EDITOR’S CORRESPONDENCE
RESEARCH LETTER
ONLINE FIRST
Use and Outcomes of Telemetry Monitoring
on a Medicine Service
T
elemetry is a powerful tool for real-time monitoring of a patient’s heart rhythm and QRS pattern. Beds with telemetry monitoring are limited and expensive in most institutions; therefore, the use
of this resource would ideally be evidence based.1 American Heart Association (AHA) guidelines provide class I,
II, and III indications for the use of telemetry, but the
focus is almost exclusively on cardiac diagnoses, such as
admissions for rule-out acute coronary syndrome or heart
block.2 However, there are far fewer data that describe
criteria for the use of telemetry in a general medical population.3 In the largest study of telemetry to date, only 121
of 2240 patients (5%) who underwent telemetry were admitted with noncardiac diagnoses.4 We performed a study
to better characterize the reasons why patients on a medicine service are placed on telemetry monitoring as well
as the frequency of clinically significant telemetry events.
Methods. A prospective, observational study was conducted in 2010 and 2011 at the University of California,
San Francisco, Medical Center, a large universityaffiliated teaching hospital. The study was approved by
the university’s institutional review board. We enrolled
a convenience sample of consecutive adult patients who
were admitted or transferred to the medicine service with
telemetry monitoring on a single unit of the hospital. Each
day, we asked the telemetry technician for new admissions and discharges from telemetry as well as the telemetry events for all patients whom we were tracking. For
each new admission to telemetry, we administered a paper or an e-mail survey to the intern, subintern, or hospitalist who admitted the patient. For each discharge from
telemetry, we administered a phone survey to the intern
or the subintern who was responsible for that patient.
Other clinical and demographic information was elicited from the electronic medical record system.
Our primary outcomes of interest were telemetry events
and management changes in response to telemetry events.
A telemetry event was defined as any change in heart
rhythm logged by the telemetry technician that was different from the admission heart rhythm. Management
changes in response to telemetry events were identified
by the primary team members when they completed the
day-of-discharge surveys.
ARCH INTERN MED
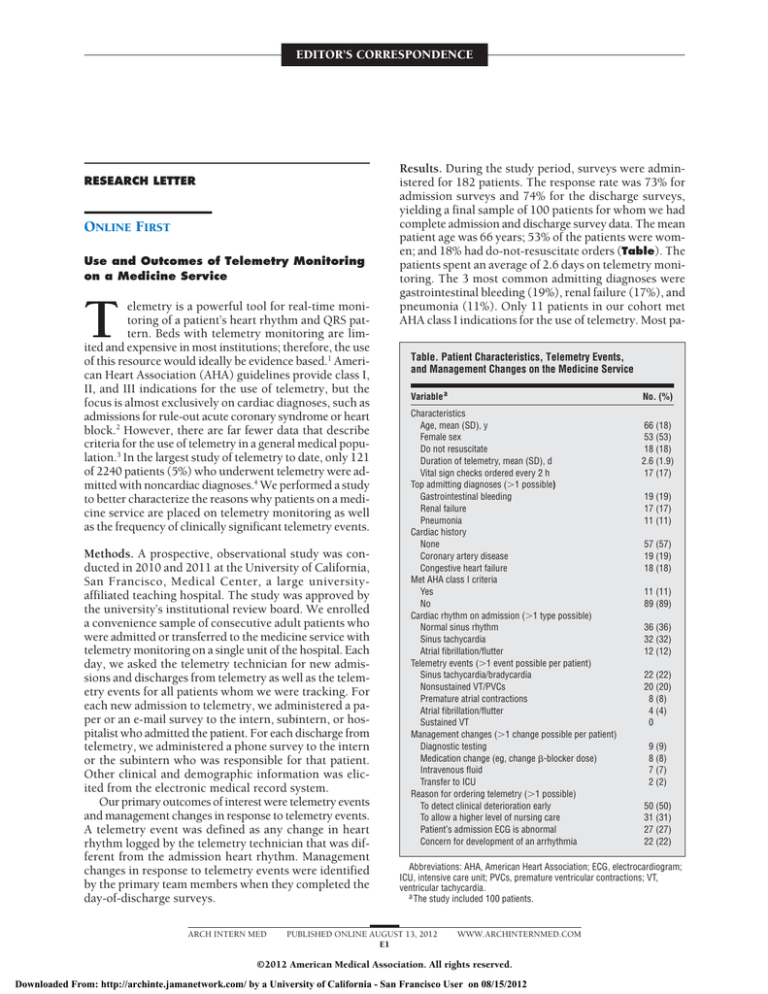
Results. During the study period, surveys were administered for 182 patients. The response rate was 73% for
admission surveys and 74% for the discharge surveys,
yielding a final sample of 100 patients for whom we had
complete admission and discharge survey data. The mean
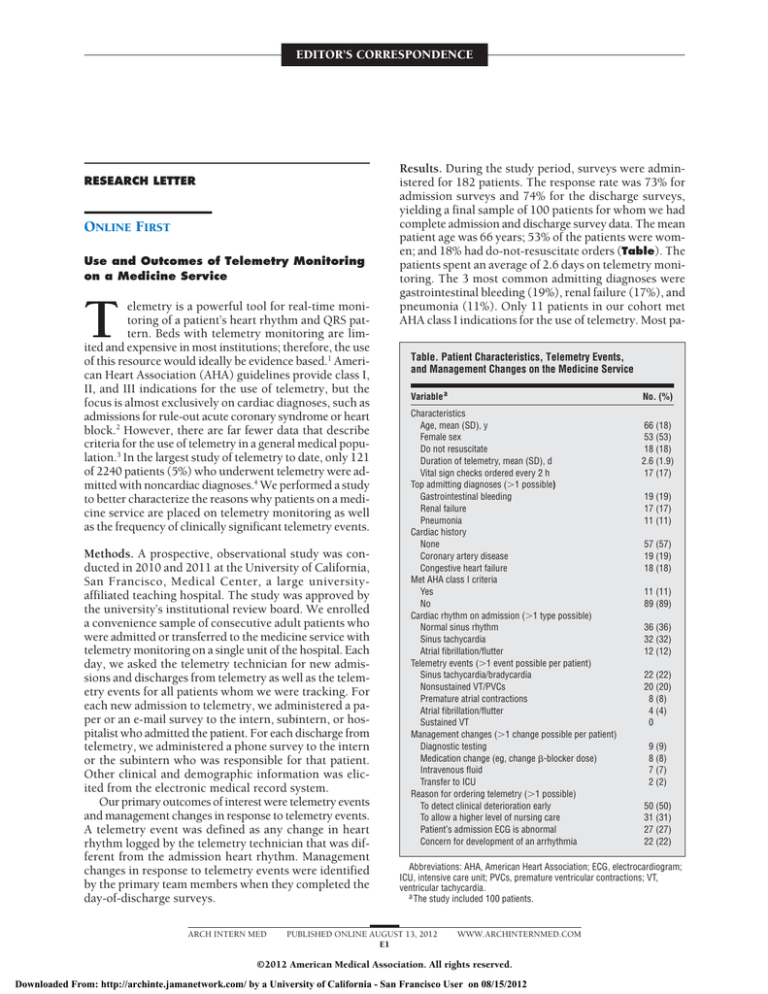
patient age was 66 years; 53% of the patients were women; and 18% had do-not-resuscitate orders (Table). The
patients spent an average of 2.6 days on telemetry monitoring. The 3 most common admitting diagnoses were
gastrointestinal bleeding (19%), renal failure (17%), and
pneumonia (11%). Only 11 patients in our cohort met
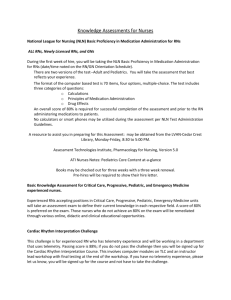
AHA class I indications for the use of telemetry. Most paTable. Patient Characteristics, Telemetry Events,
and Management Changes on the Medicine Service
Variable a
No. (%)
Characteristics
Age, mean (SD), y
Female sex
Do not resuscitate
Duration of telemetry, mean (SD), d
Vital sign checks ordered every 2 h
Top admitting diagnoses (⬎1 possible)
Gastrointestinal bleeding
Renal failure
Pneumonia
Cardiac history
None
Coronary artery disease
Congestive heart failure
Met AHA class I criteria
Yes
No
Cardiac rhythm on admission (⬎1 type possible)
Normal sinus rhythm
Sinus tachycardia
Atrial fibrillation/flutter
Telemetry events (⬎1 event possible per patient)
Sinus tachycardia/bradycardia
Nonsustained VT/PVCs
Premature atrial contractions
Atrial fibrillation/flutter
Sustained VT
Management changes (⬎1 change possible per patient)
Diagnostic testing
Medication change (eg, change -blocker dose)
Intravenous fluid
Transfer to ICU
Reason for ordering telemetry (⬎1 possible)
To detect clinical deterioration early
To allow a higher level of nursing care
Patient’s admission ECG is abnormal
Concern for development of an arrhythmia
66 (18)
53 (53)
18 (18)
2.6 (1.9)
17 (17)
19 (19)
17 (17)
11 (11)
57 (57)
19 (19)
18 (18)
11 (11)
89 (89)
36 (36)
32 (32)
12 (12)
22 (22)
20 (20)
8 (8)
4 (4)
0
9 (9)
8 (8)
7 (7)
2 (2)
50 (50)
31 (31)
27 (27)
22 (22)
Abbreviations: AHA, American Heart Association; ECG, electrocardiogram;
ICU, intensive care unit; PVCs, premature ventricular contractions; VT,
ventricular tachycardia.
a The study included 100 patients.
PUBLISHED ONLINE AUGUST 13, 2012
E1
WWW.ARCHINTERNMED.COM
©2012 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a University of California - San Francisco User on 08/15/2012
tients (57%) had no cardiac history. The initial rhythm
for most patients was normal sinus rhythm or sinus tachycardia, and the most common telemetry events were sinus bradycardia, sinus tachycardia, and premature ventricular contractions. Four patients developed new atrial
fibrillation or flutter. Nineteen patients had management changes in response to telemetry events. Because
more than 1 intervention was possible per patient, 9 patients underwent diagnostic testing, 8 had medications
changed, 7 had intravenous fluids administered, and 2
were transferred to the intensive care unit.
When asked why they chose to place their patients on
telemetry, 50% of physicians responded “to detect clinical deterioration early” and 22% responded “concern for
development of an arrhythmia.” Although our sample size
and event rate were too small to draw meaningful statistical conclusions, neither the 2 patients who required transfer to the intensive care unit nor the 2 others who developed new atrial fibrillation or flutter met AHA class I criteria.
Comment. This study differs significantly from previous studies of telemetry in that the study population comprised patients who were admitted to a medicine service, not for a primary cardiac diagnosis.4-7 We found that
very few patients had clinically meaningful telemetry
events and even fewer had events that prompted a change
in therapy. None of the patients who had significant events
would have met AHA criteria for an indicated use of telemetry. This suggests that perhaps the AHA criteria,
which were developed for cardiac patients, may not be
applicable to patients with primary medical diagnoses.
Also, few studies asked physicians why they chose telemetry. We found that a concern for clinical deterioration, rather than an explicit concern for development of
arrhythmia, drove most of the telemetry use. This finding
is notable because telemetry does not replace more frequent vital sign checks or lower nurse to patient ratios and
may lead both nurses and physicians to feel a false sense
of security regarding their patient’s monitoring.
Nader Najafi, MD
Andrew Auerbach, MD, MPH
Published Online: August 13, 2012. doi:10.1001
/archinternmed.2012.3163
Author Affiliations: Division of Hospital Medicine, University of California, San Francisco.
ARCH INTERN MED
Correspondence: Dr Najafi, Division of Hospital Medicine, University of California, San Francisco, 505 Parnassus Ave, PO Box 0131, San Francisco, CA 94143
(nnajafi@medicine.ucsf.edu).
Author Contributions: Both authors had full access to all
the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study
concept and design: Najafi and Auerbach. Acquisition of data:
Najafi and Auerbach. Analysis and interpretation of data:
Najafi and Auerbach. Drafting of the manuscript: Najafi and
Auerbach. Critical revision of the manuscript for important
intellectual content: Najafi and Auerbach. Statistical analysis: Najafi and Auerbach. Obtained funding: Auerbach.
Administrative, technical, and material support: Auerbach.
Study supervision: Auerbach.
Financial Disclosure: None reported.
Funding/Support: Dr Auerbach is supported by grant K24
K24HL098372 from the National Heart, Lung, and Blood
Institute.
Previous Presentations: This study was presented as a poster
at the Society of General Internal Medicine CaliforniaHawaii Regional Meeting; January 21, 2012; San Francisco, California; and at the Society of Hospital Medicine
Annual Meeting; April 2, 2012; San Diego, California.
1. Henriques-Forsythe MN, Ivonye CC, Jamched U, Kamuguisha LK, Olejeme
KA, Onwuanyi AE. Is telemetry overused? is it as helpful as thought? Cleve
Clin J Med. 2009;76(6):368-372.
2. Drew BJ, Califf RM, Funk M, et al; American Heart Association; Councils on
Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in
the Young. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized
Electrocardiology and the American Association of Critical-Care Nurses.
Circulation. 2004;110(17):2721-2746.
3. Chen EH, Hollander JE. When do patients need admission to a telemetry bed?
J Emerg Med. 2007;33(1):53-60.
4. Estrada CA, Rosman HS, Prasad NK, et al. Evaluation of guidelines for the
use of telemetry in the non–intensive-care setting. J Gen Intern Med. 2000;
15(1):51-55.
5. Curry JP, Hanson CW III, Russell MW, Hanna C, Devine G, Ochroch EA.
The use and effectiveness of electrocardiographic telemetry monitoring in a
community hospital general care setting. Anesth Analg. 2003;97(5):14831487.
6. Tiongson J, Robin J, Chana A, Shin DD, Gheorghiade M. Are the American
College of Cardiology/Emergency Cardiac Care (ACC/ECC) guidelines useful in triaging patients to telemetry units? Acute Card Care. 2006;8(3):155160.
7. Durairaj L, Reilly B, Das K, et al. Emergency department admissions to inpatient cardiac telemetry beds: a prospective cohort study of risk stratification
and outcomes. Am J Med. 2001;110(1):7-11.
PUBLISHED ONLINE AUGUST 13, 2012
E2
WWW.ARCHINTERNMED.COM
©2012 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a University of California - San Francisco User on 08/15/2012