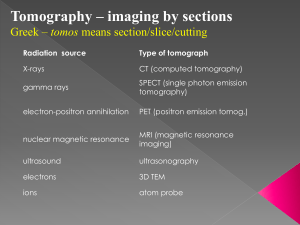
Computed Tomography Introduction to Computed Tomography [CT], and Magnetic Resonance Imaging [MRI]
advertisement
![Computed Tomography Introduction to Computed Tomography [CT], and Magnetic Resonance Imaging [MRI]](http://s2.studylib.net/store/data/010343892_1-cce268b3c5327e3bb79ee0c6832fe079-768x994.png)
Introduction to Computed Tomography [CT], and Magnetic Resonance Imaging [MRI] Computed Tomography • Collimated X-ray technique – Individual slices – Spiral slicing Daniel A. Feeney DVM, MS Professor of Veterinary Radiology College of Veterinary Medicine • Two-dimensional display of sectioned anatomy in “axial” plane with option of multi-planar reconstruction of contiguous data • Window & Level Viewing Options • Digital Images (DICOM) University of Minnesota 1 Computed Tomography 3 Computed Tomography 5 2 Computed Tomography 4 Standard Computed Tomography Voxel & Pixel Creation 6 (from Feeney, et. al.) 1 Computed Tomography Voxel & Pixel Computed Tomography (from Feeney, et. al.) (from Feeney, et. al.) CT Numbers Image 7 8 Computed Tomography [window width] (from Morgan) 9 Computed Tomography [window level] (from Morgan) 10 Computed Tomography [window/level] Computed Tomography • Intravenous Contrast Enhancement: – Usually scanned as “pre” followed by “post” contrast series using same scan parameters (e.g. kVp, slice thickness, slice interval, pitch, etc.) – Based on the use of sterile iodinated contrast medium: • Ionic (cheaper) • Nonionic (preferred for safety) • Basis of “enhancement” is X-ray attenuation from iodine in vessels or iodine that has “leaked” into tissues – Useful to outline vessels for CT angiography – Abnormalities “enhance” [appear brighter] due to: Lung Soft-tissue 11 Bone • Endothelial barrier breakdown, particularly “blood-brain” • Delayed vascular flow of blood + contrast mixture through tortuous tumor-induced vessels which lack autoregulation 12 2 Computed Tomography • Iodinated Contrast Medium: – Ionic, sterile • Meglumine and/or Sodium + Diatrizoate or Iothalamate • Approved for intravascular use • Primary uses include: – – – – physiologic organ “enhancement” blood flow detection or tracing detection of vascular leakage lower urogenital track (retrograde) opacification Computed Tomography • Iodinated Contrast Media: – Nonionic, sterile • Iopamidol, Iohexol, Ioversol,.. • Approved for intravascular (some also intrathecal) use • Primary uses include: – – – – 13 Computed Tomography physiologic organ “enhancement” blood flow detection or tracing detection of vascular leakage definition of subarachnoid space (if approved) 14 Computed Tomography Spiral CT • Standard CT: (higher resolution) – full 360o slice without table motion – image thickness 1, 2, 5, 10 mm thick made at any interval > 1mm (e.g. 5 mm thick slices @ 5 mm interval) • Spiral CT: (higher speed) – full 360o slice with table motion during the tube/gantry rotation – image generated as defined slice collimation exposed during simultaneous tube/gantry rotation and table linear motion • o Pitch = distance traveled by tube/gantry during 360 rotation slice collimation thickness – image thickness selected from dataset defined by spiral slicing reconstruction algorithm 15 Computed Tomography 16 Computed Tomography Topics • • • • • • • 17 Cranial Neurologic Deficits Spinal Neurologic Deficits Cancer Staging Nasal Disease Clarification Problematic Lameness Abdominal Mass Clarification Complex Vascular Disease 18 3 L3-L4 Disk 19 L-S Disk 21 182342 Nasal Tumor 23 L3-L4 Disk 20 L-S Disk 22 182342 Nasal Tumor 24 4 182342 Nasal Tumor 25 Neurofibrosarcoma 27 Neurofibrosarcoma.2 29 Neurofibrosarcoma 26 Neurofibrosarcoma 28 180526 Neurofibrosarcoma.2 30 5 CT References CT References • Feeney DA, Fletcher TF and Hardy RM: Atlas of Correlative Imaging Anatomy of the Normal Dog: Ultrasound and Computed Tomography. WB Saunders, Philadelphia, 1991. • Morgan CL: Basic Principles of Computed Tomography. University Park Press, Baltimore, 1983. • Brink JA, Heiken JP, Wang G, et. al.: Helical CT: Principles and Technical Considerations; Radiographics 1994;14:887-893. • Dalrymple NC, Prasad SR, Freckleton MW and Chintapalli KN: Informatics in Radiology: Introduction to the language of three-dimensional imaging with multidetector CT. Radiographics 2005;25:1409-1428. • Rydberg J, Laing Y and Teague SD: Fundamentals of multichannel CT. Radiol Clin North Am 2003;41:465474. 31 Computed Tomography 33 Magnetic Resonance Imaging 35 32 Magnetic Resonance Imaging 34 Magnetic Resonance Imaging 36 6 Magnetic Resonance Imaging Magnetic Resonance Imaging • Deposition in and Retrieval/Localization of Radiofrequency Energy from Tissue/Organs in a Static Magnetic Field • Based on protons (hydrogen nuclei) which when placed in a magnetic field (0.3 3.0+ Tesla) act like spinning tops (precessing) around the magnetic field Bo. • “Resonant Frequency” of Hydrogen [42.6 MHz/T*] • Individual slices • Volume imaging [multiple slices] • Two-dimensional display of sectioned anatomy in any plane (Digital DICOM Images) • Varied Pulse Sequences to Emphasize Fat, Water, or Paramagnetic Contrast Medium “leakage/presence” * Tesla (T) = measure of magnetic field strength with earth’s magnetic field +/- 0.00005 T 37 38 Magnetic Resonance Imaging In Bo, No RF Input Magnetic Resonance Imaging T1 (longitudinal) relaxation time is when 63% of the net magnetic vector has returned to alignment with Bo [spin-lattice] In Bo, With RF Input 0.63 Decayed Vectors Peak Vector 0.37 Decayed Magnetic Vector 39 40 Magnetic Resonance Imaging 41 T2 (transverse) relaxation time is when the net magnetic vector has decayed to 37% of its peak due to dephasing [spin-spin] • Energy states of precessing tissue protons are random • Bo field promotes alignment (spin-up or spin-down) • RF pulse changes Bo aligned protons into alignment at 90o to 180o and a higher energy state • As RF-induced alignment decays, energy is emitted and detected Magnetic Resonance Imaging • In a magnetic field Bo onto which the following are superimposed: •Longitudinal magnetic gradient (slice selection @ Larmor Hz) usually in the “Z” direction • Frequency encoding gradient (applied during signal readout) “X” or “Y” direction •Phase encoding gradient (applied between RF excitation and signal readout) “X” or “Y” direction 42 7 Magnetic Resonance Imaging Magnetic Resonance Imaging • Patient in Magnet with Slice Selected: Pixel/Voxel transverse Z longitudinal Voxels defined in the slice (selected by Bo gradient) using reversible phase and frequency gradients 44 43 Magnetic Resonance Imaging Magnetic Resonance Imaging Spin-echo Pulse Sequence 180o 180o 90o 90o TR = repetition time TE = echo time 45 46 Magnetic Resonance Imaging Image Contrast (weighting) Short TE Long TE Short TR T1W ____ Long TR PD T2W TR = repetition time TE = echo time T1W = T1-weighted (bright fat) T2W = T2-weighted (bright fluid) PD = Proton Density-weighted (grey-white matter) 47 Magnetic Resonance Imaging • Intravenous Contrast Enhancement: – Usually scanned as “pre” followed by “post” contrast series using same scan parameters (e.g. TR, TE, slice thickness, slice interval, etc.) – Based on the use of sterile gadolinium-based medium: • • • • Ionic (cheaper) Nonionic (preferred for safety) Macro-cyclic (most expensive, ? safest) Basis of “enhancement” is shortening of the T1 relaxation time due to the gadolinium derivative in vessels or which has “leaked” into tissues – Useful to outline vessels for MR angiography – Abnormalities “enhance” [appear brighter] due to: • Endothelial barrier breakdown, particularly “blood-brain” • Delayed vascular flow of blood + contrast mixture through tortuous tumor-induced vessels which lack autoregulation 48 8 Magnetic Resonance Imaging Brain Tumor • Paramagnetic Contrast Media: – Gadolinium: • • • • • Dimeglumine Gadopentate (ionic) Dimeglumine Gadobendate (ionic) Gadoteridol (non-ionic, macro-cyclic) Gadoversetamide (non-ionic) Gadodiamide (non-ionic) – For intravascular and, if approved, intrathecal use – Primary uses include: • physiologic organ “enhancement” • blood flow detection or tracing • detection of vascular leakage 49 50 Disk Herniation Lead Toxicity [Bald Eagle] 51 52 Vertebral Myeloma Brachial Plexus Tumor T2 sag T1 Gd T2 Dorsal Post Gd T1 [normal] T2 Axial 53 Pre Gd 54 9 Single, Extra-hepatic Portosystemic Shunt 55 MR References • Rummeny EJ, Reimer P and Heindel W: MR Imaging of the Whole Body. Thieme Medical, Stuttgart, 2009. • Runge V, Nitz W and Schmetts S: The Physics of Clinical MR Taught Through Images. Thieme Medical, Stuttgart, 2009. • Lin S and Brown J: MR Contrast Agents: physical and pharmacologic basics. J Mag Res Imag 2007;25:884-899. • Westerbrook C: Handbook of MRI Technique. WileyBlackwell, West Sussex, 2008. • Numerous Authors: Selected topics in MR Neuroimaging. Mag Res Clin 2006;14:127-285. 56 10