Co-occurring addiction and mental disorders
advertisement

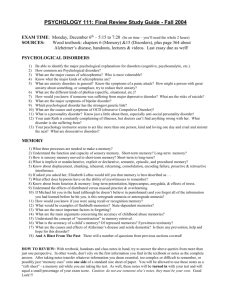
Co-occurring Addiction and Less Severe Mental Disorders Richard Ries MD rries@u.washington.edu Harborview Medical Center University of Washington Seattle, Wa DUAL DIAGNOSIS IS: TWO DIAGNOSES/ DISORDERS TWO SYSTEMS DOUBLE TROUBLE IN THE EYE OF THE BEHOLDER Examples of Dual Disorders: MENTAL DISORDERS Schizophrenia Bi-polar Schizoaffective Major Depression Borderline Personality Post Traumatic Stress Social Phobia others ADDICTION DISORDERS Alcohol Abuse/Depen. Cocaine/ Amphet Opiates Marijuana Polysubstance combinations Prescription drugs Dual Disorders for Everyone? If applied to all cases, Term has no meaning (eg Spider phobia and “Running Addiction”) Both Mental and Addiction Disorders need to be over threshold Personality Disorders, other than Borderline not usually counted Substance Induced Disorders cause diagnostic confusion CHARACTERISTICS OF THE DUAL DIAGNOSIS CLIENT IN KING COUNTY… Ries ‘89 Severity of Chemical Dependency High LH HH 2 Severity of Psychiatric Condition 1 4 Low 3 HL LL Low High Systems Problems Different Different Different Different Different Different Different Laws…commitment/confid. funding..audits etc personnel training certification sites Norms The Four Quadrant Framework for Co-Occurring Disorders A four-quadrant conceptual framework to guide systems integration and resource allocation in treating individuals with cooccurring disorders (NASMHPD,NASADAD, 1998; NY State; Ries, 1993; SAMHSA Report to Congress, 2002) High severity Less severe mental disorder/ more severe substance abuse disorder Less severe mental disorder/ less severe substance abuse disorder Low severity More severe mental disorder/ more severe substance abuse disorder More severe mental disorder/ less severe substance abuse disorder High severity Not intended to be used to classify individuals (SAMHSA, 2002), but . . . DOUBLE TROUBLE Hall Alterman Solomon Safer Drake Barbee Lyons Chen ’77 ’85 ’86 ’87 ’89 ’89 ’89 ’92 Poor out-pt attendance, discontinue Rx More mood changes, intensive staffing More noncompliance, arrests Over twice hosp. rate and criminal behav More hostility, noncompliance More psych symptoms More noncompliance, ER, jail, rehosp. Worse treatment course But what about NON- severely mentally ill co-occurring pts? Like in Addiction Treatment settings Like in Criminal Justice settings Like in Primary Care Settings Like in ER’s, especially with suicidal pts The new TIP will bring more focus on these populations Likelihood of a Suicide Attempt Increased Odds Of Attempting Suicide Risk Factor Cocaine use Major Depression Alcohol use Separation or Divorce NIMH/NIDA 62 times more likely 41 times more likely 8 times more likely 11 times more likely ECA EVALUATION Percent With Severe Suicide Rating Double Trouble: RELATIONSHIP OF ALCOHOL & DRUG PROBLEMS TO SEVERE SUICIDALITY (n=12,196) 60.0% ODDS: 2.00 50.0% ODDS: 1.23 ODDS: 1.18 Mild (n=1022) Moderate (n=2391) 40.0% 30.0% 20.0% 10.0% 0.0% ODDS adjusted for age & gender None (n=4853) Severe (n=3930) ALCOHOL OR DRUG PROBLEMS Walds = 235.41 p < .001 Ries & Russo unpub , 2003 Drug Induced Psychopathology Drug States Withdrawal Acute Protracted Symptom Groups Intoxication Chronic Use Depression Anxiety Psychosis Mania Rounsaville ‘90 Twelve-Month Prevalence of DSM-IV Independent Mood and Anxiety Disorders Among Respondents with DSM-IV Substance Use Disorders Who Sought Treatment in the Past 12 Months Disorder Respondents, % (SE) Those With Any Alcohol Use Disorder (5.81%)* Any mood disorder 40.69 (4.11) Major Depression 32.75 (4.01) Dysthymia 11.01 (2.74) Mania 12.56 (2.81) Hypomania 3.07 (1.37) Any anxiety disorder 33.38 (4.17) Panic disorder With agoraphobia 4.10 (1.54) Without agoraphobia 9.10 (2.48) Social phobia 8.49 (3.48) Specific phobia 17.24 (3.10) Generalized anxiety disorder 12.35 (3.01) Any drug use disorder 33.05 (4.23) *Data in parentheses are the percentages of respondents with the substance use disorders who Grant B, JAMA 2004 sought treatment in the past 12 months. Twelve-Month Prevalence of DSM-IV Independent Mood and Anxiety Disorders Among Respondents with DSM-IV Substance Use Disorders Who Sought Treatment in the Past 12 Months Disorder Respondents, % (SE) Those With Any Drug Use Disorder (13.10%)* Any mood disorder 60.31 (5.86) Major Depression 44.26 (6.28) Dysthymia 25.91 (5.19) Mania 20.39 (5.17) Hypomania 2.48 (1.67) Any anxiety disorder 42.63 (5.97) Panic disorder With agoraphobia 5.92 (2.19) Without agoraphobia 8.64 (3.05) Social phobia 12.09 (3.48) Specific phobia 22.52 (4.99) Generalized anxiety disorder 22.07 (5.18) Any alcohol use disorder 55.16 (6.29) *Data in parentheses are the percentages of respondents with the substance use disorders who sought Grant B, JAMA 2004 treatment in the past 12 months. Comorbidity of Depression and Anxiety Disorders 50% to 65% of panic disorder patients have depression† 70% of social anxiety disorder patients have depression 67% of OCD patients have depression* Panic Disorder HIGHLY Depression COMMON… Social Anxiety HIGHLY Disorder COMORBID OCD 49% of social anxiety disorder patients have panic disorder** 11% of social anxiety disorder patients have OCD** Diagnostic Criteria for Panic Attack A discreet period of intense fear or discomfort in which 4 or more of the following symptoms developed abruptly and reached a peak within 10 minutes: • Palpitations, pounding heart • Sweating • Trembling or shaking Adapted with permission from American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. 1994. Diagnostic Criteria for Panic Attack Continued Dizziness Chills or hot flushes Feelings of unreality Fear of losing control or going crazy Fear of dying Paresthesias Choking feeling Smothering or shortness of breath Chest pain or discomfort Abdominal distress Somatic Symptoms In Panic Disorder Gastrointestinal Symptoms Chest Pain SOMATIC SYMPTOMS Headache Dizziness Fatigue Quality of Life in Panic Disorder Panic Disorder (N = 254) 35 Major Depression (N = 738) Neither PDN or MD (N = 17,113) 30 28 27 25 20 % 16 15 14 12 12 11 10 5 2 2 0 Marital Discord (past 2 weeks) Markowitz et al. Arch Gen Psychiatry. 1989;46:984. Use Of ER (past year) Financial Dependence (welfare or disability) DSM-IV Diagnostic Criteria for PTSD Exposure to a traumatic event in which the person: experienced, witnessed, or was confronted by death or serious injury to self or others AND responded with intense fear, helplessness, or horror American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. 1994. DSM-IV Diagnostic Criteria for PTSD Continued Symptoms appear in 3 symptom clusters: reexperiencing, avoidance/numbing, hyperarousal last for > 1 month cause clinically significant distress or impairment in functioning DSM-IV Diagnostic Criteria for PTSD Re-experiencing Persistent re-experiencing of 1 of the following: recurrent distressing recollections of event recurrent distressing dreams of event acting or feeling event was recurring psychological distress at cues resembling event physiological reactivity to cues resembling event DSM-IV Diagnostic Criteria for PTSD Avoidance/Numbing Avoidance of stimuli and numbing of general responsiveness indicated by 3 of the following: avoid thoughts, feelings, or conversations* avoid activities, places, or people* inability to recall part of trauma interest in activities estrangement from others restricted range of affect sense of foreshortened future DSM-IV Diagnostic Criteria for PTSD Hyperarousal Persistent symptoms of increased arousal 2: difficulty sleeping irritability or outbursts of anger difficulty concentrating hypervigilance exaggerated startle response American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. 1994. Prevalence of Trauma and Probability of PTSD 1 40 Prevalence of Trauma Male Female 30 % 20 10 0 Witness % 1 2 Accident Threat w/ Weapon 70 60 50 40 30 20 10 0 Physical Molestation Combat Attack Rape 2 Probability of PTSD Witness Accident Threat w/ Weapon Physical Molestation Attack Combat Rape Impaired Quality of Life with PTSD 100 PTSD MDD OCD US Population 75 SF-36 50 Score 25 0 Vitality SF-36 = 36 item short form health survey Lower score = more impairment Malik M et al. J Trauma Stress. 1999;12:387-393. Social Function Common Somatic Complaints Of Social Anxiety Disorder Stuttering Palpitations “Butterflies” Beidel. J Clin Psychiatry. 1998;59(suppl 17):27. Blushing Sweating Trembling And Shaking Social Anxiety Disorder SPIN Screener Is being embarrassed or looking stupid among your worst fears? Does fear of embarrassment cause you to avoid doing things or speaking to others? Do you avoid activities in which you are the center of attention? Katzelnick et al. Presented at 37th Annual Meeting of the American College of Neuropsychopharmacology; December 14-18, 1998; Los Croabas, Puerto Rico. Social Anxiety Disorder: Educational and Occupational Impairment 0.0 -5.0 Impairment** (%) -10.0 Wages -15.0 -20.0 College Graduation Professional Or Management Positions * LSAS score in controls = 25; ** Impairment (%) refers to percentage change in wages and percentage point changes in probabilities of college graduation and having a technical, professional, or managerial job. Katzelnick et al. Presented at 37th Annual Meeting of the American College of Neuropsychopharmacology; December 14-18, 1998; Los Croabas, Puerto Rico. Therapy Plan Bio Psych Social Psych Labs Meds (anti-depressants, etc.) psychotherapy education groups process groups Couples conf. D/C planning housing, etc. CD Labs Meds (withdrawal, craving, etc.) Step work Groups AA Meetings Intervention Sober housing 1: JAMA. 2004 Apr 21;291(15):1887-96. Related Articles, Links Treatment of depression in patients with alcohol or other drug dependence: a meta-analysis. Nunes EV, Levin FR. DATA SYNTHESIS: For the HDS score, the pooled effect size from the random-effects model was 0.38 (95% confidence interval, 0.18-0.58). Heterogeneity of effect on HDS across studies was significant (P <.02), and studies with low placebo response showed larger effects. Moderator analysis suggested that diagnostic methods and concurrent psychosocial interventions influenced outcome. Studies with larger depression effect sizes (>0.5) demonstrated favorable effects of medication on measures of quantity of substance use, but rates of sustained abstinence were low. CONCLUSIONS: Antidepressant medication exerts a modest beneficial effect for patients with combined depressive- and substance-use disorders. It is not a stand-alone treatment, and concurrent therapy directly targeting the addiction is also indicated. More research is needed to understand variations in the strength of the effect, but the data suggest that care be exercised in the diagnosis of depression-either by observing depression to persist during at least a brief period of abstinence or through efforts by clinical history to screen out substance-related depressive symptoms. : Psychopharmacol Bull. 1998;34(1):11721. Related Articles, Links Fluoxetine versus placebo in depressed alcoholic cocaine abusers. Cornelius JR, Salloum IM, Thase ME, Haskett RF, Daley DC, Jones-Barlock A, Upsher C, Perel JM. All 51 patients participated in a double-blind, parallel group study of fluoxetine versus placebo in depressed alcoholics. The principal focus of this article is the one-third of the depressed alcoholics who also abused cocaine and how the treatment response of those 17 patients compared with that of the 34 depressed alcoholics who did not abuse cocaine. During the study, no significant difference in treatment outcome was noted between the fluoxetine group (N = 8) and the placebo group (N = 9) for cocaine use, alcohol use, or depressive symptoms. In addition, no significant within-group improvement was noted for any of these outcome variables in either of the two treatment groups. Indeed, across the combined sample of 17 depressed alcoholic cocaine abusers, the mean Beck Depression Inventory (BDI) score worsened slightly from 19 to 21 during the course of the study, and 71 percent of the patients continued to complain of suicidal ideations at the end of the study. The 17 cocaine-abusing depressed alcoholics showed a significantly worse outcome than the 34 non-cocaine abusing depressed alcoholics on the 24-item Hamilton Rating Scale for Depression (HAM-D) and BDI depression scales and on multiple measures of alcohol consumption. These findings suggest that comorbid cocaine abuse acts as a robust predictor of poor outcome for the drinking and the depressive symptoms of depressed alcoholics. Depress Anxiety. 2001;14(4):255-62. Related Articles, Links Paroxetine for social anxiety and alcohol use in dual-diagnosed patients. Randall CL, Johnson MR, Thevos AK, Sonne SC, Thomas SE, Willard SL, Brady KT, Davidson JR. Fifteen individuals meeting DSM-IV criteria for both social anxiety disorder and alcohol use disorder were randomized to treatment. Paroxetine (n = 6) or placebo (n = 9) was given in a double-blind format for 8 weeks using a flexible dosing schedule. Dosing began at 20 mg/d and increased to a target dose of 60 mg/d. There was a significant effect of treatment group on social anxiety symptoms, where patients treated with paroxetine improved more than those treated with placebo on both the Clinical Global Index (CGI) and the Liebowitz Social Anxiety Scale (Ps < or = 0.05). On alcohol use, there was not a significant effect of treatment on quantity/frequency measures of drinking, but there was for the CGI ratings (50% paroxetine patients versus 11% placebo patients were improvers on drinking, P < or = 0.05). This pilot study suggests that paroxetine is an effective treatment for social anxiety disorder in individuals with comorbid alcohol problems, and positive treatment effects can be seen in as little as 8 weeks. Further study is warranted to investigate its utility in helping affected individuals reduce alcohol use. Copyright 2001 Wiley-Liss, Inc. Why aren’t Antidepressants more effective in addictions patients? Psychiatric outcomes: Antidepressants only beat placebo by 20% anyway in NON addicts Study patients also get “addiction rx” Maybe addiction rx is more anti-dep, anti anx than we think…viz Schuckit 80% -> 20% This is poorly studied…maybe better with 12 step Sub Induced criteria are wrong Addictions outcomes Meds take focus off sobriety Meds reinforce sobriety Just don’t work for this Alcohol Clin Exp Res. 2001 Feb;25(2):210-20. Concurrent alcoholism and social anxiety disorder: a first step toward developing effective treatments. Randall CL, Thomas S, Thevos AK. The present study investigated whether simultaneous treatment of social phobia and alcoholism, compared with treatment of alcoholism alone, improved alcohol use and social anxiety for clients with dual diagnoses of social anxiety disorder and alcohol dependence. METHODS: The design was a two-group, randomized clinical trial that used 12 weeks of individual cognitive behavioral therapy for alcoholism only (n = 44) or concurrent treatment for both alcohol and social anxiety problems (n = 49). Outcome data were collected at the end of 12 weeks of treatment and at 3 months after the end of treatment. RESULTS: Results with intent-to-treat analyses showed that both groups improved on alcohol-related outcomes and social anxiety after treatment. Counter to the hypothesis, the group treated for both alcohol and social anxiety problems had worse outcomes on three of the four alcohol use indices. No treatment group effects were observed on social anxiety indices. CONCLUSIONS: Implications for the staging of treatments for coexisting social phobia and alcoholism are discussed, as well as ways that modality of treatments might impact outcomes. J Subst Abuse Treat. 2003 Sep;25(2):99-105. Related Articles, Links A cognitive-behavioral treatment for incarcerated women with substance abuse disorder and posttraumatic stress disorder: findings from a pilot study. Zlotnick C, Najavits LM, Rohsenow DJ, Johnson DM. This preliminary study evaluates the initial efficacy of a cognitive-behavioral treatment, Seeking Safety, as an adjunct to treatment-as-usual in an uncontrolled pilot study of incarcerated women with current SUD and comorbid PTSD. Of the 17 incarcerated women with PTSD and SUD who received Seeking Safety treatment and had outcome data, results show that nine (53%) no longer met criteria for PTSD at the end of treatment; at a followup 3 months later, seven (46%) still no longer met criteria for PTSD Additionally, there was a significant decrease in PTSD symptoms from intake to posttreatment, which was maintained at the 3-month followup assessment. Based on results from a diagnostic interview and results of urinalyses, six (35%) of the women reported the use of illegal substances within 3 months from release from prison. Measures of client satisfaction with treatment were high. Recidivism rate (return to prison) was 33% at a 3-month followup. Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study n=1774, 1 year follow-up Outpt Visits Humphreys et al ..2001 Inpt days Abstinence Rates 12 Step 13.1 10.5 45.7 Cog Beh 17 17 36.2 * all p< .001 ** 64% higher cost for CBT Dual Screening: the “Dual Cage”…………….easy, but no data ASAM pt placement………..needs experience, little or no data ASI psych…………………….short, available, good screening, good data Beck, Zung, Ham D etc…..easy, good data, may be limited Brief Symptom Inventory…easy, broad symptom mix Others……………………………see new Co-occurring TIP in 12-04 “Dual CAGE” QUESTIONS Cut Down (or stopped) Annoyed when drug/alc. use discussed Because mental symptoms worsened Because MH doctor or therapist suggested Annoyed, anxious or angry,… fights when using Admitted to ER or hospital for psych when using or not ADHD when child Guilty about use Guilty, depressed, suicidal when using or not Ever made a suicide attempt when using or not CAGE Questions Eye opener: taken drink or drug in AM to feel better Taken a drink or drug to blot out symptoms Taken drink or drug with psych med Not taken meds because of using drug/alc (forgot, avoid mixing, etc.) What are 2 or 3 reasons you use alc/drugs? What are 2 or 3 reasons you might want to stop or cut down? Medications Essential to Treatment of Severely Mentally Ill Substance Use and Not-Taking Meds are the 2 top reasons for De-Comp Should be part of court orders Monitored by Case managers, nurses, doctors For Dep/Anx, less clear Personal experience shows maximizing 12 step AND use of meds is best rx It may not be that the med(s) stopped working, but…… The patient stopped the med The patient stopped the med AND used drugs and/or alcohol…... OR lowered the med and used… OR used on top of the med…. OR used twice the dose on one day and nothing the next…. Stimulants ( cocaine/amphets) are most MSE destructive. How to use AA as a treatment partner 1. Know something about AA, its history, presence in your community, structure and content 2. Helpful Readings: Brown: A psychological view of the 12 steps AA: AA for the medical practitioner; and The AA member and medications Twelve Step Facilitation Therapy Manual Project Match, NIAAA web site Forman: “One AA Meting doesn’t fit all” One year ABSTINENCE was predicted by: • AA involvement (OR=2.9), ( n=377) • not having pro-drinking influences in one's network (OR=0.7 • having support for reducing consumption from people met in AA (versus no support; OR=3.4). • In contrast, having support from non-AA members was not a significant predictor of abstinence. Kaskutas: Addiction 2002 Double Trouble Recovery (DTR) Outcomes Members of 24 DTR groups (n=240) New York City, 1 year outcomes Drug/alcohol abstinence = 54% at baseline, increased to 72% at follow-up. More attendance = better Medication adherence, Better Medication adherence = less hospitalization Magura Add Beh 2003, Psych Serv 2002 Dual Dep/Anx RX plan Differential Dx 12 step facilitation Meds if indicated ( and I often use them) Visits: Ries 1/week ( 12 step facil and meds) AA 3x week or 90 in 90 Meet with sponsor Meet with family Low mental illness/High addictions outpt gets In most MHC’s: MD visit q 3 months CM visit q 2 wks…focus on ADL’s Maybe dual dx group 1-2 hrs/wk Limited expectations of recovery Pschotherapy time ~ 0-2 hrs week In the most Addictions IOP’s MD visit 1/ 3 months, often 1’ care CM 1:1 q 2 wks….focus on Sub use, U tox’s IOP group 3 hrs-3x week Expectations of Sobriety/progress Psychotherapy time 3-10 hrs week ( plus more AA) Report Questions Ability of National Treatment Infrastructure to Deliver Quality Care 100% 80% Percentage of Programs 60% 54% 40% 25% 20% 15% 20% 0% Closed or Stopped Services Reorganized Director in No Information Position Less Than Services, E-mail, One Year or Voicemail SOURCE: Adapted by CESAR from the McLellan, A. T., Carise, D., and Kleber, J., “Can the National Addiction Treatment Infrastructure Support the Public’s Demand for Quality Care?” Journal of Substance Abuse Treatment 25(2):117-121, 2003. For more information, contact Dr. A. Thomas McLellan at tmclellan@tresearch.org. 301-405-9770 (voice) 301-403-8342 (fax) CESAR@cesar.umd.edu www.cesar.umd.edu CESAR FAX is supported by VOIT 1996-1002, awarded by the U.S. Department of Justice through the Governor’s Office of Crime Control and Prevention. CESAR FAX may be copied without permission. Please cite CESAR as the source. New Issues in Medications for Co-occurring Addiction and Mental Disorders Richard Ries MD Medication monitoring and motivating Know who is on what and what for Know the prescriber if possible Sit in on med sessions onsite Talk to off-site doctor or nurse PRE problem!!! Know something about meds… ATTC Tech transfer centers summary New COD TIP ( Dec 04) NIMH web site, NAMI web site Medications: counselor’s role Ask the pt about : Compliance… Effectiveness… “sometimes people forget their medications…how often does this happen to you?” …ie % not taking “how well do you think the meds are working?… what do you notice… here is what I notice Side Effects…. “ are you having any side effects to the medication?… what are they… have you told the prescriber? do you need help with talking to the presciber? Medications….potential problems Can reinforce addiction denial if recovery is not integrated and supported…esp by the prescriber..( so work with them) Can be expensive, cause side effects, could be used in overdose. Encumber the pt with seeing MD, or mental health system, cost, convenience etc….ie make sure they are really necessary. Active participation in recovery can be both antidep and antianx…but if these problems continue, or disrupt recovery, meds should be considered Antipsychotics Alcohol Clin Exp Res. 2004 May;28(5):73645. A double-blind, placebo-controlled study of olanzapine in the treatment of alcohol-dependence disorder. Guardia J, Segura L, Gonzalvo B, Iglesias L, Roncero C, Cardus M, Casas M. METHODS: A total of 60 alcohol-dependent patients were assigned to 12 weeks' treatment with either olanzapine or placebo. The primary variable relapse to heavy drinking rate was evaluated by means of intention-to-treat analyses. Alcohol consumption, craving, adverse events, and changes in the biochemical markers of heavy drinking and possible toxicity were also evaluated. RESULTS: We did not find significant differences in the survival analysis between placebo and olanzapine-treated patients (Kaplan-Meier log rank = 0.46, df = 1, p = 0.50). Eleven (37.9%) patients treated with olanzapine relapsed compared with 9 (29%) of those receiving placebo (chi = 0.53, df = 1, p = 0.5). Although some adverse events (weight gain, increased appetite, drowsiness, constipation, and dry mouth) were found more frequently in the olanzapine group, differences did not reach statistical significance in comparison with the placebo group. CONCLUSIONS: We found no differences in relapse rate or other drinking variables when comparing olanzapine with placebo-treated patients. J Clin Psychopharmacol. 2000 Feb;20(1):94-8. Effects of clozapine on substance use in patients with schizophrenia and schizoaffective disorder: a retrospective survey. Zimmet SV, Strous RD, Burgess ES, Kohnstamm S, Green AI. . The authors report data from a retrospective survey of substance use in 58 patients treated with clozapine who had a history of comorbid schizophrenia (or schizoaffective disorder) and substance use disorder. Of these 58 patients, 43 were being treated with clozapine at the time of the survey; the remaining 15 patients had discontinued clozapine before the survey. More than 85% of the patients who were active substance users at the time of initiation of treatment with clozapine decreased their substance use over the course of clozapine administration. For patients who continued treatment with clozapine up to the present, the decrease in substance use was strongly correlated with a decrease in global clinical symptoms. Schizophr Res. 2004 Feb 1;66(2-3):125-35. First episode schizophrenia-related psychosis and substance use disorders: acute response to olanzapine and haloperidol. Green AI, Tohen MF, Hamer RM, Strakowski SM, Lieberman JA, Glick I, Clark WS; HGDH Research Group. METHODS: The study involved 262 patients. Patients with a history of substance dependence within 1 month prior to entry were excluded. RESULTS: Of this sample, 97 (37%) had a lifetime diagnosis of substance use disorder (SUD); of these 74 (28% of the total) had a lifetime cannabis use disorder (CUD) and 54 (21%) had a lifetime diagnosis of alcohol use disorder (AUD). •Those with CUD had a lower age of onset than those without. •Patients with SUD were more likely to be men. •Patients with SUD had more positive symptoms and fewer negative symptoms than those without SUD, and they had a longer duration of untreated psychosis. •The 12-week response data indicated that 27% of patients with SUD were responders compared to 35% of those without SUD. •Patients with AUD were less likely to respond to olanzapine than those without AUD. DISCUSSION: These data suggest that first-episode patients are quite likely to have comorbid substance use disorders, and that the presence of these disorders may negatively influence response to antipsychotic medications, both typical and atypical antipsychotics, over the first 12 weeks of treatment. Bipolar Disord. 2002 Dec;4(6):406-11. Related Articles, Links Quetiapine in bipolar disorder and cocaine dependence. Brown ES, Nejtek VA, Perantie DC, Bobadilla L. METHODS: Open-label, add-on, quetiapine therapy was examined for 12 weeks in 17 outpatients with bipolar disorder and cocaine dependence. Subjects were evaluated with a structured clinical interview; Hamilton Depression Rating (HDRS), Young Mania Rating (YMRS), Brief Psychiatric Rating (BPRS) scales; and Cocaine Craving Questionnaire (CCQ). Urine samples and self-reported drug use were also obtained. Data were analyzed using a last observation carried forward method on all subjects given medication at baseline. RESULTS: Significant improvement from baseline to exit was observed in HDRS, YMRS, BPRS and CCQ scores (p < or = 0.05). Dollars spent on cocaine and days/week of cocaine use decreased non-significantly, and urine drug screens did not change significantly from baseline to exit. Quetiapine was well tolerated, with no subjects to our knowledge discontinuing because of side-effects. CONCLUSIONS: The use of quetiapine was associated with substantial improvement in psychiatric symptoms and cocaine cravings. The findings are promising and suggest larger controlled trials of quetiapine are needed in this population. Schizophr Res. 2003 Mar 1;60(1):81-5. Alcohol and cannabis use in schizophrenia: effects of clozapine vs. risperidone. Green AI, Burgess ES, Dawson R, Zimmet SV, Strous RD. METHOD: This study involved retrospective assessment of abstinence (cessation of alcohol and cannabis use) in 41 patients treated with either risperidone (n=8) or clozapine (n=33) for at least 1 year. In 32 of these 41 patients, information was available on whether abstinence occurred during the 1-year period. RESULTS: Abstinence rates were significantly higher in patients treated with clozapine than in those treated with risperidone (54% vs. 13%, p=0.05). Eur J Pharmacol. 2003 May 9;468(2):121-7. Risperidone reduces limited access alcohol drinking in alcoholpreferring rats. Ingman K, Honkanen A, Hyytia P, Huttunen MO, Korpi ER. Department of Pharmacology and Clinical Pharmacology, University of Turku, Itainen Pitkakatu 4, FIN-20520, Turku, Finland An atypical antipsychotic drug risperidone reduced ethanol drinking of ethanol-preferring Alko, Alcohol (AA) rats in a limited access paradigm. Its effect was transient at a dose known to preferentially antagonize the 5-HT(2) receptors (0.1 mg/kg, s.c.), but long-lasting when the dose was increased to 1.0 mg/kg that also blocks dopamine D(2) receptors. Can J Psychiatry. 2002 Sep;47(7):671-5. Related Articles, Links Risperidone decreases craving and relapses in individuals with schizophrenia and cocaine dependence. Smelson DA, Losonczy MF, Davis CW, Kaune M, Williams J, Ziedonis D. OBJECTIVE: To examine the efficacy of atypical neuroleptics for decreasing craving and drug relapses during protracted withdrawal in individuals dually diagnosed with schizophrenia and cocaine dependence. METHOD: We conducted a 6-week, open-label pilot study comparing risperidone with typical neuroleptics in a sample of withdrawn cocaine-dependent schizophrenia patients. RESULTS: Preliminary results suggest that individuals treated with risperidone had significantly less cue-elicited craving and substance abuse relapses at study completion. Further, they showed a trend toward a greater reduction in negative and global symptoms of schizophrenia. CONCLUSION: Atypical neuroleptics may help reduce craving and relapses in this population. Future research should include more rigorous double-blind placebo-controlled studies with this class of medications. Comorbid Substance Abuse Associated With Noncompliance in Schizophrenia P < 0.05 Nearly half of all patients in a prospective 4-year study (N = 99) were active substance abusers (n = 42) Patients who actively abused substances were significantly more likely to be noncompliant 67% % Noncompliant 80 60 47% 40 34% 20 0 No Past Past Current History History User Hunt GE et al. Schizophrenia Res. 2002;54:253-264. It may not be that the med(s) stopped working, but…… The patient stopped the med The patient stopped the med AND used drugs and/or alcohol…... OR lowered the med and used… OR used on top of the med…. OR used twice the dose on one day and nothing the next…. Stimulants ( cocaine/amphets) are most MSE destructive. RISPERDAL® CONSTA™ Injection Kit Components Needle Pro SmartSite Access Device ® Aqueous Diluent Risperidone Microspheres Assembled RISPERDAL® CONSTA™ PRC approved with changes: 11/10/03 (RISPERDAL CONSTA Promotional slide kit) ® Device Safety Needle Risperidone + 9-hydroxyrisperidone (ng/mL) Blood Levels Over Time After Single Dose* PRC approved with changes: 11/10/03 (RISPERDAL CONSTA Promotional slide kit) 0 1 2 Antipsychotic Supplementation 3 4 5 6 Time (wk) *25-mg dose, N = 14. Data on file, Janssen Pharmaceutica Products, L.P. 7 8 9 10 11 12 Substance Induced Psychoses Amphet/Methamphetamines Cocaine Ecstacy Hallucinogens ( strong THC too) Other Rave Drugs Alcohol WD and Hallucinosis Anticonvulsants COMPARING THE KNOWN EFFICACY OF ANTIEPILEPTIC AGENTS IN BIPOLAR DISORDER Drug Mania Depression Maintenance Comments New Depakote ER Formulation 2 new maintenance studies v. lithium Gabapentin — 2 negative placebocontrolled studies in mania Lamotrigine Antidepressant activity in several controlled trials Topiramate Dose-related weight loss Valproate Carbamzepine Key: Efficacy demonstrated in > 2 placebo-controlled trials Efficacy demonstrated in one placebo-controlled or two large, active comparator trials Efficacy in two small or one large active comparator trial Efficacy only in open trials and case series Conflicting evidence of efficacy in available studies — Lack of efficacy demonstrated in randomized, controlled trials ND No data presently available Keck & McElroy, 2002 COMPARING THE KNOWN EFFICACY OF ANTIEPILEPTIC AGENTS IN BIPOLAR DISORDER Drug Mania Depression Maintenance Comments Improved tolerability & pharmacokinetics Zonisamide ND ND May produce weight loss in some patients Tiagabine ND ND More data needed regarding tolerability and efficacy Levetiracetam ND ND ND Data needed regarding efficacy and tolerability Oxcarbazepine Key: ND Efficacy in two small or one large active comparator trial Efficacy only in open trials and case series Conflicting evidence of efficacy in available studies No data presently available Keck & McElroy, 2002 Eur Neuropsychopharmacol. 2004 Aug;14(4):319-23. Related Articles, Links How real are patients in placebo-controlled studies of acute manic episode? Storosum JG, Fouwels A, Gispen-de Wied CC, Wohlfarth T, van Zwieten BJ, van den Brink W. OBJECTIVE: To determine whether the results from placebo-controlled studies conducted in patients with manic episode can be generalised to a routine population of hospitalised acute manic patients. METHODS: A list of four most prevalent inclusion and the nine most prevalent exclusion criteria was constructed for participation in previous randomised-controlled trials (RCTs). On the basis of this list, a consecutive series of 68 patients with 74 episodes of acute mania who had been referred for routine treatment were retrospectively assessed to determine their eligibility for a hypothetical but representative randomised controlled trial. RESULTS: Only 16% of the manic episodes would qualify for the hypothetical trial (male episodes 28%, female episodes 10%), ….whereas 37%, 20% and 27% of the manic episodes would have to be excluded because they did no fulfil one, two or at least three of the inclusion or exclusion criteria. CONCLUSION: Only a small percentage acute manic episodes in a routine mental hospital seem to qualify for a standard placebo-controlled RCT.. These notions should be taken into account when evaluating the results of RCTs in bipolar patients with an acute manic episode. Am J Addict 2002 Spring;11(2):141-50 The differential effects of medication on mood, sleep disturbance, and work ability in outpatient alcohol detoxification. Malcolm R, Myrick H, Roberts J, Wang W, Anton RF. A double-blind, randomized controlled trial of patients (n = 136) meeting DSM-IV criteria for alcohol withdrawal and stratified based on detoxification history were treated with carbamazepine or lorazepam for 5 days on a fixed dose tapering schedule. Mood symptoms improved for all subjects regardless of medication or detoxification history. •main effect favoring carbamazepine in reducing anxiety (p = 0.0007). •main effect of medication on sleep that again favored carbamazepine (p = 0.0186). In this study of outpatients with mild to moderate alcohol withdrawal, carbamazepine was superior to lorazepam in reducing anxiety and improving sleep. Alcohol Clin Exp Res 2001 Sep;25(9):1324-9 Related Articles, Books, LinkOut Divalproex sodium in alcohol withdrawal: a randomized double-blind placebo-controlled clinical trial. Reoux JP, Saxon AJ, Malte CA, Baer JS, Sloan KL. Veterans Affairs Puget Sound Health Care System and Department of Psychiatry, University of Washington School of Medicine, Seattle, Washington 98108, USA. joe.reoux@med.va.gov Psychiatr Serv. 2000 May;51(5):634-8. Related Articles, Links Changes in use of valproate and other mood stabilizers for patients with schizophrenia from 1994 to 1998. Citrome L, Levine J, Allingham B. METHODS: For each calendar year from 1994 through 1998, data were drawn from a database containing clinical and drug prescription information for every inpatient in the adult civil facilities of the New York State Office of Mental Health. RESULTS: In 1994 a total of 26.2 percent of inpatients diagnosed as having schizophrenia received a mood stabilizer, compared with 43.4 percent in 1998. In 1994 lithium was the most commonly prescribed mood stabilizer, for 13.2 percent of patients, followed by valproate, for 12.3 percent. In 1998 valproate was the most commonly prescribed, for 35 percent of patients, followed by lithium, for 11.3 percent. On average, patients received valproate for about two-thirds of their hospital stay, at a mean dose of 1,520 mg per day. CONCLUSIONS: The adjunctive use of valproate nearly tripled from 1994 to 1998 among patients with a diagnosis of schizophrenia. Valproate has become the most commonly prescribed mood stabilizer for this population, despite the paucity of evidence in the literature for efficacy in this use. Controlled clinical trials are needed to examine the adjunctive use of mood stabilizers, in particular valproate, among patients with schizophrenia. Psychiatr Serv. 2004 Mar;55(3):290-4. Related Articles, Links Adjunctive divalproex and hostility among patients with schizophrenia receiving olanzapine or risperidone. Citrome L, Casey DE, Daniel DG, Wozniak P, Kochan LD, Tracy KA. METHODS: A total of 249 inpatients with schizophrenia were randomly assigned, RESULTS: Combination treatment with risperidone or olanzapine plus divalproex was associated with different scores on the hostility item of the PANSS compared with antipsychotic monotherapy. •This result was not seen beyond the first week of treatment, but there was a trend toward a difference in effect for the entire treatment period. •Combination therapy had a significantly greater antihostility effect at days 3 and 7 than monotherapy. •The effect on hostility appears to be statistically independent of antipsychotic effect on other PANSS items reflecting delusional thinking, a formal thought disorder, or hallucinations. CONCLUSIONS: Divalproex sodium may be useful as an adjunctive agent in specifically reducing hostility in the first week of treatment with risperidone or olanzapine among patients with schizophrenia experiencing an acute psychotic episode. J Clin Psychopharmacol. 2001 Feb;21(1):21-6. Related Articles, Links Divalproex sodium augmentation of haloperidol in hospitalized patients with schizophrenia: clinical and economic implications. Wassef AA, Hafiz NG, Hampton D, Molloy M. Divalproex sodium has been approved for use in treating bipolar disorder. Its usefulness in schizophrenia has yet to be adequately assessed. Compared with those who received no or delayed augmentation, the earlyaugmentation group required 44.8% fewer inpatient days from the initiation of haloperidol treatment. Patient response to treatment was particularly noted in suspiciousness, hallucinations, unusual thought content, and emotional withdrawal. Early augmentation with valproate may reduce the length of inpatient stays and provide substantially better therapeutic outcomes. It is, however, premature to recommend changes in the standard clinical management of schizophrenia on the basis of the data provided herein, in view of the small sample and open-label nature of the report. Depakote with Atypical Antipsychotic: lipids Patients treated with a combination of Depakote and Zyprexa experienced a minimal increase in total cholesterol compared to the greater increase in patients treated with Zyprexa when used as monotherapy: +26.62 mg/dL for Zyprexa monotherapy (baseline: 193 mg/dL). +0.87 mg/dL for Depakote plus Zyprexa (baseline: 198 mg/dL). Patients treated with a combination of Depakote and Risperdal experienced a decrease in total cholesterol compared to Risperdal when used as monotherapy: +9.64 mg/dL for Risperdal monotherapy (baseline: 188 mg/dL). -13.44 mg/dL for Depakote plus Risperdal (baseline: 192 mg/dL). Patients in the Zyprexa monotherapy group had the highest rate of shift from a normal total cholesterol (<200 mg/dL) to a high total cholesterol (>200 mg/dL). Casey et al APA conv 2004 Lancet. 2003 May 17;361(9370):1677-85. Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. Johnson BA et al METHODS: double-blind randomised controlled 12-week clinical trial comparing oral topiramate and placebo for treatment of 150 individuals with alcohol dependence.. FINDINGS: At study end, participants on topiramate, compared with those on placebo, had • • • • • 2.88 (95% CI -4.50 to -1.27) fewer drinks per day (p=0.0006), 3.10 (-4.88 to -1.31) fewer drinks per drinking day (p=0.0009), 27.6% fewer heavy drinking days (p=0.0003), 26.2% more days abstinent (p=0.0003), and a log plasma gamma-glutamyl transferase ratio of 0.07 (-0.11 to 0.02) less (p=0.0046). Topiramate-induced differences in craving were also significantly greater than those of placebo, of similar magnitude to the self-reported drinking changes, and highly correlated with them. Topiramate for Alcohol Withdrawal: 1: Med Arh. 2002;56(4):211-2. A pilot study of Topiramate (Topamax) in the treatment of tonic-clonic seizures of alcohol withdrawal syndromes. Rustembegovic A, Sofic E, Kroyer G. Anton Proksch Institute, Vienna, Austria. 12 patients with median age of 49.5 years and median body weight of 76.3 kg were treated with topiramate twice daily for up 30 days, starting with a dose of 50 mg in the morning and 50 mg in the evening. The preliminary findings of this study suggest that topiramate is very effective against tonic-clonic seizures in alcohol withdrawal syndrome. No side effects were observed. Only two patients had loss of body weight (3-3.5 kg/4 weeks). J Clin Psychopharmacol. 2004 Aug;24(4):374-8. Vieta E,et al Effects on weight and outcome of long-term olanzapinetopiramate combination treatment in bipolar disorder. Twenty-six Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition bipolar spectrum patients received olanzapine plus topiramate cotherapy for treatment of their manic (n = 14), hypomanic (n = 6), depressive (n = 2), and mixed (n = 1) symptoms for 1 year. Three rapid cycling patients were also enrolled despite being euthymic. Thirteen (50%) patients completed the 1-year follow-up. By intent-to-treat, patients significantly improved from baseline in • • • • Young Mania Rating Scale scores (P < 0.0001), Hamilton Depression Rating Scale (P < 0.05), and Modified Clinical Global Impressions for Bip (mania P < 0.0001, Depression ( Ham) P < 0.05, ………overall P < 0.0001). Most patients gained weight during the first month of combined treatment (mean weight gain 0.7 +/- 0.6 kg), but at the 12-month endpoint, the mean weight change was -0.5 +/- 1.1 kg. Subst Abus. 2003 Jun;24(2):29-32. Gabapentin for the treatment of ethanol withdrawal. Voris J, Smith NL, Rao SM, Thorne DL, Flowers QJ. We retrospectively report on the use of gabapentin for ethanol withdrawal in 49 patients. Thirty-one patients were treated in the outpatient program and 18 in the general inpatient psychiatric unit. Positive outcomes as evidenced by completion of gabapentin therapy were achieved in 25 out of 31 outpatients and 17 out of 18 inpatients. Statistical significance was reached regarding the positive relationship between prior ethanol use and inpatient "as needed" benzodiazepine use. Both sets of data suggest that gabapentin works well for the mild to moderate alcohol withdrawal patient. Psychiatry Clin Neurosci. 2003 Oct;57(5):542-4. Related Articles, Links Open pilot study of gabapentin versus trazodone to treat insomnia in alcoholic outpatients. Karam-Hage M, Brower KJ. Alcohol-dependent outpatients with persisting insomnia were treated with either gabapentin or trazodone. Patients were assessed at baseline and after 4-6 weeks on medication using the Sleep Problems Questionnaire (SPQ). Of 55 cases initially treated, 9% dropped out due to morning drowsiness. Of the remaining 50 cases, 34 were treated with gabapentin (mean dose +/- SD = 888 +/- 418 mg) at bedtime and 16 were treated with trazodone (105 +/- 57 mg) at bedtime. Both groups improved significantly on the SPQ but the gabapentin group improved significantly more than the trazodone group. Controlled studies are warranted to replicate these findings. Med Arh. 2004;58(1):5-6. A study of gabapentin in the treatment of tonic-clonic seizures of alcohol withdrawal syndrome. Rustembegovic A, Sofic E, Tahirovic I, Kundurovic Z. In this study for thirty (30) patients with alcohol withdrawal syndrome, the response to anticolvusant gabapentin was assessed. Thirty (30) patients with median age of 57.0 years and median body weight of 79.1 kg were treated with gabapentin 3 x 300 mg daily for up 30 days. The preliminary findings of this study suggest that gabapentin is very effective against tonic-clonic seizures in alcohol withdrawal syndrome. Gabapentin was safe and well tolerated. For twenty (20) patients no side effect were observed. J Clin Psychiatry. 2003 Feb;64(2):197-201. Related Articles, Links Lamotrigine in patients with bipolar disorder and cocaine dependence. Brown ES, Nejtek VA, Perantie DC, Orsulak PJ, Bobadilla L. METHOD: Lamotrigine was started at a dose of 25 mg/day (12.5 mg/day in those taking valproic acid) and titrated to a maximum dose of 300 mg/day. The subjects consisted of 13 men and 17 women with cocaine dependence and bipolar I disorder (N = 22), bipolar II disorder (N = 7), or bipolar disorder not otherwise specified (N = 1), with a mean +/- SD age of 35.4 +/- 7.2 years. Data were analyzed using the last observation carried forward on all subjects who completed the baseline evaluation and at least 1 postbaseline assessment. RESULTS: Significant improvement was observed in HAM-D, YMRS, and BPRS scores (p < or =.02). Cravings also significantly decreased as measured by the CCQ (p <.001). Dollar amount spent on drugs decreased nonsignificantly. Lamotrigine was well tolerated, with no subjects discontinuing due to side effects. CONCLUSION: Lamotrigine treatment was well tolerated in this sample and associated with statistically significant improvement in mood and drug cravings but not drug use. The findings suggest that larger controlled trials of lamotrigine are needed in this population. Anti-opiate Addiction Meds Harm reduction:..opiates Methadone LAAM. Not given orally Suboxone Due to liver prolems ( minor) is being phased out Buprenorphine Only through Methadone agencies for Addiction Confusion when injury/pain/addiction co-occurr Combination of Bup plus Naloxone subligual Absorb the Bup, not the Naloxone If used IV then immediate Withdrawal from naloxone Practitioners need special DEA # and training Withdrawal treatment Methadone Buprenorphine Clonidine ++ Intrinsic Activity: Full Agonist (Methadone), Partial Agonist (Buprenorphine), Antagonist (Naloxone) 100 90 Full Agonist (Methadone) 80 70 Intrinsic Activity 60 Partial Agonist (Buprenorphine) 50 40 30 20 10 Antagonist (Naloxone) 0 -10 -9 -8 -7 Log Dose of Opioid -6 -5 -4 Figure 3: Induction for Patient Physically Dependent On Short-acting Opioids, Day 1 Patient dependent on short-acting opioids? Yes Withdrawal symptoms present 12-24 hrs after last use of opioids? No Yes Stop; not dependent on short-acting opioids Give buprenorphine 2-4 mg, observe 2+ hrs Withdrawal symptoms continue or return? No Yes Withdrawal symptoms return? No Yes Repeat dose up to maximum 8 mg for first day Withdrawal symptoms relieved? Yes Daily dose established. GO TO SWITCH DIAGRAM (Fig. 6) No Manage withdrawal symptomatically Return next day for continued induction. GO TO INDUCTION DAY 2 DIAGRAM (Fig. 5) Daily dose established. GO TO SWITCH DIAGRAM (Fig. 6) Drug Interactions with Buprenorphine Benzodiazepines and other sedating drugs Medications metabolized by cytochrome P450 3A4 Opioid antagonists Opioid agonists Drug Alcohol Depend. 2003 Apr 1;69(3):263-72. Related Articles, Links Opioid detoxification with buprenorphine, clonidine, or methadone in hospitalized heroin-dependent patients with HIV infection. Umbricht A, Hoover DR, Tucker MJ, Leslie JM, Chaisson RE, Preston KL. In a randomized, double-blind clinical trial, we evaluated the impact of three medications on the signs and symptoms of withdrawal and on the pain severity in heroin-dependent HIV-infected patients (N=55) hospitalized for medical reasons on an inpatient AIDS service. Patients received a 3-day pharmacologic taper with intramuscular buprenorphine (n=21), oral clonidine (n=16), or oral methadone (n=18), followed by a clonidine transdermal patch on the fourth day. Observed and self-reported measures of opioid withdrawal and pain were taken 1-3 times daily for up to 4 days. Opiate administration used as medically indicated for pain was also recorded. Observer- and subject-rated opiate withdrawal scores decreased significantly following the first dose of medication and overall during treatment. Among all 55 subjects, self-reported and observer-reported pain decreased after treatment (on average observer-rated opioid withdrawal scale (OOWS) scores declined 5.6 units and short opioid withdrawal scale (SOWS) declined 4.8 units, P<0.001, for both) with no indication of increased pain during medicati taper. There were no significant differences of pain decline and other measures of withdrawal between the three treatment groups. During the intervention period, supplemental opiates were administered as medically indicated for pain to 45% of the patients; only 34% of men versus 62% of women received morphine (P<0.05). These findings suggest buprenorphine, clonidine, and methadone regimens each decrease opioid withdrawal in medically ill HIV-infected patients. Other Addiction Meds Relapse prevention…Alcohol Naltrexone…opiate system Acamprosate…GABA system??......... just released and being evaluated in large current studies NALTREXONE IN THE TREATMENT OF ALCOHOL DEPENDENCE Cumulative Proportion with No Relapse Cumulative Relapse Rate 1.2 1 0.8 0.6 0.4 Naltrexone HCL (N=35) Placebo (N=35) 0.2 0 0 1 2 3 4 5 6 7 8 9 10 11 12 No. of Weeks Receiving Medication Volpicelli et al., 1992 ACAMPROSATE RELAPSE RATES Treatment Period 100 Follow-up Period 90 % of Abstinent Patients 80 Acamprosate 70 Placebo 60 50 40 30 20 10 0 0 24 48 Weeks 72 96 Addiction. 2004 Jul;99(7):811-28. Related Articles, Links Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review. Carmen B, Angeles M, Ana M, Maria AJ. Findings Thirty-three studies met the inclusion criteria. Acamprosate was associated with a significant improvement in abstinence rate [odds ratio (OR): 1.88 (1.57, 2.25), P < 0.001] and days of cumulative abstinence [WMD: 26.55 (17.56, 36.54]. Short-term administration of naltrexone reduced the relapse rate significantly [OR: 0.62 (0.52, 0.75), P < 0.001], but was not associated with a significant modification in the abstinence rate [OR: 1.26 (0.97,1.64), P = 0.08]. There were insufficient data to ascertain naltrexone's efficacy over more prolonged periods. Acamprosate had a good safety pattern and was associated with a significant improvement in treatment compliance [OR: 1.29 (1.13,1.47), P < 0.001]. Naltrexone's side effects were more numerous, yet the drug was nevertheless tolerated acceptably without being associated with a lower adherence to treatment (OR: 0.94 (0.80, 1.1), P = 0.5). However, overall compliance was relatively low with both medications. Medications in Patients with Addictions….potential problems Can reinforce addiction denial if Alc/Drg intervention is not integrated and supported…esp by the prescriber.. Can be expensive, cause side effects, could be used in overdose. Encumber the pt with seeing MD, or mental health system, cost, convenience etc….ie make sure they are really necessary. Active participation in recovery can be both antidep and antianx…but if serious psych problems continue, or disrupt recovery, meds should be considered For more serious problems such as psychosis and mania, immediate use of medications is indicated Sleep in recovering Alc/Addicts Abnormal for weeks/months in most Is this “normal toxicity” and to be tolerated Poor sleep associated with relapse, anx, dep, PTSD, and PROTRACTED WITHDRAWAL Medications for sleep in recovering addicts/alcoholics Treat the comorbid disorder causing the sleep problem….ie dep/anx etc, with an antidepressant And/or protracted withdrawal…..with anticonvulsants ( for one to several months) Prazosin for PTSD nightmares Anti histamines, trazedone, remeron as non-specific aids If using BZP’s, oxazepam and librium Anticonvulsants Role in alc withdrawal acute and/or protracted Role in bipolar, esp rapid cycle Role in early antipsychotic augmentation Great for ongoing sleep problems... Is this protracted withdrawal? Is there a role in craving/relapse prevention? Is there a role for PRN use in agitated Dual pts, such as 500 mg valproate, 600 mg gabapentin etc?? Anticonvulsants in alcohol withdrawal Good evidence for carbamazepine, valproate and growing for gabapentin and topiramate May even be superior in terms of safety, ability for take home doses and in some studies, even anxiety/agitation Have been shown effective in high dose BZP dependence Stay Cool and Keep Calm