Development and implementation of a transitions of care service in... ambulatory care setting in collaboration with a primary care physician
advertisement

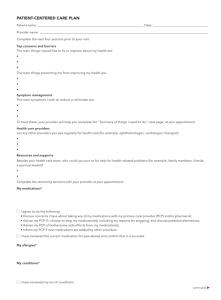
9 - 158 Development and implementation of a transitions of care service in an ambulatory care setting in collaboration with a primary care physician Rachel J. Pucel, Pharm.D., CTTS, Michael J. Rush, Pharm.D., CDE, BCACP, CTTS, Karen L. Kier, Ph.D., M.Sc., R.Ph., BCPS, BCACP Transitions of care (TOC) from a hospital to primary care physician's (PCP’s) office have been characterized as “unsystematic, non-standardized, and fragmented.” 1 Adverse drug events (ADEs) occurrence is the highest when moving from one healthcare setting or provider to another, which results in re-hospitalizations. 2 Of the 20% of Medicare beneficiaries readmitted within 30 days of discharge, an alarming 50% lacked a PCP visit between hospitalizations. 3 This lack of coordination and inadequate communication between settings/providers need to be resolved in order to reduce ADEs and readmission rates. Various models have been implemented and documented utilizing hospital pharmacist’s performing medication reconciliation, discharge counseling, and coordination with outpatient follow-up. 4,5,6,7 However, efforts need to be streamlined to the ambulatory care setting to help ensure patients have appropriate medication regimens and counseling following discharge. Primary objective: To assess the impact of a pharmacist-directed TOC clinic in a PCP setting to reduce medication-related problems. Secondary objective: To assess interventions recommended by the pharmacist and accepted in collaboration with the PCP. ONU HealthWise is an interdisciplinary disease state management and preventive medicine program. Ada Area Family Practice (AAFP) is a solo practitioner family practice office located in rural Hardin county that has a collaborative practice with ONU HealthWise. This TOC clinic will be a new service at AAFP. Inclusion: Established patients of AAFP, ≥18 yo, recently discharged from the hospital Exclusion: Cognitively impaired without responsible caregiver, or do not provide informed consent AAFP will receive notice of their established patient’s hospital discharge via discharge summary sent from hospital and/or notification from patient. Prior to potential appointment, a pharmacist team member will provide initial screening of hospital course focusing on reason for hospitalization, hospital course, medications added, stopped or changed and medication-related problems. (See After Hospital Care Plan to right) Medication-related problems include but are not limited to: duplicate therapy, wrong drug/dose, medication indicated but not prescribed, lack of indication, medication allergy, and adverse drug events. The pharmacist will utilize a modified version of Project BOOST’s 8P’s for risk assessment to determine the extent of follow-up provided. (See chart below) To provide timely access to care, the office manager will schedule face-to-face or phone follow-up appointments within 7 days of discharge in collaboration with PCP. Risk Assessment: 8P Screening tool # of Problem Medications Anticoagulants, insulin, aspirin & clopidogrel dual therapy, digoxin, narcotics Psychological Principal Diagnosis Heart failure, COPD, Pneumonia, Stroke, Cancer Polypharmacy- Number of Medications Number of medication-related problems screened for Poor Health Literacy (inability to do TeachBack) Patient Support (Absence of caregiver to assist with discharge) Prior Hospitalization/ ED visit ** This After Hospital Care Plan will be the chart note used to gather information, identify medication-related problems, and develop a plan for each patient. It will be kept with the patient’s paper chart in the physician’s office. High Risk = Face-to- Moderate Risk = Low Risk = No face follow-up Phone follow- up follow-up ≥1 0 0 Diagnosis or history No diagnosis or of depression history of depression Present Not present ≥5 1+ 1-4 0 No diagnosis or history of depression Not present 0 0 Unknown until follow-up No Caregiver Caregiver/SelfCaregiver/Selfsufficient sufficient < 6 months > 1 year > 6 months – 1 year Palliative Care Participating in No palliative care No palliative care palliative care indicated indicated ** The highest category a patient falls in will determine the extent of follow-up that patient will receive. During the follow-up visit, the pharmacist will provide comprehensive medication reconciliation, further identify medication-related problems, determine the need to adjust medications, follow-up on test results, and order additional monitoring in collaboration with PCP. Pharmacist will also provide education about patient’s disease states, medications, importance of adherence, and self-management while providing an updated, reconciled medication list to the patient, reinforcing changes in the plan, and ensuring their next PCP appointment is scheduled. Patient demographics, summarized discharged information, number and type of medication-related problems, number of interventions recommended, and number of interventions accepted by the collaborating physician will be documented. This study was approved by ONU’s Institutional Review Board. Enrollment in this study is ongoing. Since implementation in November: 3 patients have been screened; 2 – highrisk and 1 – low-risk. Patient A: On 8 medications, 1 medication-related problem – inaccurate medication list at PCP office, 1 intervention recommended and 1 accepted Patient B: On 7 medications - 6 new, 5 medication-related problems – treatment not optimal based on current evidence (3), no indication for medication (1), adverse drug event (1), 5 interventions recommended and 2 accepted Results are pending and will be submitted for publication. 1. 2. 3. 4. National Quality Forum (NQF). Safe Practices for Better healthcare – 2010 Update: A consensus Report. Washington, DC: NQF; 2010. Hume AL, Kirwin J, Bierber HL, et al. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy. 2012; 32: 326-37. Jencks S, William M, Coleman E. Rehospitalizations among patients in the medicare fee-for service program. N Engl J Med. 2009;360;14:1418-28 Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150: 178-87. 5. Coleman EA, Parry C, Chalmers S, et al. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166: 1822-8. 6. Marusic S, Gojo-Tomic N, Erdeljic V, et al. The effect of pharmacotherapeutic counseling on readmissions and emergency department visits. Int J Clin Pharm 2013;35:37-44. 7. Schall M, Coleman E, Rutherford P, Taylor J. How-to guide: Improving Transitions from the Hospital to the Clinical Office Practice to Reduce Avoidable Hospitalization. Cambridge, MA: Institute for Healthcare Improvement; June 2013. Available at www.IHI.org Authors of this presentation have no known financial or personal relationships with commercial entities that may have a direct or indirect interest in the subject matter of this presentation.