qua- 109 • OCTOBER 2010 • www.jap.org 998 CALF VASOCONSTRICTION WITH VENOUS POOLING DURING LBNP dratic regression, for each participant, was performed to examine the relationship between HR and calf BV. The coefficients of regression were compared between High and Low groups via t-tests. Additionally, correlation coefficients between total Hb and deoxygenated Hb with blood pooling were compared with a t-test. Significance was set at P ⬍ 0.05. Data were expressed as means ⫾ SE. RESULTS Ten participants completed up to ⫺60-mmHg LBNP and were characterized as having high orthostatic tolerance (High: 21.9 ⫾ 0.5 yr, 173.2 ⫾ 2.0 cm, and 62.6 ⫾ 3.1 kg). The remaining nine participants, who exhibited presyncope and did not finish the LBNP protocol, were classified as the low-tolerant group (Low: 23.4 ⫾ 1.5 yr, 174.4 ⫾ 1.0 cm, and 65.8 ⫾ 2.1 kg). Two out of nine participants categorized as low tolerance stopped the LBNP maneuver during ⫺50 mmHg, and the remainder withdrew during ⫺60 mmHg. While all data in the High group were displayed throughout ⫺60 mmHg, those in the Low group were shown up to ⫺40-mmHg LBNP. Since the 15 participants in the selective deep calf oxygenated Hb experiments either completed ⫺60 mmHg or exhibited presyncope symptoms up to ⫺60-mmHg LBNP, the deep calf NIRS comparisons were only made up to ⫺50-mmHg LBNP between the High (n ⫽ 9) and Low (n ⫽ 6) groups. Plethysmography. Blood accumulated in the calf proportional to enhanced negative pressure during LBNP (Fig. 2). There was no group difference in blood pooling in the calf muscles up to ⫺40-mmHg LBNP (P ⫽ 0.07). Maximal blood accumulation at ⫺60 mmHg in the High group was greater than that in the Low group at each tolerant maximal pressure level (P ⬍ 0.001). NIRS. Oxygenated Hb decreased as calf volume increased with LBNP in both the High and Low groups (Fig. 3). There was no difference between the slopes of the regressions of the High and Low groups (P ⫽ 0.15), but the x-axis intercept (BV threshold) in the High group was significantly higher than that in the Low group (High: 1.04 ⫾ 0.16%; Low ⫺0.25 ⫾ 0.17%, P ⬍ 0.05) and was significantly greater from zero (P ⬍ 0.05) (Fig. 3). In contrast, the x-axis intercept in the Low group was Fig. 2. Percent changes in calf volume. The measurements were performed by mercury strain-gauge plethysmography. The blood pooling during graded LBNP is presented up to ⫺40 mmHg in the low-tolerance group and ⫺60 mmHg in the high-tolerance group. Values are means ⫾ SE; n, no. of subjects. BL, baseline. *P ⬍ 0.05 vs. control; #P ⬍ 0.05 from the previous LBNP level. J Appl Physiol • VOL Fig. 3. Top: mean values for oxy-Hb as a function of LBNP for the hightolerance group () and the low-tolerance group (Œ). Values are means ⫾ SE. *P ⬍ 0.05 vs. control; #P ⬍ 0.05 from previous values. Bottom: regression analysis between oxy-Hb and calf blood volume (BV) changes. All of the individual data are displayed (high tolerance: solid or shaded symbols with solid lines; low tolerance: open symbols with dashed lines). The average regressions are shown as a thick solid line for the high-tolerance group and a thick dashed line for the low-tolerance group. not different from zero (P ⫽ 0.26). Oxygenated Hb and calf BV changes in the two groups were highly correlated (High: r2 ⫽ 0.98 ⫾ 0.01, and Low: r2 ⫽ 0.96 ⫾ 0.01). Similar results were observed when oxygenated Hb was compared with deoxygenated Hb (Fig. 4). The regressions of oxygenated Hb and deoxygenated Hb showed that, between the groups, there was no difference in slopes and that there was a difference in the x-intercept (P ⬍ 0.05). The x-intercept for the High group was greater than zero, and the x-intercept for the Low group was not. HR. HR at each pressure level, including baseline, did not differ between both groups (P ⫽ 0.92) (Fig. 5). The magnitude of the rise in HR in the Low group from ⫺20- to ⫺40-mmHg 109 • OCTOBER 2010 • www.jap.org CALF VASOCONSTRICTION WITH VENOUS POOLING DURING LBNP Fig. 4. Regression analysis between oxy-Hb and deoxy-Hb. All of the individual data are displayed (high tolerance: solid or shaded symbols with solid lines; low tolerance: open symbols with dashed lines). The average regressions are shown as a thick solid line for the high-tolerance group and a thick dash line for the low-tolerance group. 999 Fig. 6. The quadratic equations between HR and blood pooling as physiological responses. The solid lines indicate the high-tolerance group (mean: thick line; SE: thin line), and the dashed lines are mean (thick line) and SE (thin line) for the low-tolerance group. bpm, Beats/min. Inset: a sample regression for one participant from the high-tolerance group (, solid line) and one participant from the low-tolerance group (Œ, dashed line). LBNP was greater than that in the High group at the same period (P ⬍ 0.05). However, similar HR increments in the High group were found from ⫺40- to ⫺60-mmHg LBNP compared with the response in the Low groups from ⫺20- to ⫺40-mmHg LBNP (P ⫽ 0.16). Given the nonlinear nature of the HR changes with LBNP, HR responses at given leg BV changes were analyzed with a quadratic regression (Fig. 6). The second-order coefficient of the Low group was significantly greater than that of the High group (P ⬍ 0.05), indicating that the Low group had larger HR responses at given blood pooling (P ⬍ 0.05) (Fig. 6). BP. Similar results between groups were obtained in diastolic (P ⫽ 0.25) and mean (P ⫽ 0.702) BP (Fig. 7). In contrast, systolic BP in the High group decreased from ⫺10mmHg LBNP (P ⬍ 0.05). Systolic BP in the Low group did not become significantly lower than baseline until ⫺40-mmHg LBNP (P ⬍ 0.05) (Fig. 7); however, variability was higher in the Low group. Fig. 5. Heart rate (HR) responses during graded LBNP up to ⫺40 mmHg in the low-tolerance group and ⫺60 mmHg in the high-tolerance group. Values are means ⫾ SE; n, no. of subjects. *P ⬍ 0.05 vs. control; #P ⬍ 0.05 from previous values. Fig. 7. Systolic, mean, and diastolic blood pressure responses during graded LBNP up to ⫺40 mmHg in the low-tolerance group (open symbols) and ⫺60 mmHg in the high-tolerance group (solid symbols). Values are means ⫾ SE; n, no. of subjects. *P ⬍ 0.05 vs. control; #P ⬍ 0.05 from previous values. J Appl Physiol • VOL DISCUSSION In this study, we have compared leg vasoconstrictor responses to orthostatic venous pooling rather than level of LBNP. This novel approach to elicit a better understanding of the differences between low and high orthostatic tolerance has led to the major finding of vasoconstriction (estimated by oxygenated Hb in the selective deep portion of the calf) in both groups, increased at similar rates, but that the onset of vasoconstriction was delayed in the High group. Furthermore, greater HR increments in the Low group at given blood pooling (physiological stress) was also observed. One possible reason 109 • OCTOBER 2010 • www.jap.org 1000 CALF VASOCONSTRICTION WITH VENOUS POOLING DURING LBNP is that, as reported by Arbeille et al. (2), extra blood is released from the splanchnic region of tolerant subjects, and, therefore, vasoconstrictor responses in lower legs can be delayed. Responses in the calf. Although we hypothesized that calf oxygenated Hb in the High group would decrease more compared with that in the Low group, our results showed no significant difference between High and Low groups when the slopes of the regression analysis between oxygenated Hb and BV were compared (P ⫽ 0.152, Fig. 3). However, the x-axis intercept of the regression line in the High group was greater than that in the Low group (P ⬍ 0.05) and was positive (P ⬍ 0.05). Since oxygenated Hb values never increased, these results indicate a delayed oxygenated Hb reduction in the High group. It has been postulated that vasoconstriction may not occur in some participants during moderate LBNP (⫺15 mmHg) due to vasoconstriction reserve (5). Cook and Convertino (5) observed that MSNA bursts in their presyncopal participant increased 200% from baseline by ⫺15 mmHg, whereas their non-presyncopal participant did not exhibit any significant increase. Our results also indicate that participants with low orthostatic tolerance exhibit vasoconstrictor responses at early stages of an orthostatic stressor. Blood pooling in the lower body evaluated by mercury strain-gauge plethysmography between the groups was not statistically different up to ⫺40-mmHg LBNP, although blood accumulation in the Low group was slightly slower than that in the High group (Fig. 2). However, peak accumulation in the High group was greater than that in the Low group. These results are in accordance with previous observations by Sather et al. (22), who demonstrated that the High group exhibited higher peak midthigh-leg volume increases during LBNP. The ability of the high-tolerance participants to hold larger BV in the lower limbs seems counterintuitive, since vasoconstriction plays a key role to maintain MAP and reduces blood supply to the lower extremities. Sympathetic discharges to muscle vasculatures, as well as vasoactive hormones, such as reninangiotensin system and vasopressin-induced vasoconstriction. However, these hormones also act on kidneys to increase plasma retention. Plasma renin-angiotensin activities were reportedly consistently higher in the high- compared with lowtolerance individuals (4, 9). A greater increase in vasopressin in participants with high compared with the low orthostatic tolerance has been reported (4, 9). These plasma vasoreactive hormones may contribute to retention of plasma volume and subsequently allow the high-tolerance individuals to withstand higher blood pooling in the lower limbs during the 25–30 min of graded LBNP. Arbeille et al. (2) indicated that, after head-down bed rest, portal vein cross-sectional area, which was considered to be in proportion to the splanchnic blood flow (2), decreased in HUT test finishers, but, nonfinishers did not exhibit any change during LBNP. It is generally accepted that vasoconstriction in the legs is an important factor to prevent excess blood pooling (19). Furthermore, Xiao et al. (30) indicated that tilt-tolerant subjects showed high calf compliance and resistance during HUT test before head-down bed rest. Thus we have attempted to investigate the relationship of these two parameters by presenting vasoconstrictor responses as a function of blood pooling to better clarify their interrelationship. BP and HR responses. The HR response to LBNP was nonlinear, with the greatest increment occurring in the latter J Appl Physiol • VOL stages of LBNP: ⫺20 to ⫺40 mmHg in the Low group and ⫺40 to ⫺60 mmHg in the High group (Fig. 5). When expressed as function of calf volume accumulation, HR rose more rapidly in the Low compared with the High group (P ⬍ 0.05) (Fig. 6). Since there were no group differences in baseline and peak HR, as well as in BV accumulation as a function of LBNP, this may provide further evidence that low tolerance is related to less vascular capacity (22) and attenuated baroreflex sensitivity (7) to orthostatic stress than high tolerance. Given that MAP was maintained up to ⫺40 mmHg in all participants, it is likely that a greater increase in HR and earlier vasoconstriction was required to prevent a reduction in mean BP in the Low compared with the High group. This would imply an earlier sympathetic activation with BV accumulation in the Low compared with High group. Thus it seems that tolerant individuals have room to delay occurrence of vasoconstriction, possibly due to sufficient blood supply from the splanchnic region, since vasoconstriction in that region has been observed in HUT (24) and LBNP (14). NIRS estimates of vasoconstriction and venous volume in the calf. Since adipose tissue thicknesses may affect NIRS values, we measured the adipose tissue thickness for each site in a subgroup of this study (n ⫽ 13) by skinfold calliper. The calf thickness was 4.2 ⫾ 0.5 mm. Although we did not measure adipose tissue thickness at the exact site of the NIRS (26) probes for all of our participants, the selective deep-calf NIRS measurement with two detectors excluded the majority of vascular responses in skin and subcutaneous layers (16) to a depth of up to 2.0 cm in calf NIRS measurements. Thus the NIRS values in the selective deep-calf portion should not have been affected substantially by the fat tissue thickness. Finally, in a previous study (10), our laboratory suggested that deoxygenated Hb might reflect venous accumulation within the calf during LBNP. Similar results were observed for the relationship between oxygenated Hb and deoxygenated Hb (Fig. 4) as the comparison of oxygenated Hb to strain-gauge plethysmography BV (Fig. 3). The very close relationship observed indicates that deoxygenated Hb may be used for estimating lower limb venous pooling during orthostatic stress. Summary. The data did not support our hypothesis that participants with low tolerance to LBNP would have reduced vasoconstriction compared with participants with high tolerance to LBNP. The slope of oxygenated Hb compared with BV accumulation in the calf was the same between groups. Instead, we observed a delay in the onset of oxygenated Hb reductions to blood pooling in the group with high orthostatic tolerance. This early blood flow reduction in the Low group was presumably due to a lack of reserved BV, mainly from the splanchnic region (2, 24), or limited vasoconstrictor capacity (5). By the same token, the considerable HR increments from ⫺20- to ⫺40-mmHg LBNP found in the Low group were seen later in the High group from ⫺40- to ⫺50-mmHg LBNP, and greater HR increments with blood pooling were observed in the Low compared with the High group. The High group may maintain stable mean BP and venous return through release of BV to central circulation from other vascular beds, such as the splanchnic region. GRANTS This work was supported by funds to M. Saito from the Toyota High-Tech Research Program, and a Grant-in-Aid for Scientific Research from the Japan 109 • OCTOBER 2010 • www.jap.org CALF VASOCONSTRICTION WITH VENOUS POOLING DURING LBNP Society for the Promotion of Science (nos. 13680064 and 15500464). A. P. Blaber was funded by the Canadian Space Agency (no. 9F007-020213/001/ST). DISCLOSURES No conflicts of interest, financial or otherwise, are declared by the author(s). REFERENCES 1. Abe T, Tanaka F, Yoshikawa K, Fukunaga T. Total and segmental subcutaneous adipose tissue volume measured by ultrasound. Med Sci Sports Exerc 28: 908 –912, 1996. 2. Arbeille P, Besnard SS, Kerbeci PP, Mohty PM. Portal vein crosssectional area and flow and orthostatic tolerance: a 90-day bed rest study. J Appl Physiol 90: 1853–1857, 2005. 3. Brown CM, Hainsworth R. Forearm vascular responses during orthostatic stress in control subjects and patients with posturally related syncope. Clin Auton Res 10: 57–61, 2000. 4. Convertino VA, Sather TM. Vasoactive neuroendocrine responses associated with tolerance to lower body negative pressure in humans. Clin Physiol 20: 177–184, 2000. 5. Cook WH, Convertino VA. Association between vasovagal hypotension and low sympathetic neural activity during presyncope. Clin Auton Res 12: 483–486, 2002. 6. El-Bedawi KM, Hainsworth R. Combined head-up tilt and lower body suction: a test of orthostatic tolerance. Clin Auton Res 4: 41–47, 1994. 7. El-Sayed H, Hainsworth R. Relationship between plasma volume, carotid baroreceptor sensitivity and orthostatic tolerance. Clin Sci (Lond) 88: 463–470, 1995. 8. Essandoh LK, Houston DS, Vanhoutte PM, Shepherd JT. Differential effects of lower body negative pressure on forearm and calf blood flow. J Appl Physiol 63: 994 –998, 1986. 9. Greenleaf JH, Petersen TW, Gabrielsen A, Pump B, Bie P, Christensen NJ, Warberg J, Videbaek R, Simonson SR, Norsk P. Low LBNP tolerance in men is associated with attenuated activation of the renin-angiotensin system. Am J Physiol Regul Integr Comp Physiol 279: R822–R829, 2000. 10. Hachiya T, Blaber A, Saito M. Near-infrared spectroscopy provides an index of blood flow and vasoconstriction in calf skeletal muscle during lower body negative pressure. Acta Physiol (Oxf) 193: 117–127, 2008. 11. Hachiya T, Blaber A, Saito M. Changes in superficial blood distribution in thigh muscle during LBNP assessed by NIRS. Aviat Space Environ Med 75: 118 –122, 2004. 12. Hansen J, Sander M, Hald CF, Victor G, Thomas D. Metabolic modulation of sympathetic vasoconstriction in human skeletal muscle: role of tissue hypoxia. J Physiol 527: 387–396, 2000. 13. Homma S, Eda H, Ogasawara S, Kagaya A. Near-infrared estimation of O2 supply and consumption in forearm muscles working at varying intensity. J Appl Physiol 80: 1279 –1284, 1996. 14. Hughson RL, Shoemaker JK, Arbeille P, O’Leary DO, Pizzollito KS, Hughes MD. Splanchnic and peripheral vascular resistance during lower body negative pressure (LBNP) and tilt. J Gravit Physiol 11: 95–96, 2004. J Appl Physiol • VOL 1001 15. Imadojemu VA, Lott ME, Gleeson K, Hogeman CS, Ray CA, Sinoway LI. Contribution of perfusion pressure to vascular resistance during head-up tilt. Am J Physiol Heart Circ Physiol 281: H371–H375, 2001. 16. Kashima S. Spectroscopic measurement of blood volume and its oxygenation in a small volume of tissue using red laser lights and differential calculation between two point detections. Opt Laser Technol 35: 485–489, 2003. 17. Levine BD, Buckey JC, Fritsch JM, Yancy JRCW, Watenpauch DE, Snell PG, Lane LD, Eckberg DL. Physical fitness and cardiovascular regulation: mechanisms of orthostatic intolerance. J Appl Physiol 70: 112–122, 1991. 18. Mancini DM, Bolinger L, Li H, Kendrick K, Chance B, Wilson JR. Validation of near-infrared spectroscopy in humans. J Appl Physiol 77: 2740 –2747, 1994. 19. Mano T, Iwase S. Sympathetic nerve activity in hypotension and orthostatic intolerance. Acta Physiol Scand 177: 359 –365, 2003. 20. McCully KK, Hamaoka T. Near-infrared spectroscopy: what can it tell us about oxygen saturation in skeletal muscle? Exerc Sport Sci Rev 28: 123–127, 2000. 21. Rowell LB .Orthostatic intolerance. In: Human Cardiovascular Control. New York: Oxford University Press, 1993. 22. Sather TM, Goldwater DJ, Montgomery LD, Convertino VA. Cardiovascular dynamics associated with tolerance to lower body negative pressure. Aviat Space Environ Med 57: 413–419, 1986. 23. Shiga T, Yamamoto K, Tanabe K, Nakase Y, Chance B. Study of an algorithm based on model experiments and diffusion theory for a portable tissue oximeter. J Biomed Opt 2: 154 –161, 1997. 24. Stewart JM, Medow MS, Glover JI, Montgomery LD. Persistent splanchnic hyperemia during upright tilt in postural tachycardia syndrome. Am J Physiol Heart Circ Physiol 290: H665–H673, 2006. 25. Stewart JM, Weldon A. The relation between lower limb pooling and blood flow during orthostasis in the postural orthostatic tachycardia syndrome of adolescents. J Pediatr 138: 512–519, 2001. 26. Van Beekvelt MC, Borghuis MS, Van Engelen BG, Wevers RA, Colier WN. Adipose tissue thickness affects in vivo quantitative near-IR spectroscopy in human skeletal muscle. Clin Sci (Lond) 101: 21–28, 2001. 27. Victor RG, Leimbach WN Jr. Effects of lower body negative pressure on sympathetic discharge to leg muscles in humans. J Appl Physiol 63: 2558 –2562, 1987. 28. Vissing SF, Scherrer U, Victor RG. Relation between sympathetic outflow and vascular resistance in the calf during perturbations in central venous pressure. Evidence for cardiopulmonary afferent regulation of calf vascular resistance in humans. Circ Res 65: 1710 –1717, 1989. 29. Whitney H. The measurements of volume changes in human limbs. J Physiol 121: 1–27, 1953. 30. Xiao X, Grenon SM, Kim C, Sheynberg N, Hurwitz S, Williams GH, Cohen RJ. Bed rest effects on human calf hemodynamics and orthostatic tolerance: a model-based analysis. Aviat Space Environ Med 76: 1037– 1045, 2005. 109 • OCTOBER 2010 • www.jap.org