fluidskids

A FEW THOUGHTS ABOUT
FLUIDS IN KIDS
William Primack, MD
UNC Kidney Center
Chapel Hill NC USA
August 21, 2006
HOMEOSTASIS
The living organism does not really exist in the milieu exteriour (the atmosphere it breathes, salt or fresh water if that is its element) but in the liquid milieu interior formed by the circulating organic liquid which surrounds and bathes all the tissue elements, this is the lymph or plasma, the liquid part of the blood which in the higher animals is diffused through the tissues and forms the ensemble of the intercellular liquids which is the basis of all local nutrition and the common factor of all elementary exchanges.
The stability of the milieu interior is the primary condition for the freedom and independence of existence, the mechanism which allows of this is that which ensures in the milieu interior the maintenance of all the conditions necessary to the life of the elements.
Claude Bernard
Body spaces
Body spaces by age
Maintenance fluids
• Holliday M and Segar W
– Pediatrics 1957;19:824
• 100 kcal~100ml
• Their data led to the
100:50:20 protocol for the
AVERAGE hospital patient
Maintenance fluids
• Holliday M and Segar W
– Pediatrics 1957;19:824
• 100 kcal~100ml
• Their data led to the
100:50:20 protocol for the
AVERAGE hospital patient
• We never admit any kids like that!!!
MAINTENANCE FLUIDS
What makes up 100 ml/kg
Water
(ml/100 kcal)
Respiratory 40-50
Sweat
Urine
0-5
50-75
Stool water 5-10
‘Hidden intake’
Water of oxidation
Totals
(10-15)
100-125
Respiratory
MAINTENANCE FLUIDS
Abnormal losses
Water
(ml/100 kcal)
40-50
Abnormal losses
Range (ml/kg)
25-200
Sweat 0-5 0-25 urine
Stool water
50-75
5-10
0-300
0-100
‘Hidden intake’
Water of oxidation
Totals
(10-15)
100-125
Maintenance fluids
Adjustments to 100:50:20 rule
• Increase maintenance fluids
– By 12 % for each degree C of fever
– Insensible losses from 45 to 50-60 ml/100cal for hyperventilation
• Decrease maintenance fluids
– Insensible losses from 45 to 0-15 ml/100cal for high humidity (= ventilator)
Maintenance fluids
• Unless you know what you are replacing and why, using maintenance plus (e.g.
1 ½ x maintenance) is illogical
Maintenance fluids
An alternative approach
• Based on body surface area
• Use estimated insensible losses and replace all other fluid losses based on volume and content
• Recalculate as often as needed q6h-q24h
• Probably more accurate for PICU type patients
BODY SURFACE AREA
• BSA (M2) of average proportioned
•Newborn=0.25
•10 kg infant = 0.5
•30 kg child = 1.0
•70 kg adult = 1.73
•If average proportioned 3-30 kg
•BSA=(wt + 4)/30
Respiratory
Sweat urine
Stool water
‘Hidden intake’
Water of oxidation
Totals
MAINTENANCE FLUIDS
Daily water requirement
Water
(ml/100 kcal)
Water looses per M2
BSA
40-50
0-5
50-75
5-10
(10-15)
100-125
400-600
0-50
750
50-100
(150)
1300-1500
Continuing losses
• NO MATTER WHICH SYSTEM YOU USE
• It is essential to regularly reassess child for continuing losses .
• Regularly reevaluate effectiveness of your fluid prescription and modify it p.r.n.
• May need to recheck labs more than q.d.
• Reweigh more than q.d. if appropriate
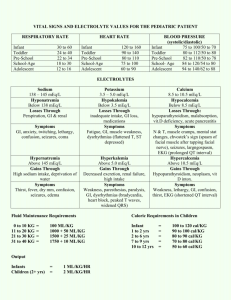
Contents of abnormal losses meq/liter
Fluid gastric
Na K Cl HCO3
20-80 5-20 100-150 0 pancreatic 120-140 5-15 40-80 40-60 small bowel 100-140 5-15 90-130 25-40 bile ileostomy diarrhea
120-140 5-15 80-120 20-40
45-135 3-15 20-115 20-50
10-90 10-80 10-110 5-35
Comparison of Electrolyte Composition of
Diarrhea Caused by Different Organisms
Etiology
Cholera
Rotavirus
ETEC
Electrolytes
(mMol/L)
Na+ K+ Cl HCo
3
88 30 86 32 mOsmols
300
37 38 22 6 300
53 37 24 18 300
Molla et al. J Pediatr 1981; 98: 835
Insensible loss
Sweat
MAINTENANCE FLUIDS
Fluids based on BSA
Water
(ml/100 kcal)
45
Water
(ml/M2)
400-600
0-25 0-200
Na
MEQ/M2
0
20
K
MEQ/M2
0
20 urine 50-75 750 0-200
Stool water 5-10
‘Hidden intake’
Totals
(10-15)
100-125
100
(150)
1300-1500
30
0
50-250
5-100
30
0
55-155
Case 1
• 1 y.o., 10 kg, child develops vomiting for
12 hours and then diarrhea for 24 hours
• On exam decreased turgor, dry mouth, BP
90/60, wt= 9 kg.
• Labs Na=140, K=4, HCO3=17, BUN=30, creatinine=0.4.
• Receives 10-20 ml/kg bolus and makes some urine
Isotonic dehydration
Isotonic dehydration correction water Na K HCO3
25 20 0 maint 1000 deficit
Isotonic dehydration correction water Na K HCO3 maint 1000 deficit 1000 total 2000
25
75
100
20
75
95
0
20
20
½ in first 8 hrs, remainder over 16 hours
Reassess for and replace continuing losses
Case 2
• 1 y.o., 10 kg, child develops vomiting for
12 hours and then diarrhea for 24 hours
• Given ‘clear fluids’.
• On exam decreased turgor, dry mouth, BP
80/50, wt= 9 kg.
• Labs Na=125, K=4, HCO3=15, BUN=40, creatinine=0.4.
• Receives 10-20 ml/kg bolus and makes some urine
Hypotonic dehydration
Hypotonic dehydration correction water Na K HCO3
20 0 maint 1000 deficit 1000
25
75 +
Hypotonic dehydration correction
(Desired Na – measured Na) X TBW
(135 – 125) meq/l X .6 l/kg = 6 meq/kg
Thus deficit= 60 meq Na
Hypotonic dehydration correction water Na K HCO3 maint 1000 deficit 1000
25
75 + 60
20
75
0
30 total 2000 135 95
½ in first 8 hrs, remainder over 16 hours
Reassess for and replace continuing losses
30
Case 3
• 1 y.o., 10 kg, child develops vomiting for
12 hours and then diarrhea for 48 hours
• Continues to drink cow’s milk
• On exam nl to ‘woody’ turgor, moist mouth,
BP 90/50, wt= 9 kg.
• Labs Na=170, K=4, HCO3=18, BUN=25, creatinine=0.4.
• Receives 10-20 ml/kg bolus and makes some urine
Hypertonic dehydration
Hypertonic dehydration correction water Na K HCO3 maint 750 deficit 1000
25 20 0 total
Lower maintenance water requirement as high ADH will decrease UO
Hypertonic dehydration initial day correction water Na K HCO3 maint 750 deficit 1000
25 20
75-65=10 25
0
20 total 1750 35 45
Target is to drop Na by 10 meq/day.
Lower maintenance requirement as high ADH will decrease UO
Reassess for and replace continuing losses
Hypertonic dehydration correction
• Lower maintanence requirment as high
ADH will decease UO
• Goal is to decrese Na by 10 meq/day
(Desired Na – measured Na) X TBW
(165 – 175) meq/l X .6 l/kg = 6 meq/kg
Thus sodium surplus= 60 meq Na
Comparison of Effect of Glucose on Net Stool Rate with
Galactose and Fructose in Perfusions Delivered Uniformly throughout Most of the Small Intestine via Multilumen Tube
600
500
400
300
200
100
Pre-perfusion
Perfusion with electrolytes and 61 mM galactose
Perfusion with electrolytes and 56 mM fructose
Perfusion with electrolytes and 58 mM glucose
Perfusion with electrolytes only
Post-perfusion
1 2 3 4 5 6 7 8 9
12-HOUR PERIODS
Adapted from Hirschhorn N et al. N Engl J Med 1968; 176
Na-glucose co-transport
Intestinal brush border
Duggan C JAMA 2004;291:2628
Outcome of Oral Treatment of 216
Patients with Rotavirus
Initial Treatment
Oral (n = 197)
Success
188 (95)
Intravenous (n = 19) 17 (89)
Total (n = 206) 205 (95)
*Requiring unscheduled treatment intravenously.
Percentages are given in parentheses.
Failure*
9 (5)
2 (11)
11 (5)
Taylor PR et al. Arch Dis Child 1980; 55(5):376-379
ORAL vs IV REHYDRATION IN MODERATE DEHYDRATION
Spandorfer et al.Pediatrics 115 (2):
295. (2005
)
ORS
• 30-50 ml/kg over 3-4 hours of ORS
• If vomiting give in sips (Pedialyte pops)
• May also add 5-10 ml/kg per diarrheal stool for ongoing losses
• Expect increased stool content
• After rehydration, CHO rich foods
• Continue nursing
ORS and other ‘clear liquids’
CHO g/l
Pedialyte 2.5
WHO ORS 2.0
Gatorade 5.9
Na
Meq/l
45
75
21
Apple juice 11.9
0.4
Coca cola 10.9
4.3
OJ 10.4
0.2
26
0.1
49
K
Meq/l
20
20
2.5
--
--
--
Cl
Meq/l
35
65
17 base
Meq/l
30
30
0
-700
13.4
656
50 654 mOsm/ kgH20
250
280
377