10_2007
advertisement
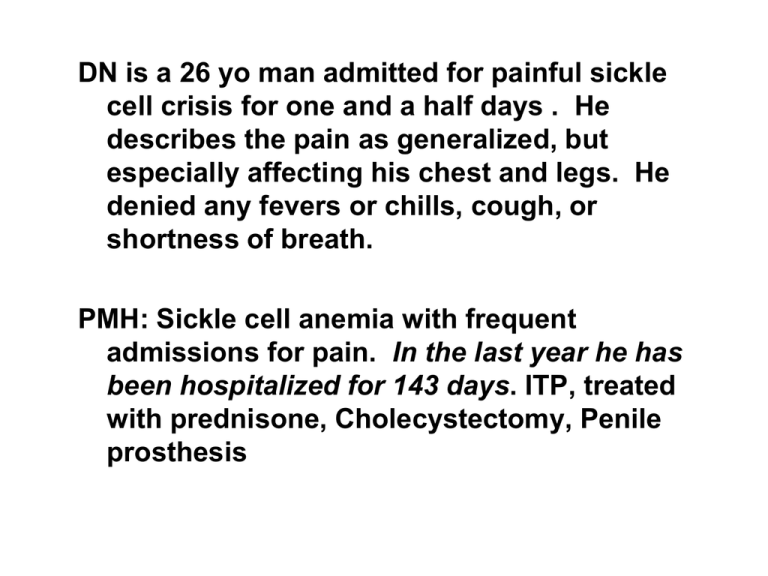
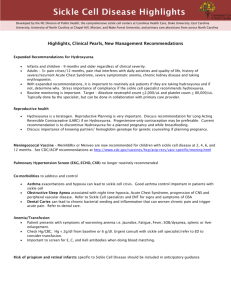
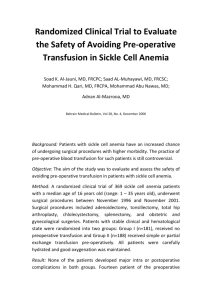
DN is a 26 yo man admitted for painful sickle cell crisis for one and a half days . He describes the pain as generalized, but especially affecting his chest and legs. He denied any fevers or chills, cough, or shortness of breath. PMH: Sickle cell anemia with frequent admissions for pain. In the last year he has been hospitalized for 143 days. ITP, treated with prednisone, Cholecystectomy, Penile prosthesis Meds: prednisone, folate, MS Contin, Dilaudid PE: thin, african-american man in distress VS: P 108 RR 18 BP 145/81 T 98 Lungs: clear Cardiac: reg rhythm, flow murmur Abd: soft, nontender, liver 8 cm Neuro: intact Labs:WBC 46 Hct 22.5 Plt 266 CXR: no effusions or infiltrates He was admitted and treated with morphine, IV hydration, and oxygen. Pain service was contacted and the patient was placed on a PCA pump. His hematocrit decreased to 17 and he received two units of PRBCs. He was slowly weaned from the PCA device and treated with oxycodone. He was discharged after 13 days in the hospital. Sickle Cell Anemia Fall 2007 Bob Richard rrichard@u.washington.edu James B. Herrick American Heart Association James B. Herrick Award For Outstanding Achievement In Clinical Cardiology “Clinical Features of Sudden Obstruction of the Coronary Arteries” published in 1912. (he also described sickle cell disease) Pauling, L and colleagues, Science Vol. 110, 1949 Internal Affections, Hippocrates (460-377 B.C.E.) “Another sickness of the spleen. It comes on mainly in the springtime and is caused by the blood. The spleen becomes engorged with blood, which evacuates into the stomach. Shooting pains in the spleen, the breast, the clavicle, the shoulder, and beneath the shoulder blade. The body’s coloration resembles lead. Sores form on the leg and become large ulcerations. The discharges with the feces are bloody and bluish green. The belly hardens and the spleen is like a stone. This one is more murderous than the one before, and few survive it.” Hemoglobins • Single base pair mutation results in a single amino acid change. • Under low oxygen, Hgb becomes insoluble HbA HbS HbF forming long polymers HbA2 • This leads to membrane changes s (“sickling”) and vaso-occlusion From Connie Noguchi, NIH Deoxygenation of SS erythrocytes leads to intracellular hemoglobin polymerization, loss of deformability and changes in cell morphology. OXY-STATE DEOXY-STATE Deoxyhemoglobin S Polymer Structure A) Deoxyhemoglobin S 14-stranded polymer (electron micrograph) B) Paired strands of deoxyhemoglobin S (crystal structure) C) Hydrophobic pocket for 6b Val D) Charge and size prevent 6b Glu from binding. Dykes, Nature 1978; JMB 1979 Crepeau, PNAS 1981 Wishner, JMB 1975 Schrier, S. ASH Image Bank 2001;2001:100248 Copyright ©2001 American Society of Hematology. Copyright restrictions may apply. An intact RBC with an eccentrically placed hemoglobin C crystal is noted in the center of the image Lazarchick, J. ASH Image Bank 2005;2005:101384 Copyright ©2005 American Society of Hematology. Copyright restrictions may apply. Clinical Consequences of Sickle Disease • • • • • • • • • • • • Vaso-occlusion (pain) Stroke Proliferative retinopathy Acute Chest Syndrome/Pulmonary Hypertension Gallstones Splenic sequestration/infarcts/hyposplenis m Renal insufficiency Avascular necrosis Spontaneous pregnancy loss Priapism Osteonecrosis Non-healing skin ulcer Hemoglobin polymerization is not the whole story • Wide spectrum of disease phenotypes • Some patients have mild disease • 24 yo AA man in the army presents to the infirmary complaining of fatigue. CBC shows a Hgb of 8.5. Retic of 4.5%. Total Bili of 3.0. He is transferred to Walter Reed and sickle cell is diagnosed. • NEJM 2007 Elderly Survivors with Homozygous Sickle Cell Disease (letter) Clinical Variability! • • • • SS vs SC vs Sβ-thal Modifier genes (Epistasis) Hgb F (α2γ2) α – Thal ? • “Polymorphisms near a chromosome 6q QTL area are associated with modulation of fetal hemoglobin levels in sickle cell anemia”. Steinberg lab, Cell Mol Biol 2004 Feb;50(1):23-33. • “Genetic dissection and prognostic modeling of overt stroke in sickle cell anemia”. Steinberg Lab. Nat Genet 2005 Apr;37(4):435-40. Senegal haplotype was associated with higher hemoglobin levels The best HbF response to HU were less likely to have their HbS gene on a Bantu haplotype chromosome Different pathophysiology Two subphenotypes? Vaso-occlusion Hemolysis (NO resistant state) Pain, ACS, AVN Pulm HTN, ulcers priapism, ?stroke HbF, WBC LDH, Bili HU more effective HU less effective Prevalence • Sickle cell anemia affects 0.16% of African-Americans (80,000 and increasing) • 1000 births a year in the US • 120,000 in Africa • Sickle trait is present in 8% • Sickle cell disease includes SS, SC, S-thal • SS makes up 50% of sickle cell disease Cooperative Study of Sickle Cell Disease, NEJM, Vol 330, No 23, 1994 Adult Sickle Cell Mortality Platt, et al, NEJM 1994 • • • • • • • Pain episodes (~1/2 ACS) Unknown Stroke Trauma Perioperative Infection CRF, CHF 22% 18% 7% 6.7% 6.7% 6.2% 15.8% Autopsy study - BJH, 2004 • 306 autopsies from 1929 – 1996 • 56 0 – 2 years old Autopsy study - BJH, 2004 Age 0-2 3-11 12-17 >18 Infection 80.4 60.6 62.1 35.1 Stroke 6.5 9.1 10.3 8.4 Therapy com. 0 0 13.8 9.9 Emboli 0 0 0 9.9 Sequestration 28.3 9.1 3.4 0.5 Chronic Organ Failure 0 3 10.3 13.1 Most deaths occurred outside of the hospital or within 24 hours of admission Mortality Studies Good prognostic markers 1. Female 2. SC 3. Hgb > 7.1 4. HbF elevated 5. WBC < 15.1 Pain in Sickle Cell Disease Natural history study of 3578 patients (Platt et al., NEJM 325:11-16, 1991): Average pain rate: HbSS: 0.8 episode per patient year HbSb0 thalassemia: 1.0 episode per patient year HbSC and HbSb+ thalassemia: 0.4 episodes per year Wide variation: 39% of patients with HbSS had no episodes of pain Only 1% of patients had >6 episodes per year 5% of patients had 33% of episodes Increased pain correlated with: Higher hematocrit (increased viscosity) Low fetal hemoglobin levels (pain rate inversely proportional to [HbF]2 Early death Pain Management BELIEVE THE PATIENT IV Fluids (D5 1/4 NS) Acute Pain Service Patient Care Plan Narcotic analgesics - AVOID meperidine (demerol): Hydromorphone (Dilaudid), MSO4 NSAIDs – Ketorolac et al., Cox 2 inhibitors O2 - for hypoxia Seamless Management of Pain in Adult Patients with Sickle Cell Diseases Donald Rucknagel1,2,3, Annette Lavender1,3, and Zahida Yasin1,3 Cincinnati Comprehensive Sickle Cell Center1, Divisions of Pediatric2 and Medical3 Hematology/Oncology, University of Cincinnati Methodolog y Background The pain of sickle cell diseases may be: 1. Acute Of variable severity. Localized Migratory Generalized Duration may be minutes, hours, days or weeks 2. Chronic We have developed a methodology over a period of years based upon the following observations: 1. Good analgesia requires utilizing equianalgesic principles; 2. If analgesia is not adequate patients will manipulate, thereby creating mistrust and conflict with medial staff; 3. Emergency department visits for moderate pain may occur simply because they lack analgesics at night and have no recourse. Our methodology , summarized in the algorithm, is based upon the following goals: 1. To assist the patient to have as normal a life style as possible; 2. To safely minimize the number of emergency department visits and hospital admissions; 3. To aggressively manage pain in a socially responsible manner. Patients are scheduled in the out-patient clinic at weekly to quarterly intervals, depending upon their needs. They are told never to allow themselves run out of analgesics for moderate pain. They can request prescriptions for small amounts of analgesics that are left at the information desk in the lobby of the University Hospital at their convenience Because of this manner with which we manage pain, we also are mindful of our obligation to administer the program in a socially responsible manner. When the pattern of use increases we first look for inter-current medical complications, such as infection or psychological stress. Integral to the preceding is excellent communication and cooperation with the emergency department. A spreadsheet there appraises them of each patient’s special needs and contains recommendations for initial analgesia, based upon tolerance of each patient evident during prior hospitalizations. Pain The visits to the emergency department appear to have decreased with the implementation of this process, as have the number of hospitalizations. Moderate Mild Out-patient Clinic NSAID and/or acetaminophen /codeine #3 (40 tabs) and/or acetaminophen/oxycodon e (30 tabs) and Patients are told that it may be necessary for us to screen urines or measure blood levels for opioids in order to better manage their pain. Discussion SR- MS (30 tabs) or SR-oxycodone (30tabs) Emergency Department 5-15 mg IV MS+ 30-60 mg (or more) SR-MS Repeat IV MS every 45-60 minutes until comfortable. or 1-3 mg IV hydromorphone + 20-40 mg SRoxycodone (or more) Repeat IV hydromorphone every 45-60 minutes until comfortable Send home or admit Leave prescriptions for patients at the information desk of the University Hospital Home In our experience, “drug seeking behavior” has five causes: 1. Inadequate analgesia; 2. Pain avoidance, due in large measure, to the psychological association of pain with mortality; 3. Self-medication of psychological illness--anxiety or depression--with narcotics; 4. Selling or trading their medications; 5. Psychological dependency. Severe In-patient Admission 30-60 mg (or more) SR-MS every 12 hrs + 5-15 mg IV- MS every 4 hrs prn Increase SR-MS* daily until breakthrough use is minimal or 20-40 mg SR-oxycodone* (or more) every 12 hours + 1-3 mg IV- hydromorphone every 4 hrs prn until breakthrough use is minimal If patient is very ill or has ileus, convert to IV, either bolus or PCA, and later back to SR medication Convert from IV to oral breakthrough using po MS or oxycodone in 12 days Discharge when stable and improving on SR-MS or SRoxycodone Should the pattern of usage and opioid screening establish one of the above diagnoses, appropriate remedies are applied. Those deemed to be psychologically dependent must be evaluated, and if necessary, treated in a dependency treatment program. Written consent must be given to communicate with this program around the issue of compliance. Failure to comply results in restrictions placed on prescribing narcotics outside the hospital, thresholds for admission to the emergency department and to the hospital are increased. EQUIANALGESIC DOSES* MORPHINE MEPERIDINE HYDROMORPHONE SR-MS SR-oxycodone SR = sustained release . IV/IM PO 10 mg 70 2 30 mg 280 10 30 20 Pain Mild Emergency Department Out-patient Clinic NSAID and/or acetaminophen /codeine #3 (40 tabs) and/or acetaminophen/oxycodone and SR- MS (30 tabs) (30 tabs) Moderate 5-15 mg IV MS+ 30-60 mg (or more) SR-MS Repeat IV MS every 45-60 minutes until comfortable. or 1-3 mg IV hydromorphone + 20-40 mg SR-oxycodone (or more) or SR-oxycodone (30tabs) Repeat IV hydromorphone every 45-60 minutes until comfortable Send home or admit Home Severe In-patient Admission 30-60 mg (or more) SR-MS every 12 hrs + 515 mg IV- MS every 4 hrs prn Increase SR-MS* daily until breakthrough use is minimal or 20-40 mg SR-oxycodone* (or more) every 12 hours + 1-3 mg IV- hydromorphone every 4 hrs prn until breakthrough use is minimal If patient is very ill or has ileus, convert to IV, either bolus or PCA, and later back to SR medication Convert from IV to oral breakthrough using po MS or oxycodone in 1-2 days Discharge when stable and improving on SRMS or SR-oxycodone Chest syndrome • New or progressive pulmonary infiltrate in a patient with sickle cell disease. – Admit and treat • At least one of the following additional features is required for the diagnosis: the onset of chest pain, a temperature higher than 38.5°C, tachypnea, wheezing, or cough. Causes and Outcomes of the Acute Chest Syndrome in Sickle Cell Disease NEJM, Volume 342:1855-1865 June 22, 2000 Infarction of the Femoral Head McMahon, L. E.C. et. al. N Engl J Med 1997;337:1293-1301 Phospholipase A2 levels as a means to diagnose Chest syndrome • Styles, LA, et al Blood 2000 • Transfusion prevents acute chest syndrome predicted by elevated secretory phospholipase A2 (BJH 2007) – 9 of the 13 patients who did not receive a transfusion developed ACS during hospitalisation versus none of those who were transfused • Can blocking phospholipase A2 prevent chest syndrome? Can we use CRP instead? Treatments • Supportive care – Hydration, O2, incentive spirometry • • • • Hydroxyurea Transfusion Stem Cell Transplant “New” agents – Clotrimazole (ICA-17043) – Chromatin modifiers (turn on fetal hemoglobin) Sickle Cell Treatment • Pediatric care • Long standing funding of the Comprehensive Sickle Cell Centers • Milestones – PROS I and II – PED HUG – STOP Sickle Cell Treatment - Adults “An Evidence-Based Approach to the Treatment of Adults with Sickle Cell Disease” ASH Education Book 2005 Multicenter Study of Hydroxyurea in Sickle Cell Anemia - Hydroxyurea reduces the frequency of painful episodes, acute chest syndrome, transfusions, hospitalizations Preoperative Transfusion in Sickle Cell Disease - Simple blood transfusion to increase the Hb level to 10 g/dL is as effective as exchange transfusion to reduce Hb S to 30% Prophylactic Transfusion in Pregnancy - Prophylactic blood transfusion to increase the Hb level to 10 g/dL compared to transfusion for Hb < 6 g/dL or for emergent indications did not improve obstetrical or perinatal outcomes but reduced the incidence of painful episodes Captopril for Albuminuria in Sickle Cell Anemia - Captopril reduces albuminuria in normotensive patients (22 patients) Poloxamer 188* for Treatment of Acute Vaso-occlusive Crisis - Poloxamer 188 reduces the duration of acute painful episodes Hydroxyurea can prevent painful episodes • Randomized, double-blinded, placebo controlled trial • Hydroxurea treatment resulted in a 44% reduction in the median annual rate of painful crises • There was also a significant decrease in the frequency of acute chest syndrome and the number of transfusions • HU was stopped for a short time in almost all cases for transient marrow depression NEJM, Vol 332, No 20, 1995 How does hydroxyurea work? Steinberg, MH, NEJM, 340:1021-1030, 1999 Effect of Hydroxyurea on Mortality and Morbidity in Adult Sickle Cell Anemia • JAMA. 2003;289:1645-1651. • 1.5 (5.8) deaths per 3-month period on HU vs 2.6 (7.9) deaths per 3 months for people off HU; (P = .04) • Increased Hgb F correlated with improved survival What effect has HU had on sickle patients? • In clinical trials, 44% decrease in hospitalizations, 40% decrease in mortality. • But a review of records in MD before and after HU approval for sickle, no change in hospitalization rates or costs • Lanzkron et al., Am J Heme, 2006 • Same group at JHU have surveyed care givers and found less than half prescribed HU to all eligible patients Transfusion in Sickle Cell • Used correctly, transfusion can prevent organ damage and save the lives of sickle cell disease patients. • Used unwisely, transfusion therapy can result in serious complications. http://www.nhlbi.nih.gov/health/prof/blood/sickle/index.htm Transfusion in Sickle Cell • Simple transfusion – give blood • Partial exchange transfusion - remove blood and give blood • Erythrocytapheresis – use apheresis to maximize blood exchange • When to use each method? Transfusion in Sickle Cell • In severely anemic patients, simple transfusions should be used. Common causes of acute anemia: • acute splenic sequestration • transient red cell aplasia • Hyperhemolysis (infection, acute chest syndrome, malaria). • If the patient is stable and the reticulocyte count high, transfusions can (and should) be deferred. Transfusion in Sickle Cell • In general, patients should be transfused if there is sufficient physiological derangement to result in heart failure, dyspnea, hypotension, or marked fatigue. • Tends to occur during an acute illness or when hemoglobin falls under 5 g/dL. Transfusion in Sickle Cell (exchange transfusion) • Except in severe anemia, exchange transfusion offers many benefits and is our first choice • Phenotypically matched, leukodepleted packed cells are the blood product of choice. • A posttransfusion hematocrit of 30 to 36 percent or less is recommended. • Avoid hyperviscosity, which is dangerous to sickle cell patients. Transfusion in Sickle Cell (exchange transfusion) Exchange transfusion: 1. Bleed one unit (500 ml), infuse 500 ml of saline 2. Bleed a second unit and infuse two units. 3. Repeat. If the patient has a large blood mass, do it again. Transfusion in Sickle Cell (exchange transfusion) • Transfusions usually fall into two categories: episodic, acute transfusions to stabilize or reverse complications. long-term, prophylactic transfusions to prevent future complications. Transfusion in Sickle Cell (exchange transfusion) • episodic, acute transfusions to stabilize or reverse complications. Limited studies have shown that aggressive transfusion (get Hgb S < 30%) may help in sudden severe illness. May be useful before general anesthesia. Vichinsky et al., NEJM 1995 Transfusion in Sickle Cell (chronic transfusion therapy) – Stroke – Chronic debilitating pain – Pulmonary hypertension – Setting of renal failure and heart failure Transfusion in Sickle Cell (chronic transfusion therapy) Controversial uses: – Prior to contast media exposure – Sub-clinical neurological damage – Priapism – Leg Ulcers – Pregnancy Transfusion in Sickle Cell Inappropriate uses of transfusion: – Chronic steady-state anemia – Uncomplicated pain episodes – Infection – Minor surgery – Uncomplicated pregnancies – Aseptic necrosis Other therapies: Potential treatment with ICA-17043 or ICA-17043 The Process of Vaso-Occlusion in Patients with Sickle Cell Disease Hebbel, R. P. N Engl J Med 2000;342:1910-1912 Other therapies: 5-aza-2'-deoxycytidine •Hypomethylating agent: results in reactivation of fetal hemoglobin Blood, Vol. 102, Issue 12, 3865-3870, December 1, 2003 Survival of sickle cell patients with pulmonary hypertension BMJ. 2003 Nov 15;327(7424):1151-5. Distribution (Panel A) and Frequency Distribution (Panel B) of Tricuspid Regurgitant Jet Velocity in 195 Patients with Sickle Cell Disease and 41 Black Control Subjects and the Association between Right Ventricular Systolic Pressure Measured by Doppler Echocardiography and Pulmonary-Artery Systolic Pressure, Measured during Catheterization (Panel C) Gladwin, M. T. et. al. N Engl J Med 2004;350:886-895 Survival after matched sibling allogeneic transplant for sickle cell BMJ. 2003 Nov 15;327(7424):1151-5. Long-term results of related myeloablative stem-cell transplantation to cure sickle cell disease Bernaudin, F. et al. Blood 2007;110:2749-2756 Copyright ©2007 American Society of Hematology. Copyright restrictions may apply. Protocol 03-DK-0170: Mini-allo stem cell transplant for sickle cell disease Eligibility: Hb SS, SC, or Sb0-thal • Severe end-organ damage – stroke or abnormal CNS vessel – pulmonary hypertension (TRV ≥2.5 m/s) – renal damage • Or modifiable complication, not ameliorated by hydroxyurea – – – – > 2 hospital admissions per year for pain crises previous acute chest syndromes red cell alloimmunization osteonecrosis of multiple joints Transplant conditioning regimen • Campath (alemtuzumab, anti-CD52 monoclonal antibody) total 1 mg/kg • TBI 300 cGy • Sirolimus (rapamycin) targeting trough level of 15 ng/mL • Stem cell infusion • Monitor for blood count recovery Hospital course during and after transplant • Tolerated conditioning (radiation and Campath infusion) without serious adverse events • No significant need for parenteral antibiotics or nutritional support • No sickle cell related events Transplant outcome (%) Donor Months post BMT CD3 (%) Donor CD14/15 (%) Donor RBC Hgb 36 13 53 100 12.9 2 7.56 / (2.27) 15 60 37 100 11.9 3 10 / (3.42) 22 44 98 100 13.3 4 8.3 / (5.35) 10 0 0 0 12.4 5 5.51 / (3.71) 12 23 98 100 12.1 6 23.8 / (2.81) 10 21 98 100 13.2 7 18.8 / (3.32) 8 39 100 100 10.9 8 20.1 / (3.04) 7 26 94 100 11.4 Pt CD34 and CD3 (per kg of recipient wt) 1 5.72 x 10 6 / (3.21 x 108) Gene Therapy? • Many different approaches • Stable transduction of the stem cell with expression in the red cells • Manipulating the expression of the various globin genes may be easier than replacing the sickle b-globin gene • Gene correction strategies are in the early stages Management Summary • New therapy offers patients with sickle cell disease a prolonged life span, with the potential to prevent or minimize complications that impair quality of life • Multi-organ screening can now detect early injury and allow corrective intervention. • Advances in transfusion therapy has resulted in improved safety. • Advances in clinical therapy include prophylactic antibiotics, red cell pheresis, and hydroxyurea. • Bone marrow transplantation has become accepted therapy for severely affected patients, but is only available for a minority of patients. Sickle Cell Disease 2007 • The first molecular disease, yet far from cured • Sickling is more complicated than Hgb polymerization • Understanding the biology of the red cell has led to possible treatment approaches Treatment Guidelines http://www.nhlbi.nih.gov/health/prof/blood/s ickle/sc_mngt.pdf 2002 – tweaked in 2004