Public Finance
advertisement

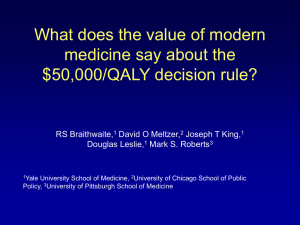
Economics 330 Economics of Health Care Dr. Greg Delemeester Spring 2010 National Health Care Expenditures Year Total Spending (in billions) Percent change Percent of GDP Per capita spending 1950 $ 13 -- 4.5 $ 82 1960 28 8.8 5.2 148 1970 75 10.5 7.2 356 1980 254 13.0 9.1 1,100 1990 714 10.9 12.3 2,814 2000 1,353 5.9 13.6 4,789 2005 1,982 7.9 15.7 6,701 2006 2,113 6.7 15.8 7,071 2007 2,240 5.6 15.9 7,423 2008 2,339 4.3 16.2 7,681 Source: http://www.cms.hhs.gov/NationalHealthExpendData/ Why do Americans spend so much on medical care? Aaron (1991) Expansion of 3rd party payment system Aging of the population Expanded medical malpractice litigation Increased use of medical technology Other factors Physician-induced demand Entry restrictions Predominance of not-for-profit providers Personal Health Care Expenditures (in billions of dollars) Private Spending Year Out of pocket Public Spending Private Insurance Federal State 1960 $ 12.9 $ 5.9 $ 2.0 $ 2.9 1970 24.9 14.0 14.4 7.8 1980 58.1 61.2 62.3 23.9 1990 136.1 204.7 172.8 63.5 2000 192.6 402.8 369.8 117.1 2005 247.5 599.8 562.3 176.9 2006 254.9 634.6 620.1 178.7 2007 270.3 665.0 661.3 188.7 2008 277.8 691.2 718.0 189.8 Source: http://www.cms.hhs.gov/NationalHealthExpendData/ 2008 National Health Care Dollar… …Where it Came From …Where it Went Private vs Public Spending on Personal Health Care Expenditures 90% 80% 70% % of PHCE 60% 50% Private Public 40% 30% 20% 10% 0% 1960 1965 1970 1975 1980 1985 1990 1995 2000 2005 2010 Spending as % of Personal Health Care Expenditues 60% 50% % of PHCE 40% Out of pocket Health Ins 30% Fed State 20% 10% 0% 1960 1970 1980 1990 2000 2010 Changes in Hospital Usage Short-Stay Community Hospital Characteristics, United States Category 1970 1980 1990 2000 Beds 4.17 4.38 3.73 2.93 (per 1,000 population) Admissions 144.0 159.6 125.4 117.6 (per 1,000 population) Average length of stay 7.7 7.6 7.2 5.8 (days) Outpatient visits 657.2 893.2 1,211.6 1,882.8 (per 1,000 population) Outpatient visits per 4.6 5.6 9.7 15.8 admission Percent occupancy 78.0 75.4 66.8 63.9 Source: Health United States, various years. 2003 2.79 2004 -- 2005 2.71 119.4 119.3 118.9 5.7 5.6 5.6 1,933.4 1,943.7 1,972.0 16.2 16.3 16.6 66.2 -- 67.3 Changes in Medical Care Delivery Shift from private to public financing Shift to 3rd party financing Changes in hospital usage and pricing Deregulation and growth in managed care Payment Structure Traditional fee structure Fee for service Retrospective payment Incentive to overspend Managed care Capitation and risk sharing Prospective payment Incentive to limit care Health Care As a Commodity Demand is irregular Asymmetric information problems Widespread uncertainty Reliance on not-for-profit providers Insurance as the primary means of payment Health System Goals Access to care Who’s covered? What’s covered? Quality of care Cost of care Private Health Insurance Coverage (under age 65, numbered in millions) With Health Insurance* Without Health Insurance Year Number Percent Number Percent 1999 161.2 68.3 38.5 16.1 2000 160.8 67.1 41.4 17.0 2001 162.4 67.0 40.3 16.4 2002 159.4 65.3 41.7 16.8 2003 157.5 64.4 41.6 16.5 2004 159.5 64.0 42.1 16.6 2005 160.1 63.6 42.1 16.4 2006 155.8 61.5 43.9 17.0 2007 157.9 61.6 43.3 16.6 * Employer-based. Source: Health, United States, 2008, http://www.cdc.gov/nchs/hus/updatedtables.htm, Table 138 and 140. Health System Goals Access to care Who’s covered? What’s covered? Quality of care Medical outcomes Medical efficacy Cost of care Who pays? How much? Review of Economic Methodology Economic Fundamentals Optimization Marginal Analysis Supply and Demand Equilibrium What are the likely consequences of the following events in the U.S market for cosmetic surgery? 1) Health insurance coverage is expanded to cover all elective procedures, such as tummy tucks, nose jobs, and liposuction 2) The FDA (Food and Drug Administration) takes all silicone-based implants off the market fearing a connection with certain connective-tissue diseases 3) Personal finance companies start a nationwide lending program for cosmetic procedures not covered by health insurance 4) Medical malpractice insurance premiums increase for plastic surgeons 5) Medical schools announce that residents in plastic surgery can be licensed after only five years instead of the current seven years Economic Fundamentals Optimization Marginal Analysis Supply and Demand Equilibrium Elasticity Welfare analysis Effects of government intervention Suppose the market for lasik eye surgery can be described by the following equations: Qd = 5100 – 6P Qs = - 400 + 5P a) b) c) d) Solve for the market equilibrium price and quantity. Calculate consumer and producer surplus. Calculate the elasticity of demand at the equilibrium. Suppose the government imposes an excise tax of $100 per surgery on eye surgeons. What is the new equilibrium price and quantity? What happens to social welfare? Competitive Market Model Many buyers/sellers Homogeneous product No entry barriers Perfect information $ MC ATC Profit max rule: P = MC AVC P1 MR1 LR Equil: π = 0 q1 quantity Market Failures Market Power Monopoly Restricted entry (AMA, CON) EOS Monopsony Externalities Communicable diseases/immunizations Uninsured and cost shifting Public goods Free-riders R&D Imperfections in Medical Markets Imperfect/Asymmetric information Agency problem (induced demand) Adverse selection Moral hazard Third-party payers Hospitals: 3¢ per $1 Physicians: 20¢ per $1 Dealing with Market Failure Collective provision Medicare Medicaid Government regulation Price controls Entry restrictions FDA Tax Policy Tax exemptions Government Failure? Economic Evaluation in Health Care The Inevitability of Trade-Offs The value of a medical intervention The inclusion of a drug on the formulary Paying for an experimental procedure Investing in new technology Is it worth it? How do we measure value to insure we get value for spending? Options for colorectal cancer screening Fecal blood test ($20) Sigmoidoscopy ($150 - $300) Barium enema ($250 - $500) Virtual Colonoscopy ($500 - $900) Colonoscopy ($800 - $1200) Is it worth the extra money? Types of Economic Evaluation Cost of illness studies Cost-benefit analyses Cost-effectiveness studies Cost of Illness Studies What does it cost? Burden of 5 chronic conditions in US (Druss et al., 2001) Mood disorders, diabetes, heart disease, asthma, and hypertension Direct cost of treatment: $62 billion Cost of treating coexisting conditions: $208 billion Lost productivity: $36 billion Role in analysis – increased awareness $306 billion Cost-Benefit Analysis Benefits today Costs Net PV = time Bt B1 B2 C0 1 2 (1 r ) (1 r ) (1 r )t The higher the discount rate, r, the lower the PV Cost-Benefit Criterion If net benefit stream is positive, project is acceptable n NPV t 1 Bt Ct t (1 r ) If ratio is greater than one, project is acceptable n B/C t 1 n Bt Ct / t t (1 r ) t 1 (1 r ) Examples Clarke (1998): mobile mammographic screening and travel cost method Ginsberg and Lev (1997): riluzole and ALS Challenges of Cost-Benefit Analysis Valuing benefits How do you place a value on a human life? Willingness-to-pay approach wealth life expectancy current health status possibility of substituting current consumption for future consumption Choosing a discount rate Cost-Effectiveness Analysis Measures health benefit by health outcome, not the dollar value of life Using the decision makers’ approach Maximize the level of health for a given population subject to a budget constraint Practical guide for choosing between programs or treatment options when budgets are limited Cervical Cancer Screening The medical evidence is clear: Cervical cancer screening saves lives. Much of the focus of cost-effectiveness research addresses issues concerning the appropriate screening interval. D.M. Eddy (Screening for cervical cancer, Annals of Internal Medicine 113, 214-226, 1990) studied the issue and estimated that annual screening for a hypothetical cohort of 1,000 22-year-old women screened until age 75 would cost $1,093,000 and would save 27.6 life years. If screened every three years instead, the cost would be $467,000 and 26.8 life years would be saved. Is annual screening cost effective? Incremental Cost-Effectiveness Ratio CB C A ICER EB E A If CA > CB and EA < EB, B dominates. If CA < CB and EA > EB, A dominates. If, however, CB > CA and EB > EA, choice is not obvious. Use CE. ICER Curve: 2 Treatments Effectiveness Large ICER = flat slope B EB EA ICER A CA CB CB C A EB E A Cost Cervical Cancer Screening: Redux D.M. Eddy (Screening for cervical cancer, Annals of Internal Medicine 113, 214-226, 1990) studied the issue and estimated that annual screening for a hypothetical cohort of 1,000 22-year-old women screened until age 75 would cost $1,093,000 and would save 27.6 life years. If screened every three years instead, the cost would be $467,000 and 26.8 life years would be saved. What is the ICER? 1,093,000 467,000 ICER $782,500 27.6 26.8 ICER Curve: Multiple Treatments Effectiveness “flat of the curve” G F D B A E C Treatments C and E are dominated Cost Measuring Costs Direct – associated with use of resources Medical Non-medical Indirect – related to lost productivity Intangible – associated with pain and suffering, grief, anxiety, and disfigurement Measuring Effectiveness Improvements in Health Surrogate measures stated in terms of clinical efficacy Blood pressure, cholesterol levels, bone mass density, or tumor size Intermediate measures stated in terms of clinical effectiveness Events (heart attack, stroke, cancer), scores on exams Final outcomes measure economic effectiveness Events avoided, disease-free days, life-years saved, quality-adjusted life years saved Problem Set 1: #16 Survival Measures Improved Life Expectancy Due to Clinical Treatment Life expectancy = area under survival function Survival probability 100% LE w/o treatment = ½(1.00-0.0)6.5 A B 90% 77% = 3.25 yrs Gain in LE during trial = ½(.90-.77)1.5 = 0.0975 yrs Gain in LE after trial = ½(.90-.77)5 = 0.325 yrs Total Gain in LE = 0.4225 yrs C Survival function for treatment group Survival function for control group D 1.5 6.5 Time (years) Quality of Life Measures: QALY Quality-Adjusted Life Year Measured on a preference scale anchored by death (0) and perfect health (1) Calculating a QALY Utility Normal 55-yr old male has LE of 25 more yrs Diabetic 55-yr old male has LE of 15 more yrs U(H1) x = healthy years t = chronic health years U(HD) 6 15 Value of one year in chronic health state is x/t Utility value of 15 years = 6/15 = 0.40 QALY of remaining 15 years = (.40)(15) = 6 years Time (years) Decision Trees Handout Mortality Rate Life Expectancy for Survivors Initial Treatment Cost Follow up cost, year 1 Annual follow up costs, all subsequent years Treatment A 2% 20 years Treatment B 5% 10 years $10,000 $5,000 $1,000 $3,000 $1,000 $500