Chapter 26 Physiology of the Digestive System
advertisement

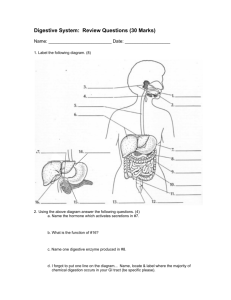
Chapter 26 Physiology of the Digestive System OVERVIEW OF DIGESTIVE FUNCTION • Primary function of the digestive system: to bring essential nutrients into the internal environment so they are available to every cell in the body • Mechanisms used to accomplish the primary function of the digestive system (Figure 26-1, Table 26-1) – Ingestion: food is taken in – Digestion: breakdown of complex nutrients into simple nutrients – Motility of the gastrointestinal (GI) wall: physically breaks down large chunks of food material and moves food along the tract – Secretion of digestive enzymes allows chemical digestion – Nutrients are absorbed into the internal environment through the GI mucosa 2 – Material that is not absorbed is eliminated 3 Digestion • All the processes that chemically and mechanically break down food into nutrients • Begins immediately after food is ingested • 2 types: Mechanical and Chemical – Mechanical – movement of the GI tract which: • Changes the physical state of food to facilitate chemical digestion • Churning of the contents in the GI lumen so they are well mixed with the GI juices • Propelling food through the digestive tract Mechanical Digestion • Mastication – reducing the food particle size through chewing, and mixes food with saliva • Deglutition – swallowing 1. Oral Stage (moth to oropharynx) 2. Pharyngeal Stage (oropharynx to esophagus) 3. Esophageal Stage (esophagus to stomach) DIGESTION: MECHANICAL – Deglutition: process of swallowing; complex process requiring coordinated, rapid movements (Figure 26-2) • Oral stage (mouth to oropharynx): voluntarily controlled; formation of a food bolus in the middle of the tongue; tongue presses bolus against the palate and food is then moved into the oropharynx • Pharyngeal stage (oropharynx to esophagus): involuntary movement; to propel bolus from the pharynx to the esophagus, the mouth (tongue), nasopharynx (soft palate), and larynx (epiglottis) must be blocked; a combination of contractions and gravity move bolus into esophagus • Esophageal stage (esophagus to stomach): involuntary movement; contractions and gravity move bolus through esophagus and into stomach 6 DIGESTION: MECHANICAL (cont.) – Peristalsis and segmentation: two main types of motility produced by the smooth muscle of the GI tract; can occur together in an alternating fashion • Peristalsis: wavelike ripple of the muscle layer of a hollow organ; progressive motility that produces forward movement of matter along the GI tract (Figures 26-3 and 26-4) 8 DIGESTION: MECHANICAL (cont.) • Segmentation: mixing movement; digestive reflexes cause a forward-andbackward movement with a single segment of the GI tract; helps break down food particles, mixes food and digestive juices, and brings digested food in contact with intestinal mucosa to facilitate absorption (Figure 265) DIGESTION: MECHANICAL (cont.) – Regulation of motility • Gastric motility: – emptying the stomach takes approximately 2 to 6 hours – while in the stomach, food is churned (propulsion and retropulsion) and mixed with gastric juices to form chyme – chyme is ejected approximately every 20 seconds into the duodenum – gastric emptying is controlled by hormonal and nervous mechanisms (Figure 26-6) » Hormonal mechanism: fats in duodenum stimulate the release of gastric inhibitory peptide (GIP), which decreases peristalsis of gastric muscle and slows passage of chyme into duodenum » Nervous mechanism: receptors in the duodenal mucosa are sensitive to presence of acid and distention; impulses over sensory and motor fibers in the vagus nerve cause a reflex inhibition of gastric peristalsis; enterogastric reflex 10 DIGESTION: MECHANICAL (cont.) • Intestinal motility includes peristalsis and segmentation – Segmentation in duodenum and upper jejunum mixes chyme with digestive juices from the pancreas, liver, and intestinal mucosa – Rate of peristalsis picks up as chyme approaches end of jejunum, moving it through the rest of the small intestine into the large intestine – Chyme normally takes approximately 5 hours to pass through the small intestine – Peristalsis is regulated in part by intrinsic stretch reflexes but also is stimulated by the hormone cholecystokinin (CCK) 12 DIGESTION • Chemical digestion: changes in chemical composition of food as it travels through the digestive tract; these changes are the result of hydrolysis – Digestive enzymes • Extracellular, organic (protein) catalysts • Principles of enzyme action – Specific in their action (Figure 26-7) – Function optimally at a specific pH (changing pH changes the shape of the enzyme) – Most enzymes catalyze a chemical reaction in both directions – Enzymes are continually being destroyed or eliminated from the body and must continually be synthesized – Most digestive enzymes are synthesized as inactive proenzymes 13 DIGESTION: Chemical Digestion (cont’d) – Carbohydrate digestion (Figure 26-9) • Carbohydrates are saccharide compounds • Polysaccharides are hydrolyzed by amylases to form disaccharides • Carbohydrate digestion begins in the mouth and continues in the small intestine with amylase • Final steps of carbohydrate digestion are catalyzed by sucrase, lactase, and maltase, which are found in the cell membrane of epithelial cells covering the villi that line the intestinal lumen – Protein digestion (Figure 26-10) • Protein compounds are composed of twisted chains of amino acids • Proteases catalyze hydrolysis of proteins into amino acids • Main proteases: pepsin in gastric juice, trypsin in pancreatic juice, peptidases in intestinal brush border 14 DIGESTION: Chemical Digestion (cont’d) – Fat digestion (Figure 26-12) • Since fats are insoluble in water, they must be emulsified by bile in small intestine before being digested (Figure 26-11) • Bile is made of lecithin and bile salts • Lecithin and bile salts form micelles around fat droplets, making them more water soluble and easier to break down • Pancreatic lipase is the main fat-digesting enzyme – Residues of digestion: some compounds of food resist digestion and are eliminated as feces 17 Secretion • Saliva is made up of: – Water – helps liquify food into chyme – mucus – protects mucosa and lubricates food for easy passage – salivary amylase – carbohydrate digesting enzyme that works best in a neutral pH – Sodium bicarbonate – helps maintain neutral pH for amylase Secretion • Gastric juice – Made up of water, mucus and digestive enzymes secreted by gastric glands within gastric pits – Chief cells: secrete inactive pepsinogen which is activated by HCl to form pepsin – Parietal cells: secrete HCl • Chloride shift and Proton pump help stomach become more acidic and blood more basic • Produce IF which binds to B12 and facilitates its absorption in the SI Secretion • Pancreatic juice – Made up of water and inactive prozymes (zymogens) • Trypsinogen is activated by enterokinase to become trypsin (protein digesting) • Trypsin activates chymotrypsin (protein), lipases (fats), nucleases (DNA, RNA) and amylase (starch) • “reverse chloride shift” secretes H+ into the blood and bicarbonate into GI lumen; neutralizes the pH of the chyme Secretion • Bile – Secreted by the liver and stored in the gallbladder – Stimulated by CCK – Delivered to the duodenum via the cystic duct into the common bile duct – Contains cholesterol, bile pigments and products of detoxification for removal through feces • Intestinal juice – Basic, mucus solution that buffers and lubricates materials in the intestine CONTROL OF DIGESTIVE GLAND SECRETION • Digestive glands secrete when food is present in the digestive tract or when it is seen, smelled, or imagined • Nervous and hormonal mechanisms control the flow of digestive juices • Salivary secretion – Only reflex mechanisms control the secretion of saliva – Chemical and mechanical stimuli come from the presence of food in the mouth – Olfactory and visual stimuli come from the smell and sight of food 29 CONTROL OF DIGESTIVE GLAND SECRETION (cont.) • Gastric secretion: three phases (Figure 26-18) – Cephalic phase: called psychic phase because mental factors activate the mechanism (sight, smell, taste and thought of food) in the medulla oblongata • parasympathetic fibers in branches of the vagus nerve conduct stimulating efferent impulses to the glands to produce gastrin (by G cells in the stomach) – Gastric phase: when products of protein digestion reach the pyloric portion of the stomach, they stimulate release of gastrin • Gastrin accelerates secretion of gastric juice, ensuring enough enzymes are present to digest food; also secreted with stomach distension – Intestinal phase: various mechanisms seem to adjust gastric secretion as chyme passes to and through the intestinal tract; endocrine reflexes involving gastric inhibitory peptide, secretin, and CCK inhibit gastric secretions 30 31 CONTROL OF DIGESTIVE GLAND SECRETION (cont.) • Pancreatic secretion: stimulated by several hormones released by intestinal mucosa – Secretin, stimulated by acid in the duodenum, evokes production of pancreatic fluid low in enzyme content but high in bicarbonate to neutralize chyme – Cholecystokinin (CCK): several functions • Causes increased exocrine secretion from the pancreas • Opposes gastrin, thus inhibiting gastric hydrochloric acid secretion • Stimulates contraction of the gallbladder so that bile is ejected into the duodenum • Bile secretion: bile secreted continually by the liver; secretin and CCK stimulate ejection of bile from the gallbladder • Intestinal secretion: little is known about how intestinal secretion is regulated; suggested that the intestinal mucosa is stimulated to release hormones that increase the production of intestinal juice 32 ABSORPTION • Process of absorption – Passage of substances through the intestinal mucosa into the blood or lymph (Figure 26-19) – Most absorption occurs in the small intestine due to the large surface area created by the villi and microvilli 33 Absorption • Mechanisms – Water is absorbed through osmosis – Movement through secondary active transport • Na+ is pumped out of the cell creating a concentration gradient allowing Na+ to move out of the GI lumen • Glucose is too large and hydrophilic to move easily through the membrane; must be transported via Na+ cotransport • Amino Acids move similarly to glucose • After absorption, nutrients move through the hepatic portal system to the liver • Liver stores excess nutrients and the rest leave via the hepatic vein into systemic circulation 35 Lipid Absorption • • • • • • Include triglycerides, phospholipids, steroids, fatsoluble vitamins Bile salts and lecithin surround fatty acid and glycerol to form micelles Micelles approach the brush border, simple lipid molecules (FA) are released to pass through the membrane Inside the cell, the FA reunite to form large fat molecules and finally form chylomicrons Absorbed by lacteals and move through lymphatic system Water soluble chylomicrons allow fat to travel through the lymph and enter blood stream. 36 37 Absorption • Fat soluble vitamins – A,D,E,K depend on bile salts for absorption • Water soluble vitamins require transport • Most drugs are lipid soluble and can pass through the membrane 39 ELIMINATION • Definition: the expulsion of feces from the digestive tract; act of expelling feces is called defecation • Defecation occurs as a result of a reflex brought about by stimulation of receptors in the rectal mucosa that is produced when the rectum is distended (Figure 26-23) • Constipation: contents of the lower part of the colon and rectum move at a slower than normal rate; extra water is absorbed from the feces, resulting in a hardened stool • Diarrhea: result of increased motility of the small intestine, causing decreased absorption of water and electrolytes and a watery stool 40 41