Understanding Sharklet™ Surface Protection Products
A novel approach to improving cleanliness
of high-touch environmental surfaces
Using surface skins featuring the Sharklet™ pattern to decrease
microbial burden on environmental surfaces
April 2012
© Sharklet Technologies, Inc.
All rights reserved
2
Understanding the Sharklet Surface Protection Technology
About Sharklet™ – A New Approach in Bacterial Control.................................................................................. 3
Technology History ............................................................................................................................................ 4
The Role of Environmental Surfaces in Hospital-Acquired Infection Rates ....................................................... 4
Sharklet Technology and Test Results ............................................................................................................... 5
The Sharklet Surface Inhibits Bacterial Attachment, Survival and Touch Transfer ....................................... 7
MRSA and MSSA – Smooth vs. Sharklet™ .................................................................................................. 7
Pseudomonas aeruginosa – Smooth vs. Sharklet ..................................................................................... 8
Vancomycin-resistant Enterococcus faecalis – Smooth vs. Sharklet ......................................................... 8
The Next Generation in Surfaces ....................................................................................................................... 8
Contact Sharklet Technologies, Inc. ................................................................................................................... 9
References ....................................................................................................................................................... 10
www.sharklet.com
3
About Sharklet™ – A New Approach in Bacterial Control
Sharklet Technologies, Inc. is a United States company based in Aurora, Colorado. The biotechnology company
develops a revolutionary surface product called Sharklet™. Unlike anything in the marketplace today, Sharklet is the
only non-toxic, biocide-free and no-kill surface pattern used to inhibit microbial contamination on surfaces. The
Sharklet pattern is manufactured into surfaces of products to create bacterial inhibition and to reduce surface-to
person transfer of bacteria.
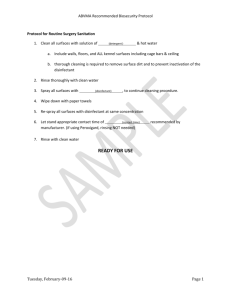
Sharklet is a patented surface technology
comprised of millions of raised,
microscopic features arranged in distinct
diamond shapes to form a continuous
micro-pattern (note the Sharklet pattern
at right). Each Sharklet diamond
measures 22 microns wide (left to right),
16 microns tall (top to bottom of a
diamond), and each feature is about 3
Scanning electron micrographs of the Sharklet micro-pattern with
microns in height. When manufactured
recessed grooves of varying lengths in silicone elastomer on the left
into the surface of products, the pattern
and the alternate version of the Sharklet pattern with raised features
cannot be seen with the naked eye or felt
on the right. Scale bars in both micrographs are 20 µm.
to the touch. For reference purposes, each
Sharklet diamond is about 1/50th the width of a human hair.
Of note, the Sharklet pattern provides bacterial inhibition through pattern alone – there are no chemicals, biocides,
disinfectants or antibiotics eluted from the surface. In tests simulating an ambient hospital environment, the Sharklet
patterned surface has shown to significantly reduce survival and touch transference of bacteria.
The Sharklet pattern is manufactured (imprinted) into the surfaces of products to create bacterial inhibition. While
multiple products that feature the Sharklet pattern are in development, Sharklet Technologies, Inc. today offers
Sharklet™ Surface Protection Products marketed under several brands including Tactivex® and SafeZone Media. The
Surface Protection Products are film-based products or “skins” that feature the Sharklet pattern imprinted into the
surface. The skins, via a variety of constructions including adhesively-backed films, are directly applied to high-traffic
touch points that harbor bacteria and serve as vectors for bacterial transfer.
Until the advent of Sharklet, kill strategies including antibiotics, disinfectants and biocides have been the primary
weapons to control bacterial growth. These kill strategies and their overuse has led to increased bacterial resistance,
causing harm to people and the environment. The World Health Organization in 2009 named resistant bacteria as a
top human health threat.
The applications and opportunities for Sharklet are numerous and the benefits of the benefits are measurable:
No risk for antimicrobial resistance. It is the shape and pattern of the surface alone that disrupts bacteria’s
ability to survive, not antimicrobial agents that contribute to the development of “superbugs.”
Defense against multiple strains of bacteria. Sharklet has shown to be effective against many Gramnegative and Gram-positive strains, including clinical isolates, in different media and flow conditions (e.g.
Staph a., MRSA, VRE, Pseudomonas aeruginosa and E. coli).
Cleaner surfaces between cleanings. The Sharklet pattern is always at work and serves as a safety net when
hand washing and cleaning protocols fail.
Ability to reduce costs with improved hygiene. In the healthcare sector, hospital-acquired infections account
for $30.5 billion in excess healthcare costs each year. The cost of these infections is estimated between
$8,000 and $15,000 per patient.
www.sharklet.com
4
Sharklet Technologies offers an effective new approach to microorganism control. The deployment of Sharkletpatterned surface products provides an opportunity to address challenges with infection control, enhance cleaning
protocols and protect bacteria-prone surfaces between cleanings.
Technology History
While the Sharklet pattern holds great promise to improve the way humans co-exist with microorganisms, the pattern
was developed far outside of a laboratory. Sharklet was discovered via a seemingly unrelated problem: how to keep
algae from coating the hulls of submarines and ships. In 2002, Dr. Anthony Brennan, a materials science and
engineering professor at the University of Florida, was visiting the United States naval base at Pearl Harbor in Oahu as
part of Navy-sponsored research. The U.S. Office of Naval Research solicited Dr. Brennan to find new antifouling
strategies to reduce use of toxic antifouling paints and trim costs associated with dry dock and drag.
Dr. Brennan was convinced that using an engineered topography could be a key to new antifouling technologies.
Clarity struck as he and several colleagues watched an algae-coated nuclear submarine leave port. Dr. Brennan
remarked that the submarine looked like a whale lumbering out of the harbor. In turn, he asked which slow moving
marine animals don’t foul. The only one? The shark.
Dr. Brennan was inspired to take an actual impression of shark skin, or more specifically, its dermal denticles.
Examining the impression with scanning electron microscopy, Dr. Brennan confirmed his theory. Shark skin denticles
are arranged in a distinct diamond pattern with tiny riblets. Dr. Brennan measured the ribs’ width-to-height ratios
which corresponded to his mathematical model for roughness – one that would discourage microorganisms from
settling. The first test of Sharklet yielded impressive results. Sharklet reduced green algae settlement by 85 percent
compared to smooth surfaces.
While the U.S. Office of Naval Research continued to fund Dr. Brennan’s work for antifouling strategies, new
applications for the pattern emerged. Brennan evaluated Sharklet’s ability to inhibit the growth of other
microorganisms. Sharklet proved to be a mighty defense against bacteria.
Similar to algae, bacteria take root singly or in small groups with the intent to establish large colonies, or biofilms. Also
similar to other organisms, bacteria seek the path of least energy resistance. Research results suggest that Sharklet
keeps biofilms from forming because the pattern requires too much energy for bacteria to colonize. The consequence
is that organisms find another place to grow or simply die from inability to signal to other bacteria. In addition to
evaluating Sharklet’s ability to inhibit biofilm formation, the technology also proved to inhibit bacteria’s ability to
attach and survive on the pattern.
The Role of Environmental Surfaces in Hospital-Acquired Infection Rates
Despite improved knowledge and greater focus prevention, incidences of healthcare-acquired infections (HAIs) have
continued to rise in recent decades. HAIs are now among the top six leading causes of death in the United States with
98,987 recorded deaths in 20021. The medical impact of these infections has been matched in magnitude by the
economic impact, which includes the costs of the treatment as well as the measures taken by the healthcare
community to control and limit the spread of infections. Efforts such as patient monitoring, active surveillance
protocols, screening-based isolation protocols, hand hygiene protocols and cleaning and disinfection procedures have
become ubiquitous to present-day healthcare epidemiology practice2,3,4.
The root of the challenge is in preventing the spread of HAI pathogens that lead to these infections. The most difficult
infections to treat are those that include antibiotic-resistant pathogens such as methicillin-resistant Staphylococcus
aureus (MRSA) and vancomycin-resistant Enterococcus (VRE), as well as spore-forming Clostridium difficile 3, 5. The
Health Care Infection Control Practices Advisory Committee (HICPAC) defines contact transmission of pathogens as
www.sharklet.com
5
occurring with a contaminated intermediate object or person (“indirect transmission”) or without (“direct
transmission”)6. It is well documented that pathogens readily contaminate environmental surfaces near patients and
can survive and persist on these inanimate surfaces for weeks to months 7,8,9,10. Examples of frequently touched
surfaces include bed rails, tray tables, telephones, bedside tables, patient chairs nurse call buttons/handsets9, 11, 12, 13.
Indirect transmission in the hospital environment occurs when these contaminated surfaces are touched; pathogens
are transferred from environmental surfaces to healthcare workers’ hands and objects, where they can then be
transported elsewhere14,15,16. In addition, recent scientific evidence confirms that patients admitted to rooms
previously occupied by patients infected or colonized with MRSA, VRE, C. difficile and Acinetobacter baumannii have,
on average, a 73 percent increased risk of acquiring the same pathogen from environmental surfaces contaminated by
the prior room occupants17,18,19,20,21,22.
In the past decade, numerous guidelines, recommendations, and standards have been introduced that relate to
improving environmental hygiene practices in healthcare settings. Healthcare infection control guidelines from the
Centers for Disease Control and Prevention (CDC) now emphasize the importance of cleaning and disinfecting ‘hightouch surfaces’ and monitoring these activities to maintain a sanitary environment in the hospital 6. These guidelines
reflect an evolving mindset that patient area environmental cleanliness in healthcare settings plays a significant role in
infection prevention and control.
Despite the increased attention to environmental hygiene, recent studies evaluating the effectiveness of
environmental cleaning have show that only 40 percent of near-patient surfaces are cleaned in accordance with
existing hospital policies2,12,13,18. Furthermore, certain multi-drug resistant organisms require specific cleaning
regimens and products, reflecting a dynamic situation that relies upon ever-changing guidelines and compliance4. In
contrast to the abundance of hand sanitizers and cleansers that have been introduced for hospital use to improve
hand hygiene, there are surprisingly few technological improvements for reducing environmental surface
contamination23.
The need for improved measures to keep environmental surfaces clean and prevent transmission of pathogens may
be addressed in the following ways:
1.
2.
Technologies / procedures to improve cleaning and disinfection of environmental surfaces
Surface technologies that reduce microbial presence on the surface.
Ideally, these two approaches would be implemented concurrently, where proper cleaning practices would be
complemented by a surface technology that reduces the risk of pathogen transmission between cleanings.
To address this need, Sharklet Technologies has developed and tested Sharklet – a novel, microscopic surface texture
to reduce microbial contamination compared to un-textured control surfaces.
Sharklet Technology and Test Results
Sharklet Surface Protection Products address a key unaddressed area of healthcare: surfaces. Today, much attention
is given to improving hand washing that reduces transfer of bacteria between people. Surface cleanliness is addressed
through the use of standard cleaning techniques including disinfection or through biocidal agents. Yet, reliance on
humans to adhere to these protocols begs the question of effectiveness.
Sharklet Surface Protection Products fill a gap in the hygiene continuum. A Sharklet-patterned surface is always at
work and provides a cleaner surface between cleanings. Sharklet surfaces also serve as a safety net when hand
washing and cleaning protocols fail. Further, the technology helps break the pathogen transmission loop by protecting
surfaces that are most often touched.
www.sharklet.com
6
Testing data demonstrates Sharklet has two general effects on bacteria to reduce surface contamination. When
compared to an un-patterned, smooth surface:
1.
2.
Less bacteria attach to the Sharklet pattern
Less bacteria survive on the Sharklet pattern over time
It is worth noting that competing strategies rely
mainly on chemical surface coatings to inhibit
bacterial adherence. The antimicrobial coating
strategy is hampered by the development of
antimicrobial resistant strains of bacteria and by
the harmful toxicity that many of these agents
rely upon for their biocidal effect. By
comparison, the Sharklet pattern adds no
chemical coatings or biocidal agents. This purely
physical approach to inhibiting microbial
attachment does not rely on the incorporation
of antimicrobial agents, thus sidestepping the
growing problem of multi-drug resistant
‘superbugs.’
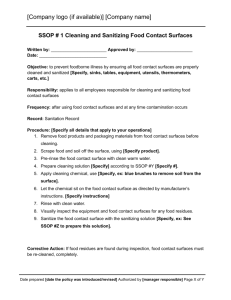
The photos above show colonies of S. aureus after one hour of
drying on surfaces. The RODAC plates were touched to surfaces
that were populated with S. aureus. The Sharklet surface in the
two top RODAC plates show significantly less attachment and
bacterial growth.
The development of antimicrobial coating methods
stem from the commonly held belief that cell
attachment is primarily influenced by the chemical
composition and activity of the surface. While this
is an important factor, the influence of surface
topography can be a significant factor in affecting cell attachment.
It has long been known that surface roughness is an important property affecting surface energy, which has motivated
the study of using micro-patterned surfaces to control cell attachment 24,25,26. While surface micro-patterns have been
studied in a trial-and-order fashion for randomly roughened surfaces and some ordered patterns, only recently has
the interrelationship of micro-pattern structure, surface energy and cell attachment been investigated 27. These
studies have indicated that geometries of ordered features designed with unique roughness properties can elicit
specific, predictable biological responses. This strategy for controlling bioadhesion represents a paradigm shift in the
current methods utilizing antimicrobial agents. Applying a surface topography, such as Sharklet, instead of using
antimicrobial agents relies upon controllably changing the surface energy so as to affect bioadhesion. Studies have
shown that the Sharklet micro-pattern is the most effective pattern of a variety of patterns studied for inhibiting
bioadhesion28.
Sharklet Technologies has performed bacterial testing in a number of environments. Testing has been performed by
numerous third parties including University of Florida, NASA (United States National Aeronautical Space
Administration), several leading U.S. medical device manufacturers and others. Numerous strains of Gram positive
and Gram negative bacteria have been tested including S. aureus, P. aeruginosa, S. epidermidis, E. coli, MRSA, VRE and
others. Testing has spanned 3 to 48 hours and between 7 and 21 days. Environments include Static (TSB, TSB+BSA,
TSB+FBS), Centers for Disease Control biofilm reactor, Static/Aerobic (no media, simulating typical room conditions,
20% relative humidity, 25-30C) and a host of others.
Testing in the following graphs was performed by Dr. Kenneth Rand, professor of Pathology and Medicine at the
University of Florida, College of Medicine.
www.sharklet.com
7
The Sharklet Surface Inhibits Bacterial Attachment and Survival
Studies have been focused on demonstrating the effect of the Sharklet surface to inhibit bacterial attachment and
survival compared to an un-textured control surface. These properties are particularly significant for use of the
Sharklet pattern on high-touch environmental surfaces, where cross- contamination can readily occur. For example, if
a high-touch surface is contaminated by an unsterile gloved hand, bacteria will readily attach to the surface and stay
alive on the surface until they are picked up by a receiving surface, such as a piece of clothing or another hand.
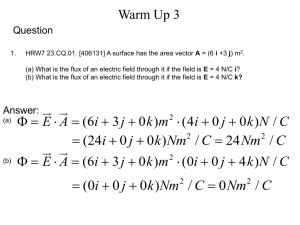
MRSA and MSSA – Smooth vs. Sharklet™
Experiments with Methicillin-resistant Staphylococcus aureus (MRSA) and Methicillin-sensitive Staphylococcus aureus
(MSSA) show significantly less attachment and survival of MRSA and MSSA on the Sharklet surface compared to a
smooth control surface after exposure to a highly concentrated suspension of the bacteria. See the table below.
*Indicates p-values of all experiments were less than 0.05.
When survival testing was extended out to 24 hours, the trends for reduced S. aureus attachment and
survival continued to hold (see figure below). Sharklet patterned and un-patterned acrylic samples were
inoculated and exposed to an aerobic environment for zero, one, three, and 24 hours of drying time. The
Sharklet samples maintained 80-99% fewer cells than the un-patterned controls. *Counts from the second
24 hour MRSA experiment were too few to count and were not included in this analysis.
www.sharklet.com
8
Pseudomonas aeruginosa – Smooth vs. Sharklet
Sharklet reduces Pseudomonas aeruginosa by 100 percent versus a smooth surface after one hour of exposure
simulating typical room conditions. Laboratory test performed on Sharklet on silicone elastomer.
Vancomycin-resistant Enterococcus faecalis – Smooth vs. Sharklet
Sharklet reduces Vancomycin-resistant Enterococcus faecalis by 99 percent versus a smooth surface of after one hour
of exposure simulating typical room conditions. Laboratory test performed on Sharklet on silicone elastomer.
These charts provide a graphical representation of Sharklet Surface Protection Product effectiveness against a variety
of bacteria in environments that are reflective of ambient conditions in a healthcare environment.
The Next Generation in Surfaces
While disinfectant solutions and regularly-implemented cleaning protocols are important in high-risk environments
such as healthcare facilities, food-preparation facilities, and public high-touch areas, surface protection between
cleanings is equally important. The Sharklet surface offers the capability to reduce bacterial burden on surfaces via
reduced bacterial attachment and survival, thereby reducing the amount of bacteria able to be transferred from the
surface to the next person coming in contact with the surface.
These outcomes provide an overall effect on bacterial cross-contamination: less bacteria attach to a Sharklet surface
compared to a smooth un-patterned surface, which results in fewer surviving bacteria over time; which results in
lesser amounts of bacteria present that can then be transferred to another contacting surface.
www.sharklet.com
9
This compound, sequential effect offers multiple levels of safeguards for the surface and the people coming into
contact with contaminated surfaces. The Sharklet surface thus offers a continuous safeguard for surfaces and people
in a manner that does not expose users to toxic chemical agents and does not actively promote antimicrobial
resistance.
Contact Sharklet Technologies, Inc.
For more information, contact:
Sharklet Technologies, Inc.
12635 E. Montview Blvd., Suite 160
Aurora, Colorado 80045
720-859-4070
Safe Touch Solutions Inc.
996 120th Street
Berwick, Illinois 61417
Tel: (309) 426.2600
www.safetouchsolutions.net
www.sharklet.com
10
References
1.
Klevens RM, “Estimating health care-associated infections and deaths in U.S. hospitals, 2002” Public Health Reports 22: 160
(2007)
2.
Carling PC, Parry MF, and Von Beheren SM, “Identifying Opportunities to Enhance Environmental Cleaning in 23 Acute Care
Hospitals“ Infect Control Hosp Epidemiol 29: 1-7 (2008)
3.
Carling PC and Bartley JM, “Evaluating hygienic cleaning in health care settings: What you do not know can harm your
patients“ Am J Infect Control 38: 5 (2010a)
4.
Sattar SA, “Promises and pitfalls of recent advances in chemical means of preventing the spread of nosocomial infections by
environmental surfaces“ Am J Infect Control 38: S34-40 (2010)
Weber DJ, Rutala WA, Miller MB, et al., “Role of hospital surfaces in the transmission of emerging health care-associated
pathogens: Norovirus, Clostridium difficile, and Acinetobacter species“ Am J Infect Control 38: S25-33 (2010)
5.
6.
Siegel JD, Rhinehart E, Jackson M, et al., “2007 guideline for isolation precautions: preventing transmission of infectious
agents in health care settings“ Am J Infect Control 35: S65-164 (2007)
7.
Huang R, Mehta S, Weed D, et al., “Methicillin-resistant Staphylococcus aureus survival on hospital fomites“ Infect Control
Hosp Epidemiol 27: 1267-1269 (2006)
8.
Kramer A, Schwebke I, and Kampf G, “How long do nosocomial pathogens persist on inanimate surfaces? A systematic
review“ BMC Infect Dis 6: 130 (2006)
9.
Boyce JM, “Environmental contamination makes an important contribution to hospital infection“ J Hosp Infect 65(S2): 50–54
(2007)
10. Dancer SJ, “The role of environmental cleaning in the control of hospital-acquired infection” J Hosp Infect 72: 378-385 (2009)
11. Carling PC, Briggs J, Hylander D, et al., “An evaluation of patient area cleaning in 3 hospitals using a novel targeting
methodology” Am J Infect Control 34: 513-519 (2006)
12. White LF, Dancer SJ, Robertson C, et al., “Are hygiene standards useful in assessing infection risk?“ Am J Infect Control 36:
381-4 (2008)
13. Carling PC, Parry MF, Bruno-Murtha LA, et al., “Improving environmental hygiene in 27 intensive care units to decrease
multidrug-resistant bacterial transmission“ Crit Care Med 38: 4 (2010b)
14. Bhalla A, Pultz NJ, Gries DM, et al., “Acquisition of nosocomial pathogens on hands after contact with environmental surfaces
near hospitalized patients” Infect Control Hosp Epidemiol 29: 149-154 (2008)
15. Hayden MK, Blom DW, Lyle EA, et al., “Risk of hand or glove contamination after contact with patients colonized with
vancomycin-resistant Enterococcus or the colonized patients’ environment” Infect Control Hosp Epidemiol 29: 149-154 (2008)
16. Morgan DJ, Liang SY, Smith CL, et al., “Frequent multi-drug resistant Acinetobacter baumannii contamination of gloves, gowns,
and hands of healthcare workers” Infect Control Hosp Epidemiol 31(7): 716-721 (2010)
17. Denton M, Wilcox MH, Parnell P, et al., “Role of environmental cleaning in controlling an outbreak of Acinetobacter baumannii
on a neurosurgical intensive care unit” J Hosp Infect 56: 106-110 (2004)
18. Hayden MK, Bonten MJM, Blom DW, et al., “Reduction in Acquisition of Vancomycin-Resistant Enterococcus after
Enforcement of Routine Environmental Cleaning Measures“ Clin Infect Dis 42: 1552–60 (2006)
www.sharklet.com
11
19. Huang SS, Datta R, and Platt R, “Risk of Acquiring Antibiotic-Resistant Bacteria From Prior Room Occupants“ Arch Intern Med
166: 1945-1951 (2006)
20. Hardy KJ, Oppenheim BA, Gossain S, et al., “A study of the relationship between environmental contamination with
methicillin-resistant Staphylococcus aureus (MRSA) and patients’ acquisition of MRSA” Infect Control Hosp Epidemiol 27: 127132 (2006)
21. Shaugnessy M, Micielli R, Depestel D, et al., “Evaluation of hospital room assignment and acquisition of Clostridium difficile
associated diarrhea” Abstract K-4194. Presented at 48th Annual ICAAC/IDSA 46th Annual Meeting. Washington, DC. October
2008.
22. Drees M, Snydman DR, Schmid CH, et al., “Antibiotic exposure and room contamination among patients colonized with
vancomycin-resistant Enterococci” Infect Control Hosp Epidemiol 29: 709-715 (2008)
23. Page K, Wilson M, and Parkin IP, “Antimicrobial surfaces and their potential in reducing the role of the inanimate environment
in the incidence of hospital-acquired infections“ J Mater Chem 19: 3819–3831 (2009)
24. Schmidt JA, von Recum AF, “Texturing of polymer surfaces at the cellular level” Biomaterials 12(4): 385 (1991)
25. den Braber 1998, de Ruijter JE, Ginsel LA, von Recum AF, Jansen JA, “Orientation of ECM protein deposition, fibroblast
cytoskeleton, and attachment complex components on silicone microgrooved surfaces” J Biomed Mater Res 40(2): 291 (1998)
26. van Kooten TG, von Recum AF, “Cell adhesion to textured silicone surfaces: the influence of time of adhesion and texture on
focal contact and fibronectin fibril formation” Tissue Eng 5: 223 (1999)
27. Carman ML, Estes TG, Feinberg AW, Schumacher JF, Wilkerson W, Wilson LH, Callow ME, Callow JA, Brennan AB, “Engineered
antifouling microtopographies – correlating wettability with cell attachment” Biofouling 22(1): 11 (2006)
28. Schumacher JF, Long CJ, Callow ME, Finlay JA, Callow JA, Brennan AB, “Engineered nanoforce gradients for inhibition of
settlement (attachment) of swimming algal spores” Langmuir 24(9): 4931 (2008)
www.sharklet.com