Congenital Heart Disease Internal Medicine/Pediatrics Lecture series
advertisement

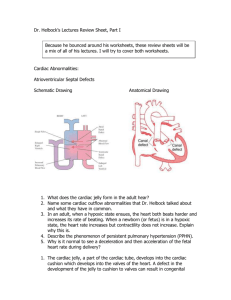
Congenital Heart Disease Part I By Katrice L. Herndon, M.D. Acyanotic Congenital Heart Disease Left-to-Right Shunt Lesions • • • • Atrial Septal Defect (ASD) Ventricular Septal Defect (VSD) Atrioventricular Septal Defect (AV Canal) Patent Ductus Arteriosus (PDA) Atrial Septal Defect • ASD is an opening in the atrial septum permitting free communication of blood between the atria. Seen in 10% of all CHD. Atrial Septal Defect • There are 3 major types: • Secundum ASD – at the Fossa Ovalis, most common. • Primum ASD – lower in position & is a form of ASVD, MV cleft. • Sinus Venosus ASD – high in the atrial septum, associated w/partial anomalous venous return & the least common. Atrial Septal Defect • Secundum ASD • Sinus Venosus ASD Atrial Septal Defect Clinical Signs & Symptoms • Rarely presents with signs of CHF or other cardiovascular symptoms. • Most are asymptomatic but may have easy fatigability or mild growth failure. • Cyanosis does not occur unless pulmonary HTN is present. Atrial Septal Defect Clinical Signs & Symptoms • Hyperactive precordium, RV heave, fixed widely split S2. • II-III/VI systolic ejection murmur @ LSB. • Mid-diastolic murmur heard over LLSB. Atrial Septal Defect • Question: What causes the systolic & diastolic murmurs of ASD? • Answer: Systolic murmur is caused by increased flow across the pulmonary valve, NOT THE ASD. Diastolic murmur is caused by increased flow across the tricupsid valve & this suggest high flow Qp:Qs is 2:1. Atrial Septal Defect Treatment: • Surgical or catherization laboratory closure is generally recommended for secundum ASD w/ a Qp:Qs ratio >2:1. • Closure is performed electively between ages 2 & 5 yrs to avoid late complications. • Surgical correction is done earlier in children w/ CHF or significant Pulm HTN. Atrial Septal Defect Treatment • Once pulmonary HTN w/ shunt reversal occurs this is considered too late. • Mortality is < 1%. Atrial Septal Defect • Question: Is endocarditis prophylaxis required for ASD? • Answer: NO Ventricular Septal Defect • VSD – is an abnormal opening in the ventricular septum, which allows free communication between the Rt & Lt ventricles. Accounts for 25% of CHD. Ventricular Septal Defect • 4 Types • Perimembranous (or membranous) – Most common. • Infundibular (subpulmonary or supracristal VSD) – involves the RV outflow tract. • Muscular VSD – can be single or multiple. • AVSD – inlet VSD, almost always involves AV valvular abnormalities. Ventricular Septal Defect Hemodynamics • The left to right shunt occurs secondary to PVR being < SVR, not the higher pressure in the LV. • This leads to elevated RV & pulmonary pressures & volume hypertrophy of the LA & LV. Ventricular Septal Defect Clinical Signs & Symptoms • Small - moderate VSD, 3-6mm, are usually asymptomatic and 50% will close spontaneously by age 2yrs. • Moderate – large VSD, almost always have symptoms and will require surgical repair. Ventricular Septal Defect Clinical Signs & Symptoms • II-III/VI harsh holosystolic murmur heard along the LSB, more prominent with small VSD, maybe absent with a very Large VSD. • Prominent P2, Diastolic murmur. • CHF, FTT, Respiratory infections, exercise intolerance hyperactive precordium. Symptoms develop between 1 – 6 months Ventricular Septal Defect Treatment • Small VSD - no surgical intervention, no physical restrictions, just reassurance and periodic follow-up and endocarditis prophylaxis. • Symptomatic VSD - Medical treatment initially with afterload reducers & diuretics. Ventricular Septal Defect Treatment • Indications for Surgical Closure: • Large VSD w/ medically uncontrolled symptomatology & continued FTT. • Ages 6-12 mo w/ large VSD & Pulm. HTN • Age > 24 mo w/ Qp:Qs ratio > 2:1. • Supracristal VSD of any size, secondary to risk of developing AV insufficiency. Atrioventricular Septal Defect • AVSD results from incomplete fusion the the endocardial cushions, which help to form the lower portion of the atrial septum, the membranous portion of the ventricular septum and the septal leaflets of the triscupid and mitral valves. • They account for 4% OF ALL CHD. Atrioventricular Septal Defect • Question: What genetic disease is AVSD more commonly seen in? • Answer: Down’s Syndrome (Trisomy 21), Seen in 20-25% of cases. Atrioventricular Septal Defect Complete Form Incomplete Form • Low primum ASD continuous with a posterior VSD. • Any one of the components may be present. • Cleft in both septal leaflets of TV/MV. • Most common is primum ASD, cleft in the MV & small VSD. • Results in a large L to R shunt at both levels. • TR/MR, Pulm HTN w/ increase in PVR. • Hemodynamics are dependent on the lesions. Atrioventricular Septal Defect • Complete AVSD Atrioventricular Septal Defect • • • • • • Clinical Signs & Symptoms Incomplete AVSD maybe indistinguishable from ASD - usually asymptomatic. Congestive heart failure in infancy. Recurrent pulmonary infections. Failure to thrive. Exercise intolerance, easy fatigability. Late cyanosis from pulmonary vascular disease w/ R to L shunt. Atrioventricular Septal Defect • • • • • • • Clinical Signs & Symptoms Hyperactive precordium Normal or accentuated 1st hrt sound Wide, fixed splitting of S2 Pulmonary systolic ejection murmur w/thrill Holosystolic murmur @ apex w/radiation to axilla Mid-diastolic rumbling murmur @ LSB Marked cardiac enlargement on CX-Ray Atrioventricular Septal Defect Treatment • Surgery is always required. • Treat congestive symptoms. • Pulmonary banding maybe required in premature infants or infants < 5 kg. • Correction is done during infancy to avoid irreversible pulmonary vascular disease. • Mortality low w/incomplete 1-2% & as high as 5% with complete AVSD. Patent Ductus Arteriosus • PDA – Persistence of the normal fetal vessel that joins the PA to the Aorta. • Normally closes in the 1st wk of life. • Accounts for 10% of all CHD, seen in 10% of other congenital hrt lesions and can often play a critical role in some lesions. • Female : Male ratio of 2:1 • Often associated w/ coarctation & VSD. Patent Ductus Arteriosus • Question: What TORCH infection is PDA associated with? • Answer: Rubella Patent Ductus Arteriosus Hemodynamics • As a result of higher aortic pressure, blood shunts L to R through the ductus from Aorta to PA. • Extent of the shunt depends on size of the ductus & PVR:SVR. • Small PDA, pressures in PA, RV, RA are normal. Patent Ductus Arteriosus Hemodynamics • Large PDA, PA pressures are equal to systemic pressures. In extreme cases 70% of CO is shunted through the ductus to pulmonary circulation. • Leads to increased pulmonary vascular disease. Patent Ductus Arteriosus • • • • • • • Clinical Signs & Symptoms Small PDA’s are usually asymptomatic Large PDA’s can result in symptoms of CHF, growth restriction, FTT. Bounding arterial pulses Widened pulse pressure Enlarged heart, prominent apical impulse Classic continuous machinary systolic murmur Mid-diastolic murmur at the apex Patent Ductus Arteriosus • • • • • Treatment Indomethacin, inhibitor of prostaglandin synthesis can be used in premature infants. PDA requires surgical or catheter closure. Closure is required treatment heart failure & to prevent pulmonary vascular disease. Usually done by ligation & division or intra vascular coil. Mortality is < 1% Obstructive Heart Lesions • Pulmonary Stenosis • Aortic Stenosis • Coarctation of the Aorta Pulmonary Stenosis • Pulmonary Stenosis is obstruction in the region of either the pulmonary valve or the subpulmonary ventricular outflow tract. • Accounts for 7-10% of all CHD. • Most cases are isolated lesions • Maybe biscuspid or fusion of 2 or more leaflets. • Can present w/or w/o an intact ventricular septum. Pulmonary Stenosis • Question: What syndrome is PS associated with? • Answer: Noonan’s Syndrome, secondary to valve dysplasia. Pulmonary Stenosis • • • • • Hemodynamics RV pressure hypertrophy RV failure. RV pressures maybe > systemic pressure. Post-stenotic dilation of main PA. W/intact septum & severe stenosis R-L shunt through PFO cyanosis. Cyanosis is indicative of Critical PS. Pulmonary Stenosis • • • • • • • Clinical Signs & Symptoms Depends on the severity of obstruction. Asymptomatic w/ mild PS < 30mmHg. Mod-severe: 30-60mmHg, > 60mmHg Prominent jugular a-wave, RV lift Split 2nd hrt sound w/ a delay Ejection click, followed by systolic murmur. Heart failure & cyanosis seen in severe cases. Pulmonary Stenosis Treatment • Mild PS no intervention required, close follow-up. • Mod-severe – require relieve of stenosis. • Balloon valvuloplasty, treatment of choice. • Surgical valvotomy is also a consideration. Aortic Stenosis • Aortic Stenosis is an obstruction to the outflow from the left ventricle at or near the aortic valve that causes a systolic pressure gradient of more than 10mmHg. Accounts for 7% of CHD. • 3 Types • Valvular – Most common. • Subvalvular(subaortic) – involves the left outflow tract. • Supravalvular – involves the ascending aorta is the least common. Aortic Stenosis • Question: Which syndrome is supravalvular stenosis found in? • Answer: Williams Syndrome Aortic Stenosis • • • • • Hemodynamics Pressure hypertrophy of the LV and LA with obstruction to flow from the LV. Mild AS 0-25mmHG Moderate AS 25-50mmHg Severe AS 50-75mmHg Critical AS > 75mmHg Aortic Stenosis Clinical Signs & Symptoms • Mild AS may present with exercise intolerance, easy fatigabiltity, but usually asymptomatic. • Moderate AS – Chest pain, dypsnea on exertion, dizziness & syncope. • Severe AS – Weak pulses, left sided heart failure, Sudden Death. Aortic Stenosis Clinical Signs & Symptoms • LV thrust at the Apex. • Systolic thrill @ rt base/suprasternal notch. • Ejection click, III-IV/VI systolic murmur @ RSB/LSB w/ radiation to the carotids. Aortic Stenosis Treatment • Because surgery does not offer a cure it is reserved for patients with symptoms and a resting gradient of 60-80mmHg. • For subaortic stenosis it is reserved for gradients of 40-50mmHg because of it’s rapidly progressive nature. • Balloon valvuloplasty is the standard of treatment. Aortic Stenosis Treatment • Aortic insufficiency & re-stenosis is likely after surgery and may require valve replacement. • Activity should not be restricted in Mild AS. • Mod-severe AS, no competitive sports. Coarctation of the Aorta • Coarctation- is narrowing of the aorta at varying points anywhere from the transverse arch to the iliac bifurcation. • 98% of coarctations are juxtaductal • Male: Female ratio 3:1. • Accounts for 7 % of all CHD. Coarctation of the Aorta • Question: What other heart anomaly is coarctation associated with? • Answer: Bicuspid aortic valve, seen in > 70% of cases. Coarctation of the Aorta • Question: What genetic syndrome is coarctation seen in? • Answer: Turner’s Syndrome Coarctation of the Aorta Hemodynamics • Obstruction of left ventricular outflow pressure hypertrophy of the LV. Coarctation of the Aorta Clinical Signs & Symptoms • Classic signs of coarctation are diminution or absence of femoral pulses. • Higher BP in the upper extremities as compared to the lower extremities. • 90% have systolic hypertension of the upper extremities. • Pulse discrepancy between rt & lt arms. Coarctation of the Aorta Clinical Signs & Symptoms • With severe coarc. LE hypoperfusion, acidosis, HF and shock. • Differential cyanosis if ductus is still open • II/VI systolic ejection murmur @ LSB. • Cardiomegaly, rib notching on X-ray. Coarctation of the Aorta Coarctation of the Aorta Treatment • With severe coarctation maintaining the ductus with prostaglandin E is essential. • Surgical intervention, to prevent LV dysfunction. • Angioplasty is used by some centers. • Re-coarctation can occur, balloon angioplasty is the procedure of choice. Questions Examination of a 3-hr old infant reveals dysmorphic features and cyanosis. Both the occiput and facial profile are flat, and the fontanelle is abnormally enlarged. The space between the great and second toe is wide, and there is a palmar crease extending across the left palm. Room air oximetry reveals a saturation 70%. Questions Of the following, the MOST likely lesion to be found on echocardiography would be A. Atrioventricular septal defect B. Coarctation of the aorta C. Hypoplastic left heart D. Total anomalous pulmonary venous return E. Truncus arteriosus Questions After a few days of poor feeding and tachypnea, a 3 week old presents with hypotension, poor central and peripheral pulses, and severe metabolic acidosis. A gallop is audible, and the heart appears enlarged on chest radiography. Hepatomegaly is marked. Questions Of the following, the BEST intervention to produce a sustained improvement is A. 100% Oxygen administration B. Dopamine infusion C. Gamma globulin infusion D. Phenylephrine infusion E. Prostaglandin E infusion Questions A term infant is born with a large ventricular septal defect. At what age is the infant most likely to first demonstrate clinical findings of CHF A. 2 days B. 2 weeks C. 2 months D. 6 months E. 12 months