Urinary Stone Disease

URINARY STONE DISEASE
Dr. Jerry Santos
Li, Kingbherly
Lichauco, Rafael
Lim, Imee Loren
Lim, Jason Morven
Lim, John Harold
Lim, Mary
Lim Phoebe Ruth
ETIOLOGY
Polycrystalline aggregates composed of varying amounts of crystalloid and organic matrix
Stone formation requires supersaturated urine
Urinary pH, ionic strength, solute concentration, complexation
Urinary constituents change dramatically during different physiologic states
ROLE OF SOLUTE CONCENTRATION
Greater concentration of 2 ions
The more likely they are to precipitate
Solubility product (K sp
) = as ion concentrations increase, their activity product reaches a specific point
Formation product (K
K sp fp
) = concentration above capable of initiating crystal growth and heterogeneous nucleation
NUCLEATION THEORY
Urinary stones originate from crystals or foreign bodies immersed in supersaturated urine
CRYSTAL INHIBITOR THEORY
• Calculi form owing to absence or low concentration of natural stone inhibitors
– Magnesium, citrate, pyrophosphate, trace metals
A. CRYSTAL COMPONENT
Stones are primarily composed of crystalline component
Crystal formation
Nucleation, growth, aggregation
Theory of mass precipitation
Distal tubules or collecting ducts becomes plugged with crystals, establishing an environment of stasis, for further stone growth
Tubules enlarge as they entire papilla, transit time is only a few minutes
Fixed particle theory
Formed crystals retained within cells or beneath tubular epithelium
B. MATRIX COMPONENT
Noncrystalline matrix component 2-10% by weight
Mainly protein with hexose and hexosamine
Matrix Calculus
assoc with previous kidney surgery or chronic UTI
Gelatinous texture
May serve as a nidus for crystal aggratation
URINARY IONS
Calcium
Major ion present in urinary crystals
95% calcium filtered at glomerulus is reabsorbed at proximal and distal tubules
<2% excreted in urine
Diuretics – hypocalciuric effect, decrease calcium excretion
Oxalate
Normal waste product of metabolism, relatively insoluble
Enters large bowel, consumed by bacterial decomposition
Excreted by proximal tubule
Supersaturation of calcium oxalate
Hyperoxaluria – bowel disorders
URINARY IONS
Phosphate
Important buffer, complexes with calcium in urine
Filtered cy glomerulus, reabsorbed in proximal tubules
Parathyroid hormone inhibits reabsorption
Uric Acid
By-product of purine metabolism
Any defect in purine metabolism = urinary stone disease
Defect in xanthine oxidase
Xanthine may ppt in urine
URINARY IONS
Sodium
Important role in regulating crystallization of calcium salts in urine
High dietary calcium – increases urinary calcium excretion
Reduces ability of urine to inhibit calcium oxalate crystal agglomeration
Citrate
Pivotal role in citric acid cycle in renal cells
Estrogen increases citrate excretion , factor that decreases incidence of stones in women
Alkalosis increases citrate excretion
URINARY IONS
Magnesium
Lack of magnesium is associated with increased calcium oxalate stone formation
Sulfate
Prevent urinary calculi
Complex with calcium
STONE VARIETIES
STONE VARIETIES
Calcium Calculi
Absorptive hypercalciuric nephrolithiasis
Resorptive hypercalciuric nephrolithiasis
Renal induced hypercalciuric nephrolithiasis
Hyperuricosuric Ca nephrolithiasis
Hyperoxaluric Ca nephrolithiasis
Hypocitraturic Ca nephrolithiasis
Non-Calcium Calculi
Struvite or Magnesium
Ammonium Phosphate
Uric Acid
Cystine
Xanthine
Indinavir
Rare
Silicate
Triamterene
CALCIUM CALCULI
•
–
–
–
–
Calcifications accumulate in collecting system
Nephrolithiasis
(calcareous) elevated urinary calcium elevated urinary uric acid elevated urinary oxalate decreased level urinary citrate
•
•
–
–
–
–
Symptoms secondary to obstruction:
Pain
Infection
Nausea
Vomiting
Asymptomatic hematuria or UTI urinary stone
ABSORPTIVE HYPERCALCIURIC NEPHROLITHIASIS
Increased calcium absorption from jejunum
Increased calcium filtered from the glomerulus
Suppression of PTH
Decreased tubular reabsorption of calcium
Hypercalciuria
ABSORPTIVE HYPERCALCIURIC NEPHROLITHIASIS
Type I
Type II
Type III
• Most severe type
• Independent of diet
• Elevated urinary calcium level
• Tx: cellulose phosphate, hydrochlorothiazide
• Dietary dependent, Most Common
• Tx: no specific
• returns to normal on calcium restricted diet
• “Phosphate renal leak”
• Decreased serum phosphate increase
1,25 dihydroxyvitamin D synthesis
• Tx: orthophosphate (inhibit Vit. D synthesis)
RESORPTIVE HYPERCALCIURIC NEPHROLITHIASIS
typically found in hyperparathyroidism calcium is released from bone in response to the increased activity of osteoclasts caused by excessive and inappropriate serum PTH levels
causes significant hypercalcemia
PTH causes the kidney to limit calcium excretion, but, with the overwhelming serum calcium load produced with hyperparathyroidism, the kidneys are forced to excrete the extra calcium into the urine, causing the hypercalciuria.
RENAL INDUCED HYPERCALCIURIC
NEPHROLOTHIASIS
• Increased tubular defect in calcium excretion
• Decrease serum calcium
•Increase PTH level
•Increase level of calcium back to kidney,
•renal tubules excrete large amounts of calcium
•elevated fasting urinary calcium level,
•normal serum calcium level, elevated PTH level
HYPERURICOSURIC CALCIUM NEPHROLITHIASIS
Excessive purine
Increased uric acid production
Increased urinary monosodium urates
Management:
Diet modification
DOC: allopurinol 300mg/day
Potassium citrate
HYPEROXALURIC CALCIUM NEPHROLITHIASIS
Increased oxalate levels
Severe dehydration
Malabsorption: increase intraluminal fat and bile
Intraluminal calcium binds to fat SAPONIFICATION
Tx: calcium supplementation
HYPOCITRATURIC CALCIUM NEPHROLITHIASIS
Increased metabolic demands of mitochondria of renal cells
Decrease excretion of citrate
Tx: potassium citrate supplementation
ACTIONS:
Citrate complexes with calcium decreasing ionic calcium concentration decrease energy crystallization
Intracellular metabolic acidosis
Hypokalemia
Fasting
Hypomagnesemia
Androgens and gluconeogenesis
UTI
NONCALCIUM CALCULI
STRUVITE
Composed of
Magnesium,
Ammonium, &
Phosphate (MAP)
Most common in women
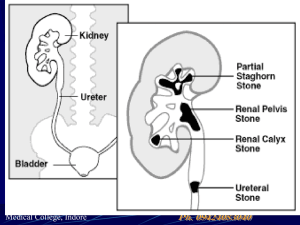
Frequently present as renal staghorn calculi
Struvite stones are associated with ureasplitting organisms
Proteus
Pseudomonas
Providencia
Klebsiella
Staphylococci
Mycoplasma
Alkaline Urinary pH
Results from the high ammonium concentration derived from the urea-splitting organisms
pH >7.2 (NV: 5.85)
MAP crystals precipitate
MAP crystals are soluble in the normal urinary pH range
(5-7)
Foreign bodies and neurogenic bladders may predispose patients to urinary infections and subsequent struvite stone formation
Stone removal is therapeutic
Long term management
Optimized with removal of foreign bodies
All stone fragments should be removed with or w/o the aid of follow-up irrigations
Acetohydroxemic acid
Inhibits the action of bacterial urease, thereby reducing the urinary pH and decreasing the likelihood of precipitations
URIC ACID
<5% of all urinary calculi
Usually found in men
High incidence of Uric Acid Lithiasis
Gout
Myeloproliferative disease
Rapid weight loss
Those treated for malignant conditions with cytotoxic drugs
Treatment
Centered on:
Maintaining a urine volume of >2L / dayand a urinary pH of 6
Reducing dietary purines or the administration of allopurinol helps reduce uric acid excretion
Alkalinization
with oral sodium bicarbonate, potassium citrate, or IV
1/6 normal sodium lactate
May dissolve calculi and is dependent on the stone surface area
CYSTINE
Secondary to an inborn error of metabolism resulting in abnormal intestinal mucosal absorption and renal tubular absorption of dibasic amino acids
Cystine
Ornithine
Lysine
Arginine
Genetic defects of cystinuria has been mapped to chromosome 2p.16 and 19q13.1
Cystine lithiasis
Only clinical manifestation of this defect
1-2% of all urinary stones
Suspected in patients with a (+) FH of urinary stones and the radiographic appearance of a faintly opaque, ground-glass, smooth-edged stone
Urinalysis: hexagonal crystals
◦
◦
◦
◦
Medical Therapy
High fluid intake (>3L/day)
Urinary alkalinization
Penicillamine
Reduce urinary cystine levels
Poorly tolerated by some patients (skin rashes, loss of taste, nausea, vomiting, & anorexia)
Mercaptopropionylglycine
Forms soluble complex with cystine and can reduce stone formation
◦
Surgical
Most stones are recalcitrant to ESWL
XANTHINE
Secondary to a congenital deficiency of xanthine oxidase
Catalyzes the oxidation of hypoxanthine to xanthine and of xanthine to uric acid
Urinary stones develop on 25% of patients with xanthine oxidase deficiency
Stones are radiolucent and are tannish yellow in color
Treatment
Directed by symptoms and evidence of renal obstruction
High fluid intake
Urinary Alkalinization
Stone recurrence
Trial of Allopurinol
Purine-restricted diet
INDINAVIR
Protease inhibitors are a popular and effective treatment in patients with AIDS
◦
◦
Indinavir
6% of patients prescribed had radiolucent stones
Indinavir calculi > only urinary stones to be radiolucent on non-contrast CT scans
Associated with calcium components
Stones are tannish red
Temporary cessation of the medication with intravenous hydration frequently allows thes stones to pass
RARE
Silicate
Associated with long term use of antacids containing silica
Surgical treatment
Triamterene
Associated with anti-hypertensive medications containing triamterene (Dyazide)
Discontinuing the medication eliminates stone recurrence
Glafenine
Antrafenine
PAIN
Colicky
Noncolicky
Usually acute in onset, relatively constant, unexpected and severe
Urinary obstruction due to a direct increase in intraluminal pressure
stretching nerve endings inflammation, edema, hyperperistalsis, and mucosal irritation
Affected by:
Stone size
Location
Degree of obstruction
Variation of individual anatomy
Patients frequently move constantly into unusual positions in contrast to the lack of movement of someone with peritoneal signs
1.
•
•
•
•
•
Renal calyx— deep, dull ache in the flank or back
Mild to severe
Frequently small may be exacerbated after consumption of large amounts of fluid the presence of infection or inflammation in the calyx or diverticulum may contribute to pain perception.
occasionally result in spontaneous perforation with urinoma, fistula, or abscess formation
2.
Renal pelvis
>1 cm in diameter - obstruct the ureteropelvic junction causing severe pain in the costovertebral angle, just lateral to the sacrospinalis muscle and just below the 12th rib dull to excruciatingly sharp, constant, boring
Radiates along the course of the ureter and into the testicle
Partial or complete staghorn calculi- are not necessarily obstructive, few symptoms, “silent” can often lead to significant morbidity, including renal deterioration, infectious complications, or both
3.
Upper and midureter severe, sharp back (costovertebral angle) or flank pain progressing down the ureter – more severe and intermittent
lodged at a particular site - less pain, especially if it is only partially obstructive
Upper ureteral - lumbar region and flank
•
Midureteral - radiates caudally and anteriorly toward the mid and lower abdomen in a curved, band-like fashion (initially parallels the lower costal margin but deviates caudal toward the bony pelvis and inguinal ligament)
4.
Distal ureter pain that radiates to the groin or testicle in males and the labia majora in females
(ilioinguinal or genital branch of the genitofemoral nerves)
This pain pattern is likely due to the similar innervation of the intramural ureter and bladder
Bladder – urgency and frequency with burning
(inflammation of the bladder wall around the ureteral orifice)
HEMATURIA
complete urinalysis : hematuria and crystalluria and documenting urinary pH
intermittent gross hematuria or occasional teacolored urine (old blood)
Rarely (in 10–15% of cases), complete ureteral obstruction presents without microhematuria.
INFECTION
Magnesium ammonium phosphate (struvite) stones = infection stones
Proteus, Pseudomonas, Providencia, Klebsiella, and Staphylococcus infections
Calcium phosphate stones
urine pH <6.6 - brushite stones urinary pH >6.6 - infectious apatite stones
All stones, however, may be associated with infections secondary to obstruction and stasis proximal to the offending calculus.
Infection pain
Uropathogenic bacterial exotoxins and endotoxins may alter ureteral peristalsis
Local inflammation chemoreceptor activation and perception of local pain
1.
Pyonephrosis—gross pus in an obstructed collecting system extreme form of infected hydronephrosis
Presentation: may range from asymptomatic bacteriuria to florid urosepsis
Renal urine aspiration - definitive diagnosis untreated renocutaneous fistula
EVALUATION
Differential Diagnosis
mimic other retroperitoneal and peritoneal pathologic states
Peritoneal signs should be sought during physical examination
History
onset, character, potential radiation, activities that exacerbate or ease the pain, associated nausea and vomiting or gross hematuria, and a history of similar pain
RISK FACTORS
1.
Crystalluria
The rate of stone formation is proportional to the percentage of large crystals and crystal aggregates.
Crystal production is determined by the saturation of each salt and the urinary concentration of inhibitors and promoters.
Urine samples – fresh, centrifuged and examined immediately
2. Socioeconomic factors
affluent, industrialized countries
3. Diet
less energy-dense diet may decrease the incidence of stones
Vegetarians may have a decreased incidence of urinary stones.
High sodium intake is associated with increased urinary sodium, calcium, and pH, and a decreased excretion of citrate;
Fluid intake and urine output
4. Occupation
Physicians and other white- collar workers have an increased incidence of stones compared with manual laborers.
may be related to differences in diet and physical activity; high temperatures may develop higher concentrations of solutes
5. Climate
—hot climates are prone to dehydration
Increased calcium and oxalate excretion has been correlated with increased exposure time to sunlight
6. Family history
Those with a family history of stones have an increased incidence of multiple and early recurrences
7. Medications
antihypertensive medication triamterene
Long-term use of antacids containing silica
Carbonic anhydrase inhibitors
Protease inhibitors in immunocompromised patients are associated with radiolucent calculi.
PHYSICAL EXAM
acute renal colic
Systemic components: tachycardia, sweating, and nausea
Costovertebral angle tenderness abdominal mass may be palpable in patients with longstanding obstructive urinary calculi and severe hydronephrosis
Fever, hypotension, and cutaneous vasodilation: urosepsis thorough abdominal examination should exclude other causes of abdominal pain
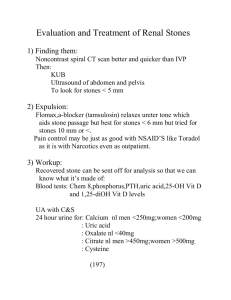
RADIOLOGIC INVESTIGATIONS
Computed tomography
imaging modality of choice in patients presenting with acute renal colic rapid and is less expensive than IVP
It images other peritoneal and retroperitoneal structures and helps when the diagnosis is uncertain
There is no need for intravenous contrast. do not give anatomic details as seen on an IVP
Uric acid stones are visualized no differently from calcium oxalate stones. Matrix calculi have adequate amounts of calcium to be visualized easily by CT.
Intravenous Pyelogram
IV injection of contrast to
visualize renal collecting systems, ureters and UB gives a comprehensive view of the patient's anatomy
50 ml of a special dye is injected into the bloodstream that is excreted by the kidneys and by its density helps outline any stone on a repeated Xray
X ray images every few minutes to determine if there is any obstruction to the dye as it is excreted into the bladder
Tomography
useful to identify calculi in the kidney when oblique views are not helpful.
visualizes the kidney in a coronal plane
identify poorly opacified calculi, especially when interfering abdominal gas or morbid obesity make
KUB films suboptimal
KUB films and directed ultrasonography
Plain frontal supine radiograph of the abdomen
Visualization of:
Renal shadows
Psoas muscle shadow
Calcification (stones, vascular, lymph node or tumor
UB shadow
Calcium radiopaque
About 10% of stones do not have enough calcium to be seen on standard X-rays (radiolucent stones)
The distal ureter is easily visualized through the acoustic window of a full bladder. Edema and small calculi missed on an IVP can be appreciated with such studies.
Ultrasound
presence of hydronephrosis (swelling of the kidney—suggesting the stone is blocking the outflow of urine)
detect stones during pregnancy when x-rays or CT are discouraged
Retrograde pyelography
required to delineate upper-tract anatomy and localize small or radiolucent offending calculi.
Visualization of urinary collecting system achieved via cystoscope, ureteral catherization and retrograde injection of contrast
Used when IVU failed to opcacify renal collecting system and ureters
Nuclear scintigraphy
radioisotopes (here called radiopharmaceuticals) are taken internally, and the emitted radiation is captured by external detectors (gamma cameras) to form two-dimensional images
Bisphosphonate markers can identify even small calculi that are difficult to appreciate on a conventional KUB film
INTERVENTION
INTERVENTIONS
Conservative observation
Dissolution agents
Relief of Obstruction
Extracorporeal Shockwave Lithotripsy (ESWL)
Ureteroscopic stone extraction
Percutaneous Nephrolithotomy
Open stone surgery
Pyelolithotomy
Anatrophic Nephrolithotomy
Radial Nephrotomy
Ureterolithotomy others
Conservative management
Majority of stones pass out within a 6 week period after the onset of symptoms depends on the size of the calculi and its location
Dissolution agents
Use alkalinizing agents
Given oral, IV or intrarenal
Relief of the Obstruction
Emergent drainage in patient with signs of UTI
Extracorporeal Shockwave Lithotripsy (ESWL)
Extracorporeal Shockwave Lithotripsy (ESWL)
CONSIDERATION
excessive weight (>300 lb) may severely limit or preclude ESWL.
Pregnant women and patients with large abdominal aortic aneurysms or uncorrectable bleeding disorders should not be treated with ESWL.
Individuals with cardiac pacemakers should be thoroughly evaluated by a cardiologist.
URETEROSCOPIC STONE EXTRACTION
Highly effective for lower ureteral calculi
Stone may be extracted using a wire basket
Or lithotrites may be placed through the ureteroscope to fragment the calculi
PERCUTANEOUS NEPHROLITHOTOMY
the treatment of choice for large (>2.5 cm) calculi; renal and proximal ureteral calculi, those resistant to ESWL, select lower pole calyceal stones with a narrow, long infundibulum and an acute infundibulopelvic angle, and instances with evidence of obstruction
Rapid cure
OPEN STONE SURGERY
Classic way to remove calculi
Mandatory to obtain a radiograph before the incision is made
Not frequently used anymore because of the morbidity of the incision, the possibility of retained stone fragments, and the ease and success of less invasive techniques
PYELOLITHOTOMY
Effective especially with extrarenal pelvis
Transverse pyelotomy - effective and does not require interruption of the renal arterial blood supply
Flexible endoscope – ensures stonefree status
Coagulum – can retrieve multiple, small renal pelvic calculi and difficultto-access caliceal calculi
Cryoprecipitate
Injected into the renal pelvis, endogenous clotting factors result in a
Jelly-like coagulum of the collecting system.
Small stones are entrapped and removed with the coagu- lum.
ANATROPHIC NEPHROLITHOTOMY
1.
2.
3.
4.
Used with complex staghorn calculi
Complete staghorn calculus
Partial staghorn calculus
Incision made on the convex surface of the kidney posterior to the line of Brodel
Occlusion of the renal artery followed by renal cooling with slushed ice
Nerve hook is helpful to tease out calculi
Repair of narrowed infundibula helps reduce stone recurrence rates.
RADIAL NEPHROTOMY
Allows access to limited calyces of the collecting system
Frequently used in blown-out calyces with thin overlying parenchyma
Intraoperative ultrasound to localize the calyx and the calculi
A shallow incision of the renal capsule can be followed by puncture into the collecting system.
Stones may be cut with heavy Mayo scissors, and remaining fragments can be retrieved.
OTHER RENAL PROCEDURES
Partial nephrectomy – for large stones in a renal pole with marked parenchymal thinnin g
Caution should be taken even with a normal contralateral kidney as stones are frequently associated with a systemic metabolic defect that may recur in the contralateral kidney
Ileal ureter substitution – to decrease pain with frequent stone passage
Autotransplantation with pyelocystostomy – for patients with rare malignant stone disease
Partial nephrectomy
Ileal ureter substitution
URETEROLITHOTOMY
Long standing ureteral calculi
1.
2.
3.
4.
5.
Preoperative radiograph to document stone location
Incision lateral to the sacrospinalis muscles to allow medial retraction of the quadratus lumborum; anterior fascicle of the dorsal lumbar fascia must be incised to gain proper exposure
Vessel loop or Babcock clamp placed proximal to the stone to prevent frustrating stone migration
Longitudinal incision over the stone with a hooked blade to expose the calculus
Nerve hook to tease out the stone
PREVENTION
FLUID INTAKE
About 1.6 L/24 h
Encouraged during mealtime
Increased approximately 2 h after meals
Encouraged to force a nighttime diuresis
METABOLIC INTERVENTION
Stone analysis
Outpatient urine collection during typical activities & fluid intake
Ca stone formers
Initial 24-h urine collection
Include tests for Ca, uric acid, oxalate, citrate,
Na, volume, & pH
Hypercalciuria: most common abnormality
ORAL INTERVENTION
Alkalinizing pH agents
Potassium citrate: oral agent that elevates urinary pH effectively by 0.7–0.8 pH units
Adverse effect: abdominal discomfort
Indications: Ca oxalate calculi 2° to hypocitraturia
(<320 mg/day), including those with renal tubular acidosis; uric acid lithiasis & nonsevere forms of hyperuricosuric Ca nephrolithiasis.
Alternative alkalinizing agents: Na, potassium bicarbonate, orange juice, & lemonade
No effective long-term urinary acidifying agents
ORAL INTERVENTION
Gastrointestinal absorption inhibitor
Cellulose phosphate binds Ca in the gut & inhibits
Ca absorption & urinary excretion
Decreases urinary saturation of Ca phosphate & Ca oxalate
Phosphate supplementation
Indicated for renal PO
4 leak
ORAL INTERVENTION
Diuretics
Thiazides can correct renal Ca leak associated with renal hypercalciuria
Prevents 2° hyperparathyroid state & its associated elevated vitamin D synthesis & intestinal calcium absorption
Hypokalemia hypocitraturia
ORAL INTERVENTION
Calcium supplementation
Indication: Enteric hyperoxaluric Ca nephrolithiasis
Ca gluconate & Ca citrate
Uric acid-lowering medications
Allopurinol
Urease inhibitor
Acetohydroxamic acid: effective adjunctive treatment in chronic urea-splitting urinary tract infections associated with struvite stones
Prophylaxis after removal of struvite stone
ORAL INTERVENTION
Prevention of cystine calculi
Penicillamine: reduces the amount of urinary cystine that is relatively insoluble
Mercaptopropionylglycine (Thiola)
BLADDER STONES
BLADDER STONES
Manifestation of an underlying pathologic condition, including voiding dysfunction or a foreign body
Most seen in men
Developing countries: frequently found in prepubescent boys
Stone analysis: ammonium urate, uric acid, or Ca oxalate stones
Irritative voiding symptoms, intermittent urinary stream, UTI, hematuria, or pelvic pain
PROSTATIC STONES
Prostatic calculi: found within prostate gland per se & are found uncommonly within the prostatic urethra
Represent calcified corpora amylacea & rarely found in boys
Usually of no clinical significance, rarely they are associated with chronic prostatitis
Large prostatic calculi: may be misinterpreted as a carcinoma
Dx: radiograph or transrectal ultrasound
SEMINAL VESICLE STONES
Smooth & hard
Associated with hematospermia
PE: stony hard gland; multiple stones present with crunching sensation
Confused with tuberculosis of the seminal vesicle
URETHRAL STONES
Originate from bladder
Develop 2° to urinary stasis, urethral diverticulum, near urethral strictures, or at sites of previous surgery
Females: rarely develop urethral calculi due to short urethra & lower incidence of bladder calculi; associated with urethral diverticula
Symptoms : intermittent urinary stream, terminal hematuria, & infection
Dx: palpation, endoscopic visualization, or radiographic study
PREPUCIAL STONES
Occur in adults
Develop 2° to a severe obstructive phimosis or poor hygiene with inspissated smegma
Dx confirmed by palpation
Tx: dorsal prepucial slit or formal circumcision