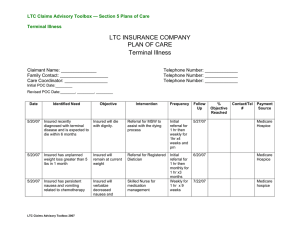
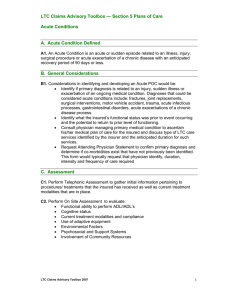
LTC Claims Advisory Toolbox — Section 5 Plans of Care Introduction
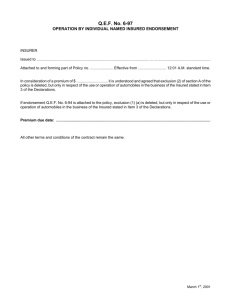
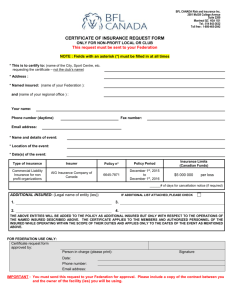
advertisement
LTC Claims Advisory Toolbox — Section 5 Plans of Care Introduction A. Introduction This section of the Toolbox features the “Operational Definition of a Plan of Care” and the development of various Plans of Care (POC) based on general conditions and prognosis. The following are the POCs and their definitions which are included in this section : • Acute: Recovery expected within 90 days or less • Terminal: Death is expected within 6 months • Long Term Progressive: Impairment is expected to last greater than 6 months with a functional decline • Chronic: Impairment is expected to last greater than 6 months with functional stability • Cognitive Impairment: An acute impairment resulting from a disease process with an expectation of recovery or a chronic impairment with deterioration and is progressive in nature. You will note that all of the documentation in this toolbox focuses on a Plan of Care as opposed to a Plan of Service. A Plan of Service does not typically attempt to monitor and/or improve functional or cognitive capacity. A Plan of Care incorporates the following: • Identified Need: Reflects the actual needs identified during the onsite assessment and from medical records received • Objective: What is the Goal of the Plan of Care is attempting to reach? • Intervention: What is the actual assistance to be provided? • Frequency: How often will the assistance be provided? • Follow Up: When is the next scheduled follow-up? • % Objective Reached: What is the progress towards achieving the Objective • Contact/ Tel#: Who is the primary contact? • Payment Source: Who is paying for the services? This can be a combination of payer sources. The purpose of utilizing various Plans of Care within your claim model/process is to manage and apply appropriate interventions based on the insured’s general condition and prognosis. This will allow the insured to achieve their highest level of independence and wellness which will result in a superior insured experience and strong operational results. Following are a few examples: • If an insured is in a skilled nursing facility with a diagnosis of a Stroke with severe paralysis, the “Chronic Plan of Care” can be applied. • If an insured is receiving rehabilitative services in a skilled nursing facility for a hip replacement and is being discharged home, the “Acute Plan of Care” would be appropriate. • If a insured is in a home care setting with a diagnosis of end stage Leukemia, you may want to use components of the “Terminal” and “Long Term Progressive” Plans of Care. LTC Claims Advisory Toolbox 2007 1 LTC Claims Advisory Toolbox — Section 5 Plans of Care Introduction Any of the elements of the “Cognitive Plan of Care” may also be applied to the above scenarios if the diagnosis exists in conjunction with an associated physical condition which is acute, chronic, etc... Once an individualized Plan of Care has been developed, it is essential for the insured, family and physician to commit to the Plan of Care. This can be accomplished by working collaboratively with all parties involved in the insured’s care from the onset. Communication through the implementation and on going monitoring of the POC is also important. This will ensure optimal results. This section also includes a sample of each type of Plans of Care discussed in this section. These samples provide LTC insurers with ideas of what could be incorporated in their plans of care. The simple style of formatting used is purposeful so that the tool can be easily replicated or reformatted if an insurer is interested in using any of this information in their Plan of Care. B. General Operational Definition of a Plan of Care B1. Care planning is an essential part of long term care. Care planning provides a ‘road map’ of sorts to guide all who are involved with an insured’s care. Ideally, to be effective and comprehensive, the care planning process must involve all disciplines that are involved in the care of the insured. The first step in care planning is an accurate and comprehensive assessment. In a nursing home/facility setting, the MDS is the starting point for assessment. Medicarecertified and licensed home health care agencies utilize the OASIS (Outcome and Assessment Information Set.) Other settings such as unlicensed home care agencies, assisted care facilities and adult day care facilities have established protocols for initial assessments and ongoing reevaluation. In addition to these assessments performed by the provider, most LTC insurers have an on site assessment tool which is completed by an independent health care professional to gather key information to help the insurer determine eligibility for benefits. Once the initial assessment is completed, a problem list is usually generated. The problem list includes the insured’s medical diagnoses and abilities with regard to cognition and ADLs and IADLs functioning. From the problem list, the appropriate interventions are identified and a POC is developed. The POC supports the insured in his/her chosen environment helping the insured to ‘age in place’ as comfortably and safely as possible. It also takes into consideration the existing factors that may influence its success. This may include the insured’s motivation in regaining a level of independence and include other factors such as any psychosocial and environmental barriers that may affect the insured’s ability to achieve the highest level of independence and overall sense of well-being possible. LTC Claims Advisory Toolbox 2007 2