P C S
advertisement
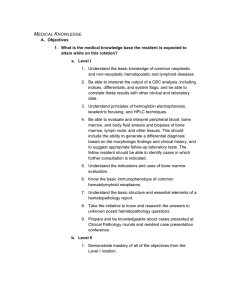
PATIENT CARE PROCEDURAL SKILLS A. Objective 1. What procedural skills must be acquired on this rotation? a. Level I 1. Grossing and triaging lymph node or hematolymphoid tissue biopsies for histopathology as well as any appropriate ancillary studies at Parkland and University Hospitals. b. Level II 1. Demonstrate mastery of all of the objectives from the Level I rotation. 2. Gain exposure to bone marrow aspiration and biopsy procedures for histopathology as well as any appropriate ancillary studies. 3. Understand the basic procedures for bone marrow processing, including factors that may compromise specimen adequacy, and the advantages and disadvantages of the various preparations. B. Plan 1. How are the procedural skills taught and by whom? a. Level I 1. Lymph node and tissue procedural skills are taught by observation and actual performance under the supervision of senior residents (a resident having completed at least one two-month rotation in hematopathology), hematopathology fellows, and hematopathology faculty. Detailed written instructions for submitting tissue for a hematolymphoid workup are provided during the rotation orientation. During the procedure, the residents will make touch preparations of the nodes and examine the "diffquick" stained slides. Based on the morphologic impression, they will select ancillary tests for which dissected tissue will be submitted (flow cytometry, cytogenetics, molecular diagnosis, or culture). b. Level II 1. Senior residents are expected to observe one bone marrow biopsy at Parkland Hospital to become familiar with this procedure. A senior resident may, if he or she chooses, perform a bone marrow under the supervision of hematology/oncology personnel. 2. Senior residents are expected to participate in a “bench rotation” in the bone marrow processing laboratory where they will learn preparation and routine staining of bone marrow aspirates, touch preparations and special staining of bone marrow aspirates including iron, myeloperoxidase, and non-specific esterase stains. C. Supervision/Assessment 1. How and by whom are the procedures supervised and the skills assessed, and how are these documented? a. Level I 1. Junior residents will be supervised directly by senior level residents, hematopathology fellows, and hematopathology faculty at the beginning of the rotation. 2. Junior residents are responsible for maintaining a log of the first three grossing or triage procedures they perform. Once proficiency in grossing and triaging at least three lymph node or other hematolymphoid specimens has been verified, junior residents may perform these procedures without direct supervision. However, fellows and attendings will be available in-house to assist, if necessary, during business hours (8 a.m. to 5 p.m.). After hours, hematopathology fellows and attendings are available to assist on call, if necessary. 3. Performance in grossing and triaging specimens will be assessed through direct observation of at least three procedures by hematopathology faculty, fellows, and senior residents. Faculty will provide direct verbal feedback regarding grossing technique for each case at the time of sign-out. 4. The rotation director will discuss verbal and written assessments provided by faculty, fellows, supporting staff, and clinicians at both the midpoint and endpoint of the rotation. b. Level II 1. Senior residents may gross and triage specimens with indirect supervision (hematopathology fellows and faculty on call to assist, if necessary). Bone marrow biopsy procedures are performed under the supervision of hematology/oncology faculty and fellows. Bone marrow processing and staining skills are learned under the supervision of laboratory technologists at Parkland Hospital. 2. Resident performance will be assessed through direct observation by hematopathology faculty, fellows, laboratory technologists and clinicians. Faculty will provide direct verbal feedback regarding grossing technique for each case at the time of sign-out. 3. Residents will complete and submit to the rotation director a checklist documenting they have observed at least one bone marrow biopsy and have participated in the bench rotation at the bone marrow laboratory. 4. The rotation director will discuss verbal and written assessments provided by faculty, fellows, supporting staff, and clinicians at both the midpoint and endpoint of the rotation. INTERPRETIVE SKILLS A. Objectives 1. What interpretive skills are important to acquire on this rotation? i. Level I 1. Be able to evaluate and interpret peripheral blood and body fluid smears, bone marrow aspirates and core biopsies, and a variety of hematology tests including CBC, reticulocyte counts, hemoglobin electrophoresis. 2. Demonstrate proficiency in bone marrow differentials. ii. Level II 1. Demonstrate mastery of all of the objectives from the Level I rotation. 2. Be able to evaluate and interpret lymph node biopsies, any hematolymphoid infiltrate in other organ/systems and flow cytometric analysis. B. Plan 1. Level I i. In the first week of the rotation, residents will participate in scheduled morning sessions with the rotation director. These sessions will include basic blood and bone marrow cell morphology at a multi-headed microscope. ii. Perform bone marrow and peripheral differential counts at the beginning of the rotation under the supervision of hematopathology faculty, fellows and senior residents. iii. The residents will be expected to prepare the assigned cases, including gathering appropriate clinical and laboratory data, reviewing the morphology, performing differential counts when applicable, and formulate their own impressions and diagnoses prior to reviewing the cases with the attending hematopathologist. The hematopathologists will discuss the cases with the residents during sign-out and finalize the diagnosis. iv. Residents are assigned to Children's Medical Center on a rotating basis to prepare morphologic reports on pediatric bone marrow and body fluids. Generally there is sufficient time for the CMC resident to sit in on the sign-out at Parkland and vice versa. v. The resident will act as a first line resource for hematology wet lab problems during business hours (8 a.m. to 5 p.m.) vi. The resident will attend and actively participate in weekly HPLC sign-out at CMC. 2. Level II i. Demonstrate mastery of all of the objectives from the Level I rotation. ii. Demonstrate the progressive mastery of lymph node/lymphoid tissue based diseases. iii. The senior resident may assist in supervising junior residents when performing bone marrow and peripheral blood differential counts at the beginning of the rotation. iv. The resident will take responsibility for some interdivisional consult cases at the discretion of the hematopathology faculty and fellows. These cases may be more complex than routine cases and require a greater level of involvement with regard to obtaining clinical history, interpreting ancillary tests, generating reports, and communicating with consulting pathologists and/or clinicians. C. Supervision/Assessment 1. How are the interpretive skills assessed and by whom? i. Level I 1. Junior residents performing bone marrow differential counts will be supervised directly by senior level residents, hematopathology fellows, and hematopathology faculty at the beginning of the rotation. Junior residents are responsible for maintaining a log of the first three bone marrow differential counts they perform. Once proficiency in performing bone marrow differential counts in three separate cases has been verified, junior residents may perform these procedures without direct supervision. However, fellows and attendings will be available in-house to assist, if necessary, during business hours (8 a.m. to 5 p.m.). After hours, hematopathology fellows and attendings are available to assist on call, if necessary. 2. Performance will be assessed through direct observation by hematopathology faculty, fellows, and senior residents, as well as through oral quizzes during daily sign-out, weekly flow cytometry conference, and unknown conferences. Faculty will provide direct verbal feedback for each case at the time of sign-out. The rotation director will administer a bone marrow differential quiz to junior residents after the first week of the rotation. The rotation director will discuss verbal and written assessments provided by faculty, fellows, supporting staff, and clinicians at both the midpoint and endpoint of the rotation. ii. Level II 1. The resident's performance will be assessed through direct observation by hematopathology faculty and fellows, as well as through oral quizzes during daily sign-out, weekly flow cytometry conference and unknown conferences. Faculty will provide direct verbal feedback for each case at the time of sign-out. 2. The rotation director will discuss verbal and written assessments provided by faculty, fellows, supporting staff, and clinicians at both the midpoint and endpoint of the rotation.