Nutritional Immunology Nutritional Regulation of Porcine Bacterial-Induced Colitis by Conjugated Linoleic Acid
advertisement

Nutritional Immunology
Nutritional Regulation of Porcine Bacterial-Induced Colitis by Conjugated
Linoleic Acid1,2
Raquel Hontecillas,* Michael J. Wannemeulher,* Dean R. Zimmerman,† David L. Hutto,‡
Jennifer H. Wilson,* Dong U. Ahn† and Josep Bassaganya-Riera*,3
*Veterinary Medical Research Institute, Nutritional Immunology, College of Veterinary Medicine, Ames, IA
50011; †Department of Animal Science, Iowa State University, Ames, IA 50010; and
‡
U.S. Department of Agriculture–Animal and Plant Health Inspection Service, Ames, IA 50010
KEY WORDS: ● lipid nutrition
● growth suppression
●
colitis
●
conjugated linoleic acid
Nutritional immunology is a novel field of research that has
rapidly evolved from studying the basic mechanism(s) of immunomodulation (1,2) to applying this fundamental knowledge in
the development of nutritionally based therapies for both human
and animal diseases (3,4). Human epidemiological studies and
animal feeding trials have uncovered a role for nutrients and
nutraceuticals (5) in preventing or ameliorating chronic recurring
diseases (i.e., neoplasic, inflammatory or autoimmune). Inflammatory bowel disease (IBD4) is a chronic recurring illness that
●
interferon-␥
●
PPAR-␥
can be nutritionally controlled (6,7). Histopathological features
consistent with IBD include mucosal inflammation and ulceration with crypt abscesses, chronic mucosal damage and branching of the crypts (8). IBD is characterized by two diseases of
unknown etiology, Crohn’s disease (CD) and ulcerative colitis
(UC) (9). Although UC is typically a diffuse change without
segmentation that is confined to the colon, CD is characterized
by segmental distribution with sharply demarcated boundaries
and may occur in any section of the gastrointestinal tract. Inflammatory lesions of the porcine colonic mucosa triggered by the
bacterial enteric pathogen Brachyspira hyodysenteriae resemble
those of human CD. Similarly to what occurs in 65 to 75% of
patients with CD (10,11), B. hyodysenteriae–induced colitis results in weight loss. Furthermore, in both human IBD and B.
hyodysenteriae–induced colitis, an immunoinflammatory etiology
contributes to the mucosal damage associated with the onset of
enteric disease (12,13).
Predisposition to IBD is controlled in part by genetic factors
(14 –16). However, environmental influences including nutrition may contribute to either preventing or promoting the
onset of disease. Nutritional interventions that ameliorate
IBD, both dietary 1,25-dihydroxycholecalciferol (6) and (n-3)
1
Presented in part at the FASEB 2002 meeting, April 20 –24, 2002, New
Orleans, LA [Bassaganya-Riera, J., Hontecillas, R., Zimmerman, D. R., Hutto,
D. L., Ahn, D. U. & Wannemuelher, M. J. Nutritional regulation of bacterial-induced
colitis by conjugated linoleic acid A26 (abs.)]. FASEB J 16(4): 26
2
Supported by the National Pork Board (grant 01134, awarded to J.B.-R.).
3
To whom correspondence should be addressed.
E-mail: bassy@iastate.edu.
4
Abbreviations used: ADFI, average daily feed intake; ADG, average daily
gain; CD, Crohn’s disease; CLA, conjugated linoleic acid; DSS, dextran sulfate
sodium; 15d-PGJ2, 15-deoxy-⌬12,14-prostaglandin J2; FACS, fluorescence-activated cell sorting; HBSS, Hanks’ balanced salt solution; IBD, inflammatory bowel
disease; IEL, intraepithelial lymphocyte; IFN-␥, interferon-␥; IL-10, interleukin-10;
PBMC, peripheral blood mononuclear cell; PPAR-␥, peroxisome proliferatoractivated receptor-␥; PUFA, polyunsaturated fatty acid; SP, single-positive; TCR,
T-cell receptor; UC, ulcerative colitis.
0022-3166/02 $3.00 © 2002 American Society for Nutritional Sciences.
Manuscript received 11 February 2002. Initial review completed 18 March 2002. Revision accepted 10 April 2002.
2019
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010
ABSTRACT Excessive intake of saturated fatty acids and/or linoleic acid favors the induction of an array of
lipid mediators and cytokines enhancing inflammatory responses. Conversely, dietary supplementation with
(n-3) fatty acids or vitamin D ameliorates inflammation and autoimmune diseases. Although it was well
accepted that conjugated linoleic acid (CLA) prevented diseases with a common inflammatory pathogenesis
(i.e., cancer and atherosclerosis), no studies were available on the roles of CLA in mucosal inflammation. The
present study was designed to investigate the anti-inflammatory actions and molecular mechanisms underlying the regulation of colonic health by CLA. We hypothesized that colonic inflammation can be ameliorated
by dietary CLA supplementation. To test this hypothesis, inflammation of the colonic mucosa was triggered by
challenging pigs fed either soybean oil–supplemented or CLA-supplemented diets with an enteric bacterial
pathogen (i.e., Brachyspira hyodysenteriae). Immunoregulatory cytokines and peroxisome proliferator-activated receptor-␥ (PPAR-␥) mRNA expression were assayed in colonic lymph nodes and colon of pigs. Colonic
mucosal lesions and lymphocyte subset distribution were evaluated by histology and immunohistochemistry.
Supplementation of CLA in the diet before the induction of colitis decreased mucosal damage; maintained
cytokine profiles (i.e., interferon-␥ and interleukin-10) and lymphocyte subset distributions (i.e., CD4⫹ and
CD8⫹), resembling those of noninfected pigs; enhanced colonic expression of PPAR-␥; and attenuated growth
failure. Therefore, CLA fed preventively before the onset of enteric disease attenuated inflammatory lesion
development and growth failure. J. Nutr. 132: 2019 –2027, 2002.
HONTECILLAS ET AL.
2020
MATERIALS AND METHODS
Experimental design. Two experiments were performed using a
total of 64 pigs (ISU swine nutrition farm, Ames, IA) with an initial
body weight of 4.8 –5.5 kg. Pigs were weaned at 14 d, penned
individually, fed experimental diets with free access to water and
handled according to the practices of animal care established by the
Committee of Animal Care at Iowa State University. In both experiments, to decrease variation, blocks of pigs were designed based on
litter of origin, initial body weight, age and gender. On d 0, antibody
titers of the 64 pigs to B. hyodysenteriae were tested by using an ELISA
as previously described (30) and found to be negative.
Experiment 1. A total of 16 pigs (i.e., eight blocks of two pigs
each) were distributed into two dietary treatments: soybean oil–
supplemented diet (n ⫽ 8) or conjugated linoleic acid–supplemented
diet (n ⫽ 8) and fed the experimental diets for 72 d before the
induction of colitis. Before challenging four of the blocks of pigs, the
experimental design was a randomized complete block. After oral
challenge with B. hyodysenteriae of four of the blocks, it became a 2
⫻ 2 factorial arrangement within a split-plot design.
Experiment 2. A total of 48 pigs (i.e., 16 blocks of three pigs each)
were distributed into three immunomodulatory (i.e., diet or immunization) treatments: 1) soybean oil–supplemented diet (n ⫽ 16), 2)
conjugated linoleic acid–supplemented diet (n ⫽ 16) or 3) soybean
oil–supplemented diet and immunized with a proteinase-digested B.
hyodysenteriae bacterin. Pigs in expt. 2 were fed the experimental diets
for 49 d before challenge.
Before challenging eight of the blocks of pigs, the experimental
design was a randomized complete block. After oral challenge with B.
hyodysenteriae of eight of the blocks, it became a 2 ⫻ 3 factorial
arrangement within a split-plot design. Pigs within the block were the
experimental units for dietary treatment, and blocks of three pigs
each were the experimental units for challenge status (i.e., infected or
noninfected).
Dietary and immunization treatments. Either a 1.33 g CLA/100
g of diet or an isocaloric and isonitrogenous soybean oil–supplemented control diet (Table 1) was randomly allotted to pens within
blocks as previously described (24). Before challenge, pigs were given
free access to feed for 72 d in four phases (I, 1 to 2 wk; II, 3 to 4 wk;
III, 5 to 8 wk; and IV, 9 to 11 wk) and 49 d in three phases (I, 1 to
2 wk; II, 3 to 4 wk; and III, 5 to 7 wk) in the first and second studies,
respectively. Between treatments, diets were formulated to be isocaloric and isonitrogenous to avoid energy- and/or protein-derived
immunological changes (31,32). Thus, in control diets, 2.21 g CLA
source/100 g of diet was replaced by 2.21 g soybean oil/100 g of diet
to maintain both the CLA-supplemented and the control diets isocaloric within phases. Pigs were fed either a CLA-supplemented or a
control diet for the entire experimental period. The CLA source was
alkali-isomerized sunflower oil (ConLinco, Detroit Lakes, MN). Diets
were formulated to maintain or exceed current recommended nutritional requirements of the National Research Council (33) for pigs.
In the second experiment, on d7, d21 and d35, the immunization
treatments (i.e., squalene control, or proteinase-digested B. hyodysenteriae bacterin) were randomly assigned to half of the blocks. Pigs
were intramuscularly (i.m.) inoculated with 2 mL of a proteinasedigested B. hyodysenteriae bacterin strain B204 in squalene as previously described (30). Pigs, feeders and feed were weighed on a weekly
basis before and after challenge to evaluate modifications in growth
TABLE 1
Composition of control diets (as-fed basis)
Control diets1
Item
Phase I
Phase II
Phase III
Phase IV
g/100 g
Ingredient
Corn
Soybean meal (48% CP)
Dried whey
Spray-dried plasma
Dried blood cells
Dry skim milk
CLA mixture2
Soybean oil
DL-Methionine
L-Lysine
Sodium chloride
Dicalcium phosphate
Calcium carbonate
Vitamin premix3
Trace mineral premix4
Selenium premix5
Calculated composition, %
Crude protein
Lysine
Methionine ⫹ cystine
Calcium
Phosphorus available
Metabolizable energy, MJ/
kg
32.69
12.00
22.00
7.50
—
21.00
—
2.21
0.18
—
0.25
1.09
0.78
0.20
0.05
0.05
49.59
21.20
17.00
3.00
2.00
1.50
—
2.21
0.23
0.19
0.25
1.72
0.81
0.20
0.05
0.05
63.08
31.00
—
—
0.50
—
—
2.21
0.07
0.20
0.25
1.60
0.79
0.20
0.05
0.05
72.36
22.00
—
—
—
—
—
2.21
0.12
0.39
0.25
1.50
0.90
0.20
0.05
0.05
24.36
1.76
0.97
1.05
0.70
21.17
1.50
0.86
0.93
0.55
20.30
1.30
0.71
0.75
0.35
16.43
1.15
0.65
0.70
0.30
14.43
14.15
14.25
14.27
1 Phase I, 1–2; II, 3– 4; III, 5–7; and IV, 8 –9 wk.
2 In CLA-supplemented diets 2.21% of CLA-60 was replaced by
2.21% of soybean oil to maintain the diets isocaloric within phases.
3 Supplied per kg diet: retinyl acetate, 1516 g; cholecalciferol, 26
g; dl-␣-tocopheryl acetate, 22 mg; riboflavin, 6.6 mg; pantothenic
acid, 17.6 mg; niacin, 33 mg; and vitamin B-12, 22 g.
4 Supplied per kg diet: Zn, 165 mg (ZnO); Fe, 193 mg (FeSO4 䡠 H2O);
Mn, 66 mg (MnO); Cu, 19.29 mg (CuSO4 䡠 5H2O); and I, 0.2 mg
(ethylene diamine dihydroiodide).
5 Supplied per kg diet: Se, 0.1 mg (Na2SeO3).
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010
polyunsaturated fatty acids (PUFA) (7), have been shown to
attenuate the symptoms of IBD. Vitamin D status modulates
the enteric immune and inflammatory dysfunction by targeting
vitamin D receptors (VDR) (17), whereas the targets for
PUFA and their bioactive derivatives (18) are peroxisome
proliferator-activated receptors (PPAR) (19). PPAR are novel
members of the nuclear receptor superfamily with several
isoforms (␣,  and ␥), of which PPAR-␥ is the predominant
isoform in immune cells and enterocytes. Functionally,
PPAR-␥ agonists modulate immune function (20) and decrease mucosal inflammation (21,22).
Two factors determine the role of lipid nutrition in health
and disease: 1) the composition and 2) the total amount of fat
in the diet (23). The present study was designed to examine
the cellular and molecular mechanisms by which the dietary
fatty acid composition modulates colonic health. More specifically, we examined the direct influence of conjugated linoleic
acid (CLA) on mucosal inflammation. CLA is a mixture of
positional (9,11; 10,12; 11,13; etc.) and geometric (cis or trans)
isomers of octadecadienoic acid with conjugated double bonds.
We previously demonstrated that dietary CLA supplementation enhances the numbers of peripheral blood CD8⫹ T-cells
(24). Depletion of this T-cell subset exacerbated inflammatory
lesions in a murine model of respiratory disease (25).
On the basis of the preventive role of dietary CLA on
diseases with an inflammatory pathogenesis (26 –28), the
CLA-induced immunomodulation of CD8⫹ cells (29) and
because PPAR-␥ agonists prevented murine experimental IBD
(21,22), we hypothesized that colonic inflammation can be
ameliorated by dietary CLA supplementation. To test this
hypothesis, pigs were challenged with an enteric bacterial
pathogen (i.e., B. hyodysenteriae). Through the bacterial challenge of pigs fed either a control or CLA-supplemented diet,
we were able to investigate the role of CLA on the progression
of enteric inflammatory diseases.
LIPID NUTRITION AND GASTROINTESTINAL HEALTH
Histopathological and immunohistochemical evaluation of colonic samples. Hematoxilin-eosin (H&E)–stained colonic sections
were histologically evaluated on the basis of mucosal thickness (i.e.,
expressed as crypt depth as a function of crypt width) and epithelial
erosions [i.e., 1) no erosion, 2) mild erosion and 3) severe erosion].
H&E slides were labeled with accession numbers lacking any reference to either the immunomodulatory or infective treatment and
were evaluated by a board-certified pathologist.
For the evaluation of colonic lymphocyte subset distributions,
frozen colonic tissue sections embedded in tissue-freezing medium
were cut on a cryostat at ⫺18°C at thicknesses from 5 to 10 m.
Sections were placed on poly-L-lysine– coated slides, fixed in 95%
methanol for 2 min and soaked in cryopreservative (0.5 mol/L sucrose, 0.006 mol/L MgCl2, 50% glycerol) for 10 min. Slides were
stored at ⫺20°C until stained. Before staining tissues with monoclonal antibodies, slides were warmed to room temperature and rehydrated in 0.5 mol/L Tris solution. Endogenous peroxidase activity was
blocked by adding 0.3% hydrogen peroxide for 10 min. Nonspecific
binding was blocked with the addition of the immunohistochemistry
buffer containing 5% normal goat serum/3% bovine serum albumin/
Tris buffer (NGS/BSA/Tris) solution at room temperature for 2 h.
Slides were incubated with the primary antibody solution overnight
at 4°C. Primary antibodies were diluted in NGS/BSA/Tris. Mouse
anti-pig CD4 primary antibody was 10⫻ supernatant from the mouse
cell line HB147 used at 1:25 dilution. Mouse anti-pig CD8␣ antibody
was supernatant from the mouse cell line HB143 used at 1:100
dilution. Both antibodies were grown in our laboratory. The mouse
anti-pig TCR␥␦ (Po-Tcr1-N4) antibody was purchased from VMRD
(Pullman, WA) and used at 1:100 dilution. The mouse anti-pig CD3
was concentrated supernatant from the mouse cell line 8E6 and used
at 1:10,000 dilution. Before the incubation with the secondary antibodies, slides were rinsed with Tris solution to wash unbound primary
antibody. Peroxidase-conjugated goat anti-mouse IgG (H ⫹ L) (Jackson ImmunoResearch, West Grove, PA) was added to slides stained
with mouse anti-pig CD4, mouse anti-pig CD3 and mouse anti-pig
TCR␥␦. The goat anti-mouse IgG (H ⫹ L) was diluted 1:300 with
NGS/BSA/Tris and incubated for 2 h at room temperature. For the
mouse anti-pig CD8␣ primary antibody, the secondary used was
biotin-conjugated goat F(ab⬘)2 anti-mouse IgG2a (Southern Biotechnologies Associates, Birmingham, AL) diluted 1:250 (in NGS/BSA/
Tris), and incubated for 2 h at room temperature. After the second
incubation, slides were treated with peroxidase-conjugated strepavidin, diluted in Tris solution (1:500) and incubated for 1 h at room
temperature. The chromagen used was diaminobenzediene (Biomedia
Corporation, Foster City, CA). Slides were counterstained with Instant Hematoxylin (Shandon, Pittsburg, PA), coverslipped with
Immu-mount (Shandon) and numbers of CD4⫹, CD8␣⫹, CD3⫹ and
TCR␥␦⫹ cells enumerated. Stained colonic sections were observed at
⫻400 magnification. Five randomly chosen sections (i.e., area 0.375
mm2) were enumerated for each pig and antibody treatment. Data
were presented as number of cells per square millimeter.
Isolation of total RNA. Colonic lymph nodes and colonic tissue
were recovered during the necropsy procedure and kept in RNAlater
(Ambion) at ⫺70°C. Total RNA was isolated using the total RNA
isolation MiniKit (Qiagen, Valencia, CA), treated with DNA-free
(Ambion) and kept in 0.02% diethyl pyrocarbonate (DEPC)–treated
water at ⫺20°C according to the manufacturer’s instructions. RNA
in samples were quantified, and the purity was determined using a
spectrophotometer at an optical density (OD)260 and OD260/OD280
ratios, respectively. All samples had OD260/OD280 ratios above 1.80,
corresponding to 90 –100% pure nucleic acid.
Reverse-transcriptase–polymerase chain reaction (RT-PCR).
Expression of interleukin-10 (IL-10), interferon-␥ (IFN-␥), PPAR-␥
and 2-microglobulin (i.e., housekeeping gene) in colonic lymph
nodes was determined using the RT-PCR procedure. Briefly, after
isolation of total RNA, 1 g of each RNA isolate from each pig was
added to a 5-L DNA digestion reaction containing 4 L of M-MLV
RT reaction buffer (Promega, Madison, WI), 0.4 L of RNase-free
water, 0.5 L of SUPERase In (Ambion) and 0.1 L of Dnase I
(Sigma Chemical, St. Louis, MO). Cycle parameters for DNA digestion were 1 cycle of 37°C, 15 min; 1 cycle of 94°C, 10 min; 1 cycle
of 4°C, 5 min. For the melting of the secondary structure, 1 L of
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010
[i.e., average daily gain (ADG)] and appetite [i.e., average daily feed
intake (ADFI)].
Bacterial challenge. Brachyspira hyodysenteriae strain B204 was
grown under anaerobic conditions in trypticase soy broth (Becton
Dickinson, Cockeysville, MD) supplemented with 5% horse serum
(Hyclone; Logan, Utah), 0.5% yeast extract (Difco, Detroit, MI) and
VPI salts. All cultures used for infection studies were ⬎ 90% motile
and had been passed in vitro 23 to 25 times. Challenge inoculum
consisted of two doses of 1010 B. hyodysenteriae organisms given orally
on 2 consecutive days (i.e., d72 and d73 or d49 and d50 in expt. 1 and
expt. 2, respectively) that was administered to half of the blocks of
pigs. Challenge inoculum was given 14 d after the third vaccination
in vaccinated pigs of expt. 2. B. hyodysenteriae is the causative agent
of the porcine dysentery.
Determination of fat content and fatty acid analyses. Fat content in the diet was determined by weighing 2 g of sample into a
50-mL test tube with 20 mL solvent (chloroform:methanol ⫽ 2:1,
v/v), and homogenized with a Brinkman polytron (Type PT 10/35)
for 10 s at high speed. Butylated hydroxyanisole (BHA, 10%) dissolved in 98% ethanol (25 g) was added to the sample before
homogenization. The homogenate was filtered through a Whatman
no. 1 filter paper (Whatman, Clifton, NJ) into a 100-mL graduated
cylinder to which was added 5 mL of a solution of 8.8 g NaCl/L. After
the cylinder was capped with a glass stopper, the filtrate was mixed
well. The inside of the cylinder was washed twice with 10 mL of Folch
2 (CHCl3:CH3OH:H2O ⫽ 3:47:48), and the contents were stored
until the aqueous and organic layers clearly separated. The upper
layer was siphoned off and 400 mL of the lower layer (chloroform
layer) was transferred to a 20-mL test tube and dried at 50°C under
nitrogen flow. Fatty acid analyses (triplicate sample readings from
each diet) of diets were conducted using a Hewlett–Packard (HP)
6890 gas chromatograph (Hewlett–Packard, Wilmington, DE)
equipped with an autosample injector and flame-ionization detector
(FID). A combined column [HP-225 column (7.5 m, 0.25 mm i.d.,
0.25 m nominal), an HP wax column (15 m, 0.25 mm i.d., 0.25 m
nominal) and an HP wax column (30 m, 0.25 mm i.d., 0.25 m
nominal) that were connected using zero dead-volume column connectors (J & W Scientific, Folsom, CA)] was used to improve separation. A split inlet (19:1) was used to inject samples (1 L) into the
capillary column. Ramped oven-temperature conditions (180°C for 1
min, increased to 230°C at 2.5°C/min, then held at 230°C for 14
min) were used. Temperatures of both inlet and detector were 280°C.
Helium was used as a carrier gas, and a constant column flow of 1.1
mL/min was used. Detector (FID) air, H2, and make-up gas (He) flows
were 350, 35 and 43 mL/min, respectively. The composition of fatty
acids was calculated as percentage composition of total peak area
(pA䡠s). Column performance and detector response were verified
using commercially available (Nu-Chek-Prep, Elysian, MN) fatty
acid standards {e.g., myristic (14:0), palmitic (16:0), palmitoleic [16:
1(n-9)], heptadecanoic [17:1(n-9)], stearic (18:0), oleic [18:1(n-9)],
linoleic [18:2(n-6)], linolenic [18:3(n-3)], arachidic (20:0), arachidonic [20:4(n-6)], eicosapentanoic [20:5(n-3)], docosapentanoic [22:
5(n-3)], docosahexanoic [22:6(n-3)], c9,t11 CLA, t10,c12 CLA,
t9,t11 CLA and c10,c12 CLA}.
Necropsy procedures. Pigs were anesthetized by administration
of Rompun (Bayer, Shawnee, KS)/Telazol (Fort Dodge Laboratories,
Fort Dodge, IA) i.m. and euthanized via electrocution. Peripheral
blood (40 mL) was collected from the subclavian vein into 50-mL
conical tubes containing 5 mL of PBS with 1000 U of heparin
(Elkins-Sinn, Cherry Hill, NJ). At necropsy, swabs of cecal and spiral
colon contents were streaked onto modified BJ blood agar plates
containing antibiotics for isolation of B. hyodysenteriae (35). Sections
of spiral colon and cecum were obtained, fixed in 10% buffered
formalin, later embedded in paraffin and then sectioned for histological examination. Samples of colon and mesenteric lymph nodes were
embedded in RNAlater (Ambion, Austin, TX) for posterior isolation
of total RNA and analysis of cytokine expression (colonic samples).
For immunohistochemistry, samples of colonic tissue were placed in
tissue-freezing medium (Triangle Biomedical Sciences, Durham, NC)
and snap-frozen in an ethanol/dry ice bath. Both samples for mRNA
expression analysis and for immunohistochemistry were stored at
⫺70°C.
2021
HONTECILLAS ET AL.
2022
ance (ANOVA) was used to determine the main effects of the
immunomodulatory treatment (control diet, CLA-supplemented
diet, or vaccine), the infective status (i.e., infected or noninfected)
and the interaction between immunomodulatory treatment and infective status. ANOVA was performed using the general linear model
(GLM) procedure of the SAS software using the TEST statement to
define the whole plot and subplot within the model in the program
(37). Differences with P ⬍ 0.05 were considered significant. In expt.
2, the whole plot error (i.e., error A) is the block within infective
status [i.e., 14 degrees of freedom (df)] and the subplot error (i.e.,
error B) is the residual degrees of freedom after accounting for the
immunomodulatory treatment (i.e., diet or immunization) variance
and the variance for the interaction between immunomodulatory
treatment and infective status (i.e., 28 df). The statistical model used
in expt. 2 was Yijk ⫽ ⫹ Infectioni ⫹ error Aik ⫹ Immunomodulationj ⫹ (Infection ⫻ Immunomodulation)ij ⫹ error Bijk, where is
the general mean, Infectioni is the main effect of the ith level of the
challenge effect, Immunomodulationj is the main effect of the jth
level of the immunomodulatory effect, (Infection ⫻ Immunomodulation)ij is the interaction effect between infection and immunomodulation, and errors A and B represent the random errors for the
whole plot and the subplot, respectively. Data for expt. 1 were
analyzed similarly using the following model: Yijk ⫽ ⫹ Infectioni ⫹
error Aik ⫹ Dietj ⫹ (Infection ⫻ Diet)ij ⫹ error Bijk. In expt. 1, the
whole plot error (i.e., error A) is the block within infective status
(i.e., 6 df) and the subplot error (i.e., error B) is the residual degrees
of freedom after accounting for the dietary treatment variance and
the variance for the interaction between dietary treatment and infective status (i.e., 6 df).
RESULTS
Analysis of fatty acid composition and fat content of the
diets. The major difference between dietary treatments
was the presence of CLA isomers in the CLA-supplemented
diet, replacing primarily linoleic acid from the control diet
(Table 2). The concentration of palmitic acid (16:0) was
TABLE 2
Fatty acid composition and fat content of diets (as-fed basis)1
Control diets (soybean oil-supplemented)2,3
Item
Phase I
Phase II
Phase III
CLA-supplemented diets3,4
Phase IV
Phase I
Phase II
Phase III
Phase IV
0.88 ⫾ 0.02
9.08 ⫾ 0.09
0.11 ⫾ 0.01
3.27 ⫾ 0.02
0.34 ⫾ 0.01
31.73 ⫾ 0.17
20.85 ⫾ 0.06
9.13 ⫾ 0.01
9.73 ⫾ 0.01
4.47 ⫾ 2.08
10.12 ⫾ 2.16
0.15 ⫾ 0.04
—
4.43 ⫾ 0.07
0.44 ⫾ 0.01
9.28 ⫾ 0.08
0.07 ⫾ 0.01
5.56 ⫾ 0.07
0.20 ⫾ 0.02
26.18 ⫾ 0.02
24.22 ⫾ 1.03
10.24 ⫾ 0.20
12.43 ⫾ 0.20
4.32 ⫾ 0.61
7.07 ⫾ 0.26
0.12 ⫾ 0.01
—
5.24 ⫾ 0.24
—
9.43 ⫾ 0.01
0.08 ⫾ 0.03
2.42 ⫾ 0.02
0.16 ⫾ 0.01
29.87 ⫾ 0.16
31.73 ⫾ 0.30
7.64 ⫾ 0.18
9.02 ⫾ 0.23
3.58 ⫾ 0.04
4.23 ⫾ 0.09
0.10 ⫾ 0.02
0.47 ⫾ 0.05
5.38 ⫾ 0.02
—
9.37 ⫾ 0.03
0.08 ⫾ 0.01
2.40 ⫾ 0.09
0.22 ⫾ 0.01
28.02 ⫾ 0.01
34.02 ⫾ 1.17
8.42 ⫾ 0.31
8.13 ⫾ 0.35
4.10 ⫾ 0.15
2.84 ⫾ 0.13
2.11 ⫾ 0.14
—
5.65 ⫾ 0.10
g/100 g
Fatty acid
Myristic acid
Palmitic acid
Margaric acid
Stearic acid
Palmitoleic acid
Oleic acid
Linoleic acid
c9, t11 CLA
t10, c12 CLA
t9, t11 CLA
Other CLA isomers
Linolenic acid
Arachidonic acid
Ether extract
1.10 ⫾ 0.01
14.76 ⫾ 0.11
0.16 ⫾ 0.03
5.76 ⫾ 0.00
0.31 ⫾ 0.03
28.83 ⫾ 0.32
49.12 ⫾ 0.47
—
—
—
—
0.17 ⫾ 0.08
—
4.54 ⫾ 0.13
0.49 ⫾ 0.00
13.61 ⫾ 0.18
0.14 ⫾ 0.01
5.76 ⫾ 0.25
0.26 ⫾ 0.01
28.13 ⫾ 0.65
51.85 ⫾ 0.58
—
—
—
—
0.18 ⫾ 0.06
—
5.17 ⫾ 0.15
—
12.89 ⫾ 0.28
0.12 ⫾ 0.01
3.25 ⫾ 0.28
0.14 ⫾ 0.02
30.26 ⫾ 0.81
52.83 ⫾ 0.88
—
—
—
—
0.20 ⫾ 0.03
0.65 ⫾ 0.05
5.41 ⫾ 0.01
—
12.43 ⫾ 0.18
0.11 ⫾ 0.01
3.68 ⫾ 0.05
0.08 ⫾ 0.11
27.58 ⫾ 0.71
54.75 ⫾ 0.59
—
—
—
—
2.15 ⫾ 0.33
—
5.67 ⫾ 0.06
1 Values are means ⫾ SEM; n ⫽ 8.
2 In control diets, the soybean oil contained cis-9, cis-12 linoleic acid (51.83%), oleic acid (30.35%), palmitic acid (12.33%), stearic acid (4.63%),
and palmitoleic acid (0.50%) representing 46.47% of the fatty acids within the CLA source.
3 Phase I, 1–2 wk; II, 3– 4 wk; III, 5–7 wk; and IV, 8 –9 wk. Within phases control and CLA-supplemented diets were isocaloric and isonitrogenous.
4 In CLA-supplemented diets, 2.21% of CLA-60 was replaced by 2.21% of soybean oil to maintain the diets isocaloric within phases. The source
of CLA contained: 1) a conjugated diene-enriched fraction with c9,t11/t9,c11 (12.36%), t10,c12/c10,t12 (13.30%), t9,t11 (13.32%), and other CLA
isomers (12.99%) representing 51.97% of the fatty acids within the CLA source and 2) a fraction of fatty acids not containing conjugated double
bonds: palmitoleic (4.37%), linoleic (1.27%), oleic (38.70%) and stearic (2.13%).
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010
Promega random hexamers were added to the digested RNA. Cycle
parameters for the melting reaction were 1 cycle of 94°C, 5 min.
After the melting reaction, the reaction mixture was placed onto ice
for 1 min. RNA was then reverse transcribed in a 10-L reaction
containing 6 L of the previously described reactions plus 1 L of
M-MLV RT reaction buffer (Promega), 1.25 L Sigma dNTP mix,
0.75 L of RNase-free water and 1 L of Promega M-MLV RT (200
U reverse transcriptase/L). Cycle parameters for the reverse-transcription procedure were 1 cycle of 37°C, 60 min; 1 cycle of 94°C, 5
min; and 1 cycle of 4°C, 5 min. The entire 10-L reaction was then
subjected to PCR amplification in a PCR reaction with a total
volume of 50 L containing 3 L of Promega 25 mM MgCl2, 4 L of
Gibco PCR buffer without MgCl2, 35.5 L of PCR water, 1 L of
forward primer, 1 L of bacward primer, and 0.5 L of Taq polymerase (Life Technologies, Rockville, MD). Cycle parameters for PCR
amplification were 1 cycle of 94°C, 2.5 min; 32 cycles of (94°C, 1
min; 55°C, 1 min; 72°C, 1 min); 1 cycle of 72°C, 10 min; and 1 cycle
of 4°C, 5 min.
To amplify IL-10, IFN-␥, PPAR-␥ and 2-microglobulin
cDNA fragments, the sequences of PCR primers were as follows:
upstream, 5⬘-GCTCTATTGCCTCATCTTCC-3⬘; downstream,
5⬘-GCACTCTTCACCTCCTCCAC-3⬘ for the IL-10; upstream,
5⬘-TGTACCTAATGGTGGACCTC-3⬘; downstream, 5⬘-TCTCTGGCCTTGGAACATAG-3⬘ for IFN-␥, upstream; 5⬘-TTCAAACACATCACCCCCCTGC-3⬘; downstream, 5⬘-GCTTCACATTCAGCAAACCTGGGC-3⬘ for the PPAR-␥ (36); and upstream,
5⬘-CTGCTCTCACTGTCTGG-3⬘; downstream, 5⬘-ATCGAGAGTCACGTGCT-3⬘ for 2-microglobulin. PCR-amplified products
were electrophoretically separated on a 1.5% agarose gel. After electrophoresis, gels were stained in ethidium bromide and photographed.
A 100-kbp ladder (100 Kbplus; Life Technologies) was used as size
standard.
Statistical analysis. Postchallenge data were analyzed as a 2 ⫻ 2
(i.e., expt. 1) or 2 ⫻ 3 (i.e., expt. 2) factorial arrangement of
treatments within the split-plot design. In the model, pig within
block was the experimental unit for immunomodulatory treatment
(subplot), and blocks of pigs within infective status were the experimental units for infection treatment (whole plot). Analysis of vari-
LIPID NUTRITION AND GASTROINTESTINAL HEALTH
2023
TABLE 3
Growth performance of pigs fed control or conjugated linoleic acid (CLA)–supplemented diets after infection with Brachyspira
hyodysenteriae1,2,3
Immunomodulatory treatment
Infected pigs4
Noninfected pigs
Item
Week
Control diet
CLA diet
Vaccine6
Control diet
CLA diet
Vaccine6
SEM
P-value5
(interaction)
ADG, g
8
9
Cum.
8
9
Cum.
8
9
Cum.
1288a
952a
1120a
1617a
1884a
1750a
796a
505a
640a
1204a
1077a
1141a
1573a
1838a
1705a
765a
585a
669a
1120a
893a
1007a
1475a
1665a
1570a
759a
536a
641a
262b
308b
289c
1162c
1033c
1083c
225b
298b
266c
985a
549b
767a
1468b
1168c
1318b
670a
470a
581b
875a
475b
675b
1448b
1409b
1428b
604a
337b
472b
115
103
75
104
129
97
81
60
49
0.001
0.57
0.004
0.11
0.08
0.04
0.002
0.14
0.001
ADFI, g
G:F
slightly lower in CLA-supplemented diets than that in
soybean oil–supplemented diets because of lower palmitic
acid concentrations in the source of CLA. In phase IV the
concentration of linolenic acid was greater than that in the
other phases because of a greater percentage of corn in the
diet. Based on the total fat content of the diets, control and
CLA-supplemented diets provided the same amount of energy within phases.
Dietary CLA and growth failure associated with bacterialinduced colitis. Before infection with B. hyodysenteriae,
diet groups did not differ in average daily gain or feed intake
(data not shown). However, when immunization with the
proteinase-digested B. hyodysenteriae bacterin was included
as a positive control (expt. 2), the growth rate of vaccinated
pigs after the third immunization was less than that of
nonimmunized groups (data not shown). After challenge
with B. hyodysenteriae, colitis-induced growth suppression
in challenged pigs fed CLA-supplemented diets was attenuated compared with that of infected pigs fed the isocaloric
control diet in expt. 1 (data not shown) and expt. 2
(Table 3).
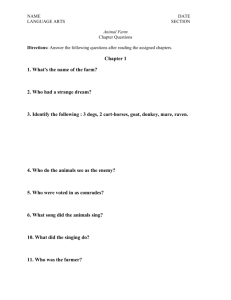
Dietary CLA and colonic cytokine and PPAR-␥ mRNA
expression. In expt. 1, after infection of pigs with B.
hyodysenteriae, colonic lymph nodes recovered from pigs fed
CLA-supplemented diets expressed cytokine profiles (e.g.,
INF-␥ and IL-10) more similar to those of noninfected pigs
than to those of infected pigs fed the control diet (Fig. 1).
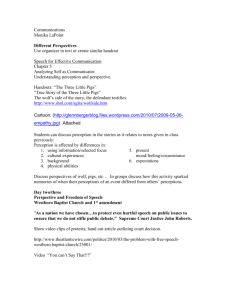
In addition, expression of PPAR-␥ in colonic tissue samples
recovered from infected pigs fed CLA-supplemented diets
was greater than that in colonic samples recovered from
infected pigs fed control diets (Fig. 2). Moreover, expression of PPAR-␥ mRNA was not detected in colonic tissue
from noninfected pigs.
Dietary CLA and “architecture” of the colonic mucosa
and lymphocyte subset distribution. Both immunization
with a proteinase-digested B. hyodysenteriae bacterin and
dietary CLA supplementation decreased the epithelial erosion associated with B. hyodysenteriae–induced colitis (Table 4). However, only dietary CLA supplementation prevented the enlargement of the colonic mucosa (Table 4,
Fig. 3A). Furthermore, the cellular infiltrate of healthy
colon was primarily lymphoplasmacytic (Fig. 3B). Infected
pigs either immunized with the proteinase-digested B. hyodysenteriae bacterin or fed CLA-supplemented diets maintained a lymphoplasmacytic infiltrate with numbers of
CD4⫹ and CD8␣␣⫹ cells not different from those of noninfected pigs (Table 5). However, infected pigs fed the
control diet showed a mixed cellular infiltrate including
neutrophils (Fig. 3B), with numbers of CD4⫹ and CD8␣␣⫹
T-cells substantially decreased (Table 5).
FIGURE 1 IL-10 and IFN-␥ mRNA are expressed in colonic lymph
nodes of representative infected pigs fed linoleic acid–supplemented
diets (i.e., lanes 2 and 4). Lane 1: noninfected pig; lanes 3 and 5:
infected pigs fed CLA-supplemented diets). Total RNA extracted from
colonic lymph nodes draining inflamed colonic tissue after infection
with B. hyodysenteriae and subjected to RT-PCR analysis.
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010
1 Pigs, feeders and waste feed were weighed on a weekly basis, and average daily gain (ADG), average daily feed intake (ADFI) and gain to feed
(G:F) were calculated.
2 Least-squares means values (n ⫽ 8) in a row for a particular growth performance criterion with different superscripts differ, P ⬍ 0.05.
3 Phase IV: 8 wk; 9 wk; and cumulative (Cum.) 8 –9 wk.
4 On d 49, eight blocks of three pigs each were infected as described under Materials and Methods. All experimentally inoculated pigs were culture
positive for B. hyodysenteriae.
5 After infection, data were analyzed as a 2 ⫻ 3 factorial arrangement (i.e., 2 infection status and 3 immunomodulatory treatments) within a
split-plot design. Infection status represents the whole plot and immunomodulatory treatments the subplot. The experimental unit for the whole plot
was a block of three littermate pigs and the experimental unit for the subplot was pig within a block. The P-value represents the interaction between
the infection status and the immunomodulatory treatments.
6 Pigs were vaccinated with a proteinase-digested B. hyodysenteriae bacterin on d 7, d 21, and d 35 of the experiment.
HONTECILLAS ET AL.
2024
FIGURE 2 PPAR-␥ mRNA expression in colonic mucosa samples recovered from infected pigs fed CLA-supplemented diets.
Total RNA extracted from healthy colon or inflamed colon of representative pigs infected with B. hyodysenteriae and subjected to
RT-PCR analysis. Colonic sections were recovered from either a
healthy pig (lane 1) or pigs with B. hyodysenteriae–induced colonic
inflammation (lanes 2 to 5). Lanes 4 and 5 were from pigs fed
CLA-supplemented diets, whereas lanes 2 and 3 were from pigs fed
soybean oil–supplemented diets.
In this study, we sought to investigate whether dietary
CLA supplementation, in action similar to that of vitamin
D (6) and (n-3) PUFA (7), ameliorated or prevented colonic inflammation. The model of colitis used involved a
noninvasive bacterial agent (i.e., B. hyodysenteriae). Thus,
mucosal lesions were not directly caused by B. hyodysenteriae but induced by the pig’s inflammatory response. CLA
ameliorated the inflammation-associated mucosal damage,
decreased growth suppression and delayed the onset of
clinical disease associated with bacterial-induced colitis.
The expression of IFN-␥ and IL-10 within colonic lymph
nodes in infected pigs fed CLA-supplemented diets resembled that of noninfected pigs. Conversely, expression of
IFN-␥ and IL-10 in colonic lymph nodes of infected pigs fed
control diets was up-regulated. These findings suggest that
supplementation of diets with CLA before the onset of
clinical disease may help prevent mucosal damage. This is a
TABLE 4
Histopathological changes of colonic tissue recovered from pigs fed control or conjugated linoleic acid (CLA)–supplemented diets
after infection with Brachyspira hyodysenteriae1
Immunomodulatory treatment
Infected pigs2
Noninfected pigs
Item
H&E colonic sections
Mucosal thickness5
Epithelial erosion6
P-value3
Control diet
CLA diet
Vaccine4
Control diet
CLA diet
Vaccine4
SEM
DV
IN
DV ⫻ IN
8.33c
0.00c
8.66c
0.16c
8.66c
0.00c
12.42a
1.74a
9.12b
0.62b
10.87a
1.00b
0.75
0.20
0.07
0.12
0.002
0.001
0.02
0.03
1 Least-squares means values (n ⫽ 8) in a row for a particular histopathological criterion with different superscripts are significantly different (P
⬍ 0.05).
2 On d 49, eight blocks of three pigs each were infected as described under Materials and Methods. All experimentally inoculated pigs were culture
positive for B. hyodysenteriae. At necropsy, sections of spiral colon were obtained and fixed in 10% buffered formalin, later embedded in paraffin and
then sectioned for blind histological examination.
3 P-value of main effects of immunomodulatory treatment [e.g., vaccine and/or diet (DV)], infection treatment (IN) and the interaction of
immunomodulatory treatment by infection treatment (DV ⫻ IN). Following infection, data were analyzed as a 2 ⫻ 3 factorial arrangement (i.e., 2
infection status and 3 immunomodulatory treatments) within a split-plot design. Infection status represents the whole plot and immunomodulatory
treatments the subplot. The experimental unit for the whole plot was a block of three littermate pigs and the experimental unit for the subplot was
pig within a block. The P-value represents the interaction between the infection status and the immunomodulatory treatments.
4 Pigs were vaccinated with a proteinase-digested B. hyodysenteriae bacterin on d 7, d 21, and d 35 of the experiment.
5 Mucosal thickness is expressed as crypt depth as a function of crypt width (e.g., a score of 5 indicates that crypts are 5 times as deep as they
are wide).
6 Epithelial erosion scores are based on a subjective scale of: 0 ⫽ no erosion, 1 ⫽ mild erosion, or 2 ⫽ severe erosion.
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010
DISCUSSION
first-time observation demonstrating that dietary CLA supplementation prevents or ameliorates the onset of experimental colitis in pigs.
The increased expression of IFN-␥ in the pigs with more
severe lesions (i.e., fed the control diet) is consistent with the
predominantly T helper (Th) 1 nature of lesions found in
patients with IBD as well as for the model of experimental
colitis used in these studies. In support of this, adoptive transfer of T-cells, which preferentially express Th1 cytokines,
induced Crohn’s-like lesions to mice that were otherwise
healthy (38). In a murine model of dextran sulfate sodium
(DSS)–induced chronic colitis, neutralizing antibodies against
IFN-␥ facilitated lesion restitution (39). IFN-␥ exacerbates
lesion development by initiating leukocyte recruitment from
the vascular space into the tissues by modulating surface expression of endothelial adhesion molecules. These microcirculatory changes may contribute to the enhanced inflammatory
cell infiltrate found in the lamina propria of pigs fed the
control diet. Although enhanced mRNA expression of IL-10
correlates with increased severity of colonic injury (40), the
up-regulation of IL-10 may be a part of a homeostatic mechanism to balance Th1 polarization. At least three functional
outputs of terminally differentiated Th cells have been characterized based on cytokine production and homing capacity:
Th1, Th2, and nonpolarized cells (41). The development of
immune-mediated mucosal damage can be triggered by both
Th1 and Th2 effector CD4⫹ cells (42) and prevented by
CD8⫹ T-cells (25). Dietary CLA may have prevented this
immunopathology by enhancing numbers of CD8⫹ cells and
favoring differentiation toward a nonpolarized Th cell subset.
Consistent with a mechanism of nutritional immunoregulation by T-cells, we previously demonstrated that CD4⫹ Th
responses to bacterial antigens were attenuated by dietary
CLA (24,43). In addition, two ligands for PPAR-␥ (i.e.,
15d-PGJ2 and ciglitazone) inhibited proliferative responses of
murine Th cell clones and freshly isolated splenocytes (20).
At the molecular level, the concentration of cytokines in
LIPID NUTRITION AND GASTROINTESTINAL HEALTH
tissues is controlled in part by mechanism(s) of transcriptional
regulation. Nuclear factor-kappa B (NF-B) is included among
the transcription factors involved in up-regulating the expression of IFN-␥ (44). Interestingly, PPAR-␥ activation was
previously demonstrated to antagonize the activities of several
transcription factors including NF-B (45). As a result of this
interference with the NF-B signaling pathway, the expression
of proinflammatory cytokines (i.e., TNF-␣, IL-6 and IL-1) is
suppressed (22) and macrophage apoptosis induced (46), both
effects with likely consequences in inflammation. Here, we
have shown that PPAR-␥ expression is up-regulated after
colonic inflammation and the concentration of PPAR-␥ is
greater in infected pigs fed CLA-supplemented diets than that
in infected pigs fed the control diets.
PPAR-␥–independent mechanism(s) have also been
shown to significantly contribute to the anti-inflammatory
actions of compounds, such as CLA, that are PPAR-␥
agonistic ligands (47). In the case of CLA, PPAR-␥–independent mechanisms of action would include CLA-induced
regulation of lipid mediator synthesis. Consistent with previous observations in liver of mice (48), the analysis of the
fatty acid composition of plasma (data not shown) revealed
that dietary CLA supplementation decreased the concentration of linoleic and arachidonic acids. The latter is a
precursor for the generation of first-phase eicosanoids (i.e.,
two series prostaglandins and four series leukotrienes) involved in early microinflammatory events (i.e., polymorphonuclear neutrophilic leukocyte chemotaxis and release
of superoxide anions) (49). Enhanced intestinal eicosanoid
concentrations closely correlate with severe histological
signs of colonic inflammation (50). Therefore, the enteric
health benefits of dietary CLA may derive in part from the
generation of an array of lipid mediators (i.e., hydroxycontaining fatty acids, prostaglandins, lipoxins and leukotrienes) that are either anti-inflammatory or not proinflammatory (18).
Dietary CLA supplementation was more effective than
immunization in preventing growth suppression and lesion
TABLE 5
Lymphocyte subset distribution in colonic tissue recovered from pigs fed control or conjugated linoleic acid (CLA)–supplemented
diets after infection with Brachyspira hyodysenteriae1
Immunomodulatory treatment
Infected pigs2
Noninfected pigs
Item
Control diet
CLA diet
Control diet
CLA diet
Vaccine4
SEM
DV
IN
DV ⫻ IN
113.78a
58.67b
237.33
55.11
113.33a
60.00b
222.67
37.33
15
17
75
31
0.22
0.04
0.39
0.63
0.26
0.004
0.59
0.20
0.02
0.53
0.86
0.09
n/mm2
CD markers
CD4
CD8␣
CD3
TCR␥␦
Vaccine4
P-value3
118.22a
67.56b
199.11
64.00
101.33a
78.22b
203.56
50.67
102.67a
90.67a
232.00
36.00
64.89b
48.00c
205.33
24.89
1 Least-squares means values (n ⫽ 3) in a row for a particular cell subset count/mm2 of tissue with different superscripts are significantly different
(P ⬍ 0.05).
2 On d 49, eight blocks of three pigs each were infected as described under Materials and Methods. All experimentally inoculated pigs were culture
positive for B. hyodysenteriae. At necropsy, sections of spiral colon were obtained snap-frozen, sectioned for staining with monoclonal antobodies
and blind immunohistochemical examination.
3 P-value of main effects of immunomodulatory treatment [e.g., vaccine and/or diet (DV)], infection treatment (IN) and the interaction of
immunomodulatory treatment by infection treatment (DV ⫻ IN). Following infection, data were analyzed as a 2 ⫻ 3 factorial arrangement (i.e., 2
infection status and 3 immunomodulatory treatments) within a split-plot design. Infection status represents the whole plot and immunomodulatory
treatments the subplot. The experimental unit for the whole plot was a block of three littermate pigs and the experimental unit for the subplot was
pig within a block. The P-value represents the interaction between the infection status and the immunomodulatory treatments.
4 Pigs were vaccinated with a proteinase-digested B. hyodysenteriae bacterin on d 7, d 21, and d 35 of the experiment.
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010
FIGURE 3 Representative colonic sections stained with hematoxylin and eosin: (A) Recovered from noninfected pigs (top panel)
and B. hyodysenteriae–infected pigs (bottom panels). Inflammation
was severe in infected pigs fed the control diet (i.e., linoleic acid–
supplemented), whereas pigs fed the conjugated linoleic acid–supplemented diet and pigs fed the control diet and immunized against
B. hyodysenteriae did not demonstrate a thickening of the mucosa.
Original magnification, ⫻63. (B) Recovered from either a noninfected
pig (left) or B. hyodysenteriae–infected pigs fed a CLA-supplemented diet (center) or a control diet (right). Lamina proprial cellular
profiles are lymphoplasmacytic (left and center) vs. mixed profiles
containing both lymphocytes and polymorphonuclear neutrophils
and dilated capillaries (right). Mucosa containing enterocytes with
normal columnar shape (left and center) vs. severe epithelial erosion
with flattened enterocytes (right). Original magnification, ⫻400.
2025
HONTECILLAS ET AL.
2026
ACKNOWLEDGMENTS
We thank M. Du and M. Byers for technical assistance, and D. C.
Beitz for his reading of the manuscript and constructive comments.
LITERATURE CITED
1. Cantorna, M. T., Nashold, F. E. & Hayes, C. E. (1994) In vitamin A
deficiency multiple mechanisms establish a regulatory T helper cell imbalance
with excess Th1 and insufficient Th2 function. J. Immunol. 152: 1515–1522.
2. Cantorna, M. T., Nashold, F. E., Chun, T. Y. & Hayes, C. E. (1996)
Vitamin A down-regulation of IFN-gamma synthesis in cloned mouse Th1 lymphocytes depends on the CD28 costimulatory pathway. J. Immunol. 156: 2674 –
2679.
3. Cantorna, M. T., Hayes, C. E. & DeLuca, H. F. (1996) 1,25-Dihydroxyvitamin D3 reversibly blocks the progression of relapsing encephalomyelitis, a
model of multiple sclerosis. Proc. Natl. Acad. Sci. USA 93: 7861–7864.
4. Cantorna, M. T. & Hayes, C. E. (1996) Vitamin A deficiency exacerbates murine Lyme arthritis. J. Infect. Dis. 174: 747–751.
5. Bassaganya-Riera, J., Hontecillas, R., Wannemuehler, M.J. (2002)
Nutritional impact of conjugated linoleic acid: a model functional food ingredient.
In Vitro Cell. Dev. Biol. 38: 241–246.
6. Cantorna, M. T., Munsick, C., Bemiss, C. & Mahon, B. D. (2000)
1,25-Dihydroxycholecalciferol prevents and ameliorates symptoms of experimental murine inflammatory bowel disease. J. Nutr. 130: 2648 –2652.
7. Geerling, B. J., Badart-Smook, A., van Deursen, C., van Houwelingen,
A. C., Russel, M. G., Stockbrugger, R. W. & Brummer, R. J. (2000) Nutritional
supplementation with N-3 fatty acids and antioxidants in patients with Crohn’s
disease in remission: effects on antioxidant status and fatty acid profile. Inflamm.
Bowel Dis. 6: 77– 84.
8. Crawford, J. M. (1994) The gastrointestinal tract. In: Pathologic Basis
of Disease (Cotran, R. S., Kumar, V. & Robbins, S. L., eds.). WB Saunders,
Philadelphia, PA.
9. Kirsner, J. B. (1991) Inflammatory bowel disease. Part I: Nature and
pathogenesis. Dis. Mon. 37: 607– 666.
10. Fleming, C. R. (1995) Nutrition in patients with Crohn’s disease: another piece of the puzzle. J. Parenter. Enteral Nutr. 19: 93–94.
11. Geerling, B. J., Badart-Smook, A., Stockbrugger, R. W. & Brummer, R. J.
(1998) Comprehensive nutritional status in patients with long-standing Crohn
disease currently in remission. Am. J. Clin. Nutr. 67: 919 –926.
12. Nagura, H., Ohtani, H., Sasano, H. & Matsumoto, T. (2001) The immuno-inflammatory mechanism for tissue injury in inflammatory bowel disease
and Helicobacter pylori-infected chronic active gastritis. Roles of the mucosal
immune system. Digestion 63: 12–21.
13. Waters, W. R., Sacco, R. E., Dorn, A. D., Hontecillas, R., Zuckermann,
F. A. & Wannemuehler, M. J. (1999) Systemic and mucosal immune response
of pigs to parenteral immunization with a pepsin-digested Serpulina hyodysenteriae bacterin. Vet. Immunol. Immunopathol. 69: 75– 87.
14. Podolsky, D. K. (1991) Inflammatory bowel disease (1). N. Engl.
J. Med. 325: 928 –937.
15. Ogura, Y., Bonen, D. K., Inohara, N., Nicolae, D. L., Chen, F. F., Ramos,
R., Britton, H., Moran, T., Karaliuskas, R., Duerr, R. H., Achkar, J. P., Brant, S. R.,
Bayless, T. M., Kirschner, B. S., Hanauer, S. B., Nunez, G. & Cho, J. H. (2001)
A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease.
Nature 411: 603– 606.
16. Hugot, J. P., Chamaillard, M., Zouali, H., Lesage, S., Cezard, J. P.,
Belaiche, J., Almer, S., Tysk, C., O’Morain, C. A., Gassull, M., Binder, V., Finkel,
Y., Cortot, A., Modigliani, R., Laurent-Puig, P., Gower-Rousseau, C., Macry, J.,
Colombel, J. F., Sahbatou, M. & Thomas, G. (2001) Association of NOD2
leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature 411:
599 – 603.
17. Veldman, C. M., Cantorna, M. T. & DeLuca, H. F. (2000) Expression of
1,25-dihydroxyvitamin D(3) receptor in the immune system. Arch. Biochem. Biophys. 374: 334 –338.
18. Serhan, C. N., Clish, C. B., Brannon, J., Colgan, S. P., Chiang, N. &
Gronert, K. (2000) Novel functional sets of lipid-derived mediators with antiinflammatory actions generated from omega-3 fatty acids via cyclooxygenase
2-nonsteroidal antiinflammatory drugs and transcellular processing. J. Exp. Med.
192: 1197–1204.
19. Jump, D. B. & Clarke, S. D. (1999) Regulation of gene expression by
dietary fat. Annu. Rev. Nutr. 19: 63–90.
20. Clark, R. B., Bishop-Bailey, D., Estrada-Hernandez, T., Hla, T., Puddington, L. & Padula, S. J. (2000) The nuclear receptor PPAR ␥ and immunoregulation: PPAR ␥ mediates inhibition of helper T cell responses. J. Immunol. 164:
1364 –1371.
21. Su, C. G., Wen, X., Bailey, S. T., Jiang, W., Rangwala, S. M., Keilbaugh,
S. A., Flanigan, A., Murthy, S., Lazar, M. A. & Wu, G. D. (1999) A novel therapy
for colitis utilizing PPAR-␥ ligands to inhibit the epithelial inflammatory response.
J. Clin. Invest. 104: 383–389.
22. Desreumaux, P., Dubuquoy, L., Nutten, S., Peuchmaur, M., Englaro, W.,
Schoonjans, K., Derijard, B., Desvergne, B., Wahli, W., Chambon, P., Leibowitz,
M. D., Colombel, J. F. & Auwerx, J. (2001) Attenuation of colon inflammation
through activators of the retinoid X receptor (RXR)/peroxisome proliferator-activated receptor ␥ (PPAR␥) heterodimer. A basis for new therapeutic strategies. J.
Exp. Med. 193: 827– 838.
23. Calder, P. C. (1998) Dietary fatty acids and the immune system. Nutr.
Rev. 56: S70 –S83.
24. Bassaganya-Riera, J., Hontecillas-Magarzo, R., Bregendahl, K., Wannemuehler, M. J. & Zimmerman, D. R. (2001) Effects of dietary conjugated linoleic
acid in nursery pigs of dirty and clean environments on growth, empty body
composition, and immune competence. J. Anim. Sci. 79: 714 –721.
25. Jones, H. P., Tabor, L., Sun, X., Woolard, M. D. & Simecka, J. W.
(2002) Depletion of CD8(⫹) T cells exacerbates CD4(⫹) Th cell-associated
inflammatory lesions during murine mycoplasma respiratory disease. J. Immunol.
168: 3493–3501.
26. Ha, Y. L., Storkson, J. & Pariza, M. W. (1990) Inhibition of benzo(a)pyrene-induced mouse forestomach neoplasia by conjugated dienoic derivatives of linoleic acid. Cancer Res. 50: 1097–1101.
27. Houseknecht, K. L., Vanden Heuvel, J. P., Moya-Camarena, S. Y., Portocarrero, C. P., Peck, L. W., Nickel, K. P. & Belury, M. A. (1998) Dietary
conjugated linoleic acid normalizes impaired glucose tolerance in the Zucker
diabetic fatty fa/fa rat [published erratum appears in Biochem. Biophys. Res.
Commun. 1998 Jun 29;247(3):911]. Biochem. Biophys. Res. Commun. 244: 678 –
682.
28. Lee, K. N., Kritchevsky, D. & Pariza, M. W. (1994) Conjugated linoleic
acid and atherosclerosis in rabbits. Atherosclerosis 108: 19 –25.
29. Bassaganya-Riera, J., Hontecillas, R., Zimmerman, D. R. & Wannemuehler, M. J. (2001) Dietary conjugated linoleic acid modulates phenotype
and effector functions of porcine CD8(⫹) lymphocytes. J. Nutr. 131: 2370 –2377.
30. Waters, W. R., Pesch, B. A., Hontecillas, R., Sacco, R. E., Zuckermann,
F. A. & Wannemuehler, M. J. (1999) Cellular immune responses of pigs
induced by vaccination with either whole cell sonicate or pepsin-digested
Brachyspira (Serpulina) hyodysenteriae bacterin. Vaccine 18: 711–719.
31. Lim, B. O., Jolly, C. A., Zaman, K. & Fernandes, G. (2000) Dietary (n-6)
and (n-3) fatty acids and energy restriction modulate mesenteric lymph node
lymphocyte function in autoimmune-prone (NZB ⫻ NZW)F1 mice. J. Nutr. 130:
1657–1664.
32. Sato, M., Iwakabe, K., Kimura, S. & Nishimura, T. (1999) The influence
of dietary protein antigen on Th1/Th2 balance and cellular immunity. Immunol.
Lett. 70: 29 –35.
33. National Research Council. (1998) Nutrient requirements of swine.
National Academy Press, Washington, DC.
34. AOAC. (1990) Official Methods of Analysis. Association of Official
Analytical Chemists, Arlington, VA.
35. Kunkle, R. A. & Kinyon, J. M. (1988) Improved selective medium for the
isolation of Treponema hyodysenteriae. J. Clin. Microbiol. 26: 2357–2360.
36. Houseknecht, K. L., Bidwell, C. A., Portocarrero, C. P. & Spurlock, M. E.
(1998) Expression and cDNA cloning of porcine peroxisome proliferator-activated receptor ␥ (PPAR␥). Gene 225: 89 –96.
37. SAS Institute Inc. (1988) SAS/STAT User’s Guide, Version 6.03. SAS
Institute, Cary, NC.
38. Aranda, R., Sydora, B. C., McAllister, P. L., Binder, S. W., Yang, H. Y.,
Targan, S. R. & Kronenberg, M. (1997) Analysis of intestinal lymphocytes in
mouse colitis mediated by transfer of CD4⫹, CD45RBhigh T cells to SCID
recipients. J. Immunol. 158: 3464 –3473.
39. Obermeier, F., Kojouharoff, G., Hans, W., Scholmerich, J., Gross, V. &
Falk, W. (1999) Interferon-␥ (IFN-␥)- and tumour necrosis factor (TNF)-induced
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010
development in infected pigs. B. hyodysenteriae were recovered from the colon of all infected pigs, regardless of dietary
treatment. All infected pigs were positive for B. hyodysenteriae, suggesting that CLA modulates the host’s immune
effector mechanisms instead of directly targeting the bacterial agent. Histological evaluation of colonic tissues demonstrated that both CLA and systemic immunization decreased epithelial erosion compared to that of the control
diet. However, only CLA prevented the enlargement of the
colonic mucosa. Comparable to immunization with a B.
hyodysenteriae bacterin (13), CLA increased the numbers of
TCR␥␦CD8␣␣ cells in peripheral blood (29) and maintained numbers of CD4⫹ and CD8␣⫹ cells in the colonic
mucosa.
This is the first report of efficacy of CLA in ameliorating
disease associated with colitis. Future studies will be designed to distinguish the PPAR-␥–independent and the
PPAR-␥– dependent mechanisms by structurally elucidating T-lymphocyte– derived lipid mediators and defining the
phenotype of tissue-targeted (i.e., enterocytes, CD8⫹ Tlymphocytes or CD4⫹ T-lymphocytes) PPAR-␥– deficient
mice, respectively. These experimental approaches may
yield novel nutritional therapies for both inflammatory and
immune pathologies.
LIPID NUTRITION AND GASTROINTESTINAL HEALTH
nitric oxide as toxic effector molecule in chronic dextran sulphate sodium (DSS)induced colitis in mice. Clin. Exp. Immunol. 116: 238 –245.
40. Egger, B., Bajaj-Elliott, M., MacDonald, T. T., Inglin, R., Eysselein, V. E. &
Buchler, M. W. (2000) Characterisation of acute murine dextran sodium sulphate colitis: cytokine profile and dose dependency. Digestion 62: 240 –248.
41. Langenkamp, A., Messi, M., Lanzavecchia, A. & Sallusto, F. (2000)
Kinetics of dendritic cell activation: impact on priming of TH1, TH2 and nonpolarized T cells. Nat. Immunol. 1: 311–316.
42. Iqbal, N., Oliver, J. R., Wagner, F. H., Lazenby, A. S., Elson, C. O. &
Weaver, C. T. (2002) T helper 1 and T helper 2 cells are pathogenic in an
antigen-specific model of colitis. J. Exp. Med. 195: 71– 84.
43. Bassaganya-Riera, J., Hontecillas, R., Zimmerman, D. R. & Wannemuehler, M. J. (2002) Long-term influence of lipid nutrition on the induction of
CD8⫹ responses to viral or bacterial antigens. Vaccine 20: 1435–1444.
44. Schindler, H., Lutz, M. B., Rollinghoff, M. & Bogdan, C. (2001) The
production of IFN-␥ by IL-12/IL-18-activated macrophages requires STAT4 signaling and is inhibited by IL-4. J. Immunol. 166: 3075–3082.
45. Ricote, M., Li, A. C., Willson, T. M., Kelly, C. J. & Glass, C. K. (1998)
2027
The peroxisome proliferator-activated receptor-␥ is a negative regulator of macrophage activation. Nature 391: 79 – 82.
46. Chinetti, G., Griglio, S., Antonucci, M., Torra, I. P., Delerive, P., Majd, Z.,
Fruchart, J. C., Chapman, J., Najib, J. & Staels, B. (1998) Activation of
proliferator-activated receptors ␣ and ␥ induces apoptosis of human monocytederived macrophages. J. Biol. Chem. 273: 25573–25580.
47. Chawla, A., Barak, Y., Nagy, L., Liao, D., Tontonoz, P. & Evans, R. M.
(2001) PPAR-␥ dependent and independent effects on macrophage-gene expression in lipid metabolism and inflammation. Nat. Med. 7: 48 –52.
48. Belury, M. A. & Kempa-Steczko, A. (1997) Conjugated linoleic acid
modulates hepatic lipid composition in mice. Lipids 32: 199 –204.
49. Levy, B. D., Clish, C. B., Schmidt, B., Gronert, K. & Serhan, C. N.
(2001) Lipid mediator class switching during acute inflammation: signals in
resolution. Nat. Immunol. 2: 612– 619.
50. Hommes, D. W., Meenan, J., de Haas, M., ten Kate, F. J., von dem
Borne, A. E., Tytgat, G. N. & van Deventer, S. J. (1996) Soluble Fc ␥
receptor III (CD 16) and eicosanoid concentrations in gut lavage fluid from
patients with inflammatory bowel disease: reflection of mucosal inflammation.
Gut 38: 564 –567.
Downloaded from jn.nutrition.org at Iowa State Univ Library on October 27, 2010