HARFORD COMMUNITY COLLEGE 401 Thomas Run Road Date of Exam:
advertisement

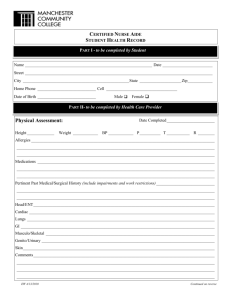
HARFORD COMMUNITY COLLEGE 401 Thomas Run Road Bel Air, Maryland 21015 443-412-2000 Date of Exam: _____ Program of Study: _____ DIVISION OF NURSING AND ALLIED HEALTH PROFESSIONS MEDICAL HEALTH EXAMINATION RECORD This report is confidential. Students are responsible for the accuracy of this information. Omitted or inaccurate information will be considered a violation of the HCC Honor Code and can result in a student’s dismissal from the program. To be completed by student: Name: Address (include city, state, zip): Emergency Contact: DOB: Sex: Telephone: Student ID# Email: Telephone: Male Female Relationship: I hereby grant the health professions program permission to contact the physician(s) or other professional(s) who have assisted me with medical conditions, mental health conditions, alcoholism, and/or drug dependency and to obtain information and records regarding these conditions. Student’s signature To be completed by Physician: Date: (Use back of form if needed for notes and explanations.) Student must be free of contagion and possess sufficient physical stamina with or without reasonable accommodations, and possess mental stability to fulfill the requirements of the program and the customary requirements of the profession. Work 10-12 hours performing physical tasks requiring physical energy without jeopardy to patient and student safety, e.g. bending, lifting, turning, and ambulating adult patients. Perform fine movements and be able to manipulate instruments and equipment. Establish and work towards goals in a consistently responsible realistic manner. Have auditory ability sufficient to monitor and assess health needs. Have visual ability for observation and assessment necessary for patient care. Possess the emotional maturity and stability to approach highly stressful human situations in a calm and rational manner. 1. The applicant has been examined and found to be in good general health. _____ Yes ______ No (explain please) 2. Is the applicant currently under medical treatment? _____ Yes (specify condition being treated) ______ No 3. Has applicant had any major illness in the past year requiring on-going care or therapy by a health professional? ____ Yes (explain please) ____ No 4. Chronic conditions (please list): 5. Has applicant had any hospitalizations, injuries, restriction of physical activity within last five years? Give dates and specify problem: 6. The applicant is fit to participate in the clinical activities of an allied health care program. _____ Yes _____ No (explain please) 7. To the best of my knowledge, the applicant is not presently harboring any infectious diseases. _____ Correct 8. Has applicant had any mental health problems? _______ Yes (explain please) _____ Incorrect (explain please) ______ No 9. Has applicant had any drug or alcohol dependency? _____ Yes (specify problems and dates) ______ No 10. Allergies -- include sensitivity/allergy to chemicals, dust, latex, etc.(please list): 11/13 PHYSICIAN------ CONTINUE ON BACK STUDENT NAME (printed) Antibody titer – Required Immunization OR ➙ Dates Immunizations Received Hepatitis (Hep B) Report 3 doses or titer results Varicella (Chicken Pox) Report 2 doses after age 12 months or titer results Measles (Rubeola) Report 2 doses after age 12 months or titer results Mumps Report 2 doses after age 12 months or titer results Rubella (German Measles) Report 2 doses after age 12 months or titer results Tetanus/Diphtheria (Td or Tdap) Report most current Td dose (within 10 years) If it has been at least 2 years since the last Td dose, and you have never had a Tdap, a Tdap is REQUIRED. Required TST (Tuberculin Skin Test) Mantoux Required (PPD) Dose 1 Date Dose 2 Date Dose 1 Date Dose 2 Date Test Date Dose 1 Date Dose 2 Date Test Date Dose 1 Date Dose 2 Date Test Date Dose 1 Date Dose 2 Date Test Date Dose Date – Td Dose Date – Tdap Administration Date: Last PPD Test Date if Positive Test Date Date Read: Induration: Individuals with a previous positive PPD Must provide date of last PPD and a copy of chest x-ray report within the last six months OR official documentation of a history or tuberculosis and completion of treatment. Seasonal flu vaccine Dose 3 Date MUST Attach Lab Results mm _____ Chest x-ray report attached _____ Documentation of disease history and completion of treatment attached. Dose Date I certify that I am a primary health care provider legally qualified to practice in the State of . I have examined the above applicant and find that the applicant is neither mentally nor physically disqualified by reason of acute, chronic, or mental conditions from the successful performance of the clinical duties required of health sciences students. Health Care Provider’s Signature Date Address Phone Health Care Provider’s Name (Printed or Stamped) HEALTH EVALUATION IS NOT VALID WITHOUT PHYSICIAN’S SIGNATURE EXPLANATIONS – FOR PHYSICIAN USE