Location of the heart
advertisement

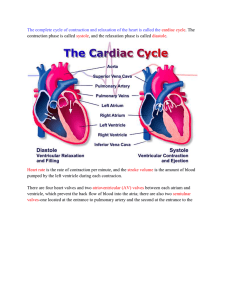
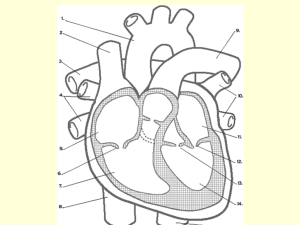
• Heart is about the size of your fist • Is a four chambered pump • Pumps over 1 million gallons per year • Over 60,000 miles of blood vessels Heart Location – Transverse Section Anterior surface of heart • Heart is located in the mediastinum – area from the sternum to the vertebral column and between the lungs Heart Orientation • Apex - directed downwards and to the left • Base - directed upward and to the right • Anterior surface - deep to the sternum and ribs • Inferior surface - rests on the diaphragm • Right border - faces right lung • Left border - faces left lung Heart Enclosed in Pericardium • Fibrous pericardium – dense irregular CT – protects and anchors the heart, prevents overstretching • Serous pericardium – thin delicate membrane – Made of two layers: • parietal layer-outer layer • visceral layer (epicardium) • pericardial cavity with pericardial fluid between the two layers. Layers of Heart Wall • Epicardium – visceral layer of serous pericardium • Myocardium – cardiac muscle layer is the bulk of the heart • Endocardium – chamber lining & valves Chambers of the Heart • Four chambers – Two upper atria (singular is atrium) • Thin-walled • Receive blood returning to heart and send it to ventricles – Two lower ventricles • • • • Thick-walled Pump blood from heart right ventricle supplies blood to the lungs (little flow resistance) left ventricle wall is the thickest to supply systemic circulation Heart Chambers and Vessels Superior Vena Cava----Right Pulmonary Artery----- ------Aorta -----------Left Pulmonary Artery ---------------Pulmonary Trunk -------Left Pulmonary Vein (2) Right Pulmonary Vein (2)--- --------Left Atrium Right Atrium-------Right Ventricle------------------- Inferior Vena Cava------- -------Left Ventricle Heart Interior and Valves -----------Left Atrium Pulmonary Semilunar Valve------- ---------Aortic Semilunar Valve -----Bicuspid (mitral) Valve Right Atrium------------Tricuspid Valve----------------- Right Ventricle------------------- --------Left Ventricle Heart Valves • AV valves close with ventricular contraction – blood pressure forces cusps to close, preventing blood from flowing from ventricle back into atria. • SL valves close with ventricular relaxation – prevent blood from returning to ventricles from pulmonary artery and aorta. Blood fills valve cusps, tightly closing the SL valves Bicuspid (mitral) Valve •When left ventricle contracts, the two cusps (leaflets) snap shut. What causes them to close? Flow of Blood Through the Heart Vena Cavae Right Ventricle Pulmonary Valve Pulmonary Veins Right Atrium Tricuspid Valve Pulmonary Trunk and Arteries Lungs Left Atrium Bicuspid Valve Aortic Valve to Aorta Left Ventricle Cardiac Muscle Tissue • Histology •Striated •Branched •Intercalated discs •Involuntary •Aerobic Two types of cardiac muscles • CONTRACTILE CARDIAC MUSCLE: - MAKE ALL THE MYOCARDIUM - CAUSE CONTRACTION OF THE HEART CHAMBERS. • AUTORYTHMIC CARDIAC MUSCLE: -SELF-EXCITABLE LIKE NERVES. -FORM THE CONDUCTION SYSTEM THROUGH THE HEART MUSCLES. -FORM THE HEART PACEMAKER. Electrical Events of the Heart • Conducting system •Consists of _______________ autorhythmic cells that initiate action potential and then carry it through heart •Components of Conducting System •Sinoatrial (SA) Node - Pacemaker •In right atrium near entrance of superior vena cava •Automatically depolarizes and starts each heartbeat •Atrioventricular (AV) Node •Receives electrical signal from SA node, delays it then sends it to ventricles •AV Bundle (of His) receives signal from AV node •Right and left Bundle Branches •Formed by division of AV bundle •Send signal to each ventricle •Purkinje fibers spread signal throughout ventricles Electrocardiogram (ECG or EKG) Tracing of Heart’s electrical activity •P wave – atrial depolarization •QRS complex – ventricular depolarization •T wave – repolarization of Ventricles •P-Q interval – time for signal to travel from SA node to AV bundle •Q-T interval – time for ventricular depolarization and repolarization Autorhythmicity • Heartbeat intrinsic because it has its own pacemaker that starts each beat •____________ The SA node is the pacemaker that starts each heartbeat by spontaneously depolarizing at the heart rate •Resulting action potential (signal) spreads from conducting system to contractile cells Cardiac Cycle – How the Heart Beats •Conducting system controls sequence of heartbeat •_________ SA node depolarizes and stimulates contraction of atria •_________ AV node receives signal, delays it, then passes it through rest of conducting system to ventricles •Assures that atria contract before ventricles •This sequence of heartbeat called normal _____________ sinus rhythm •Contraction phase of heartbeat called _______ systole •Relaxation phase of heartbeat called _________ diastole •Alternating contractions and relaxations allow heart to pump blood then refill •Diagram on next page shows steps of cardiac cycle – events of one heartbeat Animation of Heartbeat Cardiac Cycle – Events of one Heartbeat 1. Atrial and Ventricular diastole 2. Atrial systole 3. Ventricular systole •AV valves open •Ventricles fill to 70% •Completion of ventricular filling 4. Atrial and Ventricular diastole •Ventricles contract •AV valves close – lubb (S1) sound •SL valves open 50-60% of blood ejected •Ventricles relax – return to diastole •SL valves close – dupp (S2) sound Cardiac Output •Definition: Amount of blood ejected by heart in one minute •Factors affecting cardiac output •Stroke volume: Milliliters of blood ejected by ventricle per beat •Heart rate: Number of heartbeats per minute •Formula: Cardiac output = Stroke volume x Heart rate Factors Affecting Stroke Volume •Preload: •End diastolic volume (EDV) or amount of blood in ventricle before ejection •More in, more out •Contractility: •Strength of contraction •Affected by many factors including the nervous system and various chemicals Factors Affecting Stroke Volume Continued •Afterload •Tension or pressure ventricle must exert to open semilunar valve and eject blood •Determined by resting (diastolic) pressure in pulmonary trunk or aorta •Right ventricle must produce enough pressure to open pulmonary semilunar valve •Left ventricle must produce enough pressure to open the aortic valve •Does high blood pressure increase or decrease the afterload? •What long term effect might high afterload have on the heart? Factors Affecting Heart Rate •Neural Control of Heart Rate •Cardiac centers in __________________of Medulla oblongata brain •Cardiac acceleratory center •Impulses through cardiac nerves of _________________________ sympathetic division of ANS •Neurotransmitter ______________ norepinephrine accelerates heart rate •Cardiac inhibitory center (CIC) •Impulses through vagus nerve (CNX) of the ________________ parasympathetic ________________ division of ANS •Neurotransmitter _______________ acetylcholine slows heart rate •At rest, constant input by parasympathetic keeps heart beating at resting rate – called _____________ vagal tone Neural Control Diagram Accelerator Norepinephrine speeds-up heart rate Brake Acetylcholine slows the heart rate Factors Affecting Heart Rate Continued •Blood chemistry •Adrenaline (epinephrine) ___________________________________ increases rate and strength of heartbeat •High levels of thyroid hormone will speed-up heart •Changes in electrolytes (ion concentrations), especially potassium and calcium •Body temperature •What happens when you have a fever? •Changes in blood pressure •Can slow-down or speed-up heart •Will be discussed in next chapter Clinical Terms • Tachycardia: A heart rate above 100/min. • Bradycardia: A heart rate below 60/min • Asystole: Cardiac standstill, no contraction • coronary artery disease (CAD): Narrowing of the coronary arteries. • Ischemia: Decreased blood flow. • Atherosclerosis: Hardening of arteries. • Angina pectoris: Chest pain. • Myocardial infarction: Loss of living heart muscle mass. • Arteriosclerosis: Thickening of the arterial walls. • Arrhythmias: Irregularity of heart rhythm. • Heart failure: Reduced ability of the heart to pump blood. • Pericarditis: Inflammation of the pericardium.